Health in the Margins
IN THIS ISSUE
EDITORS-IN-CHIEF:
Kristen Ashworth
Nayaab Punjani
Kyla Trkulja
EXECUTIVE EDITORS:
Beatrice Acheson
Jasmine Amini
Kevan Clifford
Alyona Ivanova
Lizabeth Teshler
DESIGN EDITORS:
Ravneet Jaura (Co-director)
Jinny Moon (Co-director)
Qingyue Guo
Athena Li
Vicky Lin
Josip Petrusa
Raymond Zhang
PHOTOGRAPHERS:
Katherine Guo
Nancy Kim
SOCIAL MEDIA TEAM:
Lizabeth Teshler (Lead)
Lielle Ronen
Abigail Wolfensohn
JOURNALISTS & EDITORS:
Aria Afsharian
Stefan Aguiar
Tesam Ahmed
Yalda Champiri
Mya Chronopoulos
Sara Corvinelli
Anthaea-Grace Patricia Dennis
Clarize Donato
Mia Feldman
Sreemoyee Ghosh
Grace Gibson
Katherine Guo
Omar Hassan
Vanessa Ip
Hamzah Khan
Nancy Kim
Josephine Machado
Madeleine Matthews
Christina Pereira
Lielle Ronen
Rubab Shafiq
Steven Shen
Selina Tang
Kowsar Teymouri
Priya van Oosterhout
Abigail Wolfensohn
Saleena Zedan
By Vicky Lin, MScBMC
Letter from the EDITORS



Dear IMS,
Happy Fall!
As Nat King Cole sings, “The falling leaves drift by the window, The autumn leaves of red and gold.”
The falling leaves are definitely drifting by in beautiful colours across Toronto right now, and whether you’re admiring them from the window in campus library, at the lab, or in the hospital, we can all agree: it’s cozy season. Doesn’t it just make you want to curl up with a blanket, a hot cup of coffee, and something great to read? Luckily, we have the reading material for just that kind of day!
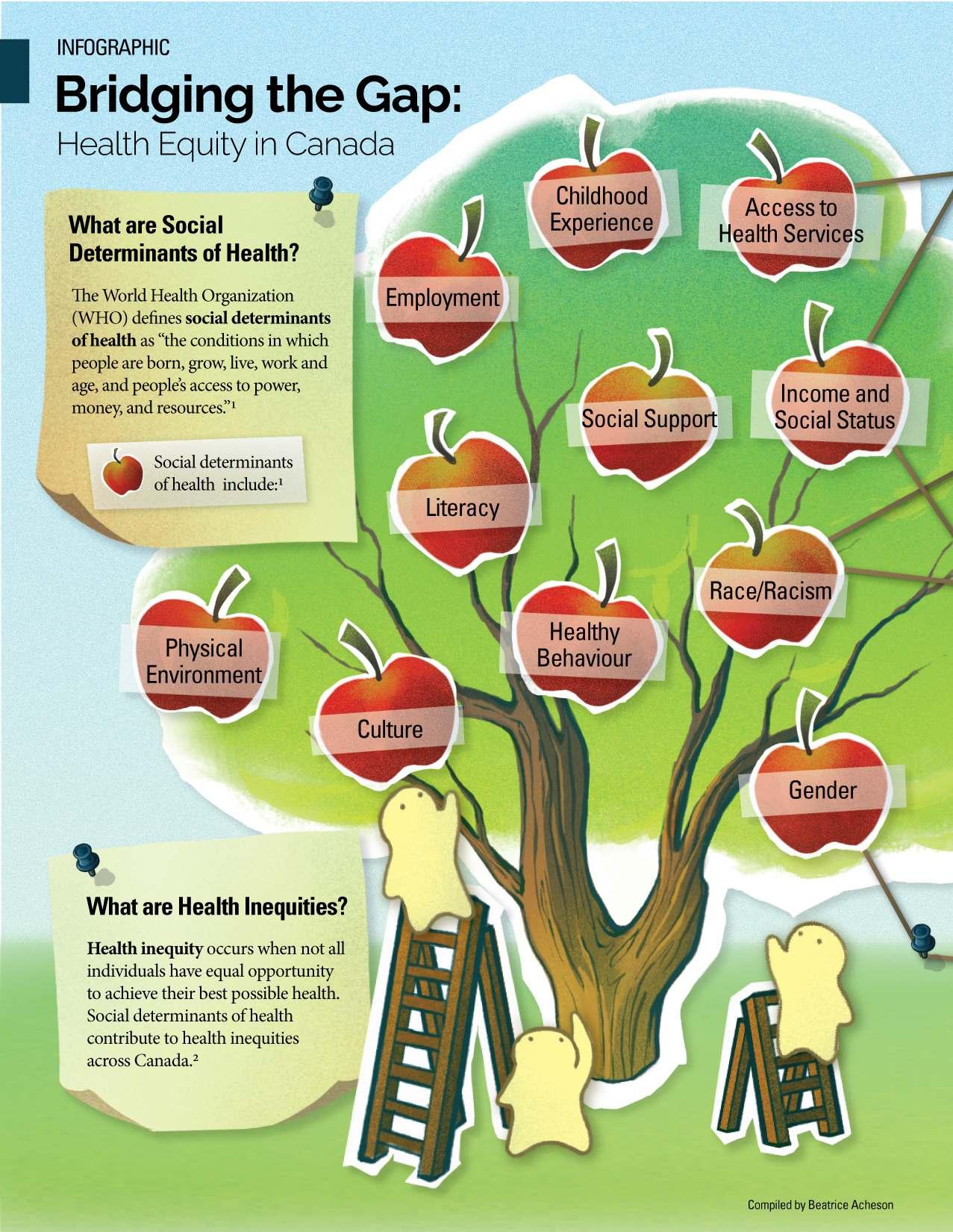
In our Fall 2025 issue of the IMS Magazine, we are excited to present the theme Health in the Margins. This issue shines a light on some of the most pressing challenges facing communities in Canada (and around the world) who have long been underserved or underrepresented in the context of healthcare policy, research, and in the clinical and hospital setting—including women, children, BIPOC individuals, LGBTQ2IA+, and other groups.
In this issue, we feature IMS faculty making significant inroads in this field right now, including Dr. Jenny Lau, who is working to break down barriers to palliative care access for those with substance use disorder; Dr. Sloane Freeman, who founded the Research Equity Advocacy in Child Health (REACH) School Network program to better connect school-aged children to health professionals; Dr. Flora Matheson, who is researching interventions to address the hidden determinants of homelessness, addiction, and criminal-legal involvement; and, Dr. Aisha Lofters, who is investigating the health inequities in cancer screening, including those related to income, race, and immigration.
Alongside this impressive line-up of featured faculty, our Viewpoint articles cover a breadth of topics that may spark some important conversations at the dinner table–from an early detection tool for ovarian cancer, to the current barriers to gender-affirming care; from seasonal affective disorder in racialized communities, to inclusive LGBTQ+ healthcare; and from the impacts of the water contamination in Canadian communities, to healthcare inequalities in our federal prisons.
We are also thrilled to spotlight two outstanding members of the IMS community—Nafia Mirza, President of IMS Students’ Association, and Dr. Anna Badner, an IMS alumna making big waves in the world of biotech.
A very warm welcome to our incoming 2025-26 team of designers, who have visually brought this issue to life—thank you, and we are grateful to have you join the team! And of course, a huge thank you to our talented team of journalists and editors, whose hard work makes all of this possible.
We hope you enjoy all of what this issue, and the changing season, has to offer!
With warmest autumn wishes,
Kristen Ashworth
Kristen is a PhD student studying the use of a human-based retinal organoid model to investigate cell therapies for genetic eye disease under the supervision of Dr. Brian Ballios at the Krembil Research Institute.
@K_Ashworth01

Kyla Trkulja
Kyla is a PhD student studying the mechanism of action of novel therapies for lymphoma under the supervision of Dr. Armand Keating, Dr. John Kuruvilla, and Dr. Rob Laister.
@kylatrkulja

Nayaab Punjani
Nayaab is a PhD student examining a neuroprotective drug therapy for cervical-level traumatic spinal cord injury at the Krembil Research Institute under the supervision of Dr. Michael Fehlings.
@nayaab_punjani


Interim
DIRECTOR’S MESSAGE
Dear IMS Community,
Welcome to a new school year!
I am delighted to welcome you to the Fall 2025 issue of the IMS Magazine, themed Health in the Margins.
This is an issue of particular importance, as it explores some of the most persistent health inequities affecting underserved groups in our society, including barriers to care, disproportionate burden of illness, and gaps in health policy and representation. At the same time, this issue highlights the exceptional efforts of members of our IMS community who are working tirelessly to address these challenges through innovative and inclusive research. Some of the featured faculty include Dr. Jenny Lau, Dr. Sloane Freeman, Dr. Flora Matheson, and Dr. Aisha Lofters—all of whom are doing groundbreaking work to improve health outcomes for marginalized communities. In addition, the Viewpoint pieces shed light on some of the most topical concerns in our healthcare system, including disparities in access to care faced by specific groups. In this issue, we are also proud to spotlight IMS student Nafia Mirza and IMS alumna Dr. Anna Badner for their exceptional leadership and accomplishments at IMS and beyond.
At IMS, our goal is to be a global leader in graduate education to improve human health. To do this, we must cultivate an environment that champions innovation, equity, and collaboration, and empowers our trainees and faculty alike to drive meaningful change in health research and care. This makes the topics covered in this issue especially significant, and I encourage you to engage with these important conversations, and to carry them forward within your own work as scientists, physicians, caretakers, leaders, and educators.
I would like to extend an enormous thank you to the journalists, editors, and designers of the IMS Magazine for their wonderful work, and to the Editors-in-Chief, Kristen, Kyla, and Nayaab, for their leadership in bringing the Fall 2025 issue to fruition. I hope the stories within these pages inspire our community to continue advancing equity, inclusion, and compassion in health research as we “turn over a new leaf” this fall.
Sincerely,
Dr. Lucy R. Osborne
Interim Director, Institute of Medical Science
DR. LUCY OSBORNE
Director, Institute of Medical Science Professor of Medicine, University of Toronto
Photo Credit: Dr. Lucy Osborne

Contributors Fall 2025

Aria Afsharian is a second-year MSc student at St. Michael’s Hospital under Dr. Andras Kapus. His research focuses on cell biology, specifically the role of signalling proteins in the antiviral immune response. Apart from the lab, Aria enjoys drawing, reading and working out.

Tesam Ahmed is a first-year MSc student working under the supervision of Dr. Daniel Felsky at the Centre for Addiction and Mental Health. Her research investigates the interaction between structural and functional brain changes and genetic factors to influence trajectories of psychosis in youth. Outside of the lab, Tesam loves to read, enjoy nature, and spend time with friends.

Yalda Champiri is a second-year MSc student under the supervision of Dr. Fehlings at Krembil Brain Institute. Her research focuses on enhancing respiratory function following spinal cord injury. She enjoys spending quality time with her puppies and exploring new restaurants when possible.

Sara Corvinelli is a PhD student supervised by Dr. Jacques Lee at the Schwartz/Reisman Emergency Medicine Institute. Her thesis is exploring innovative ways to improve delirium recognition for older people who seek emergency care. When she’s not researching, Sara enjoys ballet, nature walks, and spending time with loved ones.

Mia Feldman is a secondyear MSc student working under the supervision of Dr. Isabella Caniggia at the Lunenfeld Tanenbaum Research Institute. They are studying the placental-maternal crosstalk in cardiovascular diseases of pregnancy. In their free time, Mia enjoys reading and exploring different neighborhoods in Toronto!

Grace Gibson is a second-year MSc student in the Biomedical Communications program studying to become a medical illustrator. She aims to work in patient-facing media and outreach focused on the LGBTQ community. In her free time, Grace enjoys reading books and painting.

Omar I. Hassan is an MSc student transferring to PhD in the laboratory of Dr. Michael Fehlings. He studies neuromodulatory and regenerative strategies in spinal cord injury and has a particular focus on translation from laboratory to clinic. Currently his work is focused on restoring chloride homeostasis through repurposed pharmacological agents. Outside of the lab, he enjoys horology, falconry, and yapping over election politics.
omar_hassan1535

Vanessa Ip is finishing up their MSc working with Dr. Vicky Stergiopulos in General Psychiatry and Health Systems Division at CAMH. She is investigating the characteristics of forensic patients designated ALC in the last 5 years, the housing needs and preferences of this population, and their challenges and barriers to accessing housing. Aside from research, Vanessa has a passion for dogs, photography, and espresso.
vanessaaip

HamzahKhanisafourth yearPhDcandidateworking withsupervisorandvascular surgeonDr.Mohammad QaduraatSt.Michaels Hospital.Hisresearchfocuses onthediscoveryofnovelproteinplasma biomarkersforpredictingadversecardiovascular eventsinpatientswithvasculardisease.Outside ofresearchHamzahistheDirectorofPueblo Science,anot-for-profitorganizationthat focusesonincreasingscienceliteracyandcritical thinkinginruralandunderservedcommunities inCanadaandabroad.

Josephine Machado is a second-year MSc student working under the supervision of Dr. Andrea Knight at The Hospital for Sick Children. Her research is focused on examining the neuropsychiatric impacts of childhoodonset systemic lupus erythematosus (cSLE) through the study of brain-aging in children with the condition. Outside of research, Josephine enjoys reading, playing the piano, nature walks, and volunteering.

Lielle Ronen is a firstyear MSc student in Dr. Andrew Sage’s Lab at the Latner Thoracic Surgery Research Labs in PMCRT. Her research investigates smoking damage in donor lungs to improve post-transplant outcomes using Ex-Vivo Lung Perfusion (EVLP). Aside from research, she loves painting, baking, running and trying local restaurants in Toronto.

KowsarTeymouri isafourthyearPhDstudentworking underthesupervisionof Dr.JamesKennedyatthe CentreforAddictionand MentalHealth(CAMH). Kowsarisinvestigatingtheroleoftheimmune systemgenesinschizophreniaandhowthey areassociatedwithdifferentsubgroupsof schizophrenia.IfnotatCAMH,youcanfind Kowsartakingcareofherson, runningalongthe lakeshore,orcreatingcontentforhertravelblog. lady.kokolat



Priya van Oosterhout is a second-year MSc student working under the supervision of Dr. Yuliya Nikolova at the Centre for Addiction and Mental Health (CAMH). Priya is investigating how substance use disorders affect the way in which the brain ages, as measured by MRI data. In her free time, she enjoys trying new food, watching movies, or going on hikes.
priya.vo
Copy Editors
Tesam Ahmed
Aria Afsharian
Mya Chronopoulos
Sara Corvinelli
Anthaea-Grace Patricia Dennis
Clarize Donato
Sreemoyee Ghosh
Katherine Guo
Omar Hassan
Nancy Kim
Madeleine Matthews
Christina Pereira
Rubab Shafiq
Steven Shen
Selina Tang
Abigail Wolfensohn
Saleena Zedan
Photography Team

Katherine Guo is a second-year MSc student working under the supervision of Dr. Shannon Lange at the Centre for Addiction and Mental Health. Her work focuses on patterns of alcohol consumption and its related harms, aiming to betterunderstand the association between alcohol consumption and suicide mortality. Outside of her academics, Katherine spends her time working on various graphic design projects, taking photos, and exploring the wildlife in and outside of the city.

Nancy Kim is a first-year MSc student under the supervision of Dr. Amanda Boyle at the Center of Addiction and Mental Health. Her research focuses on neuroinflammation in different brain tumours originating from glial cells. She uses PET neuroimaging and histology studies to quantify neuroinflammation for early diagnosis and staging of these tumours. Outside of her research, she enjoys playing volleyball, exploring restaurants (mostly ramen places) and cafes (especially for matcha) near campus.
Social Media Team

Lizabeth Teshler (Lead) is a PhD student supervised by Dr. Brian Feldman at The Hospital for Sick Children. Her research investigates how to improve the clinical examination of musculoskeletal health for people with Hemophilia. Outside of research, she loves biking, spending time outdoors, and exploring new cities.

