henryford.com/transplant
Alcohol-associated liver disease program meets a unique need
Two key elements of alcohol-associated liver disease (ALD) demonstrate the need for interprofessional management. First, hazardous alcohol use and alcohol use disorder (AUD) are matters most often addressed by behavioral health and addiction professionals. Second, acute and chronic liver diseases and transplantation are the focus of hepatologists and hepatobiliary surgeons. The large and consequential gap between these biomedical and psychosocial care silos is a key reason many ALD patients do not receive the care they need. This is where Henry Ford Health has stepped in. The interprofessional Alcohol-Associated Liver Disease Program at Henry Ford Hospital provides medical and psychosocial evaluation and treatment for the breadth of ALD.
“No one specialty alone can fully treat a patient with ALD because of their many interprofessional needs,” explains Scott Winder, M.D. , senior staff psychiatrist, Henry Ford Transplant team. “ALD is complex because it isn’t just one thing; liver disease is the physical manifestation of habit, addiction, and psychological distress, we have to treat all of it.”
Jessica Mellinger, M.D. , senior staff hepatologist explains, “to be most effective in treating patients with ALD, the clinic is ideally co-located so behavioral health and hepatology are in the same space, working with the same patients at the same time,” She adds,
“We’ve created a one-of-a-kind of program in Michigan given we have ALD outreach clinics located throughout the state and virtually. There are three inclusion criteria to be seen in this clinic:
1. diagnosis of alcohol-associated hepatitis or alcohol-associated cirrhosis,
2. alcohol use within the last six months, and
3. the patient must be willing to speak with a behavioral health professional.”
The Henry Ford Health ALD Program has been designed to care for patients over the “life of the liver,” explains Dr. Mellinger. “Patients need cohesive, high-quality care whether they have earlier stages of ALD or recurrent alcohol use after liver transplant.” Many patients will require long term care. She adds, “some patients who stop alcohol become too medically well and ineligible for liver transplant but that is not a time to stop supporting them.” Dr. Winder adds, “unfortunately some patients die despite our best efforts. Yet some of the sweetest moments of my career have been witnessing people close to death stopping drinking, taking their lives back from alcohol, and restoring their dignity prior to passing away.”

The need for this type of program is significant given the high prevalence of hazardous use in society and among patients with liver disease. CDC statistics indicate that between 2017 and 2020, deaths from ALD disease rose, accelerating during the COVID-19 pandemic, with mortality increasing in every age, gender, and ethnic demographic in the U.S. Dr. Mellinger notes, “many younger people are affected, especially young women, with a disease that was once thought to primarily affect middle-aged men.”
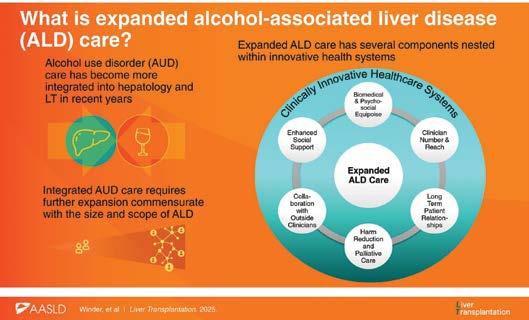
The ALD program is relatively new at Henry Ford Health. In addition to Dr. Mellinger and Dr. Winder, the ALD team includes: Syed-Mohammad Jafri, M.D., hepatologist, Shivali Patel, M.D., psychiatrist, and Cindy Kim, RN. In their recent article published in Liver Transplantation the team identifies components of ALD care that expanded beyond single clinics: biomedical and psychosocial equipoise, adequate clinician number and reach, long term patient relationships, harm reduction and palliative care, collaboration with clinicians within the health system, and enhanced social support, all nested within an innovative health system like Henry Ford, shown in Figure 1.
“Our expansion goals also include incorporating the ALD Program into alcohol rehabilitation hospitals, which to our knowledge has never been done,” says Dr. Winder. To collaborate with clinicians outside Henry Ford Health, “we plan to offer regional continuing education didactic seminars to build relationships and disseminate knowledge involving providers of many disciplines and specialties,” explains Dr. Mellinger. “We are just getting started—there so many exciting possibilities to bring excellent care to this underserved population.”
To read the article, go to: DOI: 10.1097/LVT.0000000000000638
Breakthrough in heart transplantation: Michigan’s first beating-heart transplants
Ken Miller of Ferndale woke up on his 58th birthday to extraordinary news: he was the recipient of the first beating-heart transplant in the state of Michigan. He is one of only a few people in the country to ever undergo this surgery that promises better outcomes and more access to donor hearts for those waiting.
This groundbreaking medical procedure, led by Cardiac and Transplant Surgeon Kyle Miletic, M.D. along with the Henry Ford Hospital transplant team, successfully implanted Miller’s new heart while it was still beating. Miller also received a simultaneous kidney transplant. This is believed to be the first dual-organ beating heart transplant in the country. Then, three weeks later, Dr. Miletic and the team performed a second beating-heart transplant, believed to be the second of its kind in the state. While not yet standard nationwide, beating heart transplant is now standard at Henry Ford for any case using the TransMedics OCS perfusion system.
“I woke up on my 58th birthday to a new heart, a new kidney, and thanks to this team at Henry Ford, a new lease on life,” said Miller. “I think it’s simply a miracle.”
Alongside Dr. Miletic, Hassan Nemeh, M.D., surgical director of Thoracic Organ Transplant and division head of Cardiac Surgery at Henry Ford Health , performed a second beatingheart transplant in mid-June. Dr. Nemeh explains, “beating heart transplant is novel. The first one was performed out-of-state less than a year ago.” To date, only about 70 beating heart transplants have been performed in the United States.
“These two successful surgeries represent a significant advancement in organ transplantation for Henry Ford, the state, and the region, and it offers hope to so many patients awaiting life-saving procedures,” says Dr. Nemeh. The medical world is constantly seeking novel approaches to increase organ transportation and transplantation for the approximately 3,500 people in the United States who wait. Beating heart transplants offer healthier hearts that lead to better outcomes.
This extraordinary technological advancement keeps the heart pumping during transport. TransMedics OCS perfusion system, known as ‘heart in a box’ allows viable donated hearts to be transported from further away than traditionally possible which makes the possibility of more hearts for those who are waiting.



