Charles Toulson,
Pioneering a New Era in Knee Replacement
MD, MBA


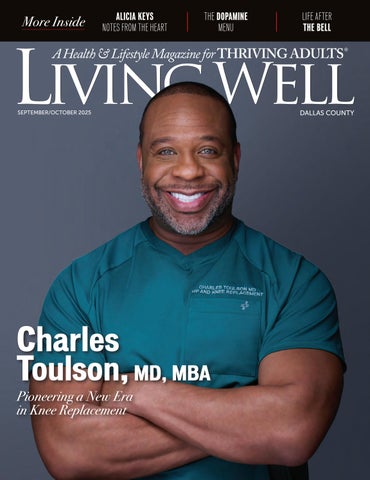
Pioneering a New Era in Knee Replacement
MD, MBA


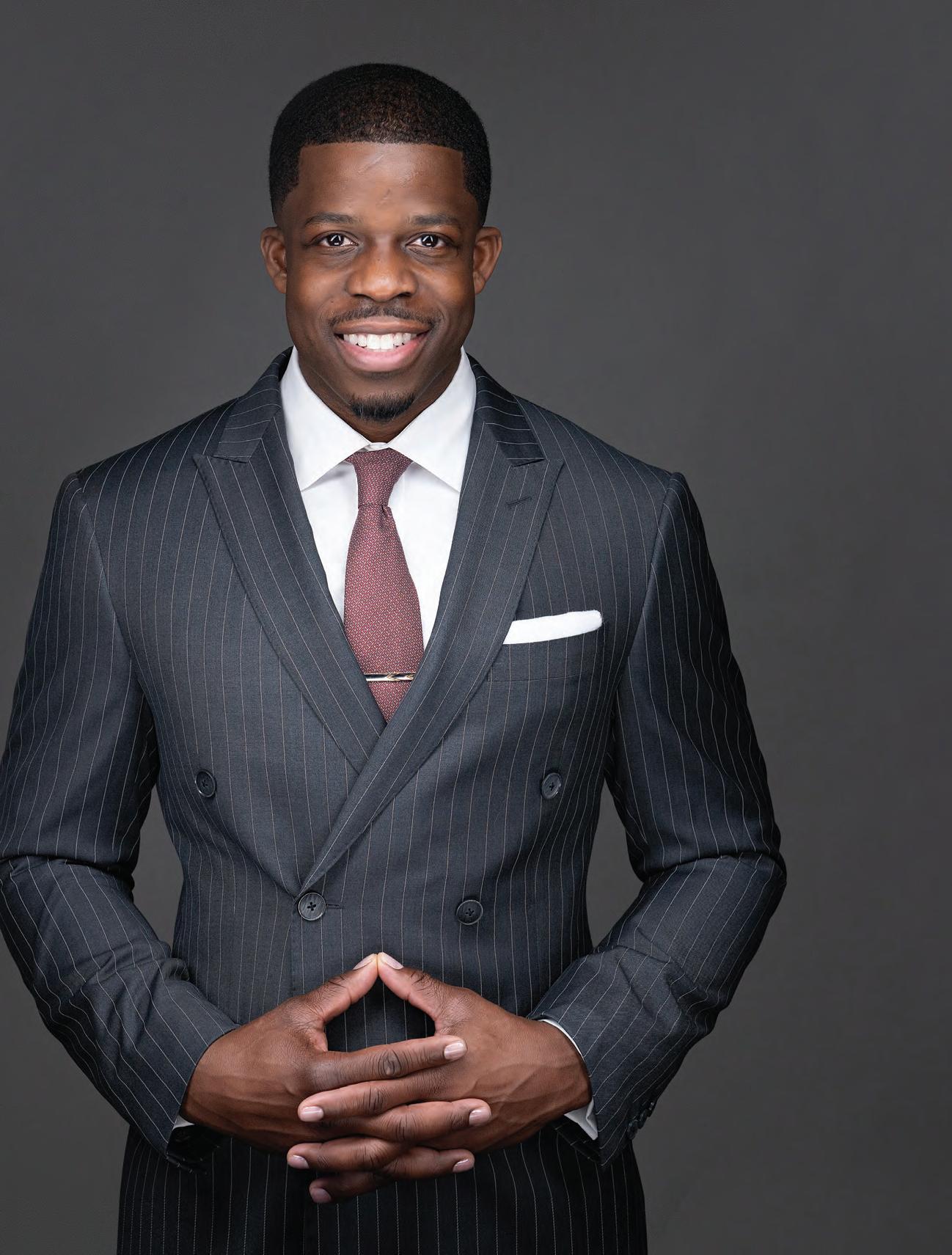
Kwame Ennin, MD, MBA, is a fellowship-trained board-certified orthopedic surgeon at Texas Joint Institute in McKinney and Plano, Texas who is an expert in hip and knee replacement procedures, adult reconstructive surgery, and nonoperative osteoarthritis care.
Dr. Ennin earned his undergraduate degree in biochemistry from the State University of New York in Stony Brook. He then went on to receive his medical education at the University of Cincinnati College of Medicine, before completing his general internship and orthopedic surgery residency at The University of Texas Southwestern Medical Center in Dallas. He is fellowship-trained in adult reconstructive surgery from William Beaumont Hospital in Michigan.
Dr. Ennin has a keen desire to educate. He is a presenter and educator to his colleagues regarding direct anterior total hip arthroplasty, total knee arthroplasty, revision total knee arthroplasty, partial knee replacement, and robotic surgery. He is committed to ensuring that the best understandings and techniques are available to all surgeons in the orthopedic community. Dr. Ennin is passionate about research. He has, throughout his career, been involved in and published numerous peer-reviewed studies.
Dr. Ennin has been a leader in the North Texas orthopedic community since 2015. He delivers personalized, patientcentered, evidence-based care for his patients. He is committed to taking care of his patient’s joints for their lifetime.
Dr. Ennin specializes in:
•Hip Replacement Surgery
•Knee Replacement Surgery
•Revision Hip and Knee Replacement Surgery
•Orthopedic Surgery
•Osteoarthritis






Total
Headache

This issue of LIVING WELL Magazine highlights the power of skill, creativity, and perseverance—qualities that shine through in each of our features.

We begin with Charles Toulson, MD, MBA, a board-certifid, fellowship-trained orthopedic surgeon whose groundbreaking SURRE KNEE approach is redefinig what patients can expect from knee replacement surgery. By combining robotic-assisted precision with a minimally invasive, muscle-sparing technique, Dr. Toulson’s method prioritizes comfort, speeds recovery, and delivers exceptional long-term results—often allowing patients to walk unassisted within days.
His dedication to excellence ensures that every patient receives the highest level of care, with outcomes that restore not only mobility but quality of life. Learn more on page 8.
From there, we turn the spotlight on Alicia Keys, a Grammy-winning artist who’s spent her career breaking boundaries in music and in life. Starting on page 24, her reflctions on self-worth, balance, and creativity might just have you rethinking how you defie success.
In The Dopamine Menu, Abigail Shaw serves up a refreshingly practical tool for lifting your mood and motivation, one small joy at a time—fid it on page 14. It’s not about overhauling your life overnight; it’s about giving yourself a gentle nudge toward better days.
Meanwhile, the article Life After the Bell, on page 43, takes us into the quiet space that follows a cancer patient’s fial treatment. It’s a moving exploration of what it means to heal, rebuild, and rediscover yourself in the chapters that follow survival.
Here’s to new perspectives, quiet courage, and the small moments that make all the difference.
Enjoy the issue!
Live well,
PRESIDENT & CEO SAM HOUSTON
VICE PRESIDENT & CFO SPRING HOUSTON
EDITOR, FEATURE WRITER & SOCIAL MEDIA SONDRA BARR
ART DIRECTOR VANESSA FRYER
ACCOUNTS MANAGER JENNIFER BEAVERS
WEBSITE LYDIA ROGERS
ADVERTISING & SALES
TEXAS: Denton County, Dallas County, Collin County
TEXAS & OKLAHOMA: Texoma Area
WRITE TO US:
Tell us who you would like to see featured on the cover, or what subjects you would like covered in upcoming editions of LIVING WELL MAGAZINE at info@livingwellmag.com
SUBSCRIPTIONS & CUSTOMER INQUIRIES
Houstons of Dallas Publishing, Inc. 102 E. Broadway, #901 Prosper, TX 75078
www.LivingWellmag.com
Phone: (214) 507-1000 Fax: (855) 248-2132
LIVING WELL MAGAZINE is a source for quality educational articles on living a healthy, vibrant life. Our focus is on connecting our readers with the latest information on a host of topics relevant to their evolving life. From cutting edge medical news and procedures to top-tier financial, legal and lifestyle information. Connecting readers to leading medical and business professionals in their community in Texas and Oklahoma.
All advertisements in this Magazine are placed by third parties. We do not control or endorse either the advertisements or their content. Further,







