FINDING
THROUGH WINTER

CORTISOL PASSING THE TORCH THIS HOLIDAY SEASON


Orthopedic
Total
Headache


FINDING
THROUGH WINTER

CORTISOL PASSING THE TORCH THIS HOLIDAY SEASON


Orthopedic
Total
Headache

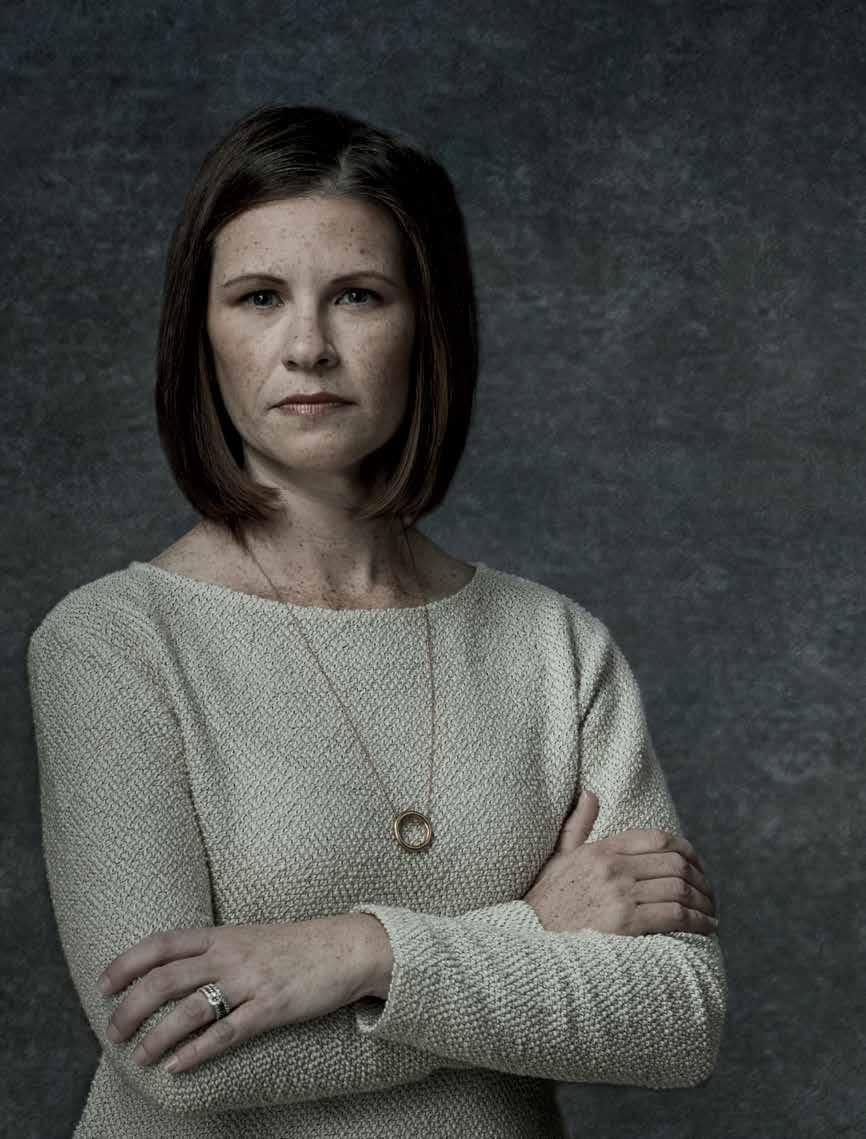
This issue is about renewal and the quiet strength it takes to keep showing up for the things that matter most. Few people capture that idea better than our cover star, Sarah Jessica Parker. Her story on page 8 looks at a life built on hard work, genuine curiosity, and an ongoing willingness to evolve. From her Broadway beginnings to her role as a mother, cultural icon, and now global creative director for a jewelry company, Parker has managed to grow with purpose while keeping her feet firmly on the ground and her priorities in check.

PRESIDENT & CEO
SAM HOUSTON
VICE PRESIDENT & CFO
SPRING HOUSTON
EDITOR, FEATURE WRITER & SOCIAL MEDIA
SONDRA BARR
ART DIRECTOR
VANESSA FRYER
ACCOUNTS MANAGER
JENNIFER BEAVERS
WEBSITE LYDIA ROGERS
ADVERTISING & SALES
As the season shifts and the days shorten, many start to feel that familiar dip in energy that comes with less sunlight and colder mornings. “Finding Light Through Winter Blues” on page 30 explores small, realistic ways to keep spirits steady when daylight fades—reminding readers that even modest daily habits, from getting outside to maintaining connection, can bring comfort, clarity, and a sense of renewal when it’s needed most.
Another piece, “Understanding Cortisol and Your Well-Being,” takes a closer look at stress and the subtle ways it can shape physical and emotional health. The story offers insight into how simple choices—better sleep, mindful movement, balanced meals, and healthy boundaries—can help restore calm and focus amid life’s constant motion. Check it out on page 46 for practical ideas that fit easily into any routine.
And for anyone noticing changes in long-held family roles this holiday season, “Passing the Torch: Finding Joy in Being the Guest Instead of the Host” offers a thoughtful reminder that stepping back doesn’t mean stepping away. Sometimes, joy simply looks different than it used to, and learning to embrace that shift can open the door to a new kind of peace and connection. Find it on page 14.
Each article in this issue encourages reflection and a fresh perspective. These are timely themes as the year winds down and new possibilities start to take shape. Living well often begins with small adjustments and a little openness to what’s next. See you in 2026.
Live well,
TEXAS: Denton County, Dallas County, Collin County
TEXAS & OKLAHOMA: Texoma Area

WRITE TO US:
Tell us who you would like to see featured on the cover, or what subjects you would like covered in upcoming editions of LIVING WELL MAGAZINE at info@livingwellmag.com
SUBSCRIPTIONS & CUSTOMER INQUIRIES
Houstons of Dallas Publishing, Inc. 102 E. Broadway, #901 Prosper, TX 75078 www.LivingWellmag.com
Phone: (214) 507-1000 Fax: (855) 248-2132
LIVING WELL MAGAZINE is a source for quality educational articles on living a healthy, vibrant life. Our focus is on connecting our readers with the latest information on a host of topics relevant to their evolving life. From cutting edge medical news and procedures to top-tier financial, legal and lifestyle information. Connecting readers to leading medical and business professionals in their community in Texas and Oklahoma.





Justin M. Kane, MD, is a board-certified orthopedic surgeon and founder of the Orthopedic Institute of North Texas (OINT). He is internationally recognized for his expertise in foot and ankle care. He is a published author and a global lecturer, who has previously served as a Professor of Surgery at Texas A & M Health Science Center College of Medicine.
At the Orthopedic Institute of North Texas, Dr. Kane and his team’s goal is your return to normal activity. They provide surgical and non-surgical solutions designed to resolve your pain.
Dr. Kane specializes in
• Bunion and hammertoe correction
• Complex foot and ankle reconstructive surgery
• Surgical and non-surgical treatment of foot and ankle disorders



It doesn’t have tobeperfect to be beautiful.


