CODE SEWAGE



Editor: William T–C Tseng, MD, MPH
Editorial Board: James Santiago Grisolia, MD; David E.J. Bazzo, MD; William T-C Tseng, MD; Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
Marketing & Production Manager: Jennifer Rohr
Art Director: Lisa Williams
Copy Editor: Adam Elder
OFFICERS
President: Preeti S. Mehta, MD
President–Elect: Maria T. Carriedo-Ceniceros, MD
Immediate Past President: Steve H. Koh, MD
Secretary: Karrar H. Ali, DO, MPH
Treasurer: Rakesh R. Patel, MD, FAAFP, MBA
GEOGRAPHIC DIRECTORS
East County #2: Rachel B. Van Hollebeke, MD
Hillcrest #1: Vikant Gulati, MD
Hillcrest #2: Stephen R. Hayden, MD (Delegation Chair)
Kearny Mesa #1: Anthony E. Magit, MD, MPH
Kearny Mesa #2: Dustin H. Wailes, MD
La Jolla #1: Toluwalase (Lase) A. Ajayi, MD
La Jolla #2: Audra R. Meadows, MD
La Jolla #3: Emily A. Nagler, MD
North County #1: Arlene J. Morales, MD (Board Representative to the Executive Committee)
North County #2: Phil E. Yphantides, MD
North County #3: Nina Chaya, MD
South Bay #1: Paul J. Manos, DO
South Bay #2: Latisa S. Carson, MD
AT–LARGE DIRECTORS
#1: Steven L.W. Chen, MD, FACS, MBA (Board Representative to the Executive Committee)
#2: Kelly C. Motadel, MD, MPH #3: Kyle P. Edmonds, MD #5: Daniel D. Klaristenfeld, MD #6: Alexander K. Quick, MD
#7: Karl E. Steinberg, MD, FAAFP #8: Alejandra Postlethwaite, MD
ADDITIONAL VOTING DIRECTORS
Young Physician: Quinne C. Sember, MD
Retired Physician: Mitsuo Tomita, MD
Medical Student: Christina Noravian
CMA OFFICERS AND TRUSTEES
Trustee: Sergio R. Flores, MD
Trustee: Timothy A. Murphy, MD
Trustee: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
AMA DELEGATES AND ALTERNATE DELEGATES
District I: Mihir Y. Parikh, MD
District I Alternate: William T–C Tseng, MD, MPH
At–Large: Kyle P. Edmonds, MD
At–Large: Sergio R. Flores, MD
At–Large: Robert E. Hertzka, MD
At–Large: Theodore M. Mazer, MD
At–Large: Albert Ray, MD
At–Large: Holly B. Yang, MD, MSHPEd, HMDC, FACP, FAAHPM
CMA DELEGATES
District I: Christopher M. Bergeron, MD, FACS
District I: Corrie D. Broudy, MD
District I: Mojgan Hosseini, MD
District I: Quinn K. Lippmann, MD
District I: Yolanda Marzan, MD
District I: Bijal V. Patel, MD
District I: Eric L. Rafla-Yuan, MD
District I: Ran Regev, MD
District I: Kristen N. Rice, MD
District I: Kosala Samarasinghe, MD
District I: Mark W. Sornson, MD
District I: Wynnshang (Wayne) C. Sun, MD
District I: Patrick A. Tellez, MD, MHSA, MPH
District I: Randy J. Young, MD
District I: Nicholas (dr. Nick) J. Yphantides, MD, MPH
RFS Delegate: Shawn A. Ali, MD
Opinions expressed by authors are their own and not necessarily those of SanDiegoPhysician or SDCMS. SanDiegoPhysicianreserves the right to edit all contributions for clarity and length as well as to reject any material submitted. Not responsible for unsolicited manuscripts. Advertising rates and information sent upon request. Acceptance of advertising in SanDiegoPhysicianin no way constitutes approval or endorsement by SDCMS of products or services advertised. SanDiegoPhysicianand SDCMS reserve the right to reject any advertising. Address all editorial communications to Editor@SDCMS.org. All advertising inquiries can be sent to DPebdani@SDCMS.org. SanDiegoPhysicianis published monthly on the first of the month. Subscription rates are $35.00 per year. For subscriptions, email Editor@SDCMS.org. [San Diego County Medical Society (SDCMS) Printed in the U.S.A.]


FEATURE
8
Code Sewage: South Bay Clinicians Confront the Tijuana River Valley Crisis By Vi Thuy Nguyen, MD, Kimberly Dickson, DO, Annie Opal Dickson, Isabella Molina, and Paula Granados, PhD
DEPARTMENTS
2
Briefly Noted: COVID-19 Vaccine • Surprise Billing • CMA Benefits
4
Summer’s Social and Mixer Was a Great Time!
13
A Medical Student Turned Physician Remembers His Mentor, Dave Bazzo By Devesh Vashishtha, MD
14
AI Is Disembodied, Wisdom Is Embodied By James Santiago Grisolia, MD
16 A Life-Changing Shunt in the Heart? By Rajeev Mohan, MD
18
The Impact of H.R. 1, the ‘One Big Beautiful Bill,’ on Healthcare By Paul Hegyi, MBA
20
Classifieds

18

Physicians Sue HHS Over Dangerous Rollback Of COVID -19 Vaccine Guidance
WHAT YOU NEED TO KNOW: A COALITION of leading medical organizations is suing HHS Secretary Robert F. Kennedy Jr. for unilaterally stripping COVID-19 vaccine recommendations for children and pregnant individuals — bypassing scientific review and undermining decades of public health safeguards. CMA strongly opposes this reckless action.

The California Medical Association is closely following a new federal lawsuit filed against U.S. Department of Health and Human Services Secretary Robert F. Kennedy Jr., who in May issued a directive ending federal recommendations for COVID-19 vaccination in healthy children and pregnant people — a move widely condemned by the medical and scientific communities.
The lawsuit, brought by the American Academy of Pediatrics and joined by several prominent public health and medical organizations, asserts that Kennedy acted unlawfully by bypassing the Centers for Disease Control and Prevention (CDC) and its independent vaccine advisory body, the Advisory Committee on Immunization Practices (ACIP). The plaintiffs argue that Kennedy’s decision disregards the established regulatory framework Congress created for making national vaccine policy, and that his directive is not supported by any new clinical evidence or public health rationale.
“The Secretarial Directive is contrary to the wealth of data and peer-reviewed studies that demonstrate the safety and efficacy of COVID vaccines for children and pregnant women,” the lawsuit states. It also notes that Kennedy’s

