NJ PSYCHOLOGIST

A Publication of the New Jersey Psychological Association
In this issue...
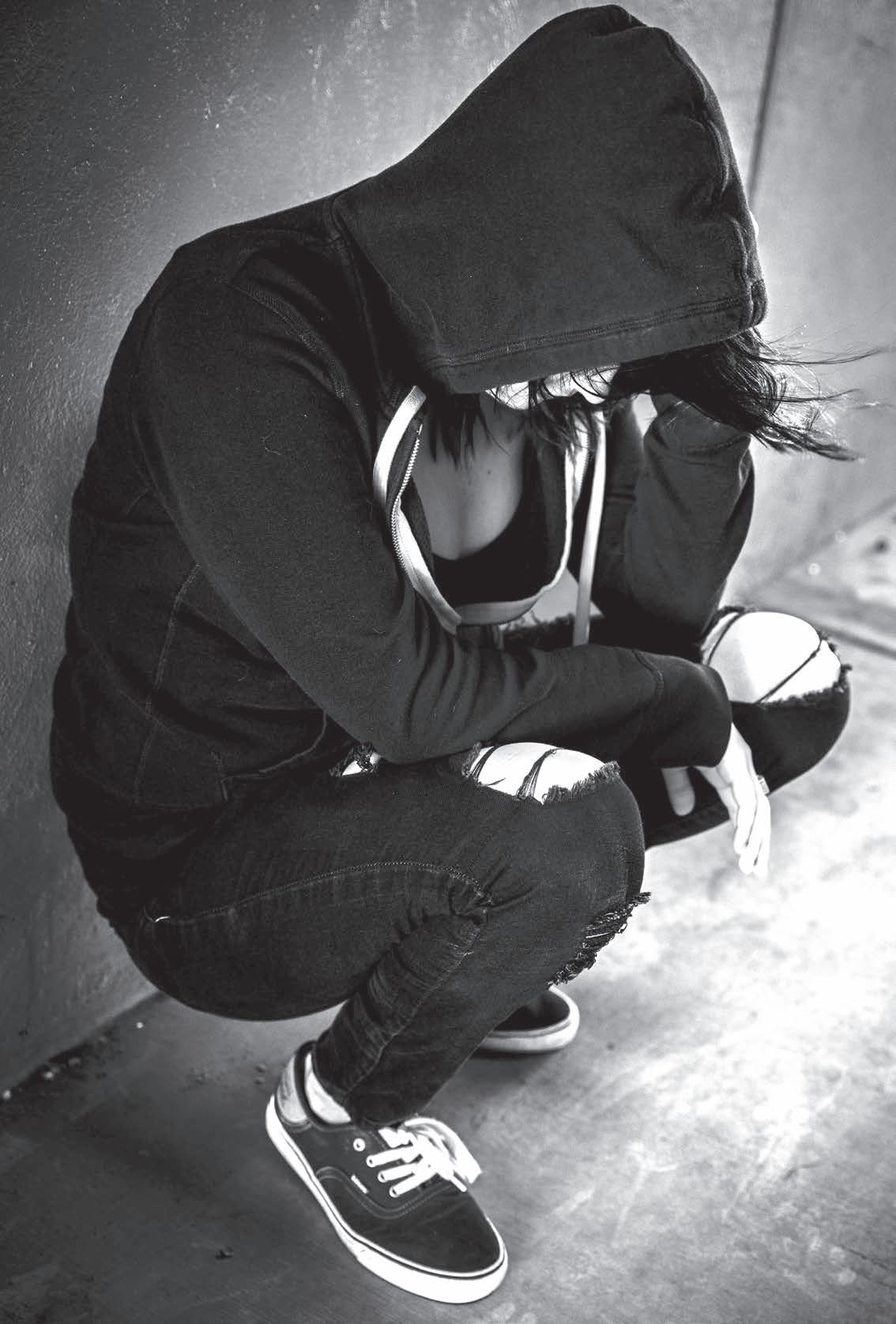
Special Section: New Jersey Department of Human Services Response to the Opioid Crisis
2 CE Credits
Ethics: “It’s Confidential...” When a Client Dies by Suicide
Critical Conversations in Continuing Education for New Jersey Psychologists
Continuing Education Requirement: Why is There an Emphasis on Addressing Diversity in Every Program?
1 CE Credit
Fall 2019 | VOLUME 69 | NUMBER 4
Table of Contents
1 Who’s Who in NJPA 2019
2 President’s Message
3 NJPA Association Life-Cycle
4 Research Briefs
5 Classified Ad
6 2019 Critical Conversations in Continuing Education for New Jersey Psychologists
8 Continuing Education Requirement: Why is There an Emphasis on Addressing Diversity in Every Program? (1 CE)
10 Ethics Update: “It’s Confidential...” When a Client Dies by Suicide
11 Welcome New Members!
12 Graduate Program: William Paterson University
13 Member News
14 Director of Professional Affairs: Scope of Practice
16 Foundation: Community Service Project Grants
19 Special Section: NJ Department of Human Services Response to the Opioid Crisis (2 CE)
25 Book Review: Howard Stern Comes Again (2019)
Who’s Who in NJPA 2019
www.PsychologyNJ.org
Editorial Board
Editor: Gianni Pirelli, PhD
Members:
Jack Aylward, EdD
Ashley Gorman, PhD
Eric Herschman, PsyD
Herman Huber, PhD
Maria Kirchner, PhD
Nathan McClelland, PhD
Anthony Tasso, PhD
Staff Liaison: Christine Gurriere
NJPA Executive Board
President: Morgan Murray, PhD
President-Elect: Lucy Sant’Anna Takagi, PsyD
Past-President: Stephanie Coyne, PhD
Treasurer: Daniel DaSilva, PhD
Secretary: Mary Blakeslee, PhD
Director of Academic Affairs: Francine Conway, PhD
APA Council Representative: Rhonda Allen, PhD
Member-At-Large:
(A) Elio Arrechea, PhD
(A) Phyllis Bolling, PhD
(A) Daniel Lee, PsyD
29
Preparation of Manuscripts
All manuscripts submitted for publication should follow APA style. Manuscripts should be edited, proofread, and ready for publication. Please prepare your manuscript in a word-processing program compatible with MS Word using Times New Roman font in 12 point type, left flush. Please submit your manuscript via e-mail to NJPA Central Office and to Gianni Pirelli at e-mail addresses below.
Editorial Policy
Articles accepted for publication will be copyrighted by the Publisher and the Publisher will have the exclusive right to publish, license, and allow others to license, the article in all languages and in all media; however, authors of articles will have the right, upon written consent of the Publisher, to freely use of their material in books or collections of readings authored by themselves. It is understood that authors will not receive remuneration for any articles submitted to or accepted by the New Jersey Psychologist
Any opinions that appear in material contributed by others are not necessarily those of the Editors, Advisors, or Publisher, nor of the particular organization with which an author is affiliated.
Manuscripts should be sent to the Editor: Gianni Pirelli, PhD
E-Mail: gpirelli@gmail.com or NJPA Central Office E-Mail: NJPA@PsychologyNJ.org
Published by:
New Jersey Psychological Association
354 Eisenhower Parkway, Plaza I
Suite 1150
Livingston, NJ 07039
973-243-9800 • FAX: 973-243-9818
E-Mail: NJPA@PsychologyNJ.org Web: www.PsychologyNJ.org
New Jersey Psychologist (USPS 7700, ISSN# 2326098X) is published quarterly by New Jersey Psychological Association, 354 Eisenhower Parkway, Plaza I, Suite 1150, Livingston, NJ 07039. Members receive New Jersey Psychologist as a membership benefit. Periodicals postage pending at West Orange, NJ and additional mailing offices. POSTMASTER: Send address changes to New Jersey Psychologist, 354 Eisenhower Parkway, Plaza I, Suite 1150, Livingston, NJ 07039.
(N) Randy Bressler, PsyD
(N) Alan Lee, PsyD
(N) Nicole Rafanello, PhD
Parliamentarian: Joseph Coyne, PhD
Affiliate Caucus Chair: Rosalie DiSimone-Weiss, PhD
ECP Chair: Michelle Pievsky, PhD
NJPAGS Chair: Christopher Thompson, MA, EdS
CODI Co-chairs: Phyllis Bolling, PhD and Aida Ismael-Lennon, PsyD
Affiliate Representatives
Northeast Counties Association of Psychologists: Nansie Ross, PsyD
Essex/Union County Association of Psychologists: Susan Esquilin, PhD
Mercer County Psychological Association: David Krauss, PhD
Middlesex County Association of Psychologists: Tammy Dorff, PsyD
Monmouth/Ocean County Psychological Association: Tamara Latawiec, PsyD
Morris County Psychological Association: Randy Bressler, PsyD
Somerset/Hunterdon/Warren Psychological Association: Janie Feldman, PsyD
South Jersey Psychological Association: Daniel Lee, PsyD
Central Office Staff
Executive Director: Keira Boertzel-Smith, JD
Director of Professional Affairs: Judith Glassgold, PsyD
Senior Communications Manager: Christine Gurriere
Continuing Education & Event Coordinator: Ana DeMeo
Membership Services Coordinator: Jennifer Cooper
Fall 2019 1
27 In Memoriam
28 NJPA Sustaining Members
from
Council
Report
APA
Efforts
30 NJPA Advocacy
Morgan Murray, PhD

Ihave much to be thankful for. Though I am writing this in early September and still have almost 4 months left in my time as NJPA president, this will be my last column in the NJ Psychologist and I feel compelled to say thank you. First to the general membership, without whose involvement there is no NJPA. Thank you to everyone that served on an NJPA committee, task force, or participated in the leadership of your local affiliate organization. It has been an exciting year, an incredible opportunity, and a privilege to do my part to advance the profession of psychology in New Jersey and our association. No endeavor like this can be accomplished alone, and I was blessed with a tremendous leadership team in our Executive Director, Keira Boertzel-Smith, JD, our President-Elect, Lucy Sant’Anna Takagi, PsyD, and our Past-President , Stephanie Coyne, PhD. I would add to this support team the tireless dedication
President’s Message

of the executive board that includes our Parliamentarian, Joe Coyne, PhD and, of course, the tireless efforts of Central Office staff, Christine Gurriere, Ana DeMeo, and Jennifer Cooper.
We moved forward on traditional guild issues this year. A prime example of this is the progress on our bill to allow graduate students and early career individuals, working to meet the requirements for licensure, to include all pre-doctoral supervision hours toward their license, and to no longer require that any must be acquired post-doctorly. Another example is that the Committee on Legislative Affairs (COLA), under Barry Katz’s leadership, worked hard to increase the transparency of NJPA’s legislative efforts, so that our membership can stay abreast of what bills we are following and where we are focusing our resources.
We also focused on efforts to expand beyond traditional guild issues (Murray, 2019) and looked at what psychology can say and do regarding many of the significant social issues that are faced in New Jersey. The Committee on Diversity and Inclusion (CODI) formed a subcommittee, Immigration Emergency Action Group (IEAG) to

to the humanitarian crisis created by the separation of immigrant families detained at four detention centers within New Jersey. The IEAG will look to collaborate with other agencies in its efforts to address the mental health needs of detained individuals. We also issued statements and endorsed statements that were based on psychological principles and consistent with the NJPA mission. This allows NJPA to use psychological science to enter into, and contribute more broadly to, the dialogue on issues related to the psychological well-being of the diverse residents of New Jersey. We also continued to develop our collaboration with the New Jersey Association of Black Psychologists (NJABPsi) and the Latinex Mental Health Association of New Jersey (LMNANJ). Our collaboration is accomplished through an affiliation of co-equals called the Inter-Mental Health and Psychological Association Coalition (IMPAC). This expansion beyond traditional guild issues is part of the changing face of professional psychology. Thank you! ❖
Reference
Murray, Morgan (Summer 2019). Expanding the Definition of Guild.
New Jersey Psychologist 2
NJPA Association Life-Cycle
Keira Boertzel-Smith, NJPA Executive Director

