





PUBLISHED BY: traveling Blender, llC. 10036 Saxet Boerne, tX 78006

PUBLISHER louis doucette louis@travelingblender.com
BUSInESS MAnAgER: vicki Schroder vicki@travelingblender.com







PUBLISHED BY: traveling Blender, llC. 10036 Saxet Boerne, tX 78006

PUBLISHER louis doucette louis@travelingblender.com
BUSInESS MAnAgER: vicki Schroder vicki@travelingblender.com
Moved to Action:

ADvERTISIng SALES:
AUSTIn: Sandy Weatherford sandy@travelingblender.com
SAn AnTOnIO: Gerry lair gerrylair@yahoo.com
For more information on advertising in San Antonio Medicine, Call Traveling Blender at 210.410.0014 in San Antonio and 512.385.4663 in Austin.
San Antonio Medicine is the official publication of Bexar County Medical Society (BCMS). All expressions of opinions and statements of supposed facts are published on the authority of the writer, and cannot be regarded as expressing the views of BCMS. Advertisements do not imply sponsorship of or endorsement by BCMS

EditoriAl CorrESpondEnCE: Bexar County Medical Society 4334 n loop 1604 W, Ste. 200 San Antonio, tX 78249
Email: editor@bcms.org
MAGAZinE AddrESS CHAnGES: Call (210) 301-4391 or Email: membership@bcms.org
SuBSCription rAtES: $30 per year or $4 per individual issue
AdvErtiSinG CorrESpondEnCE: louis doucette, president traveling Blender, llC.
A publication Management Firm 10036 Saxet, Boerne, tX 78006 www.travelingblender.com
For advertising rates and information
Call (210) 410-0014
Email: louis@travelingblender.com
SAn AnTOnIO MEDICInE is published by SmithPrint, Inc. (Publisher) on behalf of the Bexar County Medical Society (BCMS). Reproduction in any manner in whole or part is prohibited without the express written consent of Bexar County Medical Society. Material contained herein does not necessarily reflect the opinion of BCMS, its members, or its staff. SAn AnTOnIO MEDICInE the Publisher and BCMS reserves the right to edit all material for clarity and space and assumes no responsibility for accuracy, errors or omissions. San Antonio Medicine does not knowingly accept false or misleading advertisements or editorial nor does the Publisher or BCMS assume responsibility should such advertising or editorial appear. Articles and photos are welcome and may be submitted to our office to be used subject to the discretion and review of the Publisher and BCMS. All real estate advertising is subject to the Federal Fair Housing Act of 1968, which makes it illegal to advertise “any preference limitation or discrimination based on race, color, religion, sex, handicap, familial status or national orgin, or an intention to make such preference limitation or discrimination.
SmithPrint, Inc. is a family-owned and operated San Antonio-based printing and publishing company that has been in business since 1995. We are specialists in turn-key operations and offer our clients a wide variety of capabilities to ensure their projects are printed and delivered on schedule while consistently exceeding their quality expectations. We bring this work ethic and commitment to customers along with our personal service and attention to our clients’ printing and marketing needs to San Antonio Medicine magazine with each issue.

John Joseph nava, Md, President
Brian t. Boies, Md, Vice President
Ezequiel “Zeke” Silva iii, Md, President-elect
John Shepherd, Md, Secretary

rajeev Suri, Md, Treasurer and Immediate
Past President
Woodson "Scott" Jones, Md, Member
Sumeru “Sam” G. Mehta, Md, Member
M. “Hamed” reza Mizani, Md, Member
priti Mody-Bailey, Md, Member
lubna naeem, Md, Member
lyssa n ochoa, Md, Member
Jennifer r. rushton, Md, Member
raul Santoscoy, do, Member
lauren tarbox, Md, Member
Jenny Case, Alliance Representative
ramon S. Cancino, Md, Medical School
Representative
lori Kels, Md, Medical School Representative
robert leverence, Md, Medical School
Representative
Keiko McManus, Md, Board of Ethics Chair
John pham, do, Medical School Representative
Cheryl pierce-Szender, Alliance Representative
ronald rodriguez, Md, phd, Medical School
Representative
Elisa d o’Hern Col, MC, FS, Military Representative
George F. “rick” Evans, Jr., General Counsel
Jayesh B. Shah, Md, TMA Board of Trustees
Melody newsom, CEO/Executive Director
Melody newsom, CEO/Executive Director
Monica Jones, Chief Operating Officer
Yvonne nino, Controller
Mary nava, Chief Government Affairs Officer
Brissa vela, Membership Director phil Hornbeak, Auto Program Director
August trevino, Development Director
Betty Fernandez, BCVI Director
Al ortiz, Chief Information Officer
norys Alexandra Castro-pena, Md, Co-chair
John Joseph Seidenfeld, Md, Co-chair
louis doucette, Consultant
david Schulz, Community Member
Elizabeth Clanton, Md, Member
Kristy Yvonne Kosub, Md, Member
neal Meritz, Md, Member
Jaime pankowsky, Md, Member
Alan preston, phd, Member
rajam S. ramamurthy, Md, Member
Adam v ratner, Md, Member
Faraz Yousefian, do, Member
Moses Alfaro, Student Member
victoria Ayodele, Student Member
tue Felix nguyen, Student Member
niva Shrestha, Student Member
Bethanne Bradshaw, Student Member
Andrew ta, Student Member
Monica Jones, BCMS Coo, Staff Liason
trisha doucette, Editor

 By John J. Nava, MD, 2023 BCMS President
By John J. Nava, MD, 2023 BCMS President

In my own mind, there has never been a question regarding the close connection between practicing medicine and being empathetic and compassionate. I have always accepted that the privilege of helping people heal themselves carries the obligation to practice ethically. I also realize that however strongly I hold this opinion, it is strictly a personal interpretation, and gives me no right to dictate to my colleagues. While I do think all physicians share that professional obligation, each physician follows his or her own individual path of discovery for themselves, and that self-determination is to be respected. Doctors are people, and their choices are their own to make.
Where does my belief come from? I suspect it started with a robust Roman Catholic upbringing, but I also recall reinforcement in the form of a one-hour elective in bioethics when I was a medical student. During that semester, I learned the basic tenets of bioethics during a course elective offered by the Institute of Religion in the Texas Medical Center in Houston. Starting with philosophical concepts and definitions, I learned of the four pillars of ethics in healthcare, which are autonomy (respect for the patient's right to self-determination), beneficence (the duty to ‘do good’), non-maleficence (the duty to ‘not do bad’), and justice (to treat all people equally and equitably).
I also learned that altruism is a noble human motivator of concern for others expressed as selflessness. Many people feel enriched by internal approval, and gain moral superiority by acting in this manner as they help others. However, this behavior does put the person in a vulnerable position where they may be taken advantage of. This impulse toward selflessness needs to be balanced with self-care as physicians must strive to maintain work-life balance.
Effective altruism is a philosophical and social movement that developed about 10 to 15 years ago. This movement advocates using evidence and reason to maximize the benefits to others and to take altruistic action on that basis. In essence, getting the most bang for your buck is a goal in and of itself. The proponents of this movement even developed a charity evaluating nonprofit, called GiveWell, to decide which efforts were most worthy of support. The most basic application of this perspective would result in a wariness of donating money to efforts that spend the major portion of your donated funds on overhead rather than direct service to persons receiving the benefit. This is a common-sense measure that offers sound reasoning to help us decide where we will direct our support. The movement had a philosophical basis of rationalism, but when applied in a very strict manner, this sometimes can lead to unintended consequences and less than desirable results.
In the last few years, a major proponent of effective altruism was Sam Bankman-Fried, founder of the cryptocurrency exchange FTX. Crypto created an illusion of value where there existed none before. Then it moved to the marketplace, where it could be traded for more traditional units of value, like dollars. With the bankruptcy of cryptocurrency, the effective altruism movement has been criticized, and has fallen out of favor. The movement has evolved to “longtermism,” which emphasizes our responsibility to future generations, yet unborn, to donate efficiently and effectively today to create a better future world for them. What about current generations whose unmet needs cause much human suffering and exist through no fault of their own? Does this point of view devalue the current generational cohort, writing off efforts to improve their current condition? To be honest, I have never dabbled in cryptocurrency as an invest-
ment, and I would rather decide for myself which causes I want to support. Both crypto and outsourcing the responsibility of deciding where to lend support in either time or monetary donation seems to smell of snake oil to me.
I am reminded by a quote attributed to Mother Teresa, advising us that if we want to help someone, we can start with the person next to us. There are so many unmet needs within our own community, it doesn’t take long to find a worthy cause to support. Finding a charity closer to home allows us a better opportunity to monitor progress, decide on effectiveness, and maintain the support if we are able and consider it appropriate. Helping people that are here now is laying the best foundation for future generations. For the needs of those future generations, we can cross that bridge when we come to it. Though I reject the flawed logic of effective altruism, I will retain skepticism for those middleman organizations that spend most monetary donations on costs instead of direct service.
In closing, each of us is finding the work-life balance that resonates with each of our lives. I encourage all members of BCMS to establish a constant state of gratitude for all the riches of life we enjoy, and not be distracted by what we are lacking. Consider contributing your time
to committee, council or board activity at BCMS or TMA. Helping others in this way, through the action of advocacy, is empowering and life affirming. Helping others also has benefits to the volunteer. Compassion towards others has a way of spilling over into benefits from self-compassion.
I do want to remind everyone about the Out of the Darkness Community Walk — an activity of the AFSP (American Foundation for Suicide Prevention). This is an outreach activity promoted by the Physician Wellness Committee of BCMS. This event occurs on October 28, 2023 at Nelson Wolff Stadium. Check-in is at 8:30 a.m., and the walk start time is 9:30 a.m. There are opportunities for walkers, whether you decide to fundraise or not, and day of event volunteers. Everyone is welcome to participate however they would like to help. BCMS would like to walk as a group, so we do need to organize a bit. Contact Monica Jones at 210-301-4373 if you are interested!
John J. Nava, MD, is the 2023 President of the Bexar County Medical Society. He is interested in Primary Care, Clinical Research and Public Health.

Fall is one of my favorite seasons in the kitchen — earthy roasted vegetables, tart cranberries and aromatic spices like cinnamon and nutmeg all have their time to shine. But as we embrace the joys of autumn, we must also navigate the temptations of holidays and festive gatherings, which often lead to overindulgence. Here are some of my top tips to maintain balance this season.


Most varieties of produce can be found year-round in the supermarkets, but if you stick with the ones in season, you’ll find that they have the best taste, peak quality and cheapest price.
• Parsnips and cruciferous vegetables such as Brussels sprouts, cabbage and cauliflower. Try these roasted on a sheet pan with a little olive oil, salt and pepper for a great, nutrient-rich addition to any meal.
• Cranberries, pears and figs burst with flavor in the fall season. Try using cranberries in more than just your Thanksgiving meal. They are a tart addition to smoothies, salads and homemade breads.
• Pumpkins and sweet potatoes — use in both savory and sweet dishes for a meal loaded with vitamin A.
Who can resist their favorite fun-sized candy bar on Halloween? Unfortunately, eating candy by itself can cause your blood sugar to rapidly
increase, followed by a crash, which can develop into long-term health problems such as diabetes. Instead, enjoy your candy with your meal or pair it with a healthy protein for a snack. Mini M&Ms sprinkled on top of Greek Yogurt provide protein, calcium, probiotics and carbohydrates for a tasty afternoon snack that will leave you feeling energized and satisfy your sweet tooth.
No need to fear your Thanksgiving meal! Strategize by loading your plate with vegetables first, which will naturally limit the room you have to load it with the higher fat, higher calorie menu items. The USDA “MyPlate” recommends that half of your plate be fruits/vegetables, one fourth protein and one fourth whole grains. Choose turkey breast without the skin for the lowest fat content.
Relish the festive period with your loved ones! Indulging occasionally doesn't negate a generally healthy diet. Steer clear of caloriecounting stress or scale obsessions, and let the spirit of the season shine through.

