
WINTER 2023 FP MISSOURI FAMILY PHYSICIAN VOLUME 42, ISSUE 1 CELEBRATING 75 YEARS OF MISSOURI FAMILY PHYSICIANS
EXECUTIVE COMMISSION
BOARD CHAIR John Burroughs, MD (Kansas City)
PRESIDENT Kara Mayes, MD (St. Louis)
PRESIDENT-ELECT Afsheen Patel, MD (Kansas City)
VICE-PRESIDENT Natalie Long, MD (Columbia)
SECRETARY/TREASURER Lisa Mayes, DO (Macon)
BOARD OF DIRECTORS
DISTRICT 1 DIRECTOR Arihant Jain, MD (Cameron)
ALTERNATE Vacant
DISTRICT 2 DIRECTOR Robert Schneider, DO, FAAFP (Kirksville)
ALTERNATE Vacant
DISTRICT 3 DIRECTOR Emily Doucette, MD, FAAFP (St. Louis)
DIRECTOR Dawn Davis, MD (St. Louis)
ALTERNATE Lauren Wilfling, MD (St. Louis)
DISTRICT 4 DIRECTOR Jennifer Scheer, MD, FAAFP (Gerald)
ALTERNATE Jennifer Allen, MD (Hermann)
DISTRICT 5 DIRECTOR Amanda Shipp, MD (Versailles)
ALTERNATE Vacant
DISTRICT 6 DIRECTOR David Pulliam, DO, FAAFP (Higginsville)
ALTERNATE Justin Cramer, MD, FAAFP (Marshall)
DISTRICT 7 DIRECTOR Beth Rosemergey, DO, FAAFP (Kansas City)
DIRECTOR Jacob Shepherd, MD, FAAFP (Lee’s Summit)
ALTERNATE Ed Kraemer, MD (Lee’s Summit)
DISTRICT 8 DIRECTOR Andi Selby, DO (Branson)
ALTERNATE Barbara Miller, MD (Neosho)
DISTRICT 9 DIRECTOR Douglas Crase, MD (Licking)
ALTERNATE Vacant
DISTRICT 10 DIRECTOR Gordon Jones, MD (Sikeston)
ALTERNATE Jenny Eichhorn, MD (Jackson)
DIRECTOR AT LARGE Wael Mourad, MD, FAAFP (Kansas City) Krishna Syamala, MD, FAAFP (St. Louis)
RESIDENT DIRECTORS
Wesley Goodrich, MD, UMKC
Kelly Dougherty, MD, Mercy (Alternate)
STUDENT DIRECTORS
Karstan Luchini, KCU Joplin
Abby Crede, UMKC (Alternate)
AAFP DELEGATES
Kate Lichtenberg, DO, MPH, FAAFP, Delegate
Peter Koopman, MD, FAAFP, Delegate
Sarah Cole, DO, FAAFP, Alternate Delegate
Jamie Ulbrich, MD, Alternate Delegate
MAFP STAFF
EXECUTIVE DIRECTOR Kathy Pabst, MBA, CAE
ASSISTANT EXECUTIVE DIRECTOR Bill Plank, CAE
MEMBER COMMUNICATIONS AND ENGAGEMENT Brittany Bussey
The information contained in Missouri Family Physician is for informational purposes only. The Missouri Academy of Family Physicians assumes no liability or responsibility for any inaccurate, delayed, or incomplete information, nor for any actions taken in reliance thereon. The information contained has been provided by the individual/organization stated. The opinions expressed in each article are the opinions of its author(s) and do not necessarily reflect the opinion of MAFP. Therefore, Missouri Family Physician carries no respsonsibility for the opinion expressed thereon.
Missouri Academy of Family Physicians, 722 West High Street Jefferson City, MO 65101 • p. 573.635.0830 • f. 573.635.0148
Website: mo-afp.org • Email: office@mo-afp.org
CONTENTS
2021-22 Annual Reports
A Year in Review
Membership Milestones
Annual Fall Conference Recap
74th Annual Business Meeting
AAFP Congress of Delegates Addresses Priority Issues
Academic Medicine: An Antidote to Burnout for Some Celebrating 75 Years
Charting the Course for the Next Three Years
Missouri Academy Installs New Officers
Rasmussen Named MAFP Family Physician of the Year
Three Physicians Receive the MAFP Distinguished Service Award
2023 Legislative Session Has Started
Physician Wellness and Upcoming Retreat
Members in the News
Day Announcement
MARK YOUR CALENDAR
Virtual CME: Nutrition and Obesity https://www.mo-afp.org/cme-events/virtual-cme/
FP MISSOURI FAMILY PHYSICIAN
February 13-14 MAFP Advocacy Day – Courtyard Marriott, Jefferson City https://www.mo-afp.org/advocacy/advocacy-day/ February 14 MAFP Board of Directors Meeting – Courtyard Marriott, Jefferson City February 23 Virtual CME: OB/GYN and Maternal Health https://www.mo-afp.org/cme-events/virtual-cme/ March 23 Virtual CME: Men’s Health https://www.mo-afp.org/cme-events/virtual-cme/ April 27 Virtual CME: Adolescent Care https://www.mo-afp.org/cme-events/virtual-cme/ May 25
MO-AFP.ORG 3
Advocacy
6 12 15 16 18 20 21 23 35 37 39 41 42 44 45 47
Celebrating 75 Years of Family Medicine
Why do we do this? We go through years of education building enormous school loan debts (I am proud to say that I THINK mine will be paid off this year, only 27 years since finishing medical school!!). We start our professional lives working three years or more at far below minimum wage. In practice, we find our income dependent more on changing payment systems and rising overhead than the quantity or quality of our care. Regulations increasingly demand our time, electronic medical records (written by coders for billers, insurance companies, and attorneys - not for physicians), and the increasing needs of patients with administrative responsibilities passed on by insurance companies, pharmacists, and specialists.
With all this causing stress on our families and ourselves, why would anyone want to be a family physician?

The answer is clear: we can’t imagine doing anything else. There are so many incredible reasons to be a family physician. What other career gives such rewarding relationships with clients (in our case, OUR PATIENTS) while developing teamwork and strategies to improve the health of our friends, neighbors, and communities? This issue is a celebration of all the reasons, times, and stories that remind us that it is pretty remarkable to be a family physician. Every story boils down to “Personally, I love being a family physician because…”
Personally, I love being a family physician because it has allowed me to change and grow as my family and I have grown. I went through medical school planning to be a full-scope smalltown physician. Through residency, I learned that there were a few parts of that full scope that I might let go of. I was able to find a practice that fit my desires and my growing family’s needs of me. I have had the opportunity to be an independent family physician, cradle-to-grave, in a small practice in the suburban area of Liberty, MO. I have been able to be a sideline physician for the local high school, a volunteer reader in
my children’s elementary school, a nursing home physician and medical director, a vaccination consultant for a pharmacy network, a volunteer mentor for numerous students (high school, medical school, residents, nurses, NP’s, and PA’s) rotating or observing in my office, a local knowledge base for dyslexia (for patients and our school district), a yoga instructor treating trauma with interoceptive therapy, a former President and current Board Chair of the MAFP, and now (after 22 years of private practice), a full-time hospice and palliative care medical director. That’s a lot of hats, many that I didn’t know existed when I started this journey. It seems every time that I have desired or needed a challenge or a change, this career has given me a path to take - all while forging amazing relationships and experiences with my patients and coworkers. And I still love it!
2023 is the 75th Anniversary of the Missouri Academy of Family Physicians. On the heels of a few difficult years in healthcare, we have 75 years of reasons to celebrate. Through it all, MAFP is dedicated to optimizing the health of the patients, families and communities of Missouri by supporting family physicians in providing patient care, advocacy, education and research. What an amazing mission to strive for and support! Please join me in applauding our nearly 2,400 members for their dedication to the profession, and let’s make 2023 a year of celebration.
John Burroughs, MD Board Chair Liberty, MO
4 MISSOURI FAMILY PHYSICIAN January - March 2023
2023 IS THE 75TH ANNIVERSARY OF THE MISSOURI ACADEMY OF FAMILY PHYSICIANS. ON THE HEELS OF A FEW DIFFICULT YEARS IN HEALTHCARE, WE HAVE 75 YEARS OF REASONS TO CELEBRATE.



List of Facility Locations 1 Algoa Correctional Center 2 Boonville Correctional Center 3 Chillicotha Correctional Center 4 Cremer Therapeutic Community Center 5 Eastern Reception Diagnostic & Correctional Center 6 Farmington Correctional Center 7 Fulton Reception & Diagnostic Center 8 Jefferson City Correctional Center 9 Kansas City Re-Entry Center 10 Maryville Treatment Center 11 Missouri Eastern Correctional Center 12 Moberly Correctional Center 13 Northeast Correctional Center 14 Ozark Correctional Center 15 Potosi Correctional Center 16 South Central Correctional Center 17 Southeast Correctional Center 18 Tipton Correctional Center 19 Transition Center of St Louis 20 Western Missouri Correctional Center 21 Western Reception, Diagnostic, & Correctional Center 22 Women s Eastern Reception, Diagnostic, & Correctional Center Congratulations to MAFP on 75 Years of Supporting Family Medicine! Thank you to all of Missouri’s Family Medicine Physicians. CONTACT US TODAY TO FIND OUT MORE! Joni Adamson Director of Recruitment jadamson@mo-pca.org | 573-636-4222 mhpps.org MHPPS is non-profit and located within the Missouri Primary Care Association Careers that count! Pride, Passion, Purpose... MO-AFP.ORG 5
2021-22 Officer Annual Reports
John Paulson, DO, PhD, FAAFP Board Chair


Fifteen years ago, when I began my service on the Missouri Academy of Family Physician’s Board of Directors, I was the Alternate Resident Director. As I complete my service as Board Chair, I consider it a blessing to have had the opportunity to serve the MAFP in so many capacities. This organization and the people in it have been such a positive influence on my personal and professional development over the last 15 years. I cannot say thank you enough to MAFP.

I want to report that despite COVID-19 and record inflation, the organization is in good financial standing. I am proud to report that we have an experienced Board with an amazing and passionate staff that have set the course for the next 3 years with a comprehensive strategic plan focusing on Membership, Education, and Advocacy. The 2023-2025 plan is available on page 36.
Membership – We are committed to growing and supporting our members and will be highlighting awareness of benefits. We have been planning and developing new ways to connect our members in a positive and impactful way. We will continue to grow our brand awareness and increase our social media presence for recruiting, reputation, and to share information with our members.
Education – Our staff continues to routinely engage with the 6 medical schools and 12 family medicine residencies in Missouri. Recently, we have committed to reaching potential family medicine physicians by participating in Health Occupations Students of America (HOSA) activities locally and nationally. In an effort to develop and retain the top Missouri medical students within our Missouri residency programs, the team is developing the LEADS (Leadership, Engagement, Advocacy and Development Scholars) program. This is designed to promote leadership and advocacy skills while concurrently connecting students to our Missouri FM residency programs. We continue to meet with key leaders in the state to expand our residencies and advocate for our pipeline of future family physicians to meet the needs of Missourians. Last, but certainly not least, we continue to recognize our members burnout and need for wellness. We are positioning the organization to move this education and awareness to the forefront as we advocate for the health and well-being of our family physicians.
Advocacy – We are developing an advocacy curriculum that will educate our students, residents, and family physicians about advocacy. We believe that investing in this area will pay dividends
down the road when it comes to advocating for our patients and family physicians as we partner with our legislators in shaping future health policies.
My one regret is our decision to move the Annual Fall Conference away from Big Cedar Lodge in 2024. I completely support the board’s decision as the cost increase was financially unacceptable. However, I have so many memories with MAFP friends and family that have occurred as we gathered together at Big Cedar, it is still hard to say goodbye to the location even knowing it is the wise thing to do. Having said that, I am excited with our plan to rotate the location around the state so I can meet and develop memories with new physicians that I may not have had the opportunity to meet in the past.
The one thing that we need is YOU! I want to invite each of you to get involved. The way we grow and achieve success for our patients and family medicine is together. Those recognized for awards during the awards and installation ceremony at the annual meeting have volunteered their time, treasure and talent to guide MAFP to where it is today. Each bringing their unique perspective from their education and experience to ensure the Missouri Academy of Family Physicians continues to meet your needs and to provide the best patient care to Missourians. Your perspective and opinion are important.
Scan the QR code to volunteer today.

John Burroughs, MD President
The past year has been one of transition and tentative moving-forward in our world and in our profession. We have emerged from the past two years happy to connect with one another but also seeing a changed landscape. Leadership both politically and in public health are seen in America with more skepticism than at any time in our lifetimes. But our patients and neighbors have turned to us, their family physicians, with more trust than ever. Meanwhile we are feeling overwhelming fatigue from the horrors of caring for patients and families through COVID- 19, while facing increasing burdens in our day-to-day professional lives. We see little support from corporate ownership, hospitals, insurance companies, and regulatory bodies with increasing expectations without compensation. All the while, we fight to maintain our own scope of practice while we see other professions have their scope increased exponentially.
I remember telling physicians that my mother worked with in
6 MISSOURI FAMILY PHYSICIAN January - March 2023
the early 1990s that I was intending to go to medical school and become a family physician. Every one of them said emphatically, “Don’t do it. I don’t even recognize my job now.” Of course, I did not follow their advice (and neither did you). And while I often feel the same way that those well-meaning clinicians did, I don’t give the same advice to aspiring physicians that I talk to now. Because as frustrating and exhausting as my job had become as an independent physician in a two-person practice, I could not imagine doing anything else but being a family doctor. We are able to impact lives and communities as few others can, and we find ourselves learning and being impacted by those that we care for. That’s pretty amazing.
During my time on the Board of the Missouri Academy of Family Physicians (and especially the past three years on the Executive Commission), I feel more hopeful of the opportunities that we have to improve our working conditions and satisfaction while improving the lives of our communities. We have amazing leadership at the state and national levels pushing hard and gaining a larger voice where decisions are made. The AAFP in Washington, DC is one of the most effective and trusted voices in the Capitol and is an amazing source of information on the impact of primary care throughout the country.
During this past year in which I have been honored to serve as MAFP’s President, we have been able to make strides in Jefferson City. We FINALLY passed legislation to offer a tax incentive for those that open their office to precept students. Many thanks to our MAFP staff (Kathy, Bill, and Brittany) and our tireless lobbyists (Randy and Brian) for their work in bringing the bill to the finish line. And we continue to make impactful connections with our legislators as well as meetings with the Missouri Hospital Association, the director of MoHealthNet (Missouri’s Medicaid), and our osteopathic colleagues in hopes of a stronger voice in securing and expanding family practice residency slots, an increase of state investment in primary care, and improving access to care for our patients. Our Academy’s delegation took these messages to Jefferson City in February and to Missouri’s Senators and Representatives on Capitol Hill in May (in person once again).
We completed our Strategic Planning Session to chart our course for the next three years. Initiatives will continue our work to support and build our membership, provide quality and accessible education, become more impactful in our advocacy, and work to build a stronger relationship with Missouri’s residency programs and medical schools.
In order to continue this progress, we always need more support from all of you. Please consider donating to the MAFP PAC. It does make legislators listen more keenly. Please complete legislative surveys sent by our MAFP staff. It is more difficult to speak for all of our physicians as we see our own specialty become more specialized and varied. We strive to keep our Board and our Executive Commission as diverse as possible, but that is not enough to make sure that we are not advocating against our own physicians while advocating for others. We do listen,
so please keep speaking up and please consider becoming more involved in the work of the Academy. Consider contributing an article to the MAFP magazine or requesting topics for the magazine to cover. And, join us for live CME either in person at one of our amazing conferences or online with our virtual CME evenings.
Thank you again for your support of the Academy. I am excited to start my final year on the Executive Commission as Board Chair. Our future looks bright (but can become brighter)!
Kara Mayes, MD, FAAFP President-Elect