Proving hard work and heart never go out of style.
By SONDRA BARR
Sarah Jessica Parker turned 60 in March, and if the milestone gives her pause, you wouldn’t know it from the pace of her days. She still reads between appointments, still guards the ordinary rhythms of family life, and still delights in the creative problem-solving of a new project—on stage, on screen, or at a drafting table sketching jewelry. The woman who helped define a generation’s relationship with New York City and stilettos hasn’t slowed; she’s simply refined. As she puts it, fashion and life alike don’t need to be air-brushed to shine. “It doesn’t have to be perfect to be beautiful,” she said recently to writer Melanie Bromley for Hello! “Sometimes it’s the little quirks that make it yours.”
From Small-Town Roots to the Big Stage
Parker’s story begins far from Fifth Avenue. Born in Nelsonville, Ohio, she grew up one of eight children, in a home where money was scarce but creative ambition was encouraged. Her mother, Barbara, nudged the family toward opportunity, moving them to New York when Parker was 11 so several of the children could train and audition.
Two years later, she joined Annie on Broadway and eventually took over the title role. By 13, she had logged a professional résumé most adult actors covet: stage work, ballet and acting classes, and the beginnings of a film career. From that early sprint came the first starring TV role—Square Pegs—and, in time, the larger cultural moment that would knit her name to a character forever.
Overnight success often happens, not in Parker’s case. Decade by decade, she moved from Footloose and L.A. Story to Hocus Pocus and a steady rotation of plays, including How to Succeed in Business Without Really Trying, where she performed with her future husband, Matthew Broderick. Then came HBO’s Sex and the City in 1998, and an alchemy that fused Parker’s comic precision with a character’s vulnerability so indelibly that “Carrie Bradshaw” became cultural shorthand. Along the way, Parker collected six Golden Globes and two Primetime Emmys, but more telling is how she has metabolized scrutiny and success—sometimes by stepping away from the noise.
In recent seasons, she returned to Carrie in And Just Like Tht… and helped guide the decision to bring the new chapter to a graceful close. “Sometimes it’s best to gracefully walk away when things feel really right and energetic,” she told CBS Mornings this fall, adding—ever the pragmatic artist—“I’m not certain I understand what that decision means, because I could just be on hiatus.” The sentiment lands like a thesis statement for a working life built on instinct and respect for the audience: do the work, protect the joy, know when to shift.
That equilibrium extends beyond sets and rehearsal rooms. Parker and Broderick married in 1997 on the Lower East Side and now live in Greenwich Village with their son and twin daughters. The family life is ordinary in all the grounding ways—homework, dinner, logistics— and yet it coexists with the red-carpet chapter headings: 12 Met Gala appearances, including the tartan McQueen triumph in 2006 that still lives rent-free in fashion’s collective memory. For Parker, those moments are the result of long conversations and precise choices. If the public sees the gowns and camera flashes, Parker looks for work that outlasts applause. She’s the rare marquee talent who also cherishes the desk work: producing, editing, reading. As one of the 2025 Booker Prize judges, she’s reading at an industrial clip and tinkering with process to keep pace. “I have started to read with a different kind of energy,” she explained, offering a reader’s practical magic for busy lives: there’s always time—“in between appointments or calls or waiting for a bus… those little windows of time are much more valuable,” and she “just never leave[s] home without a book.”
Her parallel life in fashion and fragrance has never been a costume change; it’s an extension of curiosity. There was a long-running per-
fume line, a shoe brand that became a staple for many, and now a new chapter that feels both modern and quintessentially SJP: lab-grown diamonds. Parker recently joined Astrea London as global creative director and shareholder, partnering closely with founder Nathalie Morrison and launching a 12-piece collection.
The choice is aesthetic and ethical. “After wandering deep into the world of lab-grown diamonds, I’ve fallen in love with their possibility, their beauty, and their future,” she wrote on Instagram. For Parker, diamonds are more than dazzle: “They carry stories, history and a sense of eternity… Fashion is ever-changing, but a diamond is timeless – it becomes part of your life, your memories,” she told Bromley. The collection—featuring colored stones—debuts in Dubai on December 8, and a portion of profits will support underprivileged children in Africa, a philanthropic throughline that moves her.
If you’re tempted to confuse Parker and Bradshaw’s appetites, she’ll draw the line. “I’ve been with my husband for 33 years—I’ve got kids. My single life was far less colorful… I was much more frugal, much more thoughtful about a savings account,” she told British Vogue this spring, before sketching the chasm between Carrie’s leisure and her own decades of steady work. That sensibility was formed early. At 18, between auditions and odd jobs, she learned to make $40 cover three days. “There’s security in financial gain” and “security in being able to pay your bills,” she reflected on the Call Her Daddy podcast. Fame hasn’t insulated her from perspective. In Hello magazine, Parker declined the familiar “work-life balance” fable: “I feel peculiar and uncomfortable talking about balance. I just don’t think it’s something I should comment on, out of respect for working parents.” She pointed to the reality of people holding “two to three jobs with no support,” adding, simply, “I am choosing to be a working person.”
Parker’s relationship with nostalgia is equally pragmatic. In Vogue’s December 2021 cover story, she revealed she kept “every single solitary thing”—wardrobe, props, furniture—from Sex and the City, meticulously catalogued and stored by season and scene. It’s an archivist’s impulse, but also a creative question mark: what do we keep, and why? That blend of tenderness and clear-eyed resolve is part of her public resilience. Cultural weather shifts, opinions corkscrew online, but she’s unlikely to be whiplashed by a comment thread. It isn’t indifference so much as keeping her focus. When asked about the swirl around And Just Like Tht…—praise, criticism, and the strange subculture of people who watch to nitpick—she’s said: “I guess I don’t really care,” mindful that connection, not consensus, sustains a story.
So, what does “living well” look like for Parker at 60? It’s a life that accommodates astonishment—the thrill of Iris van Herpen wings at the 2025 New York City Ballet Gala—without requiring spectacle. It’s a desk strewn with manuscripts and a tote bag with a novel tucked inside. It’s the small anarchies of style—necklace off-center, a dash of tartan—to remind us that personal beauty resists symmetry. It’s a marriage that began in a downtown synagogue and a home life that insists on dinner, homework, and endless laundry. And it’s work. The kind that started when she was 8 and never really paused. She doesn’t romanticize the grind; she makes it humane.


“Reading is a mostly solitary experience,” she said of her Booker duties, “but judging has been hugely helpful” because it’s shared—an art form re-imagined as conversation.”
Parker’s story is, at its core, about balance. She’s managed to hold on to a sense of normalcy while living a very un-normal life. One day she might be at a gala or on set, and the next she’s home making dinner or helping with homework. It’s that mix of glamour and everyday life that keeps her grounded. She’s not chasing perfection these days—she’s just interested. Interested in new projects, in good stories, in figuring things out. Curiosity has always been her quiet superpower, whether it’s diving into a book between appointments or helping design a new jewelry line.
At 60, Parker seems settled but never still. She’s still creating, still learning, still showing that a good life doesn’t have to be flawless—it just has to be real.

Sometimes it’s best to gracefullywalkaway whenthingsfeelreally rightandenergetic.



Ronald M. Barke, MD; Chian-Huey (Amy) Hong, MD; Rosmary Sanchez, OD • Comprehensive Adult Eye Care • Light Adjustable Lens, Odyssey™, Symfony®, PanOptix, Vivity® and the Eyhance IOL • Management of Dry Eye, Glaucoma & Corneal Disease • Eyelid Surgery & Botox® • Laser Vision Correction, EVO ICL™
locations to serve you in Allen, Arlington, Dallas, Frisco, Greenville, McKinney, Mesquite, North Fort Worth, Plano, Richardson, and Rockwall.
Dr. Courtney is a board-certified orthopedic spine surgeon located in Plano, Texas. A Louisiana native, he attended Louisiana State University for medical school, and completed residency at Texas A&M followed by a fellowship at the Florida Neck and Back Institute.
SPECIALTIES:
• Back Pain
• Neck Pain
• Spine Pain
• Disc Replacement
• Microdiscectomy
• Spinal Fusion
• Minimally Invasive Surgery
• Steroid Injections
• Physical Therapy
“I believe in treating each of my patients with honesty, dignity, and respect. My patients come away from our shared interactions feeling confident, assured that they are truly in the best hands. Throughout my career, I have remained laser-focused on providing world-class care and innovation to the patients I treat on a daily basis. I look forward to getting to know you!”
us a call today 817-460-2272 or Toll-Free 800-442-5330 www.keywhitman.com







