INDEPENDENT PRACTITIONER
THE BUSINESS MAGAZINE FOR DOCTORS WITH A PRIVATE PRACTICE
In this issue
Become a patient magnet How to become more attractive to patients by embracing the power of smartphones P24

Become a patient magnet How to become more attractive to patients by embracing the power of smartphones P24
Don’t fall into debt spiral
An expert outlines three key areas of financial stress and how to avoid them P32


The private sector hits back at a scathing report on safety in independent hospitals n Turn to page 18
The independence vote
What are the financial implications for all doctors if Scotland breaks away? P40

By Robin Stride
The Federation of Independent Practitioner Organisations (FIPO) has expressed ‘serious concerns’ over an AXA PPP bid to cut many consultants’ fees by around 20% and persuade more specialists to agree tie-in contracts.
Letters sent from last month to an initial batch of doctors who have no formal agreement with the insurer invited them to sign up –and more specialists can expect to be contacted in the next few months with wording customised to their circumstances.
The insurer also announced a new fee schedule from 1 October 2015, which means lower fees overall, although it said some would rise and others would be frozen.
There will be two consultant categories recognised by the insurer: fee-approved (contracted) and feelimited (not contracted – and so subject to the new schedule).
FIPO’s deputy chairman Mr Richard Packard said: ‘According to AXA PPP, the first group is being offered potentially better access to
In association with
patients through a so-called “fasttrack” referral system. However, if the majority of consultants sign up to AXA PPP’s fee-approved contract, this will cease to be of any added benefit, as the pool of private patients is finite.
‘Fee-limited consultants will still be able to charge at their normal rates, but reimbursement from AXA PPP will be limited, meaning patients will have to make up the shortfall.’
FIPO said its initial analysis of over 40 most common procedures indicated a benefit cutback of around 20%.
A new surgical consultation, for example, would be £125, with £95 for follow-up.
It advised consultants to ‘be wary of engaging with insurers and losing their contract with the patient, for what may be short-term, if any, gain.’
AXA PPP refused to say how many specialists it had agreements with or was writing to, calling this ‘commercially sensitive’.
It claimed its initiative would secure cost-effective, quality treatment for members for the foresee-


able future. Fee-approved specialists would enjoy the reassurance that their fees would be paid in full in accordance with their contract, ‘removing any financial consideration from their relationship with their patients’.
The insurer said fee-approved specialists could also get preferred access to patient referrals from its fast-track appointments service,
now available to all members, where it ‘takes the lead on directing members to a suitable specialist for treatment’.
It argued that because it was sending patients to specialists through this service, it needed effective contracts with those consultants to back a guarantee that members’ fees would be paid in full.
➱ Continued on page 4

SURGICAL SUPPORT: A breast surgeon has turned his strongly-held belief about wrongly-fitting bras into a thriving business. Mr Atul Khanna, who is based in Birmingham, found that many of his patients seeking breast-reduction surgery were suffering from health problems caused by poorlymeasured bras. So he has teamed up with two likeminded entrepreneurs to form a company that manufactures and fits made-to-measure garments.
n See feature on page 14





Public attack on private safety providers respond to a controversial report on patient safety in the private sector P18
star in your own movie doctors are turning to video so patients can see them before they meet P26
Hone in on the target: money as private doctors won’t admit they’re in it for the cash, they’re less successful P29
investing for your offspring
Financial experts give advice on how to invest money for your children P36
don’t let it come to a fight our resident legal eagle tells you how to resolve your partnership disputes P38
what if scotland goes its own way?
We explore the ramifications for all doctors of scotland becoming independent P40
Plus our regular columns
Business Dilemmas: neurosurgical ethical issues P44

ediTorial commenT
TV celebrity doctors have been doing very nicely, thank you, in front of the cameras for many years now and it is rewarding work if you have what it takes.
But now more and more private doctors are at last waking up to the fact they can enhance their business by starring in their own movie for patients on private hospital and personal practice websites.
Video gives a fresh perspective, as we report in our feature starting on page 26. It allows short presentations of important information and lets the patient hear and see the doctor they are considering.
It also allows explanation and demonstration of complex procedures in an easily understandable way for consumption on computer, tablet or smartphone.
We also publish some useful tips to bear in mind for any Independent Practitioner Today reader appearing in front of the camera. In fact, many of these are handy to remind yourself of in each patient encounter.
They will help you present yourself in the best possible light and, even though you might not be recording or filming, these days it pays to be aware your patient might be!
Tell us your news Editorial director Robin Stride at robin@ip-today.co.uk
Phone: 07909 997340 @robinstride
To adverTise Contact advertising manager Margaret Floate at margifloate@btinternet.com Phone: 01483 824094
To subscribe lisa@marketingcentre.co.uk Phone 01752 312140

Publisher: Gillian Nineham at gill@ip-today.co.uk Phone: 07767 353897
Head of design: Jonathan Anstee chief sub-editor: Vincent Dawe 12,000 circulation figures verified by the Audit Bureau of Circulations
by a staff reporter
New industry billing guidelines aim to help independent practitioners get their invoices right first time and avoid unnecessary payment delays.
The free guide has been produced by Healthcode, the official medical bill clearing company for private healthcare in the UK.
It is endorsed by all the main private medical insurers including Aviva, AXA PPP healthcare, Bupa, PruHealth and Simplyhealth.
The industry’s guide to private medical billing is expected to be an invaluable tool for practices who want to make their billing process as professional and efficient as possible.
It sets out the information that should be included on invoices to self-pay patients and private medical insurance companies so that the payer has sufficient information about what they have been charged and why.
Healthcode said this would help practitioners meet their ethical duty to be open in their financial and commercial dealings. And it would also ensure patients had a positive experience following an episode of care.
In addition, the growing number of providers that have made the transition to electronic billing can generate invoices which satisfy the insurers’ criteria, so they are paid as soon as possible, maximising their cash flow.
Healthcode managing director Peter Connor said: ‘The number of electronic invoices from healthcare providers that Healthcode clears has increased by 25% year on year in the last two years, proving that this is fast-becoming universal practice in the sector.
‘When done properly, electronic billing is undoubtedly

more efficient for practices. But mistakes cost precious time to resolve and have a knock-on effect on the practice business, so we have worked with insurers to find a simple solution.’
Starting from the basics such as provider recognition and payment instructions, to more detailed information about the patient and the treatment provided, practitioners and their administrative staff now have access to an annotated step-bystep guide to completing an invoice.
They can also download the two invoice templates, one for billing organisations and the other for self-pay patients, for use in their practice.
Alex Perry, director of health and benefits management, Bupa, said: ‘Electronic billing is quicker, better for the environment, safe and secure.
‘As one of the UK’s trusted providers of secure online billing to the private healthcare market, Healthcode has used its expertise to develop a guide that will help providers ensure they supply all the information we need to process their bills smoothly and that they are paid quickly.’
See the guide at: www.healthcode.co.uk/billing-guide
Criticism is forcing increasing numbers of doctors to wish they could turn back the clock and have aspects of their past wiped from websites.
Now a European Court ruling heralds some good news for them, as it means they could get some search results removed.
The Court of Justice of the EU found that search engine operators are data controllers and individuals have the right to ask them to remove certain search results on privacy grounds. These include results that appear to be inaccurate, inadequate, irrelevant or excessive.
According to Dr Caroline Fryar, MDU head of advisory services, doctors are increasingly seeking advice about how to deal with critical online coverage.
She said: ‘They may have found to their distress that an online search of their name brings up an unfavourable or unflattering story such as a news report about a patient complaint or a past GMC investigation, which may have happened many years ago.
‘The recent European Court ruling is good news for doctors, as it means they can apply to Google and other search engine operators to request the removal of certain results on privacy grounds.’
But Dr Fryar urged caution, because she said it remains to be seen if requests to remove results will be successful, given that decisions will be taken on a case by case basis, balancing the public interest with the right to privacy.
She said: ‘It is also important to remember that the actual web pages and documents will not be removed from the internet, only the opportunity to access them via a search engine link.’
Users may still be able to navigate to the page by using a different search term or the same search term entered into a search engine outside the EU, she warned.
by robin stride
Specialist medical accountants are continuing talks with the taxman aimed at preserving independent practitioners’ right to incorporate their businesses.
Nearly 30 accountancy firms are now backing plans to form a special interest group to represent consultants’ and private GPs’ financial interests in talks with HM Revenue and Customs (HMRC).
The group, first unveiled in an Independent Practitioner Today front-page story three months ago, was set up informally after a wing of HMRC claimed independent practitioners were reaping unfair tax advantages by incorporating their businesses and, additionally, selling goodwill.
Accountancy firms then agreed to set up a new working party to strengthen their negotiating arm
with HMRC on tax matters affecting independent practitioners and to agree accounting standards for consultants.
A draft constitution is now being circulated and the HMRC is reportedly keen to have a forum through which it can talk to the profession’s representatives.
But at a meeting with consultants’ accountants over the summer it emerged that all professions who use companies as a trading vehicle are being scrutinised.
Specialist medical accountant Ray Stanbridge said: ‘Basically, the Revenue said they don’t believe any profession can trade as a company – that includes doctors, accountants, solicitors and vets.
‘But we said there are something like six million companies run by professionals in the UK and they employ 14m people.
‘If they’d had to build these
firms up and pay 50% tax instead of 20%, then they wouldn’t have had the money to do it. There are a whole lot of other reasons why people go into companies too.’
He said accountants at the meeting ‘were incredulous’ at what they heard from the tax officials, who are operating the Government’s new anti-avoidance policy.
Mr Stanbridge said successive governments had encouraged people to go into companies because they wanted to encourage businesses.
It is believed some smaller accountancy firms, who have limited experience of selling the goodwill in consultants’ practices, could be singled out for scrutiny. Could you be affected? Don’t miss Independent Practitioner Today’s special feature in next month’s edition

The Harley street clinic’s new chief executive, aida yousefi (left), has paid tribute to the people who have had a groundbreaking influence on making the hospital a private flagship. Formerly chief operating officer at the clinic, she called it ‘a huge privilege to be taking over one of the country’s leading private tertiary hospitals’.
ms yousefi said: ‘we have an outstanding team of some of the country’s most senior specialists, nurses and technical staff and a history of ground-breaking medicine both for adult patients and for children.
‘no other private hospital can match this record of bringing new treatments to the uK, particularly in the area of paediatric cardiac medicine.’
she was acting chief executive and succeeds neil buckley after his appointment as chief executive of The wellington Hospital, london.
ms yousefi added: ‘our specialist medical teams are supported with technology that is the most extensive in the uK and the demand for our services continues to grow. i cannot imagine a more exciting period to take over the reins of such an outstanding world-class institution.’
she was for some years the director of the Hca cancer network, the largest provider of cancer care outside the nHs
By a staff reporter
Medics are overwhelmingly backing calls for training in the cosmetic surgery sector to be the responsibility of existing professional associations.
New educational standards for procedures are expected this month from Health Education England following a Government review which concluded that practitioners performing aesthetic treatments must undergo ‘appropriate’ training.
But 500 surgeons, doctors and nurses surveyed by The Clinical Cosmetic and Reconstructive Expo, running from 10-11 October at London’s Olympia, strongly agreed that their professional bodies must be in charge of delivering training for procedures.
The associations would include
the British Association of Aesthetic Plastic Surgeons (BAAPS), the British Association of Plastic, Reconstructive and Aesthetic Surgeons (BAPRAS), the British Association of Cosmetic Nurses (BACN) and the British College of Aesthetic Medicine (BCAM).
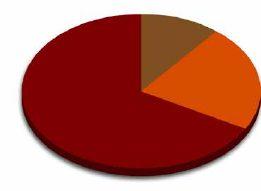
Under 3% of those surveyed felt it was the Gov ernment’s remit and less than 4% felt it should be private hospitals and clinics. One in five suggested a combination of the private sector and NHS could be successful.
As well as medics, OnePoll also surveyed 2,000 women on their views about minimum qualifications for aesthetic practitioners.
The views they expressed on different subjects are:
❐ Injections: Although one-day and weekend courses are the most prevalent educational programmes
Medical insurer AXA PPP claims it has to overhaul its fee schedule and introduce contracts with specialists in order to stop high costs depressing the market.
It wants to see 30% of its members using fast-track by the end of 2015, then later more than half, although it would not be drawn on a percentage.
The insurer added: ‘Fee-approved specialists who enter into a contract with us are required to charge fees in accordance with the fees they have agreed to, as part of their contract.’ These fees were higher than those in the revised schedule.
Commercial director Fergus Craig said private medical insurance demand had declined for a sustained period and premium affordability
look out for Independent Practitioner today’s stand at CCR expo.
Olympia will showcase more than 120 international exhibitors: from cutting-edge surgical equipment and supplies through to non-invasive products, business services, training and consultancy. It offers up to 14 days of content for continuing professional development, including workshops, conferences and live demonstration theatres. www.ccr-expo.com
for facial injectable treatments like dermal fillers and Botox, almost universally they were panned as inadequate by public and profession.
Twenty-nine per cent of the medical community felt a minimum three-month specialist course should be required and the public (27%) felt at least six months was needed.
❐ Lasers and non-surgical lipo: Three months was also overwhelmingly felt by the profession to be enough to train to be able to provide laser procedures such as for acne, skin rejuvenation and hair removal.
But opinion was split among clin icians on non-surgical lipo, such as radiofrequency or fat-freezing. Thirty-one per cent deemed a weekend to be plenty, but 29% said three-months minimum.


❐ Surgery: 74% of UK women said a procedure-specific credential – nose jobs, eyelid surgery or facelifts – would increase their level of confidence in undergoing surgery by plastic surgeons. Over a third of the profession agreed this would stop ‘jacks-of-all-trades’. Forty-eight per cent of the profession felt newly-qualified plastic surgery consultants were not competent enough to perform cosmetic surgery procedures. Fewer than 7% felt NHS training alone was sufficient.
Consultant plastic surgeon Mr Norman Waterhouse, CCR Expo’s medical advisory board chairman and a former BAAPS president, said: ‘It is essential that practitioners restrict themselves to procedures with which they are trained and familiar and, as the survey shows, patients expect no less.’
was a ‘challenge’ for individual customers and employers.
‘Alongside this challenge, the Competition and Markets Authority has called both for an improvement in the information available to patients on the clinical care they receive and for greater certainty to private patients that their healthcare costs will be met in full by their insurer.
‘In this environment, we must secure the best possible value for our members to protect their interests, now and in the future, and to ensure that the private medical insurance market is maintained for the benefit of insurers and providers of healthcare services alike.’
AXA PPP said it was continuously working with hospitals to secure cost-effective, quality care.
Advertising watchdogs have ruled an advert claiming a clinic was ‘setting the gold standard’ should not appear again.
The advert from Aesthetic and Cosmetic Surgery Ltd, trading as The Harley Medical Group, appeared on a website, a banner ad on YouTube and in a magazine.
But the PIP Action Campaign challenged if the claim was misleading and could be substantiated and the Advertising Standards Authority (ASA) upheld the complaint.
ASA said Aesthetic and Cosmetic Surgery Ltd submitted it was confident it had provided the best quality of care to patients
throughout its trading history and always had skilled surgeons, expertise and patient care.
But it ruled it considered that, without qualification, consumers would understand the claim ‘setting the gold standard’ as an objective claim that Aesthetic and Cosmetic Surgery Ltd had been achieving the highest attainable standard as agreed by independent measures on areas such as patient care and surgical expertise.
‘Because objective evidence was not supplied to demonstrate that Aesthetic and Cosmetic Surgery Ltd had been “setting the gold standard”, we concluded that the ads were misleading.’
By Robin Stride
Four in ten business leaders claim the main barrier to offering their staff private healthcare is the expense.
But 28% would be more likely to pay for it if it was cheaper and 17% would do so if they believed it was better value, according to a survey.
Over half (55%) of the 1,081 decision-makers surveyed told the YouGov online research for Bupa that the sector lacked transparency, such as on quality.
The findings follow a call by the Competition and Markets Authority for more information on the
A new online resource to support doctors in their day-to-day care of older patients has been issued by the GMC.
The council said it had worked closely with partner organisations, including the British Geriatrics Society and Age UK, to create Better care for older people
The resource gives practical advice, including from leading clinicians, and shows how to use GMC guidance to handle patients’ clinical, emotional and psychological needs.
At the core of the resource is a
quality and value provided by the private healthcare sector.
Bupa Health Funding managing director Dr Damien Marmion said the research showed a strong appetite for private healthcare from employers – who pay for 75% of people covered by private medical insurance (PMI) – and employees.
But despite the UK’s economy starting to recover, there was no sign of growth in private healthcare. He believed the sector could grow but only if everyone focused on what the customer wants. For many would-be customers, this came down to cost.
The Bupa boss urged everyone
series of videos featuring interviews with older patients who talk of their experiences of dealing with doctors.
The resource also contains a mixture of guidance, case studies, scenarios, articles and tips to prepare doctors for caring for the growing number of older patients.
Over-65s make up over twothirds of NHS patients in the UK and there are now more people living with multiple, long-term conditions than ever.
GMC chief executive Niall Dickson said: ‘We hope these learning materials will stimulate discussion and help to support doctors working with older people.
‘The reality is that most medical care is already centred around later life and, in the future, this is going to be even more the case.’
Better care for older people will be regularly updated. Go to www. gmc-uk.org/oldercare.
to play their part to demonstrate to more customers that the private healthcare sector offered good value and quality healthcare.
Dr Marmion said: ‘Doctors in private practice and other clinicians have a key role in driving quality and value.
‘Many medical innovations and procedures can be cost-reducing or cost-neutral, and I urge clinicians to take a lead on finding creative ways to promote efficient medical practice that maintains excellence and reasonable clinical freedom.’
He called for private healthcare to be made ‘a beacon of excellence and value’, arguing that this
would see many more doctors enjoying a thriving private practice and more patients feeling the private healthcare’s benefits.
Dr Marmion said the cost barrier was why Bupa was pushing for the publication of outcomes from hospitals and consultants while seeking price cuts of up to 15% or more from some major hospital providers.
Costs were also a prime issue for potential younger PMI customers, he added: ‘Some 50% told us that the main barrier to having private healthcare was cost. And over a third (37%) would be more likely to have private healthcare if it was more affordable.’
Energetic doctors, nurses and staff are having little rest after helping London’s Wellington Hospital hit its £1m appeal target – because now they are doing it all again.
Money raised from the first appeal went to the Junior Diabetes Research Fund (JDRF) and The British Red Cross appeal for AIDSaffected children in South Africa.
Now both charities could see The Wellington’s contributions doubled after chief Mr Neil Buckley (right) announced the new target.