My year serving as President-Elect has been one full of changes and planning for the future of the Missouri Academy of Family Physicians. Most notably, we held a summer strategic planning session where board members met in person to develop goals and priorities for the next three years. Following the weekend session, the commissions have worked to refine our plans, and the full board voted to approve the plan at the November board meeting. It was refreshing to meet in person with no obligations other than our discussions about our future plans.
Last year, I was asked to serve on a task force through AAFP working to develop a competitive event for HOSA Future Health Professionals. The goal was to encourage high school students to learn more about family medicine as a potential future career. This year, the competition was available for students to participate in during their state and international competitions. I traveled to Rolla for the Missouri HOSA competition, and also to Nashville, Tennessee for the HOSA International Competition. In both locations, I served as a competition judge and also presented to groups of students about family medicine as a career. I think we had a great response for the first year of this competition being available, and I expect this to grow in future years, hopefully growing the pipeline of future family physicians.
A great “first” event for me this year was the Family Medicine Advocacy Summit (FMAS) in Washington, DC. While I participated in the event virtually in 2021, this was my first time attending FMAS in person. Our Missouri delegation was able to meet with most of our US Senators and Representatives or their staff. We also enjoyed time learning about how to best advocate for our patients and fellow physicians. If you’d like to get involved in advocacy but don’t know where to start, consider coming to MAFP’s Advocacy Day in Jefferson City this year on February 14th. It’s an excellent introduction to advocacy at our state level.
I would love to see more new faces at Missouri Academy of Family Physicians events in 2023. Come join us and get involved! If there isn’t an open board position from your district, consider joining one of our commissions, which are Advocacy, Member Services, and Education. You could also attend our CME events,
2021-22 OFFICER ANNUAL REPORTS MO-AFP.ORG 7
like the Annual Fall Conference or our Virtual CME series in the spring. You can write an article for an upcoming Missouri Family Physician magazine, or apply to speak at a CME event.
Afsheen Patel, MD Vice President
The past year has provided to be an interesting year for family medicine. This is my first year serving on the Board as Vice President. It was also the first year that we were able to come out of the pandemic and attend more meetings in person. I have been with the MAFP since 2014. I have seen all that it does for its members, but to be part of the Executive Commission was a completely different experience. As my first year, I focused on learning everything that was involved in running the organization and supporting our members. It has been an incredible year and I look forward to continuing to serve over the next few years.
AAFP’s Annual Chapter Leadership Forum (ACLF) is held every year in April in Kansas City. It was wonderful to see chapter officers and members from across the country back in person. This was my first year attending the ACLF part of the conference. As a past attendee of the National Conference of Constituency Leaders (NCCL), ACLF was very different from the NCCL part. It made me realize that the organization is there not only to serve its members but also to allow them to grow in each of their practices.
We had our first board meeting of the year in February which coincided with MAFP’s Advocacy Day. It was a great accomplishment when the preceptor tax credit was passed last year. Advocacy Day is always a great experience, full of energy, and strong advocates meeting together to fight for their patients and colleagues. It is also a very informative meeting addressing MAFP’s priority legislative issues. We were able to welcome more students and residents to this meeting, helping our efforts to support the future of family medicine.
AAFP Family Medicine Advocacy Summit is held in May. This “would” be my first year attending as part of the Board. However, I was unfortunately unable to attend this year due to flights being canceled and delayed. I was ready to be the voice of family medicine in Washington, DC, and sharing my message with our elected leaders. It taught me to be even more appreciative of our Executive Commission and Kathy who helps keep everything together.
This year I have focused on working with medical students and residents. The MAFP offers a mentorship program for medical students. It is always rewarding helping a young doctor learn the ropes of practice and advocacy. I hope we will continue our efforts to keep family medicine strong for our patients and advocate for well-trained professionals to take care of our patients.
It is a pleasure to represent you on the MAFP board.
Lisa Mayes, DO Secretary/Treasurer

As a non-profit organization, the Missouri Academy of Family Physicians (MAFP) activities support its members and assist them in improving patient care in Missouri. These activities are funded by member dues, fees for member activities, and support from vendors and sponsors. The MAFP continues to be financially sound as membership, programs and services are meeting budgeted expectations. The investments have had unrealized losses; however, we still maintain a sufficient reserve for future initiatives.
The membership dues collections continue to meet projections, and income from the Academy’s CME offerings is on target. The 2022 Annual Fall Conference exemplifies the value of networking with high attendance and the maximum number of exhibitors is reached.
The 2023 budget is based on the 2023-2025 Strategic Plan with several new initiatives focusing on residents, students, expanded CME, and advocacy efforts. The board approved the plan on November 13 which will guide our budget planning process through 2025.
The MAFP Board of Directors continues to provide direct oversight of the financial operations of the Academy and ensures our funds are used and focuses on member-centered services.
RESIDENT BOARD REPORT
CAPITAL REGION MEDICAL CENTER FAMILY MEDICINE RESIDENCY
Program Director: Daniel Gibson, DO

Per Class: Three (3), Four (4), Three (3); 10 total
Chief Resident: Heghineh “Helena” Galstian, MD, 2022-2023


Updates: Now offering: Therapeutic and cosmetic Botox training
Integrative Medicine in Residency (IMR) training available Point of Care Ultrasound (POCUS) curriculum complete
2021-22 OFFICER ANNUAL REPORTS
Wesley Goodrich, DO, MPH Resident Director
8 MISSOURI FAMILY PHYSICIAN January - March 2023
Kelly Dougherty, MD Alternate Resident Director
Social Presence: Instagram: crmcfamilymedicine, Facebook: Capital Region Medical Center, Website: Family Medicine Residency | Capital Region Medical Center (crmc.org)
COXHEALTH FAMILY MEDICINE RESIDENCY
Program Director: Shelby Hahn, MD
Per Class: Ten (10), Ten (10), Nine (9); 29 total
Chief Residents: Hannah McCarthy, MD and Grant Ralston, MD, 2022-2023
Social Presence: Instagram: coxhealthfmr, Facebook: CoxHealth Family Medicine Residency, Website: www.coxhealth.com/fmr
Updates: We now have four (4) residents in our Jordan Valley (FQHC) track; next year we will have six (6).
2022 Graduates:
Jacob Bolt, MD: Baptist Health - Emergency Medicine Fellowship (Fort Smith, AR)
Rachel Brown, DO: Christiana Care (Wilmington, DE)
Margaret Givens, MD: Jordan Valley Community Health Center (Springfield, MO)
Eddie Hansen, DO: Free Market Physician (Joplin, MO)
Victoria Jackson, DO: Meritas Health Vivion (Kansas City, MO)
Shelby Laughlin, MD: CoxHealth Center Ozark (Ozark, MO)
Marion Martinez, MD: Swedish FMR – First Hill OB Fellowship (Seattle, WA)
Kristen Snyder-Hernandez, MD: CoxHealth Center Campbell (Springfield, MO)
Rachel Watson, DO: CoxHealth FMR – OB Fellowship (Springfield, MO)
Instagram: Mercy STL FM Residency (@mercy_stl_fm)
2022 Graduates:
Chelsea Daniels, DO: Mercy Fellowship Palliative CareSt. Louis, MO
Emily Govro, DO: Mercy Clinic Primary Care - Hillsboro, MO Corinne Halsted, DO: Northern Arizona Healthcare - Flagstaff, Arizona
Ha Hatley, MD: Anderson Medical Group Family PracticeEdwardsville, IL
Adam Reinagel, MD: Perryville Family Care Clinic – Perryville, MO
Shivi Yadav, DO: Optimal Medicine - Des Peres, MO
RESEARCH FAMILY MEDICINE RESIDENCY
Program Director: Kavitha Arabindoo, MD, FAAFP, MPH
Per Class: Eight (8) residents, total of 24
Chief Residents: Tina Fleres, MD; Taylor Patterson, DO; Asher Wagnon, MD
Social Presence: http://researchresidency.com/ and https:// www.instagram.com/researchfamilymedicine/
LEE’S
SUMMIT FAMILY MEDICINE RESIDENCY
Program Director: Lawrence M. Gibbs, MD
Associate Program Director: Karen Foote, MD
Per Class: Approved for 18 ACGME slots, Six (6) PGY1s in place for the 2022 – 2023 academic year
Social Presence: Family Medicine (hcamidwest.com)
STILL OPTI-NORTHEAST
REGIONAL MEDICAL CENTER FAMILY MEDICINE RESIDENCY
Program Director: Gary Bruning, DO
Per Class: Approved for 12 total ACGME slots
Chief Residents: Katherine Holbrook, DO and Molly Thompson, DO
Social Presence: www.atsuresidency.com
Updates: Matched 4 interns through SOAP, which means they will have filled all 12 ACGME slots this coming year! Elizabeth Silvey, DO – is the graduating resident this year. She is moving to the Ozarks of Southwest Missouri to practice full-scope family medicine. She is going to be doing outpatient and inpatient medicine as well as obstetrical care and some pain management procedures.
MERCY FAMILY MEDICINE RESIDENCY
Program Director: Sarah Cole, DO, FAAFP
Per Class: Six (6), 18 total
Chief Residents: Elizabeth Hoover, DO & Michele Sun, MD
Social Presence: www.mercy.net/healthcare-education/ graduate/st-louis/family-medicine/ www.facebook.com/groups/mercystlfamilymedresidency/
Updates: The Lee’s Summit Family Medicine Residency Program received its ACGME accreditation in April of 2022. We filled our inaugural class of six residents outside of the Match process and will be filling our next class of six in the Match of 2023.
SAINT LOUIS UNIVERSITY FAMILY MEDICINE RESIDENCY
Program Director: Elizabeth Keegan-Garrett, MD
Per Class: Six (6) residents, total of 18
Chief Residents: Anthony Hang, DO and Dymon Morgan, MD
Social Presence: https://www.instagram.com/slumedfam/ Updates: Graduates and plans listed below:
Kelly Dye, MD: Private Practice with Scott & White in Killeen, Texas
Bob Heiger, MD: Private Practice with Mercy Medical Group in St. Louis
Peter Ireland, MD: Private Practice with Central Vermont Medical Center in Waterbury, Vermont
Randy Jackson, MD: Faculty Position with University of California San Francisco Nesa Mohebpour, MD: Private Practice in Texas
Daniel Stevens, DO: Private Practice in Denver, CO
2021-22 OFFICER ANNUAL REPORTS MO-AFP.ORG 9
ST. LUKE’S DES PERES FAMILY MEDICINE RESIDENCY
Program Director: Dr. Joseph Eickmeyer, DO
Per class: Four (4) PGY1, Four (4) PGY2, Five (5) PGY3;
Chief Residents: Nicholas Faron, DO
Social Presence: https://www.stlukes-stl.com/DesPeres/healthprofessionals/medical-residency.html
Updates: Matched 4-interns; Graduated 5 residents:
Tyler Marler, DO: Private Practice with Mercy Medical Group, St. Charles
Andrew Perry, DO: Private Practice with Christian Northeast Hospital BJC, St. Louis
Ashlyn Patterson, DO: Private Practice with St. Luke’s Medical Group, St. Louis
Monica Unterreiner, DO: Private Practice with Southeast Hospital, Cape Girardeau, MO
Jacob Yankowitz, DO: Private Practice, Farmington, MO
UNIVERSITY OF MISSOURI COLUMBIA FAMILY MEDICINE RESIDENCY
Program Director: Erika Ringdahl, MD
Per Class: Fourteen (14) (plus 2 Sedalia R1s)
Chief Residents: Maggie Brenna, Dalton Lohsandt, Colbert Nelson, Seth Mobley
Social Presence: Instagram: @Mizzoufamilymed; Facebook: University of Missouri Family Medicine Residency Website: https://medicine.missouri.edu/departments/family-andcommunity-medicine/residency
Updates: Matched 14 R1s
2022 Graduates and plans listed below:
Zack Barker, DO: St. Francis Healthcare, East Prairie, MO; Outpatient family medicine
Beau Bounous, DO: CoxHealth Clinic, Monett, MO; Outpatient family medicine
Diane Bussan, MD: University of Wisconsin Health Cross Plains Clinic, Madison, WI; Outpatient Family Medicine
Oyen Edo-Ohonba, MD: Procedural Hospitalist Fellowship, Deaconess Hospital; Evansville, IN
Jason Fultz, DO: Crestwood Medical Group, Alabama; Outpatient Family Medicine
Veronika Kiss, MD: El Pueblo Clinic, Tucson, AZ; Outpatient family medicine
Brea Lombardo, MD: South Providence Clinic, Columbia, MO; Obstetrics, Inpatient, pursue PhD in Translational Biosciences Reiana Mahan, MD: South Providence Clinic, Columbia, MO; Outpatient FM, pursue MS in Academic Medicine
Ryan Muehling, MD: University of Nevada, Reno, NV; Sports Medicine Fellowship
Marc Propst, MD: University of Missouri, Columbia, MO; Sports Medicine Fellowship
Humza Quadri, MD: The Kearney Clinic, Kearney, MO; Outpatient family medicine
McKenzie Veldhuizen, MD: Avera Health Family Medical Center, Sioux Falls, SD; Outpatient family medicine and obstetrics
Stephanie Zafiris, MD: Dartmouth General Hospital, Dartmouth, Nova Scotia; Hospitalist
UNIVERSITY OF MISSOURI - BOTHWELL FAMILY MEDICINE RESIDENCY
Program Director: Robert Frederickson, MD
Per class: Two (2)
Social Presence: www.brhc.org/residency Updates: 2 Sedalia R1s that will spend the first year rotating in Columbia
UNIVERSITY OF MISSOURI KANSAS CITY FAMILY MEDICINE RESIDENCY
Program Director: J. Lane Wilson, MD
Per class: Twelve (12) per class, 36 total Chief Residents: Outgoing Chiefs: Chris Koehn and Holly Perkins, MD
Social Presence: https://med.umkc.edu/fm/ and https://www. facebook.com/UMKCFM/
Updates: Graduates and plans listed below:
Joshua Go, DO: Sports Medicine Fellowship, UMKC/UHLW Family Medicine Sports Medicine
Zahn Raubenheimer, MD: Emergency Medicine Fellowship, Alteon Health/Cullman Regional Medical Center- Cullman, AL
William Burkhart, MD: Direct Primary Care, Knoxville, TN; Solo Practice
Jarom Spencer, DO: Intermountain Healthcare, Las Vegas NV: Outpatient Family Medicine, PRN hospitalist
Taylor Lacy, MD: Jefferson Medical Group, Washington Township, NJ: Outpatient Family Medicine
Monica Paulson, DO: Kaiser- Clackamas, OR; Outpatient Family Medicine with Prenatal Care
Marshall Taylor, DO: St. Luke’s Health System, Independence, MO: Outpatient Family Medicine, PRN hospitalist, St. Luke’s East
Stacey Leber, DO: Sioux Falls Family Medicine Residency Faculty, Sioux Falls, SD, Full spectrum (Inpatient, Peds, OB and Outpatient)
Crystal Brown, MD: Vredenburg, MD - St. Luke’s Health System, Lee’s Summit, MO; Outpatient Family Medicine
Rebecca Aguayo, MD: Maternity Care Fellowship, Family Medicine- UMKC/UHLW
Bailey Englund, DO - Maternity Care Fellowship- Family Medicine- UMKC/UHLW
Bailey Martin, MD: St. Luke’s Health System, Hedrick Medical Group Chillicothe, MO: Outpatient Family Medicine and newborn nursery
Sonia Hussain, MD: Toronto, Canada; family practice
2021-22 OFFICER ANNUAL REPORTS 10 MISSOURI FAMILY PHYSICIAN January - March 2023
STUDENT BOARD REPORT
UNIVERSITY OF MISSOURI-COLUMBIA SCHOOL OF MEDICINE
Number of Total Graduates: 110
Number of Students Who Matched into Family Medicine: 11
Number of Students Who Matched into Missouri Family Medicine: 8
FMIG members: 150
Karstan Luchini Student Director KCU-Joplin
Abby Crede Alternate Student Director UMKC
A. T. STILL UNIVERSITY OF HEALTH SCIENCES: OSTEOPATHIC MEDICAL SCHOOL
Number of Total Graduates: 173
Number of Students Who Matched into Family Medicine: 57
Number of Students Who Matched into Missouri Family Medicine: 13
FMIG Leadership: President-Austin Sams (sa206670@atsu.edu)

Faculty Advisors: Margaret Wilson,DO and Joseph Novinger, DO
KANSAS CITY UNIVERSITY OF MEDICINE AND BIOSCIENCES –
FMIG Leadership: Katelyn Weith - kcwrmd@health.missouri. edu; Abigail Beach - beachab@health.missouri.edu; Evadne Rodriguez - ecrtgd@health.missouri.edu; Andruw Wittelsamwyb5@health.missouri.edu

UNIVERSITY
OF
MISSOURI-KANSAS
CITY SCHOOL OF MEDICINE
Number of Total Graduates: 100
Number of Students Who Matched into Family Medicine: 6 Number of Students Who Matched into Missouri Family Medicine: 4
FMIG Members: 100
KANSAS CITY
CAMPUS AND JOPLIN CAMPUS
Number of Total Graduates: 434
Number of students who matched into Family Medicine: 84

Number of Students who matched into Family Medicine in Missouri: 16
FMIG Total: 107
FMIG Leadership (FMIG is part of Primary Care Club/ACOFP at KCU)
Joplin Leadership-Allayna Scheumann (Allayna.Scheumann@ kansascity.edu)


Kansas City Leadership- President: Stephanie Cox (stephanie. cox@kansascity.edu); VP: Lauren Evelti; Treasurer: Eddy Urena; Secretary: Ryan Burch
ST. LOUIS
UNIVERSITY SCHOOL OF MEDICINE
Number of Total Graduates: 168
Number of Students Who Matched into Family Medicine: 15
Number of Students Who Matched into Missouri Family Medicine: 1
FMIG members: 200
FMIG Leadership: Co-presidents: Hannah Pang (hannah. pang@health.slu.edu) and Kevin Yu (kevin.yu.1@health.slu. edu); Jensen Vayalil-Operations Lead Faculty Advisor: Matthew Breeden, MD (matthew.breeden@ health.slu.edu)
FMIG Leadership: Presidents: Noah Brown (npbdw7@ umsystem.edu) and Abby Crede; Co-VPs: Faith Kapp and Emma Gloe; Treasurer: Camyrn Maloney; Secretary: Deborah RiveraHernandez; Primary Care Week Coordinator: Mitchell Mahan; Community Service Chair: Khyathi Thallapureddy; PR Chair: Rachel Tran; Year 1 and 2 Rep: Gouri Kallanagowdar Advisor: Aniesa Slack, MD (aniesa.slack@tmcmed.org)
WASHINGTON
UNIVERSITY SCHOOL OF MEDICINE
Number of Total Graduates: 110
Number of Students Who Matched into Family Medicine: 0
Number of Students Who Matched into Family Medicine in Missouri: 0
FMIG Leadership: Tiffany Chen (tiffanychen@wustl.edu), Flora Laurent (flaurent@wustl.edu)
WITH PRIMARY CARE
FOR PRIMARY CARE
2021-22 OFFICER ANNUAL REPORTS
Join leading independent primary care physicians and also those working in community health centers who are making a difference through Aledade Accountable Care Organizations Data Analytics & Insights | Hands-On Support | Policy Expertise Visit aledade.com to learn more