By JESS GRAY
F or many families, the holidays are woven with traditions that repeat year after year. Who makes the turkey, who sets the table with the good china, who pulls out the box of ornaments and carefully hangs the oldest ones first—it’s all part of a rhythm that becomes as familiar as the carols on the radio. And for years, perhaps decades, you might have been the person at the center of that rhythm. The host. The planner. The one who created the magic for everyone else. But what happens when that role changes?
Maybe you’re stepping back just for this season because of travel, health, or the simple fact that life has gotten busier. Or perhaps the shift is more permanent—you’ve grown older, downsized, or no longer feel able to manage the cooking, cleaning, and coordinating. Whatever the reason, sitting in the guest chair instead of the host’s seat can stir up feelings you didn’t expect.
It might be relief at first—no 4 a.m. grocery runs, no marathon of dishes stacked in the sink. Yet for many, relief soon gives way to a complicated mix of sadness, restlessness, or even resentment. You notice that things aren’t being done the way you would do them. You
miss the satisfaction of creating a welcoming table. You feel awkward in someone else’s space, watching traditions unfold differently, wondering where you belong.
If you’re experiencing this transition, you’re not alone. Roles shift in every family, and the holidays, with their heavy emphasis on ritual, can magnify the change. But this shift doesn’t have to diminish your sense of meaning. In fact, stepping back from hosting can open the door to a new kind of joy.
The first step is acknowledging that something has changed—and that it’s okay to grieve it. Hosting is about far more than logistics. For many, it represented love, service, creativity, even identity. For many, holiday traditions shows that they are closely tied to well-being and belonging, especially as we age. Letting go of that role can feel like letting go of a part of yourself.
It’s normal to feel sadness when the mantle passes to someone else. Give yourself permission to name that sadness. Maybe you miss the
By creating something new, you signal that your role is still vital to the family story, even if it looks different.
bustling kitchen. Maybe you miss the compliments on your pumpkin pie. Maybe you just miss being needed. Grief in this context doesn’t mean you’re ungrateful for what others are doing—it means you recognize that a meaningful chapter has closed. And naming that feeling is the first step toward moving forward.
Once you’ve honored what’s been lost, you can begin reframing your role. You are not “less than” because you are no longer the host. You are simply in a different seat at the same table. Think about what being a guest makes possible. You can engage more fully in conversations without worrying about the timing of the roast. You can linger over dessert without mentally tallying which serving bowls still need to be washed. You can be present in ways that were harder when your attention was split among dozens of details. It may help to see yourself not as a “retired host” but as a “memory keeper.” Share stories from past holidays. Remind younger family members of traditions they might not know the origins of. Offer encouragement to whoever has stepped into the hosting role. What they need most is not a critic, but a cheerleader who recognizes the heart behind their effort.
Of course, being a guest comes with challenges. Perhaps the mashed potatoes are lumpy. Maybe the table lacks the polish you once prided yourself on. These are the moments when it’s tempting to jump in, correct, or quietly fume. Here’s where perspective matters. Ask yourself: will this detail matter in five years? If not, let it go. What will last are the relationships around the table, not whether the napkins were folded into fans.
If you truly feel compelled to contribute, find a way to do so that doesn’t overshadow the host. Bring a favorite dish to share, offer to entertain the grandkids while dinner is finishing, or help clear plates when the meal is done. Small acts of support communicate love without taking over.
Sometimes the longing for “how it used to be” is really a longing for continuity. That’s where new traditions can help. If hosting is no longer feasible, perhaps you can introduce a ritual that feels just as meaningful, even in the guest role.
Maybe you bring a storybook each year to read aloud to the younger ones. Maybe you prepare a slideshow of old family photos to share after dinner. Maybe you start a “gratitude jar” where everyone slips in a note about what they’re thankful for, and you read them together. Traditions don’t always require hosting—they require presence, repetition, and meaning. By creating something new, you signal that your
role is still vital to the family story, even if it looks different.
Another part of this transition is flexibility. Some years you may host a small gathering in your space—perhaps a brunch, or an evening of cookies and cocoa—even if you no longer handle the full holiday meal. Other years, you may simply be the guest. Giving yourself permission to flex between roles can reduce the sting of feeling “finished.” Think of it as shifting from conductor to musician. You may no longer direct the whole orchestra, but you still add your voice to the music.
Hosting is often tied to giving. You gave your time, your energy, your home. But there is also a gift in learning how to receive. Receiving someone else’s hospitality with grace and gratitude is its own kind of offering. It allows others to step up, to grow, to practice the generosity you modeled for so many years.
In that sense, being the guest isn’t about stepping down—it’s about passing on. You’re giving someone else the opportunity to feel the joy of hosting, the pride of creating, the warmth of serving. And your willingness to receive it graciously affirms their effort.
If you find the sadness of this shift lingers beyond the holidays, it may help to talk about it. Confide in a friend who has gone through a similar transition. Share your feelings with your family—not as a complaint, but as a way of helping them understand your perspective. And if the holidays bring up loneliness or isolation that feels overwhelming, consider reaching out for professional support. According to the National Institute on Aging, older adults often experience heightened loneliness during the holiday season, which can impact both mental and physical health. Talking with a counselor, joining a community group, or volunteering your time are all ways to reconnect with purpose.
It’s easy to think joy only lives in the big, orchestrated celebrations we once managed. But joy can be just as real in quieter moments: holding a grandchild on your lap, laughing at a family joke, watching someone else’s recipe succeed (or fail) with humor.
The truth is, every role in the holiday story matters. Hosting was one chapter, and it was beautiful. Being the guest is another, with its own unique blessings. You haven’t lost your place at the table. You’ve simply changed seats. And from where you sit now, you may find a new kind of joy—a joy not of managing, but of savoring. Because in the end, the heart of the holidays isn’t about who hosts. It’s about who’s gathered, and the love that binds you together.


Dallas Brain, Spine and Skull Base Surgery is a neurosurgical practice that offers over 40 years of experience providing an innovative and collaborative state of the art approach to the care of patients with challenging neurological problems from around the world. Dr. Beshay and Dr. Coimbra have developed unique expertise in the treatment of brain tumors becoming the referral destination for the treatment of patients, especially those with complex or difficult to access tumors. They have also shown a commitment to the development of minimally invasive neurosurgical procedures including the most modern expanded trans–nasal endoscopic skull base surgical techniques and focused extradural approaches to skull base tumors.
Dr. Beshay’s interests include tumors of the brain and spine, minimally invasive spine surgery, complex spinal reconstruction, and epilepsy surgery. In addition to surgical treatment of intracranial and spinal disease, he has an interest in neurological bleeding and its reversal. Dr. Beshay’s clinical interests include: benign and malignant brain tumors, neuroendoscopy, epilepsy surgery, intracranial hemorrhage, cranial/ spinal trauma, minimally invasive spine surgery, complex spinal reconstruction with an interest in C1–C2 and occipito–cervical junction disease. Dr. Coimbra restricts his practice mostly to intracranial neurosurgery. This selective tertiary practice has fostered the opportunity to develop unique expertise and commitment to the treatment of malignant and benign brain tumors. He is an expert in the minimally invasive resection of the most complex skull base tumors, including meningiomas, acoustic neuromas, and pituitary tumors. He employs CyberKnife radiation therapy, endoscopic endonasal techniques, and an array of focused skull base approaches to create a customized treatment plan for each patient in his practice. These innovative approaches allow resection of deep, difficult, and complex tumors with minimal brain tissue manipulation and maximal preservation of function.
Dr. Coimbra and Dr. Beshay believe in customized patient care and a team approach to medicine with attention to careful selection of the least invasive and most effective treatment for each patient. Their commitment to this philosophy has resulted in maximum preservation of function, less discomfort, shorter hospital stays and durable favorable outcomes for their patients.

Board-Certified Orthopedic Surgeon | Hip & Knee Replacement Specialist
Dr. Yousuf is a nationally recognized leader in advanced hip and knee surgery, offering robotic-assisted procedures, partial knee replacements, and the anterior hip approach to help patients find relief from joint paint and move freely again.
He serves as Medical Director of Hip & Knee Surgery and Orthopedic Robotics at Baylor Scott & White (East Region) and has been honored among the Best Doctors in Dallas & Collin County. His dedication to innovation and patient care continues to set the standard in orthopedic excellence.




Brian Nwannunu, MD, MS, is an orthopedic surgeon specializing in hip and knee replacement. He cares for patients at Texas Joint Institute in Allen and in McKinney, Texas.
Dr. Nwannunu, a native of Dallas, graduated Valedictorian from the High School for Health Professions at Townview Magnet Center in DISD. He then earned his bachelor’s degree in Biology at Morehouse College in Atlanta, Georgia, where he was part of the Morehouse College Honors Program. Upon graduation, he completed his master’s degree in Physiology at Georgetown University in Washington, D.C., with a concentration on complementary and alternative medicine. Dr. Nwannunu then graduated with his medical degree from Howard University College of Medicine in Washington, D.C., where he was inducted into the Alpha Omega Alpha Honor Medical Society.
Dr. Nwannunu completed his residency in orthopedic surgery at the John Peter Smith Health Network in Fort Worth, Texas, before pursuing additional training with a fellowship in adult reconstruction at Baylor College of Medicine in Houston, Texas. In addition to his clinical training, Dr. Nwannunu enjoys mission work abroad, providing medical care and health education to populations in need. He is also one of the few official Jiffy Knee™ surgeons in the North Texas area.
He is a member of the American Medical Association, National Medical Association, American Academy of Orthopaedic Surgeons and the American Association of Hip and Knee Surgeons.
When not working, Dr. Nwannunu enjoys basketball, weight training, outdoor activities, attending art and music festivals, traveling, world news, and reading.

