ALSO IN THIS ISSUE
ANDREA COLTON, MD, BREAST SURGICAL ONCOLOGIST
JESSICA CROLEY, MD, CHI-SAINT JOSEPH HEALTH CANCER CARE CENTER
MICHELLE PALAZZO, MD, KLEINERT KUTZ
BREAST RECONSTRUCTION PLASTIC SURGEON

ERICA TAKIMOTO, DO, BAPTIST HEALTH GYNECOLOGIC ONCOLOGIST
MARGARITA TERRASSA, MD, OB-GYN, WOMEN FIRST OF LOUISVILLE
Making the Impossible Possible Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer patients have the best chance for a fully functioning life after treatment

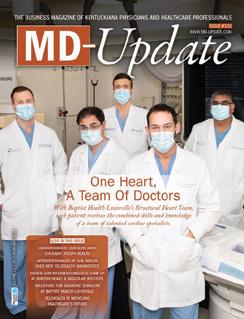
ISSUE #136 WWW.MD-UPDATE.COM THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS VOLUME 11 • #5 • O CTO b E r 2021

ISSUE #137 (December ’21) IT’S ALL IN YOUR HEAD
Neurology, Neuroscience, Ophthalmology, Pain Medicine, ENT, Psychiatry, Mental Health
ISSUE #138 (February) HEART, STROKE & LUNG HEALTH

Cardiology, Cardiothoracic, Cardiovascular, Pulmonology, Sleep Medicine, Vascular Medicine, Bariatric Surgery, Wound Care
ISSUE #139 (April) INTERNAL SYSTEMS
Endocrinology, Gastroenterology, Geriatrics, Internal Medicine, Integrative & Regenerative Medicine, Infectious Diseases, Lifestyle Medicine, Nephrology, Urology
ISSUE #140 (June) WOMEN’S & CHILDREN’S HEALTH
OB/GYN, Women’s Cardiology, Oncology, Urology, Pediatrics, Radiology, Travel Medicine



ISSUE # 141 (September) MUSCULOSKELETAL HEALTH





Orthopedics, Sports Medicine, Physical Medicine & Rehabilitation, PT/OT

















ISSUE #142 (October) CANCER CARE
Oncology, Plastic Surgery, Hematology, Radiation, Radiology


































ISSUE 143 (December) IT’S ALL IN YOUR HEAD
Neurology, Neuroscience, Ophthalmology, Pain Medicine, ENT, Psychiatry, Mental Health













Editorial topics and dates are subject to change

ISSUE #136 WWW.MD-UPDATE.COM 11 #5 O CTO r 2021 ALSO IN THIS ISSUE ANDREA COLTON, MD, BREAST SURGICAL ONCOLOGIST JESSICA CROLEY, MD, CHI-SAINT JOSEPH HEALTH CANCER CARE CENTER MATTHEW FORSTHOEFEL, MD, RADIATION ONCOLOGIST Making the Impossible Possible Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer patients have the best chance for a fully functioning life after treatment WWW.MD-UPDATE.COM VOLUME 11 #5 O CTO r 2021 ALSO IN THIS ISSUE ANDREA COLTON, MD, BREAST SURGICAL ONCOLOGIST JESSICA CROLEY, MD, CHI-SAINT JOSEPH HEALTH CANCER CARE CENTER MATTHEW FORSTHOEFEL, MD, RADIATION ONCOLOGIST MICHELLE PALAZZO, MD, KLEINERT KUTZ BREAST RECONSTRUCTION PLASTIC SURGEON ERICA TAKIMOTO, DO, BAPTIST HEALTH GYNECOLOGIC ONCOLOGIST MARGARITA TERRASSA, MD, OB-GYN, WOMEN FIRST OF LOUISVILLE Making Impossible Possible Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck patients have the best for a fully functioning life after treatment ISSUE #136 WWW.MD-UPDATE.COM VOLUME 11 #5 O CTO r 2021 ALSO IN THIS ISSUE ANDREA COLTON, MD, BREAST SURGICAL ONCOLOGIST JESSICA CROLEY, MD, CHI-SAINT JOSEPH HEALTH CANCER CARE CENTER MATTHEW FORSTHOEFEL, MD, RADIATION ONCOLOGIST MICHELLE PALAZZO, MD, KLEINERT KUTZ BREAST RECONSTRUCTION PLASTIC SURGEON ERICA TAKIMOTO, DO, BAPTIST HEALTH GYNECOLOGIC ONCOLOGIST MARGARITA TERRASSA, MD, OB-GYN, WOMEN FIRST OF LOUISVILLE Making the Impossible Possible Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer patients have the best chance for a fully functioning life after treatment ISSUE #136 WWW.MD-UPDATE.COM ALSO IN THIS ISSUE ANDREA COLTON, MD, BREAST SURGICAL ONCOLOGIST JESSICA CROLEY, MD, CHI-SAINT JOSEPH HEALTH CANCER CARE CENTER MATTHEW FORSTHOEFEL, MD, RADIATION ONCOLOGIST MICHELLE PALAZZO, MD, KLEINERT KUTZ BREAST RECONSTRUCTION PLASTIC SURGEON ERICA TAKIMOTO, DO, BAPTIST HEALTH GYNECOLOGIC ONCOLOGIST MARGARITA TERRASSA, MD, OB-GYN, WOMEN FIRST OF LOUISVILLE Making the Impossible Possible Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer patients have the best chance for a fully functioning life after treatment ISSUE #136 WWW.MD-UPDATE.COM VOLUME 11 #5 CTO b 2021 ALSO IN THIS ISSUE ANDREA COLTON, MD, BREAST SURGICAL ONCOLOGIST JESSICA CROLEY, MD, CHI-SAINT JOSEPH HEALTH CANCER CARE CENTER MATTHEW FORSTHOEFEL, MD, RADIATION ONCOLOGIST MICHELLE PALAZZO, MD, KLEINERT KUTZ BREAST RECONSTRUCTION PLASTIC SURGEON ERICA TAKIMOTO, DO, BAPTIST HEALTH GYNECOLOGIC ONCOLOGIST MARGARITA TERRASSA, MD, OB-GYN, WOMEN FIRST OF LOUISVILLE Making the Impossible Possible Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer patients have the best chance for a fully functioning life after treatment THE BUSINESS MAGAZINE OF KENTUCKIANA PHYSICIANS AND HEALTHCARE PROFESSIONALS
Gil Dunn, Publisher • GDUNN@MD-UPDATE.COM • 859.309.0720 (direct) • 859.608.8454 (cell) Send press releases to gdunn@md-update.com To participate, please contact
2022 Editorial Calendar
Welcome to the Cancer Care issue of MD-Update
It’s stated several times in this issue, but I want to bring your attention to the 50th anniversary of America’s “War on Cancer.”
In January 1971, President Richard Nixon, in his State of the Union address, announced his intention to ask for a Congressional appropriation of $100 million to find a cure for cancer.
In October of 1971, the U.S. Army Fort Detrick in Maryland, a biological warfare facility, was converted into a cancer research center. In December of the same year, Nixon signed the National Cancer Act into law, giving the National Cancer Institute special, independent budgetary status within the National Institute of Health.
The goal was to finding a cure for cancer. Are we there yet? Not quite, but getting closer.
Meet the Doctors
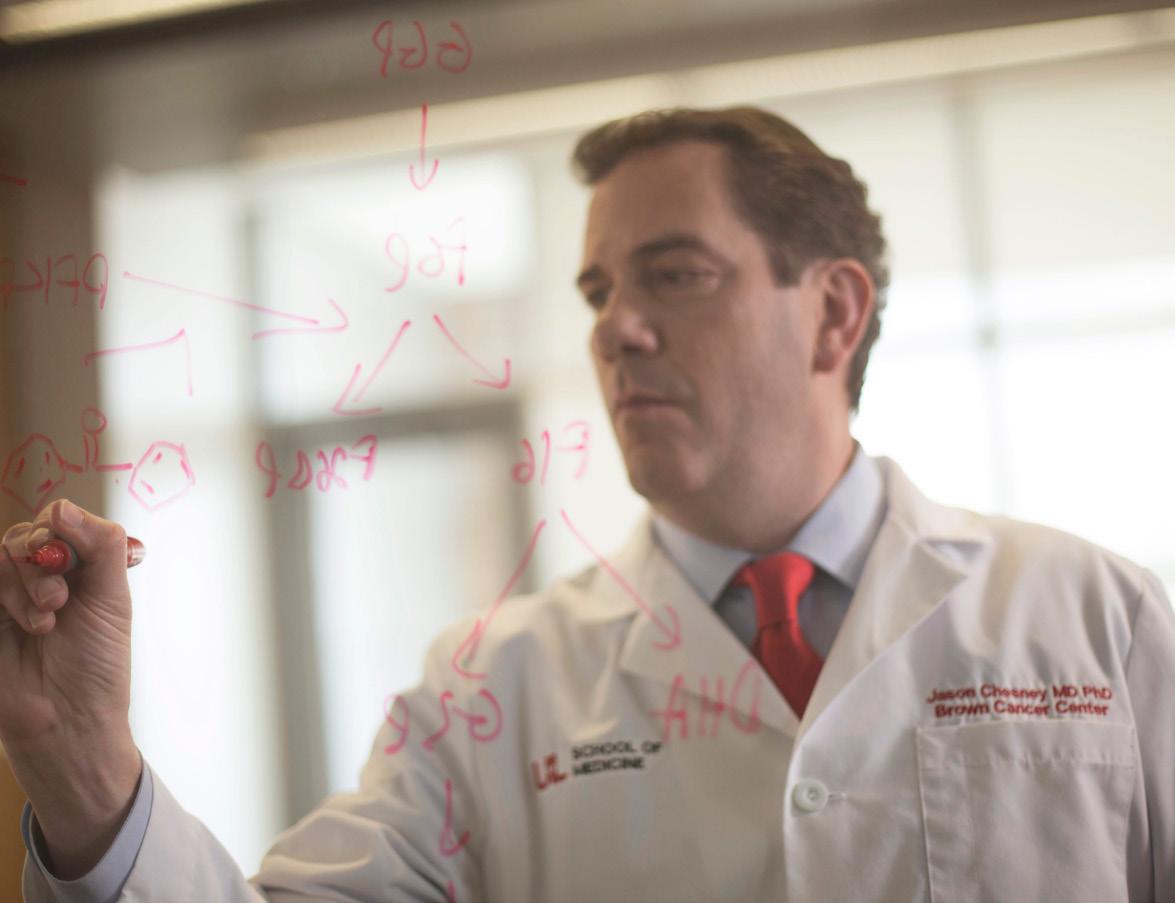
Our cover story in this issue introduces Dr. Rebecca Redman, associate professor at the UofL School of Medicine and the deputy director of clinical research for the UofL Health-Brown Cancer Center team who continue the effort to find a cure for cancer. She oversees phase 1, 2 and 3 clinical trials at Brown Cancer Center, supporting her research colleagues. Jason Chesney, MD, PhD, the director and chief administrator at Brown Cancer Center, has worked for years on advancing immunotherapy for melanoma and lung cancer.
Is it possible that a cure for cancer could come from their work? We hope so.
Screening, surgery, early detection, and prevention for breast and gynecologic cancer is the work of our Special Section doctors Jessica Croley, MD, Michelle Palazzo, MD, Margarita Terrassa, MD, Andrea Colton, MD, and Erica Takimoto, DO. I invite you to read their stories, discover their passions, and meet some of the women who are soldiers in the war on cancer. Guest columnists Whitney Jones, MD, Shana Moore, PhD, Teri Wood, PhD, Caisey RamseyJohnson, and Connie White, MD, take a deep dive into multi-cancer early detection and new guidelines for colorectal screening.
December and 2022
The December issue of MD-Update is on track with an exploration into advanced neuroscience care in Kentuckiana and new treatment modalities for chronic pain. I hope you’ll join us. The 2022 MD-Update editorial calendar is on the preceding page. If you’re a doctor, I invite you to look for your specialty and contact me. I’m sure you have a story to tell and some insight to share.
MD-UPDATE MD-Update.com
Volume 11, Number 5
ISSUE #136
PUBLISHER
Gil Dunn gdunn@md-update.com
GRAPHIC DESIGN
Laura Doolittle, Provations Group
COPY EDITOR
Amanda Debord
CONTRIBUTORS:
Jan Anderson, PSYD, LPCC Caisey ramsey-Johnson
Whitney Jones, MD
Lance Mann
Shana Moore, PhD
Scott Neal, CPA, CFP

Connie White, MD
Terri Wood, PhD
CONTACT US:
ADVERTISING AND INTEGRATED PHYSICIAN MARKETING: Gil Dunn gdunn@md-update.com
Mentelle Media, LLC

38 Mentelle Park Lexington KY 40502 (859) 309-0720 phone and fax
Standard class mail paid in Lebanon Junction, Ky. Postmaster: Please send notices on Form 3579 to 38 Mentelle Park Lexington KY 40502
MD-Update is peer reviewed for accuracy. However, we cannot warrant the facts supplied nor be held responsible for the opinions expressed in our published materials.
Copyright 2021 Mentelle Media, LLC. All rights reserved. No part of this publication may be reproduced, stored, or transmitted in any form or by any means-electronic, photocopying, recording or otherwise-without the prior written permission of the publisher.
Please contact Mentelle Media for rates to: purchase hardcopies of our articles to distribute to your colleagues or customers: to purchase digital reprints of our articles to host on your company or team websites and/or newsletter. Thank you.
Individual copies of MD-Update are available for $9.95.
2 MD-UPDATE
SEND YOUR LETTERS TO THE EDITOR TO: Gil Dunn, Publisher gdunn@md-update.com, or 859.309.0720 phone and fax
Editor/Publisher MD-Update LETTEr FrOM THE EDITOr/PUbLISHEr
Until December, all the best, Gil Dunn






ISSUE #136 3 ONCOLOGY • SUrGICAL ONCOLOGY • PLASTIC SUrGErY • GYNECOLOGIC ONCOLOGY • rADIATION ONCOLOGY • Ob-GYN ISSUE #136 18 ONCOLOGY 20 PLASTIC SURGERY/ BREAST RECONSTRUCTION 23 OB-GYNECOLOGY 26 BREAST ONCOLOGICAL SURGERY 28 GYNECOLOGIC SURGERY CONTENTS SPECIAL SECTIONS 4 HEADLINES 5 ACCOUNTING 6 FINANCE 8 OP/ED 14 COVER STORY SPECIAL SECTION: 18 ONCOLOGY 20 PLASTIC SURGERY 23 OB-GYNECOLOGY 26 BREAST SURGICAL ONCOLOGY 28 GYNECOLOGIC SURGERY 30 MENTAL WELLNESS 32 NEWS 14
Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer patients have the best chance for a fully functioning life after treatment.
Making the Impossible Possible
First-in-world Heart Implant at UofL Health – Jewish Hospital


