Revolutionizing Patient Care: The Future of Ambulatory Surgery Centers
The shift from hospital-based procedures to Ambulatory Surgery Centers (ASCs) has been accelerating in recent years, impacting workflows, healthcare design, and the patient experience. We sat down with Ron Smith, LS3P’s Raleigh Director of Medical Planning, to talk about emerging trends and the changing landscape of the healthcare market.

You’re seeing significant changes in the healthcare market these days. What’s driving these changes?
Healthcare systems are increasingly shifting outpatient “day surgery” cases from the hospital to Ambulatory Surgery Centers (ASCs). This change is accelerating for a number of reasons; ASCs are convenient and easy for patients to access and have shorter wait times. For physicians, ASCs tend to be more efficient, and they usually offer some investment opportunities to share in ownership. The payers (insurance companies) like them because the fees set by the Centers for Medicare & Medicaid Services (CMS) for procedures at ASCs are lower than in the hospital.
In North and South Carolina specifically, changes coming to the Certificate of Need (CON) requirement soon are the biggest driver. Eliminating the CON for ASCs in large population counties will lower the barrier for developers seeking to provide healthcare in freestanding ASCs. We’re already seeing that these potential changes to the playing field are driving a new market for developers, and this market will be very competitive.
Does this shift change the ways in which we think about healthcare design?
ASCs tend to be focused on one or two surgical specialties. Our designs are typically tailored for specialized end users, which might be an orthopedic or pediatric surgery center that’s like a mini hospital with everything except the beds. The whole design is very customized to the needs of a particular patient profile. We’ve designed many ASCs over the years for healthcare clients including both general surgery centers and highly specialized facilities. In this evolving market, however, we might be working directly for a developer instead of a healthcare system, and that’s a slightly different process. Developers are very focused on efficiencies to maximize return on investment, and for maximum flexibility over time rather than a specialized design – one that will work for most types of surgery.
With surgery moving out of the hospital, one great design change for us is the scale of the buildings. Where surgery departments are deep in the interior of large hospital floors, the smaller ASC buildings allow us to bring much more daylight into patient care areas and staff work areas, and this helps reduce stress for everyone.
Are you seeing changes in the footprint of ASCs as well as in the number of ASCs?
There will always be variables in program spaces due to site conditions or the nuances of the program. However, I think the biggest variable that has to be looked at very carefully from the beginning is the sterile processing department within the ASC. Each one is unique and depends on a lot of operational variables and equipment selection.
When we lay out the operating rooms, we determine what size they’re going to be – typically 500 or 600 square feet, and then that’s a block; it’s the
same with the pre-op and post-op beds. There’s a pattern to those spaces that is replicable and fairly stable. However, sterile processing is a big variable that has to be well thought out, and the earlier the better to understand the organization’s approach and expectations. We need to understand workflow optimization and equipment selection early in the process.
What about evolving technologies? Do continuous changes in medical equipment and other systems mean that ASCs need more space, or less? Equipment is always changing. We’re seeing more robotics, and more sophisticated equipment, as CMS is continually updating its list of covered procedures. Safety and technology continue to evolve, allowing for more types of ASC procedures, and more complex ones. The amount of space required is trending upwards, although, where return on investment is the primary driver, the rooms tend to be smaller.
In this changing market, if the developer is now the client and the healthcare providers are the end users, who is the primary decision maker?
We’re seeing a variety of business models in terms of ownership, and in terms of developer-led project delivery. But in all cases, the healthcare provider remains the primary decision maker. I’d say in most cases, the key decision makers during design are really the perioperative nurse managers. The Association of perioperative Registered Nurses (AORN) puts out some wonderful resources that are incredibly valuable to the design process, and we reference those often.

UNC HEALTH CARE PANTHER CREEK AMBULATORY SURGICAL CENTER
What about the patient experience? Do we have data on how patients and their families feel about the ambulatory shift?