Abigail Wolfensohn is a second-year MSc student in Dr. Mojgan Hodaie’s lab at Toronto Western Hospital. She is researching how the brain’s waste-clearance system functions in people with trigeminal neuralgia, a chronic facial pain condition. In her free time, she enjoys outdoor activities, puzzles, trying new restaurants, and playing the piano.
abbywolfen


IMS Design Team
The IMS Design Team is a group of 2nd-year MSc students in the Biomedical Communications (BMC) program. Turning scientific research into compelling visualizations is their shared passion, and they are thrilled to contribute to the IMS Magazine


ravneetjaura.com





Vicky Lin
Breaking the Stigma
Working Towards Equitable Palliative Care for People Who Use Drugs

By Lielle Ronen
Prior to the pandemic, people with opioid use disorder (OUD) were 33% less likely to receive palliative care in their final three months of life, with the gap widening to 45% during the COVID-19 period.1 Prescription opioids are essential in managing symptoms, such as pain and shortness of breath, in palliative care.2 Clinical guidelines emphasize the use of opioid therapy to relieve suffering experienced by patients with life-threatening illnesses.3 Despite the central role of opioids in providing relief during palliative care, many people who use(d) drugs face inequitable access to palliative care due to stigma from healthcare providers, restrictive prescribing practices, social inequities, and past negative experiences when accessing the healthcare system. These gaps raise significant questions, such as how healthcare systems can ensure that marginalized populations receive equitable, compassionate, and high-quality care up until the very end of life.
Dr. Jenny Lau, a palliative care physician, clinician-investigator, and medical director of the Harold and Shirley Lederman Palliative Care Centre at Princess Margaret Cancer Centre, focuses on developing strategies to deliver palliative care to marginalized populations. Dr. Lau completed her residency in family medicine at the University of Ottawa, followed by palliative care training at the University of Alberta. She then joined the University Health Network as a
palliative care physician and scientist. After witnessing the many challenges people who use(d) drugs encounter in the healthcare system, she pursued a Master of Science with a Collaborative Specialization in Addiction Studies through the Institute of Medical Science at the University of Toronto. Since that time, Dr. Lau and her research coordinator, Rebecca Bagnarol, have established a research program focused on addressing OUD in the context of life-threatening illnesses.
Dr. Lau’s research inspiration is rooted in her clinical practice, where she has observed inequitable access to palliative care for patients with a history of drug use. People who use(d) drugs are often denied access to opioids during end-of-life care due to healthcare provider fears of relapse and non-medical opioid use,4 and these barriers are compounded by additional challenges, including complex medical histories and social inequities like poverty and homelessness. She explains, “One of the goals [of her research] is to try to get a more comprehensive understanding of the needs of this patient population and to identify the gaps that they face.”
To do so, Dr. Lau partnered with Dr. Sarina Isenberg at Ottawa’s Bruyere Research Institute to use the Institute for Clinical Evaluative Sciences (ICES) provincial database to assess palliative care delivery for people with OUD, while also interviewing patients with life-limiting illnesses and OUD, their caregivers, and health care providers to better understand
their palliative care experiences. Her most recent study found that people with OUD are receiving significantly less palliative care in the last 90 days of life compared to those without OUD, especially in clinics and homes.1 The results of the study highlight the need for innovative solutions to improve palliative care for this patient population. Dr. Lau hopes to establish more tailored models of care to address medical and social needs, as well as to implement clearer guidance for clinicians to safely prescribe opioids to individuals with OUD receiving palliative care.
Dr. Lau utilizes her expertise in various clinical settings within the Princess Margaret Cancer Centre, including the outpatient palliative care clinic, inpatient palliative consultation service, and the tertiary palliative care unit. She provides care to a wide range of patients with advanced cancer, from those still in treatment to those at the end of their lives. Inspired by her interactions with patients, Dr. Lau views research as an advocacy tool. She explains, “Through my clinical practice, I identify problems that typical clinical care can’t fix, and these problems are usually systemic problems related to the delivery of healthcare.” She noted that change is underway, and adds, “Through my research, I have an opportunity to try to make a meaningful difference, to try to make a change to the care that I provide to my patients and to advocate for system-level changes.” In practice, this means amending policies and


Dr. Jenny Lau, MD, MSc Clinician-Investigator, Princess Margaret Research Institute; Clinician-Investigator, Division of Palliative Care, Department of Family and Community Medicine, University of Toronto
guidelines that exclude people who use(d) drugs, collaborating with community organizations to make palliative care more accessible, shaping clinical care to improve opioid prescribing practices, and ensuring patients with life-limiting illnesses receive adequate symptom relief. She has found that patients with OUD are more likely to access palliative care in an acute care setting.1 Care providers in acute settings can better assist with the identification and management of structural vulnerability and OUD. Moving forward, Dr. Lau hopes to build on her previous projects that have identified gaps in patient care, equipping acute care providers with the tools and
resources to improve the delivery of palliative care for this patient population.
Additionally, Dr. Lau is examining equity in cancer care for people with a history of drug use. These patients frequently experience poverty, homelessness, and mental health challenges, making it difficult to navigate a system that assumes stable housing and social supports. Dr. Lau is collaborating with Dr. Melanie Powis, scientific director for the Cancer Quality Lab at Princess Margaret Cancer Centre, to identify the structural barriers to equitable cancer care access for these individuals and develop potential solutions on how to overcome them. To do so, she is engaging with people with lived experiences of cancer and drug use, as well as key individuals and organizations. For example, Drs. Lau and Powis are collaborating with the Toronto Harm Reduction Alliance to conduct their project and to engage people who use(d) drugs to improve cancer care for them. Meaningful community engagement is a pillar of Dr. Lau’s work. She highlights, “It all boils down to working with the community, listening to the community and meeting them where they’re at.” In more ways than one, Dr. Lau works with vulnerable populations and centers her work around the voices of those with lived experience.
Dr. Lau specializes in breaking systemic barriers for these underserved populations receiving palliative care, but we all serve a role in achieving these goals and decreasing the stigma associated with OUD. Dr. Lau
emphasizes the importance of interacting with the population she intends to serve, stating that, “The easiest thing that you can do is to treat these people like humans, with respect and dignity.” She highlights the power of language to help people who use(d) drugs feel more welcome when receiving health care. The use of nonstigmatizing language to describe drug use and substance use disorders is a simple strategy that all healthcare professionals can adopt. Through her work, Dr. Lau challenges the notions associated with conventional stereotypes of people who use(d) drugs and encourages people to exercise compassion, curiosity, and a desire to understand an individual’s circumstances. Dr. Lau strives to create a more welcoming and compassionate healthcare system for marginalized populations, moving beyond judgment and towards equitable palliative care.
References
1. Lau J, Scott MM, Everett K, et al. Association between opioid use disorder and palliative care: a cohort study using linked health administrative data in Ontario, Canada. CMAJ Canadian Medical Association journal. 2024 Apr 28;196(16):E547–57.
2. Cleary J. Essential medicines in palliative care. Palliat Med. 2014;28(4):291-2. doi:10.1177/0269216314527036
3. World Health Organization. Cancer pain relief. 1986 Available from: https://apps.who.int/iris/handle/10665/43944
4. Witham G, Yarwood G, Wright S, et al. An ethical exploration of the narratives surrounding substance use and pain management at the end of Life: A Discussion Paper. Nursing Ethics. 2019 Sept 16;27(5):1344–54. doi:10.1177/0969733019871685
Photo Credit: Dr. Lau

By Aria Afsharian
Around 20 to 30 percent of Canadian children have a mental health or neurodevelopmental problem.1 Children with social inequities often experience barriers accessing health care and are less likely to receive early interventions for neurodevelopmental and mental health problems. This issue was further exacerbated by the COVID-19 pandemic, which saw increased demand for mental health services as well as increased wait times for seeing healthcare professionals.1 There are major systemic barriers that prevent school-aged children from accessing appropriate care in Canada. One innovative method for alleviating these barriers is by bringing healthcare into the schools.
This is the mission of the Research Equity Advocacy in Child Health (REACH) School Network, as discussed in our interview with its founder, Dr. Sloane Freeman, a pediatric physician at St. Michael’s Hospital and Associate Professor in the Department of Pediatrics at the University of Toronto. One of the pillars of St. Michael’s Hospital is its focus on at-risk populations. Pediatrics is an extension of this focus, as children from these disadvantaged families may face further psychosocial problems, especially at school. When asked what drove her towards pediatrics, Dr. Freeman explained, “One of the unique things about pediatrics is the population. Having the opportunity to intervene early in the life course of an individual is very rewarding, especially when you can make meaningful differences

REACHing New Heights: Bringing Healthcare into the School
that impact their future.” This sentiment motivated Dr. Freeman to start the REACH program, a system that connects school children to health professionals.
Schools emerge as a natural environment to connect children with healthcare. Children spend much of their daily time at school, and there is an established system of trust in place between the school system and families. As Dr. Freeman put it, “Merging healthcare and education allows us to overcome many barriers that families may face.” Prior research supports the association between low socioeconomic status (SES) and poor academic outcomes, psychiatric disorders, and chronic health problems in children.2 These same marginalized families also have the greatest difficulties accessing healthcare.3,4 School-based health is not new, with the United States having over 4,000 SchoolBased Health Centres (SBHCs), mostly serving low SES families.1,3,4 Research on American SBHCs have shown an improvement in vaccinations, quality of life, and academic performance, as well as lower hospitalization rates.2 In Canada, SBHCs are emerging as potential avenues for connecting underserved children to healthcare providers.
The REACH School Network is a collaboration between Unity Health Toronto’s hospital networks and the Toronto District School Board (TDSB). Currently the program has two physical SBHCs: one at Nelson Mandela Park Public School, serviced by St. Michael’s
Hospital, and the other at Parkdale Public School, serviced by St. Joseph’s Health Centre. These schools act as hubs, supporting over 150 additional schools to help connect children with mental health and developmental problems to pediatric health care. The centres are staffed by family physicians, pediatricians, therapists, and patient navigators.3 This physicianled team diagnoses and treats mental health and neurodevelopmental disorders, and collaborates with allied health professionals who provide counseling, and direct families to accessible community resources.3 Students are referred to the REACH clinics by school staff, parents, or the School Support Team (SST).3 The SST includes psychologists, social workers, teachers, and other school staff who meet monthly to discuss student wellbeing, and whether individuals’ behaviour or mental health warrants a referral to the program.3 This system is designed for the delivery of precise care to students who need it, allowing for faster, more accessible diagnosis, treatment, and support.
3
Dr. Freeman notes that since REACH and similar systems are still relatively new in Canada, feasibility studies are only just emerging, and additional research is needed to make conclusions about the efficacy of the program. A recent pilot study on the REACH program examined the feasibility of Coping Power, an evidence based cognitive behavioural intervention method, on the mental health of children.1 The 10-week program aimed to improve children’s social competency


the SBHC setting, which was unexpected given that boys are usually diagnosed at a higher rate, likely due to them displaying more obvious symptoms that help with early recognition compared to girls.2 It is believed that the increased accessibility of SBHCs may improve the detection of psychosocial disorders in girls that would otherwise be overlooked.2
can the REACH program continue its mission in connecting children with health professionals. Increased governmental awareness and visibility are necessary to ensure the continued delivery of accessible and efficient care for our most vulnerable patient populations.
and self-regulation. At the end of the study period, parents/guardians were asked to fill out a follow-up survey.1 13 out of 18 participants (parent/guardianchild dyads) who completed the program and the survey reported being somewhat or very satisfied with the program.1 An earlier retrospective feasibility study on SBHCs reviewed the charts of 379 children enrolled at a SBHC over one year.2 Most children were from low-income families whose first language was not English.2 Of the 127 children who attended the clinics, 74% received a new diagnosis and 90% received a treatment plan.2 Interestingly, more girls were diagnosed than boys in
It remains unclear whether SBHCs impact children’s academic outcomes. A recent quasi-experimental prospective cohort study on 14 TDSB schools compared measures of academic achievement between students who had access to SBHCs and those who did not during the 2016/2017 to 2018/2019 school years.3 While there was insufficient evidence to show a difference in grades, many children who accessed the SBHCs received a new neurodevelopmental diagnosis.3 Several limitations in this study, including COVIDmediated school closures, further the need for additional research on the matter.3
Nonetheless, Dr. Freeman’s passion for the vast potential and importance of the REACH program is evident. She explains that “In a perfect world, in the next decade, the program will expand. More health centres will be built, allowing us to expand throughout Toronto.” The biggest limiting factor to this expansion is funding; “Bringing this to the attention of the government and Ministry of Health is critical for our program’s sustainability,” Dr Freeman says. Only with sustained funding and support
References
1. Rasiah S, Andrade BF, Cohen-Silver J, et al. Coping Power at the REACH School Network: A pilot feasibility study. Paediatrics & Child Health [Internet]. 2024 Nov 17 [cited 2025 Aug 14];29(8):493–500. Available from: https://doi.org/10.1093/pch/ pxae060
2. Freeman S, Sgro M, Wormsbecker A, et al. Feasibility study on the Model Schools Paediatric Health Initiative pilot project. Paediatrics & Child Health. 2013 Aug;18(7):361–5.
3. Rasiah S, Jüni P, Sgro MD, et al. School-based health care: improving academic outcomes for inner-city children—a prospective cohort quasi-experimental study. Pediatric Research [Internet]. 2023 Feb 8;(94):1488–95. Available from: https://www.ncbi.nlm.nih. gov/pmc/articles/PMC9907190/
4. Freeman S, Sgro M, Mamdani M. Novel approach to health care delivery for inner-city children. Canadian Family Physician. 2013 Aug;59:816–7.

Dr. Sloane Freeman, M.D., FRCPC, MSc., UofT Department of Pediatrics
Photo Credit: Dr. Sloane Freeman
Diving into Hidden Drivers and Fragile Supports in Marginalized Populations through Flora Matheson

By Omar I. Hassan
As a liberal democracy that is shaped by social democratic values, Canada carries the duty to safeguard not only the rights of its citizens but also uphold the dignity of its most marginalized. In the face of rising homelessness,1 addiction,2 and overrepresentation of racialized individuals in the criminal-legal system,3 Canada is losing ground in upholding its own values. These issues signal major systemic failures. It is precisely in this context that researchers focused on inequities intersecting with social determinants of health become critical. Dr. Matheson, a sociologist and the Endowed Chair in Homelessness, Housing, and Health at Unity Health Toronto, recounted her experiences growing up in Prince Edward Island in a small village where there was “a lot of differentiation based on income status.” Her experience inspired her to determine the origins of these disparities. With a vested interest in addressing societal inequity, Dr. Matheson combines academic rigor and community collaboration to uncover the drivers of these systemic failures and develop innovative interventions.
Dr. Matheson provides novel and compelling new perspectives to examine inequities. She has developed a career centred around community-engagement in research that bolsters academic inquiry through lived-experiences. Instead of imposing research questions in a top-down manner, Dr. Matheson engages in dialogue with local organizations such as homeless shelters and advocacy groups to orient her research. This strategy allows her to uncover the hidden causes of marginalization.
Her significant collaborations with the Good Shepherd Ministries resulted in the first Canadian shelter-based study tying gambling to housing instability.4 The later development of the Problem Gambling App (SPRinG app) showed a novel method to extend gambling supports digitally to those without stable housing. Furthermore, Dr. Matheson has found brain injury (BI) rates to be a hidden, yet determining factor, in criminal-legal involvement–pushing for policy implementation and greater accommodation. These initiatives exemplify the strengths of Dr. Matheson’s work, which is not only scientifically rigorous but also vertically integrated in community needs.
In 2013, Dr. Matheson launched a landmark research project in collaboration with the Good Shepherd Ministries men’s shelter in Toronto. Her project revealed a troubling gap: despite a focus on services for substance use, mental health, and housing, gambling remained an unrecognized driver of homelessness. Acting on this concern, Dr. Matheson and her team conducted the first shelter-based prevalence study in Canada. Of the 264 clients interviewed, 35% reported problems with gambling, compared to just 4% in the general population.5 The nine-fold difference suggests that gambling is likely a strong contributor to housing instability. Acting on these results, Dr. Matheson and her team supported the establishment of the Gambling Addiction Program (GAP) by the Good Shepherd Ministries. Funded by the Local Poverty Reduction Fund, the three-year GAP intervention offered case management, cognitive behavioural therapy,
and support from Gamblers Anonymous (a standalone self-help group).4 Dr. Matheson recalled fondly that “clients showed great enthusiasm and described GAP as uniquely supportive and understanding of their environments and experiences.” Despite these positive responses, this program was discontinued due to a lack of funding, a recurring theme that exposes the fragility of our current program-based government models. Dr. Matheson’s work bolsters community driven priorities but is constrained by short-term policy cycles.
Building on her shelter-based research, Dr. Matheson increased outreach through digital innovation, reaching marginalized populations on a larger scale. The SPRinG (Supporting People Recovering from Gambling) app was designed by Dr. Matheson and her team to provide “flexible, accessible support for individuals experiencing problem gambling, particularly those who did not have stable housing or found themselves underserved by traditional [in-person] treatment programs,” she said. The app used evidence-based tools derived from cognitive behavioural therapy and provided easier access to educational resources and support/crisis networks.4 The design reflected a curious insight from Dr. Matheson’s work: while homelessness is often associated with disconnection, many unhoused individuals use smartphones, allowing for digital equity interventions. The SPRinG app extended care beyond the shelter walls, and provided useful resources for unstably housed individuals, mitigating risk of homelessness. Like the

(This is for spotlight photos! Delete this later.)