Dear Olivia,
How can families support loved ones receiving hospice care at home? With the hospice team in place, what is the role of the family?
~Loving Family
Dear Loving Family,
Thank you for your thoughtful question. It’s clear how much you care, and that love is one of the most powerful forms of support a person can receive during hospice care.
When hospice is provided at home, the professional team—nurses, aides, social workers, chaplains, and volunteers—is there to guide and support both the patient and the family. But you, as family, play a central role. You know your loved one’s personality, preferences, and values better than anyone. That insight helps the hospice team tailor care in a way that truly honors who they are.
Here are a few meaningful ways families can support their loved one:
1.Share what makes them unique. Let the team know about favorite music, spiritual practices,


foods they enjoy, or even how they like to be spoken to. These details help create a comforting and familiar environment.
2.Create a peaceful space. Whether your loved one prefers quiet moments with close family or enjoys frequent visits and conversation, your presence helps shape the atmosphere of care.
3.Encourage legacy projects. Some families find comfort in helping their loved one create a memory book, record stories, or write letters. Volunteers can assist with these if desired.
4.Stay connected with the hospice team. You’re not expected to do this alone. Hospice is a partnership, and your observations—changes in mood, comfort, or routines—are incredibly valuable.
Hospice is not a place, but a philosophy of care. It’s about living fully and comfortably, surrounded by love. You are not alone—many families face these tender moments, and the hospice team is here to walk alongside you.
~Olivia







We

OUR SERVICES:
Macular Degeneration
Diabetic Eye Disease
Retinal Vein & Artery Occlusions
Flashes & Floaters
Retinal Tears & Detachments
Macular Pucker/Epiretinal
Membrane
Macular Holes
Uveitis
At Texas Macula & Retina, our mission is to provide exceptional eye care with a focus on the diagnosis, treatment, and management of retinal disorders.
Dr. Adams is a board-certified Ophthalmologist and Ophthalmic Surgeon specializing in Vitreoretinal Surgery. His principal areas of interest include age-related macular degeneration, diabetic retinopathy, retinal detachment repair, macular surgery, retinal lasers, and secondary intraocular lens implantation.
Dr. Adams and his team are committed to preserving and improving the vision and overall quality of life for our patients by offering the most advanced and personalized retina care available.


magine slowly losing your vision, bit by bit, so subtly you don’t notice until it’s too late. That’s the chilling reality of Glaucoma, one of the leading causes of irreversible blindness worldwide. The most unsettling part? It often gives no warning signs.
As an ophthalmologist, I’ve met countless patients who walk into my office saying, “I see fine. Why would I need an eye exam?” Only for me to discover they’ve been quietly losing vision for years. So, let’s shine some light on glaucoma: what it is, how we treat it, and how you can protect your vision.
What Is Glaucoma?
In the simplest terms, glaucoma is a disease that damages the optic nerve, the vital cable connecting your eye to your brain. Think of your optic nerve as a bundle of a million tiny electrical wires carrying visual information. When those wires are damaged, parts of your vision fade, usually beginning with your peripheral vision (the outer edges of your sight).
The main culprit behind this nerve damage is increased pressure inside the eye, called intraocular pressure. Normally, your eye produces a clear fluid called aqueous humor to nourish its tissues, and this fluid drains out through a microscopic meshwork at the front of the eye. If that drainage system clogs or the fluid is produced too quickly, pressure builds up, like a sink with a slow drain.
Over time, that pressure damages the optic nerve. However, glaucoma is more than just a pressure problem, it’s a complex, multifactorial condition involving genetics, blood flow, and nerve health.
How Do You Treat Glaucoma?
Here’s the good news: while glaucoma damage can not be reversed, it can be stopped from getting worse. The goal of treatment is to lower the eye pressure to a safe level for your optic nerve. Depending on the case, this can be achieved through:
• Prescription Eye Drops: These are the first line of defense and work by either reducing fluid production or improving drainage. Many patients do very well with daily eye drops.
• Laser Treatments: Advances in laser technology have made procedures like Selective Laser Trabeculoplasty (SLT) both safe and effective. It helps open the drainage system, often reducing or even eliminating the need for drops.
• Surgery: For more advanced cases, surgical options such as trabeculectomy, tube shunt, or minimally invasive glaucoma surgeries (MIGS) create new drainage pathways for fluid to escape, lowering pressure more permanently.
Understanding Glaucoma Before It Steals Your Sight
By MATTHEW
Managing glaucoma is a marathon, not a sprint. Regular follow-up visits, pressure checks, and visual field testing are essential to track the disease’s progression. With modern treatments and patient diligence, most people with glaucoma retain useful vision for their entire life.
How Do I Know If I Have Glaucoma?
Unfortunately, you probably won’t. At least not until damage has already occurred. In its early stages, glaucoma is almost always asymptomatic. Vision loss begins in the periphery so you might not notice anything until you start bumping into walls and doorframes. By the time central vision is affected, significant and irreversible damage has already occurred.
That’s why routine comprehensive eye exams are so critical. A quick vision test at the pharmacy isn’t enough. Your ophthalmologist will perform a series of painless tests that can detect glaucoma before you feel any symptoms:
During a comprehensive eye exam, your ophthalmologist will perform:
• Tonometry: Measures your eye pressure.
• Ophthalmoscopy: Lets your doctor look directly at your optic nerve.
• Visual Field Testing: Maps your peripheral vision.
• Optical coherence tomography: A high-tech scan that images the optic nerve fibers.
These tests are painless, quick, and could literally save your sight.
So, who’s at risk? Glaucoma doesn’t discriminate, but certain groups are more vulnerable: people over 40, those with a family history of glaucoma, individuals of African, Hispanic, or Asian descent, and anyone with diabetes, nearsightedness, or long-term steroid use. If you fall into one of those categories, make it a habit to schedule a comprehensive eye exam every one to two years. It’s one of the simplest, most cost-effective forms of preventive healthcare you can do for yourself.
With today’s diagnostic tools and treatments, most people with glaucoma can live full lives without ever losing vision, as long as they catch it early. So schedule that exam, even if your eyes “feel fine.” Because the best way to beat glaucoma is to never let it sneak up on you in the first place.
Texas Hip and Knee Center Fellowship Co-Director and Faculty at the Anne Burnett Marion School of Medicine at Texas Christian University
Dr. David Shau is a native Texan, born in Fort Worth, TX. He graduated high school in Flower Mound, TX, and attended the University of Texas at Austin, where he studied biomedical engineering. Dr. Shau then ventured out-of-state to work at leading academic orthopedic surgery centers, including Vanderbilt University, Emory University, and University of California, San Francisco, before being recruited to return home to practice at the premier DFW joint replacement group, the Texas Hip and Knee Center (THK).
Dr. Shau has quickly built his practice through connecting with his community, committing to quality service, and delivering excellent patient care. He utilizes a variety of techniques and approaches for hip and knee care, including direct anterior hip replacements, and offers technology-assisted surgeries, such as Mako Technology for partial and total joint replacements. He also specializes in revision joint surgeries and enjoys complex, challenging cases. As a result of dedicating himself to his craft, his partners at THK promoted him to Fellowship Co-Director early in his practice. Dr. Shau also serves as a Physician Development Coach and is an Assistant Professor at the Burnett School of Medicine at TCU, where he enjoys his roles as a teacher, mentor, and coach.
In his free time, he enjoys food, sports, music, and spending time with his wife and daughter. For more information on Dr. Shau’s care philosophy and the techniques/approaches offered for hip and knee care, please visit DavidShauMD.com.




By SAMUEL ROGERS, SR.

