HEALTH CARE














Publisher
Jewish Community Foundation of Greater Phoenix


General Manager
Rich Solomon
Managing Editor
Shannon Levitt
Staff Writer
Nicole Raz
Account Executive
Jodi Lipson
Art Director
Frank Wagner
Noon Tuesday, 9 days prior to publication
11 a.m. Friday, 1 week prior to publication
12701 N. Scottsdale Road, Ste. 206

Scottsdale, AZ 85254
Phone: 602-870-9470
Fax: 602-870-0426
jewishaz.com
©2021. Phoenix Jewish News, LLC. (ISSN 1070-5848) is published less than weekly by Phoenix Jewish News, Inc., dba Jewish News. A subscription is $48 per year, payable in advance to Jewish News, Ina Levine Jewish Community Campus, 12701 N. Scottsdale Road, Ste. 206, Scottsdale, AZ 85254, telephone 602-870-9470. Periodicals postage paid at Phoenix, Arizona. POSTMASTER: Send address changes to Jewish News, Ina Levin Jewish Community Campus, 12701 N. Scottsdale Road, Ste. 206, Scottsdale, AZ 85254


We started 2021 hopeful that we would finally be able to turn the corner on the COVID-19 pandemic. Vaccines became available in January to many of our seniors, and even though the process was initially complicated and frustrating for many, appointments became easier to find and more and more people were vaccinated. People started to feel that the worst might be over.
After a long, strange 18 months filled with social distancing, carrying masks everywhere and having to figure out Zoom calls, we are now able to gather in person again, albeit with precautions and, in some cases, still masked.
Through it all, we have turned to our health care professionals for answers, support and guidance. With every twist and turn of COVID, we knew how fortunate we were to have people who were working hard to make us safe and to shine light on the facts we needed to know.
Past issues of Jewish News’ Best of …, have highlighted arts and culture, home and design and seniors. This year we are honoring many of the health care professionals who have helped Greater Phoenix’s Jewish community through this difficult and unique time. We received more nominations for this issue than ever before. It makes sense that many were excited to tell the stories of the people who were on the front lines throughout the pandemic and to honor their service in some way. In profiling our nominees, we hope we accomplished that. All of the interviews with our nominees were conducted in late spring as things were starting to look better.
Although every health care worker had a unique experience with COVID, there were several themes that cropped up again and again. Most people discussed the importance of soothing frightened patients with advice and up-to-date medical information. Most also pointed to telehealth as a great advance in technology. Even when the pandemic is over, technology will continue to be useful in caring for patients who are ill or out of town.
And many of our nominees said that even with the long hours and the constant stress, they found their jobs especially rewarding during this time. They, too, rediscovered how important it is to rely on and value one’s family and friends and not to despair in the face of the unknown.

Every year, we put out a call for nominations. The people featured inside were nominated for their work in keeping us healthy and safe. In our pages, they share some personal stories, as well as some of the ways the pandemic shaped their professions and how Judaism and Jewish values feed their work.

There are so many more people and organizations that could have been included, and we hope to hear from you about them so they can be featured in future issues of Jewish News.
Thanks for reading!
 —Shannon Levitt, Managing Editor
—Shannon Levitt, Managing Editor




The doctors of Affiliated Pediatric Dentistry and Orthodontics in Scottsdale have a strong desire to help people. Their career paths have combined health care with running a small business; and they get to use their artistic sides to create beautiful smiles.


This group of doctors was nominated by Rochelle Thomas, who has been employed at the practice for 34 years. In her tenure she has worked with several generations of doctors, and is “constantly humbled by the professionalism, quality of care, ethics and commitment that the doctors in our practice show every day to patients and employees.” Employees are treated with dignity and respect; patients are treated with care and offered an experience that makes them feel safe, she said.
Working in dentistry with children is both a challenge and an opportunity. These doctors get to teach kids the importance of caring for their teeth and also teach them not to be afraid to go to the dentist.
When COVID-19 hit and the office was closed for six weeks, the doctors spent every day making plans to reopen in a safe way. They took every possible precaution, going beyond CDC recommendations, to make employees and patients feel safe and confident. Many of the doctors
and staff are “lifers,” committed to one another and the patients of the practice.
How does your office approach patient care?
We take a very conservative approach to patient care. We have always been proud about only recommending treatment that is absolutely necessary. Our goal has always been to provide exceptional and efficient dental care while utilizing state-of-the-art technology. We strive to make each patient’s experience in our office positive and memorable.
What’s something you all love about what you do?
We love creating beautiful smiles and boosting the self-confidence of our patients. We enjoy interacting with patients of all ages, personalities and cultures. We also love being so entrenched in our community — we are all in this together.
What do you wish everyone knew about your jobs and what would people be most surprised by?
It’s the best job in the world. We are so lucky to have found a profession that brings health and happiness to so many. People would be surprised by the age range of our patients. Our practice sees
patients aged from 1 to 80 and even older. Also, many people are surprised when they hear about the amount of schooling required to be an orthodontist or pediatric dentist. Four years of undergraduate education, then four years of dental school followed by two to three years of the specialty program are required.
What were some of the biggest challenges your office faced during this past year amid the pandemic? For six weeks our offices were closed as many businesses were and our initial thought was for our team: We wanted to be sure they were provided for during this unprecedented time. Another huge challenge when preparing to reopen, was getting enough personal protective equipment to provide services. We worked with the ever-changing CDC recommendations to go above and beyond to create an environment where parents and patients felt safe while receiving dental care. We have gone to every length to ensure that anyone entering our office feels safe and comfortable including patients, family, team members and doctors.
How did COVID impact your day-today life as health care professionals?

The pandemic has had a profound impact on us. Something as simple as how we bring a patient in to the office, limiting the number of patients to ensure social distancing, having enough PPE, hand sanitizer, hospital-grade air purification systems, thermometers and completely redoing the reception area with wipeable chairs and removing shared items such as magazines are all part of it. We also had to make our little patients sad by removing video games.

What are some of the ways you foresee your industry or profession changing because of the pandemic? Zoom certainly. We implemented more virtual visits for certain appointments which saves the patients time, trips to the office and allows them to “see” us from the comfort of their own home. We will also permanently adopt some of the safety protocols we put in place; one of our favorites is wearing scrubs to work. They’re not just more hygienic but also way more comfortable.
In what ways does your office incorporate Judaism or Jewish values?


We apply Rabbi Hillel’s adage to love one’s neighbor as oneself — or patient in our case. We treat our patients as family and ask ourselves: “Would I do this for myself or my own child?” JN

Dr. Benjamin Bakall grew up in Sweden and was always interested in genetics. While still in Sweden, he started an MD/PhD program focused on ophthalmic genetics. He was fascinated by ophthalmology and the fact that the eye is a very complicated organ filled with multiple genes critical for vision.

He joined Phoenix’s Associated Retina Consultants in 2013 and is now in the process of founding a retina research foundation in order to promote local research and education on diseases affecting the retina. This is a step toward bringing novel eye treatments to the state. These new treatments will include retinal gene and stem cell therapy.
The person who nominated him, said that Bakall “understands the importance of listening and takes time for all concerns regarding both prevention and progression and clearly explains the treatment options in detail. Having a retinal disease that may cause vision loss can be scary, but Dr. Bakall is empathetic and understands your concerns and provides guidance for the best treatment options.”
Bakall also promotes upcoming research for inherited diseases that affect children in the community and he has overseen the groundbreaking positive effects of gene therapy in children with inherited eye diseases. He is also actively engaged in the community and trains medical students, local eye doctors and future retina specialists in Arizona.
In addition to his health care role, Bakall enjoys working out, hiking and spending time with family and friends. Traveling to new places is another way he spends the brief downtime he has.
How do you approach patient care?
I see people from every walk of life and my goal is to educate patients about their retinal condition and treatment options.
What’s your favorite thing about what you do?
I enjoy interacting with people and want to facilitate improving vision. I appreciate problem solving, and sometimes it is difficult to make the correct diagnosis, which may require specialized tests, including genetic testing.
What do you wish everyone knew about your job?
The retina is the tissue in the eye that detects light, and sometimes glasses cannot improve the vision if there is a problem with the retina.
What do you think would surprise people most about your job?
Eye injections are a very important treatment. And they do not hurt!
In what ways do you bring your Judaism with you to your job?
Vision loss can be scary and unsettling. I imagine myself in my patient’s situation and strive to bring as little discomfort and stress to the eye during the exam and treatment as possible.
I also strongly believe in continued education and helping my community.
What were some of the biggest challenges you faced during this past year amid the pandemic?
Continued treatment of retinal disease cannot stop, since it may result in permanent vision loss. The eye exam is unable to be socially distanced as it is a close, face-to-face interaction, which has a high risk for spread of aerosols.

“I imagine myself in my patient’s situation and strive to bring as little discomfort and stress to the eye exam and treatment as possible.”
How did COVID impact your day-to-day life as a health care professional?







We implemented frequent COVID testing, adhered to strict mask use, frequent hand-washing and limited the number of family members allowed to enter our clinics in order to reduce the risk of spreading the virus.
What are some of the ways you foresee your industry changing because of the pandemic?



We are evolving our practice to limit the spread of potential pathogens by increasing hygiene practices and still requiring use of face masks. The development and implementation of longer-lasting treatments for retinal diseases may be used in order to reduce the number of clinic visits.

Was there anything good that came out of the pandemic?


Increased awareness as the result of air-borne viral diseases has led to better sanitation techniques. The impact of emerging diseases has shown the need for global collaboration to reduce the spread of future potential epidemics. JN




Dr. Jared Berkowitz of Village Medical in Scottsdale, genuinely enjoys “being there” for his patients. He wants to be an advocate for patients and help them problem solve. That passion inspires his work in medicine. And primary care has allowed him the opportunity to get to know all his patients and build relationships with them.
When he’s not doctoring, he likes hiking, cooking and spending time with his family. He coaches his son’s little league team and his daughter is a fan of chess, which she regularly bests him at. His mom, a pre-school teacher for more than 30 years in Jewish schools, has been a strong influence on him and his family. He feels it’s important to light Shabbat candles and teach his kids about what it means to be Jewish so they grow up proud of who they are.
How do you approach patient care?
I approach it as a partnership with patients and as a relationship where we work cooperatively to better their health and achieve their goals, emotionally and physically.
What’s your favorite thing about what you do?
The challenges and the unknown of the day. We have schedules that are set but they are more suggestions and you never know what’s coming behind every door. And the relationships and getting to know patients and developing trust and breaking through barriers is all really exciting. Every patient has challenges and nuances.
What do you wish everyone knew about your job?
It’s not as glamorous as Gray’s Anatomy. There’s a reason they don’t make TV shows about primary care. You’re always needing to be there for
people in hours and after hours and the expectation is always there. You’re always asked to be present when people need you. We all sometimes need a break.
And the amount of paperwork! But I don’t want anyone to feel, ‘Oh, poor doctor.’ I’m not saying I want people to leave me alone.
What do you think would surprise people most about your job?
The surprise is how long it takes to pay off med school loans and debt!
There’s not a whole lot of surprise about the job. There’s a lot of transparency these days. You want to make sure there’s a great patient experience. There’s a lot of effort and thought that goes into creating that experience. We collaborate a lot behind the scenes to make it’s a rewarding experience for the patients.
What were some of the biggest challenges you faced during this past year amid the pandemic?
One of the biggest was being available to provide accurate, reliable information to patients. We tried to really dispel a lot of news that wasn’t necessarily true and created fear and concern.
Information was changing constantly, and we had to have patience during times of a lot of fear and concern.
How did COVID impact your day-to-day life as a health care professional?
It opened up a lot of avenues of care — predominantly remote care and telemedicine, which I think has been a great thing. It offered access to care which wasn’t there before. It’s really neat. We’re reaching a lot of patients for follow-up. Before it was challenging to get patients to follow up after you

“Putting personal things aside for others is always positive.”Dr. Jared Berkowitz PHOTO COURTESY OF JARED BERKOWITZ
initiated a therapy, to give up a day off work or burn a sick day. This improves their adherence to care.
From the quality of care standpoint it’s been a good thing. Before it was old school and you would have to come in and sit in the waiting room and take a lot of time. People who move can maintain relationships now if they’ve moved out of state as well.
What are some of the ways you foresee your profession changing because of the pandemic?