solutions to directly address service gaps but remain vulnerable to structural issues.
Good Shepherd initiative, the program was discontinued when funding expired. Dr. Matheson explained that, despite promising results, “The SPRinG app has sprung; we had to decommission the app as we could not find additional funding to keep it going. We built it with our community partners and people with lived experience. We tried to get funding through the [gambling] industry and through Government options; we even participated in the University of Toronto Early-Stage Technology (UTEST) program.” Despite promising feedback, the program was cut short due to a lack of long-term funding sources. Dr. Matheson’s approaches are innovative and provide community-informed
Alongside her work on gambling, Dr. Matheson has pushed frontiers in inequity research within the criminal-legal system. By documenting BIs in people who are incarcerated, she and colleagues found that young adults with a history of traumatic BI (those caused by external blows to the head) were over 2.5 times as likely to experience incarceration than those without, and the trend impacts both men and women.6 Further, her research found that the prevalence of these injuries increased the risk of a serious disciplinary charge by 39%.7 BI limits individuals’ abilities to navigate the criminal-legal system, from police questioning to hearings, and increases the chance of cyclical incarceration. Despite these findings, Dr. Matheson noted that “we have very few brain injury services available in Ontario with long wait lists and many of them require a formal diagnosis of brain injury to access care.” She also remarked the difficulty in getting such diagnoses, “leaving many people without access to care.” Despite this, Dr. Matheson remains hopeful. She said that with more “funding and training we can see improvement.” She continues her research in the hopes of her advocacy shaping structural change. Dr. Matheson’s findings have informed policy discussions in Ontario with calls to include BI screening in with correctional health records. This way, Dr. Matheson has ensured that her research uncovers more hidden inequities while seeking to mitigate system-level shortcomings to address such inequities.
Dr. Matheson’s work demonstrates the strengths and vulnerabilities of community-engaged health research in Canada. Whether through GAP, SPRinG, or BI screening, Dr. Matheson exemplifies a consistent pattern: her research is empirical, rigorous, community-focused, and promotes equity. These successes, however, are often dampened by programbased funding cycles. In the face of these challenges, Dr. Matheson remains determined to “keep plugging away at it” even if “our government has expanded the number of prisons rather than community healthcare.” Dr. Matheson has proved the value of her research through effective interventions, but the premature discontinuation of these programs underscores the urgent need for sustained structural investments in solutions for marginalized communities. Without such investments, Canada risks allowing further innovative and community-centred progress to wither.
References
1. Statistics Canada. Homelessness: How does it happen? (2023).
2. Miller J and Carberg C. Addiction Statistics Canada (2025).
3. Office of the Correctional Investigator. 2020-2021 Annual Report (2022).
4. Matheson FI, Hamilton-Wright S, Hahmann T, et al. Filling the GAP: Integrating a gambling addiction program into a shelter setting for people experiencing poverty and homelessness. PLOS ONE 2022.
5. Matheson FI, Devotta K, Wendaferew A, et al. Prevalence of gambling problems among the clients of a toronto homeless shelter. J Gambl Stud 2014. DOI: 10.1007/s10899-014-9452-7.
6. McIsaac KE, Moser A, Moineddin R, et al. Association between traumatic brain injury and incarceration: a population-based cohort study. CMAJ Open 2016. DOI: 10.9778/cmajo.20160072.
7. Matheson FI, McIsaac KE, Fung K, et al. Association between traumatic brain injury and prison charges: a population-based cohort study. Brain Injury 2020. DOI: 10.1080/02699052.2020.1753114.
Dr. Flora Matheson
Associate Professor at the Dalla Lana School of Public Health, the Institute of Medical Science, and the Centre for Criminology & Sociolegal Studies at the University of Toronto.
Photo Credit: Dr. Flora Matheson
Cancer Screening Inequities in Ontario
The Work of Dr. Aisha Lofters
By Kowsar Teymouri
Cancer is a leading cause of death in Canada, with one in every 2.2 Canadians expected to be diagnosed with cancer in their lifetime.1 Cancer screening has been proven to reduce cancer morbidity and mortality rates;2 thus, it is a crucial part of primary care in Ontario.3 Despite efforts to provide comprehensive cancer screening for the entire population at no cost, there are well-documented inequities across Ontario, especially for people of low socioeconomic status, people living in low-income neighbourhoods, and immigrants. These complex barriers exist at the level of the patient, provider, and overall healthcare system.
Dr. Aisha Lofters, a family physician and clinician-scientist at Women’s College Hospital, and an Associate Professor at the Institute of Medical Science and Dalla Lana School of Public Health, has dedicated her research to investigating health inequities in cancer screening. Social justice was always at the forefront of Dr. Lofters’ upbringing, which cultivated her strong interest in addressing inequalities, regardless of the career path she chose.
After obtaining her medical degree at the University of Maryland, Dr. Lofters completed her residency and fellowship in family medicine at the University of Toronto (UofT). Dr. Lofters was interested in family medicine as it prioritizes powerful, but simple tools:
prevention and screening. Dr. Lofters believes that while cancer treatment is important, “catching it early can really change the trajectory of someone’s life.” During her residency, Dr. Lofters, under the supervision of Dr. Rick Glazier from St. Michael’s Hospital, investigated cervical cancer screening in areas with higher proportions of new immigrants and low-income individuals. This project inspired her to pursue her PhD in Clinical Epidemiology and Health Care Research at UofT and later become a clinician-scientist.
Dr. Lofters’ research aims to answer the fundamental question: “Where are the inequities in care?” To do so, she leverages quantitative methods on population-level data to address where and for whom these inequities in cancer screening exist. Then, she implements qualitative methods to gain a deeper understanding of why these disparities exist and eventually identify solutions for alleviating them. Dr. Lofters believes there is an interplay between discrimination on the bases of income, race, and immigration, which contribute to these disparities—highlighting the underlying theme of health equity in her work.
Dr. Lofters’ work has a particular focus on cervical cancer screening. Her studies have demonstrated that immigrant women who are newer to the country, as well as those living in low-income neighbourhoods, had lower uptake of available screening programs.4 Screening
rates also varied among immigrant women, with the lowest rates observed in South Asian, Middle Eastern, and North African women. Considering Ontario’s universal healthcare system covers the direct financial cost of cervical cancer screening, understanding the indirect costs that prevent usage in these populations is important. To address this, Dr. Lofters, in collaboration with Dr. Mandana Vahabi, has conducted qualitative studies on Muslim women from the aforementioned countries.4,5 Cultural barriers pertaining to modesty and privacy—particularly with limited same-gendered providers—as well as access to transportation and childcare, limit visitations. Furthermore, some patients lack access to a general practitioner and have limited knowledge about cervical cancer screening, restricting their ability to self-advocate. In some instances, patients didn’t have the opportunity to be screened as the test was not offered to them. This study highlights key patient, and importantly, practitioner factors which are important to consider when determining the effective uptake of screening programs.5,6
Human Papillomavirus (HPV) infection is responsible for nearly all cervical cancer cases.7 Ontario Health recommends conducting an HPV test as part of its cervical cancer screening program.8 However, the experience of having a healthcare provider collect a vaginal swab could be traumatizing or
Looking at immigrant health is looking at the health of our population. “ “

uncomfortable for some women, which may discourage them from undergoing screening. HPV self-collection kits offer an alternative which allows patients to collect the swab at home. Currently, HPV self-collection kits have been implemented in British Columbia, Australia, and parts of Europe. Dr. Lofters has studied the acceptability and uptake of these kits in Ontario and is currently investigating the most effective ways to implement them into the province’s cervical cancer screening program. 9
In addition to the concerns associated with the screening process, some patients also delay seeking care following a previous
unpleasant experience with the healthcare system or a lack of knowledge about the symptoms. Dr. Lofters said that “in Canada, cancer is not a death sentence.” In fact, two in five Canadians will develop cancer over their lifetime, and only one in five will die from it.10 Healthcare providers should, therefore, educate patients about the symptoms and create a safe space where patients feel comfortable seeking care before it is too late.
Dr. Lofters’ work extends beyond cervical cancer. In collaboration with Dr. Ambreen Sayani, she has investigated lung cancer in marginalized communities.11 They observed that rates of lung cancer are higher among low-income individuals, and this correlates with increased smoking rates in the low-income population.11 Further stigmatization surrounding income status and smoking may compound to create additional barriers to care in these populations.11
As Canada’s immigration rates rise, Dr. Lofters emphasized that the healthcare system should monitor health outcomes in immigrants and how they are influenced by their home country, income, and immigration path. According to Dr. Lofters, “looking at immigrant health is looking at the health of our population.” In addition, Dr. Lofters believes that we, as the general public, can alleviate the healthcare disparities by recognizing and leveraging our power and privilege to support others in society.
Cancer screening has proven to reduce cancer-related morbidity and mortality. Dr. Lofters is leveraging her expertise and passion for health equity to address the needs of marginalized populations to enhance cancer screening programs in Ontario. Dr. Lofters’ advice to young investigators interested in studying health inequities is to find the niche that they are most excited about, as there are still many opportunities in this realm to address the historical gaps in the field.
References
1. CCSD | Home [Internet]. [cited 2025 Aug 13]. Available from: https://cancerstats.ca/
2. Cancer | Ontario Health [Internet]. [cited 2025 Aug 13]. Available from: https://www.ontariohealth.ca/clinical/cancer
3. Lofters AK, Mark A, Taljaard M, et al. Cancer screening inequities in a time of primary care reform: A population-based longitudinal study in Ontario, Canada. BMC Fam Pract. 2018;19(1).
4. Lofters AK, Hwang SW, Moineddin R, et al. Cervical cancer screening among urban immigrants by region of origin: A population-based cohort study. Prev Med (Baltim). 2010;51(6).
5. Lofters AK, Vahabi M, Kim E, et al. Cervical cancer screening among women from Muslim-majority countries in Ontario, Canada. Cancer Epidemiology Biomarkers and Prevention. 2017;26(10).
6. Marshall S, Vahabi M, Lofters A. Acceptability, Feasibility and Uptake of HPV Self-Sampling Among Immigrant Minority Women: a Focused Literature Review. Vol. 21, Journal of Immigrant and Minority Health. 2019.
7. Walboomers JMM, Jacobs M V., Manos MM, et al. Human papillomavirus is a necessary cause of invasive cervical cancer worldwide. Journal of Pathology. 1999;189(1).
8. Cervical Screening | Cancer Care Ontario [Internet]. [cited 2025 Aug 13]. Available from: https://www.cancercareontario.ca/en/ types-of-cancer/cervical/screening?utm
9. Devotta K, Vahabi M, Prakash V, et al. Reach and effectiveness of an HPV self-sampling intervention for cervical screening amongst under- or never-screened women in Toronto, Ontario Canada. BMC Womens Health. 2023;23(1).
10. Lifetime probability of developing and dying from cancer in Canada - Statistics Canada [Internet]. [cited 2025 Aug 20]. Available from: https://www.statcan.gc.ca/o1/en/plus/4547-lifetime-probability-developing-and-dying-cancer-canada?utm
11. Ruco A, Lofters AK, Lu H, et al. Lung cancer survival by immigrant status: a population-based retrospective cohort study in Ontario, Canada. BMC Cancer [Internet]. 2024 Dec 1 [cited 2025 Aug 14];24(1):1114. Available from: https://pmc.ncbi.nlm.nih.gov/ articles/PMC11380402/
Dr. Aisha Lofters, MD, PhD. Associate Professor, University of Toronto
Photo Credit: Dr. Aisha Lofters
Master of Science in Biomedical Communications

Winter Kraemer
Winter is a current MScBMC student with a focus on 2SLGBTQ+ Health. He is interested in communicating the complexities of healthcare to patients and healthcare providers alike. You can see more of his work on his website: winterkraemer.cargo.site
Vicky Lin is a first-year Master’s student in the Biomedical Communications program at the University of Toronto with a background in Biology from McMaster University. She has worked extensively in multimedia design and print publishing in her previous work experience and is eager to use her passion for science visualization to make tools that help make science accessible for wider audiences.
Vicky Lin
The ART of Artemisinin
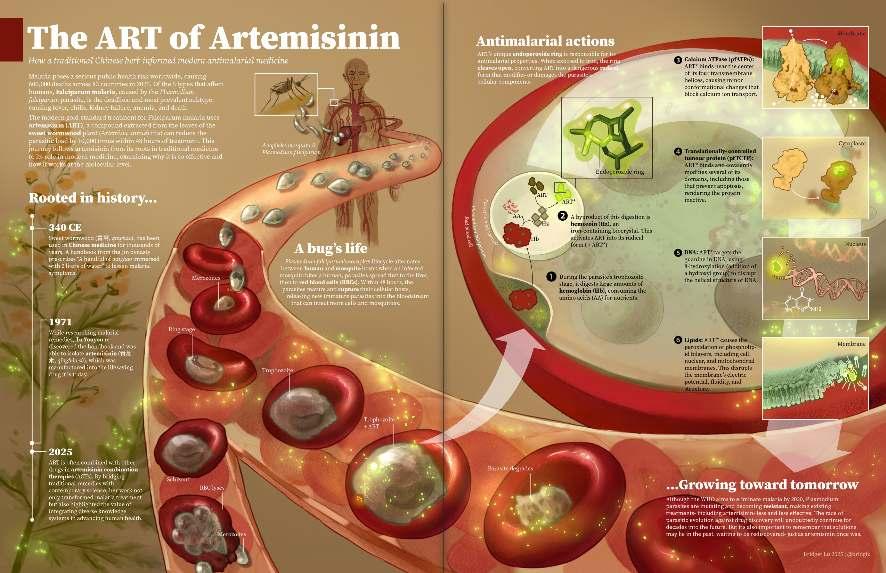
Bridget Lu
Bridget is a biomedical communications student and artist aiming to create work that’s not only accurate and informative, but also beautiful to look at. Driven by curiosity and creativity, she enjoys exploring complex ideas and creating visuals that inspire viewers to look more closely at the world around them.
Underwater Intellect: The Nervous System of the Common Octopus
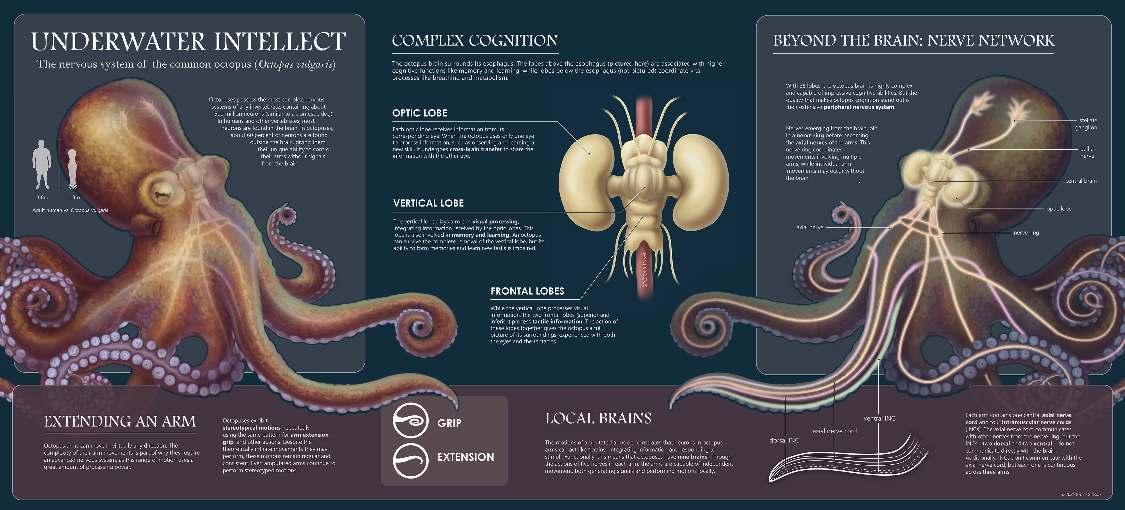

Grace Gibson
Grace Gibson is a second-year MSc student in the Biomedical Communications program studying to become a medical illustrator. She aims to work in patient-facing media and outreach focused on the LGBTQ community. In her free time, Grace enjoys reading books and painting.
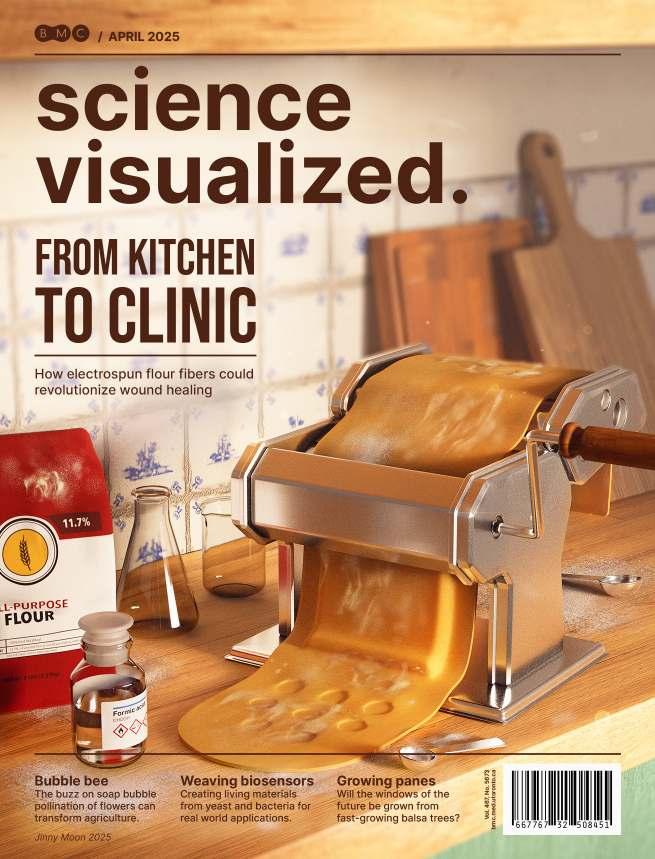
From Kitchen To Clinic

Jinny Moon is a biomedical communicator and designer studying in the Master of Science in Biomedical Communications (MScBMC) program. With a background in anatomy and cell biology, she explores how visual storytelling can bridge disciplines—translating ideas in neurobiology, mental health, and public health into meaningful connections between science and society.
* This piece was awarded the Award of Excellence in Student Still Media at the 2025 Association of Medical Illustrators Salon.

Cathy is a second-year MScBMC student in Toronto, Canada. She is particularly interested in pharmacology and toxicology, and new, inventive graphic design. You can find her work on her website at cathyzhou.com.
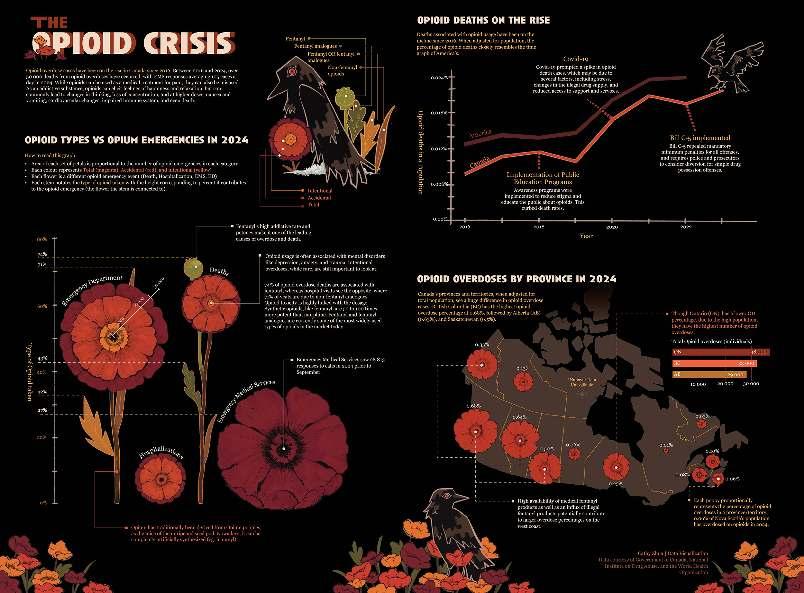
The Opioid Crisis in Canada
Cathy Zhou
Jinny Moon
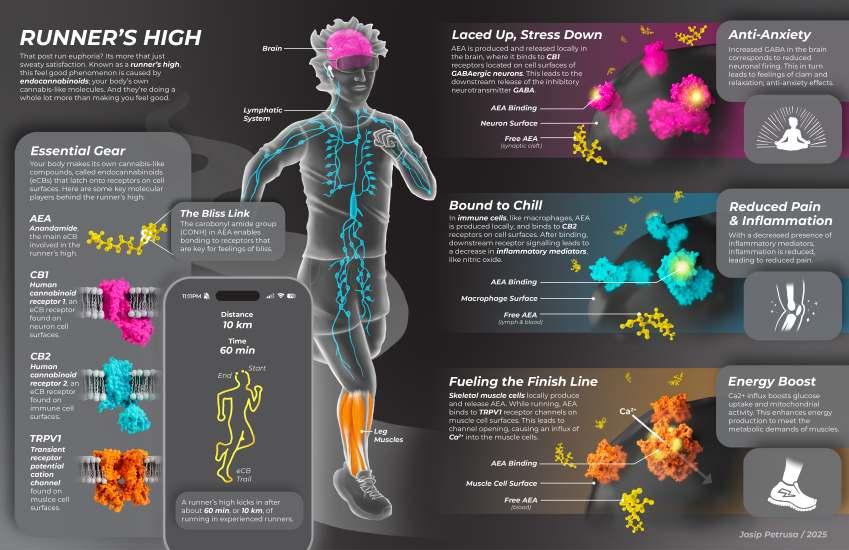

High Josip Petrusa
Josip is in his second year of studies in the Master of Science in Biomedical Communications program. He strives to bring science to life through visual storytelling, making science accessible and engaging for all.
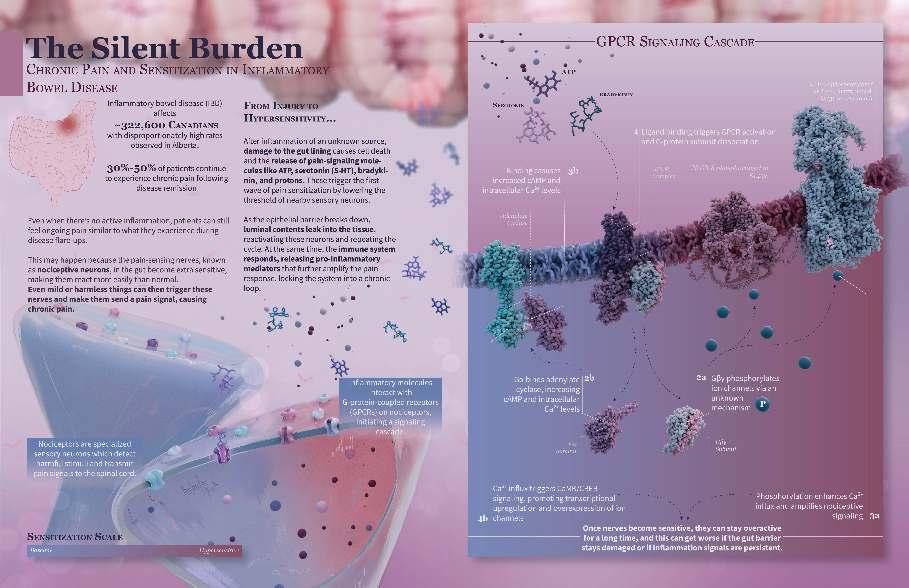
The Silent BurdenA Visualization of Chronic Pain in Inflammatory Bowel Disease

Eve Higgins
I began my journey in science communication during my BHSc in Biomedical Sciences at the University of Calgary, where I discovered the power of visuals in making complex topics clearer. Through my honours thesis on WNT signalling and later work in Dr. Derek McKay’s lab, I combined research in immunology and physiology with creating scientific figures and patient-focused resources. Today, I focus on transforming complex data into clear, engaging visuals, because great science should be accessible to everyone!
Liquid Biopsy: A Promising Application in Ovarian Cancer

By Tesam Ahmed
Ovarian cancer, the most fatal female reproductive cancer in the world, is responsible for over 240,000 new cases and 150,000 deaths in women every year.1,2 There are various risk factors associated with its development, including obesity, diet, physical inactivity, and advanced age (>65 years).3
High mortality rates in ovarian cancer are, in part, a result of its frequent late-stage detection. Decreased efficacy of surgical or pharmacological therapies result from approximately 75% of cases being diagnosed when the disease is in its advanced stages.4,5 The presentation of ovarian cancer often includes vague, nonspecific symptoms that are late in onset. In addition, surveillance is generally only reserved for populations at high-risk, such as those with known genetic mutations or a strong family history.6 The five-year survival rate for women with advanced ovarian cancer is alarmingly low, hovering around 20%.5 These statistics highlight the urgent need for improved early detection strategies.
Current ovarian cancer diagnostic tools, including serum markers like CA-125, imaging, and tissue biopsy approaches, present with limitations. CA-125 lacks adequate sensitivity and specificity in detecting earlystage disease. Tissue biopsies
are physically invasive, presents with limitations for longitudinal monitoring, and is spatially limited. Ovarian cancer treatment and diagnostics are in urgent need of tools that are minimally invasive, sensitive, and capable of detecting early or minimal residual disease (MRD), a small number of cancer cells that remain post-treatment and may lead to relapse.8,9
In this context, liquid biopsies have emerged over the past decade as a promising, non-invasive molecular screening and monitoring tool. Unlike traditional tissue biopsy, liquid biopsy serves to measure various tumour-derived components in peripheral blood: cell-free RNA (cfRNA), circulating tumour cells (CTCs), tumour DNA (ctDNA), tumour-educated platelets (TEPs), and exosomes. Tumours are hypothesized to release these components into the bloodstream via one of three primary mechanisms: secretion, apoptosis (regulated cell death), or necrosis (unregulated cell death). 9
Decoding Tumour Biology Through the Blood
Circulating Tumour Cells (CTCs) are cells deriving from the primary tumour site that have entered the circulatory or lymphatic system.10 CTCs have properties distinct from
cells of the primary tumour, and can be isolated from blood using various methods, based on their biological surface markers or underlying physical properties, including size, density, and electric charge.9,11
Cell-free RNA (cfRNA), consisting of mRNA and microRNA (miRNA) are produced as a result of high levels of gene transcription caused by quick tumour turnover. cfRNA in the plasma provides information about the body’s response to tumour growth, and about the tissue of tumour origin.12 miRNA specifically has also been implicated in tumour metastasis, genesis, and apoptosis.9
Tumour-Educated Platelets (TEPs) play an important role in the progression of tumour growth. 13 The “education” component of their name refers to the process of sequestration of tumour cell biomolecules into platelets, leading to changes in their RNA and profiles of protein expression. TEPs are involved in the systemic and local response of the body to cancer, changes in their profile make them a useful diagnostic biomarker, providing information about tumour bioactivity, and cancer progression. 14
Exosomes are small extracellular vesicles (EVs) released from both healthy and cancerous cells.9 Exosomes are released in higher
levels from cancerous cells than normal ovarian epithelial cells, providing utility in ovarian cancer detection.15 In addition, exosomes are involved in cancer progression, drug resistance, and tumour metastasis.16
Clinical Utility and Future Potential
Liquid biopsy, compared to standard techniques, offers several clinical advantages. It is noninvasive, allows for earlier detection and temporal surveillance of ovarian cancer, and for a more precise prognosis.17 By analyzing various tumour components within collected samples of plasma, treatment resistance, and molecular therapy targets can be identified. The ability of liquid biopsy to carry out non-invasive routine screening in the general population is also beneficial.9
Despite its promise, liquid biopsy is not without limitations. In my view, while these challenges are significant, they are not insurmountable. Technical challenges include variability in isolation methods, and low abundance and instability of molecules of interest. Research also suggests that liquid biopsy may be more effective when used as a complementary tool rather than singularly when determining clinical approach. I believe this emphasizes the importance of integrating tools
including liquid biopsy into a broader diagnostic strategy. Ongoing research is focused on improving methods of detection for specific cell types and establishing standardized protocols for implementation.9
It appears the future of ovarian cancer may lie in the bloodstream. In my opinion, liquid biopsy has the potential to become a crucial component of the diagnostic toolbox, as research advances its techniques and broadens its uses.
References
1. Proin ullamcorper suscipit hendrerit. Mauris lacinia tortor vel tellu Coburn SB, Bray F, Sherman ME, et al. International patterns and trends in ovarian cancer incidence, overall and by histologic subtype: Ovarian cancer trends. Int J Cancer. 2017 Jun 1;140(11):2451–60.
2. Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: Sources, methods and major patterns in GLOBOCAN 2012. Intl Journal of Cancer [Internet]. Available from: https://onlinelibrary.wiley.com/doi/10.1002/ijc.29210
3. Stewart C, Ralyea C, Lockwood S. Ovarian Cancer: An Integrated Review. Seminars in Oncology Nursing. 2019 Apr;35(2):151–6.
4. Hennessy BT, Coleman RL, Markman M. Ovarian cancer. The Lancet. 2009 Oct;374(9698):1371–82.
5. Schiavone MB, Herzog TJ, Lewin SN, et al. Natural history and outcome of mucinous carcinoma of the ovary. American Journal of Obstetrics and Gynecology. 2011 Nov;205(5):480.e1-480.e8.
6. Golia D’Augè T, Giannini A, Bogani G, et al. Prevention, Screening, Treatment and Follow-Up of Gynecological Cancers: State of Art and Future Perspectives. Clin Exp Obstet Gynecol. 2023 Aug 2;50(8):160.
7. Menon U, Gentry-Maharaj A, Hallett R, et al. Sensitivity and specificity of multimodal and ultrasound screening for ovarian cancer, and stage distribution of detected cancers: results of the prevalence screen of the UK Collaborative Trial of Ovarian Cancer Screening (UKCTOCS). Lancet Oncol. 2009 Apr;10(4):327–40.
8. Della Corte L, Russo G, Pepe F, et al. The role of liquid biopsy in epithelial ovarian cancer: State of the art. Crit Rev Oncol Hematol. 2024 Feb;194:104263.
9. Zhu JW, Charkhchi P, Akbari MR. Potential clinical utility of liquid biopsies in ovarian cancer. Mol Cancer. 2022 Dec;21(1):114.
10. Lin D, Shen L, Luo M, et al. Circulating tumour cells: biology and clinical significance. Sig Transduct Target Ther. 2021 Nov 22;6(1):404.
11. Pantel K, Speicher MR. The biology of circulating tumour cells. Oncogene. 2016 Mar 10;35(10):1216–24.
12. Roskams-Hieter B, Kim HJ, Anur P, et al. Plasma cell-free RNA profiling distinguishes cancers from pre-malignant conditions in solid and hematologic malignancies. NPJ Precis Onc. 2022 Apr 25;6(1):28.
13. Haemmerle M, Stone RL, Menter DG, et al. The Platelet Lifeline to Cancer: Challenges and Opportunities. Cancer Cell. 2018 Jun;33(6):965–83.
14. Ding S, Dong X, Song X. Tumour educated platelet: the novel BioSource for cancer detection. Cancer Cell Int. 2023 May 11;23(1):91.
15. Taylor DD, Homesley HD, Doellgast GJ. “Membrane‐Associated” Immunoglobulins in Cyst and Ascites Fluids of Ovarian Cancer Patients*. American Journal of Reproductive Immunology. 1983 Jan;3(1):7–11.
16. Tian W, Lei N, Zhou J, et al. Extracellular vesicles in ovarian cancer chemoresistance, metastasis, and immune evasion. Cell Death Dis. 2022 Jan 18;13(1):64.
17. Feng W, Dean DC, Hornicek FJ, et al. Exosomes promote pre-metastatic niche formation in ovarian cancer. Mol Cancer. 2019 Dec;18(1):124.
The Necessity of Gender-Affirming Surgery
By Grace Gibson
Recognition of transgender and gender diverse (TGD) people— individuals whose gender identity does not align with their sex assigned at birth—has greatly increased over the past decade. Correspondingly, as more people have come to identify as transgender and gender non-conforming, the medical field has seen increased demand for genderaffirming healthcare—medical treatments that contribute to a patient’s gender transition.1 Despite these interventions being medically necessary for many patients,2 the politicization of transgender healthcare and the growing movement of anti-trans legislation throughout North America threatens their accessibility to patients in need.3,4 Promoting access to gender-affirming care helps TGD people, an already underserved group, avoid further marginalization in seeking healthcare.
Gender-affirming care, also called transition-related care, consists of medical interventions like hormone replacement therapy (HRT) and genderaffirming surgery (GAS) that enables a patient’s physical traits to more closely align with their gender identity.5 This often reduces gender dysphoria, a state of distress or discomfort caused by the incongruence between one’s gender identity and physical characteristics.6 While every person’s transition is unique, many TGD people seek out one or more forms of GAS as part of their transitionrelated care.7 Though the popularity and visibility of transition-related surgeries have increased in recent years,1 these
surgeries are not as new or experimental as they may seem. Many modern forms of GAS—including orchiectomy (removal of the testes), penectomy (removal of the penis), and vaginoplasty (construction of a vagina)—originated in the early 20th century with the work of surgeon Magnus Hirschfeld at the Institute for Sexual Research in Berlin, Germany.1,9 While historical understandings of gender identity differed widely from modern standards, patients undergoing GAS at the time reported therapeutic benefits from receiving these surgeries, and outcomes only improved throughout the mid-20th century as surgeons refined and shared their techniques.1 Modern surgeons established current practices of GAS from over a century of development in surgical techniques, making many transitionrelated surgeries older than procedures like coronary artery bypass (first performed in 1960),10 heart transplantation (1967),11 and total knee replacement (1966-68).12
From the earliest days of GAS, the primary goal of surgery was to align a patient’s physical traits with their gender identity; however, secondary outcomes go beyond a simple resolution of this incongruence. Though some of these procedures may be labelled as cosmetic, there is significant evidence that receiving GAS is medically necessary and even life-saving for TGD patients.2 Postoperative GAS patients experience significant clinical benefits, including improved body image, fewer hospitalizations related to mental health emergencies, reduced suicidal ideation
and suicide attempts, and even reduced tobacco use.13 These improvements persist in both the short and long term.13,14 There is further evidence that even when patients experience complications or dissatisfaction with their surgical outcomes, few express regret for having received GAS—overall regret rates for all gender-affirming procedures are reported between one and two percent according to recent reviews.13,15,16 Gender-affirming procedures appear to offer their recipients significant improvements without equivalent drawbacks that induce postoperative regret.
Due to these factors, access to transitionrelated care is crucial for the well-being of TGD patients. Despite this, many TGD people face significant barriers to receiving healthcare, whether transition-related or not. Many healthcare providers are
undereducated about the needs of TGD patients, limiting their ability to provide culturally competent care that addresses the specific challenges that these patients experience.17,18 Some TGD people report facing discrimination or harassment from medical professionals, and even those who encounter sympathetic clinicians often find they are unaware of the healthcare needs of TGD patients, placing a burden on the patients to educate their providers.18 Beyond these barriers to accessing medical care, pursuing GAS comes with its own challenges, including outdated methods for assessing eligibility for GAS and few surgeons specializing in these procedures.2,17
Due to a rise in politically motivated transphobia, legislation aiming to limit transition-related healthcare has become prevalent throughout the United States (US) and United Kingdom (UK), with similar legislation being introduced in some regions of Canada.3,4,20 Such social and political opposition to genderaffirming healthcare is not new. In an extreme example, Nazi book burnings in the 1930s targeted Magnus Hirschfeld’s Institute for Sexual Research, where many advancements in modern GAS originated.1 For several decades following this destruction of research and medical advancement, the amount of surgeons practicing GAS remained scarce because of societal and political opposition to this kind of medical care.1 Public perceptions and awareness of TGD people have shifted since the mid-1900s; however, recent years have seen a rise in misinformation
about transgender healthcare and a surge in transphobia, leading to extensive legislation banning or limiting certain forms of gender-affirming care.3,4,19
Throughout the US, lawmakers introduced 120 anti-trans bills—many of which restricted transgender healthcare—in November and December 2024 alone,19 while in the UK, extensive anti-trans legislation has limited access to and even criminalized transition-related care in some circumstances.3 In Canada, federal protections for TGD people are currently robust, but 2024 legislation in Alberta proposed a complete ban on transitionrelated hormone therapy under the age of 16 and GAS under the age of 18, prompting some fears that Canadian federal lawmakers may follow the antitrans example set by the US and UK in the future.20 Compounded upon existing healthcare barriers and inequities, this legislation further threatens the ability of TGD people to receive gender-affirming care, including GAS.
The inequity and discrimination faced by TGD people reveal a need for improved understanding of TGD patient experiences among medical professionals, a greater effort to promote access to effective interventions like GAS, and a stronger advocacy movement for the rights of TGD people. While GAS may seem like a niche sub-specialty within the medical field, achieving healthcare equity means ensuring that all patients, regardless of their identity or background, can access the medical care they require.
References
1. Oles N, Fontenele R, Abi Zeid Daou M. Transgender History, Part II: A Brief History of Medical and Surgical Gender-Affirming Care. Behav Sci Law. 2025 Jul-Aug;43(4):351-356.
2. Tanenbaum GJ, Holden LR. A Review of Patient Experiences and Provider Education to Improve Transgender Health Inequities in the USA. Int J Environ Res Public Health. 2023 Oct 20;20(20):6949.
3. Connolly DJ, Meads C, Wurm A, et al. Transphobia in the United Kingdom: a public health crisis. Int J Equity Health. 2025 May 28;24(1):155.
4. Smallens Y. “They’re Ruining People’s Lives.” Human Rights Watch. 2025.
5. Joseph A, Cliffe C, Hillyard M, et al. Gender identity and the management of the transgender patient: a guide for non-specialists. J R Soc Med. 2017 Apr;110(4):144-152.
6. Atkinson SR, Russell D. Gender dysphoria. Aust Fam Physician. 2015;44(11):792-6.
7. Arteaga R, Dryden K, Blasdel G. Patient education and surgical decision-making in genital gender-affirming surgery. Curr Opin Urol. 2024 Sep 1;34(5):308-313.
8. Selvaggi G, Salgado CJ, Monstrey S, et al. Gender Affirmation Surgery. Biomed Res Int. 2018 Jul 5;2018:1768414.
9. Zilavy AJ, Santucci RA, Gallegos MA. The History of Gender-Affirming Vaginoplasty Technique. Urology. 2022 Jul;165:366-372.
10. Rocha EAV. Fifty Years of Coronary Artery Bypass Graft Surgery. Braz J Cardiovasc Surg. 2017 Jul-Aug;32(4):II-III.
11. Cooper DKC. Christiaan Barnard-The surgeon who dared: The story of the first human-to-human heart transplant. Glob Cardiol Sci Pract. 2018 Jun 30;2018(2):11.
12. Albana MF, Scuderi GR, Tria Jr AJ. The Evolution of Total Knee Replacements. In: The Cruciate Ligaments in Total Knee Arthroplasty. Cham: Springer Nature Switzerland; 2024. p. 3–15.
13. Almazan AN, Keuroghlian AS. Association Between Gender-Affirming Surgeries and Mental Health Outcomes. JAMA Surg. 2021 Jul 1;156(7):611-618.
14. Park RH, Liu YT, Samuel A, et al. Long-term Outcomes After Gender-Affirming Surgery: 40-Year Follow-up Study. Ann Plast Surg. 2022 Oct 1;89(4):431-436.
15. Ren T, Galenchik-Chan A, Erlichman Z, et al. Prevalence of Regret in Gender-Affirming Surgery: A Systematic Review. Ann Plast Surg. 2024 May 1;92(5):597-602.
16. Bustos VP, Bustos SS, Mascaro A, et al. Regret after Gender-affirmation Surgery: A Systematic Review and Meta-analysis of Prevalence. Plast Reconstr Surg Glob Open. 2021 Mar 19;9(3):e3477.
17. Hostetter CR, Call J, Gerke DR, et al. “We Are Doing the Absolute Most That We Can, and No One Is Listening”: Barriers and Facilitators to Health Literacy within Transgender and Nonbinary Communities. Int J Environ Res Public Health. 2022 Jan 22;19(3):1229.
18. Holloway BT, Gerke DR, Call J, et al. “The doctors have more questions for us”: Geographic differences in healthcare access and health literacy among transgender and nonbinary communities. QSW: research and practice. 2023;22(6):1073–91.
19. Taylor T. “The State of Trans Healthcare Laws in 2025.” Advocates for Trans Equality. 2025.
20. Jeffrey A. “Alberta legislation on transgender youth, student pronouns and sex education set to become law.” CBC. 2024.
SeasonalAffective Disorder in the Context of Racialized Individuals
By Vanessa Ip
With the transition to daylight savings at the end of every year, our sunlight exposure becomes limited. The decrease in sunlight, and thus vitamin D exposure, is linked to a decrease in mood. We often hear the terms “depression”, and “seasonal affective disorder” used colloquially, but what do they really entail? Seasonal affective disorder (SAD) is a clinical subtype of mood disorders with recurrent episodes of major depression occurring in a seasonal pattern,1-3 associated with recurrent depressive episodes in the fall and winter.2 Symptoms may include low mood, fatigue, changes in appetite, and loss of interest or pleasure in activities.2 Although light therapy has gained interest as a novel treatment for SAD, it is not the only option. With approximately 2-3% of Canadians experiencing SAD in their lifetime, and 15% experiencing mild SAD with symptoms of slight depression, it’s timely to bring additional regimens and strategies for equality in treatment availability to light; pun intended.3
SAD has been suggested to have further implications on racialized individuals. Previous research suggests that individuals with darker skin tones are more susceptible to vitamin D deficiencies.4 Furthermore, African Americans have been shown to be more likely to be deficient in vitamin D, as skin pigmentation reduces vitamin D production, and subsequently developing SAD.4,5 Interestingly, even individuals with darker eye colour have been linked
to increased risk for depression and fatigue compared to those with blue eyes.6 However, a common limitation in research investigating SAD is the absence of racialized population samples.7,8 Given that people of colour are at greater risk of SAD, it is important to identify the effectiveness and development of treatments.
Despite these research gaps, various evidence-based treatments for SAD have been identified for the general population and have become more popular and accessible in recent years.9 Similar to treatments for other mood disorders, pharmacotherapy involving second-generation antidepressants (i.e., selective serotonin reuptake inhibitors and serotonin-norepinephrine reuptake inhibitors) reduces depression scores and remission rates better than placebo.10 Another option is light room therapy (LRT), which is typically done in hospitals where light boxes, meant to mimic natural sunlight with 10,000 lux of white, fluorescent light, are for patients’ personal use.10,11 Although light boxes are easily accessible, there are better results with the use of LRT as opposed to light boxes in patient homes—namely due to exposure and intensity of light. In addition, light therapy requires patients to wake up and spend 30 minutes in the light, requiring behavioural commitment. But between light therapy and pharmacotherapy, which one is better? Surprisingly, some evidence suggests that light therapy may have comparative benefits to pharmaceuticals!1
One double-blind randomized controlled trial found that light therapy was equally as effective as the antidepressant fluoxetine at treating SAD.1 Therefore, the choice between the two options will often depend on personal preference and whether patients would rather adjust their morning routines or commit to taking medication.
Another treatment option involves cognitive behavioural therapy (CBT), a psychological intervention targeting maladaptive thinking and behavioural patterns which is well established in mood disorder treatment.12 Several variations of CBT exist, tailored to the unique needs of different mood disorders, with CBT-SAD leveraging psychoeducation, behavioral activation, and cognitive restructuring to specifically target winter depression.13 CBT-SAD has shown to be comparable to light therapy treatment after one year. Whereas light therapy is more accessible and less of a time commitment, CBT had more long-term effects, despite stopping the treatment.13
However, does ethnicity influence the course of SAD presentation and treatment? When looking at research with racialized samples, light treatment has been shown to be equally as effective for treating SAD amongst African-American compared to Caucasian patients.5 In addition, a study looking at hospital admissions for seasonal depression found that those of Asian race had more depressive episodes in the winter. This may be due to the lower

latitudes of where Asians originate, causing them to have more frequent depressive symptoms in response to the harsh weather found in higher latitudes.14
Beyond evidence for differing susceptibility and treatment outcomes for SAD in racialized individuals, existing systemic differences in treatment availability for mental health pose a considerable barrier for people of colour.15 This, coupled with the limited availability and insurance coverage of light boxes, make newer treatment options even less accessible.16 This disparity is further reflected in CBT-SAD treatment. Recent research supports ‘culturally adapted’ CBT as better suited for racialized individuals,17 but the more niche implementation of CBT-SAD risks generalization. Ultimately, novel SAD treatments can only be effective for racialized individuals if existing inequalities in mental health services are addressed concurrently.
The array of treatments for SAD is encouraging, opening more options for patients to explore and tailor their treatment. The current evidence suggests that light therapy and cognitivebehavioural therapy may be most effective for treating winter depression. Given recent evidence, SAD should be treated more seriously among North American people of colour, and that treatment should be consistent and repeated over time, especially in the winter months.
However, further research is necessary to better identify the genetic underpinnings and clinical outcomes of SAD, in concert with addressing systemic limitations to treatment availability. It is through more extensive research that treatments can be tailored to meet the unique needs of each individual, ensuring that no one is left behind when dealing with the cold, dark winter months.

References
1. Lam RW, Levitt AJ, Levitan RD, et al. The Can-SAD Study: A Randomized Controlled Trial of the Effectiveness of Light Therapy and Fluoxetine in Patients With Winter Seasonal Affective Disorder. The American journal of psychiatry. 2006;163(5):805–12.
2. Seasonal affective disorder (SAD) [Internet]. 2024 [cited 2025 Jul 25]. Available from: https://www.psychiatry.org/patients-families/ seasonal-affective-disorder
3. Seasonal affective disorder [Internet]. 2013 [cited 2025 Jul 25]. Available from: https://bc.cmha.ca/documents/seasonal-affective-disorder-2/
4. Stewart AE, Roecklein KA, Tanner S, et al. Possible contributions of skin pigmentation and vitamin D in a polyfactorial model of seasonal affective disorder. Medical hypotheses. 2014;83(5):517–25.
5. Uzoma HN. Light treatment for seasonal Winter depression in African-American vs Caucasian outpatients. World journal of psychiatry. 2015;5(1):138–46.
6. Goel N, Terman M, Terman JS. Depressive symptomatology differentiates subgroups of patients with seasonal affective disorder. Depression and anxiety. 2002;15(1):34–41.
7. Øverland S, Woicik W, Sikora L, et al. Seasonality and symptoms of depression: A systematic review of the literature. Epidemiology and Psychiatric Sciences. 2020;29:e31. doi:10.1017/ S2045796019000209
8. Magnusson A, Partonen T. The Diagnosis, Symptomatology, and Epidemiology of Seasonal Affective Disorder. CNS spectrums. 2005;10(8):625–34.
9. Westrin Å, Lam RW. Seasonal Affective Disorder: A Clinical Update. Annals of clinical psychiatry. 2007;19(4):239–46.
10. Kurlansik SL, Ibay AD. Seasonal Affective Disorder. American family physician. 2012;86(11):1037–41.
11. Terman M, Terman JS. Controlled Trial of Naturalistic Dawn Simulation and Negative Air Ionization for Seasonal Affective Disorder. The American journal of psychiatry. 2006;163(12):2126–33.
12. What is Cognitive Behavioral Therapy? [Internet]. American Psychological Association; 2017 [cited 2025 Jul 25]. Available from: https://www.apa.org/ptsd-guideline/patients-and-families/ cognitive-behavioral
13. Rohan KJ, Meyerhoff J, Ho SY, et al. Outcomes One and Two Winters Following Cognitive-Behavioral Therapy or Light Therapy for Seasonal Affective Disorder. The American Journal of Psychiatry. 2016;173(3):244–51.
14. Suhail K, Cochrane R. Seasonal variations in hospital admissions for affective disorders by gender and ethnicity. Social Psychiatry and Psychiatric Epidemiology. 1998;33(5):211–7.
15. Kaur N, Esie P, Finsaas MC, et al. Trends in Racial-Ethnic Disparities in Adult Mental Health Treatment Use From 2005 to 2019. Psychiatry Services. 2023;74(5):455-462.
16. Oldham MA, Ciraulo DA. Use of bright light therapy among psychiatrists in massachusetts: an e-mail survey. The Primary Care Companion for CNS Disorders. 2014;16(3):PCC.14m01637
17. Huey SJ, Park AL, Galan CA, et al. Culturally Responsive Cognitive Behavioral Therapy for Ethnically Diverse Populations. Annual Review of Clinical Psychology. 2023;19:51-78.
The Canadian Healthcare System:
Leaving the LGBTQ+ Community Behind

By Priya van Oosterhout
The rights of those who are sexualand gender-diverse (herein referred to as the LGBTQ+ community) have continued to expand within Canada over the past decades, including gradual changes to a medical system largely built on cisgender and heteronormative values.1,2 Despite such advances, the LGBTQ+ community continues to face discrimination and marginalization across Canada, including within the healthcare system.1–4 Access to quality care is not always a reality for those who identify as LGBTQ+, with many facing extended delays to care, or healthcare practitioners (HCPs) who refuse to administer treatment or medication.1,3 It is unsurprising then that people within the LGBTQ+ community face significantly poorer health outcomes as compared to their non-LGBTQ+ counterparts,1–3,5,6 with higher rates of depression,1–3,5,6 suicide,1–3,5,6 anxiety,1,3,6 cancer,1,3,6 and arthritis,1,3 to name a few. Systems-level changes need to be made in the way our healthcare system addresses the medical needs of one of Canada’s most vulnerable populations. This change may, in part, be addressed by further educating the HCPs that patients interact with at every level of care.
Inequities within the healthcare system are structural, involving a complex interaction of social, political, and cultural factors.2,3 For instance, the sociopolitical climate influences healthcare delivery, with those in less accepting communities being more likely to conceal their sexual or gender identities in anticipation
of mistreatment from medical staff.1,2 Research has shown that people in the LGBTQ+ community often report longer wait times,1 bias and discrimination in healthcare settings, and poor healthcare experiences.2–4 Other studies have found that members of the LGBTQ+ community are much more likely to avoid healthcare entirely,1,2 with one survey finding that one fifth of respondents even reported avoiding emergency medical care due to fear of maltreatment.3 However, it’s not just discrimination affecting LGBTQ+ healthcare, but also the lack of culturally competent care offered by most institutions. For example, transmasculine individuals are much more likely to avoid screening for breast and cervical cancers because of the distress associated with such tests, increasing their risk of developing advanced metastatic disease.1 A safe and culturally informed environment may mitigate reduced screening rates and healthcare avoidance behaviours, thereby providing a better medical experience.
Frankly, conversations about LGBTQ+ health are incomplete without discussing the unique medical needs of gender diverse patients. In 2019, a national survey found that 44% of transgender respondents reported an unmet healthcare need.7 Other systematic reviews have found that more than half of participants in Canadian transgender studies report negative gender-related experiences with the healthcare system,1,3 with one third being refused help, and many observing longer wait times. Much of the healthcare
needs for gender diverse individuals center around medically supervised transition, with the first point of care often being their primary physician.1 Despite this, the number of clinicians with the training to properly support this group is low, forcing many gender-diverse patients to join long waitlists or pay expensive travel costs to receive adequate care.1
With such inequalities, what are the solutions? How do you change a system with deeply engrained values that are often at odds with LGBTQ+ healthcare? The largest modifiable factor when it comes to addressing inequities the healthcare system is education.1 Surprisingly, there is no national standard for healthcare education in Canada, so there are no federal guidelines or resources to transform the current lack of inclusive curricula.1 In surveys, many HCPs have reported feeling that their lack of training negatively impacts their ability to care for patients.1 When asked, 41% of medical students at the University of Ottawa reported witnessing antiLGBTQ+ attitudes within the education system,1 and only 7% of medical students surveyed across Canada felt like they had enough knowledge to address the needs of a transgender patient.4 In fact, only one third of medical schools in Canada and the USA provide education regarding gender-affirming hormone therapy and surgical transition.1,4 With such little education, many primary care HCPs refer LGBTQ+ patients to specialists for sexual- or gender-related concerns, even

when not medically necessary. Not only does this significantly increase wait times, but LGBTQ+ patients may interpret the referral as an unwillingness to treat concerns related to their identities by their primary care physicians.1
LGBTQ+-specific education in healthcare would need to be multifaceted to truly address current disparities. Recognizing and addressing implicit biases, increasing cultural competency, and providing information regarding sexual- and gender-related treatments and procedures are all critical to familiarize HCPs with the needs of their LGBTQ+ patients. Practices like acknowledging patient vulnerability, affirming sexual and gender identities, avoiding binary language, and considering the physical discomfort of different procedures are all critical in providing a positive healthcare experience.1,4 Furthermore, interventions should be at different levels of each organization, such as creating inclusive physical environments, increasing workforce diversity, and education for both clinical and non-clinical staff. Creating a safe and comfortable environment would create a better experience for LGBTQ+ patients and reduce barriers to receiving care.1 Furthermore, ensuring adequate health education would also make HCPs more comfortable with addressing LGBTQ+ related concerns, giving them the tools needed to effectively treat their patients.
Despite there being no standardized guidelines for health education in Canada,1 there are many organizations working to close the gap in healthcare. Groups like TransCare BC, the Canadian Professional Association for Transgender Health, and Rainbow Health Ontario are all committed to creating conferences and workshops tailored to helping HCPs provide adequate healthcare for the LGBTQ+ community. Rainbow Health Ontario, for example, includes courses on being LGBTQ+-friendly, trauma-informed care, and referrals and post-operative care for gender affirming surgeries; to name a few. While it is important to showcase the incredible work of those pushing for change, the need for such organizations highlights a concerning trend. Should it not be the responsibility of medical schools to prepare their students for any patient they may treat? At the end of the day, it is the patients themselves who are forced to rely on a system that is predominantly uneducated about their needs on a good day, or actively hostile on a bad day.
In summary, the Canadian healthcare system is largely ill-equipped to treat our country’s LGBTQ+ community, exacerbating existing health disparities, and leaving one of our most vulnerable populations behind. Consequently, LGBTQ+ patients have reported discrimination, longer wait times, concealing their identities, and even avoiding medical care altogether. Many healthcare providers have also reported
feeling unprepared to adequately treat LGBTQ+ patients, with medical students even observing anti-LGBTQ+ sentiment in their training. A strong way to revolutionize LGBTQ+ healthcare is by ensuring healthcare providers have the necessary education to treat their patients. Not only should they be trained on LGBTQ+-specific medical concerns, but also in helping providers address their implicit biases, thus creating a safe and informed practice. Organizations trying to bridge the gap in the healthcare system already exist, but a lot more work is needed to truly improve the medical care of sexual- and gender-diverse Canadians.
References
1. Comeau D, Johnson C, Bouhamdani N. Review of current 2SLGBTQIA+ inequities in the Canadian health care system. Front Public Health. 2023;11:1183284. doi: 10.3389/fpubh.2023.1183284.
2. Hatzenbuehler ML, Lattanner MR, Mcketta S, et al. Structural Stigma and LGBTQ+ Health: A Narrative Review of Quantitative Studies. Lancet Public Health. 2024;9(2):e109-27. doi:10.1016/ S2468-2667(23)00312-2.
3. Zeeman L, Sherriff N, Browne K, et al. A review of lesbian, gay, bisexual, trans and intersex (LGBTI) health and healthcare inequalities. Eur J Public Health. 2019;29(5):974-80. doi:10.1093/ eurpub/cky226.
4. Chan B, Skocylas R, Safer JD. Gaps in Transgender Medicine Content Identified among Canadian Medical School Curricula. Transgend Health. 2016;1(1):142-50. doi:10.1089/trgh.2016.0010.
5. Government of Canada. Facts, stats and impact: 2SLGBTQI+ communities [Internet]. Ottawa: Government of Canada; 2025 Jun 18 [cited 2025 Jul 26]. Available from: https://www.canada.ca/en/women-gender-equality/free-to-be-me/federal-action-2slgbtqi-communities/facts-stats.html.
6. Blondeel K, Say L, Chou D, et al. Evidence and knowledge gaps on the disease burden in sexual and gender minorities: a review of systematic reviews. Int J Equity Health. 2016;15:16. doi:10.1186/ s12939-016-0304-1.
7. Trans PULSE Canada. Health and health care access for trans & non-binary people in Canada. London: Trans PULSE Canada; 2020 Mar 10 [cited 2025 Jul 26]. Available from: https://transpulsecanada. ca/results/report-1/
StillWater Runs Deep:
Exploring the
Issue
of Water Contamination in Canadian Communities and beyond
By Josephine Machado
Canada is home to 20% of the world’s freshwater reserves, and nearly 7% of the world’s annually renewable water.1 Despite this abundant water supply, Canada has, and continues to face, water crises similar to other countries across the globe. Most Canadians consider access to clean water a given, however, for thousands in Pikangikum First Nation, water supplies have become persistently unsafe, and sometimes nonexistent.2 This issue is not unique to Canada—it is a representation of the neglect that threatens the well-being of various marginalized communities. Whether they be lowincome, or consisting of visible minorities, many demographics have faced the serious repercussions of unsafe drinking water.
Pikangikum First Nation, a remote Ojibway community of about 4000 individuals located more than 500 km northwest of Thunder Bay, has faced long-standing challenges due to a lack of proper infrastructure for safe water supply.3 The most recent ongoing drinking advisory for Pikangikum was issued in February of 2024.3 This follows several advisories declared previously, including those between 2000 and 2002 as well as 2005 and 2019.4 Despite Pikangikum consisting of 500 homes, its water and sewage infrastructure are insufficiently developed.4 Most Pikangikum households lack running water, with only 109 homes having a working tap. The remainder of individuals must travel to points in the community to collect water in buckets for both drinking or cooking.5 The water
treatment plant in the community only provides services to the school, nursing station, band office, and a few government buildings.4 Still, there remains only one functioning drinking water access point within the community.4 Other options are costly and inconvenient; buckets can be filled at the lake, bottled water can be purchased at the Northern store, or flights can be taken 100 km South to Red Lake to buy cases in bulk.4 Decades of underfunding, overcrowded housing, and deteriorating water and sewage infrastructure reflect a persistent neglect of First Nations communities—neglect rooted in inequitable policies and budgetary caps that have continuously prioritized urban systems over reserve realities.
These challenges not only strain residents financially and logistically but also create significant health risks. The direct consequences of a lack of clean water range from eczema to skin infections and parasites,3,4 given that regular bathing is essential to treat recurring skin infections. More severely, individuals belonging to the community have been injured or killed whilst travelling to access water and toilet facilities.3 Furthermore, the lack of water access has contributed to the inability to adequately fight fires in the First Nation. In fact, two adults and a child were confirmed dead in a house fire in 2023, as fire trucks that could have helped douse the flames earlier were frozen.6 This follows a previous fire that claimed the lives of six adults and three children back in 2016, due
to a lack of basic firefighting equipment among other violations.7 In a 2025 CBC interview regarding the lawsuit, Carolina Budiman, senior health project manager for the Pikangikum Health Authority recounts, “We have one fire hydrant, but it only works if everything else shuts down.”4
This fragile infrastructure has now reached a breaking point. In May of 2025, Pikangikum First Nation declared a formal state of emergency over the catastrophic failure of its water and sewage systems.2 The First Nation has made it clear that dealing with this crisis can no longer be put on hold, announcing that they will be taking the Government of Canada to federal court for damages and emergency relief. 2 The statement of claim previously obtained by CBC News states that the federal government has violated Pikangikum’s constitutional, Charter, and treaty rights by failing to ensure proper access to potable water, in addition to both sewage and fire prevention systems.4 This issue is part of a larger trend. As of July 2025, 38 long-term drinking water advisories remained in effect on First Nations reserves.8 This is despite the Canadian government’s pledge made in the 2015 federal election campaign to eliminate all long-term drinking water advisories on First Nations reserves by March 2021.9 Meaningful solutions require more than simple stopgap repairs—they demand substantive federal investment guided by a combination of Indigenous sovereignty, capacity-building for maintenance, and enforceable national water safety standards that do not exempt reserves.

Grassy Narrows First Nation is yet another community in Canada that has faced similar hardships, suffering one of the most infamous water crises in Canadian history. Contamination of their river system can be traced back to the 1960’s and 70’s when nine tonnes of mercury used for paper-bleaching were dumped into the river near Grassy Narrows, causing widespread contamination.10 Just under 1,000 people live in Grassy Narrows First Nation and rely on fish as a staple component of the community’s diet. Tragically, it is estimated that 90 percent of Grassy Narrows’ population has symptoms of mercury poisoning,10 including tremors, insomnia, memory loss, neuromuscular effects, headaches, cognitive and motor dysfunction, and even death.11 Despite the federal government pledging $19.5 million dollars in 2017 for a mercury treatment centre, the construction remains incomplete as of 2025.10 This story exemplifies the continuing environmental racism, wherein systemic neglect disproportionality plagues Canada’s indigenous communities.
Calling attention to these crises is critical for achieving meaningful solutions. Renowned film, “Erin Brockovich” embodies this concept, and brought a great deal of attention to the importance of safe drinking water to the general health and well-being of communities. The movie, starring Julia Roberts, who plays American legal clerk, Erin Brockovich, recounts her role in the case of Hinkley California residents versus Pacific Gas & Electric (PG&E).12 PG&E
used hexavalent chromium to prevent pipe corrosion in its cooling system between the 1950’s and 1960’s, causing toxic chemicals to seep into the groundwater. 13 Residents of Hinkey suffered unusually high rates of cancer, asthma, recurrent bronchitis, and other illnesses.14 The cause of these illnesses were unknown until Brockovich investigated after having noticed the pattern of health concerns in Hinkley’s community, leading to her advocating for them to receive justice.13 The case ended in a $333 million settlement in 1996, the largest paid in a direct-action lawsuit in U.S. history at the time.13 Corporate accountability was made a subject of attention due to the release and popularity of the film, becoming a strong symbol of environmental activism.14 This case is a cornerstone example of bringing attention to concerns regarding environmental health and corporate responsibility, and how awareness and activism can lead to accountability and change.
The common denominator among each of these water crises is a lack of government and corporate accountability. From the promises made by the Canadian government to First Nation’s peoples, to the irreversible damage seen in the water crises that have plagued the United States, it is evident that regulatory bottlenecks and acts of corporate greed and negligence can have dire consequences. Pikangikum’s emergency is not an isolated story–it’s part of a long-standing continuum. Grassy Narrows and Hinkley also further illustrate the consequences of delaying environmental justice. These crises do not
only permanently alter lives but also act sever the trust between a government and its people. With modern day technology, the issue seems to be less so one of capability, but more to do with will. Water access needs to be prioritized lest we deem the rights of the First Nations peoples to be less than other inhabitants of Canada. Various communities have spoken out
References
1. Canada E and CC. Water use in Canada [Internet]. 2025 [cited 2025 Aug 3]. Available from: https://www.canada.ca/en/environment-climate-change/services/environmental-indicators/water-use.html
2. Staff N. Ontario First Nation seeks emergency relief in Federal Court over water crisis [Internet]. CityNews Toronto. 2025 [cited 2025 Aug 3]. Available from: https://toronto.citynews.ca/2025/05/09/ontariofirst-nation-seeks-emergency-relief-in-federal-court-over-water-crisis/
3. Ontario First Nation seeks emergency relief in Federal Court over water crisis | Globalnews.ca [Internet]. Global News. [cited 2025 Aug 3]. Available from: https://globalnews.ca/news/11172800/ontario-firstnation-seeks-emergency-relief-in-federal-court-over-water-crisis/
4. Law S. Pikangikum First Nation takes federal government to court over lack of water, wastewater infrastructure. CBC News [Internet]. 2025 May 14 [cited 2025 Aug 3]; Available from: https://www.cbc.ca/ news/canada/thunder-bay/pikangikum-first-nation-water-wastewater-1.7533789
5. Habitat for humanity canada | clean drinking water in pikangikum [Internet]. Habitat for Humanity Canada. [cited 2025 Aug 3]. Available from: https://habitat.ca/en/stories/clean-drinking-water-in-pikangikum
6. Ontario First Nation says bodies of 2 adults, 1 child recovered after house fire | Globalnews.ca [Internet]. Global News. [cited 2025 Aug 3]. Available from: https://globalnews.ca/news/9514933/opp-pikangikum-fire/
7. Staff. Nine dead in family house fire at remote Canadian indigenous community. The Guardian [Internet]. 2016 Mar 30 [cited 2025 Aug 3]; Available from: https://www.theguardian.com/world/2016/mar/30/ canada-first-nation-house-fire-nine-dead-indigenous
8. Canada G of CIS. Ending long-term drinking water advisories [Internet]. 2017 [cited 2025 Aug 3]. Available from: https://www.sac-isc. gc.ca/eng/1506514143353/1533317130660
9. Trudeau’s promise to improve First Nations drinking water years behind schedule: federal government | Globalnews.ca [Internet]. Global News. [cited 2025 Aug 3]. Available from: https://globalnews. ca/news/7836421/first-nations-water-trudeau-broken-promises/
10. Law S. Mercury poisoning near Grassy Narrows First Nation worsened by industrial pollution, study suggests. CBC News [Internet]. 2024 May 23 [cited 2025 Aug 3]; Available from: https://www.cbc.ca/ news/canada/thunder-bay/grassy-narrows-first-nation-methylmercury-study-1.7211750
11. Mergler D, Philibert A, Fillion M, Silva JD. Childhood mercury exposure and early death in Grassy Narrows First Nation, Canada: a retrospective study. Environmental Health [Internet]. 2025 Jun 23 [cited 2025 Aug 3];24(1):39. Available from: https://doi.org/10.1186/ s12940-025-01190-7
12. Erin Brockovich: California water battle “woke me up.” 2021 Mar 22 [cited 2025 Aug 3]; Available from: https://www.bbc.com/news/ world-us-canada-56462793
13. Brockovich-pg&e case | ebsco research starters [Internet]. [cited 2025 Aug 3]. Available from: https://www.ebsco.com/research-starters/law/ brockovich-pge-case
14. News ABC. Erin Brockovich: the real story of the town three decades later [Internet]. ABC News. [cited 2025 Aug 3]. Available from: https:// abcnews.go.com/US/erin-brockovich-real-story-town-decades/ story?id=78180219
Healthcare Behind Bars
Understanding
Healthcare Inequality in Federal Prisons

By Mia Feldman
In Canada’s federal prisons, prisoners are not only deprived of their physical freedom, but also of their fundamental human right to healthcare. While incarcerated, individuals are considered wards of the state, meaning the government has a legal obligation to provide a standard level of healthcare.1 Nevertheless, despite legislation, many incarcerated people in Canada continue to experience substandard healthcare. The manifest function of the carceral system is to offer a measure of safety and justice to victims of crime by removing offenders from society and limiting their freedom of mobility; however, a latent consequence of imprisonment is the alienation of other human rights, such as the right to healthcare.
In Canada, adults sentenced to two or more years in prison are sent to a federal penitentiary managed by Correctional Services Canada (CSC). Despite existing legislation, the CSC consistently fails to meet a basic standard of care.2 As a result, entering prison with a pre-existing health condition can have severe consequences. One of many examples is in the case of Garrie Garrell, who sued the federal government in 2021 over the inadequate care he received while incarcerated at Beaver Creek Institution in Gravenhurst, Ontario.3 Garrell lives with chronic obstructive pulmonary disease and heart disease which, prior to his incarceration, was manageable. While incarcerated, federal staff denied him oxygen, medication, and appointments with
specialists, resulting in an early release due to worsening health. As a result of neglectful care, Garrell is now completely incapacitated by his condition.3
When considering antecedents to healthcare inequality in prison, systemic issues are abound. Understaffing and underfunding of prison healthcare often leads to gaps in care and burnout among available clinicians and nursing staff.4 For example, a 2025 systemic review found that nurses are reluctant to take employment at prisons because of the reputation these roles have for being draining and stressful, perpetuating the understaffing.4 Policy changes that provide staff with more resources to work with, including specialized providers for specific problems (i.e. social workers for mental healthcare), may break this cycle of understaffing; however little support of this kind exists. Beyond resource barriers, the relationship between healthcare providers and inmates is shaped by a deep social divide. Canadian prisoners have reported experiencing an “us vs. them” mentality when seeking care from providers, who often hold negative attitudes towards prisoners.2,5 For example, healthcare providers may accuse prisoners of being drug-seeking or malingering and ignore their concerns.2
In addition to exacerbating pre-existing conditions, many leave prison with new health conditions they were less likely to develop before incarceration. The incidence
of HIV, hepatitis, and tuberculosis are all significantly greater in prison than among the general population.6-8 This is likely due to poor standards of hygiene, limited preventative medical practices (e.g. clean needle exchange programs), and lacking access to vaccinations.6, 7 In addition, incarceration often results in individuals developing new severe mental health disorders, such as PTSD.9 A 2015 review of incarceration and health outlines that being separated from family and witnessing violence in prison are strong risk factors for the development of mental illness.10 These physical and psychological harms reveal that incarceration is not only a legal punishment, but a public health crisis itself.
Prison as a cause of poor health has been identified in Canada for almost 10 years.11 Specifically, the very structure of incarceration—marked by isolation from community and family, restricted autonomy, the physical and psychological abuse common from prison staff, and a focus on constant punishment—directly contributes to deteriorating health.2,10,11 Researchers have identified a phenomenon known as “accelerated aging” among inmates, where the chronic stress of living in overcrowded and under-resourced prisons causes biological age to outpace chronological age by 10-15 years.12 Thus, solving this crisis requires more than simply expanding access to healthcare in prison. The evidence is clear, prison is not only a symptom of a failing healthcare system, but also a driver of poor health
outcomes itself. To uphold the health and dignity of Canadians, we must consider adopting decarceration as a central component of public health policy.
Opponents of decarceration worry about public safety and support systems of retribution. However, as it stands today, nearly three quarters of prisoners in Canada are serving time for nonviolent crimes, such as possession of illicit substances.13 Given the fairly low risk that these individuals pose to public safety and the relatively high risk of them experiencing inadequate care, alternative modes of justice, such as mandatory community service, may offer more productive strategies to manage risk. Decarceration strategies should also be paired with robust community-based supports and rehabilitation services. A 2021 review found that across the United States, programs such as early childhood education, nurse family partnerships, and provision of housing improved community health outcomes when paired with decarceration efforts.14 Healing lodges are another alternative to incarceration for Indigenous folks. Rooted in rehabilitation over punishment, they use traditional values and culturally relevant services, such as access to Elders, ceremonies, and interactions with nature to guide holistic healing.15 A 2022 report on Canadian healing lodges found that participation significantly decreased the risk of revocation of release by 54% for Indigenous men and 65% for Indigenous
women.16 Emphasis on recovery and restoration at these lodges reduces risk of future incarceration. Only by reimagining the function of justice systems and prioritizing social supports over punishment can the years of life lost to incarceration be reduced and true health equity achieved.
The health inequalities within Canadian prisons underscore a deeper truth; incarceration is an important structural determinant of health for prisoners and their families. Critically, incarceration strips individuals of autonomy, safety, and access to care, undermining the foundations of wellbeing. If we are serious about protecting public health, we must confront the prison system as a site of harm and invest in robust, community-based alternatives that centre healing and social support. Ultimately, we must recognize that decarceration is not a departure from justice, but a necessary step towards a more equitable and healthy society.
References
1. Corrections and Conditional Release Act, S.C. 1992, c. 20
2. Miller A. Prison health care inequality. CMAJ. 2013 Apr 2;185(6):E249-50.
3. Barrera J, Loiero J. This man is on his deathbed because of the health care he received in prison, lawsuit alleges. CBC News [Internet] 2021 Mar 5: CBC Investigates.
4. Shelton D, Roscoe LE, Kapetanovic TA, Smith S. The Correctional Nursing Workforce Crisis: An Innovative Solution to Meet the Challenge. J Correct Health Care. 2025 Apr;31(2):82-89.
5. Veilleux C, Roach P, Cooke L, Pfeffer G, Johnson N, Ganesh A. Implicit Bias and Health Disparities in the Incarcerated Population: A Review With a Focus on Neurological Care and the Canadian Perspective. J Neuro Res. 2022;12(2):34-42.
6. Zakaria D, Thompson JM, Jarvis A, Borgatta F. Summary of emerging findings from the 2007 National Inmate Infectious Diseases and Risk-Behaviours Survey. Ottawa, ON: Correctional Service of Canada; 2010.
7. Ford PM, Pearson M, Sankar-Mistry P, Stevenson T, Bell D, Austin J. HIV, hepatitis C and risk behaviour in a Canadian medium-security federal penitentiary. Queen’s University HIV Prison Study Group. QJM. 2000;93(2):113-9.
8. Canadian Thoracic Society. Canadian tuberculosis standards. 7th ed. Ottawa, ON: Canadian Thoracic Society, Public Health Agency of Canada; 2013.
9. Piper A, & Berle D. The association between trauma experienced during incarceration and PTSD outcomes: a systematic review and meta-analysis. J. Forensic Psychiatry Psychol. 2019 July:30(5):854–875.
10. Massoglia M, Pridemore WA. Incarceration and Health. Annu Rev Sociol. 2015 Aug;41:291-310.
11. Kouyoumdjian F, Schuler A, Matheson FI et al. Health status of prisoners in Canada: Narrative review. Can Fam Physician. 2016 Mar;62(3):215-22.
12. Reagan L, Kitt-Lewis E, Loeb SJ, Shelton D, Zucker DM. Health equity for people living in correctional facilities: Addressing bias, stigma, and dehumanization. Res Nurs Health. 2024 Aug;47(4):359365.
13. Corrections and Conditional Release Statistical Overview 2022. Ottawa, ON. Public Safety Canada; 2022.
14. Hawks L, Lopoo E, Puglisi L, Cellini J, Thompson K, Halberstam AA, Tolliver D, Martinez-Hamilton S, Wang EA. Community investment interventions as a means for decarceration: A scoping review. Lancet Reg Health Am. 2021 Dec 21;8:100150.
15. Correctional Service Canada. Healing Lodges: A path to rehabilitation and reconnection. Government of Canada [Internet] 2024 Sept 7: Let’s Talk.
16. Hanby L, Ridha T, Sullivan R, et al. Indigenous Healing Lodges: Impacts on Offender Reintegration and Community Outcomes. Correctional Service of Canada. 2022.

IMS Faculty Highlights

Dr. Vitor Mendes Pereira
Dr. Vitor Mendes Pereira is a surgeonscientist at St. Michael’s Hospital and the co-director of the RADIS Lab. His research interests include using robotics, AI, dynamic flow, imaging, and simulation to diagnose and treat cerebrovascular diseases.

Dr. Kelsey McLaughlin
Dr. Kelsey McLaughlin is an assistant professor and early-career researcher in the Department of Obstetrics & Gynecology at the University of Toronto and staff scientist in the Department of Obstetrics & Gynecology at Sinai Health System. Her research program is focused on advancing maternal cardiovascular health through hospital- and communitylevel initiatives, with recent research exploring phenotype-directed management of hypertension in pregnancy.

