Improving Patient Care with Useful Information
Dan Hurley, MD, discusses how big data impacts otolaryngology

COUNTY MEDICAL SOCIETY

22
Physicians across Arizona share their views on big data in medicine
Become an MCMS member
SUMMER 2023 A PUBLICATION
OF THE MARICOPA

















Editor-In-Chief
John McElligott, MPH, CPH

Managing Editor Edward Araujo
Creative Design
Randi Karabin, KarabinCreative.com
Cover & Featured Articles

Photography Ben Scolaro, scolarodesign.com
Advertising ads@arizonaphysician.com

Maricopa County Medical Society Board Members
President Zaid Fadul, MD, FS, FAAFP
President-Elect
Jane Lyons, MD
Treasurer Vishal Verma, MD, MBA
Secretary
Ann Cheri Foxx-Leach, MD, D.ABA
Directors
Kishlay Anand, MD, MS
Jay Arora, MD, MBA
David Carfagno, DO, CAQSM
Anchit Mehrotra, MD
Ruchir Patel, MD, FACP
Rahul S. Rishi, DO, FAAAAI, FACAAI
Karyne Vinales, MD
Resident & Fellow Director Krishna Pulivarthi, MD
Medical Student Director
Sarah Carpinelli, OMS-IV
10 Big Data and Diabetes Care Shakaib Rehman, MD, of the Phoenix VA, shares how big data helps endocrinology. 12
HealthyU Clinics Leverages Data for Improved Patient Care Shane Speirs, MD, and his team built systems that embraced value-based care. 22 In Depth: Heart and Vascular Center of Arizona Nathan Laufer, MD, discusses how cardiologists leverage RPM devices. CONTENTS 4 | From the MCMS Board President 6 | From the Editor-in-Chief 7 | MCMS Partner Program 8 | Briefs 18 | What Arizona Docs are Saying 26 | Legal Corner 28 | How To 30 | Physician Spotlight IN EVERY ISSUE 14 COVER STORY Daniel Hurley, MD, President and Chief Medical Officer at Valley ENT shares how big data can improve patient care.
How
VOLUME 5 • ISSUE 2 Digital & Social Media arizonaphysician.com ArizonaPhysician @AZPhysician @AZ_Physician B a h a r a k T a b a r s i , M D , on Treating Afghan Refugees T h a n i s V a n i g , M D , on HIV Care A l y x P o r t e r , M D , & G r e g o r y U m p h r e y , M D , on ElevateMeD C h e c k o u t t h e l a t e s t & u p c o m i n g p o d c a s t e p i s o d e s :
Augmenting the Art of Medicine

“Medicine is an art and a science.”
I heard that refrain many times while I was coming up through training. I had to learn all the science before I began to see and understand the art of medicine. In the last ten years since I finished my Family Medicine residency, there has been a total revolution in the practice of medicine. This has come on many fronts, from dramatic breakthroughs in multiple cancer drugs to robotics integration in surgery and virtual delivery of medical care. The biggest disruption in medicine is still being felt in myriad ways and that is the effect of the business of medicine and its drive for efficiency and scale. The key to this transformation has been incorporating big data and technology.
One of the lessons I learned at Harvard was that most providers get distracted by technology and its incorporation into their practice. Many of us make EMRs central to our work and typically devote twice the amount of time to data entry versus patient engagement. We over-rely on imaging and advanced testing at the expense of our hands-on clinical skills. These and many other innovations certainly have a valuable role to play but, on some level, we are all guilty of over-relying on these technologies. The first time I realized that was on a clinical rotation in Indonesia as a second-year resident. I might have had a small panic attack when I realized that UpToDate wasn’t accessible on my phone due to the lack of stable Wi-Fi.
The challenge now is incorporating big data and eventually AI in a way that augments our workflow without replacing or distracting it. Many fellow physicians share the frustration and confusion of how to incorporate an ever-expanding menu of technologies into our practice without losing touch with the art of medicine. We begin to feel like we are glorified data entrants. I believe the key is not building our workflow around technology but incorporating technology to facilitate our workflow.
An example is the Prescription Drug Monitoring Program that states use to track controlled substance prescriptions. Many EMRs have incorporated a PDMP check into their platform, allowing physicians to monitor for abuse and diversion of narcotics, benzos, etc. Having front office staff access this information and flag aberrant behavior to the provider at the time of the visit is a good way to utilize this technology. Another example is Remote Patient Monitoring devices, excellent tools to monitor relevant vitals outside the office. The problem is how to manage the deluge of data that can be generated. Building a system to identify important deviations in real time and notify staff would save a lot of extra work. The key is finding the right partners and systems to integrate.
The take home point here is that each physician’s practice is unique. We should strive to incorporate useful technologies into our workflow while keeping the doctor-patient engagement central to our day. Every time I incorporate something new, I ask myself, “Is this saving me time and expanding my ability/quality of practice?” Only you can answer that question. The challenge here is to keep asking it.
Respectfully,
Zaid Fadul, MD, FS, FAAFP MCMS Board President
Dr. Zaid Fadul's focus in medicine has been on improving patient outcomes and building better care delivery systems. He is Board Certified in Family Medicine and Addiction Medicine. He also has the privilege of serving in the US Air Force Reserve as a Flight Surgeon, where his training is focused on Occupation and Aerospace Medicine. He currently serves as the Chief Medical Officer for Steady Hand Medical and the President of the Maricopa County Medical Society. Dr. Fadul has traveled extensively as a photographer and is proficient in Spanish and conversational Arabic. His proudest moments come as a father of three with a loving and supportive wife.

4 n ARIZONA PHYSICIAN MAGAZINE
FROM THE MCMS BOARD PRESIDENT
Interested in getting involved with MCMS? Reach me at mcms@mcmsonline.com
THERE’S STRENGTH IN NUMBERS
Advocacy
Pushing policies that matter
Professional Referrals
Legal, financial, staffing, real estate, etc.


Scan to learn more about the benefits of being an MCMS member
Patient Referrals
Online directory and referral line



Physician Stories

Print and digital magazine, podcast
Networking
Happy hours and fun events
CME
In person and virtual
In 2014, the federal government required the adoption of EMRs for public and private healthcare organizations. Data exploded in volume a nd the growth of healthcare data today continues to outpace many industries.
Physicians want systems that seamlessly and securely share data and present only the relevant information in a way that is easily understood and helps the medical team to make the right decisions and present options to patients when needed. The reality is quite different.
BIG DATA IN MEDICINE
We go in depth with Nathan Laufer, MD, of Heart and Vascular Center of Arizona. A past president of the Maricopa County Medical Society, the cardiologist believes “cardiac care has improved greatly with all the monitoring data we now have available.” That’s especially true for heart monitors or loop recorders that can detect infrequent rhythm disturbances. Still, Dr. Laufer yearns for a better balance between some data that informs and most of today’s 10 to 15-page note, most of which he finds to be junk.
Shane Speirs, MD, MBA, President and Chief Medical Officer at HealthyU Clinics, shares how they leverage data at the primary care-centric multi-specialty organization. They try to avoid an overreliance on algorithms. Dr. Speirs writes, “While technology can be a powerful tool in healthcare, it is important to remember that it is not a substitute for human expertise and judgment. Algorithms and machine learning models are only as good as the data they are trained on and may not be able to account for all the nuances of a patient’s unique situation.
According to survey respondents in What Arizona Docs Are Saying, a slight majority (54%) of physicians believe their practice, clinic, or hospital leverages big data to improve care. More physicians (73%) say their EHR system leads to improved care. Fewer survey respondents believe medicine has improved with greater use of big data (4.4 average on a scale of 0 to 10).
Mandeep M. Sahani, MD, goes under the spotlight. As founder of Desert Kidney Associates, Dr. Sahani sees
nephrology as a data-driven specialty. He says, “There are calculations to establish if that individual is going to progress downward towards worsening CKD, perhaps requiring dialysis or a kidney transplant. Data helps us to forecast, and risk stratify.”
We asked Shakaib Rehman, MD, to explain how data can help diabetic patients. The Associate Chief of Staff for Education at Phoenix VA Health Care Systems details how wearable technology, retinal imaging, predictive analytics, and precision medicine apply to diabetes.
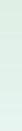
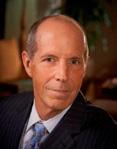
DR. DAN HURLEY

