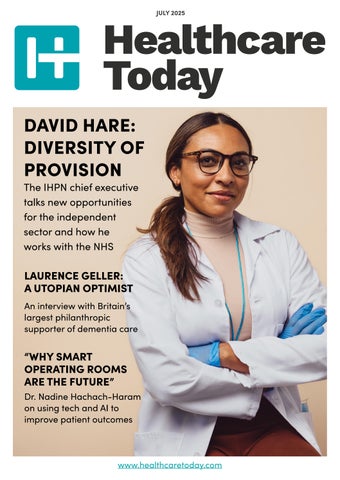
DAVID HARE: DIVERSITY OF PROVISION
The IHPN chief executive talks new opportunities for the independent sector and how he works with the NHS
LAURENCE GELLER: A UTOPIAN OPTIMIST
An interview with Britain’s largest philanthropic supporter of dementia care “WHY SMART OPERATING ROOMS ARE THE FUTURE”
Dr. Nadine Hachach-Haram on using tech and AI to improve patient outcomes

“What we are seeing now is a growing acceptance that NHS recovery and reform require capital, capacity and capability from the independent sector,” says David Hare.
“For the first time in a long while, there is now cross-party consensus in England that this is necessary...”
In an exclusive interview with Healthcare Today, the chief executive of the Independent Healthcare Providers Network talks about how private healthcare professionals plan to work with the NHS, why he expects to see opportunities in community and primary care services, and why a positive relationship with the Labour government will improve services for patients.
Also in this issue, Laurence Geller, Britain’s largest philanthropic supporter of dementia care research, talks about why dementia research needs more money and how to improve dementia care; practicing surgeon and chief executive of Proxime, Dr. Nadine Hachach-Haram, explains why digitising operating rooms and driving AI-powered insights from surgical data helps to improve patient outcomes, improve productivity and reduce workforce burnout; and much more.
We hope you enjoy!

20-23

27-31


GOVERNMENT RELEASES 10 YEAR HEALTH PLAN
WHILE the shift from hospital to community care and a greater emphasis on technology have been broadly welcomed, doctors want more details on how this will happen.
The British government has launched its long-anticipated 10 Year Health Plan, which is underpinned by what it calls “three key shifts”. This will move care from hospitals into the community through new community care centres, a greater emphasis on technology, and a priority given to preventative medicine.
Prime minister Keir Starmer said that the plan would “fundamentally rewire and future-proof our NHS”.
The government’s plan follows Lord Darzi’s diagnosis of the challenges facing the NHS last year where he assessed it was in a “critical condition” as a result of deep-rooted issues including low productivity, poor staff morale, a failure to keep up with new technology, rising waiting times, and a deterioration in the health of the nation. Shifting care out of hospitals and into the community hopes to ease the pressure on hospitals.
Neighbourhood health centres, with a range of staff, will provide easier
access to healthcare services. The intention is that community health workers and volunteers will play a pivotal role in these teams.
“By shifting from hospital to community, we will finally bring down devastating hospital waiting lists and stop patients going from pillar to post to get treated,” said health and social care secretary Wes Streeting.
Under the plan, the government has said that it intends to train thousands of GPs.
The plan has been cautiously welcomed by the medical sector.
“From what we’ve seen so far, the broad ambitions of the 10 Year Health Plan – strengthening primary and community services, boosting prevention and harnessing new technology to help make it happen –are the right direction for the NHS,” said Jennifer Dixon, chief executive of the Health Foundation.
Similarly, Kamila Hawthorne, chair of the Royal College of GPs, said that she is supportive of the government’s aspiration to shift care out of hospitals and into the community.
“It’s what is best for the NHS and, most importantly, it’s what is best for patients who want accessible care
close to home without long waits for appointments either with their GP or at hospital – but we’ve always been clear that sufficient resources and numbers of GPs will need to follow to make this a reality,” she said.
But new BMA council chair Tom Dolphin summed up the feeling of the profession. “The success of the Plan, and whether it will improve patients’ care and the public’s lives, will hinge on whether it genuinely addresses the workforce shortages, and values and empowers professionals on the front line, or just rearranges deck chairs on a sinking ship,” he said.
The government is hoping that its greater emphasis on technology will make the NHS more accessible and more efficient.
Its plans include rolling out new tools like AI scribes over the next two years to support GPs. These, it says, will end the need for clinical notetaking, letter drafting and manual data entry to free up clinicians’ time to focus on treating patients. The government estimates that saving just 90 seconds on each GP appointment can save the same time as adding 2,000 more doctors into general practice.
It also intends to use digital telephony so that all phone calls to GP practices are answered quickly.

Again, this was broadly welcomed.
“We strongly support the commitment to boosting GP availability, expanding neighbourhood health centres, and introducing cutting-edge technologies such as AI-assisted documentation and robotic surgery,” said George Maughan, director at healthcare insurance specialists THEMIS Clinical Defence.
“We firmly believe that emerging technologies are crucial to the future of healthcare - provided they are rigorously tested, benchmarked, and evaluated before widespread implementation.”
Barbara Hakin, chair of the Health Tech Alliance and former deputy chief executive of NHSE, said that she was pleased to see the prominent role given to digital and tech innovation. This shows “a clear understanding that modern healthcare must be both resilient and responsive to patient needs,” she said.
But many in the industry would have liked the government’s plans to go further.
Ian Burgess, CTO at Canary Care, a provider of smart home monitoring technology, said that calls for innovation and digital transformation must be matched by practical action.
“If the government is truly committed to supporting people, especially those living alone or with complex needs, then social care technology must be at the core of delivery, not sitting on the sidelines,” he said, highlighting the fact that too many local authorities and NHS teams are still struggling to access and implement the technology that makes a difference.
He called on ministers to be even more ambitious, a call that was echoed by Harry Thirkettle, a former NHS surgeon turned clinical entrepreneur who now heads up Health Innovation at Leeds-based consultancy Aire Logic. “These ambitions need to be backed by the kind of challenger thinking that reshaped industries like banking, where brands like Monzo started from user needs, not inherited systems.”
The challenge is that, as always, the devil will be in the details.
“While [the government’s plan] lays the foundations for an exciting future, the pace of change and the cost of implementation will need to be carefully balanced to bring this document to life and to fulfil its promise,” said Jill Mason, partner and head of health & care at law firm Mills & Reeve. “Simply saying that the approach will be rolled out, without full details on how to bring it about,
casts doubt on whether it will stick,” agreed Thea Stein, chief executive of the Nuffield Trust.
“This is hard, complex work, requiring leadership from politicians and NHS staff alike to challenge cultures and power dynamics, and create new ways to route money through the system so it doesn’t get sucked into the pressing and often urgent needs of other parts of the health service,” she continued.
It is also crucial that legislation keeps up.
“The shift from analogue to digital requires a regulatory rethink on our approach to accessing and sharing personal health data with healthcare providers and other relevant bodies,” said Gerard Hanratty, head of health and life sciences at law firm Browne Jacobson. Robust cyber security measures, widespread digital literacy campaigns and policies ensuring equitable access to digital health tools are needed, he said, as well as establishing clear ethical guidelines and standards for AI development and deployment, underpinned by rigorous testing and evaluation.
As the BMA’s Dolphin concludes. “We’ll need to see the full details to assess whether this will be possible,” he says.