LOUISVILLE The cardiothoracic surgical team at UofL Health – Jewish Hospital performed the world’s first Aeson® bioprosthetic total artificial heart implantation in a female patient on September 14, 2021. The investigational device, currently intended as a bridge to a heart organ transplant, is part of an early feasibility study (EFS) sponsored by CARMAT, a French medical device company, in partnership with the University of Louisville and the UofL Health – Trager Transplant Center. Jewish Hospital is one of four programs in the nation approved to perform this clinical trial procedure.
The surgery was led by cardiothoracic surgeons Mark Slaughter, MD, and Siddharth Pahwa, MD, both of UofL Health – UofL Physicians and the UofL School of Medicine. The same team completed the nation’s second implantation last month in a male patient also at Jewish Hospital.
“For over half of the world’s population, completion of this procedure by the Jewish Hospital team brings new hope for extended life,” says Slaughter, UofL Health surgical director of heart transplant and professor and chair of the Department of Cardiovascular and Thoracic Surgery in the UofL School of Medicine. “Size limitations can make it harder to implant artificial hearts in women, but the Aeson artificial heart is compact enough to fit inside the smaller chest cavities more frequently found in women, which gives hope
to a wider variety of men and women waiting for a heart transplant and increases the chances for success.”
More than 3,500 individuals are awaiting a heart transplant in the U.S. and 900 of them are women. There are few treatment options for patients with biventricular heart disease, when both the left and right sides of the heart are not pumping blood adequately. The Aeson device is designed to solve the limitations of current left-ventricular assist devices (LVAD), which pump blood into just one chamber, by pumping blood in both heart chambers. It is fully implanted as a heart replacement and powered by a portable external power supply.
During this procedure, the Aeson total artificial heart was implanted into a 57-year-old Kentucky woman with severe biventricular heart failure during an eight-hour surgery. The recipient had undergone cardiac surgery years before but was referred to the Advanced Heart Failure Therapies Program at Jewish Hospital earlier this year with end-stage heart failure. The patient is recovering well in the cardiovascular intensive care unit (CVICU).
“The varying pumping ability of the Aeson device increases its viability among more patients,” says Pahwa, UofL Physicians cardiothoracic surgeon and assistant professor in the UofL Department of Cardiovascular and Thoracic Surgery. “While other devices
are set at a fixed rate or create a continuous flow, CARMAT has developed the Aeson to automatically adjust the flow, creating an improved performance to meet the body’s changing blood flow needs.”
“This world-first artificial heart implant into a female patient is another demonstration of UofL Health’s commitment to both providing the world-class care of today and developing the world-class standards of tomorrow,” says John Walsh, CAO of Jewish Hospital. “We celebrate this first as a milestone and recognize the hard work of Drs. Slaughter and Pahwa and the entire team. The true impact of their work will be measured in the dozens, hundreds, and thousands of lives improved in the years to come.”
The patient who received the nation’s second Aeson implant, on Aug. 20, 2021, continues to improve at Jewish Hospital.
4 MD-UPDATE
Woman receives novel type of artificial heart –third implantation overall in the U.S.
HeAdLines
An Aeson bioprosthetic total artificial heart, made by CARMAT, is being prepared for implantation at UofL Health – Jewish Hospital.
PHOTOs BY TOM ROUnd, UOFL HeALTH
Update on Provider Relief Funds and their Audit Requirements

 BY LANCE MANN, ASSURANCE DIRECTOR
BY LANCE MANN, ASSURANCE DIRECTOR
The Health Resources and Services Administration (HRSA) announced two important updates last week related to Provider Relief Funds (PRF) and reporting requirements:
1. An additional $25.5 billion of PRF distributions
• $8.5 billion for providers that serve rural patients under the Medicare, Medicaid or Children’s Health Insurance Program (CHIP), and

• $17 billion “for a broad range of providers who can document revenue loss and expenses associated with the pandemic.”
2. A 60-day grace period for meeting PRF reporting requirements
• Implemented in order to help providers comply with PRF reporting requirements
• Although HHS will not initiate collection activities or enforcement actions during the grace period, providers will still be out of compliance if reporting is not submitted by September 30, 2021
The new guidance released a few weeks ago clarifies that entities with fiscal years ending June 30, 2021 will be the first entities
required to include Provider Relief Funds on their Schedule of Expenditure of Federal Awards (SEFA) and thus, be subject to audit of these funds. Entities with other fiscal year ends will include some or all of their Provider Relief Funds on their next fiscal year end.
For example, if you are a December 31, 2021 year end, then you will include all funds from Periods 1 and 2 (described above) in your SEFA and your December 31, 2022 SEFA will include periods 3 and 4. Below are the specific FAQs that were released by HHS.
When should Provider Relief Fund expenditures and/or lost revenue be reported on a nonfederal entity’s Schedule of Expenditures of Federal Awards (SEFA)?
Non-federal entities will include Provider Relief Fund expenditures and/or lost revenues on their SEFAs for fiscal year ends (FYEs) ending on or after June 30, 2021. Please refer to the 2021 OMB Compliance Supplement for additional information.
How will a non-federal entity determine the amount of expenditures and/or lost revenues to report on its SEFA for FYEs ending on or after June 30, 2021?
A non-federal entity’s SEFA reporting is
linked to its report submissions to the Provider Relief Fund Reporting Portal. Therefore, the timing of SEFA reporting of Provider Relief Fund payments will be as follows:
For a FYE of June 30, 2021, and through FYEs of December 30, 2021, recipients are to report on the SEFA the total expenditures and/or lost revenues from the Period 1 report submission to the Provider Relief Fund Reporting Portal.
For a FYE of December 31, 2021, and through FYEs of June 29, 2022, recipients are to report on the SEFA, the total expenditures and/or lost revenues from both the Period 1 and Period 2 report submissions to the Reporting Portal.
For FYEs on or after June 30, 2022, SEFA reporting guidance related to Period 3 and Period 4 will be provided at a later date.
As discussed in the FAQs above, we will need to wait for the FY2021 OMB Compliance Supplement to be released later this summer for more information.
If you have questions about these updates or requirements, please reach out to us for more information at lmann@deandorton.com 502.566.1005 or visit deandorton.com.
ISSUE #136 5
deandortonhealthcaresolutions.com Practice management and advisory services Medical billing and credentialing Revenue cycle management Compliance and risk management Interim practice management Accounting and financial outsourcing Human resources Technology
ACCOUNTINg
Empowering physicians to focus solely on the demands of their clinical practice
End-of-Year Planning Becomes Urgent
BY SCOTT NEAL
Last month I advised to be on your financial toes and to pay attention to what is happening around you as well as to the changes that have occurred in your own family this year. We have a checklist for 2021 end-of-year planning that I will be happy to send you. Simply ask. My email is at the bottom of this article.

Keeping up with what is going on in Congress is an occupational hazard for a forward-looking financial planner. I have never been a big fan of speculating or implementing strategy on laws that have only been proposed, but not yet enacted, by Congress. Many bills get changed just before passage, rendering moot some of the best plans constructed while Congress was still deliberating. I usually don’t expend the time and energy on such planning.
This year is different. If the House Ways and Means version is passed by the full Congress very late in the year and becomes law on January 1, 2022, there will be no time to plan for and implement tax saving strategies. Unfortunately, we must plan now. Some will dismiss the new law because they think it only applies to those with very large retirement accounts. Don’t fall for that. You certainly will be impacted if your retirement accounts are over $10 million and your income is over $400,000, but you may also be affected if you 1) have basis in your IRA (i.e. those that have made non-deductible contributions in the past), 2) are converting funds to a Roth, 3) are doing back door Roth contributions, 4) have made accredited investments
in IRAs, or 5) own over 10% in an entity owned in your retirement plan.

If Congress is to get its $3.5 trillion to spend, they must find a way to pay for it. Raising taxes, particularly on those with income over $400,000, will be in the cards. (Remember President Biden’s campaign promise that he would not raise taxes on anyone with income under $400,000.) If your income is above that threshold, you should certainly project 2021 and 2022 taxes now and determine your tax saving strategy.
Earning less money is not a tax saving strategy I recommend. However, there is going to be a lot of emphasis placed on developing plans to reduce taxable income to below the $400,000 ($450,000 for married filing jointly) thresh-
6 MD-UPDATE
From
YOU CARE FOR EVERYONE♦ WE TAKE CARE OF YOU♦ Sturgill, Turner, Barker & Moloney, PLLC ♦ Lexington, Ky. ♦ 859.255.8581 ♦ STURGILLTURNER.LAW FiNANCiAL
the business of health care to compliance to litigation defense, Sturgill Turner’s experienced health care attorneys provide comprehensive legal services to health care providers, hospitals and managed care organizations across the Commonwealth. Put our experience to work for you.
old. One of the most popular ways of doing that is through charitable contributions, either outright contributions (which are still 100% deductible this year) or via Qualified Charitable Distributions (QCD) from a retirement plan. Tax-free bonds could become much more popular to keep taxable income below the threshold.
Roth Conversions
A popular strategy for future tax savings has been Roth conversions. Recall that Roth contributions are taxable only in certain cases. Before 2010, those with income over $100,000 were prohibited from making Roth conversions. Currently, higher income limitations remain for Roth contributions, but many people who have higher incomes have gotten around that rule by doing what has been called the “backdoor” Roth conversion. To refresh your memory, a “backdoor” conversion happens when you make a non-deductible contribution to a Traditional IRA and then soon thereafter convert it to a Roth and only pay taxes on the growth. Under the new rules, starting in 2022 the “Backdoor Roth IRA” and “Mega-Backdoor Roth IRA” will be prohibited.
New RMD Rules
The bill introduces new Required Minimum Distributions (RMD) for MEGA retirement accounts. If your total retirement account balances (including all IRAs and employer sponsored plans) exceed $10 million at year end, you will be hit with a new RMD. The RMD is 50% of the amount over $10 million or 100% of the amount over $20 million in a Roth. You read that correctly. If your retirement account balances are $12 million on December 31, 2021, you will be required to take a taxable distribution of $1 million in 2022.
However, the RMD does not apply if your income is below the $400,000 ($450,000) thresholds. The strategy to deal with this will be to reduce your taxable income through charitable giving, oil & gas investments, life insurance, or large defined benefit plan contributions. Incidentally, the $10 million threshold applies separately to spouses, making filing separately a consideration for families with a non-working spouse who happens to have a MEGA IRA.
The Five-year Clock
Typically, most advisors recommend that distributions from Roth accounts will be the last money you take out of your retirement accounts. Current law states that if you take distributions within 5 years of starting a Roth, you may suffer adverse tax consequences depending on your age. If you do not currently have a Roth IRA, and all your retirement accounts are in a Traditional IRA and/or a retirement plan where you work, we believe you should start a Roth IRA, and do it NOW. Do it even with a small amount of money, such as $1,000. The goal is to start the 5-year clock running to avoid taxes and potential penalties on a future distribution should you need the funds later.
If you take nothing else from this article, just know that the legislation working its way through Congress at the time of my writing will have far reaching impact that can affect us all for years to come. Plan now for its consequences should it come to pass.
ISSUE #136 7
FiNANCiAL
Scott Neal is the president of D. Scott Neal, Inc., a feeonly financial planning and investment advisory firm with offices in Lexington and Louisville. He would love to hear from you at scott@dsneal.com or 1-800-344-9098.
Multi-Cancer Early Detection Putting Molecular Diagnostics to Work
 WHITNEY JONES, MD
WHITNEY JONES, MD
LEXINGTON This year marks the 50th anniversary of President Nixon’s “War on Cancer.”
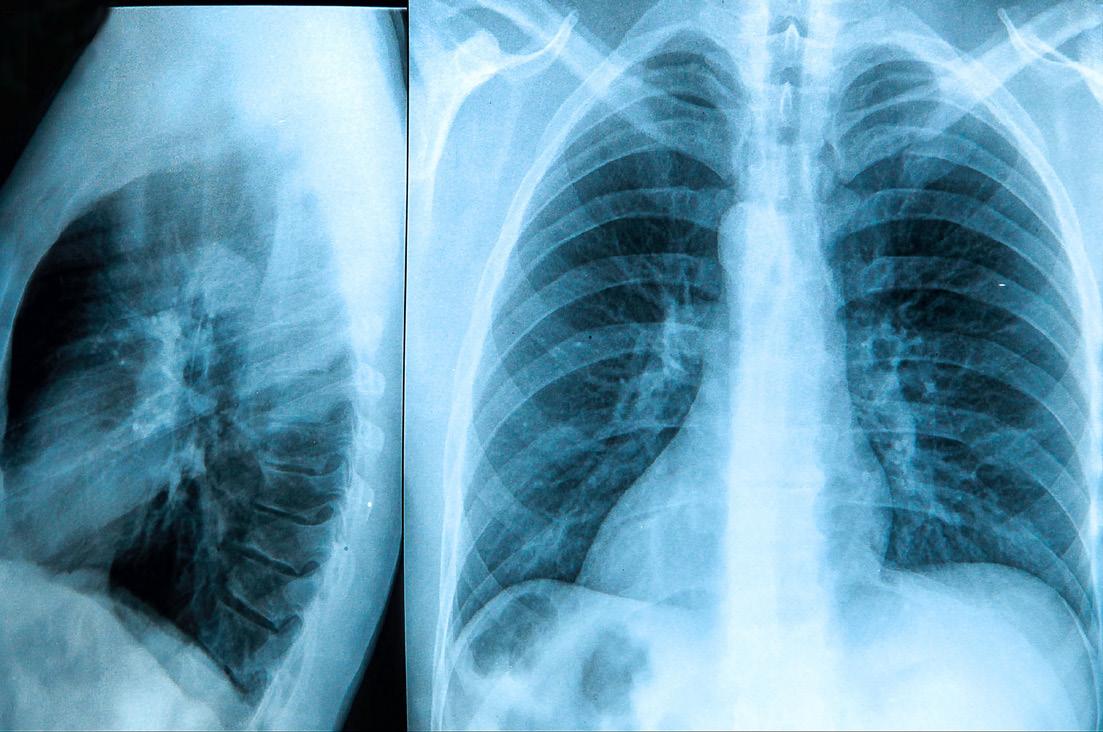
By 2030, cancer is expected to overtake cardiovascular disease as the number one killer in the nation and worldwide. While bright spots on the oncology front, including immunotherapy and the promise of CAR-T cell therapy, are helping to improve survival and prolong life, the bulk of reduction in the overall cancer mortality rate has been because of single cancer screenings as recommended by the USPSTF as well as through reductions in smoking. Suboptimal compliance with single cancer screenings — tragically low with low-dose CT screening for lung cancer — add to our current challenge to save more lives from cancer.
Unfortunately, current screenings do not cover the cancer types responsible for two thirds of all cancer cases and three quarters of all cancer deaths. Seventy-one percent of cancer deaths occur in cancers with no recommended screenings. Rather than being identified while asymptomatic, they usually are diagnosed clinically when the patient presents with symptoms, frequently in advanced stages. Developing effective single cancer screenings for the many cancers not included in USPSTF A, B, or C (s) recommendations is neither practical nor achievable due to the low incidence rates of individual cancers.
Additionally, our current USPSTF screenings are focused on sensitivity as the major metric of success but have low specificity, which generates substantial false positive results. These false positive tests must all be evaluated. The number of false positives outnumber the true positives anywhere from 6 to 20 times (i.e., mammography has a positive predictive value (PPV) of ~5%.) Positive screenings require evaluation, including invasive procedures, potential procedural complications, patient anxiety, and increased health care expenditures. A stunning 8.3 million
positive screening tests must be worked up to detect the ~200,000 screening-identified cancers found each year.
Though cancer is endemic in the population, we can identify elevated risk groups –such as those over age 50 – who have thirteen times the risk of developing cancer as the under-50 population. Other at-risk groups suitable for testing under age 50 may be those with hereditary cancer genes such as BRCA or Lynch Syndrome, survivors of childhood cancers, and those with environmental exposures such as smokers, coal miners, or first responders, especially firefighters.
Three areas have emerged to take advantage of scientific advancements over the last 10 years:
1. The human genome project, which now captures and defines the complexity of our DNA, including mutations, oncogenes, tumor suppressor genes, and epigenetics.
2. The power of DNA sequencing through technological advances which enables us to amplify small segments of DNA or RNA to qualitative and quantitative reports, thus enabling the finding of the proverbial needle in the haystack.
3. Advancements in machine learning (also known as artificial intelligence) which allow identification of differences
imperceptible to humans but clear to a trained machine classifier. Just think how fingerprints or, more commonly, QR codes, can be automatically recognized by your smart phone.
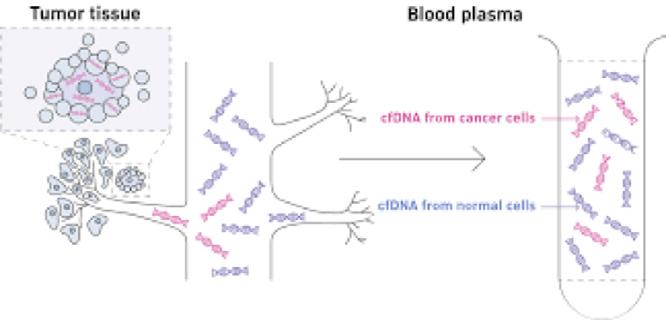
The concept of cell-free DNA is now over a decade old. First used clinically in prenatal testing, it has revolutionized obstetric care by obviating the need for invasive amniocentesis. It was in these clinical utilization scenarios that abnormal DNA signatures were identified in pregnant women who subsequently were diagnosed with cancer, spawning the research and development of multi-cancer early detection (MCED).
All cells, including cancer cells, release or “shed” DNA fragments into the bloodstream through multiple pathways, including apoptosis, secretion, or exosomes. The plasma carries the result of these processes in cell-free DNA (cfDNA). Other analytes in other fluids are being assessed (urine, ascites, saliva), but to date blood has the richest molecular information. Several types of analysis of cfDNA, including mutations, whole genome copy counts, and target methylation, have been studied as pathways.
MCEDs have been demonstrated to detect cancer from many cancer types and across stages. Sensitivity increases by increasing stage. Additionally, the sensitivity of cancer detection varies by tumor type, with aggressive cancers showing elevated levels of cfDNA shedding (lung, biliary, pancreatic, ovarian, head and neck, colorectal) compared to other cancer types which have lower levels of cfDNA shedding (prostate, breast, thyroid).
MCEDs must first identify when a cancer signal (cfDNA) is present in blood. The next critical step for a screening MCED is to accurately predict the cancer signal origin and inform the diagnostic workup. This is critical to streamline the evaluation for all involved: the provider, the health system, and most importantly, the patient. Some MCED tests require broad-based PET CT imaging to work
8 MD-UPDATE
Op-ED pHOTO BY ALEXANDRA ROGERS
Whitney Jones, MD
up the origin of a positive signal whereas others have high levels of accuracy (up to 89%) based on the blood signals alone in predicting the cancer signal origin.
To screen for many cancers that have low individual prevalence but high aggregate prevalence, population-based screenings must minimize false positive results. Thus, it is important to design these tests with fixed high specificity rates, (i.e., extremely low false positives, less than 1 percent). And, since we are simultaneously screening for multiple cancers (over fifty different cancer types in some MCEDs) aggregate sensitivity rather than individual tumor sensitivity plays a greater role. PPV (the likelihood that a positive test is a true positive) is a better measure than sensitivity alone in the MCED or traditional single-cancer screening methodology.
MCEDs also have false negatives. Not every cancer produces a detectable cfDNA cancer signal due to tumor class behavior as well as individual tumor shedding biology. Thus, there remains a need to follow through with cancer prevention through behavioral changes, guideline based single cancer screenings, and ongoing vigilance and reporting of signs or symptoms to healthcare providers.
A broad set of cancers are now detectable in their pre-symptomatic phase through MCED testing. Some of our most difficult cancers, including pancreas, ovary, liver, head and neck, lymphomas, and leukemias, generate positive signals in the pre-symptomatic phase. Multiple MCED tests are in development through multiple corporate entities, and one (Galleri, by GRAIL, Inc) is commercially

