The Advocacy & Awareness Issue
 Winter 2023 A Publication of Hearing Health Foundation hhf.org
Winter 2023 A Publication of Hearing Health Foundation hhf.org
Speaking up to make a difference

The mission of Hearing Health Foundation is to prevent, research, and cure hearing loss and tinnitus through groundbreaking research and to promote hearing health. As the largest nonprofit funder of hearing and balance research in the U.S., we are a leader in driving innovation and treatments for people with hearing loss, tinnitus, and related conditions.
This issue’s theme is Advocacy & Awareness, an acknowledgment that hearing loss can be an invisible disability because it may not be immediately obvious that someone has difficulty hearing. It is also often the case that the person with a hearing loss has difficulty accepting and by extension treating their hearing loss. We hope this issue’s stories inspire readers to address their own or their loved ones’ hearing challenges. While over-the-counter hearing aids are poised to bring greater accessibility to adult consumers with mild to moderate hearing loss, managing hearing loss effectively still benefits from input from experienced medical or hearing care professionals.
Given the links between untreated hearing loss and overall well-being, including brain health, we owe it to ourselves to be as aware of our hearing health as we are about our vision, diet, or daily step count. Let’s all take care of our hearing, for life—get hearing tested regularly, remove the stigma of using hearing devices, advocate for quieter shared spaces, be aware of sound exposure, and wear earplugs when needed. Let’s love our ears. Please enjoy this issue and share it with family and friends. Thank you for your support and for being a part of our community.
 Timothy Higdon President & CEO Hearing Health Foundation
Timothy Higdon President & CEO Hearing Health Foundation





Hearing Health
The Advocacy & Awareness Issue
Winter 2023, Volume 39, Number 1
Features 06 Living With Hearing Loss The Gene TMPRSS3 and Me. 08 Advocacy Science Is Just the Start. Daniel Fink, M.D. 12 Managing Hearing Loss If I Were the Minister of Hearing Health. Shari Eberts 13 Education What Social Media Can Teach Audiologists. Kathleen Wallace, Au.D. 14 Workplace Speaking Through Color. Matthew Masapollo, Ph.D. 18 Living With Hearing Loss Humming Again. Roberta Rubenstein Larson 21 Living With Misophonia My Misophonia Story. Kadyn Thorpe
Departments
46 Meet the Researcher Melissa Polonenko, Ph.D. Generously funded by Royal Arch Research Assistance
24 Research Spotlight On: Litao Tao, Ph.D. 26 Managing Hearing Loss Not Everyone Qualifies for OTC Hearing Aids. Stephen O. Frazier and Hansapani Rodrigo, Ph.D. 30 Living With Hearing Loss Educate, Educate, and Advocate, Advocate. Pat Dobbs 32 Advocacy A Daily Practice. Sarah Kirwan 34 Research Presenting the 2023 First-Year Emerging Research Grants Scientists. 38 Progress Report Recent Research by Hearing Health Foundation Scientists, Explained.
Publisher Timothy Higdon, President & CEO, HHF
Editor Yishane Lee
Art Director Robin Kidder
Senior Editor Amy Gross
Staff Writers Pat Dobbs, Shari Eberts, Stephen O. Frazier, Kathi Mestayer
Advertising GLM: 212.929.1300 hello@glmcommunications.com
Editorial Committee
Judy R. Dubno, Ph.D. Christopher Geissler, Ph.D. Lisa Goodrich, Ph.D. Anil K. Lalwani, M.D.
Rebecca M. Lewis, Au.D., Ph.D., CCC-A Joscelyn R.K. Martin, Au.D. Kathleen Wallace, Au.D.
Board of Directors
Chair: Elizabeth Keithley, Ph.D. Sophia Boccard Robert Boucai Judy R. Dubno, Ph.D. Jason Frank, J.D. Jay Grushkin, J.D. Roger M. Harris Cary Kopczynski
Sponsored 44 Advertisement Tech Solutions. 45 Marketplace
Hearing Health Foundation (HHF) and Hearing Health magazine do not endorse any product or service shown as paid advertisements. While HHF makes every effort to publish accurate information, it is not responsible for the accuracy of information therein. See hhf.org/ad-policy.
Cover A teen living in the Midwest, Lily created a website about variants in the gene TMPRSS3 that cause congenital hearing loss, like her own, as her Girl Scout Gold Award project.
Scan or visit hhf.org/subscribe to receive a FREE subscription to this magazine.

Sharon Kujawa, Ph.D. Anil K. Lalwani, M.D. Paul E. Orlin
Robert V. Shannon, Ph.D. Nancy Young, M.D.
Hearing Health Foundation PO Box 1397, New York, NY 10018
Phone: 212 257.6140 TTY: 888.435.6104 Email: info@hhf.org Web: hhf.org
Hearing Health Foundation is a tax-exempt, charitable organization and is eligible to receive tax-deductible contributions under the IRS Code 501(c)(3). Federal Tax ID: 13-1882107
Hearing Health magazine (ISSN 2691-9044, print; ISSN 2691-9052, online) is published four times annually by Hearing Health Foundation. Copyright 2023, Hearing Health Foundation. All rights reserved. Articles may not be reproduced without written permission from Hearing Health Foundation. USPS/Automatable Poly
To learn more or to subscribe or unsubscribe, call 212.257.6140 (TTY: 888.435.6104) or email info@hhf.org.

The Gene TMPRSS3 and Me
A teen learns about the genetic cause of her hearing loss, and is spreading the word to find out more.
My name is Lily and I am 15 years old. When I was born, I was diagnosed with profound bilateral hearing loss. At 10 months of age, I became one of the youngest in my state to receive bilateral cochlear implants. My parents were curious about the cause of my hearing loss. One expert told them they would probably never know, but my parents were determined to find out.

After connecting with a scientist at Harvard, my parents learned that the cause of my hearing loss was a variant in the gene TMPRSS3 (transmembrane protease serine 3). At the time, it was difficult for them to understand the implications. Scientists, primarily in Europe, had undertaken only a few studies. As I’ve gotten older, I’ve become more interested in this subject and learned that while there’s been progress in the TMPRSS3 field, especially in the past few years, many of the same questions and challenges remain.
Having a hearing loss makes me interested in how the world works. Hearing with very complex computers—my cochlear implants—and participating in dozens of research studies from the time I was a baby, made me interested in science. I currently attend a science-focused high school and am learning about and doing research almost daily.
As a result of my passion for solving problems, my desire to help others, and needing to find the perfect project for my Girl Scout Gold Award (the highest honor for a Girl Scout), I created TMPRSS3.org. This website is the first and only of its kind, a comprehensive, easy-tounderstand source for anyone who wants to know more about the TMPRSS3 gene and its related hearing loss.
By drawing more attention to TMPRSS3, I want to make it easier for individuals, families, universities,
hospitals, and cochlear implant clinics to research, grow the knowledge base, and create potential future treatments and discoveries about this gene. More research will ultimately benefit those impacted by this gene. The more we learn about TMPRSS3, the more we can help others.
There are more than 123 genes linked to hearing loss, and researchers in this space have a lot of competition for their attention. TMPRSS3 is the fifth most common gene causally associated with deafness. Variants of the TMPRSS3 gene are the most common causative hearing loss genes in adults undergoing traditional and hybrid cochlear implantation.
TMPRSS3 is a complex gene, and can manifest differently in each person. The pathogenic variants in TMPRSS3 at the DFNB8 locus typically cause a postlingual (after speech) high-frequency/sloping hearing loss, with a slow deterioration of remaining hearing. In contrast, the TMPRSS3 DFNB10 variant is congenital, a prelingual (before speech) profound hearing loss at birth.
Aggregating Resources
The website TMPRSS3.org includes:
» Clear, understandable information about TMPRSS3 and DFNB8/10
» Database of 96 TMPRSS3 research studies (dating back to 1996)
» Trends analysis
» Key TMPRSS3 researchers (both past and present) and links to their labs
» Genetic testing information
» Opportunities for individuals to get involved with leading-edge TMPRSS3 research
At 10 months of age, Lily was one of the youngest in her state to receive bilateral cochlear implants. Her congenital hearing loss, the result of a variant in the gene TMPRSS3, led her to create a website about the gene that is her Girl Scout Gold Award project.


I’m thankful for my advisers and collaborators who continue to help me develop TMPRSS3.org and make it the best it can be. I’ve been encouraged by all the ear scientists, ENTs, Ph.D.s, and clinical experts who have been so kind with their time and mentoring. You never know the impact of responding to emails from “a 15-year-old.”
Throughout my life and through this process of developing my Girl Scout Gold Award TMPRSS3 Resource, I have had to be a strong self-advocate. Making this site available to those who can benefit is extremely necessary and very important to me.
So I ask readers of this story to do a few things. Please share this essential TMPRSS3 resource far and wide, and if possible, link it to your website or share it on social media. I appreciate your interest in hearing loss and look forward to any collaborations in the future to advance the science surrounding the TMPRSS3 gene.
Lily lives in the Midwest with her family. For more, see TMPRSS3.org. Contact her at tmprss3@gmail.com, or through the “contact us” box on the bottom of the TMPRSS3.org homepage.
Xi Lin, Ph.D., a 2000–2002 Emerging Research Grants (ERG) scientist, coauthored a study listed on TMPRSS3.org. Applications for the 2023–2024 ERG grants cycle are due February 28. Learn more at hhf.org/how-to-apply.
Having a hearing loss makes me interested in how the world works. Hearing with very complex computers— my cochlear implants—and participating in dozens of research studies from the time I was a baby, made me interested in science. I currently attend a science-focused high school and am learning about and doing research almost daily.
Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
Daniel Fink, M.D., in front of the Swiss Alps. He says he recorded daytime sound pressure levels of 42 dBA in the Alps, with the noise coming from the wind and distant road traffic noise, and nighttime levels of 30 dBA. A-weighted decibels, or dBA, emphasize the frequencies heard in human speech.

Science Is Just the Start
My path to outreach, advocacy, and activism around too much noise, and the successes—and ongoing challenges—so far. By Daniel
Fink, M.D.I’m a retired internist and have always tried to live a healthy lifestyle, but I had no idea that a one-time noise exposure could cause auditory symptoms for the rest of my life. Unfortunately, that’s exactly what happened to me at a New Year’s Eve dinner in Los Angeles, where I live, in 2007. As midnight approached, the restaurant kept turning the music up.
My wife could tell I was uncomfortable and suggested that we leave, but I didn’t want to offend our friends. When we finally left, my ears were ringing (that’s called tinnitus) and I later found that everyday sounds that didn’t bother others were actually painful for me (that’s called hyperacusis).
I wish I could say that I suffered in silence, but the world is too noisy for that. I became reluctant to go to restaurants. I started using earplugs at movies and sports events. I asked my wife, “Am I becoming grumpier as I get older?” and she immediately responded, “It’s too late for that, dear!”
In December 2014 I read an article about hyperacusis in The New York Times. I circled it in red and showed it to my wife, saying, “This is why I don’t want to go to restaurants anymore. They are all too noisy and it hurts my ears.”
I had recently left the board of a local environmental nonprofit, after my term concluded, so I had some extra time and energy and decided to see what I could do to make the world a quieter place.
First, I had to learn about the adverse effects of noise. This wasn’t something I had
learned in medical school or during residency training. Fortunately, the world’s scientific literature is now available to anyone with a device, internet connection, and search engine.
When I read that noise not only caused hearing loss, tinnitus, and hyperacusis, but also had non-auditory health effects, I knew I had to do something.
What could I do? Just knowing the science was not enough. I had to engage in outreach, advocacy, and activism. Outreach is letting people know important information. Advocacy is the act or process of supporting a cause. Activism is direct action in support of or in opposition to one side of an issue.
My activism is admittedly atypical. Instead of speaking at public meetings, writing letters and emails, organizing a petition, or getting neighbors to put up lawn signs, I focused on learning the facts about noise and then bringing those facts to the attention of those able to change public policy. I realized I needed to flip the typical activist mantra of “think globally, act locally” on its head, thinking locally but acting globally.
Policy change has to come from the top. I wanted to easily find a quiet restaurant in which to enjoy both a meal and conversation with my wife. I started with a presentation to my local health and safety commission about restaurant noise in January 2015, but quickly learned that it would be difficult to change people’s minds about noise when 85 decibels (dB) was regarded as the safe noise level.
The National Institute on Deafness and Other Communication Disorders’ (NIDCD) webpage on noiseinduced hearing loss stated, “Know which sounds are dangerous (those at or above 85 decibels).” Plus, I could see it would be difficult to convince people that I wasn’t just a chronic complainer when the Acoustical Society of America and the America National Standards Institute define noise as “unwanted sound.”
I needed to change the nature of the conversation. I found a long-forgotten 1974 Environmental Protection Agency report online providing the only evidence-based safe noise level to prevent hearing loss as “70 dB timeweighted average” for 24 hours. In other words, our average exposure over the course of a day should be limited to 70 dB.
I realized what had happened: The NIDCD was citing the recommended occupational noise exposure level as the sound pressure level at which auditory damage begins. But the recommended occupational noise exposure level doesn’t fully prevent hearing loss in exposed workers, and it certainly isn’t safe for the public.
I found a long-forgotten 1974 Environmental Protection Agency report online providing the only evidence-based safe noise level to prevent hearing loss as “70 dB time-weighted average” for 24 hours. In other words, our average exposure over the course of a day should be limited to 70 dB.
In 2015 I was among those who brought to the CDC’s attention the fact that noise caused hearing loss in the general public, not just among workers in the workplace. (It’s also worth noting that noise exposure for the public occurs 24 hours a day and seven days a week, not just eight hours daily on weekdays at the workplace.) That led to the CDC embarking on both research and public health education about the dangers of non-occupational noise exposure.
Also in 2015, I was elected to the board of the American Tinnitus Association. I was no longer a lone-wolf activist.