Dan Hurley, MD, President and Chief Medical Officer at Valley ENT, says that, “Having the ability to know more about my patients before they show up allows me to better help them.” Our Managing Editor Edward Araujo writes that Dr. Hurley is concerned about data privacy, fearing HIPAA violations from poor access control policies, device theft, or the failure to encrypt and secure data.
VALUABLE ARTICLES
In Legal Corner, lawyers Bob Milligan and Karina Shipman of Milligan Lawless write about how the Federal government uses big data in predictive models to identify potential investigative targets for billing fraud.
Joshua Flake of Practice Pathways, National Bank of Arizona, shares tips for the process of buying into a practice. He highlights some benefits to both the buyer and seller.
Contact us at info@arizonaphysician.com with any comments or suggestions.
Enjoy the magazine.
By John E. McElligott, MPH, CPH
6 n ARIZONA PHYSICIAN MAGAZINE
Not an MCMS member? Visit mcmsonline.com/join or call us at (602) 252-2015. FROM THE EDITOR-IN-CHIEF
“THE GOAL IS TO TURN DATA INTO INFORMATION, AND INFORMATION INTO INSIGHT.”
—Carly Fiorina, ex CEO of Hewlett-Packard
WHAT IS THE PARTNER PROGRAM

Maricopa County Medical Society’s Partner Program is designed to introduce select companies to our members. MCMS strives to facilitate physician growth in all areas of their life and practice. As we work to support our members, we think there are excellent opportunities to work closely with business partners that can facilitate that growth.
Learn more at mcmsonline.com/ partner-program
Provista is a group purchasing powerhouse that has helped over 150,000 physician practices to reduce supply chain costs and streamline their procurement processes. Provista groups your purchases with all their members’ purchases to negotiate the absolute best price from the nation’s top suppliers. All the products and services you need to operate day-to-day, Provista has that covered. With Provista, there are no commitments or membership fees. With more than $135 billion in purchasing power and strong relationships with the top distributors and suppliers in the nation, Provista can deliver low prices on contracts and services to practices just like yours. Provista negotiates and implements contracts, creates unique savings programs, provides custom analytics, and connects members to an extensive network of suppliers. On top of that, they tap into a suite of services including procurement solutions, advanced analytics, and no-hassle contract implementation.

STRESS-FREE
A snapshot of the Provista extensive portfolio of products and services:
FedEx Medline
Cardinal
UMF
Midmark


McKesson
Henry Schein
Baxter
Smiths Medical



3M
Kimberly-Clark
Ecolab
AT&T
Verizon
Stericycle



Taylor Healthcare
Thryv Airgas

Lyft Staples Philips
GE
Siemens
Novaplus BD
Bayer Carrier
Trane
GROUP PURCHASING
Products & Services:
Pharmacy
Medical/Surgical

Purchased Services
Capital Equipment
Laboratory
Physician Preference
Items
TECHNOLOGY & PROCUREMENT
Envi® Materials



Management Software
OPERATIONS
Custom Analytics








Cost Savings Analysis
Benchmarking
Contract
Implementation
Custom Contracting
7 ARIZONAPHYSICIAN.COM
DISCOUNT PARTNER
GPO-ING. It’s kind of our thing.
Cool Indoor Activities for the Entire Family During the Summer
As hot weather hits Phoenix metro, here are some great indoor activities you can do by yourself or with your entire family.
ARIZONA SCIENCE CENTER
azscience.org | Discover the world of science and imagination at Arizona Science Center. Whether you’re visiting the area, or you call Phoenix home, we have something for everyone in the family to enjoy.
LEGOLAND DISCOVERY CENTER ARIZONA legolanddiscoverycenter.com/Arizona | Surround yourself with millions of LEGO Bricks, take flight on Merlin’s Apprentice, blast skeletons on Kingdom Quest ride adventure, see your favorite characters on LEGO 4D Theater, and build epic LEGO creations alongside master builders.
BUTTERFLY WONDERLAND

butterflywonderland.com | Butterfly Wonderland is the largest butterfly conservatory in America. It features a magnificent indoor conservatory that brings a tropical rainforest environment to the Arizona desert where thousands of butterflies fly freely.
PANGEA LAND OF THE DINOSAURS
pangaealandofthedinosaurs.com | Bring your entire family and enjoy over 15 dinosaurs plus exhibits, parties, and group field trips.
ARIZONA MUSEUM OF NATURAL HISTORY
arizonamuseumofnaturalhistory.org | Learn about paleontology and archeology at a great price for adults and children of all ages. You even can become a member and save on future trips to the museum.
MUSICAL INSTRUMENT MUSEUM mim.org | With over 15,000 musical instruments and associated objects, including examples from close to 200 countries and territories, the MIM has representation from nearly every inhabited continent. Come and enjoy great events, concerts and learn so much more through musical education.
FAT CATS | fatcatsfun.com | Enjoy quality food and superior entertainment or “All Out Fun,” all under one roof. With a bowling area, miniature glowing golf, and an arcade alongside a bar-style grill, there is something for the entire family.
PHOENIX ART MUSEUM | phxart.org | From art exhibits & collections, art events, to art education & workshops, there is something new and special always happening at the Phoenix Art Museum. You can enjoy the museum throughout the week or as the first stop on the First Friday tour every month.
HEARD MUSEUM | heard.org | Since its founding in 1929, the Heard Museum has grown in stature to become recognized internationally for the quality of its collections, world-class exhibitions, educational programming and its unmatched festivals. Dedicated to the advancement of American Indian art, the Heard successfully presents the stories of American Indian people from a first-person perspective. Exhibitions that showcase the beauty and vitality of traditional and contemporary art.
CHILDREN’S MUSEUM OF PHOENIX childrensmuseumofphoenix.org | One of the top children’s museums in the nation, Children’s Museum of Phoenix is a wonderful place for children ages birth to 10 to enjoy imagination, inspiration, creativity, and just a lot of fun. There are over 300 play experiences spread throughout 3 floors that will keep your child engaged and entertained.
BRIEFS NEWS AND NOTES FROM THE FIELD
8 n ARIZONA PHYSICIAN MAGAZINE
Top Foods that Help Reduce Inflammation
















Persistent and chronic inflammation can lead to many diseases such as cancer, heart disease, diabetes, arthritis, and Alzheimer’s. Here are five foods you should eat as part of your anti-inflammatory diet:
FRUITS | Berries, cherries, apples, pineapples, grapes, oranges, watermelon, pomegranate, grapefruit, and lemons. Through polyphenolic acids, vitamins, and minerals these fruits naturally help you fight inflammation.

FATTY FISH | Salmon, mackerel, tuna, and sardines. It is recommended you eat three to six ounce servings of these fish two to four times per week.





GREEN LEAFY VEGETABLES | Spinach, kale, collard greens. Through vitamin A, D, E, & K, and alpha linolenic acid, research shows these veggies help fight inflammation.

OLIVE OIL | The main anti-inflammatory effects from olive oil are antioxidants like oleocanthal, which have been known to work like Ibuprofen, an anti-inflammatory drug. On average, two tablespoons per day is enough.
NUTS | Almonds, walnuts. They are high in alpha linoleic acid (ALA), a type of antiinflammatory omega-3 fatty acid. Plus they are rich in magnesium, I-arginine, and vitamin E.