action puts physicians in the untenable position of contradicting the country’s top health official when counseling patients — further eroding trust in the medical system.
Kennedy announced the change in a social media video where he claimed the vaccines offered no proven benefit to healthy children or pregnant individuals — a statement contradicted by global research and the consensus of mainstream medical experts.
While the CDC did not formally remove the vaccine from its immunization schedule, it downgraded its guidance to “shared decisionmaking,” creating confusion for both providers and patients. The lawsuit argues this shift has made it harder for clinicians to provide clear recommendations and for practices to navigate insurance coverage and school-entry requirements.
CMA strongly opposes the agency’s efforts to dismantle vaccine guidance.
“Physicians rely on science to guide patient care. Undermining vaccine recommendations for children and pregnant individuals puts lives at risk,” said CMA President Shannon UdovicConstant, MD. “By removing strong federal guidance, this directive could disincentivize the production of COVID vaccines and lead to decreased vaccine access for those who wish to protect themselves and their children from COVID-19 and potential complications.”
CMA stands firmly with the physician community in defending sound, evidence-based healthcare policy..
CMA BENEFITS
Need Help Reviewing a Contract? CMA Members Get Exclusive Discounted Services
CALIFORNIA MEDICAL ASSOCIATION (CMA) members have access to two valuable member benefits that provide legal analysis of physician contracts — such as employment agreements, managed care contracts, hospital recruitment contracts, and more — at reduced rates.
SURPRISE BILLING
CMA-Backed Legislation Would Strengthen Enforcement of Surprise Billing Protections
BIPARTISAN LEGISLATION
recently introduced in Congress aims to strengthen enforcement of the No Surprises Act (NSA) by holding health plans accountable when they fail to pay physicians in accordance with final Independent Dispute Resolution (IDR) decisions.
The bill (H.R. 4710/S. 2420), introduced by Sens. Roger Marshall, MD (RKS) and Michael Bennet (D-CO), along with Reps. Greg Murphy, MD (R-NC), Kim Schrier, MD (D-WA), John Joyce, MD (R-PA), Jimmy Panetta (D-CA), Bob Onder, MD (R-MO), and Raul Ruiz, MD (D-CA), would increase penalties on plans that fail to comply with the payment timelines required under federal law.
The NSA, enacted in 2020, protects patients from surprise medical bills and created an IDR arbitration process to fairly resolve out-of-network billing disputes between insurers and physi-
cians. But despite the law’s intent, many health plans have failed to comply with final IDR decisions. A 2024 survey by the Emergency Department Practice Management Association found that 24% of emergency physicians reported IDR awards that were either unpaid or incorrectly paid beyond the 30-business-day deadline required by the NSA.
CMA has been a vocal advocate for proper implementation of the NSA, ensuring the dispute resolution process remains balanced and consistent with congressional intent. CMA also joined several successful legal challenges — led by the Texas Medical Association — against flawed federal rules that tilted the process in favor of insurers.
This new legislation marks a critical step toward meaningful enforcement of the NSA and reinforces the need to hold health plans accountable when they fail to follow the law.
Kessenick Gamma, LLP
Through CMA’s longstanding partnership with Kessenick Gamma, LLP, members receive discounted rates (typically 20–25% off) on comprehensive legal analysis of physician contracts. Services include a paragraph-by-paragraph review for legal compliance and business risk, with personalized consultations before and after the written analysis. For more information, including rates, see CMA health law library document #7076. To request a contract review, contact Frank Gamma at fgamma@ kessenick.com or (415) 362-6412.
Resolve – Physician Contract Review and Compensation Data
CMA members also receive discounted services through Resolve, a trusted provider of physician contract review and compensation benchmarking. Resolve offers physician-focused contract analysis backed by market data, to help physicians understand how their offers compare to the market — and negotiate with confidence. Call CMA’s legal help line at (800) 786-4262 to request your 10% discount code.
These trusted partners can help you evaluate and negotiate your contract with confidence.

Summer’s Social and Mixer Was a Great Time!
WE HAD ANOTHER GREAT TURNOUT AND A FUN time at our Summer Physician Social and Mixer at Stone Brewing in Liberty Station. The food and drink were delicious and the company was excellent on a beautiful summer evening.
So save the date for our fall mixer on Oct. 10, 5:30–8 p.m., at the UC San Diego Ida and Cecil Green Faculty Club. Come mingle, socialize, and network with your fellow San Diego County physicians. SDCMS members and nonmembers are welcome and encouraged to attend. RSVPs are required, please email sdcms@sdcms.org.

































BY
VI THUY NGUYEN, MD

CODE SEWAGE
South Bay Clinicians Confront the Tijuana River Valley Crisis
KIMBERLY DICKSON, DO
ANNIE OPAL DICKSON
ISABELLA MOLINA
PAULA GRANADOS, P h D
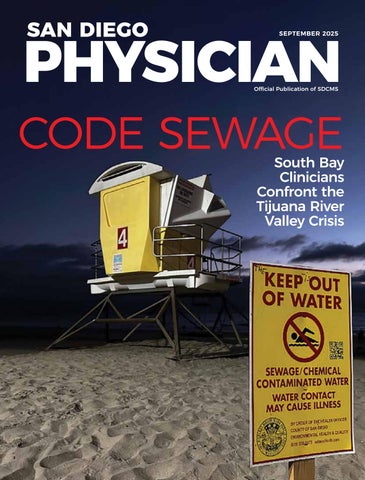
Lifeguard tower 4 in Imperial Beach.
Photo credit: Angel Granados
IMPERIAL BEACH (IB) IS A CLASSIC
Southern California town. It is an affordable, working-class surf-town rich in community and abundant with military families. It’s where our patients live, work, and raise their families. The Tijuana Watershed begins in the mountains near Mount Laguna. Water then flows into Mexico before returning to San Diego County, where it reaches the Pacific Ocean, south of IB. This watershed is the ancestral home of the southern Kumeyaay people, where indigenous communities and traditional settlements persist, and where landscape and river are considered sacred6
Today the Tijuana River has been named one of the most endangered rivers in the United States5. The watershed has been altered by the rapid growth along the border and the factories that discharge industrial pollutants. In its altered form the Tijuana River is an ecological disaster but also the source of a growing medical crisis. Annie Opal Dickson says, “As a student at Mar Vista High School, I didn’t understand what I was witnessing — the smell, the sickness, the beach closures. I thought it only affected surfers. Years later, I realize my entire community is at risk.” She suffered from severe asthma, which suddenly resolved upon moving away from the pollution during college, only to need her inhalers again when she returns home for school breaks. Isabella Molina, a second-year medical student at UC San Diego, says, “Being from Chula Vista, I saw my IB friends struggling to breathe. Their eyes turned red. Their inability to sleep soundly at night due to the stench of pollution being overwhelming. I knew the environment was out of balance.”
These personal reflections capture the frontline reality of a public health emergency unfolding in San Diego County’s South Bay. Millions of gallons a day of untreated wastewater from Mexico’s open sewer flows into the South County communities as the altered Tijuana River dumps from a concrete culvert into the valley. The river and watershed are polluted with toxic industrial waste, trash, and untreated sewage. We are now at the epicenter of an environmental and health crisis that has quietly existed for decades.
Recent data from researchers at San Diego State University and UC San Diego, coupled with firsthand reports from local clinicians9, point to an urgent need for healthcare providers to recognize and respond to the health effects of chronic environmental exposure. At South Bay Urgent Care clinic, Dr. Kimberly Dickson used to see the occasional patient who swam in the polluted ocean and developed severe diarrhea, or a Border Patrol agent with cellulitis after wading through the contaminated Tijuana River Valley3. Back then, the connection seemed straightforward: Exposure to polluted water led to illness. But now, we have come to a troubling realization: We’re treating patients who’ve had no direct contact with the river or ocean at all. Among children, Dr. Vi Nguyen noticed an uptick in asthma exacerbations and secondary bacterial infections (otitis media, sinusitis, and pneumonias) in children
from Imperial Beach and Nestor when there were reports of elevated hydrogen sulfide levels in her practice1. Their only identifiable risk factor was where they lived.
Respiratory illnesses from inhaling hydrogen sulfide fumes, persistent gastrointestinal issues, skin infections, conjunctivitis, and chronic headaches have all become alarmingly common among people who live, work, or attend school near the Tijuana River. These symptoms often intensify in tandem with the unmistakable stench of wastewater drifting across the border.
The situation has grown significantly worse since 2023, when both U.S. and Mexican wastewater treatment systems failed completely. In 2023, more than 35 billion gallons of polluted water poured across the border — making it the worst year on record11. A broken wastewater system, aging international pipes, and neglected cross-border agreements

have turned the region into what residents now describe as an “open-air sewer.” The number of pollution-related illnesses has escalated right alongside this environmental breakdown — making it clear that the health of entire communities is now being shaped not by their behavior, but by their geography.
“We’re not just treating illnesses anymore — we’re treating geography,” says Dr. Dickson. “This isn’t just about surfing. It’s about children going to school a mile from a river of sewage sludge.” During the last two years, we began experiencing personally and treating patients with sewage-related illnesses. Our front-line experience led us to meet each other during this crisis and began a marathon of organizing, trouble-shooting and trying to raise awareness. From media interviews to community health forums4 to talking to any elected official who would listen8, these last few years have
Aerial view of one of the sewage “hot spots” along the Tijuana River. Photo credit: Angel Granados
been incredibly difficult as we fought alongside thousands of community members to raise awareness on what we were seeing as part of the front-line health community.
There has finally been progress, thanks in large part to dedicated researchers, advocates, front-line clinicians, community members, and more than 50 groups that are part of the Transboundary Pollution Coalition for Advocacy and Healing4,12. We have a deep respect for the UCSD Scripps Institution of Oceanography and SDSU School of Public Health researchers who are on the front lines, collecting data in protective gear, and raising their voices when it was neither easy nor convenient. They have shown that hydrogen sulfide levels remain dangerously high in our community, and that families are suffering. Superheroes don’t always wear capes. Some superheroes wear respirators — like professors Paula Granados from SDSU and Kim Prather from UCSD and their entire team of students, researchers and volunteers.
SDSU Healthy Water Healthy Air Community Survey Results
Professor Paula Granados is sharing initial preliminary results from the SDSU Healthy Water Healthy Air Community Survey with the affected communities7 and with local medical providers so that both can be empowered. SDSU’s findings will be published in a
UCSD Scripps Institution of Oceanography research team collecting samples in the river valley.
Credit: Angel Granados