THE PUBLIC DOESN’T THINK GPS WORK HARD ENOUGH
MORE THAN threequarters (77%) of the British public do not believe GPs work hard enough.
The shocking results of a recent survey commissioned by Londonbased specialist medical accountancy firm Ramsay Brown follows a string of policies imposed on the sector, including last year’s Autumn Budget.
Conducted by leading research consultancy Censuswide, the survey polled 2,001 nationally representative members of the UK general public regarding their attitudes toward GPs, their workloads, salaries and pensions, as well as the funding they receive.
“We commissioned this survey to get to the core of the public’s attitudes toward our frontline primary care providers. We’ve seen the damaging impact government policy has had on family doctors over the past few years and wanted to understand how this has translated into public opinion,”
said Ramsay Brown partner Katie Collin.
“The data suggests that poor policy decisions have soured GPs’ reputations, with the public placing some of the blame at their door. The truth is we’re seeing worrying misconceptions that, in reality, don’t hold water,” she continued.
For Ramsay Brown, the results reveal the public’s frustration with the UK’s medical services and suggest that a concerning proportion blame primary care providers directly. For them, the data uncovers “worrying” misconceptions and only further stresses the shortcomings of government policymaking in the sector.
“GPs across the country are doing a remarkable amount of work in extremely challenging conditions. Time and time again, the government delivers funding that’s tied up in complex structures and attached to complicated conditions and targets, ramping up GPs’ workloads. Despite
this year’s funding boost, the reality is that GPs will still be overworked and under-resourced – not the opposite,” said Collin.
“This is only compounded when you consider the hoops GPs have had to jump through in the last year. From miscalculated pay increases and inaccurate pension statements to the Chancellor’s NI-raising Budget and subsequent to-ing and fro-ing over whether practices would have to foot the bill – GPs haven’t had it easy,” she continued.
The government’s damaging decisions, she believes, have unfairly tarnished the public’s perception of general practice, undermining the difficulties GPs face daily.
“At the end of the day, these misconceptions make one thing abundantly clear: without a more productive approach to health policy, the Government will only continue to erode public opinion on primary care – perhaps even past the point of no return,” she concluded.
THEMIS SIGNS FIVE-YEAR DEAL WITH QBE
THEMIS, a managing general agent that specialises in contractual medical malpractice indemnity, has announced a five-year capacity agreement with the multinational general insurance and reinsurance company QBE.
The five-year capacity agreement will provide THEMIS with dedicated capacity as it accelerates its UK presence and targets international expansion.
“This partnership with QBE represents a major step forward in our mission to provide the market with stable, reliable and innovative contractual indemnity solutions,” said George Maughan, head of client relations at THEMIS.

“Our shared vision for the future of medical malpractice insurance underpins our strategy to deliver value not only in the UK but also globally,” he continued.
Doug Walker, portfolio manager –medical malpractice and healthcare practice leader at QBE, commented: “We are proud to partner with THEMIS, whose forward-thinking approach and strong market results align perfectly with our commitment to delivering secure and sustainable solutions.”
THEMIS’s market differentiation has largely been driven by its proprietary AI-powered underwriting technology, which combines
advanced machine learning with expert human oversight. This unique underwriting intelligence not only enhances precision in risk assessment and pricing accuracy but has also significantly fuelled the company’s growth to date.
This agreement demonstrates THEMIS’s long-term commitment to the market, aligned closely with its mission to provide healthcare providers with a robust contractual alternative to discretionary indemnity for a competitive premium.
With the announcement of this new deal, THEMIS is strongly positioned as a leading contender in this evolving landscape.
WALTON CENTRE DIGITISES PATIENT RECORDS
THE WALTON Centre NHS Foundation Trust in Liverpool, the country’s only specialist neurosciences Trust, has digitised 95% of its patient records with Apogee Corporation which has led to what it calls “significant improvements” in clinical efficiency and patient safety.
A Care Quality Commission (CQC) inspection in 2019 highlighted the Trust’s mix of paper and digital case notes as a clinical risk.
“Not all systems were linked and some staff found it difficult to access some records in a timely manner. Staff could not adapt patient care plans within electronic records to address individual patient needs,” the regulator said.
The Walton Centre decided to eliminate all paper-based records and
a competitive tender process led to the selection of Apogee and its secure document scanning and data capture services.
With almost all patient records now scanned, digitised, tracked and seamlessly integrated into the Trust’s electronic patient record system (EPR), clinicians can retrieve critical patient data – including medical, treatment and device histories – to improve patient outcomes. The implementation of a new in-house scanning facility ensures any new patient documents are available in the EPR within 48 hours of outpatient attendance and seven days of discharge from an admitted episode.
The time saved from the process has allowed medical records staff to be redeployed to other departments, contributing to enhanced operational
efficiencies and a faster patient flow through the hospital. The Trust has been able to clear its backlog of 5,000 patients and can register new patients on arrival for the first time since the COVID-19 pandemic.
The project has served to improve staff outcomes too. The volume of paper documents was presenting space issues, with records stored in unsafe areas. The removal of these records has freed up so much on-site space that the Trust is repurposing an area into a long-awaited communal staff room to help support employee health and wellbeing.
All patient records at The Walton Centre are scanned and tracked through a secure end-to-end process, with each physical file undergoing rigorous quality assurance checks and maintaining a full audit trail.
TUBERCULOSIS ON THE RISE IN THE UK REPORTS UKHSA
THE UK Health Security Agency (UKHSA) has recently reported a marked increase in the incidence rate of tuberculosis cases in England, and the report suggests that this may be a growing trend.
In 2023, a total of 4,855 people were notified with tuberculosis in England, an increase of 11% compared with 2022 and an annual tuberculosis notification rate of 8.5 per 100,000.
England counts as a low tuberculosis incidence country below the WHO threshold of less than or equal to 10 per 100,000.
Provisional data for the first three quarters of last year, however, indicate a further 13.7% increase against the same period in 2023.
Numbers and rates are now above the levels seen before the COVID-19 pandemic and the annual increase in 2023 is the largest since 1971.
Individuals born outside the UK account for almost 80% of TB
notifications, however, for the first time since 2012, the rate of TB in people born in the UK has also increased.
There is likely to be an increase in clinical negligence claims write Edward Sainsbury and Katherine East, partner and senior associate respectively at Clyde & Co.
The two also anticipate that there may be an increase in employer’s liability and public liability claims, given tuberculosis’s strong association with immigration and socioeconomic inequality.
Tuberculosis is caused by bacteria of the Mycobacterium tuberculosis complex. It is spread predominantly by the respiratory route, where bacteria are aerosolised by people with pulmonary disease and are inhaled by susceptible individuals.
Sainsbury and East point out that claimants, especially those who are diagnosed with a latent tuberculosis infection, may struggle to establish causation in order to succeed in any claim. “Unlike active tuberculosis which may be definitively linked
to a source of infection via genetic sequencing, there is no means of identifying when a latent tuberculosis infection was acquired,” they say.
They point to a material contribution argument as per Holmes v Poeton rather than seek to satisfy the “but for” test. The material contribution test is already being explored in the context of COVID-19 litigation, and it’s possible that arguments for extending it to cases of tuberculosis infection may find some favour, particularly for employer’s liability claims where there is no other obvious source of exposure outside of the workplace.
It is also worth bearing in mind that another impact of the COVID-19 pandemic was the widespread introduction of a communicable disease exclusion in public liability policies, the terms of which would likely extend to employer liability.
“This raises the prospect of insurers declining coverage in public liability claims, leaving defendants to self-fund the defence of the claim, and directly liable to meet any damages and thirdparty costs,” they warn.

It started with one lie. I cited myself as the author of a paper I’d had nothing to do with, as part of a job application. I needed to get the job to move closer to my mum, who had early onset dementia.
That lie snowballed into a web of deception that included plagiarising other doctors’ work. I was in a kind of trance – fabricating lies to cover up lies. In two years, I went from being a cardiothoracic surgeon with a bright future to facing removal from the register due to dishonest behaviour.
Acknowledging the testimonials from my colleagues, the GMC tribunal panel stopped short of the sanction of erasure. I was suspended for a year, during which I went on a life-changing reflective journey supported by my Medical Protection team. It was deeply humbling when the tribunal review panel approved my return to work.
The experience made me see how priceless the support you get as a Medical Protection member is, including having access to in-house lawyers and a dedicated medicolegal consultant who is always there for you. I could not be more grateful.