The holidays are a season of reunion, of clinking glasses and sharing meals with the people who have known us the longest. For many of us, this means sitting down with family and friends we don’t see often—people who may live in other towns, practice different lifestyles, or hold vastly different opinions about how the world should work. That mix of personalities can make for colorful conversation, but it can also stir up tension. Add a splash of celebratory wine or spiked eggnog, and suddenly Aunt Edith is ready to debate the latest political headline or Uncle Leon wants to explain why the family should agree with his views on the economy, healthcare, or “the way things used to be.”
Most of us don’t come to holiday tables looking for conflict. We come to reconnect, to laugh, to share traditions, to make memories. And yet, sometimes the conversation slides sideways and you find yourself in the middle of a topic that makes everyone shift in their chairs. What do you do? How can you gracefully steer the moment away from politics, religion, or any other divisive topic without making the other person feel dismissed—or blowing up the evening?
The art of changing the subject is just that—an art. Done poorly, it can feel abrupt or insulting. Done with care, it can diffuse tension and refocus energy back on what matters: time together. Here are some thoughtful strategies for sidestepping tricky conversations during the holidays.
A well-timed joke can defuse tension faster than any lecture or lecture-avoidance tactic. When a topic turns heavy, sometimes the best thing you can do is poke fun at the situation—not the person.
For example, if someone starts raising their voice about politics, you might lean in and say, “You know, if we keep this up, the turkey is going to get cold and we’ll be forced to blame Congress for that too.” With a smile and a light tone, you’ve redirected the moment and reminded everyone of the more immediate, and more pleasant, reason you’re gathered. Humor works because it invites others to laugh with you rather than fight with you. It changes the energy in the room without calling anyone out directly. Of course, humor isn’t always appropriate—but when it is, it can be magic.
2. REDIRECT WITH CURIOSITY
Another effective way to shift a conversation is to gently turn the spotlight elsewhere. Most people enjoy talking about themselves, and asking a question that appeals to someone’s personal life can reframe the moment.
If your cousin launches into a heated debate about national policy, you might say, “That’s interesting. By the way, how’s your new job going? Last time we talked, you’d just started that big project.” By doing so, you acknowledge that you’ve heard them, but you move the conversation back to something they enjoy discussing—something that won’t lead to raised voices.
It doesn’t have to feel manipulative. Curiosity is a form of kindness. It shows you care about them beyond their opinions.
3. PLAY THE “POLITE EXCUSE” CARD
Sometimes, the easiest way to escape is just to excuse yourself. Step into the kitchen to refill your drink. Offer to help with dishes. Ask where the restroom is. These little “time-outs” give you breathing room without requiring confrontation.
The trick is to do it warmly. A simple “Excuse me, I just need to check on the pie,” or “I’ll be right back, I’m out of tea,” is often enough to reset the conversation by the time you return.
4. SHARE A STORY INSTEAD OF A LECTURE
One of the gentlest ways to redirect a tense moment is to tell a story. Stories grab attention and move the focus. If your cousin is beginning to rant about current events, you could interject with, “That reminds me of something funny that happened last week at the grocery store…” and off you go.
You’re not invalidating him, but you’re choosing to gift the group with something lighter. Stories are the opposite of confrontation— they’re invitations.
5. OFFER A SIMPLE ACKNOWLEDGMENT, THEN PIVOT
It’s important not to make people feel ignored or belittled. Often, a quick acknowledgment is all that’s needed before steering the conversation elsewhere. A polite phrase like, “I hear you, and that’s an interesting perspective. Speaking of perspectives, did you see the holiday lights on Main Street this year? They’re incredible.”
This method is like conversational aikido—you’re not fighting, you’re redirecting.
6.
I’ll admit, my personal trick is to use dessert as my secret weapon. Last year, when one of my relatives brought up a controversial news story right as we were clearing plates, I felt the tension building. Rather than jump in or argue, I blurted, “Okay, but have you seen the size of this pumpkin pie? I think it’s bigger than my dog.” Everyone laughed, and within seconds, we were in the kitchen cutting slices. Did I avoid a messy debate? Yes. Did we all get pie? Also yes. That’s what I call a win-win.
Sometimes words aren’t enough—you need action. Suggesting a quick activity can be a lifesaver. It doesn’t have to be elaborate. “Hey, why don’t we all take a walk after dinner?” or “Who’s up for a round of cards?”
When people are engaged in doing something together, it naturally redirects attention away from contentious topics. Shared activity builds camaraderie without requiring words at all.
8.
NOT THE PROBLEM If all else fails, you can appeal directly to the reason you’re all gathered. With a gentle smile, you might say, “I think we could debate this all night, but I’d love for us to keep tonight about family and the holiday.”
You’re not shutting anyone down, but you are making a respectful request that reminds everyone why they’re at the table in the first place.
The good news? You don’t have to control everyone and every conversation. You only need to control your own role in the conversation. By choosing to respond with humor, curiosity, acknowledgment, or even dessert, you’re setting the tone for connection over division.
The holidays don’t have to be perfect to be meaningful. They don’t need to be free of awkward comments, old rivalries, or differing opinions. What they need—what we all need—is grace. Grace to let a moment pass. Grace to redirect without judgment. Grace to laugh, to listen, to eat too much pie, and to focus on the threads that keep us tied together as families, neighbors, and friends.
“Where






•Around-the-clock
•Physical,
•Wound Management
•Intravenous Therapy
•Tracheotomy Care
•Physician Services
•Medication Administration
•Enteral/Parenteral Therapy
•X-Ray Services
•Laboratory Services

At KoonsFuller, we only practice family law. Which means we’re fully dedicated to serving Dallas area families and their unique legal needs. From informal negotiations to mediations, collaborative law to court proceedings, our thirty plus attorneys across four offices provide an unmatched network of expertise. Working together as a fully integrated team, KoonsFuller’s attorneys are equipped to handle estates of all sizes, cases of all complexities, and custody issues of any kind.
See what KoonsFuller can do for your family.Working together, as a fully integrated team, there is no case too large or complex for us to manage. To learn more about KoonsFuller, visit koonsfuller.com.

By STEPHANIE CARTER
On November 2nd everyone’s clock “falls back” into shorter days and the temperatures finally start to drop a bit. The tell-tale signs of fall. I always notice a shift in my mood. For a period of time, I’m excited about the charm of winter coming. Those frosted mornings, a great fireplace, sweaters, and holiday decorations, are all things I’ve missed from the previous year. Then the days of having less sunshine and it being dark going to and from work set in with a heaviness that is hard to shake.
Over the years, I’ve learned that understanding these winter blues and taking small intentional steps can make all the difference in how I experience the colder months. I know I’m not alone; many people experience a dip in energy and spirits as the seasons change and I hope sharing my journey can help someone.
I first started noticing that my low moods weren’t just occasional, they seemed to return like clockwork each year as daylight decreased. I learned that this pattern is common, and in more persistent cases, it can develop into Seasonal Affective Disorder, a type of depression tied to the fall and winter months. While the winter blues can feel like a passing fog, SAD comes with more pronounced and lasting symptoms: fatigue, irritability, oversleeping or trouble waking, cravings for certain foods, and a general sense of heaviness. For me, the key was recognizing the signs early each year, so I could mentally prepare rather than simply endure the dreaded feelings.
The lack of sunlight plays a huge role. Fewer daylight hours can disrupt our internal clocks, or circadian rhythms, affecting sleep patterns and mood. Our bodies’ chemistry shifts and serotonin levels may drop, leaving us feeling low, while melatonin rises, making us want to stay in bed longer. Over time, these changes can quietly chip away at energy and motivation. Understanding what was happening biologically gave me a sense of control; suddenly, the winter blues didn’t feel like a mysterious force, but something I could actively respond to.
Even with that understanding, the darker months still challenge me, which is why I rely on a few strategies to maintain balance and light in my life:

What matters is taking small, consistent steps to care for yourself, whether it’s getting a little more sunlight, moving your body, or reaching out to someone you trust.
• Maximize natural light exposure by spending time outdoors during daylight hours, even on cloudy days. When I can’t get outside enough, I use an inexpensive light therapy box on my desk, which simulates sunlight and can lift mood.
• Stay active through regular exercise, whether it’s walking or swimming. I’ve found that even light movement boosts my energy and focus.
• Maintain a consistent routine, including set sleep and meal times, as well as scheduling activities I enjoy. It helps keep my days predictable and my mind grounded.
• Stay socially connected by checking in with friends and family, even if it’s just a quick phone call or video chat. Human connection is surprisingly energizing.
• Practice mindfulness and relaxation, such as meditation, deep breathing, prayer, or simply sitting quietly for a few minutes to focus on the present moment.
• Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. I try to include foods with omega-3 fatty acids, like salmon, which can support both mood and cognitive function.
• Prioritize sleep, aiming for seven to nine hours nightly. A calming bedtime routine that’s the same each time, and a dark, quiet room make a huge difference. I shut off my phone at least two hours before bed.
• Maintain a healthy weight and avoid habits that undermine overall health, such as smoking or excessive alcohol consumption.
Beyond these practical steps, I’ve learned to embrace the season in its own right. Winter can be a time for reflection, creativity, and slower, more intentional living. I make a point to explore indoor hobbies I’ve neglected, make exciting plans and goals for the next year, catch
up on those books I said I’d read, or simply enjoy quiet moments by the window with a cup of coffee and my dog. Accepting that winter naturally brings a shift in mood allows me to meet the season with self-compassion rather than frustration.
I know firsthand that navigating the darker months isn’t always easy, but if I can find ways to lift my mood and stay connected, you can too. Some days are tougher than others, and that’s completely normal. What matters is taking small, consistent steps to care for yourself, whether it’s getting a little more sunlight, moving your body, or reaching out to someone you trust. And if you find that the winter blues are starting to feel heavier than you can handle on your own, seeking guidance from a mental health professional can make a meaningful difference. These days they are easy to access from the comfort and privacy of your own home. You don’t have to face it alone, and with support and a few intentional practices, brighter days are absolutely possible.