In 2016, some of my noise colleagues and I started The Quiet Coalition, under the auspices of the existing nonprofit Quiet Communities Inc. (QCi), to focus specifically on making the world a quieter place.
That year I also submitted an abstract about the safe noise level to the Institute for Noise Control Engineering. To my surprise, the abstract was accepted for presentation. I submitted a manuscript based on my talk to the American Journal of Public Health (AJPH). Again to my surprise, the editor told me that if I rewrote it as an editorial, it would be published.
The AJPH editorial appeared online in December 2016, and it has now been cited 72 times in peer-reviewed scientific and medical literature. It led to an invitation to serve as an expert consultant to the World Health Organization for its Make Listening Safe program.
In 2019 I submitted an abstract to the Acoustical Society of America (ASA) about a new definition of noise—“noise is unwanted and/or harmful sound”—with the crucial addition of “harmful.” I presented the new definition and then published it. The definition hasn’t made it to the dictionary yet, but it was the first sentence of the January 2022 American Public Health Association policy statement, “Noise as a Public Health Hazard.”
I once saw a presentation by Paul Farmer, M.D., Ph.D., whom The New York Times termed “a pioneer of public health” in his February 2022 obituary. He asked the audience, “Can one person make a difference?” He cited Mahatma Gandhi, Nelson Mandela, and Martin Luther King Jr. Farmer certainly made a difference, with his efforts to improve global health for the poor. More recently, so did climate change activist and Swedish teen Greta Thunberg.
I’m definitely not in that league, and I want to emphasize that I didn’t work alone, but always had support and advice from a small group of colleagues. The late Bryan Pollard of Hyperacusis Research introduced me to QCi founder Jamie Banks, who in turn introduced me to David Sykes, whose suggestions and encouragement led to presentations at national and international noise meetings. Gina Briggs finds items to write about, and posts almost daily blog posts, many of which have been written by pioneering noise researcher Arline Bronzaft. (All of us are now part of QCi.) Noise experts around the world have generously shared their expertise with me, and told me when I was wrong.
I Count These as Successes
» The CDC recognized non-occupational noise exposure caused hearing loss in the public.
» The NIDCD removed language from its webpage on noise-induced hearing loss that implied that auditory damage began at 85 dB.
» The CDC now states (as of 2019): “Noise above 70 dB over a prolonged period of time may start to damage your hearing.”
» The International Telecommunications Union included recommendations for lower noise exposure levels for children and other sensitive users in its Guidelines for Safe Listening Devices/Systems.
» A question about screening for hearing loss in middle-aged and older adults was referred to the U.S. Preventive Services Task Force, which reconsidered its recommendation even if the literature still didn’t support screening.
» The U.K. Advertising Standards Authority took action against Amazon for falsely advertising that headphones with an 85 dB volume limit were safe for toddlers and children.
» And now googling the term “safe noise level” gives results that say 70 dB is the safe limit, often mentioning my 2017 editorial, instead of the occupational limit of 85 dB.
But So Far These Remain Failures
» Restaurants are still too noisy. Gas-powered leaf blowers are still used in my city, despite an ordinance banning their use.
» Despite my efforts, the Federal Trade Commission hasn’t taken enforcement action against the vendors of the 85 dB headphones; and the Consumer Product Safety Commission hasn’t put warning stickers reading “This product may cause hearing loss” on personal listening devices.
» Movies and sports events are still too loud. So are weddings and birthday parties. The world remains noisy.
Quiet Activism
I’m not giving up. As I write this, I am also preparing for the December meeting of the ASA in Nashville, where I will be presenting three papers.
I will next submit manuscripts to the ASA’s journal, Proceedings of Meetings on Acoustics. A publication lends greater credibility to what I have to say, and then I can send that link around in future emails to policy makers, government representatives, and other activists.
How will I measure success? When the world becomes a quieter place.
As intermediate steps, I’d like to see 1) the Surgeon General issue a Call to Action to Prevent Noise-Induced Hearing Loss, just like the Call to Action to Prevent Skin Cancer, and 2) the HealthyChildren.org website run by the American Academy of Pediatrics share as much advice for parents about noise and the ear as it does about sun and the skin.
Please join us to make the world quieter, and to make it a better place for those with auditory disorders like hearing loss, tinnitus, or hyperacusis. I encourage you to use your talents and contacts to advocate for quieter spaces. As noise activists—or is it quiet activists?—we really can make a difference.
Daniel Fink, M.D., is the founding chair of The Quiet Coalition, the interim chair of Quiet Communities Inc.’s Health Advisory Council, and a former board member of the American Tinnitus Association. He serves as an expert consultant to the World Health Organization on its Make Listening Safe Program, and as a subject matter expert on noise and the public to the National Center for Environmental Health at the Centers for Disease Control and Prevention. This is based on his presentation at the 13th Congress (e-Congress) of the International Commission on Biological Effects of Noise in June 2021. For references, see hhf.org/winter2023-references.
Share your story: Have you advocated for quiet? Tell us at editor@hhf.org.
Support our research: hhf.org/donate.
If I Were the Minister of Hearing Health
By Shari EbertsI am a huge Harry Potter fan so when someone asked me, “What would you do if you were the Minister of Hearing Health?” my head immediately filled with images of wands and other wizardly gear. Could I simply flick my wand and make hearing loss disappear, I wondered?
Okay, back to reality.
Hearing loss makes communication difficult, and communication is the glue that binds us to the people and activities we love. Healthy hearing helps us stay connected to the things that matter to us. When people at all stages of the hearing journey—even those with typical hearing— accept this link, we will see real change.
My Healthy Hearing Priorities
1. Link healthy hearing to overall health. Hearing loss is associated with many health problems including depression, a higher risk of falls, diabetes, and cardiovascular disease. Hearing loss is also one of the largest modifiable risk factors for developing dementia. Making this information more widely known is key.
2. Beef up accessibility measures. According to the World Health Organization, 430 million people worldwide have disabling hearing loss, and this number is expected to jump to 700 million by 2050, affecting 10 percent of the population. Beefing up accessibility measures like captioning and assistive listening technologies in public spaces, entertainment venues, and online will help keep this growing population engaged.
3. Incorporate hearing into routine medical care. Why don’t doctors regularly screen for hearing loss? Perhaps they don’t understand the linkages to overall health, or perhaps they are not reimbursed for doing so. Insurance plans and medical school training must be modified to put hearing care center stage. We must also learn to understand our role in receiving proper hearing care.
4. Make hearing devices of all types affordable. Hearing aids are expensive. So are cochlear implants, but at least in the United States, implants are usually covered by insurance. New over-the-counter hearing aids for adults with mild to moderate hearing loss will help improve access, but overall affordability is lacking. We must
expand national health and private insurance plans so they include not only regular hearing tests, but also devices and aural rehabilitation services.
5. Promote hearing loss prevention. Scientists cannot yet repair damaged hearing, so we must protect it. Health curricula for students of all ages must teach how and why to protect hearing. Making the use of hearing protection cool would save millions from the challenges of hearing loss. As would better enforcement of noise protection laws.
6. Support research into treatments and cures. The more scientists learn about how hearing works (and doesn’t work), the more success they will have in developing new cures and better ways to prevent hearing loss. Governments must allocate more funds to support this work.

If I were a fantasy Minister of Hearing Health, this is what I would hope to achieve. As a real-life healthy hearing advocate, I’m already spreading the word.
Staff writer Shari Eberts serves on the Hearing Loss Association of America’s Board of Directors and is a past chair of HHF’s Board of Directors. This is adapted from her blog at livingwithhearingloss.com. Eberts and Gael Hannan, coauthors of the book “Hear & Beyond,” discuss the topic of this column on the Habits & Health podcast, at tonywinyard.com/shari-eberts-gael-hannan. For references, see hhf.org/winter2023-references.
Share your story: What would you do as Minister of Hearing Health? Tell us at editor@hhf.org.
Support our research: hhf.org/donate.
What Social Media Can Teach Audiologists
By Kathleen Wallace, Au.D.Audiologists are a tiny, but mighty, profession consisting of only 13,000 professionals to service the third most common chronic condition in the United States (hearing loss), the most common service related disability (tinnitus), the leading cause of visits to the emergency rooms (falls), and the condition for which one billion people worldwide are at risk (noise-induced hearing loss). Yet, most people don’t know what an audiologist is and pay little attention to their own ears.
When I meet new people and get asked what I do, my answer is often met with blank stares. On the occasions when someone does know what an audiologist is, it is typically a game of word associations: audiologist with hearing aid and old people or perhaps nurse with hearing screening and elementary school
This, however, doesn’t come as a surprise. Audiologists have long struggled with promoting the profession both within healthcare and among the general public.
But what tends to happen next is where things really get interesting. Once people know I’m an audiologist, friends, family, and strangers come out of the woodwork with ear questions. I have been asked about earwax at funerals, my thoughts on over-the-counter hearing aids at weddings, hearing protection at baptisms, and vertigo at birthday parties. It turns out people are actually quite curious about their ears! They just never knew who to ask.
With this insight, I took to social media to gauge the appetite for people to learn more about their ears. I decided that I’d turn the countless questions I’ve gotten in real life into short, digestible, educational videos where I answer them as if I just met you at a party. On social media as @EarDocOfTikTok, I’ve garnered millions of views, tens of thousands of comments, and thousands of followers. The comments section is (mostly) filled with more ear questions or topic requests, ranging from fairly simple
inquiries like how to pronounce tinnitus to more complex topics like why accents are so difficult to understand.
Here are a few insights I’ve gained from TikTok: » Social media challenges you to deliver your message as succinctly and clearly as possible, and to do so in an engaging manner. It has been excellent practice for counseling patients and figuring out how to boil down years of study and clinical experience into salient points.

» It has been the best market research possible, giving a pulse on how people are thinking about their ears, audiologists, areas of interest, and service delivery methods. There are a lot of opportunities for audiologists to evolve if we’re willing to listen to what our patients truly want.
» People want the guidance of a professional, but many don’t know how to get to one. Our knowledge base is more sought after than many may realize; we just aren’t reaching them in the right way. Audiologists have to continue public outreach and engagement.
My hope is these videos will help close the gap between audiologists and the public and pull the veil back on the often convoluted hearing healthcare space. By putting education and awareness at the forefront, audiologists can build the trust needed to evolve this profession and better serve our patients. All we have to do, ironically, is listen.
Find Hearing Health editorial committee member
Kathleen Wallace, Au.D., at @EarDocOfTikTok in TikTok, @drkathleenwallace on Instagram, via TunedCare at tunedcare.com, and at her practice in New York City. For more, see kathleenwallaceaud.com.
Matthew Masapollo, Ph.D., works to support, mentor, and encourage those who are perpetually underrepresented in speech science because of a lack of resources and opportunities.

As part of his research, he uses the University of Florida Gator (opposite page) to help explain speech motor control.
Speaking Through Color
The ongoing effort to train students of diverse backgrounds in speech communication and engineering research.
By Matthew Masapollo, Ph.D.Higher education has multiple missions and purposes. At a public research university like the University of Florida (UF), my home institution, producing knowledge and preparing students for careers in the years that follow is the primary objective.
A secondary objective of that education is to elevate students and prepare them for achievement and fulfillment in a wider context, as they become professionals and community leaders within the broader society. Achieving these objectives entails creating and maintaining academic environments in which the differences among people enhance rather than detract from what we are able to learn and accomplish together.
Yet, while living with difference is a ubiquitous reality today, diversity remains a central challenge. As a faculty member in the department of speech, language, and hearing sciences at UF, diversity and fairness are of great concern in my own endeavors. My laboratory, which is engaged in basic and clinical research on sensorimotor mechanisms in speech motor control, is both multicultural and multidisciplinary.
The lab draws together talented, promising students from across the UF campus to combine the latest technology, principles, and tools from
engineering and computer science with speech and hearing science to facilitate advancements in our understanding of impaired speech communication. Our ongoing Hearing Health Foundation–funded work, in collaboration with Susan Nittrouer, Ph.D., is examining speech articulation in congenitally deaf individuals who receive cochlear implants. This diversity of perspective has undoubtedly been critical to our ability to innovate and conduct high-risk/high-payoff research on auditorily guided motor control.
Unfortunately, though, our field as a whole is woefully lacking in diversity—over 90 percent of speech-language pathologists are white, and only 4 percent are Black, according to the American Speech-Language-Hearing Association’s membership data. Even fewer make it to scientific prominence in the field. Large disparities also exist between how individuals who are racial minorities receive speech therapy compared with white individuals.