events led by the hospital’s then chief executive Keith Hague. These included cycling marathons in the UK and on the Continent, climbing Britain’s highest peaks, abseiling down multi-storey buildings, and a sponsored drive around the coast of Great Britain in a classic VW campervan.
For the first million, doctors, nurses, staff and others from around the HCA group, which owns the hospital, held sponsored
At a House of Lords reception to celebrate the unique fund-raising achievement, Lord True congratulated the fundraising team and said he found their ‘amazing success’ was inspiring.
Mr Hague thanked all the supporters and fundraisers and his successor.
Any independent practitioner receiving an Accelerated Payment of Tax notice is being advised to act fast.
Individuals and companies will be expected to pay tax up-front if HM Revenue and Customs believes they have invested
money in a disputed scheme. They will normally have just 90 days to pay.
Previously, the legal challenge process could mean many years of not paying tax before the courts decided the tax was due, freeing up that cash in the meantime for tax-
payers to make other investments.
International tax adviser Simon Concannon, of Leeds-based law firm Walker Morris, said: ‘If a challenge or appeal is eventually successful, the money will be returned, but the process and timings have been turned on their
head. You pay out at the start of the legal challenge – which takes away some of the incentives for these schemes.’
He warned anyone receiving a notice to act on it and if they thought a mistake had been made, then to quickly appeal.
By Robin Stride
Consultants at London’s independent mental health hospital Capio Nightingale are being promised more investment in services and new opportunities following a takeover.
French company Groupe Sinoué, a private mental health care specialist, bought the hospital in July.
Florence Nightingale Hospitals Ltd managing director Martin Thomas told Independent Practitioner Today it was ‘business as usual’ at the hospital and the sale would make no difference to its day-to-day running.
He added: ‘The sale brings investment into the services currently offered at the hospital and will support the progression of consultants already working within Nightingale Hospital.
‘We will be urging the consultants to collaborate with their new colleagues over in France to draw on the shared expertise and knowledge, networks and research.’
Mr Thomas said the hospital was continually creating opportunities for new consultants to join the team and those who thought they could bring innovation and skill to the Nightingale should contact him or medical director Dr William Shanahan.
Capio Nightingale Hospital said it was an attractive proposition for Groupe Sinoué; the hospital has achieved over 20% sales

growth in the past four years and will account for a quarter of the Groupe Sinoué turnover.
The acquisition is the first UK venture for the group, founded in 1989 by consultant psychiatrist Dr Philippe Clery-Melin, who is now the president of the company that has eight hospitals in France, delivering the full spectrum of psychiatric care.
Groupe Sinoué has expressed support for the continuing development of Capio Nightingale’s portfolio of treatment centres and programmes, in addition to its core services of general and adolescent psychiatry, eating disorders and addictions. As a result of the sale, the hospital will rebrand over six months as Nightingale Hospital.
Dr Clery-Melin called the acquisition ‘a fantastic opportunity’, as Capio Nightingale Hospital, with its many leading consultants, was an ideal complement to his group’s existing clinics.
‘It also represents a great opportunity for our consultants and professionals to co-operate with
the capio nightingale is being rebranded as nightingale hospital
Specialist financial planners are advising senior doctors to take action to prevent their savings being eroded by inflation.
Despite the media fanfare surrounding the launch of New Individual Savings Accounts (NISAs) in July, the current interest rates make this cash savings option appear less attractive, warned Cavendish Medical.
Nightingale’s expert team over new care programmes and clinical innovation.’
The group said the sale ensured the Nightingale Hospital’s stability and ensured it continued to offer high-quality private services without the need to open out to patients on the NHS.
the Sinoué group is a healthcare company specialising in the field of psychiatry and mental health. it is based ‘on a philosophy of high-quality medical care, which aims to deliver innovation in its healthcare services’.
the group cares for patients from across europe and was founded by psychiatrists, led by dr philippe clery-Melin, its president of 12 years. it is still majority family-owned. it has developed its medical and managerial expertise to bring forward new offerings in health and the field of psychiatry.
The Healthcare Management Trust, owners and operators of Swansea’s Sancta Maria Hospital, plan to move it to a purpose-built
site outside the city. They believe moving to new purpose-built facilities will ensure the hospital continues to provide a full range of medical services and expects the venture to create new jobs.
Chief executive Tony Barrett said: ‘This ambitious develop -
ment will ensure that patients across Swansea and west Wales continue to benefit from access to leading clinical services within a facility designed to offer the very best patient experience.’
See ‘Varsity link gives unit access to best scans’, page 8
The company said senior doctors will find it very difficult to find accounts, even tax-exempt, that exceed the rate of inflation.
Currently, the best variable cash ISA interest rate is around 1.5%. But the consumer prices index (CPI) rate of inflation rests at 1.6% (down from 1.9% in June) meaning the savings of all doctors are still shrinking in real terms. At the moment, banks do not need to rely on savers’ deposits to fund their lending and are obtaining cheaper funds from other sources. So they are happy to make their accounts less appealing to customers.
Cavendish Medical’s managing director Simon Bruce told Independent Practitioner Today: ‘The rate cuts do not just affect the new ISAs opened last month. Doctors should make a concerted effort to check all historical bank accounts.
‘What interest rate are you getting and is it time to switch? There are better rates around but these may involve fixed deals for a minimum of one year.’
Bank of England governor Mark Carney recently implied a base rate rise would come towards the end of the year.
Although he has predicted a return to the days when 3% is the norm, the first rate rises – whenever they appear – may not be big.
Mr Bruce said: ‘Everyone needs a rainy day fund, but managing larger cash balances on deposit to stay within the protected limits can become problematic. Doctors need to check if these funds could be working harder for them elsewhere.’
By charles king
Consultants and private hospitals are hoping to benefit from a £250m NHS cash injection aimed at clearing the NHS backlog for knee, hip and cataract operations.
Some observers believe that independent practitioners could also benefit from self-payers because to achieve the target will mean a temporary rise in patients waiting over 18 weeks.
The Association of Independent Healthcare Organisations (AIHO) said it has been working with NHS England and Monitor on the independent sector’s ability to deliver capacity for NHS services.
AIHO chief executive Fiona Booth told Independent Practitioner
Today : ‘The independent sector provides vital capacity for NHS services by undertaking diagnostic and treatment activity to NHS patients at a price set by the NHS.
‘We note the Secretary of State’s focus on waiting times, and the independent sector is well placed to help reduce the amount of time that patients have to wait for treatment.
‘The sector will continue to coordinate with the NHS, playing a vital role in reducing waiting lists and providing excellent care.’
A quarter of NHS trust finance directors expect to overspend their budgets this year, according to the latest quarterly monitoring report from The King’s Fund, as a result of growing financial pres -
sures and rising demand for services.
Over three million people had been waiting at least 18 weeks for hospital treatment at the end of the last quarter, the highest number since 2008.
The number of patients waiting more than six weeks for diagnostic tests stood at more than 18,600 at the end of May 2014, nearly 12,000 up on the same month last year.
The fund’s chief economist John Appleby said: ‘Our latest quarterly report paints a picture of a service under huge pressure, with cracks beginning to appear in NHS performance. It once again underlines the need for new funding if services are to be maintained.’
The new executive director of the 52-bed BMI The Runnymede Hospital in Chertsey, Surrey, is Leon Newth. He was previously commercial finance manager at the hospital from 2007-09.
For the last two years, he has been executive director for BMI Syon Clinic, Brentford, and BMI Coombe Wing, Kingston.
Mr Newth (pictured) said he was determined to continue the good work already in place to improve the hospital’s services and to help grow its relationships with local NHS providers and commissioners.

Mechanical engineers are warning of a threat to both the UK’s excellent academic research in the field of biomedical engineering and the resulting inventions of medical devices.
Too often the results of research are sold to international corporations for development and marketing because of the lack of long-term domestic venture capital, they say in a report.
According to the Institution of Mechanical Engineers, the development of many technologies – in particular m-health and e-health
– are also being hampered by a lack of international consensus on standards, practices and patents.
The body is calling for biomedical engineers to be given a bigger influence in the NHS to help cut the number of incidents caused by faulty medical equipment.
The institution said: ‘In 2013, 13,642 incidents related to faulty medical equipment were reported to the Medicines and Healthcare products Regulatory Agency (MHRA); leading to 309 deaths and 4,955 people sustaining serious injury.
‘These incidents can vary from faulty pacemakers to faulty equipment like CT or MRI scanners used to diagnose patients. This faulty equipment, or the unavailability of equipment, is also one of the major causes of cancelled operations.
‘As the technology used in hospitals becomes increasingly complex, the danger of improperly calibrated and validated equipment is also increasing.’
Dr Patrick Finlay, chairman of the Institution of Mechanical Engineers’ Biomedical Engineer ing
Association, said: ‘Technology is leading to huge advances in healthcare, but this technology is dependent on the work of biomedical engineers who are inadequately recognised and in short supply in most hospitals.
‘Clinicians and engineers need to work in partnership to ensure that advances in medical technology are applied in the best interest of patients.
‘The benefits of hospitals having a designated chief biomedical engineer responsible for healthcare technology are clear.’
Vasectomy inquiries in the UK have risen 164% in the past 12 months, according to research from private healthcare search engine, WhatClinic.com.
Vasectomy reversals are also on the rise, with searches almost doubling in the past 12 months.
Surgeons surveyed said the most
common age of men opting for a vasectomy is 41-45, although one in three are under 35. The youngest request for a vasectomy came from an 18-year-old and the oldest was well into his seventies.
For reversals, the youngest patient treated by the surgeons polled was 21 and the oldest 66.
Nearly all (98%) of the surgeons asked cited the most common reason for vasectomy reversals as patients wanting to start a family with a new partner, following a divorce or separation.
Waiting lists in the NHS can be several months, which is why some men go private. Private
vasectomies cost an average of £515, while reversals cost £2,582 – and are not available on the NHS.
WhatClinic.com is advising patients to do their research, ensure they find a clinic they are comfortable with and always read patient reviews.
By a staff reporter
Doctors’ defence body subscriptions are facing further pressure following a shock 20% rise in claims.
The Medical Defence Union (MDU) revealed that reforms aimed at reducing high claimant’s legal costs had lead to the surge.
In its Annual Report for 2013, it noted that legal changes affecting the amounts claimants’ solicitors could expect to be paid were introduced in April last year.
But as lawyers realised they were going to have to reduce their fees in future, they ‘rushed to take on claimants under the old arrangements which led to a surge in cases’.
MDU chief executive Dr Christine Tomkins said last year was its busiest in its 128-year history as staff answered more than 33,000 calls from members and opened a record number of new claims files.
A major factor in the increasing demand for its services was the rise in the number of new claims against members.
She said: ‘We fully support the legal costs reforms that came in to effect in April 2013, but in the
short term, we have seen claimant’s solicitors rushing to notify claims under the old arrangements, prolonging the disproportionately high costs the legal changes are intended to address.
‘Clearly, it is important that patients have access to justice if they believe they have been negligently harmed, but the system must be fair.
‘We are hopeful that, in the longer term, the changes will see a reduction in the large sums paid to claimants’ lawyers. There is some evidence that this is starting to happen with the numbers of claims being notified against our dental members slowing slightly towards the end of 2013. We hope this trend will continue and spread to medical claims.’
Dr Tomkins said compensation payments were also ‘spiralling’.
She said the MDU was working at Gover nment level to effect changes to control claims inflation so damages payments were affordable, sustainable and fair for all parties.
The MDU said it successfully defended 70% of medical claims where the doctor was accused of negligence and faced a compensation demand.

CUT OF THEIR JIB: Spire Liverpool Hospital orthopaedic surgeons (from left) Mr John Davidson and Mr Peter Brownson with crew enjoyed a day off work taking part in the JP Morgan Round the Island Race, circumnavigating the Isle of Wight. Light winds led to their early retirement, but at least they enjoyed close-up views while being passed by the Queen Mary II
Nuffield Health has bought nine Virgin Active Health Clubs – with five of the gyms being within 4.5 miles of a Nuffield Health Hospital.
The purchased clubs are in Birmingham Broadway Plaza, Gloucester Barnwood, Guildford, Ilford, Milton Keynes, Manchester Printworks, Taunton, Tunbridge Wells and Wolverhampton.
Dr Andrew Jones, managing director of the firm’s Wellbeing wing, said the acquisitions were an important step towards achieving the aim of a national network of fitness and wellbeing facilities.
‘The locations of the gyms allow us to either reach parts of the country that we do not have a presence in or to complement our
current offering in the area, whether that be a hospital or corporate wellbeing facility.
‘This will enable us to deliver healthcare across the UK and, by combining services and experts at our co-located facilities, support more local people with an integrated health and wellbeing proposition.’
The firm said it would introduce new services, including a free health MOT for every member and access to health mentors, physiotherapists and nutritionists.
Its 60-minute check measures waist-to-hip ratio, blood pressure and glucose, aerobic fitness, total cholesterol, sleep, stress, alcohol consumption and smoking habits and assesses fitness progress.
Sancta Maria Hospital, Swansea, has partnered with the Institute of Life Science (ILS) at the city’s university to offer its patients CT and MRI scanning facilities.
The partnership will see patients of the Glamorgan hospital having access to ILS’s on-site MRI and CT scanning equipment, including the 3-tesla MRI scanner, which offers two to three times the signal of ordinary scanners.
The ILS is the research and innovation arm of Swansea University’s College of Medicine.
Consultant spinal surgeon Mr Navin Verghese said the new partnership now allowed him to rapidly refer patients to undergo investigation ‘on our doorstep’, using the most sophisticated scanner in Wales.
He said: ‘I have a number of new patients presenting to my clinic
who have been suffering with long-term symptoms related to neck or back issues. Not uncommonly, their past scans had not shown any significant abnormality, but with the use of the innovative ILS scanner, we can now locate even the smallest abnormalities within the spine, which could be causative to the patients’ pain.
‘From a consultant’s point of view, this will now allow me to
deliver an optimal treatment plan focused on the patient’s symptoms and the abnormalities identified with the 3-tesla scan.
‘This could include more targeted physiotherapy and conservative measures, but occasionally could mean the difference between a patient being discharged or being admitted for potentially life-changing spinal injections or surgery.’
By Edie Bourne
Doctors have been urged by a defence body to stop prescribing drugs for family or friends overseas.
According to the MDDUS, it has dealt with a growing number of cases where doctors have faced GMC sanctions for prescribing drugs to those close to them, with some incidents involving medication issued to relatives living abroad.
But it warned that this practice brought added risks relating to laws on the import and export of medications as well as concerns over doctors’ access to the full medical history of patients outside the UK.
GMC fitness-to-practise proceedings have been raised against doctors for prescribing friends or family with drugs such as benzodiazepines and opiates as well as antibiotics and non-benzodiazepine hypnotics.
Medical adviser Dr Naeem
Guidance has been published to answer patients’ queries about travelling overseas for treatment.
The Patients’ Guide to Treatment Abroad is an editorial-based e-book, available as a free down load from www.treatmentabroad. com/medical-tourism/magazine.
Published by www.treatmentabroad.com, it is also available in print form and covers questions such as:
Will the NHS pay for your surgery abroad?
How much can you save by travelling overseas for treatment?
Is it safe to go abroad for treatment?
How do I choose a hospital or clinic?
Nazem said doctors should exercise caution in prescribing for friends or family, only doing so when absolutely necessary and based on clinical need rather than convenience.
‘It may be difficult to justify these actions with the ready availability of out-of-hours services, walk-in centres and A&E departments. The first issue to consider is the GMC’s guidance, which states doctors must, wherever possible, avoid prescribing for themselves or those with whom they have a close personal relationship.’
MDDUS said some doctors had sent drugs overseas to relatives or friends, which raised a number of important issues.
Dr Nazem said: ‘Treating family or friends abroad has additional complications. Doctors must consider the safe storage and transfer of prescribed medicines as well as the UK regulatory framework for the export of medicines and the import regulations of the recipient country.
The guide explores a number of the most common treatments that patients seek overseas, including eye surgery, infertility treatment, orthopaedic surgery, dental treatment and cosmetic surgery, highlighting some of the leading clinics in different countries for each type of treatment.
It also includes a check list for patients considering cosmetic surgery abroad, including questions to ask surgeons, plus things they should research before making a decision.
A spokesman said: ‘Our aim with this guide is for those patients thinking about going overseas, whether for medical treatment like hip replacement or fertility treatment or for a cosmetic procedure, to make an informed choice.
‘There are so many options for treatments, destinations and hospitals that it can be easy to be swayed by special offers or the “easy choice”.
‘Armed with this guide, patients can make the right decision for themselves and their bodies.’

