BEHAVIORAL HEALTH DESIGN QUALIFICATIONS





HOK is a global design, architecture, engineering and planning firm with over 1,700 professionals across 27 offices worldwide. For decades, we have delivered transformative projects that realize our clients’ boldest visions, combining collaborative innovation with progressive design thinking to enliven organizations around the globe.
In healthcare, HOK partners with leading institutions and health systems to navigate complex challenges while creating adaptable, sustainable care environments. Our patient-centered approach produces spaces that are both cost-effective and inspiring, designed to improve clinical outcomes, enhance experiences for patients and staff, and strengthen community health.
Our healthcare portfolio speaks to our expertise: over 700 projects completed in the past five years, partnerships with more than 16 top-ranked U.S. News & World Report hospitals, and ongoing relationships with over 100 academic medical centers nationwide. This breadth of experience is supported by our integrated team of 250+ healthcare designers, researchers, planners and consultants who continuously redefine operational efficiency, quality standards and safety protocols in every environment we create.
While HOK designs comprehensive acute and ambulatory care facilities, we also excel in disciplines requiring highly specialized, evidence-based solutions. Among these is our behavioral health practice, where we create therapeutic environments that support healing, dignity and recovery for some of our most vulnerable patient populations.


Behavioral health treatment represents a continuum of care from crisis intervention through individually planned treatment to recovery. The architectural response recognizes the inherent dignity of every human being while understanding how different spaces can profoundly influence patients depending on their illness and treatment phase.
Creating effective environments requires careful balance of calming rooms, activity spaces, group areas and private niches, each thoughtfully coded while optimizing patient privacy and essential staff visibility. In late 2023, HOK launched our Behavioral Health Center of Expertise to address the growing integration of trauma-informed wellness design across diverse building types, from healthcare facilities to schools, workplaces and correctional centers.
Space is a contributing factor to healing, our design approach incorporates natural light, biophilic elements, noise mitigation and adaptable spaces to reduce stress and encourage healing. We support activity-based therapies including art, music, movement, cooking and horticulture to provide multiple positive engagement opportunities.
Wyoming State Hospital
Evanston, Wyoming
104 Beds
Alaska Psychiatric Institute
Anchorage, Alaska
72 Beds
Madison Psychiatric Hospital
Madison, Indiana
150 Beds
Evansville State Psychiatric Hospital
Evansville, Indiana
168 Beds
Oregon State Psychiatric Hospital
Salem, Oregon
620 Beds
Junction City Psychiatric Hospital
Junction City, Oregon
360 Beds
Michigan State Replacement Facility
Caro, Michigan
200 Beds
Larue D. Carter Memorial
Indianapolis, Indiana
168 Beds (Programming)
Juneau Psychiatric Hospital
Juneau Psychiatric Hospital
24 Beds
Heartland Human Services
Effingham, Illinois
Outpatient
Stone Institute of Psychiatry
Northwestern Memorial Hospital
Chicago, Illinois
30 Beds
Center for Addiction & Mental Health
Toronto, Ontario, Canada
600 Beds (Master Plan)
Long Beach Mental Health Facility & Community Living Center, US
Department of Veteran Affairs
Long Beach, California
Mental Health - Inpatient (45 Beds)
Mental Health - Outpatient
Community Living Center
Wyoming Life Resources Center
Lander, Wyoming
100 Beds
North Carolina State Hospital System
New Cherry Psychiatric Hospital
Multiple locations, North Carolina
Indiana Regional Treatment Centers
Multiple locations, Indiana
UCLA Neuropsychiatric Hospital
Los Angeles, California
120 Beds
Columbia St. Mary’s Hospital
Lake Drive Main Hospital
Psychiatric Unit
Milwaukee, Wisconsin
HOK designs for a continuum of care, often beginning with crisis intervention and/or stabilization of acute or chronic patients, followed by individually planned treatment and monitoring culminating in recovery. Our comprehensive experience includes forensic hospitals, competency restoration, civil and voluntary commitment, State mental hospitals, behavioral and mental health inpatient units, pediatric and adolescent behavioral health units, geriatric behavioral health inpatient units, med/psych units, eating disorders and substance abuse disorders treatment and recovery, behavioral health emergency care and diversion centers.
MLK Behavioral Heath Center
Los Angeles, California
131 Beds
The Joliet Inpatient Treatment Center
Joliet, Illinois
202 Beds
Western State Behavioral Health Facility
Lakewood, Washington
350 Beds
U.S. Department of Veterans Affairs
Lee County Healthcare Center
Cape Coral, Florida
San Mateo County Maple Street
Correctional Center
Redwood City, California
Davidson County
Criminal Justice Center
Nashville, Tennessee
64 Beds
The Children’s Place
Kansas City, Kansas
Providence Care Hospital
Kingston, Ontario, Canada
St. Joseph’s Healthcare Hamilton Ontario, Canada
Northville State Psychiatric Hospital
Northville, Michigan
Center for Addiction and Mental Health
Toronto and Ontario, Canada
Saint Francis Health System
Laureate Psychiatric Clinic and Hospital Campus Renovation Tulsa, Oklahoma
Southern Nevada Forensic Facility
Las Vegas, Nevada
298 Beds
Jersey City Medical Center,
Psychiatric Emergency Services
Jersey City, New Jersey
University of Iowa Health Care, Roy Carver Pavilion - Behavioral Health
Emergency Department
Iowa City, Iowa
Kedren Community Health System
Kedren Children’s Village
Los Angeles, California
Baycare Health System
St. Joseph Hospital North Behavioral Health Med/Psych Inpatient Unit
Tampa, Florida
Youthscape
Youth Counseling Center
Bute Mills
Luton, England