By RICK ALLEN
Grief is one of life’s most personal journeys. No two paths look the same, yet almost everyone will walk it at some point. It is born from love, from the deep connections we make, and from the absence we feel when someone we cherish is no longer physically here. The ache of loss can feel overwhelming, stretching into every part of our days, from the quiet of morning coffee to the moments when we instinctively reach for the phone to share news with someone who can no longer answer.
At Allen Family Funeral Options, we’ve walked alongside many families in these tender seasons, and we understand how heavy those first steps can feel. Grief is not something you simply “get over,” despite what well-meaning voices may say. Instead, it becomes a part of your life’s fabric—something you carry and, over time, learn to live with. It can reshape you, even as you search for a way forward. Giving yourself permission to feel is one of the most important first steps in that process. Our culture often rewards resilience and composure, but grief is not something that can be neatly tucked away. Allowing yourself to cry, to sit in silence, or even to laugh at a memory without guilt is part of honoring both your loved one and yourself.
Connection is another gentle healer. Many find comfort in talking about their loss with trusted friends or family members. Others seek out grief support groups where every person in the circle understands the language of loss. Talking with someone who understands can remind you that grief is a universal experience, even if your own is unique.
Recovery from grief doesn’t mean forgetting the one you’ve lost. It means learning to carry their memory in a way that doesn’t weigh you down, but instead walks beside you. It’s finding ways to live fully while keeping their presence alive in your heart. Some days will be harder than others, and that’s okay. Healing is not about replacing what you’ve lost; it’s about discovering who you are in its wake.
Small rituals can also bring comfort. Lighting a candle at a certain time each evening, visiting a favorite place you once shared, or keeping a personal memento close can help you maintain a sense of connection. Many families also find that creating a tribute, such as planting a tree or compiling a memory book, allows them to celebrate a life while processing the loss.
This is where funeral homes often become a quiet but important part of the healing process. While their most visible role is caring for the loved one who has passed, their deeper role is in caring for the living. A compassionate funeral director understands that the services they provide are not simply events; they are spaces where grief can breathe, where memories are shared, and where the first small steps toward healing can begin.
A thoughtfully planned memorial—whether traditional, contemporary, or entirely personal—can be a meaningful moment in the grieving process. It is a chance for stories to be told, for tears to be met with understanding, and for a community to gather in support. When handled with care, these moments can become an anchor in the storm, offering comfort in knowing that your loved one was honored in a way that reflects their life.
If you are grieving today, know that you are not alone. There are people and places ready to walk this journey with you, from friends who will listen without judgment to professionals who can guide you toward resources that nurture your heart.
In times of loss, having compassionate guidance can make all the difference. At Allen Family Funeral Options, we are honored to be here for families as they plan meaningful ways to honor and remember those they love. For many years, we’ve served our community by creating personal, heartfelt tributes that reflect a life well lived and offer comfort to those who grieve. Our hope is that from the moment you enter our doors, you feel the warmth, respect, and care you deserve.

At North Texas Orthopaedic & Spine (NTOS), patients of all ages are given the focused, individualized care they need in order to live fully and comfortably. The team at NTOS has a high level of expertise in the diagnosis and treatment of conditions involving the spine, joints, and bones.














Patients appreciate the practice’s ability to educate them thoroughly about their conditions and give them the tools that they need to take control of their well-being. Whether the patient is an athlete with an injury or someone who has a long-term condition that affects their daily life, the NTOS team works alongside them to get them back to a full, active life. NTOS offers treatment for shoulder pain, tennis elbow, torn ACLs, sciatica, carpal tunnel, herniated disc, scoliosis and more. These and other conditions can get in the way of your work, hobbies, and general enjoyment of life.













PLANO






























PLANO





















4090 Mapleshade Ln., Ste. 100 Plano, TX 75093









5655 W. Spring Creek Pkwy., Ste. 115 Plano, TX 75023
DALLAS Lakewood Medical Center
6243 Retail Rd., Ste. 500 Dallas, TX 75231







































































FRISCO 9990 Dallas Pkwy., Ste. 105 Frisco, TX 75033
KAUFMAN 2300 Commerce Way Kaufman, TX 75142



















































VUDHI SLABISAK, MD OrthopaedicSpineSurgeon















































































BRUCE MARKMAN, MD OrthopaedicSurgeon&Sports MedicineSpecialist

STANLEY, MD OrthopaedicSpineSurgeon



























STEVE HONG, MD Interventional Pain ManagementSpecialist



























MCKINNEY 4833 Medical Center Dr., Ste. 6E McKinney, TX 75069




























MESQUITE 1102 N. Galloway Ave. Mesquite, TX 75149


KHAWAJA IKRAM, DO OrthopaedicSurgeon



RAHUL BANERJEE, MD OrthopaedicSurgeon

HODGSON, PA-C OrthopaedicSurgery PhysicianAssistant
If you’re suffering from pain or an athletic injury, schedule an appointment with your preferred NTOS location for effective, compassionate treatment.

When you’re diagnosed with colon cancer, you need comprehensive care from renowned physicians, advanced treatment options, leading edge technology, and clinical trials. But you also need to keep being Mom. With more than 280 locations across the state, Texas Oncology provides expert cancer care and keeps you close to those you love. Because we understand that hugs from your six-year-old are an important part of your treatment plan.

By ALEXANDER HILL
I
t can be easy to overlook the importance of routine health checkups.
Yet, these regular visits to your healthcare provider are more than just a formality—they are a proactive approach to maintaining your well-being. Preventative screenings can detect potential health issues before symptoms arise, allowing for timely intervention and significantly improving health outcomes.
One of the most compelling reasons to prioritize preventative screenings is their role in early disease detection. Conditions like cancer, diabetes, and heart disease often develop silently, without noticeable symptoms. For example, breast cancer is the most diagnosed cancer in women and the second leading cause of cancer-related deaths in the U.S. Early detection through screening can significantly improve outcomes. In fact, according to the Cancer Research Institute, the survival rate for a stage I breast cancer diagnosis is over 99%. Similarly, the American Cancer Society reports that from 1975 to 2020, prevention and screening efforts have averted 4.75 million deaths from five cancer types: breast, cervical, colorectal, lung, and prostate.
Routine screenings also play a crucial role in managing chronic conditions. Regular checkups can identify risk factors for diseases like hypertension, diabetes, and high cholesterol. Early detection of these conditions allows for lifestyle modifications and treatments that can prevent more serious complications, such as heart attacks or strokes. Moreover, Cigna Healthcare reported that engaging in preventive care services is linked to better disease management, fewer hospitalizations, and a decrease in emergency room visits, ultimately contributing to significant cost savings for both individuals and the healthcare system.
Beyond physical health, preventative screenings can have a positive impact on mental well-being. Regular checkups provide an opportunity to discuss mental health concerns with a healthcare provider. Conditions like depression and anxiety can be effectively managed when detected early, leading to improved quality of life.
The benefits of routine health screenings extend beyond individual health. They contribute to overall public health improvements by identifying and addressing health issues within communities. For example, the Centers for Disease Control and Prevention’s National Breast and Cervical Cancer Early Detection Program provides screenings, diagnostic tests, and treatment referral services to underserved communities, aiming to reduce health disparities.
Despite the clear advantages, many individuals skip regular health checkups. Barriers such as high costs, lack of access to healthcare providers, and time constraints can prevent people from seeking necessary screenings. However, it’s important to recognize that many preventive services are covered by insurance, and community health centers often offer low-cost or sliding-scale fee options. Taking the time to schedule and attend regular checkups is an investment in your long-term health.
Incorporating routine health screenings into your wellness routine is a powerful way to take control of your health. By detecting potential issues early, you empower yourself to make informed decisions about your care, leading to better health outcomes and a higher quality of life. Remember, health is wealth, and investing in preventative care is one of the most effective ways to safeguard it.

