3 minute read
Pleurel Effusions
LIGULA MANGA No. 001 Pleurel Effusions
Why I chose to write about this…
Advertisement
Over the summer, I spent two weeks doing work experience at the John Ratcliffe hospital. For the first week, I was on the respiratory ward, and the second week, I was in the children’s hospital, experiencing paediatric radiology, surgery clinics, and the
woman’s hospital also. I was exposed to the reality of hospital livelihood and through multiple ward rounds, encountering the complexities and less glamorous side of the medical field. One of the most impactful things the doctors involved me in, was the insertion of a chest drain into an elderly woman’s chest. She was experiencing liver cirrhosis and as a result, had obtained a pleural effusion. The registrar showed me how the procedure was done, talking me through each step. He got me really involved in the approach; I helped with the ultrasound scan, used to locate the fourth and fifth intercostal space and then to clarify the catheter has been placed in the fluid in the pleural space. I also helped undress the woman, so the doctor could access her back, as she was frail and unable to do this herself. It resulted in a remarkable two litres of fluid being drained off this tiny woman’s chest. I stood there wide-eyed, taking in what I had just witnessed. The delicacy and precision of modern medicine amazed me as well as what the human body is capable of doing. The experience of being taught by multiple medical students, registrars and consultations over the course of the two weeks has left a lasting impact on me. It has solidified the thoughts I had about doing medicine at university.
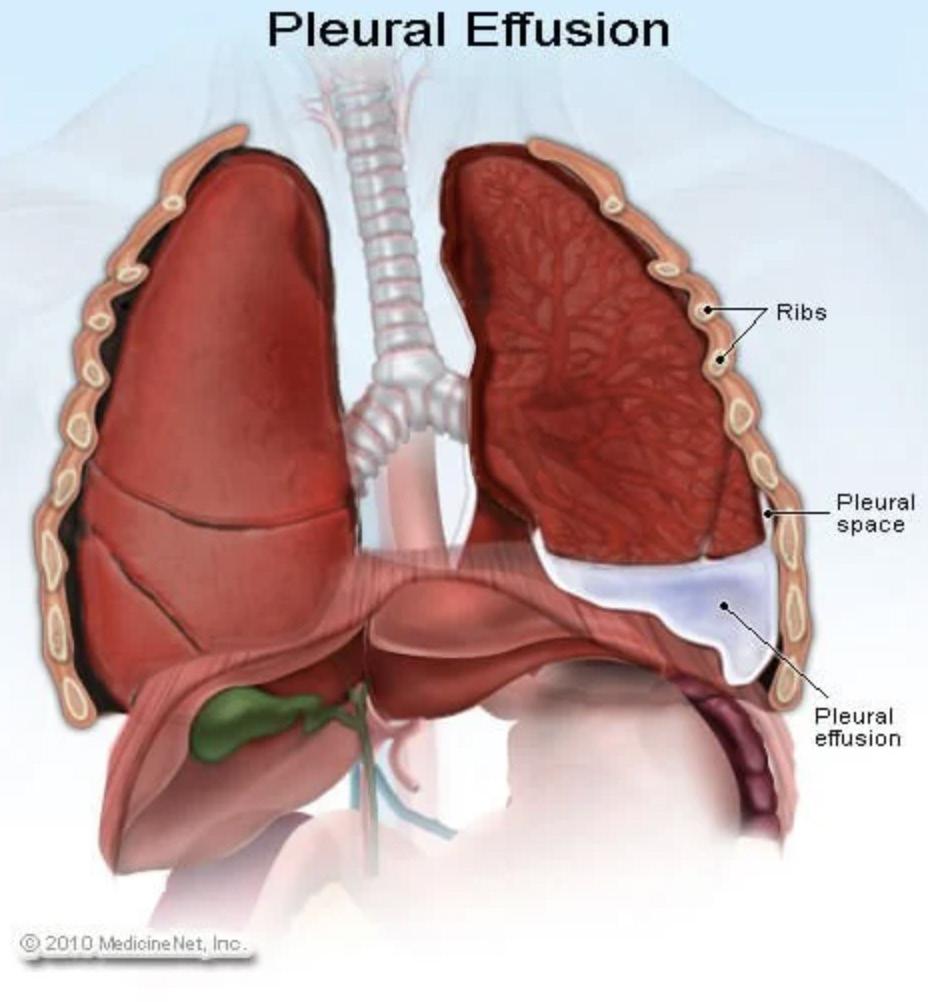
What is a pleural effusion?
A pleural effusion is an abnormal buildup of fluid in the spaces between your pleura. This is the thin membrane lining the surface of your lungs and the inside of your chest wall. Everyone has a small volume of watery fluid in the pleural space, allowing lubrication in your chest cavity for smooth breathing. This fluid can become excessive due to a number of reasons:
Causes:
-Leaking from other organs. Congestive heart failure is the most common cause of this due to the insufficient pumping of blood around your body. Both liver and kidney disease can also stimulate a
build up of fluid in your body which will leak into the pleural space. -Cancer, usually lung cancer -Infections such as pneumonia or tuberculosis
-Autoimmune conditions, for example Lupe of rheumatoid arthritis. -Pulmonary embolism: a blockage in an artery of the lungs, leading to a pleural effusion.

X rays:
On an X-ray, fluid appears a light colour, while air space looks black. This is because structures that are dense will block most of other X-ray particles so will appear white. Therefore, dense material such as metal or contrast media will show up white. Structures containing air, such as the lungs, absorb very little of the X-ray beam. Most of the beam will strike the detector after passing through the air. This results in a black appearance on X-ray. When a patient has a suspected pleu-ral effusion, X-rays are often done when the patient is lying on their side. This is so the doctor can observe whether the fluid is flowing freely within the pleural space.
Treatement:
A doctor may administer the insertion of a chest drain. A small incision is made between the patients fourth and fifth intercostal space flowed by a further dissection down into the pleural space. This is done using a plastic needle to ensure the lung isn’t punctured. A catheter is then inserted and the tube is connected to the drainage bag or chamber. The mechanism lets air/fluid out of the pleural space whilst preventing outside air/fluid from entering the pleural space. An underwater seal is used to achieve this. The distal end of the drainage tube is submerged into water, creating a hydrostatic resistance of +2cmH2O in the drainage chamber. The intrapleural pressure is normally negative however in patients with fluid in the pleural space, this pressure becomes positive. When this pressure exceeds +2cmH2O, the fluid leaves the pleural space and flows into the drainage chamber. This is because it moves from a higher to lower pressure down a pressure gradient. The fluid will then drain using gravity into the drainage chamber and won’t flow back into the pleural space.