available as a lab-developed test and has received breakthrough designation by the FDA. Expect to see multiple products developed with downward pricing pressure because of market competition.
Importantly, MCEDs are meant to complement, not replace, current USPSTF guideline screenings or recommendations such as smoking cessation. Unlike current molecular diagnostics, which are used primarily in the treatment space by oncologists, MCEDs are designed to be used by primary care physicians and specialists. Imagine this as an annual blood test added to your cholesterol, kidney function, and liver tests.
Modeled data suggest a potential reduction of ~100,000 of the over 600,000 cancer deaths annually in the US, but only if the technology can make it through the protracted regulatory process.
No wonder multiple national advocacy groups, including the Prevent Cancer Foundation and the American Cancer Society, are pushing for Medicare to evaluate a National Coverage Determination. Call on your federal congressional representatives and senators to support and cosponsor HR1946 and Senate Bill 1873 today to advance coverage by Medicare and eventually to commercial payors so that all may access this lifesaving technology.
To bend the mortality curve of cancer, we must rework the paradigm. Currently our focus and funding are on advanced cancer care. We must shift this focus to early cancer detection when treatment is less invasive and more effective. This is not an incremental
change; this is a paradigm shift.
We need to be forward thinking and proactive in building the cancer prevention, early detection, and treatment infrastructure for the next 50 years of our war on cancer. We need to be ready as new technology comes online. We need to invest upstream of late-stage clinically presenting cancer cases.
Imagine the benefit from this technology for our communities. It is a game changer. We now have screening tests which will allow us to evolve from only screening for individual cancers to screening all individuals for cancer. Finding cancer earlier, when it can be cured, is a goal we can all share.
Whitney Jones, MD, is the founder of the Colon Cancer Prevention Project and the current chair of the Kentucky Colon Cancer Screening and Prevention Program Advisory Committee.
Note:
Whitney Jones, MD, is an employee of GRAIL and holds an equity position.
NOW ONLINE
ISSUE #136 9
Op-ED
“45 is the New 50”
The New Motto for Colorectal Cancer Screening
BY SHANA MOORE, pHD, MpA TERI WOOD, pHD • CAISEY RAMSEY-JOHNSON • CONNIE WHITE, MD, MS

FRANKFORT The recent change in the U.S. Preventive Services Task Force (USPSTF) guidelines to start colorectal cancer (CRC) screening at age 45 gives us an enormous boost in our ability to reduce the incidence and severity of CRC with simple changes to our best practices. In May 2021, the USPSTF released their final recommendation statement1 on the new screening age of 45, and it has gained momentum throughout the medical and social communities. New messaging that targets adults at age 45 has already begun, but perhaps the most impactful step in the process could be the direct messaging from healthcare providers to patients,2 stating that there are simple and affordable screening options for those at average risk for CRC, steps that take only minutes in the form of stool-based tests completed at home. By starting the conversation and encouraging the screening at an early age, ideally at age 35, the incidence of CRC can be reduced.
They additionally recommend that the screening message should be repeated at least three to four times before the recommended age of initiation.3 The new motto with regard to screening is “45 is the new 50”. Providers should initiate screening messages with:
• a review of pertinent family history regarding CRC,
• a review of the importance of on-time screening and primary prevention for those with a family history, and
• a discussion of the screening options available to identify a risk-appropriate and valueconcordant preference.
In an article published early in 2020, the investigators cited data from a review of Surveillance, Epidemiology, and End Results
10 MD-UPDATE
1 USpSTF Final Recommendation Statement, 2021. https://www.uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening 2 Dyer et. al. patient-Reported Needs Following a Referral for Colorectal Cancer Screening, 2019. https://doi.org/10.1016/j.amepre.2018.08.017 3 Jones et al. Improving On-Time Colorectal Screening Through Lead Time Messaging. Cancer, 2020. https://acsjournals.onlinelibrary.wiley.com/doi/epdf/10.1002/cncr.32535
Connie White, MD, MS
Op-ED pHOTO AND IMAGES pROVIDED BY KY DEpARTMENT FOR pUBLIC HEALTH
Figure 1
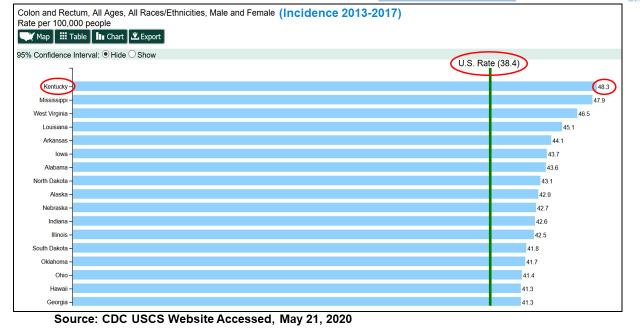
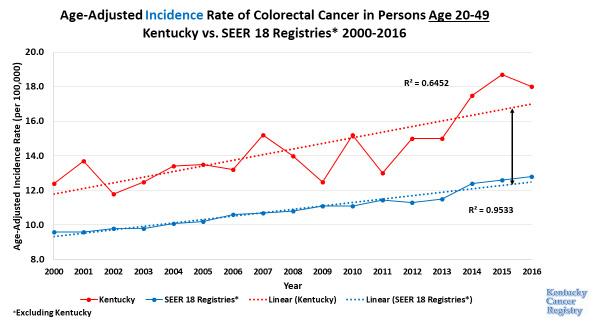
(SEER) registries and found that there was a significant increase in CRC in individuals between the ages of 49 and 50, indicating that these results “would be consistent with high rates of preexisting, undetected cancers in younger patients.” CRC incidence rates in individuals younger than 50 years of age may be underestimated, ultimately resulting in the patient “receiving a [potentially delayed] diagnosis of colorectal cancer after undergoing screening at 50 years.”4 Additionally, recent CDC US Cancer Statistics data show that Kentucky has the highest incidence rate of CRC in the nation (Figure 1).5 This supports the great need for Kentucky health care providers to be leaders in promoting the importance of CRC screening and of screening uptake in younger individuals. Companion data from 2000-2016 supports the importance of CRC screening in younger populations, as the data show there is an increase in CRC incidence in the Commonwealth in younger populations (Figure 2).6
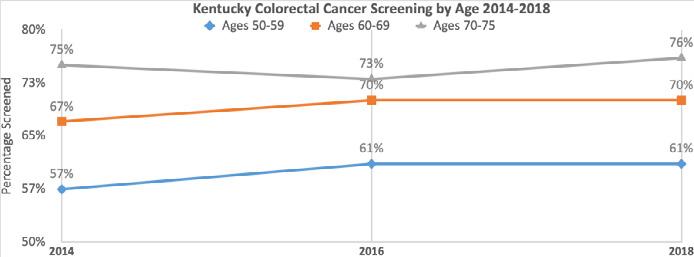
Between 2014 and 2018, Kentucky has had screening progress across populations aged 50-75, but the screening gap in younger populations, who are between the ages of 50-59, is significantly lower than older populations. The marginal upward trend in screening rates for those aged 50-59 from 2014 to 2018 was an increase of about 4%. However, in 2018 the average screening rate for an individual aged 60-69 was approximately 70%, and for those who were 70-75 years of age it was 76%. As of 2018 data displayed in Figure 3, individuals in Kentucky who were 50-59 years of age had a CRC screening rate of only 61%.7 It would be appropriate to estimate that screening rates for those who are younger than 50 would be even lower. Due to the
4 Abualkhair et al. Trends in Incidence of Early-Onset Colorectal Cancer in the United States Among Those Approaching Screening Age. JAMA Network Open. 2020;3(1):e1920407. doi:10.1001/ jamanetworkopen.2019.20407.
5 Centers for Disease Control and prevention US Cancer Statistics. 2020. https://www.cdc.gov/cancer/uscs/index.htm
6 Kentucky Cancer Registry Incidence and Mortality Data 2017 https://www.kcr.uky.edu/ and Surveillance, Epidemiology, and End Results Data, National Cancer Institute 2017. https://seer. cancer.gov/data/
7 Kentucky Behavioral Risk Factor Survey (KyBRFS), Behavioral Risk Factor Surveillance System. Cabinet for Health and Family Services, 2018. https://chfs.ky.gov/agencies/dph/dpqi/cdpb/ pages/brfss.aspx
ISSUE #136 11
Source: Kentucky Behavioral Risk Factor Survey (KyBRFS), Behavioral Risk Factor Surveillance System. Cabinet for Health and Family Services, 2018. https://chfs.ky.gov/agencies/dph/dpqi/cdpb/pages/brfss.aspx
Figure 3
Figure 2
Op-ED
Figure 4
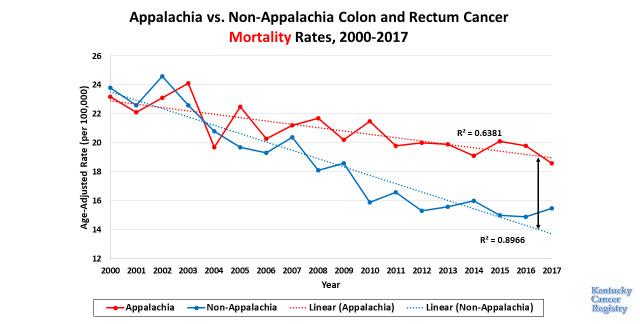
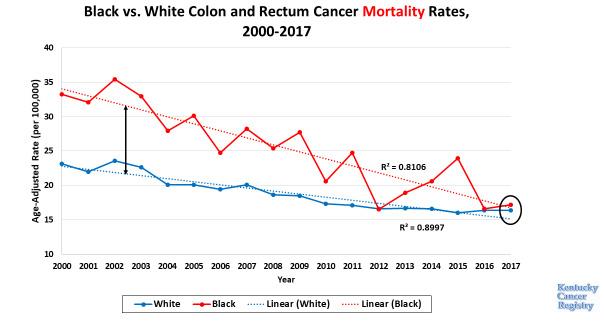
high rate of CRC mortality in the state, and the even higher CRC mortality in the state’s sub-populations, such as those who live in the
Appalachian region (Figure 4) and those who are African-American (Figure 5),8 it is clear that screening younger populations is key to
help decrease CRC incidence and mortality rates in the Commonwealth.
In an effort to encourage screening take-up in all populations in the Commonwealth, three simple practice modifications could be impactful:
1. Talk about CRC screening early—don’t wait until age 45. Encourage individuals to gather and discuss family history.
2. For patients at average risk, discuss various simple, affordable, and faster screening options, and encourage completion, including FIT and stool DNA (Cologuard).
3. Prioritize colonoscopy referrals for those with increased risk due to personal or family health history.
12 MD-UPDATE
8 Kentucky Cancer Registry Incidence and Mortality Data 2017 https://www.kcr.uky.edu/ and Surveillance, Epidemiology, and End Results Data, National Cancer Institute 2017. https://seer.cancer.gov/data/
Op-ED
Figure 5

