MISSOURI FAMILY PHYSICIAN
VOLUME 43, ISSUE 2




FAMILY MEDICINE CAREER TRANSITIONS




FP SPRING 2024
2 MISSOURI FAMILY PHYSICIAN January - March 2024
EXECUTIVE COMMISSION
BOARD CHAIR Kara Mayes, MD, FAAFP (St. Louis)
PRESIDENT Afsheen Patel, MD (Kansas City)
PRESIDENT-ELECT Natalie Long, MD (Columbia)
VICE-PRESIDENT Beth Rosemergey, DO, FAAFP (Kansas City)
SECRETARY/TREASURER Lisa Mayes, DO (Macon)
BOARD OF DIRECTORS
DISTRICT 1 DIRECTOR Arihant Jain, MD, FAAFP (Cameron)
ALTERNATE Brad Garstang, MD (Kansas City)
DISTRICT 2 DIRECTOR Eric Lesh, DO (Kirksville)
ALTERNATE Katherine Holbrook, DO (Kirksville)
DISTRICT 3 DIRECTOR Dawn Davis, MD, FAAFP (St. Louis)
DIRECTOR Lauren Wilfling, MD, FAAFP (St. Louis)
ALTERNATE Christian Verry, MD (St. Louis)
DISTRICT 4 DIRECTOR Jennifer Allen, MD (Hermann)
ALTERNATE Jennifer Scheer, MD, FAAFP (Gerald)
DISTRICT 5 DIRECTOR Amanda Shipp, MD (Versailles)
ALTERNATE Vacant
DISTRICT 6 DIRECTOR David Pulliam, DO, FAAFP (Higginsville)
ALTERNATE Misty Todd, MD (Sedalia)
DISTRICT 7 DIRECTOR Chad Byle, MD, FAAFP (Kansas City)
DIRECTOR Jacob Shepherd, MD, FAAFP (Lee’s Summit)
ALTERNATE Rachel Hailey, MD, FAAFP (Lees Summit)
DISTRICT 8 DIRECTOR Andi Selby, DO, FAAFP (Branson)
ALTERNATE Barbara Miller, MD, FAAFP (Buffalo)
DISTRICT 9 DIRECTOR Douglas Crase, MD (Licking)
ALTERNATE Vacant
DISTRICT 10 DIRECTOR Gordon Jones, MD, FAAFP (Sikeston)
ALTERNATE Jenny Eichhorn, MD (Jackson)
DIRECTOR AT LARGE Stacy Jefferson, MD (St. Louis)
Krishna Syamala, MD, FAAFP (St. Louis)
Kento Sonoda, MD (St. Louis)
RESIDENT DIRECTORS
Kelly Dougherty, MD, Mercy
Noah Brown, MD, Mercy (Alternate)
STUDENT DIRECTORS
Abby Crede, UMKC
Mikala Cessac, UMC (Alternate)
AAFP DELEGATES
Peter Koopman, MD, FAAFP
Kate Lichtenberg, DO, FAAFP
Sarah Cole, DO, FAAFP Alternate Delegate
Jamie Ulbrich, MD, FAAFP Alternate Delegate
MAFP STAFF
EXECUTIVE DIRECTOR Kathy Pabst, MBA, CAE
ASSISTANT EXECUTIVE DIRECTOR Bill Plank, CAE
MEMBER COMMUNICATIONS AND ENGAGEMENT Brittany Bussey
The information contained in Missouri Family Physician is for informational purposes only. The Missouri Academy of Family Physicians assumes no liability or responsibility for any inaccurate, delayed, or incomplete information, nor for any actions taken in reliance thereon. The information contained has been provided by the individual/organization stated. The opinions expressed in each article are the opinions of its author(s) and do not necessarily reflect the opinion of MAFP. Therefore, Missouri Family Physician carries no respsonsibility for the opinion expressed thereon.
Missouri Academy of Family Physicians, 722 West High Street Jefferson City, MO 65101
Website: mo-afp.org
• p. 573.635.0830
• f. 573.635.0148
• Email: office@mo-afp.org
Family Medicine Career Transitions
My Journey from NP to MD
Transition to Family Medicine Residency: A Brief Guide for Medical Students
A Reflection on My Journey as a Family Physician
Prepare Well to Retire Well!
Why Family Medicine?
Embracing Change: How Flexibility Shaped My Career
Contracts Are Hard, but the AAFP Makes It Easy for You to Avoid Hazards
US Primary Care Scorecard Available
Voices Matter During Advocacy Day
MAFP Priority Issues and Messages
MAFP Engages with Future Family Physicians at HOSA
Family Medicine Transition Conference for Residents and Students
MAFP Regional Family Medicine Mixer
Submit a Resolution for the AAFP 2024 Congress of Delegates
MAFP Leadership Attends AAFP Multi State Forum
Another Record Match Day
Members in the News
April 25, 2024
Virtual CME Series: How Sick Are Your Patients? Reflecting Patient Disease Burden Using the HCC Risk Adjustment Model
www.mo-afp.org/cme-events/virtual-cme/
May 23, 2024
Virtual CME Series: 2024 Advocacy and Legislative Review
www.mo-afp.org/cme-events/virtual-cme/
June 20, 2024
Virtual CME Series: Supporting Breastfeeding/Chestfeeding Families in Primary Care
www.mo-afp.org/cme-events/virtual-cme/
June 21-22, 2024
Transition to Practice Conference for Residents and Students
The Oasis Hotel, Springfield
www.mo-afp.org/transition-to-practice/
July-October 2024
Additional Virtual CME dates/topics available. Visit www.mo-afp.org/cme-events/virtual-cme/ for details.
November 8-9, 2024
32nd Annual Fall Conference
Intercontinental Kansas City at the Plaza
www.mo-afp.org/cme-events/annual-fall-conference/
MARK YOUR CALENDAR
MISSOURI FAMILY PHYSICIAN
FP
CONTENTS
4 6 8 10 11 13 14 15 18 21 23 25 28 29 29 31 32 34
MO-AFP.ORG 3

Family Medicine Career Transitions
How many of us have the jobs we thought we would when we were children? Maybe you knew from an early age that you wanted to be a doctor. My dream job was always to become a doctor – but I didn’t know anything about family medicine until medical school. How about you? Did you always want to be a family physician? If so, did you think your practice would be exactly as it is now? Probably not. We all have our personal stories and have undertaken many career transitions.
I entered medical school with my sights set on being a pediatrician. It wasn’t until my family medicine rotation that I fell in love with the depth and breadth of full-scope family practice. I loved my experience at Mercy Family Medicine Residency so much that I joined the faculty as my first job after graduation. I was able to continue with the fullscope family medicine practice that I loved while passing on my knowledge to students and residents along the way.
After practicing for several years, I developed a special interest in obesity medicine and decided to pursue additional certification. For the past few
years, I have been practicing obesity medicine, but I am regularly grateful for my family medicine training and experience.
This issue captures stories from various stages of a family physician’s career. Some may resonate with your journey, while others provide messages of hope and reflection. With 73% of AAFP members as employed physicians, we included an article about 10 Red Flags for Contract Negotiations. This article includes the link to a discussion between the American Academy of Family Physicians Executive Vice President and Chief Executive Officer Shawn Martin, JD; the MAFP Board President Afsheen Patel, MD; and me with practical contracting tips.
My days are sometimes challenging, occasionally exciting, and always rewarding. I’m thankful my career has led to this point, even if it’s not exactly where 8-year-old Kara thought she would be.

Mission Statement: The Missouri Academy of Family Physicians is dedicated to optimizing the health of the patients, families and communities of Missouri by supporting family physicians in providing patient care, advocacy, education and research. Explore the Family Medicine Career Benchmark Dashboard
your-career/family-medicine-career-benchmark-dashboard/tool.mem.html 4 MISSOURI FAMILY PHYSICIAN April - June 2024
Kara Mayes, MD, FAAFP Board Chair St. Louis, MO
https://www.aafp.org/family-physician/practice-and-career/managing-
A Scoliosis Surgery with Flexibility
Helping Kids Avoid Spinal Fusion
As a leader in vertebral body tethering (VBT), we’re proud to offer an FDA-approved fusionless spine surgery that allows kids to maintain their spinal anatomy and range of motion. For kids whose idiopathic scoliosis can’t be managed with bracing, VBT offers:
• An early treatment option for scoliosis
• A less invasive, less limiting alternative to spinal fusion
• For most, a one-time surgery that naturally adjusts as kids grow
• The ability to avoid any sort of fusion in the spine



MEET THE DOCTOR
MEET THE DOCTOR
Daniel G. Hoernschemeyer, MD, is a board-certified pediatric orthopaedic specialist, chief of pediatric orthopaedic surgery and member of the Pediatric Orthopaedic Society of North America. As a pioneer in VBT procedures, Dr. Hoernschemeyer has been performing VBT surgeries for the past 10 years and is actively teaching the next generation of pediatric spine physicians.
Daniel G. Hoernschemeyer, MD, is a board-certified pediatric orthopaedic specialist, chief of pediatric orthopaedic surgery and member of the Pediatric Orthopaedic Society of North America. As a pioneer in VBT procedures, Dr. Hoernschemeyer has been performing VBT surgeries for the past 10 years and is actively teaching the next generation of pediatric spine physicians.
To learn more or to refer a patient, call (573) 884-6132 or visit muhealth.org/vbt-for-docs.
To learn more or to refer a patient, call (573) 884-6132 or visit muhealth.org/vbt-for-docs.
MO-AFP.ORG 5
My Journey from NP to MD
Jennifer Allen, MD New Freedom Family Medicine Hermann, MO
was given a gift to go to medical school, literally. I had been a Nurse Practioner (NP) for about 8 years, practicing in rural family medicine and loving every minute of it. I had always wanted to be a doctor, and in fact felt called to medicine. My journey led me to nursing instead and I had worked through my regret about not going to medical school about a year prior. In my NP role, I was about as autonomous as I could be and had great collaborative support. Dr. Shaw and Dr. Workman in Hermann were great mentors, and I will always be thankful for their part in my journey.
My journey to family medicine began in the winter 2007and we had a terrible flu season that year. We were very busy- one of those times when every call was about the flu, and we could’ve had a drive-up window for Tamiflu! One of my patients came in and wanted to talk about all kinds of things that I didn’t really have time for that day. She asked me about why I didn’t finish school. Back then, being an NP was a bit of a novelty and some people didn’t understand that it was a degree on its own, not what happened when you didn’t finish medical school. I explained to her that life got in the way and while I’d always wanted to be a doctor, being a NP was very satisfying and I was ok with it. That’s when she said, “I really want you to be a doctor. What would it take for you to go back to school to do that?” I stared at her in disbelief and kind of brushed it off. I think I said I didn’t think it would be possible. She asked me to consider it so I said I would.
After that meeting I was consumed with anxiety. I couldn’t think. I was tremulous. I had never felt like that about anything before. I remember driving home that night and calling my mom to tell her about it. My grandmother was very sick and passed away a few days after this conversation so I don’t think my mom could absorb it either. She didn’t seem to believe me, and I didn’t feel like it was real either. I spent the next several weeks trying to ignore the whole thing. Then I got a phone call from the patient’s representative. He said that she was serious, and I should put together a proposal for what it would take for me to go to medical school. I didn’t know where to start. I worked full-time; I had children to care for at home and was now divorced. I could not just drop out of society to go to medical school. And all that