9
ADVOCATES FOR THE PRIVATE PRACTICE OF MEDICINE 602.792.3500 5050 North 40th Street, Suite 200 Phoenix, Arizona 85018 MilliganLawless.com Health Care Compliance Health Care Reform Business Transactions State and Federal Licensing Reimbursement Patient Privacy Fraud and Abuse Corporate Law Intellectual Property Employment Law Counseling and Litigation Estate Planning MilliganLawless_ad_half_060123.indd 1 6/1/23 1:06 PM
ARIZONAPHYSICIAN.COM
Big Data and Diabetes Care
Ever since electronic health records (EHR) were introduced, the amount of data has ballooned. The term “Big Data” was coined to describe the huge amount of data being collected, stored, and analyzed. Big data has been impacting all facets of health care including diabetes care. Diabetes Mellitus (DM) is one of the most common diseases that leads to high mortality and many morbidities such as blindness, heart attacks, strokes, kidney failure, leg amputations, nerve damage, etc.
Big data can help in delivering personalized care, improving patient outcomes, and possibly even preventing complications. Big data is proposed to improve the quality of life for patients, reduce disability from conditions and save cost—especially when it comes to chronic conditions such as diabetes.

Patients with diabetes produce a large amount of data. These come from outpatient visits, inpatient visits, wearable devices, and glucometers. The smartphone applications or cellular connected stand-alone devices have been exploding in use recently. These devices are connected to glucometers, flash glucose monitoring, insulin pumps and smart insulin pens. In addition, there is a plethora of wearable technology measuring daily activity, exercise, blood pressure, breathing patterns, and analyzing meal content and consumption.
For example, one of the new glucose monitoring systems allows people with diabetes to track their glucose levels in real time, with ease and without finger sticks. And when using the phone app, patients are able to manage their glucose levels. Plus, the data is easily shareable with their healthcare teams. This is just one example of how big data can transform diabetes management. Data categorization, aggregation, and analyzation can lead to better care for patients.
10
n ARIZONA PHYSICIAN MAGAZINE
BIG DATA APPLICATIONS
Retinal imaging has been used for a very long time for early diagnosis and treatment of diabetic retinopathy. Previously, ophthalmologists were reviewing these images. Now, artificial intelligence algorithms have been developed to have these images reviewed faster and more accurately. Easy-to-use retinal smartphone adapters using AI are on the horizon and will be used in the home setting and easily transmitted remotely to a central database for physicians to review.
Another application of big data in diabetes care is predictive analytics. By analyzing large amounts of patient data, including clinical data, lifestyle data, and biometric data, machine learning algorithms and artificial intelligence can identify patterns and predict which patients are at risk for developing diabetes or experiencing diabetes-related complications. This can help healthcare providers take proactive steps to prevent complications and improve patient outcomes.
Another application of big data in diabetes care is precision medicine. By gathering big data, healthcare systems and/or providers can now more quickly identify which patients would benefit from a shift in treatment, potentially preventing serious complications of chronic diseases. Such tailor-made medical treatment is called precision medicine. By analyzing large amounts of patient data, healthcare providers can identify subgroups of patients with different risk profiles, treatment responses, and underlying disease mechanisms. This can help healthcare providers tailor treatments to individual patients based on their unique characteristics, improving treatment outcomes, and reducing side effects.
IMPROVING DIABETES CARE


Overall, data has the potential to revolutionize diabetes care by providing healthcare providers with new insights into the disease and enabling personalized treatment approaches. However, there are many challenges including protecting patient privacy, safeguarding the data storage, and making sure that data is used ethically and responsibly. Another big challenge is interoperability. Data from one EHR may not be able to be captured and analyzed by another EHR system.
Recent advances in genomic precision medicine will help to identify patients at risk of developing diabetes. Individualized risk assessment can help patients manage their diabetes better. Medications are already being customized in centers where genomic medication assessment is available. Diabetic patients can have access to their past medical history and historical health recordings on a smart device. We expect that soon patients will be able to transmit retinal images and real-time health data to their medical team for guidance and advice. It is anticipated that with the help of big data tools, patients can manage their care based on their own lifestyle and personalized goals.
In summary, big data can play an important role in improving diabetes care. Diabetes is a chronic disease that affects millions of people worldwide. With the increasing availability of electronic health records, wearable devices, and other sources of health data, healthcare providers and researchers have access to large amounts of data that can help them better understand diabetes and improve treatment outcomes. ■
By Shakaib Rehman, MD, MACP, FACH, FICH, FAMIA, CSH Associate Chief of Staff for Education Phoenix VA Health Care Systems Professor & Interim Chair Department of Biomedical Informatics University of Arizona College of Medicine-Phoenix Shakaib.rehman@va.gov

11 ARIZONAPHYSICIAN.COM
How HealthyU Clinics Leverages Data for Improved Patient Care

THE CHALLENGE
Big data has become an increasingly important part of medicine in recent years. With advances in technology and the ability to collect and analyze massive amounts of data, healthcare providers can make more informed decisions and improve patient outcomes like they never have before. But how much is too much?
Are we overwhelmed by the access we have to our patient’s data? By simply having access to the data, does that make us liable if we don’t use it all to manage our patient care? Do the reimbursement models of today account for this rapid influx of information for our patients? How can we use all this data to provide the quality care our patients deserve, and enable us to take full advantage of being a valuebased care organization in the healthcare market? These are all questions we asked ourselves when we started our primary care-centric multi-specialty organization, HealthyU Clinics.
One of the challenges with big data in medicine is the potential for overreliance on technology and algorithms. While technology can be a powerful tool in healthcare, it is important to remember that it is not a substitute for human expertise and judgment. Algorithms and machine learning models are only as good as the data they are trained on and may not be able to account for all the nuances of a patient's unique situation. In addition, relying too heavily on technology can lead to a lack of empathy and personal connection between healthcare providers and patients. When we founded HealthyU Clinics and started to grow into a large multi-specialty group, we thought it was of the utmost importance to strike a balance between the use of technology and the human touch in healthcare to ensure that patients receive the best possible care. But one question remained, how do we enable our providers to use this massive amount of patient information in a way that is seamless? We wanted to develop a solution to transition our healthcare system into a next generation value-based care organization.
12
n ARIZONA PHYSICIAN MAGAZINE
THE MARKET TODAY
Our healthcare market today focuses on value-based care, as it aims to improve patient outcomes while reducing costs. The shift towards value-based care required our team at HealthyU to implement new strategies for delivering patient-centered and coordinated care across the continuum. We incorporated the use of technology by delivering a remote patient monitoring service line that allows us to monitor high blood pressure, diabetes, COPD, and weight loss. In addition, we launched statewide telehealth for patients in Arizona. Both solutions sought to enable patients to receive care remotely and providers to monitor patient health in real-time. But this was not enough. We still needed a solution that allowed us to make use of big data and analytics to tailor care to the specific needs of individual patients. We needed a system that embraced the next-generation models of care that prioritize quality and patient outcomes over volume and revenue.
THE FUTURE
The team at HealthyU developed what we like to call our ProActive Care Platform. We took every bit of data from the patient chart (lab values, vital signs, diagnoses, etc.) and packaged it into a platform that is easy to understand, and simple to use. This platform allows each provider to care for their entire patient panel, constantly identifying highrisk patients within their network, so the providers can allocate their time efficiently. The quality metric system is linked to individual patients, based on what the quality incentives are from each insurance plan, Accountable Care Organization, or Clinically Integrated Network.
HOW TO ENABLE ACCESS
HealthyU only goes so far, and we wanted everyone to benefit from our platform. By presenting all this patient data in a usable form, we now can enable providers at any organization to make use of that information to provide high-quality care to their patients.
The ProActive Care Platform is available through our partner company, Adageis. We see it as our job to enable clinicians to fully make this transition to value-based care, and that’s exactly what we have done. ■
By Shane Speirs, MD, MBA President and Chief Medical Officer at HealthyU Clinics Shane.Speirs@healthyuclinics.com







