30 YEARS STRONG! HELPING PEOPLE FACING CANCER FEEL LIKE THEMSELVES AGAIN.

30 YEARS STRONG! HELPING PEOPLE FACING CANCER FEEL LIKE THEMSELVES AGAIN.

WANEEK HORN-MILLER AND HER MOM KAHN-TINETA HORN SHARE THE IMPACT OF FAMILY AND CULTURE ON THEIR CANCER JOURNEY.
Welcome to the Look Good Feel Better magazine. Whether you are newlydiagnosed, finishing treatment, living with cancer or caring for a loved one, this edition is full of helpful tips, ideas and inspiring stories.
We proudly collaborated with subject matter experts to offer you practical advice on caring for your skin, creating a fitness plan that works for you, utilizing wigs and scarves, the benefits of mindfulness, talking to kids, managing work, and so much more.
But most importantly, we sat down with the real experts – people who have faced cancer themselves. Aisha, Michelle, Adriana, Dee-Jay, Louise, Frances, Maggie, Sophia; they’ve shared their stories to help others know they are not alone. They shared their stories for you
We hope you will join us at one of our workshops – either online or in person. There are many topics to choose from. Maybe you’d like to reclaim confidence by gaining greater control over the physical impacts of treatment. Or you’d appreciate information and support around some of the key sources of anxiety during and after cancer care, such as post-treatment nutrition. Our workshops offer useful information; they also build connections with other Canadians facing similar challenges. It’s a chance to listen, share, learn and sometimes even laugh. It’s a moment just for you.
SUSAN LARKIN President & CEO
Look Good Feel Better

One publication can’t possibly hold all the information you may be looking for.
for more resources, including how to register for one of our workshops. You’ll also find links to other supportive-care organizations.
Look for the play button on our feature articles! Just click to watch and listen as our experts walk you through skincare, fitness, scarf-tying, cosmetics, mindfulness and more.
Click this symbol to watch more content.
PRESIDENT & CEO Susan Larkin
LGFB TEAM & CONTRIBUTORS
VP, MARKETING & EVENTS Michelle Nelson DIRECTOR, FINANCE Marco Escobar
ASSOCIATE DIRECTOR, DEVELOPMENT Lisa Tobias MANAGER, MARKETING & COMMUNICATIONS Marsha Roc-Malychenkova
ASSOCIATE, MARKETING Alexandra Baglione WRITERS Tania Amardeil, Suzanne Aranda, Adriana Lombardo, Julia McEwan, Madina Tabesh
CREATIVE SUPPORT FROM A PLUS CREATIVE PRESIDENT & CEO Anastasia Adani
ART DIRECTOR Florencia Damelio
ACCOUNT DIRECTOR Kriti Bhatnagar
PRODUCTION Christine Psaila
SET BUILD, SET DESIGN, PROP & FASHION SOURCING, PHOTOGRAPHY, PHOTO RETOUCHING, VIDEOGRAPHY, VIDEO EDITING, ANIMATION by A Plus Creative
Our heartfelt thanks to all those who so openly shared their inspirational stories, including: Michelle Audoin, Frances Barnes, Louise Bell, Jodi-Ann Blackwood, Mags Bujalski, Waneek Horn-Miller & Kahn-Tineta Horn, Kelly Jessop, Dee-Jay Jodoin, Adriana Lombardo, Aisha Quashie, and Sofia, Lola, Sandra & Frank Tomassini.
Copyright © 2021. All rights reserved. Contents may not be reproduced by any means wholly or in part without written permission from Look Good Feel Better. While every effort is made to ensure accuracy, Look Good Feel Better is not liable for any errors or omissions in the magazine. LOOK GOOD FEEL BETTER® | REGISTERED CHARITY #13374 0316 RR0001
Thank you for making a beautiful difference. Our programming is made possible by volunteers across Canada who generously share their expertise, time, and compassion to support people facing cancer. We are deeply grateful for the dedication and commitment of the 1,000 volunteers who make LGFB what it is today. Visit lgfb.ca for information on becoming a volunteer, our workshops and resources.


Helping people with cancer feel like themselves again


TOP OF MIND
6 PRACTISE SELF-CARE
Mental health, self-care and social support by Madina Tabesh.
8 BE IN THE PRESENT MOMENT
Dr. Linda E. Carlson on the tool of mindfulness by Suzanne Aranda.
10 POSITIVE VIBRATIONS
When family, cancer and Indigenous culture intersect by Mark Beamish.
22 SKINCARE DURING TREATMENT
Skincare & Suncare tips with Dr. Maxwell Sauder by Suzanne Aranda.
24 DECODING YOUR SKINCARE
Expert advice to boost your skincare by Julia McEwan.
26 WHAT HAPPENS AT A LOOK GOOD FEEL BETTER WORKSHOP?
Plus, the 5-Minute Face, Makeup and Nail Care Do’s and Don’ts.
30 BODY OF WORK
Women’s body image struggles and support by Tania Amardeil.
32 HAIRCARE
Haircare, scalp care and headscarf tips & tricks.

36 MOVING FORWARD
Fitness tips from Personal Trainer and Survivor, Adriana Lombardo.
38 EATING WELL
Nutrition tips from Dietitian and Survivor, Jean LaMantia.

14 CARING FOR SOMEONE WITH CANCER
The challenges and rewards of caregiving by Suzanne Aranda.
17 HOW TO TALK TO KIDS ABOUT CANCER
Finding the right mindset and tools by Tania Amardeil.
18 IS CANCER COLOUR-BLIND?
Michelle Audoin on Black Women and Cancer by Madina Tabesh.
41 WORKING THROUGH CANCER
Managing workplace decisions and disclosures by Tania Amardeil
42 SOFIA’S STORY
Teen Sofia & family, on her unique cancer journey by Mark Beamish.

Try to not let cancer take over - find ways to control what you can.
-Louise Bell, LGFB Ambassador
Everyone who has dealt with cancer — whether it’s you or a loved one — should recognize the importance of mental health. Why does it matter so much? For Louise Bell, cancer survivor and Master of Psychology Student at the University of New Brunswick, support from loved ones, taking time for herself, and being in a good mental health space were essential in dealing with her cancer diagnosis.
Taking care of your mental health is a critical aspect of any cancer journey. Too often when medical treatments become our central focus, mental health becomes an
Putting yourself first is essential to your well-being and recovery.
Madina Tabesh
‘underrecognized’ need. We can forget that mental wellness plays a key role in improving our physical health. Louise expresses it perfectly: “If we are mentally well, then we have the capacity in ourselves to help work on our physical wellness. However, if we are not mentally well, we may not have the energy or capacity to push ourselves to do better physically.”
So, how do we take care of our mental health? Self-care is the art of practising good health habits for ourselves. It looks different from person to person and no one formula will work for everyone.
Self-care gives you more
opportunities to try and discover different options to see what works best for you. Maybe you find refuge in reading a good book. Or going for a walk. Or even binging a reality TV show that draws you in.