Dr. Rohit Mohindra
Dr. Rohit Mohindra is an emergency medicine clinician and researcher at North York General Hospital and the Schwartz Reisman Emergency Medicine Institute. His areas of research include refugee population care, using machine learning in emergency care, and opioid related cardiac arrests.

Dr. Marta Maslej
Dr. Marta Maslej is a staff scientist with The Krembil Centre for Neuroinformatics at CAMH. She co-leads the Predictive Care team, which uses interdisciplinary methods to study impacts of AI applications on mental health care, with a focus on responsible integration and health equity.

Dr. Amanda Boyle
Dr. Amanda Boyle is a preclinical PET imaging scientist in the Brain Health Imaging Centre at CAMH studying neuroinflammation, neurodegeneration, and neuro-oncology. Her research focuses on identifying novel strategies for early diagnosis of neuroinflammatory conditions such as multiple sclerosis, as well as investigating neuroinflammation and neuro-tumour crosstalk in neuro-oncology.


Dr. Charles Tator trained at U of T, where he was Chair of Neurosurgery. He founded ThinkFirst Canada, Parachute Canada, and the Canadian Concussion Centre. He is an Officer of the Order of Canada. His current research at Krembil Brain Institute is investigating treatments for spinal cord injuries and concussions. Promoted to

Dr. Danielle Bentley
Dr. Danielle Bentley is an anatomist, education researcher, and principal investigator of the ATLAS Research Lab. Primarily appointed with the Temerty Faculty of Medicine, she teaches gross anatomy and embryology at both the undergraduate and graduate levels to students across the medical health sciences.
Dr. Charles Tator
Dr. Karen Davis
Dr. Karen Davis is neuroscientist at the Krembil Brain Institute and a professor in the Department of Surgery at the University of Toronto. Her research interests include mechanisms of acute and chronic pain, brain imaging, and neuroethics.


Dr. Hans Katzberg
Dr. Hans Katzberg is Professor of Medicine, Neurology Division Head and Clinical Investigator at UHN/KBI. His research is focused on advancing minimally invasive, AI-driven electrophysiology and imaging methods for complex neuromuscular diseases. Therapeutically, he leads clinical trials advancing immunotherapies for neuromuscular junction disorders including MG and peripheral neuropathies.


Dr. Mark Boulos
Dr. Mark Boulos is a stroke and sleep neurologist at Sunnybrook Health Sciences Centre. Dr. Boulos’ research investigates the association of sleep disorders with TIA/ stroke & other neurological disorders, as well as home sleep monitoring, normative sleep data, and novel treatment interventions.

Dr. Warren Lee
Dr. Warren Lee is a vascular biologist and ICU physician. His lab works at the interface of the endothelium and inflammation and is best known for their pioneering investigation of endothelial transport of low density lipoprotein (LDL) by transcytosis, a critical early step in atherogenesis. Dr. Lee holds a Canada Research Chair in Mechanisms of Endothelial Permeability.

Dr. Sarah Neu
Dr. Sarah Neu is a reconstructive urologist and surgeon investigator at Sunnybrook. Her research interests include population-based epidemiology studies, pharmacological epidemiology, innovative surgical practices, and integrating AI into medical practice
Dr. Anirban Das
Dr. Anirban Das is a paediatric neurooncologist at SickKids, associate member of the Brain Tumour Research Center, and assistant professor in the Department of Paediatrics. His research interests are in germline cancer predisposition and immuno-biology of brain tumours, and in translating these discoveries into novel, biomarker-driven and precision immunotherapy clinical trials for children globally.

Dr. Michael Fehlings
Dr. Michael Fehlings is a professor of neurosurgery and co-director of the U of T Spine Program. He combines a clinical practice in complex spinal surgery at Toronto Western Hospital with translationally oriented research focused on discovering novel treatments for the injured spinal cord.

Dr. Stephanie Lheureux
Dr. Stephanie Lheureux is a medical oncologist, clinician-investigator, site lead of Gynecology Oncology and co-director of the Beyond Chemotherapy Program at Princess Margaret Cancer Centre. Her research interests are focused on gynecologic cancers and early drug development. Internationally, she is co-Chair of the Translational Research Committee and Director representing Princess Margaret Consortium at the international Gynecologic Cancer InterGroup (GCIG).

Dr. Andreea Diaconescu
Dr. Andreea Diaconescu leads the Cognitive Network Modeling group (cognemo.com) at the Krembil Centre for Neuroinformatics, CAMH. As an associate professor of psychiatry, she develops gamified tasks and neurocomputational models combining EEG, fMRI, and behavior to predict psychosis and suicidality.
Redefining Possibility:
Nafia’s
Journey to IMSSA Co-Presidency

By Sara Corvinelli
“When I was five, I couldn’t walk and the doctors couldn’t figure out why. Access to healthcare, and healthcare research in general, is so limited in certain parts of the world. That experience has always stayed with me. It’s things like that that inspire me to keep doing research.”
Nafia Mirza, a second-year PhD candidate at the Institute of Medical Science (IMS), shared her story on how she—as an inspiring student leader—journeyed from humble beginnings.
Born in Bangladesh, Nafia moved to Canada after facing health challenges as a child. She shared how she navigated the healthcare system with her family, thinking she would be paralyzed for life.
“I was born in a small South Asian country [Bangladesh]... their healthcare system isn’t very good. I had a lot of health issues growing up.” Reflecting on that time, she shared, “When I was five, I had GuillainBarré syndrome. And the doctors couldn’t catch on—they had no idea why. Why is this little girl paralyzed? And why can’t she walk? What’s going on? They had kind of given up.”
Nafia’s father had found someone practicing medicine in America who was able to help. The doctor agreed to visit Nafia and subsequently diagnosed her with GuillainBarre syndrome. She then began physical therapy and was able to walk again.
Beyond her own experience with the lack of research and healthcare resources,
she witnessed relatives affected by poor healthcare infrastructure: “Even today, many of my family members have died from curable diseases.” Nafia explained, “Even though we lived in the city and had hospitals, the availability of research was so limited.” Her lived experience inspired her passion for research and global health equity, motivating her to improve access and equity in science and medicine.
While attending high school in Etobicoke, Nafia was not exposed to the different pathways one could take to pursue science. Nafia explained that her high school was poorly ranked amongst schools in the school board and was underfunded; however, this did not stop her from gathering information through her network of friends who were aspiring doctors. She learned of the different undergraduate programs available at the University of Toronto Mississauga (UTM), where she went on to be a student, and grew a passion for neuroscience.
Nafia first got involved in research with the Research Opportunity Program offered at UTM. She explored pain-social cognition research working with mice. She confessed with a laugh, “I realized working with mice was the worst thing ever. They bite you.” Nafia quickly realized her dislike for animal work and pivoted her research to a psychology laboratory where she met PhD student Katie Walsh. In retrospect, Katie’s mentorship was instrumental in Nafia’s academic journey, as she reflects, “Katie was my first mentor. She inspired
me to go into a PhD.” Nafia completed her Master of Science at IMS in 2024 and is now at the Centre for Addiction and Mental Health (CAMH) studying neuroimaging in substance use disorders for her PhD.
As I tried to find a title for this article from the interviewee herself, I asked Nafia: “If you could title a documentary of your PhD life, what would it be?” She jokingly said, “From rats, to riches”. While we shared a laugh and it may seem humorous at first, it captures the essence of her journey and the obstacles she has overcome. Her life may have originated from systemic barriers and unenjoyable first research experiences, but she is now defying limits as the incoming 2025-26 IMS Student Association (IMSSA) Co-President.
Alongside research, Nafia became involved with student life early on as a general member with IMSSA by joining the Academic Affairs Subcommittee in 2022. She was shy at first, but a budding friendship with peer Hamzah Khan helped her gain the confidence to lead the 3 Minute Thesis (3MT) event.
“I joined IMSSA because I wanted to make friends. That was my only goal. I didn’t think I’d be good enough for anything more,” Nafia reflected. “But it kind of sparked something in me that I didn’t know I had.”
Nafia’s face lit up when talking about 3MT, a competition where graduate students present their thesis within three minutes with one static slide. She explained how supportive former IMS Director, Dr.
I keep going because I want to show up for others. That’s what motivates me. “ “
(This is for spotlight photos! Delete this later.)
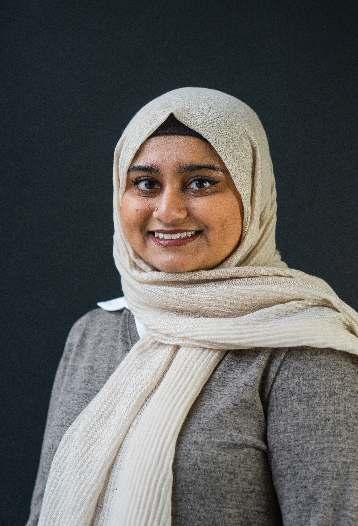
Mingyao Liu, was of the event and how it inspired her to later run for the Director of Academic Affairs: “We always invited him to the event. He kept telling me this is your event, and you need to be the one to give the closing remarks and address the audience. Afterwards he sent an email praising the event. That really gave me a lot more confidence.”
Flashforward three years, and Nafia is now the IMSSA Co-President alongside good
friend Karan Patel. As Nafia puts it, “I never thought I’d have the confidence to run for IMSSA Co-President. But I’m so glad that everything in the past few years at IMS led to breaking that imposter syndrome.”
The common thread through Nafia’s time at IMS is the motivation she has received from peers and the importance of building a network and community at IMS. She puts it simply, “You never know where your peers are going to end up one day. Building that network starts here [at IMS].”
Nafia’s involvement does not stop at IMSSA leadership, as she shared the additional roles she has taken on within IMS, including serving as a peer-to-peer mentor, being a member of the IMS Connects team and the Ori Rotstein Lecture Planning Committee, as well as volunteering with Pueblo Science and MedDash events. Most recently, she attended the Equity, Diversity, and Inclusion retreat at Hart House Farms where she shared discussions on how to improve accessibility and inclusivity at IMS.
Through her experiences navigating academia, Nafia advises students, “Don’t be afraid to get involved. It helps your career in ways you’d never expect and it’s how you meet the people who’ll become your closest friends.” Nafia sets an example to fellow and future IMS students to not let imposter syndrome get the best of you, as confidence can only be grown through action.
I have seen how involved Nafia is with the IMS student community from
playing Catan at IMSSA game nights to volunteering at events together. She inspires and reminds me to keep involving myself with opportunities at IMS—you never know the connections, friendships, and leadership opportunities that await.
“I keep going because I want to show up for others. That’s what motivates me.” This belief is clear when Nafia said, “If anyone is ever going through something in their lab, come to my office hours […] we’ll chat.”
Outside of research and academics, we bonded over shared hobbies, from binge-watching movies and television series, to drawing and reading. Nafia’s recommendations include the Star Wars movies, The Summer I Turned Pretty series, using Procreate to draw, and a recent good read The Invisible Life of Addie LaRue, by one of her favourite writers, V.E. Schwab.
What one might not expect to know about Nafia–with her gentle spirit–is that she is a metal music fan at heart. So, when she is not running 3MT or looking at brain scans, you can find her singing (or should I say screaming) along at a Slipknot concert.
I am excited to see the ways in which Nafia will enrich the student experience and make a meaningful impact on our IMS community in the coming years!
Nafia Mirza, MSc, PhD Candidate and 2025-26 IMSSA Co-President
Photo Credit: Nafia Mirza
From Bench to Biotech
Dr. Anna Badner’s Journey in Neuroscience and Innovation
By Yalda Champiri
When Dr. Anna Badner reflects on her time in the Institute of Medical Science (IMS) program at the University of Toronto, she sees it as the foundation for a career that has taken her from the research bench to the forefront of biotechnology in Silicon Valley. Today, she works at a startup company, Switch Therapeutics, that is developing conditional siRNAbased therapeutics for neurodegenerative diseases–an ambitious endeavour that combines her scientific expertise with the fast-paced environment of drug discovery. With aspirations to grow into leadership roles such as principal scientist, team lead, and eventually, vice president, Dr. Badner is charting a path defined by curiosity, adaptability, and a commitment to meaningful scientific impact.
Dr. Badner’s interest in neuroscience began during her undergraduate studies at the University of Ottawa, where she was drawn to questions exploring how the brain and spinal cord recover after injury. Inspired by the possibility of translational discoveries that could one day improve patient care, she chose to pursue graduate studies at IMS.
Her time spent in Dr. Michael Fehlings’ laboratory was a formative chapter. Immersed in translational research and in vivo disease modelling, she gained valuable exposure to cell therapy approaches and the practical considerations involved in developing
potential treatments. Her PhD work focused on traumatic spinal cord injury and experimental therapies aimed at promoting repair, which provided her with experience in techniques such as in vivo ultrasound imaging and modelling of disease processes. These skills were instrumental in helping her secure postdoctoral fellowships, as they translated directly to other areas of neurotrauma and repair research. “I really enjoyed the freedom and flexibility in the lab,” Dr. Badner recalls. “It was a place where you could follow your curiosity and learn by doing.” That environment also helped her identify the types of work that energized her most, shaping her vision for the future. Following her PhD, Dr. Badner pursued two postdoctoral fellowships that further refined her professional direction. At the University of California, Irvine, she worked with Dr. Aileen Anderson and Dr. Brian Cummings on projects involving traumatic brain injury and cell transplantation. While she valued contributing to this important aspect of the field, she observed the challenges of translating such research into largescale clinical applications. “Neurotrauma research is incredibly important,” she reflects, “but I began to realize that the opportunities for large-scale translation in that space were limited.”
Her second postdoctoral role at Stanford University, under the mentorship of Dr. Erin Gibson, opened the door to work on multiple sclerosis and remyelination,
as well as a front-row seat to the rapid growth of the biotech sector during the pandemic. The combination of her expertise and the timing of industry expansion brought exciting new career possibilities into focus. “I didn’t have one big ‘Eureka’ moment,” she explains. “It was more a series of realizations that built over time, seeing where I could grow, what I enjoyed, and how I wanted my career to evolve.”
Dr. Badner’s move into biotech began with a role at a Stanford spinout company working on CRISPR-edited hematopoietic stem cells for sickle cell disease. Here, she gained valuable insights in clinical trial operations, regulatory interactions, and working within a highly targeted drug development pipeline—expertise that would serve her well in subsequent positions. She quickly learned that industry science often operates under different constraints than academia, with highly focused goals and rapid decisionmaking. Despite the steep learning curve, she embraced the opportunity, noting that the role offered not only valuable skills but also a new perspective on how science is conducted in different settings.
She went on to join a small venture capital (VC)-backed team developing RNA-based therapeutics for Amyotrophic Lateral Sclerosis (ALS) within a Johnson & Johnson incubator, a space where young biotech companies can access labs, resources, and mentorship to

enhance their discoveries. “It was a fantastic experience,” Dr. Badner recalls. “We were just six people, so everyone’s contribution mattered. There was real opportunity to wear multiple hats, learn new skills, and a sense of shared purpose.” Presenting to the board and working in such a collaborative environment deepened her appreciation for the agility and innovation possible in small biotech companies. It also gave an understanding of investor-driven science funding, how
start-up raise capital and what it takes for a company to IPO (be listed on the public stock exchange).
Not every chapter was without difficulty. Startups can face unexpected hurdles, from funding limitations to clinical outcomes, and Dr. Badner experienced the reality of navigating these shifts. Yet, each transition brought new skills, insights, and clarity about her professional priorities. A brief return to academia at the University of California, San Francisco, reaffirmed that her future lay elsewhere. “It helped me see how much I’d grown in industry,” she says. “The pace, the problem-solving, and the variety of work, I realized that’s where I thrive.”
Dr. Badner attributes much of her success to the habits she formed during her time at IMS. Eager to contribute wherever she could, she learned specialized techniques, such as in vivo ultrasound imaging in mice, that became valuable across multiple projects. “If you can pick up a skill that others need, you become an integral part of the team,” she advises. “That mindset led to my involvement in more than a dozen publications during my PhD, and it set me up very well for the future.”
Her advice to current graduate students is grounded in experience: “Be a sponge, learn as much as you can, from as many people as you can. The momentum you build often shapes where you end up. I’ve seen that when people work hard, stay
honest, and commit to themselves, good things tend to follow.”
She is also mindful about how priorities evolve over time. “There’s no perfect formula for balance,” she says. “At different stages, you’ll focus on different things—sometimes it’s your research, sometimes it’s your health or personal life. It’s about knowing what will give you the most payoff in the long-term and trusting that you can shift focus when you need to.”
Looking ahead, Dr. Badner remains passionate about the science at the heart of drug discovery while steadily building the leadership skills needed to guide teams and projects on a larger scale. Each stage of her journey, from the academic lab to multiple startups, has deepened her understanding of how discoveries move from concept to clinic. And while the path has taken unexpected turns, she sees every step as an integral part of her growth as a scientist and innovator. “I’ve loved every part of this journey,” she reflects. “No matter the challenges, I have no regrets.”
From all of us at IMS Magazine, we thank Dr. Anna Badner for sharing her story, and we look forward to seeing how her work continues to shape the future of neurotherapeutics.
Dr. Anna Badner, PhD, IMS Alumnus
Photo Credit: Dr. Anna Badner
Health Equity Through Education
How Pueblo Science Brings Hands-On Learning to the World’s Most Remote Classrooms

