DENTAL SOLUTIONS



Through this program, Henry Schein will offer environmentally friendly products, services, and support to help dental professionals deliver high-quality care while reducing their environmental impact, as well as making improvements to all parts of the supply chain to reduce the environmental impact.
“At Henry Schein New Zealand, we are committed to environmental sustainability, and we understand that the collective actions we take today, play an important part in shaping the future of the planet and generations yet to come,” said Mike Engle, Managing Director Henry Schein New Zealand. “That is why we are delighted to announce the launch of Practice Green in New Zealand as a further extension of our commitment to promote responsible business practices in our own operations. We believe that businesses have a significant role in helping to drive positive environmental change in New Zealand.
In addition to our activities within the company, Practice Green reflects our commitment to aiding our customers through their sustainability journey.

As part of our company’s activities around Practice Green, Henry Schein New Zealand is also excited to announce our partnership with Toitū Envirocare and the recent achievement of the Toitū enviromark® bronze certification.
The Toitū enviromark programme ensures organisations are meaningfully managing their environmental impacts through a mentoring approach.
Through the programme, organisations develop, implement and maintain a robust Environmental Management System (EMS).
The EMS is independently audited annually to ensure it meets stringent requirements of continual improvement, applicable regulations and international standards.
We are dedicated to making a meaningful difference, while helping to create a more sustainable future for all.”
Henry Schein New Zealand is committed to co-creating a circular and carbon-neutral supply chain in collaboration with its supplier partners and customers.
The products that will be available through Practice Green have been carefully selected based on information provided by the supplier partner on their eco-friendly qualities, such as being reusable, made from recycled materials, biodegradable, or from sustainable sources.
The Practice Green program will continue to expand over time, with new solutions added to its portfolio as the healthcare landscape evolves.
As healthcare has a significant impact on the environment, Henry Schein believes that taking action now will help protect the planet and its natural resources, while building a healthier New Zealand and World for all.
As a Toitū enviromark bronze certified organisation we have thought about which activities our EMS must control across our site at Bush Road, Rosedale along with meeting all applicable health, safety and environmental legislation for the areas of our organisation covered by the EMS.
The team at Henry Schein New Zealand are very excited about the next steps in our environmental sustainability journey. Working alongside Toitū Envirocare we will continue to drive improvement and environmental change across our business activities.
The Henry Schein New Zealand Team









The Curing Light re-imagined. Ultradent introduces the most innovative curing light available in the world.


A sealer that can be used with any obturation method. It has a smooth consistency when mixed and is specifically designed to be delivered through the Ultradent NaviTip™ 29 ga Single Sideport tip for precise placement. This decreases risk of extrusion outside the root canal system & saves clinicians time & cost.
The Lunos® brand from DÜRR DENTAL represents a portfolio of matching products, all combined in a single system. This means the Lunos® range offers devices, consumables, and accessories for almost all steps of prophylaxis treatment.


The new environmentally friendly floss option made of natural silk and packed in a cardboard box. Tightly rolled coil with no additional plastic core.

Upgrade to a professional flossing experience with Colgate Blast Water Flosser Series 2. Blast away plaque in-between your teeth and along the gum line, to improve gum health. Choose from 5 cleaning modes and 3 nozzle heads for a unique flossing experience tailored to you.
New Plan B MiniKUT Gutta-Percha Points. Infused with Bioceramic particles, miniKUT Gutta-Percha Points offer ideal integration with any sealer formula while providing high radio-opacity. Laser inspected for Tip and Taper accuracy. Available in 2 tapers (.03, .05) and 7 tip sizes (15, 20, 25, 30, 35, 40, 45). MiniKUT GuttaPercha is colour coded according to ISO tip sizes. Pre-Sterilized in packs of 60.


EdgeOne-R Utopia is our newest and most advanced single file reverse reciprocating motion system. EdgeOne-R Utopia is an alternative to reciprocating and gold instruments. It features our FireWire Gold HeatTreatment making it efficient, safe, and flexible. Plus we added our new ultra secure, ULTRA-FIT shank and all EdgeUtopia files are provided in presterilized blister packs.




Sterile carbon steel scalpel blades packed in individual foil packs. Computer controlled grinding ensures a consistently sharp edge.

capsules is a strong, permanent solution for all generations. The material

EQUIA Forte® HT is a versatile and durable restorative solution, ideal for patients of all ages, including paediatric, geriatric and high-risk caries patients. With enhanced mechanical properties, sound marginal seal and excellent handling, EQUIA Forte® HT with





your restoration.1
The strength and handling are further improved in EQUIA Forte® HT by developing an intelligent control of distribution and interaction of these glass particles. Also, EQUIA Forte® Coat is now available in an ergonomic flip-top bottle that minimises waste. The result? A strong restorative with prolonged working time and superb handling that is excellent for bulk-fill placement, even in load-bearing Class II restorations.2
EQUIA Forte HT has been designed to make your daily restorative work as easy and efficient as possible. Since rubber dam placement and adhesive application are not required, the restoration can be finished quickly. It is a material that is easy to use, yet the longevity is not compromised.1
By reducing the number of components, this capsule uses about 25% less plastic than typical products. It is used in our flagship product EQUIA Forte HT and other products.

EQUIA Forte® HT capsule packaging has less total mass than the other products tested while wasting the least amount of packaging per gram of usable restorative, making it the most efficient packaging design.3





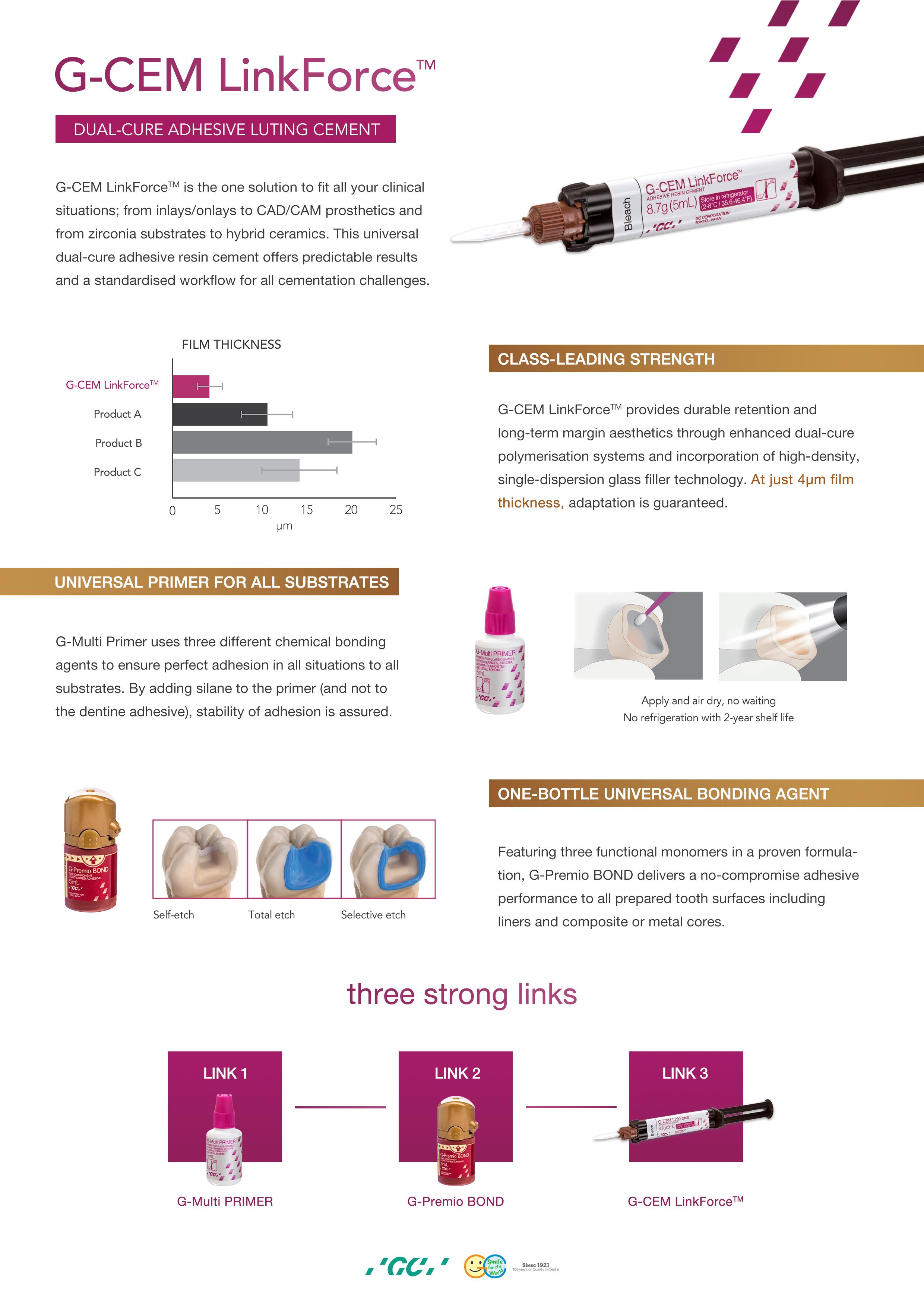
G-CEM LinkForce is the one solution to fit all your clinical situations; from inlays/onlays to CAD/CAM prosthetics and from zircona substrates to hybrid ceramics.
This universal dual-cure adhesive resin cement offers predictable results and a standardised workflow for all cementation challenges.


G-CEM Linkforce provides durable retention and longterm margin aesthetics though enhanced dual-cure polymerisation systems and incorporation of highdensity, single-dispersion glass filler technology.
At just 4µm film thickness adaptation is guaranteed.
G-Multi Primer uses three different chemical bonding agents to ensure perfect adhesion in all situations to all substrates. By adding silane to the primer (and not to the dentine adhesive), stability of adhesion is assured.

Featuring three functional monomers in a proven formulation. G-Premio BOND delivers a no-compromise adhesive performance to all prepared tooth surfaces including liners and composite or metal cores.







