Sleep disorders – overview and pitfalls
Dr. Aditya Jindal Interventional Pulmonologist & Intensivist, sleep specialist
Jindal Clinics SCO 21, Sec 20D, Chandigarh
DM Pulmonary and Critical Care Medicine (PGI Chandigarh),

FCCP





Sleep disorders
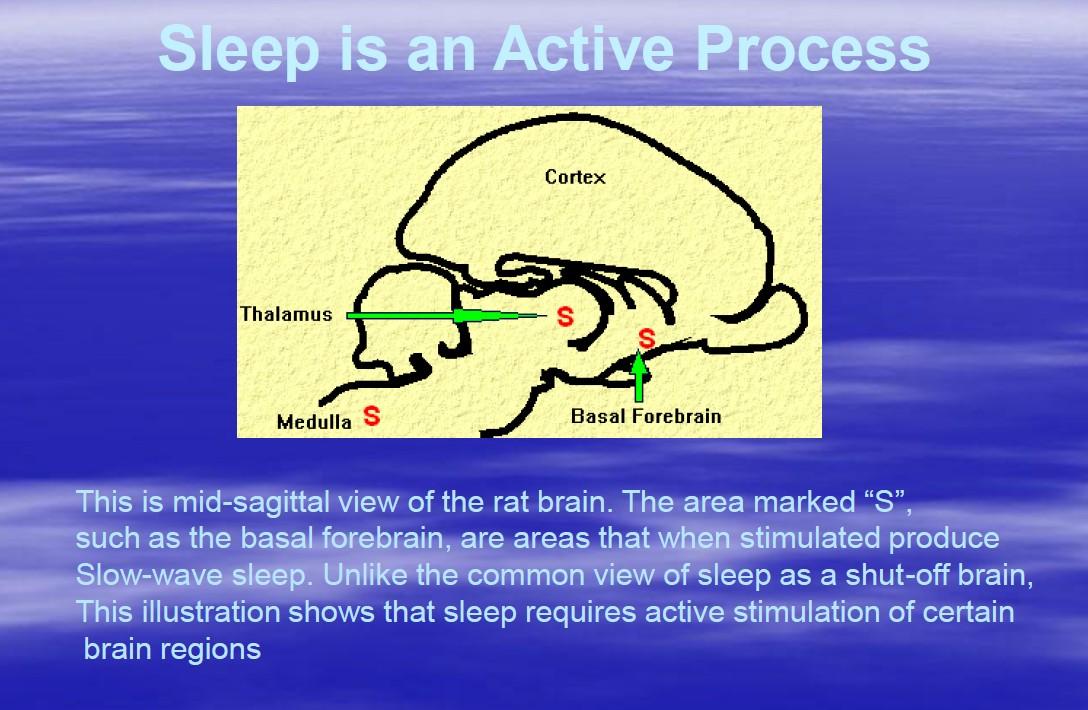
Sleep
2. Sleep related
3. Insomnias 4. Parasomnias 5. Hypersomnias 6. Circadium rhythm sleep-wake disorders
1.
related breathing disorders
movement disorders
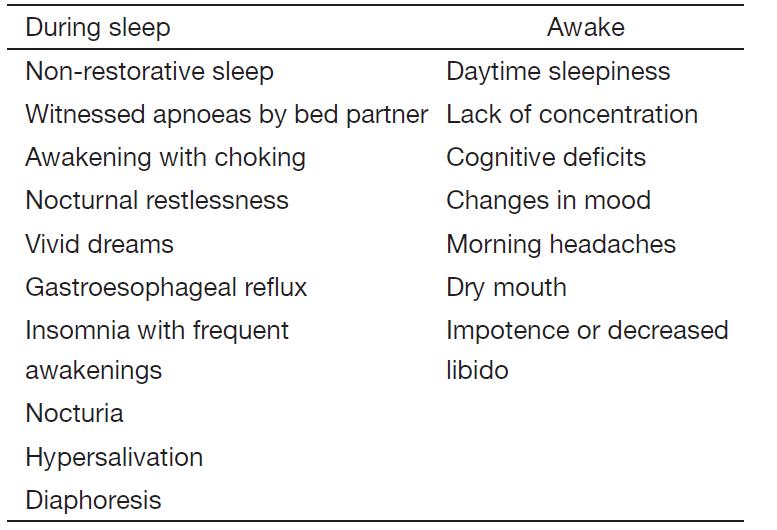
Sleep related breathing disorder • Central sleep apnea due to drug or substance • Primary sleep apnea of infancy • Obstructive sleep apnea • Sleep-related nonobstructive alveolar hypoventilation, idiopathic • Primary central sleep apnea • Central sleep apnea due to Cheyne Stokes breathing pattern • Central sleep apnea due to medical condition not Cheyne Stokes
Spectrum of sleep disorder breathing • Obesity-hypoventilation syndrome • Severe obstructive sleep apnea • Moderate obstructive sleep apnea • Mild obstructive sleep apnea • Upper airways resistance syndrome • Chronic, heavy snoring • Intermittent snoring • Quiet breathing
What is OSA?
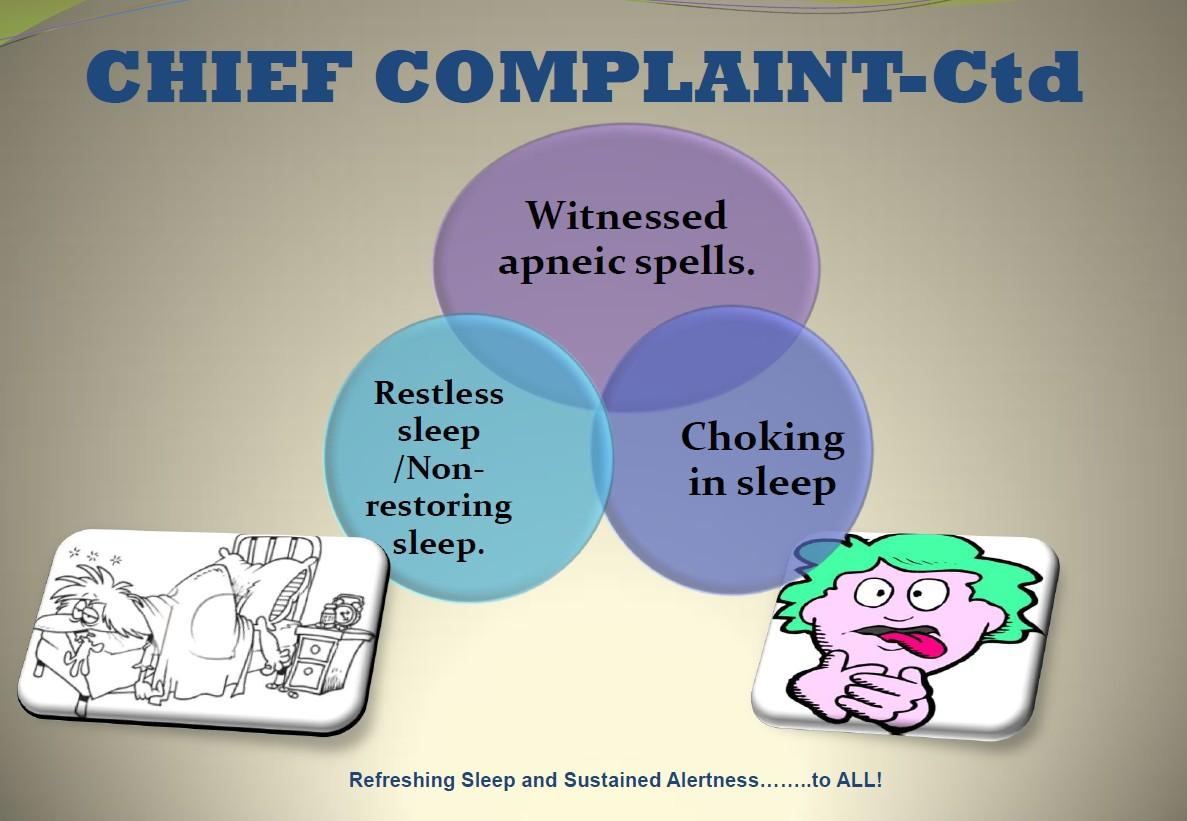
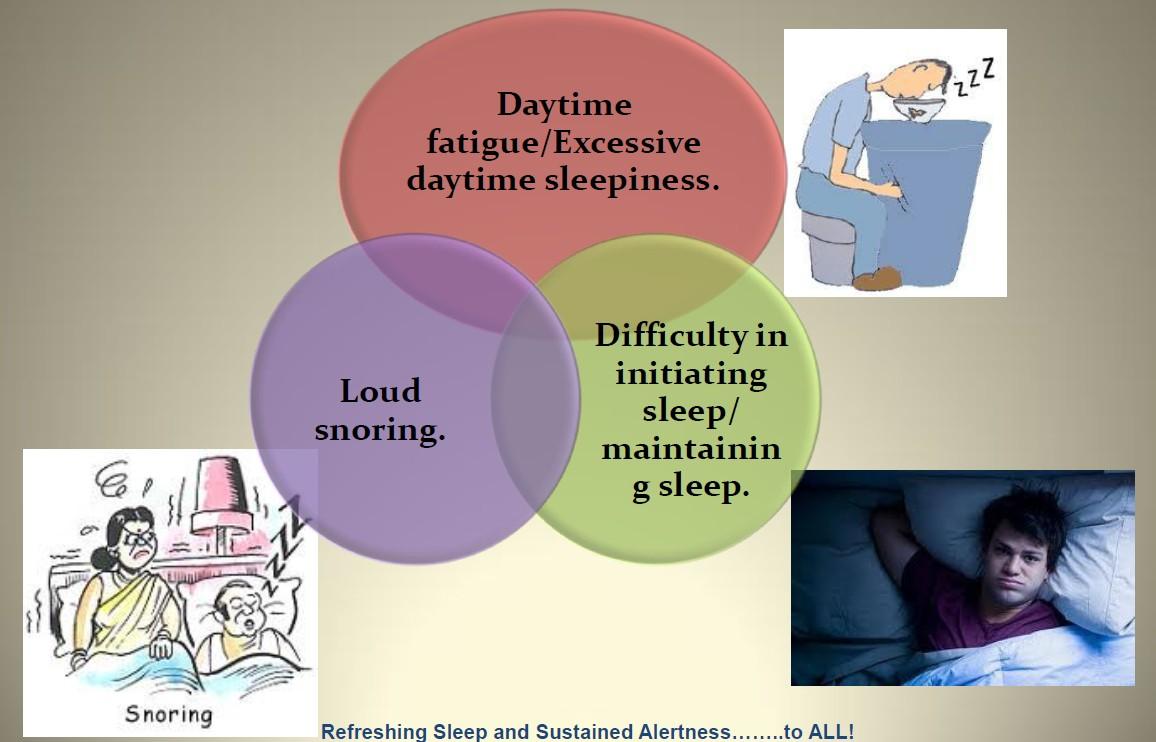
OSA is a syndrome characterized by frequent episodes of upper airway obstruction during sleep, associated with recurrent arousals, oxygen desaturation, and daytime symptoms
Pathophysiology
of OSA Interplay between three important factors • Anatomic Structural narrowing of airway • Neurologic Inadequate upper airway dilator muscle function • Mechanical Altered upper airway collapsibility