Texas Back Institute (TBI) has served the North Texas area in spine care for over 45 years. An uncompromising desire to put patients first and provide individualized spine care has helped change the treatment options available to patients for neck and back pain.
Today, TBI is a leader in artificial disc replacement, minimally invasive spine surgery, complex revision surgery, and treatment of spinal deformity. TBI has trained hundreds of surgeons, scientists, and allied health professionals now practicing worldwide. Its research institute employs state-of-the-art technology and is actively involved in many clinical trials, including artificial disc replacement, minimally invasive technologies, and robotic spine surgery. Texas Back Institute has remained one of the most academic practices in spine care. It is one of the largest multidisciplinary spine centers in the world, providing comprehensive care for neck and back pain. With a fully dedicated staff of board-certified orthopedic spine surgeons, neurosurgeons, physiatrists, and physical therapists, the TBI team works together to support its mission of helping patients get back to life. The 26 physicians at Texas Back Institute are leaders in the surgical
and nonsurgical treatment options for back and neck pain, from the most common outpatient procedures to the most complex cases. Thanks to the unmatched expertise of the medical staff, the advanced diagnostic testing, and an unparalleled commitment to patient care, the Texas Back Institute physicians can identify the potential cause of your pain and create a treatment plan specific to your needs.
Texas Back Institute has developed several spine specialty programs. These include the Minimally Invasive Spine Surgery Center, Center for Disc Replacement, Scoliosis and Spine Tumor Center, and Complex Back Surgery Center. These programs give patients access to highly-trained care teams who focus specifically on these areas of spine care, allowing patients in the North Texas area access to treatment options for their individual problems from physicians with extensive experience in these areas.
“At Texas Back Institute, finding the right solution for each patient and offering the least invasive treatment is core to our belief and the foundation for all treatment plans.” Dr. Michael Duffy.


ALLIANCE
3025 N. Tarrant Pkwy., Ste. 220 Fort Worth (Alliance), TX 76177
ARGYLE
310 FM 407E, Ste. 100 Argyle, TX 76226
DALLAS
12222 N. Central Expy. Pavilion II, Ste. 310 Dallas, TX 75243
3537 S. Interstate 35, Ste. 308 Denton, TX 76210
FLOWER MOUND
4370 Medical Arts Dr. River Walk Bldg. III, Ste. 230 Flower Mound, TX 75028
FORT WORTH
1650 W. Rosedale St. Ste. 301 Fort Worth, TX 76104
FRISCO
5575 Frisco Square Blvd. Ste. 400 Frisco, TX 75034
LEWISVILLE
500 W. Main St., Ste. 380 Lewisville, TX 75057
MCKINNEY
4510 Medical Center Dr., Ste. 106 McKinney, TX 75069
NORTH RICHLAND HILLS
4351 Booth Calloway Dr., Ste. 404 Fort Worth, TX 76180
CENTRAL PLANO
4001 W. 15th St. Ste. 455 Medical Office Bldg. III Plano, TX 75093
PLANO
6020 W. Parker Rd. Ste. 200 Plano, TX 75093
ROCKWALL
3164 Horizon Rd. Ste. 100 Rockwall, TX 75032
SASCHE
4650 President George Bush Turnpike, Ste. 100 Sachse, TX 75048

harles Toulson, MD, MBA, is an orthopedic surgeon who is committed to excellence. From a young age, he realized that his aptitude for medicine could help people living with chronic pain, and he dedicated his life to becoming a pioneer in the fild of orthopedic surgery.
Board-certifid and fellowship-trained, Dr. Toulson’s specialties and interests include adult hip and knee reconstruction, adult hip and knee revisions, and state-of-the-art robotic-assisted joint replacement. He is regarded by his patients and peers as one of the leading orthopedic surgeons in the country.
Exceptional Education and Training
Dr. Toulson’s impeccable educational pedigree includes a medical degree from the University of North Carolina at Chapel Hill, extensive training from Johns Hopkins Hospital, and sub-specialty training at the Hospital for Special Surgery in New York—the number-one ranked orthopedic hospital in the country.
The SURRE KNEE: Revolutionizing Knee Replacement
In keeping with his mission to deliver the best possible outcomes for his patients, Dr. Toulson is the founder of the SURRE KNEE—a groundbreaking approach to total knee replacement based on the Subvastus Rapid Recovery Experience (SURRE) technique. Ths innovative method combines the precision of robotic-assisted surgery with a minimally invasive, muscle-sparing approach that prioritizes patient comfort, quicker recovery, and exceptional long-term results.
Unlike traditional knee replacement methods, the SURRE KNEE spares the quadriceps tendon by working beneath the vastus medialis muscle. Ths reduces surgical trauma, which in turn minimizes post-operative pain, speeds up mobility, and allows many patients to walk unassisted within days of surgery.
When paired with robotic assistance, the SURRE KNEE ensures customized alignment and implant positioning, delivering a more natural feel and improved joint function.
Key Benefits of the SURRE KNEE Approach:
• Reduced pain and swelling compared to traditional knee replacement
• Faster recovery times, allowing patients to resume normal activities sooner
• Early mobility due to the muscle-sparing technique
• Highly precise implant placement using robotic technology

As the creator of the SURRE KNEE, Dr. Toulson has redefied what patients can expect from knee replacement surgery. His commitment to innovation, combined with compassionate, patient-focused care, ensures that each individual receives the highest level of treatment—with less downtime, better mobility, and superior results.
Dr. Toulson is also a forerunner in same-day or next-day joint replacement surgery. The reason for his success is his minimally invasive, muscle-sparing surgical technique. His patients are returning to their active lifestyle quicker than ever before.
Because the SURRE KNEE technique minimizes softtissue disruption and signifiantly lowers pain levels after surgery, many patients are able to walk within hours of their procedure. Ths rapid recovery allows them to safely go home the same day, avoiding an overnight hospital stay.
Patients benefit from:
• Lower risk of hospital-acquired infections
• Recovery in the comfort of their own home
• Earlier return to daily activities and physical therapy
• Reduced overall healthcare costs
By combining advanced anesthesia protocols, precise surgical execution, and thorough pre- and post-operative care, Dr. Toulson has built one of the region’s most effective and patient-friendly outpatient joint replacement programs.
“When patients come to see me with arthritis, we often try non-operative means of treatment before we talk about surgery,” says Dr. Toulson. Once non-operative options for hip or knee arthritis are exhausted, Dr. Toulson sits down with patients and details the benefits and the risks of a total joint replacement.
One of Dr. Toulson’s recent patients was suffering with severe arthritis in her knees. “I was having severe pain in my knees, I had difficulty going up and down stairs, steps, even the curb. It hurt so bad to walk, even short distances,” she says. The results of her bilateral (both) knee replacement procedure have been life changing. “ The surgery went wonderfully. I haven’t had any problems and every day it gets better and better. I can walk up the steps now getting into my home,” she says.
Highlights of success stories and the joy his patients express at the outcome of their hip or knee replacement surgeries—and how it’s changed their lives—are documented on his website, drcharlestoulson.com, with videos and moving testimonials.
It’s no surprise that Dr. Toulson has been named among the Best Doctors in Dallas for orthopedic surgery by D Magazine nine times and among the Best Orthopedic Surgeons in Collin County by D Magazine six times. He has also been awarded Best Orthopedic Surgeon for nine consecutive years by Living Magazine, along with being named Best Orthopedic Surgeon for the past five years by Living Well Magazine


Macular Degeneration
Diabetic Eye Disease
Retinal Vein & Artery Occlusions
Flashes & Floaters
Retinal Tears & Detachments
Macular Pucker/Epiretinal
Membrane
Macular Holes
Uveitis

At Texas Macula & Retina, our mission is to provide exceptional eye care with a focus on the diagnosis, treatment, and management of retinal disorders.
Dr. Adams is a board-certified Ophthalmologist and Ophthalmic Surgeon specializing in Vitreoretinal Surgery. His principal areas of interest include age-related macular degeneration, diabetic retinopathy, retinal detachment repair, macular surgery, retinal lasers, and secondary intraocular lens implantation.
Dr. Adams and his team are committed to preserving and improving the vision and overall quality of life for our patients by offering the most advanced and personalized retina care available.