A stable ASA 2 65 year old female presented to the practice for restorative dentistry with a medical history significant for a non-descript immunoglobulin deficiency, for which she receives regular infusions. She reports no known drug allergies. Clinically, she was diagnosed with an occlusal peripheral rim fracture leaving a food trap on tooth 14 (FDI notation). Tooth 15 featured an extensive amalgam with extreme proximity to the distal marginal ridge, which exhibited distal vertical axial fractures as a result of cyclic expansion-contraction over time. The restorative goal of minimally invasive direct dentistry would be complicated by the undoubtedly dark dentin substrate under the amalgam. A material was sought that featured both an excellent chameleon mechanism as well as physical properties to maximize the prognosis of direct restorations in this area.
The patient was subjected to topical anaesthetic prior to buccal infiltration using 1 carpule of 2% Lignocaine with 1:100,000 epinephrine. A rubber dam was affixed prior to preparation of tooth 15MO with dissection of the distal vertical marginal ridge fracture. The margins of tooth 14O and 15MOD were refined before bevelling as the ends of enamel rods facilitate better bonding relative to the sides of enamel rods. A 27 micron aluminium oxide micro air abrasion treatment was completed prior to affixing, wedge and matrix to reconstruct the mesial marginal ridge of tooth 15. A matrix-in-matrix solution was used to recreate the proximoaxial contour of 15D This provided hermetic closure at the proximogingival cavosurface margin as well as an ideal contour for the missing axial wall.
Following a total etch technique, a 2% Chlorhexidine scrub was completed for 30 seconds and the dentin blot dried to a moist state. A 5th generation bond was applied, air thinned and cured as per manufacturer instructions. Microlayers are important during the delicate first 5 minutes of hybrid layer formation, and were completed using 0.25mm increments of CLEARFIL MAJESTY™ Flow (Kuraray Noritake Dental Inc.). This technique can be expected to increase significantly the shear bond strength to dentin (1, 2). This was completed both in the proximal box floor area as well as mid-occlusally. The marginal ridge was completed using CLEARFIL MAJESTY™ ES-2 Universal (Kuraray Noritake Dental Inc.).
Since the dentin base was heavily stained, CLEARFIL MAJESTY™ Flow was used before utilizing CLEARFIL MAJESTY™ ES-2 Universal in a lobe-by-lobe creation of occlusal anatomy.
Post-operative occlusal checks verify that the restoration is conformative to occlusion and esthetically excellent with no visible marginal show.
The marginal ridges were microlayered horizontally as was the floor of the resulting Class I preparation as per a reduced layer thickness-technique modification of Nikolaenko et al (3), whereas the highest shear bond strengths were found when a 1mm horizontal layering technique was used.
CLEARFIL MAJESTY™ ES-2 Universal is at the forefront of a simplified restorative armamentarium for the modern practice.
It takes cloud-shading one step further by offering a “Universal” shaded composite featuring Light Diffusion Technology (LDT) with simultaneous ideal sculptability, optical metamerism and physical properties for use in any restorative situation in the mouth. Featuring barium glass nano fillers and proprietary pre-polymerized nanoparticle fillers, the latter boasts a high refractive matrix that is able to disperse light and fool the eye with even the thinnest of layers, obviating the need for opaquer composites in cases like the one featured.
When paired with CLEARFIL MAJESTY™ Flow in a conservative layered technique, the 81% filled flowable produces a radiographically well-demarcated layer, and the superficial CLEARFIL MAJESTY™ ES-2 Universal boasts an easy-to-polish robust single shade restorative solution that will virtually fulfil all of your restorative needs for non-bleaching patients. Physically, with compressive strength is rated at 348MPa and flexural strength at 116MPa, CLEARFIL MAJESTY™ ES-2 Universal is in the range of natural enamel and dentin. The built-in fluorescence is very enamelomimetic, which is excellent for nightclub social situations.
1. Bertschinger C, Paul SJ, Luthy H, Scharer P. Dual application of dentin bonding agents: effect on bond strength. Am J Dent. 1996;9(3):115-119
2. Magne P, Kim TH, Cassione D, Donovan TE. Immediate dentin sealing improves bond strengths of indirect restorations. J Prosthet Dent. 2005;94(6):511-519




3. Nikolaenko SA, Lohbauer U, Roggendorf M, Petschelt A, Dasch W, Franenberberger R. Influence of C-Factor and layering technique on microtensile bond strength to dentin. Dental Mater. 2004;20(6):579-585
Dr Clarence Tam is originally from Toronto, Canada, where she completed her Doctor of Dental Surgery and General Practice Residency at the University of Western Ontario and the University of Toronto, respectively. Clarence’s practice is limited to cosmetic and restorative dentistry and she is well-published to both the local and international dental press, writing articles, reviewing and developing prototype products and techniques in clinical dentistry. She frequently and continually lectures internationally. Clarence is the Past Chairperson and Director of the New Zealand Academy of Cosmetic Dentistry. She is currently one of two individuals in Australasia to hold BoardCertified Accredited Member Status with the American Academy of Cosmetic Dentistry. Clarence is an Opinion Leader for multinational dental companies Kuraray Noritake Dental Inc., J Morita Corp., Henry Schein NZ, Ivoclar Vivadent, Dentsply Sirona, 3M, Kerr, GC Australasia, SDI and Coltene and is the only Voco Fellow in Australia and New Zealand. She holds Fellowship status with the International Academy for DentoFacial Esthetics and is a passionate and approachable individual, committed to having an interactive approach with patients in all of her cases to maximize predictability.

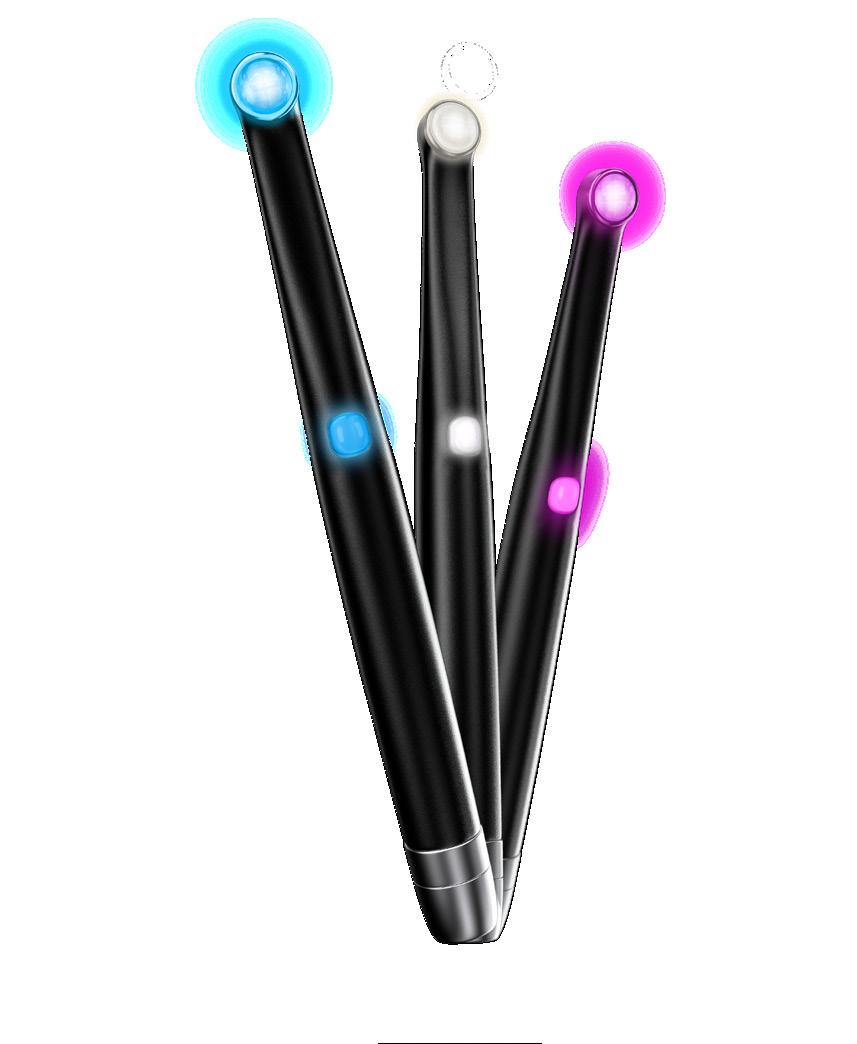
As curing light technology improves, dentists are consistently sold on irradiance (mw per cm2) as being the defining factor in beam effectiveness. While there is no doubt irradiance adds value, it does not tell the full story of how well a light will cure various materials.
Irradiance tests typically only show the irradiance of a very small portion of the light. Measuring the power distributed over the entire beam tells a more comprehensive story of its curing capabilities.
When comparing irradiance and power, think of power as the overall amount of light being put out and irrandiance as how much light is put out over a certain area.
Compare, if you will, polymerizing a restoration to lighting a room.
There’s a bulb in the center of the ceiling, and you’re standing below with a funnel. You can cover the bulb with the funnel shaped reflector and direct all the light into one small, bright spot, with most of the room remaining dark. Or you can let the bulb’s brightness cover the room evenly and be able to see everything.
“Dentists need to stop looking only for the irradiance value, and instead, look for power value as well as a good irradiance value,” says Ultradent VP of Research and Development, Neil Jessop.
“Irradiance isn’t the only metric dentists should be looking for—they should be looking for power evenly distributed over the entire surface of the tooth.”
A beam with a small, superhot center will unevenly cure a composite. A beam with uniformly dispersed power throughout provides a superior, more predictable cure. Equally distributed power allows a dentist to center the light over a tooth and fully cure the entire restoration without creating hotspots and leaving areas under-cured.
Many of the misconceptions built around irradiance stem from how it’s historically been measured. Traditional light meters, which remain the most common found in dental offices, aren’t giving dentists an accurate assessment of their curing light’s capabilities.
“Most meters that are available in the world measure the
center of the light,” Jessop says. “[Measuring devices] sample a very small part of the beam and you may be on a particular hot spot and not realize that it’s just measuring how dense the light is, or how much light is sitting in that particular spot.”
By measuring the center hotspot only, these meters ignore significant amounts—if not the majority of—the actual lens/footprint of the light. The hotspot will have a curing ability slightly wider than the hotspot itself, but the overall target can be missed.
Distributing power evenly over a larger area ensures a more consistent, quality cure compared to lights with small hotspots.
The new VALO™ X curing light is equipped with one-button activation, as well as an accelerometer, so users can cycle between the light’s power and diagnostic modes with just the wave of the wand, a light drum tap, or the push of a button.

Jessop says he frequently sees ambiguous - if not disingenuous - marketing materials given to dentists.
“The way these companies are misleading customers is that they’re measuring the hotspot of their light, which may have a very high irradiance, but which covers a very small area, compared to VALO™ X [light] which has twice the power evenly distributed over a much larger area.”
Ultradent’s research and development team created a meter to help dentists measure a light’s power and irradiance more accurately.
“The only way you can accurately measure a curing light is with a meter that takes into the account the entire area of the light with a window that’s bigger than the light, which is something that we have and sell.” He adds, “I know it’s technically confusing.
Power—which is how much light your device puts out, versus irradiance, which is how much light your device puts out over a certain sampled area, can easily be manipulated (without the right meter.)
The (Ultradent) meter is what you’re going to want when you’re measuring a light’s power to get a true power reading,” Jessop stresses.
Clinicians in the market for a quality curing light want something that will completely and dependably polymerize all light cure dental materials.
However, a light’s purported irradiance doesn’t often represent the full picture, in terms of overall power.
Instead of measuring a light’s irradiance in one hotspot, clinicians should look at how evenly the light’s power is spread out.
“Generally speaking, dentists should aim for light with power uniformity. You want to cover more tooth without oversaturating any areas,” says Jessop.
CLICK HERE to learn more about the other innovative features that make Ultradent’s VALO X curing light one of the most innovative and groundbreaking dental curing lights on the market—and check out the predecessor, the VALO™ Grand curing light, the only curing light ever sent to space.

ULT-5973
Daniel is a longtime news producer turned dental industry storyteller who’s interviewed people on every continent plus the international space station.