Traditionally, a heart is stopped, removed from the deceased donor, and transported on ice to the hospital where the transplant will occur. Donated organs placed on ice remain viable for a limited amount of time, thereby limiting the distance they can travel and, ultimately, the number of organs available for transplantation.
Dr. Miletic says, “the heart in a box is like a mini heart and lung machine that we use for traditional openheart surgery. Surgeons stop the heart at the donor hospital and put it on this machine. The machine restarts the heart and gives it all the blood and nutrients it needs to stay healthy, so while it’s traveling to Henry Ford Hospital, the heart never loses its blood supply and never stops beating until you take it off the device.”
Dr. Miletic explains, “while still on the device, we placed a cannula in the donor heart and connect it to the bypass machine that the recipient is already on. This cannula provides the recipient’s blood to the heart the entire time we were sewing it into the patient. Because the heart is getting blood flow, it keeps beating the whole time we perform the procedure. We know that multiple periods of ischemia to the heart lead to substantially worse outcomes. By preventing the ‘two-hit’ ischemiareperfusion injury that has plagued traditional OCS organ transport, we avoid a lot of the early primary graft dysfunction.”
A beating heart is a healthier heart to transplant, “if the heart only has to stop once, the muscle remains stronger and outcomes for the patient are better. It decreases the chances that the heart will need machine support, such as a balloon pump or ECMO after transplant, which can lead to longer recovery times for the patient,” explains Dr. Miletic.
“It’s more challenging to sew in moving tissue, but this patient was exceptionally suited for this transplant method,” says Dr. Miletic. “Because this patient’s heart was so damaged over the years, it had grown to twice its normal size, providing more space for us to operate. This was also his first surgery which reduces complications due to scar tissue from previous operations. In this case, conditions were near perfect for us. This heart was much stronger and more robust than we typically see after the traditional method of stopping and restarting the heart twice.” Miller did not need added support after surgery.
“In 20% to 30% of cases where the donor heart is stopped and restarted twice on the OCS, patients’ recovery involves the support of a machine such as balloon pump or ECMO. Down the line, that may lead to complications such as strokes, kidney and liver damage. Avoiding that is likely to improve long-term outcomes and make the overall recovery process easier,” Dr. Miletic explains. All studies published so far have shown significantly improved short- and medium-term outcomes with the beating heart technique compared to traditional arrested heart OCS implantation.
“I live comfortably with my rescue dog, Chip, and I’m excited to be home and relax and get back to normal—to see my children and grandchildren, to sit and play my guitar again. I’m so grateful to these doctors to be able to say that,” Miller says.
By the time Miller’s double transplant surgery began on May 31, he’d been in Henry Ford Hospital for several weeks, receiving mechanical support from a balloon pump for his failing heart while awaiting a heart transplant. He had been battling heart disease since 2013. Heart failure led to kidney failure, and the need for a kidney transplant, too. Miller and his new heart and kidney are recovering well.
Dr. Miletic was assisted by his cardiac surgery partner Dimitrious Apostolou, M.D.,Anesthesiologist Rachel Diehl, M.D. and Perfusionist Mary-Margaret Looby, a highly skilled professional who runs the heart and lung machine during surgery and regulates and monitors blood flow to the donor heart during the implantation.
Miller, who suffered a heart attack in 2013, forcing him to retire from the dairy in Livonia where he worked for 30 years, says even when other physicians told him there was not much that could be done for him unless he received a new heart, he always held onto his faith that everything would be okay.
“I knew I’d need a new heart one day. I never dreamed it would be this special,” Miller said. His family has established a fundraiser through Help Hope Live to help cover medical bills.

Second Patient
In the second beating-heart transplant case performed at Henry Ford Hospital, the donor heart was transported from nearly 2,000 miles away and was outside the body for nearly seven hours due to travel time. This transplant represented the farthest distance a heart has traveled from donor to recipient at Henry Ford. Traditionally, transplant centers have been limited in how far away they could accept offers given time constraints. With the combination of the OCS technology and beating heart technique, Henry Ford is now able to accept organs from essentially the entire continental United States, which can increase the donor pool and, ultimately, the number of transplants that can be performed.
“Even though the box gives us more time to travel, it is not unlimited, and we have seen some issues with donor heart function when the heart is out of the body for too long,”
Dr. Miletic says. “Therefore, I felt the additional protective effects of the beating heart technique were even more important for this patient.”
The donor heart worked well immediately, and the patient had a very unremarkable recovery, going home three weeks after surgery. He continues to do well to this day.
“It takes a team with extensive experience and a spirit of innovation to make a groundbreaking procedure like beating-heart transplant go off without a hitch,” says Dr. Marwan Abouljoud , director of Henry Ford Transplant “The success speaks not only to the technological skills of our surgeons, but the strength of the team that makes Henry Ford Michigan’s Transplant program so successful.”
Dr. Miletic discusses the beating heart procedure on YouTube: bit.ly/HFbeatingheart.
Decades of success: milestones built on collaborative innovation
“Decades ago we realized we needed to think differently about liver transplantation as one of the most complex specialties of medicine, it requires a lot of people with expertise in every specialty and subspecialty,” Marwan Abouljoud, M.D. , director of the Henry Ford Transplant program and liver transplant surgeon begins. “It took a lot more than we expected, but we learned along the way, gathered support and confidence in our program from our administration, physicians and community,” he notes.
For nearly 30 years, Dr. Abouljoud and his partner Kimberly Brown, M.D. , associate medical director and hepatologist, have been the visionary leaders of the innovative Henry Ford Liver Transplant program along with Dilip Moonka, M.D. , medical director of Liver Transplant who joined shortly after. They each share that the framework of collaboration within a team culture, communication and trust are the keys to delivering excellent service to each patient and each other. “That has served us well as we built and as we continue to innovate and expand the program,” says Dr. Abouljoud. Dr. Moonka adds, “teamwork is key, we have a lot of moving parts and each of us brings our expertise to care for the patient, plus we enjoy working together.”