By MATTHEW K. ADAMS, MD, MBA
They say your eyes are the windows to your soul. While that sounds poetic, as an ophthalmologist, I’ll tell you they’re actually windows to your genetics—and occasionally to your health. Let’s talk about what really determines eye color, whether that hazel sparkle says anything about your personality, how your iris shade might influence your risk for certain medical conditions, and whether you can, or should, change it.
What Determines Eye Color?
Eye color is primarily determined by genetics, specifically the amount and distribution of melanin (pigment) in your iris. Thik of melanin as nature’s paint. A lot of melanin gives you brown eyes; very little results in blue eyes; somewhere in the middle yields green, hazel, or gray. Multiple genes (at least 16 we know of) influence eye color, but the two main players—OCA2 and HERC2—are the main contributors.
And yes, your parents’ eye colors can influence yours, but it’s not as simple as “Mom’s eyes + Dad’s eyes = Yours.” While brown is generally dominant over blue and green, and green often trumps blue, eye color inheritance is a mix of dominant and recessive genes from both parents (and sometimes grandparents). That’s why two brown-eyed parents can have a blue-eyed child, or two blue-eyed parents can almost never have a brown-eyed child, unless there’s a rare genetic twist in the family tree.
Is Personality Reflected in Your Eye Color?
Ths is where science and folklore part ways. For centuries, people have claimed that blue-eyed folks are more “dreamy,” brown-eyed people are “trustworthy,” and green-eyed individuals have a “mischievous” streak. Fun to imagine, yes. Scientifially proven? Not so much.
Eye color comes down to biology, not behavioral wiring. Your iris shade doesn’t dictate whether you’re bold or shy—it’s your environment, upbringing, and life experiences that shape personality.
Does Eye Color Predispose You to Illnesses or Diseases?
Here’s where things get interesting—and a little serious. While personality isn’t determined by your eye color, some health risks are.
• Lighter eyes (blue, gray, green) have less melanin, which means less natural protection from UV light. Ths increases the risk for conditions like macular degeneration and ocular melanoma. If you have light-colored eyes, sunglasses aren’t optional—they’re a survival tool for your retinas.
• Darker eyes (brown) have more melanin, which
offers better UV protection. However, some studies suggest that people with darker irises may have a slightly higher risk for certain types of cataracts.
• Eye color can also be linked to rare genetic conditions, such as albinism, but for the vast majority of us, it’s just a pigment variation, not a red flag for disease.
Can You Change Your Eye Color?
Yes, sort of, but not without some caveats.
• Temporary changes: Colored contact lenses can give you an instant transformation from brown to blue or green to violet. Safe when fitted and prescribed by an eye care professional, dangerous when purchased from questionable online shops.
• Surgical options: A few experimental procedures claim to permanently change eye color, usually by implanting an artifical iris or using lasers to strip pigment. These carry serious risks, including glaucoma, inflammation, and permanent vision loss. Most Ophthalmologists (myself included) strongly advise against them.
• Natural changes: Your eye color can shift subtly over time due to aging, injury, certain medications, or medical conditions affecting the iris.
The safest “eye color change” is lighting, makeup, or wardrobe choices that make your natural eye color pop, without risking your vision.
The Takeaway
Your eye color is the product of complex genetic interactions and pigment chemistry, not a mystical personality decoder ring. While certain iris shades come with unique considerations for UV protection or disease risk, the best defense for any eye color is proactive eye care.
• Wearing sunglasses with 100% UVA/UVB protection
• Eating a diet rich in leafy greens, omega-3s, and antioxidants
• Keeping systemic health (blood pressure, blood sugar) in check
• Getting a routine eye exam every year, even if your vision seems perfect
Thik of it this way: your eye color is beautiful and unique, but it’s also just one small feature in an incredibly complex visual system. Protect it well, and those windows to your soul, whatever their color, will keep showing you the world in high defintion for years to come.
1. Rarest Eye Color?
Green eyes are the unicorns of the iris world—only about 2% of people have them.
2. Two-Tone Eyes Exist
Called heterochromia, it can be complete (two different eyes) or sectoral (one eye with two colors). Causes range from genetics to injury.
3. Eye Color Can “Bloom” in Babies
Many newborns have blue-gray eyes that darken over their first year as melanin develops.
4. Hazel Eyes = Light Show
Hazel eyes aren’t just brown or green—they shift color in different lighting due to scattered light and varying pigment.
5. Red Eyes Aren’t Just in Vampires
In rare cases of albinism, very little pigment makes blood vessels in the retina visible, giving eyes a reddish or pink hue.
6. Amber Eyes Are Not “Light Brown”
True amber eyes have a golden or coppery tone caused by a pigment called lipochrome.
7. Not All Blue Eyes Are the Same Blue
The shade depends on how the iris scatters light—just like the sky.
8. Eye Color and Night Vision
Darker eyes have a slight edge in bright sunlight; lighter eyes may be more sensitive in low light.

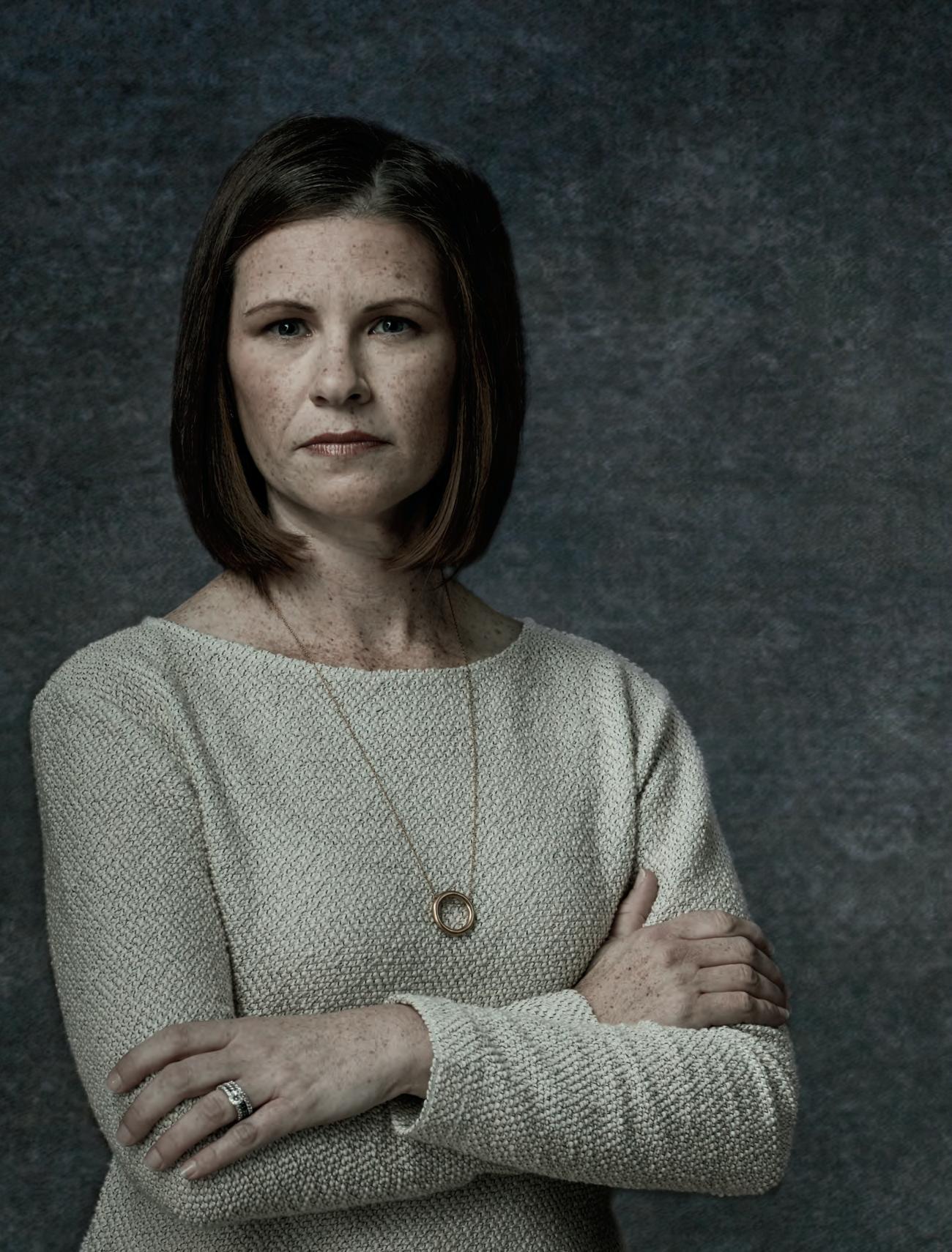
By ABIGAIL SHAW
I’ve had those days—the ones where I stare at my to-do list like it’s written in a foreign language. The coffee isn’t kicking in. The house is quiet, but my brain feels anything but calm. I want to get things done, but the motivation just isn’t there. And when I fially do something, even that feels like too much. Sound familiar?
A while ago, I stumbled across the concept of a “dopamine menu.” The idea made sense immediately. It’s basically a curated list of things that bring you joy, calm, or energy—small actions that help nudge your brain into doing the next thing. I liked the metaphor: a menu for your mood, your energy, your motivation. A little emotional room service.
So, I made one.
Not on a fancy app or color-coded spreadsheet. Just a page in my journal, scribbled during one of those afternoons where I felt low-key stuck. I grouped the things I love into rough categories—quick things, bigger things, and a few guilty pleasures that I decided to stop feeling guilty about. And here’s what happened: It worked.
I didn’t become wildly productive or start waking up with superhero energy. But on days when I felt that heavy sense of “blah,” I didn’t have to think so hard. I’d glance at my list and pick something that felt doable. And slowly—ten minutes at a time—my energy returned. Not always fast, but reliably. Here’s what I’ve learned since creating that fist dopamine menu, and why I think it’s worth making one for yourself.
Why a Dopamine
Dopamine is often called the brain’s “reward” chemical, but it’s more nuanced than that. It helps regulate things like motivation, attention, and movement. When you anticipate or experience something pleasant—hearing a favorite song, seeing a loved one’s face, even finshing a puzzle—your brain releases dopamine as a kind of “Yes, more of that, please.”
It turns out, many of the things we have to do every day (answering emails, folding laundry, paying bills) don’t generate much dopamine at all. And when we’re tired or stressed or mentally foggy, our brains need even more coaxing to get into gear.
The beauty of a dopamine menu is that it gives you a small hit of pleasure or satisfaction fist—or lets you pair it with something more mundane. It’s like warming up your brain before a workout.
How
My fist version had four sections: Quick Hits, Every Day Joys, Paired Pleasures, and Treats. That’s what worked for me. You can call your categories whatever you want.
My Quick Hits list includes things like:
• Stepping outside barefoot for a few deep breaths
• Putting on a song that makes me nostalgic
• Sending a funny meme to a friend
They’re easy, almost effort-free, and they remind me what feeling good feels like.
Every Day Joys are the things I love but sometimes forget about:
• Watering my plants and checking on their new growth
• Journaling for ten minutes with no filter
• Making a fancy version of my afternoon tea (complete with lemon or honey or a cute cup)
Paired Pleasures are things I use to make boring tasks less boring:
• Listening to a podcast while folding towels
• Burning a favorite candle while answering emails
• Watching the birds out the window while doing leg stretches
Treats are exactly what they sound like. A square of dark chocolate. Rewatching a favorite movie scene. A long bath with good music. Thigs I used to label as “unproductive,” but now see as valuable tools. Once I had it all down, I taped it to the inside of my planner. It’s not always beautiful, but it’s mine—and when I need it, I don’t have to overthink. I just pick something.
It’s Not Just for Lazy
Some days, I’m already in a groove. I don’t need a dopamine jumpstart. But the menu still helps me maintain balance. I’ll choose something from it when I feel my mood dipping, when I hit a wall mid-afternoon, or even as a way to reward myself for finshing a tough project. What surprised me most is how this approach softened the way I talk to myself. Instead of “What is wrong with me?” I ask, “What would help right now?” That shiftalone is worth a lot. And it’s flexble. As the seasons change, so does my list. In the fall, I add things like baking or switching out the porch cushions. In summer, I might put “early morning walk before it gets hot” or “ice water in a pretty glass.”
Let me be clear: a dopamine menu isn’t a magic cure. If you’re dealing with grief, burnout, depression, or deep fatigue, no list will fixthat. And there are days when the best I can do is one small thing—and
that’s okay. Ths tool isn’t about being endlessly happy or squeezing productivity out of every moment. It’s about offering your brain a lifeline when it feels stuck. It’s permission to say, “I can’t do everything, but I can do something.” It’s a nudge toward the light.
Don’t overthink it. Grab a piece of paper, and write down 10 things that make you feel:
• Peaceful
• Energized
• Cheerful
• Clear-headed
• Capable
Then sort them into categories that feel right to you. Make a pretty version if that’s your style, or keep it scrappy and real. Post it somewhere you’ll see it. You don’t have to use it every day. You don’t have to “earn” the items on it. Just give yourself the option. That alone helps rewire the belief that you’re stuck. And if it starts feeling stale? Rewrite it. Refresh it every month. I often do a new version when I notice I’m stuck in a scrollandsnack spiral that isn’t really making me feel better.
Here’s a peek at some of the items that have lived on mine lately, in case you want ideas:
• A walk to the end of the block with my camera, just to see what’s blooming
• Thee yoga poses I know by heart
• Sending an old photo to a sibling
• Coloring in a tiny corner of an adult coloring book
• Reading a few pages of a favorite memoir
• Lighting a lemon candle while working
• Watering the plants with music playing
• Dancing around the kitchen (no witnesses allowed)
Some days, I do one. Some days, I forget. But the menu is always there— waiting quietly, like a friendly nudge. Start small. Pick one thing. Let it shiftthe next few minutes. Sometimes, that’s all you need to begin again.