He can usually be found eating carbohydrates in the company of his dog.
DANIEL LEWISBI TE RA MPS & TEMPOR ARY OCCLUSAL BUILDUPS




STRUCTUR E FOR ISOL AT ION CL AMPING
J-Temp temporary resin is premixed for ease of use. It is viscous enough that it will not run, but fluid enough to be self-leveling and easy to manipulate. We recommend use with the Black Mini™ tip for simple, precise placement. When it needs to be removed,the light purple color of J-Temp temporary resin allows for easy identification














TEMPOR ARY RE STOR AT IONS




SPLINT INGBET WEEN IMPL ANTCOPINGS


Ceramics: An exceptional material. Why do ceramics have their own set of preparation rules?
Correct use
Ceramics: An exceptional material. Why do ceramics have their own set of preparation rules?
What support is available to quickly learn the proper preparation of ceramics?
Correct use
Four arguments in favor of Komet® tips:
1 Optimized diamond coating (60 μm instead of 40 μm) for shaping and finishing
Four arguments in favor of
Many dentists have to find this out the hard way: Anyone who introduces ceramics, such as zirconium oxide, into the practice must be aware of the special preparation rules. The preparation of ceramic materials is subject to completely new laws, and anyone who ignores them will have no luck with zirconium oxide in the long run. Above all, the shaping of the cavities and compliance with minimum thicknesses cause problems. When it comes to all-ceramic restorations, many practices are still in the transition phase between preparation techniques.
Ceramics: An exceptional material. Why do ceramics have their own set of preparation rules?
Many dentists have to find this out the hard way: Anyone who introduces ceramics, such as zirconium oxide, into the practice must be aware of the special preparation rules. The preparation of ceramic materials is subject to completely new laws, and anyone who ignores them will have no luck with zirconium oxide in the long run. Above all, the shaping of the cavities and compliance with minimum thicknesses cause problems. When it comes to all-ceramic restorations, many practices are still in the transition phase between preparation techniques.
Instruments
Are there any sets that help the dentist in the proper preparation of ceramics?
Many dentists have to find this out the hard way: Anyone who introduces ceramics, such as zirconium oxide, into the practice must be aware of the special preparation rules. The preparation of ceramic materials is subject to completely new laws, and anyone who ignores them will have no luck with zirconium oxide in the long run. Above all, the shaping of the cavities and compliance with minimum thicknesses cause problems. When it comes to all-ceramic restorations, many practices are still in the transition phase between preparation techniques.
Use the QR codes on this page! With their handy reference guide on all-ceramic materials, Komet offers a particularly useful aid: On 30 pages, the correct procedure is described and illustrated with many pictures. Frequently made mistakes are also pointed out. In addition, university professor Dr. Roland Frankenberger provides preparation recommendations and tips for the placement of all-ceramic restorations in a webinar. Each of the above methodsinstruments, sets, video, all-ceramic reference guide and webinar – will enable you to reach your goal of being able to handle ceramics confidently in the future.
What support is available to quickly learn the proper preparation of ceramics?
Four arguments in favor of Komet® tips:

1 Optimized diamond coating stead of 40 μm) for shaping
Instruments
Are there any sets that help the dentist in the proper preparation of ceramics?
Komet supports dentists in “ceramic thinking” with the expert sets 4562/ST (for ceramic inlays and partial crowns) and 4573/ST (for ceramic crowns). These sets were developed in collaboration with six renowned experts from dental clinics and practices. They contain instruments that are tailored to the requirements of highperformance ceramics and guarantee the user a perfectly fitting result right from the preparation stage.
Instruments
Are there any sets that help the dentist in the proper preparation of ceramics?

Komet supports dentists in "ceramic thinking" with the expert sets 4562/ST (for ceramic inlays and partial crowns) and 4573/ST (for ceramic crowns). These sets were developed in collaboration with six renowned experts from dental clinics and practices. They contain instruments that are tailored to the requirements of highperformance ceramics and guarantee the user a perfectly fitting result right from the preparation stage.
Correct use
What support is available to quickly learn the proper preparation of ceramics?
Use the QR codes on this page! With their handy reference guide on all-ceramic materials, Komet offers a particularly useful aid: On 30 pages, the correct procedure is described and illustrated with many pictures. Frequently made mistakes are also pointed out. In addition, university professor Dr. Roland Frankenberger provides preparation recommendations and tips for the placement of all-ceramic restorations in a webinar. Each of the above methods - instruments, sets, video, all-ceramic reference guide and webinar – will enable you to reach your goal of being able to handle ceramics confidently in the future.
Komet supports dentists in "ceramic thinking" with the expert sets 4562/ST (for ceramic inlays and partial crowns) and 4573/ST (for ceramic crowns). These sets were developed in collaboration with six renowned experts from dental clinics and practices. They contain instruments that are tailored to the requirements of highperformance ceramics and guarantee the user a perfectly fitting result right from the preparation stage.





2 The shape of the tips is adapted to today’s ceramic inlays (rather than the formerly used ceramic inserts) and guarantees plane lateral surfaces and rounded transitions throughout.
1. Optimized diamond coating (60 μm instead of 40 μm) for shaping and finishing
2 The shape of the tips is adapted today’s ceramic inlays (rather formerly used ceramic inserts) guarantees plane lateral rounded transitions throughout.
2. The shape of the tips is adapted to today’s ceramic inlays (rather than the formerly used ceramic inserts) and guarantees plane lateral surfaces and rounded transitions throughout.
3. More axial depth to improve the shaping of the buccal and lingual surfaces of the interproximal box as well as the floor of the box.
Use the QR codes on this page! With their handy reference guide on all-ceramic materials, Komet offers a particularly useful aid: On 30 pages, the correct procedure is described and illustrated with many pictures. Frequently made mistakes are also pointed out. In addition, university professor Dr. Roland Frankenberger provides preparation recommendations and tips for the placement of all-ceramic restorations in a webinar. Each of the above methodsinstruments, sets, video, all-ceramic reference guide and webinar – will enable you to reach your goal of being able to handle ceramics confidently in the future.

3 More axial depth to improve the shaping of the buccal and lingual surfaces of the interproximal box as well as the floor of the box.
3 More axial depth to improve of the buccal and lingual interproximal box as well the box.
4 The appropriate sonic tip is available in two sizes to suit premolars and molars.




4. The appropriate sonic tip is available in two sizes to suit premolars and molars.
4 The appropriate sonic tip two sizes to suit premolars


Every day, patients present to the dental office in need of posterior restorations. Each clinical case requires a decision whether a direct or indirect approach is best suited. Support for making the right decision is offered by StyleItaliano™.
According to the group, minimally invasive direct techniques are preferred whenever possible. In this case, follow a step by step guide which details an efficient procedure using a new bulk fill restorative to create a favourable aesthetic result.
Day in, day out, patients present in dental offices with the need for restorative treatment in the posterior region. Every time, we have to decide whether a direct or indirect treatment approach is best suited for the specific case. Support for making the right decision is offered by StyleItaliano.
According to the group, minimally invasive direct techniques should be preferred whenever possible. Thus, there is no indication for inlays, while overlays should be chosen instead of crowns in cases with severely decayed tooth structure (e. g. following endodontic treatment).

Direct composite restorations are not only preferred due to maximum preservation of healthy tooth structure, they also show a high clinical success over time, provided that the basic rules including proper isolation of the working field and correct use of adhesive techniques, are respected during treatment. In addition, innovative restorative materials like bulk fill composites enable the dental practitioner to adopt an efficient procedure.

With the most recent innovation, 3M™ Filtek™ One Bulk Fill Restorative, even the aesthetic impairment caused by a higher material translucency is a thing of the past. A true sample of this enhancement is shown in the following clinical case. The maxillary right first molar of this patient was restored with an insufficient amalgam restoration that had to be replaced, while the adjacent premolar showed a primary carious lesion needing treatment.
Conclusion
This case shows that, if a dental practitioner follows some simple rules and protocols and selects highquality materials it is easy to obtain brilliant treatment results in terms of aesthetics and function.







This is what StyleItaliano refers to as feasible, teachable and repeatable dentistry.
Dr Giuseppe Marchetti teaches the degree course in Dentistry and Masters Degree in endodontics and Restorative Dentistry, at the University of Siena. He also teaches at the Faculty of Medicine, Master of Science in Dentistry at the “Université the Méditerranée” in Marseille (France). He is an active member of StyleItaliano Group, IAED (Italian Academy Of Aesthetic Dentistry) and IAC (Italian Academy Of Conservative) and is a specialist of restorative and prosthetic, with a special interest in aesthetic dentistry.

It is clear that CBCT technology has brought tremendous advantages to dental diagnostics and treatment planning, especially in disciplines such as endodontics, implant planning and oral surgery. But what about 3D for General Dentistry?


“I’m not a specialist or doing complex cases. CBCT is more than I need.” – many GP’s disagree. One of these dentists is Dr. Daniel Butterman. He bought a 3D cone beam for one specific application, never expecting to utilise it across his entire practice. Today, it touches nearly everything and every patient he sees.
Versatile and powerful, crossing all types of dentistry
“I bought a 3D cone beam 10 years ago because I was getting into implants,” said Dr. Butterman, who has been practicing dentistry for 25 years. “I thought that was what I was buying it for. But it shocked me with all the other features and benefits. All of a sudden, it was like someone turned the light on because you can see things you couldn’t see before, from all angles. I was blown away.”
Today, he utilises his cone beam unit multiple times a day. And not just for implant patients, but for nearly every patient. It has replaced the 18 individual films his team used to capture in initial exams. The CBCT gives him more information up front, and also reduces the time his staff spends collecting those images. He uses it with restorative patients, in root canals, periodontics, extractions, orthodontics, and pretty much everything else. Dr. Butterman points to the abundance of data a cone beam delivers as the first and most powerful contributor to a practice’s ROI.
“If I can’t see something, I can’t diagnose it, and I can’t treat it,” said Dr. Butterman. “A doctor will end up with more treatments just because he or she can see more things.”
A cone beam broadcasts hidden issues in the mouth and jaw so a doctor can see them and treat them. In addition, it also allows those problems to be shown to patients in real time so they can become partners in the diagnosis and advocates for their own oral health care. In a few seconds, patients can see things like bone density that may indicate the need for grafting, or a fracture in a hidden area of the tooth. This patient education helps them become more engaged in choosing options and more open to recommended solutions.
Cone beam images can be integrated with digital scans, so a crown can be planned in CAD/ CAM software and imported into the 3D image.
“Patients can see their jaw and final crown on the screen before we even make it,” noted Dr. Butterman. “It’s shocking to them. Case acceptance is night and day.” Cone beam images can also be downloaded into a DICOM file format and sent to other colleagues or other software used in the practice.
Another way a cone beam boosts ROI is in the speed and precision with which procedures can be done. If a doctor was doing an implant case without 3D imaging, he or she wouldn’t know for sure what they would find until they flapped the tissue. Or in the case of root canals, valuable time had to be spent surveying the canal and checking for extra canals. By knowing what’s waiting underneath before the procedure starts, a doctor can approach cases, particularly complex
cases, with more confidence, according to Dr. Butterman. ROI isn’t just measured in what is done, but just as importantly, what doesn’t have to be redone or expanded into a longer appointment, or several.
Dr. Butterman has had patients come in with existing root canals who admit the tooth has never felt right but they’ve just lived with it. Regular X-rays found nothing wrong, but then he takes a 3D image! “I can’t tell you how many root canals I’ve seen that have massive infections even though the patient is asymptomatic,” said the doctor. Patients are thrilled to finally have answers to causes of pain or discomfort that couldn’t be identified before, and the patient word-of-mouth travels far and fast…another intangible ROI.
Empowering Doctors to expand dentistry – More patients in, less referrals out
3D imaging also allows doctors to choose their cases with greater assurance. Dr. Butterman now takes on more complicated implant cases and extractions he believes he wouldn’t have done before, because he can see comprehensive detail. Conversely, he has chosen to refer cases that looked simple initially, but after seeing the 3D images, he realised were more challenging than expected. It gives doctors control of the type of dentistry they want to do.
The ROI for a cone beam may not be as obvious as other technologies like same-day dentistry, but Dr. Butterman has experienced incredible production growth in the years he’s used his. The CBCT allows him to see oral health issues that he wouldn’t have seen any other way and solve them for patients.
“It’s not immediately obvious, but the next thing you know, production will be up because you can see more and do more procedures,” explained Dr. Butterman.
The big contributors to a cone beam ROI are numerous:
• An increased number of cases that are identified due to precise images that capture obscure issues
• Efficiency of treating these cases when a doctor has complete detail about what to expect
• A higher rate of predictable outcomes when challenges can be planned for in advance
• Happy patients who receive and understand the diagnosis and buy in to your treatment
For Dr Butterman, all of those factors are key to his cone beam’s ROI, but there’s one factor that is even greater for him… a single patient experience in which the cone beam discovered a bony tumour. Dr Butterman referred the patient to his doctor, and the patient called back a few months later with news that the tumour had been malignant, and the scan had saved his life!
“There is no greater ROI than that! We are in the business of solving problems,” concluded Dr Butterman. “Diagnosing is our job. If there’s a tool that makes our diagnoses more accurate, we owe it to ourselves—and our patients—to use it.”
Imagine walking down a dark pathway at night. You turn on a flashlight and suddenly you are alerted to things you couldn’t see before that could trip you up…tree roots, uneven ground, winding turns.
That’s what a 3D cone beam imaging system does inside a patient’s mouth – it takes comprehensive, highly precise images that highlight the oral cavity and surrounding anatomy in ways that traditional 2D X-rays, the standard of care, isn’t able to do.