Each of us must rigorously examine our own actions, motivations, and commitment to ensure that higher education and our profession become increasingly diverse and inclusive. Toward that end, I am constantly thinking of ways to remediate this problem and take affirmative steps to support, mentor, and encourage those who are perpetually underrepresented in speech and engineering science because of a lack of resources and opportunities to pursue an education in STEM (science, technology, engineering, and mathematics).
I actively incorporate first generation undergraduate
students of color into my research projects and engage them in the processes of creativity and innovation. Jessica Goel is a class of 2023 biomedical engineering major and the director of industry relations for the UF Society of Women Engineers. She is carrying out original research alongside me to develop optimal methods to dynamically image laryngeal (glottal) and supra-laryngeal vocal tract (lip, tongue, and jaw) structures during speech production. We are imaging individuals with congenital auditory deficits as well as peers with typical hearing using state-of-the-art electromagnetic articulography (EMA) and electroglottography.
Undergraduates who receive training in engineering and speech motor control typically have sparse access to, and gain little expertise with, these types of measurement tools and clinical populations. But in our lab, first generation undergraduates like Jessica have the opportunity to conduct world-class, mentored, hands-on research, and contribute meaningfully to the creation of new knowledge. Jessica has already co-authored several peer-reviewed journal articles—including one that made the October 2021 cover of JASA (Journal of the Acoustical Society of America) Express Letters—and presented her work at local and national meetings, which has helped her begin building a professional network.
This set of experiences has helped to set Jessica on an early path toward science. She plans to pursue a Ph.D. in biomedical engineering, with a focus on imaging and medical devices.
While living with difference is a ubiquitous reality today, diversity remains a central challenge. As a faculty member in the department of speech, language, and hearing sciences at the University of Florida, diversity and fairness are of great concern in my own endeavors. My laboratory, which is engaged in basic as well as clinical research, is both multicultural and multidisciplinary.
Recruiting undergraduate lab assistants at an annual campus research expo is an opportunity to meet with and encourage underrepresented students to consider a career in science— which many of them cannot yet imagine for themselves.


Opposite page: Masapollo is training undergraduates like Jessica Goel to conduct world-class, mentored, hands-on research and contribute meaningfully to the creation of new knowledge.
Many other undergraduates like Jessica who come from a wide range of disciplines—including linguistics; psychology; speech, language, and hearing sciences; computer science; and neuroscience—yearn to be future communication scientists and clinicians. As a result they are working with me on various research projects and manuscripts, such as through independent studies or thesis projects, that provide them with an exciting window into something that they want to do.
For example, Siddhi Kondapalli is a class of 2024 applied physiology and kinesiology major, and Ana Rodriguez is a class of 2024 speech, language, and hearing sciences major who recently received the Robert W. Young Award for Undergraduate Research in Acoustics from the Acoustical Society of America. They are each working on thesis projects using EMA to determine how the lips, tongue, jaw, and glottis work together to produce smooth and coordinated movements during skilled speech production. Aleena Alex, a class of 2025 biomedical engineering major, is exploring the role of auditory feedback in spatiotemporal coordination of speech movements in the context of an independent study project.
Cultivating a diverse and energetic lab group is a constant challenge, especially in a state like Florida which banned the use of affirmative action in undergraduate admissions. To keep the lab diverse, I utilize several recruitment and retention strategies. UF hosts an annual research expo where I am able to meet with and encourage underrepresented students to consider a career in science, which many of them cannot yet imagine for themselves. Recruitment efforts for underrepresented groups also include outreach to campus organizations, such as the Society of Women Engineers, that serve STEM education for minorities nationally.
Prospective students are also encouraged to tour the lab, attend my weekly lab meetings, and observe experimental sessions to help gauge if research might be their chosen path. Once a student commits to a research project, I am proactive in ensuring that they receive strong support as they move through their training program, and encourage them to view themselves as a young
Prospective students are encouraged to tour the lab, attend my weekly lab meetings, and observe experimental sessions to help gauge if research might be their chosen path. Once a student commits to a research project, I am proactive in ensuring that they receive strong support as they move through their training program, and encourage them to view themselves as a young colleague actively participating in the process of knowledge creation. At some point during their training, most students will experience moments where they falter, become discouraged, or think the hard work of conducting rigorous science is not worth it, and we must be in a position to support them when they need us.
colleague actively participating in the process of knowledge creation. At some point during their training, most students will experience moments where they falter, become discouraged, or think the hard work of conducting rigorous science is not worth it, and we must be in a position to support them when they need us.
Collaboration between students and faculty on research projects is especially important for underrepresented students. In science it’s so critical to have role models and peers for these groups and other people who look like you and are like you. I experienced this firsthand. As a gay man, I very much remember wanting to see more individuals with a similar identity as mine captured and represented in the scientific arena.
While I was an undergraduate at the University of Michigan in Ann Arbor, one of my faculty mentors was also gay. At that point, I had never met an “out” gay scientist before. Just being able to talk about data and theories with him made me feel like I had a place in the scientific community. Our conversations meant an awful lot to me, and I hope to be able to call on so many things that I learned from him as I continue to mentor my own students.
The bottom line is that a strong and empowering education can overturn notions of inferiority and inadequacy, and that is why we must not be silent in higher education but rather “speak through color” and persist in our struggle to foster the representation of minorities in our classrooms, clinics, and laboratories.
A 2022–2023 Emerging Research Grants scientist, Matthew Masapollo, Ph.D., is the director and principal investigator of the University of Florida’s Speech Communication Laboratory.

Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
Humming Again
A professor of literature chronicles her hearing loss journey through her personal and professional spheres.
 By Roberta Rubenstein Larson
By Roberta Rubenstein Larson
When did I first recognize that I might be losing my hearing? Perhaps it was when I became quite ill while in college and was hospitalized for a week with a severe case of mononucleosis complicated by strep throat. Among the treatments I received was streptomycin, an antibiotic that was successful for treating strep throat, tuberculosis, and other infections, but was later discovered to be ototoxic, causing irreversible damage to cochlear hair cells and the onset of permanent hearing loss in some patients. However, I knew nothing about these potential side effects at the time.
Several years later, signs of my hearing loss began to be visible—or, I should say, audible. During my early 20s, while I was visiting vacationing family members at a lake in Maine, someone commented on the haunting cries of loons calling to one another. What loons? I could not hear these unique water birds’ melancholy songs, which range over many frequencies, including high pitched notes—the same upper frequencies at which many human hearing losses are first discovered during audiological exams.
Not too long after I became aware of my hearing loss, I awoke in fright one morning. Every sound was significantly distorted, as if it had been drastically remixed inside a noisy tunnel. I immediately contacted an otolaryngologist, who diagnosed the condition as sudden sensorineural hearing loss (SSHL).
Though the cause of this audiological crisis is—like that of most hearing losses—unknown, the doctor mentioned that it may be triggered by common conditions like earwax or viruses, or more serious conditions such as head injury, side effects of certain medications, or autoimmune reactions. It may also be triggered as a reaction to sulfites used in the production of wine, which I speculated was my case, from a party the previous evening. Though treatment with steroid medication restored some but not all of my lost hearing, for decades afterward I avoided red wine entirely, regarding it as the cause of an allergic reaction I hoped never to experience again.
A Progressive Loss
During the early years of my career as a professor of literature at American University in Washington, D.C., my hearing loss inexplicably progressed. I struggled to maintain auditory competence in the classroom, boosting the hearing in my better ear through a series of increasingly powerful hearing aids. My poorer ear could not be aided because the interval between barely audible and painfully loud sounds was too small.
I dreaded the annual audiological exam. Sitting in the soundproof cubicle, I concentrated intensely on raw tones delivered at different frequencies and volumes or strained to repeat words and phrases spoken by a recorded voice. Each audiogram confirmed the downward slope of the graph as my hearing loss progressed from moderate to severe to profound.
As a professor in midcareer whose teaching directly depended on the spontaneity of class discussions rather than prepared lectures, I began to suffer from depression. I faced the prospect of early retirement from a profession I loved. Having received positive student feedback and several teaching awards, I knew I was an effective teacher—except for the challenges to comprehension posed by students who mumbled, spoke softly, or commented with a hand over their mouth.
The loss of hearing is a profoundly emotional occurrence. It is disheartening to miss key portions of dialogue in ordinary conversations, telephone chats, film voiceovers, theater performances, and virtually every other aural context. It is demeaning to be perceived as cognitively impaired when one simply asks for directions and misses crucial details in the answer.
During the peak years of the Covid pandemic, face masks made (and still make) life much more difficult for people with hearing loss. While protecting the wearer, a mask muffles speech and removes the possibility of
reading lips. Missed words particularly affect the aural rhythms of jokes, which typically depend on wordplay and a rapid reversal of listeners’ expectations. Just when one anticipates the emotional payoff that elicits laughter, the volume of the speaker’s voice drops with the punchline. We miss the joke.
In response to my diminishing hearing aptitude, I learned over time to employ two coping mechanisms. First, I spontaneously learned to read lips; second, in concentrating to comprehend speech as fully as I could, I became a very attentive listener—a valuable skill for a professor. To improve my lipreading proficiency, I took several classes offered by a woman who, when she was only 21 years old, had suddenly lost all hearing due to a severe viral infection and had become a skilled speech reader and teacher.
Ready for Implants
At this point, during my 50s, my audiologist informed me that I was profoundly deaf in both ears and recommended that I consider getting a cochlear implant (CI). With some trepidation, I proceeded to do so, receiving the first of two implants in 2000. This remarkable surgically implanted device functions by transforming sounds received by a speech processor into digital information, bypassing the damaged hair cells in the cochlea to stimulate the auditory nerve directly.
My doctor was John Niparko, M.D., the distinguished otolaryngologist and ear surgeon at Johns Hopkins University Hospital, who died at age 61 in 2016. He concurred with my preference to have the implant in my poorer ear. Since I simply could not imagine actually hearing via digitally processed sounds, I reasoned that I had less to lose if I received the implant in the unremediated ear that had not apprehended meaningful sounds for years. Though otolaryngologists have disagreed on whether implantation in the better or poorer ear in patients is the more successful strategy, clinical research has demonstrated that the difference in outcomes is inconsequential.
Fifteen years later, I received a second implant, in my once “better” ear. The speech processor, whose components were produced by Advanced Bionics (also the maker of my first processor), featured many enhancements, including rechargeable batteries that last 18 hours rather than just four hours on a single charge. But, disappointingly, it was less successful than the first one.
Because of technical advancements during the 15-year interval between my two implants, the two processors
were essentially incompatible. For the first six months after the newer device was implanted, I experienced the audiological equivalent of double vision as my brain tried to reconcile two dissimilar sound streams. Although the separate sound streams eventually merged into one, my brain continues to rely primarily on the older implant.
Outpatient CI surgery is followed by a six-week recovery period while the surgical site heals. Before my first implant was activated, I wrote in the journal I kept of this unparalleled experience:
“I’m looking forward to this adventure, as my brain learns to make sense of sounds I haven’t heard for years. I hope that in due course I’ll be able to hear without always having to see the speaker, use a phone, hear in the dark, and—maybe—enjoy classical music again. I also hope that, when I don’t have to struggle so hard to hear, I’ll relax more in my life.”
Then: The CI audiologist “turned on” the device and… I heard sounds! The problem was, I could make no sense of them. (I had been told to expect this first stage.) When my husband drove us home on activation day, I heard something coming from the car radio but had no idea whether it was speech or music.
Sound recognition and speech comprehension do not arrive instantaneously, like turning on the tap for water. Rather, new CI recipients are assisted by specially trained CI audiologists, who fine-tune (“map”) digital settings in the external processor to align with the recipient’s sound comprehension profile, and by speech therapists, who help them recognize letters and words amid a garbled stream of sound. Over time, CI recipients retrain their brains to make sense of sounds that were initially incomprehensible.
There were so many new sounds, especially environmental ones, to identify. Before my implant, I hadn’t realized that for many years I had not heard birds singing in my garden. Once I began to hear them, I recalled the unheard loon calls years earlier that were the first evidence of my hearing loss and cried with joy at these newly audible dimensions of my environment.
Initially, hearing many sounds that I did not recognize, I would ask my husband or children, “What was that?” Random sounds, such as the blip a decoding device makes as it registers the barcode on groceries, were entirely new to me. I was surprised to discover that the wood floors in my house squeaked and that the refrigerator, dishwasher, and other appliances hummed. I began to hum myself.
As I became more proficient in interpreting sounds and speech, I realized that the learning process undertaken
by new CI recipients is analogous to the way infants learn language, beginning when they first recognize their own name and advancing as repeated words emerge from a bewildering stream of noise. This process of comprehension is the essential developmental stage that commences long before babies speak their own first words. It was thrilling for me to be immersed in this process the second time around, this time as an adult who could observe while experiencing what was happening not in my ear but in my brain. When I attended my first child’s college graduation a year after my implant, I was elated to understand almost every word spoken, not only by my daughter and her friends and professors but also by the commencement speaker that year, Toni Morrison.
Hearing Gains
Placing my experience of hearing losses in context, I— like so many other people with hearing loss—am also the recipient of numerous hearing gains. We are fortunate beneficiaries of a technological revolution, including not only cochlear implants but also increasingly sophisticated hearing aids as well as assistive devices, apps in theaters and cinemas, and mobile phones. Increasingly, we can access captions on computers, television, and phones as well as in many live theaters and cinemas.
Most of these accommodations are the result of the Americans with Disabilities Act, the 1990 civil rights law that “[prohibits] discrimination against individuals with disabilities in all areas of public life….” For the most part, people with hearing loss have gained entrance to a kindlier environment that has liberated us from the woefully silent, lonely world that those before us have experienced for most of history.
I feel exceptionally fortunate. My hearing journey has ultimately been a positive one, both personally and professionally. Although I once dreaded involuntary early retirement, necessitated by my profound hearing loss, instead I continued to teach for the next 25 years. After 51 deeply gratifying years in the classroom, just three years ago, in May 2020, I retired from American University as Professor Emerita of Literature.
Roberta Rubenstein Larson lives in Chevy Chase, Maryland. For references, see hhf.org/winter2023-references.
Support our research: hhf.org/donate.
My Misophonia Story
When I was 13 years old, I was diagnosed with misophonia. This is my story. By
Kadyn ThorpeMisophonia is a brain disorder. For those who have it, certain noises will send them into a fight or flight type of response. We call these noises triggers. My triggers include loud eating, plates and silverware clanking, crunching, whispering, and many more everyday sounds. When I hear these sounds, it’s not just an annoyance that overtakes me; it’s rage.
When I was 12 years old I could tell there was something wrong with me. I remember riding in the car with my papa and having this feeling take over my body when he would chew on ice. It was a mixed feeling—rage, irritation, anxiety, and confusion all in one. My body would start to shake, and I would feel pain hearing the sounds coming from his mouth. I would start to distract myself from the pain by scratching my arms and legs, digging my nails into my skin. I know now that this is a response to the misophonia pain, to create another source of pain to try to ignore it.
I went on like this for a year, listening to my friends and family eat with their mouths open, crunching on chips, and constantly hitting their plates with their forks while eating. I thought I was insane. I was too afraid to tell anyone. I couldn’t tell them that these noises put me in a feeling of anger and pain.
I started retreating to my room when dinner was ready, but that still didn’t help. All the triggers were amplified in my head. My family could be downstairs eating and I could be upstairs, in my room, door closed and television on, and still hear the sounds of forks hitting the plate and the crunching of food as they enjoyed their meal. It was torture.
I fought it till one day, while shopping with my mom. She was walking through the store chewing gum, smacking every second louder than an airhorn in my mind. I would start walking slower, trying to get away, because I didn’t know how else to deal with it. She got mad and I couldn’t hold it in anymore. She thought I was crazy, and hearing it said out loud, I couldn’t even believe myself. What person is so sensitive that they can’t deal with everyday sounds?
After that day, I finally decided to look up my symptoms and try to find answers. I know, I know, you shouldn’t google your symptoms, but I was desperate. I found a brain disorder called misophonia, which described exactly how I was feeling, so I shared it with my mom. After that we decided we should go to the doctor to figure out what exactly was happening to me.
An Early Misdiagnosis
We made an appointment with the doctor, and when the day finally came I was so excited. I wanted someone to tell me I wasn’t crazy and the feelings I had were valid. That did not happen.
When I started to explain to my doctor what was happening, he said I did not have misophonia (keep in mind, he had never heard of it before), but rather it was my hormones that were out of whack. I was starting puberty, and that seemed like the safe answer. Not wanting to accept that I had a brain disorder, I
A recent graduate in marketing and communications, Kadyn Thorpe is sharing her story so others can understand what misophonia is.