It’s basically a curated list of things that bring you joy, calm, or energy— small actions that help nudge your brain into doing the next thing.
Dr. Scott Nodzo is a nationally recognized orthopedic surgeon specializing in advanced hip and knee replacement. A Fellow of both the American Association of Hip and Knee Surgeons and the American Academy of Orthopaedic Surgeons, Dr. Nodzo serves on national committees and as an Editorial Board Member and reviewer for The Journal of Arthroplasty. He is widely published and has contributed to leading orthopedic textbooks, including The Technique of Total Knee Arthroplasty and Operative Techniques in Orthopaedic Surgery.
Dr. Nodzo specializes in:
• Robotic-Assisted Hip and Knee Replacement Surgery
• Robotic-Assisted Partial Knee Replacement Surgery
• Augmented Reality-Assisted Hip and Knee Replacement Surgery
• Complex Revision Hip and Knee Replacement


Dr. Courtney is a board-certified orthopedic spine surgeon located in Plano, Texas. A Louisiana native, he attended Louisiana State University for medical school, and completed residency at Texas A&M followed by a fellowship at the Florida Neck and Back Institute.
SPECIALTIES:
• Back Pain
• Neck Pain
• Spine Pain
• Disc Replacement
• Microdiscectomy
• Spinal Fusion
• Minimally Invasive Surgery
• Steroid Injections
• Physical Therapy
“I believe in treating each of my patients with honesty, dignity, and respect. My patients come away from our shared interactions feeling confident, assured that they are truly in the best hands. Throughout my career, I have remained laser-focused on providing world-class care and innovation to the patients I treat on a daily basis. I look forward to getting to know you!”



• Comprehensive Adult Eye Care
• Light Adjustable Lens, Odyssey™, Symfony®, PanOptix, Vivity® and the Eyhance IOL
• Management of Dry Eye, Glaucoma & Corneal Disease
• Eyelid Surgery & Botox®
• Laser Vision Correction, EVO ICL™




Convenient locations to serve you in Allen, Arlington, Dallas, Frisco, Greenville, McKinney, Mesquite, North Fort Worth, Plano, Richardson, and Rockwall.

Brian Nwannunu, MD, MS, is an orthopedic surgeon specializing in hip and knee replacement. He care for patients at Texas Joint Institute in Allen and in McKinney, Texas.
Dr. Nwannunu, a native of Dallas, graduated Valedictorian from the High School for Health Professions at Townview Magnet Center in DISD. He then earned his bachelor’s degree in Biology at Morehouse College in Atlanta, Georgia, where he was part of the Morehouse College Honors Program. Upon graduation, he completed his master’s degree in Physiology at Georgetown University in Washington, D.C., with a concentration on complementary and alternative medicine. Dr. Nwannunu then graduated with his medical degree from Howard University College of Medicine in Washington, D.C., where he was inducted into the Alpha Omega Alpha Honor Medical Society.
Dr. Nwannunu completed his residency in orthopedic surgery at the John Peter Smith Health Network in Fort Worth, Texas, before pursuing additional training with a fellowship in adult reconstruction at Baylor College of Medicine in Houston, Texas. In addition to his clinical training, Dr. Nwannunu enjoys mission work abroad, providing medical care and health education to populations in need. He is also one of the few official Jiffy Knee™ surgeons in the North Texas area.
He is a member of the American Medical Association, National Medical Association, American Academy of Orthopaedic Surgeons and the American Association of Hip and Knee Surgeons.
When not working, Dr. Nwannunu enjoys basketball, weight training, outdoor activities, attending art and music festivals, traveling, world news, and reading.