There’s nothing permanently changed. Time heals and fortunately with the focus on vaccination and consistently talking about how important that is and doing our part, hopefully that will continue to translate to patients and their kids. We’re more aware of washing hands and talking about spreading germs and preventing the spread of viruses. Any time we can talk about that it’s great.
Was there anything good that came out of the pandemic?

A silver lining is vaccination awareness. It’s important to have that discussion and get people to recognize it’s important to do their part and stop them from spreading disease.
People coming together as a community and trusting each other and understanding about doing their part for the greater good of society by wearing a mask even when they didn’t want to was very good. Putting personal things aside for others is always positive.
In what ways do you bring your Judaism with you to your job?



I think my faith relates to my personality of acceptance and allowing myself vulnerability to be relatable to my patients. Several of them are Jewish, and maybe we use a Yiddish phrase or play Jewish geography to find out where people grew up and who their families are.
Our allWEALTH® approach is designed to align your life and wealth by providing access to institutional quality investments, life & legacy planning, and impact initiatives, such as valuesbased investing.
If we can be of service to you and your family, please contact me at (480) 696-6431 or bmeyer@beaconpointe.com.
14350 N. 87th Street, Suite 185 Scottsdale, AZ 85260 beaconpointe.com
 NICOLE RAZ | STAFF WRITER
NICOLE RAZ | STAFF WRITER
Andrea Brennan found herself at a loss when she was an occupational therapist.


People would come in complaining of pain and she couldn’t figure out what was wrong.
“People kept on coming over and over again with these issues, and I didn’t have the repertoire of skills to manage them,” she said. “They were suffering.”
In 1996, she became certified in chronic edema and lymphedema management. “I manage all things with swelling,” she said. “I fell in love with it.” She became board certified in 2000 and in 2016 became an international instructor.
“It’s really just a misunderstood condition,” she said.
What should people know about what you do?

When people have unexplained swelling in their arms or ankles, there is a way to help them.


It’s called decongestive lymphatic therapy and this is a modality that includes manual lymphatic drainage, which is a manual technique to help decongest swelling in the limbs. There’s decongestive exercises, so the patient isn’t passive, but they’re actually engaged in moving fluid. There is compression therapy. I change the internal environment of
What’s your favorite thing about what you do?
I get a patient to come in to see me on day one with a pain level of 10, and they leave with a pain level of two or three. And the next visit, there’s no pain at all. It makes me feel fabulous because I’ve really affected changing somebody’s quality of life. And if I have outcome measures, and I measure from day one to subsequent measuring, they go from a very poor quality of life to resuming life when they didn’t even know it.
How do you approach patient care?



I listen. The patient is the best person who knows their body, and if they perceive it, then it’s real. And then I educate them regarding what’s going on, and then they will understand what’s going on, the fear is down, anxiety is down. And then they participate and get better pretty quickly. There are people who suffer for five or 10 years and I can get them better within two or three weeks.
What do you think would surprise people most about your job? That I exist.
In what ways do you bring your Judaism with you to your job? It’s who I am. It’s my culture. It’s my honesty. It’s my directness. JN
“The patient is the best person who knows their body, and if they perceive it, then it’s real.”
Dr. Stanley Goldberg of Banner Health Center in Peoria, never planned to go into medicine — he majored in electrical engineering. But while working as an electrical engineer, he noticed that people around him were getting laid off because their companies had lost contracts. He decided that was too unstable of a job and went into biomedical engineering.

“My plan was to do research in medicine through biomedical engineering,” he said. He discovered, though, that he would need to have an MD in order to get grants for his research. So he went to medical school. But by the time he finished his residency, he forgot his high-level math and physics. He was nine years away from what he had set out to do, and, by then, he also had a family.
He changed plans again and became a general and vascular surgeon. “Although I kind of backed into this career, it was absolutely the right thing at the right time. And I wouldn’t change a thing,” he said.
How do you approach patient care?
Patients may have similar problems, but each patient is unique and their management has to be custom fit to each individual. We all have different co-morbidities and lifestyles.
What’s your favorite thing about what you do?
I enjoy helping people. I like seeing the results after they come in with a problem and I’m able to cure it or improve on it.
What do you think would surprise people most about your job?
Even though there are a lot of very long hours and a lot of time commitments, it’s worth it to see these people get better.
What were some of the biggest challenges you faced during this past year amid the pandemic?
I tried to maintain my own health, but I never missed one day of work. We did see some patients in the office and we communicated with patients with video conferencing and on the phone, but for the most part, people are sick, they come in, they have to be taken care of.
Are there any ways you foresee your profession changing because of the pandemic?

I think all industries are going to change. Because of the pandemic, many people have been working from home. I work for a rather large corporation, and I’m sure that there will be many of the administrative type people who will do some of their work at home. But when it comes to the doctors and the nurses and the patient direct management, I don’t see a big change.
Was there anything good that came out of the pandemic?
I think it is a plus to realize that there are things that don’t have to be done in the office. It won’t change anything for me, personally, though.
What do you do in your free time?
I do weightlifting. I horseback ride. I do some shooting. I’m a member of a model railroad club. And I spend time with my family.
In what ways do you bring your Judaism with you to work?
It’s kind of like tikkun olam. In a very, very small way it contributes to that by trying to heal individuals. And over a whole career, I think that it makes a small contribution in healing the world. Also, the morals and ethics and my family upbringing have formed a lot of my attitudes in managing and caring for people. JN
“I like seeing the results after people come in with a problem and I’m able to cure it or improve on it.”
When Dr. Fred Cucher, a non-invasive cardiologist with Phoenix Heart, was in residency, he rotated through cardiology and was impressed by its equipment and tests. “It was a hands-on specialty,” he said, and decided “I would like to do this. You have to choose something you can do for the rest of your life and enjoy it.”

No w he feels blessed working with his colleagues, an amazing multi-cultural group of cardiologists and partners who are Jews, Christians, Buddhists, Hindus and Muslims. “We care for one another and it’s a good working environment and makes it hard to retire,” he said. They started the group 40 years ago, and they’ve been held together by shared ethics and morals and by being committed to doing the right thing for people. He’s happy to be a part of it, and is in no rush to leave. In fact, he said, he’ll be practicing until they change the locks on the door.
How do you approach patient care?
People look at patient care different ways, but the right way is that I turn to the patient, because when you’re taking people’s life into your hands they want to know you will care for their well-being. I hear it all the time from patients who feel they haven’t been listened to or blown off. It’s not just giving medication. It’s caring for your patient. Have your mind set on doing the right thing, and that will never get you into trouble. That’s the best way to take care of people.
What’s your favorite thing about what you do?
The relationships with the patients. I’ve been taking care of some for about 30 years. I know their family, take care of spouses and kids, sometimes even grandkids. Establishing the relationship is gratifying and people express gratitude for getting them through crises. Life is all about relationships.
What do you wish everyone knew about your job?
They think about the clinical and technological aspects but I would want them to know the joy in doing what I do and having a positive impact on people’s lives.
What do you think would surprise people most about your job?
They would be surprised by the constant motion of what we do. There’s little time to do nothing. There’s a little time for shmoozing, but for the most part, there’s very little time to have any down moments. It’s one thing to the next. They would be surprised at how little time in the day I have.
What were some of the biggest challenges you faced during this past year amid the pandemic?
People’s fear of COVID and not seeking medical care when they should was a big challenge. Very sick people stayed at home and that’s the untold toll of the pandemic. Some didn’t have the medical care they needed. They weren’t getting tested or seeing the doctor. Telemedicine is not a good way of taking care of very sick people. It’s better for primary care people but not for us.
Too many people unnecessarily died or will die because they didn’t avail themselves of services to be diagnosed or should have gone to the hospital. Telemedicine is a pain in the neck and we had to do it for a while, but it’s terrible not to be able to examine patients or take blood pressure or do an ECG. Telemedicine is not a suitable format for cardiologists.
How did COVID impact your day-to-day life as a health care professional?

I was never out of the office even when I was doing telemedicine so I could ha ve access to patient charts. The office was probably safer during the pandemic because patients had their temps taken a nd filled out a form about any illness. We turned some away if they had something communicable. Everyone was mask ed, and with all the hand-washing my hands were almost raw despite lots of lotion. You do what you have to do.
What are some of the ways you foresee your profession changing because of the pandemic?
It showed me more of what I wanted not to do. Telemedicine is big now and I learned that I don’t want to go there.
“...when you’re taking people’s life into your hands they want to know you will care for their well-being.”
Was there anything good that came out of the pandemic?
People recognized the importance of their relationships and the absolute blessing of freedom of being able to move about freely and be together for holidays and talk over a meal. The isolation was bad and harmed a lot of people with depression and alcoholism. I wound up doing a lot of therapy for widows and widowers because they were isolated and couldn’t use technology.






In what ways do you bring your Judaism with you to your job?



I wear my kippah all the time in the office. My patients define me as a Jew and it makes me representative of all Jews for people who don’t deal with Jewish people much. It’s important that I communicate the best of what we are. An important part of what we do as physicians is chesed. The caring and sharing of chesed is an essential component of the physician and who we want to be. JN

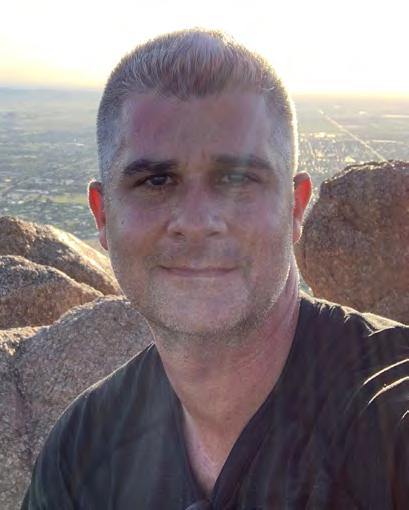
In an isolated patch of Sonoran desert north of Phoenix sits a large and unassuming house along with a few outbuildings. Driving by, one would hardly guess that it is a residential treatment facility that its founder, Mitch Prager, hopes might be an answer for those struggling to beat addiction.
But had it existed years ago, it is just the kind of place that might have saved Prager’s brother and dear friend, who both died of their addictions and who are the inspiration for his efforts.
After touring roughly 50 residential treatment centers around the country, Prager has come to understand that while there’s no panacea, providing enough types of therapy is key. He said the recovery “magic” might happen in art class, working with horses, walking in a labyrinth or even in plain old traditional therapy. He decided his facility would have them all.
Soberman’s Estate opened two years ago replete with psychiatrists, medical and nursing staff, as well as all the therapies that Prager found in his research. His brother died of an overdose, and his longtime friend died by suicide after a brief stint of sobriety. Those experiences, as well as his own struggle with alcoholism, taught Prager first-hand what addiction does to people and how difficult it is to overcome. Prager saw a way he could help others by building a facility with an all-hands-on-deck approach.
Why did you choose your profession?
The career path I chose was hotel management, then executive search recruitment. Opening Soberman’s Estate was much more than a choice. The calling to help men recover from alcoholism and addictions became my passion, purpose and mission in life.