In May 2019, the NJPA Central Office staff boxed up NJPA documentation from the 1930s through 2019, awards we received, NJPA past presidents and Psychologist of the Year plaques, desks and chairs used by past executive directors, directors of professional affairs, and staff, and boardroom furniture used by the current and past executive boards, committees, and staff for meetings and continuing education programs. A huge thank you to the Central office team, Christine, Ana, Jennifer, and Marion, for helping me with the grimy and back breaking work of cleaning out cabinets, closets, and the kitchen, hauling items to the dumpster, as well as researching and utilizing the needed vendors to make the move happen. Thank you to the NJPA Capital Improvement Workgroup Chair, Ken Freundlich, PhD, and commercial real estate advisor and broker, Mark Twentyman, Kingsbridge Realty Advisors, for their hours of time put in on the road with me during the NJPA commercial real estate hunt.
This extensive 2019 NJPA moving process caused me to pause and reflect on the NJPA life-cycles: birth through the mature operational stages. As in all association life-cycles, there is the eventual decline in interest in the association “as is” that will either result in the association’s death or rebirth. I can report that NJPA is in a rebirth stage, with all hands on deck to ensure a new and improved NJPA identity that matches the needs and expectations of the evolving membership populations. This rebirth is clearly felt with the physical 2019 NJPA Central Office move, and we will be taking full advantage of the new space to host bigger and better meetings, continuing education events, and social gatherings.
Less visible rebirth manifestations are the updating of our internal association management policies and internal efforts to account for our members’ changing advocacy and outreach expectations, as well as the evolving NJPA communications, continuing education, financial, membership, and technology needs. NJPA continues to grow the statewide “Road Show” where the NJPA/NJPAF leadership team travel around the state to various NJPA affiliate organizations, universities, institutions, Board of Psychological Examiners meetings, and legislative appointments to discuss our mission and goals, topics of interest for graduate students and early, mid- and late-career psychologists in all work settings, state and federal legislative and social advocacy priorities and efforts, and the NJPA relationship with the American Psychological Association. Central Office is working on behalf of NJPA/NJPAF leadership, committees, and our members to promote the use of virtual meeting participation so members can incorporate NJPA and NJPAF into their busy lives.
In my current role as the chair of the APA Council of Executives of State, Provincial and Territorial Psychological Associations (CESPPA), I am working hard to advance the good reputation of New Jersey and NJPA, as well as promoting our rebirth efforts at the national level. On behalf of NJPA, I accepted APA CEO, Dr. Arthur Evans’ invitation to travel to state associations to talk about professional development of psychologists and the future of psychology (September 20, 2019 NJPA visit and CE program). In October, I organized a State, Provincial, and Territorial Psychological Association’s (SPTA) membership training with APA Chief of Strategic Implementation and Membership, Ian King, MBA, to discuss retention, recruitment, understanding member populations, and the relationship between SPTA and APA membership in these changing times for association membership. We are working to get Bradley K. Steinbrecher, JD, a representative from the APA Legal and Regulatory Department to host a continuing education program on HIPAA. CESPPA
is working to strengthen the relationship with the Association of State and Provincial Psychology Boards (ASPPB) leadership and the APA Continuing Education Committee to make sure that our associations stay up to date with their ongoing efforts. Also on behalf of NJPA, I have been sure to make use of APA’s Legal and Regulatory Affairs staff as valuable resources on NJPA advocacy and regulatory issues such as telepsychology, Medicaid reimbursement, and the New Jersey Licensure Act.
I look forward to carrying these growth opportunities and rebirth efforts into 2020 to ensure NJPA stays relevant to the profession, psychologists, and the public. I acknowledge and respect the around-the-clock work of the NJPA executive board, chairs, past NJPA leaders, NJPA staff, and members who all carry the load of the evolving association work, and I appreciate suggestions to improve my work as executive director.
This association provides, for all of us, invaluable lessons about life-cycles including rebirth, professional and personal grit, humility, and the need for healthy teamwork. NJPA should be very optimistic about its future! ❖
D E C 6 Save the Date!
Fall 2019 3
Research Briefs: Fall 2019 CLINICAL PSYCHOLOGY
Treatment/Diagnostic
Goghari & Harrow (2019). Anxiety symptoms across twenty-years in schizoaffective disorder, bipolar disorder, and major depressive disorder. Psychiatry Research, 275, 310-314.
Goghari and Harrow examined the trajectory of self-reported and somaticrelated anxiety for patients diagnosed with Schizoaffective (n = 43), Bipolar (n = 47), and Major Depression (n = 109) Disorders, to explore if early reports of anxiety predicted later outcomes. Patients were assessed longitudinally, i.e., six times over 20 years. The authors found that self-reported anxiety in earlier years of illness was greater for those with Schizoaffective Disorder and Major Depression than those with Bipolar Disorder, but the three groups were similar with respect to their experience of anxiety-related symptoms across 20 years. For all patients, self-reported anxiety in early years predicted a recovery period and lower global functioning in the future.
Krajniak, Pievsky, Eisen, & McGrath (2018). The relationship between personality disorder traits, emotional intelligence, and college adjustment. Journal of Clinical Psychology, 74, 1160-1173.
Working with college first-year students (n = 246), Krajniak et al. examined the relationship between emotional intelligence (EI), personality disorder (PD) traits, and college adjustment to understand the reasons and protective factors related to dropout rates. They found that PD symptoms and EI were inversely related, and unique patterns of association emerged between PD clusters and EI deficits. Both variables were related to adjustment, but EI did not moderate the relationship between PD and adjustment, as previously theorized, but the study proposed a mediating model for future research.
Kudinova, Woody, James, & Burkhouse (2019). Maternal major depression and
synchrony of facial affect during motherchild interactions. Journal of Abnormal Psychology, 4, 284-294.
Kudinova et al. examined synchrony of facial displays of affect during positive and negative mother-child interactions (n = 341 dyads) to understand how it may be impacted by maternal history of Major Depressive Disorder (MDD). Maternal MDD history increases children’s risk of developing depression. Facial electromyography (EMG) indexed mother and child facial affect. Maternal history of MDD was associated with reduced synchrony of positive affect; reduced synchrony of positive affect was associated with an increase in the child’s self-reported sad affect after the interaction. Therefore, positive affect in motherchild interactions may be disrupted in families with maternal MDD history.
Sibrava, Bjornsson, Perez Benitez, Moitra, Weisberg, & Keller (2019). Posttraumatic stress disorder in African American and Latinx adults: Clinical course and the role of racial and ethnic discrimination. American Psychologist, 74, 101-116.
Sibrava et al. explored the relationship between experiences of discrimination and risk for developing Posttraumatic Stress Disorder (PTSD) among African American and Latinx adults with Anxiety Disorders. This 5-year longitudinal study found that African American and Latinx participants had a 35% and 15% probability, respectively, of achieving full recovery and remission from PTSD symptoms after intake. Frequency of experiences of discrimination significantly predicted PTSD diagnostic status but did not predict any other anxiety or mood disorder. Thus, racial/ethnic discrimination may play a role in the development of PTSD and contribute to its chronic course.
Psychological Assessment
Helle & Mullins-Sweatt (2019). Maladaptive personality trait models: Validat-
ing the five-factor model maladaptive trait measures with the Personality Inventory for DSM-5 and NEO Personality Inventory. Assessment, 26, 375-385.
In the context of a convergent validity study, Helle & Mullins-Sweatt examined five-factor model (FFM) maladaptive trait scales specific to personality disorders in relation to the respective general personality traits of the NEO Personality Inventory-Revised (NEO-PI-R) and the pathological personality traits of the Personality Inventory for the DSM-5 (PID-5). Results suggested that the FFM maladaptive trait scales converged with corresponding NEO-PI-R and PID5 traits. This provides validity-related evidence for these measures as extensions of general personality traits and their relation to pathological trait models as well as support for the theoretical basis of utilizing the FFM to describe DSM-5 personality disorders.
Reis, Namekata, Oehlert, & King (2019, March 14). A preliminary review of the Beck Depression Inventory-II (BDIII) in veterans: Are new norms and cut scores needed?. Psychological Services. Advance online publication.
Reis et al. examined Veterans Health Administration (VHA)-specific use of the Beck Depression Inventory-II (BDI-II) to establish normative data within this population and assess its psychometric properties (n = 152,260). These BDI-II scores were compared against Beck and colleagues’ original sample, normed on adult psychiatric outpatients and college students, as well as across veteran subgroups. Factor analyses found a 2-factor model provided best fit, supporting Beck’s original solution. However, veterans scored significantly higher on the BDI-II than the original comparison groups across diagnostic categories which may require future investigation for its use with veteran populations.
New Jersey Psychologist 4
Psychiatry/Pharmacotherapy
Abbasi, J. (2017). Ketamine minus the trip: New hope for treatment-resistant Depression. JAMA, 318(20), 1964.
Administering one dose of ketamine can cause an extreme antidepressant impact for patients with treatment-resistant depression (TRD) without having side-effects of hallucinations. Current research is concentrating on ketamine as a treatment method for TRD and major depressive disorder (MDD) with imminent risk of suicide. The variety of traditional medications used to treat depression work solely on the monoamine neurotransmitter system and only treat a small number of patients, which results in low response to treatment and high remission rates. Clinical trials determined that ketamine is a valuable element in treatment-resistant depression by creating shorter response to treatment and lower remission rates, and it is effective for patients who have been unsuccessful with other antidepressant options.
Limandri, B. J. (2019). Pharmacogenetic testing: Why is it so disappointing? Journal of Psychosocial Nursing and Mental Health Services, 57(4), 9-12.
The benefits in current pharmacogenomic testing include reduced pricing, and in susceptible populations such as children and older adults, the testing can minimize polypharmacy or inaccurate drug trials. The limitations occur from the sole concentration on the metabolism of drugs. Pharmacogenomic testing cannot predict all possible outcomes that
a medication may have on an individual. As a result, clinicians’ question whether they should supply pharmacogenomic testing for their patients as standard protocol. Weighing the patient’s and their family’s medication use history against the strengths and weaknesses of pharmacogenomic testing can assist in determining an answer.
O’Brien, McNeil, et al. (2017). New fathers’ perinatal depression and anxiety— treatment options: An integrative review. American Journal of Men’s Health, 11(4), 863-876.
The authors created a conceptual model consisting of four categories in order to better understand paternal perinatal depression (PPND) and effective treatment methods. The first category pertains to the father’s responsibility in helping their significant other with perinatal depression (PND). The second factor suggests that the concept of perinatal mental health should be recreated to be viewed as a family concern as opposed to strictly a maternal issue. The third category concentrates on the male’s conversion into fatherhood, the absence of guidance, and the idea that father-oriented therapeutic methods are important. The fourth includes how fathers with PPND can consider the treatment options including cognitive behavioral therapy, group work, e-support strategies, and supplying a safe atmosphere designed using father-specific models of care.
Koek, Roach, Athanasiou, van ‘t WoutFrank, & Philip. Neuromodulatory treat-
Classified Ads
ments for post-traumatic stress disorder (PTSD). Progress in Neuro-Psychopharmacology and Biological Psychiatry, 92(8), 148-160.
The is a review of published data involving the use of neuromodulation in PTSD. This study summarizes that the primary components include neural circuits associated with threat-sensitivity, safety learning, emotion regulation, and contextual learning. There is an increasing amount of technology-based neuromodulation methods that allow for concentrating focus on abnormal limbic circuitry, while previous approaches to neuromodulation were more non-specific.
Bushnell, Gaynes, Compton, Dusetzina, Brookhart, & Stürmer (2018). Incidence of mental health hospitalizations, treated self-harm, and emergency room visits following new anxiety disorder diagnoses in privately insured U.S. children. Depression and Anxiety, 36(2), 179-189.
In this large-scale study, the researchers identified 198,450 children from 20052014 and followed them for two-years following an initial outpatient diagnosis of an anxiety related disorder. Authors found that following this initial diagnosis, 2.0% of children had a mental health–related hospitalization, 0.08% inpatient hospitalization for self-harm, 1.4% had an anxiety-related ER visit, and 20% had any ER visit. The incidence was highest in older children with baseline comorbid depression. These incidence rates were significantly higher compared with children without an anxiety diagnosis. ❖
The NJ Psychologist accepts advertising of interest to the profession. The minimum rate for Classified Ads is $75 for up to 50 words, $1 for each additional word. For display ad information, email inquiries to NJPAcg@PsychologyNJ.org ATTN: Christine Gurriere, or call 973-243-9800. The NJ Psychologist is mailed on or about the 10th of February, May, and November. Acceptance of advertising does not imply endorsement by NJPA.
NEUROPSYCHOLOGIST/EDUCATIONAL PSYCHOLOGIST/PSYCHOLOGIST
NEUROPSYCHOlOGICAL/IQ TESTING
Central NJ: Monmouth and Ocean County.
GREAT OPPORTUNITY!: for Part Time, Per Diem, Extra Income. Neuropsychological Testing Administration; Experience with Concussions, Auto Accidents and Work Injuries a plus.
(*) Bilingual (English/Spanish) preferred as well.
Long-Term, Stable Employment. Excellent working conditions. State Licensure/Permit preferred. Please e-mail your resume to: NRABP@AOL.com
Fall 2019 5
EDUCATION AFFAIRS
2019 Critical Conversations in Continuing Education for New Jersey Psychologists
Internal Efforts
The New Jersey Psychological Association (NJPA) is approved by the American Psychological Association (APA) to sponsor live and homestudy continuing education for psychologists. NJPA maintains responsibility of the live and homestudy NJPA and NJPA co-sponsored programs and content. We take our relationship with APA and our APA sponsorship seriously and strive to continue to work with APA in our shared ongoing commitment to excellence in continuing education.
APA as a CE Resource
In August, NJPA received a copy of a special issue of the APA Professional Psychology: Research and Practice dedicated to conversation around continuing education from Director of the APA Office of CE in Psychology, Greg Neimeyer, PhD. The publication addresses topics such as continuing education best practices, the relationship between continuing education and professional competence, and assessment and outcomes associated with continuing education and interprofessional continuing education. NJPA will continue to use APA resources, such as this recent publication, to further grow the NJPA continuing education programming and standards. NJPA Executive Director and APA Council of Executives of State, Provincial and Territorial Psychological Associations (CESPPA) Chair, Keira Boertzel-Smith, is currently working at the national association level to further define and develop the role of the CESPPA liaison to the APA Continuing Education Committee. The goal of this CESPPA liaison role is to ensure that all state associations understand the APA continuing education sponsorship approval and reporting process, and that they have the best chance at maintaining or gaining APA sponsorship approval.

Internally, NJPA created the NJPA Council on Continuing Education Affairs (CoCEA), pursuant to the NJPA mission and following the NJPA strategic plan goals, that is charged with managing NJPA’s continuing education development and program review. NJPA continues to find ways to use technology enhancements and platforms for program review, event management, and organizational tools for continuing education tracking. NJPA continuing education programs are created and provided for New Jersey psychologists to be applied towards the mandatory 40 credits of continuing education related to the practice of psychology; four credits of the 40 credits in topics related to domestic violence and one credit of the 40 credits addressing the risks and signs of opioid abuse, addiction, and diversion.
Statewide and Virtual Programs
NJPA and NJPA co-sponsored live programs are held across the state of New Jersey: North, Central, and South. NJPA moved its central office space to Livingston, NJ, partially to have access to larger continuing education venue space at a discounted cost to NJPA members. NJPA also provides homestudy learning options for credit in most of our quarterly NJ Psychologist journal publications and will host upcoming recorded programs. So far in 2019, NJPA hosted, or co-sponsored, approximately 35 live continuing education programs and four homestudy learning options.
How NJPA and NJPA Co-Sponsored Programs are Unique
NJPA has the challenge of ensuring that we remain competitive and relevant in the continuing education market for the profession of psychology. What NJPA and NJPA co-sponsored continuing education programs can uniquely offer you:
1. NJPA programs take advantage of our relationship with APA, such as the September 20, 2019 program An Emerging Framework for Healthcare: Opportunities for Psy-
chologists - A day with APA CEO, Arthur C. Evans Jr., PhD.
2. NJPA looks to our current NJPA advocacy initiatives to create programs related to current New Jersey advocacy issues, such as our planned 2020 continuing education programs on the New Jersey Duty to Warn Law, New Jersey Telemedicine, and the opioid article in this journal.
3. NJPA strives to highlight our collaborative partnership in the New Jersey Inter-Mental Health and Psychological Associations Coalition (IMPAC) through continuing education programs. The goal for IMPAC is for the New Jersey Chapter Association of Black Psychologists (NJABPsi), the Latino Mental Health Association of New Jersey (formerly the Latino Psychological Association of New Jersey), LMHANJ, and NJPA to join together as equal partners to contribute their unique educational acumen, expertise, experience, and perspectives to obtain synergy as a resource to promote equality in mental health care and to zealously advocate for the mental health needs for the diverse population of the state of New Jersey. An example of our efforts was the April 12, 2019 IMPAC Shine a Light on Multicultural Mental Health Awareness in New Jersey continuing education program.
4. NJPA and NJPA co-sponsored continuing education programs are produced, reviewed, and approved by the NJPA CoCEA Programming and Review Committees with the full NJPA membership in mind. I thank our NJPA CoCEA Programming, Homestudy, and Review Committees for their hard work and dedication to developing unique and customized continuing education opportunities that impact psychologists in New Jersey. Their hard work ensures that New Jersey
New Jersey Psychologist 6
COUNCIL ON CONTINUING
Dennis Finger, EdD, Council on Continuing Education Affairs (CoCEA) Chair
psychologists are enhancing their educational growth and improve their practices for their patients.
Council Members: Past-Chair, Marc Gironda, PsyD; Past Past-Chair, Phyllis Lakin, PhD; Ray Hanbury, PhD; Mark Lowenthal, PsyD; Nathan McClelland, PsyD; Leah Anne McGuire, PhD; Sharon Ryan Montgomery, PsyD; Membership Chair, Randy Bressler, PsyD; Treasurer, Daniel DaSilva, PhD; CODI Representatives, Susan Esquilin, PhD and Abisola Gallagher, EdD.
Programming Committee: CoChairs, Leah Anne McGuire, PhD, and Sharon Ryan Montgomery, PsyD; Phyllis Bolling, PhD; Caitlin Colandrea, PsyD; Peter DeNigris, PsyD; Cassandra Faraci, PsyD; Sangeetha Nayak, PhD; Marcy Pasternak, PhD.
Review Committee: Co-Chairs, Ray Hanbury, PhD and Mark Lowenthal, PsyD; William Coffey, PsyD; Julia Conrath, PhD; Osna Haller, PhD; Martin Krupnick, PsyD; Denise Ricciardi, PsyD; Nancie Senet, PhD.
Homestudy Committee: Chair, Nathan McClelland, PsyD.

On behalf of COCEA, we express our appreciation to our Executive Director, Keira Boertzel-Smith, JD, and to our CE Coordinator, Ana DeMeo and all of the NJPA staff for all of the hard work they do for NJPA’s continuing education. We also thank our current NJPA President, Morgan Murray, PhD, for all of his help and support during 2019.
5. Lastly, attendance at live NJPA and NJPA co-sponsored programs offer opportunities to network with
your New Jersey peers before, during, and after our continuing education programs.
We hope to see you soon at an NJPA or NJPA co- sponsored continuing education program. Learn, stay updated on New Jersey laws and regulations, meet your mandatory continuing education requirements, and network with your peers! ❖
Fall 2019 7
As featured in The New York Times Magazine! Anxiety, OCD, Intrusive Thoughts? We Get It! We Specialize in the Treatment of Adolescent Anxiety and OCD. Located in New Hampshire’s Upper Valley, we are a short-term, residential treatment center. Contact Admissions: 603-989-3500 www.mountainvalleytreatment.org
Continuing Education Requirement: Why Is There an Emphasis on Addressing Diversity in Every Program?
diversity is a critical consideration for all of us for two major reasons.
Susan Cohen Esquilin, PhD

CE Diversity Requirement
Last year, NJPA received a fiveyear authorization from APA to grant psychology continuing education (CE) credits. This was a major accomplishment, as the application for this authorization was detailed and complex, and not all applicants, including other state psychological associations, received such authorization. Among other requirements, NJPA had to demonstrate to APA that issues of diversity would be addressed in every program or publication for which we would grant CE credits. In addition, when APA reviews our programs at annual intervals, NJPA must present evidence that we did what was required, i.e., that issues of diversity were, in fact, addressed. Over the last few decades, APA drafted and redrafted guidelines for work with a variety of demographic groups. Most recently, the importance of attention to diversity has been underscored by new APA multicultural guidelines (American Psychological Association, 2017) and guidelines on practice with boys and men (American Psychological Association, Boys and Men Guidelines Group, 2018), as well as work this year in APA on the development of guidelines for work with people of low income and economic marginalization and of guidelines related to race and ethnicity.
Some of our colleagues have questioned both the need for a requirement about addressing diversity in every continuing education endeavor, as well as our routine inquiry in the evaluations of each presenter at the end of every program about whether each presenter met this requirement. Some feel this attention to the issue of diversity is excessive or irrelevant. However,
Addressing
Diversity Furthers the Scientific Basis of Our Professional Work
Psychology views itself as a science, and applied psychology prides itself on using research-based evidence as the undergirding of its assessment and treatment interventions. When we learn a new intervention technique, we want and need to hear about the evidence that supports its usefulness. The question is whether the individuals with whom this technique has been used represent our client in significant ways. Has this technique been examined with clients of a variety of racial or ethnic backgrounds, including the background of our specific client? Have studies found a difference in the way men and women respond to this technique? If the subjects who have been studied are primarily White, middle class Americans, should we try the technique anyway on a client who is different from that demographically? What might we want to consider if we apply this technique to a member of a group who has not been considered in any of the research? So, the current requirement for a program approved for CE is that, prior to the program, the presenter should research the question of the characteristics of the people on whom this technique has been developed and studied. And, in the absence of available research, the presenter should raise for consideration by participants the issues that they might expect would arise if the technique is used with a person from a demographic group that is not part of the sample studied. Similarly, a discussion about a new assessment instrument should make clear who was in the normative sample. There will always be limitations regarding this question, and those limitations should be identified. Those limitations may include the complete absence of certain groups (immigrants are often omitted) and the underrepresentation of certain groups
as compared with their numbers in the population (this has often happened regarding Black people). In addition, a new assessment should report whether there are differences in how the various groups performed on the assessment instrument and provide different tables for each group or make suggestions for how to adjust for such differences in scoring. The PAI manual, for example, points out that a difference is found between White and Black participants in the standardization sample regarding only the paranoia scale. The manual discusses the likely reason for that difference and recommends a strategy for adjusting for it. Any of these shortcomings should make us cautious about relying on such an instrument for conclusions about people who are inadequately accounted for in the validation studies, and anyone presenting about a new technique should be calling attention to those limitations. Again, it would be useful in a CE presentation to then engage in a discussion with participants about what further research is needed and/or about how to use the assessment technique cautiously.
Importance of Awareness of Diversity on Clinical Rapport
New Jersey is one of the most diverse states in the United States with regards to ethnicity and religion, so the issue of diversity is particularly relevant for professional work in New Jersey. Estimates made in late 2018 indicated that, racially, New Jersey is 68.1% White, 13.5% Black, 9.2% Asian, 6.4% other races, 2.5% two or more races. Almost 40% of the population speak languages other than English, with Spanish as the most common non-English language spoken by 16.4% of the population. New Jersey is the state with the second largest Jewish and Muslim populations. It has the most Peruvians, the second largest population of Cubans, with very high numbers of Portuguese, Brazilians, Arabs, Chinese, and Italian Americans. (New Jersey Population 2019, 2018).
New Jersey Psychologist 8
Representative
CE
CODI
1
Credit
The issues raised by diversity are omnipresent, whether we are aware of them or not. A lack of awareness on our part can easily disrupt developing therapeutic alliances with clients. The clients we evaluate and treat represent a vast array of human differences based upon a variety of variables, including race, gender, socioeconomic status, sexual orientation, religion, ethnicity, ability status, immigration status, and developmental stage. In addition, we are increasingly recognizing the importance of intersectionality, e.g., how race and gender may intersect to produce significant differences in the challenges people face, in how people experience the world, and in the difficulties they present. The experiences and difficulties of White women and Black women may be very different in significant ways, so it may not be sufficient to understand something about women or something about Black people to have a more nuanced understanding of the status of being a Black woman.
Some differences are obvious when we look at a client, but many differences are invisible. We learn about them only if we are open to hearing about them. If we do not entertain the possibility that this client has a significant hidden identity that is crucial to understanding the client, we may never hear about it and the client may, in fact, simply withdraw from treatment because the client senses that we are closed to his/her experience. These hidden identities may include membership in a subculture that endorses activities that are alien or unfamiliar to the psychologist or that the psychologists never even considered might exist (e.g., a gun subculture).
Conclusion
As individual psychologists, and as a profession, we are constantly learning. As we recognize the many ways that clients may differ from one another, we must learn to integrate this recognition into our work. If our treatment and assessment methods are not built on research inclusive of people from different backgrounds, then our work is limited in its applicability and effectiveness. The new CE requirement will broaden the scope of both our sensitivity to what we do not know as well as increase our
knowledge and skills about what the research has already found. Both our growing skills and sensitivity will improve our competency as individual clinicians and the esteem in which the public holds our profession. ❖
References:
American Psychological Association (2017). Multicultural Guidelines: An Ecological Approach to Context, Identity, and Intersectionality. Retrieved from <http://www.apa.org/about/policy/ multicultural-guidelines.pdf>
American Psychological Association, Boys and Men Guidelines Group. (2018). APA guidelines for psychological practice with boys and men. Retrieved from <http://www.apa.org/about/policy/ psychological-practice-boys-menguidelines.pdf>
New Jersey Population 2019 (2018, November 30). Retrieved from <http://worldpopulationreview.com/ states/new-jersey-population/>
About the Author
Susan Cohen Esquilin, PhD, is in independent practice. Trained as a clinical and developmental psychologist, she currently focuses her practice on forensic issues. Dr. Esquilin is president of the Essex-Union County Association of Psychologists, a member of the NJPA Committee on Diversity and Inclusion, co-chair of the Immigration Emergency Action Group, and a member of CoCEA (Council on Continuing Education Affairs).
Continuing Education Instructions: Visit <www.psychologynj.org> and find the CE Homestudy Library link under the Learn tab. This will take you to the online library where you will find the article and evaluation.