Board-Certified Foot & Ankle Orthopedic Surgeon and Founder of the Orthopedic Institute of North Texas (OINT), Dr. Kane is internationally recognized for his expertise in foot and ankle care. He is a published author, global lecturer, and Professor of Surgery at Texas A&M Health Science Center College of Medicine, actively teaching the next generation of orthopedic surgeons.
Dr. Kane specializes in:
• Bunion and hammertoe correction
• Complex foot and ankle reconstructive surgery
• Surgical and non-surgical treatment of foot and ankle disorders
At the Orthopedic Institute of North Texas, Dr. Kane and his team’s goal is your return to normal activity. We provide surgical and nonsurgical solutions designed to resolve your pain.
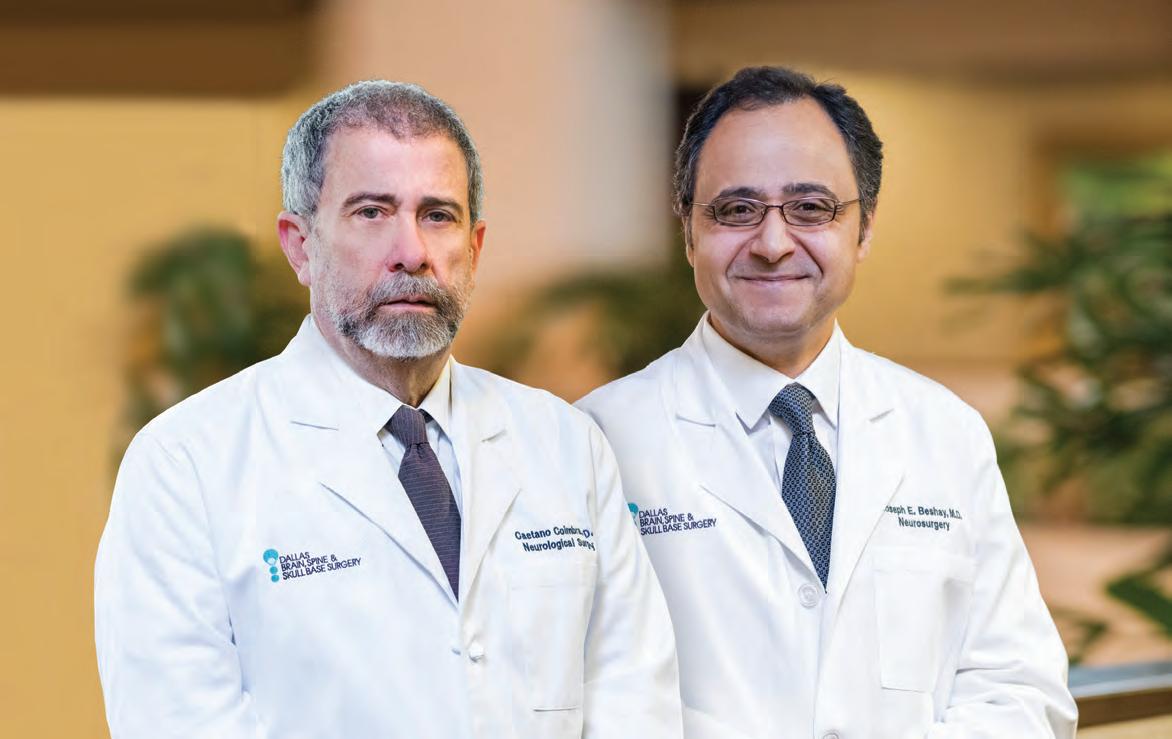
Dallas Brain, Spine and Skull Base Surgery is a neurosurgical practice that offers over 40 years of experience providing an innovative and collaborative state of the art approach to the care of patients with challenging neurological problems from around the world. Dr. Beshay and Dr. Coimbra have developed unique expertise in the treatment of brain tumors becoming the referral destination for the treatment of patients, especially those with complex or difficult to access tumors. They have also shown a commitment to the development of minimally invasive neurosurgical procedures including the most modern expanded trans–nasal endoscopic skull base surgical techniques and focused extradural approaches to skull base tumors.
Dr. Beshay’s interests include tumors of the brain and spine, minimally invasive spine surgery, complex spinal reconstruction, and epilepsy surgery. In addition to surgical treatment of intracranial and spinal disease, he has an interest in neurological bleeding and its reversal. Dr. Beshay’s clinical interests include: benign and malignant brain tumors, neuroendoscopy, epilepsy surgery, intracranial hemorrhage, cranial/ spinal trauma, minimally invasive spine surgery, complex spinal reconstruction with an interest in C1–C2 and occipito–cervical junction disease.
Dr. Coimbra restricts his practice mostly to intracranial neurosurgery. This selective tertiary practice has fostered the opportunity to develop unique expertise and commitment to the treatment of malignant and benign brain tumors. He is an expert in the minimally invasive resection of the most complex skull base tumors, including meningiomas, acoustic neuromas, and pituitary tumors. He employs CyberKnife radiation therapy, endoscopic endonasal techniques, and an array of focused skull base approaches to create a customized treatment plan for each patient in his practice. These innovative approaches allow resection of deep, difficult, and complex tumors with minimal brain tissue manipulation and maximal preservation of function.
Dr. Coimbra and Dr. Beshay believe in customized patient care and a team approach to medicine with attention to careful selection of the least invasive and most effective treatment for each patient. Their commitment to this philosophy has resulted in maximum preservation of function, less discomfort, shorter hospital stays and durable favorable outcomes for their patients.


Dear Olivia,
As a family, we believe it is time for hospice services, but there are many hospices to choose from! How do we start to decide which hospice is right for us?
~Overwhelmed with Options
Dear Overwhelmed with Options, Selecting the right hospice for your loved one is crucial, and you need to ensure that you choose a provider that aligns with your values and care goals. Ask the following important questions:
1. How often do staff members visit? You must ensure that nurses, chaplains, social workers, home health aides, and doctors are available to provide comprehensive support during and after business hours.
2. Do you offer all four levels of care? It’s essential that the hospice provides:
• Routine Care : The most common type of care, delivered in the patient’s home.


• Respit e Care : Temporary relief for caregivers, allowing them time to recharge.
• Continuous Care : A nurse on-site aroundthe-clock for managing difficult symptoms.
• General Inpatient Care : Higher-level support for severe symptoms when home care is insufficient.
3. Does your doctor make house calls? Confirm that the hospice offers home visits from doctors when necessary.
4. How can I assess your quality of care? Use Medicare.gov/care-compare to check the quality scores for Medicare-certified hospices.
These questions are vital in ensuring you choose the best hospice for your loved one. Don’t settle for anything less than the support and care your family deserves.
~Olivia






When Alicia Keys steps onto a stage, there’s an unmistakable shiftin the air. It’s not just the velvet-rich tone of her voice or the way her figers dance across the piano keys—it’s the gravity of a woman who has spent her life mastering not only her craft,but also herself. Over two decades into a career that has redefied R&B and soul, Keys continues to expand her artistry, her activism, and her influence—all while living life on her own terms. Keys has long been a cultural touchstone. From her 2001 breakout hit “Fallin’” to anthems like “No One” and “Empire State of Mind,” her songs have served as soundtracks for love stories, heartbreaks, and moments of triumph. Her career may be defied by chart-topping hits and armfuls of Grammys, but the heart of her journey is rooted in resilience, staying true to herself, and an unshakable drive to keep evolving.
Soulcare, selfworth, and the rituals that keep the Grammy-winning artist grounded.
By SONDRA BARR

Born Alicia Augello Cook on January 25, 1981, in New York City, Keys grew up in the vibrant but gritty neighborhood of Hell’s Kitchen. Raised primarily by her mother, Terria Joseph, she was surrounded by a mix of cultures, music, and street energy that would later infuse her art. At age 4, she appeared on The Cosby Show as Rudy Huxtable’s friend, but her true calling emerged when she began piano lessons at 7.
“I was drawn to the piano like it was a long-lost friend,” she’s recalled. Classical training dominated her early years, but by her teens, she was blending Chopin with jazz, soul, and the hip-hop beats of her city. By 14, she was composing her own songs; at 16, she graduated as valedictorian from Manhattan’s Professional Performing Arts School.
It didn’t take long for the industry to notice. Legendary music executive Clive Davis signed her to Arista Records in 1998, later bringing her to his new label, J Records. Her 2001 debut album, Songs in A Minor, was a revelation—a fusion of raw emotion and sophisticated musicianship. The record sold over 10 million copies worldwide and earned Keys five Grammy Awards, including Best New Artist and Song of the Year.

Here (2016), and Alicia (2020) reflcted both personal and creative evolution. “Every time I write a song, I never know how it happens,” she told NPR. “It happens, and then I’m on my knees thanking God.”
Her most recent musical chapter includes Keys (2021), the holiday album Santa Baby (2022), and an entirely new frontier—Broadway.
After more than a decade in development, Keys’s semi-autobiographical jukebox musical Hell’s Kitchen debuted Off-roadway in 2023 before moving to Broadway in 2024, earning 13 Tony nominations. Inspired by her teenage years, the show tells the story of Ali, a spirited 17-year-old navigating life with her single mother in ’90s New York.
“It’s intentionally not autobiographical,” Keys told Sunday TODAY’s Willie Geist. “Ali is a more gullible, naive version of myself. At its heart, it’s a love story between a mother and a daughter.”
The production blends her chart-topping hits with new compositions, reimagining songs like “Fallin’” in fresh contexts. Seeing icons like Oprah Winfrey and Michelle Obama in the audience was, she admitted, surreal. “It’s a new experience, a new challenge,” she told Today. “I’m a newbie in this world.”
Following her debut, Keys proved she was no one-hit wonder. Th Diary of Alicia Keys (2003) delivered classics like “If I Ain’t Got You” and “You Don’t Know My Name,” winning her four more Grammys. A collaboration with Usher, “My Boo,” dominated the charts in 2004, and in 2005, her MTV Unplugged album showcased her in stripped-down, soulful form.
In 2007, As I Am brought us “No One,” another Grammy-winning anthem. That same year, she and Jack White recorded “Another Way to Die” for the James Bond film Quantum of Solace. Her 2009 collaboration with Jay-Z on “Empire State of Mind” became a love letter to her hometown and a global hit.
Albums like The Element of Freedom (2009), Girl on Fire (2012),
For Keys, art and activism are inseparable. In 2003, she co-founded Keep a Child Alive, which provides treatment and support for families affected by HIV/AIDS in Africa and India. She has been a vocal advocate for racial justice, launching her Moonshot initiative to push for systemic reforms in underserved communities.
She’s also committed to empowering women and girls, often speaking about self-worth and self-expression. “Beauty is individuality and wisdom,” she told Glamour. “It’s a deep-down knowing of yourself.”
Her activism has a personal dimension, too. Songs like “Blended Family” reflct her role as stepmother to her husband Swizz Beatz’s children, offering a rare, empathetic portrayal of modern family life.
In 2016, Keys made headlines by stepping away from makeup for public appearances, a decision she described as a rebellion against societal expectations. “It’s not about makeup or no makeup,” she explained to InStyle. “It’s about how you want to express yourself, and what boundaries you want to set for yourself.”
Ths philosophy inspired Keys Soulcare, her skincare and lifestyle brand launched in 2020. The line promotes rituals of self-care, pairing clean beauty products with affirmations printed on each package. “Soulcare and beauty are connected,” she told Forbes. “When you are true to yourself, your authentic voice pours out.”
These days, Keys moves fluidly between her roles as artist, businesswoman, and mother, weaving them together into a life that feels entirely her own. She and Swizz Beatz, whom she married in 2010, are raising two sons, Egypt and Genesis. She encourages them to listen to their own voices—advice that took her years to embrace herself.
“I used to ask 75 people for validation before deciding what I wanted,” she admitted. “Now, I’m learning to be comfortable with my own opinion.”
She credits meditation and intentional stillness for helping her stay grounded. “It’s noisy as hell out there,” she says. “Ritual creates space so you can hear yourself.”
When asked what’s next, Keys doesn’t rattle offcareer milestones. Instead, she talks about cultivating space— being “just as productive by not moving as much.” It’s a lesson in living well that she’s earned through years of both triumph and self-interrogation.
“I want to be comfortable with the non-work, the non-movement,” she reflcts. “Sometimes I’m killing it, sometimes I fall off. And that’s okay. It’s about giving myself grace.”
From a young pianist in Hell’s Kitchen to a global icon rewriting the rules of beauty, artistry, and activism, Alicia Keys has built a life that harmonizes ambition with authenticity. Her journey is a reminder that true success isn’t just measured in awards or accolades—it’s in the ability to live fully, love deeply, and stay true to yourself, no matter how loud the world gets.
In other words, Alicia Keys is still—and always will be—a girl on fie.