Dr. Brown shares, “from inception of the program we learned to trust each other’s expertise. Our success is multifaceted, as the medical team, we uniquely establish a patient’s hepatology care before and after surgery and transplantation is the role of the surgeons.” Dr. Moonka explains “we build lifelong relationships with our patients from our first medical encounter, treating each patient until a transplant occurs and continuing post-transplant lifetime management of their immunosuppressants.”
To advance the growth of the program, Dr. Moonka shares, “unlike most specialties to grow, a strong team of clinicians is
needed to maintain excellent patient outcomes and positive patient satisfaction—we believe we have that team. We all work diligently to maintain relationships with our community of referring physicians who trust our team to care for their patients.” Dr. Moonka says, “I can’t stress enough the role of the nurses, medical assistants, social workers and psychologists. They are the face of our program.”
Through their leadership many milestones have been achieved. Since 1988 through 2024, 2,611 liver transplant patients were treated in the largest liver transplant program in Michigan. Achieving many milestones and several firsts have made the transplant program the most experienced in the state:
• FIRST IN Michigan to perform a split-liver transplant from a deceased donor (1996)
• FIRST IN Michigan to perform an adult-to-adult living-donor liver transplant (2000)
• FIRST IN Michigan to perform laparoscopic surgery for living donor liver transplantation (2008)
• FIRST IN U.S. to use sofosbuvir, investigational medication for hepatitis C post-transplant (2012)
• FIRST IN Michigan to perform a lung-liver transplant (2013)
• FIRST IN Michigan to perform an adult heart-liver transplant (2015)
Also among the first in Michigan achievements is the Henry Ford Outreach Clinics in cities throughout the state. “We started with kidney clinics, then expanded to liver clinics,” explains Dr. Brown. “Literature now shows, and so does our data, that the further you live from a transplant center, the less likely you are to receive treatment. While it’s a great competitive strategy, as other transplant centers around the country have discovered, patients have access to our transplant experts without travel.” Physicians rotate travel to the outreach clinics, patients come to Henry Ford Hospital for transplant, and they are followed posttransplant back in the outreach clinics.
Surgical Director Shunji Nagai, M.D. , Liver Transplant, Intestine Transplant and Rehabilitation and Transplant Surgery Research, explains that the liver transplant program reached another milestone. “In the first 6 months of 2025 over 100 liver transplants have been performed.” Dr. Moonka adds, “we are on pace to achieve 180, which is a 50 % increase from the prior year.”
• FIRST IN Michigan to perform a heart-liver-kidney transplant (2018) continued on page 9
Big ask, big give initiative
Asking a loved one or a friend to donate an organ is a BIG ASK. Hesitant to discuss their illness, living donor candidates struggle with starting a tough conversation about living donation. Nearly 60 kidney transplant candidates learned how to develop strategies to ask for kidney donation on March 17, 2025, in a hybrid virtual/ in person workshop presented by the Henry Ford Center for Living Donation, in collaboration with National Kidney Foundation of Michigan.
The content centered on building trust around the facts and addressing myths of living donation. Speakers included several Center for Living Donation team members: Jason Denny, M.D., director, Center for Living Donation and surgical director, Living Kidney Transplantation, Rohini Prashar, M.D., medical director, kidney transplant program; associate director, Center for Living Donation, Meghan Whittaker RN and National Kidney Foundation, Michigan team members. Several patients shared their stories, including Kristin Larkins, RN, a kidney transplant coordinator in the Henry Ford Transplant program, who donated a kidney to her mother. Martha Stella, who is both a Henry Ford Hospital nurse and a liver transplant coordinator, and a recipient of a living donor kidney transplant, also shared her story and answered questions. Other living kidney donors and recipients shared their stories including those of kidney paired donation, a scenario where living kidney donations are matched with appropriate recipients across a group of patients. “Hearing other patient’s share their experiences is inspirational to those who will soon be making the same type of ask,” Dr. Denny explains. “It’s not just about their experiences but knowing others have been successful in finding a living kidney donor is reassurance they can do the same.”





Surgical Director Dean Kim, M.D., Kidney and Pancreas Transplant and Chief of Transplant Services, Children’s Hospital of Michigan says, “we tell our patients that the best kidney is from a living donor, but we were not giving them the tools or resources to ask for that donation. Now we

are supporting out patients in their ask for a living donation.” He explains, “it’s important because a living donor kidney provides longevity for the patient over a deceased donor kidney, especially when it is a child who has decades of life to live. Through living donation, we can gather the best medical information from the donor, which means we can transplant a high quality kidney.”
Understanding the facts of living donation included:
• For the donor, all costs are covered by recipients’ insurance.
• Recovery for the donor is 4-8 weeks.
• Quality of life post-donation is equivalent to non-donors
• Donors save a life, and feelings are euphoric about their BIG GIVE.
For the recipients of a living kidney donation:
• The wait time for kidney transplantation will be lesser than deceased donor kidney transplant.
• Both the recipient and the kidney donor are healthier compared to waiting for a deceased donation.
• The donated kidney begins to function immediately and has an average lifespan of 10-15 years, which is longer than the life of an average deceased donor kidney transplant.
• If a potential kidney donor is not a match to the recipient, a paired match with another donor can be arranged.
The interactive sessions focused on seven key strategies and tools to make the BIG ASK: 1) busting myths; 2) knowing the facts; 3) how to tell the candidate’s story, 4) using the DONOR app; 5) finding and utilizing the help of donor champions and advocates; 6) creating an action plan and, 7) using resources to guide the candidate until a living donor steps forward.
“This initial community outreach workshop was very successful,” says Dr. Prashar, “we already are planning for future workshops for other geographic areas.
Candidates interested in attending the next event may contact Meghan Whitaker, RN, (email: mwhitta1@hfhs.org) who is the lead for this event and a Henry Ford Health living donor transplant coordinator.

Amanda Su, M.D.
Sr. Staff Transplant Hepatologist
Specialties: Gastroenterology, Transplant Hepatology
Board Certifications
The American Board of Internal Medicine - Gastroenterology
The American Board of Internal Medicine - Internal Medicine
Education
Weill Cornell Medical College, NY
Fellowships
Johns Hopkins University School of Medicine, Gastroenterology, MD
Johns Hopkins University School of Medicine, Transplant Hepatology, MD
Residency
Johns Hopkins University School of Medicine, Internal Medicine, MD

Gerald Scott Winder, M.D., MSc, FACLP
Sr. Staff Psychiatrist
Specialties: Psychiatry, Consultation-Liaison Psychiatry
Services: Behavioral Health
Board Certifications
American Board of Psychiatry and Neurology - Psychiatry
ABPN-The American Board of Psychiatry and NeurologyConsultation-Liaison Psychiatry
Education
University of Utah School of Medicine, UT
Fellowship University of MichiganAnn Arbor, Consultation Liaison Psychiatry, MI
Residency
University of MichiganAnn Arbor, Psychiatry, MI
Dr. Su treats patients at: Henry Ford Cancer - Detroit
Henry Ford Hospital K Building
Henry Ford Medical CenterBloomfield Twp
Hospital Privileges
Henry Ford Hospital
Henry Ford Jackson Hospital
Henry Ford West Bloomfield Hospital
Dr. Winder treats patients at: Henry Ford Hospital K Building
Henry Ford Specialty Center –Lansing
Hurley Clinic – Flint
Decades of success: milestones built on collaborative innovation
continued from page 6
Both Dr. Nagai and Dr. Moonka attribute this growth, in part, to the FDA approval in 2021 of machine perfusion during transportation of the liver which reduces ischemia damage. “This means we are transplanting healthier livers that have been perfused using human, oxygenated blood. Often the liver will be healthier than it would without perfusion, and the quality of the grafts is better,” Dr. Nagai shares. “The pool of livers has expanded and reduced a recipient’s transplantation wait time, so the patients are healthier than they would have been with a longer wait.” In addition, Dr. Moonka notes, “because hepatitis C treatment is so effective, now that hepatitis C infected livers can be used for transplant with a cure rate greater than 99%, contributing to more available organs.”
Yet, as Dr. Brown points out, “we always need more organs, and we need good outcomes for those organs. That’s where innovations like living liver donation come in, we continue to raise awareness of the need for more donors.” Dr. Moonka adds, “Henry Ford really pioneered living donor transplant in Michigan and has one of the largest experiences with this in the Upper Midwest.”
All members of the team noted, that with effective treatment for hepatitis C, there has been a shift towards patients with alcoholic liver disease and fatty liver disease seen in heavier patients who may have diabetes and elevated lipids. These patients have their own challenges, but Henry Ford has maintained outstanding outcomes.
Double- lung transplant recipient achieves the 25-year mark
Diagnosed in 1988 with Sarcoidosis, the disease caused granulomas to grow in her lungs making it increasingly difficult for her to breathe. By July of 1999, the increasing dosages of prednisone and constant oxygen that had kept her stable for years were no longer working. Her doctor placed her on the organ transplant list—she needed two lungs to survive.

Pam’s Donor
Over the 4th of July in 2000, Pam Powell would have more than one live-changing event. Pam shares “Friday while listening to Good Morning America, they talked about the number of people who would die that weekend due to drunk driving. I prayed that if someone had to die that it would be someone who could give lungs. That Saturday David and I met with our parents and expressed our desire to get married. And, during the consultation with David’s pastor, Dr. Marshall Hall, he spoke a prophetic word into my life. He stated that my condition was temporary. And that evening we got the call from the transplant coordinator ‘we’ve got lungs for you,’” Pam recalls. By 11:30 p.m. Pam and her family were at the hospital, “Overnight I received
a double-lung transplant, but I didn’t know it until the following Friday when I woke up.” David and Pam married three weeks after her release from Henry Ford Hospital.
It was not a car accident that brought Pam her new lungs. It was an allergic reaction to peanuts that took the life of 12-year-old Brad. “Brad’s parents donated many of his organs and I got his precious lungs—I have what they lost that day,” says Pam. “We met by accident at a Gift of Life transplantation event. I shared my story with the attendees and sang The Wind Beneath My Wings that day. Brad’s parents, who were there, figured out I have Brad’s lungs and introduced themselves to me—David and I became part of their family that day.” Pam says, “of all the recipients of Brad’s gifts, I am the only recipient who built a relationship with Brad’s parents, even his grandparents. From that first meeting to this day, we attend significant family events and David did the eulogy for Brad’s grandmother. We always attend the annual golf outing in Brad’s honor, which raises funds for hockey scholarships at his former high school.”
25 Years Going Strong
It has been 25 years since Pam’s double-lung transplant. Transplantation has significantly evolved in the last quarter century, notes Lisa Allenspach, M.D. , medical director of Lung Transplant and Pam’s current physician. “When Pam had surgery, we did not know what life expectancy was, we did not have the data we have available to us today through international registries where all transplant recipient data is housed.” Two registries exist: Society of Heart and Lung Transplant for all solid organs and SRTR which is available to everyone. “Bilateral lung transplant survival at 25 years is certainly in the single digits,” Dr. Allenspach explains.
Dr. Allenspach attributes three factors that make a difference in a patient’s recovery and longevity, and Pam agrees that following doctor’s orders is important:
1. Physical activity pre- and post-transplantation is mandatory.
2. Support team post-transplantation to help physically and emotionally.
3. Positive attitude, feeling like the transplant will work and being flexible.
Meet the transplant team
Abdominal Transplant
Marwan S. Abouljoud, M.D.
Benson Ford Endowed Chair
Director, Henry Ford Transplant and Hepatobiliary Surgery
Mobile Phone: (313) 433-9026
Email: MABOULJ5@hfhs.org
Atsushi Yoshida, M.D.
Division Head, Transplant and Hepatobiliary Surgery; Director, Transplant Robot-assisted Surgery
Mobile Phone: (313) 657-6192
Email: AYOSHID1@hfhs.org
Dean Y. Kim, M.D.
Surgical Director, Kidney and Pancreas Transplant; Chief of Transplant Services, Children’s Hospital of Michigan
Mobile Phone: (313) 610-7817
Email: DKIM3@hfhs.org
Shunji Nagai, M.D.
Surgical Director, Liver Transplant, Surgical Director, Intestine Transplant and Rehabilitation; Director, Transplant Surgery Research Mobile Phone: (313) 461-9645
Email: SNAGAI1@hfhs.org
Ahmed Nassar, M.D.
Sr. Staff Transplant Surgeon Surgical Director, Pediatric Liver Transplant, Children’s Hospital Mobile Phone: (313) 549-5434
Email: ANASSAR4@hfhs.org
Jason E. Denny, M.D.
Surgical Director, Henry Ford Center for Living Donation
Mobile Phone: (313) 205-9346
Email: JDENNY1@hfhs.org
Lauren E. Malinzak, M.D.
Medical Director, Transplant Inpatient Unit Director, Transplant and Hepatobiliary Surgery Fellowship Mobile Phone: (248) 891-7272
Email: LMALINZ1@hfhs.org
Abbas A. Al-Kurd, M.D.
Sr. Staff Transplant Surgeon
Mobile Phone: (313) 461-3788
Email: AALKUR1@hfhs.org
Adhnan Mohamed, M.D. Sr. Staff Transplant Surgeon Mobile Phone: (313) 920-2181
Email: AMOHAME4 @hfhs.org
Transplant Hepatology
Kimberly A. Brown, M.D.
Associate Director, Henry Ford Transplant; Medical Director, Transplant Outreach
Mobile Phone: (734) 945-9206
Email: KBROWN1@hfhs.org
Dilip K. Moonka, M.D.
Medical Director, Liver Transplant
Mobile Phone: (248) 212-5447
Email: DMOONKA1@hfhs.org
Reena J. Salgia, M.D. Chief of Hepatology, Director, Liver Cancer Clinic
Mobile Phone: (313) 812-8899
Email: RSALGIA1@hfhs.org
Yakir Muszkat, M.D. Medical Director, Intestine Transplant and Rehabilitation
Mobile Phone: (313) 598-9331
Email: YMUSZKA1@hfhs.org
Stuart C. Gordon, M.D.
Director of Hepatology Research
Mobile Phone: (313) 282-3581
Email: SGORDON3@hfhs.org
Deepak Venkat, M.D.
Medical Director, Living Donor Liver Transplantation
Mobile Phone: (313) 695-0593
Email: DVENKAT1@hfhs.org
Syed-Mohammed R. Jafri, M.D.
Medical Director, Alcoholic Liver Disease Program
Mobile Phone: (313) 575-2293
Email: SJAFRI3@hfhs.org
Allyce N. Caines, M.D.
Sr. Staff Transplant Hepatologist
Mobile Phone: (313) 932-0702
Email: ACAINES1@hfhs.org
Humberto C. Gonzalez, M.D. Associate Director, Hepatology Research Medical Director, Liver Metabolic Clinic
Mobile Phone: (313) 205-0758
Email: HGONZAL1@hfhs.org
Amanda Su, M.D.
Sr. Staff Transplant Hepatologist
Mobile Phone: (313) 439-1958
Email: ASU1@hfhs.org
Kevin Harris, M.D. Sr. Staff Transplant Hepatologist
Alcohol-Related Liver Disease
Jessica Mellinger, M.D. Sr. Staff Physician Hepatologist
Mobile Phone: (313) 428-1536
Email: JMELLIN2@hfhs.org
Gerald Scott Winder, M.D. Sr. Staff Transplant Psychiatrist
Mobile Phone: (313) 859-1558
Email: GWINDER1@hfhs.org
Transplant Nephrology
Rohini Prashar, M.D. Medical Director, Kidney Transplant Program; Associate Director, Center for Living Donation
Mobile Phone: (313) 598-3912
Email: RPRASHA1@hfhs.org
Rehan Ansari, M.D. Medical Director, Living Kidney Donation
Mobile Phone: (313) 348-8159
Email: RANSARI2@hfhs.org
Anita K. Patel, M.D.
Sr. Staff Transplant Nephrologist
Mobile Phone: (248) 996-4661
Email: APATEL2@hfhs.org
Pritika Shrivastava, M.D.
Sr. Staff Transplant Nephrologist
Mobile Phone: (313) 953-7393
Email: PSHRIVA1@hfhs.org
Sherif Metwally, M.D. Medical Director, Pancreas Transplant program
Cardiothoracic Transplant
Hassan W. Nemeh, M.D.
Division Head, Cardiovascular Surgery; Surgical Director, Heart and Lung Transplant
Mobile Phone: (630) 886-9670
Email: HNEMEH1@hfhs.org
Dimitrios Apostolou, M.D.
Sr. Staff Cardiothoracic Transplant Surgeon
Mobile Phone: (313) 673-7305
Email: DAPOSTO1@hfhs.org
Kyle G. Miletic, M.D.
Sr. Staff Surgeon
Mobile Phone: (248) 417-9583
Email: KMILETI1@hfhs.org
Daizo Tanaka, M.D.
Sr. Staff Cardiothoracic Transplant Surgeon
Mobile Phone: (313) 461-2307
Email: DTANAKA1@hfhs.org
Adam Daly, M.D.
Sr. Staff Cardiothoracic Transplant Surgeon
Mobile Phone: (313) 900-5110
Email: ADALY2@hfhs.org
Advanced Heart
Failure/Heart Transplant & Mechanical Circulatory
Support
David E. Lanfear, M.D.
VP, Research Henry Ford Health; Chief Scientific Officer; Senior Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (248) 802-5312
Email: DLANFEA1@hfhs.org
Celeste T. Williams, M.D.
Medical Director, Cardiac Transplantation; Associate Director of Quality, Heart and Vascular
Mobile Phone: (248) 497-6869
Email: CWILLIA6@hfhs.org
Jennifer Cowger, M.D., M.S. Medical Director, Mechanical Circulatory Support; Section Head, Advanced Heart Failure & Cardiac Transplant
Mobile Phone: (734) 546-4911
Email: JCOWGER1@hfhs.org
Lindsey Aurora, M.D.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 920-9650
Email: LAURORA1@hfhs.org
Waleed K. Al-Darzi, M.D.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 932-3100
Email: WALDARZ1@hfhs.org
Gillian Grafton, D.O.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 671-0277
Email: GGRAFTO1@hfhs.org
Bashar Hannawi, M.D.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 461-2272
Email: BHANNAW1@hfhs.org
Alexander T. Michaels, M.D.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 932-5296
Email: AMICHAE2@hfhs.org
Yelena Selektor, M.D.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 848-7257
Email: YSELEKT1@hfhs.org
Cristina Tita, M.D.
Sr. Staff Advanced Heart Failure and Transplant Cardiologist
Mobile Phone: (313) 610-0339
Email: CTITA1@hfhs.org
Transplant Pulmonology
Lisa L. Allenspach, M.D.
Medical Director, Lung Transplant
Mobile Phone: (248) 310-9746
Email: LALLENS1@hfhs.org
Lisa D. Stagner, D.O.
Medical Director, Pulmonary Rehabilitation
Mobile Phone: (248) 765-3012
Email: LSTAGNE1@hfhs.org
Domingo J. Franco-Palacios, M.D. Sr. Staff Transplant Pulmonologist
Mobile Phone: (313) 623-6373
Email: DFRANCO1@hfhs.org
Kaitlin H. Olexsey, D.O. Sr. Staff Transplant Pulmonologist
Mobile Phone: (313) 587-6353
Email: KHANLON3@hfhs.org
Julio C. Pinto Corrales, M.D. Sr. Staff Transplant Pulmonologist
Mobile Phone: (313) 515-9778
Email: JPINTO1@hfhs.org
Alaa Abu Sayf, M.D.
Sr. Staff Transplant Pulmonologist
Mobile Phone: (313) 850-2720
Email: AABUSEY1@hfhs.org
To refer a patient, please call:
Liver: (313) 916-8865
Kidney and Pancreas: (313) 916-1269
Heart: (313) 916-2895
Intestine and Multivisceral: (313) 916-8865
Lung: (313) 916-1471
Transplant oncology expands criteria for transplantation
The field of transplant oncology is relatively new, evolving on a national level and here in Michigan. As the topic was being discussed at national conferences, a Henry Ford Hospital multidisciplinary work group began in 2021 to consider expanding its offerings beyond patients who have end stage liver disease or traditional hepatocellular carcinoma (HCC), which are the traditional indications for liver transplant.
Shunji Nagai, M.D. , surgical director Liver Transplant, surgical director Intestine Transplant Surgery says, “the concept of transplant oncology is applied in the field of the liver, intestine and multi visceral.” Dr. Nagai leads transplant oncology surgery and Reena Salgia, M.D. is the director of the Liver Cancer Clinic and Medical Transplant Oncology.
A National Transplant Oncology Review board was created in 2025 and OPTN and UNOS changed their governing practice on donor organ use and transplant criteria in February. As a result, “some patients in the transplant oncology space may now be able to receive priority recognition and allocation for organs,” explained Dr. Salgia. “Previously, these individuals either had to have a living donor available to them or they were not candidates for transplant.” Dr. Salgia adds, “we have moved liver transplantation into the space of offering it for patients who may have previously fallen outside of established criteria.”
About 15% of liver transplant is for patients with HCC, which is the primary liver cancer, it usually develops in cirrhotic livers. Expansion of inclusion criteria for liver transplantation means, “patients with bile duct cancer like cholangiocarcinoma, those who have may have liver metastasis from colorectal cancer, patients with a neuroendocrine tumor that has metastasized to the liver may be candidates for liver transplant,” explains Dr. Nagai. This has broadened the prior scope of acceptance for patients with HCC, the most common type of primary liver cancer.