Fall 2019 9
When a Client Dies by Suicide
by the same provisions for living patients set forth in N.J.A.C. 13:428.3, 8.4, and 8.5; and
Sarah Dougherty, PsyD Ethics Committee Member
What happens when a client dies by suicide?
Hopefully you never experience such a loss. However, data shows that a therapist’s odds of losing a client to suicide, at some point in his or her career, are at least one in four, perhaps higher. And if a therapist works in a group practice or hospital setting with other therapists, the likelihood increases that, at some point, they will know a colleague who loses a patient.
What would you do?
Losing a patient to suicide is perhaps among a therapist’s greatest fears. For most clinicians, it is the outcome we dedicate our careers toward avoiding, the “termination” universally dreaded. The basic risk management considerations are learned early in clinical training: Alert and communicate with your supervisor, if you have one. Notify your insurer. Secure the client file. Do not, under any circumstances, alter the records. Each of these recommendations seems to underscore the perceived need to batten down the hatches, keep quiet, and hope for the best.
The statutes regarding confidentiality following a client’s death are equally clear. When a client dies, regardless of the cause, the therapist is bound by the same limits of confidentiality as for a living client.
Confidentiality survives the client’s death.
In the case of a client’s death:
1) Confidentiality survives the client’s death and a licensee shall preserve the confidentiality of information obtained from the client in the course of the licensee’s teaching, practice, or investigation;
2) The disclosure of information of a deceased client’s records is governed
3) A licensee shall retain a deceased client’s record for at least seven years from the date of last entry, unless otherwise provided by law.
Therapist-client confidentiality is among the cornerstones of ethical practice. Confidentiality engenders trust and reassures the client it is safe to talk about deeply personal matters without fear of exposure. However, in the aftermath of a client suicide, does “confidentiality” cast an overly legalistic shadow that potentially cultivates distrust between the therapist and the deceased client’s survivors?
Not surprisingly, following a suicide, when grieving family members know or learn of the deceased client’s mental health treatment history, they may reach out to the psychologist (and other treatment team members) as they struggle for some explanation for the death of their loved one. Often, family members are in shock, highly distraught, and possibly angry. However, unless the now-deceased client previously authorized the psychologist, in writing, to communicate or share information with the caller, the clinician is legally prohibited from sharing client information or even divulging the existence of a professional relationship with the deceased. Nor may the therapist reach out to the family, post-suicide, to express condolences or offer support. There are two exceptions available to survivors of the deceased: 1) A copy of the clinical record must be provided in response to a written court order signed by a judge; or 2) A copy of the clinical record must be provided in response to a written request from the documented executor of the deceased client’s estate, who is recognized as the deceased patient’s living “stand-in.” *
Records maintained as confidential pursuant to N.J.A.C. 13:42-8.1(c) shall be released:
2) Pursuant to an order of a court of competent jurisdiction;
3) Except as limited by N.J.A.C.
13:42-8.4, upon a waiver of the client or an authorized representative to release the client record to any person or entity, including to the Violent Crimes Compensation Board.2
The immediate aftermath of a suicide is emotionally charged and chaotic. Under the circumstances, a psychologist’s professional obligation of confidentiality may be interpreted by grieving family as stonewalling. Presumed “secrets” maintained by the treating therapist may take on disproportionate importance for the survivors, and client records, once obtained, may offer disappointingly little insight or comfort to the grieving family. Is confidentiality in the wake of a client suicide, followed to the letter, potentially harmful?

At the same time, the therapist may feel unduly burdened by his or her own feelings around the client’s death. Therapists are people, too, and feelings about a client’s suicide can be profound. It is not unusual, post-suicide, for a therapist to experience guilt, self-doubt, or shame, or to question his or her own clinical competence even when good care was provided. There may be financial concerns, fear of legal repercussions, worry about loss of professional reputation, and a reluctance to seek support from colleagues.
Who benefits from confidentiality, post-suicide?
At best, confidentiality may briefly postpone communication between the therapist and suicide survivors while the requisite release is obtained. This hiccup may give the therapist a bit more time to prepare for the encounter. More likely, however, the delay heightens anxiety for both the family and therapist and may further erode already dwindling trust.
While grief of any kind is painful, grief after suicide can be particularly complex. During “ordinary” grief, though there may be regrets, the primary tasks of grieving involve coming to terms with the absence of the person, and developing a new “relationship” with the memory of the person. In grief after suicide, the cause of death frequently eclipses memories of
New Jersey Psychologist 10 “It’s Confidential…”
ETHICS UPDATE
the life of the deceased, such that normal grieving is obstructed. Depending upon a survivor’s proximity to the actual suicide scene, the act of the suicide may constitute additional, bona fide trauma. Perceptions that a therapist is not being forthright may pose yet another barrier to processing of grief.
Perhaps there is an argument to be made for revisiting and possibly reconsidering the current parameters of confidentiality following client suicide. Potential benefits of greater openness between therapist and survivors include minimizing further trauma, reducing or deterring potential animosity, and promoting healthy grieving. Whereas it is not the therapist’s responsibility to treat family members (that would be frankly unethical), a therapist trained in grief triage could offer support and referrals to bereaved family, such that instead of being a lightning rod, the therapist could be a
resource. Being contacted by family postsuicide may be highly stressful, particularly when the therapist is feeling flummoxed about how to respond. However, training around post-suicide protocol could help prepare the therapist for survivor reaction, offer tips around self-care, and underscore the value of the therapist’s simply being present for the family. Also, hearing survivors’ perspectives about the deceased could help the therapist reach new understanding of the circumstances in which the client chose to take his or her life.
And finally, greater openness between therapist and survivors, post-suicide, is not tantamount to “spilling the beans.” Therapists are highly trained to exercise discretion and use good clinical judgment in all their professional endeavors. If confidentiality between a therapist and living client is intended to promote trust, perhaps a more open, more compassionate,
less legalistic posture with survivors in the aftermath of a client suicide could better serve us all. ❖
References
*Records also must be released 1) If requested or subpoenaed by the Board or the Office of the Attorney General in the course of any Board investigation; or 4) In order to contribute appropriate client information to the client record maintained by a hospital, nursing home, or similar licensed institution which is providing or has been asked to provide treatment to the client.
2NJ Administrative Code, Title 13, Law and Public Safety, Chapter 42, Board of Psychological Examiners (Last Revision Date 8/2018)
WELCOME NEW MEMBERS!
Licensed 5+ years
Valerie Brooks-Klein, PhD
Stacey Cohen-Meissner, PhD
Joseph Cooper, PsyD
Marilyn Denninger, PhD
Amy Dodds, PhD
Jennifer D’Ostilio, PsyD
Guillermo Gallegos, PhD
Roger Goddard, PhD
Paul Groenewal, PsyD
Michael Lindemann, PhD
Jamie Messina, PhD
Jami Messina, PhD
Elizabeth Midlarsky, PhD
John Miele, PhD
Thomas Morgan, PsyD
Maureen Nallly, PhD
Joseph Perzel, Jr, PsyD
Donna Rukin, PhD
Sandra Sabatini, PsyD
Michael Schubert, PhD
Eris Schleifer, PhD
Francis Schwoeri, PhD
Michael Shrem, PsyD
Karen Skean, PsyD
Margaret Van Sciver, PhD
Jennifer Weberman, PsyD
Licensed 2-5 years
Karen Donahue, PsyD
Mihaela Epurianu Dranoff, PhD
Michael Gross, PsyD
Aaron Gubi, PhD
Kristine Hodshon, PsyD
Jennifer Kennedy, PsyD
Natalie Nageeb, PsyD
Andrea Tesher, PsyD
Licensed less than 2 years
Kevin Giangrasso, PsyD
Corrinne Kalafut, PsyD
Amy Origlieri, PhD
Esther Reidler, PhD
Melany Rivera-Maldonado, PhD
Joshua Tal, PhD
2nd year Post-Doctoral
Juliana Claps, PsyD
Scott Thien, PsyD
Associate Member
Rachel Kalinsky, MEd
Students
Laura Betheil, MSEd
Cindy Chang, BA
Docia Demmin, MA
Mike Dikenson, BA
Beth Granet, PsyD
Gabrielle Guzman, PsyM
Molly Kammen, MA
Victoria Kealy
Marina Oganesova, MA
Yael Osman, MA
Lauren Rosenberg, MA
Phoebe Shepherd, PsyM
Anna Stadtmueller, MA
H. Gemma Stern
Fall 2019 11
PsyD program in Clinical Psychology
Our full-time, five-year, scholar-practitioner training program is accredited by the American Psychological Association When you enroll in the PsyD program at William Paterson University of New Jersey (WPUNJ), your studies will integrate academic coursework, supervised clinical training, and research experience in a small, supportive community of peers and mentors. Current and prospective students commonly say they choose WPUNJ because of the strong sense of community and care among the dedicated students and faculty.
A distinguished faculty of active scholars and practitioners, who have diverse interests in both clinical practice and research, will support your training in evidence-based assessment and intervention. The faculty offers individualized attention in our state-of-the-art complex that includes teaching and research facilities, as well as a psychology clinical training suite, featuring recording and monitoring equipment.
WPUNJ PsyD CORE FACULTY:
Michele Cascardi, PhD: Research aims to improve measurement of adolescent relationship abuse from early adolescence into young adulthood. Her work also focuses on bystander education to prevent sexual and relationship violence, as well as trauma, attachment, and social information processing theories that contribute to risk for aggressive behavior in romantic relationships. Dr. Cascardi is a consulting forensic psychologist.
Megan Chesin, PhD: Specializes in the study of impulsive-aggressive behavior and third-wave behavioral treatments, such as Mindfulness-Based Cognitive Therapy and Dialectical Behavior Therapy. Dr. Chesin is a consulting psychologist on clinical trials testing treatments for depression and suicide prevention, providing supervision to
therapists and conducting psychosocial assessments.
Jan Mohlman, PhD: Research and clinical work focus on the etiology, course and treatment of anxiety disorders across adulthood (particularly in older adults), cognition and emotion, and in investigating brain-behavior relationships in psychopathology. Dr. Mohlman is a practicing clinician.
Bruce Diamond, PhD: Specializes in clinical neuropsychology, neurorehabilitation, and cognitive neuroscience. His research uses neuropsychological assessments and computer-based measures including brain imaging/autonomic techniques with neurologic, neuropsychiatric, and neurodevelopmental populations. Dr. Diamond is a practicing neuropsychologist.
Aileen Torres, PhD: Research interests include multicultural competency, trauma-informed treatment, child abuse/ neglect, cultural adaptation of recent immigrants, and ethnic identity development. Dr. Torres is a practicing clinician conducting individual and family therapy, as well as immigration-related and child maltreatment forensic psychological evaluations.
Greg Bartoszek, PhD: Investigates cognitive, psychophysiological, behavioral, and motivational aspects of emotions and affective psychopathology. His research interests include comorbidities among mental health problems and mechanisms of change in evidence-based psychotherapies. Dr. Bartoszek is a practicing clinician.
The program has been carefully designed to prepare graduates for pursuit of clinical, teaching, or research positions in a wide variety of professional settings. Graduates of the PsyD program who wish to become licensed clinical psychologists must additionally pass a national examination and fulfill all state licensing requirements.
Graduate assistantship opportunities are available to select students with outstanding credentials. The assistantships provide tuition waivers and a stipend. Students may obtain a Master’s in Clinical and Counseling Psychology en route to the PsyD degree. After earning a master’s degree, qualified graduate students are eligible to teach as adjunct faculty to gain undergraduate teaching experience and earn additional financial support.
For more information on our PsyD program in Clinical Psychology, please visit our website: <https://wpunj.edu/ cohss/departments/psychology/psyd/>.
Students may apply for admission through PsyCAS, the Centralized Application Service for graduate study in psychology: <https://psycas.liaisoncas. com/applicant-ux/#/login>.
Drs. Michele Cascardi, Program Director (cascardim@wpunj.edu) and Uzma Ali (aliu@wpunj.edu), Graduate Admissions Coordinator, are also available by email or phone (973) 7203500 to answer your questions and provide more information.
Master’s program in Clinical and Counseling Psychology
The Master’s program in Clinical and Counseling Psychology at William Paterson University in Wayne, NJ prepares students for careers as Master’s level mental health clinicians, researchers, or to work in various human services settings. The curriculum provides a solid grounding in both theories and interventions. We emphasize clinical skills, ethical responsibility, cultural competency, self-awareness, and current body of knowledge in the scientific, methodological, and theoretical foundations of practice. In addition, we are committed to social justice work and multiculturalism to serve disadvantaged or marginalized groups in our society. Our program faculty members are