VUDHI SLABISAK, MD OrthopaedicSpineSurgeon





BRUCE MARKMAN, MD
OrthopaedicSurgeon&Sports MedicineSpecialist



JAMES STANLEY, MD OrthopaedicSpineSurgeon






STEVE HONG, MD Interventional Pain ManagementSpecialist











AMIR MALIK, MD Neurosurgeon









KHAWAJA IKRAM, DO OrthopaedicSurgeon






RAHUL BANERJEE, MD OrthopaedicSurgeon

BRIANA HODGSON, PA-C
OrthopaedicSurgery PhysicianAssistant
If you’re suffering from pain or an athletic injury, schedule an appointment with your preferred NTOS location for effective, compassionate treatment.

» Staffed by 2 Licensed, Doctors of Audiology
» Hearing Aid Fittings, Maintenance and Repairs
» Invisible Fittings/Open Fittings
» Evaluation Period On All Hearing Aids
» Hearing Evaluations For All Ages
» Wireless/Connectivity Hearing Solutions
» Battery Purchase Programs
» Custom Ear Protection
» Assistive Devices



Courtesy HEARING SERVICES OF McKINNEY
Hearing is about so much more than catching the punchline in a conversation or hearing a favorite song clearly. The tiny structures inside your ears connect directly to the health of your brain, influencing how sharp you feel, how steady you walk, and even how connected you feel to the world around you.
Research is showing that untreated hearing loss doesn’t just make communication harder—it’s linked to faster cognitive decline, dementia, depression, and anxiety. In fact, a long-term Johns Hopkins study found that people with mild hearing loss had about twice the risk of developing dementia, moderate loss tripled the risk, and severe loss increased it fivefold. That’s not just a small correlation; it’s a clear signal that the brain and ears are working together in ways we can’t afford to ignore.
When hearing starts to fade, the brain has to work harder to fill in the blanks. Ths extra mental strain can leave fewer resources for memory and problem-solving. Over time, that constant effort can contribute to cognitive decline. It’s called the “cognitive load” effect, and it’s one of several ways hearing loss impacts brain health. Another is auditory deprivation—when the brain receives less sound input, it can lead to changes in brain structure, particularly in areas responsible for memory and language.
There’s also the human side. Struggling to hear often leads to pulling back from conversations, social gatherings, and community life. That isolation has its own risks. Studies have shown loneliness can raise the risk of dementia by about 40%. Add in the frustration of missed conversations, and it’s no surprise that untreated hearing loss is also associated with higher rates of depression and anxiety.
Here’s the encouraging news: treating hearing loss can help lower those risks. A major study published in The Lancet in 2023 found that older adults at high risk for dementia who used hearing aids, along with audiologist-guided support, slowed their rate of cognitive decline by nearly 50% over three years compared to a control group. Other large reviews of research have found that hearing-aid or
cochlear implant use can cut the long-term risk of cognitive decline by almost 20% while also improving day-to-day mental sharpness.
The benefits don’t stop at brain health. Wearing hearing aids can reduce the chances of developing depression or anxiety and even lower the risk of serious falls. That’s because your hearing plays a key role in spatial awareness—helping you know where you are in relation to your surroundings.
The decision to get your hearing checked isn’t just about improving how well you hear the TV or the phone. It’s about protecting your overall well-being. Early detection is especially important because hearing loss often develops gradually. Many people don’t realize how much they’ve adapted—turning up the volume, avoiding noisy places, leaning on lip reading—until the change in hearing is undeniable. By then, the brain may have already been compensating for years.
Modern hearing aids are far from the bulky, squealing devices of decades past. Today’s models are discreet, comfortable, and smart— able to filter background noise, stream calls and music, and adapt automatically to different environments. More importantly, they can restore the clear, effortless hearing that allows the brain to focus on what matters: understanding, remembering, and connecting.
If you’ve been noticing changes in your hearing—needing to ask people to repeat themselves, missing parts of conversations, or feeling exhausted after social interactions—it may be time to make an appointment with an audiologist and have your hearing tested. Even if you’re not sure there’s a problem, a professional evaluation from an audiologist can give you a clear picture of your hearing health and whether hearing aids could help.
The sooner hearing loss is addressed, the more you can protect not just your ability to hear, but also your cognitive health, mood, and quality of life. Your ears may be the entry point for sound, but they’re also guardians of your mind. Schedule your hearing check-up today with Hearing Services of McKinney and take the fist step toward protecting both your hearing and your brain health.



Dr. Bilal Mahmood is a Cleveland Clinic trained orthopedic surgeon with fellowship training in adult hip and knee reconstruction and joint replacement. He specializes in anterior hip replacement, robotic joint replacement, hip resurfacing, total knee replacement, partial knee replacement, minimally invasive joint replacement, same-day joint replacement, complex hip and knee deformity, revision joint replacement, hip and knee arthritis, osteonecrosis, hip dysplasia, and femoroacetabular impingement (FAI).
Outside of work, Dr. Mahmood enjoys spending time with his wife and children. His hobbies include alpine skiing, baseball, hockey, biking, and travel.
He is involved with local outreach organizations for medically underserved populations. He is also involved in research and innovation to advance hip and knee joint replacement.


By WILLIAM PARKER
Studies show that consciously retraining the habits around air intake can sharply reduce the frequency of belching.
On more than one occasion, I have found myself excusing a sudden, unexpected belch—with more embarrassment than alarm. They can come from seemingly nowhere, right in the middle of a conversation. If you’ve experienced similar moments—or bloating, discomfort, or that mysterious feeling of air needing to escape—know that you’re far from alone. Belching is simply your body’s way of releasing trapped air in the upper digestive tract, but when it becomes frequent or disruptive, it may point to underlying habits or health concerns.
I’ve learned from medical professionals and trusted resources like the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) that most people burp up to thirty times a day—anything more can feel distressing or socially awkward. Often, those extra belches are linked to swallowed air, which commonly happens when eating too fast, talking while chewing, sipping through a straw, chewing gum, or even when stress encourages rapid breathing or gulping. These are all habits that invite too much air into the stomach.
Chronic belching may also be connected to acid reflux—or GERD (gastroesophageal reflux disease)—where stomach acid escapes back into the esophagus because the lower esophageal sphincter relaxes too often. Medical News Today reports that GERD affects about one in five adults, and reflux can trigger more burping as the body tries to force air upward to relieve the discomfort.
Another pattern sometimes overlooked is supragastric belching—a learned behavior where someone frequently draws air into the esophagus and immediately expels it, without letting it reach the stomach. According to UCLA Health, this type of belching often accompanies stress or habit, and speech therapy with behavioral retraining can offer substantial relief.
Gastritis—sometimes due to an H. pylori infection— can inflame the stomach lining and lead to increased belching, especially when digestion slows or becomes uncomfortable. Stomach inflammation frequently triggers gas release as your body reacts to irritation.
When belching becomes frequent, noticeable, or is paired with symptoms like heartburn, regurgitation, nausea, chest tightness, or bloating, it’s time to dig deeper. I recommend starting with your primary care physician— they can evaluate your symptoms and, if needed, refer you for an endoscopy or acid monitoring to pinpoint the cause.
If GERD is suspected, a gastroenterologist is the right specialist. Together with lifestyle guidance—like weight management, avoiding caffeine, spicy or fatty foods, not lying down after meals, and modifying medication—doctors can often help restore comfort. Many patients experience lasting improvement when dietary and behavioral changes combine with therapies such as antacids, H2 blockers, or proton-pump inhibitors, as described in resources like Verywell Health.
In cases involving supragastric belching or aerophagia, many people benefit from working with a speech-language pathologist or a behavioral therapist. Studies show that consciously retraining the habits around air intake can sharply reduce the frequency of belching.
Initially, I thought burping was just a minor annoyance. Until a gastroenterologist friend reframed it for me: “It becomes a problem when belching becomes your body’s default response to stress or discomfort, instead of a reaction to fullness.” That shifted everything.
I started making incremental changes—slowing down at meals, favoring water over soda or coffee, giving up gum and mints—and I noticed a signifiant decline in belching. I slept better, digestion felt lighter. When I felt bloated at night, I would lie on my side or pull my knees in toward my chest until relief came. Mount Sinai recommends such positions for easing trapped gas.
At the end of the day, burping is usually normal—but if belching seems to be increasing—or feels more than just quirky—don’t let embarrassment keep you from seeking answers. Reach out to your physician. Consider asking for a gastroenterology consultation. You don’t have to navigate it on your own; expert support is available, and you deserve relief and the comfort of meals you can enjoy without worry.
Burping doesn’t have to be a source of shame; it can be a source of insight—a message your body sends when something feels off. Whether it’s placing pause on meals, tweaking habits, or reaching out for medical help, there's nothing wrong with honoring that signal.
So when the question echoes within—“Why am I burping?”—let it become an invitation to listen, not panic. Notice the patterns. Make a shift.Seek support. It’s perfectly fie to ask for answers—or to take one small step forward to feel more at ease again. And that’s an answer worth exploring.