LUNCH AND LEARN SESSIONS OFFERED FOR STUDENTS DURING THE VIRTUAL A DAY IN THE LIFE OF A FAMILY PHYSICIAN SERIES 5 6MEDICAL STUDENTS PARTICIPATED IN EXTERNSHIPS AT 4 RESIDENCY PROGRAMS INITIATED THE HOSA FAMILY PHYSICIAN STATE COMPETITION AND JUDGED AT THE INTERNATIONAL COMPETITION ATTENDED THE AAFP NATIONAL CONFERENCE OF FAMILY MEDICINE RESIDENTS AND STUDENTS RESIDENTS STUDENTS PHYSICIANS91 ATTENDED THE MAFP TRANSITION TO PRACTICE CONFERENCE RESIDENTS STUDENTS 25 & & 7 A Year in Review 29.5 CME Hours Offered 22 Topic-Driven Scholarly Articles Written 162 BILLS WERE MONITORED 11 MEMBERS & PARTNERS PRESENTED TESTIMONY ON PRIORITY LEGISLATION 60 BILLS WERE PASSED 34 LEGISLATORS VISITED DURING ADVOCACY DAY 48 BILLS WERE SIGNED BY THE GOVERNOR MEDICAL SCHOOL VISITS FAMILY MEDICINE RESIDENCY PROGRAM VISITS 7 4 Active 1302 Honorary 2 Inactive 14 IMG 0 Life 198 Resident 221 Student 646 Supporting (FP) 10 Transitional 2 Total 2395 MEMBERSHIP 12 MISSOURI FAMILY PHYSICIAN January - March 2023
Let’s celebrate family medicine together! The Missouri Academy of Family Physicians is proud of our members and their leadership during the last few years. Your expertise in providing patients with the best care helped Missourians through this difficult pandemic and evolving tripledemic with COVID-19, RSV, and the flu. Through all the challenges we faced as an organization and that you addressed in your clinic, we are beginning to see a return to somewhat normal activities and pace. We did this together!
The Missouri Academy of Family Physicians held a strategic planning session in June, 2022 to guide our programs and services from 2023 to 2025 (see more on page 35-36). This plan charts our future, but we want to provide you with a snapshot of where we are today. The following highlights focus on our efforts in advocacy, education, and member services.
ADVOCACY
As you know, family medicine is the foundation of improved patient care, lower costs, and better outcomes. The MAFP Advocacy Commission, governmental consultants, and staff helped guide our advocacy efforts during the 2nd Regular Session of the 101st General Assembly on issues ranging from immunizations, scope of practice, licensure, patient safety, physician workforce, and of course, the preceptor tax credit program. We keep you apprised of these issues through a weekly report from our governmental consultants, RJ Scherr and Associates during the legislative session, January – May.
Most notably, the MAFP was the lead organization on the passage of the Preceptor Tax Credit Program which will fund up to 200 $1,000 tax credits for primary care physicians and physician assistants who precept at least 120 hours. Testimony by our members, residents, students, and other healthcare groups, supported the self-funded initiative. There was no opposition to this measure.
We routinely work with several groups to further advance family medicine and physicians. Last year, MAFP executive director Kathy Pabst was appointed as the layperson representative on the Missouri Advisory Commission for Physician Assistants.
On the national level, MAFP sent 7 members and staff to the AAFP Family Medicine Advocacy Summit to share our story with our US Senators and Congressmen/women in Washington, DC. We had 7 meetings where we discussed Medicaid payment parity, telehealth, and behavioral health integration. We have two Missouri representatives on the AAFP Commission on Federal and State Policy. MAFP members submitted at least 288 messages to our US legislators on seven key issues using the Speak Out platform. The MAFP is actively involved and monitoring issues that are important to the care you provide. We submitted letters to key leaders on scope of practice, Medicare payment, and prior authorization.
EDUCATION
MAFP delivered a variety of education offerings to our members. During the 2022 Virtual CME Series, we provided 8.0 credits of highly scientific focused education on Cancer, Geriatrics, Musculoskeletal / Sports Medicine, and Neurology. These sessions were held virtually over four nights. MAFP also offered two Virtual KSAs on Care of the Hospitalized Patient and Care of Women in conjunction with other state chapters for our members in need of ABFM certification courses. The educational highlight of the year may have been our 30th Annual Fall Conference at Big Cedar Lodge in Ridgedale, MO where we provided 13.50 credits. We were pleased to see some of our highest attendee and exhibitor registrations ever in 2022. A full report on AFC can be found in this issue.
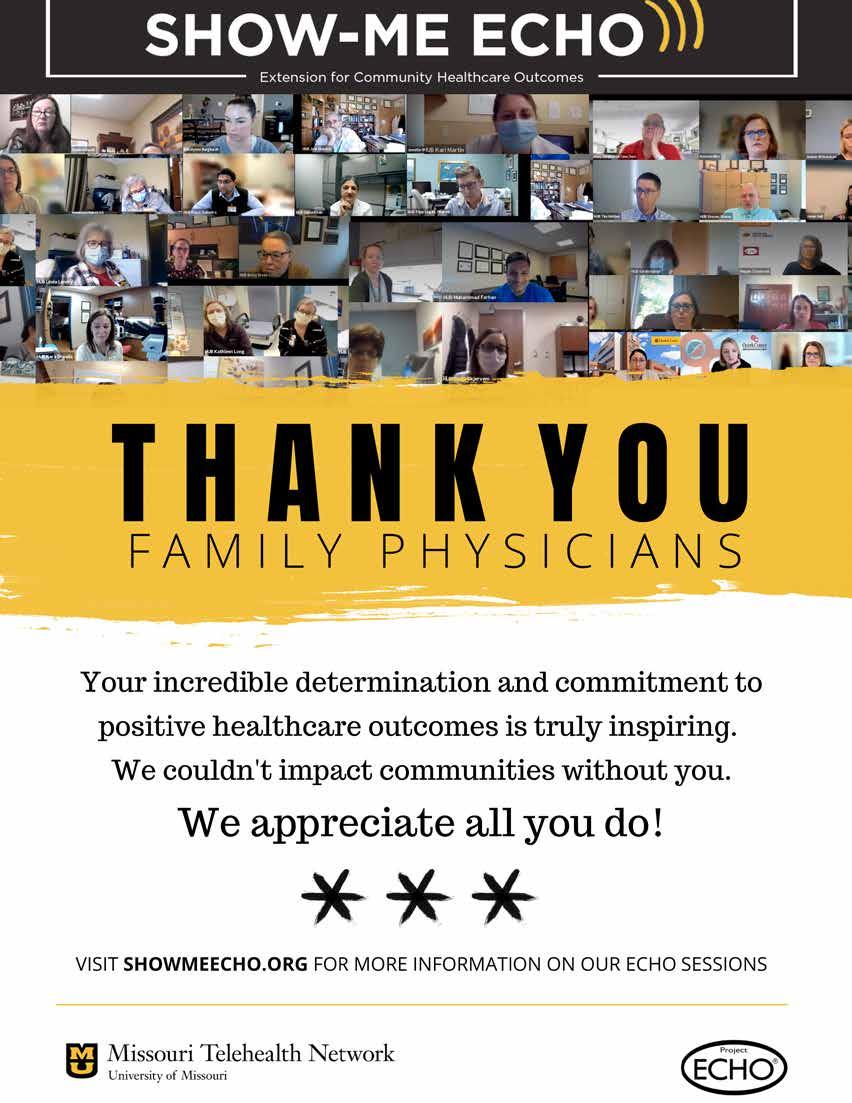
THANK YOU TO OUR PARTNERS IN HEALTH

The Missouri Academy of Family Physicians Partners in Health program recognizes community and corporate supporters as not only partners in family medicine but also recognizes their commitment to providing quality healthcare to Missourians.
Missouri Child Psychiatry Access Project

Missouri Health Professional Placement Services

Missouri Immunization Coalition

Novo Nordisk

COMMUNICATIONS
We want to share our story and activities with you and we accomplished this through our:
• Quarterly magazine, the Missouri Family Physician
• Monthly E-newsletter, the Show Me State Update

• Social Media Posts on Facebook, Twitter, LinkedIn, and Instagram
LEADERSHIP
Missouri has been recognized for many years for its dedicated leadership at the state and national levels. We sent a full slate of delegates to the National Conference of Constituency Leaders representing five identified groups: Women, LGBTQ+, Minority, IMG, and New Physicians. We sent a cadre of 5 members and 2 staff to the Family Medicine Advocacy Summit and State Legislative Conference. Resident and student delegates participated in education and governance sessions at the National Conference of Family Medicine Residents and Students. And 3 members and 1 staff are serving on AAFP commissions.
The MAFP board of directors meets three times per year and in conjunction with other events when possible. There are 37 members of the board of directors including alternate directors. The MAFP Board currently has 4 alternate director vacancies. The Executive Commission, consisting of the officers, meets monthly to address issues that arise between board meetings. Any member interested in serving on the board of directors is encouraged to reach out to the MAFP Team or any of our board members.
AAFP’s Congress of Delegates conducted business of the Academy and Missouri was represented with 2 delegates, 2 alternate delegates, MAFP Board President, and MAFP Executive Director. The MAFP introduced 1 resolution in the 2022 Congress of Delegates which was adopted as current policy. A 2021 resolution on insurance coverage for home-blood pressure monitoring units passed. There were 74 Missouri members who attended the FMX conference which was held immediately after the Congress of Delegates.
This is the story of family medicine in Missouri. You make this happen through your membership, participation, and commitment to family medicine. Keep up the excellence in your work and let’s work together to ensure the success of MAFP, you, our members, and your patients. We will celebrate our 75th anniversary in 2023 and look forward to your continued support!
THE CONFERENCE MADE ME WANT TO PARTICIPATE IN MAFP, AND I WANT TO SHARE THAT. IT WAS INTERESTING CONTENT, BUT ALSO ENJOYABLE TO MEET OTHERS IN THE FIELD. w w w . m o - a f p . o r g / r e s o u r c e s / p a r t n e r s / MO-AFP.ORG 13

14 MISSOURI FAMILY PHYSICIAN January - March 2023
MILESTONE
You are vital to the success of family medicine in Missouri. This year, we celebrate the following family physicians who have achieved a milestone membership anniversary.
55 Years of Membership
Richard Brummett, MD, FAAFP, Saint Louis, MO
Carlyn Kline, MD, FAAFP, Saint Joseph, MO
William Marshall, MD, Fayette, MO
Donald Potts, MD, FAAFP, Independence, MO
50Years of Membership
Theodore Baldwin, MD, FAAFP, Excelsior Springs, MO
Robert Dettmer, MD, FAAFP, Ironton, MO
Roger Hofmeister, MD, Columbia, MO
Thomas Mitchell, MD, Saint Clair, MO
H Rogers, MD, FAAFP, Vancouver, WA
45
Years of Membership
Mahmood Choudhury, MD, FAAFP, Springfield, MO
Devera Elcock Skimming, MD, FAAFP, New York, NY
Carl Myers, MD, FAAFP, Weatherby Lake, MO
Kerrin Papreck, MD, FAAFP, Cape Canaveral, FL
Esperanza Pimentel, MD, FAAFP, Fenton, MO
Chris Sandberg, MD, Saint Joseph, MO
Marla Tobin, MD, FAAFP, Warrensburg, MO
Daniel Vinson, MD, Columbia, MO
Michael Wurm, MD, Maryville, MO
William Zeller, MD, FAAFP, Branson, MO
40

Years of Membership
Dennis Boeke, DO, FAAFP, Stockton, MO
Kathi Clement, MD, FAAFP, Burlington, NC
David Cravens, MD, MSPH, Columbia, MO
Sisenando Galvez Jr, MD, FAAFP, Marceline, MO
Elizabeth Garrett, MD, MSPH, Columbia, MO
Lent Johnson, MD, Hannibal, MO
Guy Kline, MD, FAAFP, Ozark, MO
Vicki Kofender, MD, Stilwell, KS
James Lord, MD, Chesterfield, MO
Christian Madsen, MD, Saint Louis, MO
John Memken, MD, FAAFP, Hannibal, MO
Robert Shaw, MD, FAAFP, Willow Springs, MO
James Taylor, MD, FAAFP, Manchester, MO
Samuel Watts, MD, FAAFP, El Dorado Springs, MO
Edmond Weisbart, MD, FAAFP, Olivette, MO
W Wilson, DO, FAAFP, Ewa Beach, HI
35Years of Membership
Paul Andelin, MD, Aurora, MO
Rene Bollier, MD, FAAFP, Kansas City, MO
Jessee Crane, MD, Glencoe, MO
William Cravens, MD, Fulton, MO
Roderic Crist, MD, Cape Girardeau, MO
Druery Dixon, MD, West Plains, MO
Melanie Elfrink, MD, Marshall, MO
Jan Finney, DO, Bunceton, MO
Mary Fox, MD, Saint Louis, MO
Glennon Fox M.D., MD, Saint Louis, MO
Robert Hausam, MD, Columbia, MO
Nancy Hayes, MD, FAAFP, Mountain Grove, MO
David Kapp, MD, FAAFP, Perryville, MO
William Kimlinger, MD, FAAFP, Jefferson City, MO
Everett Koehn, DO, Liberty, MO
Sandra Lepinski, MD, Leawood, KS
Jeffrey Luerding, MD, Kansas City, MO
Scott Marrs, DO, Schertz, TX
Robert Martin, MD, West Plains, MO
David Meece, MD, Jackson, MO
Wendy Meyr-Cherry, MD, Saint Charles, MO
Ronald Nichol, DO, FAAF, Kansas City, MO
Timothy O’Keefe, MD, FAAFP, Carthage, MO
Hansa Patel, MD, Wilmette, IL
Carin Reust, MD, FAAFP, Columbia, MO
Mark Schultz, MD, Springfield, MO
Lori Smith, MD, Rolla, MO
Abbe Sudvarg, MD, FAAFP, Saint Louis, MO
James Thompson, MD, FAAFP, West Plains, MO
Scott Turner, MD, Springfield, MO
Barton Warren, MD, Richland, MO
Robert White, MD, FAAFP, Lake Ozark, MO
Jon Wilson, DO, Everton, MO
30Years of Membership
Douglas Anderson, MD, Warrensburg, MO
Bruce Bellamy, MD, FAAFP, Clinton, MO
Robert Bieser, DO, FAAFP, Cape Girardeau, MO
Pushpa Bisarya, MD, Ballwin, MO
Patricia Blair, MD, Saint Charles, MO
Steven Carder, MD, Liberty, MO
Wm Russell Detten, DO, FAAFP, Springfield, MO
Mark Ellis, MD, FAAFP, Nixa, MO
Susan Even, MD, Columbia, MO
Tawnyia Jerome, MD, Jefferson City, MO
Henry Konzelmann, MD, FAAFP, De Soto, MO
Richelle Koopman, MD, MS, FAAFP, Columbia, MO
Stacy Mevs, MD, Saint Louis, MO
James Miller, DO, FAAFP, Butler, MO
Mary Randolph, MD, Polo, MO
Roger Sacry, MD, Carthage, MO
Jennifer Scheer, MD, FAAFP, Gerald, MO
Melissa Smith, MD, Lees Summit, MO
Melanie Smolen, MD, Grandview, MO
25Years of Membership
Martin Alumno, MD, Springfield, MO
James Brillhart, MD, Columbia, MO
Jennifer Conley, MD, FAAFP, Nevada, MO
Gregory Dean, MD, Bethany, MO
Tamarah Duperval-Brownlee, MD, MBA, MPH, FAAFP, Saint Louis, MO
Michael Farris, MD, MBA, FAAFP, Springdale, AR
Katherine Friedebach, MD, Raymore, MO
Dana Granberg, MD, FAAFP, Kansas City, MO
Susan Hull, DO, Chesterfield, MO
Jennifer Jiang, MD, Cape Girardeau, MO
Mahrukh Khan, MD, Saint Louis, MO
David Knorr, DO, Palmyra, MO
Scott Kuennen, MD, Kansas City, MO
Daniel Lavery, MD, Jefferson City, MO
Shaina Reynolds, DO, Cape Girardeau, MO
Michael Rothermich, MD, Hermann, MO
Cynthia Ruffolo, MD, Boonville, MO
Heather Russell, MD, Nevada, MO
Dale Stegeman, MD, FAAFP, Waynesville, MO
Chandra Wiewel, MD, Saint Louis, MO
Congratulations ON YOUR MEMBERSHIP
MO-AFP.ORG 15



Name: AAFP ID#: Address: MD DO Other: FAAFP 16 MISSOURI FAMILY PHYSICIAN January - March 2023







Primary Care Call to Action for VTE Management: Sharpen Your Skills
in the Recognition, Treatment, and Secondary Prevention
Don’t Pull Your Hair Out! Hair Loss and Alopecia
Geoffrey D. Barnes
MD, M.Sc., FACC, FAHA, FSVM, RPVI
Mimi Propst, MD
The Role of the Family Physician in the Neurodiagnostic Evaluation of Children with Neurodevelopmental Disorders
Britton Zuccarelli, MD
Let’s Get Moving: A Comprehensive Approach to Management of Arthritis
Koopman,
FAAFP 2022 Legislative Update
FAAFP
Voran,
Is the Most Powerful Healthcare Tool in Your Patient’s Pocket? A Review of Connected Healthcare Technology
Hyperbaric Oxygen Therapy for the Family Physician: How, When, and Why to Consider for the Patient
The Role and Utility of Mineralocorticoid Receptor Antagonists in Diabetic Kidney Disease
Gersch,
FAAFP AAFP State of Family Medicine
Gersch,
FAAFP Big Danger Behind Little Doors: How to Recognize and Treat Common Pediatric Overdoses
FAAFP Clinical Pearls: End of Life Care
Getting Ahead of the Curve: Identifying and Managing Obesity in Primary Care
Can Team-Based Care and Novel Therapies Improve Outcomes in Moderateto-Severe Pediatric Atopic Dermatitis?
Heather Hammonds, MD
Peter
MD,
Keith Ratcliff, MD,
David
MD
David German, MD
Louis Kuritzky, MD
Daron
MD,
Daron
MD,
Charlie Rasmussen, DO,
John Burroughs, MD Domenica M. Rubino, MD
Mark Boguniewicz, MD
New Strategies and Best Practices in the Management of Pediatric Facial and Truncal Acne
Hilary Baldwin, MD
Treatment Strategies for Basal Insulins to Manage Time-in-Range and Glucose Variability to Improve Outcomes in Patients with Diabetes DO MO-AFP.ORG 17
Susan K. Fidler, MD
74th Annual Business Meeting
The Missouri Academy of Family Physicians held its 74th Annual Meeting during this year’s Annual Fall Conference on November 12, 2022. Leaders were elected that will take us into our 75th Anniversary year. Annual reports of the 2021-22 officers are included on pages 6-8.


John Burroughs, MD, newly elected MAFP Board Chair, presented the slate of officers who were elected by acclimation at this important meeting:
Board Chair – John Burroughs, MD, FAAFP (Liberty)
President – Kara Mayes, MD, FAAFP (St. Louis)
President-Elect – Afsheen Patel, MD (Kansas City)
Vice President – Natalie Long, MD (Columbia)
Secretary/Treasurer – Lisa Mayes, DO, fulfilling a 3-year term expiring in 2024

AAFP Delegates – Peter Koopman, MD, FAAFP, (Columbia) and Kate Lichtenberg, DO, FAAFP (Kirkwood)
AAFP Alternates – Sarah Cole, DO, FAAFP (St. Louis) and Jamie Ulbrich, MD, FAAFP (Marshall)
In addition, board members whose terms expired in 2022 were affirmed for another 3-year term. The Executive Commission fills vacant positions as they arise throughout the year. The following board members were affirmed for service on the board:
DISTRICT 1
Arihant Jain, MD, Kearney, renewing his term for another 3 years as director
DISTRICT 7
Ed Kraemer, MD, Kansas City, moved from director to alternate director for 3 years Jacob Shepherd, MD, Kansas City, moved from alternate director to director for a 3-year term
DISTRICT 8
Andi Selby, DO, Branson, renewing her term for another 3 years
DISTRICT 10
Gordon Jones, MD, Sikeston, moving to a 3-year term from alternate director to director Jenny Eichhorn, MD, Jackson, serving a 3-year term as alternate director
DIRECTORS AT LARGE WHO WILL SERVE ANOTHER ONE-YEAR TERM: Krishna Syamala, MD, St. Louis Wael Mourad, MD, Kansas City
Lastly, we had a moment of silence for our friends, colleagues, and members who passed away during the last year:
Ted Paulsell Smith MD, Rolla
John Edward Murphy MD, Pleasant Hill
Paul Anthony Williams MD, Saint Louis
William Radford Green MD, Saint Louis
Ronald D Nichol DO, Kansas City
Ambrose T Walker MD, Fort Myers
Robert L Magee MD, El Dorado Springs
Carol Therese Berner MD, Springfield
George A Richardson MD, Sarasota Thomas M Macdonnell MD, Marshfield
Paul Allan Williams MD, Lees Summit Robert Richard Pavlu MD, Carrollton Robert Leroy Wheeler MD, Harrisonville
With no further business to come before the group, the meeting adjourned. The officers were installed during the awards and installation ceremony that immediately followed the annual meeting.
75TH ANNIVERSARY ANNUAL MEETING NOVEMBER 11, 2023 BIG CEDAR LODGE RIDGEDALE, MO SAVE THE DATE 18 MISSOURI FAMILY PHYSICIAN January - March 2023
Fellows Conferred at Annual Meeting

The Degree of Fellow recognizes members who have distinguished themselves among their colleagues, as well as in their communities, by their service to family medicine, by their advancement of health care to the American people, and by their professional development through medical education and research. Fellows of the AAFP are recognized as champions of family medicine. They are the physicians who make family medicine the premier specialty in service to their community and profession. Being a Fellow signifies not only ‘tenure’ but additional work in your community, within organized medicine, within teaching, and a greater commitment to continuing professional development and/or research.
The following MAFP members were conferred by Daron Gersch, MD, FAAFP, AAFP Vice Speaker, at the November annual meeting:
Damon Broyles, MD, FAAFP (Eureka)
Dawn Davis, MD, FAAFP (St. Louis)
Nicholas LeFevre, MD, FAAFP (Columbia)
Kevin Munger, DO, MS, FAAFP (Blue Springs)
Christine Nedeau, MD, FAAFP (Kansas City)
Jacob Shepherd, MD, FAAFP (Lees Summit)
Clint Strong, MD, FAAFP (Springfield)
Congratulations! For more information and details about becoming a Fellow, visit the AAFP website at https://www.aafp.org/membership/welcome-center/ involve/fellow.html.
417-814-2142 michael.mann@coxhealth.com EXPLORE Your Possibilities LOWER COST OF LIVING 14% NONSTOP FLIGHTS 15 MILE TRAIL SYSTEM 75+ MINUTE AVERAGE COMMUTE 20 SPRINGFIELD | BRANSON MONETT | LAMAR SPRINGFIELD MISSOURI Seeking BE/BC physician Details • Locations include Springfield, Missouri, and surrounding communities • Top 100 Integrated Health System • 2018, 2019, 2020, 2021 Modern Healthcare Best Places to Work Benefits • Competitive salary and sign-on bonus • Relocation allowance and comprehensive benefits package FAMILY MEDICINE OPPORTUNITY MO-AFP.ORG 19
AAFP Congress of Delegates Addresses Priority Issues

Your Missouri Delegation traveled to Washington, DC, September 19-21, 2022, for the first in-person Congress of Delegates (COD) since the start of COVID. It was a whirlwind few days with much work accomplished but also a chance to catch up with each other. The COD is the AAFP’s policy-making body. It is part of the AAFP governance process through which members direct the work of the Academy.
In addition to our 2022 work, there were a number of resolutions from the 2021 virtual COD held over for discussion on the floor of the House. Those resolutions went through reference committees last year and were extracted from the consent calendar for discussion.
Written testimony was accepted to streamline the virtual reference committees of the last few years. This continued for the in-person reference committee meetings allowing more members to share their thoughts on different resolutions.
Keith Ratcliff, MD, FAAFP, of Washington, and Kate Lichtenberg, DO, FAAFP, of Kirkwood, served as delegates. Alternate delegates were Peter Koopman, MD, FAAFP, of Columbia, and Sarah Cole, DO, FAAFP, of St. Louis. John Burroughs, MD, of Liberty, also joined the delegation at this year’s Congress. Dr. Lichtenberg served on the Reference Committee for Quality and Practice, and Dr. Koopman served on the Credentials Committee.
The Congress began with the town hall session with AAFP leadership and discussed membership issues, administrative burden, and payment. Other hot topic issues discussed were physicians’ right of conscience and reproductive health laws. Formal presentations were made throughout the meeting.
AAFP’s annual elections were conducted, and Steven Furr, MD, FAAFP (Alabama), was chosen to serve as president-elect. Three members ran unopposed for the three vacant board positions and were elected to the board: Kisha Davis, MD, FAAFP (Maryland); Jay Lee, MD, FAAFP (California); and Teresa Lovins, MD, FAAFP (Indiana). Dr. Tochi Iroku-Malize was installed as the 2022-23 AAFP president.
HERE ARE A FEW HIGHLIGHTS FROM THE CARRY-OVER RESOLUTIONS:
Ensuring Equitable Distribution of the COVID-19 Vaccine (Adopted)
RESOLVED, That the American Academy of Family Physicians lobby for the specific inclusion of collaboration with non-governmental community organizations and clinics to address equitable distribution of the COVID-19 vaccine among communities of racial and ethnic minorities as well as undocumented individuals.
Keep Prescriber and Formulary Databases Current (Adopted)
RESOLVED, That the American Academy of Family Physicians advocate for federal legislation requiring pharmacies to verify their prescriber database and their health plan formulary database every 3 months, as is required by health insurers.
Confidentiality Protection for Non-Policy Holders in Healthcare Billing (Referred to Board of Directors)
RECOMMENDATION: The reference committee recommends that Substitute Resolution No. 606 which reads as follows be adopted in lieu of Resolution No. 606: RESOLVED, That the American Academy of Family
Physicians advocate for a policy that would exempt the requirement of an explanation of benefits when confidential services, including but not limited to, care related to family planning, HIV, sexually transmitted infections, comprehensive reproductive health services, mental health, substance use treatment, pregnancy and childbirth, are received by a non-policy holder.
Missouri Resolution Rights of Conscience (Referred to Board of Directors)
RESOLVED, That the American Academy of Family Physicians create a “Rights of Conscience Toolkit” and education for member and student use founded upon the core tenets of Osteopathic and Hippocratic medicine toward advocacy efforts in rights of conscience within training programs, hospital systems, medical societies, payer sources, and state and federal government.
ACTIONS ON SOME OF THE 2022 RESOLUTIONS
FOLLOW:
Reduction of the Prior Authorization Requirements (Substitute Resolution Adopted)
RESOLVED, That the American Academy of Family Physicians advocate for the reduction of prior authorization requirements of health insurance companies through the creation of and adoption of standardized prior authorization criteria.
Improved Access to LARCs (Adopted)
RESOLVED, That the American Academy of Family Physicians work to improve access to long-acting reversible contraceptive devices for distribution in primary care offices, and be it further RESOLVED, That the American Academy of Family Physicians work to reduce any administrative burden that increases patient wait time to obtain longacting reversible contraceptive devices through primary care practices. Increase Funding to Safety Net Hospitals (Substitute Resolution Adopted)
RESOLVED, That the American Academy of Family Physicians advocate for increased funding for safety net hospitals and hospitals that serve predominantly low-income populations.
The end of the meeting brought many announcements, including Todd Shaffer, MD, MBA, FAAFP, Kansas City, running for President-Elect of the AAFP in 2023. Keith Ratcliff, MD, was recognized and thanked for being a Delegate as he retires from the Missouri delegation. Peter Koopman, MD, was announced as Chair of the Commission for Federal and State Policy.
The next Congress of Delegates will be in Chicago October 25-27, 2023. We welcome any members to help us support Dr. Shaffer and his candidacy.
Respectfully Submitted, Keith Ratcliff, MD, FAAFP
Kate Lichtenberg, DO, MPH, FAAFP
Peter Koopman, MD, FAAFP
Sarah Cole, DO, FAAFP
20 MISSOURI FAMILY PHYSICIAN January - March 2023
Academic Medicine: An Antidote to Burnout for Some
Kimberly A. Schiel, MD, MA, FAAFP Saint Louis University School of Medicine

There is a great deal of discussion and research around the destructive effects of burnout in medicine. A physician who changes jobs in hopes of “greener pastures” is costly to the system, both in terms of patient satisfaction1 and healthcare expenditures.2
Similarly, a physician who stoically persists at a job she has come to dread may be physically present but lacking in the compassion and understanding which are so important to her patients.
Some proposed solutions to the physician burnout epidemic focus on improving physician resilience. Others try to improve the workplace
to lessen the stressors which contribute to burnout. Both approaches are helpful and necessary. There is another, less discussed way to lessen burnout: allowing physicians to do more of what they love.
Physicians who spend their time doing tasks that they find meaningful are less likely to be burned out or suffer occupational stress.3 For some physicians, this means pursuing a career in academic medicine. A 2022 study4 found that physicians with academic affiliations, when compared with peers who did not have academic affiliations, were less likely to be emotionally exhausted or to report depersonalization. Exhaustion and depersonalization decreased as time spent in teaching activities increased. Academic physicians reported higher levels of time use satisfaction and career satisfaction.
In a 2009 study of faculty physicians5, the authors asked academic physicians to quantify how much time they spent in various activities (patient care, research, education, or administration) and to rank how much meaning they found in these activities. They then correlated this information with indicators of burnout. Physicians who spent less than 20% of their time in the activity they found most meaningful were
MO-AFP.ORG 21
more likely to be burned out. In this study, only a minority of physicians listed education or research as their most meaningful activity (9% and 19%, respectively,) but this could represent an important way to reduce burnout for this subset of physicians.
How can a physician with a love for academia integrate this into an already-busy practice? The options range from a small amount of volunteer teaching to a change of career path. The simplest way to be involved in teaching is to become a volunteer preceptor. There is an acute shortage of preceptor sites to educate our medical students. A call to the nearest department of Family Medicine will be welcomed by the Family Medicine Clerkship Director. Even if a physician is located far from a medical school, rural rotations with housing in an apartment or home of a host family can be arranged. These rotations are often among the most rewarding and influential experiences of a medical student’s education.
A physician with a love for medical education can teach at a nearby medical school or residency. It may be possible to staff the “teach room” in the residency clinic a few days a month or to supervise the inpatient service on a rotating basis. They can give a recurring lecture to medical students or instruct in a Case Based Learning curriculum. They can coauthor a review article with a student or resident.
Lastly, a career dedicated to academic medicine may be right for some physicians. The rewards and challenges of teaching, research, and publishing are never-ending. One of the benefits of an academic medicine career is the privilege of being always at the forefront of medicine, always forced to keep up with constantly changing guidelines and innovations. An important part of academia is mentoring and
advising learners as they choose a career path. Advocating for family medicine is a constant reminder of the values which drew us to this field: knowledge, compassion, cost-effectiveness, quality, and selfless service.


Chairs of departments of family medicine, whether in an academic medical center or a healthcare system, should engage in conversations about career fit with their physician employees. How much of the physician’s time is spent in work they find personally meaningful? How much is spent on tasks that are misaligned with the physician’s talents and values? What specific actions can be taken to improve the alignment? If physician values can be better aligned with the reality of their workday, it might benefit the physician, their patients, and the healthcare system.
References
1. Reddy, A., et al., The Effect of Primary Care Provider Turnover on Patient Experience of Care and Ambulatory Quality of Care. JAMA Intern Med, 2015. 175(7): p. 1157-62.
2. Sinsky, C.A., et al., Health Care Expenditures Attributable to Primary Care Physician Overall and Burnout-Related Turnover: A Cross-sectional Analysis. Mayo Clin Proc, 2022. 97(4): p. 693-702.
3. Ko, S.S., et al., Family Medicine Faculty Time Allocation and Burnout: A Residency Research Network of Texas Study. J Grad Med Educ, 2020. 12(5): p. 620-623.
4. Zhuang, C., X. Hu, and M.J. Dill, Do physicians with academic affiliation have lower burnout and higher career-related satisfaction? BMC Med Educ, 2022. 22(1): p. 316.
5. Shanafelt, T.D., et al., Career fit and burnout among academic faculty. Arch Intern Med, 2009. 169(10): p. 990-5.
22 MISSOURI FAMILY PHYSICIAN January - March 2023
YOUR FAMILY MEDICINE STORIES AND WORDS OF SUPPORT MO-AFP.ORG 23
Marla Tobin, MD, FAAFP Warrensburg, MO
Growing up in small-town Missouri in the 1960s gave me a wonderful opportunity to see the role of a general practitioner becoming a family doctor and serving the entire community. This was my background as I headed to the University Missouri – Columbia to begin my college and medical school career. I decided in sixth grade that I wanted to become a doctor and began working as a candy striper and nurse aide in my teenage years at Lexington Hospital. Several of the community docs became mentors and allowed me to see a little bit of what a career in medicine could be.
By the time I entered medical school, the specialty of family medicine had begun, and I eagerly joined the Academy of Family Physicians the first week of medical school. The AAFP became my family and allowed me to have many leadership roles and opportunities to learn about the specialty. Because I enjoyed every rotation of medical school it became obvious to me that family medicine was the right choice for me and my goal became to serve my hometown – Higginsville, Missouri.
As I learned about the depth and breadth of family medicine, I explored residencies and decided to go to the family medicine residency at Duke University in North Carolina for my training. During our practice management training we talked about what our future practices would be like. Those were the days before cell phones and communications in rural areas depended upon pagers, pay phones, land lines, and CBs. I laughingly told other residents that I would just get on the CB and call “breaker, breaker, this is the doctor” to reach out to folks. I remember telling them that since there were no other family doctors in my community at that time, I might have to cover call with the local veterinarian. I could deliver livestock and I’m sure he could deliver a baby if necessary. Ironically, a few years later I did go into his office one day when he was gone and his wife asked me to restitch a cat that had dehisced. Little did I know in my residency what life is a family doctor in rural Missouri would really entail, but I eagerly headed home to practice in my hometown.
Some of the first babies that are delivered with those of classmates and church friends. One included a lethal heart abnormality that resulted in the baby living only a few days. I learned very quickly that being a family physician is about life and death and carries you through all the joys and heartbreaks an individual may have. I also became part of those families and still today celebrate their family milestones with them. Many of my patients were farmers in the community that of course knew my parents. To them I was “Ike’s little girl” or “Doris’s daughter”. Many remembered me as a 4-Her growing up and more than once as I was stitching up an old former, I teasingly asked him if he wanted me to cross stitch or embroidery. The sight of a female physician was not typical in those days. Many of my grandparents’ friends told me stories about holding me on their lap as a child. It was truly an honor to celebrate the lives of five generation families in my community.
The days were pretty crazy and so were some of the nights. The logistics of caring for patients in two hospitals 45 miles
apart, delivering babies, providing full-service hospital care including surgery, and running a busy practice involved long hours and lots of miles. I traveled to five nursing homes, was a sideline physician for football games, and was the first female doctor in seven counties in rural Missouri. I quickly learned that the best way that I could serve my community was to recruit other health practitioners to our area. We also learned to navigate privilege battles and local hospital politics. Two years after my return to the area we had expanded our clinic from one doctor in three rooms to three doctors in a brand-new clinic facility complete with the helipad to transport patients needing more acute care.
Many of the residents and students who worked with us in our practice saw the passion that we had for family medicine and experienced the warmth of our patient relationships. Students would also often ask “How do you know everything about everyone?” I would tell them that I did not have to know everything about everyone but I had a growing database of information built over years of experience and knowledge of the individual and the community and their families. I also reminded them that I learned more in my first year in practice than I had my entire 3 years of residency, and I was learning every day because no two patients were the same and no two days were alike. Behind every exam room door is a new experience waiting.
Our practice grew and we were seeing patients from several counties. We built a second office in Warrensburg, Missouri and grew to five doctors and four nurse practitioners serving our rural communities. Not only did we work in the hospitals, clinics, and nursing homes, but we reached out to the schools, community organizations, and local health connections trying to network the community together. One thing that many people don’t realize about small-town medicine is how valuable the local pharmacists are to help spot problems with patients and alert the healthcare providers to the issues before disaster occurs. Just as we made house calls and after-hours visits, they were a full-service provider for local patients providing afterhours service and a knowledge of their clients.
Some 40 years have passed since I decided to go home again. It was one of the best decisions of my life. Although I am now retired, I still am part of the families I cared for, the communities I served, and the proud practice of family medicine. Patients still seek my opinion and consider me their doctor many years later. I still tell future physicians “you CAN go home again.”
24 MISSOURI FAMILY PHYSICIAN January - March 2023
Dave Pulliam, DO, FAAFP
Higginsville, MO
Back in the day, late 1980s, I received a call from a nurse that I worked with, telling me that her 94-year-old grandfather had a leg that looked really bad and refused to come to the office.
Walter was a tough, hard-working farmer, a widower, who lived alone and continued to care for his cattle on a daily basis with the help of his family. I had seen him on occasion in the office for relatively minor problems, but he did not typically require routine
Jacob Shepherd, MD, FAAFP Lee’s Summit, MO

I have had the opportunity to serve as a family medicine physician in multiple settings. I grew up in a family of eleven children. My father, who is a family medicine physician, always said to be in family medicine, you have to practice family. I have learned how putting family before work and service before self has made me a stronger physician. I have had the opportunity to serve in the US military. I value my opportunity to serve the patients of this great state. I have gained a lot of leadership experience with my time
John Paulson, DO, PhD, FAAFP Joplin, MO
Right after residency, I took over the practice of a consummate rural family physician that had recently passed away. I was working in a town with a population of less than 2000 people. He had cared for his patients for decades and knew them as friends and family, not patients.
One older gentleman came in complaining of something that he “just needed some antibiotics for,” like his previous doctor had given many times before. This was not appropriate from my evaluation, and I requested additional testing. This gentleman was not happy at all with my recommendation for additional testing
medications.
As requested, I made a house call and evaluated Walter’s leg. Walter’s granddaughter was correct. His leg looked horrible. The entire leg was discolored and cold, with no peripheral pulse. I proceeded to give him the instructions for going to the hospital, where I felt certain they would need to amputate his leg, given the advanced stage of the apparent loss of circulation. At this point, I do not recall giving him other options. Feeling assured that I was correct, I told him that if he did not go to the hospital, he would develop gangrene and eventually die from it.
Firm but truthful, I thought.
Did I mention that Walter was stubborn? He was very quick to tell me that if he died, it would be with two legs. He would not go to the hospital.
Fast-forward a couple years, Walter always laughed and enjoyed showing me that he was walking fine on both legs. No thanks to my advice. We still maintained a great relationship until the day he died.
That has always been the challenging thing about family medicine. We don’t know all the answers, and sometimes we don’t need to. Thanks to the Healer who is not us.
and really let me know what he thought of me and my doctoring vs. the previous professional that he had been a friend and patient of for decades. To make a long story short, this complaint that he requested antibiotics for ended up being treated with cardiac bypass, likely saving his life.
Several months passed, and my wife, newborn daughter, and I were eating at a local restaurant. A woman walked by our table, stopped, and then approached. She got a little teary-eyed and said, “You’re Dr. Paulson, right?”. I said, “Yes.” She paused and said to my wife, “You don’t know me but I want to thank you both. Because of your husband, mine is still alive.” She then told me who her husband was and went on to tell us that he had told her how resistant he had been
to my recommendations and how he had given me a piece of his mind. She went into more detail about his version of what happened and how he begrudgingly went for the testing and treatment that ended up saving his life.
This is and has been extremely impactful to me during my career, and I try to share this story with as many medical students and residents as I can. We must do our very best to gain the best skills and training we can and put those to use in helping people. We must provide the best care even when they don’t understand or appreciate it. Not everyone will be rewarded with a thank you like I was, but you can be sure that there are patients out there that have said it and thought it, even when you don’t know it.
serving on the MAFP board of directors. Family Medicine is about loving people where they are, and I feel honored to have the opportunity to serve.
Pictured: Dr. Shepherd with his wife Alicia and their children, Hailey, JJ, Michael and Matthew.
MO-AFP.ORG 25
Grant Hoekzema, MD, FAAFP Creve Coeur, MO
I have been blessed to practice Family Medicine in St. Louis for the last 30 years. I have the best job that I could imagine, combining the full spectrum care of multiple generations of families with teaching residents and students to be comprehensive, personal physicians.

Family Medicine is the most rewarding and intellectually challenging specialty I could imagine, and the breadth of knowledge needed and the variety of relationships forged was what drew me to it.
Despite having no Family Medicine department or clerkship at Washington University in St. Louis, where I trained, I became committed to family medicine as a career through the influence of the local FMIG and a summer spent as a US Public Health Service - Health promotion/Disease prevention Scholar. I am a proud graduate of the St. John’s Mercy Family Medicine Residency in St. Louis. I now serve as Chair of the Department of Family Medicine in that same institution. I have been actively involved at a national level with Family Medicine Residency training as a board member of the Association of Family Medicine Residency Directors (AFMRD), also serving as President-elect, President, and past-President of the AFMRD.
From that experience as a residency program director, I have been able to since pass on those skills to the next generation of program directors by teaching. I currently sit on the In-Training Examination Review Committee for the American Board of Family Medicine, and I also was privileged to serve as Chair of the Council of Academic Family Medicine in 2013-2014.
Throughout this time in these various roles, I have come to know many amazing leaders in our specialty from all over the country and have been a strong advocate regarding the
importance of having family physicians in such leadership roles. I was selected to join the ACGME Review Committee for Family Medicine in July 2016, and since July 2020, I now serve as Chair. This last role has given me the opportunity to play a major role in shaping the future of our specialty.
In these roles, I have come to appreciate the deep roots that Family Medicine has in Missouri and how that drew me to the specialty and has since nourished my career. Our state should be proud of its tradition of modeling the best Family Medicine has to offer to our country through dedicated fullscope patient care, first-class training and mentoring, and incredible leadership at the local, state, and national level. I believe these strengths come from the day-to-day interactions with our patients, their families, and our colleagues – we live what is happening in health care in our country – in all its many settings, from the exam room to the board room. We must continue the strong tradition of melding our day-to-day experiences with patients and our leadership in medicine. Congratulations to the MAFP – here’s to 75 more years of encouraging and supporting that tradition!
Scheer, MD, FAAFP Gerald, MO
When I started medical school, I thought I wanted to be a super-specialist because Primary Care would be “boring.” During training, I realized that the specialists had such a narrow focus that the poor patient was carved up into body systems and had no way of understanding the overall plan.
So I switched to Family Medicine so I could be the doctor who could pull all those body systems together and help the patient with them all. I have not been disappointed – nor bored! There is no better feeling than seeing the understanding in a patient’s eyes when explaining why this or that is happening or why this treatment is important in a way that the patient “gets”. That feeling of connection keeps me coming to work every day, happy to be a family doc.
Jennifer
26 MISSOURI FAMILY PHYSICIAN January - March 2023
“I LIKE TAKING CARE OF VIP’S, AND THERE’S NO SUCH THING AS AN UNIMPORTANT PATIENT.” ALICIA ALBERS, MD | SEDALIA, MO
Ed Kraemer, MD Lee’s Summit, MO
I guess you could say that a “friend” convinced me to to become a Family Physician. The small town of Friend, Nebraska, that is. Friend is where I did my required Family Medicine Preceptorship for the University of Nebraska College of Medicine. During those 4 weeks, I observed what it meant to be a Family Physician, while experiencing far more clinical responsibility than on any previous rotation. I remember my first “all-nighter”, at the bedside caring for a patient with congestive heart failure in the small hospital’s only “ICU” room.
I’ve always loved variety in life. So, Family Medicine was the obvious choice for me, but that preceptorship experience sealed the deal.
My choice of Family Medicine has been reaffirmed throughout my career by many things, including:
• Developing meaningful relationship with patients, families, and healthcare teams.
• Working with fellow Family Physicians such as Dr. Steve Salanski and many other stakeholders to improve community health in Lee’s Summit.
• Teaching interprofessional students in a clinical servicelearning environment, such as UMKC’s Sojourner Studentrun Free Clinic in Kansas City.
• Working with legislators, other MAFP members (including students and residents) and staff in Jefferson City to improve the quality of health and medical education statewide through legislative advocacy.
• Clowning around with other Family Docs! Yes, that is Dr. Patch Adams! (On the right!)

I’ve always loved being a Family Physician. It has been a great pleasure and privilege!
KRISTIN WEIDLE, MD | WASHINGTON, MO
Andi Selby, DO Branson, MO
Family Medicine offers so many ways to connect with patients. One of the most powerful of these is a home visit.
I was in the last few weeks of my clinical practice before leaving to take an academic position. A spunky patient of mine had been placed on Hospice. She and her sister, also my patient, had some questions about pain management and some other symptoms. I saw the clinic appointment on my
calendar and called them to ask if we could do a home visit instead. The relief I heard in the “Really?” was all the answer I needed.
Driving 30 minutes to get to their home, bumping and splashing along the muddy country roads, I found my patient in bed, smiling, tired. I don’t know how she would have made the trip into my office. We sorted out a medical plan, and I was treated to a tour of the house and land by her sister. The genuine smiles and thanks I received from those women will last a lifetime. I was reminded once again; this is just what family does.
“FAMILY MEDICINE IS THE ONE SPECIALTY WHERE YOU HAVE THE PRIVILEGE OF TAKING CARE OF GENERATIONS. YOU ARE ALSO ABLE TO USE ALL YOUR SKILL SETS FOR A VARIETY OF CONDITIONS AND ILLNESSES. NO TWO DAYS ARE THE SAME.”
What amazing opportunities we have.
“I CHOSE FAMILY MEDICINE TO FOLLOW MY PATIENTS THROUGHOUT THEIR LIVES. I’M GRATEFUL FOR THEIR TRUST TO HELP THEM THROUGH SICKNESS AND HEALTH. I ALSO STILL ENJOY SPEAKING TO 5TH GRADERS ABOUT TOBACCO EDUCATION AND TAR WARS.”
MO-AFP.ORG 27
BRAD GARSTANG, MD | LIBERTY, MO
Josephine Glaser, MD, FAAFP

St. Louis, MO
My name is Josephine Glaser. I am at once a wife of 27 years, a mother of two daughters and two sons, a middle sister, an elderly caregiver, a friend, a mentor, a teacher, a naturalized Filipina-American citizen, a board-certified family physician, and an advocate for life.
I have testified in person and have written curriculum, testimonies, op-eds, and medical society resolutions in support of the life-affirming practice of the healing art and science of medicine grounded on absolute moral and ethical principles.
While growing up in the Philippines, I felt called into medicine in early childhood. I approach patient encounters through the lens of my Filipino heritage, logic, integrated spirituality, and the ethical application of evidence-informed science and medicine. As a result, I value and strive to approach each human being with transcendent and other-centered love, respect, humility, sensitivity, compassion, and dignity from natural beginning and end of life.
I graduated with a major in biology and a minor in psychology at Washington University in St. Louis. I received my medical degree from the University of MO-Columbia School of Medicine (GO TIGERS!). My class was the inaugural class at MU to go through the problem-based learning curriculum.
After seven years of dating, my physician husband, Paul, and I married during our third year of medical school. I delivered the first of our four children by Caesarean section two weeks before medical school graduation.
Fun fact, our graduation year was the first to use the couples match program. Another fun fact, we graduated from two different medical schools in Missouri one day apart! WOW!
We went through our respective residency programs at the University of Kentucky in Lexington--GO C-A-T-S! We practiced full-time in Kentucky for 15 years.
Following GOD’s blueprint for marriage and family, we raised our children in an intergenerational, multi-racial, and multicultural home in Kentucky and Missouri. In 2015, my husband and I felt called and affirmed to move back to St. Louis to provide elderly caregiving for my octogenarian maternal aunt.
I currently work as a primary care physician for Dedicated Senior Medical Center, a division of ChenMed, where VIP seniors are treated like family: with compassion, dignity, and respect. I represent the MAFP as the Primary Care Physician consultant for the ShowMe ECHO initiative.
I enjoy mentoring students, residents, and young physicians. I serve as the Missouri American Academy of Family Physicians St. Louis Director-At-Large, Co-Chair of the Christian Medical and Dental Associations STL Council, AAPLOG FM Section member, Euthanasia Prevention Coalition Board member, AAME MO State Director, and as the Co-Chair of the AAFP Physicians for LIFE Member Interest Group.
I love volunteering in my community. I serve as a Sunday school facilitator and the blood drive coordinator for my church. My husband and I serve as volunteer physicians at a rural clinic for Missourians who go without insurance. On multiple occasions, I’ve served as a volunteer consultant for the Abortion Pill Reversal Network. I enjoy reading, watching anime, and martial arts movies for fun.
Syamala, MD, FAAFP O’Fallon, MO
My first and best story of a family physician was my grandmother’s family doctor in India. My grandmother had a stroke with hemiplegia, and I used to accompany her to her doctor visits. Her family doctor made a connection across three generations (me being the third generation). This created a strong impact on me to choose medicine.
After completing medical school, I took USMLE boards and applied for a family medicine residency in the USA. I enjoyed the breadth of the family medicine specialty. I chose
to be a hospitalist and take care of severely ill patients. The connections that family medicine physicians make are close to none.
I have been a hospitalist for more than 5 years and bring my skills as a family medicine physician to the table. I am part of the Board of Directors for the Missouri Academy of Family Physicians, Vice President of the St. Louis Chapter of the Society of Hospital Medicine, Vice Chair of the AAFP Hospital Medicine Member-Interest Group, and various other roles.
Through these roles, I get to meet amazing family medicine doctors, some of whom take care of every health need in their communities (rural/smaller places).
Dr. Glaser in Medical School.
Krishna
28 MISSOURI FAMILY PHYSICIAN January - March 2023
FAMILY MEDICINE
DAVID KAPP, MD, FAAFP | PERRYVILLE, MO
Amanda Shipp, MD Versailles, MO
I recently came across my integrated residency admissions essay. The final line says, “I believe family medicine is the best way for me to reach my goal of becoming a doctor, the caretaker of an entire town, providing a wide spectrum of care for generations of families, while being an integral part
of the community.” Sometimes I still can’t believe I made it, working in my hometown providing care to the very people that helped me reach my full potential. I love being a part of the community I care for, smiling at patients I see in Walmart. As a rural family practice doctor, I am able to take care of pregnant women, their newborn babies, the dad, grandma, and grandpa. I am able to watch those babies grow and reach their full potential. Maybe some will even come back to our hometown to be the caretaker of the next generations.
David Campbell, MD St. Louis, MO
Since my entrance into medical school was 50 years ago, it is hard to remember a specific event that led me to family medicine. I always wanted to be a physician, and I always saw myself as a family physician.

I do remember that during my freshman year at SLU, we had the opportunity to precept with community physicians. My preceptor was a GP with a small office in south St. Louis. He was letting me take a patient’s sutures out. As I was struggling a bit to do something that I had not previously
done, I asked him a question, to which he responded, “I just want to get these sutures out in the worst way, and I think that is exactly what we are doing.”
There, of course, was a twinkle in his eye when he said that, and those “encouraging” words launched me into my career in family medicine. As far as when a more recent event occurred that reaffirmed my decision, I would say “every day.”
Having spent the first 20 years of my medical education career and the last 22 in underserved health care, I feel blessed and rewarded daily for the direction my career has taken me.
“I ENJOY
PRIMARILY BECAUSE OF THE LONGITUDINAL RELATIONSHIPS I CAN DEVELOP WITH MY PATIENTS OVER THEIR LIFETIMES.”
MO-AFP.ORG 29
Afsheen Patel, MD Overland Park, KS
Family medicine is home. I started my career in medicine at the age of 17 in Dubai. Looking back, I was probably too young to understand the implications of such an important path. I was ambitious, and the glory of emergency medicine and surgery was all I could think about. When I graduated medical school, I decided to pursue my surgical career. Nothing was more exciting than spending the night in the OR. Nothing compared to the adrenaline rush. However, on the other side were doctors who had been doing this for several years. They looked exhausted. At the end of a long shift, they would sit down and state, “as rewarding as this career is, it takes away from your personal life.” But when you are young, you do not listen to good reason or advice. So, I continued my
path in surgery. Along came my nephew a few years later. He was the most beautiful thing I had seen. He made me realize there was a lot more to life than the hospital and its long hours. It was at that time that I realized it was time for a career change. I had spent my entire time and endless hours training to operate in the OR. Life was now at a Crossroads, and I wanted something else. I had already completed my postgraduate degree in the United Kingdom. I loved it, but it was time for a change, and if medicine had taught me anything, it was that life was too short.
I completed my USMLE’s and applied to the US. I was fortunate to match at the University of Missouri Columbia. It would be an understatement if I said the transition was easy. I had moved from a different country and culture. The disease spectrum was different, and I had to learn it all again.
I was fortunate to have wonderful mentors. Dr. Erika Ringdahl was the
program director. She was always there to guide you even on your toughest days. Dr. Kristen Dean was my mentor and made me feel I could accomplish anything. And finally, Dr. Nicole Cronk who would always let you see the bright side of things. This is exactly what family medicine is: the cultivation of belonging, respect, and kindness. No matter who you are or where you come from, you are welcome.
Let it be a colleague, a patient, or a medical student, we are all in this because we love what we do. We see people. Our job is to complete them. We complete medicine. We are the foundation of medicine. It is our compassion to care that makes family medicine. Now, whenever I see a medical student, I give them the same advice I once received. There is a lot more to life, and being a family practitioner allows me to be all that.
Mark Kasten, MD, FAAFP Chaffee, MO
My decision to become a Family Doctor was cemented one day when I was on a general surgery rotation. My father was a general surgeon, and it seemed like that would be my path. One day on rounds, we visited a young woman who had just had one of her breasts removed for cancer. She was very attractive and in her early 40s. The room
was pretty full with the staff Physician, two surgical residents, and four medical students.
The surgeon, who was extremely talented and a very good person, was discussing the case with everybody and was facing away from the patient. He began to describe what was done and the technique involved. I guess maybe I drifted away for a moment and found myself looking directly at the woman’s face. She had tears running down her face as the doctor described the re-
moval of her breast. Her devastation at not being a whole woman anymore was very clear.
It was then that I decided that I could not be a doctor who focused only on “parts” of people. I wanted to see my patients as “whole people.”
“I’VE HAD PATIENTS THAT I’VE KNOWN FOR MANY YEARS, AND IT’S NEAT TO HEAR ABOUT THEIR LIVES AND THEIR UPS AND DOWNS. I LIKE TAKING CARE OF A VARIETY OF DIFFERENT COMPLAINTS. IT’S CHALLENGING AS WELL BECAUSE MEDICINE IS ALWAYS CHANGING, BUT IT’S REWARDING AND FULFILLING.”
CORAL COUCHENOUR, DO | ANDERSON, MO
30 MISSOURI FAMILY PHYSICIAN January - March 2023
Kelly Dougherty, MD St. Louis, MO
Growing up in a rural area, I didn’t know that there were physicians that weren’t family doctors, so when I began medical school, becoming a physician was synonymous with becoming a family physician.
Early in medical school, I started my journey to becoming a family physician, but I would not be where I am today without the incredibly strong female family physicians who mentored me.


As a busy intern learning the ways of the field, I continue to draw inspiration from the women who pushed me, challenged me, and supported me when I doubted myself. As I work to become the family physician I dream of becoming, I am thankful every day for the women who inspire me.
Dr. Todd, thank you for telling me to take the leap, to be confident in my abilities, and proving that you truly can make your dream job a reality.
Dr. Morris, thank you for showing me how to speak the truth, even when it isn’t the easy answer, showing me how to lead with grace, and inspiring me to give back to my mentees the way you have given so much to me.
Dr. Cole and Dr. Wilfling, thank you for teaching me during this incredibly vulnerable point in my training. When I complete my residency, I hope to lead and teach with the empathy and communication skills you display daily.
And, a special thank you to Kathy Pabst, who has aided in my journey, along with so many other family physicians. Kathy, thank you for kickstarting my advocacy journey and teaching me the ropes of Jefferson City. You have been such a gift to Missouri throughout your time with MAFP.

Cheers to 75 years of MAFP and the amazing physicians it has helped produce. I am so thankful for this community and can’t wait to see what the future holds.
Barbara Miller, MD, FAAFP La Russell, MO
I grew up in Oklahoma, with no family members alive who were physicians. Medicine was never even remotely a consideration until I got to college, changed majors from political science to biology, and then wondered what to do next – teaching or medicine? After unsuccessfully applying to graduate school, I kicked around aimlessly for a few years, working as a non-profit director, legal assistant, and then as a research assistant at Mizzou. Eventually, I realized the medicine path would include teaching (although being a teaching physician NEVER crossed my mind!), but teaching would never include medicine. Off to medical school I went…
In Oklahoma, there is a program that helps medical students pay their debts who are willing to commit to primary care and working in underserved areas. I received that scholarship, which covered half of my medical school debt. So, my decision narrowed to family medicine, pediatrics, internal medicine, OB/GYN, and emergency medicine. I was lucky enough to be included as part of a pilot program in which a few students had a longitudinal clinic experience in family medicine through the
MS3 and MS4 years, and that swayed me significantly. There was also a steady stream of feedback from surgeons, OB/GYNs, etc.: “Barbara, you are too smart for family medicine.” I am contrary and stubborn enough to want to prove those voices wrong. It takes a lot of smarts, flexibility, and a million other qualities to do this work and do it well! But the experience which crystallized the choice for me was providing OB care as an OB vs. providing that care as a family medicine doctor. Seeing pregnancy in the context of a family’s life while caring for other family members, the mother, AND the baby, that was IT!!!
And twenty years later, the experience has not disappointed. I have done nearly all we can do in family medicine in a lot of different settings. There has been joy, sorrow, frustration, exhilaration, and constant learning. I love showing medical students the breadth and depth of family medicine; many are starstruck when they see it. The work I am doing now, of developing a new residency program to bring MORE family physicians into the world, is probably the most meaningful thing I will ever do professionally. Before now, I never connected this work to that childbirth/family care experience that was so important for me, but I continue to “birth babies,” even though I am not doing it in labor and delivery anymore!
MO-AFP.ORG 31
In medical school, I learned that I enjoyed taking care of patients of all ages and really being able to lead and coordinate their care. As soon as I started my family medicine rotation, I could tell it was the best fit for me professionally. However, more than the variety of patients that I see, it’s the variety of roles within family medicine that keeps me engaged.
Family medicine has allowed me to be a teacher. I’ve been able to teach medical students, residents, fellow physicians, and, most importantly, my patients. Family medicine allows me to be a leader in my health system, my state and local organizations, and on a daily basis in my office. Some days I am a cheerleader for patients, and other days a confidante. I get to problem-solve and collaborate daily. I decided to be a family physician 15 years ago, and there hasn’t been a single day that I’ve wanted to change that.
Kristen Hemmersmeier, OMS4 Defiance, MO
To me, family medicine has been a dream of mine for many years!
Growing up, I had the pleasure of seeing the ways my own father impacted his patients in our hometown. I remember seeing him come through the door each night—having seen numerous back-to-back patients from all ages and backgrounds—only to hear him say, “I have the greatest job in the world.”
It has become evident to me that even amidst the long hours and exhaustion of challenging patient encounters, my dad believes that what he is doing holds value. His ability to restore the well-being of individuals and their families over the course of their lifetime is something very few people get the chance to do. He is able to build and establish these relationships based on mutual trust and working towards a common goal. Seeing the ways he gets to bring healing and restoration to his patients inspired me to pursue a career in medicine years ago and continues to be a major driving force behind my desire to be in family medicine.
Wael Mourad, MD, MS, FAAFP Kansas City, MO
During medical school, I intended to go into internal medicine. My mother always told me that her ideal doctor was someone who could “do everything.” That stayed at the back of my mind when facing the decision on specialty choice, especially when completing my family medicine rotation early in my fourth year.
During this four-week rotation, each week was devoted to a different area: Med Surg, OB, ambulatory care, and pediatrics. It was during my OB week that I switched my choice to family medicine. I realized that family medicine would allow me to treat adults, children, and pregnant patients.
I could do inpatient and outpatient. I could medically manage as well as employ procedural and surgical skills. I could deliver a baby as well as see a patient in the nursing home. In fact, on my last day of residency training, I did just that. I delivered a baby that morning, rounded on a nursing home patient, and had a meeting with her family that afternoon. Only a family physician can do that.
Fast forward several years and an OB fellowship later, family medicine has allowed me to go into health care administration and move the needle on quality, risk, patient satisfaction, and access to care. The doors that family medicine has opened and the opportunities that have been afforded to make a positive difference in the lives of others is something I will always be grateful for.
“I AM GRATEFUL FOR THE ABILITY TO SERVE WITH A TEAM OF DEDICATED PUBLIC HEALTH PROFESSIONALS (EMTS, EMT-PS, LPNS, RNS, LCSWS, APRNS, AND PAS) WHO PROVIDE CARE TO ONE OF ST. LOUIS COUNTY’S MOST MEDICALLY VULNERABLE POPULATIONS EACH AND EVERY DAY AT THE ST. LOUIS COUNTY JAIL.”
DAWN DAVIS, MD, FAAFP | ST. LOUIS, MO
Kara Mayes, MD, FAAFP St. Louis, MO
32 MISSOURI FAMILY PHYSICIAN January - March 2023
MONICA UNTERREINER, DO | CAPE GIRARDEAU, MO
William M. Zeller, MD, FAAFP Branson, MO
He was a helicopter pilot; I was a medical corpsman serving with the First Marine Division. Our paths never crossed while we both served our country in the Vietnam War, but oh how they would cross as we met in the emergency room one fateful Friday the 13th.
I’ll call him Bob for the purpose of this real life story. Bob returned to civilian life and continued flying helicopters while I returned to college, eventually medical school, and ultimately becoming a board certified family physician. I landed in a small rural community often laden with tourists who came to enjoy the beauty that our community offered. Bob ended up in the same community flying these tourists in his sightseeing helicopter. I flew in many helicopters in Vietnam, but never did feel comfortable in them; especially when the Viet Cong were constantly shooting at them.
Our community hospital was small, 100 beds, and had a six bed ICU. We had one general surgeon, one internist, and a handful of family physicians. At my urging, the hospital had agreed to purchase a new Bennett MA-1 ventilator, mostly used for older patients with respiratory failure. Fortunately, I was fresh out of training from a major medical center where the first critical care medicine fellowship was started by an aggressive group of research anesthesiologists and pulmonologists using high PEEP and treating traumatic lung injuries. I was fortunate enough to spend several months in their unit and little did I know that that experience would help to save Bob’s life.
I was in the emergency room when the ambulance arrived with two survivors of a helicopter crash. One was Bob, the pilot, and the other was a 7-year-old girl. Two others in the helicopter were unfortunately killed when the tail rotor on Bob’s helicopter came off at an altitude of 700 feet, and they plummeted to the ground. This occurred on the worst of days, Friday the 13th.
It was apparent to me that Bob had a flail chest. I had seen that in Vietnam as a result of explosive shrapnel and had seen it once in my residency. Bob’s flail chest was a result of him striking the center console on the helicopter. I immediately intubated Bob and put a chest tube in the right and left chest
cavities, aiding his flail chest. Both he and the 7-year-old girl had deceleration injuries to their livers and spleens as evidenced by abdominal taps (pre CT scan era). By this time we had all the doctors on our staff in the ER. Our general surgeon asked a thoracic surgeon to travel the 40 miles from a larger medical center to help him with the liver and spleen lacerations.
The 7-year-old girl recovered nicely and went home within a week, minus her spleen. Bob, who also lost his spleen, was unfortunately connected to the one and only ventilator. Both the general surgeon and thoracic surgeon agreed Bob should stay in our small hospital and not be moved, but this meant I would have to become a resident again and live at the hospital for the next 10 days managing his ventilator, managing his chest tubes until they could be removed, and caring for him until he could be extubated. He had also suffered a compression fracture of the spine and a fractured ankle as a result of the crash.
After he was extubated, I learned he was a veteran of the Vietnam War, and so as veterans tend to do, we shared old war stories about where we served and what we experienced. Our relationship became more than just doctor and patient. We would talk about cars and the war, and I would always tell Bob that I never wanted to see another helicopter as long as I lived. Bob eventually recovered and moved away; he even went back to flying helicopters. Every year, for many years, I got a nice card and flowers from Bob on the anniversary of his crash.
Then several years ago, Bob and his wife showed up in my office. He and his wife had retired and decided to move back to our community. I was happy to see an old patient, and an old friend, whose life had impacted me so much. He now had arthritis, heart and lung disease, and walked with a cane, but his spirit was still upbeat. He was still the same old Bob, always laughing at me for my fear of helicopters. I was fortunate enough to know and care for Bob and his wife for many years after that.
I recently returned from Bob’s funeral. He had made it to his 80th birthday. He was buried with full military honors. I saluted his flag draped coffin and said goodbye to my patient, my friend, and an old war buddy that I will miss so much.
All names and identifying information have been modified to protect patient privacy.
“I CHOSE FAMILY MEDICINE BECAUSE I APPRECIATE THE BROAD SCOPE OF PRACTICE THAT IT PROVIDES, AND I ALSO ENJOY GETTING TO ESTABLISH A RELATIONSHIP WITH PATIENTS FOR MANY YEARS.”
MO-AFP.ORG 33
Michele Sun, MD, Resident St. Louis, MO
Halfway through my intern year, I had an unexpected setback that crippled my mental health. I was already struggling with the rigorous first year of residency away from my family and medical school friends and felt lost. Without hesitation, my classmates came together to support me both physically and mentally and helped me stand back up. With six months left of residency, I fondly look back at the card they gave me that made me realize why I chose the field of Family Medicine. Catherine, Megan, Viola, Raphael, Ellie - I love you!
Sequita Richardson, MD, FAAFP Raytown, MO
When they ask a young medical student to choose what they want to do for the rest of their lives, they forget that our brains are not even fully mature. How are we to make such a decision based on a few rotations that we had all while trying to be on call, study for boards, and make it through the challenges of everyday life? So when asked to pick a specialty, it was like asking me to eat one Lay’s potato chip. I couldn’t pick just one, just like you can’t eat just one.
I didn’t want to limit myself when there are so many fascinating aspects of the body. So I didn’t. I decided to do it all!
There has been nothing more fulfilling in my medical career than taking care of a young woman in her pregnancy, delivering her child, and then caring for the woman and her child. I have a few families that I have taken care of for four generations of their family.
Rachel L Hailey, MD, FAAFP
Leawood, KS
That is incredible.
But if you are anything like me, these last two years have been challenging to say the least. I often have to remind myself why I chose this field in the first place. So as not to rely on my memory, I have a vase in my office full of reminders from my patients.
There are thank you cards for listening. Notes thanking me for caring for a loved one as they transitioned from this world. As of late, I received a letter thanking me for being an advocate. I think this one has had the most effect on me. Our patients get lost in the technical jargon and bureaucracy of our health care system. They want to know that someone is on their side and will care for them. Navigating our healthcare system is no small feat.
As a young medical student, I had no idea what my life as a family practice physician would have in store. Keeping families healthy is integral to our society, and I consider choosing to serve my community a privilege. I remind myself daily that I am doing God’s work!
I lost my friend Wade last year and didn’t get to say goodbye. This sweet man was the patient I’d had the longest. He started with me during residency over 20 years ago. He worked as a security guard at Baptist Medical Center and played Santa every year.


Wade loved coming to his appointments and taking yearly pictures of us. After I refused several times because it was not a “good hair day,” he started emailing me the day before. He would say, “Tomorrow’s the day - wash your hair!” I looked forward to seeing him. He saw me through my last two pregnancies and always asked about the kids like they were his own grandchildren. Every year at Christmas, he would drop off a box of Russell Stover’s dark chocolates (because they were healthier).
He was a Vietnam Vet and, a few years ago, was awarded the Bronze Star. He never talked about the war, but he was so honored to share his pictures. He would always stand when I came into the room, even with a cane, sometimes a walker, until he was in a wheelchair.
I watched him decline over the past few years, but I didn’t think it was time yet. I wish I had known; I would have gone to say goodbye and given that last long hug. Patients become our friends and touch our lives more than they know. He said he took the pictures so we could remember that our wrinkles are from our smiles. I’m so glad he did so I can always remember him. He is a reminder of why I love what I do. Despite all the hardships we endure as family practitioners, there are joys that make it all worthwhile.
34 MISSOURI FAMILY PHYSICIAN January - March 2023
Charting the Course for the Next Three Years
It’s hard to forecast the future, but with a strong leadership team, the vision of the Missouri Academy of Family Physicians can be clearly set. The MAFP Board of Directors and staff began working on the foundation for the 2023-2025 plan in January 2022 with the commission and board surveys, commission meetings, and interviews of members and staff.
These efforts aligned with the dissemination of the member services survey that was sent to all members. Vince Keenan, CAE, the strategic planner, compiled this data and presented it to the board at the June 1112 meeting at the Lodge at Old Kinderhook, Camdenton, MO. This plan is member-centric to help you provide the best care to your patients and to propel the organization forward as a leader in health care at the local, state, and national levels.
MAFP board members came to clear conclusions on the items they wish to include in the 2023-2025 plan. The infographic on page 36 summarizes the plan’s focus and goals that will drive MAFP’s initiatives during the next 36 months. Keeping in mind that we are nimble enough to address any opportunity that arises for the benefit of Missouri’s
family physicians. The last few years have taught us that we must be flexible and focused as an organization.
One of the most prominent focal points throughout the strategic plan is supporting and growing our future family medicine residents and students. Examples of tactics include increasing participation of residents and students in advocacy efforts, creation of the MO LEADs (Leadership, Education, and Advocacy Development) program, facilitating collaboration among family medicine residencies and medical schools, and support for chief residents.
In addition, physician wellness, member engagement, and awareness of family medicine were ranked as priorities. Each goal includes tactics and tasks that will direct the MAFP Education, Member Services, and Advocacy Commissions during the next three years.

Contact Kathy Pabst at kpabst@mo-afp.org if you would like to receive a complete strategic plan, including the goals, tactics, and tasks, as well as the responsible commission/staff, timeline, completion status, and resources.

MO-AFP.ORG 35
I


2023-2025 Strategic Plan –• • • • • • • • • • • • • • • • • 36 MISSOURI FAMILY PHYSICIAN January - March 2023
Missouri Academy of Family Physicians
Missouri Academy Installs New Officers

The Missouri Academy of Family Physicians installed new officers at the Academy’s 74th Annual Meeting on November 12, 2022, at Big Cedar Lodge in Ridgedale, Missouri. Serving as President last year, John Burroughs, MD, became Board Chair of the family medicine group.

Other officers include President Kara Mayes, MD, FAAFP; President-Elect Afsheen Patel, MD; Vice President Natalie Long, MD; and Lisa Mayes, DO, who completed year one of her three-year term as Secretary/Treasurer.
BURROUGHS (BOARD CHAIR)
John Burroughs, MD, of Liberty, Missouri, was installed as Board Chair. Dr. Burroughs is the medical director for Crossroads Hospice and Palliative Care. He precepts medical students from the UMKC School of Medicine and numerous nursing students. As a certified yoga instructor, he provides yoga and mindfulness classes to his patients and the community. Dr. Burroughs received his undergraduate education at Duke University, a medical degree at Wake Forest University, and residency training at the University of Utah. He is board certified by the American Board of Family Medicine. Dr. Burroughs has four children.
K. MAYES (PRESIDENT)
Kara Mayes, MD, FAAFP, of St. Louis, Missouri, was installed as President. Dr. Mayes practices at Mercy Clinic Weight and Wellness in Ballwin, Missouri. She completed medical school at Saint Louis University and residency at the Mercy Hospital Saint Louis Family Medicine Residency program. She is board certified in family medicine and obesity medicine. Dr. Mayes is married and has two children.
PATEL (PRESIDENT-ELECT)
Afsheen Patel, MD, of Lee’s Summit, Missouri, was installed as President-Elect. Dr. Patel practices at the St. Luke’s Primary Care Clinic in Lee’s Summit with a special interest in women’s health care, sports medicine, geriatric care, and primary and preventative care. She completed her medical school training at the Royal College of Surgeons United Kingdom and her residency at the University of Missouri Columbia Family Medicine Residency program. She is board certified by the American Board of Family Medicine. Dr. Patel is married and has four children.
LONG (VICE PRESIDENT)
Natalie Long, MD, of Columbia, Missouri, was installed as Vice President. Dr. Long completed her medical school and family medicine residency at University of Missouri Columbia (UMC). She practices full-spectrum Family Medicine and has a special interest in maternal mental health, opioid dependence management, and pregnancy care. She holds the rank of Associate Professor of Clinical Family and Community Medicine at the UMC School of Medicine. She resides in Columbia, MO with her husband and four children.
L. MAYES (SECRETARY/TREASURER)
Lisa Mayes, DO, of Macon, Missouri, completed year one of a three-year term as Secretary/Treasurer of the Missouri Academy of Family Physicians (MAFP) for a 3-year term. Dr. Mayes is employed by the Samaritan Hospital in Macon, Missouri, and has been practicing for 13 years. She is board certified in family medicine. She graduated from AT Still University in Kirksville and completed her residency at Northeast Regional Medical Center in Kirksville, Missouri. Dr. Mayes has three daughters.
MAFP PRESIDENT KARA MAYES, MD, FAAFP 2022 INSTALLATION REMARKS
Sarah [Cole, DO, FAAFP] has been a role model for me in so many ways since I first met her about 14 years ago as a medical student. She was an important part of my medical training, always pushing me to improve my medical knowledge and patient care. She’s been the family physician for many of my family members, including my kids and my mom. She’s been a role model for me in leadership, both at work and here at MAFP. Even when I think I’ve done all of the things, she finds a new way to push me to grow, which is why we’re currently working on a pilot to add additional training in obesity medicine for family medicine residents. But while she seems to “do it all” at work, she is also a great role model in the way she
MO-AFP.ORG 37
prioritizes her family and her own passions outside of work. And more importantly, she has become a great friend.
I also need to express thanks to MAFP’s leadership before me. I have only had great examples of leadership to follow during my time on the board. Special thanks to our most recent presidents, John Burroughs and John Paulson, for welcoming me to the executive commission and leading MAFP through the many changes that the past couple years have thrown at all of us in healthcare.
The only way we can all lead this organization while also continuing our fulltime practices as physicians is with the help of an amazing staff. Kathy, Bill, and Brittany go above and beyond their job descriptions on a regular basis, and they really make it easy for us to continue to grow the impact of MAFP.
This summer we had a strategic planning session to work on the vision for MAFP over the next 3 years. We’ll spend time as a board tomorrow finalizing the plan. I’m most excited for some of the plans we have in place to further engage students and residents in the Academy so that we can continue to grow family medicine in the state of Missouri.
Last, I want to thank all of my family for their support. My kids are often on their own for bedtimes when I’m on zoom meetings in the evenings. My husband Matt gets occasional solo parenting time when I’m traveling for these conferences and meetings, or if he’s also gone, my parents are often stepping in to help. Matt also has continued to encourage me to step into roles that I don’t quite feel ready for, like this one.
I’m incredibly excited to be leading the Missouri Academy this year. Thank you everyone for your involvement and support.
Cole Receives MAFP Exemplary Teaching Award

The Missouri Academy of Family Physicians presented Sarah Cole DO, FAAFP, of Saint Louis, Missouri, with the 2022 Exemplary Teaching Award at the Academy’s 74th Annual Meeting on November 12, 2022, at Big Cedar Lodge in Ridgedale, MO. A committee of family physicians selected Dr. Cole from nominations made by patients, community members, and fellow physicians.
The Exemplary Teaching Award acknowledges MAFP members who deserve recognition for exemplary teaching skills and individuals who have implemented outstanding educational programs and/or developed innovative teaching models.
Dr. Cole has served on the MAFP board since 2014 and is a past president. She served as co-chair of the MAFP Education Commission where she helped plan quality and scientific Continuing Medical Education (CME) for members in addition to serving as a member of the Advocacy Commission. She continues her commitment to family medicine as an alternate delegate to the AAFP Congress of Delegates.
Dr. Cole is the program director of Mercy Family Medicine Residency and supports andragogical teaching approaches for her residents. She encourages her residents to follow individualized learning plans to develop their ability to define goals and work toward them from subject-centered to learner and community-centered. Her proactive and innovative approaches to teaching at Mercy prepare our future family physicians to lead in their communities with compassion, expertise, and joy.
On a national scope, Dr. Cole is a board member of the Association of Family Medicine Residency Directors and is the liaison with the American Board of Family Medicine, where she works on a project to adjust residency curriculums to achieve graduate outcomes. One resident said she wanted “to be Dr. Cole when she grows up” – a teaching family physician.
Dr. Cole earned her undergraduate degree in biology from Truman State University in Kirksville, MO, and her medical degree from Kirksville College of Osteopathic Medicine. She completed her family medicine residency at Mercy Family Medicine Residency in St. Louis, MO.

38 MISSOURI FAMILY PHYSICIAN January - March 2023
Rasmussen Named MAFP Family Physician of the Year

The Missouri Academy of Family Physicians presented Charlie Rasmussen, DO, FAAFP, of Reeds Spring, Missouri, with the 2022 Family Physician of the Year Award at the Academy’s 74th Annual Meeting on November 12, 2022, at Big Cedar Lodge in Ridgedale, Missouri. A committee of family physicians selected Dr. Rasmussen from nominations made by patients, community members, and fellow physicians.
Dr. Rasmussen has continuously practiced full-scope family medicine in southern Missouri, including obstetrics, inpatient medicine, pediatric medicine, and adult medicine. He knew rural healthcare was his passion due to mentors sharing their joys of working in a rural community. A highlight in his career as a family physician was delivering his own daughter at a rural hospital.
Dr. Rasmussen practiced in Houston, MO, at Texas County Memorial Hospital. There he became board certified in hospice and palliative care and took a position as the director of Texas County Hospice. He currently serves as the regional director for Good Shepard Hospice in Branson, MO and describes this as one of his favorite areas of medicine.
Following his time in Houston, he and his family moved to Branson to be closer to family. In 2017 Dr. Rasmussen opened a solo practice, Table Rock Family Medicine and Obstetrics, which is a culmination of his previous experience of caring for patients throughout their lifespan. Among many other accomplishments, he has attended to the birth of over 1,200 babies.
Dr. Rasmussen describes his career in family medicine as remarkable. “There have been some incredible saves and painful losses,” he said. “If I stopped right now, I don’t think anyone would argue what an incredible and fulfilling career I have had serving the patients of rural Missouri, but I can’t wait to see what the second half of my career brings.”
The hard work continues, though, as Dr. Rasmussen has formed a partnership teaching a rural family medicine residency program in Salina, KS, on top of mentoring medical students at programs
throughout the state of Missouri. He is also in the process of starting a drug and alcohol treatment clinic with a fellow physician.
A Kansas City University Medical and Biomedical Science graduate, Dr. Rasmussen was one of the chief residents at CoxHealth Family Medicine Residency program in Springfield. He is married with one daughter and continues to reside in Branson.
2022 FAMILY PHYSICIAN OF THE YEAR SPEECH

CHARLIE RASMUSSEN, DO, FAAFP
Thank you very much for this prestigious award. I share this award with all who have helped me along the way.
I’ve spent the better part of the last 15 years in underserved areas of Missouri taking care of expectant mothers and then for the babies they delivered - their siblings and their parents and grandparents. I’ve taken care of patients of all ages - literally the spectrum of family medicine that I wrote about in my application to medical school all those years earlier…. And it’s truly been an honor. I want to thank all my patients who have entrusted me as their family physician; it’s an incredible blessing and privilege.
I have a lot more thank you’s to pass along. I want to thank Dr. Paulson, Kathy, and the Missouri academy. I’d like to thank my good friend and fellow family physician Dr. Hughes who nominated me. I’d like to thank all my residency colleagues who, to this day, are all good friends, and many are here today - mainly because I told them they HAD to come to see this!
Thank you to my team at TableRock Family Medicine and Obstetrics - my two great nurse practitioners, Hannah and Leisha, and my long-time nurse Rae Ann. They do all the work, and I take all the credit because I’m just the pretty face there.
MO-AFP.ORG 39
I want to thank some important teachers along the way - Drs. Bell, Halverson, and Sontheimer and my previous partners and friendsDr. Catie Benbow and Dr. William Wright and all the residents and students who pushed me to be a better physician and person. I want to thank all the nurses, respiratory therapist and all the other medical staff that I’ve worked with through the years that have probably taught me more than anybody else. I obviously want to thank my parents who sacrificed and helped me along the way as a first-generation physician.
A huge thanks to my wife, Stacey, with whom I couldn’t have done the things professionally that I have done - without her. She has sacrificed so much to make sure myself and my daughter succeed. And I want to thank Rylee - my smart and beautiful daughter, who I strive to set an example for everyday - she’s made some sacrifices along the way too while I’m out working my 60+ hour weeks. Rylee understands by now when I say I’m finishing rounds - I’ll be there in 15 minutes that it really means I’ll be there about an hour or two. She understands when I’m headed out the door to deliver a baby that likely I won’t be home until the following night. I hope one day, she’ll understand this purpose-driven life we all have embarked on as physicians and will appreciate the sacrifice. I believe that the life you live - is the lesson you teach, and I hope she’s learning this lesson - chase purpose in your life.
I don’t want to take up all the time here I know we have better stuff to get to, BUT I do have one more very special person to thank, and in order to do that, I adapted the last part of this speech from one of my all-time favorite speech and songwriters….Snoop Doggy Dogg. Maybe some of you have heard his songs or know this version of this speech he once gave - so here it goes!!!
Last but not least I’d like to thank…me!!
I wanna thank me for having no days off. I wanna thank me for never quitting. I wanna thank me for going hundreds of thousands of dollars in debt to become a family physician. I wanna thank me for always being a giver and trying to give more than I receive. I wanna thank me for getting out of bed at 3 am to deliver all those babies. I wanna thank me for doing more right than wrong. I wanna thank me for doing all those circumcisions and I just want to thank me …for being me …at all times!!
Millions of patients have shared with family physicians on the best and worst day of their lives, and after all the trials and hassles of the insurance companies, corporate medicine, government interference, and others things that detract from the patient-physician relationship, we still have the best jobs in the world.
Give first and without expectation, and you will get more than you’ve ever given. Emerson said it is one of the beautiful compensations of life that no man can sincerely try to help another without helping himself. These guiding principles are 100 percent true and have allowed me to enjoy my calling and remarkable career as a family physician. I believe what you focus on - is your experience. There is so much good that we do as family doctors that sometimes we just have to step back in a moment like this to see it. If you focus on the goodness of your career and your life, you’ll see more of it.
Thank you again for this award; truly one of the highlights of my career. I’ll always treasure it. Thank you!!
40 MISSOURI FAMILY PHYSICIAN January - March 2023
I OBVIOUSLY WANT TO THANK MY PARENTS WHO SACRIFICED AND HELPED ME ALONG THE WAY AS A FIRSTGENERATION PHYSICIAN
Three Physicians Receive the MAFP Distinguished Service Award

The Missouri Academy of Family Physicians presented Patrick Harr MD, FAAFP; Peter Koopman MD, FAAFP; and Keith Ratcliff MD, FAAFP, with the 2022 Distinguished Service Award at the Academy’s 74th Annual Meeting on November 12, 2022, at Big Cedar Lodge in Ridgedale, MO. A committee of family physicians selected these recipients from nominations made by patients, community members, and fellow physicians.

The Distinguished Service Award recognizes members, nonmembers, and entities for their long-time dedication to advancing, contributing, and supporting the MAFP and the specialty of family medicine.
PATRICK HARR, MD, FAAFP
Dr. Harr is a family physician from Maryville and is retired, but he still serves as the team physician for Maryville High School and Northwest Missouri State University.
Dr. Harr has served both the AAFP and the MAFP throughout his career. He held the prestigious position of president of the AAFP from 1996-1997 and the MAFP in 1989. To become president of any organization is an obligation of service through committee work and board service. Dr. Harr is no exception, with many years of sharing his knowledge and expertise at the local, state, and national levels.
In addition to his commitment to his professional organizations, he has been involved at the community level by serving on medical boards, various committees, and other volunteer work.
Dr. Harr earned his undergraduate and medical degrees from the University of Missouri Columbia. He completed his family medicine residency at the University of Rochester.
PETER KOOPMAN, MD, FAAFP
Since 2009, Dr. Koopman has served on the MAFP Board of Directors, beginning as a district director, moving to leadership roles, and is now a past president. He is currently serving as a Delegate from Missouri for the American Academy of Family Physicians (AAFP) Congress of Delegates. In addition, Dr. Koopman was recently appointed to serve as the Chair of the AAFP Commission on Federal and State Policy.
Dr. Koopman is a Clinical Family and Community Medicine Professor at the University of Missouri- Columbia. He serves as
the Elective Director for the University of Missouri Family Medicine Clerkship for the medical school and is involved in family medicine advocacy, teaching, exam creation, and mental and behavioral health care for his community. He also continues an active Family Medicine practice in Columbia.
In his spare time, Dr. Koopman volunteers at local organizations and loves music and playing the guitar.
Dr. Koopman earned his undergraduate degree in psychology from the University of Pennsylvania and his medical degree from the University of Pittsburgh. He completed his Family Medicine residency at the St Margaret’s Hospital affiliated with the University of Pittsburgh.
KEITH RATCLIFF, MD, FAAFP
Since 2003 Dr. Ratcliff has served on the MAFP Board of Directors, beginning as a district director, moving to leadership roles, and is now a past president. He is co-chair of the MAFP Advocacy Commission and fulfilling his final year of representing MAFP at the AAFP’s Congress of Delegates.
Dr. Ratcliff is a family physician at the Mercy Clinic Four Rivers Family Medicine in New Haven. He has precepted medical students and residents, in addition to training paramedics and EMTs. He has also participated in several mission trips to Honduras.
Dr. Ratcliff describes his journey with the Academy as rewarding. “I continue to learn compassion, compromise, and collegiality from some of the most passionate and engaging physicians that I have ever met,” he said. “Over the decades, our Academy has given more to me than I can ever give back.”
When he is not working or volunteering his time, Dr. Ratcliff enjoys flying across the country. He is involved in the Franklin County Honor flight and has supported over 3,000 veterans to see their memorials in Washington, DC. In addition, he and his wife, Judy, enjoy camping, riding motorcycles, working on the farm, and guiding their four children to become adults.
Dr. Ratcliff earned his undergraduate degrees in both biology and chemistry from Washington University in Saint Louis. He then earned his medical degree from the University of Missouri Columbia, where he also completed his family medicine residency.
MO-AFP.ORG 41
2023 Legislative Session Has Started
RJ Scherr & Associates
Randy Scherr and Brian Bernskoetter Governmental Consultants
The General Assembly of Missouri convened on January 4th and will close on May 12th.
With the 2022 elections, there will be new leadership, new committee chairs, and 50 new House and Senate members (out of a total of 197). With that much change, it’s customary for the Senate and House to get off to a slow start. That said, it’s difficult to predict whether legislators will hit the ground running.
The House of Representatives will be led this session by Speaker Dean Plocher (R-District 89), an attorney from St. Louis, and Majority Floor Leader Jon Patterson (R-District 30), a private practice general surgeon from Lee’s Summit. On the Senate side, they will be led by President Pro Tem Caleb Rowden (R-District 19), owner of a marketing company in Columbia, and Majority Floor Leader Cindy O’Laughlin (R-District 18) whose family business is in trucking and concrete work in Shelbina.
The last session ended on a very poor note. There was infighting between members of the Senate, including the more traditional stand-offs between the House and Senate about which priorities to advance. This session has the potential to move in a more positive direction, but it’s too soon to know.
Many Republican members of the Senate were challenged in their primary election races by candidates that were supported by the now disbanded “Conservative Caucus.” The Senate Floor Leader’s race was supported by former members of the Conservative Caucus. There is hope that this development could smooth out some of the friction in the Senate. It’s important to note for our interests that this will be the first year since 2011 when there wasn’t a doctor in the Senate. We lost a true champion for physicians when Senator Bill White lost his reelection bid.
While we can expect many of the same legislative policy issues to bubble up this session, it will be a very different lineup of legislators considering those proposals. Although this dramatically alters how proposals move through the legislative process, your participation in the legislative process will help educate legislators and identify new champions for physician issues.
The biggest scope of practice battles next session will likely come from APRNs, pharmacists, and physical therapists (PT). There are a bevy of proposals on APRN scope ranging from full repeal of the collaborative practice statutes to smaller changes. Pharmacists have been pushing the last couple of sessions to expand what they can do under the statute. Specifically,
they want to expand the vaccines they can administer and the administration of medication therapy plans. Lastly, the PTs have pushed for direct access for patients for several sessions.
In addition to scope battles, it’s likely abortion, genderaffirming healthcare, and vaccines will also be major issues for the MAFP. We need to be very mindful of the impact these proposals have on family medicine.
There is hope amongst the medical community that a proposal similar to Texas’s “Gold Card” prior authorization language can be brought forward this session. This bill was filed last session by Sen. Bill White, and thus far, another champion on this issue hasn’t been identified. The intent of the legislation is to reduce the instances of physicians required to get prior authorization if they have a track record of success with the insurer on a given procedure.
Budget battles always shape the way the General Assembly operates, and this year will be no different.
The State of Missouri is currently holding record reserves on the books ($6 billion and climbing), but state budget leaders are projecting less growth for 2023.