AI SKIN CANCER DETECTION
DEPLOYED IN
BARKING
& DAGENHAM GP SURGERIES
AI MEDICAL DEVICE
firm Skin Analytics and Together First, a group of general practices in Barking & Dagenham, have partnered to provide faster, more accurate access to skin cancer checks.
Under the partnership, Skin Analytics’ medical grade AI skin cancer assessment tool has been brought into Barking Community Hospital Community Diagnostic Centre.
This is reducing the need for GP appointments and referrals, and has cut down on wait times for urgent checks.
This is the first time the technology will be used in primary care in North East London. Patients will be able to book assessments online.
“Barking & Dagenham has high healthcare demand and limited specialist resources. By using AI to detect skin cancer earlier, we can
reduce unnecessary hospital visits and get urgent cases seen sooner. This is a game-changer for our community,” said Craig Nicolic, chief operating officer at Together First.
Skin Analytics’s tool – called DERM –is the first autonomous AI system for skin cancer detection. It can analyse moles and skin lesions for signs of cancer without needing a doctor to review the case first. The AI has been trained on a large dataset of skin images, allowing it to rule out cancer with 99.8% accuracy. This exceeds the typical 98.9% achieved by dermatologists.
DERM has been used in NHS pathways that have assessed over 145,000 NHS patients, detecting more than 14,000 cases of skin cancer. In existing NHS deployments, it has reduced the number of urgent in-person dermatologist appointments by up to 95%, ensuring that specialists focus on the most atrisk patients.
The AI analyses the lesion and provides an immediate recommendation to healthcare assistants on whether a patient can be quickly discharged (for benign lesions) or whether a specialist referral is needed.
If the AI determines a lesion is not cancerous, patients can avoid hospital visits entirely and be discharged, or be treated for other skin conditions within the community. On the other hand, patients flagged as at risk can be fast-tracked for treatment to the care of dermatologists.
“Early diagnosis is critical in saving lives from skin cancer, but long wait times mean many patients are left in limbo. By bringing DERM into GP surgeries, we’re making fast, accurate assessments available in local communities. This is not just about technology - it’s about making sure people get the care they need, when they need it,” said Neil Daly, chief executive of Skin Analytics.
BMA CALLS FOR NEW INDEPENDENT MEDICAL REGULATOR
PHILIP BANFIELD, the British Medical Association’s (BMA) chair has called for a new independent medical regulator saying that the General Medical Council (GMC), has failed to protect patients and doctors. He has called for the creation of a new medical regulator, solely for doctors.
Results from a survey of 1,539 doctors by the BMA in mid-June indicated that the majority have no confidence in the GMC and more than 80% of respondents support the creation of a new medical regulator.
In a speech at the BMA’s annual meeting, in Liverpool, he warned that the GMC’s approach to regulating physician associates has led to “incessant and unsafe blurring of professional boundaries that threaten the very foundations of practising medicine, what it means to be a doctor” and of what he calls a “dangerous obsession with substituting doctors” at the expense of patient safety.
His comments reflect the BMA’s long-standing criticism of the GMC’s
treatment of doctors and, more recently, its approach to regulating physician associates in a way that fails to distinguish them from qualified doctors. The survey of doctors shows that almost two-thirds of respondents believe the GMC is failing to keep patients safe and fulfil its primary function of protecting the public.
Doctors and their patients, he said, need a regulator that, “protects patients, treats doctors fairly”, and “puts them at the heart of its decision-making”.
The new medical regulator should have a clear statutory duty to protect
the public, rather than this simply being an overarching objective.
It should regulate doctors only, providing the public with a clear distinction between uniquely qualified doctors and non-doctor roles. It has to enforce new statutory protections of medical practitioner titles, to ensure the public is not confused by perplexing NHS job titles that blur the lines between doctors and nondoctors.
Banfield said that it is time for, “an independent regulator that once again commands the confidence of the profession”.
PRIORY LAUNCHES TREATMENT CENTRE IN LONDON
PRIORY, the UK’s largest independent provider of mental health, addiction and adult social care services, is to open a mental health and addiction treatment service in South West London called The Residence.
Located in a private wing of the Priory Hospital Roehampton, it offers a bespoke programme, designed for individuals facing complex challenges such as addiction, depression, anxiety, trauma and eating disorders.
“The Residence is designed to be more than a treatment setting. It’s a space
of safety and hope, where our clients can focus entirely on their wellbeing, free from outside pressure, supported by world-class professionals,” said consultant psychiatrist and lead clinician Donald Masi.
Clients will stay in a 1,200-squarefoot suite, complete with a master bedroom, companion room, therapy and consultation areas, and luxury amenities.
As well as clinicians and therapists, they will have access to treatments, including VR therapy,
neuromodulation, eye movement desensitisation and reprocessing (EMDR), CBT, trauma-focused interventions dialectical behaviour therapy (DBT), relapse prevention strategies, alongside a broad programme of advanced therapies.
In May, the group partnered with Cambridge University spinout Psyomics to help streamline mental health assessments.
Priory is part of the Median Group, a European provider of mental health and rehabilitation services.

GOVERNMENT TO SPEED UP CLINICAL TRIALS
THE GOVERNMENT is planning to speed up clinical trials in the UK and use the National Institute for Health and Care Research (NIHR) Be Part of Research service on the NHS App best suited to their interests and needs.
Eventually the plan will see the NHS App automatically match patients and send push notifications to their phones about relevant new trials to sign up to. It comes as the NIHR launches a UK-wide recruitment drive for clinical trials to get as many people involved in research as possible. Adults across the UK are being urged to register, with underrepresented groups including young people, Black people and people of South Asian heritage particularly encouraged to sign up.
“We know the benefits of embedding clinical research across the NHS
and beyond. It leads to better care for patients, more opportunities for our workforce and provides a huge economic benefit for our health and care system,” said Lucy Chappell, chief scientific adviser at the Department of Health and Social Care (DHSC) and chief executive of the NIHR.
In recent years, the UK has fallen behind as a global destination for these trials, with patients and the wider economy missing out. It takes around 100 days to set up a trial in Spain, but around 250 days in the NHS. The plan will see commercial clinical trial set-up times fall to 150 days or less by March next year.
Currently set up processes for clinical trials take too long as a result of unnecessary bureaucracy and duplication of activities across different agencies and sites.
The government will cut set-up times for clinical trials. Currently, trials have to agree on separate contracts with each part of the NHS they want to be involved.
The plan will introduce a national standardised contract which can save months of time, as well as simplify paperwork to remove duplication on technical assurances. This means if any authority asks for evidence from a study, it can provide it once without having to spend time reframing that evidence differently to meet separate criteria for another authority.
“Ensuring all sites are consistently meeting the 150-day or less set-up time will bring us to the starting line, but together we aim to go further, faster to ensure the UK is a global destination for clinical research to improve the health and wealth of the nation,” said Chappell.

Trusted by Clinicians, Chosen by Patients
Located in the Harley Street Health District, Pharmacierge supports over 4,500 GPs and Consultants with seamless, secure e-Prescribing apps tailored for private practitioners.
With our state-of-the-art robotically enabled dispensary and nationwide delivery, we ensure your patients receive their medications promptly, while you prescribe with confidence - anytime, anywhere.
mPrescribe®
Revolutionises private prescribing by allowing you to prescribe flexibly without a laptop, for delivery to your patients nationwide.
Medication range
Due to the range of specialists we support, we stock and source medication not typically found outside of a hospital setting, including refrigerated, controlled, injectable and biologic medication.
Courier delivery
We include same weekday delivery to London postcodes, or next weekday nationally as standard. International deliveries are also available.