Veasey, CCNA 2003
Risk of Untreated OSA
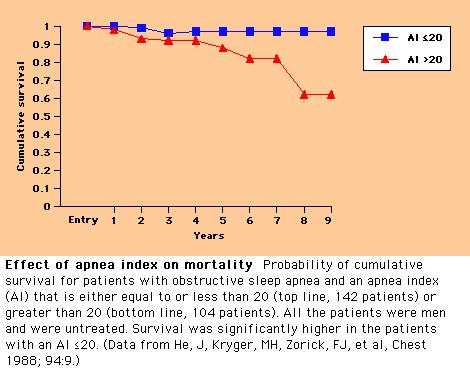
Primary events Secondary events Clinical consequences • Vibration of soft palate • Snoring • Pulmonary arterial vasoconstriction • Pulmonary hypertension • Right heart failure • Systemic arterial vasoconstriction • Systemic hypertension • Vagal bradycardia • Cardiac ischemia and irritiability • Cardiac arrhythmias • Sudden unexplained cardiac death • Cerebral vascular dilatation • Morning headache • Hypothalamic-pituitarytesticular dysfunction • Reduced libido • Impotence • Stimulation of erythropoeisis • Polycythemia • Cerebral impairment and/or damage • Excessive daytime sleepiness • Intellectual deterioration • Behavioural disorders • Sleep fragmentation • Loss of deep sleep • Excessive motor activity • Nocturnal “epilepsy” Sleep onset Upper airway narrowing Obstructive apnea ipO2,hpCO2,ipH Arousal from sleep Airflow resumption Return to sleep
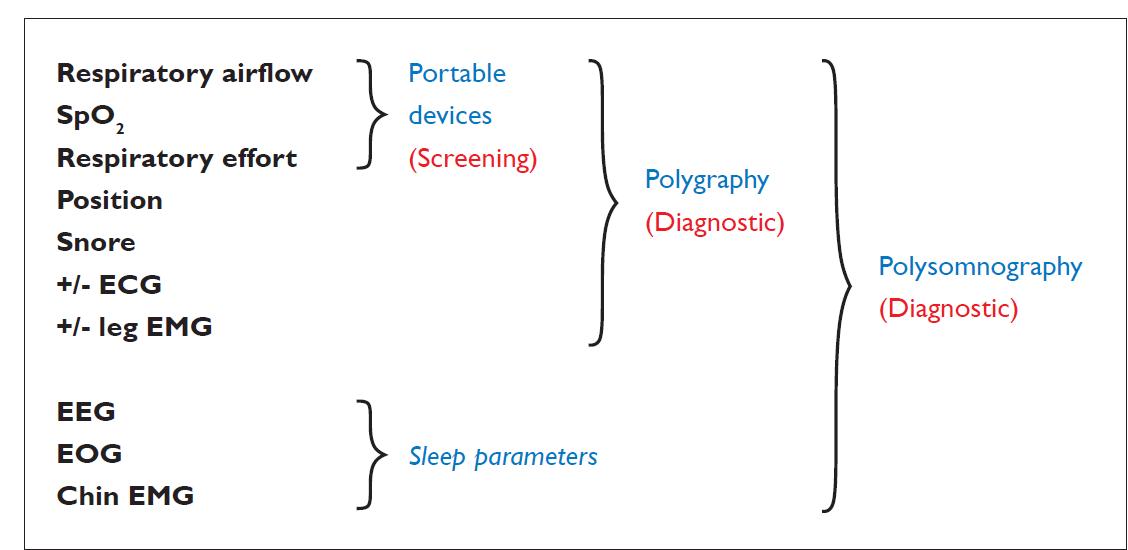
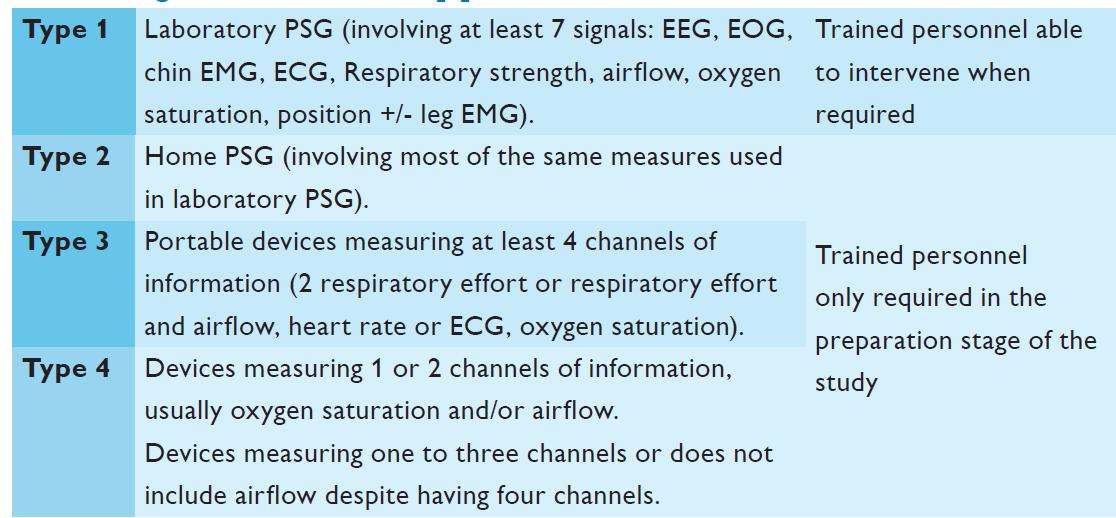
Sleep studies

Overnight
• Count number of respiratory events and divide by hours of sleep to generate AHI
polysomnography is the ‘gold standard’ for diagnosis of OSA
Sleep staging Oronasal Flow Snoring Rate, rhythm Respiratory effort Body position Leg movement SaO2 EEG EOG Flow sensor EMG Microphone ECG Thoracic Abdominal Position EMG Oximeter
Diagnosis
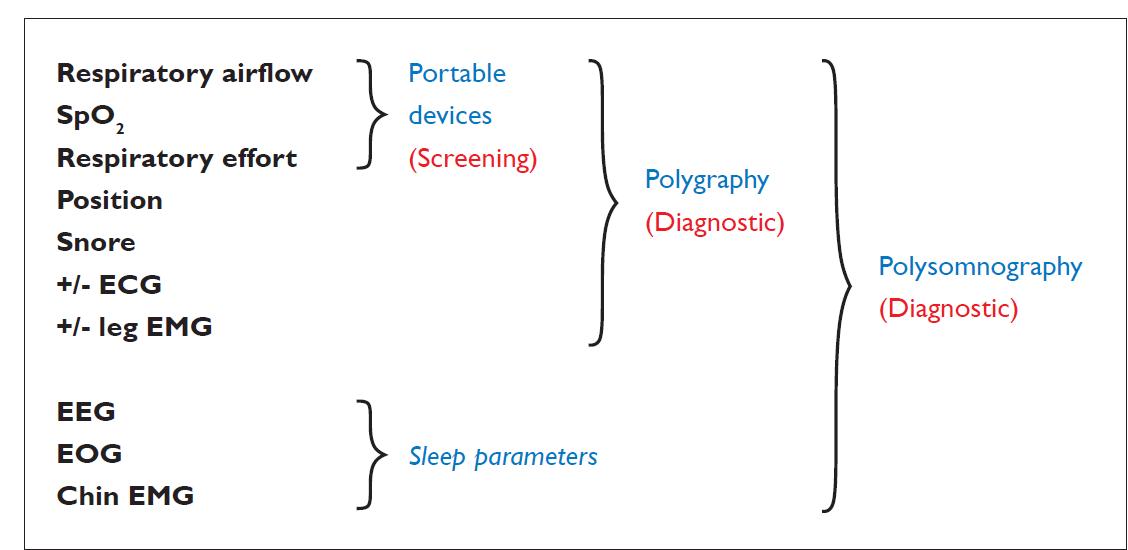
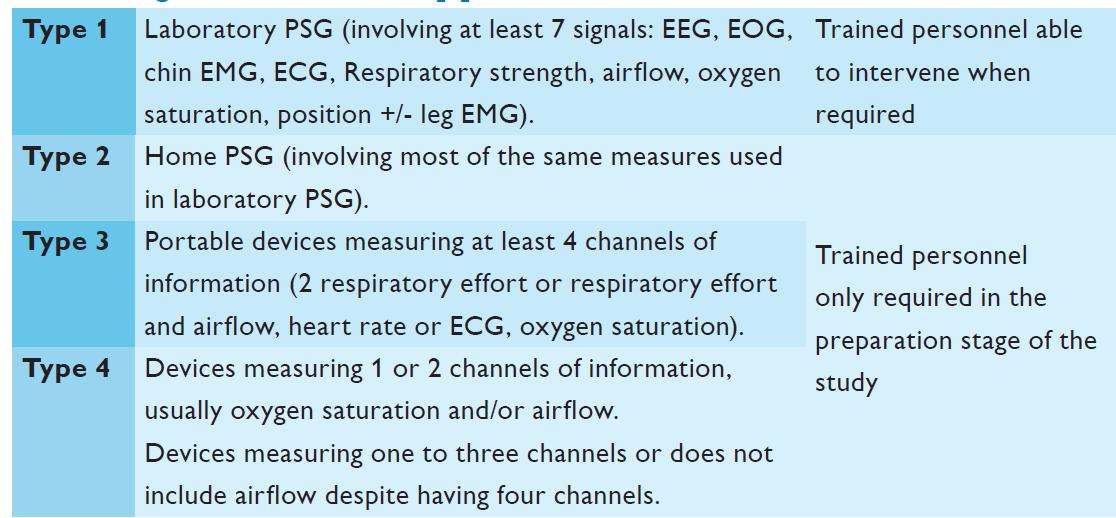
Types of PSG
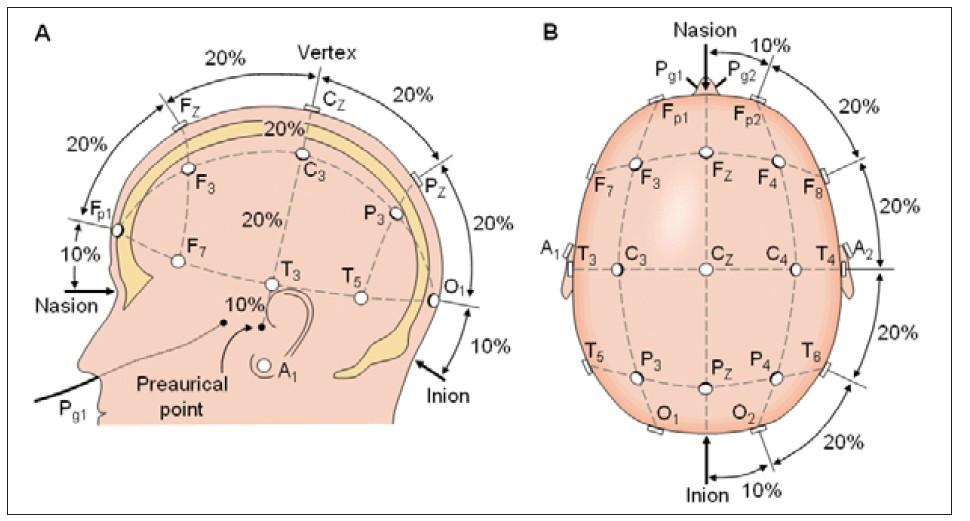
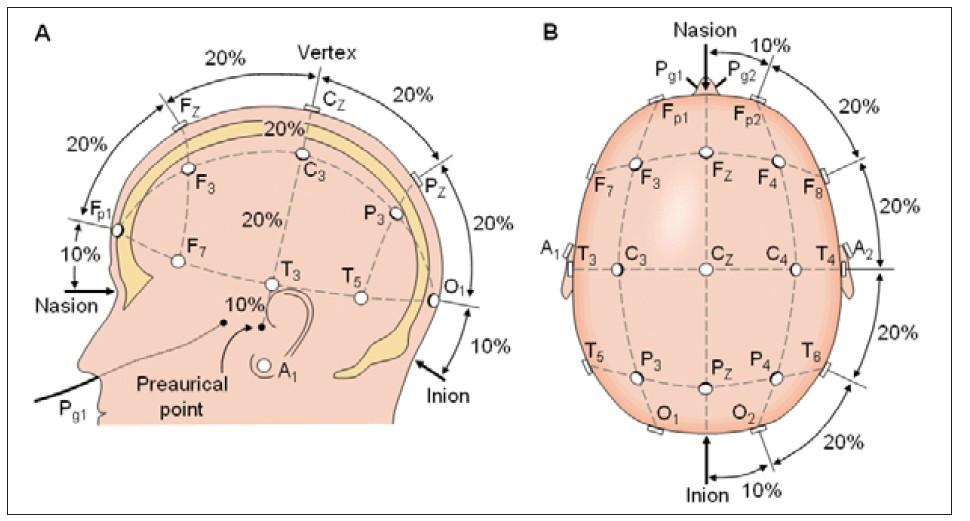
Potentials generated by the cerebral cortex