Making the Impossible Possible
Brown Cancer Center’s Rebecca Redman, MD, ensures head and neck cancer

after treatment
BY TIM CORKRAN
LOUISVILLE The treatment of head and neck cancers has long had the potential to damage sensitive, quality of life-giving tissues. Rebecca Redman, MD, at UofL Health — Brown Cancer Center is working on multiple fronts to eliminate these side effects for Kentuckians. Redman’s research and practice are centered on two things: the reality that head and neck cancer patients are living beyond their treatments at a high rate; and her belief that they deserve a future with full functionality. She is devoted to making it possible for these patients to breathe, smell, taste, chew, hear, and talk like they did before their diagnosis, and she sees a successful future powered by a variety of tools. “With smarter treatments, we are on trajectory to increase survival and minimize side effects,” she says.
Redman initially sought a bachelor’s degree in medical genetics with plans to be a genetic counselor, but the science of genetics in her undergraduate studies got her thinking about medicine. Then, a fortuitous work study placement exposed her to a philosophy which she holds to this day. Working in a pediatric oncologist’s lab, she envied his mix of lab work and seeing patients. She observed how his experience with patients enlightened his research and lab practices. “It brought together those two worlds, my interest in science and my interest in medicine,” she reflects. This informed bench to bedside approach in the form of collaboration with basic science colleagues would be one she continued in her professional life.
The Road to UofL Health
After medical school at University of Wisconsin, Redman went to UNC Hospitals, Chapel Hill for her internal medicine residency and Duke University Medical Center for a medical oncology fellowship. Her marriage to a Kentuckian got her looking at UofL Health, and she was taken by the good fit she perceived upon interviewing. The people at Brown were the key, “I felt like it was a place where I would be supported and able to treat patients in a collaborative, thoughtful way,” she says.
Head and neck cancer treatment at Brown Cancer Center is truly interdisciplinary. A patient is usually referred to Brown from their ENT physician, or possibly a gastroenterologist. The patient then gets a devoted team that includes a surgeon, medical oncologist, radiation oncologist, dietician, and speech therapist, among others. Together, they review the case and see the patient in clinic. This way the patient does not have to go to three different appointments. Most of the Brown head and neck patients have oral cavity or throat cancer issues, with some sinus and salivary glands cancers. With 60-70,000 diagnoses in the US per year, these constitute only 4% of all cancer diagnoses, but there is a high incidence in the Ohio Valley, where tobacco use and HPV cases are common. While relatively rare, head and neck cancers have a disproportionate impact, because of the basic daily functions treatment of these cancers can affect.
From Bench to Bedside and Back to Bench
Today Redman sees patients three day per week, is an associate professor at the UofL School of Medicine, the director of medical oncology service for the Head and Neck Cancer Multidisciplinary Clinic, and the deputy director of clinical research for the UofL Health — Brown Cancer Center Clinical Trials Office. She infuses each role with her concern for a patient’s life after cancer treatment, but it is in the latter where she may be having her greatest impact. She oversees all the phase 1, 2, and 3 trials at Brown, conducted by an entire team of dedicated
14 MD-UPDATE
patients have the best chance for a fully functioning life
COveR STORY
Rebecca Redman, MD, associate professor at the UofL School of Medicine, the director of medical oncology service for the Head and Neck Cancer Multidisciplinary Clinic, and the deputy director of clinical research for the UofL Health — Brown Cancer Center Clinical Trials Office.
research coordinators, nurses, and specialists, who are as fiercely devoted to improving the care of cancer patients as she is.
Clinical phase 1 trials offer two levels of hope. These trials may involve a first-time study of the agent in humans or brand-new drugs and combinations of existing drugs. For people with advanced cancer for whom standard treatments are not enough, participation in trials presents the possibility of a home run, a miracle drug breakthrough that gives them another chance. More often, however, it allows her patients a role in moving the field forward and the knowledge that they are helping tomorrow’s cancer sufferers. She says “Many of my patients find participating in phase 1 trials really rewarding.” Redman’s relationship with her patients is powerfully informed by both what she learns from collaboration with basic scientists and the meaning and hope clinical trials can bring them.
Treating with an Eye for Life after Cancer
More and more cancer patients are outliving their disease, so with an increasing emphasis on survivorship, research is focused on finding treatments that are more effective and less toxic. This is because the head and neck are very sensitive areas. Preserving the function of those organs and tissues is a major preoccupation, so Redman and her colleagues are always looking at the impact on function when considering treatment.
Traditional cancer treatments – radiation, chemotherapy, surgery – can cause complications or long-term health problems, affecting how a patient might eat, talk, hear, and breathe, not to mention how they look. Nerve damage, due to tumor removal, radiation, or some chemo drugs, can result in numbness in the jaw, throat, or neck, and scar tissue can be problematic over time. A change in how
food smells and tastes, dry mouth, and dental problems can all make it hard to eat and drink enough to get the nutrients and fluids a patient needs to live a vigorous life.
For Redman, these treatments will always have a place, but figuring out how to use them with less impact and, more importantly, finding non-invasive alternatives is a goal. “For patients to survive with as much quality of life as possible, has to be our focus,” she says. Many of her research projects have involved advancing such treatments. According to the UofL Health website, some of Redman’s projects have included novel approaches to mitigate toxicities of chemotherapy and radiation, trials of small molecules that target the metabolism of cancer cells, and harnessing the immune system to control cancer. Personalized medicine, however, is key in this, with immunotherapy among the main routes to preparing patients for a side-effect free life after cancer.
ISSUE #136 15
COveR STORY PHOTOS PROvIDeD BY UOFL HeALTH
Jason Chesney, MD, PhD, director and chief administrative officer of UofL Health – Brown Cancer Center, has led the efforts with immunotherapy clinical trials for melanoma and lung cancer, and has many participating in clinical trials.
Unmasking Tumors and Making Smart Blood Cells: A Bright Future

Redman is most excited about immunotherapy, which she summarizes simply: “The drug itself is not killing the cancer but trying to get the immune system to do so.” Making the immune system smarter is the next wave
in cancer treatment and one Redman fully expects to ride for some time. Foremost among these are checkpoint inhibitors and tumor infiltrating lymphocytes.
Checkpoint inhibitors essentially unmask a tumor, which allows the immune system to recognize the cancer as something that should not be there and destroy it. The treatment drug does not interact directly with the cancer, but rather inhibits certain proteins from binding on the tumors and concealing them from the immune system. Tumor infiltrating lymphocytes are a novel personalized medical treatment. White blood cells are extracted from a patient’s tumor, cultivated into large populations in the lab, and then this army of cancer-fighting lymphocytes is reinfused into the patient. By focusing on those lymphocytes that are already programmed to fight that cancer, it allows for a more targeted attack on the cancer cells and is being studied in conjunction with checkpoint inhibitors for increased effectiveness.
Redman summarizes that the goal of immunotherapy is “manipulating the patient’s immune system to try to make it more effec-
tive at fighting that individual’s cancer.” She feels that five years from now, cancer treatment will be all about immunotherapy. “It is here to stay, and it is a game changer when it comes to cancer treatment,” she states.
While currently immunotherapy only benefits a minority of patients, she thinks that will change, and that designing smarter drugs will make that possible. Many of her phase 1 trials are at the leading edge of this, and everyone at Brown Cancer Center is very focused on its potential. “This is incredibly important to all of us, from our trial clinicians up to our director, Dr. Jason Chesney. Kentuckians should be able to get these treatments here and not have to travel to Houston or Cleveland for them,” she concludes.
Leading Research, Empowering Patients
Back at the bedside, Redman is an advocate for patient involvement and empowerment. She supports her patients inquiring about non-traditional and alternative medicines. She says, “We don’t have all the answers. There may be things out there that can help. We

16 MD-UPDATE
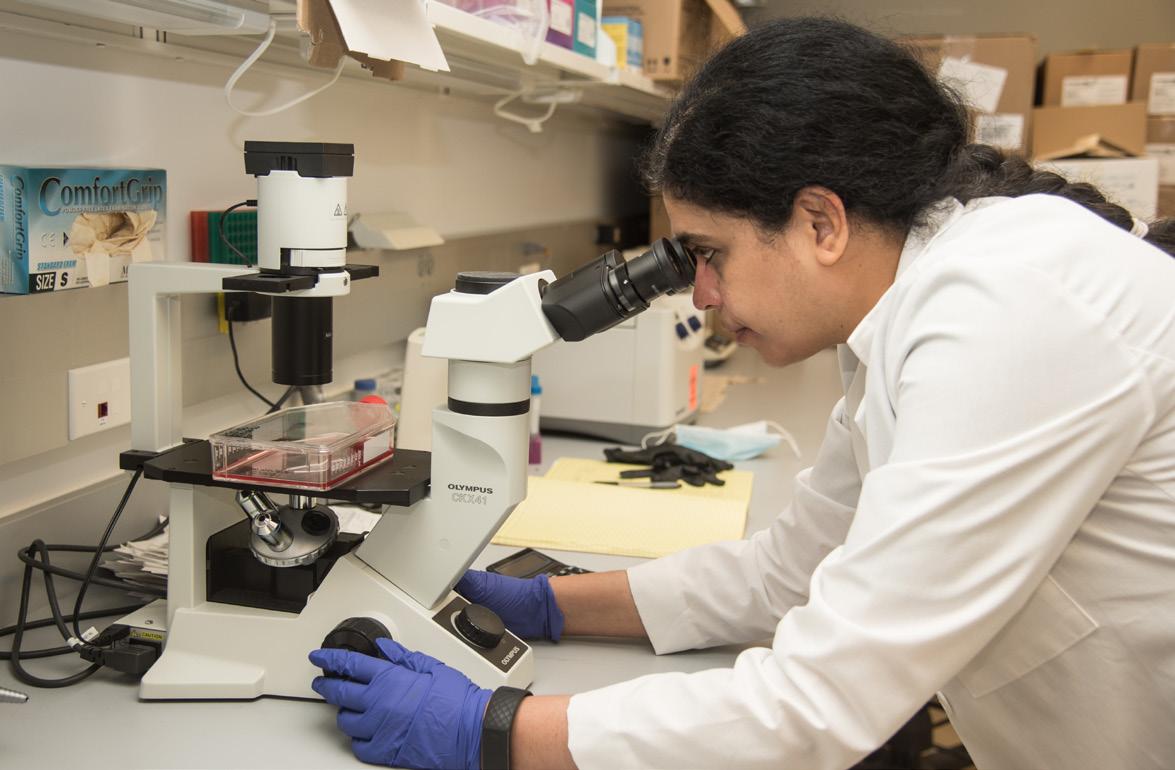
Kavitha Yaddanapuddi, PhD, is studying immune checkpoint inhibitor resistance in lung cancer patients to help develop therapies that reduce resistance and improve treatment.
COveR STORY PHOTOS PROvIDeD BY UOFL HeALTH
Levi Beverly, PhD, is part of the UofL Health-BCC clinical trials team.
have not beaten cancer yet.” She encourages patients to come with questions and ideas. “I tell them there are certainly things out there that may benefit them, but they should bring them to me so I can help them make sense of them.” She also encourages her patients to be part of clinical trials when appropriate. “My patients who have done so tell me it has been rewarding. They feel that they are part of moving cancer care forward,” she recalls.
Redman empowers and supports her patients, and she says, “I treat them as I would expect a family member to be treated; cancer treatment is a shared decision between us to decide what path to go down.” She knows that path is only getting wider and smoother, in part because of her work. “My goal is to help patients live as great a life as they can for as long as they can,” she concludes. With Redman’s research, her directorship at Brown, and her philosophy of patient care, Brown Cancer Center patients can rest assured that such an outcome is possible for them.


ISSUE #136 17
Rebecca Redman, MD, 3rd from the left with part of the Head and Neck multidisciplinary team. They offered free oral, head and neck cancer screenings at the Kentucky State Fair.
Yoannis Imbert-Fernandez, PhD, investigates metastatic breast cancer to further develop clinical trials for this population.
COveR STORY
Jun Yan, MD, PhD, director of the Center for Cancer Immunology and Immunotherapy and chief of the UofL Division of Immunotherapy.
CHI Saint Joseph Health Expands Cancer Care
A Q & A with Jessica Croley, MD
Editor’s Intro: Jessica Jones Croley, MD, is the medical director for CHI Saint Joseph Health Cancer Care, which launched an affiliation an affiliate ofwith Cleveland Clinic Cancer Center in 2019. She is board certified in hematology and medical oncology.

Please give us a brief recap of your background and medical training. Why did you choose hematology and cancer care?
(Croley) I am a native Kentuckian and had a great interest in chemistry and biomedical engineering while attending the University of Kentucky. During my undergraduate years, my father was diagnosed with sarcoma and my grandmother was diagnosed with lung cancer, spurring my interest in the applications of biomedical engineering in the field of oncology. I received my medical degree from the UK College of Medicine, where I also completed my residency in internal medicine and fellowships in hematology and medical oncology.
What are your duties as medical director? Do you still see patients in addition to administration?
My role is hybrid. My clinical focus is in breast cancer, but I see patients with a variety of hematologic and other oncologic conditions. As an active clinician, I am more able to see challenges and opportunities from both the patient and provider experience, helping me guide program strategy.
Do you have a particular area of expertise, or interest in oncology?
My area of sub-specialization is the management of breast cancer. Sub-specialization allows me to work more closely with the Cleveland Clinic Cancer Center breast cancer team to ensure best practices in the management of breast cancer. I work closely with radiologists
and patient navigators at CHI Saint Joseph Health — Breast Care Center at Saint Joseph East to expedite care from the time of abnormal mammogram or suspicious mass, to establishing care with the cancer team to initiating treatment and ultimately for survivorship care. We are a highly integrated unit that looks at patients holistically and cares for them across their continuum. Breast cancer management is highly complex, and having a team of providers is integral to an individual patient’s success.
Describe your involvement in clinical trials
I have been in practice with CHI Saint Joseph Health — Cancer Care since 2013. I am highly involved in quality processes, and have a strong interest in clinical research. Patients under my care have access to over 100 ongoing clinical trials through our national research consortium, CIRI, (CHI Institute for Research and Innovation) allowing them to receive cutting cutting-edge treatment with
the comfort and convenience of a community cancer center.
What does a week in your professional life look like?
A typical workweek includes four days of clinical services with one hour of rounding on inpatients at Saint Joseph East, eight hours of outpatient clinic visits and oversight of chemotherapy infusions and one day of administrative services, reviewing treatment protocols, quality of care, optimizing patient resources, and collaborative meetings with Cleveland Clinic Cancer Center liaisons. Throughout the week I participate in various tumor board meetings where new cancer cases are reviewed jointly by medical oncologists, radiation oncologists, surgeons, radiologists, and pathologists. These meetings are specialized by cancer type such as breast, gastrointestinal, or thoracic, allowing greater focus of care and a high level of coordination of individual services for each patient.
Talk about the CHI Saint Joseph Health Cancer Care Center and its transformation over the years within Central Kentucky.
In the past decade, CHI Saint Joseph Health — Cancer Care has evolved tremendously. Initially, we were a group of various providers operating mostly independently across our market. As part of our Cleveland Clinic Cancer Center affiliation, processes have been reviewed across all of these locations and optimized, providing patients a high level of care, whichever entry point they selected. We have streamlined operations beginning at registration including nursing, pharmacy, and support care services as well as our technical treatment protocols to ensure we are providing the highest quality of care as given at Cleveland Clinic Cancer Center, currently ranked No. 5 hospital in the 2021-22 U.S. News Best Hospitals for Cancer.
18 MD-UPDATE
SPECIAL SECTION ONCOLOgy PHOTO PROVIDED By CHI SAINT JOSEPH HEALTH
Jessica Jones Croley, MD, is the medical director for CHI Saint Joseph Health Cancer Care.
How has COVID -19 changed cancer care at CHI Saint Joseph Health?