agreed with him. In order to “normalize” my hormones, my doctor put me on the pill. Yes, the birth control pill. I was 12.
As many people know, birth control messes with your hormones, especially when you keep changing it, and we did. Every three or so months, I changed my birth control. I would change it, be off it for a couple of months, and then back on another one. I was young, so I didn’t know taking the pill at the same time every day made a difference. I would forget one night and take it in the morning, I would skip days on end because I just didn’t care enough to continue it.
It messed with my emotions, I was depressed to the point where I didn’t want to get out of bed, I lost all my interest and hated everything. I fought so hard to go back to being the person I was before, the happy-go-lucky girl I used to be, but I couldn’t. And they just kept me on the pill, changing it every time I had an issue. My emotions got worse and my reactions to triggers stayed the same.
Once my family understood, minimally, what was happening to me they tried so hard to stop smacking their lips while they ate. We bought paper plates and plastic silverware to use during dinner time. They stopped eating salads, popcorn, chips, and other crunchy foods. They did everything right, but my triggers would surround me no matter what. At school, I would take a test in a silent room while the person next to me smacked on a piece of gum. Movie theaters were a nightmare—the crunch of the popcorn, the wrestling of the candy wrappers, the groups of people whispering. I refused to go.
These noises happen everywhere, and when you have misophonia, they are louder than normal. People can usually tune them out or they don’t even notice them. When you have misophonia it’s like these are the only sounds you hear, and once you hear them, you can’t drown them out until they stop.
A Diagnosis
Finally, more than a year later, we found a doctor who understood what misophonia was. We got an appointment, but my expectations were low. I had been through so much with changing medications, my body changing, and my emotions at an all-time low, all while simultaneously trying to figure out what was happening to me every day.
When I went to see the doctor, they gave me a piece of paper and told me to answer the questions. The questions asked me about certain noises, rating them on how much they hurt to hear and how I felt when I heard them. They asked how I felt mentally and physically on a daily basis and how I decided to cope with the issues I had been having. Once I finished, the doctor reviewed it and pulled me into her office to talk to me. She told me that based on my answers, there was no question that I had misophonia.
Afterward, she decided to give me a hearing test. I sat in a room facing a wall with headphones on and a button in each hand. For 10 minutes they played clicks in my ears, and I had to push the button when I heard it.
When I finished they explained to me that I have near perfect hearing, which is the reason everything was amplified in my head. Misophonia is the brain disorder where noises send you into rage, and the people who have it have great hearing.
She started to explain misophonia to me. For the first time, I had someone who knew exactly what I was going through. The doctor sat me down and told me exactly what was happening to me. She told me that it was like the wires in my brain were crossed, so when I heard these sounds, which she called triggers, my brain took it as a threat, sending me into fight or flight mode.
“It’s similar to your brain’s response to hearing fingernails scraping down a chalkboard,” she explained.
Then came the bad news—the news that there is no cure and that there is no good way to help this; I just have to
These noises happen everywhere, and when you have misophonia, they are louder than normal. People can usually tune them out or they don’t even notice them. When you have misophonia it’s like these are the only sounds you hear, and once you hear them, you can’t drown them out until they stop.
live with it. Not to mention that this brain disorder causes people to develop depression and anxiety.
The next thing she said I remember perfectly. She told me how many people who have this disorder decide that it isn’t worth continuing, because they are having to deal with the fear of going anywhere, the fear that these emotions are going to take over your body simply because someone near you is just existing.
She told me, “I want you to know, your life is worth living, even if you think it’s too hard.” Those words have stuck with me since.
Living With Triggers
Although there are no cures for misophonia, there are ways that the noises can be limited. For me, it was hearing aids. These weren’t normal hearing aids—obviously I didn’t need noises to be louder; I needed them to be gone. These hearing aids played “white noise” in my ear, attempting to drown out my triggers, but it didn’t work. I could still hear. The triggers were quieter, yes, but not gone. Those emotions were still there, swallowing me whole.
As the years went by I figured out the places I couldn’t go to and stayed clear. I haven’t been to the movie theater in over five years. I tried a couple of times, but it always proved to be a bad idea. I would be begging for the movie to end so I could get out of there.
By no means did this ever get easier for me. I still have to muster up the courage to go to restaurants, stores, work even. Triggers surround me every day, and I have to act as if nothing is wrong.
I started keeping it more of a secret. I didn’t tell a lot of friends, and still to this day haven’t told many of my family members. I didn’t want to be treated differently. My family did everything they could to make me feel comfortable. But rather than me feeling loved and understood, I felt guilty. I didn’t want anyone to change their ways because I couldn’t
deal with the sound. Even though the emotions and my reactions to triggers were valid, I still felt that I shouldn’t be upset by this—that these noises are a part of life, and I should appreciate that I could even hear. But I didn’t.
It’s been almost 10 years since I was diagnosed, and although the emotions my triggers bring are still the same, I can try to control them because I’ve accepted that this is something that is a part of me. I can’t change it and it will never go away, but I can make it my story. I can share the obstacles I’ve had to jump through in order to come to terms with what having misophonia means.
I can share my story with people who feel the same way. I can share my story with doctors, who would otherwise think these reactions and emotions are because of changing hormones. I can help people who, just like me, wanted validation, and didn’t get it for far too long.
I wrote this so people can understand what it’s like figuring out misophonia. By no means do I believe that this is how everyone’s misophonia story goes, but this is mine. Being able to understand misophonia is the first step to understanding how to diagnose it. Although misophonia is not as prominent as other brain disorders, it’s still here. It’s still impacting lives every day not only for the people who have it, but their friends and family as well. It’s not puberty, it’s not out of whack hormones; it’s a brain disorder that needs to be addressed.
Kadyn Thorpe lives in Colorado.
The doctor started to explain misophonia to me. For the first time, I had someone who knew exactly what I was going through. She sat me down and told me exactly what was happening to me. She told me that it was like the wires in my brain were crossed, so when I heard these sounds, which she called triggers, my brain took it as a threat, sending me into fight or flight mode. “It’s similar to your brain’s response to hearing fingernails scraping down a chalkboard,” she explained.
Spotlight On: Litao Tao, Ph.D.

Hearing Health Foundation’s Hearing Restoration Project welcomed its newest member to the consortium in October 2022. Litao Tao, Ph.D., received his bachelor’s and master’s degrees at China’s Tsinghua University and his doctorate at University of Southern California, where he also did postdoctoral studies. An assistant professor in the department of biomedical sciences at Creighton University in Nebraska, Tao is part of the HRP’s Cross-Species Epigenetics working group.
What is your area of focus?
We are interested in the role of epigenetic repression (i.e., chromatin architecture and histone modifications to block gene expression) in the silencing of sensory hair cell programming in the supporting cells of the mammalian cochlea. We hypothesize that in mammals, the epigenetic silencing state of hair cell genes in supporting cells hampers reactivation of those genes and hence blocks the conversion of supporting cells to hair cells, one major hair cell regeneration mechanism found in non-mammalian animals. Investigation of the epigenetic regulatory mechanisms not only helps us understand the failure of sensory hair cell regeneration in humans, but also provides potential targets for us to manipulate the epigenetic status of genes to stimulate gene expression for hair cell regeneration toward hearing restoration.
How did you decide to get into scientific research?
Chinese Taoism teaches that every movement or change in the universe is dictated by certain rules ( ) and that people become powerful if they understand those rules. When I was a little kid, I was fascinated by Taoist stories, and I started to pay close attention to natural phenomena and wanted to understand the rules behind them. Expectedly and unexpectedly, I found myself interested in science and became a scientist instead of a Taoist.
Why hearing research?
The first time I saw the structure of the human cochlea, I was immediately drawn by the delicate structure and the beauty of sensory hair cells. On top of this, I had the good fortune to work with the late Dr. Neil Segil, who was a member of HHF’s Hearing Restoration Project. Dr. Segil welcomed me as a Ph.D. student and encouraged me to study hair cell death induced by aminoglycoside antibiotics. From these ototoxicity studies conducted in the supportive environment of the Segil lab, I developed a fondness for the science of the inner ear.
Tell us about the most exciting parts of your work. Compared with other tissues and organs, the cochlea presents unique challenges in order to be studied. This tiny organ is buried in a bony structure and contains a limited number of specialized cells. Implementing new techniques and designing novel experimental approaches to overcome these challenges is an ongoing journey in hearing research and an essential part of the job, without which many of our biggest questions would be difficult or impossible to address. The most exciting part of our work is seeing results generated successfully with these new techniques and approaches, regardless of whether they support or contradict our hypotheses.
Describe a typical day. After dropping my daughter off at school, I begin my workday catching up on email correspondence. Then I walk into the lab to greet my lab members, and if I don’t have a lecture to give, I’ll discuss experiments with them. Next, I spend an hour or two putting together lecture materials, analyzing new datasets, or preparing presentation slides. Lunch is usually followed by student presentations, journal club discussions, seminars featuring an invited speaker, or department meetings. I spend most of my time in the afternoon in various meetings and discussions with students, lab members, colleagues, and collaborators. After finishing up any paperwork, and reading and sending a few more emails, I say goodbye to the lab and head home. When it gets dark, I spend my evenings playing basketball or jogging for a little while, and then enjoy some reading or writing before bed.
Tell us about something you enjoy doing outside the lab. I like fishing. I used to go deep sea fishing or surf fishing once a week when I lived in Los Angeles, and now I am exploring the fun from lake fishing and river fishing in the Midwest. Staring at the float or pole tip quickly isolates me from the surrounding environment so that I can think about something without interruption from the world outside. Of course, the bites from fish always pull me back to the real world.
How has the collaborative approach helped your research?
The HRP’s collaborative effort from multiple groups working with a variety of species makes it possible to address this intriguing and important question: why the mammalian cochlea lost the capacity to regenerate sensory hair cells, while robust hair cell regeneration happens in non-mammalian animals.
What do you hope for the HRP over the next few years?
The HRP brings some of the greatest minds in auditory science together, supporting many diverse projects by encouraging collaboration and cooperation. This unique platform has greatly accelerated hearing research and played a significant role in advancing our knowledge of the inner ear. Over the next few years, I would like to see more resources allocated to projects geared toward the translational aspect of hearing research, with themes such as drug screening, gene delivery, and expression manipulation for potential therapeutic treatments. Of course, we cannot make this happen without the continued support from HHF and its generous donors.
Chinese Taoism teaches that every movement or change in the universe is dictated by certain rules and that people become powerful if they understand those rules.