New Jersey Psychologist 12
Graduate Program WPU
licensed psychologists actively involved in clinical practice and research in the field. They have research and clinical strengths in health psychology, trauma, resilience, racial and ethnic socialization, bilingual counseling with immigrant populations, school-based interventions, and neuropsychology. ❖
Citations of Recent Publication by WPU faculty and students
Ma, P-W., & Shea, M. (2019). FirstGeneration College Students’ Perceived Barriers and Career Outcome Expectations: Exploring Contextual and Cognitive Factors. Journal of Career Development. Online First: https://doi. org/10.1177/0894845319827650
Margolis, M. & Austin, J. & Wu, L. & Valdimarsdottir, H. & Stanton, A. & Rowley, S…& Rini, C. (2019). Effects of Social Support Source and Effectiveness on Stress Buffering After Stem Cell Transplant. International Journal of Behavioral Medicine. 10.1007/s12529-019-09787-2.
Raghavan, S. & Sandanapitchai, P. (2019). Correlates of Resilience to Trauma in a Multinational Sample. Frontiers in Psychology: Cultural Psychology, doi: 10.3389/ fpsyg.2019.00131
Raghavan, S. (2018). Cultural Considerations in the Assessment of Survivors of Torture: A Review. Journal of Im-
migrant and Minority Health, doi: 10.1007/s10903-018-0787-5.
The MA in Clinical and Counseling Psychology program is accredited by the Masters in Psychology and Counseling Accreditation Council (MPCAC) under the psychology academic standards for the period of July, 2015 through July, 2025. The priority deadline is March 1st for the Fall semester but applications will be accepted until May 1st. Fall enrollment only. To Apply, please visit PSYCAS.
Les Barbanel, EdD has a new book Return to Harmony: Conflict Management for Couples that can be purchased online from Amazon, Barnes & Noble, and Archway Publishing. The book, intended for both professional and non-professional audiences, introduces the concept of “couple intelligence (CQ)” and provides an assessment scale in the appendix that yields a CQ score, analogous to traditional measures of intelligence (IQ). The book is reviewed in the Spring issue of NJ Psychologist, Vol. 69, and is targeted for both the professional and non-professional reader.
Ruth Lijtmaer, PhD presented the paper: Marie Lang, Her Life and Work in the panel: Liberation Psychology and Psychoanalysis as Social Revolution: The Clinical and Community Contributions of Marie Langer. International Psychohistory Association (IPA) Conference : The Intersection of Psychology and History: The Contributions of Michael Eigan to Human Understanding. 5-22-19 to 5-24-18. New York, NY. She also had published: Response to Peter Petschauer’s paper: The Flame of Trauma. (2019) Clio’s Psyche,25, 3, 246-249.
Christopher Lynch, PhD has a new book titled Anxiety Management for Kids on the Autism Spectrum: Your Guide to Preventing Meltdowns and Unlocking Potential from publisher Future Horizons. You can find a description of the book on amazon.com. This is his second published book and a companion to his first publication: Totally Chill My Complete Guide to Staying Cool: A Stress Management Workbook for Kids with Social, Emotional, or Sensory Sensitivities (AAPC Publishing, 2012).
Peggy Rothbaum, PhD (Spring, 2019). Evaluating Our Focus: The national move towards population health must include humane animal care/control law enforcement professionals. Animal Care & Control Today, 30-31. (June 27, 2019) Protecting the Protector: Who is Taking Care of You? Justice Clearing House (National Animal Care and Control Association): Webinar.
Fall 2019 13
PS Form 3526 Statement of Ownership, Management, and Circulation (Requester Publications Only) 1. Publication Title 2. Publication Number ISSN 3. Filing Date NEW JERSEY PSYCHOLOGICAL ASSOCIATION/NEW JERSEY PSYCHOLOGIST 7700 2326-098X 10/18/2019 4. Issue Frequency 5. Number of Issues Published Annually 6. Annual Subscription Price QUARTERLY 4 $ 40.00 7. Complete Mailing Address of Known Office of Publication 414 EAGLE ROCK AVE STE 211 WEST ORANGE, ESSEX, NJ 07052-0075 Contact Person CHRISTINE GURRIERE Telephone (973) 243-9800 8. Complete Mailing Address of Headquarters or General Business Office of Publisher 354 Eisenhower Pkwy Ste 1150 Livingston, NJ 07039 9. Full Names and Complete Mailing Addresses of Publisher, Editor, and Managing Editor Publisher (Name and complete mailing address) Hermitage Press 1595 Fifth St Trenton, NJ 08638 Editor (Name and complete mailing address) Gianni Pirelli, PhD Managing Editor (Name and complete mailing address) Hermitage Press 1595 Fifth St Trenton, NJ 08638 10. Owner (Do not leave blank. If the publication is owned by a corporation, give the name and address of the corporation immediately followed by the names and addresses of all stockholders owning or holding 1 percent or more of the total amount of stock. If not owned by a corporation, give names and addresses of the individual owners. If owned by a partnership or other unincorporated firm, give its name and address as well as those of each individual owner. If the publication is published by a nonprofit organization, give its name and address.) Full Name Complete Mailing Address New Jersey Psychological Assoc 354 Eisenhower Pkwy Ste 1150, Livingston, NJ 07039 11. Known Bondholders, Mortgagees, and Other Security Holders Owning or Hoding 1 Percent or More of Total Amount of Bonds. Mortgages, or Other Securities. If none, check box X None Full Name Complete Mailing Address PS Form 3526-R September 2007 (Page 1) PRIVACY NOTICE: See our privacy policy on www.usps.com 13. Publication Title 14. Issue Date for Circulation Data Below NEW JERSEY PSYCHOLOGICAL ASSOCIATION/NEW JERSEY PSYCHOLOGIST 09/10/2019 15. Extend and Nature of Circulation Average No. Copies Each Issue During Preceding 12 Months No. Copies of Single Issue Published Nearest to Filing Date a. Total Numbers of Copies (Net press run) 1650 1650 b. Legitimate Paid and/or Requested Distribution (By Mail and Outside the Mail) (1) Outside County Paid/Requested Mail Subscriptions stated on PS Form 3541. (Include direct written request from recipient, telemarketing and Internet requests from recipient, paid subscriptions including nominal rate subscriptions, employer requests, advertiser's proof copies, and exchange copies.) (2) In-County Paid/Requested Mail Subscriptions stated on PS Form 3541. (Include direct written request from recipient, telemarketing and Internet requests from recipient, paid subscriptions including nominal rate subscriptions, employer requests, advertiser's proof copies, and exchange copies.) (3) Sales through Dealers and Carriers, Street Vendors, Counter Sales, and Other Paid or Requested Distribution Outside USPS (4) Requested Copies Distributed by Other Mail Classes Through the USPS (e.g. First-Class Mail) 1630 1630 0 0 0 0 0 0 c. Total Paid and/or Requested Circulation (Sum of 15b (1), (2), (3), (4)) 1630 1630 d. Nonrequested Distribution (By Mail and Outside the Mail) (1) Outside County Nonrequested Copies stated on PS Form 3541 (include Sample copies, Requests Over 3 years old, Requests induced by a Premium, Bulk Sales and Requests including Association Requests, Names obtained from Business Directories, Lists, and other soruces) (2) In-County Nonrequested Copies stated on PS Form 3541 (include Sample copies, Requests Over 3 years old, Requests induced by a Premium, Bulk Sales and Requests including Association Requests, Names obtained from Business Directories, Lists, and other soruces) (3) Nonrequested Copies Distributed Through the USPS by Other Classes of Mail (e.g. First-Class Mail, Nonrequestor Copies mailed in excess of 10% Limit (4) Nonrequested Copies Distributed Outside the Mail (include Pickup Stands, Trade Shows, Showrooms and Other Sources) 0 0 0 0 0 0 0 0 Total Nonrequested Distribution (Sum of 15d (1), (2), (3), (4)) f. Total Distribution (Sum of 15c and 15e) g. Copies not Distributed h. Total (Sum of 15f and 15g) i. Percent Paid and/or Requested Circulation ((15c 15f) times 100) 0 0 1630 1630 20 20 1650 1650 100.00 % 100.00 % 16. If total circulation includes electronic copies, report that circulation on lines below. a. Requested and Paid Electronic Copies(Sum of 15c and 15e) b. Total Requested and Paid Print Copies(Line 15c) + Requested/Paid Electronic Copies c. Total Requested Copy Distribution(Line 15f)+ Requested/Paid Electronic Copies d. Percent Paid and/or Requested Circulation (Both print and Electronic Copies) 0 0 0 0 0 0 0.00 % 0.00 % Certify that 50% of all my distributed copies (Electronic & Print) are legitimate requests. 17. Publication of Statement of Ownership for a Requester Publication is required and will be printed in the 09/10/2019 issue of this publication. 18. Signature and Title of Editor, Publisher, Business Manager, or Owner Title Date Keira Boertzel-Smith Executive Director 10/18/2019 14:47:01 PM certify that all information furnished on this form is true and complete. understand that anyone who furnishes false or misleading information on this form or who omits material or information requested on the form may be subject to criminal sanctions (including fines and imprisonment) and/or civil sanctions (including civil penalties). PS Form 3526-R September 2007 (Page 2) PRIVACY NOTICE: See our privacy policy on www.usps.com
MEMBER NEWS
OF
Judith Glassgold, PsyD

What is scope of practice?
Scope of practice defines the professional actions and treatments that a healthcare practitioner is permitted to perform under their professional license. The scope of practice is determined by the education, experience, and competencies associated with the profession. Each state jurisdiction has its own unique scope of practice for each profession.
Psychology’s scope of practice can be found here <https://www.njconsumeraffairs.gov/regulations/Chapter-42-Boardof-Psychological-Examiners.pdf> and at the end of this article.
Scope of practice defines the full range of possible interventions and treatments. Not all psychologists may have expertise in these areas (i.e., forensic psychology, developmental disabilities) and psychologists should practice only in areas where they can demonstrate competence. Further, there may be some areas where psychologists, due to specialized education and training, may be competent, but these areas are outside the scope of the practice in that particular state (i.e., psychopharmacology).
Why is Scope of Practice Important?
1. Ensuring scope of practice fits current breadth and depth of psychology training
As psychology advances and new techniques have been developed, psychological education and training have evolved and grown. The scope of practice should reflect these new areas and offer opportunities to practice all the potential interventions and techniques.
2. Ensuring scope of practice is relevant to modern settings
Scope of Practice
Scope of practice needs to be updated to ensure that psychologists can use their skills in all relevant settings, such as in integrated care (healthcare settings) and organizations (business, sports teams and organizations). Terms that describe certain principles may also evolve, and our scope of practice should reflect updated professional language.
3. Monitoring interaction with other professions’ scopes of practice
As new professions seek licensure, they may seek to define their own scope of practice. Sometimes these areas may overlap with ours or be subsets of principles developed by psychologists. Legislation defining other professionals should be scrutinized carefully to assess its impact on our profession. Clarifying the boundaries of their practices, and ensuring the wording of our scope of practice reflects new terminology is essential. While other professionals may have interventions and techniques such as psychotherapy or behavioral interventions in common with psychologists does not mean that the entire scope of practice is similar.
• Practice outside scope of practice. Psychologists should take care to practice within the scope of their current license. Additionally, these issues may become cross-profession concerns. Given the overlap across professionals in some activities (i.e., counseling), scope of practice issues can become confusing. Some professionals may not be aware of psychology’s scope of practice, or their own, and may provide services outside their scope of practice. In addition, some professionals may seek out additional training in areas such as testing that are part of psychology’s scope of practice; however, that does not mean that this activity is permitted under their scope of practice and professional license. Individuals who practice outside their scope of
practice and provide psychological services without a psychology license should be reported to the Board.
4.
Advocacy and Compliance
Psychology needs to pay attention to ongoing trends in legal and regulatory issues across the healthcare professions. Psychologists should remain alert to the scope of practice of other professionals, as well as proposed licensing acts. As a professional, we must ensure that our ability to practice to the full extent of our training is not impeded by other professionals or our own licensing act.
New Directions
Recently, the American Psychological Association updated its model licensing act that includes a scope of practice. This model act clearly delineates procedures psychologists are able to perform such as supervision and applied behavioral analysis. It also more explicitly addresses healthcare settings and organizations. It also creates new terms to define specialty practices such as applied psychology and health service provider.
“Practice of psychology” is defined as the observation, description, evaluation, interpretation, and modification of human behavior by the application of psychological principles, methods, and procedures, for the purposes of (a) preventing, eliminating, evaluating, assessing, or predicting symptomatic, maladaptive, or undesired behavior; (b) evaluating, assessing, and/or facilitating the enhancement of individual, group, and/or organizational effectiveness –including personal effectiveness, adaptive behavior, interpersonal relationships, work and life adjustment, health, and individual, group, and/or organizational performance, or (c) assisting in legal decision-making.
The practice of psychology includes, but is not limited to, (a) psychological testing and the evaluation or assessment of personal characteristics, such as intelligence; personality; cognitive, physical,
New Jersey Psychologist 14
DIRECTOR
PROFESSIONAL
AFFAIRS
and/or emotional abilities; skills; interests; aptitudes; and neuropsychological functioning; (b) counseling, psychoanalysis, psychotherapy, hypnosis, biofeedback, and behavior analysis and therapy; (c) diagnosis, treatment, and management of mental and emotional disorder or disability, substance use disorders, disorders of habit or conduct, as well as of the psychological aspects of physical illness, accident, injury, or disability; (d) psychoeducational evaluation, therapy, and remediation; (e) consultation with physicians, other health care professionals, and patients regarding all available treatment options, including medication, with respect to provision of care for a specific patient or client; (f) provision of direct services to individuals and/or groups for the purpose of enhancing individual and thereby organizational effectiveness, using psychological principles, methods, and/or procedures to assess and evaluate individuals on personal characteristics for individual development and/or behavior change or for making decisions about the individual, such as selection; and (g) the supervision of any of the above. The practice of psychology shall be construed within the meaning of this definition without regard to whether payment is received for services rendered.
5. “Applied psychologist” is one who provides services to individuals, groups, and/or organizations. Within this broad category there are two major groupings – those who provide health-related services to individuals and those who provide other services to individuals and/or services to organizations. Although licensure is generic, some of the Board’s Rules and Regulations need to account for variations in relevant training, supervision, and practice.
a. “Health service provider” (HSP) Psychologists are certified as health service providers if they are duly trained and experienced in the delivery of preventive, assessment, diagnostic, therapeutic intervention and management services relative to the psychological and physical health of consumers based on: 1) having completed scientific and professional training resulting in a doctoral degree in psychology; 2) having completed an internship and supervised experience in health care
settings; and 3) having been licensed as psychologists at the independent practice level.
b. “General applied psychologist” General applied psychologists provide psychological services outside of the health and mental health field and shall include: 1) the provision of direct services to individuals and groups, using psychological principles, methods, and/or procedures to assess and evaluate individuals on personal abilities and characteristics for individual development, behavior change, and/or for making decisions (e.g., selection, individual development, promotion, reassignment) about the individual, all for the purpose of enhancing individual and/or organizational effectiveness; and 2) the provision of services to organizations that are provided for the benefit of the organization and do not involve direct services to individuals, such as job analysis, attitude/opinion surveys, selection testing (group administration of standardized tests in which responses are mechanically scored and interpreted), selection validation studies, designing performance appraisal systems, training, organization design, advising management on human behavior in organizations, organizational assessment, diagnosis and intervention of organizational problems, and related services.
Compare this to our current scope of practice:
“13:42-1.1 SCOPE OF PRACTICE
a) The scope of practice of a licensed psychologist includes, but is not limited to, the use or advertisement of the use of theories, principles, procedures, techniques or devices of psychology, whether or not for a fee or other recompense. Psychological services include, but are not limited to:
1) Psychological assessment of a person or group including, but not limited to: administration or interpretation of psychological tests and devices for the purpose of educational placement, job placement, job suitability, personality evaluation, intelligence, psychodiagnosis, treatment planning and disposition; career and vocational planning and development; personal development; management development; institutional
placements; and assessments in connection with legal proceedings and the actions of governmental agencies including, but not limited to, cases involving education, divorce, child custody, disability issues and criminal matters;
2) Psychological intervention or consultation in the form of verbal, behavioral or written interaction to promote optimal development or growth or to ameliorate personality disturbances or maladjustments of an individual or group. Psychological intervention includes, but is not limited to, individual, couples, group and family psychotherapy, and psychological consultation includes consultation to or for private individuals, groups and organizations and to or for governmental agencies, police and any level of the judicial system;
3) Use of psychological principles, which are operating assumptions derived from the theories of psychology that include, but are not limited to: personality, motivation, learning and behavior systems, psychophysiological psychology including biofeedback, neuropsychology, cognitive psychology and psychological measurement; and
4) Use of psychological procedures, which are applications employing the principles of psychology and associated techniques, instruments and devices. These procedures include, but are not limited to, psychological interviews, counseling, psychotherapy, hypnotherapy, biofeedback, and psychological assessments.”
Question
What changes would you make to our current licensing act? What are your thoughts to APA’s model licensing act? Please send your feedback to our Director of Professional Affairs, Judith Glassgold, PsyD, njpadpa@psychologynj.org.
Conclusion
As the field of psychology advances, New Jersey psychologists have to ensure that our scope of practice stays abreast of new developments and trends in psychology, the marketplace, and other professions. This will ensure that our state licenses allow us to provide all the interventions and services that we are trained to provide. This will ensure that there is adequate access to services for patients well as employment opportunities for psychologists. ❖
Fall 2019 15
Announcing the Eight 2019-2020 NJPA Foundation Community Service Project Grants
by the NJPA Foundation Board of Trustees
President, Matt Hagovsky, PhD; Secretary, Toby Kaufman, PhD; Treasurer, Abby Rosen; Board Trustee, Regina Budesa, PsyD; Board Trustee, Richard Klein, EdD; Board Trustee, Ann Stainton, PhD; Board Trustee, Alyssa Austern, PsyD; Board Trustee, Belvin Williams, PhD; Board Trustee, Eileen Kohutis, PhD; NJPA President-Elect, Lucy Sant’Anna Takagi, PsyD; Executive Director, Keira Boertzel-Smith, JD
Each year, The NJPA Foundation identifies exemplary programs that provide psychological services to those who cannot afford it and trains doctoral students to work with these underserved populations. We invite applications from programs across the state of New Jersey, with the goal of identifying and supporting model programs from each county. Visit <www. psychologynj.org/njpa-foundation> to read more and make a donation to help us continue this important philanthropic work! We strongly encourage use of the 2020 dues bill for donations to the NJPA Foundation.
Trinitas Regional Medical Center
Trinitas Child Outpatient and Adolescent DBT Externship
Site Director - Atara Hiller, PsyD
NJPAF Funded StudentMadison Perry
Medical Center offers a full array of psychiatric and behavioral health services for children and adolescents and their family members. The students are exposed to a range of clinical experiences at the COPU, including conducting intake evaluations; providing individual cognitive-behavioral and family therapy to children, adolescents, and families with anxiety, mood, and disruptive behavior disorders; and engaging in case management with schools, psychiatric providers, and outside case managers. Students are trained in providing Dialectical Behavior Therapy (DBT) to adolescents and their families, who exhibit symptoms of borderline personality disorder and comorbid conditions.

Regional Diagnostic & Treatment Center- General Track Externship @ Newark Beth Israel Medical Center
Site Director - Karyn C. Smarz, PhD
plication will be providing treatment and assessment services for an at-risk, underserved trauma population, as part of the general externship track at the Metropolitan Regional Diagnostic and Treatment Center at Newark Beth Israel Medical Center. The Metro RDTC is one of New Jersey’s four state-designated multidisciplinary centers for the evaluation and treatment of abused and neglected children. The Center primarily serves the culturally and socioeconomically diverse children and families who reside in Essex County.
Youth Anxiety and Depression Clinic, Graduate School of Applied and Professional Psychology, Rutgers University
Site Director - Brian Chu, PhD
NJPAF Funded Students - Hillary (Gemma) Stern and Melissa Pedroza
The Child and Adolescent Outpatient Unit (COPU) at Trinitas Regional
NJPAF Funded StudentsShaneze Gayle, Megan Ingraham, Jessica Elliott, Jessica Bonumwezi

The doctoral students in this ap-
The Youth Anxiety and Depression Clinic (YAD-C) is an open specialty clinic that provides diagnostic assessment and behavioral therapies for youth with anxiety and mood problems. Youth and parents are referred from a diverse set of community sources. The served families represent a diverse range of SES and ethnic/cultural backgrounds. The clinic actively participates in community

New Jersey Psychologist 16
FOUNDATION
Top row (L to R): Madison Perry, PsyM; Melanie Andrade, LCSW; Atara Hiller, PsyD; Catharina Carvalho, PhD; E. Parham Horn, MA; Talia Clements, MA. Bottom row (L to R): Tamaki, Hosoda, MA; Shana Jones, LSW; Jiwon Yoo, MA
From (L to R): Shanzez Gayle, Jessica Elliot, Jessica Bonuwezji and Megan Ingraham
outreach activities, including conducting parent and teacher workshops at schools, attending town/school-based community fairs, and engaging in community partnerships for specific underserved populations. The clinic conducts formal diagnostic assessments, collects surveys, and assesses family interaction patterns to help us know which kinds of therapy help most.
Rutgers University, Graduate School of Applied & Professional Psychology, Foster Care Counseling Project
Site Director - Djenaba Figueroa
NJPAF Funded Students - Mir (Kamran) Meyer, Laura Betheil, Madeline Bono, Alejandra Feliz
All FCCP student clinicians provide individual, family, and dyadic therapy to youth, ranging in age from 3 to 18 years old, with significant histories of trauma. Biological parents, adoptive parents, and resource parents are involved in each child’s therapy, whenever possible, to maximize the success of treatment. FCCP attempts to overcome treatment barriers by providing inhome parent management training and family sessions when treatment barriers prevent the client’s family from attending sessions at the clinic. Additionally, FCCP provides mentors to clients to increase the opportunity for positive peer interactions. FCCP will be offering a group for adolescents involved in resource care and children with sexual abuse histories. While providing treatment, student clinicians offer training and consultation to caregivers, Division of Child Protection & Permanency (DCP&P) caseworkers, community organizations, school personnel, and other professions. They also complete
thorough intakes and post-treatment assessments at the beginning and end of treatment, respectively, and make recommendations based on findings to optimize each child’s functioning.
Newark Beth Israel Medical Center, Metropolitan Regional Diagnostic and Treatment Center (Metro RDTC) - GBCBT RDTC externship at Newark Beth Israel Medical Center
Site Director - Barbara A. Prempeh, PsyD
NJPAF Funded Students - Yael Osman, Molly Kammen, DeVante Cunningham, Matt Stahl

The doctoral students in this application will be providing treatment and assessment services for an at-risk, underserved trauma population. The Metro RDTC is one of four RDTCs in New Jersey committed to providing medical and psychological evaluations and care for survivors of child abuse and neglect. It is housed in a Child Advocacy Center that bears the distinction of being the first and only fully co-located Child Advocacy Center in New Jersey with all partners onsite. Providing services in this multidisciplinary setting allows for an integrated and coordinated response to abuse and neglect for a community in-need of significant services. Families served at the RDTC are predominantly from economically disadvantaged, urban communities.