Cone Beam applications in Endodontics
LOCATING CANALS: Root canals are complex procedures, and one reason is the challenge of mapping the canals to be sure nothing is missed and every part of the infection is dealt with successfully. To have the best chance for a good outcome, all the canals should be seen and become a part of the treatment plan.
3D imaging helps Endodontists see how many canals there are, and where they are located. Doctors save a lot of time because they can see immediately if there are unusual anomalies, like a second mesiobuccal canal or missed lingual canals, or roots right on top of sinus cavities.

If there’s an anomaly, Endodontists know before beginning the procedure and can adjust their treatment plan accordingly. In fact, a study evaluated how treatment plans were affected when cone beam imaging data was added to cases vs. only traditional X-rays.
It found in 62% of the cases, evaluators changed their treatment plans on the strength of the 3D images.

This proves it significantly influences the direction and effectiveness of a patient’s treatment, when made available, presumably for the better.
DISCOVERING
3D imaging can also help Endodontists see other conditions that are difficult, if not impossible, to see in intraoral X-rays: vertical root fracture, cracked teeth, or interior or exterior root reabsorption. A clinical assessment, which asks a lot of questions looking for red flags, is done alongside the 3D image.
DIAGNOSING PAIN:
Most doctors have been frustrated when they are unable to find a reason for patient pain because X-rays and other clinical assessments haven’t located the source. Dr. Butterman uses his cone beam with almost every patient as he believes it gives him so much detailed information to discover the source of pain, helping solve problems that were previously mysteries.
Before a single incision is made, many oral surgeons rely on a cone beam 3D imaging system to provide them with detail about the case. With a single rotation, 150200 images are taken and then put together into a threedimensional rendering with sophisticated, predictive software.
CBCT imaging is used most widely in oral surgery. It contributes valuable information applicable to many procedures done in the practice. With the insight it provides, oral surgeons can evaluate and preplan extractions, particularly of third molars; confirm measurements and proximity to other anatomical structures located close to the surgical site; and determine the quality and quantity of bone available for implant surgery.

In addition, 3D imaging allows oral surgeons to discover other pathology such as infections, tumours or cysts, and osteonecrosis. Implant dentistry and impacted tooth extraction are the two main uses for CBCT images.
Regardless of the procedure, the reason so many doctors rely on cone beam imaging is that it alerts them to potential concerns before they make an incision. They can identify areas of risk and prepare for them as well as
share that information with patients. The result is a patient who is engaged with their care and a doctor who is certain of what he or she will find when the procedure begins. This leads to faster and more successful outcomes, which is particularly important when a patient is under anaesthesia.
Impacted teeth: Valuable for surgeries that involve third molars and supernumerary teeth, the cone beam, in a single pass, maps out important anatomical structures that are close to the impacted teeth, such as nerves and sinus cavities. 3D imaging does a better job than traditional X-rays in identifying root resorption in impacted canines and provides details on relationships with adjacent teeth so adjustments can be made to the surgical plan if needed.
Implant planning and placement: A growing number of doctors who place implants say they would not do them without using a cone beam. “In implant surgery there are a lot of issues and factors that you don’t know about until you flap tissue,” explained Dr Butterman. “It’s not predictable. Now I bring the image up and the patient gets to diagnose with me.”
He notes that many times, patients come to him for a second opinion after an implant was recommended. Previously they only saw a 2D image, so they are confused and scared about treatment, particularly if the conversation involves bone grafting. He has found case acceptance increases when patients can see the 3D image.
“If they need it, they know it,” said Dr. Butterman. Doctors also gain valuable information about the quality and quantity of the bone and what size and length the implants should be. In complex cases with multiple implants, the 3D image is so precise, doctors can use it to fabricate surgical guides.
The use of cone beam imaging further advances their dentistry and confidence in taking on complicated, multi-implant patients.
The cone beam can also advise doctors and patients whether an implant should even be done. This knowledge can save a patient the time, expense, and frustration of a failed restoration.
Discovering pathology: Just as valuable is the technology’s ability to see pathology not otherwise seen in exams or 2D X-rays. It’s not uncommon for an
oral surgeon to recount cases where the cone beam identified tumours that turned out to be malignant.
Dental practices often purchase cone beam 3D imaging for a specific application. However, once doctors start using a cone beam, they discover it’s a jack-of-all-trades piece of equipment that’s more versatile and valuable than they thought. A cone beam reveals issues in the oral cavity that would otherwise go unnoticed, elevating the effectiveness of pre-treatment planning for more predictable outcomes.
In the field of periodontics, Periodontists diagnose and treat their patient’s teeth, supporting structure, and gums. The cone beam allows early diagnosis of issues around the tooth and its supporting bone and ligament structures that are not always seen by traditional 2D X-rays.
Being able to diagnose these problems early is important because the disease can progress with few obvious symptoms, damaging teeth and the surrounding bone. This is critical as advanced gum disease is linked to a higher incidence of diabetes, heart disease, and stroke, as well as loss of teeth.
The standard of care in diagnosing periodontal disease has been manual probing of pockets alongside 2D intraoral and panoramic X-rays. While those modalities still provide excellent clinical care, the 2D images do lose some detail by not capturing measurements of three-dimensional teeth. The only way to truly diagnose periodontal disease is through a detailed examination,
so adding a more precise technology to catch signs of advancement is beneficial.
Cone Beam vital to implant dentistry
In addition to identifying advancing bone and structural damage from gum disease, the cone beam is nearly indispensable to Periodontists who have expanded their practice into implant dentistry. Dr. Peter Hunt, who operates a practice that focuses on implant dentistry, purchased a cone beam more than 15 years ago. He uses his unit multiple times every day as 3D imaging gives him the power to plan out every part of the implant procedure ahead of time. He plans the placement of the implant and mocks up the position of the restoration for patient viewing. In addition, 3D images give him the ability to display the bone region for an easy visual when he discusses bone grafting, if necessary.
“The cone beam gives me a much greater sense of comfort,” said Dr. Hunt.
“In fact, in my opinion, doctors shouldn’t be placing an implant without one.”
Dr. Butterman also uses the cone beam images to make choices about the complexity of cases he accepts, and to prepare for the scenarios involved in the procedure ahead of time.
“When you do implant surgery, there are a lot of things you don’t know until you flap the tissue,” said Dr. Butterman. “I might have thought there was more bone support, or I wasn’t sure. Because of the cone beam, I can see that the implant can be done safely. It has let me confidently plan cases correctly.”

From their inception, porcelain laminate veneers have become a staple in modern cosmetic practice. Their indications include the corrections of tooth shape and position, closing of diastemas and masking tooth discoloration. In terms of aesthetics and tooth conservation, these restorations have been proven to be incredibly successful1,2.
When enhancing or rejuvenating a smile, the key is to achieve minimal tooth reduction. The conservative nature of veneer preparation allows for ultra-thin veneers that can be relatively fragile. With advances in material sciences, we now have numerous porcelains with improved aesthetics, bond strength and fracture toughness3. These materials allow the dentist to conservatively design smiles and favorably direct functional forces. However, when nonfunctional forces are applied, as in the case in bruxism, long-term success can be affected. Bruxism can complicate porcelain veneer prognosis, hence in some clinical situations, porcelain veneers may be contraindicated4,5. According to the American Academy of Orofacial Pain, bruxism is a diurnal or nocturnal parafunctional activity which includes clenching, bracing, gnashing and grinding of the teeth6. It is defined as a forcible clenching or grinding of the teeth, or a combination of both in nonfunctional movement of the jaw.
Magne et al. reported that failure rates increased in the presence of uncontrolled bruxism. Managing bruxism in the form of a nocturnal and/or diurnal splint is recommended as a preventative measure to reduce the risk of failure7,8. Occlusal splints allow the mandible to continue the nonfunctional excursive movements whilst balancing the force distribution across the arch, thus protecting the veneers.
A 34-year-old female presented with aesthetic concerns. She found her smile to be unflattering and wanted to improve her overall aesthetics and self-esteem. She wanted slightly sharper “feline” upper canines and a whiter smile.
After thorough co-diagnostic digital smile design and planning, the patient decided on 10 porcelain veneers and
2 resin veneers. The increased length of her upper canines presented a potential risk for increased lateral forces in excursive movements. In addition, the patient reported a history of bruxism.
Flat plane occlusal splint was decided as ideal and the scans were sent for Ai Design via 3Shape Design Services. This is a 15-minute design service enabling same day productions.
Material: Keyprint KeySplint Soft
3D Printer
Asiga Max UV with UltraGLOSS™ material tray and Composer software. See Figure 1
Occlusal Splint Fit
The printed occlusal splint had an incredibly accurate fit with little discomfort or noticeable pressure on the anterior teeth. Due to the digital design process and digital bite registration, only minor occlusal adjustment was required. See Figure 2
The post processing time had been all but eliminated. Apart from the standard washing and post curing requirements, trimming off the sprues at the distal saddle of the splint was the only manual labor required. This allowed us the flexibility of manufacturing and delivering a perfect occlusal splint within a day.
KeySplint soft has always had a high patient compliance due to the fit and nature of the material. Now with the release of the UltraGLOSS™ material tray, chairside fabrication has become effortless and time efficient without compromise.
Longevity of restorations (in the absence of debonding or fracture) is quintessential in successful clinical practice. Patients with bruxism exhibit a three times higher probability of debonding and eight times higher probability of porcelain fractures compared to their non- bruxing counterparts. As such, the use of occlusal splints reduces the failure rate of porcelain laminate veneers in patients with bruxism.
1. Thoroughly mix your KeySplint resin prior to pouring into the UltraGLOSS™ material tray
2. If you already have KeySplint resin in the UltraGLOSS™ material tray, it may be good practice to always clean your build tray according to the Asiga Protocol by exposing the tray to 30 seconds of UV light. Then peel off the cured resin for the base prior to mixing the resin in the tray.

3. When designing your splint, add an extra 3mm of solid form to the distal portion on the splint. This will establish a stable anchor for the splint when mounting it on the build platform. For consistent results, place the splint at a 9-degree angle as shown in Figure 1.
4. Double check that you are using the UltraGLOSS™ material tray profile in Asiga Composer and print at the receommended layer thickness of 50-microns.
5. After printing, use 2 baths with fresh 99% IPA solution. The first bath is to remove the bulk of uncured resin and the second bath is for a thorough wash for 5 mins.
6. After washing and air drying, place the splint in an oxygen free environment and cure for the recommended curing times (times are specific to curing chamber manufacturer).
7. Once cured, remove the distal extension portion with an acrylic bur and lightly buff the area. You are now ready to issue the high gloss splint.

BSc Hons (Melb) BDS Hons (Syd) MSc (Lond) MFGDP (UK) Dr Kasen Somana has been in private practice in Melbourne, Australia for almost 20 years and is the principal dentist of Signature Dentistry in Toorak. His practice has a special interest in conservative digital aesthetic fixed prosthodontics and occlusal rehabilitation.
Asiga 3D printers offer an open material architecture providing compatibility with more than 500 materials from many industry leading 3D printing polymer manufacturers.
1. Chen W, Raigrodski AJ. A conservative approach for treating young adult patients with porcelain laminate veneers. J Esthet Restor Dent. 2008;20:223-238.
2. Fons-Font A, Solá-Ruiz MF, Granell-Ruiz M, Labaig-Rueda C, Martínez-González A. A choice of ceramic for use in treatments with porcelain laminate veneers. Med Oral Patol Oral Cir Bucal. 2006;11:e297-302.
3. Freire A, Archegas LR. Porcelain laminate veneer on a highly discoloured tooth: a case report. J Can Dent Assoc. 2010;76:a126.