SDSU’s survey of 389 residents and workers as of July 1, 2025 in affected areas revealed the following symptom prevalence7:
peer reviewed journal shortly. The most compelling public health points from SDSU’s Tijuana River Valley community health survey findings relevant for physicians thus far are below. These data points help frame the clinical significance of this environmental crisis for our medical community.
Environmental Exposure Is a Social Determinant of Health
SDSU’s results and our experience has reaffirmed that environmental exposure is a social determinant of health. The communities most affected are Imperial Beach, San Ysidro, and South Chula Vista. The affected communities are predominantly Hispanic/Latino (53–90% in impacted areas), representing a clear environmental justice issue where historically marginalized populations bear disproportionate health burdens from infrastructure failures. Many residents are essential workers: construction crews, lifeguards, teachers, and Border Patrol agents. Twenty-two percent of affected residents report missing work due to pollution-related illness, creating cycles of health and economic vulnerability. We know now that there are geographic and occupational risk factors. The recent reports of Navy SEALs becoming ill during training exercises in Coronado underscore the severity of contamination levels and that even our healthiest San Diegans will fall ill when confronted with that much pollution8.
For Molina, as a South County resident and UCSD medical student, she reminds us that for some, “we live with this every day. We go to work in it, we drive through it, we sleep in homes that fill with toxic air at night. And the worst part is,
Photo

nobody comes to help us. It feels like we’ve been abandoned.”
Beyond the respiratory and infectious risks, the mental health impacts are also growing. SDSU’s survey found that4:
• 66% of residents experience moderate to severe psychological distress
• 27% screen positive for anxiety
• 21% screen positive for depression
“People are exhausted,” Molina adds. She also volunteered with the Centers for Disease Control and Prevention (CDC) and the County of San Diego Community Assessment for Public Health Emergency Response or CASPER, which found similar results to SDSU’s study where 66% of households reported mental health distress, with 12–14% screening positive for anxiety/depression using validated tools2. “We’re scared for our kids, we’re angry at the silence, and we’re tired of being the ones who have to prove it’s real,” she says.
Tijuana Sewage Is a Health Crisis With No Protocol
Despite the scale of the problem, most clinicians don’t receive training on how to treat environmental exposure from chronic, low-dose pollutants. There are no federal guidelines, no CDC response, and no streamlined pathway for residents to receive care.
As a result, many South Bay physicians are creating their own protocols. Drs. Dickson and Nguyen began separately searching for diagnosis codes in their different EMRs to try to follow these patients. Dr. Dickson recommends using ICD10 code Z77.1 (contact with and exposure to environmental
pollution) when appropriate. Dr. Sayone Thihalolipavan, our new county public health officer, and his team are coordinating this effort now across healthcare systems, and we are participating in the working groups to help document the sewage-associated illnesses. It is imperative that more physicians become involved in coordinating care and education efforts on the health effects of the sewage because no one entity can bear the entire burden. For Dr. Dickson, “My biggest concern as a physician is that this is becoming normalized. We can’t normalize this kind of exposure. We have to call it what it is — environmental racism, environmental injustice, failure of public policy.”
What Needs to Change
Community members, scientists, and healthcare workers are now calling for urgent reforms, including federal investment in cross-border wastewater infrastructure, health monitoring and exposure tracking for affected communities, air quality enforcement by state and federal agencies, emergency funding for schools and clinics in the exposure zone, and community-led decision making on future solutions. We need to treat this like the environmental disaster it is. That means mobilizing resources, prioritizing health, and holding governments accountable on both sides of the border.
What
Does This Mean for Local Healthcare Providers?
1
Screen patients from affected zip codes for Tijuana River wastewater exposure-related symptoms
2
Record pollution-related health complaints to build a clinical evidence base
3
Support expanded healthcare access and environmental health resources for affected communities
4
Participate with the County of San Diego Public Health Services’ working group on the Tijuana Sewage Public Health Crisis
5
Participate in the ongoing SDSU Healthy Water Healthy Air Community Health Survey. All community members over the age of 18 living or working in or near the Tijuana River region qualify. https://tjriver.sdsu.edu/our-survey/
During medical training we are taught to treat patients with respect and dignity. There are various approaches to addressing the Tijuana River sewage crisis. At the end of the day, real people and real communities are currently suffering physical and mental harm from sewage pollution. Our most urban underserved communities live by the U.S.-Mexico border. When a patient comes from that background, it is not their job to prove to us how sick they are. If a patient is directly or indirectly impacted by the sewage crisis, we as physicians don’t need statistics from elite institutions to prove to us that patients are feeling sick from their environment. If a patient presents to you with an illness and believes it is due to their polluted physical environment, treat them with the dignity and respect they deserve with their belief. The only way San Diego can heal from this pollution crisis is to recognize the difficulties we all struggle from in our never-ending changing world. We will work together toward a healthier San Diego, and as physicians we have a front-line duty to recognize and respond to presenting illnesses from our patients.
References:
1. ABC News. (2024, September 18). Asthma, pneumonia, migraines: Pediatrician raises South Bay air quality concerns. https://www.10news.com/news/south-bay/asthmapneumonia-migraines-pediatrician-raises-south-bay-airquality-concerns
2. Centers for Disease Control and Prevention (CDC), & County of San Diego. (n.d.). Tijuana River Valley & beach water sewage crisis: Community Assessment for Public Health Emergency Response (CASPER). https://www. sandiegocounty.gov/content/sdc/hhsa/programs/phs/ community_epidemiology/south-region-health-concerns/ casper-study.html
3. Coronado News. (2024, June 24). South Bay urgent care doctor questions scope of county’s review
4. Curry, T., Chairas, R., & Granados, P. (2025, March 27). Tijuana River Pollution Health Forum. Transboundary Pollution Coalition for Advocacy and Healing. http://tjriver.sdsu.edu/
5. Davidson, S., & Chairez, R. (2025, April 15). American Riv-


ers names Tijuana River among America’s most endangered rivers® of 2025 due to severe pollution and public health crisis. American Rivers. https://www.americanrivers.org/ media-item/american-rivers-names-tijuana-river-amongamericas-most-endangered-rivers-of-2025-due-to-severepollution-and-public-health-crisis/
6. Gamble, L., Wilken-Robertson, M. (2008). Kumeyaay Cultural Landscapes of Baja California’s Tijuana River Watershed. Journal of California and Great Basic Anthropology, Vol 28. No 2. pp. 127-151.
7. Granados, P., et al. (2025, Feb 13). Tijuana River Contamination from Urban Runoff and Sewage: A Public Health Crisis at the Border. San Diego State University School of Public Health White Paper, https://www.sdsu.edu/_files/tijuanasewage-contamination-public-health-crisis-white-paper-021424.pdf.
8. Inspector General. (2025, February 7). Management advisory: Naval Special Warfare Command should relocate, reschedule, or cancel Navy Sea, Air, and Land (SEAL) candidate water training when water bacteria levels exceed state safety standards. U.S. Department of Defense. https:// media.defense.gov/2025/Feb/10/2003644357/-1/-1/1/ DODIG-2025-067_REDACTED%20SECURE.PDF
9. Laws, J. (2025, July 2). Californians call on Donald Trump to declare state of emergency. Newsweek. https://www.newsweek.com/californians-call-donald-trump-declare-stateemergency-2093647
10. Oliphant, G. (Host). (2025, January 30). Tijuana River pollution: Speaking up for patient health with Dr. Dickson and Dr. Nguyen [Audio podcast episode]. In Stop & Talk Podcast Prebys Foundation. https://www.prebysfdn.org/stories/ podcast/stop-talk/tijuana-river-pollution-speaking-up-forpatient-health-with-dr-dickson-and-dr-nguyen
11. Smith, J. (2023, February 15). Tijuana sewage pours through San Diego border canyons after recent pipe break. San Diego Union-Tribune. https://www.sandiegouniontribune. com/2023/02/15/tijuana-sewage-pours-through-sandiego-border-canyons-after-recent-pipe-break/
12. Surfrider Foundation. (2024, October 13). Unite to heal our coast. https://sandiego.surfrider.org/unite-to-heal-our-coast



Dr. Nguyen is a community pediatrician practicing at Kaiser Permanente’s Otay Mesa office and serves as co-chair of the American Academy of Pediatrics’ San Diego Climate Change and Environmental Health Committee. Dr. Dickson is a family physician and mother practicing in Imperial Beach, and a physician member of the Imperial Beach Tijuana River Pollution Task Force. Annie Opal Dickson is a premedical student and lifelong resident of Imperial Beach. Isabella Molina is a medical student at UC San Diego School of Medicine, and lifelong resident of Chula Vista. Paula Stigler Granados, PhD, MPH is associate professor and environmental health division head at San Diego State University School of Public Health.