Rutgers University, Graduate School of Applied and Professional Psychology, Tourette Syndrome Clinic
Site Director - Graham Hartke, PsyD NJPAF Funded Students - Hyein Lee,
The Tourette Syndrome Clinic was developed in partnership between Rutgers’ Graduate School of Applied and Professional Psychology (GSAPP) and the NJ Center for Tourette Syndrome (NJCTS). The Rutgers-NJCTS Therapeutic program is offered through the Psychological Services Clinic at GSAPP that provides a variety of psychological services to the public. The RutgersNJCTS Tourette Syndrome Program offers individual and family therapy for individuals affected by TS, emphasizing evidence-based treatments for TS and related conditions. All therapists are trained in Comprehensive Behavioral Intervention for Tics (CBIT that includes Habit Reversal Training (HRT), as well as cognitive behavioral approaches for common comorbid conditions such as ADHD, OCD, ASD, and anxiety and mood disorders. Individual and family therapy may also include supportive, psychoeducational, and skill-building interventions. In addition to individual and family therapy, the clinic offers socioemotional skills groups for school-aged children and teens. Finally, the RutgersNJCTS Tourette Syndrome Program also offers a variety of additional supportive services including diagnostic evaluation, consultation on TS and associated disorders for practitioners, physicians, educators and students, assistance with referrals for physicians, and access to additional resources and services for the TS community.

Fall 2019 17
Rebecca Khiralla, Elana Fox, Norna Jules, and Emily Hendershot
(L to R): Brian Chu (director), Melissa Pedroza (student therapist), Gemma Stern (student therapist)
(L to R) Emily Hendershot, Elana Fox, Rebecca Khiralla, Norna Jules, Dr. Graham Hartke, Psy.D., Hyein Lee
GB-CBT externs at the RDTC (L to R): Matt Stahl, Yael Osman, Molly Kammen, and DeVante Cunningham
Rutgers University, Graduate School of Applied and Professional Psychology Rutgers GSAPP- Anxiety Disorders Clinic

Site Director - Andrea Quinn, PsyD NJPAF Funded Students - Joel Seltzer, Idil Franko
The Anxiety Disorders Clinic (ADC) offers low cost, evidence-based, cognitive behavioral therapy for anxiety and related disorders to both Rutgers University students and the surround community. The ADC serves a broad age range of clients, including school-aged children and adolescents, to older adults. The ADC offers Exposure with Response Prevention (Ex/ RP), an empirically supported treatment for Obsessive Compulsive Disorder that is challenging to find in the community, particularly at a cost that is feasible for families. As a result, the ADC often has
a lengthy waitlist of clients with OCD and anxiety disorders that also benefit from treatment utilizing exposure therapy.
Cognitive therapy and acceptance-based models are also utilized. In addition, the ADC offers no cost, evidence-based group and individual treatment to Veterans, providing not only a much needed service to the community, but also a highly desirable training opportunity for graduate students who hope to work with active duty and veteran populations during their internship year and/or their future careers. The ADC offers treatment for Posttraumatic Stress Disorder using Cognitive Processing Therapy and in addition, treatments are available for additional presenting challenges to both Veterans and their family members. ❖
Please donate to the NJPA Foundation!
Join Us for the 2019 NJPA Trenton Day
December 5, 2019 10:00am – 3:00pm
On Thursday, December 5, 2019, NJPA will hold a 2019 Trenton Day. NJP-PAC will be funding the day with the purpose of providing NJPA and affiliate members an opportunity to delve in to the NJ legislative process, understand how a bill becomes a law, and learn the importance of grassroots advocacy. We will hear from legislators and staff about the process in which legislation is introduced and passed. We’ll share ideas on ways that psychologists and psychologists-in-training can influence the formation of public policies, will plan to sit in for a few minutes at a public hearing, and learn some of the history of state government and its buildings. Lunch will be provided. Meeting location, directions, and parking instructions to follow. All are encouraged to join us!

If you are available to attend, please RSVP here by November 15, 2019.
<https://www.surveymonkey.com/r/9PPRTLG>
How much is it worth to you to sustain your professional future? Demonstrate what being a professional psychologist means to you by donating to NJP-PAC. If you have never given before, donate this year. If you previously donated, give more this year! Your dollars are your voice. To make a donation, go to <https://www.psychologynj.org/support-njp-pac> Monthly pledge plans are available – call NJPA Central Office to learn more!
NJP-PAC is a non-profit political action committee which makes contributions, from funds received from NJP-PAC contributors, to candidates for office and political committees in New Jersey who have demonstrated their interest in and support of psychology, without regard to party affiliation. These funds are distributed in such a manner as to advance the stature of the profession of psychology in New Jersey.
New Jersey Psychologist 18
(Front Row L to R) Dr. Andrea Quinn, Sydney Brinson, Katherine El-Sharkawy, Molly Stern, Joel Seltzer. (Back Row, L to R) Benjamin Billingsley, Megan Giles, Idil Franko, Liza Franklin, Samuel Nayman. Not Pictured- Mark Versella.
New Jersey Department of Human Services Response to the Opioid Crisis
CE Credits Maria P. Kirchner, PhD
Robert Eilers, MD, MPH

According to a National Safety Council report, Americans are now more likely to die from accidental opioid overdoses than car crashes (NSC, 2019). In 2017, which is the last year in which overdose death data is confirmed, 70,237 drug overdose deaths occurred in the US. For every drug overdose that results in death, there are many more nonfatal overdoses, each one with its own emotional and economic toll, disrupting lives and communities. This fast-moving epidemic does not distinguish among age, sex, race, or state or county lines.
Abstract:
As in the rest of the United States, the opioid crisis has become a major public health problem throughout New Jersey. Opioid-related deaths from the use of prescription opioids, heroin, and illicit fentanyl and fentanyl analogs have increased at unprecedented rates. Through the perspective of one of the state agencies tasked with addressing the problem, the New Jersey Department of Human Services, we describe how the state has responded to this challenge. Supported by targeted State investments from New Jersey Governor Philip Murphy’s opioid initiative and federal funding, and with changes in law and policy, the state developed an array of prevention, treatment, and recovery support services for those with opioid use disorder (OUD). Key objectives of these initiatives included expanding access to medication assisted treatment (MAT), reducing unmet treatment need, preventing deaths from opioid overdoses, and supporting individuals in recovery. The critical role of psychology is highlighted, as these clinicians provide evidence-based counseling and behavioral therapies for OUD that are an important part of MAT and complement recovery support services.
Introduction
The United States is facing increases in opioid use disorders (OUDs) and overdose deaths that have reached unprecedented levels (CDC; WISQUARS).
Although the focus of this article gives an overview of the actions of the Department of Human Services (DHS) that is home to both the Division of Mental Health and Addiction Services (DMHAS) and Division of Medical Assistance and Health Services (DMAHS; also known as Medicaid), DHS has worked in close partnership with other state agencies, especially the Department of Health (DOH), Department of Children and Families (DCF), Department of Corrections (DOC), and the Office of the Attorney General (OAG). These agencies have been tasked by Governor Philip Murphy to take a whole-of-government approach in combatting the opioid crisis in NJ.
The initiatives described below are not exhaustive, nor do they minimize the efforts of numerous public and private entities in NJ. This crisis has, and will continue to, demand a comprehensive and collaborative array of initiatives from both public and private entities.
The strategies that the state used to address the opioid crisis include changes in laws, policies, licensing, insurance coverage, program developments, direct funding of services, data collection, and professional and public education. Psychologists significantly contribute to effective addiction treatments by utilizing evidence-based modalities and will continue to lend their expertise and provide direct services in the future.