4. Walls AWG. The use of adhesively retained all-porcelain veneers during the management of fractured and worn anterior teeth: Part 2. Clinical result after five years follow-up. Br Dent J. 1995;178:337- 340.
5. Peumans M, Van Meerbeeck B, Yoshida Y, Lambrechts P, Van- herle G. Five-year clinical performance of porcelain veneers. Quin- tessence Int. 1998;29:211-221.
6. American Academy of Orofacial Pain. Okeson JP, ed. Orofacial Pain. Guidelines for assessment, diagnosis, and management. Chi- cago: Quintessence Publish Co; 1996. p. 49-73.
7. Magne P, Perroud R, Hodges JS, Belser UC. Clinical performance of novel-design porcelain veneers for the recovery of coronal volume and length. Int J Periodontics Restorative Dent. 2000;20:440-57.


8. Christensen GJ, Christensen RP. Clinical observations of porcelain veneers: a three-year report. J Esthet Dent. 1991;3:174-9.
DR KASEN SOMANA Principal Dentist Signature Dentistry Toorakelements™IC


Obturation System elements™IC
Obturation System
Developed by Dr. L. Stephen Buchanan
Developed by Dr. L. Stephen Buchanan

Obturation is a critical step in the root canal procedure as it helps to prevent leakage, entomb remaining bacteria and reduce the chance of reinfection. The elements IC obturation system was designed to be used with the Continuous Wave warm vertical condensation technique. The extended battery life and inductive charging base makes the elements IC the latest technology for 3D endodontic obturation without cords or wires getting in the way.



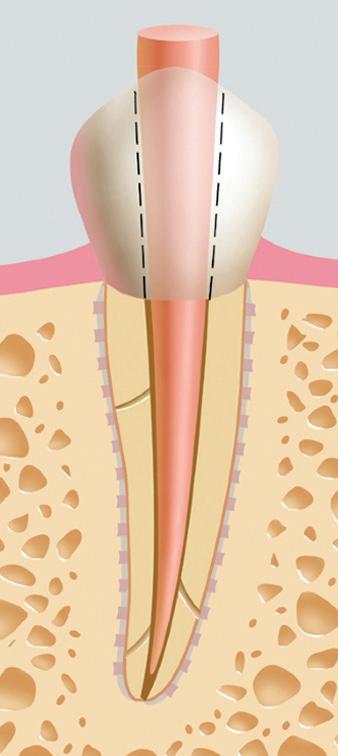



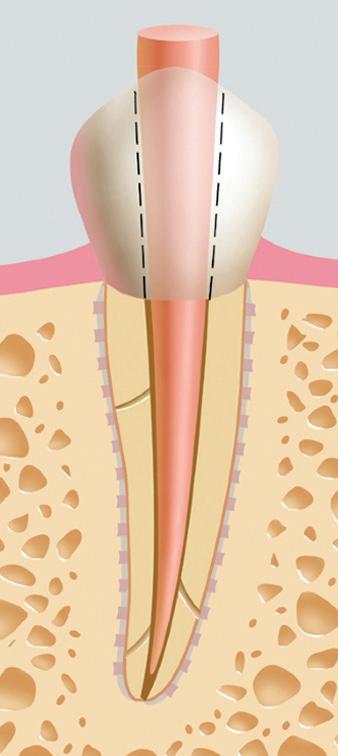

Fit the master cone (in a wet canal) to full length. Grab it at a right angle to the reference point with cotton pliers and trim the tip to be .5mm’s short of full working length.
Fit the master cone (in a wet canal) to full length. Grab it at a right angle to the reference point with cotton pliers and trim the tip to be .5mm’s short of full working length.
Pre-fit a Buchanan Heat Plugger in the canal and adjust the rubber stop to the reference point. Compare the fit plugger to the fit cone to determine the depth of the plugger in the canal – ideal is 4-6mm from the terminus.
Pre-fit a Buchanan Heat Plugger in the canal and adjust the rubber stop to the reference point. Compare the fit plugger to the fit cone to determine the depth of the plugger in the canal – ideal is 4-6mm from the terminus.
Sear the cone off at the orifice level.
#0=
#0= .75mm
#1= .80mm
#1= .80mm
#2= 1.30mm
#2= 1.30mm
Coat the apical 1/3 of the cone with sealer and slowly place it to length in the canal pumping it up and down 2-3 times.
Coat the apical 1/3 of the cone with sealer and slowly place it to length in the canal pumping it up and down 2-3 times.
Select the appropriate size
Buchanan Hand Plugger, and using the stainless steel end, firmly condense the gutta percha at the orifice.


Select the appropriate size Buchanan Hand Plugger, and using the stainless steel end, firmly condense the gutta percha at the orifice.
7 – 14
7 – 14
1-866-KAVO-KERR | kavokerr.com MKT-19-0603.A




Set the heat plugger on the cone. Activate the heat, and downpack, releasing your finger from the operating switch shy of the binding point and maintaining apical pressure for 10 seconds.
Set the heat plugger on the cone. Activate the heat, and downpack, releasing your finger from the operating switch shy of the binding point and maintaining apical pressure for 10 seconds.
Set the heat plugger on the cone. Activate the heat, and downpack, releasing your finger from the operating switch shy of the binding point and maintaining apical pressure for 10 seconds.















Activate the heat switch for a 1 second separation burst, pause 1 second and remove the heat plugger.
Activate the heat switch for a 1 second separation burst, pause 1 second and remove the heat plugger.
Activate the heat switch for a 1 second separation burst, pause 1 second and remove the heat plugger.



#0= .25
#1= .40
#0= .25
#1= .40
#2= .70
Select the appropriate Buchanan Hand Plugger, and using the NiTi end, condense the apical mass while removing any material from the canal walls.
Select the appropriate Buchanan Hand Plugger, and using the NiTi end, condense the apical mass while removing any material from the canal walls.
Select the appropriate Buchanan Hand Plugger, and using the NiTi end, condense the apical mass while removing any material from the canal walls.



Lightly place more sealer in the backfill space with the tip of a paper point.
Lightly place more sealer in the backfill space with the tip of a paper point.
Lightly place more sealer in the backfill space with the tip of a paper point.
Extrude a small amount of material to heat the needle.
Extrude a small amount of material to heat the needle.
Extrude a small amount of material to heat the needle.
Place the Backfill device needle in the canal short of the condensed fill, wait 5 seconds for the needle to reheat. Backfill the canal ½ way. Using the NiTi end of the Buchanan Hand Plugger, condense the fill.
Place the Backfill device needle in the canal short of the condensed fill, wait 5 seconds for the needle to reheat. Backfill the canal ½ way. Using the NiTi end of the Buchanan Hand Plugger, condense the fill.
Place the Backfill device needle in the canal short of the condensed fill, wait 5 seconds for the needle to reheat. Backfill the canal ½ way. Using the NiTi end of the Buchanan Hand Plugger, condense the fill.



Re-insert the needle, wait 5 seconds for it to reheat, backfill to the canal orifice.
Re-insert the needle, wait 5 seconds for it to reheat, backfill to the canal orifice.
Re-insert the needle, wait 5 seconds for it to reheat, backfill to the canal orifice.
Select the appropriate Buchanan Hand Plugger and, using the stainless steel end, condense the coronal fill.
Select the appropriate Buchanan Hand Plugger and, using the stainless steel end, condense the coronal fill.
Select the appropriate Buchanan Hand Plugger and, using the stainless steel end, condense the coronal fill.






Pre-Sterilized
Alternative for Reciprocating and Gold Instruments

• Alternative to Reciprocating Gold Instruments




• Shapes canals in a reverse-reciprocating motion
• Available sizes: R-Glide, R-20, R25, R40, and R50
• ISO color coding
• S-shaped cross-section

- Improved debris removal



• Non-cutting tip
• Available lengths: 21, 25 & 31 mm
• FireWire Blaze technology

• Sterile Packaging
• ULTRA-FIT TM Secure Shank

- Allows for real time apex locator readings

• Spectacular Gold Color Heat Treatment
• Pre-Sterilized










MTApex ™ bioceramic root canal sealer coats the wall of the canals and fills the inner spaces which promotes sealing against coronal and apical leakage. MTApex sealer forms HA on its surface to support healing, making it bioactive. 1 It’s the new addition to the MTA family!


Best of all, it easily delivers through the NaviTip ™ 29 ga Single Sideport tip! It can also be used with any gutta percha for delivery into the canal—and can be removed in case of retreatment.










The MTApex sealer is a powder and gel system consisting of an extremely fine, inorganic powder of tricalcium and dicalcium silicate (which is mixed with a proprietary gel before placement).
• Does not cause discoloration 2

• Retreatment generated less residual root filling material with less dentin removal in comparison to epoxy resin sealers3
• MTApex sealer is bioactive. It forms HA on its surface to support healing of the pulp or the root canal apices4

• Calcium silicate-based cements show potential antimicrobial activity due to high alkalinity5
See the procedure for both NaviTip ™ Single Sideport tip delivery and gutta percha application:

DELIVERING MTAPEX™ BIOCERAMIC SEALER USING NAVITIP 29 ga SINGLE SIDEPORT TIP


Remove the plunger from the clear Skini syringe. Take small portions of mixed MTApex sealer and insert in the back of the barrel or the skini syringe. Replace the plunger.

Attach the tip securely onto skini syringe. Gently press the plunger to remove the air inside the syringe.
Verify flow of sealer prior to applying intraorally.
DELIVERING MTAPEX BIOCERAMIC SEALER USING GUTTA PERCHA
Coat the disinfected and dried master gutta percha point with the mixed MTApex sealer.
Slowly insert into the canal. Add as many gutta percha points as your desired obturation technique requires.
Remove excess gutta percha at the orifice following manufacturer’s direction.
Place the sealer using the required tip in the treatment site following the listed precautions on the IFU

Insert the disinfected and dried master gutta percha point slowly into the canal.
Add as many gutta percha points as your desired obturation technique requires.
Remove excess gutta percha at the orifice following manufacturer’s direction.












As a dentist running a two-surgery practice, efficiency and productivity are paramount to providing quality patient care. Seven years ago, I invested in a Tethys Washer Disinfector from Henry Schein Dental, and it has truly revolutionised our sterilisation processes with its automated approach.

One of the standout features of the Tethys is its ability to free up my staff’s valuable time, allowing them to focus on other essential tasks. With the unit’s efficient cleaning and disinfection capabilities, my dental assistant can rely on it to handle instrument reprocessing effortlessly, ensuring optimal hygiene standards are met. The unit is very easy to use. The controls are simple and intuitive, and the cycle options are clearly labelled.
Using instrument cassettes further enhances the convenience and efficiency of the Tethys Washer Disinfector. Not only does this simplify the loading and unloading process, but it also ensures consistent and thorough cleaning of dental instruments. This streamlined approach eliminates the need for manual cleaning, saving both time and effort for my team.
Additionally, the Tethys drying cycle is an important feature for us. Its effective drying capabilities eliminate the need for manual drying, allowing my dental assistant to move the dried instruments straight to the steriliser, maximising workflow efficiency. This not only saves time but also reduces the risk of moisturerelated issues during the sterilisation process.