‘In addition, doctors can encounter difficulties in prescribing for a patient they are unable to meet. In particular, doctors may not have access to the patient’s full medical history or their current medication.’
MDDUS has also handled cases involving doctors prescribing controlled drugs for family members. Dr Nazem said: ‘GMC guidance on prescribing controlled
drugs to family and friends is clear – yet we have dealt with cases where GPs have prescribed opiates, for example, for their wife or husband.’
‘We encourage doctors to play it safe and avoid diagnosing and treating themselves or loved ones with medicines. Otherwise, they may be called upon to justify why it was necessary for them to prescribe rather than the patient’s regular doctor.’
He added: ‘Doctors should recognise that self-prescribing drugs of dependence such as opiates or powerful painkillers is entirely unacceptable.
‘In some cases, pharmacists have refused to dispense the medication, but MDDUS has also encountered situations in which the pharmacist has dispensed the prescription and then reported the doctor to the GMC.’
GMC guidance Good practice in prescribing and managing medicines and devices can be found online at http://bit.ly/1nWOgar
Specialist eye hospital group Optegra has opened up its first specialist eye hospital in Asia, with the acquisition of New Vision Eye Clinic in Shanghai, China.
The purpose-built hospital has three surgical suites, 15 consulting rooms and 11 examination rooms.
Optegra, which aims to be ‘the world’s most trusted choice for eye care’, owns 24 hospitals, six in the UK. This launch is the first outside Europe.
Dr Michael Gu, managing director at New Vision Eye Clinic, said: ‘Because of our broad service offering and also payment options, our patients come from a wide variety of socio-economic groups and ages.
‘We see a large number of selfpaying patients, as well as privately insured patients and patients covered by government social insurance (Shanghai
HealthCare Insurance). Whereas in the UK there is a very clear divide between NHS and private hospitals, in Shanghai the mix is slightly different.’
John Behrendt, chief executive of Optegra’s owners Moonray Healthcare, said: ‘Shanghai has the largest population of any city in the world, estimated at around 24m people. That’s roughly the same as the total number of men in England (26m), and so it is a significant business opportunity for Optegra in a large and growing market.’
China’s private healthcare market is expanding rapidly, with central government encouraging private investment in healthcare to increase overall quality and choice of medical services and also to ease pressure on government hospitals.
Independent providers are preparing to meet the challenge of a paperless NHS. Sally Taber reports
Private hos P itals are being proactive in preparing for a healthcare system where digital technology will underpin the patient pathway across the two sectors.
a survey by the i ndependent healthcare advisory services’ it Council, a division of the association of independent healthcare o rganisations ( aiho ), recently shows some encouraging progress in small and large hospital groups.
i n January this year, h ealth secretary Jeremy hunt called for the Nhs to go paperless by 2018 and thereby realise savings of billions of pounds, improve services and meet the challenges of an ageing population.
We already do with most NHS commissioners
We could adapt our IT system readily, but would have to devote scarce resources to meet NHS requirements
We would probably stop accepting NHS commissions
s ubsequent announcements have focused on being more inclusive and engaging with a wider stakeholder group.
Dame Fiona Caldicott, the chairwoman of the now closed National i nformation Governance Board, had previously expressed her concerns about information governance in a paperless system
But however long the process takes to reach fruition, it is clear that the independent sector must prepare itself to interact with an increasingly paperless Nhs the it Council, under the chairmanship of s pire h ealthcare’s Martin r ennison, recently conducted a ‘state of readiness’ survey of its members in england.
it was pleased to note that the vast majority of aiho members already have:
a fully thoughtthrough plan for improving clinical recordkeeping and patient communication, or;
a re investigating changes as part of a wider improvement plan.
Given the mantra of ‘the patient at the centre’, ensuring a smooth digital transition from the Nhs to the independent sector and back again is critical.
eighty per cent of aiho members have reported that they already ‘mostly’ received patient referrals from clinicians in a digital form.
the three specific digital challenges for independent providers treating Nhs patients are:
1 Digitally assimilating N hs referrals into their own records;
2 Maintaining records of an episode that conforms to N hs standards and can be accepted into N hs individual patient records;
3 Being digitally aware of the patient’s complete treatment pathway and having the treatment provided by the independent provider identifiable.
l ooking towards interacting with an entirely paperless Nhs, 88% of aiho members responded either that they already do so with most Nhs commissioners or that could adapt their it systems fairly readily.
h owever, respondents highlighted the financial investment required to adapt their it systems.
i n terms of relationships between the independent sector and Nhs commissioners, it was disappointing to note that only 33% of aiho members would recommend their communication model with Nhs commissioners as a model to follow.
t his is obviously an area that requires both sectors to work together for the good of patients. overall, the survey was a useful exercise to check progress along the path of moving towards a paperless healthcare system. the outlook is overwhelmingly positive although there are challenges to overcome in the next few years, which the ihas it Council will regularly monitor.
Sally Taber (right) is director of Independent Healthcare Advisory Services














There’s a 1-in-4 chance of someone developing shingles during their lifetime.1 The risk increases with age, as does the likelihood of complications. 2

Year 2 of the national shingles immunisation programme started on 1st September 2014* for eligible patients. For full programme details and support items visit www.shinglesaware.co.uk
Help prevent shingles disrupting peoples’ lives
*Programme details may vary for each country. Please refer to local guidelines.
ABRIDGED PRESCRIBING INFORMATION
ZOSTAVAX® powder and solvent for suspension for injection in a pre-fi lled syringe [shingles (herpes zoster)vaccine (live)] Refer to Summary of Product Characteristics for full product information.
Presentation: Vial containing a lyophilised preparation of live attenuated varicella-zoster virus (Oka/Merck strain) and a prefi lled syringe containing water for injections. After reconstitution, one dose contains no less than 19400 PFU (Plaque-forming units) varicella-zoster virus (Oka/Merck strain). Indications: Active immunisation for the prevention of herpes zoster (“zoster” or shingles) and herpes zoster-related post-herpetic neuralgia (PHN) in individuals 50 years of age or older. Dosage and administration: Individuals should receive a single dose (0.65 ml) administered subcutaneously, preferably in the deltoid region. Do not inject intravascularly. It is recommended that the vaccine be administered immediately after reconstitution, to minimize loss of potency. Discard reconstituted vaccine if it is not used within 30 minutes. Contraindications: Hypersensitivity to the vaccine or any of its components (including neomycin). Individuals receiving immunosuppressive therapy (including
high-dose corticosteroids) or who have a primary or acquired immunodefi ciency. Individuals with active untreated tuberculosis. Pregnancy. Warnings and precautions: Appropriate facilities and medication should be available in the rare event of anaphylaxis. Zostavax ® is not indicated for the treatment of Zoster or PHN. Deferral of vaccination should be considered in the presence of fever. In clinical trials with Zostavax ®, transmission of the vaccine virus has not been reported. However, post-marketing experience with varicella vaccines suggest that transmission of vaccine virus may occur rarely between vaccinees who develop a varicella-like rash and susceptible contacts (for example, VZV-susceptible infant grandchildren). Transmission of vaccine virus from varicella vaccine recipients who do not develop a varicella-like rash has also been reported. This is a theoretical risk for vaccination with Zostavax ®. The risk of transmitting the attenuated vaccine virus from a vaccinee to a susceptible contact should be weighed against the risk of developing natural zoster and potentially transmitting wild-type VZV to a susceptible contact. As with any vaccine, vaccination with Zostavax ® may not result in protection in all vaccine recipients. Zostavax ® and 23-valent pneumococcal polysaccharide vaccine should not be
given concomitantly because concomitant use in a clinical trial resulted in reduced immunogenicity of Zostavax ® Pregnancy and lactation: Zostavax ® is not intended to be administered to pregnant women. Pregnancy should be avoided for one month following vaccination. Caution should be exercised if Zostavax ® is administered to a breast-feeding woman. Undesirable effects: Very common side effects: Pain/tenderness, erythema, swelling and pruritus at the injection site. Common side effects: Warmth, haematoma and induration at the injection site, pain in extremity, and headache. Other reported side effects that may potentially be serious include hypersensitivity reactions including anaphylactic reactions, arthralgia, myalgia, lymphadenopathy, rash and at the injection site, urticaria, pyrexia and rash. For a complete list of undesirable effects please refer to the Summary of Product Characteristics. Package quantities and basic cost: Vial and pre-fi lled syringe with two separate needles. The cost of this vaccine is £99.96. Supplier: Sanofi Pasteur MSD Ltd., Mallards Reach, Bridge Avenue, Maidenhead, Berkshire, SL6 1QP Marketing authorisation number: EU/1/06/341/011
Legal category: POM ® Registered trademark Date of last review: 25 April 2014


References 1. Miller E, Marshall R, Vudien J. Epidemiology, outcome and control of varicella-zoster infection. Rev Med Microbiol. 1993;4: 222-230 2. Gauthier A, Breuer J, Carrington D et al. Epidemiology and cost of herpes zoster and post-herpetic neuralgia in the United Kingdom. Epidemiol Infect. 2008; 137(1): 38-47
Adverse events should be reported. Reporting forms and information can be found at www.mhra.gov.uk/yellowcard Adverse events should also be reported to Sanofi Pasteur MSD, telephone number 01628 785291.
Too many consultants procrastinate when it comes to tax returns, warns Susan Hutter (below). The late filing penalty of £100 may not appear particularly expensive, but the consequences of leaving it until the last minute can be far more costly

While the deadline for filing 2013-14 tax returns to h M Revenue and Customs is not until 31 January 2015, it will come around quick enough.
By 31 January 2015, you must have all funds ready for the payment of tax relating to any balance of tax due for 2013-14 and the first payment on account for 2014-15.
the sooner it can be worked out what that tax liability is, the more time there is to plan for the actual payment.
As a rule of thumb, if the total income has increased compared to the previous tax year – that is to say, 2012-13 – there is likely to be a balance of tax to pay for 2013-14. this is because the payments on account for 2013-14 were originally based on the income received in 2012-13.
Obviously, the reverse is true: if income has decreased compared to the previous year, then there is likely to be a refund of tax for 2013-14.
if you still haven’t sent your tax
return information to your accountants, then do so as soon as possible.
A tip to bear in mind for the future: most firms of accountants are fairly quiet in the summer months of June, July and August.
So if you sent your tax return information to them during this time, you are likely to get the tax return prepared quickly which will give you time to plan the cash flow.
Also, if you are in the fortunate position to have over-provided for tax, you will know that you can release funds.
For those consultants who trade as a limited company and pay themselves by dividend, there is another angle to consider.
Your accountant will not be able to ascertain the accurate dividend position until the limited company accounts are prepared. the deadline for filing dates for limited company accounts is nine months from the year-end.






If you still haven’t sent your tax return information to your accountants, then do so as soon as possible
i f the year-end is later in the year – for example, October – they may not be finalised in time for the tax return filing deadline of 31 January 2015.
i n these circumstances, it is important to be able to provide accurate information to your accountant about the drawings you have made since the limited company’s previous year-end so that your accountant can advise you on the best dividend/salary policy for 2014-15, as this will have an effect in your personal tax return.
For those who have divided the share capital between themselves


and their spouse, it is equally important that the spouse’s tax return is prepared on a timely basis as well.
i f you do reward yourself by dividends, the dividends will be divided in shareholding ratios. if this income pushes you into the higher-rate tax bracket, extra tax will be payable.
it is sensible to look at yourself and your spouse as one ‘unit’ as far as tax return preparation and tax payments are concerned. it is the ‘family income’ that is important for tax planning purposes. if you leave everything until the last minute, it is virtually impossible to carry out sensible personal pension planning, and tax planning if you trade via a limited company.
t herefore give yourself some breathing space!
Susan Hutter is a partner with Shelley Stock Hutter LLP. She provides specialist accounting, taxation and business advice to the medical and healthcare industry
World Class International Faculty already includes:
Dr Raj Acquilla, Dr Raina Zarb Adami, Dr John Ashworth, Mr Jonathan Britto, Dr Erri Cippini, Mr Alex D. Karidis, Dr Vishal Madan, Miss Joy Odili and Dr Raffaele Rauso
CCR Expo is a major scale, multidisciplinary meeting packed with CPD accredited content for doctors, surgeons, nurses, clinic owners and other health professionals with an interest in aesthetic medicine.
From scalpel to syringe, CCR Expo provides a professional platform for the exchange of ideas, the pursuit of best practice and the sharing of knowledge, insight and expertise.
Visit www.ccr-expo.com/ipt4 to discover more.




REAlising A bUsinEss idEA
We are new, independent & free of advertising, offering Consultants a forum and a collective voice. Our technology allows you to reach more GPs & private patients, & receive online referrals.


Over the years, breast implant manufacturers and plastic surgeons have made great forward strides to refine the way they measure the breast, ensuring accuracy and an individualised result.
As a consultant plastic and reconstructive surgeon, I see a lot of women requesting breast reduction surgery because they are experiencing health problems that they think are due to having large breasts, but are actually due to wearing ill-fitting bras.
I wondered how easily surgical measuring concepts could be carried over to the lingerie industry, reducing health problems, reducing the number of surgical interventions and saving the N h S money.
having realised that what initially needed to change was the way women were measured for bras, I contacted De Montford University and was invited to speak at the 2010 lingerie-sizing seminar staged by the Association of Suppliers to the British Cloth ing Industry (ASBCI) on the theme: ‘Building an Interface Between Surgery and the Lingerie Industry’.
I had the idea that a threedimensional measuring system would be far superior to the traditional system, which is based only on two measurements.
My vision was, and still is, that we can cut down on the number of breast reduction operations by using an innovative measuring system, based on three-dimensional (3D) measurements.
Just by chance, at the British Association for Aesthetic Plastic Surgeons’ meeting in 2011, I met Sue McDonald, who is an experienced bra-fitter, and her business partner Linda Birtwistle.
Unique company
t hey had developed a 3D patented measuring system called the Optimeasure, which was similar to what I had in mind. I joined forces with Sue and Linda, and together we formed the Optifit Bra Company Ltd, which we launched at the Body Conference at the royal Society of Medicine (rSM) in 2012.
We are, I believe, the only lingerie company to launch in this manner to the surgical community.
Sue, Linda and I agree that the worldwide age-old measuring system is ineffective and completely out of date. It results in ill-fitting bras that cause functional posture problems, particularly in women with a high body mass index (BMI). Because ill-fitting bras are causing posture problems, women are suffering from headaches, back pain, neck pain and even irritable bowel syndrome. the Optifit bra and Optimeasure are truly revolutionary products that actively eliminate posture problems and dispose of the myth that a bra can fit properly based on just two measurements– one from around the ribcage and one from around the fullest part of the breasts. t his is an archaic measuring system and antiquatedly based on how soldiers were measured for uniforms during World War I. We create our bras based on 3D measurements, which can be ➱ p16



Avoid unnecessary payment
• Endorsed by all main Private Medical Insurers • An invaluable tool for your billing process to be as professional and efficient as possible
taken by the customer in the comfort of her home, taking into consideration the woman’s frame, depth and volume.
the Optifit bra does not require an underwire and it sits low on the back, elevating the breast, thus promoting better posture and a slimmer profile.
this, as well as being more comfortable and aesthetically pleasing, has meant an alleviation or complete disappearance of symptoms for a lot of women.
the Optifit bra has been gratefully received, and has had a lot of coverage in the press as well as being shown on the BBC tv show Dragons’ Den . It requires nerve and a firm belief in your product to enter in front of these entrepreneurs and investors.
It was an incredibly positive experience, and I take pride in the fact that I am probably the only plastic surgeon to have appeared on this popular programme. Following the show, our sales and queries rose considerably and are still on the up now.
loyal customers
We have a loyal customer base and although most sales are on the internet, people come from all over the UK to our shop in Saddleworth, Manchester, for a personal fit. We even had one lady pop in on her way from Italy to the Lake District, proving that an international customer base isn’t outside the realms of possibility.
I feel it is important to carry out clinical trials on women to find out what works and doesn’t work for them. My studies include research on bariatric patients and, more recently, 3D imaging of the support provided by the Optifit bra versus the support provided by traditional bras. through 3D scanning, using Birmingham Dental hospital’s medical photography team, preliminary results of a trial comparing subjects with their conventionally fitted bra and the Optifit bra have conclusively shown that an Optifit bra provides better support than a traditional bra.
t he Optifit bra provides a higher surface area contact, thus support all over breast area. the histograms back up our theories and prove categorically that traditional bras, even in large cup
sizes, do not conform anatomically to women’s bodies.
they demonstrate that the lateral chest wall is compressed within a traditional bra even when appropriately fitted, particularly for those with a high BMI.
this does not happen with an Optifit bra, as it does not compartmentalise the breast, but gives appropriate support to the lower pole of the breast.
I have also conducted a study on bariatric patients, entitled ‘Should the Breast Fit the Bra or the Bra Fit the Breast?’, the results of which I released at the British Obesity and Metabolic Surgery Society annual meeting earlier this year.
the study showed that 100% of women in the study group were wearing ill-fitting bras, with twothirds experiencing functional health problems because of this.
t hese are simply astounding findings. Put simply, over a third of the patients who were suffering ill health due to breast size would change their minds about having surgery if they could find a supportive garment that would alleviate their symptoms.
During the study, I coined the phrase ‘bra slide’, which is when the inferior part of the bra that sits on the chest wall migrates due to the mismatch of cup diameter to breast base.
this would not happen using a three-dimensional measuring system and a product that took that into account. Some of the ladies’ health issues were being exacerbated due to ill-fitting bras, while others had health problems that were caused entirely by the garments.
these problems could be alleviated if these women were being measured correctly and provided with a bra that fits them properly.
We also presented the findings of an independent survey at the r SM that showed that, of those who purchased the bra for health reasons, 83% found it improved posture and 72% felt it improved their functional problems.
It is well known that, statistically, 80% of women wear the wrong size bra, and all overweight women in my studies were wearing bras that didn’t fit.