Dr. Nagai explains, “If the disease is stable for certain period of time, usually 6 to 12 months and the cancer is only in the liver, a liver transplant can be considered.” He notes, “the data suggests that liver transplant can improve their survival quite a bit compared to chemotherapy or radiation therapy. In addition, intestine transplant may be considered for patients with unresectable mesenteric tumor. “
Multivisceral transplant, meaning transplanting the liver, pancreas, and intestine at one time, can be considered for those with an unresectable neuroendocrine tumor in the abdominal organs, including the intestine, pancreas, and liver. Cancer treatment with organ transplant, is the concept of transplant oncology,” Dr. Nagai explains. “Patient selection is very important. However, as long as the patient meets the criteria, we could offer liver, intestine, and multivisceral transplant as one of the treatment options.” Henry Ford’s multidisciplinary team involved in patient selection also includes the hepatobiliary surgery team, our Henry Ford nursing liaisons and from the Henry Ford Cancer Institute, Maria Diab, M.D. , medical oncology and hematology and Parag Parikh, M.D. , radiation oncology.
“We are here as a resource for our community of physicians,” explains Dr. Salgia. “Rather than waiting until the patient becomes very sick, we want to evaluate the patient with cirrhosis in the early phase, before the patient becomes sicker or ends up in ICU. Our team streamlines care and provides multidisciplinary treatment to improve the outcomes with transplant.” Henry Ford Health is a leader in liver transplantation. Physicians are encouraged to reach out to Dr. Salgia, Dr. Nagai or any member of the Transplant Oncology team with questions or to inquire about their patients’ potential eligibility for transplantation. The team can be reached by calling (313) 916-2941.
Study Evaluates GLP-1 RA Use in Kidney
and Liver Transplant Recipients
Common among solid organ transplant recipients is diabetes mellitus (DM) and obesity, which are associated with an increased risk of graft failure. To understand the effectiveness of glucagon peptide-1 receptor agonists (GLP-1 RAs) for managing both conditions in the general population, a retrospective study conducted by Henry Ford Hospital transplant hepatologists and transplant pharmacists was published in the Journal of Pharmacy Practice and Research. It provides new data on the safety and efficacy of GLP-1 RAs in kidney and liver transplant recipients, a population often excluded from major clinical trials. This study addressed an existing knowledge gap regarding GLP-1 RA use, particularly concerning early initiation post-transplant.
Conducted at Henry Ford Health Transplant in Detroit, this retrospective matched-cohort study included 74 adult patients who had received a kidney or liver transplant. The treatment cohort consisted of 37 patients who for at least three months received a GLP-1 RA (semaglutide, dulaglutide, or liraglutide) and were matched to a control cohort of 37 recipients not receiving a GLP-1 RA. Matching was based on organ type and a diagnosis of type 2 diabetes mellitus (T2DM) at the time of transplant. Key exclusion criteria included thoracic or pancreas transplants, concurrent SGLT2i use, and pre-transplant GLP-1 RA initiation. There was no statistically significant difference in the number of patients on insulin at the baseline between the cohorts.
The study investigators reported the primary outcome was the change in median HbA1c at six months post-initiation. Secondary outcomes included changes in weight, BMI, total daily insulin requirements, number of oral diabetic agents at six months did not change in the GLP-1 RA group but increased in the no GLP-1 RA group. There was a statistically significant change in the GLP-1 RA group and no change in the eGFR between the groups.
Of the 18 patients who experienced adverse events related to initiation of the GLP-1 drug, most commonly reported were nausea, diarrhea, and abdominal pain. Of the 37 patients in the GLP-1 RA cohort, with the incidence of documented hypoglycemia, 4 and ultimately 9 patients discontinued the medicine. Nine patients that discontinued the medicine, due to an adverse event or cost, switching to alternative medication due to availability or patient preference. There was no graft loss or patient death during follow up.
Table 1 indicates an evaluation of hemoglobin A1c and weight management outcomes between cohorts.
Discussion and Implications for Future Research
The study investigators reported that significant reductions in body weight and BMI with moderate reductions in HbA1c and overall daily insulin requirements were observed. Although our study did not find a statistically significant reduction in HbA1c compared to previously published literature, our study observed a similar HbA1c reduction of 0.5% and more patients in the GLP-1 RA cohort achieving HbA1c <7%. Although a very small patient population, the lack of significant reduction of HbA1c in our study deserves an explanation and raises a conundrum.
The main take away is that GLP1 in transplant is safe and effective, but not always accessible to patients due to cost, insurance ever changing rules and hesitation to use this type of agents on a recently transplanted individual. This study provides the basis for larger prospective studies that can highlight benefits of this type of medicines.
Importantly, the findings suggest that GLP-1 RAs are a seemingly safe and effective option for managing weight and BMI in kidney and liver transplant recipients, with a modest effect on glycemic control. These findings held true even when therapy was initiated early post-transplant, with similar discontinuation rates as previously reported in the literature. The study investigators note that underscores the critical need for larger, prospective, randomized controlled trials. Future research should aim to confirm these findings and evaluate the long-term impact of GLP-1 RAs on cardiovascular and renal outcomes in the solid organ transplant population, as well as to identify the optimal timing for initiating therapy.
To read the full study:
https://doi.org/10.1002/jppr.1953
Henry Ford Transplant outreach clinics
There are Henry Ford Transplant outreach clinics throughout Michigan, plus virtual consultations and visits are available.
Transplant Clinics
Henry Ford Hospital 2799 West Grand Blvd. Detroit, MI 48202
Heart Transplant
Henry Ford Advanced Heart Failure Clinic – Bloomfield Township
Henry Ford Medical Center 1961 S. Telegraph Road Bloomfield Township, MI 48032
Henry Ford Advanced Heart Failure Clinic – Brownstown
Henry Ford Medical Center – Brownstown 23050 West Road Brownstown, MI 48138
Henry Ford Advanced Heart Failure Clinic – Clinton Township
Henry Ford Macomb Hospital 5855 19 Mile Road Clinton Township, MI 48038
Henry Ford Advanced Heart Failure Clinic – Dearborn
Henry Ford Medical Center - Fairlane 19401 Hubbard Dr Dearborn, MI 48126
Henry Ford Advanced Heart Failure Clinic – Jackson 1100 E. Michigan Avenue, Suite 100 Jackson, MI 49201
Henry Ford Advanced Heart Failure Clinic – Royal Oak
Ernst Cardiovascular Center Beaumont Hospital 3601 W. 13 Mile Road Royal Oak, MI 48073
Henry Ford Advanced Heart Failure Clinic – Saginaw
Henry Ford Specialty Center 5375 Hampton Pl Saginaw, MI 48064
Henry Ford Advanced Heart Failure Clinic – Sterling Heights
Henry Ford Medical Center 3500 15 Mile Rd. Sterling Heights, MI 48310