"Your mobile app changed my life!"
— Dr Dominic Paviour, Consultant Neurologist "Intuitive and secure." — Dr Tim Wigmore, Consultant Intensivist & Anaesthetist
Join thousands of clinicians today. Download the app and register online www.pharmacierge.com/register





$140 MILLION INVESTMENT IN NEW THERAPIES FOR NEUROPSYCHIATRIC DISORDERS
DRAIG THERAPEUTICS, a clinicalstage company focused on the treatment of neuropsychiatric diseases, has launched having raised $140 million (£107 million) in the last nine months.
The oversubscribed Series A financing was led by Access Biotechnology, with participation from Canaan Partners, SR One, Sanofi Ventures, Schroders Capital along with seed investors SV Health Investors, which co-founded the company, and ICG.
Draig was formed through a partnership between Cardiff University’s Medicines Discovery Institute and SV Health Investors and launched in 2024. SV Health Investors and ICG provided initial seed funding and built the company. It is the largest investment into a spinout from Cardiff University.
Draig Therapeutics will target key processes in the brain – the glutamate and GABA pathways – to develop new and more effective treatment options.
“We have unique scientific expertise in safely and effectively modulating the core Glutamate and GABA pathways in the brain, which play a critical role in neuropsychiatric disorders.
“Our knowledge of balancing the chemical neurotransmitters in the brain in neuropsychiatric conditions underpins Draig’s pipeline of novel treatments,” said Simon Ward, director of Cardiff University’s Medicines Discovery Institute and of Draig Therapeutics.
The new funds will enable Draig Therapeutics to advance its lead candidate drug, DT-101, into Phase 2 trials this year for Major Depressive Disorder. DT-101 was designed to allow effective modulation of the AMPA receptor without compromising safety. This was borne out in data from a well-tolerated Phase 1a programme in over 60 subjects, which clearly demonstrated target engagement using the novel technique of magnetoencephalography and will be presented at an upcoming scientific meeting.
The funding will also enable Draig Therapeutics to advance two other drugs towards clinical development next year.
The Medicines Discovery Institute was launched at Cardiff University in 2017, with supportive funding from the European Regional Development Fund through the Welsh Government’s Sêr Cymru scheme, to translate the latest biomedical research into new therapies. Significant investment was also received from the Wellcome Trust, Medical Research Council, Medr (formerly known as the Higher Education Funding Council for Wales), and The Wolfson Foundation.
“From the outset, we were drawn to Draig’s bold scientific vision and the founding team’s deep expertise in unlocking high value but previously difficult-to-drug targets in neuropsychiatric disorders,” said Charles Dunn, Principal at SV Health Investors. “Built around an exciting clinical-stage asset, Draig is a perfect example of SV’s strategy to create and build world-class companies around innovative science to deliver high-impact drugs to patients and address major unmet needs.”


RECOMMENDATIONS FOR SCOTTISH MENTAL HEALTH IMPROVEMENTS
DEVELOPED by mental health nurses and students, and academics, with support from carers and people accessing mental health nursing care, Scotland’s Mental Health Nursing Review has a number of recommendations to improve standards of care.
Recommendations include ensuring people accessing services have meaningful involvement in their mental health nursing care; improving support for newly qualified mental health nurses and sharing best practices; considering specific education needs for rural and island settings; and improving access to post-registration learning for mental health nurses across all sectors.
A new implementation group will be established to ensure effective collaboration, delivery, monitoring and evaluation of the review actions.
“The report and its recommendations, mean that patients and mental health nurses who deliver services now and, in the future, will benefit from the reforms,” said Alex McMahon, chair of

the review and former chief nursing officer.
“It will be important to ensure these recommendations are implemented, and one aspiration I and others share is that we will attract and retain even more people into undergraduate
nursing degree programmes,” he continued.
The Mental Health Nursing Review started in 2024 and was an action within the government’s Mental Health and Wellbeing Strategy’s Workforce Action Plan 2023-2025.
ARCTURIS TO USE LEEDS TEACHING HOSPITALS PATIENT DATA
LEEDS TEACHING Hospitals
NHS Trust has signed a multiyear strategic partnership with Oxford-based Arcturis, which uses multi-modal data to support the development of precision medicines.
This agreement will see the Trust provide comprehensive, real-time access to diverse and enriched health data that is geographical representative of the UK population.
“By combining our clinical expertise with Arcturis’ data science and analytic capabilities, this partnership
has the opportunity to accelerate the development of new therapies and improve patient outcomes,” said Paul Jones, chief digital information officer at the Trust.
This partnership will bring Leeds Teaching Hospitals clinical expertise and specialism across a range of therapeutic areas including cardiology, neurology and oncology into the Arcturis network.
The Arcturis network has been approved by the Health Research Authority, the NHS ethics body, and is
designed for diverse types of real-world data including medications, laboratory tests, pathology reports, clinical notes and unstructured data into standardised, disease-specific datasets.
These datasets are then used to generate precision data insights that support activities across the drug development pathway including clinical trials, regulatory submissions and post-authorisation safety studies. All insights generated use anonymised patient data.






EARLY DIAGNOSIS OF SEPSIS IS NEEDED
DESPITE extensive national work and awareness campaigns, the recognition of sepsis remains an urgent and persistent safety risk.
A series of three reports from the Health Services Safety Investigations Body (HSSIB) emphasise that patients and family members are not always listened to when expressing concerns about a loved one’s condition deteriorating. Each report examined individual cases of sepsis relating to different conditions – in one, a patient with diabetes and a foot infection; in another, a patient with severe abdominal pain; and, in the third report, an older patient with a urine infection.
The patient’s experience is analysed in depth in each report, with input from the healthcare providers (this spans GPs, hospitals – wards and emergency departments –ambulance services and nursing homes), individual healthcare staff, and one of the family members of all the patients.
“These reports provide examples of patient safety incident investigations under the Patient Safety Incident Response Framework (PSIRF).
However, they also show a consistent pattern of issues around the early recognition and treatment of sepsis,” said Melanie Ottewill, senior safety investigator at HSSIB.
Although the reports are about different events, there were some common findings in relation to the recognition of sepsis.
They reiterate the difficulty of diagnosing sepsis in its early stages and show how quickly a person with sepsis can deteriorate.
All three reports demonstrate the importance of listening to a family’s concerns about their loved ones. And two of the three reports emphasise the importance of confusion as a sign that a person’s health is deteriorating and the importance of involving family members in assessing changes in a patient’s mental state.
“These findings must be shared widely across NHS trusts – both for the valuable learning around sepsis and as a model for patient safety incident investigations under PSIRF,” said Ottewill.
In response to the reports, Ron Daniels, founder and chief medical officer at the UK Sepsis Trust, called for a commitment from health ministers on the development and implementation of a standardised treatment plan that ensures patients receive the right care.
“By responding effectively and reliably to sepsis, our health service can save lives and improve outcomes for the thousands of people affected by this condition every year,” he said.
He was backed up by Gemma Bedford, managing associate at Freeths in Nottingham.
“Urgent improvements are imperative to ensure that fatalities are reduced and that these horrendous incidences do not continue to occur,” she said.
DAVID HARE DIVERSITY OF PROVISION
DAVID HARE has been chief executive of the Independent Healthcare Providers Network (IHPN), the only membership network for independent healthcare providers, since 2014. In that time, he has consolidated industry representation and grown membership from just over 20 members to 100 today. He talks to Healthcare Today about how the independent sector plans to work with the NHS, why he expects to see opportunities in community and primary care services, and why a positive relationship with the Labour government will improve services for patients.
Paying for treatment has become, as you say, the “new normal”. Is the independent sector now essential to the NHS?
The independent sector is essential to the NHS – and, I believe, to the health of the nation more broadly. What we are seeing now is a growing acceptance that NHS recovery and reform require capital, capacity and capability from the independent sector. For the first time in a long while, there is now crossparty consensus in England that this is necessary.
This shift was clearly signalled by the partnership agreement signed between the sector and the NHS in January, accompanied by a strong statement from the government that it intends to work with the
The chief executive of
the Independent Healthcare Providers Network
talks new opportunities for the independent sector and how he works with the NHS.
Written by Adrian Murdoch.
independent sector to improve NHS services.
Alongside this political shift, there is also growing public acceptance of private healthcare – whether people are choosing to fund it themselves or through private medical insurance One in seven people in the UK now have private medical insurance, a figure not seen since before the financial crash in 2008. Increasingly, private healthcare is becoming normalised – both as part of the NHS landscape and as a separate system – and the public appears broadly comfortable with that.
How would you respond to critics who claim that NHS use of the independent sector is a form of privatisation?
The debate around “privatisation” has, for far too long, held back meaningful healthcare reform in this country. The involvement of the independent sector in frontline service delivery does not mean that patients will have to pay for
treatment, nor does it suggest anything is being taken away from the NHS.
Yet the term is often used in conjunction with phrases like “the Americanisation of healthcare” –and, in my view, that is irresponsible and misleading scaremongering. It plays on fears that the NHS, already under immense pressure, is somehow at risk of being lost. Fortunately, there is no longer a political champion for that frankly nonsensical argument.
The cross-party consensus now in place gives us a real opportunity to move beyond this kind of unhelpful narrative.
To what extent can the independent sector help the NHS reduce waiting times, and what are the limits to its capacity?
In terms of pure capacity, the independent sector is
HARE PROVISION