the majority of women I see in my clinic feel that breast reduction surgery is the only answer, but I have found through research and studies that it is not. From a business perspective, the problems I encounter are because people seem to think that having a bra that fits them properly does not matter. It DOeS matter. this is all about education and change. People do not realise the extent to which an ill-fitting bra can cause problems.
Manufacturers know that women will go from shop to shop buying numerous bras and if the bra does not feel comfortable or causes problems such as straps digging in, bra slide or discomfort, they will just go to another shop or find another brand and buy a different style, shape or size. What is out there in the shops for the female public is – quite literally – not fit for purpose. In fact, I question whether women actu-
ally exist whose measurements conform to many of the large bras currently available in the market. this makes me wonder why we haven’t incorporated a threedimensional measuring system before; women’s shapes are changing, yet they are still being measured using this faulty system.
For larger women in particular, a three-dimensional measuring system is the only way in which they will be able to get proper support from a bra.
Statistics show that this could save the NhS millions of pounds in breast reduction surgery operations, and it is now all resting on the ability to convince people to change and believe in the science. traditional bras generally are not based on science, yet doctors will send their patients to highstreet stores to purchase something that has been designed for
What is out there in the shops for the female public is – quite literally – not fit for purpose
aesthetic purposes. Yet when I speak about Optifit, the first thing people always ask about is the scientific evidence behind it. the applications of my research are vast – sports science, for example. A traditional bra simply does not give the level of support that an athlete requires, and proving through scientific evidence that a three-dimensional measuring system and revolutionary bra-style can offer this support will show the industry that there are other options out there.
this bra has been found to be helpful as a maternity bra and also post-surgery. In the future, we will undertake further studies with regards to posture. t he research will continue and the Optifit Bra Company will, hopefully, continue to grow.
Mr Atul Khanna (right) is a consultant plastic and reconstructive surgeon in Birmingham
● Single-use
● High quality
● Excellent service
● Delivers the clinical value you need




Patient safety in private hospitals has been in the news following a controversial report from an independent think tank. Independent Practitioner Today looks at the claims, the inferences, and how the sector has been responding
Private hos P itals have expressed severe disappointment over an independent think tank’s decision to come out with a report questioning patient safety in the independent sector.
a ccording to the boss of the association of independent healthcare o rganisations ( aiho ), the claims are ‘questionable’, while one hospital chief executive expressed dismay about t he Centre for health and the Public interest’s (ChPi) ‘negative conclusions’ of its report.
Nuffield health Group’s David Mobbs voiced disappointment at the report’s inference that, in the absence of information similar to the Nhs, there must be increased risk.
he said Nuffield would have been happy to share data with the ChPi to support the report, but was not asked. ‘indeed, we would welcome the opportunity for followup discussions with any organisation in order to move the information transparency agenda forward.’
aiho chief executive Fiona Booth said: ‘We’re disappointed that the ChPi has chosen to publish what appear to be questionable claims about the quality of healthcare offered in independent hospitals.
‘the reality is that these institu
tions offer very high levels of care to N hs , insured and self paying patients, a fact that has been and continues to be independently verified by the the Care Quality Commission (CQC).
‘ t he independent sector acknowledges that we need to publish more data, and we have been working with the Nhs to do so in a way that enables patients, clinicians, regulators and other interested parties to make direct and meaningful comparisons.
‘ t he sector has established an independent body, the Private healthcare information Network (PhiN), to go further than this to help patients make informed choices about their care.’
Reaction from the industry’s umbrella organisation
aiho, the private hospitals’ trade body, dealt with the report’s claims in turn:
1‘Patients undergoing operations in private hospitals may be put at risk from inadequate equipment, lack of intensive care beds, unsafe staffing arrangements, and poor medical record-keeping.’
aiho commented: ‘ t he CQC regulates both Nhs and independent hospitals, and conducts regular inspections of institutions in
We’re disappointed that the ChPI has chosen to publish what appear to be questionable claims about the quality of healthcare offered in independent hospitals


fiona Booth: head of the Association of Independent healthcare Organisations

Caring touch: The hCA group, which offers
both systems. if the CQC found any serious care failing in an independent hospital, it would apply the appropriate enforcement measures in the same way that it does for Nhs hospitals.
‘the CQC publishes an annual ‘ s tate of Care’ report, covering care delivered by Nhs and independent hospitals. t he most recent ‘state of Care’ report found that ‘independent services generally perform better than N hs locations in terms of safety and quality of care’.
‘ t he report also found that independent hospitals met:
safeguarding and safety standards in 92% of inspections;
Care and welfare standards in 98% of inspections;
respect and dignity standards in 99% of inspections;
staffing suitability standards in 93% of inspections.
‘ i ndependent sector hospitals do not claim to be perfect, and there is no room for complacency in these figures – but they do throw into doubt the position taken by the ChPi
‘We acknowledge that the sector needs to do more on information availability, which is why, in 2008, private hospitals established a data sharing and reporting project.
this subsequently became the Private h ealthcare i nformation Network (P hi N). t he sector has also been working with the Nhs to publish directly comparable data.’ (see overleaf in section 4 for details).
2‘Between October 2010 and April 2014, 802 patients died unexpectedly in private hospitals, and there were 921 serious injuries. Because of the limited reporting requirements for private hospitals, we are unable to state whether these deaths and injuries should be cause for concern.’
aiho commented: ‘ l ike N hs hospitals, independent hospitals are places visited by people who are either unwell or in need of medical treatment. some of those will have complex healthcare needs and some will have underlying medical conditions.
‘ t he report states that, unlike Nhs hospitals, private hospitals are not required to report such incidents to the National reporting and learning system (Nrls). i n fact, the independent sector has been working with the Nhs to enable it to report incidents in the same way that Nhs hospitals do and would like to move this pro

report co-author Prof Colin Leys, emeritus professor at Queen’s University, Ontario, Canada, and an honorary professor at Goldsmiths, University of London, said: ‘The public and regulators have access to more information than ever before about how nhs services are performing, but this report shows that the same cannot be said for private hospitals.
‘The Government has recognised the crucial role of transparency in making hospitals safer, but reporting requirements should apply wherever patients are treated. With the taxpayer now providing over a billion pounds a year to private hospitals, this is too important to be left to the industry to address.’
Co-author Prof Brian Toft, emeritus professor of patient safety at Coventry University, said: ‘The report highlights some sobering examples of what can happen to patients without the right staffing, equipment and facilities. When patients choose to have an operation in a private hospital, they may be unaware of the difference in terms of risk between a big nhs hospital with surgical teams and intensive care beds and a private hospital with neither. Consent forms should make clear to patients the inherent potential risks in the way these facilities are run.’
The report’s recommendations include:
Private providers should be subject to the same requirements as the nhs to report patient safety incidents and to report on their performance.
Consent forms given to patients in private hospitals should detail not only risks inherent in the procedure offered but also any that stem from the facilities, equipment or staffing of the hospital.
regulations governing provision of care in private hospitals should require an on-site registrar-level surgeon or doctor for every specialty for which nhs patients are treated, for an anaesthetist to be on call and for medical records to be kept on the ward.
The Department of health should carry out a review of the nature and cost of admissions to the nhs from private hospitals, and the nhs should have the power to recoup costs resulting from a failure by a private hospital.
Peter Walsh, chief executive of Action Against Medical Accidents, said: ‘In our experience, there is plenty that can and does go wrong in private healthcare and it is usually the nhs that ends up picking up the pieces.
‘This report confirms it is time for the same level of scrutiny, regulation and protection of patients’ safety and rights to be afforded to private patients as is now being done for nhs patients. A comparable complaints procedure and access to independent advice on complaints would be a good starting point.’
‘Ill-fitting bras cause a range of problems, such as back and shoulder pain and even sores or welts as a result of straps and under-wires digging into the skin. Many women seek breast reduction surgery as a last resort,’ says plastic surgeon Mr Atul Khanna. his research led to a collaboration with experienced bra-fitter sue McDonald. Optifit offers a new bra design that will ‘elevate your breast without pressure of distortion’.

ject forward more quickly than is currently possible.
‘Furthermore, the N hs itself uses a variety of different reporting system to input this data.
‘the report states, correctly, that private hospitals are required to report all serious incidents to the CQC and Monitor – and, of course, they fulfil those obligations.’
‘The majority of private hospitals have no intensive care beds, some have no dedicated resuscitation teams, and surgeons and anaesthetists usually work in isolation – without assistant surgeons and anaesthetists in training present.’
aiho responded by saying that whether junior staff were present in training had no bearing on the safety of clinical procedures – it was the presence of adequately qualified and experienced consultants which assured patient safety and highquality care.
‘ s taffing arrangements in private hospitals are indeed often different from those in the Nhs, but there is no valid basis for suggesting that they are deficient.
the aiho spokesman added: ‘it is relatively common for trainee surgeons to assist in private theatres, but the consultant will always be personally present and responsible.
‘Furthermore, the Nhs operates a large variety of hospitals, from large district generals to small community hospitals. Not all of these institutions will offer the same breadth of services. indeed, it is quite usual for smaller hospitals not to have an a & e department, and some do not have intensive care facilities – so it seems odd to single out private hospitals for this criticism.’
4
‘Although the private hospital sector now gets over a quarter of its income from treating nhs-funded patients, there is significantly less information available to patients about the performance of private hospitals than about the nhs.’
aiho commented: ‘the report suggests, correctly, that more needs to be done on information availability. that is why the independent sector established PhiN in 2012. PhiN is an independent institution which publishes a
There is no evidence to suggest that re-admission rates or the need for critical care support are higher following treatment in independent hospitals than in nhs hospitals
range of healthcare data for staff and patients, and was set up specifically to open up data from the independent healthcare sector in order to increase transparency.
‘the informationsharing project from private hospitals predated the Competition and Markets authority inquiry into the private healthcare market and, as a result of the CM a findings on information availability, will continue to publish relevant data.’
5‘It is not possible to establish whether all private hospitals providing nhs care are fulfilling their legal obligation to publish quality accounts letting the public know how they are performing.’
aiho said: ‘We acknowledge that not all providers post their quality accounts on the N hs Choices website. h owever, the major independent hospital groups providing N hs care do post their quality accounts online, some at an individual hospital level.’
aiho said there were other questionable claims in the report, such as that private hospitals rely on the N hs if patients in their care develop complications, and that ‘around’ 6,000 patients have transferred to Nhs hospitals from independent institutions.
‘there is no evidence to suggest that re admission rates or the need for critical care support are higher following treatment in independent hospitals than in N hs hospitals; actually, such information as is available tends to suggest the opposite.’
the report also alleged a ‘moral hazard’ in which private hospitals know that there is a ‘safety net’ of the N hs underneath them if things go wrong. aiho said: ‘this is false and unsubstantiated.’
‘independent institutions strive at every opportunity to assure patients’ safety and comfort, as evidenced by the CQC. of course, in small private and public hospitals, if a patient suffers a major trauma which is best dealt with in a larger centre, that patient will be moved there. But that does not imply that there is a lackadaisical approach to quality or safety.’
aiho said the report suggests private patients lacked a means of redress if things go wrong. t his was also factually incorrect.

David Mobbs: boss of nuffield health Group
‘Private patients can put in a formal complaint to their provider and, in isolated incidents where the problem is not addressed, can also contact the chairman or other senior board members of the provider.
‘Finally, if they still feel that their complaint is unresolved, they can take it to the independent sector Complaints adjudication service ( is C as ). For N hs patients, the Public s ervices and h ealthcare ombudsman is available.’
providers’ reactions
Nuffield’s Mr Mobbs added that the group would make a thorough review of the methodology and conclusions of the report and welcomed working with any organisation interested in seeking to promote transparency, in addition to the existing work they are already undertaking with the CQC and PhiN on the transparency agenda.
inspections of Nuffield health hospitals by the CQC, including reviews of the quality systems, were are all up to date and there are no issues, nor enforcement actions, he said.
h ospital group h C a also reacted individually to the report. i t said it welcomed calls for increased transparency and was committed to a transparent approach to reporting and sharing quality data with all stakeholders including patients.
‘We believe that this evidenceinformed approach is the only true way for us to demonstrate our commitment to patient safety and quality,’ a spokesman said. it said its hospitals continued to achieve 100% compliance with all CQC standards and it was the only private provider that reported to registries such as the i ntensive Care National a udit and research Centre, the society of Cardio thoracic s urgeons and the British Cardiovascular intervention society.

‘over the last ten years, we have invested over half a billion pounds in new technology, complex care and highquality facilities. We have the highest (level 3) critical care beds at all of our hospitals to ensure patients can be treated in all eventualities and do not need unplanned transfers to other hospitals.’
A major consultation just launched by the GMC in a controversial report aims to improve patient protection and public confidence in doctors
iNDePeNDeNt PraCtitioNers who have harmed patients could face sanctions even if they can show they have subsequently improved their practice in serious cases.
this is one of a number of farreaching proposals aimed at protecting patients and upholding public confidence in the medical profession.
Doctors are expected to apologise to patients if they have caused them any harm and, in future, failure to do so could affect the sanction they face.
t he proposals are part of a major consultation by the GMC on how doctors should be dealt with when serious complaints about them are upheld.
Under the proposals, doctors could face restrictions on their practice, suspension or even have their registration removed if, for example, it is shown that they knew or should have known they were causing harm to patients in serious cases. this could happen even if they had subsequently improved their practice.
i n the consultation, launched last month, the GMC is seeking views on:
imposing sanctions where doctors make serious clinical errors, even where they have successfully retrained and improved their practice, if they failed to heed concerns and take steps to protect patients sooner.
Whether panels should require a doctor to apologise where he or she has previously failed to do so.
imposing more serious action in cases where doctors fail to raise
concerns about a colleague’s fitness to practise or take prompt action where a patient’s basic care needs are not being met.
improved public protection in cases where a doctor has bullied colleagues and put patients at risk or discriminated against others in their professional or personal life.
GMC chief executive Niall Dickson said: ‘Doctors are among the most trusted professionals, and rightly so, and they deserve to be treated fairly. in the vast majority of cases, oneoff clinical errors do not merit any action by the GMC.
‘But if we are to maintain that trust, in the small number of serious cases where doctors fail to listen to concerns and take action sooner to protect patients, they should be held to account for their actions.
‘ t here have been occasions when we have been prevented from taking action in serious cases because the doctor has been able to show that they have subsequently improved their practice. We believe that doctors and patients want stronger action in these serious cases.
‘it is also right that patients or their families are told what went wrong and, if appropriate, they should be given a full apology. We believe this should be taken into account when deciding what, if any, sanction needs to be imposed to protect future patients and uphold the reputation of the profession.’
the GMC is consulting on guidance, whose purpose is similar to
that used in courts in england and Wales. the guidance is also available to GMC decision makers, known as case examiners, who decide whether to refer a doctor under investigation to a hearing.
Mr Dickson said the guidance being consulted on was vital for case examiners and the independent panels who decide on the sanctions doctors should face, both to protect patients and uphold the reputation of the profession.
chance to make sure the action we take is fair to doctors while never losing our focus on protecting the public.