Henry Ford Advanced Heart Failure Clinic – Southfield
Henry Ford Providence Southfield Hospital 22250 Providence Dr., Suite 705 Southfield, MI 48075
Henry Ford Advanced Heart Failure Clinic – West Bloomfield
Henry Ford West Bloomfield Hospital 6777 W. Maple Road West Bloomfield, MI 48322
Henry Ford Advanced Heart Failure Clinic – Wyandotte
Henry Ford Wyandotte Hospital 2333 Biddle Road Wyandotte, MI 48192
Henry Ford Advanced Heart Failure Clinic – Henry Ford St. John Hospital
Henry Ford St. John Hospital 22201 Moross Road, Suite 356 Detroit, MI 48236
Liver, Small Bowel, and Multivisceral Transplant
Henry Ford Liver, Small Bowel and Multivisceral Transplant Clinic – Bloomfield Township
Henry Ford Medical Center 1961 S. Telegraph Road Bloomfield Township, MI 48302
Henry Ford Liver Transplant Clinic –Columbus
Henry Ford Medical Center 39450 W. 12 Mile Road Novi, MI 48377
Henry Ford Liver Transplant Clinic –East Lansing
Michigan Gastroenterology Institute 1650 Ramblewood Dr. East Lansing, MI 48223
Henry Ford Liver Transplant Clinic – Flint 1125 Linden Rd., Suite 300 Flint, MI 48532
Henry Ford Liver Transplant Clinic – Fraser 15717 15 Mile Road Clinton Twp., MI 48035
Henry Ford Liver Transplant Clinic –Grand Blanc
8275 Holly Rd., Suite 2 Grand Blanc, MI 48439
Henry Ford Liver Transplant Clinic –Grand Rapids
1000 East Paris Ave. SE, Suite 214 Grand Rapids, MI 49546
Henry Ford Liver Transplant Clinic –Grayling
1200 W. North Down River Rd. Grayling, MI 49738
Henry Ford Liver Transplant Clinic –Jackson
Henry Ford Jackson Hospital 744 East Michigan Ave., Suite 301 Jackson, MI 49201
Henry Ford Liver Transplant Clinic –
Michigan State University
Michigan State University Clinic 4660 S. Hagedorn Road, Suite 600 East Lansing, MI 48823
Henry Ford Liver Transplant Clinic –Muskegon 1675 Leahy, Suite 324B Muskegon, MI 49442
Henry Ford Liver Transplant Clinic –Saginaw
Henry Ford Specialty Center 5375 Hampton Pl. Saginaw, MI 48064
Lung Transplant
Henry Ford Lung Transplant Clinic – Bloomfield Township
Henry Ford Medical Center
1961 S. Telegraph Road Bloomfield Township, MI 48032
Henry Ford Lung Transplant Clinic –Columbus
Henry Ford Medical Center 39450 W. 12 Mile Road Novi, MI 48377
Henry Ford Lung Transplant Clinic –Grand Blanc
8220 S. Saginaw St., Suite 800 Grand Blanc, MI 48439
Henry Ford Lung Transplant Clinic –Grayling
1200 W. North Down River Road Grayling, MI 49738
Henry Ford Lung Transplant Clinic –Hurley Hospital
1125 S. Linden Rd., Suite 300 Flint, MI 48532
Henry Ford Lung Transplant Clinic –Jackson
900 E. Michigan Ave., Suite 105 Jackson, MI 49201
Henry Ford Lung Transplant Clinic –Michigan State University
Michigan State University Clinic 4660 S. Hagedorn Road, Suite 405 East Lansing, MI 48823
Henry Ford Lung Transplant Clinic –Saginaw
Henry Ford Specialty Center 5375 Hampton Pl Saginaw, MI 48064
Henry Ford Lung Transplant Clinic –Sterling Heights
Henry Ford Medical Center 3500 15 Mile Rd. Sterling Heights, MI 48310
Kidney and Pancreas Transplant
Henry Ford Kidney and Pancreas Transplant Clinic – Bloomfield Township
Henry Ford Medical Center
1961 S. Telegraph Road Bloomfield Township, MI 48032
Henry Ford Kidney and Pancreas Transplant Clinic – Flint
G3404 Miller Road Flint, MI 48507
Henry Ford Kidney and Pancreas Transplant Clinic – Hurley Hospital 1125 S. Linden Rd, Suite 300 Flint, MI 48532
Henry Ford Kidney and Pancreas Transplant Clinic – Jackson 744 W. Michigan Ave., Suite 301A Jackson, MI 49201
Henry Ford Kidney and Pancreas Transplant Clinic – Michigan State University
Michigan State University Clinic 4660 S. Hagedorn Road, Suite 405 East Lansing, MI 48823
Henry Ford Kidney and Pancreas Transplant Clinic – Pontiac
Michigan Kidney Consultants, P.C. 44200 Woodward Ave., Suite 2109 Pontiac, MI 48341
Henry Ford Kidney and Pancreas Transplant Clinic – Saginaw
Henry Ford Specialty Center
5375 Hampton Pl Saginaw, MI 48064
Michigan’s Transplant Outreach Clinics expand locations
Henry Ford Transplant is Michigan’s most advanced transplant program. It continues to expand its network state-wide to provide pre- and post-transplant care to reach patients who would not have access to transplant services otherwise.
The current Henry Ford Transplant Outreach Clinics are established by organ, explained Kimberly Brown, M.D., director of Outreach Clinics and transplant hematologist. “Our specialists travel to the patients because data indicates those who live in areas furthest from transplant centers are more likely not to receive treatment from a specialist.”
A mixed delivery model includes virtual visits when possible. Dr. Brown explains that “through virtual visits our specialists can deliver quality care to our patients, and patients appreciate less travel and show up to their virtual visits.”
The opportunity to develop partnerships with local health care providers for their services is a bonus. “As we developed our network of Transplant Outpatient Clinics, this was an important consideration to help patients receive diagnostic testing close to home,” explains Dr. Brown.
To schedule your patient for a transplant consultation, contact one of the Transplant Outreach Coordinators or call 1-855-85-TRANSPLANT.
Henry Ford Kidney and Pancreas Transplant Clinic –West Branch 648 Progress St., Suite 101 West Branch, MI 48661
Henry Ford Kidney and Pancreas Transplant Clinic – Ypsilanti 5333 McAuley Drive Reichert Building, Suite 403 Ypsilanti, MI 48197
= Coming early 2026
TEAM Heart Failure Trial: LVAD therapy earlier
The TEAM Heart Failure Trial is a novel trial examining LVAD therapy in the less sick and is one of three programs (Cleveland Clinic and MUSC) serving as study leads through National PI representation. The work Henry Ford’s Gillian Grafton, D.O., did with heart failure and CardioMEMS™ Heart Failure System to identify how pulmonary HTN is a risk factor for adverse outcome in heart failure support this effort. In this trial, CardioMEMS™ will be used to identify high risk patients who may benefit from earlier LVAD.
The excellent outcomes achieved by our surgeons and medical practitioners (including doctors, nurses, APPs, PT, OT, psychology, etc.) is on the map nationally and played a large part in our clinical selection.
Jennifer Cowger, M.D., section head of Advanced Heart Failure, Transplant, and Mechanical Circulatory Support says , “currently, LVADs are only approved for patients who are very ill—in cardiogenic shock in the ICU or requiring inotropes to support their heart. We recognize there are patients with heart failure who have a high risk of death within two years despite being treated as an outpatient. Since LVAD survival has greatly improved over the last decade, we want to see if we improve longterm survival for a subset of patients with heart failure by putting in LVAD before they become critically ill.”
The success of this trial will expand the patient candidacy for LVAD and increase LVAD volumes at Henry Ford and will also impact these numbers nationally.
This team will use all their resources to advance the care they can offer to patients today and tomorrow. They bring hope to patients who otherwise might not receive the best care. As Dr. Cowger shares, “our Advanced Heart Failure Program is very special. The talent is fierce. The dedication unwavering. Every team member shines bright. They have worked so hard to get to this point and deserve this recognition.”
The surgical PI: Hassan Nemeh, M.D.
The surgical PI: Kyle Miletic, M.D.
The medical PI: Lindsey Aurora, M.D.
National PI: Jennifer Cowger, M.D.