The patient experience isn’t necessarily a driver for this trend, but it’s definitely a factor to watch. The scale and singular focus of an ASC can lead to a much smoother procedure for patients and their caregivers. The buildings are smaller, easier to navigate, usually have convenient parking and spacious waiting rooms, and are likely to be closer to a patient’s home than a remote hospital hub. A large hospital often has multiple buildings and wings connected in an ad-hoc way, which can be confusing and tiring for people trying to manage a stressful day. I’ve had some conversations with strategic planning consultants who are beginning to analyze the consumer market aspect of the ASC trend; it’s likely we’ll have more data on that soon.
The trend towards ASCs has ebbed and flowed a bit over the years. Have we reached a tipping point towards more permanent change?
At the end of the day, ASCs are part of the overall outpatient ambulatory shift that is very much in progress. It is really happening solidly this time. I think it’s due in part to evolving technologies; we can do more types of procedures, more safely, on an outpatient basis now. Policy changes from CMS are a driver, seeking to reduce costs overall. CMS is constantly updating the list of surgical procedures that can be performed in ASCs and setting reimbursement rates that are as much as 40% lower than in the hospital. So, CMS is pushing while the market is pulling, accelerating this trend.
ASCs are a “win-win” for providers and patients. Higher volumes and more covered procedures means a viable business model for owners and providers. And smaller, human scale buildings with generous daylight and the latest technology mean a positive experience for patients and their families.
Meet Ron
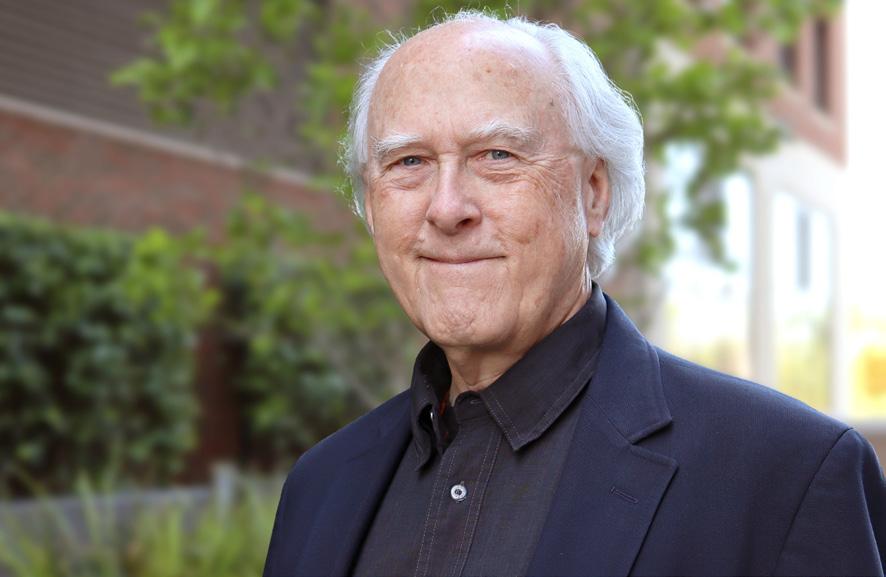
Ron Smith, a Board Certified healthcare architect and past president of the AIA Academy of Architecture for Health (AAH), brings 40 years of healthcare planning and design experience. Ron’s design expertise includes strategic master planning, functional and space programming, collaborative stakeholder engagement, medical planning, and design. His built work includes ambulatory surgery centers, hospitals, cancer centers, academic medical centers, primary and specialty care clinics, federally qualified health centers, and long-term care facilities. As an active member of the AAH, Ron is an advocate for shared knowledge among healthcare architects and clients on how the healthcare environment affects the well-being of both patients and staff. He is the founder of the AIA AAH Research Initiatives Committee, the author of a resource page on Therapeutic Environments for the Whole Building Design Guide, and an affiliate member of the American College of Healthcare Executives. Ron earned his BFA in Interior Architecture from the Rhode Island School of Design and he is certified in Lean for Healthcare.