NEW FORENSIC HOSPITAL
Lakewood, Washington
THIS 350-BED FORENSIC PSYCHIATRIC HOSPITAL WILL PROMOTE A HOLISTIC APPROACH TO REHABILITATION AS PART OF THE STATE’S VISION FOR TRANSFORMING BEHAVIORAL HEALTH.
HOK has been selected to design a 350-bed behavioral health hospital in Lakewood, Washington, a Tacoma suburb. Built to replace the existing 151-year-old Western State Hospital, the new hospital will support the state’s vision of providing transformational behavioral healthcare.
The focus of the new hospital will be forensic to relieve other areas of campus to make room for Civil patients. Programs and design elements will foster a therapeutic, safe environment based on evidence-based healthcare practices. The hospital also will promote research and innovation by fostering partnerships with local academic institutions.
SUSTAINABLITY
LEED Gold Targeted Net-Zero Energy Targeted Mass Timber, Cross Laminated Timber (CLT)
SIZE
550,000 sq. ft. 350 Beds
COMPLETION
2027
COST
$947 M




KEDREN COMMUNITY HEALTH CENTER INC.
Los Angeles, California
Kedren Health has committed to expanding the psychiatric services available to the South Los Angeles community by developing the Kedren Children’s Village, a campus of comprehensive behavioral health services that cover the full continuum of care for children aged five to twelve.
Kedren Community Health Center is a nonprofit organization founded in 1965 with a mission to reduce disparities in access to healthcare services in disadvantaged communities and reduce chronic/acute illnesses that disproportionately affect economically-disadvantaged and ethnically diverse children, youth, individuals and families.
The goal of Kedren’s Children’s Village is to relocate, consolidate, and expand Kedren’s children’s mental health and ancillary services into a single-site, one-stop medical home with wrap-around services to tackle poverty at its roots and fulfill their mission and vision.
The village, being designed by HOK in a design-build partnership with McCarthy, will be comprised of several holistic services and facilities, including:
• mental health clinic and intensive outpatient program
• primary care clinic and center for integrated care
• psychiatric urgent care center
• 24-bed inpatient psychiatric unit
• 16-bed residential sub-acute unit
• transitional housing structure, for families of patients who need immediate housing while waiting for more permanent placement
SIZE
110,000 sq. ft.
COMPLETION
2027
COST
$150 M







REPLACEMENT HOSPITAL
Los Angeles, California
One of the first Design-Build projects at UCLA, the transformation of the former Olympia Medical Center into a state-of-the-art neuropsychiatric hospital by HOK and McCarthy for UCLA Health showcases how we leveraged our comprehensive adaptive reuse expertise to meet critical healthcare needs.
This renovation transforms four disparate and dated hospital buildings into a unified care facility for patients experiencing mental and behavioral health challenges. One major challenge was the low floor-to-floor heights which conflicted with patient anti-ligature safety requirements. HOK worked with Mechanical Engineers to locate equipment on the roof and in the basement, and designed portions of the mechanical system on the exterior to maximize ceiling heights.
Effective engagement with UCLA stakeholders was pivotal to the project’s success. We established multiple meeting levels for various groups including the Steering Committee, Design-Build Core Team, Hospital Champions, and User Groups. The Core Team acted as the project’s quarterback, convening weekly to address design-related queries and keep the project on track.
Our vision was to transform this former medical center into a healing urban oasis. Patients and families are welcomed by a lushly planted garden creating a calming experience as they begin their behavioral health journey. We created a separate staff garden as a respite area for caregivers to recharge and reduce stress. Using warm, natural materials and large windows, we created a strong indoor/outdoor garden connection. Rooted in biophilic design principles, the interior promotes a home-like feeling that creates calmness and tranquility as patients and families heal.
SIZE
170,000 sq. ft.
COMPLETION
2027
COST
$145 M