"Social support is one of the most important factors to navigating a cancer journey.”
Do you enjoy catching up with friends? Perhaps you feel more like yourself when talking to people going through a similar experience. Reaching out to others and joining support groups for people with cancer can give you a sense of community and help minimize the feelings of loneliness. Speaking on her own experience, Louise suggests, “social support is one of the most important factors to
navigating your way through a cancer journey.”
Participating in supportive programs like Look Good Feel Better can have real, lasting benefits. One research study found that support programs can result in a significant reduction of depressive symptoms and an improvement in self-esteem for women going through cancer treatment. Self-care has beneficial effects on psychological
outcomes in cancer treatment and the well-being of women undergoing treatment.
Taking care of your mental health and practicing self-care can look like laying in bed for the day after treatment or phoning a friend and laughing until your belly hurts. You are not alone. Seeking the support you need from your family, friends, or care team is often the first step towards feeling more like ‘you’.
Try our Self-Care checklist to help you manage your stress and nourish your mind, body and spirit:
Mindfulness helps reduce stress and shows kindness to ourselves and others.
Suzanne Aranda

Acancer diagnosis may cause a fair share of fears, uncertainties, and the feeling that you have lost control. Mindfulness has been proven to be a helpful tool to help manage stress, improve mood, decrease blood pressure and gain balance. But what is mindfulness, and where to start?
We asked the question to Dr. Linda E. Carlson, Clinical Psychologist and Professor in the Faculty of Medicine at the University of Calgary and coauthor of The Art and Science of Mindfulness who shared with
us her definition of mindfulness and some practical tips.
First, let’s get some of the misconceptions out of way. Mindfulness is not about clearing your mind of all thoughts, nor always being peaceful or calm, and you definitely don’t need to be seated in front of the ocean, eyes closed, hair floating in the wind to be mindful. Rather, mindfulness is a way of being in the world and a continuous practice. Dr. Carlson defines mindfulness as, “paying attention on purpose in the present moment with an open and accepting attitude.”
Humans have between 50,000 to 70,000 thoughts per day and studies have shown that about 50% of them are not about what is happening in the present moment – we are the masters of mind wandering! But when we are not paying attention to the present, our thoughts are either in the past ruminating about things we can’t change, or racing into the future and worrying about the unknowns.
Mindfulness is a practice, that will help you BE in the present moment. As any practice, it requires some training.
Be Kind to Yourself!
Be patient with yourself while going through the process. Your mind is going to jump around, and it is part of the experience. It’s all about acceptance and practice!
Book Some Time!
Incorporate 30, 20 or even 10 minutes to your daily routine, if that is what you can do! A regular practice is key to make it part of your life and rewire your brain.
BREATHE IN. AND OUT.
Calm your mind with easy, breathing exercises you can do anywhere!
RELAXING
Supporting people through all phases of a cancer diagnosis.
Listen to calming, guided breathing exercises. Check out our digital edition at lgfb.ca.
SQUARE BREATHING
in out pause pause in pause out
Post-Treatment Nutrition
Advanced Skincare Areola Tattooing And more to come

GO TO LGFB.CA FOR MORE BREATHING AND MINDFULNESS EXERCISES TO GET YOU STARTED.
YOU CAN ALSO CHECK OUT YOUR FAVOURITE APP STORE FOR MINDFULNESS TOOLS.
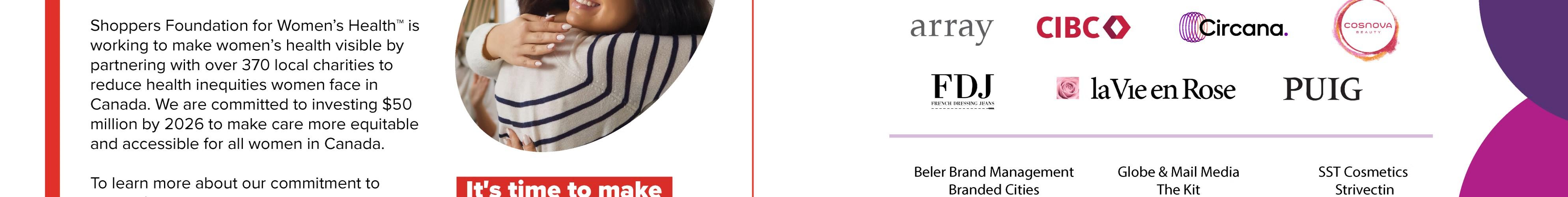
A mother and daughter discuss Indigenous culture, cancer, and the true value of life.
Mark Beamish

KAHN-TINETA HORN
She’s always been dedicated to promoting Indigenous heritage and communities – a passion she shares with Waneek, her three other daughters and extended family. At various times, she’s been a film actress, political activist, fashion model and civil servant. In 2010, she was diagnosed with breast cancer.
She’s a strong, Mohawk woman raised in the Kahnawake Territory near Montreal. Her athletic resume includes co-captain of Canada’s Olympic water polo team at the 2000 Sydney Games, torchbearer at the 2006 Winter Games; and a member of Canada’s Sports Hall of Fame. Today, she calls herself a ‘Warrior Woman’, motivator and businesswoman. Recently, our LGFB team chatted with the mother-daughter duo.

K: When they called me from the hospital and told me the results of the biopsy, I just went blank. I didn’t know what to think, I didn’t even know what to do.
W: I found out my mom was diagnosed with cancer from my oldest sister, It was like this sudden shock went right through my whole body.
W: I 'm really lucky. I come from a big family: there's four sisters, but we have a lot of other extended sisters and nieces, and my husband also was in medical school at the time….
So, it wasn’t just me. My oldest sister really took the lead…. And she said, ‘Mom needs to be around happiness, she needs to be around life.’ We had to be strong, like she was always there for us…
Talking to my sisters, we all said we need to show up as a team and I think, hopefully we did that. We all tried to be there for Mom –and each other.
K: I sat quietly for a couple of days, and when I came to terms with the diagnosis I said, ‘Well I'm getting these vibrations from my children, my grandchildren and they're all dealing with it well, and I realized this was the solution.’
We share these vibrations, this connection. I've always told my kids this is our power. This is the power of the family. The power of the people…. We’re given that by creation. That helped me a lot.
I also asked my best friend, ‘Do you think you could come with me to my treatments?’ and she said yes.