Like with everything, our day-to-day processes shifted to allow social distancing, masking, and other precautions. The biggest change was the increased use of telehealth, which has been a tremendous benefit to cancer patients who may be sick, or weak, or otherwise have difficulty with transportation to and from the cancer facility. Vaccination allowed cancer patients to get back to a more normal lifestyle, but unfortunately the recent surge of the Delta variant is particularly ominous for our immune suppressed patients. I would plead with anyone who is unvaccinated to discuss the safety of COVID-19 vaccines with your health care provider and reconsider to help protect this particularly high-risk population.
What’s on the horizon for cancer care at CHI Saint Joseph Health?
Precision medicine continues to grow in the field of cancer treatment. In medical oncology,
there are dozens of new drugs approved each year which target individual mutations or other aspects of cancer growth, most of which are more effective and less toxic than traditional chemotherapy. Some cancers are even able to be treated without the use of chemotherapy. More and more, we rely on tumor sequencing to develop a “roadmap” of treatments that are likely to be beneficial over an individual patient’s cancer course, as opposed to treating all patients with a certain cancer in the same manner. Radiation oncology is becoming more and more targeted as well. Stereotactic body radiation allows pinpoint accuracy, minimizing radiation to healthy tissues and optimizing the dose given to tumors. Newer techniques often require fewer treatments as well.
Describe your personal philosophy of care.
My personal philosophy of care is holistic cancer care, treating the whole patient with cancer as opposed to the cancer only. Many
times, there are barriers to care including patient preference, impact on lifestyle, finances, and other health concerns that factor into decision making for treatment. It is imperative to solicit all of these elements from patients and maintain a focus on function and quality of life while attempting to prolong life with chemotherapy or other cancer treatments. I see the cancer journey as a joint one between the patient and oncologist and feel very humbled to be able to support patients in that.
For patient referrals, chisaintjosephhealth.org/hope 859.313.HOPE
ISSUE #136 19
(4673)
844.940.HOPE (4673) Your business is healthcare, You know what care looks like, maybe your bank should too. Equal Opportunity Lender Republic Bank & Trust Company Loan Originator ID #402606 Give Emily Miller, Private Banking Officer, a call at (859) 266-3724 NMLS ID # 419242 21RB1198_MD_Ad_Update.indd 1 5/21/21 12:07 PM SPECIAL SECTION ONCOLOgy
Toll free:
Parlaying Personal Experience into Patient Care
Being fellowship trained in hand surgery and breast reconstruction keeps Michelle Palazzo very busy.

20 MD-UPDATE
SPECIAL SECTION PLASTIC SurgEry
Michelle Palazzo, MD, board-certified plastic surgeon with Kleinert, Kutz, and Associates, is also the program director for the Christine M. Kleinert Institute Fellowship in Hand and Microsurgery, which was started by Harold Kleinert, MD, nearly 50 years ago. She works with over 1,500 national and international alumni fellows.
PHOTO By gIL DuNN
By DONNA ISON
and the Kentucky Society of Plastic Surgeons.
LOUISVILLE/
NEW ALBANY,
IN Few physicians can say they have been both surgeon and patient for the same procedure. However, Michelle Palazzo, MD, now performs similar reconstructive surgery to the one she underwent as a patient after being diagnosed with ductal carcinoma in situ (DCIS) and having a subsequent mastectomy and breast reconstruction. Her diagnosis occurred during her chief year of plastic surgery residency at St. Louis University.
Palazzo, a board-certified plastic surgeon with Kleinert, Kutz, and Associates uses this experience to better relate to her own breast reconstruction patients. She states, “I’ll share with them that I do understand what they’re going through—though not exactly, because everybody’s different—and that, 15 something years ago, I was in their shoes and having to learn about what my options were to try to take care of the cancer.”
Since her own diagnosis and surgery much has changed for Palazzo, both in her life and in the realm of breast reconstruction. Following her recovery, Palazzo traveled to Washington, D.C., to complete a year fellowship in reconstructive & aesthetic surgery of the breast at Georgetown University under Scott Spear, MD, who was one of the top breast reconstructive surgeons in the nation at the time.
Prior, Palazzo had garnered her bachelors and master’s degrees in engineering from the University of Illinois, along with a medical degree from Southern Illinois University School of Medicine. She had also completed a residency in general, plastic, and reconstructive surgery at St. Louis University. After leaving Washington, Palazzo embarked on a one-year fellowship at the Christine M. Kleinert Institute for Hand and Microsurgery in Louisville.
She joined Kleinert Kutz as staff in 2006. Currently, in addition to being a partner, Palazzo is the program director for the Christine M. Kleinert Institute Fellowship in Hand and Microsurgery as well as a clinical professor of hand surgery at the University of Louisville. She is also the current president of the Ohio Valley Society of Plastic Surgeons
Since taking on the role of fellowship program director five years ago, Palazzo has worked to make certain both the fellows and faculty are in compliance with all rules and regulations set forth by the Association of Graduate Medical Education. She also works with the over 1,500 alumni fellows who have graduated from the program, which was started by Harold Kleinert, MD, nearly 50 years ago.
Of the position, she says, “It’s like taking care of 16 kids from all around the world. And so that’s been quite an adventure, but I love working with the fellows.”
Every Day is Jam Packed and Different
On a weekly basis, Palazzo’s schedule is packed with clinic visits; hand surgeries to address issues including carpal tunnel, ganglion cysts, broken bones, and other injuries; and breast reconstruction. She also works with dermatologists on skin cancer cases, especially those that are on more visible areas, such as the face, and are thus more “cosmetically important.”
Her patients come from “all walks of age,” ranging from toddlers with conditions like congenital trigger fingers to individuals in their 90s with carpal tunnel. “It’s all ages, it’s men and women. That’s one thing that’s really cool about plastic surgery is that we work on all age groups,” said Palazzo.
Of course, due to her personal experience, some of Palazzo’s most rewarding work is with the breast surgeons, primarily with Baptist Floyd and Baptist Louisville, who call on her to complete the reconstruction portion of complex surgeries to achieve the best aesthetic result.
Improvements in Breast Reconstructive Surgery
Since her first exposure as an engineer in graduate school working with a surgeon to determine the strength and longevity of breast implants, Palazzo has seen significant improvements in this specialty. First, in the use of biologic tissue to create a sturdy scaffolding to help support the breast in lieu of having to take tissue from other parts of the body. Tissue
The Sientra AlloX2 tissue expander is used in breast reconstruction. It is unique because there is an integrated drain connected to a port that can be accessed through the skin like a chemoport. In addition, it has the traditional expansion port to fill the expander with saline.

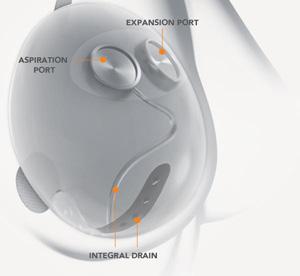
“I use this expander now almost exclusively for expander/implant-based breast reconstruction.”
— Michelle Palazzo, MD
expanders with a drain built into them are also now available, which allows the surgeon to access collected fluid and avoid accidentally puncturing the breast implant with a needle. Another major change is in the planning of incisions and use of different incisions. Palazzo says, “With the plastic surgeon and general surgeon working together, we can plan the incisions for lumpectomy and make better patterns for scars. It’s done not necessarily so we can make the scars better, but so that we
ISSUE #136 21
SPECIAL SECTION PLASTIC SurgEry
are able to place them in a better position so that they’re less noticeable.”
Fat grafting—taking fat from one area of the body to transplant in another—has also made great strides. According to Palazzo, “The use of fat grafting for reshaping the breast in areas that need it after a mastectomy or radiation has also helped greatly with breast reconstruction in recent years.”


With these innovations, Palazzo believes in making certain her patients are also aware of all of the latest alternatives for their treatments. She states, “I like the patients to be informed of all their options, so that they can make an informed choice in their treatment and be an active participant in their treatment. I don’t want to just tell them what to do.”
With a commitment to keeping patients informed, Palazzo addresses two common misconceptions: “Some patients have a concern that they can only get their breast reconstruction done within two years of having their breast cancer or that they can only get

it fixed once and can’t have revisions. That’s a common fallacy that I hear from my patients.” She stresses there is no set time limit when reconstructive surgery can be completed and reconstructive surgery does not have to be one and done.
On the flip side, if Palazzo could send one message to oncologists and general surgeons, it would be to involve the plastic surgeon as early in the process as possible. This affords better planning for their surgery, the incision, and all aspects of the procedure. Having patients meet with their plastic surgeon early in the process also leads to greater confidence and comfort on the patient’s part.
Palazzo encourages oncologists to “Send patients as early and quickly as they can, so








we can plan the steps necessary to get the best aesthetic outcome and treatment for their breast cancer.”
From someone who has been both patient and surgeon, that sounds like a good plan.
22 MD-UPDATE
SPECIAL SECTION PLASTIC SurgEry
Michelle Palazzo, MD, is the current president of the Ohio Valley Society of Plastic Surgeons and the Kentucky Society of Plastic Surgeons. She is also a clinical professor of hand surgery at the university of Louisville.
PHOTO By gIL DuNN
The Evolution of Gynecological Cancer Care
An in-office surgery suite adds comfort and convenience to comprehensive care
LOUISVILLE The years 1971-1972 were pivotal for cancer treatment for women in the U.S. Three prominent, well-known women, Betty Ford, Happy Rockefeller, and Shirley Temple Black, publicly announced that they had breast cancer. President Richard Nixon declared a “war on cancer,” and Title IX of the Educational Act, which mandated equal access to all educational opportunities for both sexes, led to more women than ever before entering medical school.
By the mid 1990s, breast cancer awareness had entered the American cultural mainstream and pink ribbons were a recognizable symbol promoting mammogram screening and treatment. Breast cancer is still the deadliest cancer for women. But now there’s a new focus on screening and treatment for other female cancers, such as ovarian, uterine, cervical, and endometrial. Teal-colored ribbons for ovarian and cervical cancer awareness are the new signs of the times.
Enter Women First of Louisville
If Title IX in 1972 resulted in more women entering medical school, by 1988 the result was Women First of Louisville Obstetrics and Gynecology, the first all-female practice in the area. Founded by and for women, the medical practice was dedicated to bringing a unique female perspective and the latest technology to provide women of all ages with comprehensive obstetrical and gynecological care.
With 11 board-certified female physicians at the helm, Women
First is no stranger to leading the way in women’s health care. Their goal is to ensure that each phase of comprehensive care, from evaluation with state-of-the art equipment to the diagnosis and surgical solution, can be performed right in the office.
By offering many minimally invasive, in-office surgical procedures, Women First has found the way to optimize the patient experience. “We have continued to broaden our strategies so that we can better meet patient demand for convenience as well as costeffective, quality care,” says Executive Director Denise Kirkham. “We currently offer in-office services such as endometrial ablations for heavy periods, treatment of abnormal pap smears, and bladder Botox® for urinary incontinence. By expanding into a larger surgery suite over two years ago, we offer a more comfortable and caring environment for our patients.”

ISSUE #136 23
SPECIAL SECTION OB-GyNECOLOGy
Margarita Terrassa, MD, in the waiting room of the calm, comfortable, in-house surgical suite at Women First.
PHOTO By ALEXANDRA ROGERS
Meet Margarita Terrassa, MD
After completing her undergraduate degree at Syracuse University in Syracuse, New York, Margarita Terrassa, MD, who is board-certified in obstetrics and gynecology, received her medical degree from Ponce School of Medicine in Ponce, Puerto Rico and completed a residency at Tulane University Hospital in New Orleans, Louisiana.
The majority of doctors now specializing in OB-GYN are female, creating a paradigm shift in women providers caring for women. Terrassa, who serves as the medical director for the Women First in-office surgery and procedure suite, says, “We are very proud to be the pioneers in offering surgical procedures in the comfort of our own office space.”
Specialty-Focused and Patient-Oriented
Decades ago, an OB-GYN practice was judged successful by the number of babies delivered. Think the “baby boom” from 1945 to 1965. A gradual shift occurred in the past
several decades when OB-GYN generalists began tracking one subspecialty or the other. Some of the Women First physicians practice gynecology exclusively. Some have a mixed practice of obstetrics and gynecology with advanced training in robotic surgery.
With a comprehensive diagnostic approach to caring for all of a woman’s reproductive organs, Women First physicians are laser-focused on screenings and surgical treatment of cancer in the early stages. Additionally, not all presentations of abnormal bleeding or pelvic pain are cancerous. That’s where the comprehensive care approach is key, as is knowing their patients and their history. “At Women First, we treat our patients how we would want to be treated,” says Terrassa. “I treat my patients as if they were part of my family.”
The In-House Surgical Suite at Women First

The benefits of having their own in-house surgical suite are numerous, says Terrassa. The atmosphere is calm, comforting, and relaxed.
Family members have a private waiting area. The wait time for procedures is much shorter than a hospital visit, because the patients are scheduled for maximum efficiency and turnaround time between patients is less. “Many of our patients refer their friends because their surgical experience was that good,” says Terrassa.
The gynecological surgeons at Women First are able to perform a wide range of procedures such as diagnostic ultrasounds for a variety of conditions; endometrial ablation; hysteroscopy for examining the uterine cavity; LEEP (loop electrosurgical excision procedure) to remove abnormal tissue from the cervix to confirm a cancer diagnosis or treat pre-cancerous cells; and urodynamics, which examines the functionality of the bladder when urinary incontinence is present.
When a patient has persistent abnormal uterine bleeding, the Women First surgeons can perform a hysteroscopy-guided examination for polyps, fibroid tumors, and scar tissue. Uterine ablation, heating of the uterine lining, can also be performed to help abnormal bleeding.
24 MD-UPDATE
SPECIAL SECTION OB-GyNECOLOGy
Performing a hysteroscopy to inspect the uterus is one of many procedures done in-house at Women First. Pictured are (l-r) Kim Aldridge, CMA, Jamie Baldwin, LPN, and Margarita Terrassa, MD.
PHOTO By GIL DUNN
When a patient presents with a miscarriage from four to ten weeks of gestation, the Women First surgeons clean the uterus of cellular and tissue debris, under sedation. Patients’ partners are encouraged to attend, as it can be an emotional experience for the woman, so it helps to have a partner present. “We care for our patient and her partner with equally comforting care,” says Terrassa.
The in-office surgeries can be performed with or without anesthesia, depending upon the patient’s preference and the procedure. Most procedures are performed relatively quickly, in 15-20 minutes, and then the patient is able to recover comfortably in the office setting and leave the same day.
Well Woman Care
Every woman needs to begin having pap smears by age 21 and continuing through age 70, says Terrassa. Women First also recommends having the HPV, human papilloma virus, vaccination starting at age 12 through 26. Cases of HPV, and other sexually transmitted diseases such as chlamydia, gonorrhea and syphilis, are still present in the U.S. and are sharply rising, up 30% between 2015 to 2019, according to CDC data, released in April 2021. Additionally, the CDC has identified HPV as a causal agent of cervical, vulva, and vaginal cancer.
“The benefits of getting the HPV vaccination highly outweigh the very rare cases of negative side-effects,” says Terrassa. Women First strongly encourages yearly cervical pap smears for their patients. “We listen to our patients’ problems and do the appropriate workups, which can include ultrasound that can lead to the early diagnosis of potentially malignant pathology,” she says.
Pelvic pain is a common condition for women after childbirth, Terrassa states. “Our typical gynecological work-up for a woman presenting with pelvic pain includes an ultrasound to rule out any masses of the ovaries that could have ovarian cancer pathology.”
Birth control pills reduce a woman’s risk for ovarian and endometrial cancer because they keep the lining of the uterus so thin that cells do not build up as sites for cancerous cells. “They also prevent ovulation,” says Terrassa. Without
ovulation, there are fewer possible lingering cells that can mutate into cancer. More common contributing risk factors for gynecological cancer are smoking, obesity and genetics.
Terrassa and her colleagues at Women First strive to educate their patients on the signs of abnormal uterine bleeding so prevention and treatment can take place as soon as possible. Similarly for cervical cancer, she commends pediatricians for vaccinating many young boys
and girls with the HPV vaccine to stop the disease from spreading. “I believe we will see fewer and fewer uterine and cervical cancers in the future because of our efforts to educate our patients, because of HPV vaccines, and because the next generation is smoking less and exercising more,” says Terrassa.
From 1988 to whatever the future brings, the OB-GYN doctors at Women First of Louisville will be pioneers of comprehensive care.