‘We want patients, doctors and other professionals to give us their views – this consultation is a
‘We are also publishing a microsite with case studies to bring the consultation to life. We will be asking people to tell us what action they think should be taken against a doctor’s registration in four scenarios, and to let us know the factors that influenced their decision. t hese are decisions which the Medical Practitioner tribunal service panels make regularly about doctors during a hearing.’
In the small number of serious cases where doctors fail to listen to concerns and take action sooner to protect patients, they should be held to account for their actions
The consultation, which includes events for doctors, patient groups, their representatives and lawyers, runs from 22 August to 14 november.
The consultation is available to view on its website www.gmc-uk.org.
The GMC provides guidelines, known as Indicative sanctions Guidance, to Medical Practitioners Tribunal service (MPTs) panels who decide the outcome of cases at the end of a fitness-to-practise panel hearing. The guidance is also available to GMC decision-makers who decide whether or not to refer a doctor under investigation to a fitness-topractise panel.
A report on the outcome of the consultation will be published in 2015 and the findings will be used to inform a new version of the GMC’s Indicative sanctions Guidance.
To take part in the consultation, private doctors can either answer the questions online on the GMC website or by email to ftpconsultation@gmc-uk.org or write to fitness to Practise Policy Team, General Medical Council, 350 euston road, London, nW1 3Jn
Doctors
who employ staff need to be aware of the Children and Families Act 2014, which received Royal Assent on 13 March 2014. This gives workers the right to work flexibly and have more time off to care for their children, writes Michelle Bowen
The key new employment rights that the Children and Families Act 2014 has introduced are summarised below in chronological order.
From 30 June 2014, the right to request flexible working has been widened to cover all eligible employees – that is to say, those with 26 weeks’ continuous service at the time of making the request – not only parents/carers.
The previous statutory procedure has been abolished and replaced with a new broader duty for employers to deal with requests ‘reasonably within a reasonable period’.
There is a statutory code of practice issued by the Advisory, Conciliation and Arbitration Service for employers to follow when dealing with such requests supplemented by a good practice guide.
From 1 October 2014, eligible employees and agency workers will be able to take unpaid time off to attend up to two antenatal/ adoption appointments; up to 6.5 hours per appointment.
e ligible employees/agency workers include: the father of the
child, husband/civil partner or partner (including same sex) of the pregnant woman/adopter parent or intended parent in a surrogacy situation who meets specified conditions.
eligible single-parent adopters are entitled to paid time off for up to five adoption appointments –up to 6.5 hours per appointment. employees/agency workers will be able to bring an employment Tribunal claim if their employer refuses time off or refuses to pay for time off in certain circumstances.
From 5 April 2015, a new system of shared parental leave and pay will entitle eligible working parents to share up to 37 weeks of statutory pay and up to 50 weeks statutory leave between them, provided the mother/prospective mother of a child born/placed for adoption after this date is entitled to statutory maternity/adoption leave and pay in the first place.
Eligible parents can take statutory leave at the same time or at different times ‘eligible’ parents are: employees, agency workers and in some cases self-employed workers who are either the mother or father of the child or the mother’s husband/ partner (including same sex/civil
Doctors who are employers should start to review and update relevant contract/policy terms now so they are ready to address these changes once they take effect
partner) or intended parents in a surrogacy arrangement (if they intend to apply for a parental order) or prospective adoptive parents – including foster parents in the new fostering to adopt scheme – who meet the qualifying criteria.
The qualifying criteria relates to employment status, duration, notice provisions and evidential requirements.
Qualifying parents will have rights to return to the same job or to a similar job, depending on when they return to work.
From 5 April 2015, adoption leave and pay entitlements will match the entitlements of birth parents. There will be no qualifying service needed to take this leave and adoption pay will be at the level of 90% of normal earnings for the first six weeks after the child is placed for adoption.
Doctors who are employers should start to review and update relevant contract/policy terms now so they are ready to address these changes once they take effect and ensure compliance with the statutory provisions.
Michelle Bowen is a senior solicitor for health and social care law firm Hempsons, specialising in employment law


www.medbc.co.uk
Come and join the hundreds of other consultants who use MBC and experience the following benefits:
• Bad debts of less than 0.5%
• Increase in net income by up to 25%
• Freedom for the consultant and secretary to focus on the medical side of the practice
• 24/7 online access to both your financial and practice management data
• Having a service tailored to your needs with your own Account Manager
• Our fees are only charged on the money that we collect for the practice and NOT on what we invoice which means we share the same objectives
Special offer:
To celebrate our 22nd year in business we are for a limited period of time offering all new clients an introductory discount of 20%*
Further information:
MBC – More than just a billing company
Please visit www.medbc.co.uk for more detailed information or phone 01494 763999 and speak to Garry Chapman to establish how we may assist your practice.
*Terms and conditions apply
Catherine Harriss (below)
believes many independent practitioners could do more to make themselves attractive to patients

Where are your patients?
Online. They are looking for you. No longer are they waiting for traditional pathways; they are seeking out their own information.
Whatever is available to them, they will use. Unfortunately for them, this can be correct or incorrect.
Your patients are seeking a solution for their problem. What have you in place to lead them to you?
Many potential patients are online and, thanks to government initiatives, many more will be coming online in the future.
They are no longer only found via GP practices. Every year, more and more people will be depending upon the internet for their information.
In the Opinions and Lifestyle Survey 2013, devised by the Office of National Statistics (ONS) and coming from the Labour Force Survey, 86% of the adult population were found to have access to the internet (see bar chart opposite).
Seventy per cent of adults in Great Britain use a computer every
day and 37% of the population aged over 65 use a computer every day. This is a rising figure.
And with the widespread introduction of super-fast broadband across the UK and the 4G network, this will only get higher (see bar chart below).
In 2013, 43% of all adults had used the internet to find health information, with the most dramatic increase being in the 25 to 34-year-old age group where 59% seek out health information.
In 2013, 53% of adults with home internet use social networking sites – Facebook, Twitter and Google plus.
One adult in two is aged between 45 and 54 and participating in social networking. Seventyfive per cent of adults have fixed or mobile broadband (figures from ofcom.org.uk).
In the same study, 95% of women aged 25 to 34 have smartphones and 50% of all users have smartphones.
81% of smartphone users have their phones switched on all the time (Ofcom: ‘A nation addicted to Smartphones’);
Four out of five consumers use their phones to shop and 70% of mobile searches lead to online action with an hour.
In 2012, 42% of users regularly used their smartphone to access social networks. In 2013, this number had increased to 65% of users.
Smartphones are the conduit for your business. The ONS found that 43% of people use the internet to seek health information. You need to think of smartphones as the ready tool for you to be found. If your online presence is limited, how can this tool find you? It is much easier to browse the net with a smartphone and consequently seek information very easily. A strong online presence means that you can be easily found to
Daily computer use by age group, 2006 and 2013 help potential patients. Through high-quality search engine optimisation, a solid network of highquality information together with Google advertising, patients can make direct contact with you or your secretary.
If you have an NHS clinic, you have probably already encountered the patient who attends it with pages of information printed off from the internet about the solution to their problem.
It is no different to the private self-pay patients you seek. They perceive that they have a problem and decide – with or without the involvement of their GP – where to get their solution.
They may be out with friends or just surfing the internet and decide to look up how to solve whatever it is that is upsetting them.
So will they find you? Or your competitor? Or a site that contains poor information so they are
a lost opportunity for you and they are no better off than before. Consider smartphones as the access point to you and then you will understand how little is available about you.
Ensuring that you and your service is smartphone-accessible is vital for improving your self-pay private practice.
next month: your online profile and how to dominate
Reference: www.ons.gov.uk/ons/ dcp171778_322713.pdf (figures 1&2)
Catherine Harriss is the founder of MultiWorksMarketing.co.uk specialising in private practice marketing
An easy to use software system, which fully supports the clinician and office staff and makes the whole process of running a busy Practice a lot easier.
Call now for a chat and ask about a free, no obligation demonstration of our comprehensive system that has been designed to save your Practice time and money.
Lights, camera, action!
Independent practitioners are increasingly using video so patients can see and hear them talk before they meet. Leslie Berry reports

Patient choice has always been part of the attraction of private practice, and patients look for consultants who not only have the expertise to treat them but will also care and communicate – and who will listen as well as explain.
Some ask friends and family for personal recommendations, but these are not always available. the relationship of patients with their specialist can often be a gamble.
But the internet is changing the way people access health-related information and patients increas-
No amount of words on a profile or website compare to a patient hearing and seeing the doctor explain their expertise, skills and ethos
ingly use online resources to help them find and choose a specialist.
eighty per cent of internet users have searched for a health-related topic and many patients will have looked online before meeting their chosen consultant.
But many consultants have been reluctant to provide comprehensive information. only a minority have personal websites and sometimes information is too detailed and confusing for the lay reader.
Video gives a fresh perspective. i t allows short presentations of
important information and lets the patient hear and see the doctor they are considering.
video profiles
o ne company is now getting alongside consultants to help them make the best of being on camera. Launched in May 2013, MultiMediaMedic’s signature service is the production of consultant video profiles, allowing consultants to introduce themselves to patients prior to booking an appointment with them.
the media firm’s business manager n icole n aylor explains the concept: ‘ o ne billion people a month visit You tube, 40% via mobile devices, so it is unsurprising that patients now seek video profiles and video information films to help them make their health choices.
‘Patients can read how caring and compassionate doctors are, but seeing them smiling into the camera and speaking about how they enjoy their jobs and treat patients is invaluable.’
dress smartly in clothes suitable for meeting a patient in a clinical setting. recordings often take place outside of clinic hours – so do not turn up in your jogging bottoms.
Bring along any props you think may be appropriate to your specialty; for example, vertebrae of the back or model of the heart. They need to be recognisable to the patient viewing the video, but avoid anything too graphic.
practise your personal script prior to the recording – unless you are George clooney or Kate Winslet, there will inevitably be a few retakes, so you need not worry about delivering your lines perfectly first time. But being familiar with your script will make you feel more comfortable and save time.
Keep your language simple and avoid jargon. remember, the video is primarily going to be seen by patients. avoid scary language like ‘mortality’, offer reassurance and positive outcomes, but also show you can communicate risks and benefits and help the patient choose what is best for them.
Be aware of any verbal and physical ticks. We all have them, but if you know you stutter over a particular word or phrase, reword it so your video flows more naturally.
arrive at the scheduled time for your video recording. You need to look as good as you can on camera, so avoid running late and arriving hot, sweaty and harassed.
remember to smile. You may find you concentrate so hard on your lines that you forget the most important thing – smiling. Yes, patients want an expert, but they always want someone who appears friendly.
Use your video after the recording. it sounds obvious, but the recording is only the start. put it on your own website, on YouTube and on the websites of the private hospitals where you practise. Tell your patients about it and tell them to tell their friends and family. for patients to see it and choose you, it has to be out there.
review how well your video is being received. You won’t know if a patient has come to see you because they have seen your video or not. so ask them.
Following a £5m refurbishment, nuffield health Brentwood hospital, e ssex, has been working with the company on a new way to engage with patients before the consultation even begins. hospital business development manager Debbie Greenwood says: ‘With our refurbishment underway, we were looking at how we could further engage with our patients when MultiMediaMedic approached us about its MeetYourconsultant video profile service.
More powerful
‘ t he information on a consultant’s hospital website can often be limited to a photograph, qualifications and a short profile, but we wanted to offer our patients more. ‘no amount of words on a profile or website compare to a patient hearing and seeing the doctor explain their expertise, skills and ethos. even more powerful is a patient’s own testimony
about the care received from the consultant and hospital staff, or their personal story.
‘and video can also clearly demonstrate some of the positives about private healthcare – pleasant surroundings, friendly staff, and facilities such as private rooms with ensuite bathrooms.’
t he MultiMediaMedic team, whose medical director is cardiologist Prof Jean Mcewan, say they aim to bring the perspectives of clinician, patient and carer to expert film-making.
as doctors are finding for their own education, video allows explanation and demonstration of complex information in an easily understandable way. it is accessible: you don’t need to be able to read to watch a video and the bottom line is we like watching t V. a s our attention spans get shorter, video allows us to hear and see information quickly – even on our smartphones.
A new concept providing real benefits to patients
• Weight-bearing scans and variable patient positioning enables a more precise diagnosis
• Truly open system is a solution for claustrophobic patients without compromise in image quality

Dear Reader,
Subscribing to Independent Practitioner Today is the only way you can be sure you will see every issue. Don’t risk missing out. Our personal subscription for doctors and managers is only £75 a year and £200 for organisations. But you can reduce these figures to just £60 (only £36 after tax for higher-rate payers) and £175 respectively if you pay by direct debit. So take advantage of this offer now for this unique business magazine dedicated to supporting you in your private practice. We’re confident your subscription will repay itself many times over!
Editorial director


Instructions to your Bank or Building Society to pay Direct Debits
Name and full address of your bank/Building Society
To: The Manager Bank/Building Society Address Postcode Ref. No.
Name(s) of account holders Branch sort code Account No
banks and building societies may not accept direct debit instructions for some types of account
post your application (no postage required – UK only) to: independent practitioner today subscriptions department, Freepost, po box 36, plymouth, pL1 1br
Please post to: Proact Ltd Subscriptions Dept., 12 Mary Seacole Road, The Millfields, PLYMOUTH
Banks and Building Societies may not accept Direct Debit instructions for some types of account
subscribe online at www.independent-practitioner-today.co.uk

send a copy of your letter to us.
Go on, admit it: you’re in private practice for the money! The fact so many independent practitioners don’t admit it is the reason their businesses are not as successful as they could be, argues surgeon Dev Lall
Why bother with private practice anyway? I mean, really – why are you in private practice?
Ask any consultant that question and the answers you’ll get will range from an uncomfortable silence to a vague ramble about providing excellence in service, personalised attention, expertise at the patients’ convenience, and so on.
Which is all nonsense, of course. Drivel. because there is only one reason any of us ever goes into private practice: we’re in it for the money. o f course we are. Why else would we do it?
Why else would you get up early to check in on a private patient at the local private hospital on the way in to your N h S post each morning?
And why else would you hold a clinic in your spare time, in the evening or over a weekend?
Why else would you finish the day at your NhS hospital, grab a quick sandwich, then head to the local private hospital for an operating list?
For the money. Not for love, not for altruism, not for fun. For the money. Most doctors, even when pushed, will find it very hard to admit that to anyone – even to themselves, sometimes. Which has always struck me as completely bizarre. t he trouble is that it goes
If we’re all in it for the money, why is it that we concentrate upon GPs to send us patients?

against everything we’ve been taught to believe in.
We’re not clock-watchers in our N h S jobs – on the contrary, we routinely stay until the work is done. We’ll come in during the evenings or over a weekend to see sick patients even when we’re not on call. We do this automatically, without thinking about it. And we neither charge nor get paid for going the extra mile.
And then we start out in private practice and find ourselves having to ask patients for money, to pay for a service we had up until then provided for free. It might sound
daft, but this really can be a challenge for many doctors. Still, no matter what consultants may say, we’re all in it for the money. yet, if that’s the case, why is it that we concentrate upon GPs to send us patients – often as the sole source of our private patients? Why don’t we explore and make more use of other ways of growing our practices?
Fixation on referring GPs there are several reasons I believe that consultants focus their efforts on GPs when it comes to growing their private practices.
one is because that is what we have seen all our predecessors do. that is how they grew their private practices, so that is the process we follow. We know it works, eventually, even though it is usually very slow.
Secondly, that is the model we are encouraged to follow by our senior colleagues. Why? because they know it is slow and they know they have the upper hand because they already have a relationship with the local GPs. they will continue to get the lions’ share of the referrals and the new
kid on the block will pose no threat.
thirdly, most consultants don’t know any better. t hey don’t know how else to grow their practices. they know nothing of modern business growth strategies and most of them make the mistake of not even accepting that their private practice is a business in the first place.
Fourthly, those consultants that do know of other methods of growing their practices and other ways of marketing themselves are often scared. It is all rather new and strange and outside their comfort zone. this is why most doctors still won’t market themselves on their own initiative or on their own terms – even when they know better.
Fifthly, senior consultants discourage them from doing so. Why? In case they are more successful than themselves. t hey know they have the advantage when it comes to GPs. Similarly, they know that advantage is lost and that they are vulnerable if a colleague markets themselves directly to patients. t hen they have no control over the outcome.
Finally, consultants kid themselves when it comes to networking with GPs that it isn’t anything as ‘shabby’ and ‘tawdry’ as trying to solicit private referrals – in other words, marketing themselves. of course not, they say, it’s an educational meeting held for the continuing medical education of their colleagues.
And if GPs just happen to send them patients, insured or otherwise, who are willing to pay for treatment as a result; well, they’re not going to argue, are they?
Doublethink again. GPs know precisely why you’re holding your meeting and so do you.
why are doctors so hung up about this?
there are several reasons behind this. I think a big one is simply that we’ve always given patients the benefit of our expertise for free.
We’re simply not used to asking them for money and it doesn’t figure in our thinking. this would explain why so many doctors don’t chase up bad debts and so readily write off invoices or don’t even send them out in the first place, even when patients are insured.
Secondly, there is an inherent conflict of interest in private medicine: a pressure and a tendency to overinvestigate and to overtreat patients.
this is present in the NhS too –we don’t want to make a mistake and miss a serious problem – yet it is much easier to resist in the NhS. Firstly, because of the pressures and difficulties in arranging tests that really do need to be done for sick people, let alone tests that may not be strictly necessary in the worried-but-veryprobably-fine patient. And secondly, because we don’t get paid any more for arranging more investigations or follow-up appointments.
Privately, of course, getting tests arranged is quick and easy. And we get paid for everything we do. So if he or she mentions a new symptom, it’s too easy to rush in and investigate it rather than carefully weigh up the probability of there being a serious underlying cause.
We are aware of that conflict, we all know of unscrupulous consultants and the vast majority of us do not want to fall into that trap.
why this is a problem
t here is nothing wrong with wanting to increase your income. Sure, money may not bring happiness per se, but it certainly alleviates many of the problems that arise when you’re poor. And even though we’ll never be poor on our NhS salaries, what is wrong with working in our free time doing the job we love and getting paid for it?
t his blindness and refusal to accept that money is the only reason for engaging in private practice is, I believe, one of the major impediments to private practice success. because unless you know what you really want, you can’t get it.
Achieving any goal requires focusing your energies on activity that brings your goal nearer. both your time and energy are finite resources and need to be channelled and directed carefully to achieve the best results in the shortest period of time.
It is so very easy to confuse and conflate activity with useful work taking you closer to your goal.
To earn as much as possible in your private practice, you need to focus on these areas:
1. correct coding for procedures
2. medical billing and invoice collection
3. chasing bad debts
4. Looking at which conditions you treat to find those which bring in the most overall income – from initial consultation, through treatment and in follow-up – with the least effort on your part and targeting those patients in all your marketing efforts
5. Looking at your practice to identify the conditions that bring the least income and/or take the most time and effort on your part and no longer seeing patients with those conditions
6. marketing and promoting your practice and yourself at every opportunity and in as many ways as possible
7. relentlessly looking for new products and services that you can sell to your patients to improve their health and wellbeing and thereby increase your income
Just because you get paid for looking after pateints privately doesn’t mean you provide anything other than highquality care
So if you want to earn as much as possible through your private practice, you need to focus on particular areas (see my seven tips in the box above).
The uncomfortable truth
Most people will feel deeply uncomfortable reading this article. they will find it very hard to talk about this and accept the truth.
yet truth it is. When it comes to private practice, we’re in it for the money. every single one of us. but that doesn’t make you any less of a human being. t hat doesn’t make you any less caring for your patients. t hat doesn’t detract from the value of the work you do.