Get the whole story. Check out our digital edition at lgfb.ca and watch the full video.
Having someone you love be so close to the edge, reminds you that life is so precious.
K: My oldest daughter was the one that said, ‘Well now you must start exercising.’ I said OK, and I did it. Then I said, ‘I will try and write one story a day, for a year.’ And I tried to do that – I didn’t succeed completely, but I did a lot of great stories. That probably did me a world of good.
One of my grandchildren asked me, ‘Do you have any secrets to life?’ I said, ‘Well I never abuse anybody, I never let anybody abuse me and I take care of my appearance.’
K: I like to give them my complete cancer story and explain everything that I did, and then I say, ‘OK, now you have to figure it out for yourself.’
W: I would ask, ‘What can I do for you?’ because really that's all you can do. Be that person that helps. And that's how families get through cancer diagnoses—whether family by blood or family by choice.
My mom is always full of encouragement – no matter what someone is going through. She always has a story and this way of making me feel like I can handle it. All my life, she would say to me, ‘Be good to yourself, be kind to yourself.’ Trust that you have the knowledge or the energy to support each other. Start saying to people, “You’ve got this!”

W: One of the greatest gifts, if there can be a gift from this experience, is that it made me stop and do regular check-ins with my friends.
That's what cancer teaches you: don't wait until someone gets sick, send them a card, call them...because having someone you love be so close to the edge, reminds you the value of life and life is so precious.
We all came together to help our mom and now she's in her 82nd year and as vibrant as ever. She keeps telling me ‘I’ve another 20, 25 years to live’, she says. ‘What am I going to do for 25 years?’ I'm like, ‘I don't know, cause a ruckus, I'm sure!’ (Laughter).
Mukluks are an important gift in many Indigenous cultures that signifies a new journey in life. Waneek gave this beautiful pair of warm, Manitobah® Mukluks to her mom for her cancer journey. She proudly wore them during every radiation treatment. “It got me through it,” Kahn-Tineta remembers.
Taking on the role of caregiver can be challenging yet rewarding.
Suzanne Aranda
When someone you love and care about receives a cancer diagnosis, it can be difficult and stressful for you as well. You want to be supportive and helpful, but it is not always easy to know how. How can you show your support? Caring for someone with a cancer diagnosis is
never one-size-fits-all.
Your loved one’s needs may change during and after cancer treatment. From day-to day tasks around the house, to helping track appointments and prescriptions, to filling out forms, to simply being there and listening... and much more.
WE ASKED WOMEN FROM OUR LGFB WORKSHOPS TO SHARE WHAT ‘GIFTS’ THEY RECEIVED FROM THEIR CAREGIVERS.
Whenever I broke down or was doubtful, my spouse explained what was next with a calm attitude and a smile on his face. He boosted my confidence.
I
am unashamedly my own woman. The BEST thing my partner did was to let me choose how we take care of me - my way.
I thought I could look after myself… but my daughter took on being my caregiver. I didn't realize how much of a difference it would make!
A gal from my hometown made me a prayer blanket with butterflies and messages from my church community. It gave me peace and comfort.
My best friend told me that I needed to use my energy to fight cancer so I let my loved ones help in every other way. She said, "I need to be able to help you - so please allow it." Because of her words, I never hesitated to ask for help.
My best friend periodically drops off a little surprise signed "Love - Your Secret Admirer". It makes me smile every time.
My 83-year-old mother flew in to be with me for treatments, sitting in a hard metal chair for up to 8 hours and never once complained. She would stay the week and do the housework too.
I had someone who would just listen…you need to share what you are experiencing. I never felt judged or alone - it was ok to cry with her and to feel the way I was feeling.
My husband has taken over the cleaning and cooking… he also knows when to step back and let me do what I can when my energy levels are up.
The school I work at made a quilt with personal notes from all the students to inspire me through the journey.
My neighbours supported my son through my treatment – knowing he was active and spending time with friends helped me feel better.
I joined a Peer Support Group, and my mom made all my favourite comfort foods for us.
My former colleague drove from Abbotsford to Coquitlam for 6 mornings of radiation to look after my 2-yearold daughter as I didn't have childcare. And she usually arrived with baked goods for the family as well!
My extended family took turns coming to appointments and writing down the important things I needed to remember and read my questions if I forgot them.
The medical staff is critical in providing care, but you too are an integral part of the cancer care team, and your help and support can have a huge influence on the physical and emotional well-being of your loved one.
Being someone’s rock during this challenging time can be rewarding yet also overwhelming at times. In the whirlwind of providing care, you can easily forget your own needs and feelings, putting them aside to focus on the patient. By ‘filling your cup first’ and taking care of yourself, you will be better able to take care of your loved one.
You are making a big difference in the life of someone with cancer. It is a wonderful gift, just remember to take care of yourself, too! Top
Take a break. Try meditation, go for a walk with a friend, escape into a book or TV show, or whatever helps you to relax.
Don’t try and do it all – delegate tasks to family and friends. Many people want to help but don’t know where to begin. Just ask!
Find support for yourself within your own circle or join a local support group for caregivers (in-person or online). The resources are there to be used.
Conversations with children can be difficult, but the right mindset and tools can help.
Tania Amardeil
Breaking the news about a cancer diagnosis to children is tough – but essential. For Aisha Quashie, diagnosed with stage 3 non-Hodgkin’s lymphoma in November 2019, sharing her diagnosis with her kids — 16-year-old Amari and 11-yearold Ayana — was one of the most challenging parts of her journey.
“Cancer feels like such an adult subject,” says Aisha. “You always want to seem like you have things together — that you’re strong and can handle anything. You don’t want to show weakness because they need you to take care of them.”
Explaining her diagnosis and treatment plan to her children was emotional, but Aisha is glad that she chose to approach the discussion with honesty and vulnerability.
“When I told them, they broke down,” says Aisha. “They were really scared but being honest helped. I was upfront about what to expect, and the treatment I’d go through.