I am currently reviewing the Tethys Handpiece Accessory which is designed to complement the Tethys Washer Disinfector, offering a solution to the internal and external cleaning of dental handpieces.
The accessory’s high-level disinfection cycle eliminates potential pathogens, providing an added layer of safety for our patients and staff.
The tank size of the Tethys could be a challenge to bigger practices that use more instruments, however, its quick cycle time ensures that dirty instruments are processed and disinfected within 35 – 45 minutes depending on what cycle is used.
For us, there is no hold-up or wait time for instruments. Should there be a delay in the reprocessing workflow, then it is more important to have disinfected instruments waiting for the steriliser, rather than dirty drying instruments waiting to be cleaned. The unit cleans instruments well and they come out shiny. On the odd occasion, a grossly soiled fluted bur may require reprocessing.
Over the past seven years, I have had no issues with the Tethys Washer Disinfector. Its reliable performance has consistently met our practice’s needs, providing peace of mind that our instruments are consistently cleaned and disinfected to the highest standards.
In conclusion, the Tethys has been an invaluable addition to our practice. Its ability to streamline our sterilisation processes, reduce manual labour, and ensure optimal instrument hygiene, has improved our overall efficiency. I highly recommend this unit to fellow dental professionals looking to enhance their practice’s productivity and maintain best-practice sterilisation protocols.
 DR ALEX AUBONE BDS
DR ALEX AUBONE BDS
The procedures required to prepare a contaminated reusable device ready for its intended use involve several steps. Known as instrument reprocessing, these steps follow an orderly flow from cleaning through to sterilisation and storage.
In our ‘Steps into Steri’ series, we have discussed Step 1 - receiving, cleaning, and decontamination, Step 2 –Preparation and Packaging, and Step 3 - Sterilisation. In this fourth and last instalment of our Steps into Steri series, we proceed to Step 4 – Storage, to explore the key considerations and best practices for instrument storage.
Proper storage of processed instruments plays a critical role in maintaining their sterility and ensuring their quality for patient treatment. The shelf life of sterilised items is not solely determined by time, but is influenced by storage conditions such as temperature, ventilation, and humidity. So rather than time, a concept called ‘EventRelated Shelf Life’ is commonly used in healthcare settings to determine the expiration date or recommended storage duration for sterilised instruments.
The term ‘event-related’ signifies that the shelf life is related to specific events or factors that may compromise the sterility of the instruments, therefore, affecting the length of time that they remain sterile and suitable for use.
These events can include the packaging integrity being compromised, the instrument packs being exposed to excessive humidity, temperature fluctuations, or similar conditions that could potentially impact their sterility.
By employing event-related shelf life, dental practices can ensure that sterilised instruments are stored properly and remain sterile until they are needed for a procedure.


Regular monitoring, inspection, and quality assurance processes are typically put in place to assess the instruments and make informed decisions regarding their usability and storage duration.
Critical items must maintain their sterility until the point of use. Sterilised semi-critical items and noncritical items must be protected from contamination before re-use.
Store items in a clean, dry, dust-free environment outside the contaminated zone. Splashes of fluids and aerosols produced during clinical treatment or instrument reprocessing pose significant risks. Moisture, whether from wet surfaces or splashes with water and other liquids, can lead to contamination.
To prevent packs from being placed on a wet benchtop use Aquasorb Lint Free Cloths (MJ-AQ_) These thick, super-absorbent microfibre cloths will absorb 315% of their own weight without dripping.

Storage areas with dedicated drawers or cupboards for wrapped sterilised instruments will provide added protection against environmental contamination. Transparent doors or locating the stored items at an appropriate height facilitates easy visibility.

The storage area should be adequately sized to prevent the items from being densely packed together, as overcrowding increases the likelihood of packaging integrity being compromised.
High humidity should also be avoided, as it can lead to dampness-related issues. Keeping sterilised instruments in sealed tubs (ZC-20Z459 & ZC20Z463D) helps minimize the risk of contamination.
If open shelves or racks are used for storage, items must be positioned at least 250 mm above the floor and 400 mm away from ceiling fixtures. The Zirc tub and tray rack (ZC-21Z410) can save on counter space as several tubs or trays with covers can fit into one rack. The covers will protect items from dust accumulation. The racks may also be used to store instrument cassettes.


Areas used for instrument storage require periodic cleaning as part of the environmental cleaning process. Surface management can be achieved with a clinical detergent like Majac’s ProDet (MJ-PD5) to help maintain a contaminant-free environment for your stored instruments.
ADA, https://www.ada.org.au/Dental-Professionals/Publications/Infection-Control/Guidelines-for-Infection-Control/Guidelines-for-Infection-Control-V4.aspx
Dental Council, https://www.dcnz.org.nz/assets/Uploads/Consultations/2015/Infectionprevention-and-control-practice-standard-effective1May16.pd The
Orotol® Plus and MD 555 are an unbeatable duo that helps suction systems and amalgam separators to retain their value.
Daily disinfection of the suction unit is a matter of routine in every surgery. Nonetheless, around half of all suction units suffer from reduced performance due to deposits and blockages. The reason: although most suction units are disinfected, no additional cleaning is performed.
However, this aspect is crucial, after all, we are dealing with lots of aggressive substances here, such as blood, secretions, tooth material, filling materials or prophylaxis powders.
These can form a tough sludge. This leads to blockages that can lead to a drop in performance and a complete standstill of the surgery as a result of failure of the suction system.
Not only can Orotol® Plus and MD 555 cleaner prevent this, but at the same time they also offer extremely good compatibility with all the materials*.
The two concentrates complement each other perfectly. While the alkaline disinfectant, Orotol Plus, rigorously tackles bacteria, fungi and viruses, the acidic MD 555 cleaner reliably removes deposits that are difficult to dissolve from all parts of the suction system, including from the pipes.
Our quality promise
Orotol® Plus and MD 555 cleaner:

• Effective removal of biofilm and deposits from all components of the suction system and permanent prevention of their build-up if used on a regular basis
• Extremely gentle on materials
• Ensure that suction systems and amalgam separators retain their value a best possible

• Recommended by leading equipment manufacturers
• Market leaders in Europemade in Germany
Orotol® Plus reliably kills and inactivates microbes throughout the entire suction system (wide scope of action: bacteria, yeast and viruses incl. HBV, HCV, HIV).
MD 555 cleaner reliably dissolves and removes incrustations of difficultto-dissolve salts, lime and prophylaxis powders (including pearl products).
* Only when Orotol® Plus and MD 555 cleaner were used together as a system, was it possible to demonstrate material compatibility on all parts of the suction system during the annual tests.
Prophylactic treatment is a crucial aspect of dental care, and as dental professionals know, every patient is unique and requires a tailored approach to treatment. That’s where the Lunos prophylaxis system from Dürr Dental comes in, offering a range of products that impress with their flexibility and versatility.
Lunos does not prescribe a fixed treatment concept or one that only relates to a specific application area. Instead, practitioners can decide for themselves which form of treatment should be used for each patient. The Lunos portfolio includes a range of products that can be used for various patient needs, ensuring a comfortable and effective experience for both the practitioner and the patient. These include a powder jet handpiece, various prophy powders and prophy pastes. The offering is rounded off with consumables that are reusable, like the prophy rings and aerosol cannulas that can be reprocessed, reducing consumer waste.
Lunos offers two different prophy pastes. The 2-in-1 paste offers the versatility of having an abrasive paste break down into a fine paste within 10 seconds of use due to the friction of the prophy cups. This allows clinicians to confidently remove stains without having to worry about leaving a rough surface area for their patients, which would normally result in an increased uptake of stains between visits.



The super soft paste offers options for children and patients with increased sensitivity due to exposed dentine or the presence of prosthetics due to its RDA value <5 and offers hydroxyapatite as a remineralisation agent. Sodium fluoride is also available in the mint flavour for the 2-in-1 paste.
The prophylaxis cushion rounds off the Lunos range, offering patients a comfortable experience in the dental chair. Made from viscoelastic foam, the cushion is easily moved due to the velcro fastener while maintaining infection control due to its ability to be disinfected with wipes during the pack down and the ability to remove the cover to wash it. Gone are the days of covering the cushion with plastic bags.
Overall, the Lunos prophylaxis system offers dental professionals a flexible and versatile range of products to cater to each patient’s specific needs. By providing effective and comfortable dental prophylaxis, the Lunos system is a must-have for any dental practice looking to provide top-quality care to their patients.


Introduction
For dental practitioners and their patients, latex exposure can cause allergic reactions ranging from contact dermatitis to life-threatening anaphylaxis.

An unprecedented rise of latex allergy in dental and medical health care providers (HCPs) and individuals with specific health problems followed the adoption of measures to prevent the spread of infections (HIV, Hepatitis) and bloodborne pathogens. It is estimated that more than 13 million people worldwide have a latex allergy.1
Data (2016) indicates that the average prevalence of latex allergy worldwide remains 9.7%, 7.2%, and 4.3% among healthcare providers, susceptible patients, and the general population, respectively.1
Investigations have shown that up to 17% of HCPs are sensitised to the allergenic proteins in latex and those at the highest risk of sensitisation include dental assistants, operating room personnel, hospital housekeeping and emergency medical technicians.2,3
What causes latex Allergies 1,4,5
Latex allergy occurs when a person’s immune system reacts to certain proteins found in natural rubber latex (NRL). Of some 250 proteins in NRL, 15 have been identified as allergenic proteins that can elicit a hypersensitive immune response. Prolonged and repeated exposure to latex-allergenic proteins increases the risk and sensitisation to NRL (presence of latex specific e.g. antibodies) is a prerequisite to latex allergy. Latex-sensitive individuals are asymptomatic and generally unaware of their antibody status. Latex allergy occurs following latex exposure and is a systemic reaction leading to a range of reactions, as outlined in the infographic.
Exposure to NRL allergenic proteins occurs via mucous membranes, the vascular system, direct skin contact and inhalation. Inhalation occurs when the cornstarch inside powdered latex gloves binds to latex allergens and becomes airborne during the donning and doffing of gloves.
Population at risk of latex allergy 5 :
• HCPs such as dentists, dental assistants, physicians, nurses, laboratory clinicians, medical technicians
• Individuals with specific health problems including atopy (history of allergy)
• Spina bifida
• Myelodysplasia
• Urogenital abnormalities
• Multiple surgical interventions
• Food allergies (bananas, kiwi, avocado, and chestnuts).
Healthcare workers including dentists and dental hygienists are the most affected occupational group for latex allergy due to their frequent donning and removal of latex gloves.1
Data shows that up to 17% of healthcare workers are sensitised to latex.2
Due to their frequent repeat exposure, all dental professionals who use latex gloves should be considered at high risk for allergic reactions.5 Even as many dental practices transition away from latex gloves, latex allergy remains a highly prevalent occupational health hazard among practitioners.

That is partly because latex is present not only in gloves but also in common dental products such as dental dams, bite blocks, mixing bowls, syringes, suction tips, oxygen masks, adhesive bandages and more.
The frequency with which dental practitioners contact additional latex products may not be as high as the exposure to allergens from a latex glove.

Due to recent advancements in technology, nitrile gloves have significantly improved, making them a popular alternative to latex gloves in dental clinics. These gloves are now more comfortable to wear, offer better grip, and have increased puncture and chemical resistance.
As a result, dental clinics may opt for nitrile gloves to provide better protection to their staff and patients.
For more information, please reach out to your Ansell or Henry Schein Representative.
1. Wu M, McIntosh J, Liu J. Current prevalence rate of latex allergy: Why it remains a problem? J Occup Health. 58(2):138-144. March 2016
2. Dermata A, Arhakis A. Latex Allergy in Dental Care. Balk J Dent Med. Vol 18, 2014.
3. Burkhart C, Schloemer J, Zirwas M. Differentiation of Latex Allergy from Contact Dermatitis. Contact Dermatitis. Vol. 96, December 2015.
4. Pien L. Latex Allergy. Cleveland Clinic Center for Continuing Education. Disease Management. Published 2010. Reviewed 2017. http://www. clevelandclinicmeded.com/medicalpubs/ diseasemanagement/allergy/latex-allergy/
5. Katelaris C. Latex Allergy Diagnosis and Management. World Allergy Management. September 2016
Avoidance of latex is critical to managing latex allergy. Research shows that when measures were taken to minimise latex exposure during dental treatment, 81% of latex-allergic patients did not suffer adverse reactions.6
Additionally, management protocols for latex allergy are recommended, including steps to evaluate both staff and patients for their risk of latex allergy, guidelines to create a latex-safe environment, education about latex allergy and emergency preparedness for adverse patient or staff reactions, should they occur.7
6. Kean T, McNally M. Latex hypersensitivity: a closer look at considerations for dentistry. Journal of the Canadian Dental Association 2009
7. Hamann C, Rodgers P, Sullivan M. Prevalence of Type I Natural Rubber Latex Allergy Among Dental Hygienists. Journal of Dental Hygiene, Vol.79, No. 2, Spring 2005.
Infection Prevention is critical in the field of Dentistry. Pathogenic microorganisms can infect both patients and dental workers and spread through contact with contaminated surfaces, instruments, and equipment.
Whiteley is a leading global innovator in infection prevention solutions. We are a family-owned Australian business, who have been operating since 1933. Our TGA licensed manufacturing facility is based in Newcastle, NSW. Unlike many other suppliers in the domestic infection prevention field all our research and development is conducted in Australia.
Whiteley is committed to world leading research and innovative product development in the field of hygiene, cleaning, and infection prevention and control products.