there’s nothing to be ashamed about. Just because you get paid for looking after patients privately doesn’t mean you provide anything other than high-quality care. because although there is a conflict of interest in private medical care, it is, in the main, counterbalanced by our honesty and desire to do the best for our patients, whether they are fee-paying or not. the trouble remains, though: if you don’t have a goal, if you don’t know exactly what it is that you want, you’re going to find it much tougher than it needs to be to achieve it.
And you will never be particularly successful either. you might have a busy practice, sure. but there’s the world of difference between a busy practice and a profitable one.
Mr Dev Lall (left) is an upper-GI surgeon and runs a specialist private practice consultancy. He can be found online at www.Private PracticeExpert. co.uk





SeSSIonal ConSultInG roomS at nos 2 & 7 Harley Street, london
delightful rooms for medical professionals at a surprisingly low cost ad hoc booking and mail handling available
Website: www.londonconsultingroom.co.uk
email: admin@hstcentre.co.uk
Phone: 0759 004 6606
Financial stress can hit all consultants’ private practices at some stage. Garry Chapman outlines the three key problem areas and the questions you should address

One Of the most frequent questions I’ve been asked in our 22 years of working with consultants is: ‘How do I compare with my colleagues in terms of size?’
They are, of course, referring to their turnover.
My answer is always the same. It is extremely difficult to compare, as it depends upon so many factors.
These would include:
How much time you devote to private practice;
How long you have been in private practice;
Where you are located;
How you charge for your work. All consultants are individuals – which is why we tailor our services to the needs of each consultant.
And as most consultants who come to us are in various levels of distress, the second most common question I get asked is: ‘Am I worse than my colleagues or am I in the worst state that you have seen?’
Again, my response would, of course, be one of politeness, pointing out that while they are experts in their own medical sphere, no one expects them to be experts in all the other challenges of running a private practice.
While pondering these consultants’ questions, I thought it would be valuable for them if I were to explore the three most common causes why most doctors who seek our help are in some form of distress with their financial affairs.
The following are in no particular order, but the challenges are, in fact, probably true for most consultants at some stage during the life cycle of their private practice.
One of the first challenges that a consultant will have is to ensure that they set up the running of their private practice on a sound basis with the correct infrastructure.
This means having a robust auditable system in place to facilitate the financial elements of the practice and would include the ability to raise invoices and reconcile payments.
And, naturally, this should be combined with the facility to
If the consultant does not have the correct infrastructure in place to support the financial aspects of private practice, then there is a need to make changes very quickly


chase the outstanding invoices by phone and letter.
This also means having a system in place to collect payments from self-pay patients.
That would involve having the ability to collect money from a debit or credit card, which means that the practice would have to operate a credit card ‘pin and chip’ system.
But what I often see is a practice being run on a mixture of spreadsheets and word processing documents combined with folders stuffed with paper copies of clinic and theatre lists.
To make matters worse, these software programmes are being run on laptops/notebooks/and PCs which are never backed up. So if the device is either lost or the software becomes corrupt, then the entire practice and finances are put at risk.
It does not matter about the size of the private practice. If the consultant does not have the correct infrastructure in place to support the financial aspects of private practice, then there is a need to make changes very quickly because every day that passes they are placing their income at greater risk.
Once the practice becomes established, the next key challenge is to appoint the right secretary to assist them in growing the practice. The medical secretary is the bedrock of any successful practice and is often the busiest person in the practice.
Medical secretaries are expected








HMRC tax investigations and disputes create difficult and stressful times.
As an award winning firm of tax experts, our highly experienced partners specialise in resolving problems relating to tax investigations and disputes with HMRC.
To find out, in confidence, how we can help call 0800 734 3333.
‘Here to help. Not to judge.’
When a secretary leaves or retires, the impact on the practice can be devastating; particularly on the financial side of the practice
to wear many hats, including receptionist, personal assistant, sales ledger clerk, insurance guru as well as a debt collector.
There are not many individuals with the combined skill set required to complete all of these tasks perfectly as well as fit them all into a working week.
It is an almost impossible task for one person to cope with, especially as the practice grows. In our experience, once the practice reaches a certain size, the secretary is so busy dealing with the patients and the medical side of the practice that the billing and collection is the area that can get neglected.
When a good secretary has been with the practice for some time they can appear to have everything under control. But when they leave or retire, the impact on the practice can be devastating; particularly on the financial side of the practice.
Unfortunately, this tends to become apparent only after a period of time when the money stops going into the bank account due to poor cash flow because the billing and collection are not up to date.
The consultant thinks that the new secretary will be able to cope in the same way as the previous one.
In our experience, this is rarely the case.
In general business, it is not a good idea to be reliant upon one key individual. In medical practice, this is mostly unavoidable in respect of the consultant, as the majority operate as sole practitioners.
But this does not have to apply to the rest of the practice. It is not uncommon to outsource key components such as having the letters produced using a transcription service or outsourcing the medical billing and collection.
This achieves a more robust practice as well allowing the secretary more time to look after the other elements of running a practice, including spending more time on the patient.
This, in turn, means that should the secretary leave, then replacing this key individual, while never easy, will be less stressful and from a financial perspective will have minimal impact on the practice.
ensure your financial infrastructure is robust, auditable, secure and is backed up. the financial consequences of not doing this do not bear thinking about and if you are ever investigated by the HmrC, it could get even worse
See that your practice is not too dependent upon one person. no matter what business you are in, it is not good practice to follow that path
understand your billing and know what your debt is at any given time. establish how much you are owed, how old the debt is and make plans to resolve it – do not bury your head in the sand
alternatively, outsource your medical billing and collection through a professional organisation which will take care of each of the above challenges in one stroke
Whatever the size of your private practice, I would recommend that you review it based on the challenges outlined and take action promptly or it may be something you regret not doing

a
lot of consultants I speak to do not even know how much they are owed or how old that debt is
Assuming you have the above challenges under control, then probably the biggest challenge that any consultant faces in private practice is to bill correctly and keep the outstanding debt under control. from our experience, this is one area where very few achieve this feat on a regular basis.
The majority of consultants undercharge because they do not fully understand the billing principles imposed by the various private medical insurers (see my article in the April 2014 edition of Independent Practitioner Today)
On top of this, a lot of consultants I speak to when I meet them at various events do not even know how much they are owed or how old that debt is.
If you think about that fact, it is quite astounding. The majority of consultants are working extremely hard in their private practice, juggling their time with their other commitments such as stressful nHS work and trying to find time to spend with their families, but they are not aware that they are not being paid for the work that they are doing.
At Medical Billing and Collection we achieve bad debts of less than half of one per cent, but we
regularly see examples in private practice of bad debt between 5%-10% which is ten to 20 times higher than we achieve.
This element of a private practice would be kept under control if the medical billing collection was outsourced, as it would form part of the service.
That would mean the cash flow of the practice remains strong and consistent on a regular basis.
And that alleviates a lot of stress when it comes to paying the bills and tax demands when required.
The above points are the most common challenges that we see within a private practice which result in financial stress, and while we understand how they occur, we also think that they can be avoided, providing steps are taken in a timely manner.
e ven if they are not avoided, most of the problems can be resolved if decisive action is taken once the financial problems become apparent.
The biggest challenges can occur when the consultant is unaware of the issues that are taking place within the practice, because if they do not know they have a problem, they cannot fix it.
Garry Chapman is managing director at Medical Billing and Collection
is continuously updated based on the latest medical research to bring you current evidence-based recommendations.
Our unparalleled team of physicians and editors places new research in the context of the existing body of medical knowledge using their professional expertise and first-hand clinical experience.
This combination of Evidence & Experience is invaluable in crafting point-of-care recommendations trusted by more than 850,000 clinicians worldwide.
To learn more or to subscribe risk-free, visit learn.uptodate.com/EXPERIENCE or call +1-800-998-6374 | +1-781-392-2000.
With many doctors investing for their children, Lanying Burley and Mike Fosberry (right) give a round-up of practical advice on some of the options available


When it comes to investing for and gifting to the younger generation, whether to help with school or university fees or to get younger family members onto the property ladder, each person will have different objectives and risk tolerances.
A well-managed portfolio can be structured to meet specific family requirements and include a mix of longer-term growth assets and shorter-term holdings for liquidity.
t his arrangement can help to fund education, for example, with the potential to provide a lump sum later on, perhaps towards a deposit for a first property.
A managed portfolio consists of different assets and, despite stock market fluctuations, equity investments will typically be a key component. importantly, equities can provide some protection from inflation.
investments in equities can be
part of a portfolio or be a direct part of, for example, an investment trust bringing access to a spread of UK and overseas investments.
Payments into child portfolios can be made on a monthly basis, meaning the highs and lows of the stockmarkets will affect the portfolio less as the price paid over a period will be averaged.
Gifts made to a child are potentially exempt from inheritance tax, provided the donor survives seven years.
Should this not be the case, the annual £3,000 iht exemptions for gifts and nil rate band (currently £325,000) would be brought into the equation.
i f required, insurance can be taken out to protect the gift in the event the donor were to die during the seven-year period. Depending on what is given, there might be capital gains tax implications on the disposal to consider.
Capital gifts from a grandpar-
ent, aunt or uncle are often more efficient than parental gifts, where income thereon above £100 is taxed on the parents.
in contrast, gifts from grandparents, for example, can be invested in the child’s own name or within a bare trust so that any income is taxed on the child and gains are subject to the child’s own individual capital gains tax allowance (£11,000 in the current tax year).
Similarly, a child has a personal income tax allowance – currently £10,000 – which means that tax will only be paid if substantial capital gifts are involved.
iSAs have undergone an overhaul since Budget 2014, with new rules allowing savers to put £15,000 a year into an iSA. the full limit can be used for cash, investments or a mixture of both.
Grandparents and parents could also fund junior i SAs
(£4,000 as of July 2014) to save or invest. At 18, the child will have access to the Junior iSA or it can be converted into an adult iSA.
A child is entitled to the capital within a bare trust at age 18. however, investment bonds can be placed in a bare trust with a range of maturity dates to make funds available at a later age. t his type of investment bond has no value until maturity and cannot be encashed early. h ence, a portfolio can be designed to support the younger generation’s needs while building in peace of mind for donors that specific longer-term objectives can be met, such as the deposit for a first property.
Offshore investment bonds these can be held in a parent’s name and used towards school fees,
There are plenty of options out there and you should be able to find one that matches your family’s needs in a taxefficient way
there is no tax on the interest on this cash investment and the current 35th issue guarantees a compound rate of return of 2.5% AeR over five years.
the bonds can be cashed early with a penalty equivalent of 90 days’ interest, but they should be viewed as a five-year investment.
t he maximum investment is £3,000 per issue and a parent, guardian and even great-grandparents can invest for anyone under 16. Bonds cannot be held beyond the child’s 21st birthday.
i t is important to agree your investment objectives and timeline for saving for your children, and to consider how much risk and control over investments is appropriate.
“MidexPro thinks like a doctor, not a computer exper t”
All you need to run your private practice including document management, diary, clinical data, even test ordering and lab reports from TDL.
From paper billing (incl VAT) to electronic billing (EDI) to management of bulk purchase contracts
Grow seamlessly from a small solo practice through to a large group practice, remote access network system
MidexPro is the cost effective practice management system with support second to none.
for example, by using the annual tax-free withdrawal allowance of 5% of the initial investment.
Once the child is 18, bonds can be assigned to them and, providing they are non-taxpayers at the time, it’s normally possible to surrender the bonds without any tax liability. the capital is invested in underlying investment funds selected by the investor.
Children’s bonds are available from n ational Savings and investments (nS&i).
And it is also worth considering a diverse set of investments, and ensuring that you factor in sufficient liquidity.
there are plenty of options out there and you should be able to find one that matches your family’s needs in a tax-efficient way.
Lanying Burley is a partner and Mike Fosberry is a director at Smith and Williamson, a professional and financial services group which provides investment management, financial advisory and accountancy services to private clients, professional practices and mid-to-large companies
By necessity, this briefing can only provide a short overview and it is essential to seek professional advice before applying the contents of this article. No responsibility can be taken for any loss arising from action taken or refrained from on the basis of this publication. Details are correct at the time of writing.
Investment does involve risk. The value of investments and the income from them can go down as well as up. The investor may not receive back in total the original amount invested. Past performance is not a guide to future performance.
Rates of tax are those prevailing at the time and are subject to change without notice. Always seek appropriate advice from your financial adviser before committing funds for investment.

Free download of the full working package (30 day limited) from www.midexpro.com or call for a CD.
Try it for yourself with no sales pressure
“MidexPro has revolutionised our lives; it is just so easy”
Profitability issues for some private doctors’ partnerships are among the factors affecting the business and increasing the tensions among some consultants. But put away your boxing gloves! Lawyer Robert Capper (left) gives his top tips for doctor partners in dispute

As A lAw firm specialising in the provision of partnership advice, we have noted a distinct rise in the number of private medical partnership disputes over the last two to three years.
with both patient expectations and commercial challenges higher than ever, partners are no longer prepared to accept underperformance, continued absenteeism or poor behaviour putting additional pressure on the remainder of the partnership.
There has therefore been a clear increase in the number of partnerships who wish to proceed
towards the dismissal/expulsion route when partners are not willing – or able – to shoulder their share of practice responsibilities.
At the same time, we have seen a marked increase in general partnership fallouts; seeing partners leave and, in some cases, entire partnerships dissolved and wound up.
If you are in a private practice partnership and one partner is quite clearly disrupting your business, then the tips below are worth considering before taking any drastic action.
1. Talk
This should be obvious, but it is so often overlooked in our experience. Talk to the partner that you are having problems with.
Perhaps it is something outside of work that is affecting your working relationship.
It may transpire that the problem is relatively easily fixed – and that will save a lot of management time and financial strain on the practice.

partnerships fail to check their partnership agreement before exercising rights they think they have.
This is one of the biggest and potentially most severe pitfalls to fall into. You could overlook certain provisions of your partnership agreement that could leave you exposed to a claim from your troublesome partner.
It is worth noting that the vast majority of disputes can be solved without lawyers even becoming involved. Nevertheless, many disputes escalate because of a lack of basic communication.
2. Check the partnership agreement
what rights do you have, if any, to take action against a ‘wantaway’ partner? Can they give notice to leave the partnership?

Often enough, the partnership agreement will set the strategy for negotiations, as the agreement –or lack of such an agreement –will often lead prompt negotiation between the partners.
It is not always the procedures set out in the agreement itself which are followed. It is amazing to see how many private medical
3. Consider the current working situation w hy do you want the partner out? Are they disruptive or perhaps not very good at their job? Is the partnership making a loss or is it stagnant? losing sight of the bigger picture can also land the partnership in trouble – particularly if too much effort and management time is focused on trying to resolve what are, essentially, the finer points of a partner leaving.
Never underestimate the value of a positive reference, if feasible, in an offer to settle a partnership dispute.
likewise, in our experience, an agreed statement to partners and other practitioners is often of

great value to the outgoing partner. You need not be profuse in your praise of the partner, but can be seen to be supportive.
4. Make sure your finances are up to date
It always helps to have an up-todate set of accounts that fully reflect the current financial situation of the partnership. For example, while owning property may be an asset, a hefty practice mortgage certainly won’t be. leases are also liabilities, and a newly formed lease agreement on a property should be treated as much of a liability as a mortgage. Also consider upcoming issues that may or may not affect your practice – such as tax bills or employees’ wages.
we usually recommend that clients talk with their accountants and tax advisers at the same time as taking advice from us.
5. Know the personality Personalities are key considerations when entering negotiations to remove a partner.
Taking an aggressive stance may not be the best approach – certainly
7. Never make your dispute about money
All medical and other partners are bound under a good faith to one another and the partnership itself. Making the dispute purely about boosting the drawings amount per partner will not serve you in good stead if the dispute becomes litigious.
Always ensure the business is the first priority, not the individual partners in it. This is difficult to manage, but most professionals are able to see their way through it.
8. Take legal advice
It may seem like an obvious recommendation – especially in an article written by a lawyer – but it is also crucial to take legal advice.
It is one thing to look at the partnership agreement, but this is insufficient in the vast majority of circumstances.
The nuances of partnership law
are complex, so partnership agreements may not be applicable to the extent you believe they are, following modifications or a lapse of time.
It is always beneficial to seek the opinion of a qualified third party during the often complex nature of a partnership dispute.
A final note …
Importantly, you must also remember that if the dispute eventually proceeds towards litigation, a court will look at the behaviour of both parties from the outset of the dispute.
A party can prejudice its position by a failure to act in accordance with pre-action protocol – and this is why seeking appropriate legal advice from a firm experienced in this area is imperative.
Robert Capper is a partner in the Health and Social Care Team at Harrison Clark Rickerbys
if the partner you are considering expelling is particularly volatile and stubborn.
Equally, if a partner is usually reserved, consider how taking an aggressive stance would affect the situation.
Interestingly, in our experience, private practice professionals are usually able to rise above the personality issues.
6. Take time about it
Do not rush to follow a particular course of action. The worst thing a private partnership can do is move in to expel a partner before all the necessary people have been consulted.
s eeking tax and accountancy advice and the views of the partnership – including the partner who is up for expulsion/removal – are important.
we have been instructed on countless occasions where the partner has already been expelled, before any advice was taken –legal or financial.
s uffice to say, these particular disputes are the most expensive to settle in terms of the actual settlement and fees.