Overview of the Opioid Crisis
Overdose deaths in the US have been increasing for three decades, with annual
totals of drug-related deaths doubling over the last decade (CDC, 2019). According to Centers for Disease Control and Prevention, National Center for Health Statistics, Americans’ life expectancy dropped for the very first time since World War I for three consecutive years, due, in part, to the country’s surge in drug overdose deaths and climbing suicide rates. The overprescribing and misuse of synthetic opioid pain medications have been considered the primary drivers for the dramatic increase in opioid deaths in the last few years. Although synthetic opioids are manufactured by pharmaceutical companies, they are also manufactured illegally in clandestine labs and distributed through the illicit drug market; the prime example is fentanyl that is a synthetic opioid considered 50-100 times more potent than morphine and has surpassed heroin as the opioid most often responsible for overdose deaths in the US (CDC, 2019). Use of heroin has also been increasing in recent years as prescription drugs have become more difficult to obtain and heroin is less expensive and more widely available. Some of the greatest upsurges in heroin use have occurred in demographic groups with historically low rates of heroin use: women, the privately insured, and people with higher incomes (CDC, 2019).
Drug-related deaths in NJ have been increasing every year for more than the past decade. While the total number of overdose deaths was 843 in 2010 and 1,587 in 2015, this number jumped to 2,529 in 2016 and 2,685 in 2017, approaching eight overdose deaths per day on average. The number of deaths in 2017 represents an increase of approximately 24% over the 2016 death toll (approximately 6 per day). The 2018 data on overdose deaths (unconfirmed) is 3,118 (NJCARES). Heroin is the drug most often implicated in drug-related deaths in NJ, probably because highly pure heroin can be obtained relatively cheaply. Nevertheless, fentanyl deaths in NJ have also shown a major rise. While 417 deaths were classified as fentanyl-related in 2015, this number increased in only two years to 1,429. None of the increases in other
Fall 2019 19
SPECIAL SECTION
2
substances, heroin, morphine, cocaine, oxycodone or methadone reached such a disproportionate high. The data confirm that opioid use has become a pervasive problem throughout NJ and is not limited by race, ethnicity, or socio-economic group.
New Jersey’s Initial Response to the Opioid Crisis
At a press conference in Camden, in January 2019, Governor Philip Murphy publicly pledged that he was committed to increasing access to evidence-based prevention and treatment programs; supporting recovery; building sound data systems and strong system-wide infrastructure; and enforcing laws to stop the supply of illicit drugs and support diversion initiatives. The governor’s commitment was evidenced by his proposing and securing $100 million in new State funding to combat the opioid epidemic in 2018 and continuing this funding in 2019.
The governor also called for a datadriven and person-centered response to the opioid crisis, with a whole-of-government response focused on increasing access to what works, including naloxone (otherwise known as Narcan) to prevent opioid overdose deaths and medicationassisted treatment (MAT) for individuals with substance use disorders.
In June of 2019, Governor Murphy announced free distribution of naloxone, the opioid overdose reversal drug, at participating pharmacies throughout NJ in what is believed to be the largest single day distribution of naloxone in the country, a total of 16,000 naloxone kits, or 32,000 doses, were distributed for free, with no prescription or identification required, by participating pharmacies in the state.
Also, in 2019, the governor announced that Medicaid lifted prior authorization requirements for medicationassisted treatment, new reimbursement incentives for providers to offer MAT, new investments in training healthcare providers on opioid use disorder treatment, and new clinical supports to help healthcare providers manage patients with substance use disorder.
The governor’s initiative is also investing in recovery supports through employment training and supportive housing for those impacted by opioid use.
Preventing Opioid Overdose and DrugRelated Deaths
The State’s earliest actions tried to stem the rising numbers of opioid overdose deaths. Police, Emergency Medical Technicians, and other first responders around the state started to carry and, in many cases, utilize naloxone to reverse opioid overdoses and prevent deaths. Nevertheless, few individuals at the side of an overdose victim had carried naloxone or knew how to respond to an overdose emergency. In May 2013, NJ enacted the “Opioid Antidote and Overdose Prevention Act,” allowing physicians to prescribe naloxone to anyone in a position to assist others during an overdose. The Act also provides both civil and criminal immunity and from any professional discipline for health care professionals and other persons involved in prescribing, dispensing, or administering naloxone. More significantly, immunity from arrest, prosecution, or conviction for drug offenses is also in effect when any person, in good faith, seeks medical assistance for the victim of an overdose. Finally, the Act authorized the DHS to develop a bystander training program that includes the use of naloxone in overdose emergencies.
Subsequently, DMHAS, in collaboration with the Governor’s Council on Alcoholism and Drug Abuse (GCADA), awarded funding to three organizations to establish regional Opioid Overdose Prevention Programs (OOPPs) that provide at-risk individuals and others with naloxone rescue kits and educate and train them on how to prevent, recognize, and respond to an opioid overdose. In addition to targeting individuals with an Opioid Use Disorder (OUD), their families, friends, and associates, the programs provided training and kits to medical service teams, HIV programs and other community-based public health organizations, fire departments, homeless shelters, community health clinics, personnel at statewide school districts, medical and clinical staff at jails, and residential drug treatment programs.
Another early State initiative, the Opioid Overdose Recovery Program (OORP), sent trained peers to emergency rooms to engage individuals who had just been reversed with naloxone with the goal of encouraging treatment. The peers (primarily individuals in recovery)
and patient navigators (a newly created position, described below), provide nonclinical assistance, recovery support, and appropriate referrals for assessment and substance use disorder (SUD) treatment while also maintaining follow-up with these individuals. When an individual has been reversed from an overdose, recovery specialists are notified and deployed to the emergency room within one hour. OORP workers follow-up with these individuals for at least eight weeks. In most instances, services are provided 24 hours a day by OORP workers. Recovery specialists are accessible and on-call in the specific locations where services are provided. The OORP program is in 54 of 78 Emergency Departments (EDs) and in all 21 counties. Internal reports from these counties suggest the proportion of individuals, who are linked to services following an overdose, have increased significantly after OORP was launched.
In September 2016, DMHAS was awarded a grant from the Substance Abuse and Mental Health Services Administration (SAMHSA), Center for Substance Abuse Prevention, to implement the Opioid Overdose Prevention Network (OOPN) initiative. This data-driven public health collaboration with universities and other state agencies targeted highneed communities that are identified as “Prevention Pathways.” Prevention Pathways uses evidence-informed, substance abuse mitigation strategies that utilize a comprehensive approach designed to prevent, reduce, and eliminate drug abuse and misuse in NJ. A critical partner is the NJ State Police Regional Operations & Intelligence Center (ROIC) is a state-ofthe-art facility that collects data on crime, illicit drug retrievals, and overdoses. It combines data from several sources, such as state, public, and behavioral health and the drug monitoring initiatives, on hospital encounters, naloxone deployments, and drug-involved arrests and deaths, and then aggregates, analyzes, and maps the data to target treatment and prevention services.
Restricting the Prescribing of Opioids
Another early action was the February 2017 passage of a new law that limited the prescribing of opioids to prevent misuse and development of opioid dependency. The law was hailed by some as the toughest opioid prescription law in the nation.
New Jersey Psychologist 20
In addition to limiting the initial prescription of opioids in the treatment of acute pain to a five-day supply, the law requires that prescribers consider non-opioid alternatives for pain, warn patients about the potential of addiction, and make the goal to stop opioids short-term. Prescribers need to use the lowest effective opioid dose and to stop subsequently opioids for acute pain. If patients require chronic opioid use, the law mandates that prescribers create a pain-management treatment plan and a documentation of a discussion of risks with patients.
Another requirement was signing up for the state’s Prescription Monitoring Program (PMP) that gave prescribers critical information about their patients’ misuse of prescribed medications. The effects of the law are difficult to evaluate, but the widespread publication of the perils of opioids and the potential penalties that physicians faced for inappropriate prescribing, along with the increased training of physicians, seemed to have an effect; the state began to see a gradual trend toward lower rates of opioid prescriptions in subsequent years.
In September 2016, NJAssessRx initiative was implemented, allowing interagency sharing of the state’s PDMP data and the capability of using data analytics to identify prescribers, prescriber groups, and patients at high risk for inappropriate prescribing and nonmedical use of opioid drugs. Informed by the data, communities and populations were strategically targeted for services or education. The focus was on youth (ages 12-17) and adults (18 years of age and older), who are being prescribed opioid pain medications, controlled drugs, or Human Growth Hormone, and are at risk for their nonmedical use.
Funding for New NJ DHS Opioid Initiatives
State and federal governments recognized that a major increase in funding was necessary to address what was broadly recognized as a national crisis. The Comprehensive Addiction and Recovery Act, known as CARA, signed by President Obama on July 22, 2016, became the first major federal addiction initiative that had been passed in four decades and provided $181 million mostly for harm reduction and prevention services. The passage of the 21st Century Cures Act followed, and
it provided $1 billion for treatment to address the opioid crisis. In May 2017, the Cures Act provided NJ with almost $13 million annually for two years to fund new initiatives. In December 2017, the state received additional federal funding of $5 million for pregnant women, new mothers, and their babies. The State Targeted Opioid Response Initiative (STORI), as the Cures Act funding initiative is called, is primarily administered by DMHAS and is designed to provide service for at-risk individuals with OUD, including veterans, individuals released from incarceration in the last 60 days, and young and older adults. The STORI initiative encompasses a wide range of programs and services, including prevention, treatment, recovery support, and training. The primary treatment component is the development of a fee-for-service initiative providing assessment, outpatient, intensive outpatient, short-term residential, and medication assisted treatment services (MAT).
The STORI was followed by another major congressional funding called the State Opioid Response (SOR) Grant that was awarded in 2018. This federal grant of $21.5 million annually has allowed NJ to continue and to significantly expand its actions. The key objectives of the SOR grant are to increase access to MAT, reduce unmet treatment need, and reduce opioid overdose-related deaths through the provision of prevention, treatment, and recovery activities for OUD, including the abuse of prescription opioids, heroin, and illicit fentanyl and fentanyl analogs. In March 2019, DMHAS received notification of an additional $11.2 million in available funding through the SOR grant, bringing the total federal funding that the state has received since December 2017 to $50.7 million.
Expansion of Treatment for Opioid Use Disorder
In 2018, Governor Murphy proposed and secured a new $100 million investment of state funding to combat the opioid epidemic. The Department of Human Services, the Department of Health, the Department of Children and Families, the Department of Corrections, the Department of Labor, the Department of Community Affairs, and the Office of the Attorney General comprise an
interagency group working collaboratively to implement this funding.
Prior to the passage of the Affordable Care Act, SUD treatment and support services generally had limited coverage by private insurance plans and Medicaid coverage did not extend to many lower income individuals. However, after the passage of the Affordable Care Act (ACA) in 2010, benefits for addiction treatment began increasing in the individual insurance market, in addition, Medicaid expansion increased health care coverage for individuals with incomes up to 138% of the federal poverty level. The ACA required insurers to provide SUD treatment services as part of an “Essential Health Benefits” package. Together, these actions significantly expanded access to SUD services.
To ensure that individuals know how to access services, NJ operates a 24-hoursa-day, 7-days-a-week addictions hotline (1-844-ReachNJ or 844-732-2465) where people who have SUD or their loved ones can get immediate help and referrals from live, NJ-based, trained addiction counselors, regardless of their insurance status. The center enlists trained counselors who receive calls, authorize treatment services, and then make a “warm handoff” to treatment providers, ensuring that follow up linkages are made.
New Jersey also has a waiver from federal regulations allowing for Medicaid coverage of residential treatment despite the federal limits on payment for Institutions for Mental Disease (IMD). The waiver has allowed NJ Medicaid to expand coverage for residential drug and alcohol treatment. Initially, Medicaid in NJ provided coverage for withdrawal management and short-term residential services, but it also began to cover long-term residential services. Residential services are critical for those with the most severe OUD, especially for those whose conditions are complicated by a co-occurring physical or mental health condition.
Promoting an Evidence-Based Treatment Model
According to the definition endorsed by the Substance Abuse and Mental Health Administration (SAMHSA), MAT refers to the use of medications (e.g., methadone, buprenorphine, and naltrexone), accompanied by ongoing counseling
Fall 2019 21
and cognitive-behavioral therapies. When compared with a traditional abstinence approach, outcomes for MAT in combination with therapy, show greater decreases in use of illicit drugs, better functioning of the individual, reductions in criminal activity and drug-related infectious disease, as well as increases in survival overall. MAT is consistent with the new conceptualization of OUD that is based on a chronic disease model (White, Boyle, Loveland, & Corrington, 2005).
A 2019 expert committee report (Medications for Opioid Use Disorder Saves Lives) found that a majority of individuals who suffer from SUD do not receive any treatment and that only a fraction of this population receives medications for OUD. The report stresses that MAT is essential for some to sustain their recovery, and for many this treatment needs to be long-term <https://www. integration.samhsa.gov/clinical-practice/ mat/mat-overview>. Since a combination of psychopharmacological and therapeutic modalities yields the best outcomes for treating OUD, health care practitioners who offer these kinds of evidence-based therapies can have an important impact in reducing opioid use. In addition, for those individuals who initially began taking opioids for pain, medical marijuana, and CBT for chronic pain can also provide alternative pain management strategies to decrease opioid use.
Unfortunately, there are a few factors that affect proper access to medications for OUD. Methadone as a form of MAT has been available for several decades and shown to be a very effective treatment for OUD. However, it is only dispensed by federally regulated methadone clinics that require almost daily attendance and these clinics are not in every community. Another barrier is the stigma associated with SUD services, especially with taking methadone. Since the two other drugs that are recognized within MAT, buprenorphine and naltrexone, can be given as prescriptions in a physician’s office, treatment there is less stigmatizing. However, federal laws require special training and certification (DATA 2000 Waiver) in order for physicians and other practitioners to prescribe buprenorphine that limits the numbers of prescribers available. Because buprenorphine can be prescribed in physicians’ offices and other outpatient
settings, training more prescribers to increase access to this medication is one of the major goals of NJ’s OUD treatment. In addition, relatively few office-based psychiatrists or addiction medicine physicians accept Medicaid, requiring the Medicaid beneficiaries and non-insured people to pay for services out of pocket, which is a hardship. Medicaid had required prior authorization before the drugs could be prescribed but, in a major policy shift, prior authorization for all forms of MAT for treatment of SUD was removed in April 2019. With this critical change in place, practitioners are now more likely to become treatment providers for individuals with OUD that will result in improved access to treatment.
Office Based Addiction Treatment
DHS is also home to the State Medicaid agency (Division of Medical Assistance and Health Services) that, in addition to lifting prior authorization requirements for MAT under Governor Phil Murphy, also launched a major new initiative in July 2019 designed to expand access to MAT. Medicaid based the approach on the “hub and spoke” treatment model, variants of which had been implemented in Vermont and Virginia. In this model, specialty SUD clinics, such as OTPs, serve as the ‘hubs’ and treat patients with more complex needs; meanwhile, the ‘spokes’ are office-based practices and primary care settings in which most patients with more routine needs are treated. The Medicaid agency called the new initiative Office Based Addiction Treatment, or OBAT. The office-based practitioners (e.g., family physicians, psychiatrists, medical specialists, advanced practice nurses) would prescribe buprenorphine and naltrexone, and they would have office-based navigators to assist in making referral arrangements for counseling and community supports. To assist OBAT practitioners, Medicaid increased reimbursement for intake and assessment and funded a new position called the navigator, whose role is to arrange social services and supports for patients and to help monitor their progress.
The OBAT system of OUD services, also referred to as the MATRx, allows a two-way referral of patients with other Medicaid funded providers. Office-based providers can refer patients needing a higher level of medical and/or addiction
services to specialty providers (e.g., SUD treatment agencies, Certified Community Behavioral Health Clinics, Federally Qualified Health Care centers, etc.) or to one of two Centers of Excellence (COEs). The state contracted with Rutgers University and Cooper/Rowan University to serve as COEs for the OBAT initiative. In addition to providing MAT services, these centers are available for treatment and consultation referrals of individuals with complex needs, such a co-occurring medical problems and mental health issues. If practitioners without extensive experience prescribing buprenorphine feel they need support to stand-up a MAT practice, the centers are also providing MAT training and will be available to provide mentors to these practitioners.
In addition to the OBAT model, the state has also been promoting ‘low threshold treatment’ programs that provide immediate access to medication in non-traditional settings and sites, syringe exchange programs (known officially as Harm Reduction Centers), and EDs. Funding was just awarded for the provision of low threshold buprenorphine at two syringe exchange programs. EDs in some of the major hospital systems have been dispensing and prescribing buprenorphine for patients with OUDs, frequently after they have been treated for an overdose. The State Department of Health is also allowing paramedics to carry buprenorphine to ease withdrawal symptoms after patients are revived with naloxone. As the number of EDs providing buprenorphine is low, DMHAS is committed to increase those numbers. After administering buprenorphine, some EDs are providing a “warm handoff” to aftercare services to receive ongoing counseling, recovery, and other support services. Immediate access to these services is crucial for many individuals with OUD leaving EDs to prevent relapse and reduce risks of overdose after withdrawal from opioids since their tolerance to opioids might have changed.
A pilot program was established in the Atlantic County jail that provides methadone to inmates using a mobile van from the local OTP and funded by the DMHAS. The state is currently exploring opportunities to assist county correctional facilities to establish MAT programs or to enhance their existing MAT services for
New Jersey Psychologist 22
inmates. Since these individuals will need follow up services when released to the community, efforts also focus on establishing effective follow-up recovery services.
Peer-based Recovery Support Services
Individuals with SUD seeking recovery and support have traditionally gone to self-help groups or 12-step programs, such as Narcotics Anonymous. While these groups can be effective and are still an important resource, recovery and support services are increasingly being provided by dedicated peer-run recovery support programs. Peer-based recovery support services are designed to deliver nonprofessional, nonclinical help to assist individuals to achieve long-term recovery from SUDs (Bassuk et. al 2016). Unlike with many of the more traditional self-help SUD groups and support programs, these peer services are complementary with MAT services.
Peer specialists are embedded in treatment and support services throughout NJ’s system of care; the peer specialist and navigator roles in the Opioid Overdose Recovery Program (OORP) services are examples of such a program. Recovery support services are based on a “holistic definition of recovery as a self-directed process of change through which individuals improve their health and wellbeing and strive to achieve their full potential” (SAMHSA, 2011). Given the overwhelming evidence that peer-based initiatives are highly effective in recovery-oriented approaches to treatment and care for those individuals with SUD (and mental illness), peer services are funded in a variety of settings:
• Peer-led volunteer-driven Community Peer Recovery Centers (CPRC). These are places where those in recovery can find help, fellowship, and a safe haven. Peer workers provide mentoring, coaching, care coordination, social and recreation activities, life skills and vocational training, support groups, wellness classes, workshops, and other assistance.
• Recovery support services are provided for students at Rutgers University and The College of New Jersey, and an initiative will be expanded to other NJ public colleges, universities, and community colleges to enable the schools to pro-
vide recovery and substance-free housing to students in recovery, students at risk of SUD, and students not in recovery, but who choose not to misuse alcohol and illicit drugs.
• Recovery support services specifically designed for opioid-dependent pregnant women are delivered in the Maternal Wrap Around Program (MWRAP) that provides intensive case management and recovery support services for women during pregnancy and up to one year after giving birth. Intensive case management focuses on developing a single, coordinated care plan for pregnant/postpartum women, their children, families, and significant others.
• The Opioid Overdose Response Team (OORT) is a new initiative and involves outreach by teams of peer recovery specialists to individuals who were reversed from an overdose by Emergency Medical Services, but refused transport to the ED.
• A peer curriculum and training is being developed for peers working as volunteers in police departments as part of the Law Enforcement Assisted Addiction and Recovery Referral Program (LEAARRP). This will enable peers to assist individuals to make self-determined choices about their recovery pathway following arrest.
• A recovery support program, for incarcerated individuals with OUD being released to the community, has been implemented to provide continuity of care and comprehensive medical, substance use treatment and social services.
• Partnership for Success (PFS) provides prevention education and services to young people who are involved with the Department of Children and Families - Children’s System of Care. PFS targets underage drinking, marijuana use, and misuse of prescription drugs/ opioids by youth ages 9-20 throughout the state. Prevention strategies include outreach, education, and training services to communities and families.
Provider Training and Public Education Initiatives
Increasing the Number of Buprenorphine Practitioners
With funding from Governor Murphy’s opioid initiative, the state is significantly increasing the number of practitioners who can prescribe buprenorphine to expand to MAT. DATA Waiver Training is expected to be provided to more than 1,000 practitioners. To support primary care practices that are an important component of Office Based Addiction Treatment (OBAT) services, navigator-specific training is also offered since they will be an integral part of these practice settings. Because of stigma, misunderstanding, and discrimination that might affect practitioners working with individuals with SUD and their willingness to provide MAT in their practices, Rowan University was tasked with developing an interactive educational program for physicians and health care professionals addressing stigma.
Reducing the Prescribing of Opioids
The state has several initiatives that have attempted to reduce the prescribing of opioids. The newest initiative is the Opioid Reduction Options (ORO) that was developed to reduce the prescribing of opioids for pain management in EDs. The ORO approach acknowledges that for most painful conditions, opioids should not be the first line of treatment. This is modelled on non-opioid pain management programs in EDs around the country, including the Alternatives to Opioids program at St. Joseph’s Hospital in NJ. Through this initiative, hospitals and their EDs will develop an ORO plan that details the implementation of clinical protocols that call for non-opioid prescriptions, pain management therapies, and other alternative procedures. The goal is to reduce the proportion of patients receiving opioid prescriptions written in EDs to 12% or lower that is significantly lower than the 17% mean rate of opioid prescriptions written in the ED nationwide.
DHS has also been collaborating with DOH on an initiative funded through the governor’s investment to increase access to electronic health records (EHR) of patients receiving SUD care. The SUD Promoting Interoperability Program (SUD PIP) goals include modernizing the EHRs of SUD providers and allowing these to
Fall 2019 23
a platform for the sharing of electronic records. A survey of SUD providers indicated this as a critical need in the effectiveness of treatment. Greater sharing of records with healthcare providers will promote better communication and encourage treatment referrals between the SUD providers and the healthcare community.
Developing Opioid Data Dashboards
Having comprehensive real time data related to the opioid crisis is paramount to inform public health policies and practices. Thus, the state developed two websites that provide detailed information about drug-related trends in NJ. The Opioid Data Dashboard on the New Jersey Department of Health (DOH) website (<https://www.state.nj.us/ health/populationhealth/opioid/>. This real-time dashboard allows interactive data visualizations on its display, with data indicators obtained from multiple sources, including the DOH, the Division of Consumer Affairs, the Office of the Attorney General, and other law enforcement bodies. The State’s Attorney General launched the other website, NJ Cares <https://www.njcares.gov/> providing NJ-specific data on opioid and other drug-related overdose indicators, including data on opioid prescriptions, naloxone deployments, drug-related hospital visits, crime statistics, and treatment statistics.
The Future
Efforts must continue to close the treatment gap by providing more timely access to SUD treatment. Prevention efforts must increase to stop the development of an addictive disorder and solid recovery services provided to support individuals from relapsing. The further expansion of low threshold MAT programs, especially in EDs, and of interim SUD services, will certainly help here. Increased integration of SUD services in primary health care settings is also needed, as the evidence shows that individuals with OUD view healthcare settings as more accessible than specialty addiction programs mostly due to the reduced association with stigma and discrimination. Integrated services will help to address the needs of individuals with OUD who have comorbid mental illness and chronic
physical health conditions, including chronic pain, cancer, and heart disease that are known to be more prevalent among individuals with SUD. Access to integrated services will be facilitated as the state works to develop a single unified licensing structure for behavioral health and primary health care programs.
To address the sources of fentanyl and heroin that are responsible for the recent surge in overdose deaths, the New Jersey State Police started a task force to coordinate drug interdiction efforts with other agencies. Recent raids on drug mills have had a measurable impact on the supply of these deadly agents, and these raids may have been a factor in the reduction in the number of drug-related deaths in recent months. The public health partnership that has been formed between state health care agencies and the State Police has considerable potential to improve data collection and analysis. Data will be necessary to determine whether anticipated outcomes for the state’s initiatives have been realized. To effectively provide recovery support services, peer specialists need adequate training and follow-up supervision, as well as pathways for peer training and credentialing. To sustain the states multiple OUD initiatives, support for training and for development of the behavioral health professional and peer specialist workforce will be needed.
Conclusion
More than ever before, New Jersey residents with OUD are being guided into evidence-based treatment and are being supported in their recovery. After the initial state efforts were aimed at reducing overdose deaths, New Jersey has focused on expanding access to treatment and recovery supports, and on prevention initiatives. The evidence base for treatment and maintaining recovery from opioid use is especially strong for MAT that includes cognitive behavioral therapies, and peer recovery support, in addition to providing access to safe and effective pharmacotherapy. However, to engage practitioners, individuals with OUD, and the public, education to reduce the stigma associated with OUD is critical.
Many people who struggle with addiction and enter addiction-specific treatments might benefit from either additional or follow-up services that licensed
clinical psychologists can offer in private practice settings. Psychologists in private practice might also consider partnering with OUD facilities, primary care offices, and/or EDs to act as valuable collaborators in the treatment of individuals suffering from an OUD. With an array of complimentary changes in place, dramatically better outcomes could be achieved with the focus on long-term recovery and prevention. ❖
References:
Bassuk, E.L.; Hanson, J.; Greene, R. N.; Richard, M.; Laudet, A. Peer-Delivered Recovery Support Services for Addictions in the United States: A System Review. Journal of Substance Abuse Treatment 63 (2016) 1-9.
Centers for Disease Control and Prevention, National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) [online]. Retrieved <https://www.cdc.gov/injury/ wisqars/2019/05/30>.
National Academics of Sciences, Engineering, and Medicine. 2019. Medications for Opioid Use Disorder Save Lives. Washington, DC: The National Academies Press. Retrieved from https://doi.org/10.177226/2531/201 9/05/30/19.
The State of New Jersey. NJ Cares. Retrieved from <https://www.njcares. gov/04/25/2019>.
U.S. Department of Health and Human Services, Substance Abuse and Mental Health Services Administration, Center for Behavioral Health Statistics and Quality. (2018). National Survey on Drug Use and Health 2016 (NSDUH-2016-DS0001). Retrieved from <https://datafiles. samhsa.gov/2019/05/30>.
White W, Boyle M, Loveland D, Corrington P. What is Behavioral Health Recovery Management? A Brief Primer 2008 Feb 13; 2005. [Web Page]. <www.addictionmanagement. org/recovery%20management.pdf>.
Continuing Education Instructions: Visit <www.psychologynj.org> and find the CE Homestudy Library link under the Learn tab. This will take you to the online library where you will find the article and evaluation.
New Jersey Psychologist 24
Book Review: Howard Stern Comes Again (2019)
Anthony F. Tasso, PhD Chair, Department of Psychology & Counseling Fairleigh Dickinson