First patients receive BrioVAD™ LVAD at Henry Ford
The Advanced Heart Failure team, including Hassan Nemeh, M.D., chief of cardiac surgery, implanted four of only a few patients across the United States with the BrioVAD™ system, a left ventricular assist system (LVAS). Henry Ford is one of only eight centers in the United States to take part in the INNOVATE Trial, making the FDA-approved BrioVAD™ heart pump available. It is anticipated that 2-3 additional patients will soon receive the heart pump.
This device represents a significant advancement in the establishment of technologies available to address advanced heart failure. A novel small MagLev pump with a large diameter rotor and long blades is designed to create a low turbulence blood flow path, which minimizes blood damage while optimizing patient fit. This new pump is under trial for permanent heart support for patients with endstage heart failure or recalcitrant cardiogenic shock. This trial is important as it provides another option to only one other FDA-approved device.

The surgical PI: Hassan Nemeh, M.D.
The surgical PI: Daizo Tanaka, M.D.
The site PI: Gillian Grafton, D.O.
National Leadership Panel: Jennifer Cowger, M.D.
Study analyzes use of living kidney DONOR app
Living-donor kidney transplantation offers patients a chance to receive an organ sooner, with longer graft survival and in a more elective setting compared to a deceased-donor kidney transplant. Living donation is associated with improved survival, reduced expenses, and enhanced quality of life for patients with end stage renal disease as compared to deceased donor kidney transplantation.