I reinforced the fact that I was going to get better and be OK.”
Alyssa Gallant, Certified Child Life Specialist at the Nanny Angel Network, which provides free, specialized, childcare resources for mothers with cancer, echoes this sentiment. “Parents think that if they keep their cancer diagnosis from their children, their children will be more protected and feel less sad,”
to your kids’ questions and prepared to help them manage. “It’s important to let kids know there’s someone they can go to when they have questions,” she says. “If there’s another support person, that can also be helpful.” Lastly, Gallant notes the importance of using age-appropriate language and correct terminology (like tumour, chemotherapy, or surgery), when speaking to kids, as
As a parent, you always want to seem like you have things together — that you’re strong and can handle anything.
she says. “Often… it’s the opposite. When children have more information, they feel more prepared.”
Gallant also notes that because kids are so intuitive, they often already know that something is going on. Having the real facts is better than letting young imaginations run wild. She advises being open
euphemisms can be confusing. Believe in your strength and ability to support your children, cancer diagnosis or not. “It’s tough because you’re going through so much and you have these little people that are looking to you for support,” says Aisha. “It’s OK to let your kids see you not be OK, because that’s life.”
Michelle Audoin is driving change by highlighting the unique experience of Black women with cancer.
Madina Tabesh
When Michelle
Audoin was diagnosed with cancer in 2017, she wasn’t expecting to become an advocate for Black women facing cancer. But for this teacher, wife and mother of two, speaking out about her own experience and encouraging other Black
women to do the same was a necessity.
“My breast cancer was already at an advanced stage, but the healthcare professionals didn’t realize that until after the initial biopsy. I had to really advocate for myself at this time.” Michelle notes that Black women have unique challenges in the cancer care space that others may not. For instance, “in Canada we don’t collect race-based data and that’s problematic. Some forms of breast cancer affect Black women differently. And if Black women aren’t aware of their risk, they won’t speak out for themselves. I think Black women need to know they can be at risk.”
After a diagnosis, knowing what to expect during treatment helps many women feel prepared. But when the images available in doctor’s offices, pamphlets, and television are of women who don’t look like you, it can be difficult for BIPOC
(Black, Indigenous, People of Colour) people to feel supported or ready to take on their diagnosis.
“I was two years into breast cancer and hadn’t seen myself reflected in the materials I received”, says Michelle. “There is also a lack of other racialized or Black women in clinical trials. I know for me and other Black women, we experienced side effects from treatment that were not on the list. When you bring this up, your medical team may not even have the information, or take your concerns seriously. But, when you talk to other Black women, they also experience the same sideeffects.”
For Michelle, speaking up and being gentle with herself was key throughout her diagnosis. She played a key role in creating Uncovered: A Breast Recognition Project , with Rethink Breast Cancer highlighting the unique experience of Black women with cancer in both words
When the images are of women who don’t look like you, it can be difficult to feel supported.

My breast cancer was already at an advanced stage... I had to really advocate for myself.


“I
How to advocate for yourself and get more out of visits to any healthcare provider. and photography. Michelle also connected with LGFB to help inform its programming, training, imagery and language to better reflect a diverse community.
Michelle is driving change in how Black women with cancer are supported and seen in Canada. She hopes that by sharing her story, she will inspire systemic change as well as show other Black women with cancer that their experiences are valid and inspire them to share their stories, so they can feel better supported.
Get the whole story. Check out our digital edition at lgfb.ca and watch the full video.

PRE-APPOINTMENT:
Make a list of all medications you take.
Write down your questions & concerns.
Ask a friend or family member to join you for support.
Compile your family history if it is available to you.
Check if your hospital offers translation services if needed.
APPOINTMENT DAY:
Remember to bring your Health Card and/or necessary documents.
Bring your list – it’s okay to ask questions and advocate for yourself!
Take notes to help you remember later – your support person is also a second set of ears.
Clarify next steps and timing before leaving.
POST-APPOINTMENT:
Review notes and fill any prescriptions given.
Call doctor’s office for clarification, if needed.
Schedule next visit or tests, if needed.

- Patrice Neale, LGFB Participant


Dr. Maxwell Sauder, Onco-Dermatologist, shares his top tips for impacted skin: CLEAN, REPAIR AND PROTECT!
Stick to the skincare basics: Cleanser, Moisturizer and Sunscreen. The more products you use, the more you risk skin irritation.
Creams or balms will better hydrate your skin. For overly dry skin, apply ointment –especially on lips and hands.
Cancer and its treatment can cause a variety of changes in your skin. It may become extra dry and irritated, change colour and texture or be more sensitive to the sun. A healthy skincare regimen can help you manage and feel good in your skin.
Look for skincare products that are gentle, hydrating, hypoallergenic, fragrancefree and PH neutral. Products for eczema or sensitive skin are a good option.
Avoid alcohol-based products, and antiageing ingredients such as retinol, Alpha Hydroxy Acids (AHAs) or scrubs/ exfoliating products that may irritate or dry skin.
Regardless of your skin type, the sun can damage skin any time of year.

The sun can damage skin any time of the year. Sunscreen is a must for everyone, every day – whatever the weather. And radiation and chemotherapy treatments, as well as some medications, can increase susceptibility to sunburn and skin damage.
Choose sunscreens with UVA/UVB broadspectrum protection, SPF 30 or higher.
For sensitive skin, mineral sunscreens may cause less irritation.
To avoid an ashy residue – look for easily-absorbed or tinted sunscreens. Apply sunscreen 15 minutes before sun exposure; reapply every 90 minutes.
Apply sunscreen daily and liberally to all exposed skin, including lips, ears, scalp, sides and back of the neck and the chest.
You are still exposed to damaging UV rays even in the shade. Stay out of the sun during peak hours (11 a.m.-3 p.m.).
Always wear a hat – preferably one with a wide brim of about three inches.
Apply sunscreen first if wearing makeup.



If treatment is impacting your skin, make sure you follow our simple steps on page 32. But if your skin isn’t impacted, or you’re done treatment and want to amplify your skincare routine, we’ve tapped the experts for their top advice.
Julia McEwan
Vitamin C is a workhorse ingredient. This overachieving antioxidant helps improve uneven skin tone, fine lines, dullness and rough texture. It also helps prevent oxidative stress caused by free radicals. “Antioxidant molecules help to neutralize these harmful atoms by giving up some of their own electrons,” says Dr. Vincent Richer, a medical and cosmetic Dermatologist at Pacific Derm. Think of it as nature's “off” switch.



If you've noticed your skin getting drier as you age, or that's just your skin type, one active ingredient to be on the lookout for is hyaluronic acid, especially in a serum. The molecule, famous for holding 1000 times its weight in water, helps brings moisture to the surface of your skin. In the right formulation, it
A serum and moisturizer combo can enhance your skincare routine —but what is the difference? "Serums are formulated to penetrate deeply into the skin to deliver targeted active ingredients," says Dr. Arisa Ortiz, a Harvard-trained, board-certified dermatologist. This means they’re thinner and lighter to their creamier counterparts and also a more powerful delivery method. "Moisturizers help to reinforce the surface of the skin and work to increase hydration," she adds.
Whether you are a product minimalist or maximalist, the order you apply your skincare matters—both for your skin’s health and the products’ efficacy. For the less-is-more folks, keep it simple: cleanser, moisturizer, sunscreen. If your routine is more robust: cleanser, toner, serum(s), eye cream, moisturizer, face oil, sunscreen. Looking
can produce immediate plumping effects, leaving skin looking dewy. But for folks with very dry skin or who live in a dry climate, Dr. Julia Carroll, dermatologist and co-owner of Compass Medical, suggests layering moisturizer on top of your hyaluronic acid serum to seal it in and provide a barrier to moisture loss.
At a Look Good Feel Better workshop, women with cancer can learn how to manage the appearance-related impact of cancer and its treatment in a small supportive group.