Texas Back Institute (TBI) has served the North Texas area in spine care for over 45 years. An uncompromising desire to put patients first and provide individualized spine care has helped change the treatment options available to patients for neck and back pain.
Today, TBI is a leader in artificial disc replacement, minimally invasive spine surgery, complex revision surgery, and treatment of spinal deformity. TBI has trained hundreds of surgeons, scientists, and allied health professionals now practicing worldwide. Its research institute employs state-of-the-art technology and is actively involved in many clinical trials, including artificial disc replacement, minimally invasive technologies, and robotic spine surgery. Texas Back Institute has remained one of the most academic practices in spine care. It is one of the largest multidisciplinary spine centers in the world, providing comprehensive care for neck and back pain. With a fully dedicated staff of board-certified orthopedic spine surgeons, neurosurgeons, physiatrists, and physical therapists, the TBI team works together to support its mission of helping patients get back to life. The 26 physicians at Texas Back Institute are leaders in the surgical
and nonsurgical treatment options for back and neck pain, from the most common outpatient procedures to the most complex cases. Thanks to the unmatched expertise of the medical staff, the advanced diagnostic testing, and an unparalleled commitment to patient care, the Texas Back Institute physicians can identify the potential cause of your pain and create a treatment plan specific to your needs.
Texas Back Institute has developed several spine specialty programs. These include the Minimally Invasive Spine Surgery Center, Center for Disc Replacement, Scoliosis and Spine Tumor Center, and Complex Back Surgery Center. These programs give patients access to highly-trained care teams who focus specifically on these areas of spine care, allowing patients in the North Texas area access to treatment options for their individual problems from physicians with extensive experience in these areas.
“At Texas Back Institute, finding the right solution for each patient and offering the least invasive treatment is core to our belief and the foundation for all treatment plans.” Dr. Michael Duffy.

ALLIANCE
3025 N. Tarrant Pkwy., Ste. 220 Fort Worth (Alliance), TX 76177
ARGYLE
310 FM 407E, Ste. 100 Argyle, TX 76226
DALLAS
12222 N. Central Expy. Pavilion II, Ste. 310 Dallas, TX 75243
DENTON
3537 S. Interstate 35, Ste. 308 Denton, TX 76210
FLOWER MOUND
4370 Medical Arts Dr. River Walk Bldg. III, Ste. 230 Flower Mound, TX 75028
FORT WORTH
1650 W. Rosedale St. Ste. 301 Fort Worth, TX 76104
FRISCO
5575 Frisco Square Blvd. Ste. 400 Frisco, TX 75034
LEWISVILLE
500 W. Main St., Ste. 380 Lewisville, TX 75057
MCKINNEY
4510 Medical Center Dr., Ste. 106 McKinney, TX 75069
NORTH RICHLAND HILLS
4351 Booth Calloway Dr., Ste. 404 Fort Worth, TX 76180
CENTRAL PLANO
4001 W. 15th St. Ste. 455 Medical

Courtesy HEARING SERVICES OF McKINNEY
» Staffed by 2 Licensed, Doctors of Audiology
» Hearing Aid Fittings, Maintenance and Repairs
» Invisible Fittings/Open Fittings
» Evaluation Period On All Hearing Aids
» Hearing Evaluations For All Ages
» Wireless/Connectivity Hearing Solutions
» Battery Purchase Programs
» Custom Ear Protection
» Assistive Devices



As an audiologist, I’ve heard every excuse under the sun for avoiding hearing aids. “They’re ugly.” “They won’t help.” “I can’t afford batteries.” These aren’t just old wives’ tales—they’re myths that keep people from better hearing and, more importantly, better health. It’s time to clear the air and encourage a fresh look at what today’s technology really offers.
Let me start with compelling news. Recent research continues to confirm what we’ve long suspected: hearing aid use is linked with better cognitive health. A large UCLA Health study this year showed patients with hearing loss who wore hearing aids had a lower risk of dementia (UCLA Health). Another study of over half a million people found hearing loss raised dementia risk by 7 percent—but that risk diminished significantly with hearing aid use (JAMA Otolaryngology). In other words, dismissing hearing aids as cosmetic ignores a much bigger truth: they’re about protecting both mind and memory.
Myth #1: “Hearing aids are bulky and outdated.”
Many still imagine the oversized devices of decades past. But the devices I fit today are slim, discreet, and often nearly invisible. Many patients forget they’re even wearing them—until they notice how much better life sounds.
Myth #2: “They won’t work with my phone or streaming devices.”
This was once a complaint, but the technology has leapt forward. Modern devices connect directly to smartphones and TVs, streaming calls and music seamlessly. They also adapt automatically to noisy environments like restaurants or traffic. The frustration of missing words on a conference call is largely a thing of the past.
Myth #3: “I can’t afford batteries.”
Rechargeable models are now standard, with batteries that last all day after an overnight charge. No more scrambling for replacements— just plug in at night like you do with your phone.
Myth #4: “They won’t improve my hearing.”
Every case is unique, and while there are some types of hearing loss that hearing aids cannot correct, it’s rare that properly fitted devices don’t improve clarity in meaningful ways. The truth is, hearing aid benefits vary person to person—because each of us experiences hearing loss differently. What is certain is that leaving hearing loss
untreated increases the risks of social isolation, accidents, and added strain on your brain.
Myth #5: “I tried one before and it didn’t work.”
That’s like giving up on glasses after one bad prescription. Sometimes the wrong model or poor settings are to blame. With updated technology and careful fine-tuning, many patients who once rejected hearing aids are amazed at the difference.
Myth #6: “I only need one.”
Wearing two aids provides spatial awareness—helping you pinpoint where sounds come from and improving safety. Just as two eyes give depth perception, two ears give balance and clarity.
Myth #7: “Big-box bargains are just as good.”
While large retailers sell hearing aids, they typically can’t match the individualized care of a private practice. Hearing aids are not onesize-fits-all; they require precise adjustments, regular maintenance, and long-term follow-up. At Hearing Services in McKinney, we provide comprehensive testing, customized fittings, and ongoing support so your devices work for you—not just out of the box. That personalized care is what ensures you truly get the most benefit from your investment.
Myth #8: “Hearing aids won’t affect brain health.”
While nothing guarantees prevention of dementia, mounting evidence shows hearing intervention slows decline in many cases. In fact, the landmark ACHIEVE trial found hearing treatment reduced cognitive decline by nearly 50 percent among high-risk older adults. Ignoring hearing loss as “just aging” could accelerate a path that’s otherwise preventable.
If you’ve noticed yourself asking people to repeat things, cranking up the TV, or missing parts of conversations, don’t dismiss it. A professional hearing evaluation is a simple first step that can reveal far more than you think.
Hearing is more than a sense—it’s connection, safety, stimulation, and joy. Music, laughter, whispers, shared stories with loved ones— these are not small things. They are life itself.
Hearing aids aren’t about admitting defeat. They’re about reclaiming connection, protecting your brain, and living fully engaged. When the myths fade, better hearing begins.