Las Vegas, Nevada
The progressive treatment model is highly effective in creating incentives for behavioral management, positive engagement in patients/clients, and opportunities for enhanced interaction between care providers and patients to optimize outcomes.
The proposed Southern Nevada Forensic Facility (SNFF) project is based on a progressive treatment model in which patients/clients gain more autonomy and access to more normative environments through participation in programs and behavioral modification. The patient/ clients begin their journey from highly restrictive environments and schedules with focus on one-on-one therapies and once stabilized are engaged in more social, interactive, and enrichment programs including physical activity, art/activity-based therapies, and movement beyond the inpatient unit to the “neighborhood” treatment area. Once patients/clients have progressed toward stability and are being prepared to participate in more “normal” settings, they gain access to the “Downtown” shared activity/therapy space where socialization is broadened beyond their unit cohorts and expanded activities and therapies are offered, such as sports gym, music therapy, more outdoor access.
The progressive treatment model is highly effective in creating incentives for behavioral management, positive engagement in patients/clients, and opportunities for enhanced interaction between care providers and patients to optimize outcomes. This model has been implemented in many psychiatric hospitals in the last decade and proven effective in not only improved outcomes, but also better staff engagement and satisfaction, and reduced anxiety.





Lander, Wyoming
The state of Wyoming hired HOK | architecture+ to develop a strategic plan for mental health facilities in the state.
The Wyoming Life Resource Center in Lander serves those with developmental disabilities and those with dual diagnoses of psychiatric and developmental disabilities. In the context of the overall state healthcare system, this facility is envisioned as a transitional step toward reintegration into local communities for those being discharged from the State Hospital. Much of the existing campus will be replaced with new buildings including eight 10 bed & two 8-bed cottages, yielding a total of 96 beds, day program buildings, a medical clinic, and a recreation and therapy building. The cottages provide small groups of residents and staff that focus on living communally in a residential environment. Five cottages are skilled nursing units for medically frail clients, two cottages are intermediate care facilities for dual diagnoses clients, and three cottages are skilled nursing facilities for clients with brain injuries, dementia, or psychiatric illness.
The Evanston location consolidates civil and forensic inpatient units, administration, and support services that were spread throughout an existing campus into a single building. New treatment spaces, outdoor recreation areas, and central support functions all contribute to increased operational efficiency and a therapeutic healing environment. Phased construction will allow existing beds to be relocated into new construction with subsequent renovations to the existing inpatient building for administrative and support functions.
SIZE
175,000 sq. ft.
104 Beds
COMPLETION
2021
$ 77.8 M