How do you approach patient care? At Soberman’s Estate, patient care is individualized and regularly updated. Compassion is the key ingredient in our medically sophisticated, clinically excellent, holistic — mind, body, soul — treatment program.
What’s your favorite thing about what you do? What would surprise people about Soberman’s?
I love attending alumni events and watching our alumni help our current clients. Previously, I was a professional magician and I occasionally utilize magical effects as visual aids during presentations to staff and clients.
What do you wish everyone knew about your job?
Recovery is possible, and there should be no guilt or shame about having the disease of alcoholism or addiction.
In what ways do you bring your Judaism with you to your job?
We light Shabbat candles, Chanukah candles, we have mezuzahs, offer kosher food and we have rabbis on our team to study with our clients and facilitate weekly spiritual education groups.
What were some of the biggest challenges you faced during this past year amid the pandemic?

We believe that everything is an opportunity to either celebrate or learn from and we coined the term “in the spirit of continuous improvement.”
We reduced our maximum number of clients to eight from 10 and celebrated the fact that we are on five acres and are a very safe place to quarantine. When clients could not travel by air because of the pandemic, our driver transported them to and from their homes up to 500 miles away.
“The calling to help men recover from alcoholism and addictions became my passion, purpose and mission in life.”Mitch Prager at Soberman’s Estate PHOTO COURTESY OF MITCH PRAGER
How did COVID impact your day-to-day life as a health care professional?


We teach men how to recognize and respond to anxiety, depression, stress. So, as professionals, we implemented a program to remind each other to set aside additional self-care time to ensure we were taking care of ourselves so we could help others — basically, we utilized this opportunity to practice what we preach.
Was there anything good that came out of the pandemic?
More people are becoming aware that life is precious, family is precious and gratitude and acceptance are the key to happiness. JN
JEWISHAZ.COM

us
jewishaz.com

jewishaz.wordpress.com
facebook.com/JewishAZ
twitter.com/phxjnews
instagram.com/phxjnews
pinterest.com/jewishaz

Hillary K. Peck has been practicing dentistry at the same address since 1995. The Phoenix building has carried her name since 2014: Peck Family Dentistry, PC.

When Barry Bernell retired, Peck and her husband purchased his practice and combined it with their own.
“Barry’s patients were very gracious in allowing us to provide their dental care,” she said, noting her patients have been with her through thick and thin.
“They were here to lend support and comfort when my husband, Kevin, was sick and passed away in 2018. I owe my patients tremendous gratitude for their comfort, support, and giving me a reason to get up in the morning.”
David Tuckman, who nominated Peck, said she is “prompt and thorough.”
Why did you choose this profession?
My late father was a dentist in southwestern Pennsylvania. I spent many hours observing and helping out in his practice as I was growing up. I knew that dentistry was the profession for me.
How do you approach patient care?
We are a family-oriented practice. We enjoy getting to know our patients and listening to them. We approach each patient’s treatment in a manner that is specific to their unique needs.
What’s your favorite thing about what you do?
I enjoy being able to get my patients out of pain, getting to know them and, hopefully, make a positive difference in their health.
What do you wish everyone knew about your job?
Good dental health is paramount to good overall health. We welcome being your partners in achieving optimum health.
What do you think would surprise people most about your job?
Surprisingly, some people actually enjoy coming to the dentist.
In what ways do you bring your faith with you to your job?
Although I am not Jewish, I enjoy learning about other cultures, traditions and religions. Many of my Jewish patients have been gracious enough to share their experiences with me and have made me feel welcome in their community. It is my hope that I can share that same sense of community with my patients.
What were some of the biggest challenges you faced during this past year amid the pandemic?
Like everyone, we faced uncertainty, supply challenges and engineering challenges in trying to keep everyone safe while still meeting the needs of our patients.
How did COVID impact your day-to-day life as a health care professional?

As a health care professional, my staff and I felt a strong commitment to the safety of our patients. Consequently, we were very careful and creative in staying quarantined as much as possible, especially since a large number of our patients would be most at risk.
What are some of the ways you foresee your profession changing because of the pandemic?
I think that many of the changes that we have incorporated in the office — air purifiers, disposable gowns, face shields, added housekeeping procedures — are here to stay. It is probably a change for the positive.
Was there anything good that came out of the pandemic?
I think that everyone has been more patient and considerate in realizing that we are all in this together, and that everyone is trying to do their best.
On a personal note, it was nice to have some unexpected time with my daughters who would normally be away at graduate school.
What do you do in your free time?
I enjoy spending time with my family, my animals and gardening. JN
“We approach each patient’s treatment in a manner that is specific to their unique needs.”
As a naturopathic physician, Mona Morstein spends a lot of time with patients. On a patient’s first visit, she takes an hour and a half to do a comprehensive intake and exam. The second treatment visit is one hour and each follow-up is 30 minutes. During that time she is looking for any imbalances that might be causing harm to her patient.

What’s your favorite thing about what you do?
It’s really great helping people heal naturally, uncovering why they have the symptoms or condition they do and helping them get it under control or eradicate it with naturopathic care. Although I am licensed to prescribe medications, that isn’t, in general, the focus. Using nutrition, vitamin/minerals, nutraceuticals, botanical/Chinese/Aruvedic botanicals, acupuncture, IVs, vertebral manipulation, lifestyle counseling and prolotherapy is very rewarding.
What do you wish everyone knew about your job?
I have a Bachelor of Science in foods and nutrition from ASU, did four years of naturopathic medical school in Portland, Oregon and did my residency there, too, We are fully licensed as physicians in Arizona. Conventional medicine is absolutely awesome in many different ways. I had brain surgery and recovered fully, which is amazing; my friend had his thumb reattached to his hand, which is now functional, which is also amazing. People had their lives saved in hospitals from many different serious conditions, including COVID-19. However, it’s important to know there may be times when naturopathic medicine can step in, find answers and initiate treatments that may be curative.
What do you think would surprise people most about your job?
I am the equivalent, essentially, of a primary care practitioner who does integrative medicine. I do the same regular tests, do appropriate imaging and prescribe medications. We are also licensed to do
minor surgery, but I choose to not do that in my practice.
What were some of the biggest challenges you faced during this past year amid the pandemic?
Screening patients and wearing masks all day long. We’ve done very well using naturoapthic medicine to successfully address acute COVID patients, seniors, kids, diabetic patients and the patients with post-COVID syndrome. But I didn’t have too many challenges, to be honest. We adapted and started doing more telemedicine, which patients really appreciated.
What are some of the ways you foresee your industry or profession changing because of the pandemic?

