Tapered Pro Conical Clinical Case Report



Clinician Information







Dr. Zadeh is an Associate Professor at the USC School of Dentistry and a Diplomate of the American Board of Periodontology. He received his doctor of dental surgery degree from USC School of Dentistry in 1987. He has also completed advanced clinical education in Periodontology and earned a PhD degree in immunology from the University of Connecticut, Schools of Dental Medicine and Medicine.
Dr. Zadeh directs the Laboratory for Immunoregulation and Tissue Engineering (LITE), funded by the National Institutes of Health. He has extensive publication track record and serves as editorial reviewer for several international scientific journals. He also serves on an advisory panel to the Center for Scientific Review of the National Institutes of Health. Dr. Zadeh is the Director of the USC Periodontal and Implant Symposium, and the USC Comprehensive Surgical and Restorative Implant Training Program. He also maintains a part-time private practice limited to Periodontology in Southern California.


• Patient presented to his restorative dentist after his anterior two crowns fractured off (1).
• Intraoral radiograph revealed the extent of tooth structural loss (2).
• Options of Endodontics treatment, crown lengthening and restoration was discussed with the patient, but he opted to have the teeth replaced with dental implants (3).
• The restorative dentist placed provisional on the central incisor teeth (4).









• Patient presented with provisional restorations on his central incisors. The gingival contours were optimal, and the gingival phenotype was thick (1 & 2).

• The alveolar bone was intact, and the alveolar crest was approximately 4mm apical to the restorative margin (3).





• The central incisors were extracted using a minimally invasive protocol. The alveolar bone and gingival tissues were intact after extraction (1).
• Extracted central incisors (2).
• Two BioHorizons Tapered Pro Conical implants of 3.8 x 15mm were placed according to the plan (3).



3
• Implants immediately after installation (4). 1


2




4


• Implants immediately after installation (1).
• Scan bodies were installed to allow the implants to scanned for fabrication of custom abutments and definitive restorations (2).
• Periapical radiograph verified proper seating of the scan bodies (3).
• Intra-oral scan image after scanning the implants (4).









• Titanium temporary abutments were installed (1).
• Screw-retained provisional restoration was fabricated (2).
• Composite bone graft was generated by adding iPRF to Miner-Oss corticocancellous allograft (3). (The implant drivers were positioned into the implants to protect them while bone was used to fill the horizontal gap between the sockets and the implants.)
• After removal of the implant drivers bone graft appears to fully fill the horizontal gap between the sockets and the implants (4).









• Screw-retained provisional restoration was placed into the implants (1).
• Prior to complete searing of the provisional, LPRF was placed to protect the graft material (2).
• The provisional restoration was fully seated (3).


• Screw retained provisional restoration was placed (4). 1 3 2 4







Radiograph of implants, grafts and Provisionals (1).
Clinical view at two days post-operative visit (2). Clinical view at two days post-operative visit (3).
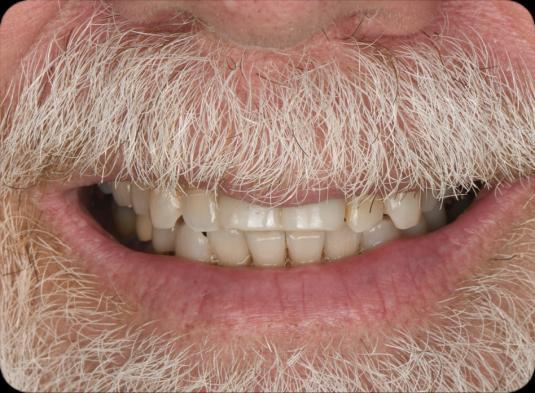
Patient’s smile after implantation and previsualization (4).










A N K T
Y O U !