Caro and Northville, Michigan
HOK and architecture+ are designing two transformative psychiatric facilities for Michigan State that replace outdated institutional models with innovative wellness villages centered on recovery and human dignity.
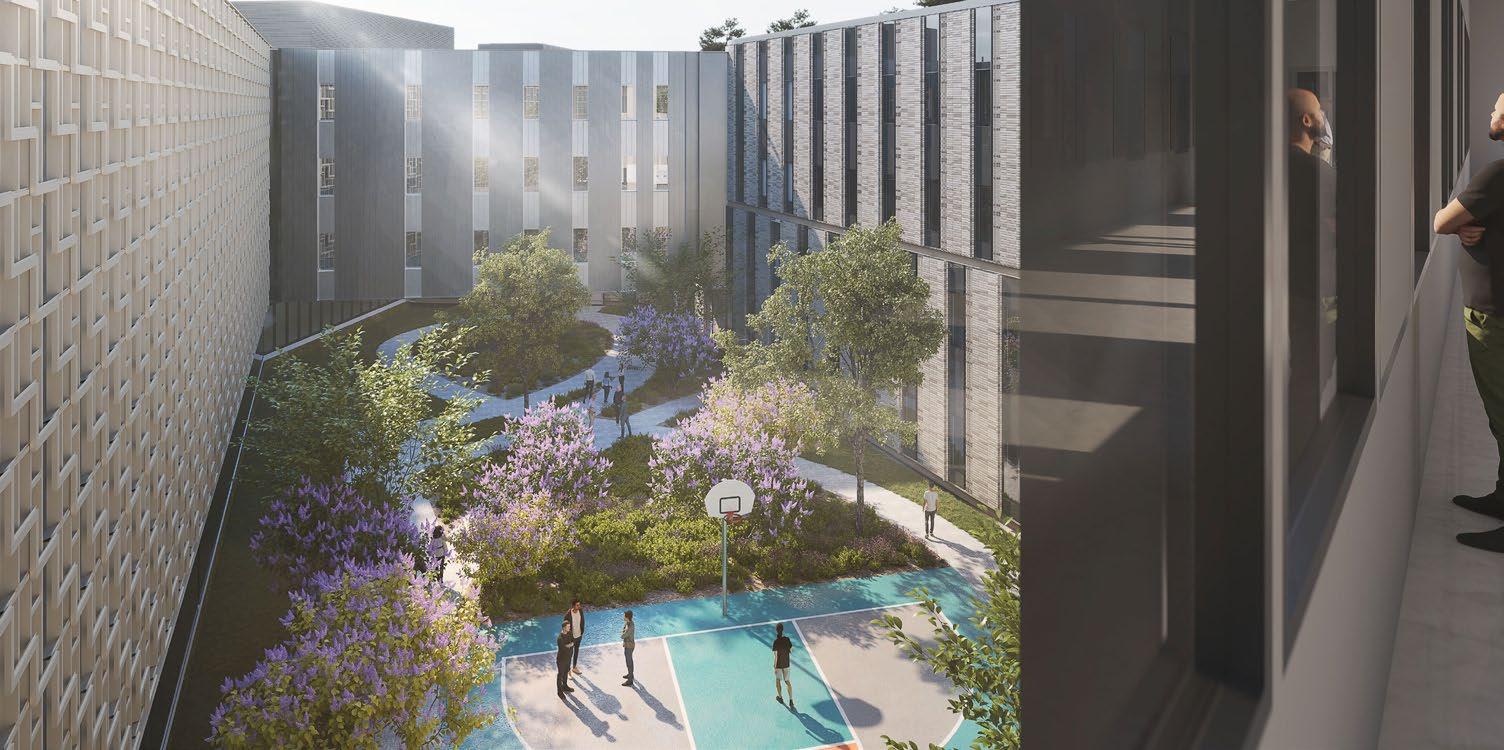
Both the 100-bed Caro Center replacement and the new Northville hospital embody a revolutionary “house-neighborhood-downtown” concept that mirrors everyday community life. These facilities move beyond traditional institutional design to create healing environments where patients progress through carefully sequenced spaces that support their daily routines and recovery journey. The Caro project transforms an archaic cottage-based system into a modern facility featuring flexible unit clusters without traditional nurse stations, maximizing staff-patient interaction on a dramatic 30-acre site overlooking the Cass River.
The design aspirations for both facilities focus on creating wellness villages that celebrate diverse paths to patient healing while facilitating efficient operations. Each hospital connects inhabitants to nature through abundant daylight, outdoor views, and therapeutic courtyards that serve as natural buffers and contemplative spaces. The architectural approach emphasizes welcoming, home-like character through coordinated material palettes, simple clean forms, and calm, understandable spaces that reduce institutional stigma. Working within strict budget constraints, the design team implemented innovative value engineering processes to optimize every building component. These projects represent a fundamental shift toward humane psychiatric care environments that support both patient wellness and operational excellence.






Los Angeles, California
As a pioneering project, the MLK Center delivers highly integrated, easily accessible mental health, substance use and medical services across the continuum of care to the County’s residents.
The MLK Behavioral Health Center replaced the original 1970s hospital building. As one of the first of its kind, the facility provides integrated residential, outpatient and support services for all ages of Los Angeles’ most vulnerable populations, including psychiatric and metal health, substance use disorder, clinical and urgent care, and probation department services.
Rising five stories above grade with one basement level, this adaptive-reuse project renovated the existing interior to coincide with the new program. The design also includes upgrades to the various building systems, exterior façade and site improvements, and a refresh of the building and entrance canopy. Furthermore, the building’s rooftop courtyard was re-purposed for recreational use.
By preserving the existing structure of the original building, which remained closed since 2007, the design reduced demolition and construction costs and the amount of embodied carbon associated with new construction. Façade and building core improvements ensured that the facility was up to code. At the same time, upgrading the building’s HVAC and MEP systems and using the existing OSHPD power and chilled water system increases energy and water-use efficiency, resulting in additional operating cost savings. The center is also powered by on-site solar energy.
SIZE
500,000 sq. ft.
COMPLETION 2020
COST
$240 M





TRAUMA-INFORMED EARLY CHILDHOOD EDUCATION PROGRAM AND COUNSELING CENTER
Kansas, City, Missouri
The Children’s Place (TCP) is a not-for-profit center that supports the developmental and mental health needs of young survivors of abuse, neglect and other trauma.
HOK led the design for the renovation of an existing 35,000 sq.ft. structure that is on the leading edge of integrated healing and learning environments. Having outgrown their existing, dated facility, TCP needed to provide a place of learning and healing for abused, neglected and traumatized children of Kansas City that is both safe and secure while evoking a welcoming, open, fun and calming atmosphere meeting regulations for both child care and counseling spaces.
HOK worked with The Children’s Place to develop a strategic vision document that identified future goals and programmatic needs to grow their mission. This document guided every decision from site selection to classroom design which led to integrated therapy infused child care spaces. Classrooms were carefully placed to allow natural sunlight and direct access to the private outdoor playground allowing healing and learning to occur simultaneously. Environmental graphics were utilized inside and out to create a sense of place for both the children and the surrounding community. HOK worked within a modest budget for this not-for-profit entity.
A place for discovery, mastery and exploration with flexible classroom, therapy, and community space that will allow The Children’s Place to grow and provide much needed services to their local neighborhood and all of KC for many years into the future.
SIZE 35,000 sq. ft.





INPATIENT/OUTPATIENT MENTAL HEALTH FACILITY
Long Beach, California
In order to best serve the 21st century veteran population, HOK is re-imaging the long term stay resident housing and introducing contemporary buildings to best fulfill mental health patient needs of the VA Long Beach Medical Center.
Three separate facilities will cover a large part of the campus and redefine its central spine and residential core with upgrades to the existing Central Plant Facilities.
Although there are more requirements for the Inpatient Mental Health Building than the Community Living Center, the overall design goal is still to be as patient-centered and non-institutional as possible. The building has two 15 bed units on level one with central common rooms and associated support space. The units have shared socialization spaces with direct connections to secure landscaped courtyards and terraces. The design features very large picture windows, in order to provide maximum views out to the lushly planted healing gardens. Select elements are clad in wood and have residential elements designed to be warm and inviting. The shared indoor spaces are connected to outdoor rooms and courtyards.
Total Campus: 332,000 sq. ft.
Community Living Center: 153,000 sq. ft.
Inpatient and Outpatient Mental Health Facilities: 145,000 sq. ft.
Connecting corridors: 5,000 sq. ft.
5 story parking structure
COMPLETION
2013
COST
$220 M







INPATIENT TREATMENT CENTER
Joliet, Illinois
The state-of-the-art facility serves as a national model for mental health treatment in corrections, and provides a healing environment for patients and inmates.
For decades, the Illinois Department of Corrections has been host to some of the most violent and mental unstable inmates in the United States. Under increased pressure from the legal community, form within the system and from advocates of treatment and human rights, the IDOC took action on creating a new facility to address these various issues.
In 2022, a new purpose built mental health treatment facility was open to deliver world class best practice treatment for 200 of the most critically needy inmates in the system. 150 single cell mental health rooms in combination with 50 medical rooms will form the foundation for this program. A new, modern administration building, along with central plan, kitchen, laundry and recreation and program facilities give patients unprecedented access to care. The new facility not only exceeds all relevant correctional standards, but also meets public health standards and as well being fully ADA compliant.
CERTIFICATION
Tracking LEED v4 Silver Certification
SIZE
185,000 sq. ft.
COMPLETION
2022
COST
$152 M






CRIMINAL JUSTICE CENTER
METROPOLITAN GOVERNMENT OF NASHVILLE & DAVIDSON COUNTY
Nashville, Tennessee
The Davidson County Metro Criminal Justice Center offers a mission-driven approach to detention, diversion and treatment in downtown Nashville.
The Davidson County Metro Criminal Justice Center offers a mission-driven approach to detention, diversion and treatment in downtown Nashville. The building houses Sheriff’s Office staff and up to 1,000 inmates.
HOK’s contemporary design blends the often-competing missions of security and treatment. The materiality and massing relate to the surrounding historic civic buildings and courthouse while creating a forward-thinking, modern environment.
An extended civic plaza and new public garden with trees and fountains connect the building to the courthouse and City Hall and act as a public gathering place. From the civic plaza, visitors enter the Center through a glass lobby that promotes the open relationship between the county government and community.
SIZE
405 ,000 sq. ft.
872 Beds
60 Mental Health Beds
COMPLETION
December 2019
COST
$133 M