I think telemedicine is going to continue to be a pretty common way of seeing patients. There will probably be continued treatment of COVID and post-COVID syndromes as it’s unlikely the virus will ever be fully contained.
Was there anything good that came out of the pandemic?
Knowing the effectiveness of naturopathic medicine in treating this new virus was good to learn. Otherwise, not so much. I was only able to visit my aged mother in Los Angeles once last year, which was very upsetting. My Chabad stayed open with masks, social distancing and reduced congregants in the shul, but I always went, as I enjoy services.
In what ways do you bring your Judaism with you to your job?
It’s vitally important that I am a “good Jew” in all aspects of interactions, and am respectful, kind, fair, thoughtful, someone people can talk to. I am very involved with making sure that patients are treated well, ensuring they feel my clinic listens to them, answers their questions and makes things smooth and efficient. My patients are well aware I’m Jewish. I discuss Jewish holidays in clinic newsletters, there are mezuzot on doors in my clinic, Jewish items in my office. JN
“Conventional medicine is absolutely awesome in many different ways... however, it’s important to know there may be times when naturopathic medicine can step in, find answers and initiate treatments...”
Mona MorsteinPHOTO COURTESY OF MONA MORSTEIN
Thank you, readers, for letting your voices be heard once again. The ballots have been counted, the results are in and we are excited to announce this year’s winners. We invite you to read about, share and enjoy these great businesses and organizations that have earned your vote. Congratulations to all of our winners!
DOCTOR
Dr. Jay S. Friedman, Scottsdale
Runner-Up: Dr. Tamara Lieberman, Jewish Family & Children’s Service, Phoenix
NURSE
Victoria Flowers
Lauren A. Schwartz
HOSPITAL
HonorHealth, multiple locations
Runner-up: Mayo Clinic Hospital, Phoenix
NONPROFIT
Paradise Valley Community Food Bank, Paradise Valley
Runner-up: Jewish Family & Children’s Service, Phoenix
SUMMER CAMP
Shemesh Camp at The J, a program of Martin Pear JCC, Scottsdale
Runner-up: Camp Canyon Jewish Outdoor Adventures, Flagstaff
OVERNIGHT CAMP
Camp Daisy and Harry Stein, Prescott
Runner-up: Friendly Pines Camp, Prescott
SPECIAL NEEDS CAMP
Camp Gesher – online enrichment program
Runner-up: The Friendship Circle Summer Camp, Phoenix
HILLEL
Hillel Jewish Student Center at ASU, Tempe
Runner-up: UCLA Hillel, Los Angeles
ARIZONA AREA COLLEGE/UNIVERSITY
Arizona State University, Tempe
Runner-up: Grand Canyon University, Phoenix
ART GALLERY/MUSEUM
Musical Instrument Museum, Phoenix
Runner-up: Desert Botanical Museum, Phoenix
ATHLETIC CLUB
Martin Pear JCC, Scottsdale
Runner-up: Camelback Village Racquet & Health Club, Phoenix
CASINO
Talking Stick Resort, Scottsdale
Runner-up: Gila River Hotels & Casinos, multiple locations
CHILDREN’S ENTERTAINMENT
Phoenix Zoo
Runner-up: Arizona Science Center, Phoenix
CHILDREN’S/TEEN PROGRAMMING
Jewish Family & Children’s Service, Phoenix
Runner-up: Mountain Region BBYO, multiple locations
COMMUNITY EVENT
Greater Phoenix Jewish Film Festival
Runner-up: The Allan J. Flader Community-Wide Drive-Through Purim Parade at Martin Pear JCC, Scottsdale
FAMILY-FRIENDLY ACTIVITY
Butterfly Wonderland, Scottsdale
Runner-up: Beth El Congregation’s Shabbat service, Phoenix
FITNESS CENTER
Martin Pear JCC, Scottsdale
Runner-up: EōS Fitness, Scottsdale
GOLF CLUB
Gainey Ranch Golf Club, Scottsdale
Runner-up: Scottsdale Silverado Golf Club
HOTEL
Fairmont Scottsdale Princess
Runner-up: JW Marriott, Desert Ridge
MUSIC VENUE
MIM Music Theater, Phoenix
Runner-up: Symphony Hall, Phoenix
NONPROFIT ORGANIZATION
Jewish Family & Children’s Service, Phoenix
Runner-up: Congregation Beth Israel, Scottsdale
PARKS/HIKING TRAILS
McDowell Sonoran Preserve Gateway Trail, Scottsdale
Runner-up: Camelback Mountain, Phoenix
PERFORMING ARTS VENUE/ORGANIZATION
ASU Gammage, Tempe
Runner-up: Musical Instrument Museum, Phoenix
PLACE TO TRAVEL IN ALL OF ARIZONA
Sedona
Runner-up: Grand Canyon National Park
PLAYGROUND
McCormick Stillman Railroad Park, Scottsdale
Runner-up: Congregation Beth Tefillah, Scottsdale
SPORTS ORGANIZATION
Arizona Diamondbacks, Phoenix
Runner-up: Arizona Cardinals, Glendale
STAYCATION DESTINATION
JW Marriott, Desert Ridge
Runner-up: Sedona
YOGA CLUB
Yoga on the Rocks, Scottsdale
Runner-up: Desert Song Yoga & Healing Arts, Phoenix AFTER CARE PROGRAM
Club J, a program of Martin Pear JCC, Scottsdale
Runner-up: Beth El Congregation Early Childhood Center, Phoenix
PRESCHOOL
Chanen Preschool, Scottsdale
Runner-up: Temple Chai Early Childhood Center, Phoenix
PRIVATE SCHOOL/DAY SCHOOL
Pardes Jewish Day School, Scottsdale
Runner-up: Brophy College Preparatory, Phoenix PUBLIC SCHOOL
Pinnacle High School, Phoenix
Runner-up: Desert Mountain High School, Scottsdale
HEBREW SCHOOL
The Mark L. Haberkorn Religious School of Congregation Beth Israel, Scottsdale
Runner-up: Temple Chai Religious School, Phoenix
SPECIAL NEEDS SCHOOL
New Way Academy, Phoenix
Runner-up: AZ Aspire Academy, Tempe
SPECIAL NEEDS PROGRAMMING
Gesher Disability Resources, Scottsdale
Runner-up: New Way Academy, Phoenix
YOUNG ADULT PROGRAMMING
Bureau of Jewish Education’s Hebrew High of Greater Phoenix
Runner-up: Jewish Family & Children’s Service, Phoenix
BAGEL
Chompie’s Restaurants and Bakery, multiple locations
Runner-up: New York Bagels ‘N Bialys, Scottsdale
BAKERY
Macarons That Matter, Phoenix
Runner-up: Chompie’s Restaurants and Bakery, multiple locations
BAR
The Vig McCormick Ranch, Scottsdale
Runner-up: Culinary Dropout, multiple locations
BRUNCH
Chompie’s Restaurants and Bakery, multiple locations
Runner-up: EGGstacy, multiple locations
GROCERY
AJ’s Fine Foods, Scottsdale
Runner-up: Fry’s, multiple locations
ICE CREAM/FROZEN YOGURT
Sweet Republic, Scottsdale
Runner-up: TIE
Menchie’s Frozen Yogurt, multiple locations
Zoyo Neighborhood Yogurt, multiple locations
JEWISH DELI
Chompie’s Restaurants and Bakery, multiple locations
Runner-up: JJ’S Deli, Scottsdale
KOSHER BAKERY
Chompie’s Restaurants and Bakery, Phoenix
Runner-up: Lior the Baker, Scottsdale
KOSHER GROCERY
Fry’s Marketplace & Deli, multiple locations
Runner-up: Imperial Market & Deli, Phoenix
PIZZA
Grimaldi’s Pizzeria, Scottsdale
Runner-up: Fired Pie, Scottsdale
RESTAURANT
Steak 44, Phoenix
Runner-up: Kitchen18, Scottsdale
BEST CONTRACTOR
Sonoran Classic Builders, Scottsdale
Runner-up: Paul Barresi LLC, Phoenix
ELECTRICIAN
Parker & Sons, Phoenix
Runner-up: Copper King Electric, Scottsdale
FLOORING
Arizona Tile, Scottsdale
Runner-up: One Source Flooring & Interiors, Phoenix
HVAC
Howard Air, Phoenix
Runner-up: Hobaica Services, Phoenix
INTERIOR DESIGN
Barbara Kaplan Design Dimensions, Scottsdale
Runner-up: Katz Design Group, Phoenix
LANDSCAPER
Desert Foothills Landscape, Cave Creek
Runner-up: Triple “J” Lawn Service, Phoenix
PEST CONTROL
Green Mango Pest Control, Chandler
Runner-up: Truly Nolan Pest Control, multiple locations
PLUMBER
Phoenix Plumbing & Drain Service
Runner-up: Integrity Plumbing and Drain, multiple locations
ROOFING/SIDING/DECKS
Pinnacle Roofing, Phoenix
Runner-up: Prime Roofing, Mesa
WINDOWS
ABC Glass Company, Phoenix
Runner-up: Arizona Window and Door Store, Scottsdale
ALTERNATIVE SHABBAT SERVICE/PROGRAMMING
Congregation Beth Israel, Scottsdale
Runner-up: Tempe Chai, Phoenix
CHABAD
Chabad of Scottsdale
Runner-up: Chabad at ASU, Tempe
FAMILY-FRIENDLY SHABBAT SERVICE
Temple Solel, Paradise Valley
Runner-up: Congregation Beth Israel, Scottsdale
JUDAICA SHOP
Jacki Cohen Glass Art Designs, Scottsdale
Runner-up: Temple Chai Gift Shop, Phoenix
SPECIAL NEEDS SHABBAT SERVICE
The Friendship Circle, Phoenix
Runner-up: Simchat Shabbat-Gesher Disability Resources, Scottsdale
COSMETIC SURGERY
Scottsdale Plastic Surgeons
Dr. David A. Hecht, Scottsdale
DENTIST
Affiliated Pediatric Dentistry & Orthodontics, Scottsdale
Runner-up: Dr. Michael B. Lebowitz, Phoenix
ER/HOSPITAL
HonorHealth, multiple locations
Runner-up: Mayo Clinic, Scottsdale
GASTROENTEROLOGIST
Dr. Stuart Triester, Scottsdale
Runner-up: Dr. Janet Reiser, Scottsdale
LASIK CENTER
Horizon Eye Specialists & Lasik Center, Phoenix
Runner-up: Dr. Jay L. Schwartz, Scottsdale
MENTAL HEALTH PRACTITIONERS
Pam Ruzi, LMSW, APHSW-C, A.T.R.-BC
Runner-up: Therapy With Heart, Scottsdale
OB/GYN
Dr. Julie B. Kwatra, Scottsdale
Runner-up: Dr. Courtney A. Hunt, Scottsdale
ORTHODONTIST
Affiliated Pediatric Dentistry & Orthodontics, Scottsdale
Runner-up: Dr. Steven H. Goldstein, Scottsdale
ORTHOPEDIC PRACTICE
Dr. Robert Mileski, Scottsdale
Runner-up: OrthoArizona, multiple locations
PEDIATRICIAN
North Scottsdale Pediatric Associates
Runner-up: Paradise Pediatrics, Scottsdale
URGENT CARE
Banner Urgent Care, multiple locations
Runner-up: HonorHealth Urgent Care, Thompson Peak, Scottsdale
VEIN CLINIC
Dr. Joshua D. Cohen, Tri-City Cardiology, Mesa
Runner-up: Arizona Vein and Laser, multiple locations
VET
Lookout Mountain Veterinary Clinic, Phoenix
Runner-up: All Creatures Animal Clinic, Phoenix
VISION CARE
Dr. Randall R. Tozer, Scottsdale
Runner-up: Horizon Eye Specialists & Lasik Center, multiple locations
ADVERTISING AGENCY
Evolve Public Relations and Marketing, Scottsdale
Runner-up: HMA Public Relations, Phoenix BANK
Chase Bank, Scottsdale
Wells Fargo Bank, Phoenix
CREDIT UNION
One AZ Credit Union, multiple locations
Runner-up: Desert Federal Credit Union, Phoenix BARBER
Gold Scissors Barbershop, Scottsdale
Runner-up: Great Clips, Sonora Village, Scottsdale
CAR WASH
Weiss Guys Car Wash, multiple locations
Runner-up: Cobblestone Auto Spa, Scottsdale
DRY CLEANERS
Tide Dry Cleaners, Scottsdale
Runner-up: Prestige Cleaners, Inc., multiple locations
FACIALS
MedSpa 810, Scottsdale-Shea
Runner-up: JW Marriott, Desert Ridge
FINANCIAL PLANNER
Bruce Meyer, Beacon Pointe Advisors, Scottsdale
Runner-up: TIE
Barton Spector Wealth Strategies, Scottsdale
Buckman & Corning Financial Strategies Group, Scottsdale
INSURANCE AGENCY
Summit Insurance Advisors, Scottsdale
Runner-up: Josh Epstein, Farmers Insurance Group, Scottsdale
LAW FIRM
Woodnick Law PLLC, Phoenix
Runner-up: Gust Rosenfeld PLC, Phoenix
MANI/PEDI
Desert Nails Spa, Scottsdale
Runner-up: Fancy Nails, Phoenix Massage
MASSAGE
JW Marriott Scottsdale Camelback Inn Resort & Spa
Runner-up: MedSpa 810, Scottsdale-Shea
PET GROOMER
Wag N’ Wash Natural Pet Food & Grooming, Scottsdale Puff & Fluff Grooming, Phoenix
REAL ESTATE AGENT
Amy Rosenthal, HomeSmart, Scottsdale
Runner-up: Bryce Schotz, You Call The Schotz of West USA Realty
REAL ESTATE AGENCY
R.O.I. Properties – Beth Jo Zeitzer, Phoenix president, designated broker
Runner-up: Nikki Bernstein/ NikkiB Group | Berkshire Hathaway
Home Services Arizona Properties
SALON
Sassoon Salon, Scottsdale
Runner-up: D’Ambrosio Salon, Scottsdale
SPA
JW Marriott Scottsdale Camelback Inn Resort & Spa
Runner-up: The Phoenician, a Luxury Collection Resort, Scottsdale
WAXING
European Wax Center, multiple locations
Runner-up: Lorna’s Heavenly Skin Studio, Scottsdale
BACHELOR OR BACHELORETTE PARTY
W Scottsdale Hotel
Runner-up: Orange Sky, Talking Stick Resort, Scottsdale
CATERER
Levi Catering LLC, Phoenix
Runner-up: M Culinary Concepts, Phoenix
EVENT VENUES
Arizona Jewish Historical Society, Phoenix
Runner-up: Chateau Luxe Event Venue, Phoenix
DJ
Jacob Mandelbaum, JManEntertainment, Scottsdale & Greater Phoenix
Runner-up: Event Smart Productions, Scottsdale
FLORIST
Cactus Flower Florists, Scottsdale
Runner-up: Desert Poppy, LLC, Scottsdale
PHOTOBOOTH
GreenScreen Entertainment & Novelties, Phoenix
Runner-up: Picture This AZ! Photo Booth Co, Phoenix
PARTY PLANNER
Jody Stachel at Events 13, Scottsdale
Runner-up: The Event Genies, Scottsdale
PHOTOGRAPHER/VIDEOGRAPHER
Stephanie Heymann Photography, Scottsdale
Runner-up: Lori Krenzen Photography, Scottsdale
BEST PLACE TO BUY SUITS/TUXEDO
Celebrity Tux and Tails, Tempe
Runner-up: Mr. Formal Arizona, Phoenix
BOUTIQUE
Diva Divine Boutique, Scottsdale
Runner-up: Kiss Me Kate Boutique, Phoenix
BRIDAL SHOP
Laurie’s Bridal and Formal, Scottsdale
Runner-up: Quintessential Bride and Formal Wear, Scottsdale
CAR DEALERSHIP
Chapman BMW On Camelback, Phoenix
Runner-up: Earnhardt Car Dealerships, Scottsdale
EYEWEAR
Sassy Glasses Optical Boutique, Phoenix
Runner-up: Tager Optical, Phoenix
FORMALWEAR
Laurie’s Bridal and Formal, Scottsdale
Runner-up: Mr. Formal Arizona, Phoenix
FURNITURE/MATTRESS STORE
Buffalo Collection, Scottsdale
Runner-up: American Furniture Warehouse, multiple locations
JEWELER
London Gold, Scottsdale
Runner-up: E.D. Marshall Jewelers and Diamond Engagement Ring Store, Scottsdale
MENSWEAR
Well Suited, multiple locations
Runner-up: Nick’s Menswear, multiple locations
MUSICAL INSTRUMENT STORE
Musical Instrument Museum, Phoenix
Runner-up: Ziggie’s Music, Phoenix
SHOPPING MALL
Scottsdale Fashion Square
Runner-up: Kierland Commons, Scottsdale
55+ COMMUNITY
Vi at Silverstone, Scottsdale
Runner-up: TIE
The Palazzo Senior Living, Phoenix Sagewood, Phoenix
ALZHEIMER’S/DEMENTIA CARE
Beatitudes Campus, Phoenix
Runner-up: Maravilla Scottsdale
ASSISTED LIVING
La Siena, Phoenix
Runner-up: TIE
Assisted Living of Scottsdale Beatitudes Campus, Phoenix
HOMECARE SERVICES
Cypress HomeCare Solutions, Scottsdale
Runner-up: Connections in Home Care, Phoenix
HOSPICE CARE
Hospice of the Valley, multiple locations
Runner-up: Madrona Hospice & Palliative Care, Scottsdale
INDEPENDENT LIVING
La Siena, Phoenix
Runner-up: Maravilla, Scottsdale
SENIOR ACTIVITIES
La Siena, Phoenix
Runner-up: TIE
Beatitudes Campus, Phoenix
The Palazzo Senior Living, Phoenix
SENIOR CENTER
JFCS Center for Senior Enrichment, Phoenix
Runner-up: Beatitudes Campus, Phoenix
SENIOR PROGRAMMING
JFCS Center for Senior Enrichment, Phoenix
Runner-up: Martin Pear JCC, Scottsdale