a million NHS patient referrals are withdrawn or blocked from the system and subsequently offered to private patients. That figure gives a sense of the untapped capacity that could be made available immediately if demand were better managed.
With the right market conditions, there is also scope for further investment in new services and facilities. In recent years, independent providers have built and operated community diagnostic centres, bringing much-needed additional capacity. The same approach could be applied to a new wave of diagnostic centres or dedicated surgical hubs.
Beyond capacity, the independent sector can make a vital contribution to improving
productivity. That includes working in partnership with NHS trusts to raise efficiency in key areas such as diagnostics, where throughput remains a challenge. There is significant potential here – but success depends on partnership. The private sector cannot achieve this alone. It needs the NHS itself to function more effectively.
How do you see the role of independent providers evolving within the NHS?
I think we’re already seeing signs of that evolution. There has been a wave of new market entrants moving into different parts of the healthcare system. Cataract treatment is a prime example. Ophthalmology is now the only major speciality where median waiting times are shorter than they were before the pandemic. That improvement is almost entirely due to new capital investment, expanded services and overall low waiting times. We’re now seeing similar developments in other choice-based services, as well as in areas such as ADHD, where new private sector providers are moving into the mental health space.
What are the operational and financial challenges that independent healthcare providers are facing?
Like all healthcare providers, the independent sector in the UK is affected by the global shortage of healthcare professionals. The private sector is by no means immune. In our annual industry barometer, which we publish on our website, workforce issues consistently rank among the top concerns raised by our members – particularly around access to highly trained professionals.
That said, the private sector tends to perform well when it comes to staff retention. There’s significantly less churn, and the sector places a strong emphasis on empathy and supportive working environments.

We’re also seeing more clinicians actively choosing to move from the NHS into the independent sector. Many are drawn by the calmer, more predictable working conditions and a greater ability to focus on patient care – what brought them into the profession in the first place. On the financial side, while inflation has eased over the past year or so, the earlier energy price spikes and broader inflationary pressures created serious challenges –particularly in terms of construction costs and capital investment. These pressures have been especially acute for providers working closely with the NHS. Given the financial constraints within the NHS, price increases for contracts have not kept pace with inflation. As a result, providers have had to work harder and more efficiently just to maintain margins.
Do you think that regulatory frameworks like the Care Quality Commission adequately reflect the risks and structures of independent provision?
The independent already delivering volumes of NHS
We work closely with the Care Quality Commission (CQC) to help ensure it understands the independent sector – particularly the differences between how we operate and how the NHS does. We have an excellent regulation team here that engages with the CQC every day to support that effort.
In many cases, the CQC’s understanding of the sector is quite

independent sector is delivering record care.
strong. The sector’s performance record reflects that progress: 94% of Independent Healthcare Providers Network (IHPN) members are now rated as “Good” or “Outstanding”. That marks a significant improvement from where we were seven years ago and is the result of a great deal of work on both sides.
Providers across the sector have made real efforts to improve
standards, while the CQC has also worked hard to better understand independent provision and to regulate it appropriately. While challenges remain – and we acknowledge that the CQC itself is undergoing a period of rebuilding – we’re working closely with its new leadership team to ensure that the upcoming changes to the assessment framework are fit for purpose and fully reflect the needs of the independent sector.
How does IHPN work with NHS England, the Department of Health, and other stakeholders to shape healthcare policy without being seen as lobbying for profit over public interest?
We try to be transparent in our approach. When a trade association lobbies purely to generate more income for its members – particularly at the expense of service users or the organisations delivering care – that’s neither credible nor sustainable. In our experience, the Department of Health in England, and indeed
governments in other parts of the UK, are quite attuned to that. They tend to engage with industry in a mature and thoughtful way. There’s a good comparison to be made with how government engages with the pharmaceutical sector: it’s a sophisticated relationship that acknowledges commercial realities, but also recognises the shared goal of delivering better care.
Where industry engagement is narrowly focused on profit and earnings, government tends to take a step back. But where there is genuine alignment – on improving regulatory environments, securing the right policy and funding frameworks, and ultimately ensuring the best outcomes for patients – then meaningful conversations can and do take place.
What is your dream? How should governments engage with independent providers to design long-term NHS strategy?
I believe the government is taking a number of positive steps. We are now just six months into a new Labour administration, and given Labour’s recent history on NHS policy, the signing of a strong and constructive partnership agreement between the government and the independent sector is especially welcome. It commits both sides to a series of actions aimed at improving services for patients – and that, I think, is a very encouraging starting point.
The priority now is to ensure that those commitments are delivered and that real progress is made. Beyond that, we need wider recognition across the entire healthcare system that a diversity of provision is a strength. These approaches should not be seen as substitutes for the NHS, but as complementary. They can help ensure more timely access to care while easing pressure on public services. Because at the end of the day, we are all NHS patients too.
“THE CAPABILITIES AREN’T FULLY
Matea Deliu, the NHS’s clinical lead for primary care digital delivery in South East London, talks about what’s going right, what’s going wrong and what’s on the horizon for AI in the NHS.
Written by Glen Ferris.
AS AN ASSOCIATE medical director and GP with a passion for integrating digital innovations into healthcare, Matea Deliu very much has skin in the game when it comes to the NHS’ continued move towards AI integration.
Part of her role as clinical lead for primary care digital delivery in South East London is to drive the adoption of advanced technology to enhance patient care and streamline services, so she’s perfectly placed to tell Healthcare Today about further government investment into the NHS app, AI accuracy and digital exclusion.
As part of a £50 million upgrade from the government, the NHS app will become the default method to send appointments, screening invitations and other important information to patients. Will this keep on top of demand?
The NHS app intends to be, effectively, a patient portal geared towards patient needs. In its current format, it’s doing some things right. It’s capturing data, giving access to appointment bookings, prescription requests… things patients

didn’t have before. But it’s still relatively clunky. The capabilities aren’t fully realised yet.
In reality, £50 million is probably not enough. The app needs integration with existing tools like the Joy app that already handles community services well, as well as apps from Age UK, VCSE (Voluntary, Community, and Social Enterprise) groups, social prescribing and so on. Right now, NHS app integration is painfully slow.
When we piloted AccuRx SMS integration in SouthEast London, the process took far longer than it should have. This isn’t
CAPABILITIES OF AI REALISED YET”
necessarily the app developers’ fault, they’re resource-constrained. The question is whether £50 million can build an open platform with which others can integrate if they can’t develop everything in-house. It’s a good step, but we’ll need to prioritise strictly patient-centred improvements.
Does the continued turn towards digital tools increase the risk of exclusion of low-income and elderly groups?
This is the age-old question about digital exclusion. I categorise patients into three groups:
First, the digitally savvy who use technology daily. They’ll adopt AI naturally.
Second, the digitally enabled but not tech-savvy. They have devices but need training. Organisations like the Good Things Foundation are vital here in teaching digital literacy skills.
Then there are the digitally excluded, which splits further: those who consciously opt out –they love their landlines and always will – and those excluded by socioeconomic factors. For the latter, we need practical solutions such as loaner phones and data dongles. But we shouldn’t force tech on those who’ve deliberately avoided it. The key is using AI to create efficiency gains that free up capacity