Headlines, conferences, podcasts and national reports are filled with reports of “burnout,” “moral injury” and resignation in healthcare. The subtitle of Dr. Wendy Dean’s book If I Betray These Words asks “…why it’s so hard for clinicians to put patients first.” For some doctors, the business and busyness of medicine negate the equal exercise of the heart and head in their calling.
Thankfully, there are scientifically proven answers to the crisis of moral injury and burnout in medicine. Emerging evidence demonstrates that doctors can embrace caring in medicine that satisfies body, mind and spirit, as well as fiscal bottom lines. In their book Compassionomics, Drs. Stephen Trzeciak and Anthony Mazzarelli detail and discuss the voluminous evidence that attention to compassionate care increases quality, safety and value in medicine.
Given the pace and complexity of medical practice, many doctors doubt that time is available to engage patients sufficiently to hear their concerns and address them empathetically. While re-engineering the ecosystem remains essential to optimizing medical care, there are demonstrated techniques that can improve a doctor’s compassionate approach to the patient encounter. Dr. Helen Riess, researcher and author of The Empathy Effect, says that increasing empathy and compassion in medical care does not require increased time in the clinical encounter. Empathy can save time through elicitation of the patient’s truest concerns.
Dr. Riess tells us that empathy is the human capacity enabling “…us to be moved by the plights and emotions of others.” Drs. Trzeciak and Mazzarelli indicate that “…empathy (the feeling and understanding component) is a prerequisite for compassionate behavior (the action component) …”
Doctors may believe that empathy is a special innate gift, but empathy can be learned like any other clinical skill in medicine (see Resources). Both The Empathy Effect and Compassionomics detail multiple studies of the benefits for clinician and patient when compassionate
care can be offered. They offer equally instructive warnings on how failures of compassion cost patients, providers, the health system and community at large.
Though the benefit of compassionate care may be proven, the practical pressures remain as multiple parties ask doctors to assume new and added roles in managing the Social Determinants of Health (SDOH), Trauma Informed Care (TIC), social isolation, and other components of patient and provider well-being. These new duties seem outside and beyond the control of the traditional doctor-patient clinical encounter. Yet finding a way to address them seems more pressing now than ever. Kahl and Heitland cite evidence in their editorial that the predictive role of loneliness in causing cardiovascular disease (CVD) “…was stronger than that of lifestyle risk factors including smoking, depression scores, physical activity and diet.” Patients’ outcomes are affected by place, a sense of belonging, and even their understanding of their place in the universe. Not surprisingly, insurers like Cigna and health systems such as the Veteran’s Administration are adopting “Whole Person” approaches that include SDOH and even spiritual dimensions of health as part of new measures of health and well-being (see Resources).
Despite best practices, there may be circumstances requiring that a physician and patient must part ways. Detailing the circumstances and procedures is beyond the scope of this article. Physicians should consult their professional society, Texas Medical Association (TMA), or their liability carrier for guidance on when and how this may be done. Determining boundaries is critical to recognizing that even the most skillful, compassionate physician may have cause to part with a patient. In a time when physician “burnout” is at a record high, we should extend empathy and compassion towards colleagues and ourselves as we pursue the art and calling of medicine.
Addressing all of these multiple components seems daunting. Many changes in reimbursement models, staffing, training and social environment remain entrenched and unreformed. There are some
“The practice of medicine is an art, not a trade; a calling, not a business; a calling in which your heart will be exercised equally with your head.”
Sir William Osler
bright spots, however. For example, the Center for Innovation in Family Medicine offers tools, training and re-engineered workflows to help practices address what matters most to doctors and patients alike (see Resources). Specialty societies and medical societies also produce helpful tools to aid in work life transformation. Undoubtedly, much remains to be done to reform payment models and quality measures, and to shift the focus from proxy measures of performance that have little correlation with the heart of medicine’s call. However, renewed skills and acts of compassion can do much to restore the joy of medicine today.
Compassion and Training Resources: Astute Doctor
Improving doctor-patient encounters through improved communication on what matters. www.astutedoctor.com

Compasionomics
Evidence that caring matters — resources, research and updates. www.compassionomics.com
Empathetics
Evidence, training and other resources. www.empathetics.com
Spiritual Care Training for Healthcare Providers https://gwish.smhs.gwu.edu/program/transforming-practice-healthsettings/ispecc-training-course
Communication: General and Special Topics: CHEST®: First 5 Minutes
Building patient trust and co-agenda setting training for more effective patient encounters. www.chestnet.org/Learning-and-Events/First-5Minutes
Texas Medical Association CME
Trauma Informed Care: Noncompliant or traumatized, enhancing communication to improve patient safety and professional satisfaction, communication skills for dealing with difficult patients, spirituality, leadership and values in the world of medicine. www.texmed.inreachce.com
Texas Health Steps
Addressing adverse childhood experiences through trauma-informed care, culturally effective healthcare. www.txhealthsteps.com
Whole Person Care: Cigna Vitality Measure www.newsroom.thecignagroup.com/vitality
Center for Innovation in Family Care
www.healingworksfoundation.org/clinician-as-healer-in-primary-care
Veterans Administration Whole Health Care www.va.gov/wholehealth
References:
Silverman, ME (2010). The Quotable Osler. Philadelphia: American College of Physicians
Dean, W (2023). If I Betray These Words. Lebanon: Steer Forth Press
Trzeciak, S (2019). Compassionics. Pensacola: Studer Group
Riess, H (2018). The Empathy Effect. Boulder: Sounds True
Kahl, K G, Stapel, B & Heitland, I (2023). A lonely heart is a broken heart: it is time for a biopsychosocial cardiovascular disease model. European heart journal, 44(28), 2592–2594. https://doi.org/ 10.1093/eurheartj/ehad310
Edward Dick, MD, is a Board-Certified Family Physician and Director of Clinical Complex Care for Methodist Healthcare Ministries.

Have you ever boasted about having a strong immune system? Or, alternatively, wondered why you seem to get extra sick extra often? Common sense suggests that people respond differently to sickness and stress. But so far, there has not been an easy way to verify this hunch or to consistently measure what may be a core, underlying aspect of health.
National Institutes of Health-supported researchers proposed a new framework for understanding what they call immune resilience: the capacity of some people to avoid illness and/or bounce back more quickly when they do get sick with viral infections or other inflammatory stressors. They found that people who maintain good immune resilience, even in the face of immune system stressors, tend to live longer and to stay healthier.
Importantly, the researchers also developed accessible tools for measuring immune resilience in both healthcare settings and clinical research. Now, instead of turning to an online quiz to try to discover your "real age," you may be able to gauge the strength of your immune system by taking a simple lab test.
Those tests could help doctors factor in immune resilience before surgeries or during checkups to predict patient risks and outcomes. Another measurement is based on the expression of certain genes. These tests could help researchers control for immune resilience in clinical trials, uncover connections between immune resilience and aging, and learn more about how and why immune resilience is eroded in some persons but not others facing the same inflammatory stressor.
The paper, published June 13 in the journal Nature Communications, combines findings from around 48,500 people in different studies conducted in Africa, Europe and North America. The research involved a global team led by Sunil Ahuja, MD, a professor of medicine at The University of Texas Health Science Center at San Antonio and director of the Veterans Administration Center for Personalized Medicine.
The research team found that, as in other facets of life, resilience at an immune level is related to both what you are up against and how you respond. According to the researchers, low levels of inflammatory stress combined with highly competent immune responses were most protective for health. Still, some people managed to maintain high immune function even in the face of lots of inflammatory stress, a finding that raises new opportunities for research into longevity and health.
Like people’s emotional responses, immune systems can essentially overreact, under-react or respond gracefully when they sense an attack. The ability to respond effectively is called immunocompetence, which the researchers assessed by two different metrics.
The first metric involves measuring the proportional mix of two different types of T-cells, which are the white blood cells that activate when the body responds to threats. These two types, CD8+ and CD4+, are already frequently measured for patients with HIV and AIDS. Researchers identified a specific mix that predicted the best immunocompetence. They created an immune health grade (IHG) to capture how well people align with this mix on a scale of one to four, with IHG-I being the most protective and IHG-IV being the least. A simple lab test can measure that mix for individuals.
In clinical studies, though, researchers can't always order T-cell labs. So, the authors found a different metric researchers can look at instead, using a person's RNA samples to look at clusters of genes. Some of our genes change their expression in response to infections or other inflammatory stressors. The researchers found one pattern of gene expression that was associated with survival, which they called survival-associated signature or SAS-1. SAS-1 comprised genes related to immune competence, and higher expression of these genes correlated with survival.
They also found another cluster of genes and gene expression associated with lower resilience and premature death. That mortality-associated cluster they termed MAS-1. MAS-1 comprised genes related to inflammation, and higher expression of these genes correlated with mortality. When the body kicks into gear — whether in response to the flu or simply to allergy season — that response is known as inflammation.
The researchers found that, like the T-cell metric, these patterns of gene expression can be used as a proxy for overall immune resilience. A mix of high SAS-1 gene expression and low MAS-1 gene expression, which the researchers labeled optimal immune resilience, correlated with general longevity, as well as a wide variety of specific positive health outcomes, like survival from sepsis and COVID-19, resistance to acquiring HIV infection, a slower rate of progression to AIDS, avoiding recurring cancer after a kidney transplant, and avoiding flu symptoms.
To tease apart the roles of immunocompetence and inflammation in immune resilience, the researchers looked at people likely to face high,
medium and low levels of immune stressors in their daily lives. For low levels, they looked at thousands of people participating in studies on aging. For medium levels, they looked at people with autoimmune disorders, kidney transplants or COVID-19 infections, along with sex workers exposed to sexually transmitted infections. For high levels of immune system activation, they looked at people living with HIV, who experience consistent inflammatory stress because their immune systems misread lots of things as threats.
The researchers found that immune resilience can change during inflammatory stress. In T-cell readings before and after flu season or COVID-19, as well as after volunteer challenges with common respiratory viruses, the researchers found that immune resilience goes down while the immune system is actively inflamed and fighting a threat. For most people, once the threat had passed, the metrics of immune resilience returned to levels that preceded the threat. But for other people, metrics dropped and stayed lower for months.
The researchers found that periods of inflammatory stress can degrade immunocompetence, making our bodies less effective at responding to future risks. In other words, what doesn't kill you may make you weaker, not stronger. But that's not true for everyone: the researchers found that a subset of people maintained consistently good immunocompetence over their lifetimes, despite repeated threats. That finding may open new avenues for research into longevity.
Researchers couldn't predict beforehand whose immune function would degrade or remain steady after each threat. But they did find that more competent immune systems were associated with lower mortality. COVID-19 patients, for example, were less likely to die if they pre-