Dr. Sarah Nicholas, like most other doctors who go into oncology, did it for personal reasons. Witnessing one of her cousins get diagnosed with cancer at a young age set her up to see some very hard realities firsthand, and seeing her family deal with illness really spoke to her, she said. “It put me on a path.”
Her eventual career choice was also helped by her strong interest in science. And when she started medical school, “I knew it would be oncology — just not which flavor. And then I stumbled on radiation oncology,” she said.
A recent transplant from the East Coast, Nicholas enjoys hiking and exploring the area with her family. She also likes cooking, spending time with her two kids, ages 4 and 2, and they recently added a new puppy. She practices at Banner MD Anderson Cancer Center in Gilbert.
How do you approach patient care?
When I meet with a patient, it’s important to get to know them as a person and understand what’s important to them outside the hospital to get a sense of where their priorities are. Not all care is the same. As a whole, we’re moving towards more personalized medicine and that helps me come up with the treatment plan.
What’s your favorite thing about what you do?
It’s different from medical oncology. People think of cancer and generally think about their surgeon or chemo doctor.
There are three different prongs to cancer treatment, and we, radiation oncologists, play an equal role. But not all cancers need radiation. Depending on the cancer, radiation can be the only treatment and sometimes it’s palliation and sometimes it’s in combination with surgery or chemo.
We work in group settings with the
surgeons and medical oncologists to come up with a comprehensive cancer plan, and I like the teamwork element.
It’s an honor and a privilege to treat my patients. I don’t take it lightly. It’s an honor that patients allow me to be involved in their life and in their care.
What do you think would surprise people most about your job?
Most people are surprised to learn what radiation is. They ask if they will be radioactive. They’re fascinated by the equipment. I’m using highpowered x-rays so they ask if I’m like a Ghostbuster. And, in my nerdy way, I think it’s cool.
You see the chemo going in and you have a scar from surgery. What I do is less tangible to patients, so I have to explain a lot. The people who trained me explain the evolution from then to now. Now we can get better outcomes because we can aim the beam better. People come in with many preconceived notions.
What were some of the biggest challenges you faced during the pandemic?
The biggest thing was that a lot of people stopped getting screening colonoscopies or mammograms. Unfortunately, I think we’re seeing people who missed things and we’re seeing tumors at a later stage. I’m hoping as things normalize, we can go back to catching things.
Screening brought down death rates from cancer. And I’m hoping this is only a blip. Everything was so backlogged. I’m hoping it will go back to normal.
How did COVID impact your day-to-day life as a health care professional?
I’m mainly in an outpatient setting so all of the patients I was seeing were screened. Unless there was

“It’s an honor that patients allow me to be involved in their life and in their care.”Dr. Sarah Nicholas PHOTO COURTESY OF BANNER HEALTH
an urgent case in the hospital I wasn’t exposed. Going into work I felt relatively safe compared to other physicians. But it really altered our work flow. We transitioned as many patients as possible to telehealth.
And there are a lot of shorter regimens of radiation that would have taken longer for our field to adopt in clinical practice, but because of COVID they were more quickly adopted. Things were published while COVID was out. People would opt for shorter treatments. It’s too soon to tell but things look good.




What are some of the ways you foresee your profession changing because of the pandemic?


Studies published for rectal and breast cancer are calling for shorter treatments. We recommended that for people who were eligible.
From a patient perspective I think it’s great. They gain time and it’s good for quality of life.
Was there anything good that came out of the pandemic?
Things were adopted more quickly in routine practice. Telehealth is very convenient for patients.
My nuclear family spent a lot more time together, which I loved.

In what ways do you bring your Judaism with you to work?

Not all patients are religious but I do think being religious gives me a comfort to talk to patients and help them connect with their faith and belief in order to get through their illness. Having a cancer diagnosis, people are vulnerable and anxious, and even if they’re not religious, they find solace in their religion and this helps me to have a dialogue. JN

Dr. David Tessler gets asked about “looking at people’s butts all day” on a regular basis, he said. But that is “not really what happens” during a colonoscopy.
“When the scope is in position and the exam is underway, I am looking at a video screen,” he said. “The entire colonoscopy procedure is performed with the utmost respect to a patient’s dignity.”
Tessler was in his rotation in gastroenterology as a medical student, and immediately knew that he had found his calling.

“Gastroenterology is a complex field of medicine that involves the perfect marriage of medical management of intestinal, liver and pancreatico-biliary diseases with the ability to perform endoscopic procedures to prevent, diagnose and often treat those medical problems,” he said.
He practices at Central Arizona Medical Associates in Mesa.
How do you approach patient care?
It starts with remembering that every patient is an individual, not a diagnosis. There is often a hidden agenda, something that concerns them and brings them to my office. There are a lot of cancers in the GI system and the possibility of a malignancy is often on my patients’ minds. For example. I really try to get to the root of their concern so an appropriate diagnosis can be made or I can ease their concerns when a cancer is not found.
What’s your favorite thing about what you do?
I really enjoy the hands-on aspect of endoscopic procedures. Moreover, I enjoy building relationships with patients. My favorite aspect of medical care, however, is those situations where you truly impact a patient’s life in a positive fashion. To experience the genuine appreciation by a patient for what I have done for them is worth all of the extra nights and weekends I have worked over the years.
What do you wish everyone knew about your job?
Medicine is a tough career and it’s not for everyone. Being on call, working weekends, being woken up at night all take their toll on a person. However, if you love what you do, as I do, there is no better profession than gastroenterology.
In what ways do you bring your Judaism to your work?
I practice medicine with three Jewish principles in mind.
G-d created man in his own image. To me, that underscores the sanctity of the human body. I do not take lightly the decision to perform any medical procedure.
Love thy neighbor as thyself. I make decisions about my patients’ care as if they were part of my own family.
Lastly, pikuach nefesh , the concept of the importance of saving a human life, helps guide many of my urgent decisions.
What were some of the biggest challenges you faced during this past year amid the pandemic?

At the start of the COVID pandemic, the first challenge was the uncertainty of it all. Would we be able to continue to see patients in person? Would we be able to continue performing endoscopic procedures for patients? Were we doing everything we could to make patients feel safe and comfortable? From a business standpoint we were concerned whether we would be able to keep our doors open and keep our staff employed and safe. From a personal standpoint, would I be able to continue to work seeing patients with COVID at the hospital on a daily basis, and keep my family safe?
How did COVID impact your day-today life as a health care professional? The majority of my medical practice involves outpatient work. With the decrease in elective procedures and office visits I spent more time working in the hospital. That involved more driving back and forth and required me to be more flexible with my schedule than
“The concept of the importance of saving a human life helps guide many of my urgent decisions.”
usual. Additionally, I was on call more often, meaning working more weekends. On top of that, there were more frequent meetings involving the hospital, office and ambulatory surgical center making constant adjustments to policies and procedures to ensure we were always putting patients’ safety and security at the forefront.

On a personal level, spending extra time with my children, who are both out of the house, was a blessing. That was special time that my wife and I never thought we would have again.



Professionally, the push for telemedicine has been great for many patients. It has allowed office visits in the safety of one’s own home. I also have patients who drive from all over Arizona

to see me. For some of them, telemedicine appointments can save a day off work and a four-hour-round-trip drive for a 30-minute appointment.

Although I always prefer to see my patients in person, telemedicine has a role and is here to stay.
One of the main disease states we deal with in gastroenterology is colon cancer. Colon cancer can be prevented by getting screened, which is the process of testing completely asymptomatic individuals. You do not need to have symptoms or a family history of colorectal cancer to be at risk. Everyone should be screened for colon cancer by colonoscopy or one of the other approved noninvasive tests. I see preventable cases of colon cancer all too often. Please get screened! It can save your life.
Dr. Rebecca Schaffer became a dentist simply because she loves taking care of people. Ever since she had a unique experience helping people with disabilities at a summer camp, she knew she wanted to help people who were often at the margins of society.

She’s volunteered in Guatemala with SPEAR education in Scottsdale, a foundation which has helped create infrastructure in that nation. And she’s especially happy about the way they’ve incorporated care for people with special needs in the country.
She’s also on the Ryan White Maricopa County committee for people with HIV as well as treating people with eating disorders.
“Schaffer’s heart has always been into caring for others, particularly those with special needs,” wrote one of Schaffer’s patients to nominate her. As a longtime Phoenix dentist, Schaffer cares for patients with special needs in her private practice and as a faculty member at the ATSU Arizona School for Dentistry and Oral Health in Mesa.
“Dr. Schaffer is the epitome of the best Phoenix has to offer,” continued the nomination letter. “She has improved the lives of countless patients in the Valley.”
Why did you choose your profession?
I became a dentist because I love taking care of people and it was a good fit for me. I specialized in treating patients with disabilities and complex medical histories because of a unique experience I had as a teenager when I worked at a camp for people with disabilities. The people I met in my role at the camp inspired me and I wanted to spend my life taking care of people who were underserved or marginalized.
How do you approach patient care?
Every single person is an individual with individual needs, and every single person is worthy of appropriate and comprehensive care.
People need to understand that there can’t be health without oral health; we can’t continue to separate the mouth and teeth from the rest of the body. We’re one organism and everything works together.
What’s your favorite thing about what you do?
All of it really. I also teach at AZ dentistry in Mesa and I love teaching.
I also specialize in a new specialty in oral facial pain. People have problems, headaches and pain in the face that’s not necessarily caused by teeth. This is a new specialty just recognized by the American Dental Association.
What do you wish everyone knew about your job?
I wish people would not be so afraid of the dentist. We’re not bad people. I wish people would take better care of their teeth, watch their diet and be more concerned about their health so they wouldn’t just come for problems. We just want to help people, but a lot of times they come when they’re already in so much pain it creates a difficult situation.
What do you think would surprise people most about your job?
People would be surprised knowing how much overall health is impacted by oral health and how much a healthy mouth contributes to a healthy body.
What were some of the biggest challenges you faced during this past year amid the pandemic?