University
Long-time radio disc jockey and self-proclaimed “King of All Media,” Howard Stern, released his third book in May 2019. The book, Howard Stern Comes Again, published by Simon and Schuster, is a collection of what Stern believes are his most intimate and impressive on-air interviews, all of which occurred during the latter half of his four-decade career.
These sit-downs with well-known actors, comedians, musicians, and TV personalities are nothing short of profound. The immensely interesting interviews offer insight into these public figures’ variety of talents, allowing the audience to learn details about them not known prior to their Stern Show appearance. These conversations are even better than advertised and absolutely make the book worth the price of admission. The depth and breadth with which Stern is able to assay the inner experiences of his interviewees undergird his reputation as an interviewer par excellence.
While fascinating, one might ask, “Why is Howard Stern’s book being reviewed here, in a professional psychology journal?” After all, this is the radio guy (in)famous for instigating an incalculable number of celebrity feuds; for cajoling women to strip naked on his radio program; for creating a radio environment riddled with flatus, silliness, and sophomoric humor. Wasn’t it Howard who soared above the crowd at an MTV awards show as “Fartman,” complete with his buttocks on full display? In other words, is the NJ Psychologist an appropriate venue for the man who is the very definition of “shock jock?”
A fair question, and one certainly expected to be asked by any socially conscious psychologist. My unequivocal opinion is yes, Howard Stern Comes Again most deservingly warrants a review here. While the interviews are deeply profound and akin to material that regularly emerges in
New York, NY: Simon & Schuster.
our consulting rooms, this is not the most salient reason to discuss the book in a psychology journal. Instead, I contend Howard’s personal revelations that he peppers throughout the book, show exactly why psychologists should give it a read. Stern imbues the pages of Comes Again with descriptions of his developmental experiences and emotional struggles, delicately delving into how they fomented a simmering hostility that compromised his ability to connect with others. He pinpoints how his inner turmoil accounts for a considerable amount of his early personal and professional life. Crucially, Stern informs the reader that he no longer operates in this fashion. Splattered across the 500-plus pages is evidence of how Howard developed insight into this antipathetic means of relating to others and how he worked to make amends to those who suffered thanks to his acerbic tongue.
How did he accomplish this? Psychoanalysis. Yes, wild-man Howard Stern found psychoanalysis and intensive psychotherapy as the vehicle to facilitate his authentic personal and professional change.
At the start of Comes Again, Howard reports on a relatively recent cancer scare. He describes how this confrontation with mortality, an incident that resoundingly debunked his belief in his own omnipotence, functioned as a significant impetus for writing this book. Comes Again, Howard writes, serves as atonement for his more contentious, and (in his opinion) unflattering early interviews. Stern hopes the book will function as a solid springboard to rewriting his legacy. Oh, and he thought this writing project would be an easy way to make a fast dollar. While Howard realized early on that writing this book was quite difficult, the public’s reaction to Comes Again seems to indicate he is succeeding in revamping his image.
Although Stern has hundreds of worthy interviews at his disposal, I believe the ones he selected are significant based on his interest in his subjects’ confrontation
of existential topics. In his pre-transcript comments, Howard weaves in themes of loss, trauma, empathy, admiration, and contrition; this commentary functions like a psychoanalytic dialogue by honing in on his hopes, regrets, feelings, fantasies, and associations vis-à-vis the life stories of his interviewees. For example, Stern identifies with Madonna’s iconoclastic past and empathizes with her early traumatic family loss, and notes how the impact of death on Stephen Colbert, Rosie O’Donnell, and Anderson Cooper evokes associations of his own mother’s experience of death and the subsequent effects it had on her mothering of Howard. He professes admiration for, and inspiration from, a broad range of talents (e.g., Jon Stewart, Chris Rock, Bill Murray, Jay-Z, Steve Martin, Lady Gaga, Jimmy Kimmel, David Letterman), describes how he relates to Jerry Seinfeld’s preoccupation with producing comedic material, and explains how he identifies with Vincent Gallo’s rage. Stern exhibits a sincere admiration for Joan Rivers’ unapologetic demeanor and an overall respect for Tracy Morgan.
Perhaps one of his most prominent themes is that of regret and remorse. Howard expresses contrition for his prior hostility toward Rosie O’Donnell (with whom he now has a close friendship) as well as for his mockery of many others, even those he holds in high regard (e.g., Jon Stewart, David Letterman). Howard even reveals his posthumous guilt for his treatment of Robin Williams, whom he believes he unfairly attacked during his one and only interview with the actor and comedian a couple decades ago. Stern delves into his interviews with Ellen DeGeneres (which he considers his most emotional) and Conan O’Brien (which he believes may be his best ever).
Setting aside the commentary Stern provides, the transcripts highlight his brilliance as an interviewer. However, in Comes Again Howard says he was not a good interviewer prior to his experience at the other end of the metaphorical micro-
Fall 2019 25
phone: his encounter as a psychoanalytic patient. Respectfully, I view this statement as categorically false and likely hyperbolic (nothing unfamiliar to Stern). My perspective is based on nothing less than three decades of painstaking Howard Stern Show research, my investigative methodology consists of listening to his radio program dating back to my adolescence in the late 1980s (all in anticipation of this book review, of course). Yet, my assertion is supported by more objective empirical data Howard himself offers in this book, such as when he reveals that ABC offered him a Barbara Walters-like interview show in the early 2000s. Since the nascent years of his radio career, Stern, when not on the attack, has exhibited an uncanny ability to create a holding environment of sorts, where subjects are relaxed and, emblematic of the psychotherapy hour, often reveal more about themselves than anticipated.
Howard has a history of demonstrating a sincere, nonjudgmental appreciation of the complexity of the human experience. His keen ability to explore both the lighter and darker sides of others without an air of moral superiority has always been, in my opinion, his greatest professional virtue. This capacity to illuminate the broad range of his interview subjects, whether an exalted celebrity, an everyday person on the street, the proverbial dregs of society, or one of the social misfits who regularly visits his show (aka “The Wack Pack”), is always far more entertaining than his hostile rants or the cascade of naked women that once populated his radio program. This aptitude only accelerated after he began psychotherapy. It appears that it took the experience of truly being heard, in an analytic fashion, for him to be able to hear and subsequently empathize with his subjects. In other words, he needed a relationship with an intimate “audience” of one (his therapist) to truly connect with his interviewees in concert with his audience of millions (his listeners).
Today, his perspicacity that was once weaponized to exploit others is now a tool brandished to support, elucidate, and empathize, all predicated on his capacity for vulnerability, that he utilizes to provide a space for his subjects to disclose more than they thought they would. Put differently, Howard’s interviews shifted from “gotcha” to “help-ya.” Where this exemplary ability to appreciate the broad
range of people’s psychologies stems from is unclear, but what is evident is that while he has always been comfortable exploring the disquieting aspects of others, today he seems more at ease with his own.
I believe Howard Stern’s stellar interview style is grounded partially in the fact that he has always been the embodiment of contradiction. For example, despite a history of misogynic antics, he consistently demonstrates a willingness to advocate on behalf of women (as discussed in his 2016 profile in the New York Times); he is considered unsuitable for children, yet he morphed into a beloved family entertainer while on America’s Got Talent. At one time, Howard was deemed too raunchy for regular radio that contributed to his move to satellite radio. Now unencumbered by the constraints of governmental parameters (i.e., the Federal Communications Commission rules) or other parochial entities, Stern paradoxically converted his show into a more socially acceptable, PGrated program. I contend these contradictions help account for Stern’s enduring appeal, whereas most other so-called shock jocks are limited to an evanescent public relevance.
The Stern machine has been rolling for decades, seemingly gaining momentum, despite the many predictions of a hastier fade into oblivion as a function of his age (65 years old) and his move to satellite radio (that requires a subscription plan) more than a decade ago. His omnipresence during his promotion of Comes Again on TV, radio, and in print appears to confirm his reign as the King of All Media. Reports by media experts prognosticating his professional irrelevance were greatly exaggerated.
In fairness, the Howard Stern phenomenon has always been difficult to comprehend. During the rapid early ascendency of the Stern Show, “experts” struggled to understand the copious amount of time his fans spent tuned in to the program. Upon investigation, they found the most frequent reason his followers did so was “because they wanted to hear what he would say next.” The truly vexing finding, at least to stuffy radio executives, emerged when polling nonfans and even those harboring disdain for Howard. When queried about why the disinterested listeners and self-proclaimed Stern haters remained engaged with his
show even longer than fans, the primary reason given was “because they wanted to hear what he would say next.”
Perhaps Howard Stern Comes Again represents a repetition compulsion, similar to when fans and nonfans alike remain glued to hear what he’ll say next. For the ardent fan, the book provides an even deeper window into the development of Stern the person and Stern the radio personality, proffering keen perspectives into the mutually interactive evolution of each. The casual listener will, if nothing else, appreciate the reflective stance of one of the best interviewers on the planet. Surprisingly, the vociferous Stern hater may enjoy Comes Again the most, as this reader will realize the man they always considered a mere shock jock (or worse), who ostensibly appears simplistic and shallow, is clearly appreciative of the complexities within himself and others.
The commentary and transcripts in Comes Again pull the curtain back on the man whose early career was fueled by unneturalized rage, sex and aggression, “pure id,” as Howard himself confesses. Today, he has converted his approach from primitivity to rationality, from self-absorption to self-actualization. All readers bear witness to the transformational power of intensive, insight-orientated psychotherapy. They will hear a man in his sixties repeatedly state how psychoanalytic work changed his life: how it helped empower him to become closer to others; to no longer deem others a threat but instead work to foster closeness; to find the courage to apologize to those he viciously targeted; to lean on his ongoing psychotherapy experience to develop an authentic interest in others, even while countering his own narcissistic desires; and to deeply appreciate his wife, daughters, and parents.
Comes Again is uniquely packaged as part memoir, part career cherry picking, and part declaration of contrition. Stern’s willingness to allow his audience a glimpse of several of his long-standing struggles has been a slow, steady progression, from his early days of radio in that he portrayed himself as infallible (a defense belied by his anxiety-riddled squeaky intonation), to his mid-career period (circa his Miss America book) when he divulged his struggles with obsessive-compulsivity and psychosomatic-based back pain, to the present day when (born out of his psycho-
New Jersey Psychologist 26
therapeutic experience) he allows others access to his psychological vulnerabilities. Today, Stern demonstrates a healthy balance between revealing enough to connect with his guests and audience and protecting his loved ones’ privacy.
Something that struck me when reading Comes Again and listening to Stern during his book tour is how his intrapsychic and interpersonal processes pre-therapy to now seem to parallel the Kleinian process of proactively moving from the paranoid-schizoid to the depressive position. Anchored in a fear of annihilation, Howard’s early withdrawal from intimacy gave him the illusion of being capable of warding off anxieties. This was apparent in his near-myopic professional aim to obliterate those seen as a threat. The psychic tax of such a position was insufferable; it ultimately resulted in distress, dysphoria, and mind-body breakdowns along with any number of personal and professional relationships fractured or forgotten. Howard now demonstrates the more complex and psychologically healthy characteristics of the depressive position capable of apprehending that others are whole objects (rather than disparate good and bad parts). This is evident in his jettisoning of his fears of persecution and annihilation and the subsequent need to destroythat is replaced with the realization of the power of his own aggression and how he might use it to help rather than harm.
During the book’s promotion, there was not a single interview in which Howard failed to extol the virtues of his ongoing psychoanalytic experience. In fact, he went so far to state that he believes meaningful, lasting change is not possible without the aid of intensive psychotherapy, and that he hopes his words will serve as a public service announcement for those, primarily men, prone to diminish the necessity of mental health treatment. Howard Stern, the man who brought us Butt Bongo Fiesta, Crucified by the FCC, and New Year’s Rotten Eve, is now an ambassador for psychotherapy. From Fartman to analysand? Wow…Howard continues to shock.
A quote from Comes Again encapsulates the power of psychotherapy. When reflecting on his early aggressiveness compared to his current more open and empathic stance, Howard comments:
“The hard-ass pose I’ve tried to main-
tain just doesn’t work for me anymore. That posture was useful when I was young. It provided an almost impenetrable shell that protected me from feeling need.
If I denied my own humanity, I would not go hungry for human kindness, touch, and most important love. It was a safe world but a lonely one, a kind of prison. So finally, after many years, I began to tear down some very well-constructed walls. I needed to do that if I was going to have a successful marriage…as well as a deeper and more loving relationship with my fantastic daughters. I once needed solitary confinement, but I was now willing to leave the safety of my incarceration and take a step outside.” (pg. 19)
Although this book is ripe with data that reflects Stern’s personal growth and how it has transformed his professional work, please don’t think for one minute that the adolescent humor that once defined him is confined to the Stern Show archives. One needs to look no further than the title of this book to realize that his juvenile humor persists. Remnants of the id remain alive and well.
Despite Howard’s notable personal progressions, he openly acknowledges there is more psychotherapeutic work to be done. This is an impressive admission to make. While I am well aware that a therapist’s desires should never impinge upon a patient’s subjective goals, I have an admittedly narcissistic fantasy regarding Stern’s continued treatment. Much of Comes Again touches on how he has made amends with those he once targeted. This is laudable. However, I hope another group beleaguered by Howard will receive an apology: psychologists. Anyone who has listened to Stern pontificate about the merits of psychotherapy during his on-air stream of consciousness knows he repeatedly anoints psychiatrists as the “right” psychotherapists; psychologists are the lesser of the two. Perhaps his continual growth, augmented by his daughter’s pursuit of a doctorate in clinical psychology, will bring about a mea culpa to our profession. This is my none-too subtle prompt; given that in Comes Again Howard admits to being highly suggestible, perhaps we can hope to receive our apology soon. Time will tell.
Stern is on record as harboring a level of embarrassment regarding his first two books (Private Parts and Miss America)
and intimates that they should be shelved permanently. At the risk of sounding unempathic to Howard’s feelings, I feel there is value in reading (or rereading) both books, not only for their raw humor but also to more fully understand Howard the professional and Howard the person. I contend that reading those two books prior to picking up Howard Stern Comes Again will highlight the evolution of the shock jock who revolutionized radio. Or rather, his continued evolution, as his professional and personal journey is far from complete. ❖
References:
Stern, H. (1993). Private Parts. New York, NY: Simon and Schuster.
Stern, H. (1995). Miss America. New York, NY: ReganBooks.
About the Reviewer: Anthony F. Tasso, Ph.D., ABPP is Professor of Psychology and Chair of the Department of Psychology and Counseling at Fairleigh Dickinson University in Madison, NJ. He also maintains a private practice in Whippany (Hanover Township), Morris County, NJ.
Joseph Ganz, PhD
NJPA Member, 33 years
Luise Gray, PsyD
NJPA Member, 32 years
Ira Mintz, PhD
NJPA’s first Director of Professional Affairs
Charles Zadikow, PsyD
NJPA Member, 50 years
Fall 2019 27
In Memoriam
Mitch Abrams, PsyD
Rhonda Allen, PhD
Amy Altenhaus, PhD
Mark Aronson, EdD
Alyssa Austern, PsyD
Jeffrey Axelbank, PsyD
Kyle Barr, IV, PsyD
Thomas Barrett, PhD
Louis Barretti, PhD
Theodore Batlas, PsyD
Amy Becker-Mattes, PhD
Leslie Becker Phelps, PhD
Roderick Bennett, PhD
Todd Bennett, PsyD
Rhea Bensman, PsyD
Helen Berman, PhD
Nancy Bloom, PsyD
Monica Blum, PhD
Alice Bontempo, PsyD
Randy Bressler, PsyD
Richard Brewster, PsyD
Natalie Brown, PhD
Charles Buchbauer, PhD
Diane Cabush, PsyD
Rosemarie Ciccarello, PhD
Jennifer Cleveland, PhD
Karen Cocco, PhD
Sidney Cohen, PhD
Deniz Colak, PhD
Louise Conley, PhD
John Corbisiero, PhD
Joseph Coyne, PhD
Stephanie Coyne,PhD
Daniel DaSilva, PhD
Richard Dauber, PhD
Bernice Davis, PsyD
Sarah DeMarco, PsyD
Promila Dhillon, PhD
Phyllis DiAmbrosio, PhD
John Diepold, PhD
Rosalie DiSimone-Weiss, PhD
Charles Dodgen, PhD
Rosalind Dorlen, PsyD
Edward Dougherty, EdD
Frank Dyer, PhD
Nick Economou, EdD
Daniel Edelman, PsyD
Lynn Egan, PsyD
Susan Esquilin, PhD
Sean Evers, PhD
Roberta Fallig, PhD
Janie Feldman, PsyD
Stephen Feldman, PhD
Thank you 2019 Sustaining Members!
By advancing your level of membership to Sustaining Membership status, you have generously demonstrated your additional support of your professional association. We thank you for your commitment and dedication to your organization!