13 ARIZONAPHYSICIAN.COM
Questions? Contact us. A world-class healthcare center serving the Southeast Valley 1840 & 1910 S Stapley Dr, Mesa, AZ stapleymedicalcenter.com Perry Gabuzzi, CCIM 602.513.5116 perry.gabuzzi@kidder.com Rachael Thompson 602.513.5122 rachael.thompson@kidder.com 2-story Lobby entrances with high-end finishes 181,899 SF Medical office with suites ranging from 1,200 to 21,000 SF ±2M SF Retail amenities within 1/4 mile of the property Brand new Courtyard with seating areas & shade structures Signage rights and exterior loaded suites available Generous tenant improvement packages available
Improvivng Patient Care with Useful Information

14 n ARIZONA PHYSICIAN MAGAZINE
Is there too much data available in medicine? “There should not be,” states Dr. Dan Hurley. “Having the ability to know more about my patients before they show up allows me to better help them.”
“Big data is an amorphous term,” he says. Big Data can describe many things but looking at the data in the health records systems, one of the challenges is that there isn’t always a shared platform to the data that physicians access. The lingering question is why does big data matter? It should allow physicians to learn more about their patients before, during, and after visits.
Most proponents of big data in medicine, like Dr. Hurley, believe that having the ability to gather, process, and analyze quality information will help them to diagnose their patients better. Do proponents of big data see problems now or on the horizon? Of course, they do, yet the risk is worth the reward of providing better answers to patients for treatment or, more importantly, for preventative medicine in the future. Even so, there are those against more access to patient data because of privacy issues, the inability to break down large amounts of data properly, and high costs.
A CAREER IN OTOLARYNGOLOGY

Dan Hurley, MD, began his medical journey believing he was going to be a pediatrician. After learning more about the ear during ENT rotations, he chose to become an otolaryngologist. He would go on to graduate from St. Louis University School of Medicine in 1996. Then, he completed both his internship and residency at St. Louis University Hospital. During medical school, he met his future wife, and with her parents living in Arizona, he decided that was where he would practice medicine.
Dr. Hurley began by teaming up with a more seasoned ENT physician. After a few years, they went their separate ways, leaving Dr. Hurley as sole practitioner. He believes
that collaboration and compromise are vital in running a medical practice successfully. He decided to team up with seven other practices to form Valley ENT in 2007. The group now has over 21 locations, 41 physicians, 5 physician assistants, and 21 audiologists.
Dr. Hurley is the President and Chief Medical Officer at Valley ENT and is currently in law school. Being an administrator “has taught me to listen more and to take something from every situation,” states Dr. Hurley. He focuses more on seeing pediatric ENT patients at this point in his career.

Dr. Hurley currently suffers from a disability that stops him from having a full-time schedule. In 2022, after nearly six months of being in pain, Dr. Hurley was diagnosed with chondrosarcoma in his pelvic bone. He had a hemipelvectomy with reconstruction with a 3D printed implant and artificial hip. His experience as a patient helped him improve on the way he cares for patients at Valley ENT and even inspired him to go to law school.
VALLEY ENT AND BIG DATA
How does an ENT multi-location medical practice leverage big data? Dr. Hurley and his team use electronic records in the form of eClinicalWorks. This has a portal for communication and a function (Healow Insights) that allows the physicians to access external data such as visits outside the practice, diagnosis, clinical impressions, and lab work performed. The degree of shared data is still limited but hopefully will continue to improve over time. They also use clearinghouses like Innovation Care Partners, which
15 ARIZONAPHYSICIAN.COM
“There is just too much data, making physicians ask themselves if they are using data to work for them or are they working for data. There is no easy button that configures the most pertinent data to each patient or physician’s needs.”
offers a database of information from laboratories, imaging facilities, and hospitals.
Yet, these databases aren’t always easy to use. Sometimes, he says, “There is just too much data, making physicians ask themselves if they are using data to work for them or are they working for data. There is no easy button that configures the most pertinent data to each patient or physician’s needs.”
Valley ENT also gathers and shares data through their EMR apps and portals, which allow medical staff the opportunity to communicate directly with patients. Although Dr. Hurley still finds them somewhat clunky, these apps and portals have improved in the last decade and should continue to do so.
Dr. Hurley likes to emphasize the camaraderie between medical providers at Valley ENT. He says, “Everyone provides value and has a voice on the team, from the front and back office to the audiologists to the physicians.”

MAKING SENSE OF IT ALL
Dr. Hurley believes that more patient information is valuable but only if we can make sense of it. He believes that may be achieved in the future through machine-learning techniques and artificial intelligence, which could help sift the massive amounts of data into something more pertinent and usable physician-patient interactions. Learning health systems will hopefully revolutionize medical practice through the reallocation of resources, such as clinical staff having time to do other tasks and giving more time and guidance for physicians to accurately diagnose complex diseases. Once we have the systems using the data to allow more direct physician-patient interaction, we will be headed in the correct direction.
There is plenty of room for improvement, especially when it comes to electronic medical records. Dr. Hurley wants to see more standardized platforms that talk to each other more freely and securely. He feels that EMRs should either be a public utility regulated by the government or a private system that all physicians can access as needed across platforms.
It’s not all rosy or smooth sailing ahead. Dr. Hurley is concerned about privacy issues
16 n ARIZONA PHYSICIAN MAGAZINE Learn more on Dr. Hurley's thoughts on big data at arizonaphysician.com/dan-hurley-md
On the Personal Side with Dr. Dan Hurley

Q: If you could describe yourself in one word, what would it be?
A: Persistent
Q: Do you have family? Pets?
A: I am the 5th of 6 children. I am married to Traci who is a pediatrician. We met in med school. We have three children (ages 22,20,17). The oldest two want to go to med school.
Q: Do you have a hidden talent most people would not know about you?
A: I am better than average at driving in reverse.
Q: What career would you being doing if you were not a physician?
A: Process improvement, my dream job previously was to go into an organization and work/shadow every position in the company for a couple weeks and then try to harness the "inside knowledge" of every position to optimize the organization. After my recent experience in medicine as a patient, I am working hard to bring transparency and accountability to the medical decision making that causes denial and care delay on the insurance side. That is my impetus for studying law.
Q: What book are you reading right now, or recently?
A: Two books. Can't Hurt Me by David Goggins, and After the Ivory Tower Falls by Will Bunch.
Q: What is your favorite movie?
A: Cool Hand Luke as a movie in general and one of the best movie quotes of all time: "What we have here is a failure to communicate."
Q: What is your favorite food?
A: Chicken Wings
Q: What is your favorite local restaurant?
A: Spinatos

Q: What is your favorite activity outside of medicine?
A: Hiking but my fake half pelvis has put a bit of a damper on that. I also love watching my kids play basketball, but they have almost grown out of that.
and HIPAA violations with big data, as well as the ongoing need for information security across platforms. Optimizing the sharing of data for patient care can raise concerns as to whether this information could be used to affect insurability. As data grows exponentially this becomes more challenging.
IN CONCLUSION
As a physician, Dr. Hurley has a positive perspective of the three Vs of big data, namely volume, velocity, and variety. He sees the evergrowing volume of data about his patients, the velocity at which data are processed, and the wide variety of data that Valley ENT analyzes. The ability to share information to help patients is much better than it was 10 years ago but we need to get the information more effectively sorted so it can be used to bring the personal nature back to the physician-patient relationship as opposed to having physicians staring at screens during appointments.
Becoming a patient provided Dr. Hurley with a different perspective on how valuable data sharing across practices can be in optimizing patient care. His physicians are leveraging information to provide him with high quality care. The experience set a new bar of excellence that he wants all physicians to emulate. He places a high value on collaboration, compromise, and building relationships with fellow physicians, other clinical staff, his patients, and his own doctors. ■
By Edward Araujo Managing Editor Arizona Physician earaujo@mcmsonline.com