In good news for people with lower immune resilience, the researchers also found that immunocompetence may improve over time.
For degraded immune systems, it appears that just getting a break from inflammatory stress may help immunocompetence rebound. One group of sex workers, for example, had frequent unprotected sex at the beginning of the 10-year study — meaning lots of sexually transmitted infections for their immune systems to fight off. But over the next decade, they shifted to using safer sex practices. Researchers found that when their immune systems had fewer infections to fight, their immunocompetence was able to bounce back. It is possible that reducing inflammatory stress in other contexts could also help to strengthen immune resilience over time, reducing the risk of poor health outcomes.
Looking at people from ages 9 to 103, the researchers found a mix of immune resilience levels across each age bracket. While levels of immune resilience declined with age, some younger persons had lower immune resilience levels, whereas some older persons preserved metrics of optimal immune resilience. Often, age has been used as a proxy for immune status. For example, in response to the COVID-19 pandemic, older people were advised to be more cautious. However, within each age bracket, people differ in their susceptibility to severe COVID-19 outcomes; conceivably, these differences may relate to susceptibility to preserve versus degrade immune resilience during COVID-19.
The researchers also found that women tended to have higher immune resilience than men — but at an individual level, it's impossible
continued on page 16
continued from page 15
to guess immune resilience just by looking at gender. Screening for immune resilience as well as factors like age and gender could allow for more individualized and accurate advice about risks.
The researchers also hope that learning more about how immune resilience works can have a wide variety of benefits for people and for society. On an individual level, screening for immune resilience may help people better understand their health risks and make choices accordingly. It may also help doctors monitor treatment responses to severe viral infections or other illnesses that erode immune resilience. From a research perspective, balancing clinical trials by immune resilience levels, as well as by factors like age, gender, race and ethnicity, may help clarify how different people will respond to vaccines or other drugs.
Finally, from a public health perspective, understanding the importance of reducing inflammatory stress may lead to new strategies for addressing health disparities on a broader scale, so that more people have the opportunity to recover optimal immune resilience and lead longer, healthier lives.
References:
Immune resilience despite inflammatory stress promotes longevity and favorable health outcomes including resistance to infection. Ahuja SK, Manoharan MS, Lee GC, McKinnon LR, Meunier JA, Steri M, Harper N, Fiorillo E, Smith AM, Restrepo MI, Branum AP, Bottomley MJ, Orrù V, Jimenez F, Carrillo A, Pandranki L, Winter CA, Winter LA, Gaitan AA, Moreira AG, Walter EA, Silvestri G, King CL, Zheng YT, Zheng HY, Kimani J, Blake Ball T, Plummer FA, Fowke KR, Harden PN, Wood KJ, Ferris MT, Lund JM, Heise MT, Garrett N, Canady KR, Abdool Karim SS, Little SJ, Gianella S, Smith DM, Letendre S, Richman DD, Cucca F, Trinh H, Sanchez-Reilly S, Hecht JM, Cadena Zuluaga JA, Anzueto A, Pugh JA; South Texas Veterans Health Care System COVID-19 team; Agan BK, Root-Bernstein R, Clark RA, Okulicz JF, He W. Nat Commun. 2023 Jun 13;14(1):3286. doi: 10.1038/s41467-023-38238-6. PMID: 37311745.
https://pubmed.ncbi.nlm.nih.gov/37311745/
Sunil Ahuja, MD, is the Director of the Veterans Administration Center for Personalized Medicine at the VA hospital in San Antonio. At the University of Texas Health Science Center, he holds the President's Council/Dielmann Chair for Excellence in Medical Research and is a tenured professor in the Departments of Medicine, Microbiology, Immunology and Biochemistry. Dr. Ahuja is the recipient of many prestigious awards, including the NIH MERIT Award, Doris Duke Distinguished Clinical Scientist Award, Burroughs Welcome Clinical Scientist Award in Translational Research, and Elizabeth Glaser Scientist Award in Pediatric AIDS Research, as well as election to the American Society of Clinical Investigation and Association of American Physicians.



n his inaugural speech as AMA President, Dr. Jesse Ehrenfeld stated, “Physicians across the country continue to shoulder the weight of enormous challenges. Yet despite these immense pressures, we physicians continue on. We do the work. We provide compassionate care. We make a difference. We change lives.” What he didn’t mention is that while we are busy taking care of our patients, our families and our obligations, we forget to take care of ourselves. We get so caught up paying our past school debts and focusing on securing a safe future for ourselves and our family that we forget to live in the present. I have had many friends die young due to illness compounded by intense stress from the challenges that are beyond our control.
As an Ob Hospitalist, we have a unique set of challenges. We serve as first responders to pregnant and unaligned gyn patients, and we also take care of sick pregnant patients who are transferred to a higher care. We deliver obstetric patients and perform emergency surgeries due to miscarriages and ectopic pregnancies. Is it rewarding? Most times, yes. Definitely! We worry about being criminalized for taking care of our female patients. However, I leave in the morning knowing that due to physician-guided/team collaboration, we are able to avoid bad outcomes and provide elevated patient care.
The thing that we don’t realize is that the body keeps the score. At some point, something must give and typically it’s our body, our health, our minds. A medical career is tough. For my colleagues who have been able to keep it all together, sincerely I admire you and secretly wish I was you. For the rest of us, the struggle is real. Brene Brown once said that people are doing the best that they can. I must believe that this is true in others, so that I can understand that it’s the truth in me. I’m truly doing the best that I can.
I have always been a big girl. I was the first and probably only 200lb dance team member in my school’s history. Prior to my 40’s, I had an active lifestyle; I had participated in several sprint triathlons, beach-tobay relays and hotter-than-hell bike races. I was one of the first adapters to CrossFit when it began. Then the injuries started, the movement decreased, and the workload piled on. I started with my first autoimmune diagnosis in 2013 and began seeking more healthy lifestyle options. I have been mostly pescatarian during this time, however I have had my lapses. In 2019, after 10 years of being in a high-stress working environment, I developed diabetes. I was so ashamed; I couldn’t tell anyone. I was angry with myself and told myself that I should have known better. I researched and read so much that I ultimately became a diplomate of
the American Board of Obesity Medicine.
GI Joe lied when he said that knowing is half the battle. The mistaken idea that “knowing” is enough to change your behavior is a fallacy according to the Yale Professor, Laurie Santos. It is one of two parts, and they are not equal. The most important part is to know something and put it to use. The emphasis is to have action on the knowledge. In the June issue of San Antonio Medicine, Dr. Katipally, (one of my ex-residents - so proud of you!), wrote an excellent article detailing the prevalence of chronic disease and the impact it has on the system. He details his call to action through the creation of a program that follows the principles of Lifestyle Medicine.
For my colleagues who have it together, two thumbs up. For the rest of us who have room to improve, this is a call to action. We must give ourselves grace and self-compassion. The one thing that I have learned from my millennial students and residents is that they are able to set boundaries for better life/work balance. They put their own oxygen masks on first before going out in the world and saving lives. Life is too short and the call to action is now to commit to living a healthier lifestyle.
Take a moment and reflect on a time when you were fun. What comes to mind? What were you passionate about? Do you feel it now?
How can you get it back?
Joseph Campbell, whose writings inspired George Lucas’ creation of Star Wars and who George Lucas refers to as “his Yoda,” is famous for The Hero’s Journey. In both The Hero’s Journey and the quote “Physician, heal thyself,” the journey includes leaving for an adventure. I was told once by my attending, “Even Jesus had to leave Nazareth to be known as the Messiah, for had he stayed in Nazareth, he would only always be the carpenter’s son.” As I have journeyed through my career, first in academics, FQHC, border medicine, private practice, hospitalist and now back in academics at UIWSOM, I have followed my bliss through the thick and thin of things, experiencing joy, disgruntlement and laughter, and feeling most the sense of fulfillment when training and aiding in the formation of future physicians and having patient relationships.
It is said that we are all seeking a meaning for life but what I feel we are really seeking is the experience of being alive again.
COVID/SNOVID showed us how precarious things are and that it is vital to find ourselves living in the now, making healthier lifestyle choices. To reiterate the six pillars of lifestyle medicine, this includes: good sleep, hygiene, eating plant-based diets, exercising 30 minutes daily, maintaining community and family time, decreasing/stopping substance use, and spending time to destress by doing activities that make you happy. In January, we started a Walk with a Doc chapter with the sponsorship of TMA. This is what I strive to do daily for a better tomorrow.

Do. Or do not. There is no try.



Ozempic and other injectable weight loss medications are a hot topic in the healthcare community right now. Many providers are not trained to provide behavioral counseling and support to their patients while administering these medications, and as a result may not achieve the most effective and safest possible long-term outcomes. My work as a member of a multi-disciplinary behavioral healthcare team at the Bariatric Counseling Center has allowed me to see how a variety of behavioral interventions support patients’ desired outcomes with these medications and help prevent endangering their health.
Effective behavioral interventions help keep patients safe by enhancing their motivation and self-efficacy regarding habit change, and by increasing their ability to recognize and successfully navigate common
barriers to the successful use of weight-loss medications. Those who are directly prescribing weight loss medications can do several things inoffice from a behavioral perspective to enhance patient safety. Because of the way that weight loss medications can impact mental health, screening for current and historical psychiatric symptoms can help reduce the risk of inducing mania, anxiety, eating disorders and suicidal ideation with an inappropriate medication. With less severe psychiatric side effects, like mild anxiety or depressive symptoms, providers can monitor and manage with appropriate medications. Patients are also well-served when their providers help them to identify side effects that may cause discomfort. Providers can proactively help them to manage risks of constipation, nausea and malnutrition with medications and instruction on managing these with diet and movement.

The efficacy of weight loss treatment with medications can also be enhanced when complemented by direction on changing eating behaviors. Eating more slowly and methodically can help people to recognize fullness cues before they become uncomfortably full. If discovered to be doing so, patients should be directed not to induce vomiting when nauseous or overly full, due to the risk of developing increasingly disordered eating habits. For those whose eating habits are driven by food cravings and hunger, they may struggle with making decisions about what and how to eat without those cues, and may then be at risk for undereating; they may benefit from education about how to schedule their meals and about basic nutrition. Other patients may not eat when nauseated, even though many people often experience nausea because they are hungry and find eating relieves their discomfort. Patients can benefit from direction to try to eat at their next mealtime, even when nauseated.
Providers may want to refer their patients to dietitians and mental health professionals to handle these and other aspects related to their patients’ eating habits and mental health that could impact their success with weight loss medications. Many people use food to cope with emotional distress and may find their distress increases when they cannot engage in binge eating or emotional eating any longer to relieve stress, anger, sadness, etc. Mental health professionals can help patients to improve their abilities to cope with uncomfortable emotions without relying on food to do so. Mental health professionals can also help patients to develop the interpersonal skills to manage “food-pushers” at social events and family members who are not supportive of changing the home food environment as well as other relationship stressors that can be barriers to lifestyle changes. Patients may need support with creating habits and other behavioral changes to support the desired outcomes of the medications, and they may need help structuring their schedules, their meals, and their movement activities. Patients may need to develop new hobbies that are less focused on preparing and consuming food, as these hobbies may be less fulfilling with a lessened appetite and can result in low mood. When clients are better prepared for a new lifestyle, they will experience less anxiety about going off the medications eventually and will feel more confident that they have made real changes to their lives that benefit them, with or without the addition of medications, and feel more motivated to maintain their behavioral changes for the long-term.

Dr. Sara Hamilton is a licensed clinical psychologist and the clinical director of the Bariatric Counseling Center. She believes successful health interventions focus on helping people to make changes that are meaningful to them and are sustainable long-term. At the Bariatric Counseling Center, she leads a multi-disciplinary team that approaches the treatment of obesity from a behavioral health perspective.