Not Everyone Qualifies for OTC Hearing Aids
Relatively basic over-the-counter hearing aids, indicated for mild to moderate hearing loss among adults, may end up pushing features like directional hearing and telecoils into prescription hearing aids for more severe types of hearing loss.
By Stephen O. Frazier and Hansapani Rodrigo, Ph.D.The intent for the over-the-counter (OTC) hearing aids that made their debut in October 2022 was to serve the needs of adults with a mild to moderate hearing loss. The models range from the very basic to those having a variety of advanced features such as Bluetooth capability, directional mics, rechargeability, smartphone apps, and even telecoils. Consumer sales will make the final determination as to what attributes in hearing aids and their accessories are important to this subgroup of the nation’s nearly 29 million people the National Institute on Deafness and Other Communication Disorders says could benefit from being fitted (if they are not already) with hearing aids.
The Survey
Adults with a hearing loss greater than mild to moderate will still need to be fitted with prescription hearing aids to adequately address their condition. A 2021 survey holds insights into what features this group wishes to have in their hearing aids.
Nearly 15,000 hard of hearing participants who have varying degrees of hearing loss and all age groups participated in a 21-question survey, conducted by Vinaya Manchaiah, Ph.D., and colleagues, with the results published in the Journal of the American Academy of Audiology.
The responses to the survey were also used online in a different report by Abram Bailey, Au.D., and team on Hearing Tracker. Hansapani Rodrigo, Ph.D., an assistant professor in the School of Mathematical and Statistical Sciences at the University of Texas Rio Grande Valley,
Oppopsite page: Listed in order from top to bottom, these are the attributes that people with severe to profound hearing loss want in their hearing aids.
collaborated on the original study. She provided the statistics on the 4,027 survey participants who had a severe to profound hearing loss—that is, those who don’t qualify for OTC hearing aids—for this article.
The Results
According to the report in the Journal of the American Academy of Audiology, the four most common attributes identified as “extremely” or “very” important for the overall group—those with hearing loss that ranges from mild to moderate to severe to profound—were:
» improved ability to hear friends and family in noisy settings (88.3 percent)
» reliability (85.1 percent)
» improved ability to hear friends and family in quiet settings (75.3 percent)
» physical comfort (74.3 percent)
For the severe to profound (S/P) group, the top four attributes rated “extremely” or “very” important were:
» improved ability to hear friends and family in noisy settings (88.9 percent)
» reliability (85.8 percent)
» improved ability to hear friends and family in quiet settings (84.1 percent)
» improved hearing on mobile telephones (71.2 percent)
Not surprisingly, both the overall group and the S/P group rated ability to hear well in noisy settings as the
most important attribute desired in hearing aids. But the S/P group seems to have more difficulty hearing even in quiet settings compared with the overall group. Reliability was more important to the S/P group, as was being able to hear well on cell phones.

Streaming audio, whether from a mobile phone or TV, ranked higher in the minds of the S/P group than the full group and stood at 54.3 percent for mobile phone streaming (versus 48.5 percent for the full group) and 51.6 percent for TV streaming (versus 45.5 percent).
The S/P group was less concerned about the visibility of their hearing aids (33 percent) than was the full group at 44 percent.
As for the ability to recharge the devices, it was less important to the S/P group at 32 percent than to the full group who rated it at 39 percent. Surprisingly, in this increasingly technological and digital world, the ability to control hearing aid volume and settings using a smartwatch was almost equally unimportant to the two groups, with the S/P group at less than 12 percent and full group at 15 percent.
Of Loops and Microphones
Being an advocate for hearing loop technology, I was disappointed that just 27.9 percent of all respondents felt that the ability to receive audio broadcast by a hearing loop through their hearing aids was important. Among the S/P group, 35 percent indicated this often ignored technology is still an important capability—and I consider this group, because of their greater hearing loss, to be more hearing impacted and therefore more experienced hearing aid consumers.
It is also worth mentioning that telecoil-equipped hearing aids and a cell phone with a jack for a neck loop would help those who wish for the ability to better converse on cell phones.
Even my audiologist was not aware that many remote microphones now, in addition to streaming sound they “hear,” contain a telecoil. This means they have the capability to stream the sound from a hearing loop directly to hearing aids that don’t have telecoils using Bluetooth. Among the S/P group, 26 percent felt the availability of this kind of remote microphone was extremely or very
important, versus 21 percent of the overall group.
Another thing to point out is that since the ability to stream sound to hearing aids from a variety of sources was rated very important by so many respondents, streaming is almost a “must have” for hearing aid buyers. For the many hearing aid wearers whose devices do not contain telecoils, the advent of remote microphones such as Starkey’s Remote Microphone Plus can ensure improved communication access since these remote microphones can connect to hearing loops. The Oticon EduMic not only has a telecoil, it can also connect to the signal from an FM assistive listening system.
Questions Remain
OTC hearing aids may shrink the overall size of the client pool for prescription devices but have little or no impact on the group whose hearing loss is severe to profound, who will continue to need to purchase prescription hearing aids.

Will the price of prescription hearing aids go up to make up for income lost to OTC competition? Will other hearing aid makers join Starkey in developing an OTC hearing aid? Will the features the S/P group both want and need be discontinued in order to lower the price to compete with the new OTC kid on the block?
Will the burgeoning online sale of all types of hearing aids (OTC and prescription) result in less availability of inperson care from a local audiologist or hearing instrument specialist? Will more hearing care offices unbundle their services to treat online and OTC hearing aid buyers?
We’ll continue to monitor the hearing aid market and optimistically hope that the greater accessibility and affordability will benefit all.
Trained by the Hearing Loss Association of America as a hearing loss support specialist, staff writer and New Mexico resident Stephen O. Frazier (left) has served HLAA and others at the local, state, and national levels as a volunteer in their efforts to improve communication access for people with hearing loss. Contact him at hlaanm@juno.com. For more, see sofnabq.com and loopnm.com.
Hansapani Rodrigo, Ph.D., is an assistant professor at the School of Mathematical and Statistical Sciences, University of Texas Rio Grande Valley, in Edinburg, Texas.

For references, see hhf.org/winter2023-references.
Share your story: What is your top must-have in hearing aids? Tell us at editor@hhf.org.
Support our research: hhf.org/donate.
Being an advocate for hearing loop technology, I was disappointed that just 27.9 percent of all respondents felt that the ability to receive audio broadcast by a hearing loop through their hearing aids was important. Among those with severe to profound hearing loss, 35 percent indicated this often ignored technology is still an important capability—and I consider this group, because of their greater hearing loss, to be more hearing impacted and therefore more experienced hearing aid consumers.




Educate, Educate, and Advocate, Advocate
By Pat DobbsI grew up with typical hearing, but now I rely on my bilateral cochlear implants to hear. So although I live in the hearing world, I sometimes feel like a ghost, hanging around but unable to participate when I can’t follow conversations.
I’ve been learning how to do something about it. It’s a simple lesson that I must remind myself to keep practicing: Advocate through education with a good sprinkling of humor and persistence.
Here’s how.
When eating out. I ask my dining companions to look straight at me when they talk, speak louder (and maybe more slowly wouldn’t hurt), and try to speak one at a time. Most of the time, my friends react positively to this—after all, they want me to hear them.
It’s a pain to remind them when they forget, which inevitably happens, but I’m getting over it. I need the education and patience as much as they do.
When in a public venue. Interested in attending a play, lecture, or movie? What about a school board meeting? In theaters, auditoriums, and lecture halls, it’s not a question of interacting with your companions. It’s a technology problem. Many venues have not installed the assistive listening devices that have been such a boon to the hearing loss community. In this case, advocate and educate.
Call the theater or meeting place ahead of time and ask about the accommodations they have made for people with hearing loss.
And please be respectful if they tell you there will be a sign language interpreter available.
Ask if they have installed a hearing loop, which will work with your telecoil-enabled hearing aid or cochlear implant. Or maybe they have an FM or IR system. If they do, where are the devices? How often do they check or test them? You don’t want to end up at a place where the technology is present but broken or inoperable.
When there is a screen. Another accommodation is captioning. My preference is open captions, where the captions are displayed on the screen so your eyes focus in one place. Some theaters and other public venues display closed captions on your tablet or phone, which is better than no captions at all, but your
One tip: Call the theater or meeting place ahead of time and ask about the accommodations they have made for people with hearing loss.
focus must go back and forth.
When I go to see a play, I tell patrons around me I’m using my tablet for the captions. After all, I don’t want to create the embarrassment recently experienced by an actor on Broadway who mistakenly called out a patron with a hearing loss for using her tablet; the actor thought she was recording the performance.
When, more broadly, you need to remind folks it’s the law.
The Americans with Disabilities Act (ADA) says that public venues must provide reasonable accommodations for people with disabilities, and hearing loss is included. But there is no ADA police force—those of us who need accommodations must be the force who educates the operators of these venues, and advocate for our right to have them.
This is where you need to exercise all your advocacy muscles. And a group working together is going to be more effective than just one person making a timid complaint. After all, providing hearing accommodations requires investments in time, effort, and money on the part of the venue. Consider asking your local chapter of the Hearing Loss Association of America to get involved so you can fight the good fight, together.
Celebrate Wins
Berkeley, California, introduced curb cuts citywide back in 1971. There were plenty of opponents to this expenditure of public funds to create dips in sidewalks that allowed the smooth transition from raised sidewalks to streets a few inches below, and then back up again to the sidewalk on the other side of the street. But disabled veterans and others advocated so effectively that the curb-cut phenomenon became a reality.
And guess what? After the uproar died down, everybody realized it was in the community’s interest to have curb cuts, so they’ve become almost universal, to the joy of moms pushing strollers, people schlepping wheeled luggage, and kids riding skateboards.
Captioning is now becoming the norm across social media. Although it is still something you have to proactively enable on your TV set, if you’re on Instagram or YouTube, for instance, you’ll have noticed automatic captions are routine.
This is due not only to steadfast advocacy efforts but also because it turns out the majority of people like to
watch their videos with the sound off. And that means needing the captions to follow what is happening. As a result of this demand, social media platforms have made it super easy for content creators to add captions to their videos. So we all benefit from captioning, with or without a hearing loss.
Be Seen
I have gotten thoroughly tired of being a ghost at my own party. Haven’t you? I’ve made it my mission to speak up, for myself and for our community. Speak up to your friends, your family, even your annoying uncle who just doesn’t get it. Speak up at public meetings. Educate your local officials, the guys who own the local theater, and the convention center in your city: It’s your right to have accommodation for your hearing loss.
I know you can do it, too.
Pat Dobbs began to lose her hearing in college, and when she reached her mid-50s, lost most of her hearing in both ears. She is now the proud owner of bilateral cochlear implants, and an enthusiastic advocate for the hearing loss community. She has spoken and written widely on the topic of hearing loss. In 2011 she founded the Hearing Loss Association of America, Morris County Chapter, New Jersey, and today is president of the international online hearing loss support group, Say What Club, saywhatclub.org. Having moved to Deer Isle, Maine, she is forming the Downeast Chapter of HLAA. If you are interested in learning more, email Pat at pat@coachdobbs.com. For references, see hhf.org/winter2023-references.

Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
A Daily PRACTICE
By Sarah KirwanI was 33 when I was diagnosed with multiple sclerosis (MS). I was in Los Angeles, experiencing what I could only imagine were the worst moments of my life, and I was alone. Only days later, I attended my first self-help group and I didn’t belong. I was young, with full mobility and a high cognition level, and I was at a much different place in my life than other attendees. I was talking about dating, and they were talking about grandchildren. I left the meeting determined to create a support system for myself and other young people living with MS.
Three months later, I joined a fellow MS warrior to launch a self-help group for people in their 20s, 30s, and 40s—the Young Person’s Group. A decade later, YPG is thriving in Los Angeles and has expanded to include teens living with MS. It was my first step on a journey I continue today, and the first time I recognized myself as the inherent activist I am.
Alliance for Justice defines advocacy as any action that speaks in favor of, supports or defends, argues for a cause, or pleads on behalf of others. And I had no idea that with this step into advocacy, I had managed to incorporate all three types—self, individual, and system. Self, meaning I needed the self-help group to be effective for me. Individual, meaning I wanted to create a system of support for other young people. And system, meaning I was creating a new opportunity to support members of the MS community. Self-advocacy is tricky because it’s often easier to fight for someone else’s needs rather than fighting for your own. Until it’s necessary.
In 2019, I was diagnosed with superior semicircular canal dehiscence, which went undiagnosed and misdiagnosed for almost a decade. MS and SSCD share symptoms, such as fatigue, migraines, and vertigo. However, the one symptom I was experiencing, which could only be connected back to SSCD, was autophony, or hearing my organs moving internally. It was debilitating
Sarah Kirwan (back row, right) and the wheelchair basketball team she helps lead.

me and I couldn’t find a provider who believed me. Years into this process, I successfully diagnosed myself. It didn’t matter, so I continued begging providers to help me.

Looking back, I see that as a white, cisgender woman with bachelor’s and master’s degrees, who speaks English as a first language, and who has experience working in healthcare and insurance settings, I am the most wellpositioned to get the care I need. But it took me almost a decade to get relief. And that means people from marginalized and under-resourced communities, which are disproportionately communities of color, will never have the same opportunity I had for their own relief. I am dedicated to changing that narrative.
In 2020, I launched my small business, Eye Level Communications, providing strategic services that help businesses implement disability inclusion with confidence. Recently, I helped transition the women’s wheelchair basketball team I’ve played on for seven years to a new, sustainable, nonprofit model.
For me, advocacy is a way of life. It’s the work we do to ensure access and inclusion for ourselves and all members of the disability community. It’s our dedication to creating and holding space for conversations—at eye level—that connect people to one another, their communities, and themselves.
Sarah Kirwan lives in California. She wrote about her SSCD diagnosis in the Winter 2022 issue, at hhf.org/magazine. For more, see eyelevel.works.
Share your story: Tell us your hearing loss journey at editor@hhf.org.
Support our research: hhf.org/donate.
aid


ts inside your ear and costs only $14 999 be every bit as good as one that sells for $2,400 or more?
The answer: Although tremendous strides have been made in Hearing Aid Technology, those cost reductions have not been passed on to you. Until now...













The MDHearing™ NEO uses the same kind of technology incorporated into hearing aids that cost thousands more at a small fraction of the price. Over 800,000 satis ed MDHearing customers agree: High-quality, digital, FDA-registered rechargeable hearing aids don’t have to cost a fortune. NEO is a medical-grade, digital, rechargeable hearing aid offering sophistication and high performance; and works right out of the box with no time consuming “adjustment” appointments. You can contact a licensed hearing specialist conveniently online or by phone — even after your purchase at no cost. No other company provides such extensive support. Now that you know...why pay more?
PLUS... It ts inside your ear.







Presenting the 2023 First-Year Emerging Research Grants Scientists
Through the Emerging Research Grants (ERG) program, Hearing Health Foundation (HHF) provides seed money to scientists working across the entire spectrum of hearing and balance research, including many underfunded areas. Since 1958, ERG grants have played a foundational role in the careers of many academic researchers and clinicians in hearing and balance fields.
The competitive ERG program awards grants to only the most promising investigators. Recipients are exceptionally well-positioned to win future grants from the National Institutes of Health and other federal research funders, leading to dramatic innovations in the field. Congratulations to the 2023 first-year grantees. For a full list of all 15 recipients, including those who earned second-year funding, see hhf.org/erg.
Francisco BarrosBecker, Ph.D. University of Washington
Project: Aminoglycoside compartmentalization and its role in hair cell death
Description: Hair cells, located in the inner ear, are highly specialized cells that have a central role in hearing and balance. We observed that hair cells, when exposed to different aminoglycoside antibiotics, could die rapidly or in a delayed manner. Microscopy imaging of this process showed that aminoglycosides leading to a delayed death tend to localize inside membranous structures called vesicles, inside hair cells. We hypothesize that the capture and delivery of aminoglycosides into vesicles is protecting the hair cell and delaying the toxic effects of these drugs.
Using the genetic and optical advantages of the zebrafish, coupled with super-resolution microscopy
and automated image analysis, we aim to understand how vesicles collect and contain aminoglycosides within them. Each individual vesicle is part of a much larger and intricate vesicular network, and the activity of this network is essential for normal cell function. Unfortunately, how the vesicular network works in hair cells is not well understood. With this grant we aim to describe key steps during the process of aminoglycoside uptake and delivery into vesicles. In addition, tracing the maturation of vesicles containing aminoglycosides will help us better understand where toxicity, and therefore cell death, is triggered.
Long-term goal: To develop new tools that will help the scientific community to deepen our understanding of the vesicular network in hair cells, both during stress and normal conditions. We will develop novel fluorescent probes to mark the different compartments in the vesicular network. This will allow for the visualization of the drug as it transitions through various levels within the vesicular network. In order to better analyze these structures, we will pair these images with custom-made image analysis
algorithms that will allow us to study vesicles in a deeper way.
Overall, these tools will allow us to open new research avenues that will help us to further understand how aminoglycosides, and other drugs with ototoxic effects, like cisplatin, a cancer chemotherapy drug, are killing hair cells. Our results could help direct new research and lead to novel therapeutic treatments to avoid further hearing loss in patients undergoing these treatments.
Since the start of his scientific studies in Santiago, Chile, Barros-Becker has always been interested in understanding how cells and organisms can respond to their surroundings. Through his doctoral studies with Anna Huttenlocher, M.D., Ph.D., at the University of Wisconsin–Madison, he was able to study how immune cells migrate through complex environments and how they interact among them when actively responding to a wound. Currently he is a postdoctoral fellow in the lab of David Raible, Ph.D., at the University of Washington.
Project: Apical cochlear mechanics after cochlear implantation
Description: Cochlear implants are electrical devices that stimulate the inner ear to help restore hearing. Some implant patients are also fitted with a hearing aid that amplifies sound at the low frequencies. This hybrid implant approach maximizes the sound quality for these individuals who still have low frequency hearing. Unfortunately, some of these patients lose low frequency hearing following receipt of the cochlear implant, and the mechanisms are unknown.
One theory states that scarring caused by the presence of the cochlear implant disrupts the normal movement of sound waves through the inner ear. Using advanced imaging techniques that simultaneously measure nanometer scale vibrations, this project aims to reproduce cochlear implant-induced hearing loss in a rodent model and measure exactly how implantation and scarring influences the function of the inner ear at low frequencies. We will use the images we collect to build a 3D map of the scarring inside each cochlea and compare this data to the mechanical performance of the cochlea and hearing thresholds. If we can establish a cause for this hearing loss
we can take steps to prevent it, leading to much improved quality of life for recipients of hybrid cochlear implants and possibly expand eligibility criteria for implantation.
Long-term goal: To establish, treat, and prevent implant-induced hearing loss. This mechanics project is the first time the vibration of the inner ear has been measured in the presence of a cochlear implant, and there is much to discover—such as measuring the efficacy of drugs that help suppress scarring, and testing different electrode designs. Refining use of optical coherence tomography will also benefit research on other diseases of the inner ear, such as Ménière’s disease. Optical coherence tomography has the potential to play a big role in the future of both basic hearing science and hearing restoration.
Burwood completed his doctorate in auditory physiology with Ian Russell, Ph.D., and Andrei Lukashkin, Ph.D., at the University of Brighton, U.K., and is currently a postdoctoral researcher in the lab of Alfred Nuttall, Ph.D. (a 1989–1990 ERG scientist), at Oregon Health & Science University. Both roles focused on cochlear mechanics, and the latter introduced him to the power and versatility of optical coherence tomography.

Thank You to Our Grants Reviewers
As always, HHF extends its profound thanks to our peer reviewers, a revolving group of research scientists and clinicians who donate their time and expertise to provide comprehensive review of each and every ERG proposal HHF receives. Without these reviewers’ dedication to advancing hearing and balance science, supporting newer investigators’ careers, and sustaining HHF’s mission, HHF could not direct our donors’ support to the innovative and promising research HHF has had the privilege of funding since 1958.
Support our research: hhf.org/donate.
Carolyn
McClaskey, Ph.D.Medical University of South Carolina

Project: Age and hearing loss effects on subcortical envelope encoding

Description: As we get older, it often becomes difficult to understand speech in noisy environments such as a crowded restaurant. Changes in auditory temporal processing are known to partly underlie these communication difficulties. Such altered temporal processing, including distorted neural encoding of sound envelopes, may arise from age- and hearing loss-related changes to subcortical auditory structures. This project uses a combination of behavioral, electrophysiological, and neuroimaging measures to assess how the auditory midbrain changes with age and age-related hearing loss and how this affects envelope encoding and speech-in-noise recognition.
Sharlen Moore, Ph.D. Johns Hopkins UniversityProject: Modulation of neuro-glial cortical networks during tinnitus
Description: Tinnitus can be conceived as a disorder in which auditory and non-auditory brain areas are dysregulated and hyperexcitable, leading to the constant perception of a sound not externally generated. Neuromodulatory areas that send widespread signals across the brain have the potential to be responsible for this dysregulation as a change in gain or sensitivity.
Targets of these neuromodulatory areas can be either neurons or glial cells. Glial cells make up approximately half of the cells in our brain. They do not communicate through electric signals but do receive similar inputs as neurons do, and they also have the potential to modulate neuronal gain. This research will allow us to better understand the contribution of glial cells receiving inputs from longrange neuromodulatory centers to an overall hyperexcitability phenotype in auditory regions that gives rise to the perception of tinnitus.
Long-term goal: To better understand how age and age-related hearing loss alter the neural signaling of the auditory system (specifically the auditory midbrain) and negatively impact speech communication, so that we can work toward developing effective clinical interventions and improving communication for older adults and adults with age-related hearing loss.
McClaskey earned her doctorate in psychology and cognitive science at the University of California, Irvine, and completed her postdoctoral studies in auditory neuroscience in the Hearing Research Program at the Medical University of South Carolina. She is now a research assistant professor in the department of otolaryngology at the Medical University of South Carolina. Her 2023 Emerging Research Grant is generously funded by Royal Arch Research Assistance.
Long-term goal: To understand the complexity and temporal sequencing of tinnitus effectors with an integrative perspective, and to consider the interplay of diverse cell types that may lead to tinnitus, in order to provide an updated interpretation of this disorder; and to use glial cells as a key therapeutic target to treat tinnitus.
Moore received her doctorate in neuroscience from the Max Planck Institute of Experimental Medicine in Germany, with Livia de Hoz, Ph.D., and Klaus-Armin Nave, Ph.D., studying the role of myelin in mice auditory processing. She then returned to her native Mexico for postdoctoral studies at the Institute of Cellular Physiology, the National Autonomous University of Mexico, with Francisco Fernández de Miguel, Ph.D. She studied extrasynaptic serotonin release in the leech and participated in a project to understand how sounds modified the perception of visual art. She is now in the lab of Kishore Kuchibhotla, Ph.D., at Johns Hopkins University to study neuromodulatory circuits that influence learning and to understand the role of astrocytes in context-dependent high-order functions. Her 2023 Emerging Research Grant is generously funded by the Les Paul Foundation.