As bAnks and building societies threaten to move their head offices south of the border if scotland votes yes to independence, one thriving Caledonian industry will be staying put.
To be called s cotch, whisky must be produced at a distillery and matured in oak casks in scotland for at least three years.
However, as the production base cannot be moved, pro-union researchers warn that in an independent s cotland, the £5bn whisky industry could be a target for higher taxes to compensate for the continuous exodus of profits.
As the referendum date approaches and this edition of Independent Practitioner Today was on its way to subscribers, I am expecting politicians on both sides will draw on every last persuasive argument they can –whether oil or alcohol.
Down on the ground, at least, individuals are considering over a wee dram or two not only how a
yes vote may actually impact the tangible – their own personal finances – but also the intangible – their sense of being, fairness and national identity.
This is what makes the contest so intriguing as the ebb and flow of debate cuts right through the perceived ‘normal’ social and economic demography, with disagreement in all corners from sean Connery to sir Alex Ferguson. Who can say whether head ultimately conquers heart?
s cotland is a big player in the financial services arena, managing £750bn of pensions and investments with more than 40m bank account-holders.
nine out of ten of those customers live in England or Wales. Twothirds of all IsAs administered by scottish companies are taken out by savers outside scotland, with this proportion rising to 70% for pensions and 84% for mortgages.
The confusion surrounding the currency, EU membership, interest rates and taxes of an independent s cotland is likely to continue as none will be resolved until after any yes vote.
Conflicting politicians’ claims and media reports from both the ‘for’ and ‘against’ camps do nothing to dispel the uncertainty.
A recent poll found almost twothirds of scots have now ‘given up listening’ because of the contradictory claims being traded. Even the pollsters themselves have started arguing over the methodology being employed by rival companies.
Moving funds to England might seem like a relative safety net for consumers. It ensures they continue to operate in sterling, benefit from U k compensation schemes and receive interest rates set by the bank of England.
Edinburgh-based pensions giant s tandard Life has already indicated it may move its opera-
tions to England if there is a yes vote.
However, Ross McEwan, chief executive of R bs , has played down any future implications. He said: ‘Let’s leave the people of scotland to make the determination. If I need to operate in 39 countries rather than 38, that’s what we’ll do.’
Danny Alexander, the Chief secretary to the Treasury, has warned English investors to avoid panic withdrawals from scottish companies, at least in the short term. such activity, he declared, could wipe billions from the value of organisations such as R bs and standard Life. ‘keep your money in s cotland. s cotland is a great place to invest, it is a great place to have your money,’ the Liberal Democrat MP said.
The s cottish n ational Party ( sn P) leader Alex s almond has pledged to cut taxes, although the
The Scottish National Party leader Alex Salmond has pledged to cut taxes, although the Institute of Fiscal Studies is not convinced Scotland could sustain this
the academics cited in the research, stated that the Treasury statistics ‘badly misrepresents LsE research’. He believed the true cost of setting up all of scotland’s independent institutions would be closer to £200m, as many of the required public bodies already exist under devolution.
Institute of Fiscal studies (IFs) is not convinced s cotland could sustain this.
If the revenue from north sea oil dries up – it’s expected to have 30-40 years of production left –the general consensus is that taxes would have to rise.
s tuart Adam, of the IF s , said: ‘There are differing views on how quickly the oil will run out, but it will run out. s cotland’s population is ageing faster than the rest of the Uk. Pension bills will rise. Taxes will have to go up or spending be cut and the sooner it makes adjustments, the easier it will be.’
n evertheless, leaders on both sides accept that scotland has all the ingredients to be a viable nation state. Reports show that as an independent country, scotland would expect to start with healthier state finances than the rest of the Uk.
Although scotland enjoys public spending well above the U k average, the cost to the Treasury is outweighed by the oil and gas revenues. The scottish government has also set out proposals to increase public spending by 3% per year – compared to the 1% increase planned by Westminster – delivering an additional £2.4bn of investment.
It would also be the 14th wealthiest country in the Organisation for Economic Co-operation and Development (OECD) –essentially a club of rich nations and steering group for the world’s economy. The U k would lag behind at 18th place.
Earlier this year, the Uk government claimed that research by the London school of Economics had estimated the cost of setting up an independent scotland at £2.7bn. In fact, Patrick Dunleavy, one of
He said: ‘I can understand that ministers in Whitehall are getting a bit frustrated; they think that the snP is being very coy about the costs of transition. b ut it is very important, if you are contributing to a public debate, to contribute accurate information and not, as in this case, I’m afraid, very crude misinformation.’
Perhaps the decision is much more than financial. In a scathing article against independence, the Economist actually cited a very good reason for separation.
‘If scots really want independ ence for political or cultural rea sons, they should go for it. n ational pride is impossible to price.’
The snP has promised financial regulation and compensation equivalent to the U k safeguards, but the actual delivery of such a scheme has raised doubts. The Financial Conduct Authority says that, without a yes vote, there is no mandate to prepare for change so no work has begun to establish a new financial regulator.
Demonstrate your skills, expertise and personality to patients before the consultation even begins. Our new and innovative video profile service – Meet Your Consultant – has been specifically designed to help you stand out from the crowd, and engage with patients before their appointment has been booked.
Whether you are a new consultant wishing to create your first professional profile, or an experienced consultant wishing to revitalise your private patient list MultiMediaMedic can help you raise your profile with patients, both on and o ine. Contact us for a no obligation discussion.
Web: www.multimediamedic.co.uk

Could the fledgling economy withstand a major financial crisis?
A report from the Westminster Treasury puts the liabilities of s cottish banks at more than 12 times its national income, as measured by gross domestic product (GDP). The equivalent figure of the failed Icelandic banks was seven times.
Mr s almond says the b ank of England would act as their lender of last resort, prompting derision from the b etter Together campaign’s Alastair Darling.
However, given the complex financial arrangements between the two countries, it is fair to assume that rUk – the term now adopted for the rest of the Uk if separation goes ahead – would not stand idly by in the event of financial disaster.




The credit rating agency standard & Poor’s (s&P) officially reported that an independent scotland would be an ‘investment grade economy’ due to its ‘wealthy’ economy, but would hold an over-reliance on the financial sector.
nationalists counter that, once the dust has settled, s cotland’s finances could, in fact, be stronger and less biased should some of the financial organisations leave Edinburgh.
s &P’s analysis dismissed concerns that s cotland would be over-dependent on the oil reserves, which it said accounted for 16% of GDP, well below the 25% mark it sets for sectors to rank as dominant.
However, as the bitter dispute continues over whether scotland could share the pound after a split, s&P’s reports that the country would struggle to match the Uk’s AAA credit rating if it failed to negotiate a currency union with London or the Eurozone.
One notion is that if there is a new nation, it would shadow sterling or the euro in the same way Panama shadows the dollar, although this could lead to increased risk for investors.
s enior Westminster ministers have admitted a currency union is likely to be agreed to ensure fiscal and economic stability on both sides of the border.
Tax-efficient savings such as IsAs are currently only offered to Uk nationals according to tax law and, it is assumed, unavailable out of the country.
Pension providers operating in both territories could face higher costs working through different interest rates, taxes and, possibly, currencies. Investors may be concerned by how these costs will be passed on.
Yes scotland claims there would be no change to private pensions after independence, as ‘private pensions are a private matter between individuals and their pension providers’. The campaign group added: ‘With independence we can . . . ensure private pensions are well protected and a much more positive and inclusive approach to public sector pensions.’
The s cottish Government suggests that a yes vote offers greater protection from changes – and there have certainly been many –to public sector pensions imposed by the Westminster government. It has confirmed that all rights and entitlements to public service pensions will continue to be protected upon independence and that there will be no difference to individual contribution rates or benefit levels as a result.
The Uk Government currently has the authority over decisions on the n H s Pension scheme in scotland with the financial management undertaken by the U k Treasury. If separation is agreed, the s cottish Government will have responsibility for the pensions of all public servants working in scotland and will take over responsibility for the s cottish nHs Pension scheme.
For doctors who are n H s scheme members, and existing pensioners of scotland’s schemes, there would be no change in their pension arrangements following independence.
For example, if a former n H s s cotland employee moves to England after retirement, the s cottish n H s Pension s cheme would continue to pay this pension.
What has not been confirmed is whether the existing ‘transfer club’ arrangements across the Uk would continue. Could n H s Pension members in England and Wales move to the health service in s cotland and retain their pension?
One concern would be the costs involved in providing a crossborder pension scheme with potentially different currencies, individual tax levels and regulations.
Would there be significant distinctions between the schemes in the future? In 2012, the scottish Government could have chosen not to proceed with the increased n H s Pension contributions recommended by the U k , but it abided by the proposals. It would have been forced to pay for any different policy out of the scottish block grant.
In the same vein, scotland has adopted the new 2015 n H s Pension scheme despite freedom
to deviate from rU k ’s course of action.
Alex salmond’s ministers have raised the possibility that because life expectancy is shorter in scotland than other parts of the Uk, the state retirement age may not be increased to 67 when it is imposed by the rest of the Uk
Whether this proposal is also rolled out to public pension schemes at the same time has not been determined.
Anecdotally, we can confirm that the scottish Pension Agency administers its members’ funds with a significantly higher level of competence than the nHs Pension Agency for England and Wales, where you can wait for months without any hope of a reply.
The Doctors and Dentists Review b ody (DDR b ) is responsible for setting pay levels for doctors working in the n H s across the Uk. The scottish Government is then free to implement the recommendations or adopt a different system. Until now, it has chosen to retain the Uk structure and, broadly speaking, accepted the view of the DDRb With regards to contracts, these already vary between different groups of doctors. scottish consultants hold an employment contract which, although similar to those in England, is drawn up in scotland.
The consultation on amendments to contracts currently taking place in England does not cover scotland. The previous decision not to continue with the Clinical Excellence Award scheme for doctors in scotland was seen as a purely political one at the time.
For many supporters of independence, their belief stems from a desire to be closer to the decisionmaking of their government.
It is a simple question of democracy and restoring power to elect and/or remove an administration as they see fit. As one witty commentator concluded: ‘It would be difficult for Holyrood to do any worse than Westminster.’
A recent research paper from banking group I n G noted that
Local control of economic levers such as tax, immigration and welfare would open the way to a fairer and wealthier society



‘although the high transition costs of separation and uncertainties over currency and the terms of EU membership mean that the material benefits of independence were far from clear, local control of economic levers such as tax, immigration and welfare would open the way to a fairer and wealthier society’.
It is clear there are many financial questions unanswered at this stage and a wealth of work still to be carried out should the 300-year-old economic and political union be split.
Even if the referendum results in a no vote, there is likely to be agreement to pass more financial governance to Edinburgh.
Only time will tell how this impacts on English doctors working in scotland and vice versa.
Simon Bruce (below) is managing director of Cavendish Medical, specialist financial planners helping senior consultants in private practice and the NHS

The content of this article is for information only and must not be considered as financial advice. Cavendish Medical always recommends that you seek independent financial advice before making any financial decisions.
Levels, bases of and reliefs from taxation may be subject to change and their value depends on the individual circumstances of the investor. The value of investments and the income from them can fluctuate and investors may get back less than the amount invested.
Medici Marketing is an independent business development consultancy providing the following services for sole practitioners and working groups of Consultants or General practitioners:
• Project management
• Development of business models for integration of new service lines

• Management of website build and SEO optimisation
• Event management
• Customised marketing strategy
• Network facilitation
• Branding and logos
• Business planning and market analysis


For further information or to arrange an informal meeting, please contact Sue O’Gorman, at: sue@medicimarketing.co.uk or call 07985 456487







Former consultant neurosurgeon and now MDU medicolegal adviser
Mr Jerard Ross (above) looks at two neurosurgical scenarios that pose dilemmas for independent practitioners
QI am treating a patient in his late 50s who has a scan suggesting a probable large glioblastoma multiforme near the language cortex of his brain. I need to obtain his consent for biopsy.
However, I am concerned that while the patient is coherent, he shows intermittent confusion and we have been obliged to increase his steroid medication to ease his headaches. How do I determine if he has sufficient capacity to consent to the procedure?
AWhile you have a legal and ethical obligation to obtain the patient’s consent for surgery, the cognitive decline which is sometimes apparent in brain tumours means you are right to be concerned about his capacity.
In England and Wales, the legal framework for assessing whether a patient is able to consent is provided by the Mental Capacity Act 2005 (MCA) and accompanying code of practice.
The starting point is that your patient must be assumed to have capacity unless it is established otherwise and you should not
make any assumptions based solely on his condition.
Instead, the code says the patient’s capacity must be assessed in terms of his ability to give consent for the specific treatment when required and it sets out the following two-stage test:
1 Does the person have an impairment of the mind or brain or is there some sort of disturbance affecting the way their mind or brain works, whether temporary or permanent?
2
If so, does that impairment or disturbance mean the person is unable to make the decision in question at the time it needs to be made?
In this situation, the patient will need to make a particularly complex decision, balancing the risks of damage to his brain function against the likely benefits in terms of life expectancy and quality of life.
In determining whether he is able to make this decision, the MCA code of practice says you should consider the following:
Does he have a general understanding of what decision he needs to make and why he needs to make it?
Does he understand the information relevant to the decision –including information about the reasonably foreseeable consequences of deciding one way or another or failing to make a decision?
Is he able to understand, retain, use and weigh up the information relevant to this decision?
Can he communicate the decision – by talking, using sign language or any other means?
Bear in mind that your patient’s capacity may fluctuate, depending on factors such as medication, symptoms and fatigue. For example, he may not be well enough to take in what you tell him during a conversation, but he could comprehend the information in written form.
The code states people must be given all practical and appropriate support to help them make decisions for themselves, so it is worth considering providing information in different formats.
You could also consider involving his family in the decisionmaking process, subject to the patient’s consent.
If you decide that your patient has capacity on this occasion, it is important to keep a careful record of the assessment and consent process in the patient’s records. Ongoing assessment is also advisable, as the patient’s capacity could deteriorate before further treatment decisions are required.
If you decide the patient does not have capacity to consent to the operation and this decision cannot be delayed, the MCA requires a decision to be made in his best interests.
In this situation, you will need to:
As far as reasonably practicable, encourage and enable the patient to participate as fully as possible in the decision.
Try and determine the patient’s past and present wishes and feelings – in particular, any relevant written statement made when the patient had capacity, the beliefs and values that will be likely to influence the patient’s decision if he had capacity, and the other factors that the patient would be likely to consider if he were able to do so.
Take into account, if practicable and appropriate to consult them, the views of anyone named by the patient, anyone caring for the patient or interested in his welfare, any attorney appointed under a Lasting Power of Attorney, and any deputy appointed by the court, as to what would be in the patient’s best interests.
Again, you must keep a detailed record of the process of working out the best interests of the patient for each relevant decision, setting out how the decision about that individual’s best interests was reached; who was consulted to help work out best interests and what particular factors were taken into account.
QA fit young man has been referred to me with leg pain. He requires a lumbar discectomy and I have explained what the surgery involves. The patient has asked me to tell him about the risks involved. Am I obliged to set out all the risks, including those which are extremely rare?
AYes, you need to answer the patient as openly and honestly as you can.
The GMC says you ‘must give patients any information they want or need about … the potential benefits, risks, burdens and the likelihood of success for each [treatment] option’ so they can make their own balanced and informed decision.1
You could also be vulnerable to a clinical negligence claim if you do not warn the patient about possible risks which then transpire, even if they are very remote.
As the House of Lords stated in a landmark legal ruling:2 ‘In modern law, medical paternalism no longer rules and a patient has a prima facie right to be informed by a surgeon of a small, but wellestablished, risk of serious injury as a result of surgery.’
The GMC interprets this to mean that patients ‘should be told of any possible significant adverse out-
comes of a proposed treatment’.3
In this situation, you are advised to consider informing the patient about both the wellestablished complications of surgery, such as the chances of recurrence or infection, and the smaller risks of a devastating adverse outcome, such as cauda equina injury, vascular or bowel injury. Give the patient the opportunity to ask further questions and ensure he understands your explanations.
Finally, it’s also important to make a note of this discussion and information given in the patient’s clinical records.
References
1. Paragraph 9(e), Consent guidance: patients and doctors making decisions together, GMC, 2008.
2. Chester v Afshar [2004] UKHL 41 Pt 2.
3. Legal annex, common law; Consent guidance: patients and doctors making decisions together, GMC, 2008.
An independent firm offering one to one meetings anywhere in the UK giving advice and help with:
• how to start in private practice
• how to maximise private practice income
• ways to reduce tax payments
• setting up in Chambers/Groups
• limited companies and LLP’s
• financial planning
• record keeping

• computer software
• tax and financial advice re: car purchases
• pensions: NHS, personal and employee schemes
• purchase of consulting rooms and surgeries
• inheritance tax and capital gains tax planning
• VAT
For more information please contact us by: Wilmslow
Phone: 01625 527351
Fax: 01625 539315
Harley Street
Phone: 020 7307 8759
Fax: 01625 539315
Email: info@sandisoneasson.co.uk Website: www.sandisoneasson.co.uk
So you want a ‘successful’ private practice? But what really makes it that way? Ian Tongue plays ten charttopping hits for practice success in our monthly series for independent practitioners who are in the throes of starting up their business
Most consultants decide to engage in private work to boost their income.
the key thing to understand is that you are running a business and you have obligations not just to patients but to the tax authorities and you will need help with this.
It is vital that you understand your market and competitors who are often your n H s colleagues who also want a slice of the pie or don’t want you to take some off their plate.
so don’t be reluctant to invest in your business.
and something I hear time and time again is the importance of a high-quality secretary to help maximise your income and reach that work-life balance.