RE-ENTRY AND ENHANCED ALTERNATIVES TO CUSTODY TRAINING (REACT) CENTER
Modesto, California
The REACT project continues the expansion of the Public Safety Center (PSC) adding a vital step to the continuum of care provided.
The Public Safety Center expansion offers a continuum of care for the detained. The REACT project continues the expansion of the Public Safety Center adding a vital step to the continuum of care provided at the PSC. The REACT includes 288 transitional beds in medium and minimum-security units, jail administrative spaces, secure and nonsecure classroom and training space, kitchen, laundry, and outdoor recreation space. It is designed to be the desired destination for detainees with a more normalized environment, access to a variety of programs, outdoor areas, and a normalized space for family unification.
Key to the project are the program spaces for adult education, religious services, counseling, self-help classes, mental health evaluations/classes, and other life-skills and job/career preparatory programs to help reduce recidivism and assist with rehabilitation.
When inmates are in a stable condition they are placed in an appropriate detention environment. All of which have program and medical/mental spaces immediately adjacent to the sleeping quarters. Many of the units have program spaces available in the dayroom. The design was reviewed by the Sheriff’s PREA compliance officer and provides a safe and secure environment for all ages, races, and genders.
SIZE
288 beds COST
$40 M





LAUREATE PSYCHIATRIC CLINICS AND HOSPITAL
Tulsa, Oklahoma
This project represents a comprehensive transformation of psychiatric care delivery through strategic renovation and modernization. It has undergone extensive improvements that enhance functionality and capacity while meeting contemporary standards for specialized mental health treatment.
The campus transformation begins at the Administration Building, which serves as the primary patient entry point with a new exterior canopy and ambulance bay streamlining transfers. The first floor houses an updated Clinical Admissions Department alongside specialized outpatient services.
McDonald Hall represents the most significant transformation, with the existing building shell receiving its first complete fit-out since the 1980s. Moore Hall serves dual populations through comprehensive updates addressing both geriatric and specialized eating disorder care. The second floor has been re-imagined for female adolescent eating disorder patients, with 22 patient rooms including private and ADAcompliant spaces, therapist offices, classrooms, group therapy rooms, and a training kitchen with dining area for consultations.
Wells Hall serves as the nutritional heart of the campus through renovated and updated kitchen facilities preparing meals and specialized dietary requirements for the entire complex. This building features multiple dining environments including dedicated eating disorder rooms where therapists dine alongside patients.
The Overall Building houses recreational therapy offices, a multipurpose visitor room, art therapy spaces, and a fitness center supporting holistic treatment approaches.
COMPLETION
2027
COST
$80 M






ROY CARVER PAVILIONBEHAVIORAL HEALTH EMERGENCY
Iowa City, Iowa
The Crisis Stabilization Initiative represents a groundbreaking redesign of emergency behavioral health services at University of Iowa Health Care (UIHC), challenging conventional approaches through innovative facility design and clinical protocols.
Facing dramatically increasing behavioral health presentations across all age groups—particularly among pediatric and adolescent populations—UIHC needed to transform its emergency psychiatric services beyond a simple expansion of the existing EmPath Model.
Through collaborative problem-solving, the project team relocated the behavioral health expansion to the South side, enabling a more robust program while creating unexpected opportunities for pediatric ED renovation. This decision challenged earlier planning studies and established an integrated “for all” behavioral health emergency unit model addressing unique clinical needs across age demographics. The solution incorporates dedicated observation spaces for both behavioral health and general medical emergencies, alongside specialized training protocols to enhance care delivery and safety. Throughout implementation, the team navigated infrastructure constraints and adapted to evolving clinical perspectives, creating flexible spaces responsive to changing healthcare needs.
The initiative has delivered remarkable improvements across emergency department metrics, including enhanced throughput, reduced admission rates, improved financial performance, higher patient satisfaction, and decreased length of stay across age groups. This project demonstrates the value of challenging assumptions and embracing iteration in healthcare innovation. By pursuing a more adaptive approach to behavioral health emergency services, UIHC has established a model that effectively serves community needs while maintaining operational excellence, offering valuable insights for healthcare leaders facing similar challenges.
SIZE
18,500 sq. ft.
COMPLETION 2024




JAIL AND BEHAVIORAL CARE CENTER
Oklahoma City, Oklahoma
The Oklahoma County Jail and Behavioral Care Center in Oklahoma City will have 2,328 beds in the new jail.