Learn how to care for sensitive skin plus tips & techniques for managing the loss of brows and lashes, adding colour back to the face, makeup hygiene and sun safety.
Learn about options available for postsurgery and beyond, what to expect at a breast form fitting, tips for where to find financial coverage, and more.

See a demonstration on various head coverings, what to consider when selecting a wig, easy scarf-tying techniques, plus caring for your scalp during and after treatment.

This special workshop just for teens includes skincare, on-trend make-up tips to feel your best and a demonstration of fun styles for caps, wraps and hair alternatives.
’’Actively care of helped control want to as sick.’’


“ “ Actively taking care of myself helped me regain control - I didn’t want to be defined as sick. -Adam, workshop participant

What exactly happens at a Look Good Feel Better workshop? Whether you choose to join us in-person or online, you’ll be warmly welcomed by a team of our professionally-trained volunteers. Along with a small group of women, you’ll learn tips and techniques for taking care of your skin and how to use makeup to manage changes to your skin, brows and lashes. And, you’ll receive a kit of beautiful products for home you can use for practice. We’ll also show you different types of wigs and scarf-tying techniques so you can choose the best options that feel right for you. At our breast care workshop, we’ll talk about the different options available for bras, forms and other garments for when you are going through treatment and post-surgery, plus how to care for sensitive skin. Beyond the practical information, the workshops are an opportunity to be with a group of women going through a similar experience, to share and be heard, to ask questions and most importantly, take time for yourself.
I looked at myself in the mirror for the first time since I started treatment, feeling beautiful.
Meet Jodi-Ann Blackwood. Our 5-Minute Makeup artist is also a new Canadian, mother of 3 and cancer survivor.

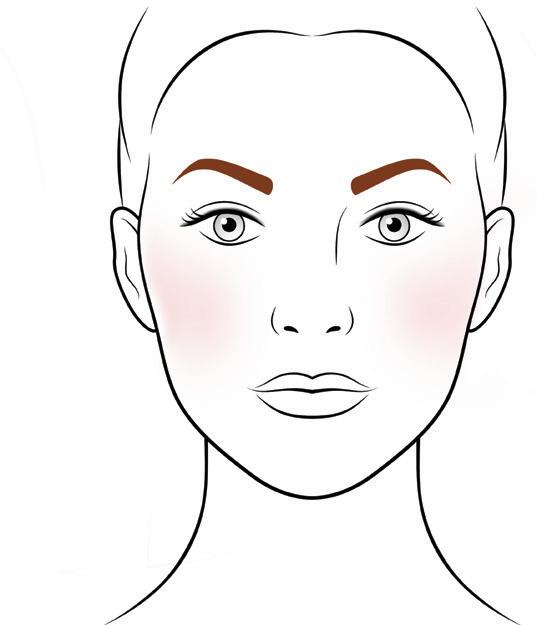
Giving yourself a little boost doesn’t need to take long. When you’re low on time or energy, 5 minutes can help you feel more like yourself. Cleanse and moisturize, protect with sunscreen, then follow these quick steps for a fresh look.

CONCEALER
1 2
Dot concealer under eyes or any areas of discolouration then blot with clean fingers or sponge.


If you like, a foundation or BB cream can quickly even-out skin tone. Dot foundation on forehead, nose, chin and cheeks then blend outwards from the centre of your face.


BLUSH

Give yourself a smile to find the apples of your cheekbones, then dab on blush using a cotton ball. Use any blush left on the cotton ball on your nose, forehead and chin to give a little glow.
Fill in or recreate your brows. Hold a brow pencil straight up against your nose, lined up with the inside corner of your eye. Draw a dot at the brow bone at this point.



Eyeliner can help recreate lost or thin lashes. Use a pencil eyeliner to draw small dots close to the roots of the lashes and then draw a line to connect dots. Use a cotton swab to sweep a dark eye shadow over the eyeline to soften the look and help it last longer.
Place the pencil diagonally from the bottom corner of your nose past the outside corner of your eye and draw a dot. This is the end of your brow.
Next, look straight ahead, place the pencil parallel to the outside edge of your iris and place a dot at the highest point of where the brow line should be. This is the arch of the brow.
Connect the dots into a brow line with light, feather-like strokes of colour, making the brow fuller on the inside corner and thinner as it moves out.
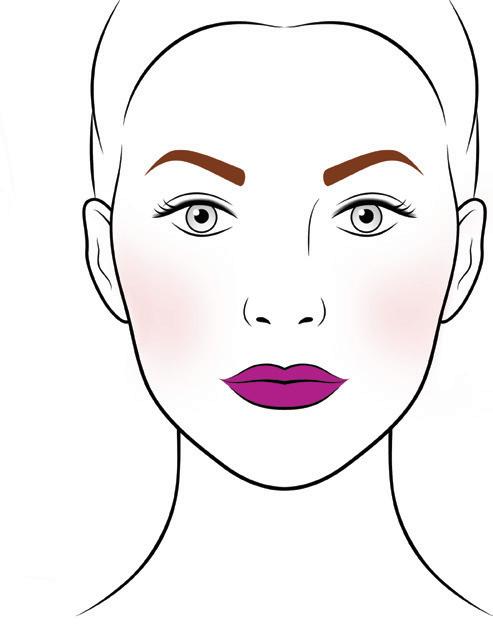
Finish up with a moisturizing lip colour – go bold, go muted or mix it up, depending on the day! LIPS


Makeup hygiene is even more important during treatment as your immune system can be
compromised. Keep bacteria out of your products by using disposable applicators such as cotton balls, sponges, or mini spatulas.
SMART MAKEUP DO'S & DON'TS
• Wash your hands before skincare & makeup application.
• Don’t reuse applicators or double-dip.
• Use products you can pump or squeeze out – if you must

dip, use a mini spatula.
• Close all lids right away.
• Never share your cosmetics.
• Avoid testers – if you can’t, only try on your wrist or back of your hand.