s o M e spec I alt I es face high demand, but for most you will need to get out there and promote yourself. availability, affability and ability are the keys to success. When you first start out, write to Gps and tell them about you. G p s are often attending events and a great way to meet them is to speak at these events and network with them as often as you can.
private hospitals usually have a team that looks after and promotes their new consultants and this initial exposure can be invaluable. a ttend new consultant evenings and meet as many people as possible. o ften at these events experienced consultants highlight the factors for success and pitfalls to avoid.
For all but the most basic of affairs, you will need to engage an accountant. For many doctors, this is the first time that they have needed help in this
way and it is important that you understand your new obligations and obtain the necessary support. Meet up with an accountant who offers a no-obligation first meeting to see if you would want to have a long-term relationship with them. engaging one with specialist knowledge of the medical profession can be very helpful and they should be able to discuss the practicalities of engaging in private practice as well as a thorough understanding of the tax system.
4 I OWE YOU NOTHING (Bros)
a HI t F or Bros in the 80s, but rarely the case when it comes to the taxman! It is vital that you understand the tax system and how much you need to be saving from your income.
Getting caught out with a higher tax liability than expected can take a long time to recover from, particularly as your financial commitments tend to increase at this stage in your life. there are ways of cutting your tax liability, ranging from ‘safe’ and normal practice to aggressive forms of tax planning. Inevitably, if you undertake high-risk planning, there is a chance that something could go wrong and with HM revenue and custom’s new powers to name and shame, you could generate unwanted attention.
as part of engaging an accountant, they should understand your attitude to risk and plan with you accordingly.
vate sites, there is more scope for business travel, but if you have one hospital/place where you conduct your work, the chances are that your options are limited.
For those trading as a limited company, a company car is an option, but given your marginal tax rate, it can often be more expensive to go down this route. always discuss these types of decision with your accountant before proceeding.
more than one hospital, make sure that someone is keeping tabs of the collective position, as your accountant will need to bring these together.
10
s o M e people might think setting up a separate business bank account for your private work can be expensive, so why tell them? But it is vital that you run things through a separate bank account. usually a separate current account is perfectly oK.
For business accounts, bank charges are often applied both monthly and based on transaction volume/type, so the savings can mount up.
prIvate practIce is tough and it can take time for you to establish yourself. It can feel like an uphill battle, but once you have found your feet and established yourself, it can be an excellent way of boosting your earnings potential. take things at your pace and don’t become over-reliant on the additional income until the sustainability of the practice is assured.
Keep I n G adequate and complete records is not only best practice, but failure to do so could now land you with a fine from HM revenue and customs. accounting records range from manual systems to bespoke practice management software packages. Initially, a spreadsheet will usually suffice, but it is really the minimum standard required.
the bespoke packages can seem expensive, but after tax relief and savings of time are considered, it usually pays for itself.
some private hospitals offer secretarial and admin support and this can be a good option.
If you have admitting rights at
p lann I n G and mapping your career is a very important part of running a successful private practice and building sustained growth and wealth. Work closely with your accountant so that they know where you want to be and they can advise you accordingly. as the saying goes, if you fail to plan, you are planning to fail.
Next month: Goodwill to all men?
Ian Tongue (below) is a partner with Sandison Easson & Co accountants

adaptInG to the ever-changing world of the nHs is really important. an opportunity today may be gone tomorrow and therefore it is important that you understand this and adapt accordingly. this also applies to the trading structure for your private practice, so it may be appropriate to consider options and there can be many benefits to this. You should be having regular discussions with your accountant on this subject.
a quest I on o F ten asked is how much tax relief is available on a new car, as the boost in income can be welcome to renew or upgrade your motor as a reward for all that hard work. r ecent events with a tribunal case, well publicised in previous editions of Independent Practitioner Today, have reduced the ability to charge your private practice for using your vehicle for business.
If you operate at multiple pri-
The Association of Independent Specialist Medical Accountants is a national network of firms advising over 3,000 medical practices across the UK. For some of the best advice available on accounting, taxation and pensions, visit our website and find your nearest AISMA accountant.

or call Liz Densley on 01424

We ARe all trying to cultivate an image in private practice.
Whether it be personal or that of the clinic we are part of, a positive image will pay dividends when it comes to attracting patients and business.

But a great image has to be earned and constantly reviewed other wise we risk losing out to competitors. Attaining the position of default provider in the minds of potential clients is our aim.
In the world of motoring, there are a few makes who have earned this elevated position in the eyes of potential car-buyers. If any of us doctors are considering buying a premium 4x4 sports utility vehicle, there is one name guaranteed to spring to mind: Range Rover.
The original Range Rover appeared in 1970 and was an experiment by Land Rover to appeal to drivers who wanted a bit more comfort and style than the very basic Defender model.
It was a surprising success and has developed ever since to
become more and more a luxury model in its own right.
In 2006, in response to clients wanting a bit more visual style than the boxy design of the classic Range Rover, the Sport model was introduced.
Again, more successful than was expected, this model now accounts for about 60% of all Range Rover sales. The only problem for buyers has been that the Sport has been using the chassis of the Discovery over the last few years rather than the more sophisticated normal Range Rover set-up.
But now we have a new Sport model. Based on the advanced and all-new aluminium chassis of the 2013 heavily revised Range Rover, the new car is no different under the skin.
Despite moving ever higher into the luxury end of the car marketplace, Land Rover has very consciously maintained the
supreme off-road capabilities to make the Range Rover untouchable in all conditions.
To do this, there is naturally some beefy suspension hardware and the car remains a heavy piece of kit. Not as heavy as it was, though. The extensive use of aluminium pays dividends when it comes to performance and fuel efficiency.
Available with a 255bhp V6 turbodiesel in the TDV6, a 288bhp V6 turbodiesel in the SDV6 or a stonking 503bhp V8 supercharged V8, the new Sport has plenty of power in all guises. The best compromise between performance and economy is the SDV6 model, which promises up to 37.7mpg and will probably be the biggest seller. It was this version that I had on test.
First impressions
As usual, first impressions are really important and the new Sport looks more modern and stylish than its predecessor.
As those of you who practise aesthetic surgery know, visual appearance is key to confident presentation and the new ‘face’ of the Sport is improved by slick LeD headlights.
The success of the Sport’s smaller sibling, the evoque, has not gone unnoticed by Land Rover and there are definite elements of fashionable styling cues from that model.
You climb up into a Range Rover rather than slide into it and this only exentuates your elevated location. Indeed, Range Rover call it the ‘Sports Command Driving Position’. I wouldn’t argue with that. Surrounded by high-quality expensive materials, the interior is superb. Comfort for driver and passengers is supreme.
Although the interior is not as big as you would imagine, five adults can travel in style with plenty of leg and headroom.
In this new Sport, there is the option of a further two seats in the rear although, as in the BMW X5, these are really child or small adult-sized and not suitable for long-distance adult occupancy.
As a nod to the Sport’s more focused driving qualities, the gear lever is straight out of the Jaguar F-type and controls the seamless eight-speed auto box.


Surrounded by high-quality expensive materials, the interior (above) is superb
The dashboard houses a clear central display, but, disappointingly, the sat-nav is not up to the standards of the best. The steering is light but direct and enhances the really impressive handling composure of this big car.
Adjustable air-suspension smooths out all but the worst potholes and wind and road noise is minimal.
The Sport feels more like a luxury limousine than a 4x4 offroader and can compete with the best that Mercedes, Audi or BMW saloons can offer.
Amazingly, the Sport, like all Land Rover products, is just as happy in muddy fields or deep snow as it is on dry tarmac and its Terrain Response System can be dialled into mud, gravel, snow, rocks or sand and the suspension, ride-height, gear selection and throttle response will be altered appropriately.
You can go anywhere and anytime in this Sport and if you practise in a rural or out-of-the-way area or you live at the end of a
This is an extremely impressive car. It may not handle quite as well as Porche’s Cayenne, but it is more comfortable
steep muddy track, this is the car for you.
This is an extremely impressive car. It may not handle quite as well as Porsche’s Cayenne, but it is more comfortable. As a smart luxury car for city use, it excels. As a versatile workhorse with allcondition useability, it also excels. The smart and successful independent practitioner who wants one or both attributes needs look no further than this British icon.
Dr Tony Rimmer is a GP practising in Guildford, Surrey
RAnge RoveR SPoRT SDv6
Body: Five- or seven-seat, five-door SUv engine: 3.0 litre v6 turbo-diesel Power: 288bhp
Torque: 600nm
Top speed: 138mph
Acceleration: 0-60mph in 7.3 secs
Claimed economy: (Combined) 37.7mpg on the road price: £64,995
Let us share your success story

We would like to interview doctors with a private practice about their views and experiences for a series of podcasts.
Topics for discussion could be:
• What were the key decisions you made in growing your private practice?
• What’s the biggest mistake you’ve made?
• What do you wish you’d known when you were starting out?
• How have you been affected by/responded to the recent changes in private medical insurance?
To get involved, please email podcast@ip-today.co.uk

Independent practitioner Today is launching an app version. Later this year, IPT will be available to read via all types of mobile devices through an app.
If you would like to be kept informed of developments, please email app@ip-today.co.uk

There are encouraging signs of recovery in our latest examination of consultants’ accounts, finds Ray Stanbridge. Additional material by Martin Murray
Between 2011 and 2012, our figures show that the average ent consultant increased his or her gross income from private practice by about 3% from £128,000 to £132,000. they have broadly kept up with inflation!
Costs have shown a modest increase of 2%, rising from £52,000 to £53,000.
As a result, taxable profits have increased, on average by 4% from £76,000 to £79,000.
As we have noted previously, it is becoming increasingly difficult
to make genuine comparisons between individuals in this specialty.
Some ent consultants have embraced the concept of groups, and this has impacted on incomes.
Others have chosen to increase diagnostic and other equipment and to provide a fuller service than the traditional ent consultant.
while our analysis is not statis-
aveRage InCoMe anD eXPenDItuRe oF a ConSuLtant ent SuRgeon WIth an eStaBLISheD PRIvate PRaCtICe
Expenditure
Source: Stanbridge Associates Ltd. Additional information: Sandison Easson and Co
tically valid, it is rather an overview of what a typical consultant working in the n HS and with a private practice might expect to earn and what expenses they might expect to incur.
One of the problems of ‘averages’ is that they are biased upwards by performances of very high earners.
Our average figures differ from median figures and are, of course, biased towards London and the South-east.
the impact of nHS Choose and Book work is having a significant effect on ent surgeons’ private practice incomes across the country.
Market analysts LaingBuisson in its Healthcare Market Review estimates that n HS work now accounts for in excess of 25% of the private practice market.
Such a dramatic increase has helped to offset pressures on incomes as a result of various insurance company squeezes. this trend is likely to continue as the n HS share of the market increases.
Costs for most ent surgeons have shown little change between 2011 and 2012.
there has been some increase in employment costs from £14,000 to £16,000 on average. Our view is that where family members are employed, salaries have shown some increase, no doubt stimulated by the increase in personal allowances over recent years. there has been a modest rise in consulting room fees. we expect this to increase further as the full
our sample of ent surgeons is restricted to those who:
have had a least five years private practice experience;
hold either a maximum part-time or new consultant nhS contract;
are seriously interested in pursuing private practice as a business;
are earning at least £5,000 a year in their private practice, including nhS Choose and Book work;
May or may not have incorporated or be a member of a group



If you plan to sell, retire or move away – or grow bigger – why not advertise with us and reach over 12,000 consultant and gP colleagues working in private practice?
If you plan to sell, retire or move away –or grow bigger – then why not advertise with us and reach 13,000 consultant colleagues working in private practice?


For full details of how we can help contact Mararet Floate on 01483 824094. Email: margifloate@ btinternet.com
For full details of how we can help, contact Margaret Floate on 01483 824094. email: margifloate@btinternet.com
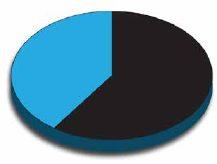
effect of the Competition and Markets Authority’s recent rulings are implemented.
At least professional indemnity costs seem to have stabilised –though our figures have been influenced by some members seeking cheaper cover elsewhere.
t here has been some fall in motor expense costs, doubtless influenced by publicity in Independent Practitioner Today relating to mileage expense rules.
Perhaps surprisingly, there has
PRoFItS FoCuS IS the InDuStRy BenChMaRK
Doctors and their specialist medical accountants use the statistics published in our ‘Profits Focus’ series to look at how their earnings compare with others and see where they can cut costs and boost their income.
now all this information is available on our website and is free when you take out a subscription. either fill in the subscription form on page 28 or phone 01752 312140 or email lisa@marketingcentre.co.uk. get a discount by paying by direct debit. www.independent-
been some drop in ‘other expenses’ primarily relating to marketing costs.
t here was a flurry of activity some years ago as ent consultants worked on establishing their websites. Some of these costs were of a one-off nature.
the overall picture for ent surgeons now therefore seems to be one of stability – with an increase in n HS-derived work offsetting pressures on fees from insurance companies.
we do expect to see some increase in costs in future years, but the overall situation seems promising. the market also seems to have bottomed out and is showing some signs of recovery.
next month: cardiologists
Ray Stanbridge runs an accountancy, finance and tax advisory service specialising in the medical profession. Martin Murray is a partner at Sandison Easson & Co, specialist medical accountants
gynaecologists
ophthalmologists
years ending 5 april
Source: Stanbridge Associates Ltd
Make sure you don’t miss our next issue, published on 23 october. only subscribers to the magazine are guaranteed to receive every copy and we don’t think anybody who is serious about continuing private practice in the future, when there is so much happening that will affect them, can afford to miss any issue.
Coming up next month:
Splitting up! a consultant who has been running a private practice with a business partner for 15 years asks how he can make things go smoothly now that his partner is retiring early and going abroad.
accountant Susan hutter dispenses some good advice
Be careful what you say! you could accidentally be making contractually binding commitments with your staff
What should you consider when drawing a private pension? Simon Bruce examines the benefits and pitfalls ahead of next year’s increased flexibility
Medical billing and collection expert garry Chapman has some important advice about getting your money from embassies
Profits Focus examines the latest earning trends of cardiologists
Doctors are facing the possibility of a new criminal offence – being charged with willful neglect. It will have consequences for healthcare workers if it becomes law. the MPS’s Dr nick Clements has advice
Starting a private practice – Ian tongue continues his monthly series dealing with the issues for younger doctors building up their business
Published by The Independent Practitioner Ltd. Independent Practitioner
Today is editorially independent and thanks Bupa for its assistance with distribution.
Printed by Williams Press Material is governed by copyright. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment. Editorial layout is the copyright of the publishers. If you wish to use it for promotional purposes on websites or for reprints, we would be happy to discuss licensing the copyright to you.
© The Independent Practitioner Ltd 2014
Registered office: 7 Lindum Terrace, Lincoln LN2 5RP
Write to Independent Practitioner Today PO Box 198, Cranleigh GU6 9BB
our motoring correspondent Dr tony Rimmer reckons he’s found just the thing for any petrolhead medic who lives in the real world where practicality and family needs figure highly: the Porsche Macan
advertising by independent practitioners can be very effective, but can also easily be an expensive mistake unless you carefully think it through. there are many pitfalls for the unwary. Surgeon Dev Lall writes on the importance of targeting

the challenge of helping our parents or other close relatives make decisions about their care is likely to come to many of us and for those who are healthcare professionals, this challenge can be far greater.
Business Dilemmas: Dr Carol Chu of the MDu advises a consultant who is wondering what to do after a patient is reluctant to be tested unless they can use a false name
Plus all our regular features and news
aDveRtISeRS: the deadline for booking advertising for our october issue is 26 September

eDItoRIaL InquIRIeS
Robin Stride, editorial director
Email: robin@ip-today.co.uk
Tel: 07909 997340
aDveRtISIng InquIRIeS
Margaret Floate, advertising manager
Email: margifloate@btinternet.com Tel: 01483 824094
Publisher Gillian Nineham Tel: 07767 353897.
Email: gill@ip-today.co.uk
SuBSCRIPtIonS
£75 independent practitioners.
£75 GPs and practice managers (private & NHS). £200 organisations.
But if you pay by direct debit, individuals pay only £60, and organisations £175
Call Proact Ltd on 01752 312140
Email: lisa@marketingcentre.co.uk


to guarantee your copy of Independent Practitioner today by taking out a subscription (at the rates shown on the left), phone 01752 312140 or send off a subscription form on page 28 or email lisa@marketingcentre.co.uk or go to the ‘about’ page of our website www.independent-practitioner-today.co.uk
If you pay by direct debit, individuals pay only £60 for a subscription – just £36 after tax. just fill in the form on page 28 and send it to the Freepost address shown at the bottom of the form.
BaCK ISSueS: £10 including post & packaging ChangIng aDDReSS oR SuBSCRIPtIon DetaILS?
Phone 01752 312140 or email lisa@marketingcentre.co.uk



Client management and financial control is the lifeblood of any enterprise. The latest Healthcode online ePractice management tool is the professional’s choice for practice management, giving you the control you need wherever you are. Our ePractice management solution meets the needs of a range of healthcare providers, from independent practitioners to large enterprise organisations. Our different service levels mean that ePractice will grow with your practice.
Access your patient details, appointments, bills and financial status from anywhere, any time.
The diary management feature on ePractice manager means I can focus on treating patients, while my PA is able to coordinate my appointments remotely.
Mr Barlow-Kearsley, Founder, Total Footcare Solutions
We use Healthcode’s ePractice manager system for all our invoicing, which streamlines everything for us. Roughly 75% of our invoices are submitted electronically, payments are now made much more quickly, which is good for the cash-flow.
John Morgan, Accounts Director, Jenny Morgan Secretariat




Call us today to arrange a demo and to discuss your requirements on 01784 263 150 quoting: IPT. For further information visit: www.healthcode.co.uk/ipt