EEG
10-20 electrode placement
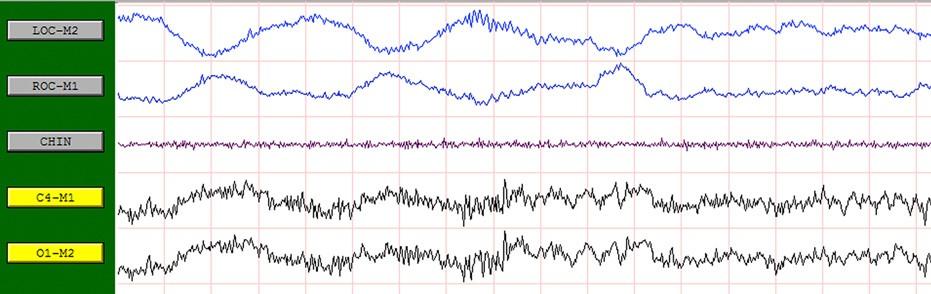
Sleep staging
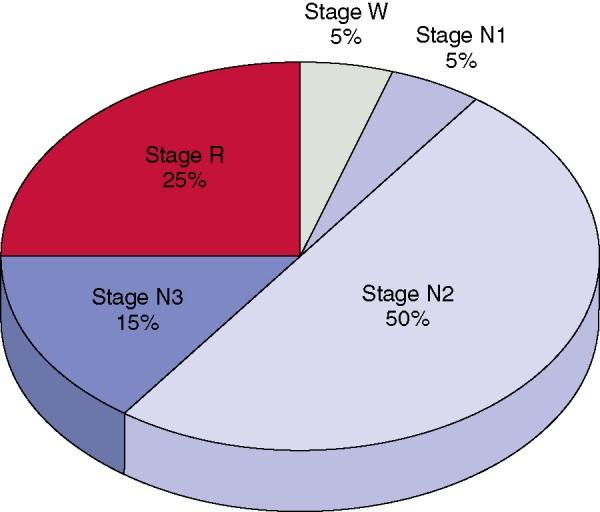
Rechtschaffen and Kales (R and K) 1967 stage W,N1-4 & R
AASM 2007stage W,N1-3 & R
•
•
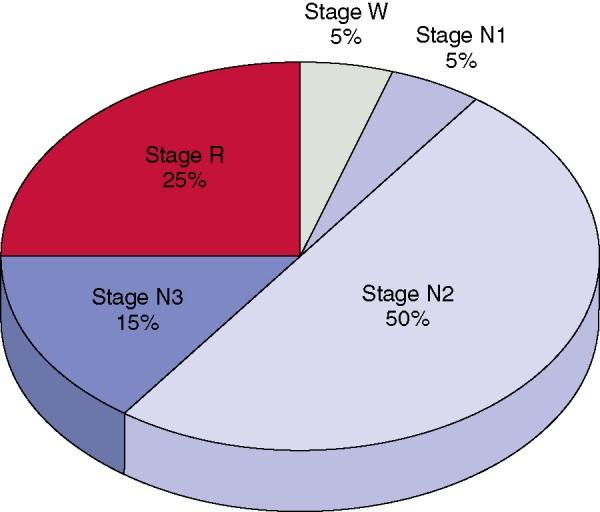
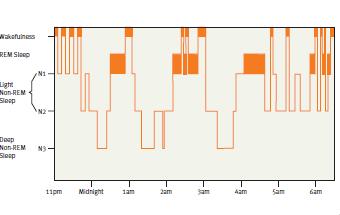
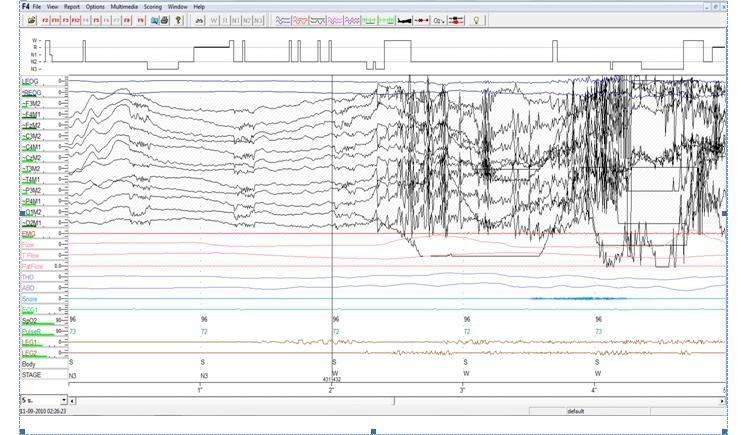
Hypnogram in normal adult
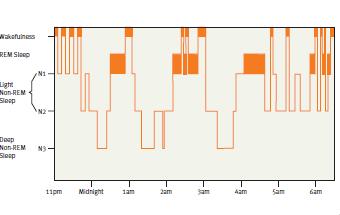
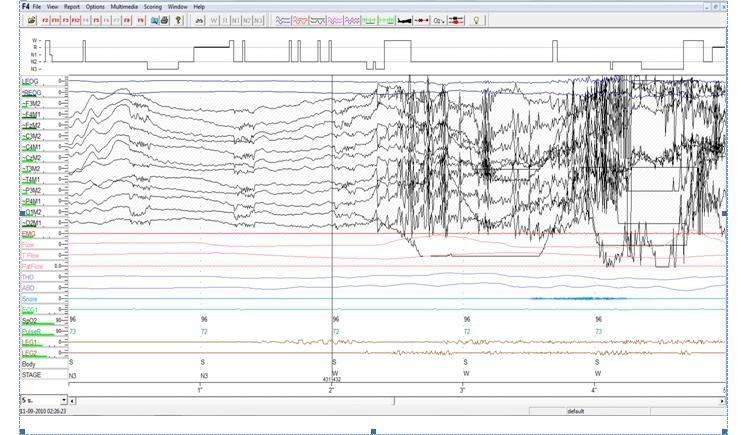
Hypnogram in OSA pt
Stage N3 N2 N1 R W 21:03:53 23:00 00:00 01:00 02:00 03:00 04:00 05:00 06:00
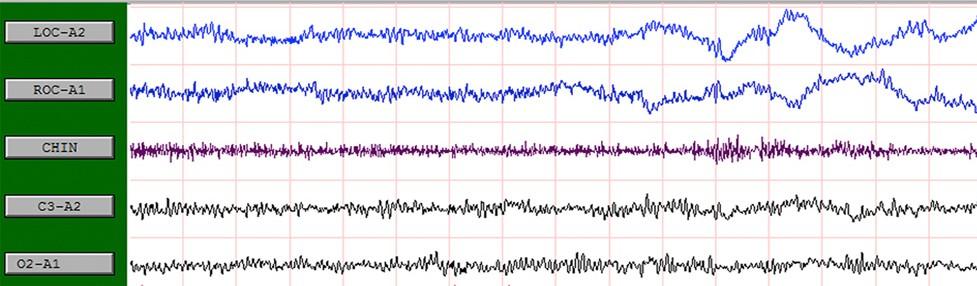
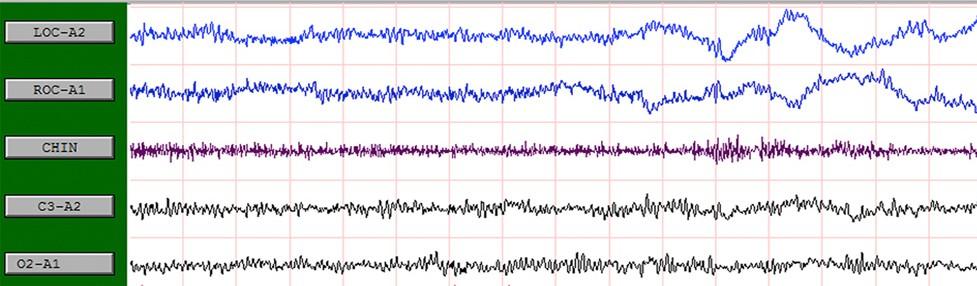
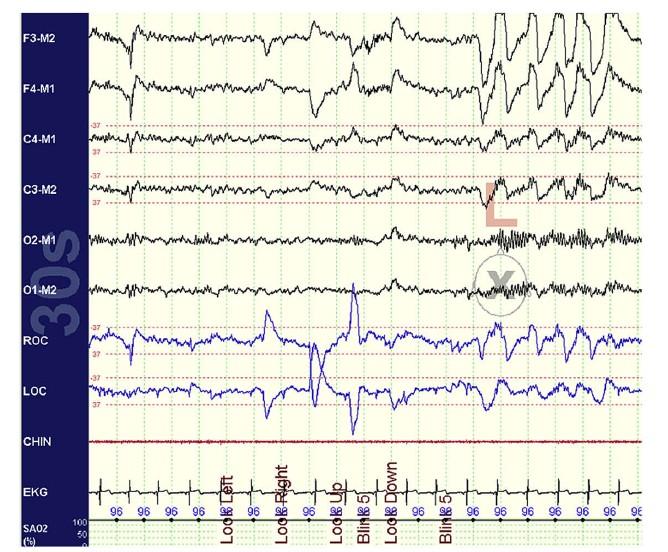
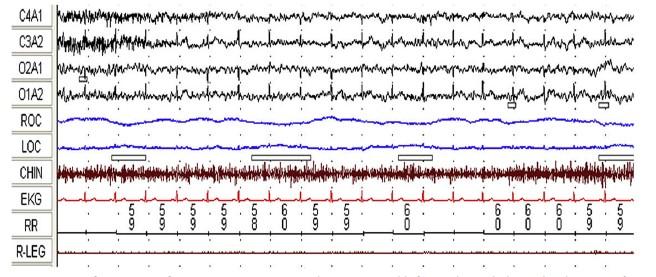
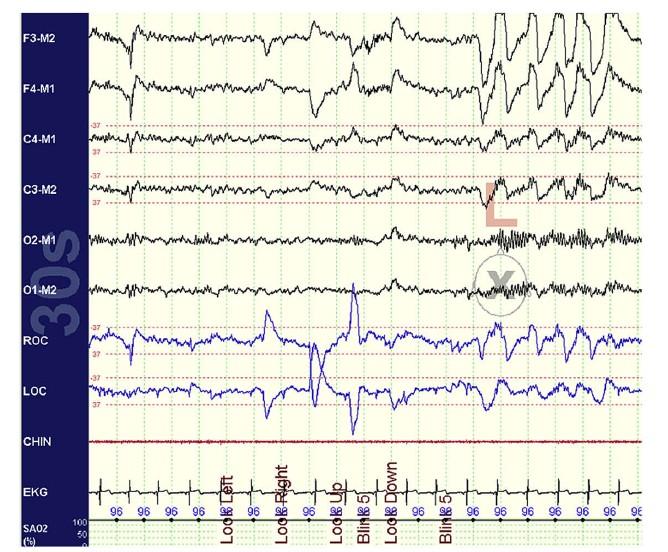
Awake Alpha rhythm-trains of sinusoidal 8-13 activity over occipital region ; attenuating with eye opening
Eye blinks- conjugate vertical eye movementsat a frequency of .5-2hz REM may be seen with initial deflection lasting < 500msec
Submental EMG - relatively high tone
NREM 1
slow eye movements: conjugate, regular , sinusoidal eye movement with initial deflection >500 msec
vertex sharp waves low amplitude 4-7 Hz/ mixed frequency activity
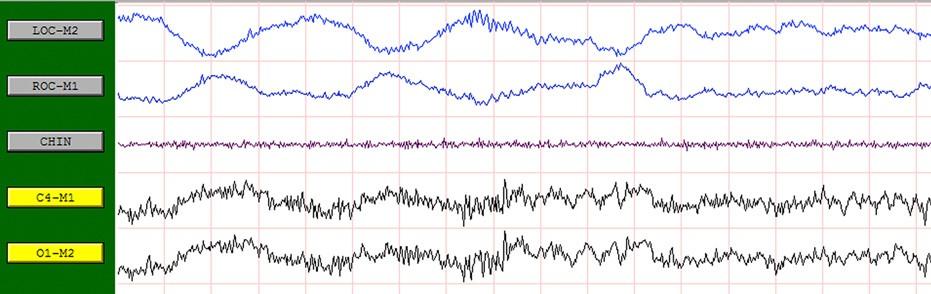
NREM 2

• • • • • • • •




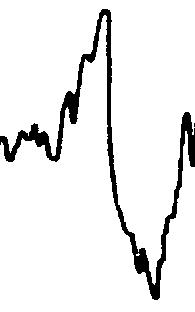
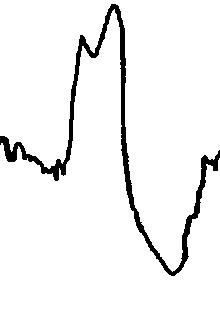
• Sharp, slow waves, with a negative then positive deflection • No amplitude criteria • >.5 second in duration • Central in origin
K Complexes K Complexes