Infection Prevention in the Dental Industry
Dental workers and their patients can be exposed to a range of pathogenic micro-organisms. These organisms can be transmitted through contact with contaminated objects such as instruments, equipment, and environmental surfaces.
Good hand hygiene and surface disinfection practices are critical in reducing the risk of contamination between dental workers and patients.
Whiteley offers a range of products suitable for creating a clean and safe environment in the dental practice setting.


These products include surface cleaners, disinfectants, instrument cleaners and hand hygiene products. In May 2020, the Therapeutic Goods Administration (the TGA) confirmed that Viraclean® [AUSTL 69000], “Kills Coronavirus, SARS-CoV-2 (COVID-19)”.
Long the flagship product within Whiteley’s range of disinfectants, Viraclean® was the first product in Australia approved by the TGA to carry this disinfection claim against the COVID-19 virus. Viraclean® is a Hospital Grade Disinfectant intended for use on a wide range of healthcare surfaces.
Effective surface cleaning and disinfection, particularly of high touch areas (i.e. doorhandles, benchtops etc.) combined with good hand hygiene practices will assist in protecting your staff and patients, especially as we move into the winter months that inevitably bring higher rates of colds and flus.
Ensuring hand sanitisers are easily accessible for patients in the waiting rooms, and staff in the practice rooms, will assist in minimising the risk of infection. The entire range of Whiteley’s hand hygiene products are manufactured in Australia and include Bactol® Alcohol Gel antibacterial hand rub (TGA registered, AUST R 155397), the Dermalux range of hand soaps, and Bactol® Moisturiser.
Bactol® Alcohol Gel provides antibacterial hand cleansing without the need for water. It has been specially formulated with a natural emollient to replace the skin’s lipids.
This helps maintain skin integrity and prevents moisture loss leaving your hands hygienic, soft and replenished. Bactol® Alcohol Gel has been developed in compliance with the EN1500 testing standard for alcohol-based hand rubs.


Good hand hygiene is critical in preventing the spread of germs in dental practices. There are 5 simple steps you can take to improve hand hygiene compliance:
1. Ensure sanitiser dispensers or bottles are conveniently located.
2. Increase monitoring and surveillance.
3. Choose products staff like using. This is the quickest and best method of increasing hand hygiene compliance rates.
4. Use signage like the 5 Moments of Hand Hygiene posters to promote effective hand hygiene practices.
5. Encourage your team to provide feedback to each other on hand hygiene.








Dr.
StyleSkulpt 1
Posterior Occlusal Shaper
HF-TNTAM1
DESCRIPTION
PART CODE
Cone Socket Mirror Handle, Satin Steel MH6

#5 HD Mirror MIR5HD
StyleSkulpt 1, Posterior Occlusal Shaper TNTAM1
StyleSkulpt 2, Universal Thin PFI TNTAM2
StyleSkulpt 3, Curved Ball Burnisher TNTAM3
Posterior Sickle Scaler, EverEdge 2.0


StyleSkulpt Kit
S204S9E2
TNTAMKIT*
*Kit contains instruments in 5-instrument cassette
StyleSkulpt 2
Universal Thin PFI

HF-TNTAM2
StyleSkulpt 3
Curved Ball Burnisher



HF-TNTAM3
Clarence’s practice is limited to cosmetic and restorative dentistry. She is well-published to both the local and international dental press, writing articles, reviewing and developing prototype products and techniques in clinical dentistry.

She frequently and continually lectures internationally.
Clarence is the Chairperson and Director of the New Zealand Academy of Cosmetic Dentistry.
She is currently one of two individuals in Australasia to hold Board-Certified Accredited Member Status with the American Academy of Cosmetic Dentistry.
Clarence is an Opinion Leader for multinational dental companies Kuraray Noritake, J Morita Corp, Henry Schein NZ, Ivoclar Vivadent, DentsplySirona, 3M ESPE, Kerr, GC Australasia, SDI, Coltene, Triodent and is the only Voco Fellow in Australia and New Zealand. She holds Fellowship status with the International Academy for DentoFacial Esthetics. She is a passionate and approachable individual, and is committed to having an interactive approach with patients in all of her cases to maximize predictability.
DR CLARENCE TAM
HBSc, DDS, FIADFE, AAACD
Auckland, New Zealand
henryschein.co.nz
With the development of adhesive dentistry, the need for moisture control and adequate isolation is paramount for long term predictability and success with both direct and indirect dental procedures.
The last few years with the Coronavirus pandemic have also raised unprecedented concern with dental practitioners exposed to the aerosol from patients mouths during clinical procedures.
The use of rubber dam, along with mouth rinses and disinfection may offer benefits to safeguard and minimise transmission of air-borne micro-biological attack. The advantage of rubber dam include:
• Moisture control – preventing saliva, blood, gingival crevicular fluid from interfering with clinical procedures. This is particularly important for optimal adhesion when potential for moisture contamination can reduce or inhibit correct adhesion and cause premature failure of restorations. It is often quite a task to manage patients to prevent them from conversing, closing or swallowing. With the presence of rubber dam this precludes some of these possible adverse scenarios affecting any possible moisture contamination.
• Patient protection –the use of endodontic instrumentation and medicaments are prevented from being ingested or aspirated. It may also minimise any debris raised from removing old restorations, fractures from also inadvertently dropping in the oro-pharangeal area. The patient often finds it quite relaxing and
comfortable once they are accustomed to the rubber dam. Not having liquids at the back of their mouth needing to be constantly sucked up by high-speed evacuation may be much more comfortable.
• Visual access – the use of rubber dam allows access into the mouth, enabling lips, cheeks and tongue to be retracted away from the working region. This improves access and visualisation. The use of a coloured rubber dam with the contrasting colour can also allow better visualisation and photography of the teeth. It may also allow retraction of the gingival tissues with appropriate rubber dam clamps allowing unimpeded access to carious or subgingival margins.
• Minimisation of infection transmission
The creation of aerosols during dental procedures along with the proximity of the dental team exposes them to the potential of infective respiratory diseases and salivary microbiological load. The use of rubber dam provides an aseptic field and may assist to reduce the possibility of infection risks.
Recently, a dental company has improved on current rubber dam offerings with the addition of a pre-printed rubber dam.
This is a powder free latex rubber dam black in colour. HySolate Black Edition (Coltene) was created to allow for higher contrast and, thus, improved visibility during procedures.


Theutilisation of rubber dam has always been taught to be mandatory for endodontic procedures however the indication for use extends also to restorative dentistry in assisting to perform procedures optimally, efficiently, and safely.
The black colour is nonreflective surface with no glare to contend with during treatment. The material consistency is medium in strength allowing excellent retraction of the tissues.
The addition of the pre-printed template, marked on the rubber dam with the position of the teeth ensures that the holes are punched in the correct positions on the dam easily and accurately.
Historically, one would have to mark the dam with a rubber stamp, which sometimes would rub off, so the saving in time and convenience is a welcome addition.
For those that prefer a non-latex rubber dam the Hysolate Non-latex range has a Flexi-dam which may be preferred for those that don’t like the medium to heavy retraction from conventional rubber dams.
This rubber dam is also excellent for the full arch isolation technique due to the ability to stretch without tearing the rubber dam.
It is often commented placement of rubber dam is a difficult procedure and the time to apply the dam is excessive, or it can feel uncomfortable for the patient.

Utilising the correct technique and with the new rubber dams available on the market allows efficient application and can reduce clinical procedure time as well as safeguarding the clinical team from unnecessary exposure to harmful micro-organisms.
View Hysolate Range ISOLATION
Protects teeth from acidic food and drinks
Buffers dental plaque acid from bacteria
Great for patients with braces or aligners
Tooth Mousse Plus with 900ppm fluoride

Available in 5 delicious flavours

For dry mouth sufferers
Great for patients on medications causing dry mouth Neutral pH and sugar-free Available in 5 delicious flavours

Stimulates saliva flow and protects teeth
Sugar-free with long-lasting flavours
Available in refreshing mint flavour
Super soft wedge-shaped floss Micro-fibre technology
5 x more fibres than existing floss Available in refreshing mint flavour

GC Tooth Mousse (TM) and Tooth Mousse Plus (TMP) are amongst the most well researched dental products today, with an evidence base of over 150 journal papers and 7 systematic reviews. This article summarises the most common applications that involve daily use of these products, applied with a clean finger or brush onto the teeth just before bed.

For infants and young children, TM reduces colonisation of the mouth by cariogenic Streptococcus mutans bacteria, with a corresponding rise in health-associated oral bacteria such as Strep. sanguinis and Strep. salivarius, and lowered acid production by dental plaque. TM increases mineral levels in primary teeth affected by molar-incisor hypomineralisation, or developmental defects of enamel.
In patients undergoing orthodontic treatment, TMP is more effective for preventing the development of enamel lesions around brackets than conventional fluoride products. It is highly effective for reversing active white lesions in orthodontic patients.
For high caries risk adults, both active and arrested enamel carious lesions can be reversed. Arrested lesions require a pre-treatment (such as short acid etch) to enhance porosity. Likewise, developmental enamel defects and fluorosis in permanent teeth can be reversed back to a normal appearance. For fluorosis, a longer acid etch pre-treatment (2 minutes with agitation) is needed, with enamel microabrasion to remove surface stains and enhance penetration.
Tooth Mousse is highly effective for treating sensitive exposed cervical dentine, by laying down an acid-resistant layer of mineral, even in patients with poor salivary flow or gastric reflux.


In tooth wear cases, TMP will remineralise tooth structure substrate prior to bonding adhesive materials. In patients having home bleaching using peroxide gels, TMP will treat tooth sensitivity from exposed root surfaces.
It will also cause an enamel lightening effect which reduces the yellow colour of teeth.
In older patients, TM and TMP will arrest lesions of root surface caries where the root surface has softened but not yet cavitated.
They can also be applied in a smear on overdentures and partial dentures to help protect abutment teeth from caries.
Local application of TMP onto glass ionomer cement restorations that contain CPP-ACP (e.g. Fuji VII EP) will recharge the reservoir of these materials so that they can continue to release bio-available calcium, phosphate and fluoride ions.
Long term daily application of TM and TMP can also reduce the likelihood of patients with dry mouth developing tooth wear or dental caries, but combined chemical actions and biological (prebiotic) effects.
MinerOss® Putty is uniquely a 100% allograft that includes a powerful combination of mineralised cortical/ cancellous chips with demineralised cortical fibers for optimal implant site development.
All natural carrier
MinerOss® Putty features an allograft collagen carrier which eliminates artificial carriers, fillers or binding agents that don’t assist in bone formation.
cortical/cancellous chips with demineralised cortical includes a powerful combination of mineralised
Improved clinical handling
fibers for optimal implant site development..

MinerOss® Putty maintains moldable, cohesive handling characteristics to easily fill irregular defects.
all natural carrier
High mineral content
MinerOss® Putty features an allograft collagen carrier which eliminates artificial carriers, fillers or binding agents that don’t assist in bone formation.