There was an exponential increase in clenching and grinding and facial pain and stress-related pain problems. If I didn’t understand pain I wouldn’t have known how to help people.
And there was the challenge of reassuring patients it was safe to come to the office. So many challenges really. Keeping up with the science and helping people through an unimaginable time in history and then dealing with a lot of patients who lost loved ones.
“Every single person is an individual with individual needs, and every single person is worthy of appropriate comprehensive care.”Dr. Rebecca Schaffer PHOTO COURTESY OF REBECCA SCHAFFER
What are some of the ways you foresee your profession changing because of the pandemic?


For the most part I’m really proud of my profession. We provided a safe environment and complied with CDC guidelines, incorporating new ways, like teledentistry, for treating patients. Finding innovative ways to help people was necessary. It was predicted that dentists and hygienists would transmit the virus but it’s been very low.

I’m proud of us for stepping up to do what was necessary.
Was there anything good that came out of the pandemic?
Some people might have reassessed their values and what was important to them, but it’s been a pretty difficult time.
In what ways do you bring your Judaism with you to work?
As a small child I was raised in a Conservative home but now I’m Reform, and our primary goal is tikkun olam, and I live by that. That directs everything I do. I don’t know that I would be doing what I’m doing if it weren’t for my Jewish upbringing. JN

OVERNIGHT CAMP
Winner: Camp Daisy and Harry Stein Prescott AZ

NONPROFIT ORGANIZATION


Runner-up: Congregation Beth Israel, Scottsdale
PRESCHOOL
Winner : Chanen Preschool, Scottsdale
HEBREW SCHOOL
Winner: Mark L. Haberkorn Religious School

ALTERNATIVE SHABBAT SERVICE/PROGRAMMING
Winner: Congregation Beth Israel, Scottsdale

FAMILY-FRIENDLY SHABBAT SERVICE


Runner-up: Congregation Beth Israel

Bob Roth didn’t choose his profession in health care so much as it chose him. Before he founded Cypress HomeCare Solutions in Phoenix in 1994, he had a successful consumer product goods career, “and then, all of the sudden I became ‘an accidental caregiver,’” he said.

Roth’s mother suffered five heart attacks over a 24-hour period and was placed in a drug-induced coma. She also spent 30 days in intensive care. “It changed all of our lives,” he said.
When she came out of the hospital, she was a different person: Her heart didn’t function normally and she suffered from small cognitive deficits due to oxygen deprivation to her brain. She had been “the beacon and the North Star of our family, and everything revolved around her,” Roth said. Together with his siblings and his father, Roth cared for her the rest of her life. They all became experts on how to access limited home-care resources and the best practices for care giving at home.
Cypress HomeCare became the way Roth could help other families in a situation similar to his.
Maryglenn Boals nominated Roth because his team of caregivers offer support that allows people to remain in the comfort of their own home through illness or advanced aging. She called Roth “a pillar in the aging industry here in Arizona who is known throughout our industry as a valuable resource and a person committed to improving the lives of some of Arizona’s most vulnerable individuals.”
Making a difference in the lives of the people that we serve. It is an incredible feeling and an honor to be able to take the weight of the world off a loved one’s shoulders and let them know that you have it. So many people have lived such incredible lives, and to be there to assist them in their final years is truly a blessing.
I think people would be surprised just how good it feels to be able to help others, even if it is to listen and serve as an adviser. I love this about what we do.
To do this work, we acquired the assistive equipment so that we could have a full-service caregiver training lab on our premises, which we created in 2005. It is referred to as the Joan S. Roth Caregiver Training which provides training to caregivers and families in the community for free.
I have been at the helm as managing partner since December 2003. We have grown our agency to be one of the most respected caregiver
agencies in the state and in the country.
I am frequently looking for ways to innovate the home care business and recently joined the Honor Care Network of San Francisco to prepare for Arizona’s aging population. Within the next six years, an estimated 95,000 personal care aid job openings will exist. Joining the Honor Care Network will help meet that demand with access to more caregivers, new technology and operations support.
What were some of the biggest challenges you faced during this past year amid the pandemic?

The COVID pandemic consumed our lives all at once. There were many societal and business challenges that needed to be addressed, and if it were not for video, Zoom and the internet, the outcome of this pandemic could have been far different. Thank G-d it happened during 2020 and not 1990.
For me, the shift to a work-from-home routine was something we had already done nearly 10 months earlier when we joined the Honor Care Network. Moving from an in-person visit to video visits was a change, that while not ideal, worked out for us with our referral network partners. As for our care delivery operations it posed a challenge. There is no substitute to spending time with a client and their family in the safety and comfort of their home. An in-person consultation was a challenge for our care management team. We could do these virtually, but in-person required us to learn how to don and doff personal protection equipment, and make more of an abbreviated visit. In-person visits are the gold standard in assessing a client’s needs and it’s not unusual to be visiting with a client for an hour or more. During the pandemic our visits were no more than 20 minutes. Workforce was a challenge prior to the pandemic, and as a result of the lockdown, many of our care givers could no longer work for reasons that were related to their concern for getting the virus to having to be home to look after their children because the schools and daycare centers are closed.
In what ways do you bring your Judaism with you to your job?
I always think of tikkun olam — to heal and repair the world. There is no greater act of kindness than assisting the elderly, and to be able to do this is truly a blessing. We work to help one client, or should I say older adult, at a time. And the more we can assist, together we can heal the world. JN
“So many have lived such incredible lives, and to be there to assist them in their final years is truly a blessing.”Bob Roth PHOTO COURTESY OF BOB ROTH
When Jessica Levin-Bozek MA LPC was growing up, she knew she wanted to help people. But even though her mother, sister and brother all work in the mental health field, she didn’t consider counseling. Eventually, she followed her family’s lead, and now that she is a counselor with Jewish Family & Children’s Service, she couldn’t be happier about her decision.

“It’s about being passionate about what you do,” she said. “It’s not a job because it provides me with purpose and meaning and I feel grateful to do that. ”
Looking around, she sees how hard life is for some people, and said, “sometimes it’s nice to have a third party to reach out to for support.”
She hopes to reduce the stigma in mental health care as well. “It’s changing already. I feel we’ve come pretty far with big strides in exposure to the fact a lot of people experience anxiety and depression. We need to reach out for that just like any physical ailment. We want it to be normalized,” she said.
What’s your favorite thing about what you do?
I get as much from my clients as they do from me at times. I can continue to learn and grow as an individual. Awareness and insight are what this career has given me and exposure to different perspectives.
The continuing education is enjoyable. You want new strategies and ways to work with clients. I really enjoy that aspect. It’s about creating connections. Being a good therapist is having the right fit with your clients. It’s important that you both feel comfortable in the relationship in order to help them through the complications of everyday life. I’m grateful they allow me to be on the journey with them. It’s a beautiful profession.
What do you wish everyone knew about your job?
People are the expert for their own life. People have a great understanding of themselves and I bring out those insights and help them connect the dots. Then they have these beautiful epiphanies.
What were some of the biggest challenges you faced during this past year amid the pandemic?
Transitioning and adapting to a new form of counseling was tough. Being in a virtual setting or over the phone — virtually you can at least still get non-verbal cues but not on the phone. That’s been a little bit challenging. I would prefer physical meetings but this has taught us that you can do counseling
from home and it’s given flexibility to some of our clients who struggle with transportation or mobility. At JFCS my team goes to homes and sees clients. Not having the drive time allows us to schedule more appointments. But we have to be cautious to incorporate self-care so we don’t burn out ourselves. We want to be present for our clients.
What are some of the ways you foresee your profession changing because of the pandemic?

Virtual appointments will continue because it’s easier than taking time away from work or having to drive a long way to an appointment. Working with younger kids is more challenging virtually because I like to do hands on things with them. So, that’s more of a challenge. But with older teens it hasn’t been a barrier doing it virtually. Sometimes older adults have had the barrier of technology but they’ve learned and they feel more comfortable.
Being comfortable on Zoom, being yourself, can be difficult because you have to be present and you can see yourself on the screen so it takes time to get used to it.
Was there anything good that came out of the pandemic?
It reminds us as humans that we are adaptable. Even with something as catastrophic as this, we have the ability to look at things through a different lens. People spent more time with kids and families, more time reaching out to others even on the phone. We found new ways to socialize and reinvent ourselves. It took us to a place where we had to slow down in life. We’re focused on instant gratification, but this made us slow down.
We also asked our clients this about what they’re focusing on now that they didn’t before in our sessions.
I’ve been very blessed to have a family that values each others’ time and company. Just having a strong upbringing, and Judaism incorporates this, teaches that family and acceptance and togetherness is important, and we embrace that.
Having the cultural connection to my heritage is important. We don’t usually talk about religion, but if patients need the family or faith-based connection I can help with that, bringing together different pieces of the puzzle for them and getting them to the place they want to be, Judaism helps with that. JN
“Sometimes it’s nice to have a third party to reach out to for support.”Jessica Levin-Bozek MA LPC PHOTO COURTESY OF JESSICA LEVIN-BOZEK
Dr. Igor Yusupov’s mom died of cancer when he was just 10 years old.
“I think the calling to medicine stemmed from that experience,” he said.
In preparation for medical school, he did research at Mount Sinai Hospital where he worked with cardiologists and thought he would go into something dealing with cardiac disease. But, once in medical school he found his true passion was in surgical specialties.
“There’s just something about being in the anatomy lab, and dissecting a cadaver, which was a donated body that you have the privilege to touch and learn from, it was just a very touching experience,” he said.
As he went through school he discovered neuroscience “and it just blew me away.”
So, he put the two together and became a neurosurgeon. He founded Arizona Brain & Spine Center where he is a community neurosurgeon treating things like herniated discs, nerve impingement as well as neck and back pain.
Pediatric neurologist Tamara Zach, who nominated him, wrote “He has helped countless people with back pain” and “many patients have reported how talented and gifted this doctor is.”


When people need my services, it is already devastating on their personal life, their psychological well-being, their physical well-being, and so it’s a major milestone in their life. Once you realize how humbling It is to be part of that particular experience, you sort of change your attitude. I can’t just be a doctor because my specialty can be very cold and impersonal because it’s a surgical specialty on a very devastating problem. But it doesn’t have to be. Relating to them on a personal level is where I connect the best.
When I see my patients, I talk to them as human beings, not as a doctor, and they appreciate it. A lot of the medical jargon and the technical stuff that I would use will never be understood by anyone. It took me 17 years of training — there’s no way I can appreciate what a lay person knows anymore. And so I try to use normal language with them and just have a chat about what their life has been like and what I can do to help, and people seem to appreciate it.
What’s your favorite thing about what you do?
It’s the gratitude from seeing a patient’s life completely destroyed by their problem, and then they’re walking away a few days after surgery, and they get their life back.
What do you wish everyone knew about your job?
I think it’s important for people to understand that the more they know, the more they’re educated about their general health, about their body — it makes my job a lot easier. When a patient comes in, and they have some idea of how the body works and what ails them, it is a lot easier to understand what’s going on and how I may be able to help. A lot of my day revolves around education, because if a person who comes in seeking my help is not educated about their problem or the solution, it’s not going to be possible for me to convince them it’s the right thing to do. But once they’re educated, they make that decision.
What do you think would surprise people most about your job?
Unfortunately, spine care has been fraught with a lot of negative publicity and negative outcomes in the past. We have, as a community of neurosurgeons, changed that
“When I see my patients, I talk to them as human beings, not as a doctor, and they appreciate it.”Dr. Igor Yusupov PHOTO COURTESY OF IGOR YUSUPOV
drastically and the outcomes are actually excellent. Unfortunately, I have a lot of patients who are coming in for the first time and they’re very scared and very afraid of surgery. The surgery has become a non-threatening option. It’s not as passive as physical therapy, which is a non-surgical option, but at the same time, it is no longer what it used to be. So I hope people will become more and more accepting of what a surgical option can offer them, rather than delaying it until things become unbearable, because, in retrospect, everyone who has the surgery with me says, ‘I wish I’d done it years ago because of how easy it was to go through the process.’