NREM 3 •>20% Delta Activity ( .5-2 Hz with amplitude >75 uV)is seen over frontal region •no eye movements •EOG leads will only pick up the EEG activity •about thirty to forty five minutes after sleep onset •far more difficult to awaken
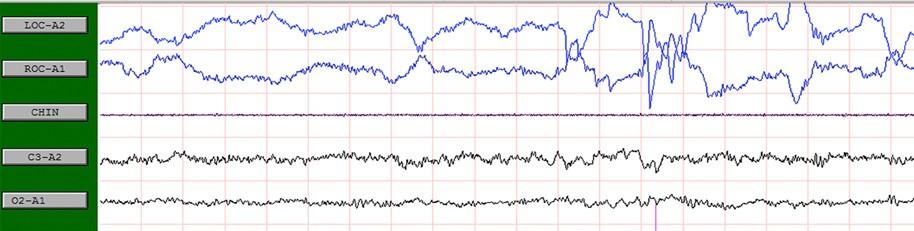
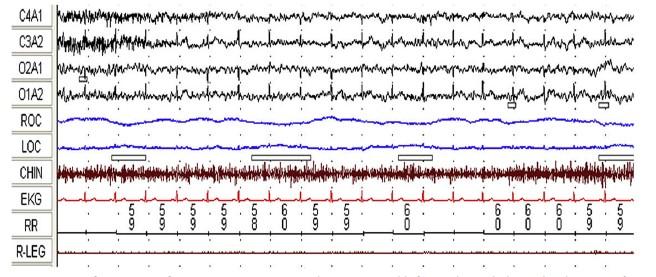
Stage R
•Brain suddenly becomes much more active.
•REM-conjugate, irregular, sharply peaked eye movements with initial deflection< 500 msec
•Low chin EMG activity
•Sawtooth waves- low amplitide sharply contoured or triangular (26hz); over central head regions
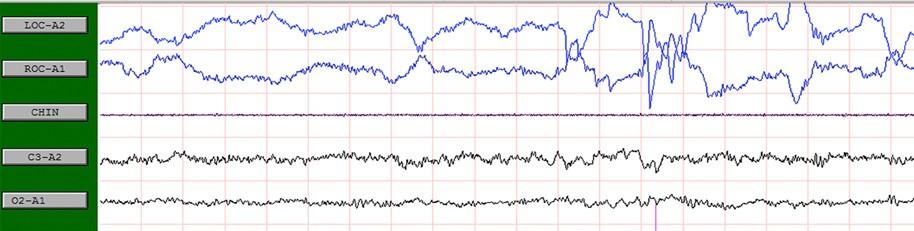
• E1 • M1 • M2 • E2 • CHIN EMG
EOG and EMG Placements
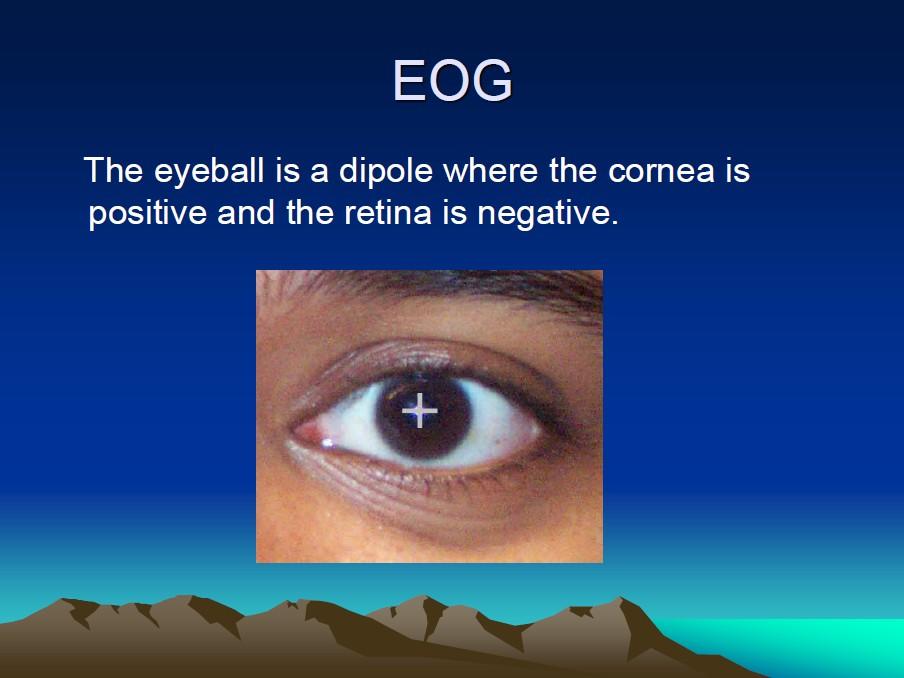
Corneoretinal potential
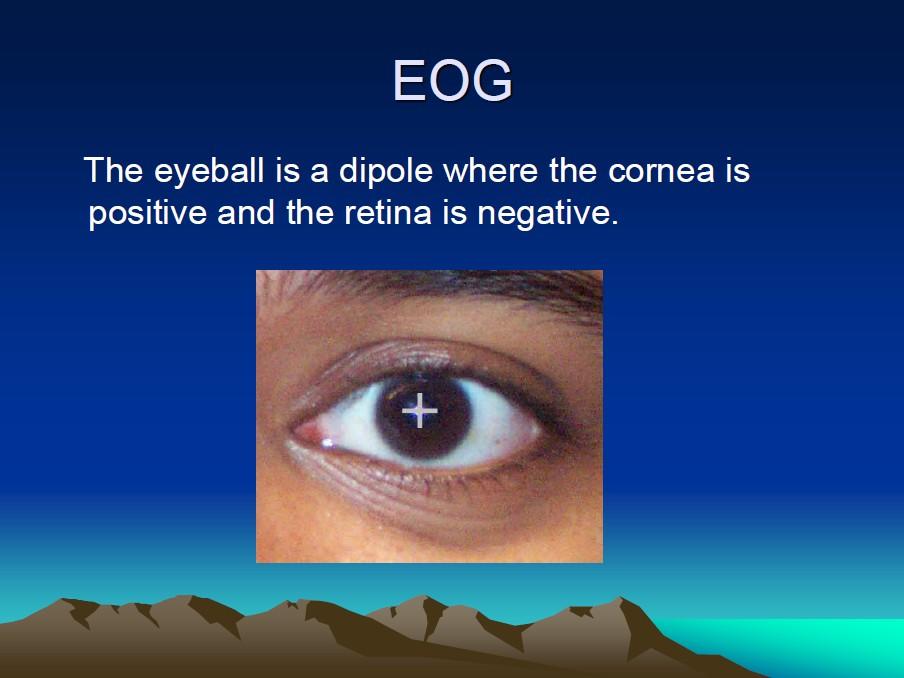
EMG placement

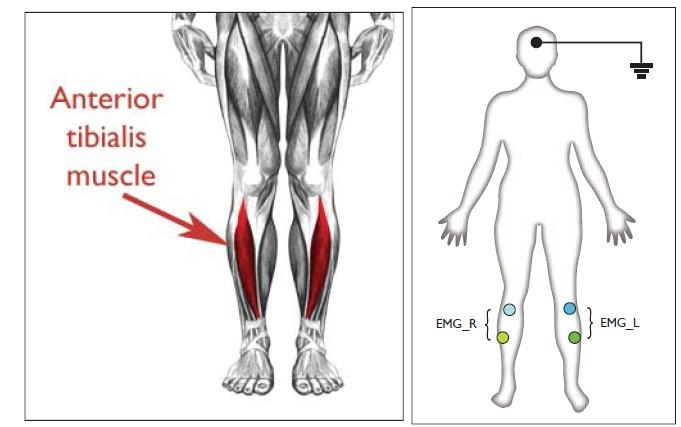
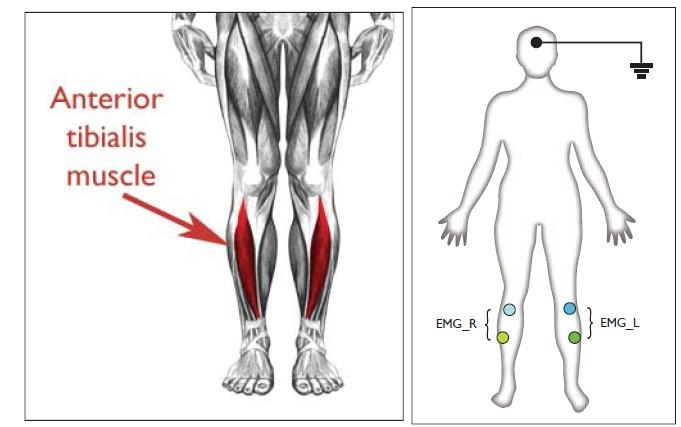
Leg EMG
Position sensor