ISSUE #136 25
SPECIAL SECTION OB-GyNECOLOGy
Offering Options and Elevating Education
Breast surgical oncologist uses compassion and technology for better outcomes
 BY DONNA ISON
BY DONNA ISON
LEXINGTON In the third grade, Andrea Colton, MD, MPH, wrote a book titled “My Grandpa’s Open-Heart Surgery,” chronicling the observations and lessons she’d gained at Cleveland Clinic visiting her grandfather while he recovered from a heart attack and subsequent surgery. The book was even replete with hand-drawn illustrations of her grandfather recuperating in his hospital bed and an anatomical representation of the heart.
Of the experience, Colton says, “I got to see him hooked up to all the different machines in the ICU and they explained that this was ‘keeping grandpa alive.’ About the surgery, they actually explained, ‘We connected this artery to this artery and this artery to this artery.’ And, so from that experience, I decided I wanted to be a surgeon.”
After attending the University of Kentucky and achieving a BS in dietetics, Colton received her medical degree and master’s of public health from St. George’s University in Grenada.
Colton states that her interest in public health came from her desire to have an impact on a larger patient population in addition to her surgery patients. “Working with one person helps that one patient, but public health helps a larger population,” she says. She remembers a fellow church-goer who had put off getting a mammogram until a lump was found in her breast. “I felt that by encouraging people to do small things for their health, they could have better outcomes and that spurred my interest in public health.”
Colton did her general surgery internship at Einstein Medical Center in North Philadelphia in Pennsylvania and a five-year
general surgery residency at Conemaugh Memorial Medical Center in Johnstown, Pennsylvania. While there, she was exposed to a variety of different types of surgery—vascular, cardiothoracic, plastic, endocrine, cancer, colorectal—but was having trouble finding a specialty that suited her personality. After working with Patti Anne Stefanick, MD, who headed a breast surgery private practice, Colton knew she had found the right fit.
Of watching Stefanick with her patients, Colton says, “I remember going in, and she was holding their hands and talking to them, easing their fears and just reducing their anxiety levels. It made a really big impact on me. From that mentorship, I applied for a fellowship for breast surgical oncology.”
From Texas to the Bluegrass
Upon completing her fellowship at the University of Texas Southwestern in Dallas, Colton decided to return to Kentucky and join Lexington Clinic. This decision was largely based on the fact that Colton wanted
a say in how her practice was set up and her patient protocols, particularly the amount of time allotted for each encounter. She states, “Breast surgery is not something that you can just say, ‘Hey, you’ve got appendicitis, and we need to take it out. And here’s how we’re going to do it.’ Our job is to explain all the different options, with the risks and benefits, and allow the patient to make the decision that is best for them. And that ultimately requires some time. It’s a lot more complex than you can discuss in a few minutes.”
Colton cares for both malignant and benign breast disease and performs excisional biopsies, nipple sparing mastectomy, skin sparing mastectomy, and partial mastectomies with oncoplastic techniques, optimizing cosmetic results as a Hidden Scar-trained surgeon. The vast majority of her patients are middle-aged and above women, though she occasionally encounters younger women and men with breast disease.
Advanced Technology for Improved Results
With breast cancer, across the board, technology has vastly improved the surgeon’s ability to make certain that tumors are removed with adequate margins. Two, in particular, have elevated efficiency: radio-frequency identification (RFID) tags and 3D mammography within the OR.
Colton explains, “If we cannot feel the malignancy within the breast, we use a localization called a radio-frequency ID tag. This is essentially a microchip that we place in the breast. Then, I am able to tell exactly how far away I am from the microchip.” A large area of calcifications may require multiple
26 MD-UPDATE
SPECIAL SECTION BrEAST SurgICAL ONCOLOgY
Andrea Colton, MD, MPH, breast surgical oncologist at Lexington Clinic
PHOTO BY PAuL MArTIN
RFIDs placed in different areas to indicate the margins.
The 3D mammogram machine allows the surgeon to see one-millimeter slices of the specimen to evaluate exactly how close they are to any of the edges to determine whether further tissue needs to be taken to prevent additional surgery at a later time.

Breast cancer surgery has also advanced in its aesthetic abilities. Oncoplastic surgery, in which tumor removal and reconstructive surgery occur at the same time for breast conservation, allows for much better cosmetic outcomes. Two options are the Goldilocks mastectomy option and the Hidden Scar technique.
Colton explains the Goldilocks method: “If a patient has a good amount of subcutaneous tissue, then it facilitates us being able to remove all of the breast tissue in a pattern, which is very similar to a breast reduction. The tissue that is left in place is subcutaneous tissue, which is not at risk for breast cancer. And so that subcutaneous tissue is rearranged
in a way that makes a full or small mound that resembles a breast.” Oftentimes, this breast contouring results in surgery being undetectable while a patient is clothed.
The Hidden Scar procedure, which she currently performs on 95% of her patients, strives to make individuals more comfortable with their breast surgery results while unclothed. This technique involves hiding the incision around the areola, in the inframammary fold along the bottom of the breast, or in the axilla. Colton states, “I have patients that come back, and they say, ‘Oh my gosh, my doctor couldn’t even find your incision. It was so small and so hidden.’”
For more complete or complex cases requiring an implant, reconstruction is performed by a plastic surgeon who places a tissue expander or an implant at the time of the initial surgery, after Colton has removed all the breast tissue.
Ultimately, beyond actually performing their surgery, Colton sees her job as empowering the patients to be able to make an educated decision. On that note, there is something important Colton says in closing: “The biggest thing I want women, or anyone with breast cancer, to know, is they have a lot of options and they need to feel comfortable with whom they’re working with. Most women don’t really understand that they have the ability to choose whether you remove all your breast tissue or whether you get reconstruction or whether you have a small or large surgery. The vast majority have a lot of options that they don’t realize they have.”
From observing open heart surgery to performing breast reconstruction, Colton has followed her passion, and her patients are better for it.
Dr. Andrea Colton provides services in breast surgery and cares for both malignant and benign breast disease processes. She also performs nipple sparing mastectomy, skin sparing mastectomy and partial mastectomies with oncoplastic techniques.
Dr. Colton is also a Hidden Scar trained surgeon, a procedure that effectively treats the cancer while optimizing cosmetic results.
Dr. Colton can be reached at 859.258.4932.
Your doctors for life .
ISSUE #136 27
1221 South Broadway | Lexington, KY 40504 lexingtonclinic.com/breastcancercare
ANDREA COLTON, MD, MPH BREAST SURGEON | LEXINGTON CLINIC CENTER FOR BREAST CARE
“The biggest thing I want women, or anyone with breast cancer, to know, is they have a lot of options.”
SPECIAL SECTION BrEAST SurgICAL ONCOLOgY
— Andrea Colton, MD, MPH
BY JIM KELSEY
LOUISVILLE Growing up, Erica Takimoto, DO, was always skilled in science and math – two great strengths that could easily lend themselves to a number of careers. For instance, as an undergrad at Midwestern University in Glendale, Arizona, near her hometown of Scottsdale, she toyed with the idea of being a pilot. Oddly, it was an English class that helped determine her decision to become a gynecologic oncologist.
“I did an English paper where I compared and contrasted Eastern versus Western medicine approaches, and I found that to be extremely fascinating,” Takimoto says. “From there the seed was planted and it just kind of took off.”
Takimoto received her DO degree from Nova Southeastern University College of Osteopathic Medicine in Fort Lauderdale, Florida. Then she completed an obstetrics and gynecology residency at St. Vincent Mercy Medical Center, Toledo, Ohio. After practicing as an OB-GYN for a couple of years, she completed a gynecology oncology fellowship at Florida Hospital Cancer Institute in Orlando. Her most recent move came
Knowledge Is Power
A calculated journey led Erica Takimoto, DO, to Baptist Health Louisville’s first gynecology oncology program

earlier this year when she was recruited to help launch the first-ever gynecology oncology program at Baptist Health Louisville. Her clinical focus includes gynecologic cancers, laser surgery, ovarian cancer and ovarian masses, radical pelvic surgery, robotic gynecologic cancer surgery, trophoblastic disease, uterine cancer, and uterine masses.
While her math and science background helped drive her towards a medical career, she says it was her mother, a nurse, who instilled in Takimoto the qualities necessary to treat cancer patients.
“Cancer patients are a very special population,” Takimoto says. “They have a pretty severe affliction with a terrible disease process. It really requires a high degree of medical knowledge, but also a very high degree of compassion.”
Gynecological Oncology Was the Perfect Fit
Compassion first led Takimoto to consider pediatric oncology, but she found OB-GYN to be a better fit.
“I really enjoyed the surgical component of OB-GYN, so that’s what I pursued,” Takimoto says. “Then I discovered that part
PHOTOS BY ALEXANDrA rOGErS
of gynecology is cancer focused, and I said ‘That’s what I want to do.’”
Now she is doing what she wants to do every day. She treats cancer patients via both surgery and chemotherapy in women of all ages, with most of her patients being post-menopausal. She treats cancers of the ovary, fallopian tube, peritoneum, uterus, cervix, vulva, and vagina. Her most common patients are those with endometrial cancer. More rare cases include pregnant women who develop cervical cancer or an ovarian mass or tumor.
Her patients are generally referred to her by their primary care physician or gynecologist. Takimoto understands that a patient referred to her is bound to come in with a certain amount of fear and worry. She finds it helpful to start from the beginning and work through exactly what the patient can expect and what the steps of treatment will be.
“I start by gaining an assessment as to what they already understand,” Takimoto says. “Then we talk about the disease process, upcoming plans, the short-term and longterm game plan. We talk about what they can expect at every step of the way because knowledge is empowering and it helps to alleviate that fear.”
28 MD-UPDATE
SPECIAL SECTION GYNECONOLOGIC SurGErY
A Collaborative Team Approach
Central to that game plan is the continued presence of Takimoto and her team, who manage the patient’s care every step of the way. Each physician at the Baptist Health Louisville gynecology oncology program is joined by a physician assistant, a nurse clinician, and a medical assistant, along with a team of office managers and schedulers. They also work closely with radiation oncology, medical oncology, and other specialty surgical services physicians.
Most patients come to Takimoto having been thoroughly screened, and it us up to her to determine the course of treatment, which can include any combination of surgery, radiation, and chemotherapy.
“Some cancers will require surgery up front, some of them are advanced stages or inoperable. Some we can get to surgery eventually, if we use chemotherapy first,” Takimoto says. “Every scenario is unique, and you have to assess the whole patient.”
For those who are eligible for surgery, Takimoto performs both robotic and non-robotic procedures, noting that she developed her robotic surgery skills during her three-year fellowship. She says that the robotic technology offers extreme precision in addition to
decreased blood loss, operating room time, pain, and length of hospital stay.
“The decision for robotic or non-robotic is based on where the cancerous tumor is located, how big the tumor is, if it involves any other organs, and the patient’s ability to tolerate the procedure,” Takimoto says. “If a patient is not optimal for surgery, it can be because the cancer is too extensive, perhaps it has metastasized to a different organ, or the patient may not be medically healthy enough.”

Genetic Testing Is Optimal
Like many other cancers, risk factors for gynecological cancers include lifestyle, age, obesity, and genetics. It is the genetic component that is the most promising for early detection or prevention.
“We are able to diagnose genetic risk,” Takimoto says. “So patients can come in now for a prophylactic surgery, whereas we were previously at the mercy of whenever the disease decided to create symptoms. If you know that you have a genetic predisposition to ovarian cancer or fallopian tube cancer, the recommendation from the American College of Obstetricians and Gynecologists, in agreement with Society for Gynecologic Oncologists, is to have removal of the tubes
and ovaries at age 35 or at the completion of childbearing, whichever one is sooner.”
The genetic advancements take the spotlight, but Takimoto is also encouraged by improvements in treatment options that are more targeted to each specific patient and their diagnosis.
Targeted Chemotherapy
“It’s very exciting that we have new treatment modalities,” she says. “For a long time, there hadn’t been any changes in the role of chemotherapy. More targeted treatment options are now opening up based on the tumor’s specific genetic markers. Basically, the tumor is showing us its cards, its weaknesses. We are able to exploit those weaknesses to attack the tumor.”
Gathering information, searching for answers, and being decisive worked throughout Takimoto’s journey from prospective pilot to gynecological oncologist. It’s a methodology that promises to help her patients on their path to recovery, just as it helped Takimoto find the place she was meant to be.
“Baptist Health Louisville has needed a gynecological oncologist for a long time,” she said. “I’m honored to be able to fulfill that role.”
ISSUE #136 29
“robotic technology offers extreme precision in addition to decreased blood loss, operating room time, pain, and length of hospital stay.”
SPECIAL SECTION GYNECONOLOGIC SurGErY
– Erica Takimoto, DO
Mom Guilt? How to Give Yourself — and Your Loved Ones — a Break.
BY JAN ANDERSON, PSYD, LPCC
“Good moms don’t have fun without their kids around.”
You might be surprised at the woman who confessed this thought and when it crossed her mind.

The thought intruded into the mind of Jessica Rohr, PhD, a professor at Baylor College of Medicine. It barged in while Rohr was celebrating her anniversary with her husband (who, by the way, reported absolutely no guilt in being away from their daughter for their special occasion.)
Mom Guilt. “That pernicious feeling that comes from not doing things a certain way, or doing them too much or doing them wrong, according to some unknowable and ever-changing rule book,” according to Dr. Rohr.
What Triggers Mom Guilt?
Research from Finland has identified some specific Mom Guilt triggers. The first five ways to trigger an inner critic attack are clear cut:
1. Actual or imagined aggression
2. Wanting to leave in some way
3. Being gone in some way
4. Favoring one child over the other
5. Not corresponding to your own or others’ idea of a good mother.
It’s the last trigger that gives you an idea of what Dr. Rohr meant by the “unknowable and ever-changing rule book”: Not corresponding to your own or others’ idea of a good mother. That leaves mothers vulnerable to being judged or shamed by just about anyone.
There’s Plenty of Guilt to Go Around.
In Germany, it’s known as rabenmutter, or raven mother, referring to the blackbird that pushes chicks out of the nest — a slur used to shame mothers like Manuela Maier. It happened when Maier decided to return to work and signed up her 9-year-old son for full-day classes
at his primary school — and found herself ostracized by other mothers and openly criticized by her neighbors and family. In a local store, someone even screamed at her, asking her why she had children if she couldn’t take care of them.
Despite a labor shortage and growing economic necessity, the rabenmutter attitude persists, and Germany now has one of the world’s lowest birthrates. (And a chancellor who, not surprisingly, is childless.)
Even more dramatically, Japan’s 2018 birthrate fell to the lowest level since 1899, when record-keeping began.
It’s still an either/or decision for many women who love their children and love their work.
Why am I talking about this? You may be surprised at reasons 2, 3, and 4 for my interest in Mom Guilt.
1. My clients who are mothers.
2. Their husbands.
3. Wine moms.
4. Mother and adult-child estrangement.
The Evolution of the Good Mother Archetype.
But first, some context. The Good Mother archetype is seared into our evolutionarily evolved survival system, especially mammals. In contrast, as soon as reptile eggs hatch, the offspring are pretty much ready to survive on their own. Not much bonding with Reptile Mom is necessary. Not so with mammals, especially human beings, who are born much more immature and require a prolonged developmental period to adapt to their environment. We have by far the longest developmental period — It takes us 25-30 years for the prefrontal cortex to finish developing. That kind of brainpower is good for our adaptability, but required the evolution of a unique caregiving system. Our mammalian system motivates parents to bond with their offspring so they’ll want to hang around and take care of the kiddos.
What does this mean every time a twenty-first-century mom feels overwhelmed, resentful, or just plain tired? It’s a train wreck of conflicting emotions with her inner critic, ready to pounce and do its evolutionarily-inspired job, reinforced by other members of our mammalian caregiving species.
Mom Guilt is not Just an Issue for Mothers. It’s Also an Issue for the Men Married to Them.
That’s why I was surprised to hear a prominent mainstream American religious leader proclaim that the only biblically approved roles for women are “mother and grandmother.” Really? What happened to the role of … wife?
That glaring omission doesn’t seem to mesh with the men I encounter in my counseling office or out in the real world. These men would like to have their wives back. Their secret shame? A father feeling resentful or even jealous of his own kids, knowing that
30 MD-UPDATE
MENtAL WELLNESS
they mean more to his wife than he does. The displacement of the husband as his wife’s primary emotional bond is men’s most-cited slippery slope into an unhappy marriage.
In “therapy world” we say that the strength and stability of the family system depend more than anything else on the husband-wife bond. My take? I don’t know if we can or should try to override that maternal instinct too early in our children’s lives. Instead, my concern kicks in when the maternal bonding pattern gets stuck in overdrive and subtly destabilizes the marriage, making the entire family system more fragile.
So, is it possible for mothers to find a way to extend into ordinary life situations the airline industry adage — to put on your oxygen mask before trying to help your child (or anyone else, for that matter)? It’s a big undertaking, but it’s important that we persist.
chunks. So my focus right now is on this particular slice of the parenting pizza:
1. Husbands who are looking for ways to reclaim their “I come first” place in the hearts of their wives and
2. Wives who realize that, while they have very real systemic societal issues to navigate, the place to start is with the voice of their own “Inner Patriarch.”
Adventures with the Good Mother Archetype.
Here are my three most surprising discoveries (so far) about the Good Mother archetype:
1. It’s not about “freeing yourself” from the Good Mother archetype. We absolutely need that evolutionarily-evolved part of women to keep functioning, just as it is.
2. Relief from what I call the Too Good Mother doesn’t involve judging or trying to fix, change, or get rid of this part of
Your Inner Feminist may not be of
as much help as you think in making progress with your Good Mother. (For now, you’ll have to trust me on this. It will require another article to dissect why.) Mothers and adult-child estrangement and the “wine mom” movement are both weighty enough issues to deserve their own articles as well. So stay tuned!
It’s more about how to gently pry your Good Mother’s fingers off the steering wheel of your life and shift her into the passenger seat, so you can freely choose to channel her energy in just the right amounts for the right reasons. And let her voice take its place among the other worthy committee members in your head. In other words, it gets a little more democratic between your ears, so there’s not just one voice that’s heard and only one vote that counts when making decisions.
Next Up? The Good Enough Mother. Look forward to hearing more about this fascinating variation of the Good Mother in future articles!
more control
At ProAssurance, we work to protect medical professionals and support their patient safety efforts with custom healthcare professional liability insurance solutions.
If a malpractice claim is made, we listen and provide experienced counsel, bringing clarity and fair treatment to the claims process.
Healthcare Professional Liability Insurance