Board-Certified Orthopedic Surgeon | Hip & Knee Replacement Specialist
Dr. Yousuf is a nationally recognized leader in advanced hip and knee surgery, offering robotic-assisted procedures, partial knee replacements, and the anterior hip approach to help patients fid relief from joint paint and move freely again.
He serves as Medical Director of Hip & Knee Surgery and Orthopedic Robotics at Baylor Scott & White (East Region) and has been honored among the B est Doctors in Dallas & Collin County. His dedication to innovation and patient care continues to set the standard in orthopedic excellence.
3800 Gaylord Pkwy., Ste. 810 Frisco, TX 75034
5220 W. University Dr. Physician Bldg. 2, Ste. 300 McKinney, TX 75071
4716 Alliance Blvd. Pavillion II, Ste. 600 Plano, TX 75093
7217 Telecom Pkwy., Ste. 100 Garland, TX 75044




WE OFFER CUSTOM AND STERILE MEDICATION COMPOUNDING.
At Syed, we’re not your typical community pharmacy. We are committed to providing top-notch pharmaceutical services and wellness products to ensure you and your family stay healthy and happy. We have great selections of over-the-counter medicines, medical equipment, assortments of nutritional supplements, and many more health care services.

Our experienced and friendly staff are here to support you with personalized care and expert advice. Some of our services are:
Compounding Services
Personalized compounding tailored to you—now offering sterile compounding to support your care.
• Eye drops, Injections, etc.
• Hormonal needs (Testing of both men and women)
• Pet needs
• ODT/Troches/Capsules
• Creams, Ointments, Lotions, Patches
• Weight loss medications
Vaccination Services
Walk-ins welcome! We offer a variety of vaccinations.
• Seasonal flu
• Shingles
• Hepatitis A/B
• Tdap, RSV, MMR
• Travel Vaccines
• Pneumonia
• COVID-19
• & More!
Weight Loss
Flu season is here— protect yourself with a walk-in vaccine today.
Feel good in your body! Our weight loss program is designed to provide you with the support, education, and motivation you need on your unique journey. We are proud to offer comprehensive weight loss packages including our highly popular weight loss injections.
SyedPharmacy.com • (469) 206-2077
18484 Preston Road, #300 Dallas, TX 75252
Point-of-care Treatment
Quick and convenient testing services while saving time and money by avoiding unnecessary urgent care needs.
• Walk-in service
• Covid Rapid / PCR
• RSV / Covid Antibody testing
• Flu A and B / Strep
• HIV & STD testing
• Diabetes HbA1c testing
Medical Equipment, Sales & Supplies
Let us help you maintain an active and more independent lifestyle with our line of durable medical equipment and abundant selection of other medical supplies.
• Wheelchairs, Scooters
• Walkers, Rollators, Canes
• Bath chairs, Bedside Toilets
• Long and Short-Term DME Rentals
• Compression socks
• Sports/Injury braces and supports
• Incontinence supplies
• Diabetes management supplies
• …and more!

By JULIA PORTER
There was a time when the dinner table was the heart of our homes—a place where daily stories were shared, connections were reinforced, and support was offered effortlessly. Now, in many American families, that ritual has quietly faded away.
In those early years, our dinner table wasn’t about fancy meals or perfect etiquette. It was about presence. We’d trade off—ne of us grabbing the ice for the glasses, another setting the table, someone always asking, “How much longer?” Mom would ask about my day, my dad shared stories, and my siblings and I, in turn, joined the conversation. Sometimes we laughed, sometimes we argued, but always, we processed the day together. Those conversations taught us to listen, to speak honestly, and to be seen in a family setting.
Today, so many of us move through evenings with individual routines: someone catches up on work, another scrolls their phone, after school events running long, and dinner becomes a solo or drive-thru affir. The family table becomes a catchall—unopened mail, lap-
builds resilience, trust, and understanding over time.
tops, groceries—its original purpose buried beneath modern clutter. Meals are eaten on the go, conversations scattered, and the beautiful architecture of daily sharing often vanishes.
Growing up, I realized that simple mealtime dialogue matters. One nationally representative study of parents in the United States (Project EAT) found that families who eat together regularly report stronger emotional bonds and better awareness of what’s going on in each other’s lives. Teens, for example, who share meals with their parents are less likely to engage in risky behavior and more likely to feel heard and supported.
In my own household, that shifthappened gradually. As schedules grew complicated, evenings turned into fragments. My daughter recalled glimpses of our table—occasional shared plates, curt greetings, and silent meals. The space lost its meaning, and so did we, just a little bit. It didn’t seem like a big deal. It became our new routine.
It was only when I paused to think about what was missing that I noticed. I missed hearing about her day. I longed to share stories of small wins or quiet frustrations. My husband sometimes drifted upstairs after eating his dinner, and I found myself lingering in the kitchen with mine—longing for connection.
Reclaiming that ritual didn’t require elaborate dinners—just intention. One evening, I invited everyone over for supper without expectation or agenda. No phones, no background noise. Conversation felt awkward at fist. But slowly, the table began to hum again.
My daughter shared about projects at school. My husband talked about ups and downs at work. I shared bits of my world too. The shift wasn’t dramatic, but it was signifiant. We weren’t just eating; we were reconnecting.
Family therapists often describe mealtime as “talk therapy by stealth.” In that structured, predictable setting, children feel safe sharing fears and joys, and parents model emotional openness. That regular contact builds resilience, trust, and understanding over time.
We weren’t aiming for perfect meals—some nights were sandwiches, others were store-bought takeout, and occasionally cereal. What mattered was sitting down together, unplugged. “Dinner’s ready! I’d love to hear your day.” No corrections or life lessons—just conversation. Some moments were joyful, others awkward or thoughtful. The act itself created space to share, to question, to laugh, and occasionally to heal.
Not everyone has a formal dining room—and we didn’t always ei-
ther. At times, we gathered around the kitchen counter or nestled in folding chairs at a small table. What mattered was not the setting, but the consistency. Even twenty-minute meals offer emotional benefit, if the table holds presence.
I noticed how habits shifted over time. Our children grew older, some moved away, but I ensure the weekly table habit continues— sometimes for holiday dinners, sometimes even via video call. The ritual holds meaning, no matter the changes around us.
It’s not that family life becomes flawless. Conflits still arise. Tiredness still sets in. But returning to the dinner table models a valuable lesson: showing up matters. When we eat together, listen without judgement, and honor presence, we teach emotional intelligence by example. Those subtle lessons resonate far longer than any lecture.
Our table also became a place of celebration—graduations, promotions, holidays, even Monday nights. The stories we exchange, repeat and pass on become part of our shared family memory—our emotional legacy.
I want to be clear: restoring the table won’t fixeverything. It won’t soothe deep wounds overnight. But it revives opportunity. If the table is empty too often, it’s possible we’re losing more than meals—we’re losing shared experience, mutual understanding, and emotional intimacy.
When the table is cluttered or overlooked, maybe it’s time to reclaim it. Begin with a gentle invitation: “Can we all eat together tonight?” Even once a week sets rhythm. Escort meals with a question like: “What was today like?” or “What’s someone you’d like to thank this week?”
You don’t need perfect timing or fancy plates. You simply need presence and a genuine invitation to share—to speak and be heard. Over time I learned that our table symbolized more than food. It symbolized connection. Taking your seat—even when no one else does yet—is a way to bring possibility back into the room.
Families don’t unravel in crises—they driftapart amid the silences. The greatest courage can be found in bringing back shared conversation—one dinner, one story, one invitation at a time.
You simply need presence and a genuine invitation to share—to speak and be heard.