The following speech was given by Mayor Ron Nirenberg this past June 4, 2023, at the annual U.S. Conference of Mayors’ meeting in Columbus, Ohio. These words officially launched a no-cost, online and public access educational campaign, CompassionateUSA. This people-centered campaign was created by San Antonians for San Antonians and now reaches across the nation and around the world.
We are here today to present an earnest and honest remedy to the political polarization, civil discord, racialized violence, and the far-reaching impacts of a global pandemic.
The tragedy that struck just a year ago and 80 miles away from the City of San Antonio in Uvalde, Texas exacerbated the need for both urgent and drastic change. The following U.S. Conference of Mayors’ annual meeting was painfully colored by the recent horrors, but our convening afforded leaders across the country to engage in conversations to guide our country toward a more compassionate path.
As chair of the Mayors and Business Leaders Center for Compassionate and Equitable Cities within the U.S. Conference of Mayors, I – and I’m sure many of you — returned home determined to be a catalyst for change and progress.
Local conversations with my friends, family and colleagues resulted in a bright vision and collaborative effort between the City of San Antonio, the Alamo Colleges District, and our greater community to build a true foundation for compassion.

And today, together, we are proudly launching CompassionateUSA — which will continue our spirit of collaboration to build and demand a brighter future for our nation.

The concept of compassion is rooted in the Golden Rule, to treat all others in the ways we wish to be treated. It is an ethic that has existed in some way, shape or form in every tradition or culture that humanity has created — a testament to our collective understanding that compassion is the basis to healing our suffering.
Roughly 160 days have passed in 2023, yet our nation has faced over 200 mass shootings. Think about that for a second — we are currently averaging more than one mass shooting a day in this nation. If more guns, more weapons and more violence were the appropriate responses to such a gruesome plague, the United States would have been the safest country on this planet a long, long time ago.
And I think many in this room would agree, then, that exhibiting compassion and care in the face of such atrocities is the epitome of strength. We can stand strong against this needlessly protracted suffering by simply learning how to better care for one another.
Because the COVID-19 pandemic unequivocally worsened our collective mental health — isolation, loneliness, job loss, financial instability, illness and grief have taken their toll. Today, 90 percent of American adults believe our country is facing a mental health crisis.
Though it may seem basic, a systemic foundation of compassion is desperately needed in order to physically and emotionally heal as a nation.
And we know that the educational system continues to experience significant disruptions — hundreds of thousands of students never returned to school. These young minds and lives are unaccounted for and tragically at-risk.
It’s incumbent upon us — many of whom lead the largest concentrated populations in the world — to leave a legacy of compassion. It is in our DNA. There is truly no argument against exuding compassion throughout our communities.
And now that we’ve discussed the “why” of CompassionateUSA, it’s time for the “what” — what next, what can we do, what should we do, to make our communities more caring — so here’s a glimpse of what San Antonio is gifting the U.S. Conference of Mayors: www.CompassionateUSA.org
At the interactive CompassionateUSA website, you will find free videos, micro-courses, tool kits and resources to share and implement this no-cost catalyst for change.
So now, I invite every one of you to join in this people-centered campaign. On behalf of our children and future generations of our nation, pledge today to become a CompassionateUSA Partner. Together, I’m confident that we possess the power to fundamentally and foundationally reshape the trajectory of our nation.
Thank you, fellow mayors, leaders and friends for choosing a better path for our communities.
For more information and utilization of CompassionateUSA, as well as to become a Partner and to see who all the CompassionateUSA Partners are, go to www.CompassionateUSA.org.
It is no secret that pharmaceutical companies are in the business of making money for their shareholders, and that they pour billions of dollars into clinical trials for new treatments for our patients. However, in the era of modern oncology, the goal of many companies’ pipelines is to develop targeted options that benefit a small fraction of patients whose tumors express targetable mutations. The emergence of targeted therapies, as well as the increasing prevalence of oral oncolytic treatments, lends an air of optimism for future patients. In the meantime, however, patients receiving treatment in the present are suffering for the lack of reliable supplies of backbone chemotherapy drugs, which have long been produced by suppliers of generic medications.
In February of 2023, Accord Healthcare announced delays in the production of cisplatin. Like many pharmaceutical companies that produce generic medications, Accord works with an overseas manu-

facturer — in this case, Intas Pharmaceuticals — and imports to the U.S. from India. An inspection of Intas’s plant in November of 2022 revealed multiple production problems, microbial contamination, lapses in record keeping, and a general lack of oversight that led to a “cascade of failure” by the FDA report.1 The report would be laughable if it wasn’t so horrifying.
First approved in 1978, cisplatin is widely used in the treatment of many cancers, alone and in combination with other chemotherapy drugs. There are malignancies for which cisplatin has no equivalent drugs that can be used in its stead. Accord is the largest domestic supplier of cisplatin, and these production delays created a cascade effect, increasing demand on the other four producers, who have not been able to keep up with the increased demand. Supply became critically limited over the following months, and national media outlets published articles relating the stories of affected patients. The FDA has
taken the unprecedented action of allowing the import of cisplatin from a Chinese manufacturer to increase supply.
Drug shortages are nothing new in medicine, often triggered by drug recalls and manufacturing issues. Rarely, though, do they reach the public conscience to the degree that the recent chemotherapy shortages issues have. Physicians and practices have responded by limiting use of cisplatin to treatment of malignancies for which there are limited choices (e.g., early stage bladder cancer and testicular cancer), and selecting non-cisplatin-containing regimens for other patients. The downstream effects have led to decreased availability of other drugs, such as carboplatin, 5-fluorouracil and capecitabine.

Also recently announced was a shortage of fludarabine, another chemotherapy agent widely used in the treatment of acute leukemia and stem cell transplant. As with cisplatin, a manufacturer announced the shortage, and physicians turned to other suppliers to make up the shortfall and began to consider options to make a short supply of critical medication stretch further. In many cases, this means restricting the use of drugs to patients who have no other possible regimens. While these other regimens are still highly effective, they often come with undesirable side effect profiles, longer chair times, or admission to the hospital for inpatient administration.
The simple explanation is the economics of the marketplace. Prices of generic drugs have seen a literal race to the bottom over the last decade, and with it, the profit margins for the companies that manufacture them have dramatically decreased. While improved access to low-cost generic medications is a thing to be celebrated in many cases, the loss of potential profit has led many companies to exit the generics marketplace. The companies that have stayed in have found ways to cut corners, and in several cases, one such cut corner is poor oversight of the overseas factories that supply both active pharmaceutical ingredients and finished product. The morality of profit for lifesaving medications is a discussion for another day, but the quality control issues that cause production delays and lead to dangerous supply issues cannot wait.
In a report by Anthony Sardella, a senior research advisor at Washington University in St. Louis, to the U.S. House Subcommittee on Oversight and investigations, he makes the obvious case for a return to generic manufacturing. He references the API Innovation Center in St. Louis, Missouri, a non-profit corporation, which is creating infrastructure and cooperation between academic institutions and drug manufacturers, with the goal of reintroducing the domestic manufacture of critical drugs.2 Encouraging reinvestment in the generic drug market will require creative solutions to ensure success. Consideration
of subsidies and tax breaks for participating companies may also go a long way towards encouraging renewed participation in the market.
The short-term solutions to the current shortages involve patient selection — creation of institutional policies that ensure that the patients receive these medications are those who will benefit the most from receiving them. In time, factories will pass inspections and reopen. In the meantime, the choices that we are required to make will, in many cases, almost certainly lead to poorer outcomes. Some patients will experience longer chair times. Some may require more aggressive side effect management or have poorer tolerance to alternate regimens. If we run out of life-saving medications, for which there are no other good options, some patients will die.
The time to lay the groundwork for the next cascade of chemotherapy drug shortages — of all drug shortages — is now. An aggressive focus on safe practices in overseas facilities is the “right now” solution. Engaging with local leaders and lawmakers on the local, state and national levels to encourage engagement and investment in the creation of safe domestic drug manufacturing is the way forward. As physicians, it is our responsibility to advocate solutions for our patients.
References:
1. FDA. (2022) U.S. Food and Drug Administration. Inspection Report, Intas Pharmaceuticals Limited. Available at: https://www.fda.gov/media/164602/download (Accessed: June 29, 2023)
2. Sardella, A. (2023) Memorandum drug supply chainsd1dth6e84htgma.cloudfront.net, Examining the Root Causes of Drug Shortages: Challenges in Pharmaceutical Drug Supply Chains. Available at: https://d1dth6e84htgma.cloudfront.net/ Oversight_Hearing_Memo_Drug_Shortages_5_11_23_ed33e75c 70.pdf?updated_at=2023-05-09T15%3A55%3A15.132Z (Accessed: June 29, 2023)

Iwas banging on the doors of the prison hospital staircase at 7:00 am, with three patients left to see. It was the first week of the new year and my first week back on service, diving headfirst into the Internal Medicine wards after a relaxing winter hiatus from medical school. One of my patients changed my perspective on healthcare. He had been incarcerated for over 25 years, and had developed uncontrolled hypertension, type 2 diabetes mellitus, and chronic kidney disease. The first morning I met him, I reviewed his chart on EPIC for a few minutes before entering his room and running through the usual rounding questions. When I asked about his stomach pain and rectal bleeding, he told me that it had been going on for nine months. I was skeptical that he had not been worked up by a physician until now. It turned out that his last admission for rectal bleeding had resolved before he got to the hospital, and he was quickly discharged back to his unit. It took many months for him to get transported and seen again by a physician.
Over time, I grew more empathetic for his situation. After being incarcerated for so long, he had limited knowledge of many things and a weak understanding of medical jargon. During his admission, he became newly diagnosed with colon cancer. When the attendings would discuss imaging results, next steps and consequences of his diagnosis, his face would always be blank and lost. He was very scared of surgery and wanted someone to explain to him step by step what would happen to resect the mass. I remember staff would get easily irritated when interacting with him due to his neverending questions while they were on a time crunch with dozens of patients. It was most evident when he refused to sign consent forms because he couldn't read and wanted someone besides the doctor to explain them to him. In most situations with patients, I feel helpless because there's no quick fix that I can offer them. However, I had the opportunity after rounds to chat with him thoroughly and answer some of his hesitations. He