ISSUE #136 31
HEALTHCARE PROFESSIONAL LIABILITY INSURANCE ProAssurance.com MENtAL WELLNESS
Baptist Health Primary Care Welcomes Jeevanjot Virk, MD, Family Medicine

LOUISVILLE Jeevanjot Virk, MD, has joined Baptist Health Louisville Primary Care Medical Group. Virk’s services include well visits and disease prevention, health maintenance, and care for urgent conditions. Virk’s practice is located at Baptist Health Medical Group Primary Care 11600 Main Street, Louisville, KY 40243
THE PAIN TREATMENT CENTER of the Bluegrass
THE REGION’S LARGEST FREESTANDING PAIN TREATMENT FACILITY BALLARD WRIGHT M.D., PSC
The Pain Treatment Center of the Bluegrass announces our partnership with CHI Saint Joseph Health system. As one of the oldest and largest private multidisciplinary pain centers in the region, delivering comprehensive pain care, The Pain Treatment Center of the Bluegrass will be the preferred pain management provider to all hospitals in the CHI Saint Joseph Health system. The Pain Treatment Center of the Bluegrass will now be performing its procedures at CHI Saint Joseph Health Outpatient Surgery Center.
NEUROLOGY/NEUROIMAGING
Peter D. Wright, M.D. Medical Director Director of Neuroimaging

ANESTHESIOLOGY
Ballard D. Wright, M.D. Founder and Medical Director
Dennis Northrip, M.D.
Karim Rasheed, M.D.
ADDICTION MEDICINE
Traci Westerfield, M.D.
FAMILY PRACTICE
Laura Hummel, M.D.
Marc Manley Named Executive Director of Cardiovascular Services at Baptist Health
LEXINGTON Marc Manley, MSN, RN, NE-BC, has been named executive director of Cardiovascular Services at Baptist Health Lexington.
PHYSICAL MEDICINE AND REHABILITATION
Lauren Larson, M.D.
INTERNAL MEDICINE
Anand Modadugu, M.D.
PALLIATIVE CARE
Christopher Lyon, M.D.
BEHAVIORAL MEDICINE
Narda Shipp, APRN
Kellie Dryden, LCSW
Marie Simpson, LCSW
PHYSICAL THERAPY
Jason Goumas, PT, CSAS
PHYSICIAN ASSISTANTS
Lois Wright, MBA, PA-C
Celeste Christensen, PA-C
Shari Pierce, PA-C
Jing Ye, PA-C
NURSE PRACTITIONERS
Becky Moore, APRN
Teri Partin, APRN
Lynne Shockey, APRN
Dijana Duval, APRN
April Luttrell, APRN
Tabitha Knight, APRN
LEXINGTON: 2416 Regency Rd. SOMERSET: 110 Hardin Ln., Ste. 4 (859) 278-1316 ext 258 (859) 276-3847 pain-ptc.com
During his career, Manley has held numerous healthcare leadership roles in community health systems, academic medical centers, and EMS/air medical operations. Other roles have included critical care transport nurse with Central Baptist Hospital and chief flight nurse for air medical programs in Kentucky and Georgia.
Manley earned his MSN with a focus in executive leadership and BSN from Chamberlain University. He is board-certified as a nurse executive. His passion is team development, nursing leadership development, and creating an environment of transparency and collective focus.
Leigha High, MD, joins Baptist Health OB/GYN

LEXINGTON Leigha High, MD, has joined Baptist Health Medical Group OB/GYN, located at 1700 Nicholasville Road, Suite 702 in Lexington.
High is a graduate of East Tennessee State University James H. Quillen College of Medicine and completed her Obstetrics and Gynecology residency at the University of Florida College of Medicine at Jacksonville. She is a member of the American College of Obstetrics & Gynecology and the American Association of Gynecologic Laparoscopists.
32 MD-UPDATE News
PHOTOS PROVIDED BY BAPTIST HEALTH
Chioma Chinelo Nwagbara, MD, Joins CHI Saint Joseph Medical Group in London Cardiologist brings international experience to medical team

LONDON Chioma Chinelo Nwagbara, MD, has joined CHI Saint Joseph Medical Group – Cardiology in London, specializing in percutaneous coronary intervention. Growing up, Nwagbara witnessed her father’s passion for the medical field. As a physician himself, his joy for his work inspired her to pursue her own dream of becoming a doctor.
Nwagbara received her master’s in public health with an emphasis in biostatistics at the University of North Texas. She received her medical education at the University of Nigeria Enugu campus. Nwagbara also received the recognition of being a Biostatistics and Evaluation Services Training scholar from the University of North Texas Health.
Professionally, Nwagbara has performed research for the University of Alabama at Birmingham and the University of North Texas. She has also worked as a physician for the Institute of Human Virology, Nigeria.
“During my medical residency, I had the chance to experience what’s called a catheterization laboratory,” says Nwagbara. “Essentially, this an examination room where doctors find potential artery abnormalities. I was intrigued with how a visit to this lab could change the trajectory of a patient’s illness and treatment. This began my interest in cardiology intervention.”
Nwagbara is accepting new patients and will practice at 1025 Saint Joseph Lane in
London. To make an appointment with Dr. Nwagbara, visit www.chisaintjosephhealth. org or call 606.864.4040.
Fred Odago, MD, Joins CHI Saint Joseph Medical Group in Lexington
After a decade of scientific research, Odago joins local neurology team

LEXINGTON Fred Odago, MD, has joined CHI Saint Joseph Medical Group in Lexington as a neurologist. Growing up, Odago says he was subliminally influenced into the medical field by his uncle, who was the family’s first physician. Odago eventually became a medical researcher; however, 10 years later, he entered medical school. The change of heart came after he realized he would have more of an impact as a physician in a clinical setting, rather than as a basic scientist within a lab.
“I was a nontraditional student when I went to medical school,” says Odago. “I’d done a lot of research, and at that point realized I was
ready to go into clinical practice. In medicine, I’m able to see the impact of medical research on patients directly. I’m still research-minded and was drawn to neurology due to the active research that is still ongoing to address neurological conditions such as ALS and because, historically, doctors are often trying to find answers that aren’t always clear.”
Odago received his medical degree from the University of Kentucky after working in research positions for a decade. Prior to employment or attending medical school, Odago was one of 30 international students from Kenya selected to attend Berea College in central
Kentucky.
Professionally, Odago has received various professional accolades including Resident of the Month from the Department of Neurology at UK, and has participated in more than 15 publications, abstracts, and presentations throughout his career.

SEND YOUR NEWS ITEMS TO MD-UPDATE > news@md-update.com ISSUE #136 33
Your
GRAPHIC DESIGN • INTERACTIVE PUBLICATIONS • PROJECT MANAGEMENT and more... www.provationsgroup.com PHOTOS PROVIDED BY CHI SAINT JOSEPH HEALTH
Source for Graphic Design since 2003
Saint Joseph Volunteer Guild Awards Scholarships to Local Students
Teens awarded for completing 75 hours of hospital volunteer work
LEXINGTON The Saint Joseph Hospital Volunteer Guild has awarded four scholarships to local students for their volunteer work at various CHI Saint Joseph Health hospitals. The four students selected are
• Annah Baldwin, a Madison Central High School graduate attending EKU;

• Rileigh Smith, a Frederick Douglass High School graduate attending UK;
• Victoria Lowe, a Bryan Station High School graduate attending Hanover College;


• Sarah Burress, a Henry Clay High School graduate attending Bluegrass Community and Technical College.

The four recipients have individually completed 150 hours of volunteering. Each student will receive a $2,000 scholarship toward their college education. For consideration, the recipients each held a 3.0 grade-point average during high school and submitted a personal essay about their interests and career goals.
“Each year we award students who exemplify the values of our organization,” says Jane Foldes, scholarship chair, Saint Joseph Hospital Volunteer Guild. “We are proud of the robust philanthropic opportunities CHI Saint Joseph Health provides to our communities and the abilities it provides to these students to pursue their careers.”
$1 Million Investment Enhances Heart Care in South Louisville
LOUISVILLE UofL Health – Mary & Elizabeth Hospital announced it has a new cardiac catheterization lab and is now providing enhanced heart care in south Louisville. With a $1 million investment, Mary & Elizabeth Hospital now has two cath labs and has expanded its team to ensure 24/7 care for heart attack patients.
“When someone has a STEMI heart attack, they need to get to the nearest cath lab as quickly as possible,” says Melisa Adkins, CEO at UofL Health – Mary & Elizabeth Hospital. “These expanded services will positively impact the lives of those living in south Louisville and beyond by bringing life-saving care closer to home.”
Expanded STEMI coverage at Mary & Elizabeth Hospital now provides around the
clock access to care that can stop a heart attack in progress. By working with EMS partners,
doctors get vital data needed to make a diagnosis while the patient is enroute to the hospital. Once the patient arrives, a special heart care team immediately transports the patient to the cath lab, allowing physicians to clear the blockage sooner.
“The additional cath lab, along with 24/7 STEMI coverage, helps our team provide lifesaving care faster than ever before, “ says Arun Ummat, MD, medical director of cardiology at UofL Health—Mary & Elizabeth Hospital. “When an EKG comes to me on my cell phone, and I determine the patient is having an acute heart attack, all I have to do is press a button and the whole team is activated.”
The new cath lab is operational and STEMI care is now available at Mary & Elizabeth Hospital 24/7.

34 MD-UPDATE NEwS
Annah Baldwin
Sarah Burress
Victoria Lowe
Rileigh Smith
Arun Ummat, MD, medical director of cardiology at UofL Health—Mary & Elizabeth Hospital
PHOTOS PROVIDED BY CHI SAINT JOSEPH HEALTH AND UofL HEALTH
Three New Physicians Join Lexington Clinic
LEXINGTON Lexington Clinic welcomed three new physicians in August 2021.

Rebekah McDaniel, DO, has joined family medicine at Lexington Clinic East. McDaniel completed a residency at St. Elizabeth Family Medicine Residency Program in Kentucky and received her medical degree from Lincoln Memorial University—DeBusk College of Osteopathic Medicine, Harrogate, Tennessee. She provides services in urgent care and family medicine, including care for minor injury and illness, diagnosis and treatment of sprains or strains, treatment of general illnesses, treatment of lacerations, and work injury treatment, labs, and x-ray.

Marina Saad, MD, has joined hospital medicine based out of CHI Saint Joseph Health Office Park. Saad completed her residency in Internal Medicine at Manatee Memorial Hospital, Bradenton, Florida, and received her medical degree from Ross University School of Medicine, Portsmouth, Dominica. She is an internal medicine physician and provides services and care for inpatients at CHI Saint Joseph Health.
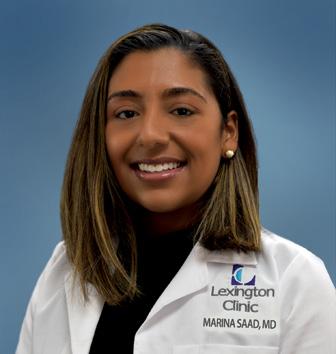

Adele Amine, DO, has joined endocrinology and is based at the main Lexington Clinic facility on South Broadway. Amine received her medical degree from the University of Pikeville – Kentucky College of Osteopathic Medicine. She completed her residency at Henry Ford in Michigan and fellowship training in endocrinology at the University of Kentucky. Amine
provides services in general endocrinology and metabolism, diabetes mellitus, obesity and lipid-related disorders, thyroid and parathyroid disorders, pituitary disease, osteoporosis and adrenal disorder. Lexington Clinic was founded in 1920

and is Central Kentucky’s oldest and largest group practice with more than 200 providers in 30 different specialties and has more than 25 locations throughout Central Kentucky. Lexington Clinic serves more than 600,000 patients every year.
Retirement Goal Line? Where
To help clients reach their goals, each member of our team has been chosen for their unique talents: responsibility, strategic thinking, ideation, empathy, achiever, futuristic, analytical, intellection, maximizer, and discipline, just to name a few. Thinking clearly. Caring deeply.