Cancer treatments can affect your nails. Most changes are mild, but some may be more severe and uncomfortable, depending on how different medications impact your nails. Ask your health care team what to expect from your treatment plan. Nails may become more brittle and break more easily. You may also notice grooves, colour changes, sensitivity, faster or slower growth, or that nail beds lift up. Changes often go away after treatment ends, though it may take a few months because nails grow slowly. Try to prevent problems proactively and address any nail issues right away.
SMART NAIL CARE DO'S & DON'TS
• Keep your nails short – but don’t cut cuticles (gently push back instead).
• Massage cuticles with cream or oil.
• Wear gloves for chores –avoid fungal infections by not keeping hands in water too long.
• Wear clear/light polish or nail hardener to protect nails, and use a nonacetone polish remover.
• Avoid artificial nails as they may increase chances of infection.
• Inform your doctor if you see inflammation, pain, redness, lifting of the nail bed, etc.
• Skip the nail salon during treatment – or bring your own tools.
Tania Amardeil
For many women living with cancer or in remission, changes in their appearance can be a major source of concern and anxiety. This is not vanity. Much of our identity is related to our physical appearance from how we wear our hair to what clothes we put on. Body shape and size, including breasts, are often tied to a woman sense of self, self-expression, sexuality, and self-esteem.
Appearance-related impacts of cancer can be temporary (like hair loss and skin changes) or more permanent (like surgery or scarring). They can all affect women at a time when they may already feel vulnerable, which can negatively impact their mental and emotional health.
For many women facing a cancer diagnosis, there's enough to cope with emotionally without also feeling that there's no space to speak about body image issues or that it is somehow selfish or vain to worry about them. For DeeJay Jodoin, a B.C. woman in remission, changes to her physical appearance like hair loss and weight gain were hard to accept. “It [cancer treatment] alters your appearance. You want to get back to the way you were, but it takes time.”
“Women going through cancer treatment often experience a change in their body image and in their relationship with their body,” says Monique Voorn, a social worker at the Simcoe Muskoka Regional Cancer Centre in Barrie, Ontario. “They may be unhappy about how their appearance has changed, whether they’ve had breast surgery or scars they don’t like, or lymphedema. Sometimes, a woman may not have had significant visual changes to her body but feels like her body has failed her or that she can’t count on it.”
There can also be physical changes that women may not
expect. “With radiation, there are skin changes,” notes Larissa Dyck, an oncology nurse in Calgary, Alberta. “The area that’s treated can end up darker and may take a while to fade, and skin can get tighter and be uncomfortable for some patients, causing a loss of range of motion. Keloids - a type of raised scar that can arise after a surgery — can be a particular concern for women of colour specifically. Weight can be an issue, too. Being on hormones can cause weight changes that can turn women’s body image completely upside down and they can get really down on themselves.”
It takes time for women
to recognize and appreciate the full impact of the changes they’ve undergone during their cancer journey. “It’s often near the end of treatment when it really hits women what they’ve been through and all the changes they’ve undergone – physical and otherwise,” says Dyck. “When patients are finished their treatment, they expect things to go back to normal — but they may still be on long-term hormones or medication, and that’s when it can be really hard for these women. They expect their bodies to just bounce back, and they want to go back to work and exercise, but things aren’t the same as before.”
While physical symptoms can affect women in a finite number of ways, the emotional experience is different for everyone. “When some women lose their hair with chemo, they’ll proudly wear a head scarf,” says Dyck. “Other women have a complete loss of identity and want to wear a wig. They may fear that their partners won’t be attracted to them.”
Social Worker Monique Voorn agrees: “There’s a wave or rollercoaster ride of emotions in any type of cancer. There’s a lot of grief. We grieve all kinds of changes or losses in our lives that cancer brings — to your body, to your innocence, and to the carefree way that you may have used to experience life.”
Every woman’s experience, perspective and cancer journey are unique. They want to be listened to as individuals, and they don’t want assumptions to be made about how they feel about their body. Allowing and
accepting different experiences, reactions, and stages of grieving is part of the process. Every decision – from choosing a wig versus scarf, or breast reconstruction versus breast forms or living flat – is personal and empowering to each woman. With the right tools and support, women can gain confidence in their ability to restore or renew their sense of self — however they may choose to define it.
There are many programs offering practical and emotional support, as well as individual options. Share your concerns with your medical team and ask for help. Check out your hospital’s resource library or the many online options.

The second thing I did was google hair loss.”
For so many women, the potential of losing their hair during treatment is one of their top concerns. Hair loss is most often temporary. There are many ways to take care of your scalp, plenty of wig options should you choose to wear one, and some great fashion options to help you get creative and express yourself!
Like you, your scalp deserves tender love and care. An itchy scalp is a common side effect–whether you have lost hair or not. Massage an anti-dandruff shampoo into your scalp and let it sit for 2 to 5 min. The antiinflammatory properties can be very soothing. But don’t use it more than twice a week as it can be drying as well – the opposite of what you want! When moisturizing your face, don’t be shy to go all the way up onto your scalp and give it another nice massage.
If you still have your hair and are itchy or red underneath, ask your doctor if a prescription antiinflammatory lotion is right for you. If so, make sure you follow the directions, including tapering use over a prolonged time period.
You may have heard about scalpcooling to minimize hair loss during treatment. Scalp-cooling is available in Canada through a handful of providers. Check with your medical team to ensure it is appropriate for your cancer type and treatment. To date, scalpcooling is not covered under insurance plans. To be effective, scalp-cooling must be used during every chemotherapy treatment.
Style your headscarf with cool, easy options:
1
TUBE STYLE
Place the tube on your head and simply tie the excess back in a ponytail using a hair elastic. Easy to use and wear!

3

Using a rectangular scarf – centre it on your head and tie it behind either ear. Let it dangle or twist it together & create a bun.
2
Using a rectangular scarf, centre it on your head and bring 2 ends to the back, then one side. Twist the ends, place over top and tuck in ends.


Using a square scarf, fold it in half into a triangle. Tie in a front knot & tuck in the middle corner. Done!
4
Looking for more tips? Check out our digital edition at lgfb.ca to watch the full video.