for traditional access methods. As one clinician told me: “AI helps the techenabled group so we can better serve those who need face-to-face care”.
Concerns have been raised about AI accuracy. How do we ensure that all data is reported precisely?
It’s important whenever you implement an AI tool that you should also have a clinical safety officer to guide that implementation. With every tool, regardless of its complexity, there are risks. A clinical safety officer can be useful for teams as you go through the system that’s being implemented and look at everything that could potentially go wrong.
From the AI misidentifying a patient or not effectively triaging to the right place, pinpointing all the risks that can happen from a patient safety perspective is of vital importance. Risks happen with human clinicians, right? So, we can never minimise risk, we can only put in place mitigating factors.
Crystal ball time! Where do you see AI and digital transformation taking UK primary care in the next couple of years?
Where I find AI helps is a lot of the admin burden of workload that I have to go through every single day. There are a lot of back-end processes that are low in terms of risk, but actually high reward. If I can save time by, let’s say, being able to summarise notes from patient records in two seconds, as opposed to trawling through pages and pages and dashboards and dashboards, that’s where I would like to see AI playing a strong part.
LAURENCE GELLER: A UTOPIAN OPTIMIST

TALKING to Laurence Geller
CBE is like being hit by a whirlwind. After a business career that started in hospitality, he is now the country’s largest philanthropic supporter of dementia care research and determined to improve the lives of those who suffer from the disease.
Not only is he chief executive at dementia care provider Loveday & Co, he is also chancellor of the University of West London where he founded the Geller Institute of Ageing and Memory (now the highest rated dementia research organisation in the UK and Europe) and the Geller Commission.
Here, he talks passionately to Healthcare Today about the need for investment in dementia research, why we need to look at dementia care in the UK and why he refuses to settle for mediocrity.
Dementia has been many times described as the defining medical challenge of our time. What, in your opinion, makes it so urgent and so under addressed?
Dementia is a profoundly destructive disease – not just for the individual, but for everyone around them. It is always fatal. It destroys far more lives than just the one affected. The emotional toll on loved ones and carers is immense. Unlike some other conditions, dementia erodes a person slowly, and everyone responds differently to the disease. That unpredictability adds to the burden on families.
What makes it urgent is that we have an ageing population. As longevity increases, so too does the risk of dementia. The Alzheimer’s Society often highlights that one in three of us will develop dementia – a statistic that is probably accurate and rising with age.
But the level of investment in dementia research is startlingly low.

People with dementia are often in the wrong place, receiving the wrong care at the wrong time.
Just 20-25% of the funding that goes into cancer research is allocated to dementia. Only recently have major pharmaceutical companies begun reinvesting – there are now, I believe, around 16 to 19 promising trials underway – but even these focus on addressing aspects of the disease rather than offering a cure.
What is Britain or what are countries that are dealing with this getting right?
We – along with countries like New Zealand and Australia – have a better chance of tackling dementia on a national scale than the US. The US doesn’t have a centralised health system, and many aspects of healthcare are devolved to individual
states. Having said that, the US does invest more than any other country in pharmaceutical research. When it comes to potential cures, or at least treatments that can delay the disease, they are ahead.
In the UK, though, there’s a major problem: fragmentation. Organisations have historically worked in silos. Until we brought them together through the Geller Commission, there wasn’t even a formal forum for them to talk to each other. Fundraising is similarly fragmented, and much of it is focused on cure rather than care. That said, I do think the UK is getting some of its research priorities right – particularly when it comes to identifying what can be

done around early diagnosis and testing. There is momentum. Many in government see dementia as a national imperative – even if it’s one of several.
Does AI play a significant future in dementia care? Or is it diverting us from what we should be doing.
If you look at what’s happening in hospitals, there are no standardised diagnostic tools, no agreed treatment protocols, no clear admission or discharge criteria for dementia. We’ve developed some good practices in individual places – the work of the British Geriatrics Society, for example, is excellent – but they haven’t been adopted nationally.
The consequence is that people with dementia are often in the wrong place, receiving the wrong care at the wrong time. It’s bad for them and bad for the system. It’s also incredibly expensive. We’ve costed it at Loveday, and our high-end model works out at about £120,000 per bed per year. That level of care is appropriate for some people, but 70% of those beds are filled with people who don’t actually need that intensity of support – they’re there because there isn’t another option. It’s a waste of money and of human potential.
That’s why we’ve invested so heavily in monitoring and technology – not just for efficiency, but to improve care and reduce avoidable harm. At
Loveday, we use acoustic sensors, pressure mats, in-ceiling monitors and discreet CCTV to track nighttime activity. We can tell if someone is snoring more than usual, if they’ve left their bed, or if they’re showing signs of incontinence. That data is reviewed every morning and allows us to adjust each person’s care plan.
The next step is to feed that data into AI systems that can identify patterns and predict problems – for example, spotting the early signs of a urinary tract infection, which is one of the most common reasons people end up in A&E. We’re working with UCL in London on this, and our hope is that eventually, we’ll be able to offer the same technology to people in their own homes.
What we desperately need is the same level of passion and structure that is seen in nursing for carers.

Why did you set up the Geller Commission?
My original hope for the Geller Commission was that it would change the world. When we looked seriously at what could make the greatest difference to the nation, it came down to money. Specifically, how money is being wasted because of a lack of system-wide coordination in dementia care.
At the moment, too many people with dementia end up in hospital not because they need acute medical care, but because there’s nowhere else for them to go. What they really need is well-structured, consistent care. We’ve seen at Loveday that
people live longer and avoid hospitalisation when they’re cared for properly.
If we could stop even 10% of avoidable admissions, the savings in bed nights – or more accurately, bed years – would be staggering.
What changes do you think are needed for caregivers to meet the growing demand?
What I want – what we desperately need – is the same level of passion and structure that is seen in nursing for carers.
That means national standards and recognised educational pathways.
It means turning care work into a career, not just a stopgap.
At Loveday, I pay my staff more than the average. We provide better working conditions, and we experience far lower turnover as a result. Why? We’ve created a more humane environment, and that starts with valuing the people who work in it.
But this needs to be system-wide. We need structured roles – junior carers, senior carers – and clear career progression. One size doesn’t fit all. That’s where education is so critical, and yet getting national standards in place has been one of the hardest things I’ve ever tried to do.