SEND YOUR NEWS ITEMS TO MD-UPDATE > news@md-update.com ISSUE #136 35
FEE-ONLY FINANCIAL PLANNING 800.344.9098 | DSNEAL.COM See how we think about money. dscottneal.com Do you know your next move? We can help!
is your
Rebekah McDaniel, DO
PHOTOS PROVIDED BY LEXINGTON CLINIC
Marina Saad,MD Adele Amine, DO

Know A Good Doctor? We Do. YOUR RESOURCE FOR THE BEST IN KENTUCKY HEALTHCARE Now available online • 90,000+ visits! www.md-update.com .com
BEING CENTERED ON YOU BRINGS OUT THE BEST IN US.
FOR 2021-22, BAPTIST HEALTH LOUISVILLE HAS BEEN RECOGNIZED as the Best Hospital in the metro Louisville region by U.S. News & World Report. Our hospital earned high-performing ratings in nine areas: abdominal aortic aneurysm repair, aortic valve surgery, colon cancer surgery, COPD, diabetes, heart attack, heart bypass surgery, knee replacement, and stroke. We would like to extend our gratitude and congratulations to the physicians, staff and volunteers who made this possible. To learn more about our nationally recognized care, visit BaptistHealth.com
BaptistHealth.com Corbin | Floyd |
| La Grange | Lexington | Louisville | Madisonville | Paducah | Richmond
Hardin



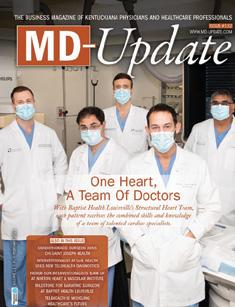








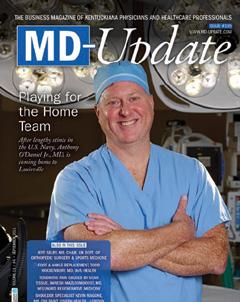

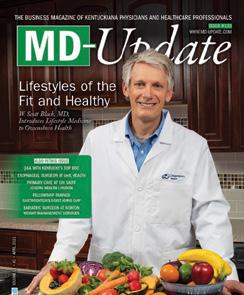
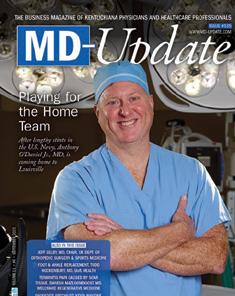







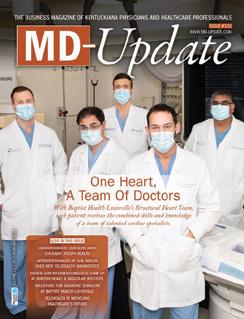
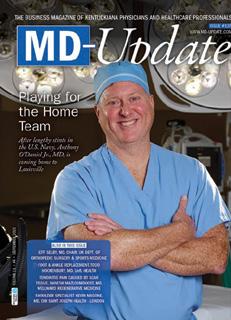
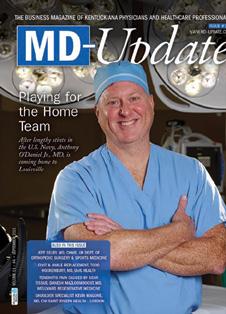







































 BY LANCE MANN, ASSURANCE DIRECTOR
BY LANCE MANN, ASSURANCE DIRECTOR



 WHITNEY JONES, MD
WHITNEY JONES, MD
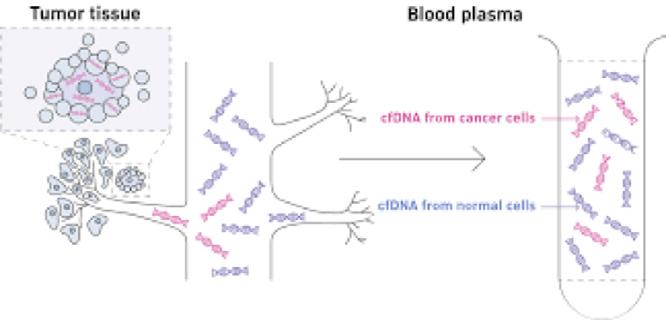


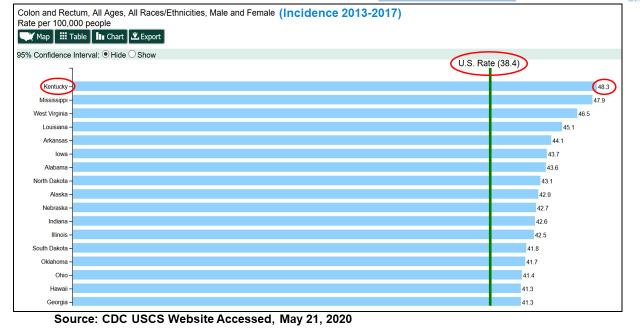
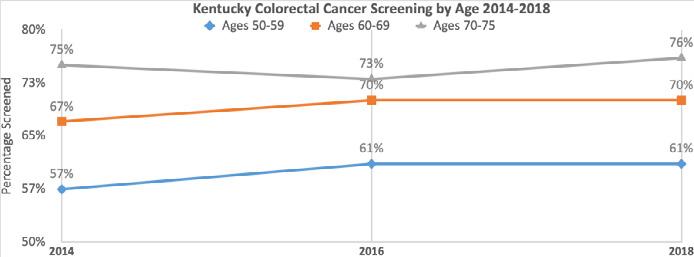
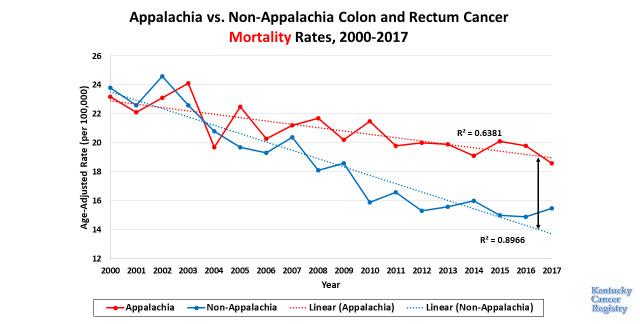
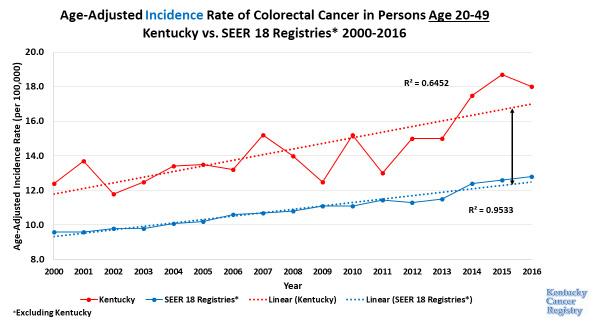
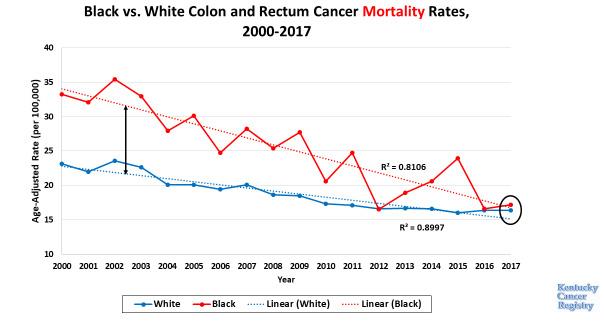


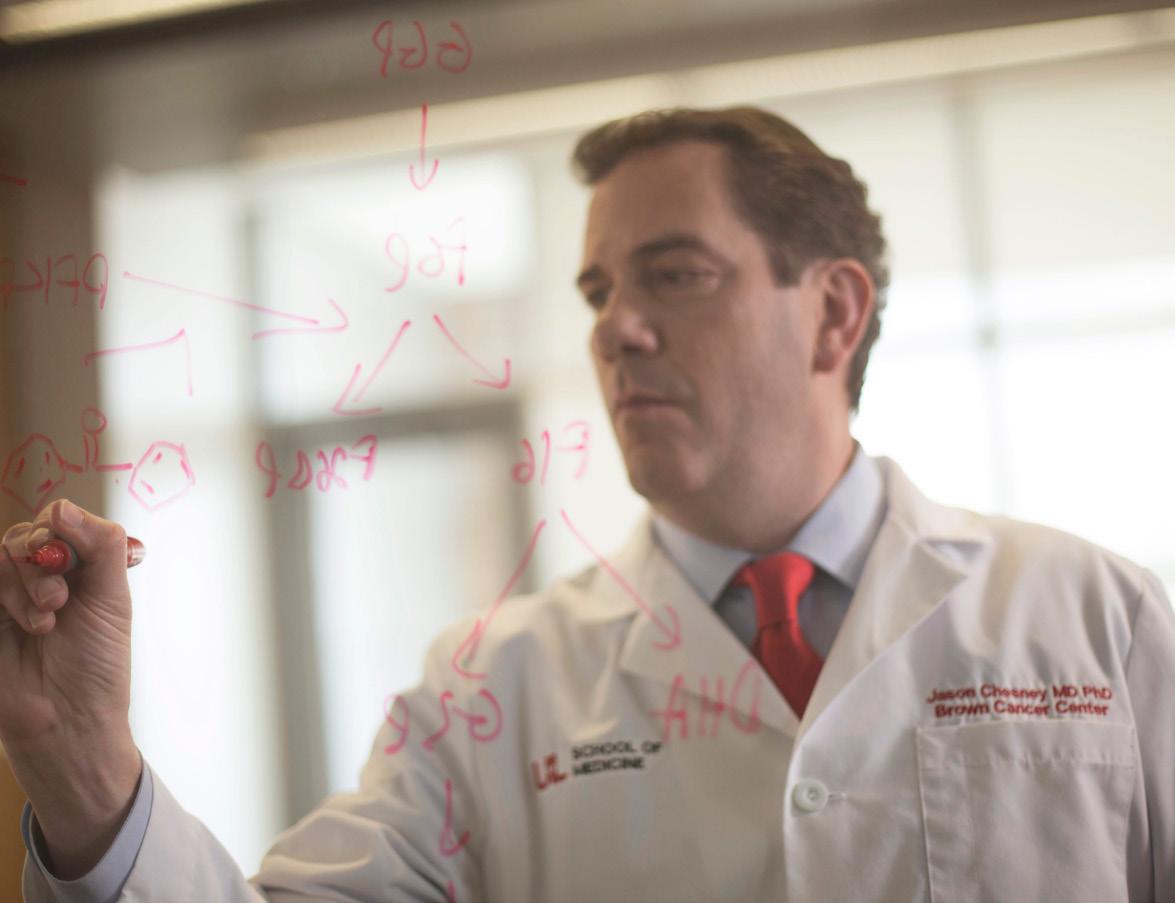



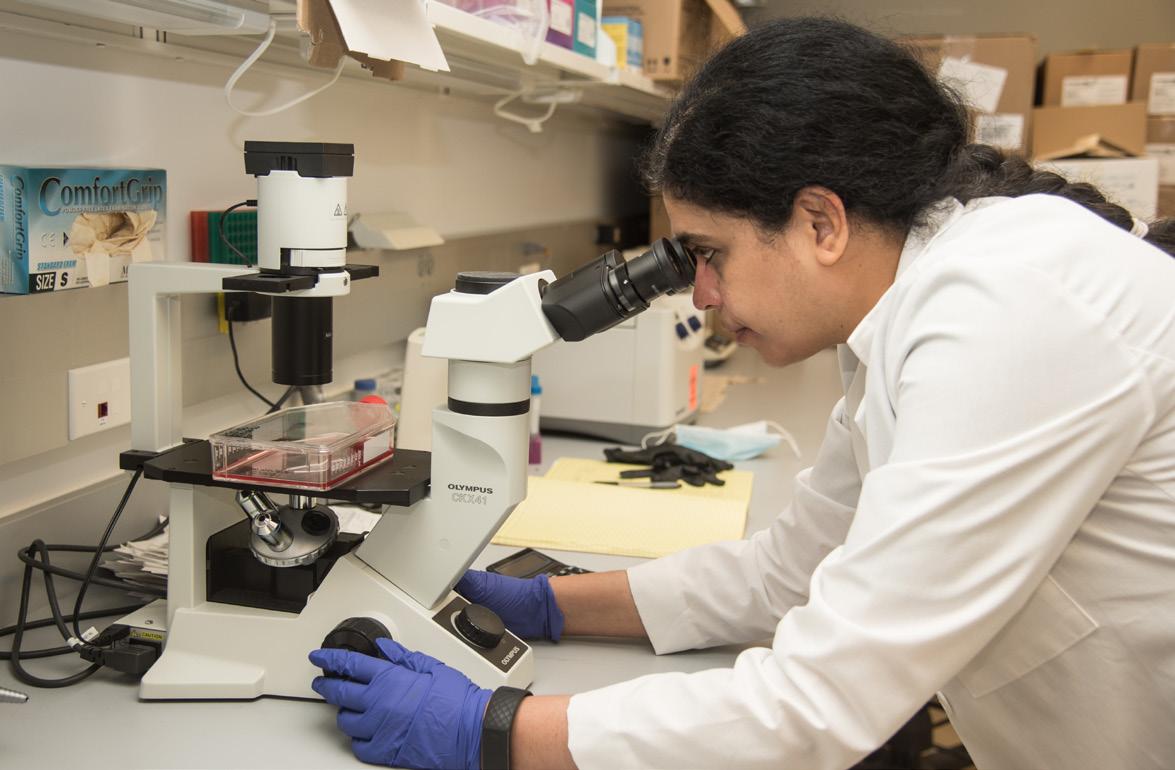



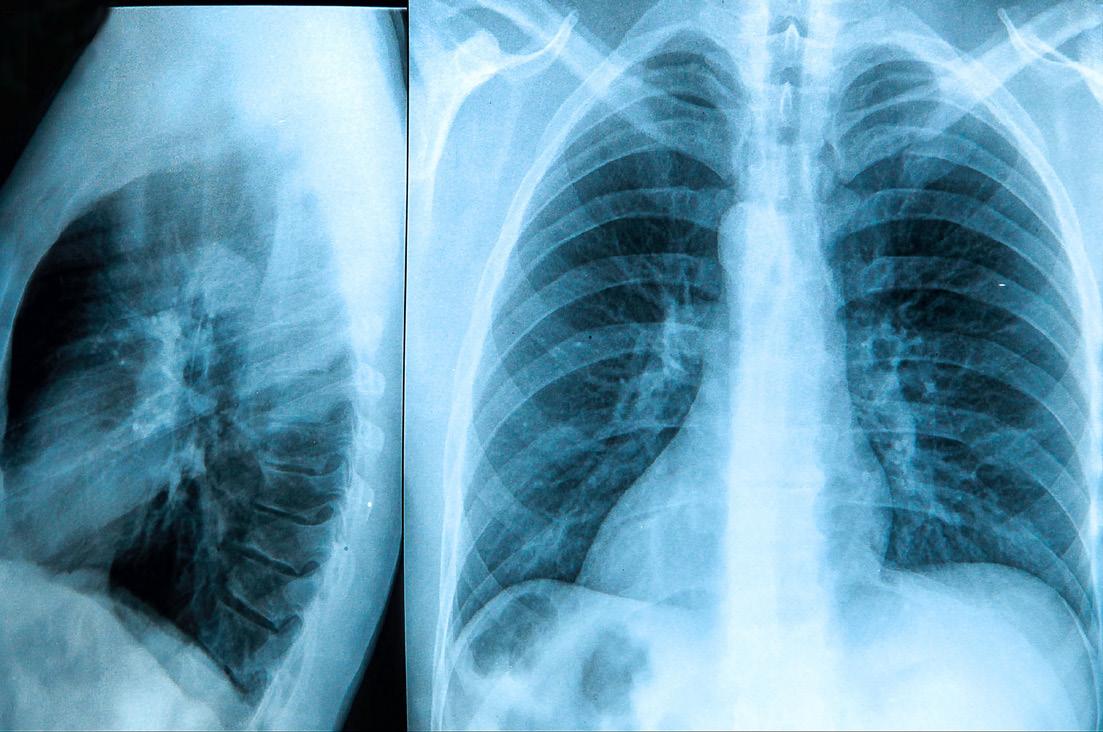


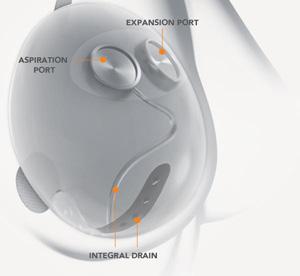














 BY DONNA ISON
BY DONNA ISON