However, studies have shown there are barriers to living-donor kidney transplantation. Rohini Prashar, M.D. , medical director, Kidney Transplant Program and associate director, Center for Living donation explains, “candidates are hesitant to discuss their illness and to start a conversation about living donation which creates a barrier to finding a living donor.” Previously, studies where interventions that ranged from educational programs to living donation champion programs, indicated the goal of increasing living-donor kidney transplant was not achieved. “These activities are time intensive, and the candidates are uncomfortable asking directly for a donation, making these interventions less effective,” Dr. Prashar adds.
To address these barriers, Johns Hopkins University developed an application that allowed candidates to share their need for a living donor through a collaboration with Meta (Facebook). Transplant candidates who used the DONOR app had six times more inquiries, however it was not clear if these inquires translated into actual transplants in the duration of the study.
Dr. Prashar explains, “we reported prospective single-center experience of the use of DONOR app in 51 adult kidney-only transplant candidates on the Henry Ford Hospital wait list between April 2021 and December 2022.”
living donor inquires that can potentially lead to living-donor kidney transplants.”
In this study conducted at Henry Ford Transplant, compared with matched waitlisted controls, the candidates using the DONOR app were 8.7 times more likely to have a potential living donor come forward on their behalf. Despite having no potential of a living-donor at the time of enrollment, 93 (3.6 per patient), potential living donor inquiries were received on behalf of 26 candidates with 2 receiving living-donor kidney transplant and 1 directed-deceased donation.
“Use of the DONOR app could overcome challenges in obtaining a living-donor, with a less burdensome, time-intensive approach,” says Dr. Denny.
Due to the higher prevalence of End Stage Renal Disease (ESRD) in African Americans, compared to other racial groups, a sub analysis in the African American participants was conducted. This group was more likely to be single/divorced (60% vs. 29%; p = 0.03), have lower median household income ($33,000 [IQR: $32,000–$57,000] vs. $59,000 [IQR: $49,000–$71,000; p = 0.001], a higher ADI at the state (9 [IQR: 3–10] vs. 5 [IQR: 2–8] decile; p = 0.007), and national level (92 [IQR:51–99] vs. 65 [IQR: 38–86] percentile; p = 0.006). The total number of views/ shares from the posts and potential living-donor inquiries were similar between African Americans and the rest of the cohort.
This study confirms that education alone to overcome barriers to living kidney donor transplant is resource intensive and may not appeal to all candidates. In this study, the DONOR app was found to be an easy and affordable method by utilizing the abundance of social media platforms to not just increase living-donor inquiries and interest but also to progress to actual living-donor kidney transplantation.

Inclusion criteria included candidates who had no potential living donor at the time of enrollment. A requirement of inclusion was access to internet or social media and a smartphone. Dr. Prashar further explains, “a 1:3 iterative matching was used to identify matched controls while adjusting for the following variables: age, sex, race, blood type, time on waitlist, and panel-reactive antibody.
Jason Denny, M.D. , director, Center for Living Donation and surgical director, Living Kidney Transplantation, Henry Ford Health explains, “the objective of this study was to understand the positive impact use of the DONOR app has on potential
The DONOR app was implemented with current staff at Henry Ford Transplant and did not require any additional hiring or funding sources. Dr. Denny encourages, “transplant providers and centers to consider the use of this toolkit to support patients to find a living kidney donor and reduce disparity in access to the life-saving gift of organ transplantation.”
Dr. Denny concludes, “we learned from this study that posting the living-donor candidate’s story on social media using the DONOR app increases living-donation which leads to improved survival, reduced expenses, and enhanced the quality of life for patients with end stage kidney disease as compared to deceased donor kidney transplantation.” He adds, “there’s no doubt that encouraging the widespread implementation of the DONOR app leads to tremendous gains for the recipient and the economy. It is a win all the way around.”
To read the entire study: https://doi.org/10.1111/ctr.70118
Phone: (313) 916-2941
Fax: (313) 916-4353
Email: MABOULJ5@hfhs.org
Web: henryford.com/ transplant

Michelle “Cookie” Crossley, R.N., B.S.N.
Mobile Phone: (248) 219-2326
Email: MCROSSL1@hfhs.org Christina Somers R.N., B.S.N. Mobile Phone: (313) 622-4352 Email: CSOMERS1@hfhs.org
https://issuu.com/hfhealth


Katie Dandron, R.N.
Mobile Phone: (313) 353-3990
Email: KDANDRO1@hfhs.org