The facility is a replacement jail for Oklahoma County and will include all security levels of housing (maximum, medium, minimum, behavioral health) and include all support spaces for the jail including: food service, laundry, central plant, medical clinic, behavioral health clinic, intake/booking, vehicle sallyport, new courtrooms, administrative space, program areas for inmates, training facilities and dining areas for detention officers. The building will include secure parking for officers and open public parking.
The facility also includes 60 beds in an adjacent Behavioral Care Center (BCC) that will be divided into three units of 20 beds each for 40 males and 20 females plus a common services and administrative pod that includes counseling rooms, exam rooms, and medical spaces for the Oklahoma County entity. The BCC will serve as a diversion center for detainees who are brought to the facility who may have committed a low-level crime and can be diverted to behavioral care in lieu of being booked into the jail. As a freestanding licensed psychiatric hospital per FGI Guidelines, the BCC will also allow staff to divert frequent offenders and those needing evaluation for a higher level of mental health intervention away from the detention facility. This facility will reduce the jail inmate population and will significantly decrease behavioral health treatment costs for Oklahoma County.
The facility is being designed to include durable, low-maintenance materials, abundant natural lightning housing areas to aid in management of inmates, normative environment, and meet strict security requirements, ACA and ADA requirements, and have capability for expansion in the future.
Jail - 646,041 sq. ft. Jail
Jail Administration, Courts - 102,420 sq. ft.
Behavioral Care Center - 69,438 sq. ft.
Central Utility Plant - 19,921 sq. ft.
Total - 837,820 sq. ft.
COMPLETION
2027





WOMEN’S AND MEN’S CAMPUSES
Boise, Idaho
The new IDOC facilities will respond to the values of the State of Idaho while creating a safe environment for users and the broader community. The design will respect and protect the dignity of each person in custody, as well as each visitor and employee in the building—creating a safe environment for all. The vision for this campus is to be efficient, welcoming, timeless, sustainable, daylit and most importantly—secure.
The design intent for the proposed campus is to function as a healing environment that incorporates connections to nature, equitable access to recreation areas, locations of respite, educational programming and career training opportunities. These factors will reflect a community experience, foster connections and restore victims of crime within a serene and secure location.
The ethos of each design option provides a humanistic approach to the proposed campus, a process that harmonizes the wellness and resiliency of the human experience with the preservation and rehabilitation of the natural environment. Designing with nature and using biophilic principles cultivates an atmosphere of tranquility and rejuvenation, enhancing community and staff well-being within the campus.
SIZE
290,000 sq. ft.
COMPLETION
2027
COST
$160 M






Brooklyn, New York
The new Brooklyn detention facility is the first project being constructed in the Borough Based Jail Program (BBJP), to replace Rikers, under the New York Department of Correction (DOC), delivered by the NY Department of Design and Construction (DDC).
This project was programmed and designed in partnership with these agencies as well as Correctional Health Services (CHS) and other city stakeholders. The new facility was originally programmed for 886 beds but was expanded to 1,040 beds within the original city zoning conditions. Overall, the building is over approximately 20 stories high and roughly 1M gross sq. ft. in size.
The 1,040 beds are subdivided into 42 separate units form levels six through fourteen. Each unit has between 19 and 36 people in custody (PIC) and full support in terms of outdoor recreation, multipurpose, counseling and meal distribution. Each offering more intensive floor has a cluster support for the PICs.
The fourteenth level offers full programming for the entire facility including classrooms, a gym and a horticulture program. This facility accommodates approximately 100 parking spaces, a NYPD sallyport, and full sallyport and loading dock functions at cellar and ground levels. Further, the facility provides full and separate lobbies for both staff and the public. The public will have access to visiting facilities on the fourth level. Staff functions occupy the first through third levels, and include comprehensive.
SIZE
1 M sq. ft.
1,040 Beds COMPLETION 2028
$2.985 B






CRISIS RESPONSE CENTER
Philadelphia, Pennsylvania
The University of Pennsylvania Health system retained HOK to lead the programming, planning, operational analysis and design for the relocation of Pennsylvania Hospital’s Crisis Response Center (CRC), previously located at the Hall Mercer Building on Pennsylvania Hospital’s campus.
The CRC is a key aspect of the Behavioral Health service line for Pennsylvania Hospital, and the overall Penn Medicine organization. It serves Philadelphia as the primary facility for emergency psychiatric care for the Center City area and its surrounding neighborhoods, including specific relationships with the City of Philadelphia’s outreach programs.
With behavioral health becoming more of an emphasis in modern healthcare, the clinical team for this project seeks to be on the leading edge of delivery of care in this highly specialized and unique setting. In keeping with the history of the institution, compassionate care for those in need of the behavioral health services provided by the CRC is the primary goal of this project.
SIZE
15,000 sq. ft.
$9 M