better understood the risks and benefits of the surgery after I had explained it to him. Consequently, the residents were later able to obtain his consent without difficulty. I know his health problems won't disappear, but being able to reduce his anxiety about his situation and put him at ease made a noticeable difference in the following days when I would see him.
Social determinants of health, such as limited control over diet/medications, unforgiving living quarters, lack of education, and limited access to highly trained healthcare professionals, further exacerbate prisoners' health outcomes. A landmark research article by Massoglia et al. explored how low-income and minority individuals are more likely to be incarcerated, directly putting them in a position where they will have limited access to healthcare services. They point out that incarceration exacerbates existing health inequalities related to race and socioeconomic status.1 Addressing issues like this would require a root cause analysis and a multifaceted approach to reduce mass incarceration and provide more access to providers.
Providing healthcare to prisoners is a challenging situation that no one is prepared for until they do it. Prisoners often have multiple chronic conditions that are poorly managed, resulting in higher healthcare utilization and increased healthcare costs, but most importantly, poor outcomes. A common theme I have noticed is that many patients are marked as "nonadherent to medication" when in reality, a social issue had determined their poor health. I have heard all kinds of barriers to medical care, from transportation, money, insurance denials, pharmacy miscommunication, and clinicians forgetting to put in the refill order. A systematic review found that food insecurity, housing instability and social determinants overall were significantly (p<0.05) associated with lower medication adherence. 2 This highlights the need for physicians to further research health outcomes related to social determinants. We must avoid prescribing medications that prison patients can’t get in their unit pharmacy or that insurance companies will deny in the free world once they are released. It’s important to discuss these issues with care managers, which I have had multiple opportunities to do, and it has taught me a lot about the nonmedical work physicians must do.
Over time, I have come to realize that providing healthcare to prisoners requires a different approach than providing healthcare to the general population. The lack of resources, the high prevalence of chronic illnesses and limited access to care make it essential to prioritize advocacy, patient education and effective communication to ensure prisoners receive appropriate care. I have also come to appreciate the importance of multidisciplinary care teams in addressing the complex health needs of prisoners. Simple tasks, such as performing an Echocardiogram on a high-risk patient who required two guards at the door, proved to be difficult. This specific scenario I ex-
perienced ran for multiple days, with the Echo tech reporting each day that the guards were not available on time, and that other patients needed echos and could not wait. There is an endless list of systematic failures that lead to further decompensation in patient health across hospitals.
As I now work with more free-world patients in Internal Medicine, I am able to compare and contrast how there are different social determinants of health. My free-world patients are significantly more limited by money. Money can buy better education and thus health literacy, better medications, and stress-free visits to doctors without worrying about bills. It was difficult to think about prison patients' inability to read. A recent article discussed how health literacy is associated with various determinants of health, such as education, income, social disadvantage, and access to healthcare, which play a significant role in addressing health disparities. The article emphasizes the importance of interventions that improve health literacy and empower individuals and communities to take action on social and economic determinants of health. They stated that effective improvements in health literacy leads to better utilization of preventive services and medical adherence, and can positively impact behaviors that ultimately decrease disease burden.3
This experience taught me that healthcare providers need to be more aware of the social determinants of health affecting unique patient populations and the impact they have on their health outcomes. It has encouraged me as a future physician to be more considerate of the factors that have played into a patient’s health, and although I cannot change the past, I can do my best to mitigate future issues for them.
References:
1. Massoglia M, Pridemore WA. Incarceration and Health. Annu Rev Sociol. 2015 Aug;41:291-310. doi: 10.1146/annurev-soc-073014112326. PMID: 30197467; PMCID: PMC6124689
2. Wilder ME, Kulie P, Jensen C, Levett P, Blanchard J, Dominguez LW, Portela M, Srivastava A, Li Y, McCarthy ML. The Impact of Social Determinants of Health on Medication Adherence: a Systematic Review and Meta-analysis. J Gen Intern Med. 2021 May;36(5):1359-1370. doi: 10.1007/s11606-020-06447-0. Epub 2021 Jan 29. PMID: 33515188; PMCID: PMC8131473
3. Coughlin SS, Vernon M, Hatzigeorgiou C, George V. Health Literacy, Social Determinants of Health, and Disease Prevention and Control. J Environ Health Sci. 2020;6(1):3061. Epub 2020 Dec 16. PMID: 33604453; PMCID: PMC7889072
Sai Kamma is a 4th year medical student in Texas. He is interested in procedural medicine and is pursuing residency.

Much has been written about preventive measures that need to be instituted in patients diagnosed with peripheral arterial disease (PAD). These include antiplatelets agents, possible low dose rivaroxaban in some, statins as tolerated, proper glycemic control, blood pressure management, smoking cessation, a walking program, and possible vasodilator therapy, such as cilostazol for claudicants. A frequent afterthought has been to recommend “a proper diet,” although there is no stated agreement about what a proper diet should be.
There is abundant literature on dietary management in patients with cardiovascular disease, although not specifically as it relates to PAD. The literature is often confusing, with conflicting claims. This article will focus specifically on the Mediterranean diet and the use of alcohol, since these two subjects have been studied fairly well in relationship to PAD.
The Mediterranean diet is characterized by a high intake of fruit, vegetables, legumes, nuts and whole grains, a low intake of processed meat, a higher intake of fish, and a low consumption of dairy products except for fermented products such as yogurts. Total intake of lipids can be high, except those monounsaturated fats — such as those seen in olive oil — are predominant, as opposed to saturated lipids. A liberal use of olive oil is also characteristic of the Mediterranean diet. The PREDIMED trial was a primary prevention trial carried out in Spain, where the primary endpoint was MI, stroke and cardiovascular mortality. Participants randomized to a Mediterranean diet supplemented with four tablespoons of extra virgin olive oil per day had a hazard ratio of 0.69 of reaching the endpoint. Subsequent analyses did show the benefit of that diet in preventing both diabetes and PAD, and lowering the incidence of PAD in diabetic patients. The data has since been replicated in studies carried out outside of the Mediterranean Sea basin. In part, the benefits of olive oil are believed to be related to the anti-inflammatory effects of polyphenols present in the oil.
Beyond the Mediterranean diet, higher intakes of vitamin C, E and fiber were associated with decreased risk of PAD (Edinburgh Artery Study), likely as a result of the antioxidant nature of these factors. The American Heart Association guidelines call for dietary fibers of 25-30 grams per day, limiting sodium intake to less than 2 grams per day, and avoiding highly processed foods. Food processing adds sodium to foods, in addition to polysaturated fats and extra carbohydrates. A low to no carbohydrate diet (so called keto) has not been specifically studied with regards to PAD.
Interestingly enough, the AHA website recommends a diet with “preferably no alcohol.” Heavy drinking is unquestionably linked to adverse health effects such as cirrhosis, hypertension and cardiomyopathy, to name a few. However, moderate alcohol consumption is actually as-
sociated with a decreased prevalence of coronary heart disease and peripheral arterial disease. The Mediterranean diet usually allows for some light alcohol intake. In the Physicians Health Study, individuals who consumed one drink per day had a relative risk for PAD of 0.68 after adjusting for other potential confounding factors. A drink is usually defined as 1.5 ounces of liquor, 5 ounces of wine or 12 ounces of beer. The benefits are most obvious in middle aged individuals with cardiovascular risk factors. The benefits are believed to be related to favorable effects of alcohol on lipid profiles (increased HDL), coagulation parameters (lower fibrinogen and vWF), a decrease in CRP, and a reduction of insulin resistance. The type of alcohol seems to be of relevance in this regard. Red wine appears to offer more protective effects than other types of alcohol. A meta-analysis of 13 studies reported that red wine intake decreased vascular disease by 32 percent, as opposed to only 22 percent for beer. The benefits of red wine are related to its flavonoid contents. Flavonoids increase nitric oxide production, decrease expression of adhesion molecules on the endothelium, decrease LDL oxidation, and decrease platelets aggregation, all of which leads to decreased inflammation and atherogenesis.
In summary, moderation in all aspects of dietary management seems to be the key in helping prevent PAD, including alcohol usage. Learn more about this condition with educational articles and videos provided by the board-certified, highly specialized surgeons who make up our team at Peripheral Vascular Associates (PVA). We offer these resources on our website at PVAsatx.com as a way of raising awareness within our community.
References:
Estruch R, Ros E, Salas-Salvado J et al. Primary prevention of cardiovascular disease with a Mediterranean diet supplemented with extra virgin olive oil or nuts. NEJM 2018; 378:e34
Ciccarone E, Di Castelnuovo A, Salcuni M et al. A high score Mediterranean dietary pattern is associated with a reduced risk of peripheral arterial disease in Italian patients with type 2 diabetes. J. Thrombosis Hemostasis. 2003; 1: 1744
Camargo CA, Stampfer M, Glynn R et al. Prospective study of moderate alcohol consumption and risk of peripheral arterial disease in US male physicians. Circulation 1997; 95(3): 577
Szmitko PE, Verma S. Anti-atherogenic potential of red wine: clinician update. Am. J. alry aPhysiol. 2005; 288(5): H2023
Boulos Toursarkissian, MD, is a vascular surgeon and endovascular specialist at Peripheral Vascular Associates (PVA). He is a member of the Bexar County Medical Society (BCMS) and adjunct Professor of Surgery at the UT Health Sciences Center.


 By Andrew Ta
By Andrew Ta
In 2008, a group of ambitious medical students at The University of Texas Health San Antonio (UTHSA) Long School of Medicine collaborated to create Connective Tissue, the school’s literature and arts journal. It started out as short and succinct, spanning only 26 pieces with no unifying theme. Fifteen years later, after scores of editorial boards passed through, positively contributing to and constantly updating the journal, Connective Tissue has evolved to become the vibrant and full journal it is today with more than 200 submissions for 50 selected pieces. The medical humanities play a central role in healthcare, and Connective Tissue is an outlet for this within the San Antonio community.
Medicine, at its core, stems from human connection. Patients enter a social contract in which they must be vulnerable and share personal and intimate details of their lives with their healthcare provider, and trust that they will receive the help they need, whether in the form of new medications, therapies or surgeries. For many people in healthcare, it is this human connection and the opportunity to create a lasting, positive impact on patients that draw us to medicine.
This holds true for many of the staff at the Charles E. Cheever Jr. Center for Medical Humanities & Ethics (CMHE) at UTHSA who run Connective Tissue. Dr. Kristy Kosub, who has worked with Connective Tissue since 2016 and has been pivotal in expanding the scope of the journal, says that “when you are [with a patient], you realize stories are embedded within medicine, and an HPI (History of Present Illness) is not just a list of medical symptoms but also the life of the patient behind [them].”
Indeed, patients must be vulnerable with and trust their provider for effective care. This openness, however, is often unilateral and unrequited. Physicians do not have the same obligation; they are not required to be vulnerable with their patients to do their job well, yet they are privy to the details of their patient’s personal life. A physician can spend their entire lives listening to and supporting their patients, but patients do not have the same privilege of hearing the personal lives of their physician, leading to a disconnect and otherness from the patients they serve.
Connective Tissue (and similar literary journals) help bridge this gap, serving as an outlet and forum for writing and visual arts within
Carreta Tica School of Medicine,healthcare. The journal has expanded to include visual arts, photography, 55-word stories and literature submissions to showcase the diverse talents of our broad medical community and foster inclusivity. Pieces range from an idyllic photo of Zion Canyon to a poem about refugee families to a reflection from anatomy lab. This open creativity is what drives Connective Tissue — it is a place where, even if you do not have extensive art experience, you still have the opportunity to put work out to be noticed and celebrated. It is a forum for us as healthcare workers, for once, to be vulnerable and open with the people we serve, no matter how much experience or talent we have, and help to mitigate the disconnect between physicians and patients.
The audience is not limited to those outside of medicine, however. Importantly, other students, physicians and healthcare workers also have access to Connective Tissue. Dr. Rachel Pearson, a pediatrician and assistant professor in the CMHE, argues that “a lot of premed and medical students are taught to accept knowledge as fact and to apply it, but the medical humanities … facilitate critical thought about the profession within society … and make space for us as trainees to actively think about and reimagine our work.” When creating and reading the works
Artist’s Note: I took this photo as I was nearing the end of a 24-hour shift and waiting for an incoming critical patient. As I stood on the landing deck with the sun about to rise, I found myself thinking that this was the calm before the storm. (This photograph won Honorable Mention in Photography in the 2023 Connective Tissue journal.)

of people who share the same experiences as us, we are forced to reflect, examine and reinvent the ideas pervading our practice of medicine. By sharing these insights, we create solidarity amongst students and professionals who share similar educational experiences. Our lives do not exist in isolation, and there is a community of scholars who relate to the nuanced struggles of medicine and can support us.
On a personal level, I hope that readers who pick up copies of Connective Tissue are as amazed as I am to see how talented and creative the people around us are. Without a doubt, the students around us are brilliant and will become excellent physicians. I did not know, however, that we could also be so insightful and reflective, raw and vulnerable, and understand the uncomfortable realities of medicine.
continued from page 31

It is a privilege to be able to read and appreciate these perspectives, and I am glad there is an outlet for this in San Antonio.


At the end of our interview, Dr. Pearson endorsed the medical humanities by stating, “Medicine creates an incredible place for hearing and honoring stories that theoretically anyone can access.” Connective Tissue creates this space within our community to nurture empathy and humanitarian values in all of our healthcare workers and enhance the vision of the CMHE to "prepare tomorrow's healers to act with compassion and justice."