Project: Identifying hearing loss through neural responses to engaging stories
Description: Spoken language acquisition in children with hearing loss relies on early identification of hearing loss followed by timely fitting of hearing devices to ensure they receive an adequate representation of the speech that they need to hear. Yet current tests for young children rely on non-speech stimuli, which are processed differently by hearing aids and do not fully capture the complexity of speech.
This project will develop a new and efficient test—called multiband peaky speech—that uses engaging narrated stories and records responses from the surface of the head (via EEG, or electroencephalography) to identify frequencyspecific hearing loss. Computer modeling and EEG experiments in adults will determine the best combination of parameters and stories to speed up the testing for use in children, and evaluate the test’s ability to identify hearing loss.
This work lays the necessary groundwork for extending this method to children and paves the way for clinics to use this test as a hearing screener for young children—and ultimately our ability to provide timely, enhanced information to support spoken language development.
Long-term goal: To develop an engaging, objective clinical test that uses stories to identify hearing loss in young children and evaluate changes to their responses to the same speech through hearing aids. This goal addresses two important needs identified by the U.S. Early Hearing Detection and Intervention program and will positively impact the developmental trajectory of thousands of children who need monitoring of their hearing status and evaluation of outcomes with their hearing devices.
Polonenko received her doctorate in neurophysiology with the Institute of Medical Science at the University of Toronto. An audiologist and neuroscientist who trained in Canada, she completed postdoctoral studies in neuroscience and biomedical engineering at the University of Rochester Medical Center and is now an assistant professor in the speechlanguage-hearing sciences department at the University of Minnesota. Her 2023 Emerging Research Grant is generously funded by Royal Arch Research Assistance.
Support our research: hhf.org/donate.
The ERG program is a competitive process that awards grants to only the most promising investigators. Recipients are exceptionally well-positioned to win future grants from the National Institutes of Health and other federal research funders, leading to dramatic innovations in the field. In fact, ERG alumni have gone on to be awarded an average $47 for every dollar of investment through ERG (2002–present).
Recent Research by Hearing Health Foundation Scientists, Explained


In this image from eLife, scanning electron micrographs of reprogrammed hair cells show similar hair cell-like structural features. Arrows indicate individual reprogrammed hair cells.

Molecular Barriers to Overcome for Hair Cell Regeneration in the Adult Mouse Cochlea
About 430 million people around the world experience disabling hearing loss. Hearing loss can happen when any part of the ear or the nerves that carry information on sounds to the brain do not work in the usual way.
For instance, damaged hair cells in the inner ear can lead to hearing loss. “These cells allow the brain to detect sounds,” says Amrita Iyer, Ph.D., the first author of a November 2022 paper published in eLife. During this project, Iyer was a graduate student in the lab of Andrew Groves, Ph.D., a professor and Vivian L. Smith Endowed Chair in Neuroscience and of molecular and human genetics at Baylor College of Medicine.
Hair cells are generated during normal development, but this ability is progressively lost after birth as mammals mature. “When hair cells are lost in mature animals, the cells cannot be naturally regenerated, which can lead to permanent hearing loss,” Iyer says.
Transcription factors promote the expression of certain genes and prevent the expression of others. By changing the pattern of gene expression, the team hoped to lead cells to a state in which they would regenerate hair cells in mature animals, like what happens during development.
“We compared the reprogramming efficiency of the hair cell transcription factor ATOH1 alone or in combination with two other hair cell transcription factors, GFI1 and POU4F3, in mouse non-sensory cells in the cochlea, the part of the inner ear that supports hearing,” Iyer says. “We did this at two timepoints—8 days and 15 days after birth, assessing the extent of hair cell regeneration in mice.”
To study the structure of the hair cell bundles generated by reprogramming, Iyer collaborated with the lab of Yehoash Raphael, Ph.D., at the University of Michigan to perform scanning electron microscopy imaging on the cochleae of mice conditionally overexpressing these

transcription factors. The images clearly showed that the hair cell bundles were in accordance to what is observed on inner hair cells during development. Further studies showed that these cells also had some characteristics that suggested that they were capable of sensing sound.
“We found that although expressing ATOH1 with hair cell transcription factors GFI1 and POU4F3 can increase the efficiency of hair cell reprogramming in older animals compared to ATOH1 alone or GFI1 plus ATOH1, the hair cells generated by reprogramming at 8 days of age—even with three hair cell transcription factors—are significantly less mature than those generated by reprogramming at postnatal day one,” Iyer says.
“We suggest that reprogramming with multiple transcription factors is better able to access the hair cell differentiation gene regulatory network, but that additional interventions may be necessary to produce mature and fully functional hair cells.”
Transcription factor–mediated reprogramming and its underlying biology may enable fine-tuning of gene therapy approaches for hearing restoration. —Ana María Rodríguez, Ph.D., Baylor College of Medicine
This originally appeared on the Baylor College of Medicine website. Coauthors and Emerging Research Grants (ERG) alumni Andy Groves, Ph.D. (far left), and Yehoash Raphael, Ph.D., are members of HHF’s Hearing Restoration Project, along with the late Neil Segil, Ph.D.
This figure from Cell Reports shows the different groups of cells in the typical chicken utricle. Learn more at hhf.org/blogs/cell-type-identity-ofthe-chick-balance-organ.
Cell-Type Identity of the Chick Balance Organ
A major goal of the work conducted by Hearing Health Foundation’s Hearing Restoration Project (HRP) in recent years has been to obtain a complete set of genes that are active in each cell type in the chicken inner ear. In 2021 my laboratory provided an inventory of all genes expressed in the chicken hearing organ, also known as the basilar papilla.
Now, one year later, we have inventoried the genes expressed in the chicken utricle, an important balance organ. In our study in Cell Reports in September 2022, we identified genes that define three different sensory hair cell types and two distinct supporting cell groups.
The avian utricle, in contrast to the basilar papilla, continuously produces new hair cells throughout the animal’s life. Our team identified the sequence of gene expression changes in supporting cells during this natural process of new hair cell production. This knowledge will be important in future comparative studies where the HRP plans to compare the repertoire of genes active during hair cell regeneration in chicken and zebrafish with existing gene expression in the mouse and human inner ear.

Hair cell regeneration does not naturally happen in mice and humans, and therefore, it will be important to identify the genes that are missing in supporting cells from these species. This knowledge, in turn, will guide the selection of candidate genes for potential future therapeutic approaches.
This paper concludes a string of three publications by our lab in 2021 and 2022 that establish a baseline for investigating the molecular mechanisms of auditory hair cell regeneration in chickens. Although still a work in progress, our team will present multiple abstracts at the February 2023 Association for Research in Otolaryngology
meeting in Orlando, where we will discuss novel findings about the molecular pathways that initiate auditory hair cell regeneration in birds.
This is an exciting time for us and the HRP consortium because it demonstrates that the long-term investment into a systematic research approach with different animal models was worthwhile. We have now identified the first events that lead to proliferative hair cell regeneration in birds, which provides new leads that can be translated to mice and ultimately to humans.

The ability to monitor 20,000 genes in parallel in every individual cell in the regenerating inner ear is extremely powerful. It also provides an incredible challenge to identify the significant genes that ultimately can be targeted with a drug-based approach. We are off to a promising start, and we tackle this large puzzle with an incredibly motivated team. We are thankful for the support from Hearing Health Foundation that enables this work. —Stefan Heller, Ph.D.
Support our research: hhf.org/donate.
Apparent Benefits of Cochlear Implantation Before Age 2
Early childhood deafness generally has a profound and lasting impact on educational and career attainments later in life because it reduces the quality and quantity of language experience, thereby inhibiting the acquisition of spoken language and literacy abilities. Cochlear implants, however, can enhance the quality and quantity of linguistic input and facilitate the development of spoken language and literacy skills in early onset childhood deafness.
We studied the categorization of speech sounds in two groups of adult cochlear implant (CI) users with earlyonset deafness and a group of 21 hearing controls. Thirty of the CI users were implanted before age 4 (early CI group), and 21 were implanted after age 7 (late CI group). We evaluated listeners’ identification and discrimination of speech sounds along a voicing continuum consisting of the syllables /ba/ vs. /pa/, and a place of articulation continuum consisting of the syllables /ba/ vs. /da/.

Our paper in the Journal of Speech, Language, and Hearing Research in November 2022 showed that, for the /b/–/p/ contrast, when voice onset occurs at about 20 milliseconds (ms) or less after release of air pressure behind the lips, CI users with early onset deafness generally perceive the sound as /b/. But when voice onset occurs at longer intervals, it is generally perceived as /p/.
The accompanying figure illustrates the probability of an average listener in each group identifying the stimuli on the /ba/–/pa/ continuum as /ba/. The /ba/–/pa/ category boundary for each listener group is denoted by a dot on their curve. Stimuli to the left and above the /b/–/p/ category boundary were identified as /ba/, while stimuli to the right and below the boundary were identified as /pa/.
For each group, the /b/–/p/ contrast was quite sharp, as reflected in the steep slope of the curve in the vicinity of the /b/–/p/ category boundary. The average /p/–/b/ boundary was located at 17.3 ms for the hearing listeners and only 5 to 6 ms longer for listeners in the CI groups.
Distinctive identification and discrimination functions were observed for each group on both the voicing and place of articulation continua, indicating similar performance between CI users and hearing controls and between the early and late CI groups. Compared with hearing participants, however, the CI groups generally displayed longer/higher category boundaries, shallower identification function slopes, reduced identification consistency, and reduced discrimination performance.
This figure from the Journal of Speech, Language, and Hearing Research shows the results of a speech identification task. Learn more at hhf.org/blogs/apparent-benefits-of-cochlearimplantation-before-age-2.
The results also showed that earlier implantation was associated with better phoneme categorization (PC) performance within the early CI group, but not the late CI group. Within the early CI group, earlier implantation age but not PC performance was associated with better speech recognition. Conversely, within the late CI group, better PC performance but not earlier implantation age was associated with better speech recognition.
This indicates that, within the early CI group, the age a child receives a CI affects their eventual development of phoneme (speech sound) categories in adulthood, and that the linguistic categories within each CI group closely resemble those of hearing controls. Importantly, individuals implanted prior to age 2 seem to acquire top-down processing abilities that enable them to become more proficient at speech recognition than those implanted in later years, whose speech recognition generally appears to proceed from the bottom up.
These findings provide valuable insight into the interaction between the learner’s age (developmental period effect) and their linguistic experience (quality and quantity of linguistic input) in early development. We find a midsize developmental period effect occurring before age 4, which partly determines PC ability, as well as another midsize developmental period effect associated with the acquisition and use of top-down linguistic processing, occurring around age 2. —Joseph Bochner, Ph.D.
A 2017 ERG scientist generously funded by Royal Arch Research Assistance, Joseph Bochner, Ph.D., is a professor at the National Technical Institute for the Deaf at Rochester Institute of Technology.


Nicotine Injections Reduce Age-Related Changes in the Older Mouse Brain
Older adults can experience difficulties understanding speech in challenging environments, even in the absence of significant hearing loss. This indicates deteriorated processing in the aging central auditory system, and this may lead to reduced communication and social activities. Epidemiological studies have demonstrated a link between the degradation of communication, social activities, and declining cognitive abilities.
To improve central auditory processing in older adults, it may be necessary to use a combination of hearing aids and behavioral and pharmacological treatment approaches. Currently no pharmacological approach exists to improve central auditory processing, and it is also unclear if neural circuits in older adults can be reactivated to a “young” level.
Neural oscillations—electrical activity in the central nervous system that occur spontaneously and in response to stimuli—at specific frequency bands are associated with cognitive functions and can identify abnormalities in cortical dynamics. In this study published in Neurobiology of Aging in December 2022, Khaleel Razak, Ph.D., and team analyzed electroencephalogram (EEG) signals recorded from the auditory and frontal cortex of freely moving mice across young, middle, and old ages, and found multiple robust and novel age-related changes in these oscillations.
The paper notes that prior research has shown that manipulating specific neuron signaling pathways by nicotine administration can enhance sensory acuity, reaction time, and attentional and cognitive performance. Other research showed that these pathways are impaired in the aging auditory system. Therefore, the team hypothesized that nicotine administration would reduce age-related impaired cortical processing in old mice.
Razak and colleagues found that an acute injection of nicotine (0.5 mg/kg) in old mice partially or fully reversed the age-related changes in EEG responses. Nicotine had no effect on auditory brainstem responses, suggesting the effects occur more centrally.
Importantly, their data suggest that the auditory circuits that generate “young” responses to sounds are present in old mice, and can be activated by nicotine.
The researchers write that a number of nicotine-like, non-addictive drugs that target cognitive deficits in Alzheimer’s disease and other age-related disorders have been developed. This data in aging mice strongly suggests that topical or oral nicotine or nicotine-like substances may be profoundly beneficial for aging humans with central auditory processing disruptions.
This is adapted from the paper in Neurobiology of Aging. A 2009 and 2018 ERG scientist, Khaleel A. Razak, Ph.D., is a professor of psychology and the director of the graduate neuroscience program at the University of California, Riverside. Razak’s 2018 grant was generously funded by Royal Arch Research Assistance.
Support our research: hhf.org/donate.