I didn’t want to just survive, I wanted to thrive.
- Frances Barnes, LGFB Participant
As small as it might sound, being told you can rock a wig if you choose to, impacted me positively.
Frances Barnes, Workshop Participant
LGFB is about connection – More than ever, women need that emotional support.
Aida
Tahiri, Workshop Participant
Be kind to yourself. Stay positive.
Changes to your appearance can be the toughest. When I started gaining control over my appearance, I started gaining back control over my mental health, too.
Sarah Issa, Teen Workshop Participant
For anyone trying to hold it all together for their loved ones…make time for yourself. The best way to be there for others is to first be there for yourself.
Milena Commisso, Workshop Participant
I
would advise anyone going through cancer treatment to be kind and gentle to themselves… with their time, energy, and/or expectations.
Christine B., Workshop Participant
The LGFB workshop connects you to other women. It validates your experience. You know that you are not alone.
Shelley Mckenna, Workshop Participant
The only choice we have is the way we react. I choose to inject joy and laughter into any situation that calls for it.
Laura Jean Falla, Workshop Participant
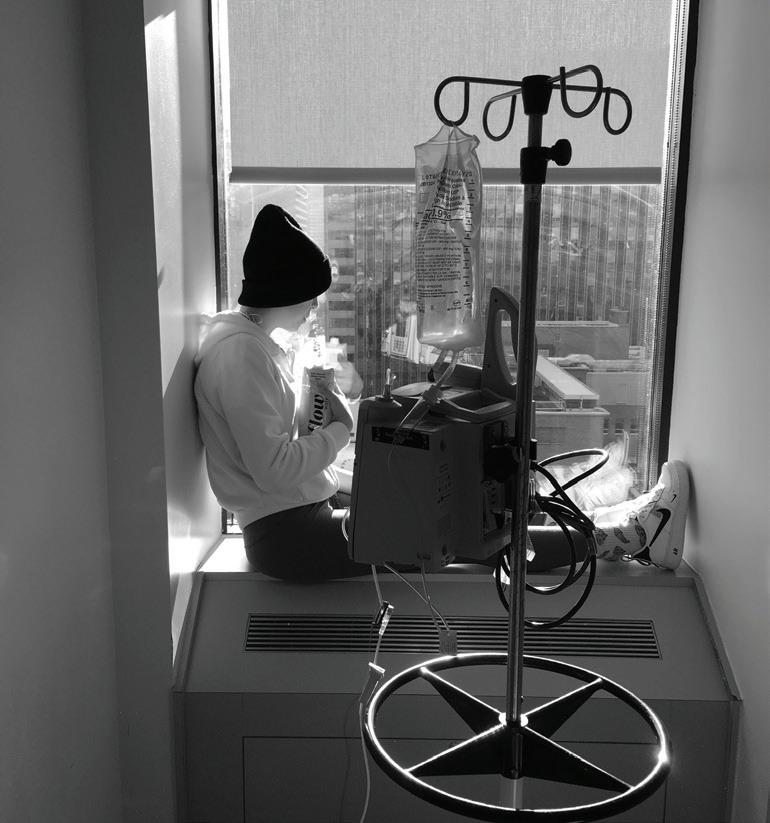
Adriana Lombardo was diagnosed with leukemia at just 17 years old. She underwent more than 2 years of chemotherapy, followed by a hip replacement.
Today, Adriana is 24 and a Certified Personal Trainer passionate about health.
Adriana Lombardo


• Maintains or improves your physical abilities.
• Prevents muscles from wasting due to inactivity.
• Improves your self-esteem.
• More likely to keep social circle.
• Lessens symptoms of tiredness & fatigue.
• Improves your quality of life.
Your goal is to stay as active as possible so your exercise plan should be personal, safe, and include activities you like doing. If you already exercise, you may need to do less, or lessen the intensity. Always keep your cancer care team informed of your activity level during treatment.
Many side effects improve within a few weeks after treatment ends, but some may last longer or appear later during recovery. Understanding this will help you gradually modify exercise intensity as needed. Always listen to your body and its needs (like rest vs. movement).
Looking for more tips? Check out our digital edition at lgfb.ca to watch the full video.



Easy strategies can help you stick to your exercise program:
• Set short-term and long-term goals.
• Mix in different activities (like yoga, dancing, or tai chi) to stay fresh.
• Invite friends, family, or co-workers to exercise with you.
• Track your exercise progress.
• Recognize and reward your achievements.

Most cancer patients experience fatigue, but research shows a link between regular exercise and reducing fatigue. It also helps you manage normal daily activities without major difficulties. Any aerobic activities that raise your heart rate – like walking or jogging – can help.
• Schedule a daily routine so you’re active when you feel your best.
• Get regular, light-to-moderate intensity exercise.
• Get some fresh air.
• Balance activity with rest so it doesn’t interfere with nighttime sleep.
• Ask for help when you need it.
Always check with your doctor before starting any exercise program. Consider consulting with an exercise professional who is aware of your cancer and treatment plan to ensure the best exercise plan for you.
At the Look Good Feel Better workshops, we often hear how important it is to feel seen, understood, and not alone when facing cancer. This podcast was inspired by our workshop participants and the crucial need for connection.
•You Have Cancer – Now What?
•This Is Supposed To Be Normal?
•Living With Cancer
•Support Systems
•Navigating Nutrition And so much more
Inspired by the community and the connection we see in our workshops.






A Dietitian and Survivor Shares Her Best Nutrition Tips.
Tania Amardeil
Focusing on nutrition gives cancer patients a greater sense of well-being and control.
Women who have been diagnosed with cancer or who are in remission have a lot on their minds — and nutrition may not be high on their list. Yet, nutrition can be a critical part of one’s cancer journey.
Jean LaMantia, a Torontobased registered dietitian, and cancer survivor, recommends approaching nutrition in two phases: Phase 1: Nutrition that will help you get through your treatment, and Phase 2: Nutrition Post-Treatment as a positive step to potentially prevent recurrence.

“During my lymphoma treatment, I had severe nausea and vomiting, and so I had to get strategic about what I could eat and what I could keep down,” says LaMantia.
While you’re going through treatment, don’t worry about eating the “perfect” diet. LaMantia recommends taking this pressure off and simply eating in a way that helps manage your side effects.

Eating cold and room temperature foods, as they have less aroma and are less likely to trigger nausea

Prioritizing highly-nourishing foods, especially protein sources

Plating food beautifully on a small plate to combat low appetite

Adding extra calories to your meal with a drizzle of extra virgin olive oil
Post-treatment, nutrition can play an important role in your recovery and healing.
“After treatment, cancer survivors who are in remission can experience a lot of anxiety, worrying about recurrence,” says LaMantia.
Proactively doing your best to eat healthy foods that could lower your risk of recurrence


can put your mind at ease. “I find that it can be very empowering and can help you take back control,” adds LaMantia.
According to LaMantia, the key is to focus on foods that are supportive of the immune system, anti-inflammatory, and proven to target cancer cells.