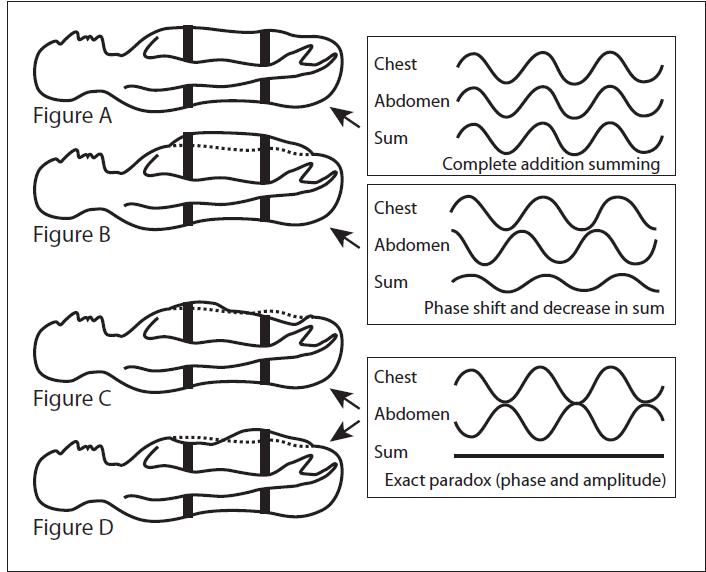
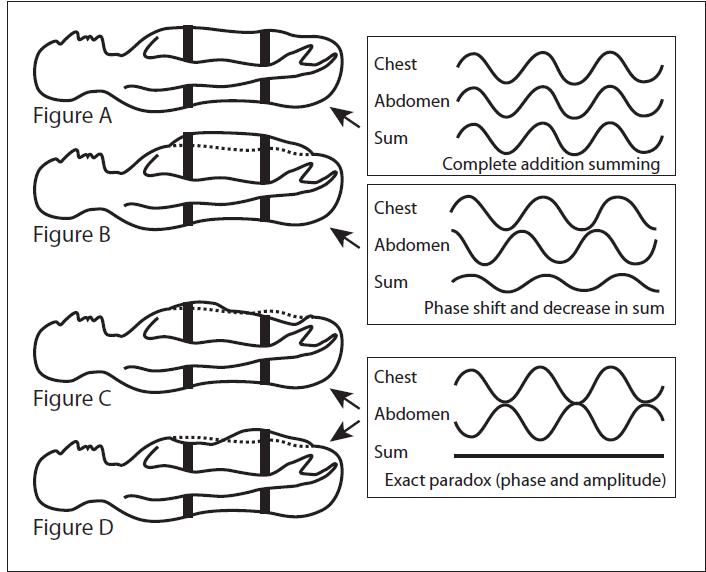
Thoraco-abdominal movements
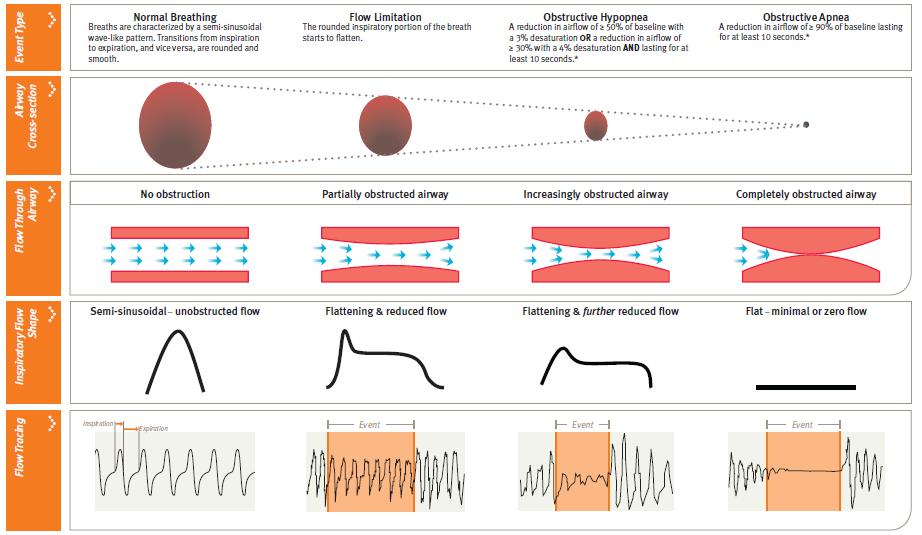
Flow tracing
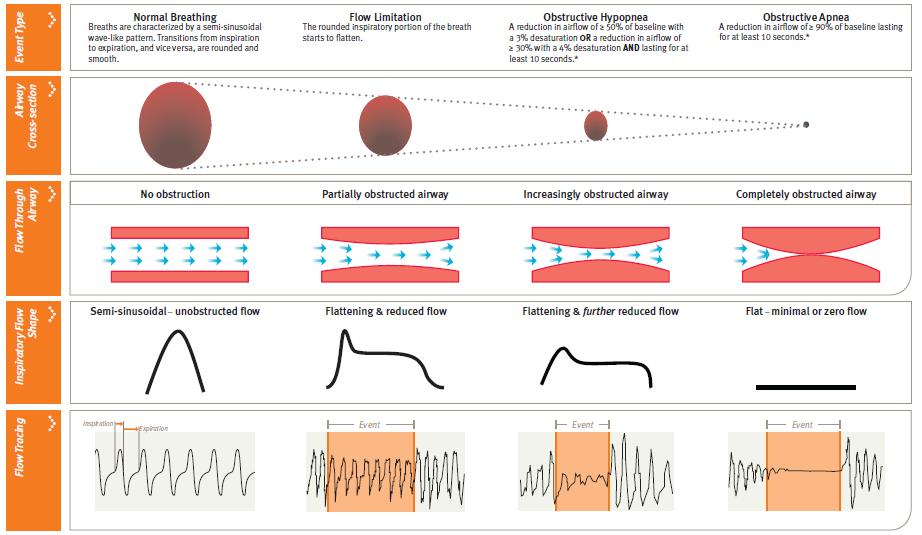
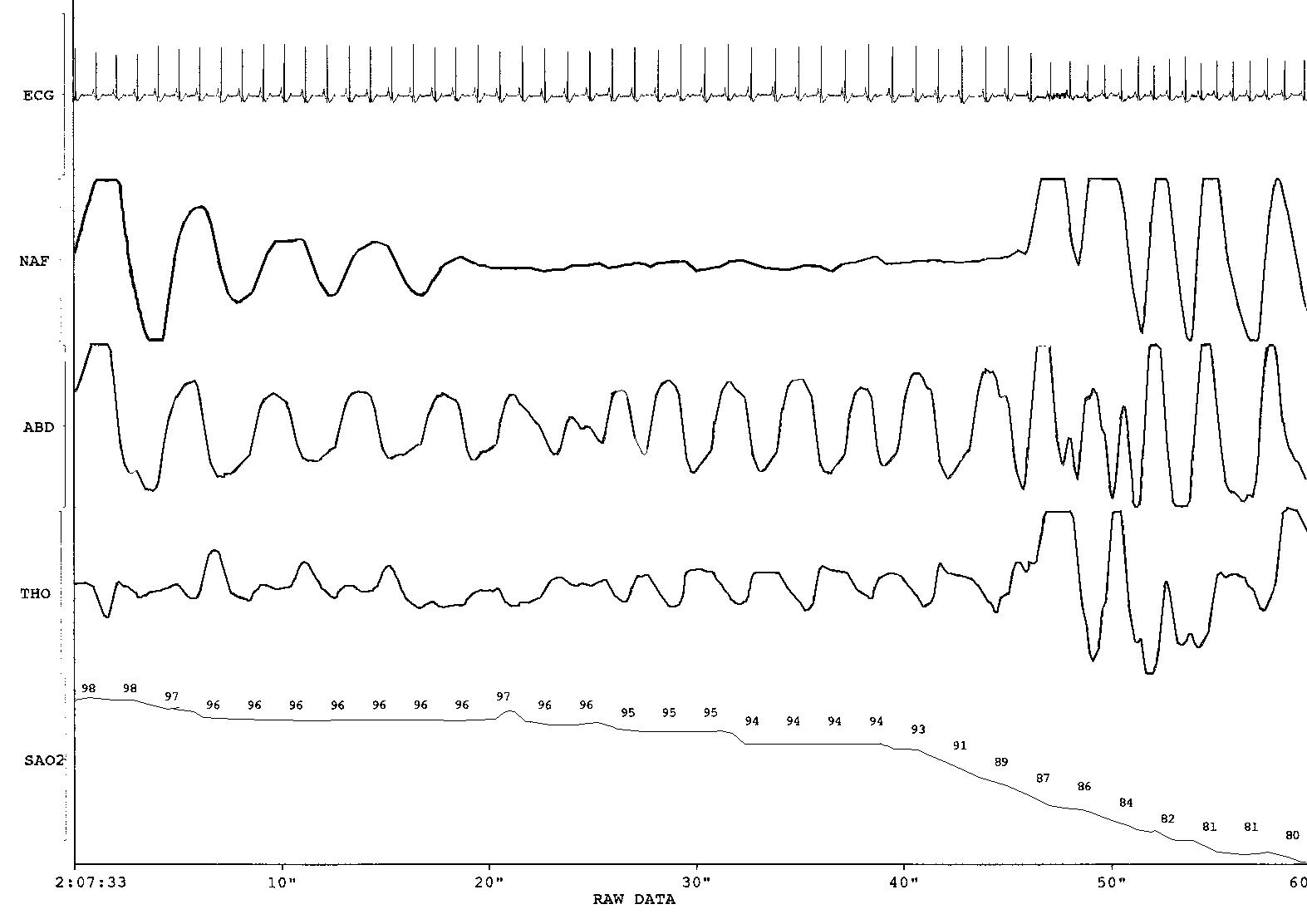
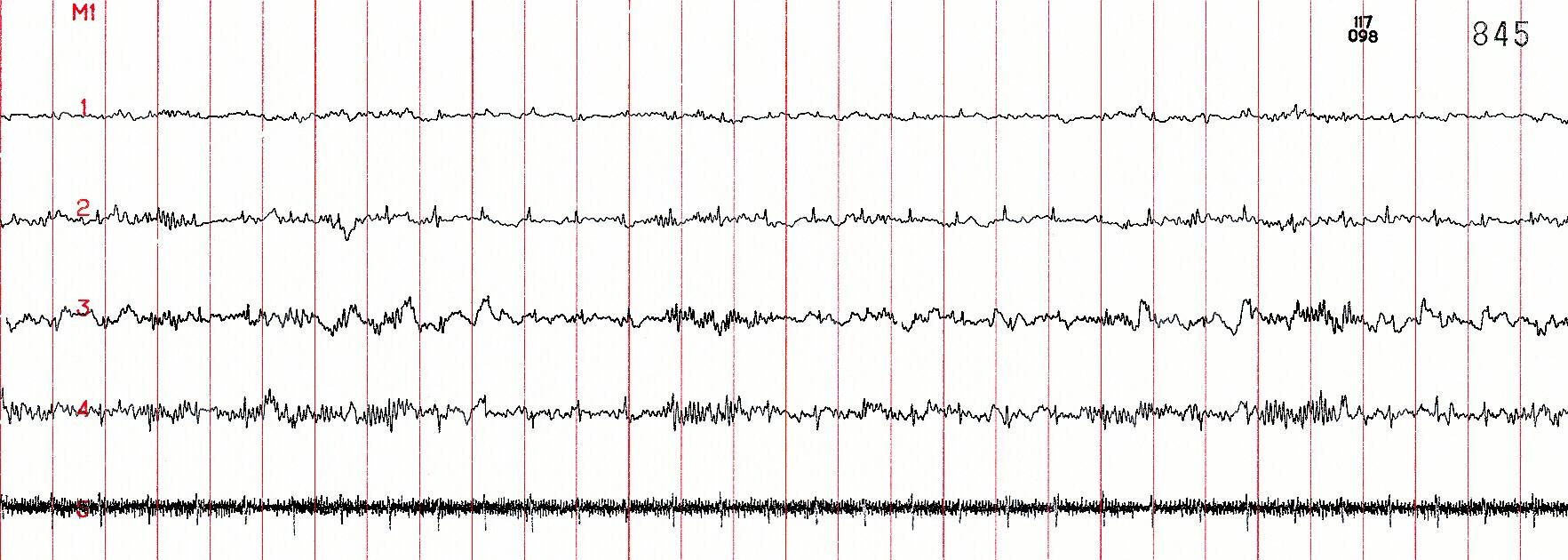
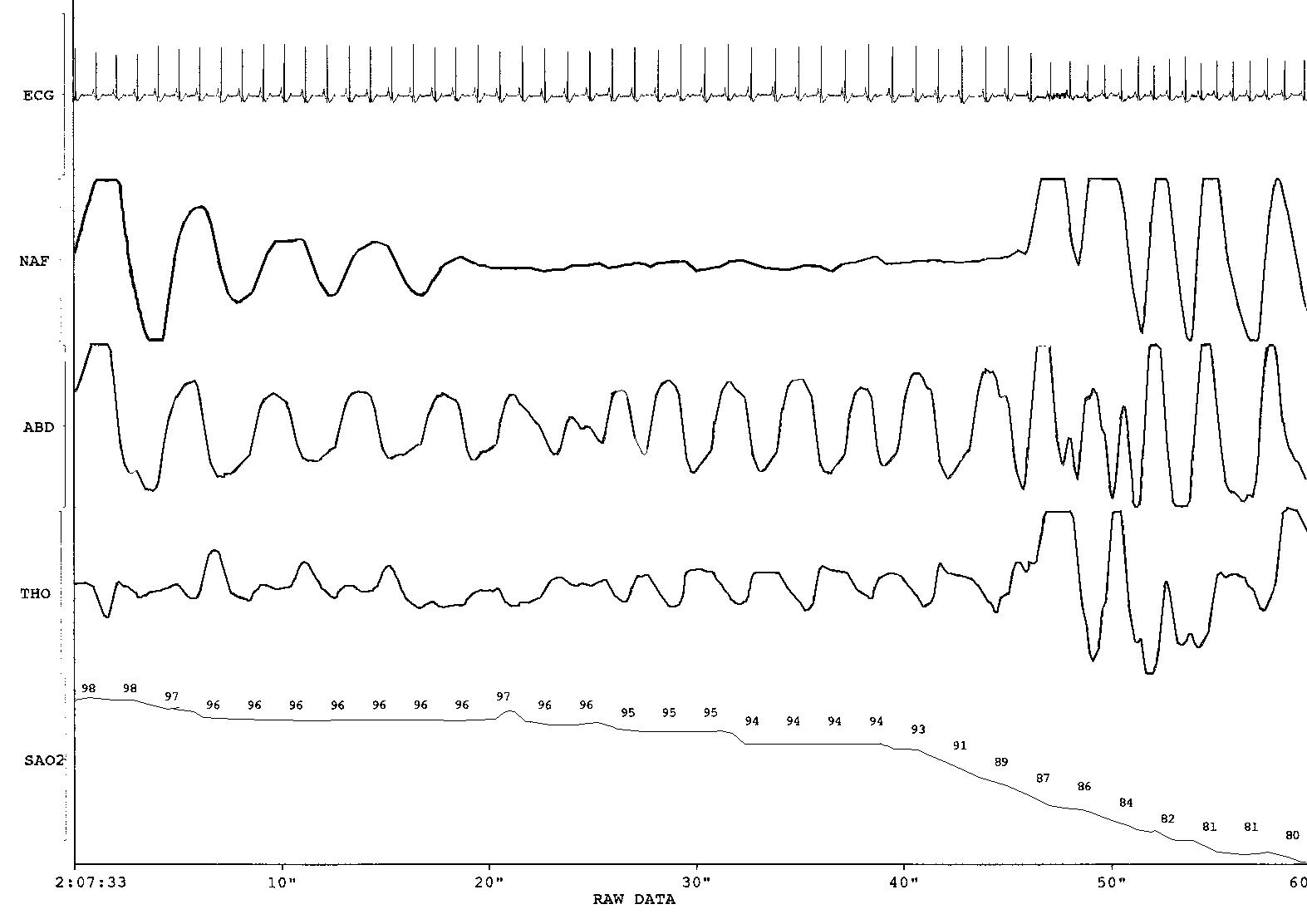
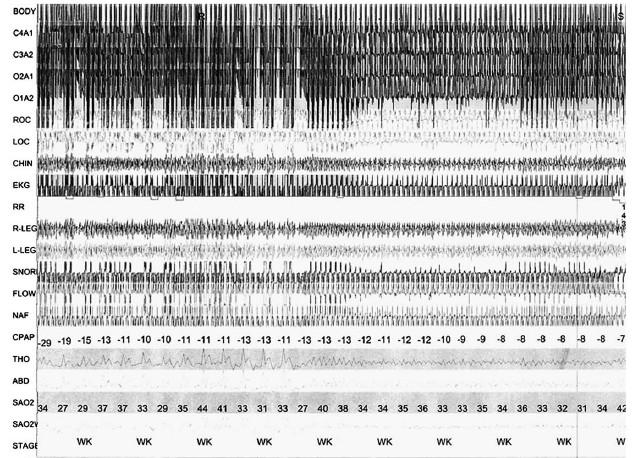
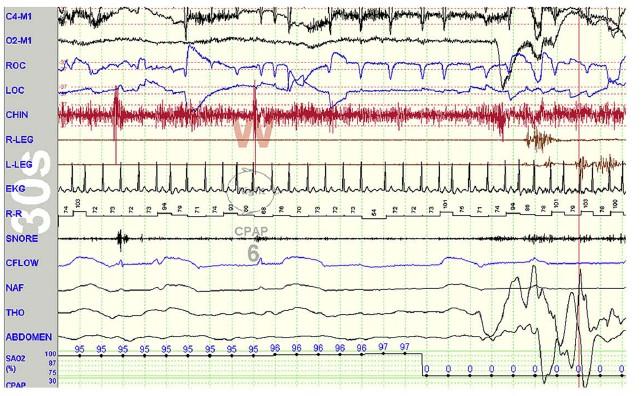
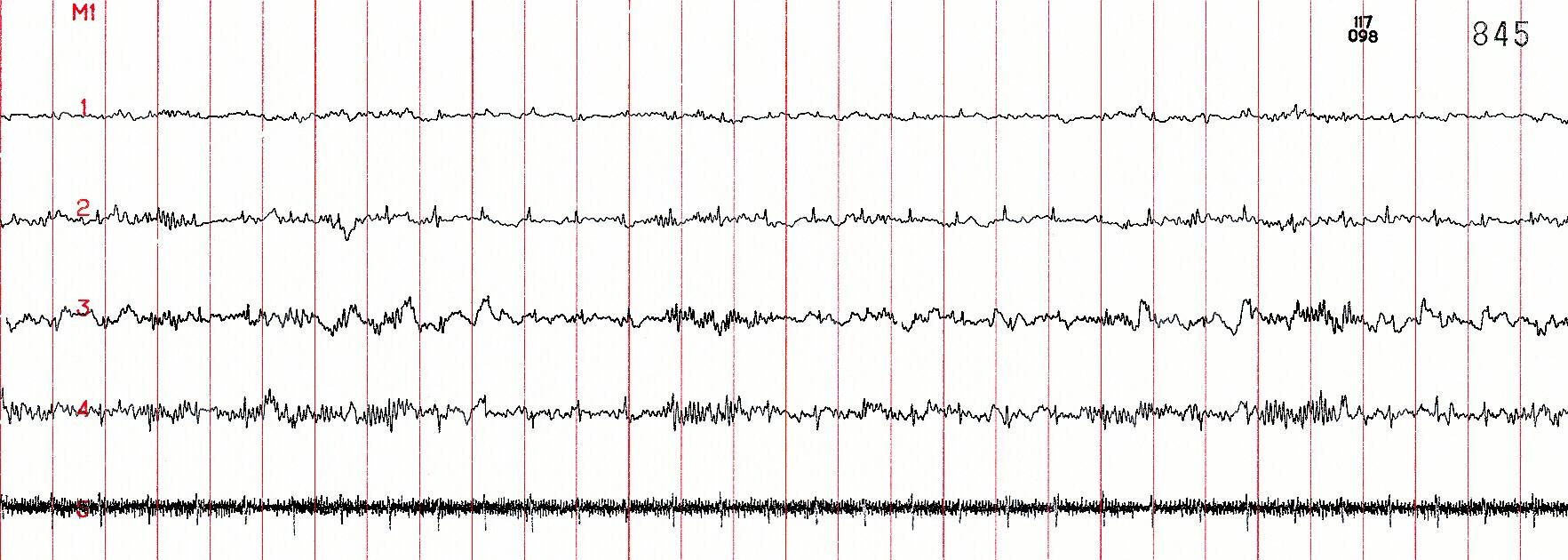
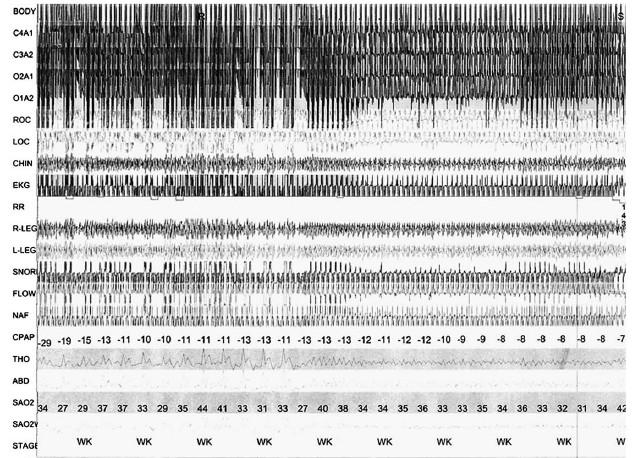
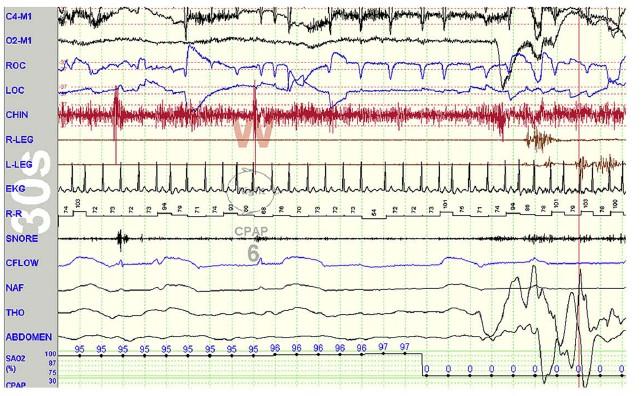
Obstructive Apnea A complete blockage of the airway despite efforts to breath. Notice the effort gradually increasing ending in airway opening. Blood oxygen levels reduce to < 3% of basline value Inhal e Exhal e Airway obstructs Airway opens Paradoxi ng Paradoxing Ends EKG Airflow Thoraci c effort Abd. effort SAO2 Effort gradually increases
Abd. Effor t
SAO
SAO