17 ARIZONAPHYSICIAN.COM
What DOCS Arizona are Saying
Does your practice, clinic, or hospital leverage big data to improve care?
For a big hospital system, I would say we are still in our infancy with this. —David
Shprecher, MD
As a strong proponent of and early adopter in regenerative orthobiologics medicine. I’m using “big data” through registries of treatments, doses, outcomes to best guide my own treatment plans. For example, the type of platelet rich plasma (dose, total number of platelets, concentration of platelet above baseline, neutrophil rich or poor), where and when to inject, how to optimize the patient before and after the injections. This is about precision medicine at its best and sharing data with others in this space is crucial in advancing the field, especially when it’s a “wild west” of unscrupulous players who are unqualified and using not legal substances in their quest for money over patients.
—Tammy Penhollow, DO
Running reports of missing gaps of care, patients who have not followed up, patients who are due for screening and immunization, etc. —Ching Wang, MD
We contribute to the American Academy of Ophthalmology Iris Registry. —Robin Demi Ross, MD
Yes 93%
If so, how?
Through continuity and coordination of care.
—Donald Toatley, MD
We use EMR tools to highlight best practices. —Michael Underhill, DO
For data compilations and bi-monthly meetings. —James Carpenter, MD
We use the National Trauma Data Bank (NTDB). —Helen Markowski, MD
We don’t, but our EMR and practice management systems sell our data for money.
—Robert Cravens, MD
Data on no-shows, outcomes, completeness of records, provider productivity and other measures are tracked to impact efficiency and quality of care.
—Michel
Sucher, MD
American Academy of Ophthalmology IRIS Registry helps ophthalmologists leverage useful live data to support clinical outcomes. —Jeffrey Edelstein, MD
We are utilizing a self-service analytical tool inherent in our EMR, which allows users to slice and dice large data sets to perform clinical inquires and explore research opportunities.
—Anthony
Dunnigan, MD
We look at every aspect of the healthcare experience to deliver the right care at the right time at the right place. —Richard Dobrusin, DO
Use claims data to identify patterns in care & care gaps; integrate clinical & survey data.
—Anita Murcko, MD
No 32% Yes 54% I Don’t Know 14% Read more by visiting arizonaphysician.com/docs-big-data 18 n ARIZONA PHYSICIAN MAGAZINE
Does your electronic health record (EHR) system lead to improved care?
Average = 4.4
How can medicine benefit from big data?
Accurate and timely diagnoses. —Donald Toatley, MD Research. —Edward Taxin, DO
If the data is delivered and coalesced into meaningful use, it can help paint an accurate picture of the current clinical state of a patient or healthcare delivery system.
—Michael Underhill, DO
Individual physicians, especially those in small private practices, can pool their data with other similar practices to achieve a greater “N” and allow us all to glean from the information and take that back to our practices.
—Tammy Penhollow, DO
Analytics. Machine based learning and it can create algorithms. —David Carfagno, DO
There is certainly the potential for more evidencebased decisions, but there is also the potential for overwhelming amounts of data, with “signal to noise” loss and the potential for patients to misuse data from personal trackers, which I see daily in practice.
—Melanie Cloonan-Schulte, MD
Monitor for trends in prescribing or ordering that are harmful or wasteful of resources. —David Shprecher, DO
There needs to be better attention to the consistency, quality and accuracy of clinical information entered to EHRs. I think right now “big data” is at risk of being “garbage in, garbage out.” —David Saperstein, MD
Assists with patient population health management and which patients need more attention to care.
—Ching Wang, MD
Collectively reviewing data and providing patients with the data to make informed choices. —Robin Demi Ross, MD
Lots. But currently it only benefits pharma, insurance, and hospitals. —Robert Cravens, MD
It can improve quality of care, outcomes, and practice efficiency. —Michel Sucher, MD
Get rid of government mandates and allow private businesses and health care researchers to grow the databases that provide useful solutions to practice management and patient interfaces. This will promote clinically useful documentation instead of endless useless bullet points. Jeffrey Edelstein, MD
The ability to quickly transform large amounts of data into knowledge at key points in the patient’s journey, including at the bedside or in the exam room, is a significant gamechanger. —Anthony Dunnigan, MD
Statistical tracking. Cleanliness of claims.
—Richard Dobrusin, DO
Focus efforts on your community. —Helen Markowski, MD
Image interpretation in radiology & pathology, drug development, drug safety and efficacy, better primary and secondary prevention by integrating disparate data sources, true precision medicine that integrates environmental, genetic lifestyle and other factors to tailor care, care delivery systems optimization for operations and resource utilization, alternate payment strategies and dependable algorithms for real-time patient monitoring.
—Anita Murcko, MD
Zero
Yes 73% No 27 %
On a scale of 0 to 10, indicate how much medicine has improved with greater use of big data.
equals no improvement and 10 equals extraordinary improvement.
19 ARIZONAPHYSICIAN.COM
Adequate documentation.
—Donald Toatley, MD Security. —Edward Taxin, DO
It’s not delivered in a meaningful way to help the clinician make needed changes. It’s just data without intent.
—Michael Underhill, DO
If big data is paid for by insurance companies or pharma, I am very suspicious about the intent and the conclusions. Both are extremely corrupt, and profit driven. With CEOs of 5 of the insurance companies making >$20m/year, we can easily conclude that the company focus is not the best interest of patients (or physicians), but rather on their bottom line.
—Tammy Penhollow, DO
The loss of privacy. Big data will be used by insurance companies to cut care and save money. —Jeffrey Taffet, MD
Too much focus on details with loss of big picture and data may not always be accurate. Patients may overrely on this and try to function as their own doctors, using this data in ways it should not be used and failing to consult professionals.
—Melanie Cloonan-Schulte, MD
EMRs, particularly CERNER, are so poorly designed those clinicians (at least on the outpatient side) are not able to utilize it effectively. This leads to a “garbage in, garbage out” phenomenon where so much of the data in the chart is in error or redundant. It is very difficult to accurately measure trends or do population level research. Furthermore, each hospital system has a very long way to go to make its data interoperable in a way that can screen out duplicates between systems. It is a complete mess. As a clinician we rarely have all the patient’s data in one place or feel confident that we do.
—David
Shprecher, DO
There needs to be better attention to the consistency, quality and accuracy of clinical information entered into EHRs. I think right now “big data” is at risk of being “garbage in, garbage out.” —David Saperstein, MD
Accuracy. —Ching Wang, MD
I’m always protecting the patient’s identity. Data being used by insurance companies to create decreased access to care like preventing sight saving cataract surgery. —Robin Demi Ross, MD
I feel like a college athlete. Taking all the risk, doing all the work, and getting no reward for the collection of the big data. We need a program just as they have instituted at the NCAA. —Robert Cravens, MD
Used to cut costs and utilization at the expense of patient safety and quality of care.
—Michel
Sucher, MD
Less human instinct and depersonalization.
—
David Carfagno, DO
Big data is only as good as its inputs and has the potential to make incorrect conclusions based on faulty premises and impacted by who is inputting the data. The current state of big data in medicine is still in evolution having the potential for good, but equal risk of creating false conclusions.
—Jeffrey Edelstein, MD
On a scale of 0 to 10, indicate how receptive you are to incorporating big data into your practice of medicine.
Zero equals not receptive and 10 equals very receptive.
What concerns do you have about big data in medicine? Average 5.8 Read more by visiting arizonaphysician.com/docs-big-data 20 n ARIZONA PHYSICIAN MAGAZINE
May not always apply to or reflect immediate local population, environment.
—Helen Markowski, MD
Care needs to be taken to understand the data modeling and algorithms that transform the data and make it actionable. I prefer the terms “assisted intelligence” or “augmented intelligence”--technology paired with trained clinicians and intuitive interfaces with an opportunity for patients to also participate and help drive their care will promote more efficient care and healthier populations.
—Anthony Dunnigan, MD
The doctor-patient relationship has been destroyed. Doctors now spend less time on physical exams and much more time on data entry. Some doctors even turn their backs on the patient to face a screen. There is a gigantic volume of prepopulated nonsense in the records. This has slowed the ability to efficiently see patients. The EMRs do not speak to each other. Data from visits should easily be loaded into the caring provider’s charts. The volume of care repetition is staggering and wasteful. —Richard Dobrusin, DO
Lack of standards and expectations for transparency (black box problem); liability related use; risk of bias, discrimination & unrepresentativeness; data quality; privacy issues; data ownership; need for or reliance on those with technical expertise.
—Anita Murcko, MD
That the term may just be a catchy term without real meaningful impact. There aren’t unlimited healthcare dollars, and so much already seems to be spent on research that is so far from directly helping patients.
—Jane Lyons, MD
Learn more about the participating physicians
Donald Toatley, MD, MBA, MHA Southwest Contemporary Women’s Care
WEB | swcwc.net
Edward Taxin, DO Retired
Michael Underhill, DO Mayo Clinic
WEB | mayoclinic.org
James Carpenter, MD Village Medical
WEB | villagemedical.com
Tammy Pennhollow, DO Precision Regenerative Medicine
WEB | precisionmedprp.com
Adam Koelsch, MD
Adam R Koelsch MD PC
WEB | doctorkoelsch.com
Melanie D. Cloonan-Schulte , MD Melanie D. Cloonan-Schulte MD
WEB | drmcloonan-schulte.com
David R. Shprecher, DO Banner Sun Health Research Institute
WEB | bannerhealth.com
David Saperstein, MD Center for Complex Neurology
WEB | complexneurology.com
Ching Wang, MD Sunset Community Health Center
WEB | mysunsethealth.org
Jeffrey Taffet MD Biltmore ENT
WEB | biltmoreent.com
Robin Demi Ross, MD, MPH, CPH Global Retina Institute
WEB | globalretinainstitute.com
Robert Cravens, MD Tucson ENT
WEB | tucsonent.com
Michel Sucher, MD
Sucher Medical Management LTD
David Carfagno, DO Scottsdale Sports Medicine
WEB | scottsdalesportsmedicine.com
Jeff Edelstein, MD
Jeffrey Paul Edelstein MD LTD
WEB | jpemd.com
Glenn Brown, MD
Glenn H Brown MD PLLC
WEB | browndermatology.com
Anthony Dunnigan, MD, MBI Valleywise Health
WEB | valleywisehealth.org
Richard Dobrusin, DO Cigna
WEB | cigna.com
Helen Markowski, MD HonorHealth
WEB | honorhealth.com
Anita Murcko, MD, MACP, FAMIA Arizona State University
WEB | asu.edu
Jane Lyons, MD
Dignity Health
WEB | dignityhealth.com
21 ARIZONAPHYSICIAN.COM
ARIZONA PHYSICIAN: Does your practice leverage any data from outside sources?