By CHRISTOPHER EVANS
There’s a moment many patients look forward to during treatment—the ringing of the bell. It signals the end of chemotherapy or radiation, and the beginning of something new. Friends cheer, nurses smile, and photos are taken to mark the victory. But what happens after the bell? What does life look like when the appointments slow down, the medications taper off, and the rhythm of survival gives way to silence?
For many, the end of treatment isn’t as neat as it sounds. It is both a milestone and a mystery. Survivors step into a chapter with no map, no clear timeline, and often, no one checking in daily. The support that once felt constant may fade as routines return to “normal.”
But what is normal, really? The truth is, life after cancer isn’t a return to what was. It’s the beginning of something entirely different. The American Cancer Society acknowledges that survivors can face lingering physical and emotional side effects that may not go away just because treatment has ended. Fatigue, anxiety, sleep disturbances, and fear of recurrence are all common experiences. According to the National Cancer Institute, nearly 60 percent of survivors report experiencing anxiety and uncertainty in the months following their fial treatment.
Ths new normal can feel like walking a tightrope between relief and vulnerability. On one hand, you’re thankful. On the other, you might feel a bit lost. You’re supposed to feel triumphant, and you do— but not all the time. Sometimes you feel guilty for not feeling more grateful. Sometimes you wonder why it still hurts when the hardest part is supposedly over.
I spoke with a woman recently who described it best: “I rang the bell and went home. I stood in my kitchen and thought, now what? I didn’t recognize my body or my emotions. I wasn’t the person I used to be, but I wasn’t sure who I was becoming either.”
That identity shiftis very real. It’s a rebirth in a way. And just like anything newly born, it takes time to grow into the world. For some, life after treatment is a season of reflction. For others, it’s a slow journey of rebuilding—physically, emotionally, and spiritually.
Ths is where faith can be a lifeline. Not necessarily the loud, bold kind of faith that demands certainty, but the quieter kind that whispers in the dark, “You’re not alone.” The kind of faith that doesn’t need all the answers to feel at peace. In the Bible, we see countless examples of people navigating the in-between: the wilderness before the Promised Land, the waiting between Good Friday and Easter morning.
Continued on page 44
The truth is, life after cancer isn’t a return to what was. It’s the beginning of something entirely different.
These stories remind us that uncertainty is not the absence of God— it’s often the space where grace takes root.
One of the hardest parts of this new chapter is learning how to trust your body again. During treatment, every ache had a meaning, every symptom needed a response. After treatment, the vigilance doesn’t just disappear. You may still scan for signs, wondering if something is coming back. You may hesitate before planning too far into the future. And that’s okay. It takes time to reestablish a sense of safety.
Mental health professionals often refer to this phase as “post-treatment transition.” According to the Dana-Farber Cancer Institute, this stage is commonly marked by an emotional dip. During treatment, people often feel they have a clear purpose and a team of professionals rallying around them. Afterward, they may feel like that structure has vanished, leaving them to rebuild it on their own.
Ths is why connection is so important. Talking to others who have walked the same road can offer immense comfort. Whether it’s a formal support group, a casual coffee with a friend, or a shared moment at church, human connection grounds us. It reminds us that we don’t have to figue this out alone.
Spiritual practices can also bring rhythm to this new reality. Whether it’s daily prayer, journaling, or simply taking a quiet walk to reflct, these practices help tether us to something steady. For some, returning to church or exploring Scripture becomes a way to make sense of the journey. For others, listening to worship music or writing gratitude notes is a way of connecting to peace. There’s no right or wrong here—just whatever brings light into the room.
It’s important to acknowledge the grief that comes with survivorship. You may grieve the loss of who you were before the illness. You may grieve the time, energy, or relationships that changed along the way. That grief is valid. Naming it doesn’t mean you’re ungrateful—it means you’re human.
One helpful perspective I’ve heard is to approach this time like recovery from a long journey. You wouldn’t run a marathon and then expect yourself to hop on a bike the next day. You would rest. You would hydrate. You would slowly return to your routines, honoring your body’s limits. The same grace should apply now. Give yourself permission to heal beyond the hospital. Healing is not linear. It’s layered, unpredictable, and deeply personal.
You might also fid that your values shift.Thigs that once seemed urgent may now feel less import-
ant. You may crave deeper connections, quieter days, or more meaningful work. You may start to ask bigger questions, or seek more intentional ways to spend your time. These shiftsare not something to fear. They’re part of the transformation. They’re signs of life taking root in a new way.
If you are in this season now, I want you to know this: you are still healing, and healing deserves as much tenderness as treatment did. The world may expect you to move on, to bounce back, to act like everything is okay. But it’s okay if you’re not there yet. It’s okay if you never return to “before.”
Because life after the bell is not about going back. It’s about learning how to go forward. With a new sense of self. With a heart that knows how to hold sorrow and joy at the same time. With a spirit that still believes, even in the quiet.
Let this chapter be slow. Let it be sacred. Let it be whatever you need it to be.
And if your faith feels shaky or your strength feels thin, remember: even mustard seed faith can move mountains. Even small steps count. Even silence can hold healing.
You rang the bell. And that was brave.
Now comes the rest of your story—and it matters just as much.


Florian F. Dibra, MD is a board-certified, orthopedic surgeon located in Frisco, Texas who has extensive knowledge in hip and knee orthopedics and treats operative and non-operative hip and knee arthritis. He focuses on minimally invasive muscle-sparing total hip and knee replacement, anterior hip replacement, partial knee replacement, robotic joint replacement and complex hip and knee replacement revisions. Dr. Dibra is specialized in MagicKnee and MagicHip, muscle-sparing techniques with robotic technology.
Dr. Dibra graduated with honors from Villanova University in Pennsylvania. Soon after, he received his medical degree, with cum laude honors from the esteemed Jefferson Medical College in Philadelphia, Pennsylvania. He completed his orthopedic surgery training at the University of Florida. He continued at the University of Florida Health Hospital to complete his fellowship in Adult Arthroplasty with an emphasis in hip and knee reconstruction. During Dr. Dibra’s surgical training, he accomplished several publications, book chapters, and poster presentations.
Dr. Dibra’s family consists of his wife and two children. In addition to English, he is fluent in Albanian, Italian, and proficient in Spanish.



Texas Hip and Knee Center Fellowship Co-Director and Faculty at the Anne Burnett Marion School of Medicine at Texas Christian University
Dr. David Shau is a native Texan, born in Fort Worth, TX. He graduated high school in Flower Mound, TX, and attended the University of Texas at Austin, where he studied biomedical engineering. Dr. Shau then ventured out-of-state to work at leading academic orthopedic surgery centers, including Vanderbilt University, Emory University, and University of California, San Francisco, before being recruited to return home to practice at the premier DFW joint replacement group, the Texas Hip and Knee Center (THK).
Dr. Shau has quickly built his practice through connecting with his community, committing to quality service, and delivering excellent patient care. He utilizes a variety of techniques and approaches for hip and knee care, including direct anterior hip replacements, and offers technology-assisted surgeries, such as Mako Technology for partial and total joint replacements. He also specializes in revision joint surgeries and enjoys complex, challenging cases. As a result of dedicating himself to his craft, his partners at THK promoted him to Fellowship Co-Director early in his practice. Dr. Shau also serves as a Physician Development Coach and is an Assistant Professor at the Burnett School of Medicine at TCU, where he enjoys his roles as a teacher, mentor, and coach.
In his free time, he enjoys food, sports, music, and spending time with his wife and daughter. For more information on Dr. Shau’s care philosophy and the techniques/approaches offered for hip and knee care, please visit DavidShauMD.com.



Robert Brunner, MD is a general urologist with Urology Clinics of North Texas serving patients in our Dallas office cated at Texas Health Presbyterian Hospital Dallas. A native of Toledo, Ohio, Dr. Brunner combines a robust academic foundation with extensive clinical expertise. He graduated magna cum laude from the University of Notre Dame, earning dual degrees in Economics and PreProfessional Studies. He then earned his Doctor of Medicine (MD) degree from the University of Toledo College of Medicine and Life Sciences, where he was inducted into the prestigious Alpha Omega Alpha Honor Medical Society.
Following medical school, Dr. Brunner completed his residency in Urology at Baylor College of Medicine in Houston, Texas, where he received comprehensive training in all aspects of adult urology. He developed specialized expertise in the management of stone disease and in the use of robotic-assisted surgery, particularly with the Da Vinci robotic system. Dr. Brunner is skilled in treating a wide range of both benign and malignant urologic conditions, with a particular focus on leveraging advanced robotic technologies to improve surgical outcomes and accelerate patient recovery.
Committed to providing exceptional care, Dr. Brunner is passionate about staying at the forefront of urologic advancements, ensuring that his patients benefit from the latest techniques and innovations in the fild.

• Bladder Cancer
• Blader Stones
• Enlarged prostate or benign prostatic hyperplasia (BPH)
• Erectile dysfunction
• Kidney stones
• Low Testosterone
• Male sexual dysfunction
• Overactive bladder
• Penile curvature or Peyronie’s disease
• Prostate Cancer
• Stress urinary incontinence (Male & Female)
• Testicular Cancer
• Ureteral Cancer
• Ureteropelvic juncion (UPJ) obstruction
• Urethral stricture
• Urinary retention
• Urinary tract infection (UTI)
PRIMARY OFFICE LOCATION: Urology Clinics of North Texas 8230 Walnut Hill Lane, Prof. Bldg. 3, Ste. 700, Dallas, TX 75231 (214) 691-1902 | urologyclinics.com




TheraCare Home Health brings the expertise and resources of a hospital to the comfort of your home.
We offer individual care including nursing, rehabilitation and social services. In addition, our expert clinicians and therapists provide specialized care for a wide range of conditions.
Our care teams strive to make the transition to home as seamless as possible, so you can focus on what’s most important – your health.

TheraCare Home Health services are covered by Medicare and many commercial insurance plans.
Speak to a TheraCare Home Health representative for more information about insurance coverage and Medicare Eligibility.