A Medical Student Turned Physician Remembers His Mentor, Dave Bazzo
By Devesh Vashishtha, MD
Editor’s Note: The passing of former SDCMS President David Bazzo has produced a strong reaction from many. He touched a large number of lives in different ways — as a physician, educator, medical community leader, sports doctor, and wellness advocate. We have been asked to share this tribute from a medical student, now physician, who Dave mentored.
EIGHT YEARS AGO, AS A FOURTHyear medical student, I had the privilege to attend the California Academy of Family Physicians’ annual Sacramento advocacy meeting. I was a proud junior member of our ever-robust San Diego delegation, which included stalwarts like Dr. Anthony Chong, Dr. Kristin Brownell, and of course the inimitable Dr. Dave Bazzo. At the time, Dave was serving as president of the San Diego County Medical Society.
I first met Dave through my thirdyear primary care clerkship at UC San Diego, during which he gave me a passing grade for having missed the mandatory clerkship orientation. I was disappointed by this outcome because I wanted to go into family medicine and get honors. But Dave would not budge on his decision. Dave was a person of principle: You do things the right way, and success will come.
Soon after this clerkship, I committed fully to family medicine and Dave became one of my closest mentors. We booked flights to Sacramento together
and I was happy to be seated on the plane next to Dave and his wife, Sabrina.
After de-boarding the plane in Sacramento, Dave and I were walking together when we heard a call overhead: “Medical emergency on plane docked at gate 16. Any available doctor requested for help.” Without hesitating, we quickly walked over to the plane. In the far back row on the right, there was a man in his thirties who was sweating and confused. Dave quickly triaged the situation, ensured the man was stable, and waited with him until paramedics arrived.
Although I was just standing next to Dave as he provided medical assistance, the Southwest crew was enormously grateful to both of us. I remember how delighted Dave was, grinning ear to ear, after the crew presented us each with a flight voucher. Dave was a man who enjoyed the blessings in his life.
The next several years passed by in a blur as I moved to Seattle to complete family medicine residency, and my wife and I were blessed with a son and daughter. I kept the advocacy work alive through involvement in the WAFP and AAFP, and Dave continued as president of CAFP and as chair of the UCSD Department of Family Medicine, supporting hundreds of physicians, residents, and
medical students. Dave somehow managed to keep in touch, wishing me happy birthday on Facebook every year that I was in residency, even though I never responded. As I wrapped up my PGY-3 year in Washington, a pivotal phone call with Dave reminded me of the welcoming community I had in San Diego.
Soon after I moved back to San Diego in 2021 and started work as a family physician at an FQHC, Dave was diagnosed with brain cancer. He went on hospice right as I joined an annual advocacy meeting in Sacramento in March of 2025.
During the meeting, I thought about Dave many times. I thought he would be proud of family physicians calling for investing 15% of all healthcare dollars on primary care. If Dave was there, he would be regaling us with stories of his prior trips to Sacramento, remembering his favorite places to visit, and perhaps making off-color remarks about last names of legislators.
After wrapping up the advocacy meeting and reaching the Sacramento airport early, I was waiting for my flight when I saw an elderly woman lying flat on her stomach in the middle of the terminal, surrounded by Southwest crew members. She was an 87-year-old who had fallen. She had a bloody nose and a large bleeding gash on her forehead.
In a few moments, with the help of some gloves and plenty of tissues, I helped her sit up, worked with another physician to stop the nosebleed, and controlled the bleeding from her forehead laceration. Unlike my last in-flight emergency with Dave, I was in charge and I moved fast and confidently, relying on my seven years of experience as a family physician. After the paramedics came and took over, I was rewarded with a Southwest voucher.
I chuckled inside and walked over to find a snack, thinking about Dave the whole time. I am sure he would have been thrilled.
Advisory Committee and the CAFP Legislative Affairs Committee.
Dr. Vashishtha is a family physician living in Rancho Peñasquitos. He serves on San Diego County’s Behavioral Health Advisory Board, as well as on a Medi-Cal

AI Is Disembodied, Wisdom Is Embodied
By James Santiago Grisolia, MD
WRITING ON AI IN MEDICINE IN our May issue, Dr. William Tseng, our editor-in-chief, issued “an invitation to reimagine the cognitive landscape of medicine.” Many physicians fear that AI will replace us, and in fact, the startup Mechanize in San Francisco aims to fully replace physicians and multiple other jobs “as fast as possible” per The New York Times. However, if we follow Will’s call to “lead with both innovation and heart,” AI will only enhance our work as doctors.
Patients come to us for personalized assessment and diagnosis. AI can collect data across the internet or other large databases, but data is not wisdom. Data does not become wisdom until it’s brought into context: the patient’s own idiosyncrasies and preferences, what the insurance will cover, what’s practical and desirable for that particular patient. Our job remains the same: bringing objective data into the personal context of this body, this patient, this family. Only now, we’ll also weed out AI hallucina-
tions and other miscues that won’t be obvious to the patient. For years, we’ve been contextualizing and correcting misinformation that patients read and misunderstand on the internet, so we have the skillset baked in to deal with AI misinformation, and AI tools can help with note-writing, prior authorizations, and thinking of the odd diagnosis that we forgot to consider.
Our personal presence remains critical. The pandemic taught us that telehealth falls somewhere between emailing and the in-office visit; we all know the increased engagement that flows from sitting together, engaging, picking up nonverbal cues, and interactions between patient and family. These nuances guide us, often in a different direction than our initial plan.
Recently, I stumbled on this quote from Sigmund Freud’s On Psycho -
therapy: “It is no modern talk but a dictum of old physicians that these diseases are not cured by the drug, but by the doctor, by the personality of the physician in so far as it exerts a psychic influence.” Besides guiding our diagnosis, our presence with the patient has a healing effect, sometimes much more than the treatment we recommend. And compliance with the treatment rests on the doctorpatient relationship. We must inspire confidence, address their objections, listen to the family’s concerns, and meet them. AI offers a deceptive air of objectivity, but for many patients, human-to-human contact must “close the deal” to get compliance, just like any salesperson.
And touch is important, the ancient “laying on of hands.” When I was a preteen, I once went with my father to visit a family friend in the hospital. Dad got his MD in Spain, but went directly into biochemistry research as soon as he finished his internship. Yet I noticed when he spoke to this friend in the hospital, he made a point of holding his hand and touching his shoulder. Later he explained to me that touch is a critical foundation of our role as physicians. I was amazed that my dad had absorbed this so deep in his bones that the lesson survived decades of work in the biochemistry lab. We will do well to remember and celebrate this same lesson, employing AI as another useful tool to help us approach the mystery of each body’s wisdom.
Dr. Grisolia is a neurologist, former editor of San Diego Physician magazine, and former chief of staff at Scripps Mercy Hospital.