DR. LAUFER: We do. We’re involved in the MeritBased Incentive Payment System (MIPS), and we do quality metrics using the American College of Cardiology Pinnacle Registry. We can pick the criteria that we'd like to submit. We have had a 95 to 100% success rate. If we don't measure up, then we would take a cut in Medicare fees. We have always gotten an increase by doing these submissions.
Heart and Vascular Center of Arizona
AP: Which wearables do your patients use and would you say that they work well?
DR. LAUFER: Wearable devices have a wide range of potential clinical applications, including screening for atrial fibrillation, hypertension, obstructive sleep apnea, heart failure, and cardiovascular fitness. As the use of wearable devices grows, we need a multifaceted approach to integrate these technologies effectively and safely into routine clinical practice. We also have implantable defibrillators and pacemakers. We have loop recorders that measure arrhythmias. Each company has its own website, and it becomes very time-consuming for us to do this on our own. We did that for many years but now have a company that collates all the data from implantable devices and sends us alerts.
22 n ARIZONA PHYSICIAN MAGAZINE IN DEPTH
Learn more about Heart and Vascular Center of Arizona by visiting arizonaphysician.com/hvcaz
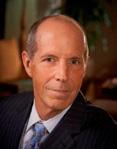
We sat down with Nathan Laufer, MD, CM, FACC, FCCP, FACP, FRCP(C), founder and Chief Medical Officer at Heart and Vascular Center of Arizona to discuss big data and its impact on cardiology and his practice.
A CONVERSATION WITH
AP: Does the evidence show that tracking data would help to prevent serious episodes like cardiac arrest?
DR. LAUFER: It depends on which implantable device we get data from. Heart monitors or loop recorders are designed to find rhythm disturbances that occur so infrequently that we cannot find them on routine 24 hour or 2-week wearable monitors.

In patients with a history of atrial fibrillation we may want to know if our medication is working. If they have had an ablation procedure, patients may not feel their recurrent atrial fibrillation. This is an excellent way of monitoring the patients. We do pick up quite a bit of atrial fibrillation in patients who may have had a previous warning stroke, or TIA, where their rhythms in the hospital are completely normal. We may find atrial fibrillation a month or two later using these implantable devices. We can also pick up other rhythm disturbances that can cause passing out spells and treat them appropriately.
AP: Are the devices paid out of pocket?
DR. LAUFER: The implantable loop recorders and wearable monitors are covered by insurance. We sometimes have to fight to get authorizations and are usually successful. Other patients may need a pacemaker. Today, all implantable devices come with a transmitter at the side of the bed that transmits data through a third party to our computers. We’ll know if patients have fast rhythms, slow rhythms, or ventricular tachycardia. We also have defibrillators that we implant for patients who have weak heart muscles or have had a cardiac arrest.
AP: Does the data just tend to grow and grow? Is it too much?
DR. LAUFER: It depends on what we do with it. For each individual patient, it is fine. They're subcategorized in their electronic record, and we know how to find the data we need. We need bigger servers all the time, and we're paying a fortune in IT support to keep it all functional in the cloud. Once you start paying for IT support, it never stops!
AP: Does it help to have the patient more involved in monitoring their own care?
Dr. Laufer: It’s very helpful to have patients monitor their weights and blood pressures. However, they don't have access to the transmitted data that we have access to. In the future, more patients will be able to track more data.
23 ARIZONAPHYSICIAN.COM
“As the use of wearable devices grows, we need a multifaceted approach to integrate these technologies”
—Nathan Laufer, MD
AP: Has cardiology improved or declined with greater use of data?
DR. LAUFER: I think cardiac care has improved greatly with all the monitoring data we now have available. However, managing our data is very cumbersome, and there are only so many hours in the day. The company that monitors our implantable devices was offering to send all kinds of alerts to the cell phones of all our physicians. We said that there is a point in time where we don't need all this data immediately. We need to sleep at night. For something urgent, we will get alerts. We have an infrastructure in our practice with triage nurses and nurse practitioners. They field phone calls. They look at transmissions. We also have a full-time device nurse who does in office device monitoring and imports the data to the patients’ charts. So, we have a huge costly infrastructure to be able to take care of our patients. However, insurance companies keep beating us up on reimbursement. When the overhead is higher than the revenue, we're going to have a major problem.
AP: What do you think about security and privacy of data?
DR. LAUFER: Security has become much tighter than it was in the early days. However, there is always a concern that hackers may be able to get in and turn off a defibrillator just like they can start a car remotely. We routinely assess our cybersecurity with our IT firm looking for gaps. We also have cybersecurity insurance to protect our network and electronic medical records. Ransomware has happened to hospitals. Very few want to publicize that they've actually paid a ransom because it's bad for their image. Hospitals are bigger targets than cardiology practices. One of the things that was supposed to be a promise of electronic medical records is that all these different systems would be integrated at some level. That has never really come to fruition. There is no interoperability. All these computer systems are potential gaps where security could be compromised.
AP: Are we heading in the right direction?
DR. LAUFER: It’s all very complex and big data means ‘Big Brother’ is watching, which is probably why all these electronic records were mandated in the first place. In the old days, I would sit with a Dictaphone in front of a patient. They would hear everything I was saying, and I'd be looking them in the eye and we'd have a conversation. The dictation would then be transcribed. I would then sign off on the record a day or two later and it would get mailed to the referring physician. Now, instead of a 2-page note, it's a 10 to 15-page note, most of which is junk. This has nothing to do with patient care. When I receive records from other physicians, or send notes to them, everybody knows to cut to the chase, which is really in the few lines at the beginning or at the end of the note. Everything else is data for quality metrics for insurance companies and for Medicare and AHCCCS.
n ARIZONA PHYSICIAN MAGAZINE 24 IN DEPTH
HEART & VASCULAR CENTER OF
ARIZONA
By the Numbers
8
AP: What do you see as the largest obstacles in running a practice today?
DR. LAUFER: Prior authorizations are very cumbersome. I see no reason for this. We spend too much time with peerto-peer discussions or appeals to take care of our patients. Our authorization success rate is close to 95%. The truth is physicians’ costs are less than 5% of the dollars spent on healthcare. And yet we're the low hanging fruit that everybody beats up on. Many physicians are getting fed up or burned out by the bureaucracy when they just want to take care of patients.
AP: A very high percentage of cardiologists are hospital employed. What are some of the biggest opportunities of running your private practice?
DR. LAUFER: Independence. I'm seeing a swing nationally by employed physicians who are not happy and want to go back to private practice. They don't want to have to deal with hospital administrators. They don't trust them and mostly for good reasons. We have one physician in our practice who was in a group for 17 years. His practice was sold to a hospital, and they cut his salary by a third a year later and so he left that group. Whenever we have physicians interviewing with a hospital, we have them meet this gentleman who usually talks them out of it.
AP: What are the impacts of growth for EMRs and quality metrics?
DR. LAUFER: That's what's leading to burnout. Most physicians want to spend time looking at patients and not looking at computer screens. There are physicians who spend most the evenings or weekends catching up on their charting. Plus, in our field, we are also on call at night for cardiac emergencies. Healthcare today is very complex and cumbersome for physicians and patients. ■
74 EMPLOYEES:
Includes: medical assistants, technicians, billers, schedulers, authorization specialists, and front office staff.
SERVICES PROVIDED:
noninvasive, invasive, and interventional cardiology, electrophysiology, nuclear cardiology, cardiac PET scans, echocardiography, and peripheral vascular imaging.