Central
Apnea Airflo 2
w Airflo w Thor. Effor t 2
Thor. Effor t Abd. Effor t
ECGECG
Airflow
Thoracic Effort
Abdominal Effort SAO2

EKG
Inhale
Exhale
> effort with paradox Paradox ends
Airflow reduction SAO2 desaturation
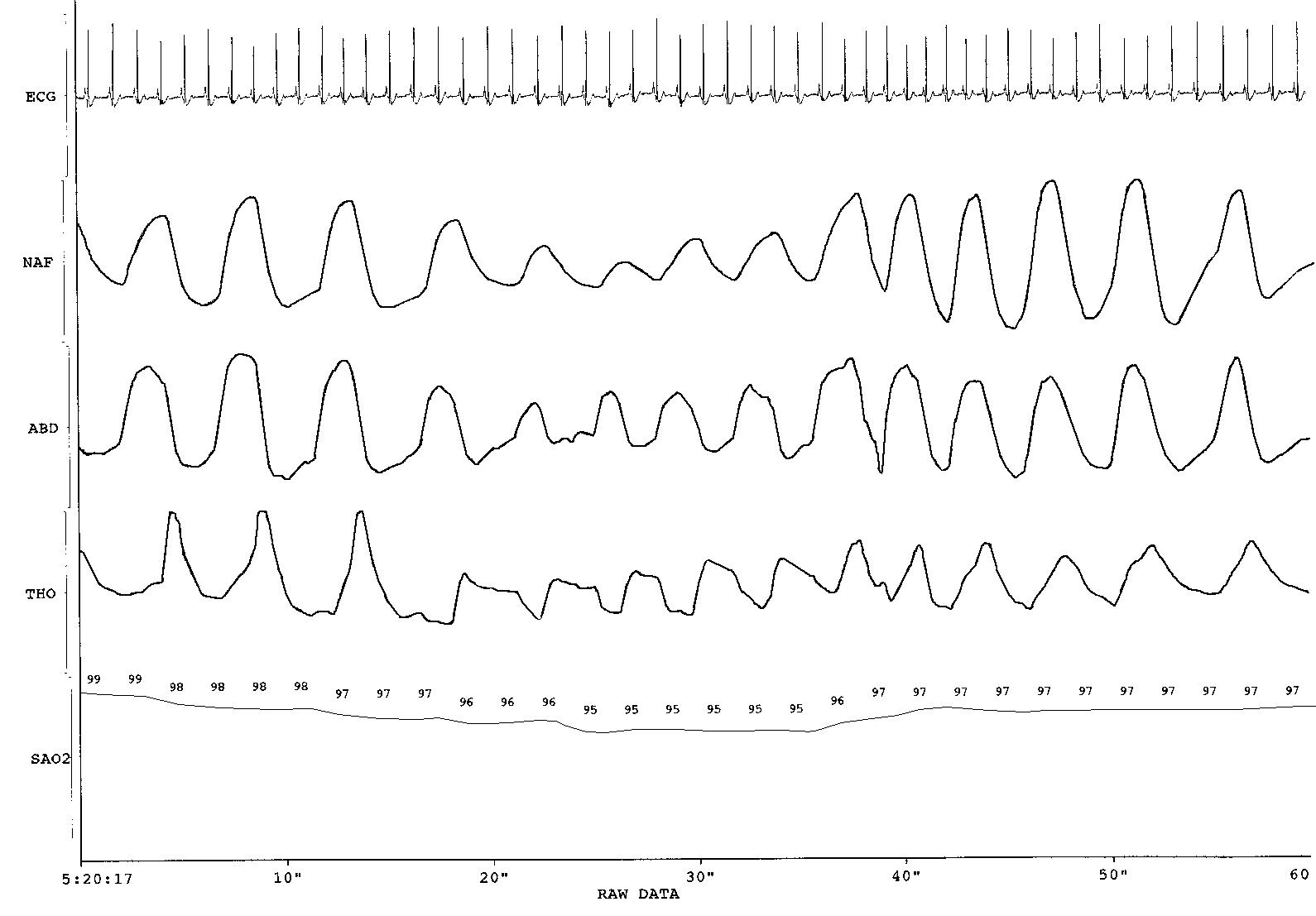
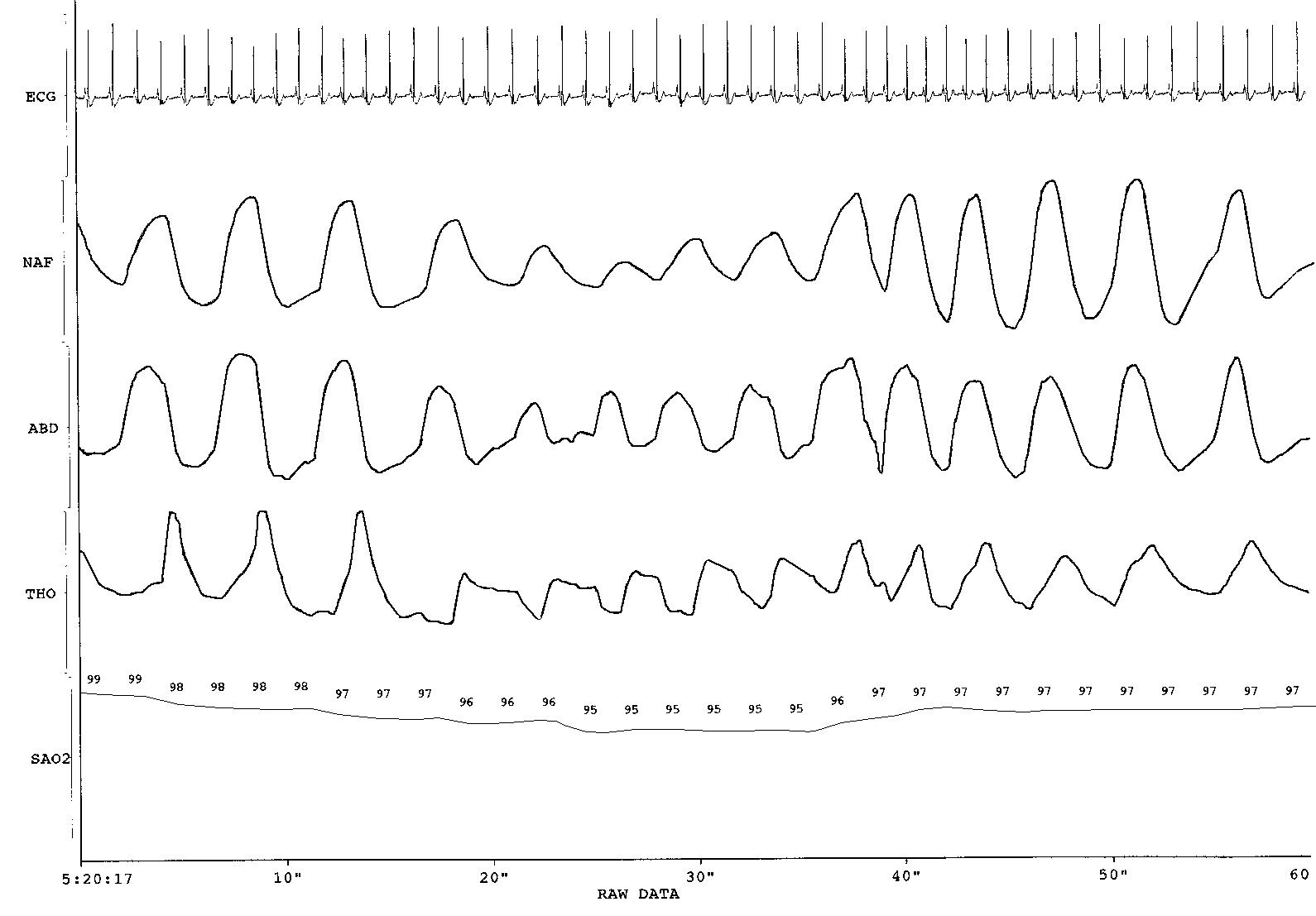
Hypopnea This is an 18 second hypopneic event. The airflow signal is reduced by approximately 50% during this event.
Scoring SDB Severity Mild Moderate Severe AHI 5-15 15-30 >30 RDI 15-20 20-40 >40
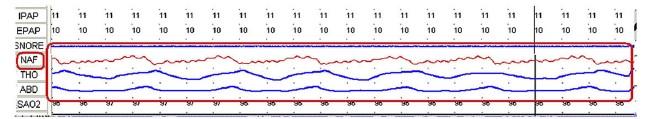
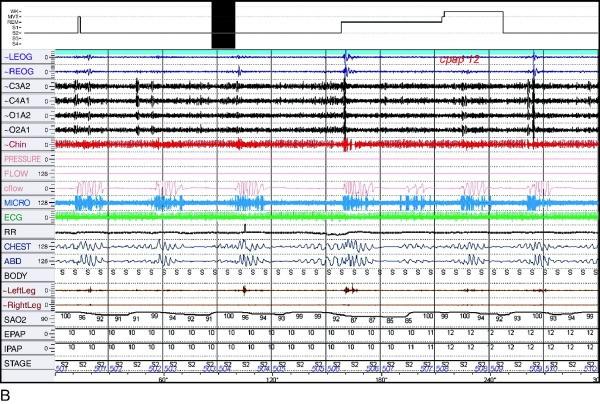
OSA Treatment: CPAP