FBy LIANG MEI CHEN
all is upon us, bringing with it the familiar sights and sounds of the season, it’s a timely reminder to pay attention to our health. The changing weather often ushers in an uptick in colds, flu, and other illnesses. While it’s easy to feel at the mercy of these seasonal bugs, understanding how our bodies defend themselves, and how we can support these natural defenses, can make all the difference. Think of your immune system as a well-coordinated security team, always on alert to protect you from invaders. It’s a complex network of cells, tissues, and organs that work together to defend the body against harmful substances, germs, and cell changes that could make you ill. When functioning properly, you might not even notice it at work. But when it’s compromised, that’s when you feel the effects.
The immune system includes white blood cells, antibodies, the lymphatic system, the spleen, and bone marrow. These components collaborate to identify and neutralize threats, such as bacteria, viruses, and other pathogens. Interestingly, once the immune system defeats a microbe, it keeps a record of it, allowing for a quicker and more efficient response if the same pathogen enters the body again.
While the immune system is designed to protect us, certain lifestyle factors can weaken its effectiveness. Chronic stress is one such factor. Prolonged periods of stress can lead to elevated levels of cortisol, the body’s primary stress hormone. High cortisol levels can suppress the effectiveness of the immune system, making the body more susceptible to infections and slowing down the healing process. It’s essential to find ways to manage stress effectively. Practices such as mindfulness, meditation, deep breathing exercises, and engaging in hobbies can help reduce stress levels and, in turn, support immune function.
What you eat plays a crucial role in how well your immune system functions. A diet rich in fruits, vegetables, whole grains, and lean proteins provides the essential nutrients your body needs to produce immune cells and antibodies. For instance, vitamin C, found in citrus fruits, and zinc, present in nuts and seeds, are vital for immune health. Additionally, staying hydrated is often overlooked but is equally important. Water helps transport nutrients and oxygen to cells, flushes out toxins, and supports overall cellular health.
Sleep is another cornerstone of a robust immune system. During sleep, the body undergoes repair and regeneration processes, including the production of immune cells. Chronic sleep deprivation can impair these processes, making the body more vulnerable to infections. Adults should aim for 7–9 hours of quality sleep per night. Establishing a regular sleep routine, creating a restful environment, and limiting screen time before bed can enhance sleep quality.
Regular physical activity is beneficial for overall health and plays a significant role in supporting the immune system. Moderate exercise increases the circulation of immune cells in the body, enhancing the body’s ability to detect and fight off pathogens. Activities such as walking, cycling, swimming, and yoga can be both enjoyable and effective in boosting immune function. It’s important to note that while regular exercise strengthens immunity, excessive or intense exercise without adequate rest can have the opposite effect and suppress immune function.
While a balanced diet should be the primary source of nutrients, certain supplements can help fill nutritional gaps, especially during the colder months when access to fresh produce may be limited. Vitamin D, for example, is produced by the body in response to sunlight exposure. During fall and winter, when sunlight is less abundant, supplementing with vitamin D can support immune health. Other supplements, such as vitamin C, zinc, and probiotics, may also offer benefits. However, it’s essential to consult with a healthcare professional before starting any new supplement regimen to ensure it’s appropriate for your individual needs.
Carrying excess weight can strain the body’s systems, including the immune system. Maintaining a healthy weight through a balanced diet and regular physical activity can enhance immune function and reduce the risk of chronic diseases that can compromise immunity.
Certain habits can weaken the immune system. Smoking, for instance, damages the respiratory system and impairs immune responses. Excessive alcohol consumption can suppress the production of immune cells and increase susceptibility to infections. Limiting or avoiding these habits can help maintain a strong immune system.
Social connections and mental well-being are often underestimated in their impact on immune health. Engaging in meaningful relationships, participating in community activities, and maintaining a positive outlook can reduce stress and promote overall health.
Remember, small, consistent actions can lead to significant improvements in health and well-being. Thrive, flourish, and live well!


Diane S. Litke, MD Diplomate American Board of Orthopaedic Surgery
Dr. Litke is a passionate artist, both in her spare time and as an orthopaedic surgeon. At L&W Orthopaedics, she approaches every orthopaedic problem with an eye toward restoration of function and mobility. With a deep knowledge of the inner workings of the body’s most active and important joints, Dr. Litke is able to repair most hip, knee, and shoulder problems, giving her patients the freedom to move again. Assisting her skilled hands, she uses the latest state-of-the-art robotic equipment for accuracy and precision, delivering a powerful combination of experience and technology to all of her patients.



Dr. Litke earned her medical degree at the University of North Carolina Chapel Hill. She went on to complete her orthopaedic residency at the University of South Carolina in Columbia South Carolina. She is certi ed by the American Board of Orthopaedic Surgery, and is a Fellow of American Academy of Orthopaedic Surgery and a Fellow of the American Associaion of Hip and Knee Surgeons. Dr. Litke is the medical director of the Orthopedic Department for Methodist Health System and is a liated with the Methodist Richardson Medical Center, where she is the director of the joint program. When she’s not working, Dr. Litke enjoys photography and cycling.
Please call 972.498.4791 to schedule an appointment.

By EVELYN REED

Cortisol, often referred to as the “stress hormone,” is produced by the adrenal glands in response to stress. It plays a crucial role in various bodily functions, including regulating metabolism, reducing inflammation, and controlling the sleep-wake cycle. While cortisol is essential for managing short-term stress, chronic elevation due to prolonged stress can have detrimental effects on the body. Stress can often feel like your unavoidable companion. It’s easy to feel overwhelmed. However, adopting simple strategies to manage stress and cortisol can lead to improved health and well-being.
Impact of Chronic Stress on Health
Prolonged exposure to high cortisol levels can disrupt nearly every system in the body. It can lead to:
• Weight Gain: Elevated cortisol levels can increase appetite, particularly for high-calorie foods, leading to overeating and weight gain, especially around the abdomen.
• Sleep Disturbances: High cortisol can interfere with sleep patterns, leading to insomnia or poor-quality sleep, which in turn can exacerbate stress.
• Immune System Suppression: Chronic stress can weaken the immune system, making the body more susceptible to infections.
• Digestive Problems: Stress can affect digestion, leading to issues like indigestion, bloating, or irritable bowel syndrome.
• Mental Health Issues: Long-term stress is associated with anxiety, depression, and cognitive impairments.
Understanding these effects underscores the importance of managing stress effectively.
Simple Strategies to Manage Stress
Fortunately, there are several practical ways to reduce stress and lower cortisol levels:
• Regular Physical Activity: Engaging in regular exercise, such as walking, swimming, or yoga, can help lower cortisol levels and improve mood.
• Adequate Sleep: Prioritizing quality sleep is essential. Aim for 7-9 hours per night, and establish a regular sleep routine.
• Mindfulness and Relaxation Techniques: Practices like deep breathing, meditation, and progressive muscle relaxation can activate the body’s relaxation response, counteracting the effects of stress.
• Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, and lean proteins can support overall health and help manage stress.
• Social Connections: Maintaining strong relationships and seeking support from friends, family, or support groups can provide emotional resilience.
• Time Management: Organizing tasks, setting realistic goals, and taking breaks can prevent feelings of being overwhelmed.
Incorporating these strategies into daily life can significantly reduce stress levels and improve overall health.
The Importance of Relaxation
Relaxation is more than just a luxury; it’s a necessity for maintaining health. Regular relaxation helps to:
• Restore Energy: Taking time to relax allows the body to recover from the physical effects of stress.
• Improve Mood: Relaxation techniques can enhance feelings of well-being and reduce symptoms of anxiety and depression.
• Enhance Focus and Productivity: A relaxed mind is more focused and efficient, leading to better performance in daily tasks.
• Promote Better Relationships: Managing stress through relaxation can improve interactions with others, fostering healthier relationships.
Stress is an inevitable part of life, but its impact on health doesn’t have to be detrimental. By understanding the role of cortisol and implementing simple stress management strategies, you can enhance your well-being and lead a healthier, more fulfilling life.
Josh Creel, DC is a chiropractor with Airrosti, a healthcare group that specializes in rapid recovery for soft tissue injuries by utilizing manual therapy—a hands-on treatment used to alleviate pain, improve mobility, and promote overall physical well-being. In nearly all cases, this allows for rapid recovery, complete injury resolution, and lasting results. In-clinic patients should expect to see dramatic improvement after the first visit, and most patients experience complete injury resolution in as few as three visits (based on in-clinic and Remote Recovery patientreported outcomes).
Dr. Creel has been serving the McKinney/Prosper area for 10 years and provides patients with an individualized treatment plan, and uses a variety of techniques, including joint mobilization, soft tissue manipulation, and muscle energy techniques to address specific musculoskeletal issues and promote recovery.
Dr. Creel graduated with honors from Mississippi State University. Soon after, he received his Doctor of Chiropractic degree from Parker University in Dallas, Texas. In Dr. Creel’s free time, he enjoys all types of fitness activities and spending time with his wife and three children. Dr. Creel is an active member of Lighthouse Church in Prosper, TX.

www.airrosti.com


Florian F. Dibra, MD is a board-certified, orthopedic surgeon located in Frisco, Texas who has extensive knowledge in hip and knee orthopedics and treats operative and non-operative hip and knee arthritis. He focuses on minimally invasive muscle-sparing total hip and knee replacement, anterior hip replacement, partial knee replacement, robotic joint replacement and complex hip and knee replacement revisions. Dr. Dibra is specialized in MagicKnee and MagicHip, muscle-sparing techniques with robotic technology.
Dr. Dibra graduated with honors from Villanova University in Pennsylvania. Soon after, he received his medical degree, with cum laude honors from the esteemed Jefferson Medical College in Philadelphia, Pennsylvania. He completed his orthopedic surgery training at the University of Florida. He continued at the University of Florida Health Hospital to complete his fellowship in Adult Arthroplasty with an emphasis in hip and knee reconstruction. During Dr. Dibra’s surgical training, he accomplished several publications, book chapters, and poster presentations.
Dr. Dibra’s family consists of his wife and two children. In addition to English, he is fluent in Albanian, Italian, and proficient in Spanish.



TheraCare Home Health brings the expertise and resources of a hospital to the comfort of your home.
We offer individual care including nursing, rehabilitation and social services. In addition, our expert clinicians and therapists provide specialized care for a wide range of conditions.
Our care teams strive to make the transition to home as seamless as possible, so you can focus on what’s most important – your health.