Foods high in vitamin E (especially wheat germ and almonds)

Spices including Ginger & Turmeric


Omega 3 fatty acids (found in fish like salmon, mackerel, rainbow trout, sardines, herring, and anchovies)

Whole grains (quinoa, wild rice and whole grain pasta)

Garlic and onions

Cruciferous vegetables (broccoli, cabbage, brussels sprouts, cauliflower, and kale)

Protein foods (S kinless poultry, low-fat yogurt, dried peas, beans or lentils)
Managing work-related decisions and disclosures is personal for working women with cancer.
Tania Amardeil
Every working woman living with cancer faces challenging and deeply personal decisions. Whether you take time off work or continue working through your treatment, whether or not you choose to disclose your diagnosis to your colleagues and supervisors, and how you will approach your return to work – are all choices that are yours to make.
Approximately 62% of those diagnosed with cancer return to work within the first year, although they may require accommodations. Physicallydemanding jobs, changes in priorities, and the severity of the illness and treatment side effects may affect one’s ability to return to work. By contrast, factors that make returning to work easier following treatment include workplace accommodations (flexible hours, duties, and job site), having a good relationship with supervisors and colleagues, support at work and at home, tailored workplace rehab, and clear advice from one’s doctor about capabilities and limitations. Every woman’s circumstances are unique, and so every woman’s experience will be too.
For Frances Barnes of Medicine Hat, Alberta, choosing to work throughout her cancer treatment was a way to continue doing something she loves — working as a career life coach.
“I love my job and working gave me an opportunity to get out of my own head,” she says. “In some ways, it was a saving grace during COVID and cancer. For three days a week, I could listen to other people’s stories and not think about my own.” Having a part-time, flexible schedule and an online job enabled Frances to continue working and to coordinate her chemo treatment with her work.
Choosing not to disclose her cancer diagnosis to her coaching clients was a deliberate decision for Frances. “When you coach, it’s all about the people you coach”, she says. “If they’d known that I had cancer, they would’ve worried about me and thought about me, and it’s not about me.”
For other women, being open with their clients and colleagues may be the most natural route. “One thing that I’ve learned by going through cancer is that every person’s journey is personal and different,” says Frances. “Give it thought and do what’s right for you.”
By law, employers must make reasonable changes, such as changes in work hours or duties, to help you do your job during or after cancer treatment. cancerandwork.ca/survivors
Family ties, the Teen LGFB Workshop and beyond.
Mark Beamish
Think back to those teenage years. Feeling selfconscious about your appearance, dealing with social anxiety, hormonal changes, and the struggle for more independence. Now, add a cancer diagnosis into the mix, and you have an inkling of what Sofia Tomassini lived through in 2019. She vividly remembers her reaction: “I was diagnosed two days before my 14th birthday with Hodgkin's Lymphoma. The biggest question I had was “why me?”
Her mother Sandra recalls the beginning of the journey. “It was around Halloween, Sofia told us that she felt a lump over her collarbone. Our family doctor recommended she get an ultrasound. The initial results were not what the doctor expected, so we went for a second one. A throat specialist looked at it and realized we need to do a biopsy, urgently. It was the longest 2 to 3 weeks of our lives, waiting for those results.”
“The toughest part was the in-between,” Sofia’s father

Frank recalls. The family went back and forth, “between being positive, to planning for the what ifs, to thinking that it could be much worse.” After the diagnosis, Sofia entered Sick Children’s Hospital in Toronto, and the tight-knit family shifted their mindset to the task at hand. Younger sister Lola remembers first hearing the news. “My
parents just sat me down and told me Sofia has been diagnosed with cancer, but it's treatable – and this is what we're going to do.”
While at SickKids, Sofia first learned about Look Good Feel Better and their Teen Workshop.
She decided to attend a workshop with her sister Lola, to learn about skincare,
-
Frank, Sofia's father

makeup tips and hair alternatives. Sofia credits the warm and welcoming workshop volunteers with helping her feel, “less selfconscious while going through treatment.” Sharing the workshop with Lola made it even more special. “I had my sister with me, so it was always easier with her. I think it's great for young girls, especially that are my age. It makes you feel better. It made
the treatment go by faster.” Sandra describes the workshop as, “a real bonding experience” for her daughters.
Sofia also practised self-care to help keep herself strong. “Mentally, I had to focus on myself, and I had my family there for me, but social media has a huge impact today on kids, so I put my phone down. I just made sure to stay positive.”




“In my school there was even more pressure to look a certain way: all the girls have long hair; all the boys have short hair. That was the only thing that scared me – losing my hair. That was a big thing for me. It was OK to have short hair. It was a choice that I could control.” Sofia showed great maturity while facing appearance-related changes, such as losing her hair, and will always remember one gesture of support, “my grandfather
shaved his head for me, so it was very rewarding and nice to have somebody else with such short hair.” Frank was impressed by Sofia’s choice, “I’m proud of her for making that decision on her own. I think letting go of that worry, and not being concerned about hair anymore was liberating for her.”
Frank is proud of how the family rallied to face the challenge. “We went directly into a mode of what do we
need to do to get from here, to back to full health?” Everyone had a role to play: Frank focused on Sofia’s nutritional needs, Sandra tracked medications, and Lola kept everyone on schedule. Sandra remembers the optimism, “we had a lot of support. We had each other, so we knew we were going to be okay.”
After Sofia’s treatment, the Tomassini family found out two neighbourhood teens were also dealing with cancer.
Sofia offered to be a resource for them. “We related in having cancer and how we grew up. We just chatted when they needed somebody else to talk to.”
What advice do the Tomassinis now offer to families beginning their own cancer journey?
For Sofia it’s the power of staying optimistic. “Don't think ‘why me?’ Think about, ‘I'm going to be done with this! I'm going to beat this!’ Focus on yourself, stay happy, eliminate all distractions possible. Stay positive. That helped me.”
Mom, Sandra recommends creating a strong network of family and friends: “Build that foundation…make sure you have a good support system.”
Sofia’s strong and constant companion Lola enjoyed distracting and laughing with her sister as she was in and out of the hospital. Lola’s message is simple: “Just be yourself,




“I had my sister with me - it was always easier with her.“

“We had each other, so we knew we were goingtobeokay.”



don't think about your sibling having cancer. Just think of them as your sibling. Be strong for them.”
For Sofia, her cancer journey was integral to where she is heading in the future. Inspired by her medical team, she has decided to become a doctor herself so she can help others. “Now that I am 16, I can start thinking about universities and that path of being an Oncologist.”
Today, Frank looks back on the experience thoughtfully. “Cancer became part of our family journey, part of our story. These things help make you stronger to enable you to overcome adversity and change when you need to.”
Get the whole story. Check out our digital edition at lgfb.ca and watch the full video.