Andrew Ta is medical student at the Long School of Medicine, Class of 2026. He is the 2023 Student-Faculty Collaborative Practice President overseeing the six student-run free clinics and is the 2023-2024 writing lead for Connective Tissue, the school's literature and arts journal. Andrew is also a member of the BCMS Publications Committee.

As a former contact tracer during the initial months of the COVID-19 pandemic, I have had countless conversations with people who tested positive for the virus. Most of these conversations followed a similar course and blend together, but one in particular left me feeling especially drained and frustrated.
The call began like any other, with routine questions about symptoms, potential exposures, and the need to isolate from others; however, as the conversation continued, it became clear that the woman on the other end of the line was not taking the virus seriously at all. She laughed off my questions and dismissed my concerns, telling me that the virus was a conspiracy and the media was grossly exaggerating the dangers.
This was my first interaction with a COVID-19 conspiracy theorist, and I was flabbergasted by the words I was hearing. I tried to elucidate the severity of the situation and convey the importance of taking precautions to prevent the spread of the virus, but she continued to brush me off. She told me she had gone to a wild party with friends the night before she started feeling symptoms, and she had no intention of canceling her plans for the coming weekend.
I was stunned by her attitude. It was clear she was not taking our conversation seriously and was putting herself and others at risk. I remained calm and professional but decided a blunt approach was necessary to get through to her. I told her that her behavior was reckless and that she was endangering the lives of others.
To my shock, she began to cry. She told me she had been grappling with the isolation of quarantine, and she felt like the virus had taken everything from her. She had lost her job, her friends and her sense of purpose, and she did not know how to cope. She said she felt like the virus was a punishment for something she had done wrong, and she didn't see the point in trying to protect herself or others.
My heart shattered as I listened to her story. It was clear she was struggling with more than just the virus — she was battling fear, isolation and despair, all of which were compounded by conflicting information she had been receiving since the start of the pandemic. I realized my anger and frustration had been misplaced, and what she needed was empathy and understanding.
I took a deep breath and tried to connect with her on a more personal level. I shared my own struggles with the pandemic, and I told her that I empathized with how difficult it could be to stay positive in the face of so much uncertainty. I tried to reassure her that there was hope, and by taking precautions, she could help protect herself and others.
To my relief, she seemed to respond to my words. She calmed down and began to share more information with me about her potential exposures. She even agreed to cancel her plans for the weekend, and to stay at home until her symptoms subsided and her isolation period ended.
As we wrapped up the call, I felt a swirl of emotions. On one hand, I was grateful I had been able to connect with her and to help her see the importance of taking precautions. On the other hand, I was frustrated by the misinformation and fear that had led her to doubt the severity of the virus.
Now, as a medical student, I occasionally reflect back on that conversation and the power of empathy and understanding in the healthcare setting. It reminds me that every person has their own struggles and fears, and our role is to provide support and guidance, even in the face of resistance.

 Rajeev Pathapati is a medical student at the Long School of Medicine, Class of 2025.
Rajeev Pathapati is a medical student at the Long School of Medicine, Class of 2025.

When scaling your medical practice, it’s important to consider these 10 factors to ensure the growth and sustainability of your practice.
1. Paint a holistic picture: Should you scale? If so, how and why? Answer the following about your goals for the future of your practice:
• Vision and mission statements
• Corporate values (company culture)
• Goals and objectives
• Development strategies
• Marketing (research, competitive analysis, marketing, and sales plan)
2. Develop a comprehensive financial plan: Outline your financial goals, projected revenues, expenses and investment requirements. This serves as a roadmap for your practice's growth, aiding in informed decision-making, setting realistic goals and measuring performance as you scale.
3. Analyze profitability: Evaluate key financial metrics such as revenue per patient, average revenue per procedure and gross margin. Identify areas where you can optimize revenue and reduce costs.
4. Evaluate funding options: Determine how you will finance your practice’s expansion by exploring options such as bank loans (including Small Business Administration – [SBA]), lines of credit, angel investors and venture capital. Consider the terms, interest rates, and repayment schedules associated with each option and incorporate into your financial plan.
5. Efficient billing and revenue cycle management: Implement streamlined billing processes to ensure timely and accurate collections. Consider outsourcing billing services if necessary. Optimize your revenue cycle management to minimize claim denials and optimize cash flows.
6. Scalable cost structure: Identify where you can streamline operations and reduce expenses. Implement cost-saving measures such as negotiating better pricing with suppliers, optimizing inventory management and implementing energy-efficient practices.
7. Staffing and human resources: As your practice grows, assess your staffing needs and hiring requirements. Consider the cost of adding new team members and ensure you have recruitment and training processes in place. Evaluate the benefits and risks associated with hiring additional staff versus outsourcing certain services.
8. Insurance coverage and risk management: Review your insurance policies to ensure they provide adequate coverage as your practice expands. Assess potential risk and implement risk management strategies to protect your practice and mitigate financial liabilities.
9. Technology and infrastructure investments: Determine the technological infrastructure required to support the scaling of your practice. Consider investments in electronic medical records (EMR) systems, patient management software, telemedicine capabilities and other digital tools that can enhance efficiency, patient experience, and can help to protect your practice from fraud attempts.
10. Compliance and regulatory considerations: Ensure your practice remains compliant with relevant healthcare regulations and industry standards. Stay current with changes in billing and coding requirements, data security regulations and other legal obligations to avoid potential penalties and financial risks.
As you grow, it’s advantageous to consult with financial professionals, such as accountants or financial advisors, who specialize in the healthcare industry to gain tailored advice for your growth goals.
Maria Breen, Executive Vice President, Private Banking Manager at Texas Partners Bank is a financial expert who uses her over 30 years of financial services experience to help her clients build the lives and legacies they envision. She is also the director at large for San Antonio Medical Group Management Association (SAMGMA) and committee co-lead for Impact SA. With a deep-rooted love for serving others, Maria sees private banking as an extension of her passion for taking care of people in her community.
The mission of the Bexar County Medical Society (BCMS) is to serve and represent the member physicians of Bexar County in providing quality healthcare for their patients and the public. Membership is limited to the physicians of Bexar County, and as such, verification of credentials is done for every new member.

Prior to 1981, BCMS verified the credentials of new members through an arrangement with the Travis County Medical Society. On July 7th, the BCMS Board of Directors carried the motion to create a Central Credentialing Program, meaning that the BCMS Membership department would do new member credentials verification in-house.
Over the next few years, various hospitals expressed interest in credentials verification services. On April 5, 1984, the BCMS Board of Directors approved the formation of the BCMS Central Verification Program (BCMS CVP). Services were expanded to include full initial appointment and reappointment primary source verifications. The Nix, Southwest General, Oaks Psychiatric Health System and San Marcos Treatment Center were some of the first to sign contracts.
BCMS CVP grew very quickly, and the decision was made to create a separate corporation. Bexar Credentials Verification, Inc. (BCVI) is a for-profit corporation founded on September 28, 1998. The original formation agreement was between Bexar County Medical Society Management Holding Company, Inc., a Texas corporation (MHI), Texas Medical Association Health Care Liability Claim Trust, d/b/a/ Texas Medical Liability Trust, a Texas insurance association (TMLT), and FPIC Services, Inc., a Florida corporation (FPIC).
The BCVI founder and president, Robert “Bob” Needs, had a vision that BCVI would become a nationwide Credentials Verification Organization (CVO). He was a man of great passion and hope. His excitement was contagious and encouraging. Sadly, he passed away on May 12, 1999. His unexpected death sent the company into a rapid downward spiral. Up until that point, the investors had been
kept in the dark regarding the financial state of the company. BCVI was operating in the red – deep, dark red. Panic ensued, major changes were made, the staff was drastically cut, consultants were brought in, and BCVI was in a fragile place.
Honestly, the choice for the Board of Directors was obvious to me – shut it down. For many of us, closure seemed inevitable. It took a while for me to realize that the Bexar County Medical Society (BCMS) had a level of commitment to BCVI that was beyond my comprehension. Failure was not an option. At great expense, BCMS patiently covered and guided us. During the next three years, BCVI remained in the red.
In 2003, the Board of Directors for BCMS hired a new Chief Executive Officer, Stephen “Steve” C. Fitzer. He was a leader like I had never experienced. For the first time in its life, BCVI became a profitable company with a good reputation. Steve rehired the former Director of Operations for BCVI, Mary Jo Quinn, who became the voice and face of BCVI. Sure, it takes a whole team to make a company successful, but there are certain people that make it all happen.
Steve and Mary Jo have since retired, but their impact on the company is without measure. The obvious choice to replace Steve was Melody Newsom, a twenty-year veteran of BCMS, who shares the same leadership style, and Mary Jo’s shoes were filled by Betty Fernandez, who is incredibly gifted in leadership and customer service. I guess prayers really do get answered.
Kris King is the Director of Software Services for Bexar Credentials Verification, Inc. He has been with the company since March, 1999.

Betty Fernandez is the Director of Operations for Bexar Credentials Verification, inc. She was a Credentialing Specialist for the company for 11 years, and February 2024 will mark her three-year anniversary in management.

On Friday, September 22, 2023, the Bexar County Medical Society (BCMS) hosted a Press Conference in celebration of our 170th anniversary. Established in September of 1853, BCMS is the oldest county medical society in Texas and the first to be organized under the State Medical Association of Texas. The Society seeks to promote high standards of medical care in the community, advocating on behalf of physicians and patients while providing beneficial services to its physician members.
Bexar County Medical Society President-ElectDr. Zeke Silva’s opening remarks:
It is my honor to share and celebrate the rich history and enduring legacy of the Bexar County Medical Society, a foundational pillar of medical excellence in Texas.
January 1853: In a historic assembly of 48 visionary physicians in Austin, the Texas State Medical Association was formed. By September of that same year, the Bexar Medical Society was chartered, becoming the first component medical society in our state. The Society underwent name changes, from the Western Texas Medical Association to the West Texas Medical Association, finally settling on its present name in 1903.
As the oldest county medical society in Texas, our legacy and leadership run deep. Among the notable figures in our history, Dr. George Cupples stands out. He had the unique distinction of being the first president of both BCMS and the Texas Medical Association. Dr. Cupples, along with Drs. Lyons, Howard, Scholmann, Herff, Giddings, Hoffman, Schaffter and Weisselberg were the pioneering founders of BCMS.
Since its inception, 126 presidents have helmed its leadership, including, in the past 20 years, the first three female physician presidents leading BCMS.
BCMS is not just the third-largest county medical society in Texas but the eighth-largest in the entire nation, with about 5,800 members. A con-


nection that's worth noting is that all 120 county medical societies in Texas maintain a joint membership with the Texas Medical Association (TMA).

The TMA stands proud as the nation's largest state medical association, with over 55,000 members. BCMS members span all recognized medical specialties and include MDs, DOs, military physicians, fellows, residents and medical students.

Over the decades, BCMS had various office locations. In 1919 its first official site was at North St. Mary’s St. and Lexington Ave. By 1933, a permanent spot was secured at 202 W. French Place. In 2015, our new stateof-the-art building was erected in Shavano Park, winning the "Project of the Year" award from the American Subcontractors Association.
BCMS has been a steward of medical history. Our Rare Books Library was generously donated to the University of Texas Health Science Center Medical School in 1970. The collection now resides in the special P.I. Nixon Medical Historical Library’s History of Medicine Room, which, by the way, is fireproof. Furthermore, our current offices house an impressive collection of antique medical equipment, furniture, books and journals — all testament to our rich heritage.
In conclusion, the Bexar County Medical Society isn’t just about numbers and names; it's about the unwavering commitment to medical excellence, patient advocacy and a deep-rooted connection to our community. As we remember our past, we're filled with hope and ambition for a healthier future for all Texans. Thank you. continued on page



EVENT continued from page 37








BCMS has reestablished the retired physician group, which has been named “The 1853 Club” (BCMS was originally founded in 1853). Other than opportunities for collegiality, guest lectures on topics of interest are being planned. The 1853 Club is planning to meet quarterly for lunch or other events. The group will also act as a senior advisory resource to offer opinions as requested by the BCMS Board of Directors or a BCMS committee(s). The 1853 Club will also serve as mentors for young physicians.