Dialectical Behavior Therapy at Sharp Mesa Vista Hospital
If someone is struggling with emotional dysregulation, dialectical behavior therapy (DBT) can help. Sharp Mesa Vista Hospital’s DBT Informed Skills Intensive Outpatient Program teaches patients the coping skills they need to better manage severe emotional reactions, intense anxiety, impulsivity, self-harm, suicidal thoughts and highconflict relationships. DBT is one of the evidence-based therapy modalities provided by Sharp Mesa Vista in an intensive outpatient setting.
“Many patients turn to our program for assistance with symptoms such as self-harm, impulsivity and challenges in managing anger. They often face frequent interpersonal issues as well,” says Dr. Claire Clark, a licensed clinical psychologist at Sharp Mesa Vista.
Dr. Clark explains that the program is tailored to treat patients challenged by emotional dysregulation, including people with a diagnosis of borderline personality disorder, PTSD or bipolar disorder. Symptoms of these conditions can include suicidal ideation and intense feelings of shame or guilt.
“Relationships can often act as a significant trigger for patients. Our program aids patients in adjusting their emotional baseline to better manage their thoughts and feelings,” says Dr. Clark.
The clinicians in the program — including psychologists, nurses and therapists — guide patients through the four modules of DBT:
• Mindfulness — practicing being in the present by noticing thought processes and emotions without judgment
• Distress tolerance — understanding thoughts and feelings and replacing harmful behaviors with healthy coping mechanisms
• Emotional regulation — describing thought processes and emotions and being more in control of feelings
• Interpersonal effectiveness — properly communicating desires and needs to other people and practicing assertiveness

Practicing acceptance is fundamental to the program, enabling patients to gradually incorporate healthy behavioral changes.
“As clinicians, when we assist patients in accepting and validating their feelings through DBT, it helps them release shame and self-hatred,” says Dr. Clark. “This process can ultimately rebuild and strengthen relationships, including the relationship patients have with themselves.”
The program spans eight weeks, with patients engaging in both group and individual therapy during the first five weeks. Throughout the program, each patient collaborates with a psychiatrist on medication management. Additionally, family therapy is available for people who wish to participate.
The DBT Informed Skills Intensive Outpatient Program stands out due to its combination of group and individual therapy, along with medication management. Additionally, the diverse team of clinicians at Sharp Mesa Vista provides extensive knowledge and expertise in treating a range of mental health conditions.
“We’ve discovered that many patients can relate to each other in group therapy within our program, even if they haven’t faced the exact same relationship challenges,” says Dr. Clark. “Group therapy offers a safe space for patients to practice the skills we aim to impart to them.”
Dr. Clark notes that the program accommodates adults of all ages, who gain from sharing and learning from one another’s experiences.
“I feel immense gratification witnessing patients heal, feel empowered by our program, and enhance the quality of their relationships,” says Dr. Clark.
If you or a colleague are aware of a patient who can benefit from this program or other services provided by Sharp Mesa Vista, you can make a referral by calling 858-836-8434 or visiting sharp.com/mesavista
A Life-Changing Shunt in the Heart?
Scripps La Jolla Hosts Landmark Clinical Trial of Novel Heart Failure Treatment
By Rajeev Mohan, MD

FOR ALL THE LIFESAVING PROGRESS
cardiology has made over the decades, with dramatically increased survival rates for coronary heart disease and acute heart attacks, there’s one area where we’ve lost ground.
Heart failure. The mortality rate is higher now than it was 25 years ago.
That’s because of the nearly seven million Americans who have heart failure — a number projected to top 10 million by 2040 as obesity and diabetes rates soar — more than half suffer from an intractable form called heart failure with preserved ejection fraction (HFpEF).
HFpEF patients breathe normally at rest but become immediately breathless with any physical activity, even just rising from a chair or walking. Diagnosis can be challenging because the signature symptom, shortness of breath, has so many other possible causes.
HFpEF has stubbornly resisted cardiology’s best efforts at treatment. Patients with HFpEF, 60% of whom are women, have high pressure in the left
ventricle and left atrium of the heart, which cannot adequately fill during exertion. Drug therapies have little effect, and patients face frequent hospitalizations and a steadily deteriorating quality of life.
Now, however, there’s a “hole” new treatment option under study: creating a permanent opening in the heart wall to balance the pressure. Scripps Clinic La Jolla is one of about 65 sites worldwide currently participating in RESPONDER-HF, a confirmatory, randomized clinical trial of the Corvia Atrial Shunt.
The shunt is an elegantly simple device implanted between the left and right atria. When physical exertion increases the left atrial pressure, blood
flows through the device into the right atrium, relieving the pressure and allowing the patient to breathe easier.
In prior studies going back more than 10 years, nearly 700 atrial shunts have been safely implanted, identifying a specific subset of HFpEF patients who respond really well –- those without latent pulmonary vascular disease and without an implanted pacemaker or defibrillator.
One such patient is Amy Vasquez, now 63, a senior solutions architect from San Marcos who was diagnosed with heart failure in 2016 after she suddenly found she couldn’t walk her dogs around her neighborhood without gasping for air. In 2020, she received the device as part of a clinical trial and improved so quickly that shortly thereafter she was swimming with dolphins in Mexico. Today, she continues to thrive and works full-time.
To most cardiologists, an opening in the heart wall is something to be repaired, and deliberately creating one is counterintuitive. But the evidence is growing that for HFpEF patients like Amy who fit the responder profile, this device can have a significant impact.
Most family physicians have heart-failure patients who have been to the emergency room many times, people whose treatment options are exhausted and whose prognosis is grim. For them, this trial could prove to be to be a window of opportunity to a better quality of life.
The Corvia® Atrial Shunt is an investigational device and is limited by U.S. law to investigational use. For more information, visit clinicaltrials.gov (NCT05425459). Physician referral and enrollment details can be found at https://
Dr. Mohan, a board-certified cardiologist at Scripps Clinic La Jolla specializing in advanced heart failure and trans plant cardiology, serves as the principal investigator for the RESPONDER-HF trial at Scripps. The study has been approved by the local Institutional Review Board (IRB).













The Impact of H.R. 1, the ‘One Big Beautiful Bill,’ on Healthcare
By Paul Hegyi, MBA
DESPITE MILLIONS OF TEXT messages sent by healthcare providers across the nation, tens of thousands of calls and emails to members of Congress, and pleas from Democrats and Republicans alike to stop Medicaid cuts, the U.S. House of Representatives took action in July that will decimate care for millions across the country.
House Resolution 1 (H.R. 1), the “One Big Beautiful Bill,” cuts Medicaid (Medi-Cal here in California) and the Affordable Care Act (ACA) by $1.2 trillion over the next 10 years. Direct impacts are difficult to quantify as many of the changes are scheduled to take effect in 2027 or are otherwise awaiting implementation rules from the various agencies that oversee the impacted programs.
Initially, ACA premium tax credits are set to expire this year. Therefore, the Congressional Budget Office (CBO) estimates that five million ACA recipients nationwide will lose affordable coverage and nearly two million in California will either lose coverage or have to pay 66% higher premiums. CMA urged Congress to extend the expiring tax credits as 24 million Americans are covered by ACA marketplaces and Covered California. New requirements for ACA coverage include pre-enrollment verification of eligibility, will end auto-renewals, restrict subsidized ACA coverage eligibility for certain immigrants, and will bar individuals who enroll during a special enrollment period from receiving tax credits or cost-sharing assistance. The legislation establishes new mini-
mums for either work requirements, mandated engagement in education programs, or community service activities totaling 80 hours per month for certain able-bodied Medicaid recipients ages 19–64 — mostly adults on the ACA Medicaid Expansion program. There are exceptions for pregnant women, parents/guardians of dependent children under age 14, foster youth under age 26, disabled veterans, the medically frail, the disabled on SSI, seniors, and others. States must have programs in place effective Dec. 31, 2026.
CBO estimates that the onerous paperwork required to provide employment verification will result in more than 4.8 million otherwise eligible adults losing coverage (1.4 million in California).
One victory achieved during the development of H.R. 1 was the guarantee of Medicaid was protected for the traditional populations of children, pregnant women, the disabled, seniors, and veterans who will not lose coverage but could lose services and access to care.
Further, uncompensated care costs are estimated to increase by $42 billion — $9.5 billion in California.
Changes to provider tax threatens Prop 35 and other existing funding sources. The new law requires provider taxes to be uniform among all taxed entities within each category of provider taxes (hospital, nursing home, managed care organization, or intermediate care facility). States may be given a transition period of up to three years from enactment, but this is at the discretion of the HHS Secretary.
The Prop 35 MCO provider tax and California’s hospital quality assurance fee (HQAF) received waivers from HHS
for meeting the uniformity criteria that requires all taxed entities — hospitals, nursing homes, managed care organizations, and others — to be taxed equally. California’s MCO tax and hospital QAF will need to change to meet this new uniformity requirement. For instance, under the MCO tax, all Medicaid and non-Medicaid managed care plans in CA would need to be taxed at the same rate. The current MCO tax has waiver approval through Dec 2026 but it could be threatened by the legislation.
The legislation also creates barriers for students to pursue careers in medicine, further exacerbating physician workforce shortages. For new loans after July 1, 2026, the final bill imposes a cap on federal student loan borrowing for medical school up to a $200,000 lifetime cap in addition to a $50,000 undergraduate borrowing cap. Federal graduate PLUS loans are eliminated for new borrowers starting
in the 2026–2027 academic year and for existing borrowers for the 2029–2030 academic year.
In total, 217,000 California healthcare jobs are expected to be lost due to these changes, totaling $37 billion in reduced economic output.
While the combined changes made by H.R. 1 will be devastating to healthcare, there were modest bright spots. Medicare physician payments receive a 2.5% increase for 2026. Given the massive Medicaid and ACA funding cuts in the bill, this is an important investment in Medicare physician funding and a higher rate in 2026. We plan to continue advocating for a long-term overhaul to Medicare that includes annual inflation-based updates.
Paul Hegyi is the CEO of the San Diego County Medical Society.