How do you ensure that the research conducted at the Geller Institute of Ageing and Memory translates into actual improvements in care homes or community care?
I wish I had a neat answer for how to bring about change – but let me give you an example. I used to be quite a good schoolboy rugby player and played at national level.
During the pandemic, Oliver Dowden, the then secretary of state for sport, called me and asked me to work with civil servants to create proper, consistent concussion protocols. At the time, decisions were left to referees, but we already knew that repeated concussion could lead
to dementia. That was the link to my work.
We brought in the devolved nations, worked with international experts and collaborated with all the key government departments and sporting bodies.
Getting the protocols adopted across professional sports wasn’t easy. But ultimately, the professional game has the infrastructure to support such changes and they did take it on.
Since then, other countries have followed. Australia has adopted similar protocols; New Zealand has them; Canada is discussing them;
and various sporting bodies in the US are now looking closely at our model.
Do I think there’s a single method to get things done? No. There’s no template. What it takes is passionate leadership, relentless lobbying, and the courage to put your head above the parapet.
How should the care industry be interacting with the NHS?
Above all, it’s about refusing to settle for mediocrity.
You need people who are willing to stand at the front, take risks and lead.
You need people who will put their heads above the parapet. That’s what leadership is. And in this work, it’s not just passionate leadership –it’s compassionate leadership too.
Of course, it also requires money. Fundraising is vital. Over the years, I’ve not only raised funds – I’ve also given away a large portion of everything I’ve earned.
The future lies with people like me –and, I hope, with a new generation of people far better than me. People better educated, with more intellectual scope. I’ve never been afraid of failure, and I don’t feel any shame in trying and falling short. But I believe strongly in the need for leadership.
You can’t have just soldiers – you need generals too. You need planners, risk-takers, people willing to be mocked, to lose money, to be shouted down, even thrown out of government offices.
I know it might sound idealistic. I am, without apology, a naive, utopian optimist. I’ve never been embarrassed to say that. And I will never stop trying. Because if not me, who? And if not now, when?
It really is as simple as that.
THE RELENTLESS battle against healthcareassociated infections (HCAIs) continues in hospitals and care homes worldwide. Despite advancements in medical science and rigorous hygiene protocols, these threats persist, jeopardising patient safety and placing an immense burden on healthcare systems.
The recently published UKHSA Point Prevalence Survey starkly highlighted this persistent challenge, revealing the presence of HCAIs in 7.6% of patients – a concerning 1% increase from the 2016 survey. For the most vulnerable, such as orthopaedic patients and children, this figure surged to as high as 16.6%. These aren’t just statistics; these are people at risk, suffering from prolonged hospital stays and battling even more resistant health threats.
Bacterial and viral resistance is a dynamic and evolving threat, constantly demanding vigilance and innovative preventative measures. From the spectre of hospital superbugs like MRSA to the more recent global challenge of COVID-19, medical environments are themselves fertile grounds for pathogen transmission.
It is therefore no longer acceptable to rely on inert, old-fashioned plastic products, which are currently acting as a medium for HCAI cultivation and transmission. Healthcare professionals cannot overlook the safety of their surfaces and need to adopt smarter plastic solutions for their equipment and environment with urgency.
The danger of HCAIs lies in their silent spread. While direct patientto-patient transmission is a concern, contaminated surfaces and objects –known as fomites – play a significant role in disseminating dangerous pathogens. Picture a hospital ward: door handles, light switches, bed rails, IV poles, medical device
SMART PLASTICS: THE UNSUNG HERO AGAINST HEALTHCARE
casings, and even patient gowns and masks are constantly touched by numerous individuals. Each contact point becomes a potential vector for bacteria and viruses.
Traditional plastics, while indispensable for their versatility and cost-effectiveness in healthcare, offer no inherent protection against microbial colonisation. By contrast, these surfaces can become reservoirs for dangerous microorganisms, facilitating their transfer and persistence within healthcare environments.
This is where smart plastics, specifically antimicrobial plastics, emerge as a revolutionary layer of defence. Unlike surface coatings that can wear off or require constant reapplication, antimicrobial plastics are integrated directly into the plastic during the manufacturing process.
This means the antimicrobial properties are embedded throughout the material, providing
Michael Laurier, chief executive Environmental Technologies, continued reliance on inert healthcare settings is a dereliction patient safety.
a continuous, long-lasting and proactive barrier against contamination that does not diminish over time or with cleaning.
How do these smart plastics work?
The active ingredients within these formulations are designed to disrupt microorganisms, whose lifespan depends on many factors. Viruses must invade the cells of a living host to replicate, while bacteria do not need a living host to replicate, but both bacteria and viruses can survive for several days on surfaces. Surfaces of almost any kind can therefore be a continuing source of infection.
If antimicrobial plastics are used during the plastic manufacturing process it makes plastic surfaces
PLASTICS: HERO IN THE FIGHT HEALTHCARE INFECTION

executive of Symphony Technologies, explains why the inert plastics in critical dereliction of duty to
lethal to microbes. For bacteria, this might involve interfering with cell wall synthesis or protein production, leading to their incapacitation or destruction. For viruses, the mechanism often involves denaturing their protein coats or disrupting their genetic material, rendering them non-infectious. This robust, multi-faceted approach ensures a broad spectrum of efficacy against a wide array of pathogens.
They have been rigorously tested to prove effectiveness against a formidable list of dangerous organisms, including COVID-19, MRSA, E. coli, Salmonella, Listeria, Pseudomonas and Aspergillus Niger.
The impact of this technology is not theoretical; it is demonstrably
effective. Antimicrobial plastic gloves and masks have already been proven to achieve a 99.9% virus reduction. The potential impact, if every plastic glove donned, every mask worn, and every surface touched in a healthcare setting possessed this quality, would be immense. A small change in plastic production and procurement can have a significant impact on reducing surface contamination and lowering the risk of infections.
The applications of these plastics in healthcare are pervasive. Personal protective equipment, such as plastic gloves, masks, caps, shoe coverings and even gowns made from man-made fibre, with builtin antimicrobial properties, offer enhanced protection for both healthcare workers and patients.
Mattress covers, bed rails and medical device casings can actively combat microbial growth, meaning that surfaces that have to be constantly touched have a layer of built-in protection. Similarly, high-
touch environmental surfaces, such as door handles, light switches, and wall panels can now become selfsanitising.
Medical supplies and equipment packaging can maintain sterility and prevent contamination from external sources – an added layer of protection on an already sanitary product. Components of medical equipment such as stethoscopes and infusion pumps can also be manufactured with inherent antimicrobial defences.
It is important to understand that antimicrobial plastics are not a silver bullet to completely prevent infection, nor a replacement for sterilisation protocols and good housekeeping. Instead, they serve as another layer of defence working in tandem with existing control measures – and one that cannot be neglected any longer.
Plastic is a core part of healthcare; it’s everywhere, and when lives are at stake, outdated plastic products are unacceptable. The continued reliance on inert plastics in critical healthcare settings where pathogens thrive is a dereliction of duty to patient safety. Yet the healthcare sector has always been at the forefront of innovation to improve patient outcomes. Thus, the adoption of smart, antimicrobial plastics represents the next logical, essential step in this ongoing evolution.
Embedding antimicrobial plastics universally into hospital and carehome environments is a tangible, effective strategy that healthcare professionals can deploy to address stubbornly high infection rates and improve patient outcomes at very little extra cost. Smart plastics are not just an innovation; they are an imperative for a healthier future.
The time for these changes is now – universally and urgently – before more patients are needlessly harmed by preventable infections.