Dennis Finger, EdD
Christine Fingerroth, PsyD
Resa Fogel, PhD
Pamela Foley, PhD
James Fosshage, PhD
Kenneth Freundlich, PhD
Antonia Fried, PsyD
Thomas Frio, PhD
Abisola Gallagher, EdD
Kenneth Gates, PsyD
Leslie Gilbert, PhD
Marc Gironda, PsyD
Ronald Gironda, PhD
Linda Glazer, PsyD
Elizabeth Goldberg, PhD
Gary Goldberg, PhD
Wayne Goldman, PhD
David Gomberg, PhD
Lois Goorwitz, PhD
Ora Gourarie, PsyD
Hadassah Gurfein, PhD
Mathias Hagovsky, PhD
Cynthia Haines, PsyD
Osna Haller, PhD
Raymond Hanbury, PhD
Jeffrey Harrison, PhD
Steven Hartman, PhD
John Hennessy, PhD
Susan Herman, PhD
Susan Herschman, PsyD
Lauraine Hollyer, PhD
Ann Nikolai Houston, PhD
Lisa Jacobs, PhD
Alison Johnson, PsyD
Kyung Jung, PhD
Nancy Just, PhD
Jeffrey Kahn, PhD
Paula Kaplan-Reiss, PhD
Robert Karlin, PhD
Charles Katz, PhD
Toby Kaufman, PhD
Thomas Kavanagh, PsyD
Eileen Kennedy-Moore, PhD
Richard Kessler, PhD
Lisa Kestler, PhD
Stanley Keyles, PsyD
Joel Kleinman, PhD
Steven Korner, PhD
Deirdre Kramer, PhD
David Krauss, PhD
Phyllis Lakin, PhD
Robin Lang, PsyD
Eli Leiter, PhD
Roman Lemega, PhD
Ilana Lev-El, PsyD
Robert Levine, PhD
Monica Lintott, PhD
Neal Litinger, PhD
John LoConte, PhD
Rebecca Loomis, PhD
Mark Lowenthal, PsyD
Konstantin Lukin, PhD
Marc Lyall, PsyD
Marilyn Lyga, PhD
David MacIsaac, PhD
William MacLaney, PsyD
Daniel Mahoney, EdD
Stanley Mandel, EdD
Melissa Rivera Marano, PsyD
Bonnie Markham, PhD, PsyD
Nicole Martell, PsyD
Neil Massoth, PhD
Shirley Matthews, PhD
John McInerney, PhD
David Mednick, PsyD
Wilda Mesias, PhD
Marshall Mintz, PsyD
Barry Mitchell, PsyD
Noreen Mohle, PhD
Ruth Mollod, PhD
Sharon Ryan Montgomery, PsyD
Gregory Moore, PsyD
Caridad Moreno, PhD
Sandra Morrow, PhD
Daniel Moss, PhD
Richard Mucowski, PhD, EdD
Morgan Murray, PhD
Susan Neigher, PhD
Jeffrey Newenhouse, PsyD
Hulon Newsome, PsyD
Daniel Noll, PhD
Cheryl Notari, PhD
Denise Novaky, PhD
Carly Orenstein, PsyD
David Panzer, PsyD
Craig Pearl, PsyD
Francesca Peckman, PsyD
Mark Pesner, PhD
Michele Rabinowitz, PsyD
Nicole J. Rafanello, PhD
Jonathan Rapaport, PhD
Richard Rapkin, PsyD
Howard Rappaport, PsyD
Gina Rayfield, PhD
Lori Rayner-Grossi, EdD
Ann Reese, PhD, PsyD
Ellen Reicher, PhD
AnnaMarie Resnikoff, PhD
Laura Richardson, PhD
Marion Rollings, PhD
Amelia Romanowsky, PsyD
Barbara Rosenberg, PhD
Francine Rosenberg, PsyD
Elissa Rozov, PhD
Anne Rybowski, PhD
Nicole Safonte-Strumolo, PhD
Carole Salvador, PsyD
Peter Schild, EdD
Jay Schmulowitz, PhD
Natalie Schuberth, PsyD
Ellen Schwartz, PhD
Margot Schwartz, PsyD
Nancie Senet, PhD
Eileen Senior, PsyD
Laura Shack-Finger, EdD
Arline Shaffer, PhD
William Shinefield, PsyD
Nancy Sidhu, PhD
Ronald Silikovitz, PhD
Jane Simon, PhD
Jeffrey Singer, PhD
Tamara Sofair-Fisch, PhD
Jeffrey Spector, PsyD
Mary Ellen Stanisci, PhD
Jakob Steinberg, PhD
Deana Stevens, PsyD
Jeffrey Stone, PhD
Vincent Stranges, PhD
Luc akagi, PsyD
Anthony Tasso, PhD Sant'Anna T y
H. Augustus Taylor, PhD
Tamsen Thorpe, PhD
Barbara Tocco, EdD
Jonathan Wall, PsyD
Virginia Walters, PsyD
Arnold Washton, PhD
Beth Watchman, PhD
Virginia Waters, PhD
Daniel Watter, EdD
Allen Weg, EdD
Aaron Welt, PhD
Norbert Wetzel, ThD
James Wulach, PhD, JD
Joshua Zavin, PhD
Stanley Zebrowski, PhD
Michael Zito, PhD
New Jersey Psychologist 28
Report from APA Council - August 2019
The Guidelines for Psychological Practice for People with Low-Income and Economic Marginalization are the first APA guidelines to address the needs of low-income people, who are underserved, understudied, and diverse, says Cindy L. Juntunen, PhD, a professor at the University of North Dakota and chair of the low-income guidelines task force.

posthumous presidential citation.
The Council of Representatives of the American Psychological Association met in Chicago, IL on August 7th and 9th 2019.
Chicago is lovely in the summer, with the backdrop of Lake Michigan and plenty of deep-dish pizza options. I was again honored to have the opportunity to represent New Jersey at the APA Council of Representatives meeting.
The following is a summary of the major decisions and votes at this meeting. Some of what is reported below is excerpted from a meeting summary provided to council members from APA
On Wednesday morning, Jean Carter, PhD provided Council with the financial report.
Council also received an update from APA’s CEO, Dr. Arthur Evans. He highlighted that recently crafted statements and policies all have the common thread of reinforcing our strategic goals. APA has also been working much faster to release statements in timely fashion. For example, we were able to craft and release a statement on gun violence just hours after the latest tragedies. We are also working and collaborating with major organizations and partnerships in the country to strengthen psychology’s voice.
For one of the first motions on the floor, Council was asked to approve amending the Association Rules to add four additional seats to the Board of Professional Affairs (BPA) as follows: three APA members to be nominated by the Board of Directors and elected by Council; and the past-chair of the Council of Executives of State, Provincial and Territorial Psychological Associations (CESPPA) serving ex-officio. BPA recommended these changes due to the additional responsibilities BPA will undertake as a result of the sunsetting of the Committee for the Advancement of Professional Practice (CAPP) at the end of June 2019. This motion passed by 98.8 %.
Council also voted overwhelmingly in favor of two sets of guidelines.
The guidelines are an important step for a couple of reasons, she says. The first is that research finds that low-income and economically marginalized individuals are far more susceptible to health and mental problems than those with more resources but have less access to needed services.
The second is that psychologists typically have more resources than many of the clients they serve. So, to provide culturally informed care, it’s critical that they reach outside their comfort zones and determine more effective ways of providing services, for example, by offering sliding scale fees or shorter sessions that better accommodate these clients’ budgets and work schedules.
Also important, according to the guidelines, is viewing poverty in a structural context.
In addition, the council approved the Race and Ethnicity Guidelines in Psychology: Promoting Responsiveness and Equity that update research on the effective understanding and treatment of ethnically and culturally diverse clients and help psychologists develop stronger tools to respond appropriately to them.
A business item that addressed adding an Early Career Psychologist to the agenda planning group was approved by 99.4 %.
An amendment was proposed that would permit the current Member-atLarge or the early career psychologist member of the Council Leadership Team whose term is ending, to be able to run for chair-elect. This passed by 78.2%.
On Wednesday afternoon, recently deceased members were honored. Additionally, on Wednesday afternoon, the Committee on Early Career Psychologists presented Division 42 with a recognition for promoting the expertise of early career psychologists and encouraging early career involvement in leadership.
On Friday morning, Dr. Ronald Rozensky was presented with the Raymond D. Fowler Award for Outstanding Member Contributions. Additionally, Dr. Alberto-Garcia was presented with a
A motion that generated a lot of discussion and back and forth commentary was when Council was asked to approve amendments to the APA bylaws and association rules that would create a new membership category for masters and doctoral students. This approved amendment to the APA bylaws and association rules would create an official membership category for graduate students that specifically gives them voting rights after one year. Those rights include the ability to vote for president-elect, members-at-large of the Board of Directors, apportionment and bylaws amendments. I had proposed an amendment to the motion that would limit this graduate student member category with voting rights to only doctoral level students. That amendment did not pass.
Council also voted to allow an amendment to the original proposal that will change Associate Members’ waiting period for voting privileges from five years to one year. These proposed bylaw changes were approved by a 73% vote. APA voting members will receive the ballot for both items on Nov. 1.
APA’s Council of Representatives overwhelmingly approved the 2019 APA Immigration and Refugee Policy Statement <https://www.apa.org/about/policy/apaimmigration-policy.pdf> that encourages psychologists to use their training to treat and advocate on behalf of immigrants, refugees, and people seeking asylum in the United States.
More than 98% of council members voted in favor of the policy that highlights the psychological stresses faced by immigrants, refugees and their families, and supports the need for policies and practices that consider their well-being, including medical, psychological and social services.
I am proud to be your representative to APA. I am also now the Memberat-Large of the executive board of the Caucus of State/Provincial/Territorial Representatives, a role that I am hopeful will expand my ability to ensure that the concerns of my fellow New Jersey psychologists continue to be addressed. ❖
Respectfully submitted,
Rhonda Allen, PhD Council of Representatives (NJ) (2019-22)
Fall 2019 29
APA COUNCIL REPORT
Rhonda Allen, PhD
APA Council Representative (NJ) (2019-22)
NJPA Advocacy Efforts
State Advocacy
NJPA is committed to strengthening our political outreach and advocating for the interests of NJ psychologists and mental health issues that are important to the public. Over the years, our advocacy took many forms. Through our Committee on Legislative Affairs (COLA) and our Governmental Affairs Agent (GAA), NJPA is instrumental in maintaining standards of psychology practice in NJ, protecting patients’ rights, and supporting public policy. NJPA also monitors State Rules and Laws that regulate the profession, and maintains a liaison with the NJ Board of Psychological Examiners so we are always informed about any changes that may affect our members.
State Advocacy Highlights -
January 2019 - Introduction of NJ Licensing Act Legislation Bill A5307 that streamlines psychologist training requirements and amends P.L. 1966, c.282, to increase the public’s access to psychologists by increasing flexibility in the timing of supervised hours for licensure.
March 2019 - Submission of NJPA Public Comments for the BoPE proposed regulations requesting broad interpretation and clarification of the opioid continuing education requirement, and worked with the American Psychological Association to submit comments requesting clarification regarding the telemedicine and telehealth proposed regulations.
March 2019 - met with the Attorney General to establish the Attorney General’s Duty to Warn Law Workgroup. This workgroup will address the details about the Duty to Warn law amendments.
April 2019 – Bill S3099 Behavior Analyst Licensing Act was discussed with bill sponsor Senator Loretta Weinberg’s office, including discussion of the
unintended consequences to the public and the field of psychology. NJPA is collaborating with APA on this issue, and we will continue to be a resource for the bill sponsor.
July 2019 - Discussion with Majority Leader, Assemblyman Louis Greenwald’s office regarding access to care in New Jersey. These access to care initiatives are particularly relevant to individuals in underserved areas of the state.
August 2019 - Presented Assemblywoman Valerie Vainieri Huttle with the 2018 NJPA Legislator of the Year Award.
September 2019 - NJPA notified members of the opportunity for public comments for the BoPE proposed regulations degrees earned outside of the USA.
September 2019 – NJPA and NJPA Foundation Leadership attended an Essex/Union Psychological Association (EUCAP) meeting where Assemblywoman Mila M. Jasey, a former New Jersey public health nurse, was the featured guest. The discussion with Assemblywoman Jasey focused on mental health access by K-12 through college age school children and young adults, the trauma informed and restorative justice movements, cultural competency, opportunities for psychologists to speak with community leaders, as well as the New Jersey legislative process.
October/November 2019 - Planning began for the December 5, 2019 NJPA Trenton Day, (see page 18) to be funded by the NJP-PAC. This day will provide NJPA and affiliate members with an opportunity to delve in to the NJ legislative process, understand how a bill becomes a law, and learn the importance of grassroots advocacy. We will hear from legislators and staff about the process in which legislation is introduced and passed, and shared ideas on ways
that psychologists and psychologists-intraining can influence the formation of public policies.
November 2019 - Presentation of the 2019 NJPA Legislator of the Year Award to Senator Joseph Vitale.
November 2019 - Introduction of Maiden Names bill - Assemblywoman Valerie Vainieri Huttle has agreed to introduce legislation on behalf of NJPA that would modify the New Jersey Division of Consumer Affairs’ policy regarding the use of legal names on licenses and other professional materials to allow for the use of maiden names.
Federal Advocacy
Every year, the American Psychological Association gathers delegates from the 60 state, provincial, and territorial psychological associations, as well as American Psychological Association staff and committee members, at the Practice Leadership Conference to provide advocacy training for leaders in the field of psychology. Following several days of training events, the delegates head to Capitol Hill to meet with their congressional and state representatives. In March 2019, the New Jersey Psychological Association delegates met with the following New Jersey representatives’ and senators’ offices to discuss cosponsoring two bills that remove barriers to quality mental health access for Medicare patients through bills HR884 and HR1301 and preserving mental health and substance use disorder coverage in Medicaid and private health insurance plans under the Affordable Care Act. Lastly, we enjoyed having a dialogue with them about important social advocacy issues.
Rep. Tom Malinowski (D-NJ-07); Rep. Jeff Van Drew (D-NJ-02); Rep. Andy Kim (D-NJ-03); Rep. Mikie Sherrill (D-NJ11); Rep. Frank Pallone (D-NJ-06); Rep. Bill Pascrell (D-NJ-09); and Sen. Bob Menendez (Senator D-NJ).
New Jersey Psychologist 30
by NJPA President, Morgan Murray, PhD, COLA Chair, Barry Katz, PhD, and Executive Director, Keira Boertzel-Smith, JD
Social Advocacy
NJPA is working on making significant contributions to the general public, policy makers, and its own membership by providing scientifically based psychological information to guide informed advocacy and decision-making on issues that affect the mental health and general well-being of the diverse people of New Jersey. NJPA will continue to develop and disseminate public statements on current societal issues. This effort might also include publicly endorsing statements that has been made by the American Psychological Association. Examples of statements we have both created and endorsed include: NJPA, through the New Jersey Inter-Mental Health and Psychological Associations Coalition (IMPAC), Recognizes the 400th Anniversary of the first Africans who arrived in 1619, ushering in the Era of American Slavery; NJPA Endorses the Statement of APA President in Response to Mass Shootings in Texas, Ohio; NJPA Celebrates Pride Month and the Progress Against the Oppression of Homophobia it Represents for Members of the LGBTQI+ Community; NJPA addressed the mental health needs of refugees, immigrants, asylum seekers, and detainees.
The NJPA executive board approved a Committee on Diversity and Inclusion (CODI) subgroup – the Immigration Emergency Action Group (IEAG) that will explore how to address the mental health needs of those directly and indirectly affected by the immigration crisis. This group will also explore the feasibility of working toward changing existing immigration policies and laws based on psychological research that demonstrates the detrimental short and long-term effects of the current practices (E.g., separation of immigrant families). The IEAG will increase the positive impact of their efforts by seeking opportunities to collaborate with non-profit groups and other professional associations that are working to promote the welfare of immigrants detained in New Jersey.
Our Successful Changes in New Jersey Law Over the Years
2017 Authorization of the provision of healthcare services through telemedicine and telehealth, and supplementing various parts of the statutory law.
2014 Professional Corporation Act -
inclusion of psychologists
2013 Jurisprudence Exam in New Jersey
2010 Direct Payment of Benefits to Outof-Network Providers requires third party payers to reimburse psychologists directly when patient assigns benefits
2004 Capacity for Guardianship through the Civil Practice Committee, Superior Court of NJ
2000 Lawsuit against MCC Behavioral Care, Inc. successfully settled
1999 Prompt Payment (supported)
1999 Mental Health Parity (Coalition) [Serious Mental Illness]
1997 Health Care Quality Act (supported)
1997 Competency Evaluations in Criminal Cases
1996 Hospital Privileges
1996 Lawsuit filed against MCC Behavioral Care, Inc.
1993 Counselors Licensing (opposed)
1991 Duty to Warn
1989 Temporary Disability
1985 Peer Review
1974 Freedom of Choice
1966 Psychology Licensing Law Signed ❖
Fall 2019 31

Becoming disabled during your working years happens more than you might imagine. If you are seriously injured or become ill and cannot work, can your loved ones continue to pay the bills and still live comfortably?


Trust Endorsed Income Protection (Disability Income) Insurance* is the key to providing you and your family with income and financial stability while you get well and get back to what you do best.
Apply for this coverage with rates often lower than similar insurance available to the general public. If you already have disability insurance, compare the rates of The Trust’s Income Protection Plans against what you already own at trustinsurance.com. You may achieve substantial savings.
* Coverage is individually underwritten. Policies issued by Liberty Life Assurance Company of Boston, a Lincoln Financial Group Company. Plans have limitations and exclusions. For costs and complete details, call The Trust or visit www.trustinsurance.com Sample rates: $2,500 Monthly Benefit –LifeStyle 65 Plan, 90 Day Waiting Period Age Quarterly Premium 35 $55.25 40 $70.50 45 $103.00 50 $121.25 55 $141.00 Choose the plan that fits your needs! Watch the Q&A video What You Need to Know About Income Protection Insurance at trustinsurance.com. 1-800-477-1200 INSURANCE PROGRAMS For Psychologists, By Psychologists On Your Feet 7.5x10 BW.indd 1 8/1/2019 10:06:15 AM



Hiring Mental Health Professionals Just Got A Lot Easier Get your jobs in front of the NJ mental health community! Introducing The New Jersey Psychological Association Career Center Representing mental health professionals in a variety of settings: private practice, clinics, academia, research, schools, industry/organizations NEW! EXCLUSIVE MEMBER PRICING! MORE OPTIONS A BETTER WAY TO HIRE Members can now take advantage of discounted member rates! Simply log in with your NJPA account today and receive the discount at checkout! Promote your open jobs: ~Sponsor your job posting for increased exposure! ~Feature jobs in our weekly email blast The Friday Update Promote your employment opportunities to our highly targeted audience by placing your job openings in front of high quality, motivated candidates who are actively seeking their next career move! GET STARTED TODAY! careers.psychologynj.org 973-243-9800 www.psychologynj.org