REPLACEMENT PSYCHIATRIC HOSPITALS
Salem and Junction City, Oregon
Comprehensive Campus Transformations Bridging Historic Preservation with Modern Mental Healthcare
The restoration and expansion of Oregon State Hospital represents one of the West Coast’s most significant mental health facility transformations, combining the careful preservation of a historic 1883 Kirkbride Building with the development of a new 174-bed treatment center on a separate 92-acre site. Together, these projects create a comprehensive 620-bed replacement system for Oregon’s primary state mental health institution.
The historic Salem campus restoration brought seismic upgrades, façade restoration, and window refurbishment to the original Kirkbride Building while integrating new structures through an interior circulation spine that connects “downtown” treatment areas with “neighborhood” residential malls. This thoughtful design creates 22 outdoor courtyards where patients can access nature without institutional barriers like fencing and barbed wire.
The new Junction City facility sits within agricultural landscapes, pastures, and wetlands, with building forms that echo the region’s journey from the fertile Klamath Valley to the coastal and Cascade mountain ranges. The 174-bed center houses a mix of civil and forensic adult patients across hospital beds, secure residential treatment facilities, and independent living cottages, all designed around a “Journey of Recovery” philosophy emphasizing healing, organic, and light-filled spaces.
Both projects represent a shift from traditional unit-based care to a recovery-based treatment mall concept, prioritizing individualized treatment plans and creating uplifting environments that harness the healing power of nature through visual connections to the outdoors and nature-inspired color palettes. The result is a modern, efficient, and humane campus system that honors the facility’s historic significance while establishing new standards for psychiatric care delivery.
850,000 sq. ft.
sq. ft. 620 Beds
Beds





Shiva Mendez
CID, IIDA, LEED AP BD+C, EDAC, CCHP
Principal | Behavioral Health
Practice Leader

Virginia Pankey
AIA, LEED GA, EDAC
Principal
| Behavioral Health Practice Leader
As a Behavioral Health Practice Leader, Shiva brings recognized expertise in behavioral health environments with more than 30 years of experience as a medical planning and design professional. Her specialization includes pragmatic design solutions, knowledge of behavioral health products and systems, and comprehensive understanding of applicable codes and considerations for adolescent mental health facilities.
Drawing from extensive experience planning outpatient pediatric and adolescent clinics, Shiva understands environmental triggers for diverse young users and guides design teams in creating welcoming spaces that empower children and families, provide choice and control, and reduce anxiety. Her collaborative approach involves working closely with project teams, facility leadership, and diverse stakeholders to develop environments that support therapeutic goals.
Shiva’s design considers integrated safety features, security systems balanced with therapeutic openness, and acoustic and sensory considerations that enhance user experience.
Virginia is a recognized leader in the planning of healthcare facilities, including focuses in acute care and behavioral health. She practices purpose-driven architecture, creating environments for individuals with behavioral and mental health needs across the continuum of care. Her experience ranges from programing through design development and construction administration. Her strength as a communicator allows her to facilitate discussions with the client that increase operational efficiency in the design or encourage collaboration in the planned facility. She is driven by curiosity, which leads to innovation in design and industry guidelines.
Virginia prioritizes addressing current challenges, anticipating future scenarios, and designing for flexibility to accommodate evolving technology, equipment, and processes over the building’s lifespan. She serves on the Health Guideline Revision Committee for the Facility Guidelines Institute, co-chairing the Behavioral and Mental Health Topic group, has spoken at conferences, and published white papers on behavioral health facilities.

AIA, NCARB
Principal |
Practice Leader
Kristen has over 15 years of experience in the architecture industry as a licensed architect, programmer, and planner and is highly adept at a variety of aspects of the design process including program management, facility analysis, and construction documents. She is well versed as a justice, courts, and juvenile planner, which is made robust by her experience as a medical and mental health Subject Matter Expert. Her versatility has led to her involvement in projects all over the country, focusing on Trauma Informed Design, master planning, and security analysis. Kristen is well-known for her client-focused approach to design, considering all aspects of the project from beginning to completion, and is passionate about the quality and outcome of the spaces she designs.
Kristen approaches justice and correctional projects with exceptional sensitivity, recognizing that many youth in these facilities have experienced significant trauma and require environments that support healing rather than further harm. Her design philosophy emphasizes creating spaces that maintain necessary security while preserving dignity and promoting rehabilitation.
“Throughout my career, I’ve been striving to make healthcare more humane by breaking the false choice between safety and humanity. People who are alone with their thoughts need a therapeutic environment that supports them and builds trust with their caregivers while maintaining safety.”
- Shiva Mendez
“I’m personally drawn to behavioral health knowing and loving people who struggle with these challenges, as so many of us do. I want to thrive in purpose and mission-driven work and I believe the environment makes a difference in healing. What we do facilitates the betterment of mental health patients through whole person care.”
- Virginia Pankey
“I want to provide solutions that change the lives of people using behavioral health facilities – people who have been the most forgotten and almost shut off from society. As designers, we’re responsible for an environment that reflects dignity and promotes comfort when someone is dealing with emotional struggles and chemical imbalances they didn’t necessarily choose.”
- Kristen Zilch-Markos