So many people were devastated and some of them lost their loved ones — it’s hard to say something good came out of it. But I think what I see in the community, I appreciate: People are cooking more at home, they are exercising more, they’re more conscious about their health and well-being. JN

JEWISHAZ.COM




Hospice of the Valley, a not-for-profit, was founded in 1977 by a group of volunteers to provide comfort, dignity and compassionate care to the community.

Lin Sue Cooney, director of community engagement, said health care workers who choose a career in hospice feel it’s a calling.
“They want to walk alongside people during one of the most vulnerable times of life, and help them through each stage of their advanced illness with support, education and a deep desire to enhance their quality of life so they can enjoy the time they have left,” Cooney said.
The organization does not turn anyone who needs care away, regardless of insurance or financial circumstances.
Rachel Behrendt, senior vice president of operations, also highlighted how she brings her Jewish faith to the work she does.
What were some of the biggest challenges Hospice of the Valley faced during this past year amid the pandemic? Many of our patients live in facilities such as nursing homes and group homes. When COVID hit Arizona, families were not permitted to visit their loved ones in facilities or hospitals, even at the end of life. It was heartbreaking to see how hard this was for them. Hospice of the Valley
nurses were not only a ray of sunshine, they were a bridge between patients and family members. Fortunately, we also were able to safely convert three of our nine inpatient care homes into COVID units, so we could dress family members in PPE and allow them to be at the bedside of their loved ones. Another challenge, especially for dementia patients, are the surgical masks, shields and goggles that health care workers wear now. It’s harder to convey a smile when it’s hidden, so our care teams use their eyes and voices to convey their smiles now.
Personal protective equipment may become a more standard procedure as we experience different strains of highly contagious illnesses. This global crisis showed us how crucial it is to stay mission-focused and cultivate a strong culture foundation. It was our north star guiding us through the pandemic to meet challenges without losing quality or compassion to provide the care our patients depend on.
How does Hospice of the Valley approach patient care?
We strive to meet each patient where they are with their individual needs — physically,

“It is a privilege to care for people during a most sacred time.”Hospice of the Valley workers PHOTO COURTESY OF LIN SUE COONEY
emotionally, socially and spiritually, as well as to support family members. We do that with tender and skilled care, pet and music therapy, aromatherapy and companionship from volunteers. Our care teams laser focus on their wishes and try their best to make any last dreams come true if possible, like a special dinner, a bedside wedding or drive-by birthday celebration.




Our teams had to instantly learn new safety protocols, even before it was clear what kind of virus we were dealing with, yet they showed extraordinary courage and dedication, continuing to care for patients who needed us more than ever. Many patients and families were isolated without a support system and could no longer go out and get groceries, so staff let us know of essential needs and we started programs like emergency grocery shopping and delivery by our volunteers. The anxiety level of patients was high, so we created virtual and phone volunteer opportunities to provide support. Our staff was supported with mindfulness meditation classes and on-site help with self-care and wellness.
COVID required us to develop new systems — for staff safety and patient safety — and to develop new ways of connecting with patients and families. We needed to address multiple fears — anxiety about COVID and its impact — in addition to the fears that our patients and families experience on an end-of-life journey.


Many silver linings came from the pandemic. We appreciate the value of human connection even more. We rely on each other more for strength, support and encouragement. Teamwork, resilience, flexibility, innovation — all these things came into play. In the field of hospice care, we are very aware of how precious and sacred life is, but this was driven home during this long past year. There is no question that our entire staff is stronger, more mission-driven and
committed to providing compassionate care than ever. Every one of us has been changed to see such suffering and all of us are more devoted to easing it, with beautiful care and support.
The use of technology allowed people to stay connected. The rapid pace of vaccine development showed the strength of collective work and purpose in achieving a goal at a speed otherwise not attainable. And it helped many of us realize how much we take for granted. We suddenly understood the power of human connection and many of us will refocus on those connections as we fully emerge from the pandemic.
What should people know about working at Hospice of the Valley?
It is not sad or depressing. It is a privilege to care for people during a most sacred time and help them leave this life with comfort, dignity and peace in their hearts. That level of caring also extends to colleagues. The people here care about each other as much as they care about the patients and families we serve.
What would surprise people most about hospice workers?
Hospice workers are not only consummate professionals who happen to be kind and caring, they’re funny, clever, highly intelligent, creative,
motivated and just so much fun to be around. Many people would be surprised at the immense enjoyment and peace we receive in caring for our patients and families. We deeply value their trust in us.
In what ways do you, Rachel, bring Judaism to your work?




The Jewish values of tzedek (justice), tikvah (hope), kehilla (community), chesed (loving kindness) and refuah (healing) are present every day. We provide justice by serving all who come to us, regardless of their ability to pay and regardless of who they are. We provide hope by showing patients and families they are not alone as they journey in the final chapter of their lives. We want them to know that we are there to ensure their comfort and support them along the way. We provide loving kindness by treating everyone with love and compassion. And we provide healing by listening and supporting all through the journey and then afterwards, with bereavement care for families.
As an NIJH-certified Jewish hospice, we are proud that our values so closely mirror the values of Judaism. And we are equally proud to provide culturally compassionate care that is tailored to meet the needs of Jewish people on hospice. JN


Dr. Michael B. Lebowitz liked the idea of mixing medicine, art mechanics and engineering when he decided to become a dentist. But the biggest allure was “the luxury of dealing with people,” he said. “If you don’t like people, usually you become a surgeon, but if you want to relate with people, this is perfect.”
The long-term relationships Lebowitz has formed have been built over generations. His Phoenix practice originally opened in 1917, and he is the third doctor to own it in 104 years. “It’s not just worrying about today. I can look back at patients who have been here 50 or 60 years,” he said. “I can look at my predecessor and see what he did for 40 years.”
The real thing that sets him apart from other dentists, is that he feels a responsibility to be there for his patients and to help them manage care through their lifetime — not just for the moment.

How do you approach patient care?
My practice has a tremendous history, and we treat patients as generational. We make recommendations because we know how people respond and we know what happens over a lifetime. Sometimes it’s just helping people get by and you do what you have to to keep them going.
A couple of the families we see are four generations.
What’s your favorite thing about what you do?
My favorite part is that my patients are family after 30 years of doing this. It’s like watching your family grow up.
What do you wish everyone knew about your job?
It’s not all about us, it’s all about the patients. I’m lucky to have the luxury of that.
What do you think would surprise people most about your job?
We look at the whole person and their
overall habits and lifestyle — not just a tooth. We’re involved in all levels and we make referrals. We have the full conversation.
What were some of the biggest challenges you faced during this past year amid the pandemic?
The biggest challenge is after COVID hit, as a doctor and business owner, everyone is looking to us for answers and safety and you’re having to sift through all the information and put people at ease and keep them in a safe environment. Information would change day to day and they expect us to have the answers. Every day you’re filtering through the information to find safety protocols and other things.
I have to say we did a very good job. We implemented fogging, decontaminating and HEPA filters and we looked at air flow and advanced sucking procedures. We made changes and bought new equipment.
We never heard of fogging before, but it was something good because the virus travels through the air and this decontaminates the room within two minutes.
What are some of the ways you foresee your profession changing because of the pandemic?

In certain respects, a lot of this is not new. We dealt with this with AIDS. When I started we didn’t have to wear gloves. My second year in school, they were mandatory. There are certain things we’ve implemented that probably aren’t going away like HEPA filters to reduce viral load in a space. We didn’t really worry about that before.
Disinfectant foggers and taking temperatures may not be maintained, but it won’t go away quickly. Most of the protocols we’ve used are still critical. We always treat every patient as if they have every disease. We assume everyone has something. This virus is
“We look at the whole person and their overall habits and lifestyle — not just a tooth.”
very transmissible through the air, which is very different than the others.








Was there anything good that came out of the pandemic?
That’s a tough one. Not a whole lot I would say.
Personally, I controlled my schedule better and slowed down a bit. It made us control our day and patient flow better. It made us more aware of managing patients coming and going out of the office so it did help us take a look at when we were trying to do too much too fast. Patients became more accepting of time management.


In what ways do you bring your Judaism to work?




You give, not for recognition, but anonymously. You do it because that’s what you do, and that’s a basic premise of Judaism that I’ve always taken to heart. JN


Esther Lapin wanted to do something challenging for a career. She wanted to master a specialty in the health care field, as well as to make a meaningful contribution to the welfare of others. But she couldn’t decide where her path would lead.
So when a college adviser suggested respiratory therapy, she took the time to find out exactly what the job entailed. Happily, she has found in it a career she really enjoys and one that meets her duel goals of mastering a skill while helping people.

How do you approach patient care?
Every time I approach a patient, I try to imagine that this person is a close family member. This invariably guides my approach to the patient and drives my attentiveness and helps to ensure that I am doing all that can be done. I make sure to connect with the other health care professionals and discuss plan of care, just as I would if the patient were a family member, so we are all working together to ensure best patient care.
I need to be able to leave work and know that I did everything I could for my patients.
What’s your favorite thing about what you do?
The reward of seeing the positive results of my work, which is life sustaining for my patients and life affirming for me, is the best part. There really is no better feeling than seeing a patient in the ICU fighting for his or her life and then to see them on the general floor getting ready to walk out the door.
I had a patient recently, who went into cardiac arrest, needed CPR and was placed on a ventilator. We as RTs were at the bedside for every step. I walked into his room the next week on our general cardiac floor and there he was sitting up in bed, with no supplemental oxygen and fully alert. I was amazed and filled with joy. We were able to successfully sustain his life and the experience was so life
affirming for our team. We felt incredibly self-actualized.
What do you wish everyone knew about your job and what would surprise them?
As a trained RT, or any profession for that matter, the focus is so much on how good you are at what you do, and perhaps less so on who you are. And that profoundly impacts what you do and how well you do it. Particularly in the health care field, your human side and emotional strength greatly enhance how good you are in your job.
Our emotional resources are so often called upon, which we need to manage effectively. Working in a trauma center, there are many patients who come in and were fine one day, but for whom sadly we need to withdraw care the next due to the inevitability of death. We need to be able to hold ourselves together for other patients and each other while at the same time feeling grief for the failing patient’s family.
School does not train you for this. Our work is so much more than technicians and practitioners — we need to provide social, emotional and spiritual support to our patients, our teammates and ourselves.
What were some of the biggest challenges you faced during this past year amid the pandemic?