Sarah Cole, DO, Program Director at Mercy Family Medicine Residency, presented testimony before the House Health Care Cost Study Group in October. Her testimony can be found on page 45, which addresses the barriers to expanding family medicine residencies, and the capacity to do so.
It is sure to be another interesting legislative session, and we are looking forward to providing you with weekly updates on legislative and regulatory issues.
Preceptor Tax Credit Implementation Slow
As you know, the Missouri Academy of Family Physicians had a huge win last session with the passage of the Preceptor Tax Credit Program. Although the bill calls for implementation in January 2023, the rules have not yet been finalized. They are in the process of being crafted by the Missouri Department of Health and Senior Services and the Missouri Board of Healing Arts. The legislation states that the collection of the additional license fee shall begin on January 1, 2023. The board has been surveyed on an emergency rule. As of the time of this publication, the outcome of that vote is unknown. The process for claiming the tax credit will be included in the proposed rules once they are published.
The preceptor tax credit is available to a primary care physician or physician assistant who precepts a medical student
42 MISSOURI FAMILY PHYSICIAN January - March 2023
or physician assistant for a minimum of 120 hours of communitybased instruction in family medicine, internal medicine, pediatrics, psychiatry, or Ob/Gyn. A community-based faculty preceptor may add together the amounts of preceptorship instruction time separately provided to multiple students in determining whether he or she has reached the minimum hours required under this subdivision, but the total preceptorship instruction time provided shall equal at least 120 hours to be eligible for the tax credit. The $1,000 tax credit is allowed for each preceptorship, up to a maximum of $3,000 per year, and

does not receive any direct compensation for the preceptorships.

For example, if you precept four students for 30 hours each in spring 2023, that would qualify for one $1,000 tax credit on your 2023 taxes which will be filed in 2024. The tax credit cannot be applied to past or future income taxes due. There are only 200 tax credits available each year, and they will be awarded on a first-come, first-served basis. You should always consult your accountant for any income tax questions.
Look to MAFP for additional information on the preceptor tax credit as it becomes available.

SEhealth.org For questions, contact Brooke Schlitt at 573-519-4511 or bschlitt@sehealth.org The Southeast Missouri region is nestled along the banks of the Mississippi River and provides exceptional recreational opportunities with lakes, fishing, hunting, hiking, swimming pools, parks, tennis courts, racquetball courts, golf courses and country clubs, along with outstanding school systems, historical sites and other attractions. Be a member of a dedicated and inspired team. JOIN US TODAY! Competitive Salary + wRVU-based Productivity Incentives Signing Bonus Relocation Assistance Residency Stipend if sign early Student Loan Repayment 6 weeks paid time off + Paid CME Allowance Full Benefits, including Health, Dental, Vision, FSA & 403 (b) options Limited Call, No Weekends, No Obstetrics Large established practice in State-of-the-Art Facility Subspecialty and Mid-Level Support Network of more than 50 care locations in 13 communities, including hospitals, primary and specialty care clinics representing over 30 clinical specialties. Collaborative, positive integration within SoutheastHEALTH furthering strategic development of regional services. SoutheastHEALTH has approximately 2,400 employees and serves a population of approximately 675,000, primarily in a three-state area Seeking FAMILY PRACTICE PHYSICIANS 2023 LEGISLATURE IMPORTANT DATES DECEMBER 1, 2022 – BILL FILING OPENS JANUARY 4, 2023 – SESSION CONVENES FEBRUARY 13-14, 2023 – MAFP ADVOCACY DAY MAY 12, 2023 – LAST DAY FOR BILLS TO BE CONSIDERED MAY 13, 2023 – LAST DAY TO PASS BILLS MAY 31, 2023 – SESSION ADJOURNS JULY 14, 2023 – GOVERNOR’S APPROVAL BY AUGUST 27, 2023 – EFFECTIVE DATE OF LAWS SEPTEMBER 2023 – VETO SESSION MO-AFP.ORG 43 43 MISSOURI FAMILY PHYSICIAN January - March 2023
Physician Wellness & Upcoming Retreat
A Perspective from Amanda Shipp, MD and John Paulson,
PhD, FAAFP on the AAFP Leading Physician Wellness Program
 Amanda Shipp, MD Versaillies, MO
DO,
John Paulson, DO, PhD, FAAFP Joplin, MO
Amanda Shipp, MD Versaillies, MO
DO,
John Paulson, DO, PhD, FAAFP Joplin, MO

Iwas accepted into the inaugural class of the AAFP Leading Physician Wellness program in 2020. I found myself surrounded by other physicians who went through similar struggles with burnout and wanted to change the system. We learned about the power of gratitude, mindfulness, and loving-kindness. We identified personality traits like perfectionism and people-pleasing that helped us achieve so much but were now standing in our way. We learned to change our mindset, be good enough, set healthy boundaries, and reframe difficult situations.
My hospital announced a Chief Wellness Officer, and I volunteered for the physician wellness committee. I shared my story on burnout panels for residents and students. I signed up for PeerRx to have a physician buddy supporting me. I also joined a committee to plan a wellness retreat for Missouri physicians.
I still start to feel burned out at times, but I’ve learned my warning signs, and now I know how to reach out for help to put out the flames.
Recently, I completed the AAFP Leading Physician Wellness certificate program. I learned how to identify burnout and a handful of things one can do to address it, primarily focused on self-care. As an academician, I have had the opportunity to share what I have learned regarding wellness with various learners in multiple venues. Thanks to this program, I have initiated wellness efforts within my department and at the university level as I now serve on the University’s inaugural wellness council.
This program has had a significant impact on me both personally and professionally. I have learned how to objectively and subjectively measure my wellness at any time and address those areas of weakness accordingly. I’m trying to improve my ability to translate what I have learned to pass it on to others who need such skills.
The one thing that I wasn’t expecting was how this program has renewed my passion and curiosity. I have become fascinated with discomfort science and hope to learn about and master its potential as a possible solution for burnout. Self-care and wellness should not be seen as weaknesses. It’s the key to sustainable healthcare and maximizing our potential as a profession.
Dr. Shipp and I are on the planning committee for a collaborative wellness retreat for Missouri physicians, and I hope to be able to share some of what I have learned with those who choose to attend.
SAVE THE DATE Physician Wellness Seminar October 20-22 Margaritaville Lake Resort Osage Beach, MO Cosponsored by: MAOPS, MAFP, MSMA
44 MISSOURI FAMILY PHYSICIAN January - March 2023
DO YOU HAVE NEWS TO SHARE?
Email it to office@mo-afp.org for review. We love to hear from our members!
Pabst Appointed to Advisory Commission

Kathy Pabst, MBA, CAE, MAFP Executive Director was appointed to serve as the designated layperson on the Missouri Board of Healing Arts, Advisory Commission for Physician Assistants. This commission guides, advises and make recommendations to the Board of Healing Arts. The commission is also responsible for the ongoing examination of the scope of practice and promoting the continuing role of physician assistants in the delivery of health care services.
Family Medicine Residencies: Opportunities & Barriers to Increasing Missouri Family Medicine Residencies
The Missouri House Health Care Cost Study Group was formed over the summer to identify opportunities to increase Missouri’s physician workforce. Sarah Cole, DO, Program Director, Mercy Family Medicine Residency, presented testimony on behalf of the MAFP to this informal group. She presented an overview of a graduate medical education study that the MAFP conducted of all the Missouri family medicine residency programs.
Her virtual testimony noted that according to the Kaiser Family Foundation Missouri is ranked 2nd worst of all the states with the most unmet need for primary care physicians. Outside of Delaware, we have the fewest number of primary care physicians available per capita to our state population. According to the Rural Information Hub, of the 114 counties in Missouri, 113 are considered fully or partially a primary care health profession shortage area. Only ONE county in Missouri is NOT a primary care shortage area.
She continued sharing that Missouri has more than an adequate number of medical students. According to the 2021 State Physician Workforce Data Report, Missouri enrolls 4,555 medical students, ranking 3rd in the nation for the number of medical students enrolled per capita. This represents a 32% increase over the past 10 years, as Missouri’s medical schools have both expanded and opened satellite campuses.
Unfortunately, what Missouri does NOT have is an adequate number of residency spots to train those 4,555 medical students. Residency programs have simply not been funded to keep pace with the increase in medical school enrollment. As a result, about a third of Missouri’s medical school graduates are forced to look to other states for residency training. One way to stop this hemorrhage and reduce primary care shortage areas is to expand the number of primary care residency training spots in-state.
As with every venture, there are barriers to think around. In this case, barriers to increasing family medicine residency capacity are funding, faculty and facilities.
Funding: Funds are needed either to start a residency or to
maintain it. Because the funds needed to start a new residency run in the neighborhood of $750,000 and the time to do so takes up to 3 to 4 years, a more feasible approach is to simply expand existing residencies. Because even this incurs some recurring, annual, direct expenses per resident, one-time funding is not a long-term solution.
Faculty: Missouri is already a family physician shortage state and those already in practice labor long hours to care for their patients. It will take creativity to recruit and retain family physicians to serve as mentors and faculty to resident physicians in a way that ensures equitable distribution of training without compromising patient access or safety.
Facilities: More residents and faculty in a clinic also means more patients and so physical space must be considered.
Once funding, faculty and facilities are secured, additional spots within an existing residency must be approved by an accrediting body, but this takes weeks to months, not years.
Missouri has 12 existing family medicine residencies, primarily located around Columbia, Jefferson City, Joplin, Kansas City, Kirksville, St. Louis, Sedalia and Springfield. Some of these programs – typically those that are large or public-university-sponsored--have already expanded using alternate resources. According to a 2021 survey by the MAFP, it may be the smaller and community-hospitalbased programs that currently have the most capacity to expand with state fiscal assistance.
Putting this all together, the Robert Graham Center projects Missouri needs 687 family physicians by the year 2030, which is an 18% increase from today. The MAFP surveyed existing family medicine residencies in 2021 and determined a potential capacity increase of 17 residents/year. If Missouri were to provide funding for this capacity for even three years, it can train an additional 51 family physicians, or a 21% increase, which closes the gap projected by the Robert Graham Center.
To summarize, state-funded expansion of existing family medicine residencies may provide Missouri a solution to its primary care physician workforce deficit.
MEMBERS IN THE NEWS MO-AFP.ORG 45
Mercy
Medicine
Second-Year Resident Physicians | Class of 2024



















Family
2022-2023 Resident Roster Your life is our life’s work.
STL_37046 (4/22/22)
Peyton Bennett, DO Rikki Koebler, DO Mafeth Lim, DO Jason Maddox, DO Lauren Malinowski, DO Hannah Yasin, MD
Third-Year Resident Physicians | Class of 2023
Elizabeth Hoover, DO Viola Hoxha, MD Megan Landis, DO Catherine Baker, MD Michele Sun, MD Raphael Yang, MD
First-Year Resident Physicians | Class of 2025
46 MISSOURI FAMILY PHYSICIAN January - March 2023
Kelly Dougherty, MD Ashlyn Edwards, DO Rebecca Jadwisiak, DO Emily Shank, DO Sarah Spearman, DO Jordan Wills, MD
Reprint due to misprinting in previous issue.




–
pm Legislative Briefing and Dinner,
8:00 – 9:00 am – Buffet Breakfast at Courtyard Marriott 9:00 am – 1:00 pm – Legislator Appointments (Scheduled by MAFP staff) 11:30 am – 1:00 pm – Buffet Luncheon at Courtyard
1:00 – 4:00 pm – MAFP Board of Directors Meeting We encourage you to invite a colleague, medical student, or resident and join you to promote the importance of family medicine and primary care.
your opportunity to educate your State Senator and State Representative
issues
affect you, your profession, and your patients.
your lodging reservation at the Courtyard
MO,
Be
Family
to receive the discounted rate
reservation
Any reservations
that date are subject to availability. Limited complimentary lodging is available with
to residents and students. To request a complimentary
JOIN US AT THE COURTYARD MARRIOTT & THE MISSOURI STATE CAPITOL, JEFFERSON CITY, MO ADVOCACY DAY FEBRUARY 1314, 2023 REGISTER ONLINE: WWW.MO-AFP.ORG/ADVOCACY/ADVOCACY-DAY/ YOU ARE THE VOICE OF MISSOURI FAMILY PHYSICIANS!
MONDAY, FEBRUARY 13 6:00
8:30
Courtyard Marriott TUESDAY, FEBRUARY 14
Marriott
This is
on
that
Make
Marriott, 610 Bolivar Street, Jefferson City,
65101, 573-761-1400.
sure to reference the Missouri Academy of
Physicians
of $131 per night. The last day to make a
in our block is January 20, 2023
made after
preference
room, contact Kathy Pabst at kpabst@mo-afp.org or 573-635-0830.
Missouri Academy of Family Physicians
722 West High Street
Jefferson City, MO 65101
Each session will offer 2.0 CME Credits. Sessions are held from 6:00-8:00 pm via Zoom.



February 23 OB/GYN and Maternal Health April 27 Men’s Health March 23 Adolescent Care
May 25 Nutrition and Obesity
Learn more and register online: www.mo-afp.org/cme-events/virtual-cme




















































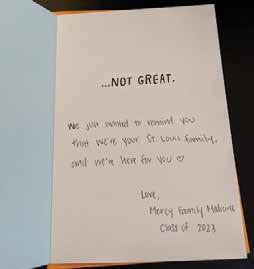











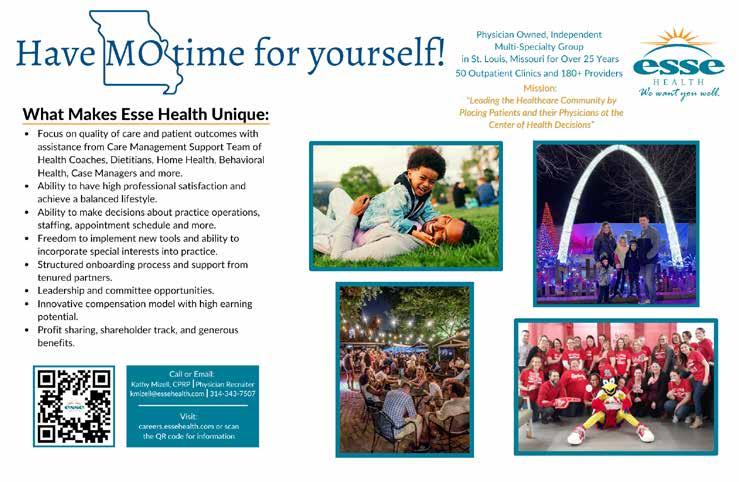






 Amanda Shipp, MD Versaillies, MO
DO,
John Paulson, DO, PhD, FAAFP Joplin, MO
Amanda Shipp, MD Versaillies, MO
DO,
John Paulson, DO, PhD, FAAFP Joplin, MO



