By Hamzah Khan
It was the final day of our week-long teaching seminar with Pueblo Science in the remote community of Santa Teresita Dumaran in the Philippines. We had been teaching students how to use and individually program their own soil sensors, to detect when crops needed watering, addressing their community’s need to monitor and maintain adequate watering for their coffee crops. At the end of the session, a young boy approached us. He seemed sad, with tears in his eyes—a stark contrast to the previous days when he was engaged, insightfully answering questions and diligently coding his robot with his team. He expressed his disappointment that we were leaving but thanked us for coming to his town and for the rare opportunity to take part in the session. He radiated excitement about the possibility of us returning next year. It was clear that his tears were of happiness, appreciation, and hope, not sadness.
This moment stuck with me.
This is why I work with Pueblo Science—to give students like him a chance to learn, explore their curiosity, and encourage them to think about pursuing careers in science. Pueblo Science’s model is simple: empower educators and inspire students through hands-on, engaging science education that reflects the needs of the community, using low-cost and locally available materials. Through their efforts, I have had the privilege of working in remote communities, from North Spirit Lake First Nations Reserve, a fly-in only Northern
Ontario community, to Banjarmasin, a river town in Borneo, Indonesia. In these communities, it’s more than science education, it’s about bringing opportunity, inspiration, and engagement. Science education should be for everyone, not only for those with the resources to access it.
What is Pueblo Science?
Pueblo Science is a Canadian charity co-founded by University of Toronto alumni Dr. Mayrose Salvador and Professor Cynthia Goh. The charity aims to increase scientific literacy in underserved communities around the world, creating lasting and sustainable impact by providing local teachers with the knowledge, skills, and tools to effectively deliver engaging science content to future students.
I had the opportunity to ask Mayrose what motivated her to start this organization. She was inspired to create Pueblo Science by her own experience being born and raised in a remote community in the Philippines, where the river beside her house was their lifeline— they used it for everything, including drinking. As a child, Mayrose often experienced stomach pain but did not understand why until she learned about bacteria in her high school science class. After this, she encouraged her community members to start boiling the river water before drinking it, and the change was dramatic. While pursuing her science degree in university, she realized that many of the health and environmental

problems in her community could be prevented through delivering education in a way that was meaningful to their daily lives.
This idea came back to her when she started her entrepreneurship course at the Impact Centre UofT, with supervisor, and co-founder of Pueblo Science, Dr. Cynthia Goh, who had also grown up in a remote village in the Philippines. Together, they pledged to change how science was taught, making it hands-on and related to the community’s lived experiences. They started Pueblo Science by designing classroom activities using locally available materials and training teachers to incorporate these strategies in lesson plans. Eventually, the goal expanded to empower critical thinking in students and to apply their scientific knowledge by designing solutions to community problems.
Hamzah Khan and a group of students after our Robotics competition in Dumaran, Philippines.
Photo Credit: Hamzah Khan

Mayrose shares her advice to students who are looking to make a difference: “Get out into the real world, visit communities, talk to people, and listen to their stories. That’s where you’ll discover the challenges that truly matter.” She emphasizes that to make a difference, you must surround yourself with others who share the same goal. “The world isn’t short on challenges. It’s waiting for people who care enough to do something about them. You don’t need to have all the answers, you just need to start. Innovation begins with action.” This sentiment resonates deeply speaking to the courage it takes to move from ideation to implementation.
Educating About Health
At the root of many global health disparities is a lack of education. By improving health literacy, people can make informed decisions, seek care, and understand the healthcare disparities that affect their communities. Pueblo Science strives to achieve this by incorporating health education into their sessions. In Indonesia, cardiovascular disease (CVD) is the leading cause of death, with CVD-related deaths more than doubling from 1990 to 2019, according to the Global Burden of Disease study.1 To address this, our trip included a session on heart disease where students learned to create and code their own heart rate monitors, and use them to measure changes in heart rates during exercise or meditation. To further develop their understanding, we created simple heart models to demonstrate how exercise increases blood flow through the heart and supports a healthy cardiovascular system.
In the Philippines, dengue fever poses a significant threat to public health.2 Approximately 794,000 cases of dengue occur every year, with 80% of dengue feverrelated deaths occurring in individuals under 20 years old.2 To address this, we taught students about the immune system, and how our body induces fever to fight infection. The students then created their own temperature sensor to track their body temperature over time, learning to apply it to detecting illness and preventing complications associated with high fevers.
By embedding these health topics in their hands-on science lessons, Pueblo Science aims to make health education that is not only engaging but helps students connect scientific knowledge to their own lives and the health of their community.
Learning Goes Both Ways
Teaching and working with students are at the heart of Pueblo Science’s work, but for me, something just as meaningful has been realizing that learning doesn’t flow in just one direction. On trips with Pueblo, I go to teach, but I leave having been taught about resilience, community, and tradition. Knowledge exists outside of research papers and textbooks, it flourishes in the people around you, in your community, in your culture. In North Spirit Lake, we went ice fishing with local leaders, while in Indonesia we learned about Ikat, a traditional form of tie-dye, and in Dumaran, we snorkeled through an untouched coral reef with a local conservationist who has dedicated his life

to protecting the marine ecosystem. These experiences remind me that knowledge isn’t just found by pipetting in the lab or creating a regression model. It can be found in the wisdom of the community’s elders on that ice lake, the hands of the artists weaving a story through Ikat on a cloth, or the passion of a local acting as a guardian of the corals. As an instructor with Pueblo, you come as a scientist hoping to inspire a community, and you leave inspired by the community, with cultural humility, an appreciation for traditions, and an understanding that knowledge comes in many forms.
To get involved with Pueblo Science, check out our website at: https://www.puebloscience.org/.
Muharram FR, Multazam CECZ, Mustofa A, et
Pueblo Science Co-Founder Dr. Mayrose Salvador.
Photo Credit: Mayrose Salvador, Pueblo Science
Sylvia Plath’s The Bell Jar and the Pathologization of the Female Experience

By Josephine Machado
“To the person in the bell jar, blank and stopped as dead as a baby, the world itself is a bad dream.”
Stigmatized for decades, women’s mental health has been made a weaponised issue used to falsely imply that the capabilities of females in society are inferior to that of their male counterparts. Sylvia Plath’s semiautobiographical novel, The Bell Jar (1963), addresses this concept through the lens of protagonist Esther Greenwood. Esther is an ambitious, independent, 19-year-old college student pursuing a prestigious internship in New York City during the summer of 1953, who gradually spirals into a profound depression as she navigates the intricacies of societal pressures on women, mental health struggles, and complex manifestations of intrapersonal conflicts. The poetic nature with which Plath speaks about topics of such serious and vulnerable nature reflects the struggles endured by many women in the 50s and 60s—a product of a culture that dismissed psychological suffering as feminine weakness, when in actuality, this suffering was a result of the biases directed towards women in their various pursuits. As illustrated in the introductory quote, Plath’s bell-jar-metaphor is a representation of an era in which genderbased prejudices were evoked by both psychiatric professionals and society at
large, revealing how women’s distress was often treated, not with empathy, but with alienation and imprisonment.
As Esther’s mental health worsens throughout the progression of the novel, the commonality of medical misconduct during that period of history becomes more apparent—particularly misconduct directed towards women. Soon after seeking psychiatric help, Esther receives electroshock therapy (ECT), a treatment that remains controversial today. Her first treatment—administered by a male doctor—is brutal and inhumane, as it was performed without anesthesia. He doesn’t bother to explain the procedure to Esther or earn her trust. She recounts, that she had “wondered what terrible thing it was that I had done” to deserve such pain. The doctor’s indifference to Esther’s pain reflects the broader objectification of female suffering, where women’s bodies are treated as passive sites for intervention as opposed to individuals deserving empathy and informed care. However, her second doctor, a woman named Dr. Nolan, confirms that it’s “not supposed to be like that…if it’s done properly, it’s like going to sleep.” She assures Esther by stating “I’ll tell you about it beforehand and I promise you it won’t be anything like what you had before.” For almost 30 years, anesthesia was not administered to patients receiving ECT, leaving them at risk for fractures, psychological trauma, and cardiovascular events. Plath criticizes how pseudoscientific and crude practices were inflicted on vulnerable patients,
especially young women, without consent or discussion, despite the information for proper protocol being available at the time. Two recent studies led by the Centre for Addiction and Mental Health (CAMH) have shown the efficacy of ECT when administered properly. Their analyses reveal that among individuals admitted to the hospital with depression, ECT has shown no evidence for a clinically significant increased risk for serious medical events, and is associated with a significantly reduced risk of death by suicide in the year following discharge.2,3 This contrast underscores that even therapies that are proven effective, can still be made a traumatic experience, when proper bedside manner is not made a priority in patient care.
The novel highlights the stigmatization of women’s mental health, particularly through Esther’s mother, who cannot accept her illness. After a moment’s believing her daughter had recovered, she states “I knew my baby wasn’t like that…like those awful dead people at that hospital. I knew you’d decide to be all right again.” Esther’s mother likening her to “dead people” encapsulates the abandonment at the heart of Plath’s critique by illuminating society’s propensity to assign women struggling with mental illness to a liminal state between life and death. She highlights the issue of women’s potential being confiscated prior to even being given the chance of recovery, and the false idea that mental health struggles are a

“choice.” Esther’s mother is not the only one who lacks respect for her hardships, as her ex-boyfriend regards her condition as an obstacle ruining her marital prospects, reciting “I wonder who you’ll marry now, Esther, now you’ve been here.” The intersection of stigmatization and misogyny is made evident by his implication that she has been rendered tainted and undesirable as a woman who has endured mental health struggles.
Esther’s experiences of sexism prior to her stay in the asylum are one of many avenues by which she was led there. Prior to her admission, Esther attends a party, and is assaulted by a man named Marco, who during the attack utters the words “Yes or no, it is all the same.” Esther fights Marco off by punching his nose, but is left shaken and disoriented, having suffered a heinous, life-altering experience. The terror in this scene exemplifies the violent and dehumanizing attitudes with which many women have been both regarded and treated. His actions are a true expression of the objectification of women, illustrating how society at large can be just as hostile towards young women as the asylum itself.
In addition to the violence she experiences, it is evident that Esther feels the pressure of the mid-century feminine ideal to be conventionally attractive, pleasant, and compliant—which directly conflicts with her ambition during a time in which the idea that women can be multifaceted was often rejected. This paradox is represented in what may be the most famous lines to
come from Plath’s novel, often regarded today as the “Fig Tree Analogy”:
“I saw my life branching out before me like the green fig tree in the story. From the tip of every branch, like a fat purple fig, a wonderful future beckoned and winked. One fig was a husband and a happy home and children, and another fig was a famous poet and another fig was a brilliant professor…I saw myself sitting in the crotch of this fig tree, starving to death, just because I couldn’t make up my mind which of the figs I would choose. I wanted each and every one of them, but choosing one meant losing all the rest.”
The cumulative effect of these societal pressures contributes to Esther’s sense of suffocation, communicated through the analogy of the “bell jar” feeling of being trapped, confined, and unable to breathe freely under the weight of expectation. Society’s expectation of what a “true” and “pure” woman should emulate sparked an internal conflict in Esther’s mind. Ultimately, this conflict had fractured her self-perception and contributed to her descent into major depression.
In telling Esther’s story, Plath exposes the systemic neglect and punitive practices surrounding women’s mental health, urging us to reconsider how we perceive and respond to female suffering. The issue of women’s mental health is not new—and must not to be forgotten. We’ve come a long way since Plath’s lifetime, launching multiple initiatives to challenge
mental-health stigmas and empower women. Organizations like the National Suicide Hotline and Kids Help Phone, as well as activism movements such as “Bell Let’s Talk” and #MeToo, demonstrate how individuals of diverse backgrounds have banded together to advocate for those who aren’t being heard. However, the fragility of this progress should not be overlooked. It is imperative that we continue to rise and advocate for one another, as to avoid returning to a darker time.
“How did I know that someday—at college, in Europe, somewhere, anywhere—the bell jar, with its stifling distortions, wouldn’t descend again?”
References
1. Plath S. The Bell Jar. 1st Harper Perennial Modern Classics deluxe ed. New York: HarperPerennial; 2006. 244 p. (Harper Perennial modern classics).
2. Kaster TS, Vigod SN, Gomes T, et al. Risk of serious medical events in patients with depression treated with electroconvulsive therapy: a propensity score-matched, retrospective cohort study. The Lancet Psychiatry [Internet]. 2021 Aug [cited 2025 Aug 2];8(8):686–95. Available from: https://linkinghub.elsevier.com/retrieve/pii/ S2215036621001681
3. Kaster TS, Blumberger DM, Gomes T, et al. Risk of suicide death following electroconvulsive therapy treatment for depression: a propensity score-weighted, retrospective cohort study in Canada. The Lancet Psychiatry [Internet]. 2022 Jun [cited 2025 Aug 2];9(6):435–46. Available from: https://linkinghub.elsevier.com/ retrieve/pii/S2215036622000773
Indonesia, Beyond Bali

By Kowsar Teymouri
After a week of attending the World Congress of Psychiatric Genetics in Singapore, my husband and I boarded a short flight to explore one of our bucket list countries, Indonesia. We were greeted with motorcycle horns, warm smiles, and Nasi Goreng—famous Indonesian fried rice—as soon as we landed in Jakarta. While you might think “Bali” when you hear “Indonesia”, let me tell you that Indonesia is way more; 17,507 islands, to be exact! There was so much to see, and we decided to sample four islands: Java, Borneo, Bali, and Nusa Penida.
Java, the world’s most populous island, surprised us at every turn. After wandering through the old town of Jakarta, where we felt the footprints of Dutch occupation, we headed to Yogyakarta. The first day, we hiked the green terraces of rice paddies, where we were warmly welcomed by the local farmers. The next day, we visited Merapi, one of the active volcanoes in


Java, and interestingly, it had its largest eruption since 1872 in 2010, where over 350 of its residents lost their lives. The village was completely covered in lava, and I couldn’t help but ask our young guide why he was still living there, to which he said, “We are from Merapi, and we die in Merapi.” Next, we wandered through three tiers of Borobudur temple, the largest Buddhist temple in the world, and we were enchanted by its 72 bell-shaped stupas, each holding a Buddha statue. We ended the day at Prambanan, the famous Hindu temple, and watched the sun set behind its 240 structures.
Borneo was the highlight of our trip: Four days cruising through the Kumai River on a Klotok boat, waking up to see the sun rise over the Tanjung Puting National Park. We got to see six primate species in the wild, including the endangered orangutans, the amusing proboscis monkeys, and the energetic macaques. From night trekking to see the shiny eyes of the nocturnal animals in the forest to visiting different feeding platforms where orangutans swung through the trees to
get their daily fruits, we were in awe. Tanjung Puting is one of the two natural habitats of the orangutan, and it is the home of Dr. Birute Galdikas, one of the trio of women—including Jane Goodall and Dian Fossey—appointed by Dr. Louis Leakey to study great apes. We left the island with a heart full of respect for anyone contributing to the rehabilitation of orangutans.
Our trip ended in Bali, where the lush greenery, mesmerizing Hindu temples, beautiful waves of the ocean, and the offerings on the sidewalks will be forever engraved in our hearts. A day trip to Nusa Penida, the pocket-sized island just south of Bali, completed our Indonesia trip, where we got to experience its cliff-edge roads and swim with manta rays and sea turtles while snorkelling. Indonesia was a heaven on earth, and we left with shoes covered in ash, salt on our skin, and a promise to return.
Rice terraces of Java Island - Yogyakarta
Family of Orangutans at the feeding station in Camp Leaky, Borneo
Selfie with the monkey at the monkey forest, Ubud, Bali
Photo Credit: Kowsar Teymouri
Photo Credit: Kowsar Teymouri
Photo Credit: Kowsar Teymouri
UofTTalks 2025
Exploring Modern Stressors on Aging and Health

By Hamzah Khan, Stefan Aguiar,
If you were walking down Sussex Avenue on the night of June 13th, 2025, you might have seen people streaming out of Innis Town Hall. If you were not, what happened was this: a team of graduate students from the Institute of Medical Science (IMS) hosted UofT Talks 2025, an annual TED-Talk style symposium that has become a keystone event for the IMS. It features science communication that bridges researchers, students, and the broader community. This year’s event, titled “Growing Up Today – Modern Stressors on Aging and Health,” was a thoughtprovoking discussion on how 21st century problems such as technology affect sleep and circadian rhythm and explored how these disruptions can impact health across the lifespan.
UofT Talks began as a small initiative but has now become a stand-alone event funded through the IMS Student, Alumni, and Faculty Engagement (SAFE) Committee, which supports and funds IMS-based committees and groups. According to the events official statement
on their website the goal of the event has evolved to “create a dynamic space that facilitates engagement and education, and challenge misconceptions about multi-faceted, complex scientific, and health-related topics.” Each year, a diverse group of students strive to make an inclusive, multi-perspective event through presentations and panel discussions with researchers, industry members, and community members. Over the years the theme of UofT Talks has covered a wide variety of topics, from the opioid crisis to food science.
In 2025, the dynamic line-up of speakers featured researchers in neurobiology, microbiology, and public health, offering unique perspectives on how modern stressors can shape and impact health. Dr. Dawn Bowdish, a professor at McMaster University, discussed how the evolving human microbiota alongside the immune system can impact frailty and susceptibility to disease. In addition, he spoke on the role of microbiome-based nutrition to support healthy aging. Dr. Andrew Lim, a neurologist and sleep researcher at the University of Toronto, talked about sleep misalignment caused by artificial lighting and technology, and how it can impact cognitive function and emotional resilience. Lastly, Dr. Susan Deering, a family physician in Toronto and climatehealth advocate addressed how climate change can act as a biological stressor for vulnerable populations. The panel was moderated by Dr. Ross Upshur, professor at the Dalla Lana School of Public Health,
who helped showcase the connection between these multiple disciplines.
This year UofT Talks was led by two members of the UofT Talks 2024 team: Stefan Aguiar and Anthaea-Grace Patricia Dennis. Stefan is a third-year PhD candidate whose research focuses on psychosocial oncology–particularly, as it relates to patients with advanced cancer considering medical assistance in dying (MAID). Anthaea-Grace Patricia is a second-year PhD candidate and conducts research on applications of machine learning techniques for early detection of Parkinson’s disease and associated cognitive impairment.
When asked why they joined the UofT Talks team, Stefan explained that initiatives like UofT Talks are an amazing opportunity for students to learn about a fascinating field of research and disseminate important scientific discoveries to people that are not familiar with the world of science. Anthaea-Grace Patricia and Stefan enjoyed leading the annual event so much that they have decided to continue in their roles for UofT Talks 2026. They hope to keep the momentum going from UofT Talks 2025, as they truly enjoyed the commitment, company, and journey in creating a successful conference! “A large part of our success was our organizing committee,” Anthaea-Grace Patricia said, “and we hope that the incoming IMS students will be just as drawn to UofT Talks as we were when we initially joined.”
Anthaea-Grace Patricia Dennis