ADDITIONAL SERVICES : Cardiac and peripheral interventions, implanting of pacemakers and defibrillators.
HOSPITAL SERVICES: Advanced procedures such as percutaneous aortic valve implants, carotid stents, and higher risk coronary interventions.
4 LOCATIONS
Central Phoenix West Phoenix Globe Show Low
Connect with Heart and Vascular Center of Arizona at heartcenteraz.com
25 ARIZONAPHYSICIAN.COM
IN 1998
FOUNDED
PHYSICIANS
NURSE
10
PRACTITIONERS
Interested in having your medical practice/hospital showcased in Arizona Physician? Let us know at info@arizonaphysician.com
Big Brother’s Using Big Data to Investigate Physicians
Many of us have heard the term big data more and more in recent years, but what is big data? Big data refers to the technologies used to store, analyze, and manage large amounts of information. The use of big data provides the power to analyze and find patterns in large amounts of information far more quickly and accurately than before.
The Department of Health and Human Services (“HHS”) and its Office of the Inspector General (“OIG”) have begun to use big data to detect suspected fraud and abuse in federal healthcare programs. In 2015, OIG created the Office of the Chief Data Officer. The Office of the Chief Data Officer works closely with the Centers for Medicare and Medicaid Services (“CMS”) to obtain vast amounts of healthcare data for analysis. Data analytics tools are applied to healthcare data, to lead OIG to physicians and other providers who might be engaged in fraudulent activity.

26 n ARIZONA PHYSICIAN MAGAZINE Learn more by visiting arizonaphysician.com/big-brother-big-data LEGAL CORNER
OIG is also using big data in predictive models. This allows OIG to identify trends and outliers, who might then become potential investigative targets. Once OIG identifies new trends and types of fraudulent schemes, its data analytics tools allow it to identify and target similar instances of fraud. OIG also uses data modeling to generate provider risk scores. Using various statistical methods, providers are rated as high, medium, or low risk. Providers flagged as high risk will be subject to more scrutiny from the OIG.
In October 2021, the Department of Justice (“DOJ”) announced that the use of data had led to the discovery of a fraudulent billing scheme. Four companies were charged with promoting improper billing involving P-Stim electro-acupuncture devices; the physicians who used the devices were charged with fraudulent billing. These P-Stim devices are not covered by Federal healthcare programs, but the companies selling the devices made false representations that P-Stim devices were reimbursable under billing codes meant for surgically implanted neuro-stimulators. These representations led to improper billing by physicians, resulting in thousands of dollars per billed P-Stim procedure. These improper billings were discovered by applying analytics to healthcare claims. DOJ offices across the country pursued and settled various False Claims Act (“FCA”) cases against P-Stim sellers and physicians, recovering millions.

According to Fall 2022 Semiannual Report to Congress, OIG expected nearly $4 billion in recoveries resulting from OIG audits and investigations occurring between October 1, 2021, and September 30, 2022. Approximately $1 billion of this amount relates to audit findings, and approximately $3 billion relates to investigative work. These audit and investigatory findings were driven largely by the use of data analytics.
By way of example, the OIG used data analytics to identify 1,714 providers (out of approximately 742,000) whose billing for telehealth services during the first year of the COVID-19 pandemic posed a high fraud risk to Medicare. OIG concluded that these 1,714
providers had suspect billing on at least 1 of 7 measures that OIG felt might indicate fraud, waste, or abuse of telehealth services.
Per Christi A. Grimm, the HHS Inspector General, “HHS-OIG continues to provide essential, data-driven oversight and enforcement to drive positive change in HHS programs and for individuals they serve.” Since the focus on the use of data analytics, more non-qui tam False Claims Act cases have been filed than ever before. DOJ initiated 100 more FCA cases in 2020 than it did in 2019, resulting in the most non-qui-tam FCA cases filed in almost 30 years. The 296 nonqui tam and 652 qui tam cases reported for 2022 reflect an increase over 2021’s new case numbers of 212 and 598, respectively.
So, what does this mean for physicians? While big data can be used to identify fraud and abuse, it can also be used by providers to catch and correct potential billing errors and avoid the scrutiny of the OIG.
Practices should consider incorporating data analytics into their audit and compliance programs, to minimize the risk of enforcement actions and investigations. Early identification and correction of potential improper billings can help practices avoid being caught up in costly investigations and prosecutions. ■
 Karina A. Shipman, JD, MBA Associate Attorney Milligan Lawless, PC karina@milliganlawless.com
Karina A. Shipman, JD, MBA Associate Attorney Milligan Lawless, PC karina@milliganlawless.com
 Robert J. Milligan, JD Shareholder Milligan Lawless, PC Bob@milliganlawless.com
Robert J. Milligan, JD Shareholder Milligan Lawless, PC Bob@milliganlawless.com
27 ARIZONAPHYSICIAN.COM
Benefits of a Practice Buy-In
For buyers and sellers
Practice ownership is the goal for many physicians, but there is more than one way to get there, and that path looks different for everyone. When most physicians think of getting into practice ownership, they think they need to start their own practice or buy an existing one. But an often-overlooked method that can be a great fit for many physicians is a partial practice buy-in.
WHAT IS A PRACTICE BUY-IN?
A practice buy-in is when a physician buys a portion of the ownership of an existing medical practice, and the existing owner(s) remain as partners. The portion that is purchased can be anywhere from 1-99% of the practice, but usually works best when all the partners have an even split of the ownership. With a buy-in there are multiple benefits to both the buyer and the seller.

BENEFITS OF A BUY-IN FOR THE BUYER
1 | The main benefit is that the buyer gets to buy in to a practice that is already thriving and has solid cash flow, as opposed to starting up a new practice and having to build the cash flow up from zero.
2 | Having a partner that already has years of experience running the practice on a business level. This mentorship can be priceless. If you own a practice on your own that’s something you don’t usually have access to.
3 | Stepping into practice ownership as a partner adds a significant asset that you can build as a legacy for your family.
4 | Increase your income overnight by adding profit distributions to your personal bottom line.
28 n ARIZONA PHYSICIAN MAGAZINE
TO Learn more by visiting arizonaphysician.com/practice-buy-ins
HOW
BENEFITS OF A BUY-IN FOR THE SELLER
There are 2 main reasons for a seller wanting to do a buy-in, and the benefits for eaach can vary.
1 | SELLER WANTING TO SLOW DOWN FOR RETIREMENT:
Having a younger doctor buy in as a partner will give you an extra set of hands to take over some of your patient load.
Allows you to reduce hours or days so you can start dipping your toe into retirement.
Get access to part of the equity in your practice now. This allows you to use the proceeds from the sale to invest, pay off debt, or prepare for retirement however you see fit. It also helps ease tax obligations by breaking up the sale of your practice into multiple events.
2 | SELLER WANTING TO GROW THE PRACTICE:
Increase the practice production capabilities overnight by adding another set of hands to treat patients.
Take some of the responsibilities of practice ownership off your plate. Dividing some of the day-to-day tasks with a partner will free up more of your time so you can treat more patients.
Having a partner that is as invested in the success of the practice as you are is a proven method for growing and sustaining a practice much better than if you just add an employee doctor to your staff.
HOW TO COMPLETE A PRACTICE BUY-IN
So, if you’re now thinking that a practice buy-in is right for you, you may be wondering how to go about completing one. There are 5 main steps to any successful practice buy-in:
1 | THE FIRST STEP IS TO MAKE SURE THAT IT’S A GOOD FIT. There’s nothing worse than getting into a bad partnership, so take some time to vet your potential partner. Make sure they are a good fit on a professional, ethical, and personal level. It’s also a good idea to make sure that your treatment ideology and vison for the future of the practice are in alignment.
2 | STEP TWO IS TO NEGOTIATE the sales price for the buy-in, the terms, ownership percentages, and partnership structure.
It is usually a good idea to get a professional 3rd party opinion on value of the practice to help determine what the sales price should be.
3 | APPLY FOR FINANCING.
Working with a bank that has a division that specializes in healthcare practice financing is critical to your success. This is where National Bank of Arizona and Practice Pathways can help.

Loans for practice buy-ins are typically structured with the doctor that is buying in as the borrower (either personally or with the entity they will hold their % of the practice ownership in), and with the practice itself as a corporate guarantor.
4 | Have a lawyer draft a sales contract and agreements that are fair to all parties involved.
5 | Close on the buy-in, transfer the ownership, and enjoy your new partnership!
A practice buy-in truly can be a great option for both buyer and seller. Just as you would advise your patients to come see you, instead of just looking on Web MD for a diagnosis, it’s important that you connect with experienced professionals to make this process as smooth and successful for you as possible.
By Joshua Flake Vice President, Practice Pathways Joshua.Flake@practicepathways.com
29 ARIZONAPHYSICIAN.COM
PHYSICIAN SPOTLIGHT
Mandeep M. Sahani, MD, of Desert Kidney Associates

on Big Data
Q: What does big data mean to you?
A: Nephrology is a data-driven specialty. The basis of our diagnosis for kidney issues is based on data. Data defines our clinical approach to that patient because either you have it, or you don’t. You either have chronic kidney disease or you don’t.
Q: You’re saying nephrology leans heavily on quantitative data?
A: Yes, as opposed to qualitative data. A cardiologist’s patient could have chest pain coming from either the heart or from a musculoskeletal origin, whereas we do a blood test and discover variation in that patient’s grating. And then we conclude that there is chronic kidney disease or acute kidney disease. We could potentially come to a diagnosis even before we walk into the patient’s room. Having data presented in a format that we can use gives us a good idea of what conversation we’re going to have with the patient.
Q: How often and what data is needed to monitor patients with kidney disease?
A: That would depend upon the stage of the chronic kidney disease, which has five stages. For stage 1, we’d want to see the patient and get the data maybe once or twice a year. For stage two to three, maybe every six months or so, and then stage 4 is every quarter. Stage five is every month and then once you’re on dialysis, it’s either once or twice a month. Once we get the data, we compare it to the trends. There are calculations to establish if that individual is going to progress downward towards worsening CKD, perhaps requiring dialysis or a kidney transplant. Data helps us to forecast, and risk stratify. They help us to see whether co-morbidities are causing or influencing a chronic disease like diabetes. One very important point is how we educate patients and empower them to understand what the data means in their continuum of disease progression. Then, we discuss what interventions we can collectively put in place that will influence the disease progression.
Q: Do you find that most patients can easily understand it?
A: That’s up to us and how we break it down for them. Certain patients get it right away, like people who are tracking other parameters of health like steps, heart rate, blood pressure. We’re accountable to get them up to speed on recognizing that data is very important, especially relating to kidney disease.
Q: What impacts have you seen so far?
A: We just started last year. The challenges were getting the right data for the right population and, in this instance, the data was given to us by the CMS demonstration project called Kidney Care Choices or KCC, which takes in the patients who are at risk for CKD-4 and CKD-5 and are dialysis patients. We had some challenges identifying members, getting to those members, getting them to understand what this means for them, and why we’re doing these interventions. But towards the end of the year, we saw significant improvement in other metrics of how we measure one kidney care cohort versus another. ■
MANDEEP SAHANI, MD, MS CEO/CIO Desert Kidney Associates
30 n ARIZONA PHYSICIAN MAGAZINE
msahani@desertkidenymd.com desertkidney.com
Two Decades of Asset Protection Law Experience

20 years National Asset Protection Legal practice in 2023
20 YEARS OF FOCUS
2023 marks 20 years of legal practice devoted exclusively to asset protection, wealth preservation and risk management planning. Often at the referral of Arizona’s best lawyers and advisors, we help protect billions of dollars in personal assets for a national client base of thousands of successful clients including:

• Real Estate Investors
• Business Owners and Entrepreneurs
• Physicians
• C-level Execs
• Family Business Owners
• And Some of Arizona’s Most Successful Lawyers!
IKE DEVJI Founder and Managing Attorney PRO ASSET PROTECTION Of Counsel, Davis Miles McGuire Gardner Of Counsel, Lodmell & Lodmell
We have a wide range of cutting edge strategies available that include both well proven conventional domestic planning, offshore strategies and plans that combine the best of both.
Asset Protection Attorney IKE DEVJI, J.D. 8245 N 85th Way, Suite A • Scottsdale, AZ 85258 • (602) 808-5540 • www.ProAssetProtection.com
are here to help you MAKE IT, KEEP IT and PASS IT ON.
We



Mutual Insurance Company of Arizona® Trusted Medical Professional Liability Protection Backed by Financial Strength MICA remains steadfast in its financial foundation and the ongoing ability to share success with our members through our dividend program. To learn more, call 800-681-1840 or visit www.mica-insurance.com/why-choose-mica. THE EXCLUSIVE MPL CARRIER FOR MCMS MEMBERS Arizona Physician Magazine 326 E Coronado Rd, Suite 101 Phoenix, AZ 85004 (602) 417-2303 information@arizonaphysician.com





























































































 Karina A. Shipman, JD, MBA Associate Attorney Milligan Lawless, PC karina@milliganlawless.com
Karina A. Shipman, JD, MBA Associate Attorney Milligan Lawless, PC karina@milliganlawless.com
 Robert J. Milligan, JD Shareholder Milligan Lawless, PC Bob@milliganlawless.com
Robert J. Milligan, JD Shareholder Milligan Lawless, PC Bob@milliganlawless.com