The first luncheon was held on July 11, 2023, at the BCMS head

quarters. TMA Immediate Past President Gary Floyd, MD, was our guest speaker and talked about a broad range of legislation that passed or didn’t during the 2023 legislative session.


The next luncheon for The 1853 Club will take place on October 10, 2023, at 11:30 a.m. at the BCMS headquarters. Spouses or guests are welcome to join us!
If you are interested in receiving information about this and other 1853 Club events, please call the BCMS Membership Department at 210-301-4371 or email membership@bcms.org.


We encourage you to use our supporting vendors whenever you or your practice needs supplies or services.
Sol Schwartz & Associates P.C. (HHH Gold Sponsor)
Sol Schwartz & Associates is the premier accounting firm for San Antonio-area medical practices and specializes in helping physicians and their management teams maximize their financial effectiveness.
Jim Rice, CPA 210-384-8000, ext. 112 jprice@ssacpa.com www.ssacpa.com
“Dedicated to working with physicians and physician groups.”
Kreager Mitchell (HHH Gold Sponsor)
At Kreager Mitchell, our healthcare practice works with physicians to offer the best representation possible in providing industry specific solutions. From business transactions to physician contracts, our team can help you in making the right decision for your practice.
Michael L. Kreager 210-283-6227
mkreager@kreagermitchell.com
Bruce M. Mitchell 210-283-6228
bmitchell@kreagermitchell.com www.kreagermitchell.com
“Client-centered legal counsel with integrity and inspired solutions”
BANKING Broadway Bank (HHH Gold Sponsor)
Healthcare banking experts with a private banking team committed to supporting the medical community.
Thomas M. Duran
SVP, Private Banking Team Lead 210-283-6640
TDuran@Broadway.Bank
www.broadwaybank.com

“We’re here for good.”
Synergy FCU Member Services
210-750-8333 info@synergyfcu.org www.synergyfcu.org
“Once a member, always a member. Join today!”
Betty Fernandez Director of Operations
210-582-6355
Betty.Fernandez@bexarcv.com
www.BexarCV.com
“Proudly serving the medical community since 1998”
Genics Laboratories (HHH Gold Sponsor)

Genics Laboratories offers accurate, comprehensive and reliable results to our partners and patients. Genics Laboratories is committed to continuous research, ensuring our protocols are always at the peak of current technology.
The Bank of San Antonio (HHH Gold Sponsor)

We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Brandi Vitier
210-807-5581
brandi.vitier@thebankofsa.com www.thebankofsa.com
Amegy Bank of Texas (HH Silver Sponsor)
We believe that any great relationship starts with five core values: Attention, Accountability, Appreciation, Adaptability and Attainability. We work hard and together with our clients to accomplish great things.
Robert Lindley
SVP | Private Banking Team Lead 210-343-4526
Robert.Lindley@amegybank.com
Denise Smith
Vice President | Private Banking
Yulia Leontieva Managing Partner, Physician Liaison
210-503-0003 yulia@genicslabs.com
Kevin Setanyan Managing Partner
210-503-0003 kevin@genicslabs.com
Artyom Vardapetyan Managing Partner
210-503-0003 www.genicslabs.com
“Accurate results in record time.”
Livingston Med Lab (HH Silver Sponsor)
High Complexity Clia/Cola accredited Laboratory providing White Glove Customer Service. We offer a Full Diagnostic Test Menu in the fields of Hematology, Chemistry, Endocrinology, Toxicology, Infectious Disease, & Genetics. Robert Castaneda (CEO) 210-316-1792
Robert@livingstonmedlab.com www.livingstonmedlab.com/home
Oakwell Private Wealth Management (HHH Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Elizabeth Olney with Edward Jones (HH Silver Sponsor)
We learn your individual needs so we can develop a strategy to help you achieve your financial goals. Join the nearly 7 million investors who know. Contact me to develop an investment strategy that makes sense for you.
Elizabeth Olney Financial Advisor 210-858-5880
Elizabeth.olney@edwardjones.com
www.edwardjones.com/elizabeth-olney "Making Sense of Investing"
Aspect Wealth Management (★★★ Gold Sponsor)


We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
210-343-4502
Denise.C.Smith@amegybank.com
Scott Gonzales
Assistant Vice President | Private Banking
210-343-4494
Scott.Gonzales@amegybank.com www.amegybank.com
“Community banking partnership”
Synergy Federal Credit Union (HH Silver Sponsor)
Looking for low loan rates for mortgages and vehicles? We've got them for you. We provide a full suite of digital and traditional financial products, designed to help Physicians get the banking services they need.
“Trusted Innovative, Accurate, and STAT Medical Diagnostics”
Bexar Credentials Verification, Inc. (HHHH 10K Platinum Sponsor)
Bexar Credentials Verification Inc. provides primary source verification of credentials data that meets The Joint Commission (TJC) and the National Committee for Quality Assurance (NCQA) standards for health care entities.

Aspect Wealth Management (HHH Gold Sponsor)
We believe wealth is more than money, which is why we improve and simplify the lives of our clients, granting them greater satisfaction, confidence and freedom to achieve more in life.
Michael Clark, President 210-268-1520
mclark@aspectwealth.com
www.aspectwealth.com
“Get what you deserve … maximize your Social Security benefit!”
Conviva Care Center (HHH Gold Sponsor)

Conviva’s value-based care model allows physicians to deliver high quality, personalized care and achieve better outcomes, while feeling free to focus on health equity and patient outcomes.
Kim Gary
Senior Physician Recruiter
812-272-9838
KGary4@humana.com
www.ConvivaCareers.com
“Fuel Your Passion & Find Your Purpose”
HOSPITALS/ HEALTHCARE FACILITIES
Luis Chapa
MD/CEO
210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/ “An Unparalleled Scribe Experience”
INSURANCE
TMA Insurance Trust (HHHH 10K Platinum Sponsor)
TMA Insurance Trust is a full-service insurance agency offering a full line of products – some with exclusive member discounts and staffed by professional advisors with years of experience. Call today for a complimentary insurance review. It will be our privilege to serve you.

Wendell England Director of Member Benefits
512-370-1776
wendell.england@tmait.org
800-880-8181
www.tmait.org
“We offer BCMS members a free insurance portfolio review.”
MedPro Group (HH Silver Sponsor)
Rated A++ by A.M. Best, MedPro Group has been offering customized insurance, claims and risk solutions to the healthcare community since 1899. Visit MedPro to learn more.
Kirsten Baze, RPLU, ARM AVP Market Manager, SW Division
512-658-0262
Fax: 844-293-6355
Kirsten.Baze@medpro.com www.medpro.com
Henry Schein Medical (HH Silver Sponsor)
From alcohol pads and bandages to EKGs and ultrasounds, we are the largest worldwide distributor of medical supplies, equipment, vaccines and pharmaceuticals serving office-based practitioners in 20 countries. Recognized as one of the world’s most ethical companies by Ethisphere.
Tom Rosol
210-413-8079
tom.rosol@henryschein.com
www.henryschein.com
“BCMS members receive GPO discounts of 15 to 50 percent.”
UT Health San Antonio MD
Anderson Cancer Center (HHH Gold Sponsor)
UT Health provides our region with the most comprehensive care through expert, compassionate providers treating patients in more than 140 medical specialties at locations throughout San Antonio and the Hill Country.
UT Health San Antonio Physicians
Regina Delgado Business Development Manager
210-450-3713
delgador4@uthscsa.edu
UT Health San Antonio MD
Anderson Mays Cancer Center
Laura Kouba
Business Development Manager
210-265-7662
norriskouba@uthscsa.edu
https://uthscsa.edu/
Appointments: 210-450-1000
UT Health San Antonio

7979 Wurzbach Road
San Antonio, TX 78229
SERVICES Provider's Choice Scribe Services (HHH Gold Sponsor)
Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar
COOyaguilar@pcscribes.com
915-691-9178
Texas Medical Liability Trust
(HHHH 10K Platinum Sponsor)
With more than 20,000 healthcare professionals in its care, Texas Medical Liability Trust (TMLT) provides malpractice insurance and related products to physicians. Our purpose is to make a positive impact on the quality of healthcare for patients by educating, protecting, and defending physicians.

Patty Spann
512-425-5932
patty-spann@tmlt.org
www.tmlt.org
Recommended partner of the Bexar County Medical Society

Alamo Capital Advisors LLC

(
★★★★ 10K Platinum Sponsor)
Alamo Capital Advisors is focused on Sourcing, Capitalizing, and Executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new development acquisitions and sales, lease representation and financial (RE)-structuring for existing investments.
Jon Wiegand, Principal 210-241-2036
jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
MEDICAL BILLING AND COLLECTIONS SERVICES
Wave Online (★★★ Gold Sponsor)
Professional Analysis focusing on Low Collections, High Denials Rates. Our Business Intelligence tools will identify Cash Pockets and Cash Leakages. With a 360degree view on your practices’ financials, we can tune your AR for best performance. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations 726-228-1097
saranraj@wavemt.com
https://rcmwave.com/ “Innovation towards Solutions”
The Bank of San Antonio Insurance Group, Inc.

(HHH Gold Sponsor)
We specialize in insurance and banking products for physician groups and individual physicians. Our local insurance professionals are some of the few agents in the state who specialize in medical malpractice and all lines of insurance for the medical community.
Katy Brooks, CIC 210-807-5593
katy.brooks@bosainsurance.com www.thebankofsa.com
“Serving the medical community.”
Wave Online (★★★ Gold Sponsor)


Our team of professionals will act as your extended AR office enhancing your revenue through our proprietary metrics and claim management systems. In addition, you keep 100% control of your RCM. Contact us today for a no cost evaluation.
Saranraj (Raj) Venkatesh
Vice President – RCM | Sales and Client Relations
726-228-1097 saranraj@wavemt.com https://rcmwave.com/ “Innovation towards Solutions”
Commercial & Medical Credit Services (HH Silver Sponsor)
A bonded and fully insured San Antonio-based collection agency.
Henry Miranda 210-340-9515
hcmiranda@sbcglobal.net www.cmcs-sa.com
“Make us the solution for your account receivables.”
Healthcare Leaders of San Antonio (HH Silver Sponsor)
We are dedicated to nurturing business connections and professional relationships, exchanging knowledge to enhance leadership, and creating career opportunities for healthcare and other industry leaders in a supportive community.
David Neathery President 210-797-8412
healthcareleaderssa@gmail.com
Gary Meyn, LFACHE Vice President 210-912-0120
gmeyn@vestedbb.com
https://healthcareleaderssa.com/ “Come, Learn, Connect!”
The Health Cell (HH Silver Sponsor)
“Our Focus is People” Our mission is to support the people who propel the healthcare and bioscience industry in San Antonio. Industry, academia, military, nonprofit, R&D, healthcare delivery, professional services and more!
Kevin Barber President
210-308-7907 (Direct) kbarber@bdo.com
Valerie Rogler Program Coordinator
210-904-5404
Valerie@thehealthcell.org www.thehealthcell.org
“Where San Antonio’s Healthcare Leaders Meet”
San Antonio Medical Group Management Association (SAMGMA) (HH Silver Sponsor)
SAMGMA is a professional nonprofit association with a mission to provide educational programs and networking opportunities to medical practice managers and support charitable fundraising.
Lindsey Herman Nolan, MHR, CMPE President info4@samgma.org www.samgma.org
Oakwell Private Wealth Management (★★★ Gold Sponsor)
Oakwell Private Wealth Management is an independent financial advisory firm with a proven track record of providing tailored financial planning and wealth management services to those within the medical community.
Brian T. Boswell, CFP®, QKA Senior Private Wealth Advisor 512-649-8113
SERVICE@OAKWELLPWM.COM
www.oakwellpwm.com
“More Than Just Your Advisor, We're Your Wealth Management Partner”
Provider's Choice Scribe Services (★★★ Gold Sponsor)

Our accurate and complete documentation helps our customers focus on what’s most important, their patients. Let us take on the task of documenting your patient encounters, it’s what we do.
Yoceline Aguilar COO
yaguilar@pcscribes.com
915-691-9178
Luis Chapa MD/CEO 210-796-4547
lchapa@pcscribes.com
www.providerschoicess.com/ “An Unparalleled Scribe Experience”
Alamo Capital Advisors LLC

(★★★★ 10K Platinum Sponsor)
Alamo Capital Advisors is focused on Sourcing, Capitalizing, and Executing investment and development opportunities for our investment partners and providing thoughtful solutions to our advisory clients. Current projects include new development acquisitions and sales, lease representation and financial (RE)-structuring for existing investments.
Jon Wiegand Principal 210-241-2036
jw@alamocapitaladvisors.com www.alamocapitaladvisors.com
Favorite Healthcare Staffing (HHHH 10K Platinum Sponsor) Serving the Texas healthcare community since 1981, Favorite Healthcare Staffing is proud to be the exclusive provider of staffing services for the BCMS. In addition to traditional staffing solutions, Favorite offers a comprehensive range of staffing services to help members improve cost control, increase efficiency and protect their revenue cycle.
Cindy M. VidrineDirector of Operations- Texas 210-918-8737
cvidrine@favoritestaffing.com
“Favorite Healthcare Staffing offers preferred pricing for BCMS members.”


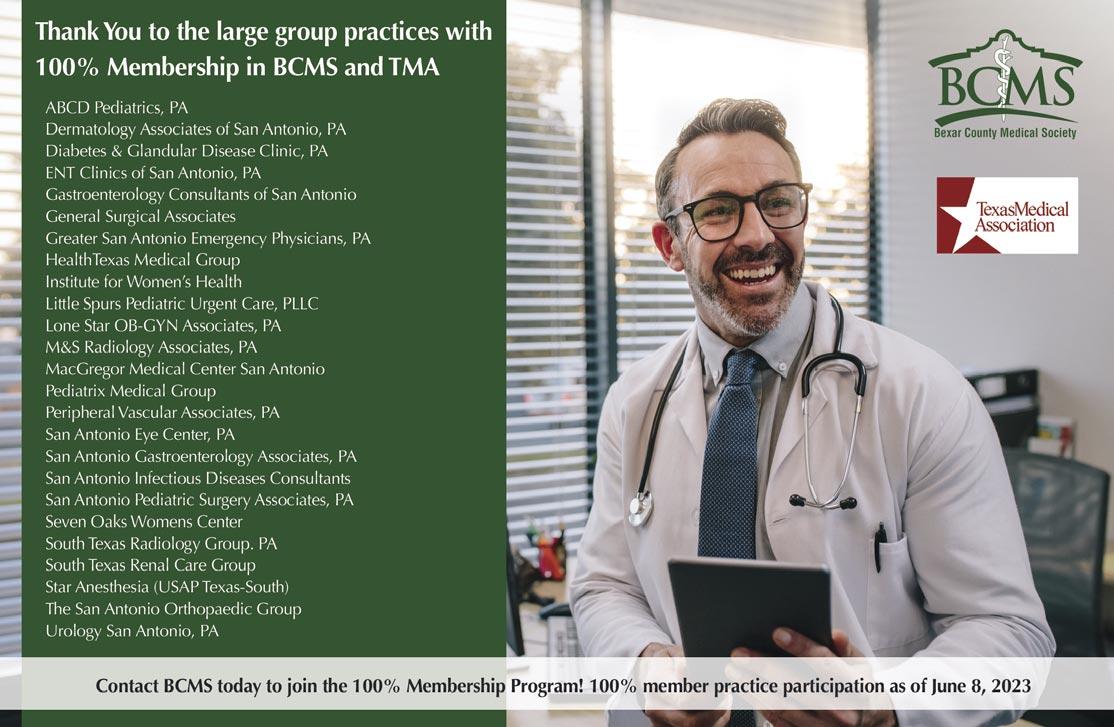




 By Stephen Schutz, MD
By Stephen Schutz, MD
In 1968, Porsche introduced a T, or “Touring,” version of their popular 911 in an effort to appeal to enthusiasts who wanted 911 goodness but couldn’t afford the more expensive versions. The 911T wasn’t a big hit, but it did reasonably well and helped the company grow and evolve. Interestingly, it wasn’t until 50 years later in 2018 that Porsche released a second 911T, this time based on the 991.2 Carrera platform.
Like the 1968 version, the 991.2 911T “remix” wasn’t a sensation but neither did it bomb, so it was no surprise that Porsche released a new 992-based Carrera T in late 2022.
For the record, the 992-gen Carrera T is a base model 911 with a 7speed manual transmission combined with the Sports Chrono Package, mechanical limited-slip differential, thinner glass and rear seat delete to save weight, and Porsche's PASM active suspension system with sport-tuned dampers. There are other add-ons, but that’s mostly it.
The base Carrera comes with a 379-HP twin-turbocharged 3.0liter flat-six engine paired with an eight-speed PDK automatic transmission, whereas the more expensive Carrera S increases output to 443-HP and can be ordered with Porsche's 7-speed manual. The Carrera T couples the lower horsepower version of the flat-six with the 7-speed manual, which is a good thing. You can buy a Carrera T with the PDK, but doing so negates some of the T's weight savings. Plus, it’s completely lame.
Since exterior clues are minimal, it would take a true Porsche “fanboi” to spot a Carrera T in the wild. It sits slightly lower than other Carreras, has (deletable) graphics on the lower door panels, and adds the cool smoked wheels, which I love.
Inside, charcoal cloth seats with nice pinstriping are the first things you notice, but the absence of the rear seats also grabs your attention. Fortunately, the shelf left once those seats are gone can comfortably house numerous pieces of luggage. (If you prefer, the rear seats can be retained at no cost.)
The optional “Interior” package adds some pizazz inside via seatbelt coloring and embroidered logos on the headrests and floor mats in your choice of Slate Gray or Lizard Green. Leather trim for the doors and dashboard is also available, as are 18-way power-adjustable seats. Porsche's carbon-fiber racing-style bucket seats, typically GT-modelonly fare, can also be selected. While it’s nice that Carrera T customers can choose the perfect-for-track-day carbon fiber seats unavailable in other non-GT 911s, I’d go with the 18-way seats. They’re endlessly adjustable and much easier to live with.
OK, enough of that, how about driving the Carrera T — what’s that like? It’s great. The 911 generally drives very well, and the T does even better in some situations than other Carreras. While the T is down 64HP to the Carrera S and 94 to the GTS, it hardly feels underpowered. Yes, I could feel the power deficit compared with a Carrera S I had driven recently, but it wasn’t significant.
More important was the improved shifter, which is better than the
one in the S and is now approaching the 997 generation 911 6-sp manual, which is generally considered one of the best manual gearboxes ever offered in a Porsche.
A quick aside: when the 991 version of the 911 launched in 2012, replacing the 997, it featured a new 7-speed manual transmission that was supposed to be better — it’s as good as the old 6-speed but now has an overdrive to save fuel and decrease emissions, was the pitch. Only the 7-speed wasn’t nearly as good. It felt rubbery, imprecise and just bad. When the 991.2 gen 911 launched in 2016, the gearbox improved slightly, and when the 2018 Carrera T came out, it was finally decent. The 992 911S incorporated the improvements from the 991.2 Carrera T, and the 992 Carrera T moves things forward even more with a shorter throw shift lever and even better feel. Thank you, Porsche.
All those changes and reduced sound deadening mean that driving the Carrera T on fast back roads with sweeping curves is a joy. Turn-in is quick and precise, and down-shifting and braking before an especially tight turn energize your soul.
Long freeway stints are noisier than most drivers would like, however, and running errands in town is probably better done in an Escalade. But for true driving enthusiasts, this is the 911 to buy.
Porsche is now offering a 911 variant that harkens back to a model from 1968 that was all about driving fun, and I love it. The 2023 Carrera T is modern and full of tech, yet also a blast to drive. The Carrera T starts at $118,050. Options, which are plentiful in any Porsche, can add significantly to that number. If you buy one with the manual, I promise you’ll experience many happy driving miles for years to come.

As always, call Phil Hornbeak, the Auto Program Manager at BCMS (210-301-4367) for your best deal on any new car or truck brand. Phil can also connect you to preferred financing and lease rates.
Stephen Schutz, MD, is a board-certified gastroenterologist who lived in San Antonio in the 1990s when he was stationed here in the U.S. Air Force. He has been writing auto reviews for San Antonio Medicine magazine since 1995.

11911 IH 10 West San Antonio, TX 78230
Coby Allen 210-696-2232
Audi Dominion 21105 West IH 10 San Antonio, TX 78257
Anthony Garcia 210-581-0512
Northside Chevrolet 9400 San Pedro Ave. San Antonio, TX 78216
Charles Williams 210-912-5087
Chuck Nash Chevrolet Buick GMC 3209 North Interstate 35 San Marcos, TX
William Boyd 210-859-2719
Kahlig Auto Group
Bluebonnet Chrysler Dodge Ram 547 S. Seguin Ave. New Braunfels, TX 78130
Matthew C. Fraser 830-606-3463
Kahlig Auto Group
Northside Ford 12300 San Pedro San Antonio, TX
Marty Martinez 210-477-3472
Kahlig Auto Group
North Park Lexus at Dominion 25131 IH 10 W Dominion San Antonio, TX
James Cole 210-816-6000
Kahlig Auto Group
Northside Honda 9100 San Pedro Ave. San Antonio, TX 78216
Jaime Anteola 210-744-6198
Kahlig Auto Group
14610 IH 10 West San Antonio, TX 78249
Mark Hennigan 832-428-9507
Land Rover San Antonio 13660 IH 10 West San Antonio, TX
Cameron Tang 210-561-4900
North Park Lexus 611 Lockhill Selma San Antonio, TX
Jose Contreras 320-308-8900
North Park Subaru 9807 San Pedro San Antonio, TX 78216
Raymond Rangel 210-308-0200
North Park Lincoln 9207 San Pedro San Antonio, TX
Sandy Small 210-341-8841
Kahlig Auto Group
North Park Subaru at Dominion 21415 IH 10 West San Antonio, TX 78257
Phil Larson 877-356-0476
Mercedes Benz of Boerne 31445 IH 10 West Boerne, TX
James Godkin 830-981-6000
Cavender Toyota 5730 NW Loop 410 San Antonio, TX
Spencer Herrera 210-581-0474
Mercedes Benz of San Antonio 9600 San Pedro San Antonio, TX Al Cavazos Jr. 210-366-9600
Kahlig Auto Group
North Park Toyota 10703 Southwest Loop 410 San Antonio, TX 78211

Justin Boone 210-635-5000
As of June 1, 2023, our loan rate will be 5.0% for 60 months with approved credit.
9455 IH 10 West San Antonio, TX 78230
Douglas Cox 210-764-6945