Balance Control in People With Hearing or Vestibular Loss in One Ear
Recent studies have demonstrated a relationship between hearing loss and an increased risk of falls and reduced balance performance, but it is unclear whether this applies to people with hearing loss in one ear (unilateral) and typical hearing on the other ear. While unilateral hearing loss was once considered to have no functional limitations, data now suggests that it may lead to participation restrictions in social, family, and work settings.
We are investigating three theories regarding balance in individuals with hearing loss:
1) When healthy individuals perform balance tasks in complex sensory environments, they tend to respond to sensory perturbations (e.g., moving visual environments) by increasing their body sway. If a sense is impaired (e.g., such as loss of balance or vision) people tend to over-rely on the other senses for balance. People with vestibular loss tend to be visually dependent and sway more than healthy controls when the visual environment is moving. Do people with hearing loss rely more on visual and somatosensory input because of the loss of auditory input?
2) The auditory and vestibular system are anatomically very close. Do people with hearing loss rely more on visual and somatosensory input because they also have undiagnosed vestibular loss?
3) Individuals with hearing loss compensate for the loss of auditory cues by using a “feed-forward” mechanism for balance—relying on prior expectation and motor planning rather than responding to dynamic sensory cues. If so, people with hearing loss would not increase their sway with changing visual load as expected in healthy controls.
For our study published in PLOS ONE in October 2022, we recruited people with unilateral vestibular loss or with unilateral hearing loss, along with healthy controls. The mean ages for the three groups ranged from 48 to 62.

We analyzed postural sway (from a force platform) and head sway (from a virtual reality headset) in response to two levels of auditory cues (none or rhythmic sounds via headphones), visual cues (static or dynamic), and somatosensory cues (floor or foam) within a simulated, virtual three-wall display of stars. We found no differences with the rhythmic auditory cues. The effect of foam was
This figure from PLOS ONE shows the postural sway front to back when people are standing on the floor (red) or foam (green). Learn more at hhf.org/blogs/balance-control-in-people-with-hearingor-vestibular-loss-in-one-ear.
magnified in the unilateral balance loss group compared with controls for front to back and side to side postural sway, and all head directions except for side to side.
The vestibular loss group had significantly larger front to back and side-to-side postural and head sway on the static scene compared with controls. Differences in pitch, yaw, and roll emerged between the balance loss group and controls only with sensory perturbations.
The unilateral hearing loss group did not increase their postural sway and head movement with the increased visual load as much as controls did, particularly when standing on the foam. They also did not increase their side-to-side sway with the foam as much as controls did.
These findings support theory #3, suggesting that individuals with hearing loss in one ear employ a compensatory strategy of conscious control of balance. Overall, in this study patients with vestibular loss disorders had exaggerated responses to sensory stimuli, as expected, while the unilateral hearing loss patients’ response to stimuli was less reactive, demonstrating a stiffer posture.
Patients with hearing loss in one ear appear to have more conscious control over their response to sensory cues in their environment, resulting in a more deliberate control of balance with less degrees of freedom to respond to changes in the environment, almost like a guarding behavior. The functional implications of these preliminary findings need to be tested in future research.
Anat V. Lubetzky, PT, Ph.DA 2019 ERG scientist, Anat V. Lubetzky, PT, Ph.D., is an associate professor at New York University’s department of physical therapy.

Neural tests to assess if important speech elements are heard could be equally useful in children and adults.
How Can We Measure Hearing Aid Success in the Youngest Patients?

In infants and children too young to participate in hearing tests, using neural responses to sound is a reliable way to assess how well they hear. Neural responses to sound are routinely used in audiology clinics for diagnosis to infer the degree and type of hearing loss in very young babies and in older children who may have additional developmental challenges.
However, the use of neural responses to sound to infer how well hearing aids—a common first form of intervention—provide access to speech is less well established. Such tests with hearing aids require the use of speech so hearing aids function the way they would during everyday conversations.
We have been working toward a clinical test that plays the word “susashee” and records neural responses tagged to each sound. The sounds are chosen and modified such that neural responses can help us infer whether low, mid, and high frequencies are accessible to the listener with or without hearing aids, and the extent to which hearing aids make each of these frequencies accessible to the listener.
Hearing all these frequencies are critical for speech understanding and speech and language development during early years of life during which rapid brain development occurs. Our previous work has shown that such a neural test could be useful to assess access to speech in adults with hearing loss using hearing aids, and can be measured in young infants in their sleep.
In our recent study funded by Hearing Health Foundation and published in the Journal of Speech,
Language, and Hearing Research in October 2022, we assessed whether neural responses could predict audibility and inaudibility of low, mid, and high frequency speech played at soft to loud levels in children ages 5 to 17 as accurately as in adults, and whether analysis of neural responses using different statistical metrics can influence its accuracy.
Our results demonstrate that neural tests are equally accurate in children and adults, and the type of analysis did not influence accuracy in children. Accuracy of predictions increased at high frequencies, but this was similar in both adults and children.
Further, in a parallel study published in the Journal of Association for Research in Otolaryngology in August 2022, we were able to confirm that the same analysis features pertaining to neural response delays could be used in children and adults without substantial impact on estimation of such responses. We are currently evaluating the accuracy of this neural test in children with hearing loss with and without hearing aids as well as advancing our analysis strategies to improve the accuracy of predictions for clinical use. —Viji Easwar, Ph.D.
A 2019 ERG scientist funded by the Children’s Hearing Institute, Viji Easwar, Ph.D., is the lead researcher of the pediatric hearing research program at the National Acoustic Laboratories in Sydney, Australia.

For references, see hhf.org/winter2023-references.
Support our research: hhf.org/donate.
This sponsored page shows current trends in technology.
Tech Solutions
CapTel® Captioned Telephone


Enjoy the phone again with confidence! Ideal for people with hearing loss, the CapTel® Captioned Telephone shows captions of every word the caller says over the phone. You can listen to the caller, and read the written captions in the CapTel® display screen. Only CapTel® gives you several models to choose from, including contemporary touch-screen options and traditional telephone styles. All CapTel® phones include a large display screen, adjustable font sizes and colors, and a built-in answering machine that shows captions of your messages. CapTel® gives you the confidence to reconnect over the phone, knowing you won’t miss a word! Visit CapTel.com.
InnoCaption
InnoCaption provides real-time captions, your way. We are dedicated to empowering the deaf and hard of hearing community to make phone calls with confidence! Utilizing both live stenographers and automated speech recognition technology (ASR), InnoCaption lets you choose your caption style.
Funded by the FCC, InnoCaption is offered at no cost for eligible users and our service is available 24 hours, 7 days a week. InnoCaption keeps you connected to all life’s special moments and ready to take on everything your day has in store.
To learn more about how InnoCaption can improve your quality of life and get answers to any questions, contact us at support@innocaption.com or visit innocaption.com.
These featured products are paid advertisements. To advertise in Hearing Health magazine, email hello@glmcommunications.com or call 212.929.1300.
Supporters of Hearing Health
STOP paying for cellular service you don’t use and only pay for what you need. Plans start at $10 per month. Phones start at free. Great prices on certified pre-owned phones with warranty.

affinitycellular.com 844.831.2218
Try for free! Bladder leak protection that actually works. Our super absorbent pads & underwear keep you dry and comfortable day and night. Satisfaction guaranteed. 250,000+ happy customers. 24 hour customer support.


becausemarket.com/hhf 800.267.8016 page 29
Captioned Telephone
CapTel captioned telephone shows word-for-word captions of everything a caller says over the phone. Like captions on TV—for your phone. Helps people with hearing loss enjoy phone conversations, confident they’ll catch every word.
captel.com 800.233.9130

pages 44, 47
When it comes to understanding what’s said on the phone, Hamilton CapTel makes all the difference. Reliable and accurate captions ensure clarity on every call— eliminating the frustration even a simple phone call can make for people with hearing loss.
hamiltoncaptel.com 877.455.4227 page 2
InnoCaption is the only mobile app that offers real-time captioning of phone calls through live stenographers and automated speech recognition software—the choice is yours. Our technology makes phone calls easy and accessible!
BecauseMarket.com/HHF 800-267-8016
The Les Paul Foundation inspires innovative and creative thinking by sharing the legacy of Les Paul through support of music education, recording, innovation, and medical research related to hearing.

innocaption.com pages 5, 44
les-paul.com 212.687.2929 page 36
The MDHearing NEO is a medical-grade, digital, rechargeable hearing aid offering sophistication and high performance. Our smallest hearing aid ever. 45-day risk-free trial. Buy one, get one free! Use code EE26 and get free shipping.
trymdneo.com 800.982.5311 page 33
Hearing damage from too much noise is entirely preventable. Our hearing is too important to everyday life—and our overall health—to take for granted. Let’s all take care of our hearing, forever.
hhf.org/keeplistening
Picture Your Company Logo Here
All Hearing Health advertisers and other partners are featured on this Marketplace page at no additional charge. Please join our community of supporters. 212.929.1300

Emerging Research Grants (ERG)
As one of the only funding sources available for innovative research, HHF’s ERG program is critical. Without our support, scientists would not have the needed resources for cutting-edge approaches toward understanding, preventing, and treating hearing and balance disorders.
Meet the Researcher
Melissa Polonenko, Ph.D. University of Minnesota–Twin CitiesPolonenko is an audiologist and neuroscientist who trained at Western University and the University of Toronto in Canada. She completed her postdoctoral training in neuroscience and biomedical engineering at the University of Rochester Medical Center and is now an assistant professor in the department of speech-language-hearing sciences at the University of Minnesota. Her 2023 Emerging Research Grant is generously funded by Royal Arch Research Assistance.
i’ve worked as a pediatric audiologist and experienced the importance of new tests that don’t require a behavioral response for young populations. Our field has mainly used very brief sounds, which can tell us a lot about hearing, but I’ve become more interested in how we can use more complex and real-life sounds such as continuous speech in our assessments.
my current project to identify hearing loss through neural responses will develop a new and efficient test—called multiband peaky speech—that uses engaging narrated stories and records electroencephalogram (EEG) responses from the surface of the head to identify frequency-specific hearing loss. Computer modeling and EEG experiments in adults will determine the best combination of parameters and stories to speed up the testing for use in children, and evaluate the test’s ability to identify hearing loss. In the future I’d like to see clinics use this test as a hearing screener for young children to help provide timely, enhanced information to support spoken language development.
as far back as i can remember , science has fascinated me! Originally I wanted to become a physician, but I became hooked to sensory science when I took a sensory psychology elective during my undergraduate studies. This is where I learned about the field of audiology and how the field is very multifaceted.
helping people was always a passion of mine, so that’s why I followed the route of becoming a clinician and then clinician-scientist. Soon I think we will see much more
translational work, bridging our expanding understanding of the neural underpinnings of how we use our multiple senses and applying that understanding to innovative ways to assess and treat hearing and balance challenges.
my grandmother had a progressively worse hearing loss and we could see how that impacted her ability to communicate and interact with family, especially as her dementia also progressed. Working with her during my clinical degree in audiology helped me to consider the real-life functional consequences of hearing while approaching my research.
i am an identical twin. My sister specializes in binocular vision (how your two eyes work together) and I specialize in binaural hearing (how your two ears work together)! We both pursued work in how senses combine bilateral information.

Melissa Polonenko, Ph.D., is a Royal Arch Research Assistance award recipient. Hearing Health Foundation sincerely thanks RARA for their ongoing commitment to research in the area of central auditory processing disorder.
We need your help funding the exciting work of hearing and balance scientists. Please consider donating today to Hearing Health Foundation to support groundbreaking research. Visit hhf.org/how-to-help.



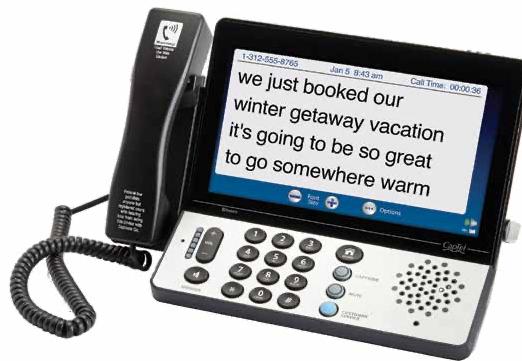
YOU CAN MAKE A DIFFERENCE NOW
announcing a planned giving matching challenge
Planned giving, also called estate or legacy giving, means a gift that your favorite charity receives upon your passing. It is a gift for the future.

A generous, anonymous donor has launched a challenge that will match your planned gift now. This enables Hearing Health Foundation to continue funding the life-changing science that benefits the millions of people who live with hearing and balance challenges.
Your planned gift will be matched when you make a bequest to HHF or name us as a partial beneficiary of a retirement fund or life insurance policy.
Here’s how the matching challenge works:
» For any planned gift of up to $10,000, HHF receives a match of $1,000.
» For any planned gift of $10,000 or more, HHF receives a match of $10,000.
» For larger planned gifts, HHF receives a match of $100,000.
Please email Harriet Hessam at hhessam@hhf.org to let us know about your planned gift or for more information.
Please scan this QR code to learn more about Hearing Health Foundation’s extraordinary planned giving matching challenge.
Don’t have a will? Create one for free with our partner FreeWill at freewill.com/hhf.

You can make a difference NOW as well as in the FUTURE .Ann Pruitt has named HHF in her estate plans.