anxiety was stressful until a series of random events happened that changed my path forever. I saw a friend I hadn’t seen in a long time. She was a NP and told me that she was in medical school and still working. That was an “aha” moment! I learned about Oceania University of Medicine (OUM). The mission of this medical school is to provide a medical education to people who otherwise could not get one due to geography, age, etc. They used the internet to bring people together from all over the world. They wanted to provide doctors to underserved parts of the world. They had a special interest in nurse practitioners. This seemed like a possibility, so I talked to my children and office staff. They were all supportive. My office manager grabbed me by my shoulders and said, “Why wouldn’t you do this?”
Then I met with some of my best friends and told them about the offer. I lamented that I was too old since I was going to be 38! That meant I’d graduate when I was 42 years old, not the typical age of a new doctor. My friend Trish said the words that released me, “Jen, you’re going to be 42 someday whether you are a doctor or not.” Mic drop. It seems so simple to see it now, but then it was earth shattering. It was after that I started to consider, “What if I did do this?” When I changed my perspective, the anxiety melted away and I literally felt the weight lift. I looked up and told God I was listening and would do what he was telling me to do.
I enrolled at Oceania University of Medicine in March of 2008. The program was not accredited when I started but due to the visionaries of the time and students like me, we went through the process of being fully accredited and received that distinction before I completed my program. That allowed for full Educational Commission for Foreign Medical Graduates (ECFMG) certification which is needed to practice with a full license in the US. The first 2 years of the program used the internet to allow me to be in class with other students around the world. It was quite an experience to be educated with medical students from other countries. We all had the common dream of becoming physicians and for whatever reasons could not go the traditional route. My journey had a hurdle in year 2 when I found that my new husband and I were blessed with a baby. I considered quitting my program because
I
6 MISSOURI FAMILY PHYSICIAN April - June 2024
being a physician and completing residency was going to be that much harder with a baby (at 42!). I weighed my options and realized that this whole journey was part of my original calling to medicine, and I needed to continue this path. My daughter is 13 today and tells people that she went to medical school before she was born! The second 2 years were clinical rotations that I was very fortunate to secure locally. Most medical schools have contracted relationships with teaching hospitals. They don’t allow students from other programs to rotate with them. Back then, Oceania did not have contracts with any programs (they do now) and we had to find rotations on our own. This is the rate limiting step for some people. For me it was imperative that I secured rotations as close to home as possible. But before I could get these rotations, I had to pass the USMLE step I exam.
The USMLE Step 1 exam required weeks and weeks of study. We started studying when we started school 2 years prior. It was really fascinating to see the growth in how we answered questions in the very beginning to how we answered in year 2. Huge growth happens. I cannot even begin to explain the difference in knowledge base from nursing and NP school to medical school. At Oceania since it was a program fighting for recognition and accreditation, we had to take mock exams to make sure we were ready. They wanted a perfect first take pass rate to prove that we were getting quality education. Many of us got together in the US and studied. I spent 10 days at a prep program in California with Dr. Tarman Aziz who had been faculty at OUM and started his own prep program. He is one of the greatest teachers in the fundamentals of medicine that I have ever met. I sat for my step 1 exam 8 months pregnant and then waited for my scores. The envelope came right before the baby came! My middle son offered to open it for me, but I needed to know my score and was so worried about failure. It is nearly impossible to secure a residency slot as an International Medical Graduate without passing step 1 on your first attempt. My hard work paid off and I passed.
My school administration recommended that I wait and apply for the match a year later. This would have meant no job, no school, or anything for a whole year and didn’t want to wait. My choices were already limited since we had a life here in Missouri and I couldn’t realistically do residency very far away. My choices were in St. Louis or if I had to, maybe Springfield or Columbia. Because I needed to know if I could start late, I randomly emailed Dr. Grant Hoekzema, then the director of the family medicine residency at Mercy, and just asked if that was a possibility… like “hypothetically, asking for a friend…” His response was brief. He wrote, “Being off cycle may be problematic for any program, but there is no penalty for trying.” I took this to mean, “Sure, go for it!” And so, I forged on and started the process of applying to the match.
Your school must release you to be eligible to sit for the step exams. And you must schedule the test to get the results in time for interviews for the Match. Interviews have a narrow window because you must submit your rank list for Match by February! Plus, I was scheduled for a rotation in Samoa, a requirement for my school, that lasted January 3- - March 31, 2012. So, I had to have my results back to interview before Christmas break because I would be unavailable during the entire time others were interviewing. Whew! Like so many things on this divinely inspired journey, it just worked out. I applied for 2 interviews. The day my Step 2 scores dropped was the day I got my invitations to interview. I had never been so relieved. My high Step 2 scores reflected the knowledge and experience gained from my clinical experience as a nurse and NP which added to my portfolio.
IT IS ASTOUNDING THE AMOUNT OF KNOWLEDGE I GAINED IN MY MEDICAL SCHOOL AND RESIDENCY TRAINING DESPITE BEING A NURSE AND NP FOR NEARLY 17 YEARS COMBINED
Then came the daunting task of arranging clinical rotations. I had to take a maternity leave, so I had some time to make this happen. I strategized by starting out with psychiatry. It’s a 4 week, 9-5 style rotation that I hoped would make the transition from new mom to medical student a little easier. Once again, I was blessed with a gift. A friend recommended someone for me to rotate with and because he was the head of his department, he was able to help secure the contract. This process is hard and took every minute of the 8-week maternity leave that I had to complete. The contract was between the graduate medical education department of the teaching hospital and my school which is located in Samoa - a world away. I was finally approved and started my first rotation. Every rotation is an audition in this kind of program. I had to perform exceptionally well so that I could continue. Each rotation had to be secured individually and each time a new contract had to be created. Looking back on this the stress was ridiculous, but you do what you must.
My first rotation led to my next and so on. I was extremely fortunate to secure rotations back-to-back without any gaps. I was already off cycle because of the maternity leave. Getting too far off cycle would have put me behind for the step 2 exams and applying to match. As my third year ended, I needed to start applying for residency. I projected to finish medical school in June, maybe July. Residency starts July 1 for most family medicine or internal medicine programs, so this was going to be a problem.
When Match Day came, I got the great news that I had matched. Later that week, I found out I matched at Mercy Family Medicine, my first choice. I was thrilled. For me, residency was the culmination of a dream of mine since childhood. The nostalgia, the history, the halls of medicine, the whole experience was perfect. My NP training had given me skills to communicate with people and establish rapport. It had focused on acute problems, health promotion, patient education, and disease prevention. Despite those 8 years, I quickly realized that family medicine residency was so much more. Medical practice requires a deeper, broader scope encompassing complex differential diagnoses and multiple organ systems. Ordering the correct tests, asking different questions, choosing appropriate medications while considering the context of the patient’s medical condition and history. Residency is the culmination of the thousands of hours in the classroom and clinical rotations Complete supervision by attending physicians allowed us to shape our role identity and own the responsibilities we face daily as physicians. Residency was 10,000 hours of supervised training, far more than what I had experienced in my NP program. To this day, it is astounding the amount of knowledge I gained in my medical school and residency training despite being a nurse and NP for nearly 17 years combined. In my third year, I was honored by my peers and attendings to be a Chief Resident. My experience through medical school and residency training helped me grow the courage to go on to own my own independent practice. Today, I consider being a physician an honor and a privilege and I am so thankful for my gift and all the people along the way who were a part of it.
MO-AFP.ORG 7
Transition to Family Medicine Residency: A Brief Guide for Medical Students
 Noah Brown, MD, PGY-1 Mercy Family Medicine Residency St. Louis, MO
Noah Brown, MD, PGY-1 Mercy Family Medicine Residency St. Louis, MO
First off, congratulations!
You’ve made it! You’re finally at the end of your medical school career. You’ve matched and I am sure that you are so excited for the next step in your career and your life. And, if you’re anything like me, you’re also wondering what all of this exactly entails. In this article, I hope to be able to shine some light on what the transition to residency looks like and some tips for a successful beginning to the next step in your journey in family medicine.
Finances
This topic itself could easily be discussed to exhaustion, as this is a broad topic. Here, though, I want to focus on some big points to look for as you become a resident.
You will now have an income! Yay! This is such a great feeling, but you want to make sure you have a plan with the money that you earn. With this, my first tip is to make a budget. It takes a little bit of leg work to first create your budget, but once you do get it created, it will make it so much easier to keep track of everything. Spend your money on paper first! There are also plenty of example budgets (including budgets for medical residents) that you can look at to make sure you do not miss anything. Make sure to also account for various insurances (health, disability, life, etc.) and retirement contributions in your budgeting, most of which will be new for you but all of which are
important. I also encourage you to take a look at your budget at least once a month and update it when necessary. Once you get everything initially put together, this part is pretty easy and doesn’t take too much time.
Second, do not forget about your student loans. This is not the most fun thing in the world to think about, but it is better to think about it now than when you are on the wards taking care of patients. Look through the repayment plans, use the various tools that are out there for comparing the plans to each other, and consider applying for a plan. Something else to consider are loan repayment programs, like the Public Service Loan Forgiveness (PSLF) program. If you do choose to pursue this route, there is a process you’ll have to go through to apply for PSLF before you will be able to make the qualifying payments. Of note, there are other programs out there, offered by state governments and the federal government, that do help with loan repayment.
Take Advantage of Resources
The transition from medical school to residency is certainly a unique one. You are going from working with a resident or attending to take care of patients to directly taking care of your own patients. It is truly an honor and privilege to get to do this, and, with this, there will be extra responsibilities. You will start getting refill requests for prescriptions, questions from patients on a variety of topics, and questions from colleagues about your patients, among others. Making the adjustment to learn how to manage patients at the same time you are trying to manage your inbasket/inbox can be overwhelming. It is completely normal to have questions as you adjust to these new responsibilities, so please do not be shy, embarrassed, nervous, or scared to ask questions. We have all been in the place that you will soon be. We all remember the questions that came up in our


8 MISSOURI FAMILY PHYSICIAN April - June 2024
The transition from medical school to residency is certainly a unique one. You are going from working with a resident or attending to take care of patients to directly taking care of your own patients.
minds when we were refilling medicines or answering our patients’ questions. Your upper-level co-residents and faculty are there for you, so use them as a resource.
Additionally, as you begin your journey in family medicine, there are so many people there to support you outside of your residency. Please consider being involved in our family medicine organizations. The American Academy of Family Physicians and the Missouri Academy of Family Physicians have amazing resources that are available to you as a resident. From the incredible journals that these organizations publish to their conferences where you can learn and network to the opportunity to get involved with your local, state, and federal legislators plus a number of other resources found on their websites, joining these organizations is truly worth your time. Be sure to ask your residency coordinator to see if they already pay or will pay for your membership with these organizations.
Work-Life Balance
This is an incredibly important topic. In residency, especially at the beginning as you are learning a new EMR and working on your

efficiency, it is easy to bring your work home. If you do not remember anything from this article, please remember this: it is imperative to have a separation between work and home. When it is time to go home, please go home. Try your best not to take your work home with you. If there are clinic notes to finish, they will be there the next day. Now, there are some things that will require your more immediate attention or things that do need to be done before you leave for the day, so it will be important to learn how to prioritize these things. But I encourage you to remember that, if something can be delayed and it’s 6:30 p.m. after a full day of clinic, please go home and relax.
One of the mistakes that we, as a medical community, have made, and continue to make, is that we do not take time for ourselves. We are used to sacrificing our time at home to pursue this field, as medical school is a very busy time in your life. You are trying to study for exams, finish your research projects, get the “Honors” on your rotations, all to get to this point: graduation and residency. Now, I am not advocating for you to lose that drive and passion, but it is so easy to let medicine consume our lives. I encourage you to try to find a balance. Whether that means taking a break during lunch to go on a walk before your afternoon clinic starts, going out to that new restaurant you’ve been wanting to try, or going to that St. Louis Cardinals or Kansas City Chiefs game, whatever it is that brings you joy, please don’t neglect it. Your passions outside of medicine will keep you grounded and will be one of the best things you can do to help prevent burnout.
I hope that these tips will be helpful for you as you begin your residency journey. While these are general tips, I would also encourage you to reach out to residents at the program you will be attending to get even more specifics as you transition into your program.
Congratulations again and welcome to family medicine!
MO-AFP.ORG 9
A Reflection on My Journey as a Family Physician
 Julia Flax, MD, FAAFP Chief Population Health Officer, CoxHealth Network Springfield, MO
Julia Flax, MD, FAAFP Chief Population Health Officer, CoxHealth Network Springfield, MO
Reflecting on my career as a family physician, I am compelled to acknowledge the transformative journey that has evolved over the years. The narrative of my professional life is woven with threads of challenges, perseverance, and a profound sense of purpose.
The early years of my career were a whirlwind of responsibilities – balancing the demands of a family with the rigors of my job as a family physician. Juggling patient care responsibilities, administrative duties, and the joys and challenges of life demanded an unwavering commitment. Those were years marked by tight schedules while trying to find an equilibrium between work and life responsibilities. Despite the challenges, I found fulfillment in the meaningful connections formed with patients and the knowledge I was making a positive impact on their lives.
As the years progressed, my perspective underwent a significant shift. The initial demands of a burgeoning career and family gave way to a newfound realization – the importance of giving back. Volunteering became a means to repay my community and profession that shaped my identity.
One avenue through which I found fulfillment in contributing was through active engagement with the Missouri Academy of Family Physicians. The Advocacy Commission emerged as a platform where
I could channel my passion for healthcare into meaningful action. Collaborating with state legislators, advocating for policies that enhance the quality of patient care, and being a voice for the medical community continually challenges my abilities and propels me to learn new things. Advocacy, with its intricate web of legislative complexities and policy dynamics, has become a stimulating arena where I am constantly pushed to expand my skill set. This work has compelled me to stay abreast of evolving legislative landscapes, navigate the complexities of healthcare policy, and improve my skills of persuasive argumentation. Advocacy has not only been a catalyst for professional and personal growth, but a pathway to continuous learning and a means to actively influence the landscape in which healthcare operates.
My role as a delegate to the National Conference of Constituency Leaders, representing the women constituency, has added another layer to my journey. By providing the opportunity to amplify the voices of women in the medical field, the conference provides a stage to exchange ideas, advocate for gender equality in healthcare, and contribute to a collective vision for the future of family medicine.
In conclusion, my career as a family physician has evolved from a phase of demands to one of purposeful engagement. This stage of my career is defined by a heightened sense of duty – the responsibility to give back, to advocate for positive change, and to mentor the next generation of family physicians. Volunteering and advocacy have become a significant part of my professional identity, allowing me to contribute meaningfully to the profession which has been the cornerstone of my life. As I continue this phase of life, I am filled with gratitude for the opportunities to give back, to shape the future of family medicine, and to inspire others to embrace the transformative power of their own journeys.
10 MISSOURI FAMILY PHYSICIAN April - June 2024
 Ed Kraemer, MD Kansas City, MO
Ed Kraemer, MD Kansas City, MO
happily accepted the MAFP’s recent invitation to write an article about transitioning to retirement. After all, I am in that transition process myself, so I should be a subject matter expert, right? Once I sat down to put pen to Word document, however, I began to question my qualifications for this task.
You see, I am not fully retired yet. My current “transition” stage finds me working most of the time anyway, or so it seems. (I’ve cleverly cut back to full-time work for half-time pay!) And to be honest, I’m not entirely sure what my own “postretirement” life will look like yet.
But one thing I am sure about is that every doctor is different with regard to their current work situation, sense of job satisfaction, health status, family/social/financial situation, interests, and hobbies.
For many physicians, our professional life has not only defined what we do, but, to some extent, who we are. A retirement mantra of “I don’t have anything scheduled today/tomorrow. I can do whatever I want” might sound great. But is that a successful strategy for a doctor who is accustomed to a fulfilling career with a busy schedule and multiple personal and professional interactions every day?
Here is some advice I have heard from “successful” retirees:
• Consult your financial advisor to develop a long-term plan.
• Retire when you are personally ready…not before.
• Have a transition plan to get yourself ready. (What are you retiring to?)
• Think about what will be your new purpose…your reason for getting up in the morning? What will give your retired life meaning? What brings you joy?
Some additional thoughts (and notes to self):
• Transition to retirement by cutting back on work commitments over time.
• Pick a target date. Discuss this with your family, employer, financial advisor, etc.
• Make sure that your sense of self, satisfaction, fulfilment, and purpose begin to involve other sources in addition to your work…sources that you can maintain and build upon as you retire.
• Consider continuing some aspects of “work” after retirement (paid vs. volunteer) that give you the most fulfillment with the least stress. Make these as flexible as possible to allow some spontaneity for travel, family events, etc. Some may be done remotely, such as teaching or meetings on Zoom. Choose things you are passionate about and things that feed your soul! Some ideas:
» Teaching (Medical school; Residency; PA Program; etc.)
» Community health initiatives
» Free clinic or health department
Prepare WELL to Retire Well!


I
MO-AFP.ORG 11
» Medical missions
» Consultant work (whatever that might mean for you)
» Non-medical volunteer service work
• Maintain your medical license? ABFM? CME?
• Maintain AAFP/MAFP/KCAFP membership. (Consider “Life Membership” when you turn 70 or fully retire.)
https://www.aafp.org/membership/join/life.html
• Join social groups…making new friends and maintaining longstanding relationships.
• Increase your physical activity; exercise/fitness; yoga; pickleball?
• Make healthier food choices.
• Turn interests into healthful and fulfilling hobbies.
• Move??? (But will your kids/grandkids/friends really come visit you frequently in your distant retirement utopia? Or will you find yourself moving back closer to them in a few years?)
• Maintain a sense of mindfulness and gratitude.
• Grandkids!!!
My own evolving retirement transition story:
Through the years, in addition to my “routine” family medicine group practice in Lee’s Summit, I served as a family medicine preceptor to Mizzou medical students, while also getting involved in community health initiatives and boards. Many years ago, I cut back a bit on my clinical practice schedule and increased my teaching responsibilities, including serving as a “Docent” for year 1-and-2 medical students from the UMKC School of Medicine.
About 6 years ago, I further expanded my health professions educator activities to include both med students and PA students. With my own patient panel continuing to expand at the same time, however, it became clear that “something had to give.”
After nearly 30 years as a family doctor, I elected to discontinue my patient care responsibilities except for supervising in a student-run clinic.
This was a huge career shift, but I was ready to dedicate my time to teaching and community service. As you’d expect, there is much that I miss about patient care, but I have adjusted and feel quite fulfilled with my work as a health professions educator. And somehow, it seems that my former patients have survived at approximately the same rate as when I was caring for them!
More recently, I (finally!) got around to setting my retirement target year as 2026. In that year, with a little luck, I will turn 70. Yes, I have informed those who should be aware of this. (e.g. family, employer, financial advisor). I’m guessing that I may need a reminder or nudge from them as I get closer to that target! In the meantime, I look for ways to cut back further on my work commitments, with mixed results, I admit.
My post-retirement vision includes, at least initially, some flexible volunteer work-ish activities, such as guest-teaching, and perhaps selected community service activities. These are things that I find very fulfilling and relatively low stress. I look forward to becoming a Life Member of the AAFP, MAFP, and KCAFP with only 1 final dues payment!
I also envision more time for a fitness routine, yoga, reading, photography, perhaps poetry, travel, spontaneous social interactions, and of course family. (Where’s Leo???)
And finally, a note of thanks to my wife, Mary Duryea. As with most things, she is way ahead of me on this subject. Mary has been a happily retired family physician for nearly 20 years. Among other accomplishments, she has enjoyed a second career as a yoga instructor, author, yoga therapist, and “Mimi” to our grandson, Leo.

But one thing I am sure about is that every doctor is different with regard to their current work situation, sense of job satisfaction, health status, family/social/ financial situation, interests, and hobbies.

12 MISSOURI FAMILY PHYSICIAN April - June 2024

decided to go into family medicine long before I got my acceptance letter to medical school. I worked for my own family doctor after college and quickly fell in love with his practice and his patients. There was so much variety! And also, a lot of common “family medicine things.” You know the “things” diabetes, hypertension, chronic pain, vasectomies, colposcopies, hypertension, diabetes, and “oh by the way, this chest pain” at 5 o’clock things.
It was the perfect introduction to medicine for me. It was a oneprovider practice where I had first hand exposure to every encounter with barely any of the responsibility. I roomed 20-40 patients a day as quickly as I could and hand wrote my notes in their paper charts. We had to see a lot of people because, apparently, it kept the lights on. I learned the basic skills, like how to take a blood pressure and what an A1C was. So many times, I had to help explain to people their congestion was viral and antibiotics weren’t necessary. The biggest takeaway for me, though, was that before my doctor practiced there, his dad had practiced there and their patients had all been getting care from them for over 30 years. It was a sense of community and connection that really made me excited to go to work every day. I’m forever grateful for that experience because without it, I might be working my way up the chain in a steel factory or a meat packing plant.
Heading into medical school, it was a blessing to already know I was going into family medicine. It took the pressure off the need to sift through specialties and gave me freedom to grow into the specialty I love. Medical school is hard. I remember coming home one semester of medical school for an annual checkup and I told my doctor that school was the hardest activity I had ever picked for myself to do. He just laughed and looked at my chart and said, “Well, what did you expect? Of course it’s hard.”
I’m learning now as a resident that this job just keeps getting harder, until it one day doesn’t. I haven’t quite reached that day yet,
Why Family Medicine?
Karstan Luchini, DO, PGY-1 University of Missouri - Kansas City Family Medicine Residency Kansas City, MO
but they tell me it’s coming. Reflecting on my pre-med days and time as a medical student is an odd mental exercise I have been doing recently. I remember, back then, that I only had ever imagined getting into medical school and studying for the first USMLE. It is hard to believe that I’ve now finished 3 levels of board exams and almost an entire year of residency.
If I were to change anything, I think I would have given the imposter syndrome less time to create anxiety in my brain. Being in medical school really puts a person around some of the smartest people in the world and it is very easy to let an inferiority complex sink in. If I could go back, I would have just studied a little more when I needed to and taken more time off when I had the opportunity. At the end of it all, no one remembers everything, and we all must update ourselves on the latest guidelines every two years anyway.
If I could thank anyone for getting me this far, it would be my dad. Not because my mom and my brother or the rest of the family had nothing to do with this process, but because he supported me every step of the way. Until the day he died, he reminded me to never go through the motions and to always work hard. Honestly, being born the son of a farmer, there were no shortages of manual labor or hard work. I always had to work hard. The lessons I learned from him gave me the grit and persistence I needed to make it through all the hard exams, the early morning rounds, and even teaching myself medicine in the middle of a worldwide pandemic.
I know the last part of this article doesn’t have a whole lot to do with family medicine, but I think sometimes it is important on our path to attending-hood to stop and be grateful for the things that got us here. I could go on forever listing all the reasons I love family medicine, but I feel compelled to share this message.
Take a second after reading this to call your family or your version of Dad and tell them, “Thank you. I wouldn’t be here without you.”
I
MO-AFP.ORG 13
Embracing Change: How Flexibility Shaped My Career
Sonoda,
MD, FASAM, AAHIVS Saint
Louis University Department of Family and Community Medicine
St. Louis, MO
Are you happy?”
If the answer is yes, that’s wonderful! However, if you’re feeling uncertain or unhappy, it might be time to reassess your workstyle and/or lifestyle. I firmly believe that career goals and the definition of a successful career vary for each. There isn’t a one-size-fits-all “perfect” professional role for family physicians. Rather, it is a matter of whether we are happy with what we do as a family physician. The journey begins with understanding our priorities. Once you’ve identified your priorities, explore job options aligning with your priorities and values. Remember, securing a job that makes you happy isn’t the final step since your values can change over time. Therefore, it’s crucial to regularly reassess your job satisfaction, values, and lifestyle to maintain a fulfilling (“happy”) career.
Let me share my personal career journeys from medical school to the current position. I hope that my experience will be helpful in guiding the future careers of current medical students, residents, fellows, and practicing physicians.
Medical School (Japan)
I initially aspired to be a cardiologist, drawn to the logical pathophysiology of cardiovascular conditions. However, a clinical cardiology rotation experience with a patient smoking cigarettes right before a stent placement was a turning point for me. It is certainly rewarding to save a life in the field of cardiology, but I felt that my passion didn’t align with cardiologists’ roles in practice. Instead, it highlighted the importance of patient education and preventive medicine. At that time, family medicine wasn’t a recognized specialty in Japan (established in 2018), and I had never heard of the word “family medicine” before meeting my mentor Dr. H, who had completed his family medicine residency and fellowship in Pittsburgh and became a faculty physician at our medical school. He shared his experience in Pittsburgh, which inspired me to pursue a similar path. I still vividly remember my first-time learning about family medicine

Dr. Sonoda with his mentor Dr. H.
at his office. I felt that this was exactly what I was looking for. Four years later, I got matched into my top choice in Pittsburgh (the same residency program where Dr. H was trained).
Residency
When I started my residency training, I didn’t have any particular interest in HIV infection. During my internship, there was a transformative lecture by a guest speaker, an HIV track director Dr. L, who was so inspiring and passionate about what he does. I simply felt “I would like to work with him regardless of topics” because of his impressive teaching skills and passion for HIV. I learned the power of medical education since it can change someone’s career just within an hour. Several months later, I got selected to be an HIV track resident, and I was so excited to finally work with him. However, he decided to leave the US before I started working with him. As I was already selected for the track resident, I decided to take advantage of the wonderful opportunity to learn deeply about HIV infection with a new track director who took over his position. Unexpectedly, it was one of the best decisions that I have made in my career. A new track director Dr. M was well trained both in the field of HIV and addiction medicine as a family physician. She showed me how important it is to take care of HIV and substance use disorder at the same time, as both conditions involve sensitive conversations. It inspired me to seek an addiction medicine fellowship. Fortunately, a brand-new addiction medicine fellowship was just developed, and they were looking for the first fellows during my PGY-3 year. That’s how I got into my addiction medicine fellowship.
Faculty
My current role encompasses clinical practice (primary care, addiction medicine, and HIV), medical education, and research as a faculty physician at Saint Louis University School of Medicine. Additionally, as a primary speciality advisor of our department at Saint Louis University, I am responsible for giving advice to all medical students applying to family medicine. It is my honor to help guide students in their critical career decision process.
When I introduce myself as a specialist in HIV and addiction medicine, many people may assume that I was interested in those fields at the beginning of my residency training; however, that’s not my journey as described above. I decide on my career whenever I get inspired. Currently, I do love what I do as a family physician. I will continue to assess my value and priority as time goes on.
Now, it’s your turn. Please take a moment and ask yourself.
“Are you happy?”
Kento
14 MISSOURI FAMILY PHYSICIAN April - June 2024
 Steven Furr, MD, FAAFP AAFP President
Steven Furr, MD, FAAFP AAFP President
Contracts Are Hard, but the AAFP Makes It Easy for You to Avoid HAZARDS
We know that primary care is the backbone of the U.S. health care system. This has been true for a long time, but the dynamics of the physician workforce are changing. Most family physicians 73% of AAFP members — are employed.
So, it’s never been more important that we who make up the primary care workforce stay vigilant and proactive when we enter into employment contracts.
The process of reviewing contract language and negotiating for yourself isn’t easy. But your Academy is here to help. I want to remind you of some powerful resources including a roundup of 10 red flags to watch out for as you prepare to negotiate an employment contract.

Red Flag No. 1: Subjective pre-employment conditions and requirements
Physician employment agreements often require that various conditions be satisfied before employment can begin. Conditions that are subjective could cause a delay in your start date or cancellation of the agreement entirely. Examples of subjective conditions include the employer needing to obtain approval from a board or committee or needing to review your references.
How to navigate:
• Know all the pre-employment requirements and discuss them with your lawyer.
• Find out if these conditions have delayed or canceled employment agreements in the past.
• Give yourself enough time to meet all the conditions by the required date.
• Make sure your references are reliable and timely and give references a heads up that someone will be contacting them.

Red Flag No. 2: Employment agreement takes effect upon signing and locks you into the agreement for a significant period.
If you are bound to the term of an employment agreement upon signing, you may need to comply with the agreement even though you have not started working for the employer.
For example, suppose you sign an employment agreement on Jan. 1, 2024, with a July 1, 2024, start date. Our fictional employment agreement takes effect when it is signed, and states that once you begin work, you can voluntarily exit the agreement only after working one full contract year. On March 1, 2024, you receive a better job offer and want to accept it, but you can’t because any termination before June 30, 2025, is a breach of the employment agreement.
How to navigate:
• Discuss with your lawyer when the agreement will take effect.
• Let the employer know as soon as possible if you do not intend to start employment at all or on the agreed-upon start date.

Red Flag No. 3: Contract states only a minimum number of patient hours per week and allots no time for administrative work or other tasks.
Many contracts state that the physician must devote a minimum of 40 hours to patient care not considering administrative tasks (e.g., electronic health record entry, prior authorizations, reviewing test results, referrals). A physician with a role 100% dedicated to patient care should understand how many hours in the workweek will be devoted to patient care rather than to administrative tasks.
How to navigate:
• Make sure the agreement contains enough information so that duties and schedules are clear.
• Be clear and open about your schedule expectations.
• Confirm the agreement aligns with conversations you’ve had with the employer about your schedule.

Red Flag No. 4: In an independent practice, the contract expires when you become eligible for equity, even if no equity is offered.
When future equity in a practice is an option, physician employment agreements often expire immediately when the ownership opportunity arises. If an offer is not made or is not promptly made, this approach can leave you without a written contract until ownership documents are signed. Even worse, if no equity offer is made, this can leave you without a contract or a job.
How to navigate:
• Request that the employment agreement be written to continue until it is terminated by one of the parties according to the terms of the agreement or it is replaced with a new agreement or partnership documents.
• Alternatively, ask that the offer of employment be made for a fixed period before expiration, which allows you time to negotiate the buy-in documents and sign them before the contract expires.

Red Flag No. 5: Contract allows the employer to accelerate your termination date when you give notice.
Employers sometimes write contracts that include a termination-without-cause provision, specifying that a physician providing the proper notice required under the agreement in good faith can be summarily terminated and no longer receive any compensation. Essentially, this means that if you give notice, they can terminate you immediately, ending your employment and your paycheck before you anticipated. For an example of how such a provision might be worded, download the AAFP memberexclusive resource A Family Physician Guide to Employment Contracts (https://www.aafp.org/content/dam/AAFP/documents/ practice_management/restricted/physician-contract-guide.pdf).
MO-AFP.ORG 15
How to navigate:
• Focus on your exit strategy when reviewing a new contract so you aren’t surprised when an agreement is terminated.
• Discuss revising the contract so you continue to receive compensation and benefits for the entire notice period.

Red Flag No. 6: Subjective reasons for termination, such as reputation or opinions about conduct
An agreement should ideally require your employer to give you written notice of the cause for termination (e.g., failing to satisfy requirements of the agreement, failing to complete medical records in a timely manner, failing to comply with a policy) and an opportunity to fix alleged breaches or deficiencies within a reasonable period of time.
How to navigate:
• Inquire whether such a subjective termination provision requires the employer to act reasonably and in good faith when terminating a physician.
• Download A Family Physician Guide to Employment Contracts (https://www.aafp.org/content/dam/AAFP/ documents/practice_management/restricted/physiciancontract-guide.pdf) and know the questions you should be able to answer about termination before signing any agreement.

Red Flag No. 7: Broad geographic regions in noncompete provisions
Many noncompete provisions try to restrict a physician from competing with any employer locations or anywhere a physician ever practiced while employed. The reasonableness of the geographic provision will depend on the location of the practice, the specialty, and from how far away the practice attracts its patients.
An example of an increasingly common and overly broad noncompete provision is one that would limit you from working for a new employer located within a certain radius of your previous employers’ sites even if you now practice outside the noncompete area. For example, you accept a job at Smith’s Clinic, 100 miles away from your previous employer and well outside the 50-mile noncompete radius. However, Smith’s Clinic is part of Jones Health System, which has a clinic next door to your previous employer. Some noncompete provisions are written in such a way that you can’t work at Smith’s because of the distant affiliation with a clinic in the noncompete area.
How to navigate:
• Look for contract language to be clear and specific so you understand your obligations.
• Clearly understand the exact location to which the geographic noncompete is tied.
• If the location is described as where the physician spends a certain percentage of time or effort at the time of termination, it is important to understand how time and effort will be measured. From the physician’s perspective, choose as high a percentage as possible so that the noncompete covers fewer locations.

Red Flag No. 8: Noncompete provisions that interfere with a patient’s right to select their physician
Non-solicitation provisions restrict you for a period of time from soliciting your former employer’s patients, employees, or independent contractors who may have worked for the employer. However, some contracts may also prevent you from treating any patient you saw while employed by a practice even if you
did not solicit the patient. As family physicians, we enjoy seeing patients over their lifespan and seeing multiple generations of a family. Noncompete provisions such as these can prevent us from the very relationship and care our patients rely on us for.
How to navigate:
• Work with a lawyer who can help you strongly challenge these types of provisions, which interfere with a patient’s right to select their physician.

Red Flag No. 9: Required compliance with written materials that are not provided with the contract
It is not unusual for an employment agreement to refer to outside documents. Outside documents included in the contract by reference are generally considered terms of the contract. Examples of outside documents include rules and regulations, policies, handbooks, ethical guidelines, bylaws, and similar materials. An employment agreement will often reference payer contracts; contracts between the employer, hospital, and other organization(s); and similar materials.
How to navigate:
• Obtain all copies of these outside documents. They may provide valuable information about working for the employer.

Red Flag No. 10: Verbal promises are made but are not included in the contract.
It is not unusual for an employer to reject making changes in writing and instead provide verbal reassurances. This process can be frustrating. If faced with this situation, think about your concerns and whether they are deal breakers. Signing an employment agreement with the belief that a term will be changed in the future or won’t be enforced can be a mistake. You typically cannot rely on verbal promises, emails, and side letters.
How to navigate:
• If you decide to sign the agreement with the verbal reassurances only, be sure you understand the termination provisions in the agreement and know what your exit strategy will be if these verbal, nonbinding promises are broken.
At the AAFP we always try to deliver more, so I’m going to leave you with one bonus item to consider.
Malpractice coverage: If you’re moving from one employer to another, you need to know if your new employer is going to provide tail coverage. If you have an occurrence policy — which means the policy will cover you no matter when the malpractice occurred — you will not need tail coverage. However, an occurrence policy is rare now, and most malpractice coverage is a claims-made policy. Always try to negotiate tail coverage into your employment contract; otherwise, you will be responsible. Tail coverage can be two to three times an annual malpractice premium.
My hope for every one of our members is that we find and enjoy long careers in work environments that allow us to focus on our patients and in improving the health and wellness of our communities. The AAFP has resources available that help equip us with tools to make well-informed employment decisions, and our state chapters like the Missouri AFP can guide members toward local resources. Finding the right job, negotiating the contract, and feeling good about the long-term agreement you’ve entered into can be daunting, but it’s the gateway to spending time caring for patients. The AAFP is here to help.

Contract Negotiation Conversation Video for Family Physicians
Shawn Martin, JD, AAFP EVP/CEO discusses important contract considerations with MAFP Board Chair Kara Mayes, MD, FAAFP and MAFP Board President Afsheen Patel, MD.
https://www.youtube.com/watch?v=DJDKvpAwt0w&feature=youtu.be
16 MISSOURI FAMILY PHYSICIAN April - June 2024
Agreement is effective

2
opinions about conduct
10 3
effective period SIGNING YOU IN Contract only states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK V ERBAL P R OMIS E S a r e made but N O T INCLUDED in the co n t r a c t 10 6 TERMINATION SUBJECTIVE REASONS reputation or about conduct 3 Agreement is effective for a lengthy period UPON SIGNING LOCKS YOU IN & SUBJECTIVE pre-employment conditions & requirements Contract only states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK ACCELERATE YOUR TERMINATION DATE Contract allows employer to when you give notice V ERBAL P R OMIS E S a r e made but N O T INCLUDED in the co n t r a c t 10 1 6 FOR TERMINATION SUBJECTIVE REASONS like reputation or opinions about conduct 2 CONTRACT EXPIRES In independent practice upon eligibility for equity EVEN IF N O EQUITY IS OFFERED 4 5 3 REGIONS BROAD GEOGRAPHIC in non-compete provisions 7 9 8 NOT PROVIDED REQUIRED COMPLIANCE with wri en materials that are with the contract INTERFERE WITH A PATIEN T ’S RIGHT Non-compete provisions that to select their physician AGS Employment Contract Contract only
V ERBAL P R OMIS E S e made but TERMINATION REASONS or conduct
RED F L AGS Physician Employment Contract Contract only states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK ACCELERATE YOUR TERMINATION DATE Contract allows employer to when you give notice 6 FOR TERMINATION SUBJECTIVE REASONS like reputation or
states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK
3 Agreement is effective for a lengthy period UPON SIGNING LOCKS YOU IN &
5 3 Contract only states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK V ERBAL P R OMIS E S a r e made but N O T INCLUDED in the co n t r a c t
for a lengthy period UPON SIGNING LOCKS YOU IN & RED FL AGS Physician Employment Contract SUBJECTIVE pre-employment conditions & requirements Contract only states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK ACCELERATE YOUR TERMINATION DATE Contract allows employer to when you give notice VERBAL PROMISES are made but NOT INCLUDED in the contract 10 1 6 FOR TERMINATION SUBJECTIVE REASONS like reputation or opinions about conduct 2 CONTRACT EXPIRES In independent practice upon eligibility for equity EVEN IF NO EQUITY IS OFFERED 4 5 3 REGIONS BROAD GEOGRAPHIC in non-compete provisions 7 9 8 NOT PROVIDED REQUIRED COMPLIANCE with wri en materials that are with the contract INTERFERE WITH A PATIENT’S RIGHT Non-compete provisions that to select their physician Agreement is effective for a lengthy period UPON SIGNING LOCKS YOU IN & RED FL AGS Physician Employment Contract SUBJECTIVE pre-employment conditions & requirements Contract only states per week and allots MINIMUM PATIENT HRS NO TIME FOR ADMIN WORK ACCELERATE YOUR TERMINATION DATE Contract allows employer to when you give notice VERBAL PROMISES are made but NOT INCLUDED in the contract 10 1 6 FOR TERMINATION SUBJECTIVE REASONS like reputation or opinions about conduct 2 CONTRACT EXPIRES In independent practice upon eligibility for equity EVEN IF NO EQUITY IS OFFERED 4 5 3 REGIONS BROAD GEOGRAPHIC in non-compete provisions 7 9 8 NOT PROVIDED REQUIRED COMPLIANCE with wri en materials that are with the contract INTERFERE WITH A PATIENT’S RIGHT Non-compete provisions that to select their physician MO-AFP.ORG 17









US Primary Care Scorecard Available
Identifies Demand, Workforce, and Funding Challenges
The second national Primary Care Scorecard released this spring reveals an intensifying primary care crisis and identifies five reasons why access to affordable, quality primary care services is expected to get worse.
Developed by researchers at the American Academy of Family Physicians’ Robert Graham Center and co-funded by the Milbank Memorial Fund and The Physicians Foundation, The Health of US Primary Care: 2024 Scorecard report and data dashboard examine critical measures of primary care performance nationally and across all states. Key findings include:
1. The primary care workforce is struggling to meet population demands.
• Despite a rapidly aging population with higher levels of chronic disease, the number of primary care physicians (PCPs) per person has decreased.
• The share of all clinicians practicing primary care (including nurse practitioners and physician assistants) stagnated around 28% between 2016 and 2021.
• PCPs declined from 68.4 to 67.2 per 100,000 people between 2012 and 2021.
• There has been a 36% jump in the share of U.S. children without a usual source of care over the last decade and a 21% increase among adults.
• Demand for PCPs will only increase with time. The National Institute of Health estimates that the number of people 50 or older with at least one chronic disease will increase by 99.5%, from 72 million in 2020 to 143 million by 2050.
2. The primary care sector is experiencing a workforce exodus and lacks real-world community training opportunities.
• Primary care residency does not mean primary care practice. In 2021, 37% of all physicians in training specialized in primary
care, yet only 15% of all physicians were practicing primary care three to five years after residency. The remainder subspecialized or became hospitalists who do not work in community settings.
• In 2020, only 15% of primary care residents spent a majority of their time training in community settings (outside of hospitals and academic health centers) signaling that many residents may lack adequate experience practicing in real-world clinical environments.
• In 2020, fewer than 5% of primary care residents spent the majority of their training in Teaching Health Centers or rural training tracks, two programs that historically serve disinvested communities. Research indicates physicians who train in Teaching Health Centers are more likely to practice in underserved communities.
3. The US continues to underinvest in primary care, despite diminishing supply and growing demand.
• The share of total US health care spending devoted to primary care stayed under 6% from 2012 to 2021.
• Since 2019, investment in primary care has steadily declined across all major health care payers; this decline has been most pronounced for Medicare reimbursements for primary care services and providers, which have dropped by 15%.
• The compensation gap between primary care physicians and specialists discourages residents from choosing primary care.
4. Cumbersome electronic health records burden primary care physicians.
• In 2022, more than 40% of family physicians rated the usability of their electronic health record (EHR) systems as unfavorable. Over 25% reported overall dissatisfaction with their current EHR system.
18 MISSOURI FAMILY PHYSICIAN April - June 2024
• According to the American Board of Family Medicine, 16% of family physicians reported spending four or more hours per day on EHRs, taking time away from patient care.
5. Inadequate research funding impacts primary care access and quality.
Since 2017, only 0.3% of federal research funding (administered through the National Institutes of Health, the Centers for Disease Control and Prevention, the Agency for Healthcare Research and Quality, and the U.S. Food and Drug Administration) per year has been invested in primary care research, limiting new information on primary care systems, delivery models, and quality.
A lack of adequate data on the prevalence of hybrid primary care payment (a combination of fee-for-service and per-person payments) and the training of nurse practitioners and physician assistants), for example, makes it difficult to track progress on the implementation of high-quality primary care.
“As more and more patients struggle to get appointments with primary care practices, policymakers must come together to address the primary care crisis,” said Milbank Memorial Fund President Christopher F. Koller. “By prioritizing investments in primary care and expanding our physician workforce today, we can ensure that everyone in every community has access to high-quality primary care in the future.”
Key State Scorecard Findings:
Workforce: Alaska ranks second among all states, following Idaho (38.2%), for having 36.2% of its clinician workforce in primary care overall (compared to 28.6% nationally) and first for primary care clinician density in the most disadvantaged areas, with 269 clinicians per 100,000 people (compared to 111.7 clinicians per 100,000 people nationally).
Training: North Dakota is the highest-ranked state for physician training measures, with a larger share of new doctors entering primary care (36.4%) each year than the national average (21.6%) and a high rate of physicians, physician assistants, and nurse practitioners working in primary care at 26.6%, 44.2%, and 39.4%, respectively. hgG
Investment: Oregon has the highest overall investment in primary care, with 7.7% of all health care spending going to primary care, compared to the national average (4.7%). The state also has the highest primary care spending for commercial payers (9.1%) and Medicaid (9.2%), compared to the national averages of 5.6% and 4.7% respectively.
The Scorecard was developed in response to a call for an annual tracking tool to inform primary care policy issued by the National Academies of Sciences, Engineering, and Medicine in their 2021 report, Implementing High-Quality Primary Care Rebuilding the Foundation of Health Care. This seminal report provides policy recommendations for federal and state governments, health care organizations, and payers to strengthen primary care.
“Primary care is the cornerstone of our health care system, playing a pivotal role in improving our nation’s health by delivering accessible and timely care to those in need,” said Ripley Hollister, MD, a board member of The Physicians Foundation and a practicing family physician. “The findings and recommendations from the second national Primary Care Scorecard highlight that investment in primary care is vital for the future of health care. The report implores us to embrace and advance solutions that support primary care and allow everyone to live longer, healthier lives.”
Read the Reports:
https://www.graham-center.org/content/dam/rgc/documents/ publications-reports/reports/2024-scorecard-final-report.pdf
https://www.milbank.org/primary-care-scorecard/

MISSOURI MATERNAL HEALTH ACCESS PROJECT
Same-day consultation with perinatal psychiatrist: Monday-Friday - 9:00am-4:30pm
Schedule at your convenience via phone call or online!
- Care coordination services
- Live trainings, webinars, and other educational materials on perinatal mental and behavioral health
ENROLL IN MHAP TO ACCESS...
please contact the MHAP program:
@missouri.edu https://redcap.link/Registration_Form ENROLL TODAY
For questions or more information,
musompsychiatrymh1
MHAP is a statewide perinatal psychiatry access program designed to give health care providers the resources they need to confidently identify and manage their patients’ perinatal mental and behavioral health conditions.
MO-AFP.ORG 19
FREE ONLINE CME
Prenatal exposure to alcohol and other drugs are leading cause of birth defects and neurodevelopmental abnormalities in the United States.
This course and PI-CME activities are designed to support family physicians and their team members in enhancing Screening, Brief Intervention, and Referral to Treatment (SBIRT) for prenatal alcohol and other substance use for improved patient outcomes.
PI-CME ACTIVITY:
Stage A: Assessing the current practice by gathering baseline data.
Stage B: Implementing appropriate interventions to improve SBIRT for prenatal alcohol and other substance use.
Stage C: Evaluating the impact of interventions by collecting a new set of data and comparing it to the baseline.


https://www.aafp.org/cme/all/maternity/addressing-prenatal-alcohol-and-other-substance-use.html
1 in 7 pregnant people report current alcohol use in the past 30 days.
Nearly
LEARN MORE
www.aafp.org/family-physician/patient-care/careresources/substance-use/excessive-alcohol-use.html


Alcohol SBI is relatively simple to do, and family physicians are uniquely positioned to effect significant change.
This ad is supported by the Centers for Disease Control and Prevention (CDC) of the U.S. Department of Health and Human Services (HHS) as part of a financial assistance award totaling $603,907.00 with 100 percent funded by CDC/HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement, by CDC/HHS, or the U.S. Government.
20 MISSOURI FAMILY PHYSICIAN April - June 2024

Voices Matter During Advocacy Day
On February 27 a record number of family physicians, residents, and medical students joined their voices in unison to promote and support family medicine under the dome. Over 50 members amplified our message through their meetings with senators and representatives in their offices, in the halls, and in the side chamber. Priority issues this year focused on scope of practice for nurse practitioners, safeguarding the physician and patient relationship, public health, prior authorization, and non-complete contract clauses. A complete listing of the priority issues and legislation discussed can be found on pages 23-24.
This year’s outreach event was similar to past years with a detailed legislative briefing on Monday evening. This session was held at the Courtyard Marriott and offered virtually via Zoom and covered topics about advocacy, engagement, Missouri legislation, and the MAFPPAC. Peter Koopman, MD, and Sarah Cole, DO, Advocacy Commission Co-Chairs, presented information about the role of members and impact they have on legislation. MAFP Governmental Consultants Brian Bernskoetter and Randy Scherr provided an in-depth overview of the priority legislation and MAFP’s position on each issue.
Convenient Speak Out messages were available to those who were unable to attend, but still wanted to use their voice. Sharing information about scope of practice for mid-level providers and adaptive questionnaires were just a click away to further amplify our message. The education differences, access to care, and recent studies were highlighted in the message on scope of practice. Solutions to the physician workforce shortage were offered in this email for our legislators to consider. The second message on adaptive


MO-AFP.ORG 21
health questionnaires acknowledges the advantages of technology in healthcare, but clearly states that the patient and physician relationship cannot be established through an adaptive questionnaire. These messages are customizable to include your personal story.
In addition to the priority legislation document, legislators were provided with an easy-to-read infographic on the education differences, geographic location, and increased health care costs of nurse practitioners.
I found it beneficial to hear more in-depth discussion about the issues and helping with the development of our talking points.
A hearing on SB 911 was held on Advocacy Day. This measure would preempt local laws, ordinances, orders, rules, or regulations on the sales of tobacco products, alternative nicotine products, and vapor products with state law. Ed Kraemer, MD, testified on behalf of the MAFP in opposition to this legislation. His message supported local regulations which raised the minimum age to purchase tobacco, alternative nicotine and vapor products to 21. And, the local ordinance made it illegal to sell these products to anyone under 21. MAFP opposes SB 911 because state law will supersede these local laws across the state that already in effect. However, federal law raised the age on the purchase/ sales of these products is 21, and federal law supersedes state law. We support our local municipalities and health departments in their efforts to protect their communities. We will continue to advocate for legislation to reduce the devastating health consequences that are the result of the use of tobacco products, alternative nicotine products, and vapor products.





We encourage you to contact your legislators to become a resource for them on health care legislation and issues. You can find your legislator online at https://www.senate.mo.gov/LegisLookup/Default Save the date for 2025 Advocacy Day on February 24-25 at the Courtyard Marriott, Jefferson City. Tell Lawmakers to Reject NP Scope of Practice Expansion Bills:
YOU WERE
TO
IN THIS YEAR’S EVENT, YOU CAN
PLAY
AND
QR
IF
UNABLE
PARTICIPATE
STILL
AN ACTIVE ROLE
SUBMIT YOUR SPEAK OUT MESSAGE BY SCANNING THE
CODES BELOW.
https://fammedpac.aafp.org/take-action/alertid/320/ Tell Lawmakers to Reject Adaptive Questionnaires: https://fammedpac.aafp.org/take-action/alertid/321
22 MISSOURI FAMILY PHYSICIAN April - June 2024
MAFP Priority Issues and Messages
•
•
• increased the patient’s length of stay, raised the cost of emergency department care, raised the 30
• –
•
•
•
•
not only meet today’s demand for physicians,
• MAFP supports immunizations to protect Missouri’s infants, children, adolescents, adults, and seniors.
• • •
• –
MO-AFP.ORG 23
• –
• –of “telehealth services” to include audiovisual and audio “telehealth services” may be provided.
• –
• –
• –
• –
• –
• –of “telehealth services” to include audiovisual and audio “telehealth services” may be provided.
• –
• –of “telehealth services” to include audiovisual and audio “telehealth services” may be provided.
• –
• –
• –
• –
• –
• –
• –
• –no longer than 365 days and not extend further than 50 miles from the physician’s office address.
• –
• –
• –
• –’
• –
• –no longer than 365 days and not extend further than 50 miles from the physician’s office address.
• –no longer than 365 days and not extend further than 50 miles from the physician’s office address.
• –’
• –’
24 MISSOURI FAMILY PHYSICIAN April - June 2024

MAFP Engages With Future Family Physicians at HOSA
For at least the past three years, MAFP and AAFP have supported HOSA – Future Health Professionals – at the state and national levels. HOSA is an international student organization recognized by the U.S. Department of Education and the Health Science Education (HSE) Division of ACTE. HOSA’s two-fold mission is to promote career opportunities in the health care industry and to enhance the delivery of quality health care to all people. HOSA provides a unique program of leadership development, motivation, and recognition for middle school and high school students interested in pursuing careers in health professions. HOSA is 100% health care. MAFP participated at the 2024 Missouri State Leadership Conference at Rolla High School in Rolla, MO on March 25 and 26 with 1,754 participants from 87 local chapters/schools registered – the largest registration ever.
MAFP President Elect Natalie Long, MD and Alternate Resident Board Member Noah Brown, MD served as judges of the Family Medicine Physician Competitive Event where 10 students presented about family medicine. Both Dr. Long and Dr. Brown were impressed with the level of preparation and knowledge the competitors exhibited with Dr. Brown saying, “Based on the quality of presentations and understanding of family medicine these students exhibited, we will have some great family physicians in the future!”
Following the competitive event, Drs. Long and Brown presented to 20 students in a packed classroom about the realities of family medicine and what a career as a family physician can entail. The students were attentive during the hour-long presentation and left with a deeper understanding of life as a family physician. Dr. Long said, “I was blown away with how thoughtful the students were with their questions. Several questions focused on work-life balance as a family physician and they were amazed by the depth and breadth of our work as family physicians.”

While Dr. Long and Dr. Brown were judging and presenting, MAFP Assistant Executive Director Bill Plank, CAE worked the MAFP booth in the exhibit hall. In keeping with the record-breaking trend, this year’s exhibit hall was also the largest ever although Family Physicians were the only physician specialty represented. Students appreciated a document titled “9 Signs You May Be a Future Family Physician” almost as much as the basket of Starburst candy. Many students stopped by to ask about medical school, residency, what family physicians do, how they work in the healthcare team, and other questions that indicated an interest in family medicine.
Although a date has not been set for the 2025 SLC, MAFP will have a presence again. Please reach out to us at office@mo-afp.org or call at (573) 635-0830 if interested in helping with this wonderful event in the future.

Family Physician MO-AFP.ORG 25
9 Signs You May Be a Future

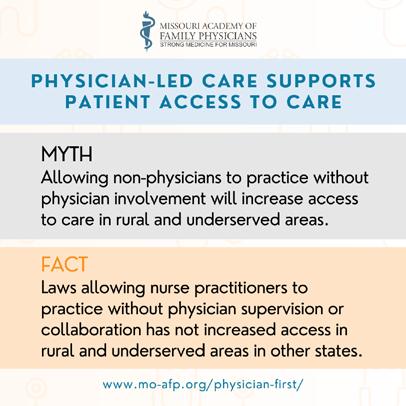
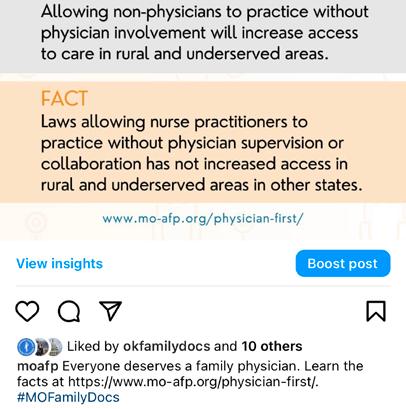




Physician-Led Care Supports Patient Access to Care Join the Campaign - Share our Posts on Social Media Connect with us on social media @moafp #MOFamilyDocs Learn more by visiting: www.mo-afp.org/physician-first/ 26 MISSOURI FAMILY PHYSICIAN April - June 2024
Join the Fight for Health Equity


Boost adult minority immunization rates with free CME.
Boost adult minority immunization rates with free CME.
Adults from racial and ethnic minorities are disproportionately affected by vaccine-preventable diseases.
Adults from racial and ethnic minorities are disproportionately affected by vaccine-preventable diseases.
Boost adult minority immunization rates with free CME.
Help us close the gap.
Boost adult minority immunization rates with free CME.
Help us close the gap.
Boost adult minority immunization rates with free CME.
Explore these free CME opportunities to encourage adult vaccinations at each patient visit:
Adults from racial and ethnic minorities are disproportionately affected by vaccine-preventable diseases.
Adults from racial and ethnic minorities are disproportionately affected by vaccine-preventable diseases.
Adults from racial and ethnic minorities are disproportionately affected by vaccine-preventable diseases.
Help us close the gap.
Explore these free CME opportunities to encourage adult vaccinations at each patient visit:
Help us close the gap.
• Updates to ACIP Pneumococcal Recommendations
Help us close the gap.
Explore these free CME opportunities to encourage adult vaccinations at each patient visit:
• Updates to ACIP Pneumococcal Recommendations
• Increasing Immunization Rates Among African American Communities
Explore these free CME opportunities to encourage adult vaccinations at each patient visit:
• Increasing Immunization Rates Among African American Communities
• Updates to ACIP Pneumococcal Recommendations
Explore these free CME opportunities to encourage adult vaccinations at each patient visit:
Become an immunization champion today.
• Updates to ACIP Pneumococcal Recommendations
• Increasing Immunization Rates Among African American Communities
Become an immunization champion today.
• Updates to ACIP Pneumococcal Recommendations
Become an immunization champion today.
• Increasing Immunization Rates Among African American Communities
• Increasing Immunization Rates Among African American Communities
Get Started: www.aafp.org/become-champion
Get Started: www.aafp.org/become-champion
Become an immunization champion today.
Get Started: www.aafp.org/become-champion
Become an immunization champion today.
Acknowledgments: The AAFP “Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations” Project is supported by a Cooperative Agreement from the Centers for Disease Control and Prevention (6 NU66IP000681-02-01) (The authors are solely responsible for the content and do not necessarily represent the official views of the CDC)
Get Started: www.aafp.org/become-champion
Get Started: www.aafp.org/become-champion
Acknowledgments: The AAFP “Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations” Project is supported by a Cooperative Agreement from the Centers for Disease Control and Prevention (6 NU66IP000681-02-01) (The authors are solely responsible for the content and do not necessarily represent the official views of the CDC)
Acknowledgments: The AAFP “Improving Adult Immunization Rates Among Racial and Ethnic Minority Populations” Project is supported by a Cooperative Agreement from the Centers for Disease Control and Prevention (6 NU66IP000681-02-01) (The authors are solely responsible for the content and do not necessarily represent the official views of the CDC)
Acknowledgments: The AAFP “Improving Adult Immunization Rates Among Racial and Ethnic Minority
MO-AFP.ORG 27
Join the Fight for Health Equity
HOPS2304243
HOPS2304243
HOPS2304243

Missouri family medicine residents and students are invited to the Missouri Academy of Family Physicians Transition to Practice Conference on June 21-22, 2024 at the Oasis Hotel in Springfield. This conference is all about learning, networking, and relaxing! Family medicine residents and medical students interested in family medicine will learn practical tools to use as they begin residency or their careers after residency. Every participant will leave the conference with resources, ideas, and best practices to become a Missouri family physician.
All MAFP resident and student members are invited to attend at no cost. Registration is supported by the Family Health Foundation of Missouri. One night’s lodging will be provided based on double occupancy.

Learn more and register by visiting https://www.mo-afp. org/transition-to-practice/
FRIDAY SCHEDULE SATURDAY SCHEDULE
Registration and Lunch
Oasis Hotel & Convention Center
2546 N Glenstone Ave, Springfield, MO 65803
Welcome, Overview and Introductions
Opening Keynote – From Family Farm to Family Medicine
Misty Todd, MD
Breakout Sessions
Students: Insights from Family Medicine Residency Directors
Lawrence M Gibbs, MD, MSEd, FAAFP
Barbara Miller, MD, FAAFP
Misty Todd, MD
Residents: Contract Negotiations to Protect You
Heather Rooney McBride, JD
Practical Finance Tips the Professionals Never Tell You
Kelly Dougherty, MD
Beyond the Clinic: Professional Development for Family Physicians
Kathy Pabst, MBA, CAE
MAFP Family Medicine Mixer at BigShots Golf
1930 E Kearney St, Springfield, MO
Sponsored by:

Breakfast
Putting the Family in Family Physician
Lauren Wilfling, DO
Charlie Rasmussen, DO
Demystifying Family Medicine Practice Settings Panel Discussion
Barbara Miller, MD, FAAFP – Rural Medicine
Charlie Rasmussen, DO – Multisite Full Spectrum Family Physician
Beth Rosemergey, DO, FAAFP – Academic Medicine
Lauren Wilfling, DO - Employed Physician
Procedures Workshop: Joint Injections and Implantable Contraception
Barbara Miller, MD, FAAFP
Mariam Akhtar, MD
Missouri Mingle Networking with Missouri Residencies and Recruiters
Wrap Up - Grab and Go Boxed Lunches
SUPPORTED BY:





and students are invited to the Missouri Academy Conference on June 21-22, 2024 at the Oasis about learning, networking, and relaxing! Family interested in family medicine will learn practical after residency. Every participant will leave practices to become a Missouri family physician. members are invited to attend at no
28 MISSOURI FAMILY PHYSICIAN April - June 2024

MAFP Regional Family Medicine Mixer

You’re invited: June 21, 2024 at BigShots Golf (1930 E Kearney St, Springfield, MO 65803) from 6:00 – 8:00 p.m. This event is held in conjunction with the Family Medicine Resident and Student Transition to Practice conference (see page 28).
Discover more about MAFP advocacy initiatives, programs, leadership opportunities, and Political Action Committee. Sign up to socialize and network with other family physicians in your community, keeping you connected with your peers. Dinner will be provided (sponsored By CoxHealth).
In lieu of a registration fee, donations to the Family Health Foundation of Missouri and/or the PAC are encouraged. Register for this event, and learn more about upcoming mixers at https://moafp.formstack.com/forms/regional_meetings_2024.
Other networking events are being scheduled for St. Louis, Kansas City and central Missouri. Watch your email for more details.
https://moafp.formstack.com/forms/regional_meetings_2024

Submit a Resolution for the AAFP 2024 Congress of Delegates

Missouri Academy of Family Physicians members are invited to make a recommendation to the MAFP Board of Directors to consider a resolution to be submitted at this year’s AAFP Congress of Delegates (COD), September 23-25, 2024 in Phoenix, AZ.
The MAFP considers many issues that are important to our members. The American Academy of Family Physicians COD meets annually to develop and set policy for the AAFP and to elect its officers and the AAFP Board of Directors.
More information about submitting a resolution can be found on our website https://www.mo-afp.org/about/congress-of-delegates/.
MO-AFP.ORG 29














30 MISSOURI FAMILY PHYSICIAN April - June 2024




MAFP Leadership Attends MultiState Forum

The annual Multi-State Forum was held in Phoenix, Arizona, February 24-25, 2024, with MAFP leadership and team attending the two-day conference. MAFP delegates this year were MAFP Board Vice President Beth Rosemergey, DO and President-Elect Natalie Long, MD. Kathy Pabst, Executive Director, and Bill Plank, Assistant Executive Director, also attended the event. State chapter staff and volunteer leaders participating in this regional event include Missouri, Arkansas, Nebraska, Iowa, Kansas, Illinois, Colorado, Texas, California, Arizona, Oklahoma, and Montana. This Forum is always an excellent opportunity for learning and networking among peers.
Kristina Diaz, MD, MBA, Arizona AFP President and AFMRD President, opened the conference on Saturday morning with a warm Arizona welcome and update about Family Medicine Residency Education. Shawn Martin, AAFP EVP/CEO provided an interactive State of the AAFP discussion with questions about AAFP and its strategic direction. Ashley Bentley, MBA, CAE, Manager, Workforce Development and Student Initiatives at AAFP provided an update on “Building the Workforce: Strengthening Pathways to Family Medicine
Careers.” Saturday afternoon consisted of an AAFP Chapter Relations update, AAFP News from AAFP Board Member Gail Guerrero-Tucker, MD, MPH, a panel discussion with Arizona legislative staffers on effective advocacy techniques, an overview of the impact of podcasts with Steve Brown, MD, FAAFP, and concluded with an ABFM Update from Gary LeRoy, MD, FAAFP.
Sunday morning provided attendees with an opportunity to discuss state legislative updates and best practices, an overview of a new AAFP Program titled Family Medicine Champions, and an overview of the California Residency Program Collaborative. Julie Harrison, Senior Manager for State Policy at AAFP, provided an update on Federal legislation with a question-and-answer session. The meeting concluded with a session from Ed Paul, MD; Bill Thrift, MD; and Jim Dearing, DO on how retiring physicians can inspire the next generation to become active in family medicine.
MO-AFP.ORG 31
Another Record
The 2024 National Residency Match Program (NRMP) had the most family medicine positions available in history marking the 15th straight year of growth in positions offered. Family medicine offered 5,231 positions, 124 more than in 2023, and 13.6% of positions offered in all specialties.
A total of 4,595 medical students and graduates matched to family medicine residency program this year. Here’s a breakdown of those matches:
• 1,535 U.S. allopathic medical school (MD) seniors
• 1,493 osteopathic medical school (DO) seniors
• 749 U.S. international medical graduates (IMGs)
• 562 foreign IMGs
• 68 previous graduates of U.S. MD-granting schools
• 44 previous graduates of DO-granting schools
The Missouri Academy of Family Physicians is excited to support medical students entering Missouri family medicine residency programs and would like to extend a warm welcome to those coming from out-of-state schools.
Congratulations to all!
Data from nrmp.org and aafp.org.
Match Day


Abby Crede (University of Missouri Kansas City School of Medicine) matched into University of Missouri Columbia Family Medicine Residency.
Andruw Wittels (University of Missouri Columbia School of Medicine) matched into University of Missouri Columbia Family Medicine Residency.
32 MISSOURI FAMILY PHYSICIAN April - June 2024



 Julia Snodgrass (University of Missouri Kansas City School of Medicine) matched into Research Family Medicine Residency.
Emily Dircks (Southern Illinois University School of Medicine) matched into University of Missouri Columbia Family Medicine Residency.
Jolene Glaude (University of Missouri Kansas City School of Medicine) matched into University of Missouri Kansas City Family Medicine Residency.
Julia Snodgrass (University of Missouri Kansas City School of Medicine) matched into Research Family Medicine Residency.
Emily Dircks (Southern Illinois University School of Medicine) matched into University of Missouri Columbia Family Medicine Residency.
Jolene Glaude (University of Missouri Kansas City School of Medicine) matched into University of Missouri Kansas City Family Medicine Residency.
MO-AFP.ORG 33
Chad Sullivan (University of Missouri Kansas City School of Medicine) matched into University of Missouri Kansas City Family Medicine Residency.
CoxHealth Joins ACLM Cohort

CoxHealth Family Medicine Residency Program was accepted into the March 2024 cohort of American College of Lifestyle Medicine (ACLM) Interest Groups. First year resident, Erica Casey, MD, will serve as the president of the group, which will provide lifestyle medicine education and activities for CoxHealth residents, along with medical students, university students, physicians, and others in the system.
UMKC Residents Receive DiRenna Foundation Scholarship
Wesley Goodrich, DO, MPH, and Ann Abbott Marin, DO, residents at UMKC’s Family Medicine Residency Program recently received the DiRenna Foundation Scholarship. This scholarship is given to osteopathic family physicians in a Missouri family medicine residency program who plan to stay and practice in Missouri. Drs. Goodrich and Marin were awarded this scholarship at the MSACOFP 2024 Winter Family Medicine Update. Congratulations to both!


Mercy Family Medicine Awarded GME Funds

Mercy Family Medicine Residency is one of the inaugural recipients of funds from the Missouri Graduate Medical Education Grant Program. The program plans to grow from six residents per class to eight per class as a result of the grant, with a renewed focus on health professions shortage areas. “We are extremely grateful to Representative Kent Haden, the Missouri legislation, and Governor Mike Parson for their commitment to improving the health of all Missourians by growing the number of physicians training in underserved geographic areas and fields of medicine,” said Sarah Cole, DO, FAAFP, Program Director. Learn more about the grant program by visiting https://health.mo.gov/living/ families/primarycare/gme/.
DO YOU HAVE NEWS TO SHARE? Email it to office@mo-afp.org for review. We love to hear from our members!
THE NEWS 34 MISSOURI FAMILY PHYSICIAN April - June 2024
MEMBERS IN
MO-AFP.ORG 35

Missouri Academy of Family Physicians 722 West High Street Jefferson City, MO 65101 32ND ANNUAL FALL CONFERENCE Save the Date NOVEMBER 8-9, 2024 Intercontinental Kansas City at the Plaza WWW.MO-AFP.ORG/CME-EVENTS/ANNUAL-FALL-CONFERENCE/ Earn up to 13.5 CME Credits Early bird pricing available Scan QR Code to learn more and register!














 Noah Brown, MD, PGY-1 Mercy Family Medicine Residency St. Louis, MO
Noah Brown, MD, PGY-1 Mercy Family Medicine Residency St. Louis, MO

 Julia Flax, MD, FAAFP Chief Population Health Officer, CoxHealth Network Springfield, MO
Julia Flax, MD, FAAFP Chief Population Health Officer, CoxHealth Network Springfield, MO
 Ed Kraemer, MD Kansas City, MO
Ed Kraemer, MD Kansas City, MO






 Steven Furr, MD, FAAFP AAFP President
Steven Furr, MD, FAAFP AAFP President


























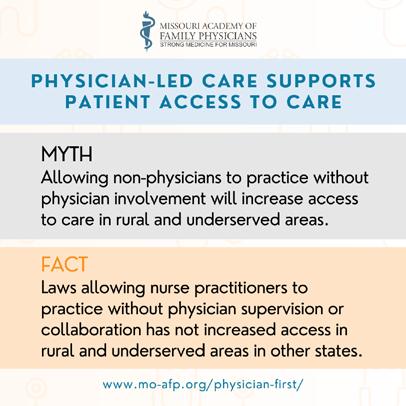
































 Julia Snodgrass (University of Missouri Kansas City School of Medicine) matched into Research Family Medicine Residency.
Emily Dircks (Southern Illinois University School of Medicine) matched into University of Missouri Columbia Family Medicine Residency.
Jolene Glaude (University of Missouri Kansas City School of Medicine) matched into University of Missouri Kansas City Family Medicine Residency.
Julia Snodgrass (University of Missouri Kansas City School of Medicine) matched into Research Family Medicine Residency.
Emily Dircks (Southern Illinois University School of Medicine) matched into University of Missouri Columbia Family Medicine Residency.
Jolene Glaude (University of Missouri Kansas City School of Medicine) matched into University of Missouri Kansas City Family Medicine Residency.