Offering a 50:50 ratio of mineralised cortical/ cancellous chips and demineralised cortical fibers, MinerOss® Putty is designed for enhanced regenerative capacity.
Mineralised allograft chips have been proven to provide a natural scaffold to support new bone formation and demineralised allograft bone has been proven to stimulate bone regeneration.
MinerOss® Putty maintains moldable, cohesive handling characteristics to easily fill irregular defects.
The combination of both has been shown to significantly generate more mean vital bone and less residual graft material in as little as 18 weeks.1
Offering a 50:50 ratio of mineralised cortical/cancellous chips and demineralised cortical fibers, MinerOss® Putty
regeneration. The combination of both has been shown to significantly generate more mean vital bone and less scaffold to support new bone formation and demineralised allograft bone has been proven to stimulate bone is designed for enhanced regenerative capacity. Mineralised allograft chips have been proven to provide a natural
MinerOss® Putty is uniquely a 100% allograft that residual graft material in as little as 18 weeks.1
Applications include
• periodontal defects
applications include
• periodontal defects
• extraction socket grafting
• extraction socket grafting
• peri-implant defects
• peri-implant defects
• crestal and lateral sinus augmentation
• crestal and lateral sinus augmentation
• lateral and vertical ridge augmentation
• lateral and vertical ridge augmentation
Ordering Information
BH-MIN-PT0-5
MinerOss Putty 0.5cc Syringe $322+gst
ordering information
BH-MIN-PT1-0
MinerOss Putty
MinerOss Putty 1.0cc Syringe $464+gst
MinerOss Putty




BUY x5
Tapered Inter nal Implant or any Biologics*
GET x1
Tapered Inter nal Implant or Biologics++
BUY x10
Tapered Inter nal Implant or any Biologics*
GET x3
Tapered Inter nal Implant or Biologics++
BUY x50
Tapered Inter nal Implant or any Biologics*

E T BU Y& ++
GET x20 G
What is the key ingredient in tooth whitening systems?
The active chemical ingredient used in most professional whitening systems is hydrogen peroxide, which is delivered as either Carbamide peroxide or Hydrogen peroxide. Hydrogen peroxide contains a single oxygen - oxygen bond, known as the peroxide bond - this is weak and unstable. When it breaks it decomposes into water and oxygen and releases free radicals. It is these free radicals that are reactive with other substances and have the ability to breakdown compounds that have colour or darker shades, called chromogens. These chromogens cause staining to our teeth, both intrinsic and extrinsic. The breakdown of these compounds means there is a reduction in the discolouration and hence a lighter looking tooth. 1
What type of delivery methods are there for whitening treatments?
There are different whitening methods available and when deciding which option to go for, the advantages and disadvantages of each option should be explored and clearly explained to patients. Staying up to date on new technologies and innovations in whitening is also important for dental professionals so they know what options are available for patients. The two main types of professional whitening are;
1) Take Home Whitening
Home whitening has traditionally involved the patient wearing custom trays for the indicated length of time either during the day or at night as indicated for the given whitening product. There are also whitening systems such as Optic White Light Up Take Home, that uses a LED Device instead of custom made trays along with a unique 6% hydrogen peroxide serum, this system is indicated for 10 minutes a day for ten days to provide up to 7 shades whiter teeth.
2) In-Chair Whitening
In-chair or in-office teeth whitening treatment is ideal of patients who want faster results. Traditional in-chair systems use a higher-concentration of peroxide and therefore require a gingival barrier to reduce the risk of gingival irritations or gingival burning.

Many systems will also use a light-releasing device to activate the hydrogen peroxide. The Colgate Optic White Light Up In-Chair system uses a unique 10% hydrogen peroxide serum and an Indigo LED device to achieve up to 5.9 shades whiter in just a thirty minute treatment*.

The most frequently occurring side effect during tooth whitening is sensitivity. This typically lasts between 1 and 4 days. It occurs because the hydrogen peroxide molecules are able to penetrate not only the enamel, but through the dentine and to reach the pulp. Another side effect, which can occur when hydrogen peroxide touches the gingiva is gingival irritation and in some cases burning. This may also factor in what options you offer for some patients. This is why it is important to be aware of other options with formulations designed for minimal or no sensitivity including lower concentrations, new application methods and shorter treatment times such as the Colgate Optic White Light Up range. Dental professionals should screen all their patients for any aesthetic concerns about their smile and whether whitening can address these. If whitening is being offered in your practice, this should be displayed as an option within the practice so patients are aware this is a treatment that you offer. From there, you and the patient can determine which type of whitening treatment would work best for them. Refer to leaflet for full instructions
Reference
1. Carey C. M. (2014). Tooth whitening: what we now know. The journal of evidence-based dental practice, 14 Suppl, 70–76. https://doi.org/10.1016/j. jebdp.2014.02.006
The bioaerosols generated during dental procedures pose a potential risk for the spread of infections to dental personnel and patients.(1,2)
Aerosols can stay suspended in the air for up to four hours after dental procedures and can travel distances of up to three metres from the original source. This can result in dental personnel being exposed,
infected aerosols can linger past when protective equipment is removed. (1,2)
Patterns of bacterial splatter and aerosol can be used to understand how a virus can spread during dental procedures. Even when a high-volume suction is used, there can be positive contamination. (3)
The most heavily contaminated areas are an operator’s face (this may be possible even under the visor and mask), arm nearest the patient, and the patient’s body. The assistant’s face and arm are also often in the contamination zone. (3)
When an effective preprocedural rinse is used, there is a mean reduction in the number of colony forming units of 64.8% when compared with control.(1)
as




SUPER. FAST. WHITENING. Pola Rapid is the new in office whitening treatment that safely whitens teeth in just 24 minutes.
• 150% Faster Treatment Time
• Enhanced Blue Gel For Faster Application

• Built In Desensitisers
“I find Pola Rapid a beautiful, easy-to-use product. It is simple to apply and remove with its non-stick and enhanced blue gel formula.
Pola Rapid is the new in office whitening treatment that safely whitens teeth in just 24 minutes.
150% FASTER TREATMENT TIME

A great product to use by clinicians for in-chair whitening with minimal chair time and patient sensitivity, but reliable and immediate results.”
ENHANCED BLUE GEL FOR FASTER APPLICATION
BUILT IN DESENSITISERS
FLUORIDE RELEASING TO STRENGTHEN TEETH CLINICAL CASE STUDIES
Pola Rapid 38% “Pola Rapid has exceptional colour saturation for enhanced visibility during intraoral application. The new non-stick bleaching gel stays where you apply it, and easily wipes away clean with no mess.

"I find Pola Rapid a beautiful, easy-to-use product. It is simple to apply and remove with its non-stick and enhanced blue gel formula. A great product to use by clinicians for in-chair whitening with minimal chair time and patient sensitivity, but reliable and immediate results.”
I found the new system fast, reliable to use with minimal sensitivity for patients”
DR MILES CONE Fellow American College of Prosthodontists Diplomate Americn Board of Prosthodontics, Nuance Dental Specialist, Portland, Maine USA



AFTER BEFORE
intraoral
The new non-stick bleaching gel stays where you apply it, and easily wipes away clean with no mess. I found the new system fast, reliable to use with
TOTAL USES 56
CLINICAL RATING 92%
Key features: In-office whitening system l 38% Hydrogen Peroxide
l Dual-barrel syringe dispenser with brush-tip applicato
Use a surgical suction to remove the whitening gel between applications for fast and precise removal.






Description
SDI sdi.com/au/au
Pola Rapid is an advanced in-office tooth whitening system:
Key features
• Whitens teeth with an incredibly fast 24-minute application time.
Double check the barrier between each application and make sure there are no areas of leakage.
• Features built-in desensitizers and fluoride.
• In-office whitening system 38% Hydrogen Peroxide
• Uses a 38% hydrogen peroxide formulation.
• Simple and precise application.
19 CLINICAL EVALUATORS
• Dual-barrel syringe dispenser with brush-tip appl icator

TOTAL USES 56
• In-office teeth whitening.
Description
Unique Attributes
CLINICAL RATING 92%
• Blue gel makes for easy application and visibility.
Pola Rapid is an advanced in-office tooth whitening system:
Key features: In-office whitening system
• Faster system - this material only requires 24 minutes of treatment, significantly reducing patient time in the chair.
l Dual-barrel syringe dispenser with brush-tip applicato
• Features built-in desensitisers and fluoride.
• The brush tip allows you to place very easily.
• Light is not necessary; however, the light can be used with the whitening attachment and the Pola Stand.
• Uses a 38% hydrogen peroxide formulation.
• Simple and precise application.
Pola Rapid is an advanced in-office tooth whitening system:
• Whitens teeth with an incredibly fast 24-minute application time.
Indication
• Features built-in desensitizers and fluoride.
• Uses a 38% hydrogen peroxide formulation.
• In-office teeth whitening.
• Simple and precise application.
Indication
Unique Attributes
• Blue gel makes for easy application and visibility.
• In-office teeth whitening.
• Blue gel makes for easy application and visibility.
• Faster system - this material only requires 24 minutes of treatment, significantly reducing patient time in the chair.
• Faster system - this material only requires 24 minutes of treatment, significantly reducing patient time in the chair.


• The brush tip allows you to place very easily.
• The brush tip allows you to place very easily.
• Light is not necessary; however, the Radii Xpert light can be used with the whitening attachment and the Pola Stand.
• Light is not necessary; however, the light can be used with the whitening attachment and the Pola Stand.
• Use a surgical suction to remove the whitening gel between applications for fast and precise removal.
Make the time to take before and after photos. It really shows the patient the difference. Even I did not realize there was such a big difference for a couple of patients until I looked at the photos later.
“GOOD RESULTS, EASY TO USE, AND NO LIGHT NEEDED.”
• Double check the barrier between each application and make sure there are no areas of leakage.
“Instructions were easy to follow and time for the procedure was excellent.”
“I really liked the brush tip and simplicity of the packaging.”
• Make the time to take before and after photos. It really shows the patient the difference. Even I did not realise there was such a big difference for a couple of patients until I looked at the photos later
Use a surgical suction to remove the whitening gel between applications for fast and precise removal. Double check the barrier between each application and make sure there are no areas of leakage.


“Easy application.”
“The quick chair time is amazing. I had patients who have had other brand name in-office whitening comment they this was so much faster and they got better results.”
Evaluator’s comments
“Color of the gel allowed easy visibility in placing.”
Make the time to take before and after photos. It really shows the patient the difference. Even I did not realize there was such a big difference for a couple of patients until I looked at the photos later.
“I feel that it worked well both with and without the Radii Xpert light.”
“GOOD RESULTS, EASY TO USE, AND NO LIGHT NEEDED.”
“Instructions were easy to follow and time for the procedure was excellent.”
“The brush applicator takes a little getting used to. It makes the applicator tip overall wider than you may be used to.”
“I really liked the brush tip and simplicity of the packaging.”
“Easy application.”
“Worked nicely and didn’t drive sensitivity on root exposure patient - able to control application.”
“Instructions were easy to follow and time for the procedure was excellent.”
“The quick chair time is amazing. I had patients who have had other brand name in-office whitening comment they this was so much faster and they got better results.”
“I really liked the brush tip and simplicity of the packaging.”
When dispensing the first amount, it was difficult to get the mixing of material just right - seems like a lot wasted.”
“Color of the gel allowed easy visibility in placing.”
“Easy application.”
Evaluation Summary:
“I feel that it worked well both with and without the Radii Xpert light.”
“The quick chair time is amazing. I had patients who have had other brand name in-office whitening comment they this was so much faster and they got better results.”
Compared to Competitive Products:
“The brush applicator takes a little getting used to. It makes the applicator tip overall wider than you may be used to.”
“Color of the gel allowed easy visibility in placing.”
“I feel that it worked well both with and without the Radii Xpert light.”
“Worked nicely and didn’t drive sensitivity on root exposure patient - able to control application.”
“The brush applicator takes a little getting used to. It makes the applicator tip overall wider than you may be used to.”
“When dispensing the first amount, it was difficult to get the mixing of material just right - seems like a lot wasted.”
Worked nicely and didn’t drive sensitivity on root exposure patient - able to control application.”
“When dispensing the first amount, it was difficult to get the mixing of material just right - seems like a lot wasted.”
Evaluation Summary: Compared to Competitive Products:

