

Exploring the Human Form
Art and Anatomy by the Henry Vandyke Carter Club at Grand Canyon University in Phoenix, Arizona

Isabella M Rystrom
This is a pencil drawing of a human skull with exposed facial and neck muscles, focusing on anatomical accuracy and shading to create depth. I wanted to capture the structure of the bones and soft tissue to maintain a realistic look. The contrast and detail in the muscle fibers were especially fun to work on, helping me realize the complexity of the body.
Isabella M Rystrom
Dr. O. Clarkson
This is a pencil drawing of a human skull with exposed facial and neck muscles, focusing on anatomical accuracy and shading to create depth. I wanted to capture the structure of the bones and soft tissue to maintain a realistic look. The contrast and detail in the muscle fibers were especially fun to work on, helping me realize the complexity of the body.
Dr. O. Clarkson
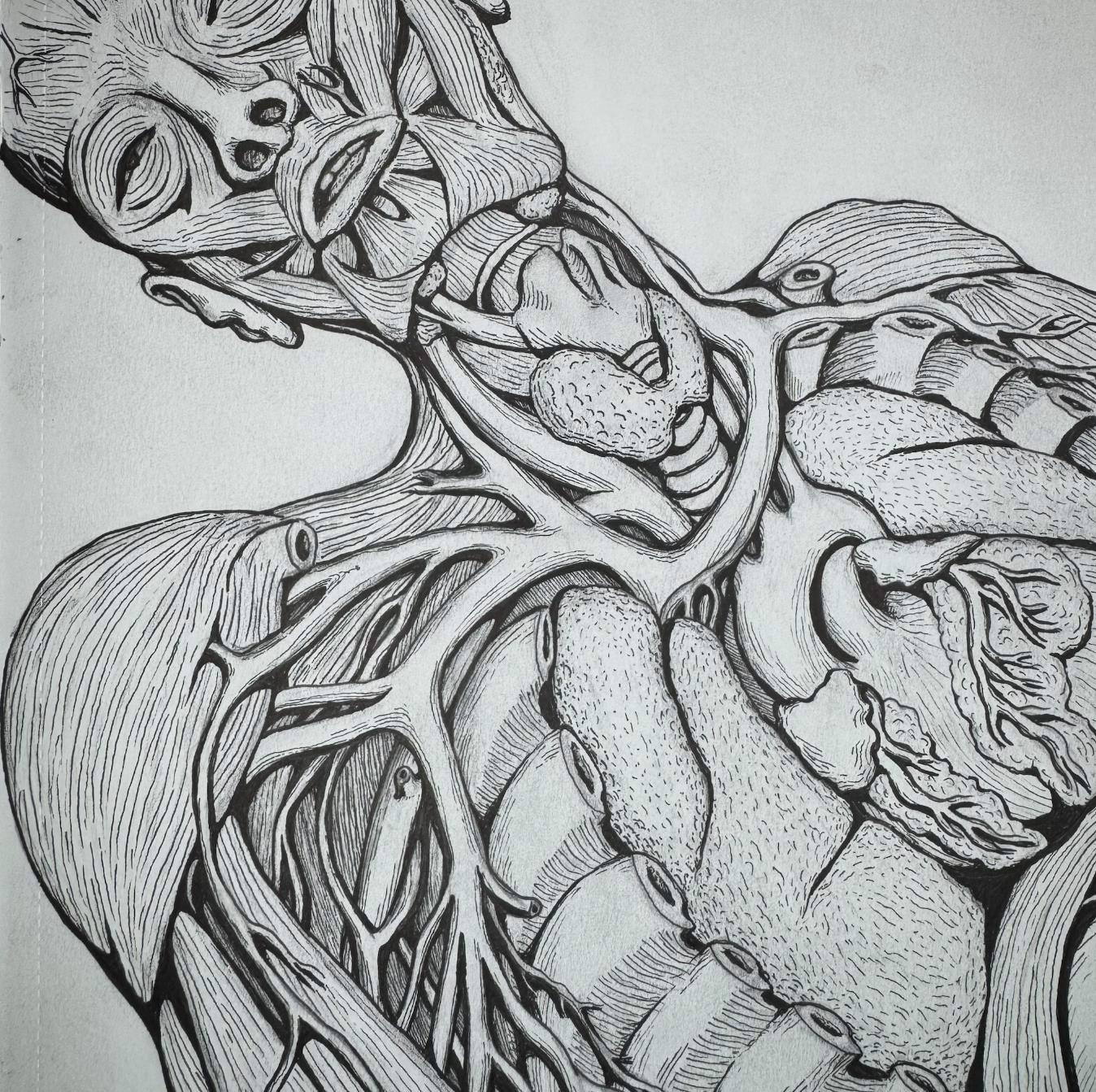
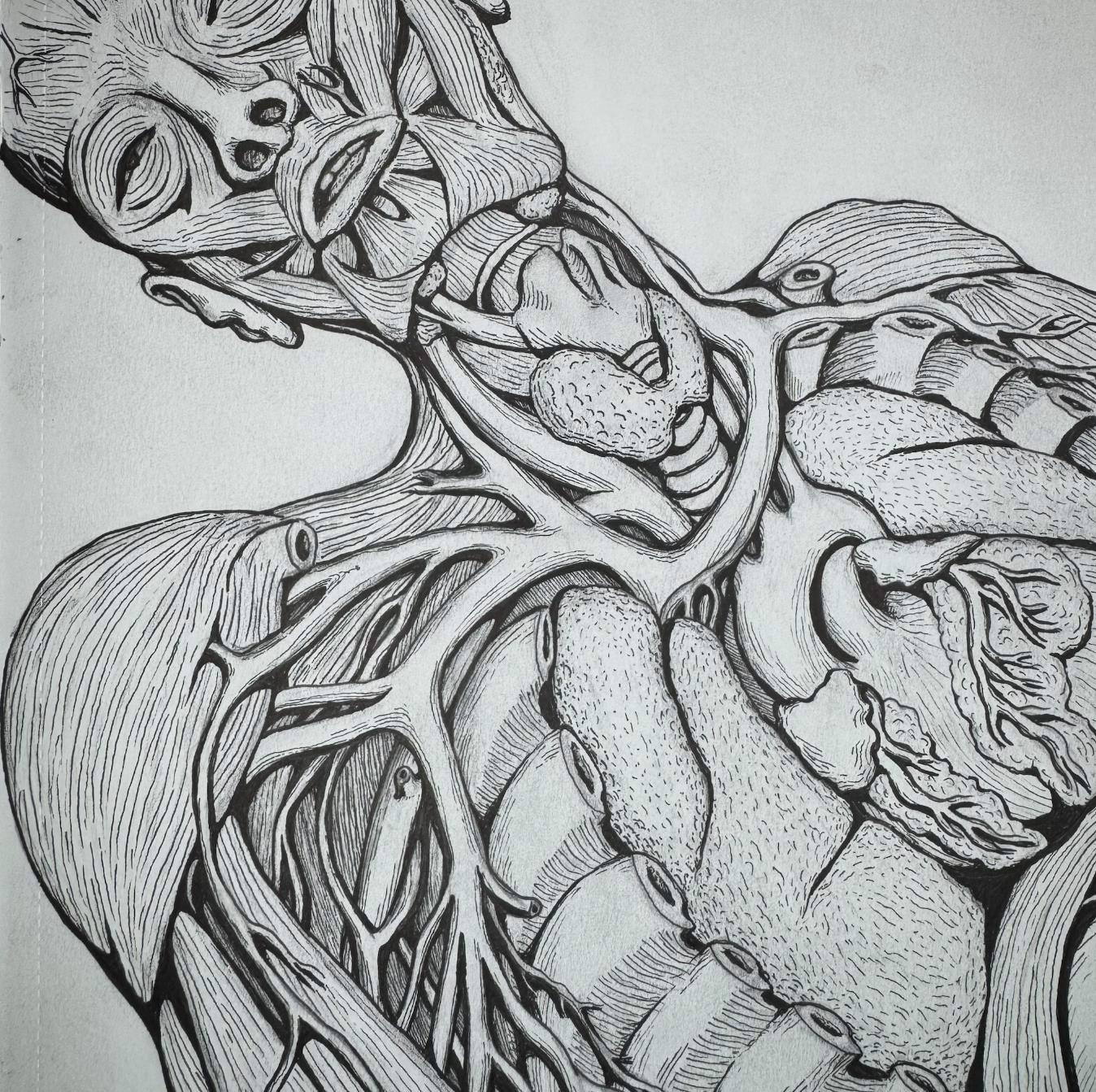
This detailed ink drawing showcases the complex structure of the human head and torso, with a focus on the facial muscles, neck structures, and internal organs. The artist’s careful attention to anatomical accuracy highlights the intricate network of muscles, veins, and bones, while the shading creates a dynamic, three-dimensional quality. The combination of line work and cross-hatching emphasizes the depth and realism, offering a detailed exploration of human anatomy.

This detailed ink drawing showcases the complex structure of the human head and torso, with a focus on the facial muscles, neck structures, and internal organs. The artist’s careful attention to anatomical accuracy highlights the intricate network of muscles, veins, and bones, while the shading creates a dynamic, three-dimensional quality. The combination of line work and cross-hatching emphasizes the depth and realism, offering a detailed exploration of human anatomy.



Sydney A Hernandez
This intricately detailed graphite drawing presents a lateral crosssection of the human skull and cervical spine, revealing the delicate architecture of the brain within. The contrast between the rigid bone structure and delicate form of the brain creates a compelling visual tension, symbolizing fragility and resilience of the human body.
Sydney A Hernandez
This intricately detailed graphite drawing presents a lateral cross section of the human skull and cervical spine, revealing the delicate architecture of the brain within. The contrast between the rigid bone structure and delicate form of the brain creates a compelling visual tension, symbolizing fragility and resilience of the human body.
Dr. O. Clarkson
Dr. O. Clarkson
This detailed drawing of a human skeleton emphasizes the intricate structure of the ribcage, clavicles, and pelvic bones. The shading and linework bring a three-dimensional quality to the illustration, showcasing both anatomical accuracy and artistic skill. The drawing serves as a strong representation of the human skeletal system, focusing on key elements essential for understanding human anatomy.
This detailed drawing of a human skeleton emphasizes the intricate structure of the ribcage, clavicles, and pelvic bones. The shading and linework bring a three-dimensional quality to the illustration, showcasing both anatomical accuracy and artistic skill. The drawing serves as a strong representation of the human skeletal system, focusing on key elements essential for understanding human anatomy.


MCMS
A Home For All Physicians Across Arizona
As a pediatric physician practicing in Arizona, I have come to deeply value the power of community within medicine. Being part of a professional network that understands our daily challenges and actively works to amplify our voices, celebrate accomplishments, and advocate for sustainable healthcare systems is essential. That is exactly what the Maricopa County Medical Society (MCMS) offers: a home for physicians who want to connect, lead, and grow.
As a longtime member, advocate, and Board President, I can confidently say MCMS has been instrumental in strengthening my career and deepening my ties to Arizona’s medical community especially after relocating from California. From relationshipbuilding and educational opportunities to leadership and advocacy, MCMS continues to enrich my journey.
Membership is where connection begins. You gain access to exclusive resources, practice support, and a peer network that values your voice. From CME opportunities to business development, MCMS is here to help you thrive.
We are especially proud to support private practices pillars of community health by addressing challenges like staffing, regulatory changes, and reimbursement. Our resources and advocacy efforts are designed to empower these practices to grow and remain independent.
Through monthly networking and CME events, MCMS brings together healthcare professionals across specialties and career stages, building meaningful relationships and creating space for mentorship, collaboration, and community.
We do not just listen we advocate. Our members actively shape healthcare policy through MCMS led events, policy roundtables, and direct engagement with elected officials.
Another meaningful way to engage is through Arizona Physician, our quarterly magazine that amplifies member voices and showcases research, innovation, and personal stories. We invite you to contribute whether it is an opinion piece, clinical insight, or marketing feature.
Whether you are just starting out or decades into practice, MCMS welcomes you. Let us shape the future of Arizona medicine together. Visit mcmsonline.com to learn more.
Jane Lyons, MD MCMS Board President

Dr. Jane Lyons is a Pediatrician, who provides care for patients in both the inpatient and outpatient setting. She works locally in Phoenix as well as providing rural locum hospital based care. Dr. Lyons completed her medical training in San Diego, CA, has two young children, and enjoys the outdoors, cooking, and spending time with family and friends.
Championing Change
The Vital Role of Physician Advocacy in Healthcare
In today’s fast-paced, digitally connected world, meaningful storytelling in healthcare has never been more essential or more accessible. At Arizona Physician, we understand the incredible privilege and responsibility of being a voice for Arizona’s medical community. Whether it is a physician’s journey, a student’s first steps into medicine, research and innovation, medical school expansion, or the ripple effect of new health policy, we are committed to capturing and sharing these stories that move, inform, and inspire.
We know that staying connected is more than just being informed, it is about belonging. That is why we have invested in creating new digital experiences that meet you wherever you are, while still holding true to the richness and credibility of print journalism.
A MODERN MAGAZINE AT YOUR FINGERTIPS
We know how busy your lives are. The pace of medicine does not slow down, and neither does your commitment to patients, education, and community. That is why we have worked to make Arizona Physician more accessible than ever before.
We are proud to offer our full issues through Issuu, a seamless digital platform that mirrors the feel of flipping through a traditional magazine but with interactive elements that elevate your reading experience. Whether you are between appointments, enjoying a quiet moment at home, or catching up on your tablet during a flight, Issuu offers an elegant, user-friendly way to flip through articles, photos, and features just like reading the printed magazine, but with the convenience of a screen. You will find clickable links with easy navigation, interactive features, and a digital layout that honors the beautiful design and thoughtful content you have come to expect from our publication.
ARIZONAPHYSICIAN.COM:
A HOME FOR HEALTHCARE VOICES
Our digital home, ArizonaPhysician.com, has become so much more than an archive. It is a growing, dynamic platform designed to connect physicians,
advocates, and thought leaders across Arizona. There, you will find exclusive web content, Maricopa County Medical Society updates, upcoming event details, continuing medical education (CME) opportunities, and updates on healthcare policies that matter to you.
It is also a space where your voice matters. Whether through opinion articles, featured interviews, or member spotlights, we invite you to share your ideas, insights, and innovations. By amplifying diverse perspectives, we strengthen the collective voice of Arizona’s medical community.
We are also proud to introduce several new features designed to reflect and elevate the experiences of our readers:
A Medical Journey–A tribute to the knowledge and impact of those who have shaped Arizona’s healthcare landscape, while offering thoughtful guidance to those approaching retirement.
Hot Topics with a Physician “Spotlight” In-the-moment commentary and discussions with practicing physicians on today’s most pressing issues, from policy shifts to cutting-edge treatments.
Physician to Physician–Honest, peer-topeer conversations that promote mentorship, camaraderie, and real talk among those who know this profession best.
EXPANDING REACH, DEEPENING CONNECTION
What drives us is not just a commitment to content but a commitment to connection. Our goal is to provide value, foster dialogue, and offer a platform where healthcare professionals feel seen, supported, and celebrated. We believe that digital innovation should amplify human connection, not replace it. That is why we are building stronger bridges between our print issues and digital content, blending timeless storytelling with modern access.
We are also continuously exploring ways to partner with you, our members, contributors, and readers to keep this publication reflective of your lived experience. Arizona Physician is not just about healthcare in Arizona. It is about the people who make that care possible, every single day.
LET US KEEP THE CONVERSATION GOING
Whether you have been part of our journey since we began in 1955 or are just discovering us with this issue, thank you for being here. Your involvement, insights, and continued support drive our mission forward and help shape the stories we share.
As you explore our content on Issuu and ArizonaPhysician.com, I invite you to stay curious, get involved, and share your story.
Together, we are not just documenting the future of healthcare, we are helping to shape it.
With Gratitude,

Desire’e Hardge, MBA
Arizona Physician Editor-in-Chief
MCMS CEO & Executive Director


Desire’e M. Hardge, MBA, serves as the CEO & Executive Director of MCMS and the Editor-in-Chief for the Arizona Physician magazine. Desire’e brings over 19 years of experience across both for-profit and non-profit sectors. She has successfully led organizations through
and






BRIEFS
NEWS AND NOTES FROM THE FIELD

The Power of a Transition Ritual
For physicians, the shift from work to home isn’t always clean. You may physically leave the hospital or clinic, but your mind stays there—replaying patient interactions, secondguessing decisions, or mentally triaging tomorrow’s chaos. Without an intentional break between roles, it’s easy to carry the weight of the day into your home, your relationships, and even your sleep.
That’s where transition rituals come in. These are brief, deliberate actions that signal to your brain: this part of the day is over. It might be changing out of scrubs, playing a specific

playlist on your commute, or taking a short walk before stepping inside. Some physicians sit in their car for two minutes, eyes closed, breathing deeply before shifting gears. Others use a go-to coffee mug or say a specific phrase to themselves as they lock up for the night.
Think of it as a controlled experiment in Pavlovian conditioning—except you’re both the subject and the scientist. Over time, these rituals train your brain to associate specific cues with decompression and psychological reset. You already have rituals to begin your clinical day (hand hygiene and chart review). Why not give the end of your day the same intention?
It doesn’t have to be elaborate. It just must be yours. Even a brief, consistent act can help you stop being “on,” so you can show up more fully for the rest of your life. And with current technology, you can even automate some of them.
Here are 10 ideas to help you keep your work at work—and show up for yourself at home:
1. Change out of scrubs immediately when you get home.
2. Listen to a specifwic playlist or podcast on your commute.
3. Take a short walk before stepping inside.
4. Sit in your car with your eyes closed for 90 seconds, focusing only on your breath.
5. Say a mental goodbye to your last patient of the day.
6. Light a candle or turn on soft lighting.
7. Make yourself a cup of herbal tea or another comfort drink.
8. Water your houseplants—extra points if you talk to them.
9. Put on a favorite album or show— bonus if it’s on vinyl or something you physically engage with.
10. Go directly to your charging station, plug in your phone, and walk away.

5 Mental Health Tips for Physicians
Physicians often face immense pressure and demanding schedules, which can take a toll on their mental health. Here are five practical tips to help physicians maintain their mental well-being:
PRIORITIZE SELF-CARE
Physicians should make time for self-care to recharge and prevent burnout. This includes regular exercise, healthy eating, adequate sleep, and engaging in hobbies or activities that bring joy and relaxation.
SEEK SUPPORT
Connecting with colleagues, friends, or family members can provide crucial emotional support. Additionally, joining peer support groups or seeking professional counseling can offer a safe space to discuss challenges and stressors.
SET BOUNDARIES
It’s essential for physicians to set clear boundaries between work and personal life. This might involve scheduling time off,
limiting work-related communication after hours, and ensuring time is allocated for personal activities.
PRACTICE MINDFULNESS
Mindfulness techniques such as meditation, deep breathing exercises, and mindful walks can help physicians stay present and reduce stress. These practices can improve focus and emotional resilience.
CONTINUOUS EDUCATION
Staying informed about mental health resources and strategies can empower physicians to better manage their wellbeing. Attending workshops, reading relevant literature, and participating in mental health training can be beneficial.
By implementing these tips, physicians can foster a healthier work-life balance and enhance their overall mental health. Remember, taking care of oneself is not a luxury, it’s a necessity for providing the best care to others. Designing

BANNER ESTRELLA MEDICAL CENTER - PHOENIX ARIZONA

MORE WAYS TO BREATHE EASIER INDOORS
1. Invest in an air purifier (or two). Look for models with true HEPA filters and activated carbon layers. Place one in your bedroom and one in your main living or workspace, where you spend the most time. For offices with shared air systems, a desktop purifier can help reduce personal exposure.
2. Monitor indoor air quality. Small sensors now track PM2.5, VOCs, CO2 levels, and humidity. Devices like Airthings, Awair, or even smart thermostats can give real-time data to guide when to ventilate, purify, or dehumidify.
3. Maintain ideal humidity levels (30–50%). Too dry, and the nasal passages get irritated; too moist, and you invite mold and dust mites. A small humidifier or dehumidifier can help regulate this balance, especially in older buildings with poor insulation.
4. Reduce VOC exposure. Many cleaning products, air fresheners, and even new furniture off-gas volatile organic compounds (VOCs). Opt for fragrance-free, low-VOC products when possible, and air out new purchases before bringing them into living spaces.
5. Keep shoes at the door.
A simple habit that prevents outdoor allergens, pollutants, and microbes from being tracked through the house. Especially helpful if you’re treating patients in a variety of environments.
6. Use vent fans regularly.
In kitchens, bathrooms, and laundry rooms, this helps control humidity, reduces VOC buildup from cooking, and prevents mold growth.
7. Schedule HVAC maintenance.
At least once a year, have a technician inspect, clean, and tune up your system. Dirty ducts and coils can circulate dust, mold, and allergens without anyone noticing.


Holistic Education for a Changing World
A CALLING ROOTED IN FAMILY AND SERVICE
Dr. Kemper has worked at Midwestern University for 22 years and has been serving as the Dean of the Arizona College of Osteopathic Medicine (AZCOM) since 2007. She is also the Chair of the Professional Education Committee and a past President of the Arizona Osteopathic Medical Association.
Her path to medicine began in childhood, when she found the texts and notes of her grandfather, who was a physician. Though she had never met him in person, she pored over the books and knew she wanted to explore her own career in healthcare.
She further refined her interest, choosing osteopathic medicine when she saw how the holistic approach helped her mother recover from a particularly difficult car accident.
Following medical school, Dr. Kemper began her career with the National Health Service Corps, establishing a medical family practice in Tempe and providing care for underserved populations in Phoenix.
She invested in teaching opportunities from the beginning, widening her circle of impact by taking on students at her practice, and then establishing a family medical residency at Tempe St. Luke’s Hospital, where she also served as Director of Medical Education.
“I felt like I needed to pay it forward,” she said. “People had done that for me, so I needed to do it for them.”
Since joining Midwestern University’s Arizona campus in 2001 and becoming Dean of AZCOM in 2007, Dr. Kemper has led a curriculum and culture that prepares future osteopathic physicians to meet both the technical and interpersonal demands of modern healthcare.
EDUCATING THE WHOLE PHYSICIAN FOR WHOLE-PERSON CARE
At the heart of AZCOM’s philosophy is a comprehensive, patient-centered approach. Students receive rigorous biomedical training alongside instruction in osteopathic principles, communication, and ethics.
“Osteopathic philosophy is that the body has an inherent ability to heal itself,” Dr. Kemper said. “Each person is a body, mind, and spirit.”
And a community is no different, she said.
“Treating a community holistically makes just as much sense as treating an individual holistically—you need to take all factors into account: environment, history, genetics, culture, and faith.”
AZCOM serves its community by prioritizing a variety of education, outreach, and service-based programs.
“The thing that I really love the most about being Dean is, I see students come in whose dream was to be a physician, and I see them graduate years later and they have actually become what they wanted to be.”

One example is Health Outreach Through Medicine and Education (HOME). Students go out with supervisory faculty to care and provide education for the Valley’s unhoused population.
AZCOM also does extensive outreach at the high school level, shedding light on the pathways to a career in healthcare.
“We bring them on campus, and they get to do a sort of mini medical school,” Dr. Kemper said. “That’s a really great program, and it’s fun to see the next generation.”
With clinical rotations beginning in the third year, AZCOM students are embedded in a wide range of healthcare settings, allowing them to translate their classroom education into real-world application.
AZCOM nurtures strong partnerships and affiliations with community-based physicians and healthcare centers to provide meaningful clinical training.
Partnerships such as the Abrazo Family Medicine
Residency clinic located on the Abrazo Central Campus in north central Phoenix; and the HonorHealth Mountain Vista Medical Center, Family Medicine Residency in the east valley of the Phoenix metro area are vital in developing confident, compassionate physicians.
Arizona’s current and anticipated shortage of primary care physicians is a growing concern that places a significant toll on both physicians and patients. Additional Graduate Medical Education funding for in-state residency spots is a high priority for organizations like AZCOM who are working to address these shortages.
“It hurts everybody, the shortage of family medicine,” she said.
“It hurts the patients that can't find care; it hurts the patients that feel they're not getting the care they want because their doctors are too busy; it hurts the physicians like crazy because they are overworked and have a way larger patient load than they need; Burnout gets to be huge—it’s a crisis.”

Dr. Kemper said that about half of AZCOM’s students graduate into primary care, and about one third of graduating students match in Arizona.
In addition to residency spots in the Valley, AZCOM also sponsors residencies in rural Arizona communities, as well as requiring all students to complete a rural rotation.
“We want them to taste that part of practice, because you will never choose a rural community if you don’t realize it’s a lovely way to live your life,” she said.
EQUIPPING STUDENTS FOR A TECHNOLOGICAL AND TRUST-CHALLENGED ERA
Medical education has changed dramatically in the last decades and so have the challenges facing today’s students.
Integrating technological advancements, database management, and the potential presented by recent AI developments is a necessary adjustment in preparing today’s medical students to be knowledgeable yet flexible as they face a future of increasing uncertainty.
One program AZCOM has been piloting recently is C3DO, a National Board of Osteopathic Medicine project for on-campus standardized assessment of fundamental clinical skills.
During the COVID-19 Pandemic clinical hands-on assessments were removed, to preserve isolation and virtual education needs.
While this may have been a necessary step, Dr. Kemper shared her concern that this may have negatively impacted physicians, graduating them without some of the patient interaction skills they need. She hopes that tools and programs like C3DO could help students develop and demonstrate the required skills.
COVID-19 also brought with it a wave of misinformation that has swept away the average patient’s trust, widening the gap between physicians and patients.
“I think a lot changed, and we are trying to back to where doctors are respected,” Dr. Kemper said. “It’s very hard to earn trust and very easy to lose it.”
Clear communication, strong interpersonal skills, and prioritizing the doctor-patient relationship as one of teamwork will be core elements in rebuilding that trust.
AZCOM curriculum is evolving to meet these training needs with a new generation of students who may not have the experience interacting with others in the same way that they are expected to once they enter the workforce.

“We need to show them what it looks like to develop professionally,” Dr. Kemper said. “They need to communicate in a way that’s understandable using basic language, not slang.”
And, with electronic medical recording dominating so much of physician’s time both in and out of the office, modeling ways to connect and communicate with patients around technology will be key in building relationships.
She shared several examples of phrases physicians can implement to bring the patient to your side of the screen. Things like asking the patient if you can take a moment to confirm a drug interaction or turning the laptop screen toward the patient during consultation.
“That is what we are trying to teach students,” she said. “Because then technology is a tool that you can use with the patients. You can sit down next to them and say, let’s look at this together.”
“It’s a piece that that we, as older physicians, had to learn, and we want the younger generation to learn so their patients feel heard and seen and cared about,” Dr. Kemper said.


for pain medicine. Week after week, she saw plane after plane of wounded service members arrive.
“I must have placed thousands of nerve blocks, and hundreds of catheters,” she said.
Following residency, she served as a staff anesthesiologist in Okinawa and Rota, Spain, and deployed to Djibouti in support of Operation Enduring Freedom.
“I opened and ran acute pain clinics to help prevent us from needing to send people back to the United States for care,” she said.
After her military service, Dr. Penhollow chose to sub-specialize in pain management and chose the Stanford University School of Medicine program for its biopsychosocial model—a multidisciplinary approach aligned with her philosophy.
“I like the integrative conferences where we would have physical therapy, occupational therapy, pain psych and the pain doctors there for each new patient, to look at everything from all of those angles,” she explained.
“ ”
“As an anesthesiologist, I’ve spent years understanding pain better. As a regenerative pain specialist, I focus on healing, not masking symptoms. My military background instilled in me the discipline to seek the highest standards in everything I do, and that carries into this practice.”
But when she entered the traditional, insurance-based pain medicine world, she found it fundamentally misaligned with her values. Working in a high-volume orthopedic group, she felt constrained by a system that prioritized procedures over patient care.
“I felt like I was bartering—I would continue to do destructive procedures, and patients would continue to get opioid prescriptions,” she said.
“I know I don’t belong in that churn and burn sick care system, and I would rather quit medicine than be a part of that kind of pain medicine.”
So, she walked away. And, after a period of regrouping while practicing anesthesiology, she eventually launched her own private practice—on her own terms.
A PRACTICE BUILT ON ETHICS AND PRECISION
At Precision Regenerative Medicine, Dr. Penhollow has created a space where time, transparency, and trust take precedence. Her direct-pay model allows her to bypass the limitations of insurance and focus on whole-body treatment.
She subleases a modest office and employs a single remote staffer to handle calls. Everything else she does herself.
“I’m able to spend the quality time with my patients that I believe they deserve, and that regenerative medicine requires, because it is a partnership,” she said.
She treats a range of injuries and conditions: from acute hamstring and quad tears in athletes to mild and advanced osteoarthritis, disc injuries, rotator cuff issues, and tendinopathies like tennis or golfer’s elbow.
Traditional insurance often limits treatment to one region at a time, she explained, but pain rarely respects anatomical boundaries.
“If you have knee pain, you can’t not look up the chain to the hip and the spine,” she emphasized. “You can’t not look down the chain to the ankle.”
“We also address inflammation, sleep, mood, all these things go together because this is whole-body treatment.”
Direct primary care and specialty care models are growing in popularity in response to an increasingly cumbersome healthcare system that has allowed insurance executives to dictate care, shunting the burden onto physicians and their patients.
For other physicians thinking of pursuing direct-pay models for their practice, Dr. Penhollow emphasized the importance of taking the time to prepare and build a foundation of savings or funding, so that you can make the switch all at once.
Attempts to make the change “gradually” leave physicians grappling with the inherent duplicity of a hybrid model, as they try to determine who and where to charge for what, and when.
Finding mentors, building community, and considering multi-specialty collaborations can provide additional support.
“I love contributing to and leading in a field that is health-focused and improves quality of life and longevity. I help active adults regain mobility and function without surgery, using regenerative medicine tailored to their needs. But I’m also here to disrupt the status quo.”
REGENERATIVE ORTHOBIOLOGICS AS CONSTRUCTIVE CARE
Chronic pain affects over 51 million U.S. adults, with 17 million experiencing high-impact chronic pain that limits daily activity.
“Simply put, and I know this won’t win me friends,” Dr. Penhollow said, “traditional pain management is destructive.”
“Regenerative orthobiologics is constructive,” she emphasized. For example, radiofrequency ablation—a common pain treatment—can lead to nerve denervation, muscle atrophy, and spinal instability. Regenerative medicine aims to intervene early and optimize healing rather than mask symptoms.
While regenerative orthobiologic therapies such as Platelet Rich Plasma had their start in professional athletics, Dr. Penhollow’s patients range from athletes to grandparents to weekend warriors.
“I believe we’re all an athlete, we all have that within us,” she said. “Maybe it’s dormant, maybe it’s something you’re ready to reengage with, maybe you’re motivated by what’s going on in your life right now.”
Not every patient is a candidate for regenerative treatment. Dr. Penhollow described the ideal patient for her practice as someone who wants to be an engaged and active participant.
Some patients may expect medical treatment to be a simple matter of an office visit, a procedure, and a prescription. But cell regeneration takes preparation and time, and holistic healing can’t be short-changed.
“This is not magic,” Dr. Penhollow says. “It takes hard work; it takes changes to your lifestyle. You need to commit.”
LIVING THE PHILOSOPHY
Dr. Penhollow doesn’t just advocate for whole-body wellness, she lives it. An avid hiker, gardener, and yogi, she stays active not just to maintain health, but to stay grounded and energized in her work. Outside the clinic, she’s also a French-trained home chef and an aspiring sommelier, constantly exploring new ways to bring joy, creativity, and connection into her life.
“Clinics prioritize marketing over medicine, offering one size fits all injections without proper evaluation or long-term strategy, and that’s not regenerative medicine. It’s just hope in a syringe. So, I call out that misinformation I expose unregulated and unethical regenerative practice, and that’s what motivates me.”
Balancing her personal and professional world isn’t just a goal, it’s part of the same philosophy she shares with her patients: that healing and health come from intention, movement, and meaning.
“For me, it’s about doing things I love with people I love, and that balances the intensity of the business,” she said.
FIGHTING MISINFORMATION, AND DEFINING THE FIELD
With regenerative medicine gaining popularity, the field has also become vulnerable to hype and exploitation. Misinformation and scam treatments proliferate online, endangering patients and discrediting legitimate practitioners.
Dr. Penhollow is working to raise the bar.
She’s not just pushing back against misinformation— she’s actively shaping the future of the field. She is an advisory board member of The Orthobiologic Institute (TOBI). She also teaches hands-on labs to physicians learning bone marrow aspiration, lectures to both medical audiences and the general public, and addresses often-overlooked topics like menopause-related frozen shoulder and musculoskeletal health in women.
“My mission is to define regenerative medicine through innovation, integrity, and individualized care,” she said.
She also stays active in teaching as an instructor in anesthesiology for the Mayo Clinic College of Medicine and Science, and as a supplemental consultant for the Department of Anesthesiology & Perioperative Medicine at Mayo Clinic Phoenix.
In addition to clinical care and medical education, she runs an educational YouTube channel to help patients understand the science of regenerative medicine, vet providers, and make safe choices.
“Precision medicine and orthobiologics isn’t just about offering the treatments,” Dr. Penhollow said. “It’s about setting the ethical standard in a field where misinformation thrives.”
Social media use has become a ubiquitous and necessary element of both personal and professional life but speaking up on these platforms can still be intimidating. Physicians are subjected to additional scrutiny as they face ethical, licensing, and legal risks with their channels.
These risks can be mitigated through a variety of safeguards and strategies, and the potential benefits for education and professional development make it a risk worth taking.
Dr. Penhollow began her own YouTube journey as a continuation of her educational efforts, because she knew that online was a space where she could reach the most potential patients.
She encourages more physicians to join her in the digital space. “We have the authority, we have the training, but we often don’t have the reach,” she noted.
“We should be the ones they are listening to,” she said. “Physicians should be the ones who drown out the hype, the ones in front of people scrolling on Reddit and Facebook.”
She recommends that physicians interested in joining the digital fight against misinformation find a mentor to help them navigate the unfamiliar landscape.
“I have a coach, and she has 175 thousand followers, and she is making quite a bit of waves in the industry, and she is known as the expert,” she said.
She echoed the much-shared advice: do it scared.
“You just need to start. We don’t go with perfectionism, we start,” she said. “Patients enjoy seeing a human rather than a robot, particularly in the time of AI.”
THE FUTURE OF REGENERATIVE MEDICINE
One of the most exciting developments in regenerative medicine today for Dr. Penhollow is the ability to customize PRP and BMAC injections based on patient biology and data.
Both PRP and BMAC are alternate therapies designed to harness the body’s naturally occurring healing processes. Patient blood or bone marrow fluid is drawn and processed, concentrating growth factors, proteins, and platelets that can then be re-injected to accelerate healing and reduce inflammation.
Evidence shows that the optimal platelet count for large-joint PRP is around 10 billion. For BMAC, the target is 4,500 colony-forming units per fibroblast.
Using advanced testing, Dr. Penhollow can establish a patient’s baseline and calculate exactly how much blood, or bone marrow, to draw to reach that target.
Technique matters, from the size of the syringe to the draw speed and depth. So does delivery.
“You can’t overstate the importance of treatments by somebody who’s well-trained, collecting enough blood
Learn more about Dr. Penhollow and her medical journey by visiting arizonaphysician.com/tammy-penhollow-do.

or bone marrow with outstanding technique, and then delivering it with fluoroscopy or ultrasound guidance,” Dr. Penhollow emphasized.
These new developments in the field enable physicians to customize effective treatments for their patients with increased accuracy and more reliable results.
You can say to the patient, “given all the findings about you, given my results based on all the data that’s collected, I can predict this type of outcome for you,” Dr. Penhollow said. “And I think that’s exciting.”
She’s also keeping a close eye on treatments involving cultured mesenchymal stem cells, still in the earlier stages of research and development.
“I think it’s going to allow us to reach people with more severe injuries,” she explained. “So, I think that’s really exciting, coming down the pipeline.”
A CALLING BEYOND THE CLINIC
For Dr. Penhollow, medicine is more than a profession, it’s a calling that demands precision, courage, and conviction. Whether she’s treating a patient, mentoring a peer, or standing at a podium, she brings the same
unflinching dedication to evidence-based care and ethical integrity.
In a healthcare landscape too often shaped by profit-driven systems and misinformation, she has chosen a different path—one built on transparency, trust, and truth. She’s not only building a practice that reflects her values; she’s helping shape an entire field so that others can do the same.
“Because patients deserve more than the hype, they deserve results backed by science,” Dr. Penhollow said.
Dr. Penhollow’s story is a reminder that meaningful change doesn’t come from waiting. It comes from showing up, speaking out, and doing the hard work every day. ■

By Dominique Perkins Associate Editor Arizona Physician azphysician@mcmsonline.com
PIONEERING CARE THROUGH TEAMWORK AND INNOVATION
GOING IN DEPTH: ASSOCIATED RETINA CONSULTANTS
Vision is one of our most cherished senses, and for millions, its loss can profoundly impact daily life. At Associated Retina Consultants (ARC), patients with complex eye conditions benefit from pioneering research, state-of-the-art technology, and an unwavering commitment to personalized care.
We sat down with Dr. Benjamin Bakall, director of clinical research and the Inherited Retinal Disease Clinic, to discuss ARC's team of specialists and their dedication to providing advanced treatments while maintaining a patient-centered approach.
A LEADER IN RETINA CARE
Dr. Bakall brings a wealth of expertise to ARC. Originally from Sweden, he completed his medical training and earned a PhD in genetic retinal disease at Uppsala University. His journey led him to the University of Arizona for an ophthalmology residency and then to the University of Iowa for a medical retina fellowship. Today, Dr. Bakall oversees numerous clinical trials and leads innovations in retinal treatments.



SERVING A DIVERSE ARIZONA POPULATION
For over 50 years, ARC has been at the forefront of retinal care in Arizona. Founded in 1974, the practice has grown into the state's largest independently owned retina-only private practice, serving patients throughout the region.
Ophthalmology, like many specialties, faces physician shortages, particularly in Arizona. ARC addresses this need by offering treatments for a broad range of conditions, from cataract surgery to retinal detachments, macular holes, epiretinal membranes, and uveitis—everything from tears to tumors.
Dr. Bakall specializes in inherited eye diseases, some of which are extremely rare. For example, retinitis pigmentosa, a genetic disorder affecting 1 in 30,000 people, is one of the most common yet rare retinal diseases.
“
“I personally enjoy being a retina specialist with the high level of complexity of diseases and the diagnostic challenges combined with the fascinating research and emerging pipeline of novel treatments.”
The most common cases at ARC involve age-related macular degeneration (AMD), a condition that blurs central vision as the macula is damaged by aging. According to the National Eye Institute, AMD is the leading cause of vision loss in older adults.
Treating this condition, and others, in Arizona presents a unique challenge due to the state’s significant "Snowbird" population—patients who split their time between Arizona and other states. This migrating patient base complicates coordination with out-of-state primary care providers, insurance companies, and various administrative tasks.
ARC has developed effective communication strategies to overcome these challenges, ensuring patients receive the coordinated care they need in a timely manner.
“I think we are really good at sending out notes,” Dr. Bakall said, noting that receiving notes from other providers is often more challenging.

ADVANCING RETINA TECHNOLOGY AND RESEARCH
Ophthalmology, especially retina care, is highly technology-driven, and advancements in imaging have revolutionized the ability to diagnose and treat patients.
“We can really see minute pathology, and that helps us to guide treatment,” Dr. Bakall said.
ARC employs dedicated ophthalmic photographers and technicians who manage specialized imaging and testing, including photos, cross-sectional scans, ultrasounds, angiography, and electroretinograms, among others. This comprehensive diagnostic approach allows ARC to deliver precise and personalized care.
Beyond clinical care, ARC is also deeply committed to patient education. Through outreach initiatives, the team provides patients and their families
“We think it's really important that we're there to prevent vision loss and keep people's vision going, because that’s crucial to be able to have an enjoyable life.”
“ ”
with resources to manage progressive vision loss, stay informed about new treatments, and learn strategies for coping with reduced vision.
Physicians and associates participate in monthly health expos, provide community resources on retinal health, and give talks at assisted living centers. They also host continued medical education events and conduct training for other eye care providers.
A lifelong passion for Dr. Bakall, research is a central focus at ARC.
In addition to his role as director of clinical research, he also serves as the president for the Retina Research Foundation of America, a nonprofit dedicated to advancing education and novel research in retinal diseases.
Since Dr. Bakall took on the role of research director, the number of clinical trials at ARC has expanded significantly. “I think this year we’re going to have over 20 active clinical studies for retina diseases,” he says.
These trials include promising gene therapies that are increasingly being explored for conditions like Wet Age-Related Macular Degeneration (Wet AMD).
Wet AMD is a leading cause of central vision loss in older adults, and while current treatments involve monthly injections, ARC’s research into gene therapy aims to offer longterm solutions that could manage the condition with a single injection.
With several new FDA-approved treatments already in use, Dr. Bakall is excited about the rapid pace of advancements in the field. ARC remains at the forefront of these innovations, continuously pushing the boundaries of what’s possible in retinal care.
As ARC continues to lead the way in retina care, their dedication to advancing treatments, fostering collaboration, and supporting both their patients and staff remains unwavering. With a forwardthinking approach to research and a compassionate, patient-centered philosophy, ARC is not just shaping the future of retinal care in Arizona—it is transforming the lives of countless individuals. As they move ahead, their commitment to excellence and innovation promises to ensure that patients receive the highest standard of care for years to come, further cementing ARC’s legacy as a pillar of vision health in the community. ■

By Dominique Perkins Associate Editor Arizona Physician azphysician@mcmsonline.com

Associated Retina Consultants
BY THE NUMBERS
Services Provided
Diagnostic Testing, retinal surgery, inherited retinal disease, ocular tumors, eyedaptic glasses, and clinical trials.
Conditions Treated
Age related macular degeneration, retinopathy, chorioretinopathy, choroidal nevus, diabetic retinopathy, flashes & floaters (pvd), low vision, macular edema, macular holes & puckers, ocular tumors, photodynamic therapy, retinal artery occlusion, and uveitis.
13 Locations
Phoenix, Casa Grande, Cottonwood, Flagstaff, Gilbert, Goodyear, Mesa, Payson, Peoria, Prescott, Prescott Valley, Scottsdale, and Sedona
Connect with ARC

DR. ROBERT KRAVETZ
A LIFE IN MEDICINE, A LEGACY IN HUMANITY
Some doctors leave a legacy in textbooks or on hospital walls. Dr. Robert Kravetz’s legacy lives in glass display cases, lecture halls, and the grateful memories of patients and students alike.
A retired bioethicist, gastroenterologist, collector of medical antiques, and beloved medical historian, Dr. Robert Kravetz, MD, embodies the golden era of American medicine while offering a thoughtful critique of the modern system. His story is a window into what medicine once was— and a guidepost for what it still can be.
AN EARLY CALLING AND A LASTING CONTRIBUTION
Dr. Kravetz found his passion, and his talent, for medicine early on.
He greatly admired his uncle, who was a general practitioner. And as an Eagle scout he became very adept at first aid, winning tournaments and eventually becoming an instructor.
He entered medical school at the end of his third year of college, to avoid a language requirement he obstinately didn’t want to take.
“I tell my grandchildren I’m not a college graduate,” he said, laughing. “Isn’t that so strange to think?”
He attended New York University School of Medicine and completed a fellowship in gastroenterology at Yale New Haven Medical Center.
“I tell all my students three things: we’re in this room to learn; we’re in this room to laugh and have lots of fun; and we’re in this room to leave all of your stress and anxiety in the hallway.”
Given the scope of his career, from private practice to education, Dr. Kravetz is uniquely positioned to comment on the significant changes in medical school education over the last decades.
Lectures, lab, and general coursework filled the entirety of his first two years at medical school in 1956. He didn’t see any patients until his third and fourth year, during clinical rotation.
Today’s medical students begin training in doctoring in their first and second year, often pairing with a community physician mentor to learn communication and clinical skills and to gain early exposure to patient care.
“I think it’s better that they start seeing patients early, because then you can correlate your learning with the patients,” he said. “But I would still change a lot.”

Dr. Kravetz joined the faculty of the University of Arizona College of Medicine—Phoenix, where he currently teaches clinical medicine to first- and second-year students. Dr. Kravetz also teaches medical history to fourth-year students, which marries two of his greatest passions: medical education and medical history.
Dr. Kravetz gifts each of his history students a medical antique from his collection, selected for their chosen specialty to guide their research— and to start collections of their own.
A COLLECTOR OF STORIES AND SCIENCE
The first antique Dr. Kravetz purchased was a small porcelain toothpaste jar he found in a thrift store for 25 cents. A humble start to what has become the largest collection of medical and apothecary artifacts in the southwest.
“The antiques represent a window into the past and represent how far we have come in medical diagnosis and treatment,” Dr. Kravetz said.
During a fateful visit to a small New England town, he found a drug store that dated back to 1840. When he asked the owners if they had any old items he could see, they handed him the key to a storage room and told him to have a look.
“It was antique heaven!” he said. He purchased the entire collection on the spot, rented a large moving van, and drove away with 60 crates filled with 130 years of history.
A few of his all-time favorite finds through the years: a drug chest from the revolutionary war; a complete amputation kit from the civil war; a 16thcentury Delf drug jar that he found someone using as a pencil holder; and a leech jar that he purchased from a drug store in Las Vegas for $250 and later sold at auction for $6,000.
For Dr. Kravetz, each artifact is more than an object—it’s a story, a legacy, and a reminder that medicine is built on human experience.
His donated collection is displayed in 40 cases at locations across the Valley, including Abrazo Central, Encompass Health, The Legacy Foundation, a museum of medical history at the University of Arizona College of Medicine—Phoenix, and at the Maricopa County Medical Society, where he has been a member since he first arrived in Arizona in 1965.



The first antique Dr. Kravetz ever purchased. Though he did sell it at one point, he later bought it back for its sentimental value as the beginning of his collection.
“Watching medicine over six decades, one sees the rise and fall of many theories, diagnoses, and treatments.”

He was assigned to the Phoenix Indian Hospital through the Public Health Service and started his own practice shortly thereafter.
The years he practiced have been considered by many to be the golden years of medicine – full of remarkable breakthroughs in research and technology, combined with physician autonomy and financial independence.
The breakthrough that had the most dramatic impact on his practice was the introduction of fiberoptic endoscopy—an innovation that transformed gastroenterology diagnostics and therapeutics.
“We had rigid scopes; they were made of steel,” he recalled. “It was like swallowing a sword.” Fiberoptic technology made the procedure more comfortable, more accurate, and more widely accessible, offering a clear view into the body that was once impossible.
A PHILOSOPHY OF CARE
Even as new technologies reshaped clinical practice, Dr. Kravetz never lost sight of medicine’s deeper purpose. His approach was shaped not only by technical innovation, but by a humanistic model of care that placed compassion and dignity at the heart of the physician-patient relationship.
“I was fortunate to have trained with three of the most prominent humanists in medicine during my formative years,” he said, naming Dr. Lewis Thomas, celebrated author and mid-century physician-humanist, Dr. Edmund Pellegrino, a founding figure in modern medical ethics, and Dr. Howard Spiro, professor emeritus of medicine and founder of the Program for Humanities in Medicine at Yale School of Medicine.
Humanism is a philosophical movement that began during the Renaissance and has been at the core of the medical profession since its inception. The ideology positions human beings as essentially good and capable of great improvement through reason and learning. Human life and dignity are highly valued, and technology is considered essential for solving problems.
Throughout Dr. Kravetz’s career he has been a strong voice for preserving humanism in medicine, particularly through his book, Medical Humanism: Aphorisms from the Bedside Teachings & Writings of Howard M. Spiro, MD
Dr. Kravetz remembers a time when initial consultations with new patients were scheduled for a full hour.
Today, however, corporate interests have leaked into the noble practice of medicine, robbing physicians of

autonomy, time with their patients, reimbursement, and public trust.
A broad sweep of misinformation, particularly in the wake of the COVID-19 pandemic, has further eroded public trust in physicians, experts, and in essential medical innovations such as vaccines.
Physicians everywhere are working to re-forge that trust and build connection with their patients in the little time they have.
“Every doctor should develop their own little technique,” Dr. Kravetz recommends. One of his? Moving his chair to sit beside patients as they talked.
“If there wasn’t a chair in the room, I would go get one,” he said.
Taking an extra moment to ask about a patient’s day, making eye contact, a handshake, a personal farewell, small gestures can have significant impact.
A PHYSICIAN’S ENDURING TOUCH
After more than five decades in medicine, Dr. Kravetz has turned his attention to teaching, curating, and tending to the roots—both literal and figurative—of a profession he has always loved.
His impact is woven through generations of students, the artifacts of medical history, and a philosophy that centers human dignity in care. Even in retirement, Dr. Kravetz continues to shape the future of medicine through his teaching and mentorship.
In a healthcare system often defined by speed and metrics, his legacy reminds us to slow down, sit beside our patients, and listen. ■

By Dominique Perkins Associate Editor Arizona Physician azphysician@mcmsonline.com

“When physicians can reclaim autonomy and independence, they can practice medicine with joy.”
physician at the VA. As her career progressed, she realized her limited voice and little control over her schedules and patients were leaving her feeling frustrated and disconnected from her goals as a physician.
“While I love the medicine and pathophysiology of the disease process in the hospital setting—because you can see everything work faster—I realized that the only longitudinal whole person care gave me that true lasting joy of being able to change the course of someone’s life for the better.” she said.
She started asking herself, if I had my own voice and ability to make a change, what would I do?
And after careful planning and preparation, she opened Build Health MD, a membershipmedicine practice, in 2024.
“My frustration resolved the moment I decided to start my own practice,” she said. “In one sweep, the membership medicine model removes the bureaucracy and the barriers to effective, efficient care.”
She sees most of her patients monthly and enjoys the flexibility this gives her to personalize the care each patient receives. Even going so far as to include yoga and fitness training for patients trying to increase their strength and mobility.
NAVIGATING THE DIRECT-PAY MODEL
Direct pay healthcare models are not new, but in the last few decades they have become a steadily growing trend in the healthcare landscape as both patients and physicians search for a path through the murk of insurance

payment models, and being able to deliver the care in a way that’s appropriate to the issue at stake—whether it’s by phone, video, clinic, home, or a café.”
THE REWARDS OF RECLAIMING PRIMARY CARE
For others considering transitioning to a membershipbased practice model, Dr. Nachiappan shared a little of her own experience in navigating business challenges.
“It’s not as flashy as, ‘Drop 10 pounds and glow by lunchtime,’” she laughed. “But real health isn’t a quick fix—it’s a journey. And while slow, life-changing medicine isn’t always the easiest sell, it’s the only kind that truly lasts.”
Though it will take longer to find the patients who truly value what you offer, she promises it is worth it.
“Then you do form long-term relationships,” she said. “And you can sleep better knowing that you actually helped and touched people’s lives.”
Another business strategy Dr. Nachiappan has employed in her practice is to require a minimum contract length, at least initially.
This ensures she will have the time to fully address and resolve her patient’s issues and enjoy the longitudinal care that she has found to be so rewarding.
She shared an experience early in her practice’s formation when she made an exception: a patient came in requesting a solo consultation. It seemed both straightforward and urgent, not to mention she was just starting out and could use the business, so she capitulated.
After performing the exam and giving her recommendations, the patient left. But days later she found herself still thinking about that patient, plagued with questions:
Did it get better? Worse? Did they know what next steps they need to take? Had they turned up in an emergency room somewhere since leaving her “one time visit”?
“It made me worried,” she said.
So much so that she finally made a follow-up call providing additional consultation, and then another, and another.
“I realized: this does not work,” she said of “one-time” care. “I’m better off being a primary care physician.”
This realization solidified her identity and strengthened her practice.
“I love my job as a primary care physician at Build Health, MD,” she said. “And because the focus is on building health for life, I get to live my calling every day. Helping patients create healthier, fuller lives is the most rewarding part of all”. ■

By Dominique Perkins Associate Editor Arizona Physician azphysician@mcmsonline.com
Mental Wellness in Medicine
Simple Strategies to Transform Patient Care and Physician Well-Being
As a military and civilian Primary Care Physician (PCP), I have witnessed firsthand the profound impact mental health has on both individual well-being and the healthcare system at large. Mental health is not a peripheral concern; it is central to our collective ability to provide compassionate, effective care. Yet, despite its importance, mental health remains underprioritized in many clinical settings. Arizona Physicians are on the front lines, and we play a critical role in integrating mental wellness into everyday practice.
THE INTERSECTION OF
MENTAL HEALTH AND PUBLIC HEALTH
The mental health of healthcare providers and patients alike is inextricably linked to public health outcomes. Research shows that untreated mental health conditions such as anxiety and depression exacerbate chronic illnesses, increase healthcare costs, and reduce quality of life for patients. For physicians, burnout, compassion fatigue, and depression are not just personal challenges, they are systemic issues that compromise patient safety and care quality. Alarmingly, an estimated 300400 physicians die by suicide annually in the U.S., underscoring the urgency of addressing mental wellness within our own profession.
As Arizona continues to face challenges such as provider shortages and increasing patient demand, prioritizing mental health is not just ethical, it is essential for sustaining our healthcare workforce and improving patient outcomes.


THREE SIMPLE STRATEGIES TO INCORPORATE MENTAL WELLNESS CHECKS
Physicians are uniquely positioned to identify early signs of mental health challenges in their patients. Here are three practical ways you can integrate mental wellness checks into your practice:
NORMALIZE MENTAL HEALTH
DISCUSSIONS Begin every patient visit with a brief mental health check-in. Simple questions like, “How have you been feeling emotionally?” or “Have you noticed changes in your sleep or mood?” can open the door to meaningful conversations. Tools such as the Patient Health Questionnaire (PHQ-9) or Generalized Anxiety Disorder (GAD-7) scale can be seamlessly integrated into intake forms for more structured screening and tracked longitudinally to assess progress.
LEVERAGE COLLABORATIVE
CARE MODELS
Behavioral health integration (BHI) is a proven approach to addressing mental health needs alongside physical health care. By embedding behavioral health specialists within your practice or establishing referral pathways with local mental health providers, you can ensure patients receive timely, coordinated care. This model also reduces stigma by framing mental health as an integral part of overall wellness.
PROMOTE SELF-CARE AMONG YOUR TEAM
Physicians cannot pour from an empty cup. Encourage mindfulness practices, peer support groups, or even brief “mental wellness huddles” during shifts for your colleagues and staff. Leading by example—whether through practicing mindfulness yourself or openly discussing challenges—can foster a culture where seeking help is normalized rather than stigmatized.
WHY THIS MATTERS NOW
Mental health is often described as the “invisible epidemic,” but its effects are anything but invisible. In Arizona, where access to behavioral health services can be limited due to rural geography and provider shortages, primary care physicians often serve as the first (and sometimes only) line of defense against mental illness. By incorporating these simple strategies into your practice, you can make a profound difference in your patients’ lives while also protecting your own well-being.
A CALL TO ACTION
As physicians, we have both the privilege and responsibility to lead by example when it comes to prioritizing mental wellness. I urge you to act today:
Start small by asking one new question about mental health during patient visits.
Advocate for system-wide changes that integrate behavioral health into primary care.
Commit yourself to your own self-care and encourage your colleagues to do the same.
Together, we can create a healthcare environment that values mental wellness just as much as physical health, a shift that will benefit not only our patients but also ourselves and our profession. Let us rise to this challenge with the same dedication we bring to every other aspect of care. The time for change is now. ■

By Lt. Col. Zaid Fadul, MD, FS, FAAFP MCMS Board President 2023
Why Email Marketing Matters for Physicians
ENHANCING PATIENT COMMUNICATION AND GROWING YOUR PRACTICE
In today’s digitally driven healthcare environment, physicians face increasing pressure to deliver exceptional care and connect meaningfully with patients outside their clinic. While patient care remains the priority, building a thriving practice also requires clear, consistent communication, and email marketing offers one of the most effective, low-cost ways to do just that.
Whether you run a private practice, a specialty clinic, or are part of a more extensive healthcare network, email marketing can help educate patients, boost engagement, foster loyalty, and grow your practice.
THE RISE OF PATIENT-CENTERED COMMUNICATION
Today’s patients are more informed and digitally savvy and expect proactive, personalized communication from their providers. They want updates about their health, appointment reminders, and answers to frequently asked questions delivered quickly and conveniently.
Email marketing gives you the tools to meet those expectations in a HIPAA-compliant, scalable way. It helps physicians build trust, strengthen relationships, and keep patients engaged and informed throughout their healthcare journey.
WHY PHYSICIANS SHOULD CONSIDER EMAIL MARKETING
Here are seven reasons why email marketing is worth integrating into your practice’s communication strategy:
1. Email Builds and Maintains
Strong Patient Relationships
Regular emails allow you to stay connected with patients between visits. Whether it’s a monthly

newsletter, post-visit follow-up, or seasonal health tips, your messages reinforce the patient-provider relationship and show you care beyond the exam room. That ongoing touchpoint helps foster loyalty and longterm engagement with your practice.
2. Email Educates and Empowers Patients
One of the greatest values physicians can provide outside of direct care is education. Through email campaigns, you can share:
Preventive care reminders
Answers to common health questions
New treatment options or technologies available in your practice
Tips for managing chronic conditions
Insights on current health topics
This empowers patients to take a more active role in their health, improving outcomes and reducing unnecessary visits.
3. Email Improves Appointment Attendance and Reduces No-Shows
Automated email reminders are a proven way to reduce no-shows and late cancellations. By sending out appointment confirmations, check-in instructions, and reminders a few days before a visit, you’re helping patients plan and stay on track with their care schedules. You can also use email to fill last-minute openings, promote walk-in availability, or encourage patients to schedule annual exams.

Preparing your Patients for Extreme Heat and Poor Air Quality

The American Lung Association is working with physicians, community partners and lung health advocates to support people with lung disease who are facing health complications due to climate change.
Climate change can cause extreme weather and worsen air quality, which can be harmful to the lungs. While everyone is impacted by the negative effects of climate change there are several groups that are particularly affected by poor air quality:
People living with lung disease
Children
Older adults
People of color
People who work outdoors
Physicians play a critical role in helping their patients protect their lung health.
HAVING THE CONVERSATION
Physicians should have discussions with their patients encouraging them to monitor air quality in their homes. Should physicians feel unsure about how to begin a conversation about air quality with their patients, they can try asking open-ended questions like “What do you know about air pollution?,” or they can share a personal story about how air pollution or extreme weather may have affected them.
Part of the conversation can include ways to empower your patients by discussing various methods to protect their lungs when air quality is poor. These actions may include how to check and monitor outdoor air quality using the Air Quality Index (AQI). On days when the AQI is orange, red, purple or maroon, patients should take additional steps like staying hydrated, visiting a cooling center, and limiting time spent outdoors.
Patients who work outdoors, are surrounded by dust, chemicals, fumes or vapors, these exposures may also affect their lungs. Physicians should encourage their patients to take the American Lung Association’s brief five-question assessment to understand how work-related exposures can affect their lung health.
Physicians are critical to raising awareness about the overwhelming health burden caused by poor air quality and climate change. Physicians can access free tools and resources through the Lung Association to improve patient care by:
Hosting the 30-minute training, “The Impact of Poor Air Quality on Patients with Lung Disease,” which builds awareness about air pollution and lung disease and equips providers with resources to improve the care of patients during unhealthy air days. This training is offered to healthcare organizations in Maricopa County. To schedule a training, please contact Maddie.Blair@lung.org.
Implementing sustainable, patient-centered quality improvement practices. Take the “Health System Air Quality Preparedness Assessment,” and upon review, the Lung Association will provide physicians with feedback on their practice’s

current extreme heat and air quality efforts and ways to strengthen them.

When patients living with chronic lung disease are exposed to poor air quality, they may experience more wheezing, coughing, shortness of breath or acute exacerbations. Physicians can empower patients with lung disease and offer additional support and education by:
Explaining how to use a COPD or asthma action plan as a way to monitor their lung disease symptoms and understand the steps to take when symptoms get worse.
Discussing medication-related heat safety tips which include not leaving medication delivery devices like inhalers or oxygen equipment in a hot car or enclosed space.
Sharing information about the American Lung Association’s Lung Health Navigator Program. This program is designed for people living with COPD or asthma and includes free, personalized, one-on-one lung disease education offered over the phone or through virtual platforms like Zoom.
Learn more about climate change advocacy efforts in Arizona and access all the free resources, programs and assessments shared in this article at Lung.org/az-climate. ■

By Maddie Blair, MPH Manager, Nationwide Health Promotions American Lung Association Maddie.blair@lung.org


OVERVIEW | Arizona Advanced Surgery (AAS) provides patients with the highest quality surgical care and the latest surgical techniques. Surgeons at AAS deliver expert surgical care while minimizing disruption to patients’ lives. They routinely perform minimally invasive procedures that dramatically reduce risks and recovery time.
SERVICES AND CONDITIONS TREATED | Bariatric surgery, colon & rectal surgery, general surgery, laparoscopic surgery procedures, plastic surgery, robotic surgery, surgical oncology, trauma surgery, and vascular surgery.
NUMBER OF PHYSICIANS | 45
LOCATIONS | 14 offices in Chandler, Gilbert, Glendale, Goodyear, Mesa, Peoria, Phoenix, Scottsdale, and Surprise
MAIN OFFICE | 2945 S Dobson Rd, Mesa, AZ 85202 480-969-4138
WEBSITE | arizonaadvancedsurgery.com
TOP SPECIALTY | PEDIATRICS

OVERVIEW | Pediatrix physicians and staff focus on the overall well-being of children. They believe each child is a special individual; thus, they consider the specific needs of the child at each visit. Likewise, Pediatrix address parents’ concerns to help families meet the needs of their children. In cases of children with special needs, Pediatrix coordinates referral care from specialists to ensure the process of care moves smoothly for parents. Children not only experience special attention at Pediatrix; they also receive the finest medical care.
SERVICES AND CONDITIONS TREATED | Care of premature infants, care for children with special needs, adolescent care, ADHD management, pediatric nutrition & obesity prevention.
NUMBER OF PHYSICIANS | 8
LOCATIONS | 2 offices in Phoenix (Black Canyon & Happy Valley)
MAIN OFFICE | 15650 N Black Canyon Hwy, STE 100, Phoenix, AZ 85053 | 602-866-0550
WEBSITE | pediatrixmd.com
TOP SPECIALTY | UROGYNECOLOGY

OVERVIEW | As the foremost urogynecology practice in Phoenix, Arizona, Valley Urogynecology Associates offers exemplary care to patients with urinary and gynecologic issues. Valley Urogynecology Associates emphasizes a strong quality of life for every patient. The team offers a variety of treatment options, from conservative nonsurgical care, like lifestyle changes and medication, to advanced treatments, including minimally invasive vaginal surgery and robotic surgery.
SERVICES AND CONDITIONS TREATED | Hysterectomies, urinary incontinence, thermiVA, overactive bladders, fecal incontinence, pelvic organ prolapse, sacral nerve stimulation, bladder Botox, Vesicovaginal fistula, vaginal suspension, rectovaginal fistula, robotic surgery, laparoscopic surgery, and urethral bulking.
NUMBER OF PHYSICIANS | 4
LOCATIONS | 1 office in Phoenix
MAIN OFFICE | 1616 E Maryland Ave, Phoenix, AZ 85016 602-788-1521
WEBSITE | valleyurogynecology.com

OVERVIEW | The doctors at Vascular & Interventional Partners are renowned in the Phoenix area for their knowledge and specialized procedural skills. Our expertise comes from decades of combined experience treating some of the most complex medical conditions in Arizona. Our team’s commitment to improving the health and wellness of our patients has helped us become one of the most respected interventional radiology (IR) divisions in the state.
SERVICES AND CONDITIONS TREATED | Oncology, venous disease, neurovascular, men & women’s health, spine care, dialysis access, Gi interventions, arterial disease treatment, join pain treatment.
NUMBER OF PHYSICIANS | 7
LOCATIONS | 2 offices in Scottsdale and Glendale
MAIN OFFICE | 22455 N Miller Rd #B100, Scottsdale, AZ 85255 | 480-613-3445
WEBSITE | vipinterventional.com
OVERVIEW | Valley ENT is a multi-practice physician group that specializes in otolaryngology, allergy, audiology, and facial plastics. No matter the ear, nose, and throat problem, the physicians and providers at Valley ENT can take care of the problem with expertise and care.
SERVICES AND CONDITIONS TREATED | Adult ENT services, allergies & asthma, facial/cosmetic surgery, snoring & sleep apnea, dizziness & balance, head & neck cancer, swallowing & speech issues, hearing loss & hearing aids, sinus conditions & nasal surgery, thyroid, parathyroid & salivary issues.
NUMBER OF PHYSICIANS | 39
LOCATIONS | 18 offices in Phoenix, Glendale, Chandler, Mesa, Scottsdale, Flagstaff, Green Valley, Sierra Vista, and Tucson
MAIN OFFICE | 9097 E Desert Cove, STE 250, Scottsdale, AZ 85260 | 480-614-0499
WEBSITE | azvent.com
TOP SPECIALTY | NEPHROLOGY

OVERVIEW | DKA physicians are tireless advocates for Arizona patients vulnerable or already suffering from CKD and those experiencing end-stage renal disease (ESRD). Their mission is to meet the varied needs of each patient, provide value and excellence in their care, and work to improve every patient’s quality of life.
SERVICES AND CONDITIONS TREATED | Chronic kidney disease treatment, kidney transplant management, kidney stone management, kidney transplants, dialysis, diabetic neuropathy, hypertension treatment, hematuria.
NUMBER OF PHYSICIANS | 14
LOCATIONS | 16 offices in Phoenix, Avondale, Chandler, Mesa, Casa Grande, Florence, Gilbert, Globe, Lake Havasu, Maricopa, Prescott, San Tan Valley, Show Low, and Sun Lakes.
MAIN OFFICE | 612 W Baseline Rd, Mesa, AZ 85210 480-834-9039
WEBSITE | desertkidney.com

OVERVIEW | DISC is an orthopedic spine center of excellence practice serving spine patients in the greater Phoenix, Arizona area. DISC surgeons treat a wide array of spine conditions such as herniated disc, sciatica, spinal stenosis, and degenerative disc disease. DISC provides compassionate and customized patient care to those suffering in pain.
SERVICES AND CONDITIONS TREATED | Artificial disc replacement, endoscopic spine surgery, selective endoscopic discectomy, endoscopic visualized dorsal rhizotomy, and endoscopic foraminoplasty.
NUMBER OF PHYSICIANS | 5
LOCATIONS | 6 offices in Phoenix, Gilbert, Glendale, and Scottsdale
MAIN OFFICE | 1635 E Myrtle Ave, STE 400, Phoenix, AZ 85020 | 602-944-2900
WEBSITE | sciatica.com

OVERVIEW | AOC provides multiple levels of comprehensive primary ENT care including the diagnosis and management of all diseases of the ears, nose, throat, and sinuses.
SERVICES AND CONDITIONS TREATED | Management of pediatric airway, cancer, skill base surgery, neuro-otology, advanced head & neck surgery, craniofacial surgery, ENT diseases, pediatric otolaryngology, laryngology, endoscopic sinus surgery, audiology & hearing aids, voice & swallowing disorders, thyroid & parathyroid.
NUMBER OF PHYSICIANS | 8
LOCATIONS | 3 offices in Phoenix, Glendale, and Mesa
MAIN OFFICE | 4530 E Shea Blvd, STE 180, AZ 85028 602-264-4834
WEBSITE | aocphysicians.com

OVERVIEW | Associated Retinal Consultants has an experienced team of Arizona eye specialists that diagnose and treat vision problems. Their focus is on the retina and macula (the back of the eye) and the vitreous humor (gel like tissue) in the eye.
SERVICES AND CONDITIONS TREATED | Retinal diseases, ocular oncology, inherited retinal disease, retina surgery, and clinical trials.
NUMBER OF PHYSICIANS | 10
LOCATIONS | 13 offices in Phoenix, Gilbert, Goodyear, Mesa, Scottsdale, Peoria, Prescott Valley, Prescott, Casa Grande, Cottonwood, Flagstaff, Payson, and Sedona.
MAIN OFFICE | 1750 E Glendale Ave, Phoenix, AZ 85020 602-242-4928
WEBSITE | associatedretinalconsultants.com
TOP SPECIALTY | RADIATION ONCOLOGY

OVERVIEW | Radiation Oncologists of Central Arizona, LLP (ROCA) has been offering compassionate, cutting-edge cancer treatment to Valley residents for over 20 years at the premier hospital-based cancer centers in metro Phoenix. ROCA physicians are internationally recognized leaders in advanced radiotherapy technology and have introduced state-of-the-art therapies to the Valley. ROCA physicians have also provided Arizona’s cancer patients access to clinical trials through collaborative research organizations.
SERVICES AND CONDITIONS TREATED | Lung cancer, breast cancer, prostate cancer, brain cancer, trigeminal neuralgia, abdominal cancer, acoustic neuroma, and arteriovenous malformations (AVM).
NUMBER OF PHYSICIANS | 4
LOCATIONS | 1 office in Phoenix
MAIN OFFICE | 4611 E Shea Blvd, STE 120, Phoenix, AZ 85028 602-441-3845
WEBSITE | phoenixcyberknifecenter.com
TOP SPECIALTY | KIDNEY, LIVER, & PANCREAS SURGERY

OVERVIEW | Arizona Transplant Associates has continued to wage war on cancer for decades.
SERVICES AND CONDITIONS TREATED | Whipple procedures, liver resections, liver transplants, kidney transplants, kidneypancreas transplants, pancreas transplants, and other pancreas & bile duct resections.
NUMBER OF PHYSICIANS | 6
LOCATIONS | 1 office in Phoenix
MAIN OFFICE | 2218 N 3rd Street, Phoenix, AZ 85004 602-252-2543
WEBSITE | aztransplant.com
TOP SPECIALTY | OPHTHALMOLOGY

OVERVIEW | At Retinal Consultants of Arizona, they diagnose and find new innovative treatments for retinal conditions. Their goal is to provide patients the best possible outcomes for their unique retinal needs.
SERVICES AND CONDITIONS TREATED | Diabetic macular edema, diabetic retinopathy, flashes, floaters, macular degeneration, macular holes, macular pucker, posterior vitreous separation, retinal artery occlusions, retinal detachment, retinal tears, retinal vein occlusions, and uveitis
NUMBER OF PHYSICIANS | 7
LOCATIONS | 15 offices in Phoenix, Gilbert, Mesa, Peoria, Scottsdale, Bullhead City, Flagstaff, Kingman, Payson, Prescott, Yuma, and Yuma Foothills
MAIN OFFICE | 1101 E Missouri Ave, Phoenix, AZ 85014 602-222-2221
WEBSITE | retinalconsultantsaz.com

OVERVIEW | At Arizona Preferred Surgeons, their surgeons are skilled in complex decision making and diagnosis, as well as treatment and management.
SERVICES AND CONDITIONS TREATED | From anal fistula & fissures, appendectomies, breast surgery, colon cancer surgery, colonoscopies & upper endoscopies, Crohn’s & Ulcerative colitis, diverticulitis, fecal incontinence, gallbladder surgery, gastric resection, hernia surgery, hemorrhoids, and Nissen Fundoplication.
NUMBER OF PHYSICIANS | 3
LOCATIONS | 1 office in Glendale
MAIN OFFICE | 18699 N 67th Ave, Glendale, AZ 85308 602-995-0822
WEBSITE | azpreferredsurgeons.com
TOP SPECIALTY | PAIN MANAGEMENT

OVERVIEW | Mountain View Headache and Spine Institute provides one-on-one chronic pain management services. In addition to medication management, they offer a variety of pain-relieving therapies.
SERVICES AND CONDITIONS TREATED | Bone Marrow Concentrate, injections, infusions, nutraceuticals, and manual therapy.
NUMBER OF PHYSICIANS | 3
LOCATIONS | 2 offices in Phoenix and 1 in Peoria
MAIN OFFICE | 2222 E Highland Ave, STE 110, Phoenix, AZ 85016 | 602-767-0007
WEBSITE | mountainviewheadacheandspine.com
TOP SPECIALTY | DERMATOLOGY

OVERVIEW | Arizona Dermatology is proud to be a leader in the skin care industry and they strive to provide the highestquality medical dermatology, skin cancer treatments, cosmetic procedures, and med spa aesthetic services in Arizona. They use advanced techniques, expertise, and state of the art technology that allow them to provide unparalleled skin care results.
SERVICES AND CONDITIONS TREATED | Medical Dermatology (wart removal, acne treatments, psoriasis treatments, rosacea treatments, vitiligo treatments, melasma treatments), skin cancer (skin cancer screening, Mohs therapy skin cancer treatment), Botox, facial fillers, and Medspa services (intense pulse light therapy (IPL), micro-needling, chemical peels, vascular laser, dermaplaning, and microdermabrasion).
NUMBER OF PHYSICIANS | 6
LOCATIONS | 5 offices in Phoenix, Paradise Valley, Apache Junction, Mesa, and Show Low
MAIN OFFICE | 4835 E Cactus Rd, STE 155, Scottsdale, AZ 85254 | 602-996-3050
WEBSITE | arizonaderm.com
TOP SPECIALTY | PEDIATRICS

OVERVIEW | Pleasant Pediatrics was founded in 2008 by a devoted husband-wife team with a vision of providing compassionate, family-centered care. The Pleasant Pediatrics logo of three joyful children (inspired by the founders’ triplets) represents their inspirations and commitment to nurturing every child’s wellbeing.
SERVICES AND CONDITIONS TREATED | Routine well child exams, sports physicals for school, immunizations, TB skin testing, hemoglobin, urinalysis, rapid strep treatment, flu testing, pregnancy testing, antibiotic injections, circumcision, ear lavage, frenectomy (tongue tie), umbilical granuloma, and nebulizer treatments.
NUMBER OF PHYSICIANS | 16
LOCATIONS | 8 offices in Peoria, Glendale, Ahwatukee, and Phoenix
MAIN OFFICE | 9059 W Lake Pleasant Pkwy, STE E540, Peoria, AZ 85382 | 623-322-3380
WEBSITE | pleasantpediatrics.com

OVERVIEW | Neurology Associates Neuroscience Center is a multi-disciplinary practice that takes a comprehensive approach to physical and mental health and well-being. In addition to neurology they offer other related specialties.
SERVICES AND CONDITIONS TREATED | Neurology conditions treated include epileptology, movement disorders, multiple Sclerosis, and stroke. Related medical services include MRIs, neuropsychological evaluations, physical therapy, and psychiatry. Holistic services include cognitive rehabilitation, counseling, and naturopathic medicine.
NUMBER OF PHYSICIANS | 5
LOCATIONS | Chandler, Mesa
MAIN OFFICE | 2201 W Fairview St, STE 1, Chandler, AZ 85224 | 480-800-4890
WEBSITE | neurologyassociates.com
TOP SPECIALTY | FAMILY MEDICINE

OVERVIEW | Ark Family Health prioritizes patients by providing affordable, direct primary care. Direct primary care allows patients unlimited and direct access to their physician by paying a flat monthly membership fee.
SERVICES AND CONDITIONS TREATED | General primary care, same or next day appointments, 24/7 urgent care, in-house procedures, diagnostics, labs & imaging, low-cost medications, gynecology, and behavioral health.
NUMBER OF PHYSICIANS | 3
LOCATIONS | Peoria, Gilbert
MAIN OFFICE | 8514 W Deer Valley Rd, STE 100, Peoria, AZ 85382
WEBSITE | arkfamilyhealth.com
TOP SPECIALTY | PSYCHIATRY

OVERVIEW | Choulet Performance Psychiatry is revolutionizing mental health care for today’s professionals and their families. They have a deep understanding of achieving mental excellence. They guide patients to optimize performance in all facets of life and help them enhance overall life satisfaction.
SERVICES AND CONDITIONS TREATED | Concierge psychiatry, executive mind health assessments, psychology, sleep medicine, and concierge care.
NUMBER OF PHYSICIANS | 5
LOCATIONS | Phoenix, Paradise Valley, Scottsdale, AZ, Beverly Hills, San Diego, CA, Dallas, TX, and Bellevue, WA
MAIN OFFICE | 7373 N Scottsdale Rd, STE C190, Scottsdale, AZ 85253 | 480-448-6571
WEBSITE | chouletperformance.com
TOP SPECIALTY | VASCULAR SURGERY

OVERVIEW | Veincare of Arizona understands the importance of vein health in the overall well-being of their patients. They offer innovative, effective, and comprehensive care for varicose veins and other venous diseases.
SERVICES AND CONDITIONS TREATED | Varicose vein treatments include laser vein ablation, radiofrequency vein ablation, clarivein, transcatheter embolization, venaseal, and sclerotherapy.
NUMBER OF PHYSICIANS | 1
LOCATION | Sun City West
MAIN OFFICE | 13626 W Camino Del Sol #100, Sun City West, AZ 85375 | 623-584-7874
WEBSITE | veincarearizona.com
Advocacy
Pushing policies that matter


Patient Referrals
Online directory and referral line

Professional Referrals
Legal, financial, staffing, real estate, etc.
Scan to learn more about the benefits of being an MCMS member


CME In person and virtual

Physician Stories
Print and digital magazine, podcast
Networking
Happy hours and fun events
Focused on Physicians Like You! Become a Member Today.
Phoenix, AZ 85004
(602) 417-2303
information@arizonaphysician.com
“As
Edward G. Marley MICA President and CEO