Patients Lose Health Coverage
They become uninsured, delay care and get sick.

Emergency Departments Get More Crowded
Hospital emergency departments and physicians are required by federal law to provide care to uninsured patients.

Patients Are Forced Into Debt
When patients can’t cover their medical bills, hospitals and physicians are forced to pick up the cost.

Commercial Insurance Rates Soar
To cover the cost of providing emergency care to uninsured patients, providers are forced to raise rates on private insurance.

Hospitals and Physician Offices Close
Hospitals can’t take on the increased financial burden and are forced to close along with surrounding physician practices and nursing homes, and the community’s health care workforce is let go.

The Local Economy Falters and People Lose Jobs
Health care providers are often the largest employers in a community. Without this workforce and customer base, local businesses suffer.

States Cannot Absorb Cuts
States will reduce Medicaid coverage and benefits, cut funding from other programs and/or raise taxes.
CLASSIFIEDS
PRACTICE ANNOUNCEMENTS
CRANIO/MAXILLOFACIAL AND HEAD & NECK
SURGERY: Accepting new adolescent and adult patients seeking evaluation and management of head and neck masses, multidisciplinary assessment of oral/facial cancers and reconstruction, nasal airway assessment and functional rhinoplasty, corrective jaw surgery including jaw advancement for obstructive sleep apnea, cleft and craniofacial reconstruction, maxillofacial fracture management and secondary facial and jaw reconstruction. We work with Medicare, Tricare, most PPO insurance plans, and some HMO plans. Referrals may be called in to (619) 452-7332, or emailed to jaw@scrippshealth.org. [2887-0808]
VIRTUAL SPEECH THERAPY AVAILABLE: Accepting new pediatrics and adult patients. We accept FSA/ HSA, Private pay, Medicare, Medi-Cal, and several commercial insurance plans pending credentialing. Visit virtualspeechtherapyllc.org or call (888) 855-1309.
PSYCHIATRIST AVAILABLE: Accepting new patients for medication management, crisis visits, ADHD, cognitive testing, and psychotherapy. Out of network physician servicing La Jolla & San Diego. Visit hylermed.com or call (619) 707-1554.
PHYSICIAN OPPORTUNITIES
UCSD DEPARTMENT OF FAMILY MEDICINE | FACULTY POSITIONS AVAILABLE: UCSD Department of Family Medicine seeks motivated faculty to join our team in clinical, teaching, and scholarly roles. Faculty participate in comprehensive patient care, resident and fellow education, and research or quality improvement initiatives. We welcome candidates with diverse experiences and a passion for family medicine, community engagement, and academic medicine. Opportunities are available at various academic ranks, with salary commensurate with experience, rank, and step. Join a collaborative, supportive environment committed to excellence in primary care and education. Apply here: https://apol-recruit.ucsd.edu/ JPF04341. [2889-0822]
OB/GYN PHYSICIAN | PHMG ESCONDIDO: Palomar Health Medical Group is seeking a full-time, board-certified/eligible Obstetrics and Gynecology Physician to deliver comprehensive reproductive care, including labor and delivery management, gynecologic surgeries, and OB call rotations. The ideal candidate will possess strong surgical skills, California licensure, and a commitment to maternal health. We offer competitive compensation, performance-based incentives, and a collaborative team environment. Please email CV to clayton.trosclair@palomarhealth.org or phil. yphantides@phmg.org. [2882-0626]
FAMILY MEDICINE/INTERNAL MEDICINE PHYSICIAN | PHMG RANCHO PENASQUITOS: Palomar Health Medical Group is seeking a Family Medicine or Internal Medicine Physician (MD/DO) to join our multispecialty practice at our Rancho Penasquitos clinic location. Experienced physicians and new graduates are encouraged to apply. Clinic schedule is Mon-Fri, outpatient only, no weekends or holidays. We offer competitive salary of $300k/year or more depending on experience. In addition, we offer productivity and other bonuses, PTO, CME reimbursement, health, dental, vision insurance, participation in 401K with partial employer match, short and long-term disability, and life insurance. Student loan repayment assistance is also available. Join Palomar Health Medical Group, where we’re reimagining healthcare with compassion, excellence, and integrity. Please email CV to clayton. trosclair@palomarhealth.org or phil.yphantides@ phmg.org. [2881-0626]
FAMILY PRACTICE | INTERNAL MEDICINE
PHYSICIAN: La Jolla Village Family Medical Group is seeking a PT/FT primary care physician to join our well-established private practice. We’ve been caring for our La Jolla/UTC area neighbors for 35+ years
providing comprehensive, longitudinal care to patients of all ages. Call responsibilities are minor; hours consistent with a healthy work/life balance. Our office is new, clean, modern, and well-appointed. Our clinical team is collegial, passionate, and close-knit, with a supportive, cohesive support staff. A true private practice where physicians practice artfully and build enduring relationships with patients and colleagues. Seeking a Board-certified, California-licensed MD/ DO physician, passionate about medicine and looking to establish roots in a practice dedicated to the art of good medicine. Competitive salary and excellent benefits including medical, dental, vision, and retirement. Send a cover letter and CV to jcataluna@lajollafamilymedical.com. [2880-0520]
CLINICAL DIRECTOR | BEHAVIORAL HEALTH
SCIENCES | COUNTY OF SAN DIEGO: The County of San Diego is seeking a dynamic physician with a passion for building healthy communities. This is an exceptional opportunity for a California licensed, Board-certified Physician to help transform the local behavioral health continuum of care and lead important work within the Health and Human Services Agency’s Behavioral Health Services department. Visit governmentjobs.com to view a detailed brochure outlining the duties and responsibilities of the position and file your application. Anticipated Hiring Range: $310,000 to $320,000 annually. In addition to the base salary, the incumbent may receive a 10 % premium for Board Certification or a 15 % premium for Board Certification and Sub–specialty. [2877-0225]
VENOUS DISEASE SPECIALIST | NORTH COUNTY: La Jolla Vein & Vascular, the premier vein care provider in San Diego, is seeking a highly skilled and experienced Venous Disease Specialist to join our team at our newest location in Vista, CA, nestled in the stunning coastal region of North County San Diego. This full-time position offers competitive salary and benefits, including profit-sharing and a 401(k). Our state-of-the-art facility operates Monday through Friday, with no weekend or night shifts, promoting an excellent work-life balance. Ideal candidates may also consider a locum or locum-to-hire arrangement. Join us in making a difference in our patients’ lives while enjoying your dream location! Email cv to jobs@ ljvascular.com. [2875-1030]
PART–TIME PRIMARY CARE PHYSICIAN: Primary Care Clinic in San Diego searching for part-time physician for 1 to 2 days a week, no afterhours calls. Please send CV to medclinic1@yahoo.com. [2872-0909]
OB/GYN POSITION AVAILABE | EL CENTRO: A successful Private OBGYN practice in El Centro, CA seeking a board eligible/ certified OB/GYN. Competitive salary and benefits package is available with a tract of partnership. J-1 Visa applicants are welcome. Send CV to feminacareo@gmail.com or call Katia M. at (760) 352-4103 for more information. [2865-0809]
COUNTY OF SAN DIEGO PROBATION DEPT.
MEDICAL DIRECTOR: The County of San Diego is seeking dynamic physician leaders with a passion for building healthy communities. This is an exceptional opportunity for a California licensed, Board-certified, physician to help transform our continuum of care and lead essential medical initiatives within the County’s Probation Department. Anticipated Hiring Range: Depends on Qualifications Full Salary Range: $181,417.60 - $297,960.00 annually. As part of the Probation Administrative team, the Medical Director is responsible for the clinical oversight and leadership of daily operations amongst Probation facilities’ correctional healthcare programs and services. As the Medical Director, you will have significant responsibilities for formulating and implementing medical policies, protocols, and procedures for the Probation Department.