5 Questions to Monitor CPAP • Snoring despite CPAP? • Weight change since CPAP started? • When was equipment last checked? • Still symptomatic? • Problems?
CPAP Compliance -Widely variable rates 50-70% overall –-Probably need >4 hrs. nightly for response –-Compliance determined early on
CPAP Compliance • Man or Machine? – Man • -Monitoring- Compliance feedback • -Education/Reassurance/Reevaluation • -Partner involvement – Machine • -Humidification- Warm Vs. Cold • -Mask- Nasal Pillows, Full Face, Other • -Blower- Bi-level, Auto-titration • Berry RB. Sleep Med (1): 175; 2000
• Auto-CPAP offers no benefit over fixed CPAP in terms of efficacy on the AHI
• It has not been established that unattended auto-CPAP titration is safe without a previous diagnostic PSG
• Some, but not all, studies indicate auto-CPAP results in a lower cumulative CPAP level. However, the importance of the amount of applied pressure on CPAP adherence is not consistently demonstrated
• Auto-CPAP has variable effects on adherence
Practice points: Auto-Adjusting CPAP
OSA Treatment: Surgery • Laser-assisted uvulopalatoplasty (LAUP) – AASM: not advised for OSA • Uvulopalatopharyngoplasty (UPPP) – 40% patients achieve AHI < 5 • Somnoplasty or Radiofrequency volumetric tissue reduction (RFVTR) – Role has yet to be fully defined • Maxillofacial surgery – Infrequently performed, but can be very effective
Radiofrequency Ablation

-Programmable levels of radiofrequency energy delivered by a proprietary disposable device into upper airway structures causing tissue necrosis and fibrosis -Less painful; ambulatory procedure -Unlikely to be singularly effective for most OSA -May be effective in combination procedures -Minimal peer-reviewed data
Oral Appliances



Tongue advancing device

Sleep related disorders in other specialities

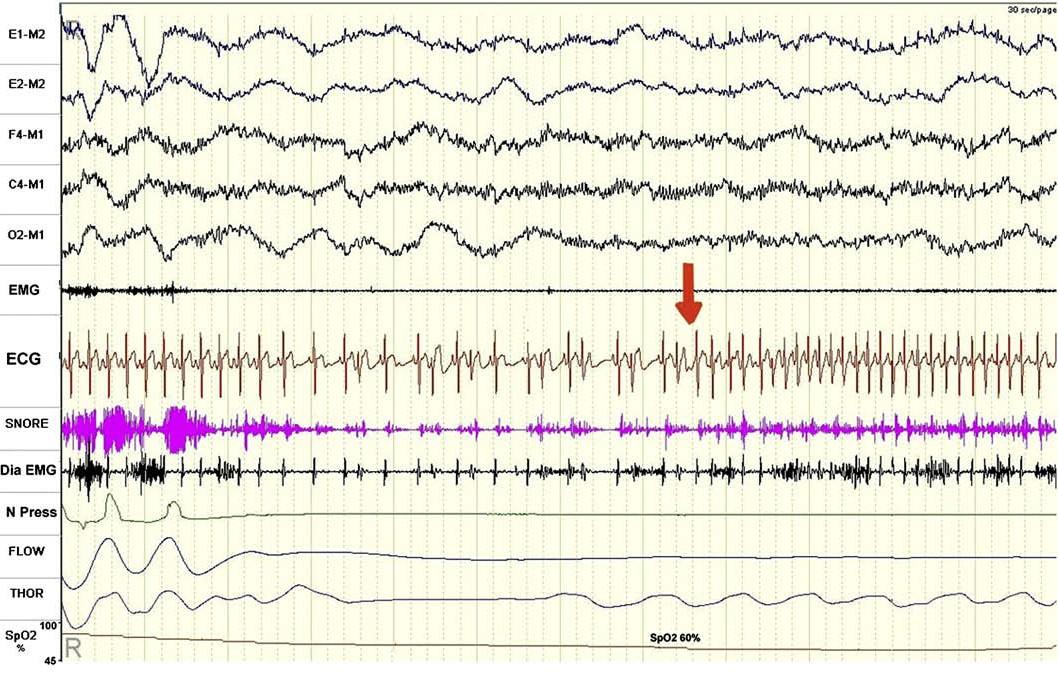
VPC, tachycardia in OSA pt
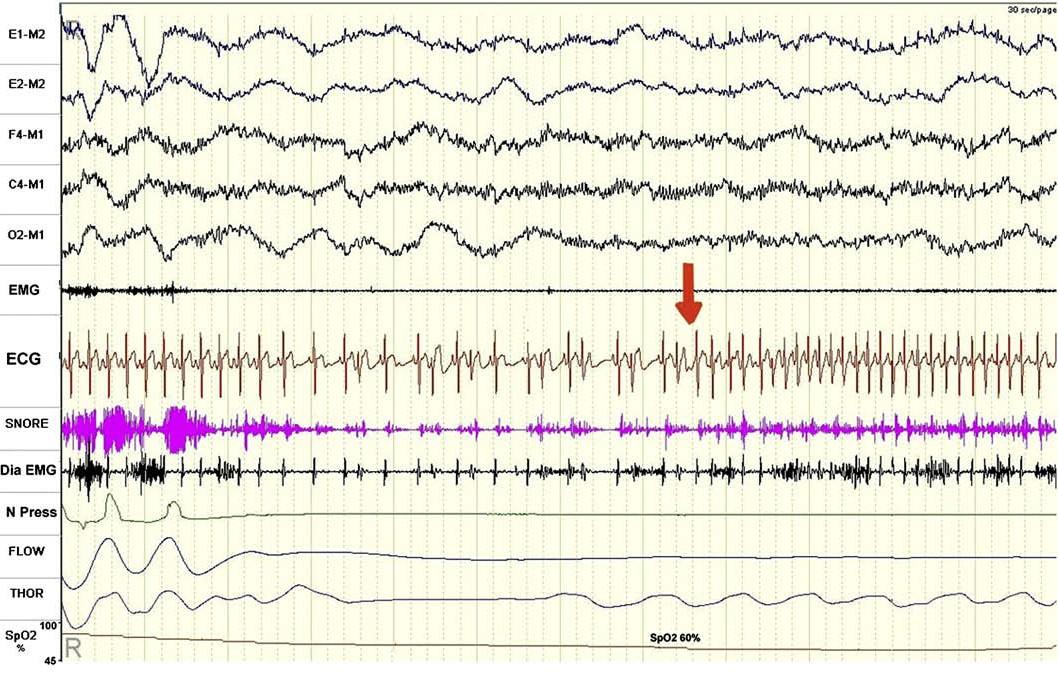
After CPAP


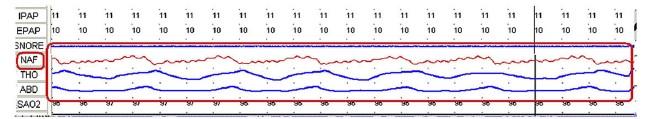
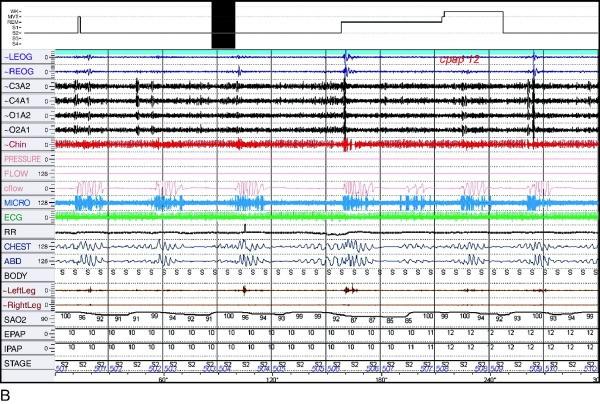
CSR • If there is at least 3 consecutive cycles of cyclical crescendo and decrescendo change in breathing amplitude • + atleast one of the below : 1. 5 or more central apnea / hypopnea per hr of sleep. 2. The cyclic cresendo and decresendo change in breathing amplitude has a duration of atleast 10 consecutive mins. CSR has variable cycle length that is most commonly in the range of 60 seconds.
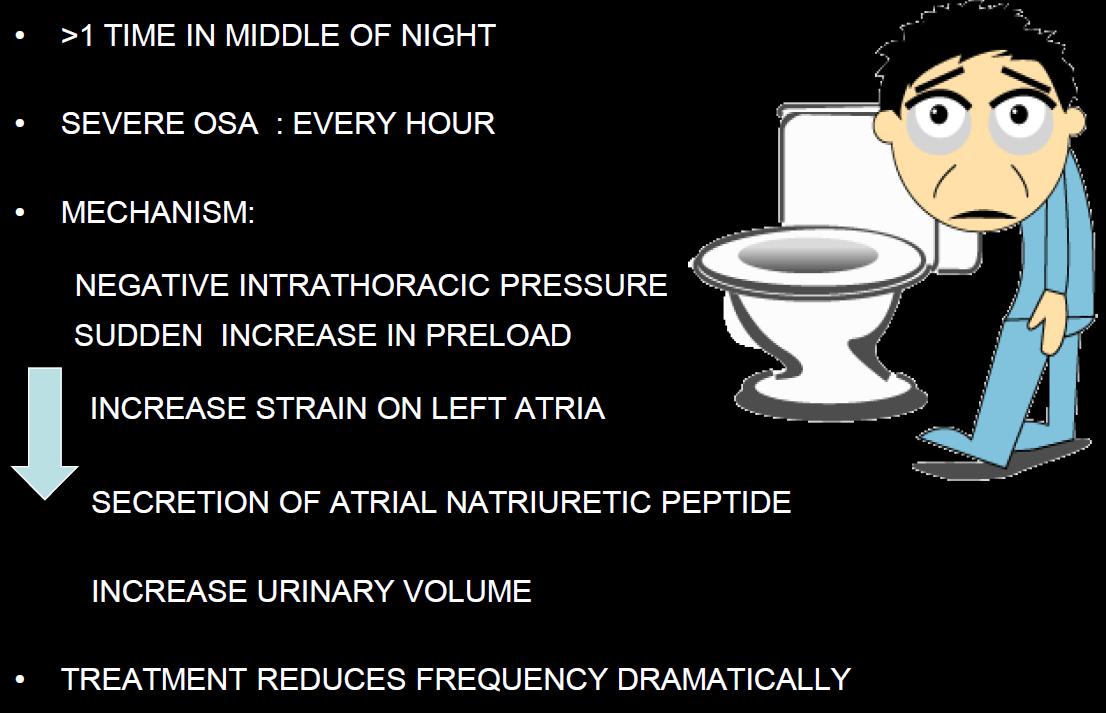
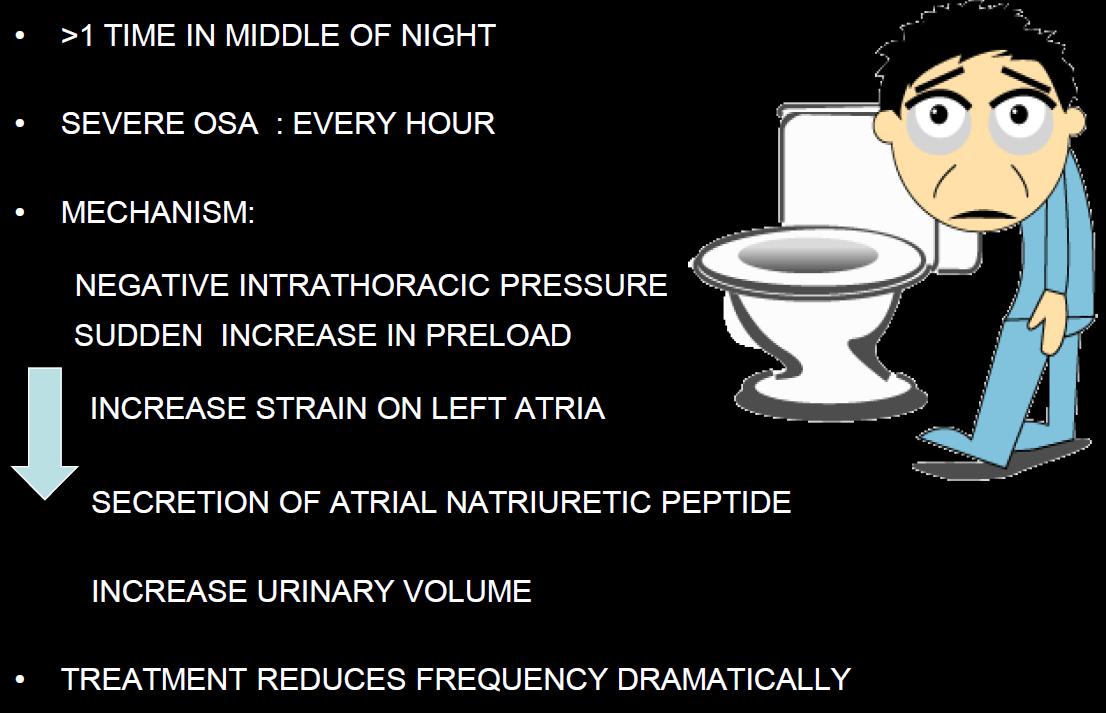
Nocturia
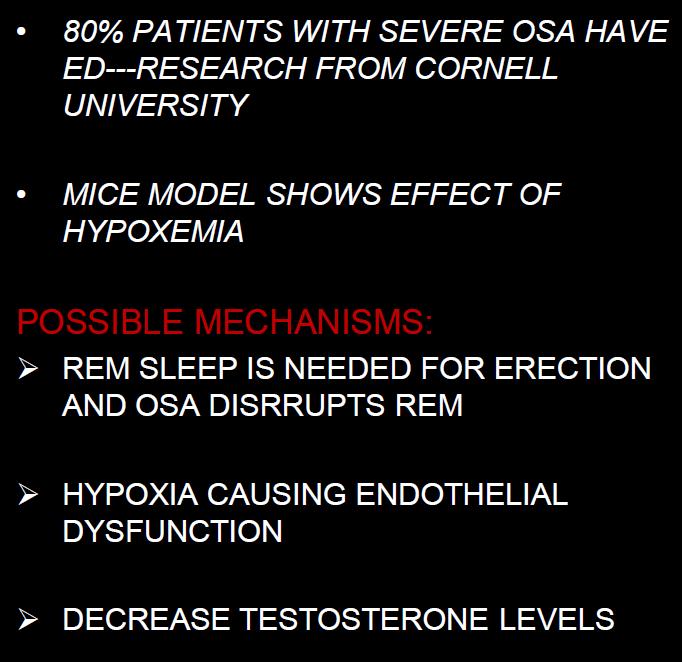
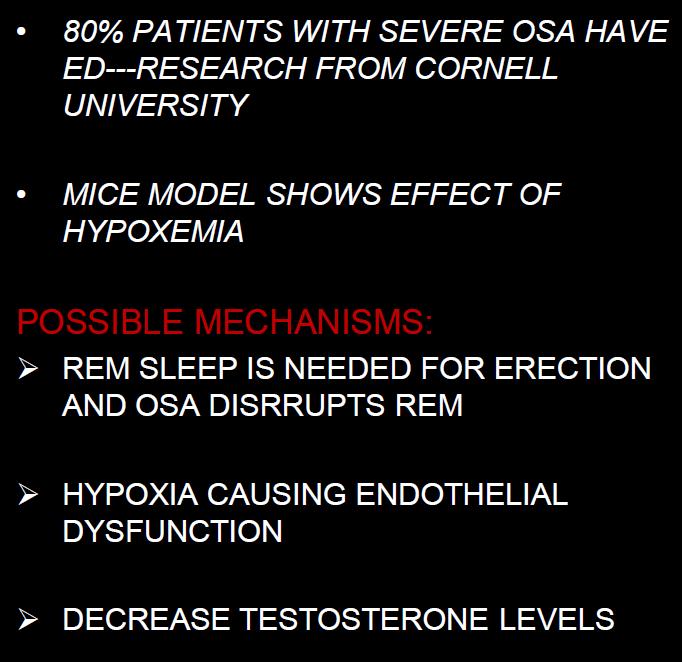
Erectile dysfunction