The work demand during the pandemic grew tremendously. My typically busy 12-hour shift suddenly became a blur of highly intensive activity, increased stress and urgent life and death decisions. The days were very long and emotionally and physically draining. One of the hardest parts was seeing patients who were completely alone with no family to comfort them or advocate on their behalf at their time of greatest need. It was terribly heartbreaking.
As a result, in addition to our medical roles, we became their family to the extent that strangers could substitute for family. We were the ones to sit by
“We need to be able to hold ourselves together for other patients and each other while at the same time feeling grief for the failing patient’s family.”
their side, hold their hand and, when they felt they could hold on no longer, whisper in their ear words of solace and comfort so that they knew they were not dying alone.
Another challenge was being there for my family and protecting them. It was immense pressure to make sure I did not bring anything home. My 4-year-old son came to understand that Mommy was not available to give him a hug and a kiss or sit down for dinner and hear about his day, until she was clean.
Finding the energy on my days off to concentrate on family time and be present was a challenge. Work was completely depleting, but I couldn’t forget my role as a mother and a wife and tried to make sure I was also at the front lines of those positions, as well.
What are some of the ways you foresee your profession changing because of the pandemic?


Pre-pandemic, RTs were somewhat the orphan-child in the medical team working behind the scenes with the cardiologists, pulmonologists and their supporting nurses taking center stage. The pandemic thrust RTs into the spotlight of the urgent care team and proved them to be an indispensable part of patient critical care.
Doctors and other health care departments now increasingly rely on us for patient care, advice and involvement.

Looking towards the future of the profession, I foresee RTs being more front and center in patient care and getting the acknowledgment and recognition that they so much deserve. Their input will be critical in patient evaluation and in deciding treatment regimens.
I foresee RTs collaborating more with other departments to help expand knowledge. Already, in our facility, we just opened a new operating room position; we have an RT assisting anesthesia in surgeries; and RTs are now being relied upon to put in certain cardiac monitoring IV lines. The pandemic really transformed the RT profession from an ancillary one to a primary care one. It will be interesting to see how this is reflected in RT training in schools.
Was there anything good that came out of the pandemic?
I believe that we must always look for the good in all situations even though it can sometimes be difficult to see that proverbial silver lining. In the case of the pandemic, with all the tragedy that I witnessed, I definitely can also see some good that came out of it.
People cherish family and friends more and the time they spend together. There were many unfortunate people who did not see any family members or friends in person for a whole year. This took an enormous toll on them and forced all of us to recognize how important surrounding
yourself with others really is.
Working from home also was a blessing in disguise for many who were able to be more involved in everyday living with their family. It helped them grow closer and put in perspective the richness they miss while not at home.
The pandemic also gave many of those who lost their jobs, a chance to recalibrate, refresh and restart.
For us health care workers, we got to be a part of something huge. We were on the frontline and were needed more than ever. We impacted so many and poured our souls into what we did. We all came out of this more humble, proud of our job and so grateful.
In what ways do you bring your Judaism with you to your job?

One of the lesser-known mitzvot in the Torah is Vehalachtah B’drachav — And you shall walk in G-d’s ways. (Deut. 28:9) This alludes to a human obligation to attempt to emulate G-d’s ways in order to become closer to Him. Just as he is merciful and compassionate, we too should make every effort to be merciful and compassionate.
My job allows me to practice mercy and compassion every hour that I am on the wards. This in turn strengthened my capacity for compassion thereby making me a better professional, wife and mother, while also bringing me closer to G-d. JN
Dr. Victor Zach describes neurology as “a perfect balance of science and medicine,” which is what drew him to the field.
He received his medical degree from State University of New York Downstate Medical Center College of Medicine, and completed a residency at Albert Einstein College of Medicine as well as fellowships in vascular neurology and neurocritical care at the Mount Sinai School of Medicine. He’s been in practice for 10 years and works at Neurocritical Care Stroke of Arizona in Phoenix.

Pediatric neurologist Tamara Zach, who nominated him, wrote “not only did he bring neurocritical care to the Valley 10 years ago — with its life-saving capabilities for stroke patients as well as trauma patients — but he also has developed several stroke centers. These centers have helped countless patients to recover and have received multiple awards for their excellence.”
Zach said he approaches patient care as an opportunity to help during a severe, neurological illness. “The focus is on getting ahead of the illness in a carefully planned out way,” he said. He also works to share his expertise with the patient and his or her family “by simplifying the complexities of the disease and the treatment.”
What’s your favorite thing about what you do?
The procedures are my favorite thing. One of them involves drilling a small opening in the skull and inserting a small tube into the patient’s brain in an effort to save them from a buildup of pressure. This is done when the patient is in a sudden coma after a severe trauma, stroke or bleeding into their head. Watching the patient then wake up from the coma days to weeks later is extremely satisfying when this occurs after such a procedure is performed to save them.
What do you wish everyone knew about your job?
Everyone should know that we have state of the art neurocritical care capabilities and that we are always available to patients in highly critical conditions. Our interventions work best when they can be accomplished within the first 24 to 48 hours after the patient has this onset of the severe neurological disease.
What do you think would surprise people most about your job?
Many would be surprised how good some of the patients look months to years after their initial neurocritical care illness. We have folks, especially younger people in their 20s to 40s coming back to us all of the time having survived gunshot wounds to their head, scary motorcycle and motor vehicle crashes and even a plane crash. We also have had younger patients with seemingly non-survivable bleeding into their brain make a very decent recovery.
What were some of the biggest challenges you faced during this past year amid the pandemic?
The largest challenge was the barrier of maintaining proper communication with the families of the critically ill patient while the hospitals were forced to restrict visitation.
What are some of the ways you foresee your profession changing because of the pandemic?
We have formed tightly-knit bonds with our ICU colleagues and anticipate that this teamwork will result in better overall outcomes for patients with non-COVID illness after the pandemic.
How did COVID impact your day-to-day life as a health care professional?

COVID added the challenge of a rapidly spreading, easily transmissible disease to the complexity of managing a patient with an emergent neurological illness. This is neurocritical care on “hard mode.”
the pandemic?
As strange as this may sound, the answer is yes. It feels like we have better camaraderie and even better communication amongst the different specialists within the ICU. We have all spent so much time there together that we have been able to learn more from one another and become better as a team.
If someone needed to reach out for a patient transfer from an ER or an ICU, their doctor can reach out to our transfer center at (480) 323-7363. JN
“Many would be surprised how good some of the patients look months to years after their initial neurocritical care illness.”
Brothers Dan and Tal Gafni opened Dental Brothers with their mom in mind. She was so afraid of going to the dentist she would have to be sedated for treatment.

“My training was to be able to take care of her,” said Dan Gafni. “But then what I found out is that really half the population is quite apprehensive.”
His practice is designed for so-called “high-fear patients,” with an atmosphere meant to make even the most frightened patients feel welcome and calm.
“How they feel and the kind of experience they get in terms of treatment helps them overcome their fear,” he said. In some ways, that’s the easy part. “We put time and energy and focus on it and they’re great again — but then it’s making sure they’re staying healthy, which is the hard part.”
He said it is most rewarding to see high-fear patients come into their hygiene appointments with a smile on their face, instead of tears.
John Liffiton, who nominated Dan and Tal Gafni, said “Dental Brothers make going to the dentist something natural and comfortable to do through their professionalism and their sincere interests in their patients on both medical and personal levels.”
Dental Brothers has a location in Mesa and another in Phoenix. Dan Gafni spoke on behalf of the practice.

Why dentistry?
I felt that dentistry would be able to provide what I was looking for: helping people and being able to spend time with them and have a real relationship with them. And a family-life balance, so I can still be there for my family and kids. I also love working with my hands. I come from a family of individuals that work with their hands. So it was just kind of the perfect scenario for me, and for my brother as well.
You mentioned forming relationships with patients. Tell me more about that.
There is a very intimate relationship between dentists and patients and outcomes. When someone finds a dentist, they’ll normally stay with them as long as they don’t fail them for the rest of their life. And they bring their kids and their grandkids.
How do you and your brother approach patient care?
In our logo it says “Family to family care.” We are a family-owned practice. My brother and I, my mother is the bookkeeper, and my dad was the architect of the practice and he’s also the handyman. We treat our patients like family.
Tell me your favorite thing about what you do.
It’s really that moment when those highfear patients look at their smile for the first time.
What do you wish patients knew?
There is a way to get them out of fear. These patients that are apprehensive feel like they’re stuck. Once they walk into our practice, they realize they have options, they’re empowered, they take action and then they get their joy back. So I guess a message to those patients is that there is a solution, there’s a way and that trauma and this fear that paralyzes them from taking action could be resolved.
How do you and your brother bring your Judaism with you to the practice?
It starts with our culture. It is inclusive and social. It’s about treating everyone in a certain way. And I think our employees really experience that and develop that mentality when they work in our practice. And growing up in Israel, serving in the military, it’s all about a team effort, community effort, uniting and working towards the same goal — and treating everyone like everybody matters. JN
“It’s all about a team effort, community effort, uniting and working towards the same goal — and treating everyone like everybody matters.”Dan Gafni, left, and Tal Gafni. PHOTO COURTESY OF DAN GAFNI
Immediate past president of the Arizona Medical Association, Dr. Ross Goldberg was front and center during the pandemic.
He worked with different parts of the state government to navigate the health crisis, and spoke with news outlets about what people needed to know to be safe.
“I was frequently meeting with state leaders and other stakeholders to find ways to mitigate the spread, do testing, do contact tracing, and once the vaccines were available, how to distribute the vaccines, how to get that message out to the public — so I got a lot of on-the-job media training to represent everyone,” he said.
It was a whirlwind year that included obtaining personal protective equipment from China for association members, lobbying and giving advice about vaccines and distribution.
Goldberg thinks telemedicine is here to stay post-pandemic, and maybe even some COVID-era safety protocols depending on the percentage of the population that gets vaccinated.
“I learned how vulnerable some of our systems are, and why we need to do better to have a stronger public health infrastructure in place, God forbid we ever have something like this again,” he said.
Goldberg is the vice chair of surgery at Valleywise Health in Phoenix and a District Medical Group surgeon. He discovered his passion for surgery during college.

While studying at Emory University he became an EMT and one of his close friend’s dad was head of Emory’s transplant center. When he was a junior, he shadowed him on the job.
“I went on a donor run as a junior college student, just to go with him and see what it was like to go get a liver. The second I walked in the operating room, I knew I had to be a surgeon,” Goldberg said.
We have the ability to really have a direct impact on someone. It’s, at times,
instantaneous: You come in with a problem, I’m gonna try to fix it and get you feeling better. It’s the trust. It’s an immense connection you have with people. I know people better than their families do, because I know them literally inside and out. If someone’s coming to me and asking me to take care of them, and putting their lives in my hands, it’s a tremendous honor. It’s a very humbling thing. And it’s wonderful to be able to take care of people. I really enjoy seeing people that we’re able to help. And then they come see us afterwards and are very thankful. It’s very fulfilling, I love doing it, and I love helping people.
How do you approach patient care?

We go out of our way to provide that evidence-based high-quality care for every patient, and work with the patient to find the best ways to provide that care.
What do you think would surprise people most about your job?
Well, the unfortunate thing is that there are a lot of TV shows about my job. They have been all over the place, but people may not realize one of the more accurate TV shows I’ve ever seen produced about what our lives are like is “Scrubs.”
I have fun at work, believe it or not, I enjoy what I do. Yes, we have music playing in the operating room at times. We are actually happy and it’s a big happy team in the operating room and we are working together to take care of someone.
In what ways do you bring Judaism with you to your job?
That idea that it is a responsibility to make the next day better, I think that’s a big tenet that runs through my daily existence as a physician and a surgeon. JN
“If someone’s coming to me and asking me to take care of them, and putting their lives in my hands, it’s a tremendous honor.”Dr. Ross Goldberg
