PART–TIME CARDIOLOGIST POSITION AVAILABLE: Cardiology office in San Marcos seeking part–time cardiologist. Please send resume to Dr. Keith Brady at uabresearchdoc@yahoo.com. [2873-0713]
INTERNAL MEDICINE PHYSICIAN: Federally Qualified Health Center located in San Diego County has an opening for an Internal Medicine Physician. This position reports to the chief medical officer and provides the full scope of primary care services, including diagnosis, treatment, and coordination of care to its patients. The candidate should be board eligible and working toward certification in Internal Medicine. Competitive base salary, CME education, Four weeks paid vacation, year one, 401K plan, No evenings and weekends, Monday through Friday 8:00am to 5:00pm. For more information or to apply, please contact Dr. Keith Brady at: uabresearchdoc@yahoo.com. [28740713]
FAMILY MEDICINE/INTERNAL MEDICINE
PHYSICIAN: San Diego Family Care is seeking a Family Medicine/Internal Medicine Physician (MD/ DO) at its Linda Vista location to provide outpatient care for acute and chronic conditions to a diverse adult population. San Diego Family Care is a federally qualified, culturally competent and affordable health center in San Diego, CA. Job duties include providing complete, high quality primary care and participating in supporting quality assurance programs. Benefits include flexible schedules, no call requirements, a robust benefits package, and competitive salary. If interested, please email CV to sdfcinfo@sdfamilycare.org or call us at (858) 810-8700.
PHYSICIAN POSITIONS WANTED
PART–TIME CARDIOLOGIST AVAILABLE: Dr. Durgadas Narla, MD, FACC is a noninvasive cardiologist looking to work 1-2 days/week or cover an office during vacation coverage in the metro San Diego area. He retired from private practice in Michigan in 2016 and has worked in a San Marcos cardiologist office for the last 5 years, through March 2023. Board certified in cardiology and internal medicine. Active CA license with DEA, ACLS, and BCLS certification. If interested, please call (586) 206-0988 or email dasnarla@gmail.com.
OFFICE SPACE / REAL ESTATE
AVAILABLE
AVAILABILITY OF UTC MEDICAL OFFICE: Office in UTC area. 2–3 exam rooms, ample waiting room, 2 private offices. Ground floor location. Just one block from 805 exit. Close to Genesee Ave, all major shopping and restaurants in UTC. Parking available. Ground floor office, handicapped accessible. Six month–one year lease available with possibility to renew. Call (619) 585-0476. Ask for Alisha. [2890-0825]
GORGEOUS BOUTIQUE OFFICE SPACE IN PRIME LOCATION FOR PER DIEM RENTAL: A newly remodeled and meticulously decorated medical office in University Heights, close to UCSD and Scripps Mercy, available for share including one large furnished patient exam room plus ample shared space (front office, patient wait room, kitchen). Looking for specialty physician preferably and able to do per diem or monthly agreement. The office is shared with 1 other provider and is located on Park Blvd near Adams Ave. Available immediately and turnkey ready. Please contact info@prosperaima.com or (619) 206-4232 for more information. [2883-0804]
OFFICE SPACE FOR LEASE | AESTHETIC SET-
TING: Take your practice to the next level with this beautifully appointed office space available in a modern, fully equipped clinical environment. Whether you’re already in aesthetics or starting an aesthetic practice, we offer flexible, high–end rental options. Rentals include use of PicoSure Pro Laser and Potenza Microneedling with Radiofrequency, two private treatment rooms and staff breakroom in a professional, clean and serene setting. Available Mondays, Tuesdays, Thursdays & Fridays at $1,000/ day between the hours of 8:30am–5:00pm. Ideal for dermatologists/plastic surgeons, cosmetic physicians, nurse injectors or other licensed professionals in the
aesthetic field. Must see to appreciate the quality and atmosphere. Contact us today at Vivian@sandiegomobiledoctor.com to schedule an in-person tour of this great opportunity. [2886-0804]
OFFICE SPACE FOR LEASE | MEDICAL SETTING:
Take your practice to the next level with this beautifully appointed office space available in a modern, fully equipped clinical environment. Whether you’re in primary care or specialty medicine, we offer flexible, high–end rental options. Rentals include use of two medical exam rooms and waiting (lobby) area in a clean, professional setting. Available Mondays, Tuesdays, Thursdays & Fridays at $350/half day or $600/day between the hours of 8:30am–5:00pm. Ideal for primary care physicians and specialists seeking flexible space. Must see to appreciate the quality and atmosphere. Contact us today at Vivian@sandiegomobiledoctor.com to schedule an in–person tour of this great opportunity. [2885-0804]
OFFICE SPACE FOR SUBLEASE | SOUTHEAST
SAN DIEGO: 3 patient exam rooms, nurse’s station, large reception area and waiting room. Large parking lot with valet on-site, and nearby bus stop. 286 Euclid Ave, Suite 205, San Diego, CA 92104. Please contact Dr. Kofi D. Sefa-Boakye’s office manager: Agnes Loonie at (619) 435-0041 or ams66000@aol.com. [2869-0801]
LA JOLLA/XIMED OFFICE TO SUBLEASE: Modern upscale office on the campus of Scripps Hospital — part or full time. Can accommodate any specialty. Multiple days per week and full use of the office is available. If interested please email kochariann@ yahoo.com or call (818) 319-5139. [2866-0904]
SUBLEASE AVAILABLE: Sublease available in modern, upscale Medical Office Building equidistant from Scripps and Sharp CV. Ample free parking. Class A+ office space/medical use with high-end updates. A unique opportunity for Specialist to expand reach into the South Bay area without breaking the bank. Specialists can be accommodated in this first floor high-end turnkey office consisting of 1670 sq ft. Located in South Bay near Interstate 805. Half day or full day/week available. South Bay is the fastest growing area of San Diego. Successful sublease candidates will qualify to participate in ongoing exclusive quarterly networking events in the area. Call Alicia, (619) 585-0476.
MEDICAL OFFICE FOR SALE OR SUBLEASE: A newly remodeled and fully built-out primary care clinic in a highly visible Medical Mall on Mira Mesa Blvd. at corner of Camino Ruiz. The office is approximately 1000 sq ft with 2 fully equipped exam rooms, 1 office, 1 nurse station, spacious and welcoming waiting room, spacious reception area, and ADA accessible restroom. All the furniture and equipment are new and modern design. Ample parking. Perfect for primary care or any specialty clinic. Please contact Nox at (619) 776-5295 or noxwins@hotmail.com. Available immediately.
RENOVATED MEDICAL OFFICE AVAILABLE | EL CAJON: Recently renovated, turn-key medical office in freestanding single-story unit available in El Cajon. Seven exam rooms, spacious waiting area with floor-to-ceiling windows, staff break room, doctor’s private office, multiple admin areas, manager’s office all in lovely, drought-resistant garden setting. Ample free patient parking with close access to freeways and Sharp Grossmont and Alvarado Hospitals. Safe and secure with round-the-clock monitored property, patrol, and cameras. Available March 1st. Call 24/7 on-call property manager Michelle at the Avocado Professional Center (619) 916-8393 or email help@ avocadoprofessionalcenter.com.
OPERATING ROOM FOR RENT: State of the Art AAAASF Certified Operating Rooms for Rent at Outpatient Surgery of Sorrento. 5445 Oberlin Drive, San Diego 92121. Ideally located and newly built 5 star
facility located with easy freeway access in the heart of San Diego in Sorrento Mesa. Facility includes two operating rooms and two recovery bays, waiting area, State of the Art UPC02 Laser, Endoscopic Equipment with easy parking. Ideal for cosmetic surgery. Competitive Rates. Call Cyndy for more information (858) 658-0595 or email Cyndy@roydavidmd.com.
PRIME LOCATION | MEDICAL BUILDING LEASE OR OWN OPPORTUNITY IN LA MESA: Extraordinary opportunity to lease or lease-to-own a highly visible, freeway-oriented medical building in La Mesa, on Interstate 8 at the 70th Street on-ramp. Immaculate 2-story, 7.5k square foot property with elevator and ample free on-site parking (45 spaces). Already built out and equipped with MRI/CAT machine. Easy access to both Alvarado and Sharp Grossmont Hospitals, SDSU, restaurants, and walking distance to 70th St Trolley Station. Perfect for owner-user or investor. Please contact Tracy Giordano [Coldwell Banker West, DRE# 02052571] for more information at (619) 987-5498.
KEARNY MESA OFFICE TO SUBLEASE/SHARE: 5643 Copley Dr., Suite 300, San Diego, CA 92111. Perfectly centrally situated within San Diego County. Equidistant to flagship hospitals of Sharp and Scripps healthcare systems. Ample free parking. Newly constructed Class A+ medical office space/medical use building. 12 exam rooms per half day available for use at fair market value rates. Basic communal medical supplies available for use (including splint/ cast materials). Injectable medications and durable medical equipment (DME) and all staff to be supplied by individual physicians’ practices. 1 large exam room doubles as a minor procedure room. Ample waiting room area. In office x-ray with additional waiting area outside of the x-ray room. Orthopedic surgery centric office space. Includes access to a kitchenette/indoor break room, exterior break room and private physician workspace. Open to other MSK physician specialties and subspecialties. Building occupancy includes specialty physicians, physical therapy/occupational therapy (2nd floor), urgent care, and 5 OR ambulatory surgery center (1st floor). For inquiries contact kdowning79@gmail.com and scurry@ortho1.com for more information. Available for immediate occupancy.
LA JOLLA/UTC OFFICE TO SUBLEASE OR SHARE: Modern upscale office near Scripps Memorial, UCSD hospital, and the UTC mall. One large exam/ procedure room and one regular-sized exam room. Large physician office for consults as well. Ample waiting room area. Can accommodate any specialty or Internal Medicine. Multiple days per week and full use of the office is available. If interested please email drphilipw@gmail.com.
ENCINITAS MEDICAL SPACE AVAILABLE: Newly updated office space located in a medical office building. Two large exam rooms are available M-F and suitable for all types of practice, including subspecialties needing equipment space. Building consists of primary and specialist physicians, great for networking and referrals. Includes access to the break room, bathroom and reception. Large parking lot with free parking for patients. Possibility to share receptionist or bring your own. Please contact coastdocgroup@ gmail.com for more information.
NORTH COUNTY MEDICAL SPACE AVAILABLE: 2023 W. Vista Way, Suite C, Vista CA 92082. Newly renovated, large office space located in an upscale medical office with ample free parking. Furnishings, decor, and atmosphere are upscale and inviting. It is a great place to build your practice, network and clientele. Just a few blocks from Tri-City Medical Center and across from the urgent care. Includes: multiple exam rooms, access to a kitchenette/break room, two bathrooms, and spacious reception area all located on the property. Wi-Fi is not included. For inquiries contact hosalkarofficeassist@gmail.com or call/text (858) 740-1928.
MEDICAL EQUIPMENT / FURNITURE FOR SALE
FRIDGE AND FREEZER EQUIPMENT AVAILABLE | MINT CONDITION: Pristine medical cold storage refrigeration equipment available for purchase by Champions for Health, SDCMS’ philanthropic 501(c)3. Used to store vaccines. Includes 2 (two) commercial-grade Accucold ARG49ML 49 cu ft upright pharmacy refrigerators each with two glass doors, automatic defrost, digital thermostat and stainless steel cabinets (83.75” H x 55.25” W x 31.0” D), plus 1 (one) pharmaceutical-grade TempArmour BFFV15 compact freezer built to ensure stable temperatures and virtually eliminate supply losses (26.5” H x 25.0” W x 31.0” D). All units were acquired new, in use between 2-4 years and in very gently used condition. Units meet all CDC guidelines for vaccine storage. Asking price for each fridge is $4,000 OBO and $2,500 OBO for the freezer. Purchase individually or as a set. Contact Adama at (858) 300–2780 or adama. dyoniziak@championsfh.org. [2879-0502]
NON–PHYSICIAN POSITIONS AVAILABLE
NURSE PRACTITIONER | PHYSICIAN ASSISTANT: Open position for Nurse Practitioner/Physician Assistant for an outpatient adult medicine clinic in Chula Vista. Low volume of patients. No call or weekends. Please send resumes to medclinic1@yahoo.com. [2876-1121]
POSTDOCTORAL SCHOLARS: The Office of Research Affairs, at the University of California, San Diego, in support of the campus, multidisciplinary Organized Research Units (ORUs) https://research. ucsd.edu/ORU/index.html is conducting an open search for Postdoctoral Scholars in various academic disciplines. View this position online: https://apolrecruit.ucsd.edu/JPF03803. The postdoctoral experience emphasizes scholarship and continued research training. UC’s postdoctoral scholars bring expertise and creativity that enrich the research environment for all members of the UC community, including graduate and undergraduate students. Postdocs are often expected to complete research objectives, publishing results, and may support and/or contribute expertise to writing grant applications https://apol-recruit.ucsd. edu/JPF03803/apply. [2864-0808]
RESEARCH SCIENTISTS (NON–TENURED, ASSISTANT, ASSOCIATE OR FULL LEVEL): The University of California, San Diego campus multidisciplinary Organized Research Units (ORUs) https:// research.ucsd.edu/ORU/index.html is conducting an open search for Research Scientists (non-tenured, assistant, associate or full level). Research Scientists are extramurally funded, academic researchers who develop and lead independent research and creative programs similar to Ladder Rank Professors. They are expected to serve as Principal Investigators on extramural grants, generate high caliber publications and research products, engage in university and public service, continuously demonstrate independent, high quality, significant research activity and scholarly reputation. Appointments and duration vary depending on the length of the research project and availability of funding. Apply now at https://apol-recruit.ucsd.edu/ JPF04188/apply. [2867-0904]
PROJECT SCIENTISTS: Project Scientists (nontenured, Assistant, Associate or Full level): The University of California, San Diego, Office of Research and Innovation https://research.ucsd.edu/, in support of the Campus multidisciplinary Organized Research Units (ORUs) https://research.ucsd.edu/ORU/index. html is conducting an open search. Project Scientists are academic researchers who are expected to make significant and creative contributions to a research team, are not required to carry out independent research but will publish and carry out research or creative programs with supervision. Appointments and duration vary depending on the length of the research project and availability of funding: https://apol-recruit. ucsd.edu/JPF04189/apply. [2868-0904]
8690
Day at the Races
Del Mar Thoroughbred Club – Crosby Celebrity Suite Friday, November 21, 2025
Join us for Champions for Health’s Day at the Races at the Del Mar Thoroughbred Club. Enjoy an exclusive afternoon of exciting horse racing, delicious food, and refreshing drinks while supporting vital healthcare programs for San Diego’s underserved communities.
12:00 pm – 4:00 pm (1st race is at 12:30 pm)
Del Mar Fairgrounds 260 Jimmy Durante Blvd, Del Mar, CA 92014 For sponsorship information, please contact Gabriela Stichler at gabriela.stichler@championsfh.org or at 858-300-2789 • Race4Health.givesmart.com