ADHD
Depression
Bipolar disorders
Alcoholism
PTSD
• Psychiatry –
–
–
–
–
•
–
•
–
Gastro
GERD
Dental
Bruxism
1. Artifacts 2. Misdiagnosis 3. Superadded apnoea 4. Inadequate relief
Pitfalls
POPPING ARTIFACT

MOISTURE ARTIFACT
Equipment malfunction
Oximetry probe malfunction
ECG artifact
Eye movement artifact
Complex sleep apnea
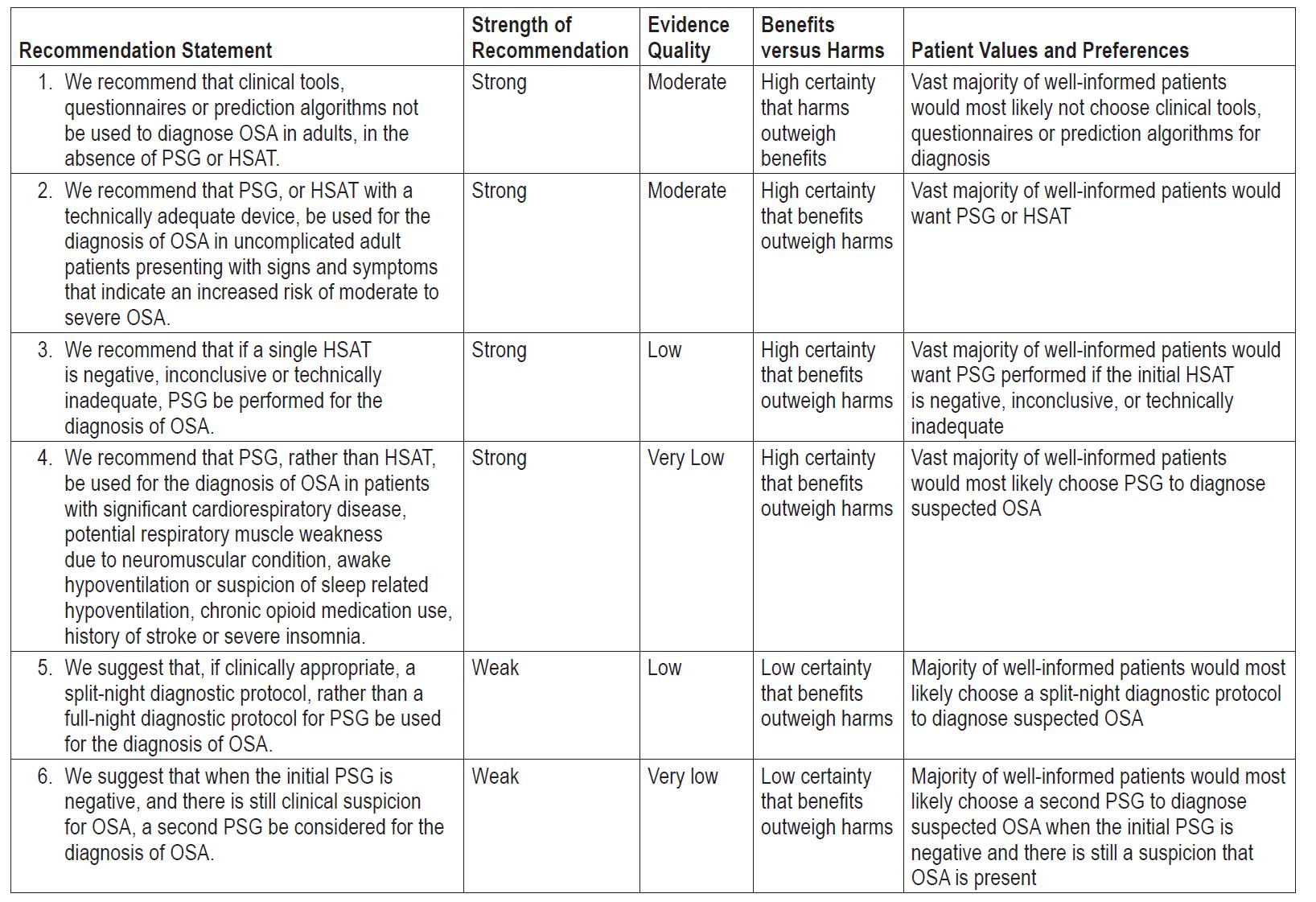
Kapur et al.
Clinical
practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med.
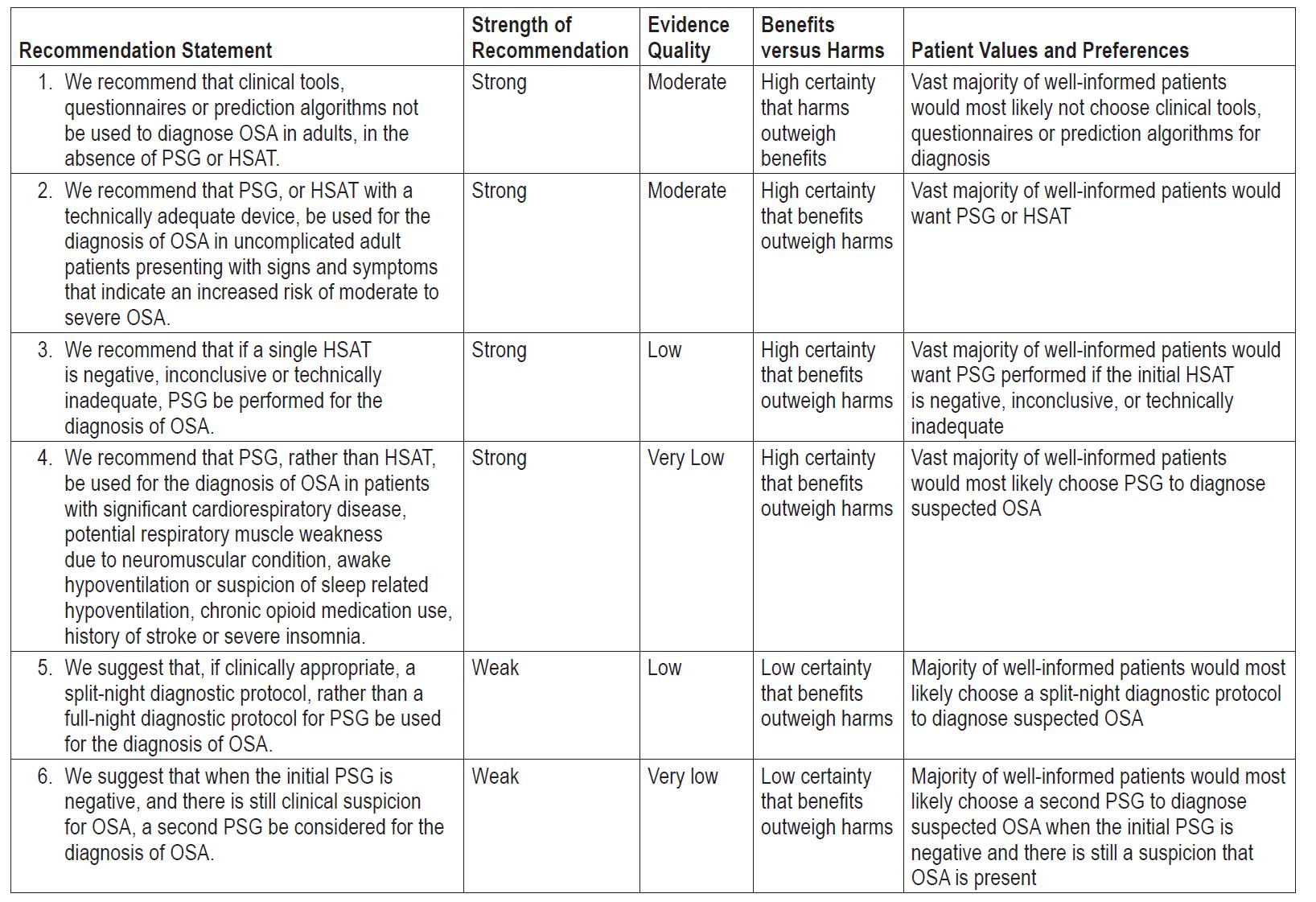
2017

Take home message 1. Have a high index of suspicion 2. In hospital/ clinic study (both diagnostic & titration) is recommended 3. Use home sleep testing only if parameters are met 4. Be aware of sleep related non-respiratory disorders 5. Be ready to tackle problems!