“WHY SMART OPERATING ROOMS ARE THE FUTURE”
AS A PRACTISING surgeon and the founder and chief excutive of Proximie, a fast-scaling healthtech firm, Dr. Nadine HachachHaram feels that the key to optimising efficiencies in the operating room is through virtual collaboration and smart data sharing.
Here, she explains why digitising operating rooms and driving AIpowered insights from surgical data helps to improve patient outcomes, improve productivity and reduce workforce burnout…
What problem were you trying to solve when you set up Proximie?
I’m a practising surgeon, so I’ve seen the fundamental challenges of healthcare and surgery first-hand. With surgery, there is a huge supply-and-demand gap. We have loads of patients on waiting lists. We have finite operating rooms (ORs) and we’re not going to build 100 more operating rooms or create hundreds of more surgeons overnight. How are we going to connect expertise, share best practices and accelerate the delivery of care in a safe and proactive way?
Operating rooms are hugely expensive assets for a hospital and, when you think about the equipment, the staff, the real estate and so on, it’s all quite analogue. Patients are wheeled in, surgery is done, and patients are wheeled out, someone writes up the case notes, and it’s onto the next…
Proximie’s solution was intelligent, connected operating rooms. They are, I feel, a real solution for optimum efficiency because they can help us scale expertise by allowing us to train twice as many doctors and nurses in
half the time and also virtually connect to any expert who can guide you and give you expertise during a case. Additionally, smart operating rooms allow you to collect and synthesise data sets, collating the data sitting on medical record systems and devices into actionable insights that optimise operational workflow. Early results showed we could increase productivity by up to 24%.
How has this been received by people working in these operating rooms?
There’s a huge appetite for solutions that take off that burden, especially since healthcare workers spend about 30% of their time on documentation. The key insight was that it can’t be one operating room here, one operating room there, you have to go enterprisewide to create truly smart, connected, data-driven ORs. This means building tools to automate your operation notes, your coding and so on… The more you can remove the human from repetitive task loops, the more staff can practice at the top of their license. With a presence in 800 hospitals across 50 countries, the Proximie model is proving effective.
The NHS is such a patchwork of so many different elements. How do we tackle the issue of that connectivity?
We’re in about 30% of NHS hospitals already, but there are still challenges with the NHS. You still have to go from hospital to hospital, going through approval processes at each stage. I hope that more central power will streamline this issue soon. In the meantime, although some are frustrated with the pace of the NHS to adapt to change, we believe we can add a lot of value and so we’re working with hospitals up and down the country really to help them bring that value.
How do you see AI changing surgical training and collaboration in the next five years?
Not every AI model needs to become a company, which is why we built a platform where researchers can deploy models without starting businesses. Imagine a small team creates a blood loss detection algorithm, for example, they shouldn’t need to build a sales team to get it into ORs. This collaborative approach means the models themselves become commoditised. It’s about deployment in clinical contexts. We’re already running other people’s models in our system to accelerate real-world impact.
How do regulatory challenges within the UK compare to, say, the US and Europe?
Every country has its preferred approaches, so going global requires difficult choices early on. We own the whole stack, we have no third-party dependencies that might work in one market but not another. This meant building flexibility to work with AWS, Azure, or other regional cloud providers from day one. But, once you’ve done the hard work of compliance, scaling becomes about proving value. That’s why we invested early in getting the architecture right, it’s now paying dividends across 50 countries.
As a leader in clinical and tech innovation, what lessons have you specifically learned at the intersection of medicine and entrepreneurship?
I feel privileged to sit at this intersection because having walked the walk as both clinician and entrepreneur

OPERATING FUTURE”
changes your perspective. Too often, people opine about innovation without having to execute. My role is to help technologies with good product-market fit demonstrate return on investment quickly by connecting entrepreneurs, providers and investors. The urgency comes from knowing the status quo in healthcare doesn’t work anymore.
As it pertains to healthcare, do you feel that disruption is the way forward, considering how reluctant some healthcare providers can be to evolve?
Walking in with a hammer isn’t the answer, but neither is accepting the status quo. The sweet spot is when hospitals help co-develop solutions and solve problems through collaboration.
Evidence of change is everywhere. Hospitals now hire chief AI officers and innovation teams. While five years ago, digital ORs seemed impossible, today they’re becoming the gold standard.

HIS LEADERSHIP in guiding national-scale healthcare programmes through critical transformation has led him to the conclusion that it’s time to start over and think differently.
Just as Monzo transformed the banking industry, Michael Hardman’s view is that focusing on the digitisation of existing assets is stalling progress. Reflecting on the plans, he shares with Healthcare Today how a proposed challenger hospital model could feasibly help take the NHS 10 Year Health Plan to its ultimate conclusion.
A bold vision needs brave interpretation
The 10 Year Health Plan indeed delivers a compelling vision: a health system that is digital-first, inclusive and resilient. The ambition is clear. Patients will benefit from better, seamless, connected care; clinicians will be equipped with real-time data and smarter tools; and healthcare will become more accessible to every community. But setting out this long-awaited vision is just the beginning. The more urgent question is how we translate this all into practice? Upgrading systems alone will not be enough. If we are serious about transformation on this scale, we need to go further and rethink fundamental assumptions, including those surrounding what a hospital is and needs to be in the years ahead.
It’s time to collectively challenge the status quo
Core to the new plan is the commitment to a Single Patient Record, more integrated communitybased care and digital tools that support both self-management and system-wide visibility. Importantly, these goals are more than technical milestones as achieving them means tackling the deeply ingrained defaults of our current system, which is built around buildings, centralised
RETHINKING INFRASTRUCTURE FOR THE NHS’S DIGITAL FUTURE
After many years of being parachuted in to patch up distressed hospital systems, Aire Logic’s Michael Hardman is advocating for a radical new approach to healthcare IT.

decision-making and disjointed technologies. We’ve explored this call for change in a recent report, The Everywhere Hospital, posing the question: what if we were to start from scratch? What kind of care system would we design if digital capabilities, clinical intelligence and patient agency were built in from the very beginning?
Rethinking ‘Hospital’ as infrastructure, not place
For more than a century, the hospital has been the physical heart of healthcare delivery. But what happens when the needs, behaviours, and expectations of patients - not to mention the technologies that serve them - move
beyond those physical boundaries? A distributed care model where digital interfaces, community resources and specialist hubs work together as a unified system, could reduce waiting times, alleviate pressure on overstretched services and bring care closer to those who need it. The hospital therefore becomes less of a location and more of a blueprint. A flexible, responsive framework for care that moves with people, rather than asking people to move around it.
Practical alignment with the 10 Year Health Plan
Much of what we’ve proposed in the Everywhere Hospital concept mirrors the aspirations now embedded in the
INFRASTRUCTURE
FUTURE

10 Year Health Plan. A user-governed and interoperable patient record directly supports the goal of a Single Patient Record, while addressing long-standing fragmentation.
The reimagining of the NHS App as a control centre for personal health makes sense only in a system where individuals are empowered to lead their own journeys, rather than simply receiving services. Similarly, retiring outdated legacy systems becomes more feasible when we design processes for the present instead of digitising what no longer fits. Perhaps most crucially, hybrid models that combine digital-first convenience with in person care, when it matters most, show how inclusion and efficiency can coexist.
Mindset shifts, not just tech shifts
Working with this model comes with very obvious challenges, of course. Transforming infrastructure is one thing; shifting culture and mindset is another. True change means revisiting the assumptions we’ve internalised about professional identity, institutional authority and patient participation.
Building adaptive, modular systems can feel uncomfortable - especially in a sector where reliability, regulation and stability rightly matter. But clinging to systems only delays the kind of improvement that patients and healthcare professionals deserve.
Bridging public and private: A shared responsibility
The 10 Year Health Plan recognises that innovation won’t come from within the NHS alone. Successful collaboration is not about handing over control but rather creating space for experimentation, where public services, the private sector and independent thinkers can work side-by-side.
We should welcome contributions that push the conversation forward, even when they unsettle us. That’s what we’re trying to do with The Everywhere Hospital. We don’t claim to have all the answers but we see value in constructively challenging the status quo - particularly at a time when conventional answers are proving insufficient. It’s important to remember that when you design digital systems in healthcare, you’re not just building software, you’re making decisions about trust, access, autonomy and equity. This also presents us with a huge window of opportunity to do things better than we’ve done them before.
From ambition to architecture
The 10 Year Health Plan gives us a destination and what we need now is the architecture to help get us there. In other words, the physical, cultural and technical scaffolding to support this level of transformation.
Some of that will involve investment in new platforms and skills but, just as importantly, will be the willingness to let go of broken structures and stagnated mindsets. Perhaps the most responsible move is not to modernise but to begin again, guided by the needs of today rather than the habits of the past.
In healthcare, as in technology, progress doesn’t always mean iteration. Sometimes it requires a radical rethink.
THE INS AND OUTS OF MEDICAL INDEMNITY
Medical Protection explores the legal obligations for every doctor working in the UK and explains the range of benefits offered by theirs services.
EVERY doctor working in the UK is legally required to have adequate indemnity before beginning practice. This is to cover legal defence fees if a patient sues for negligence, and any compensation awarded to the patient.
Doctors whose indemnity falls short of ‘adequate and appropriate’ protection can have their licence removed by the GMC [1]
For those working in the NHS, the minimum legal requirements are covered by the employer through state-backed indemnity schemes, although there is no state indemnity for GPs working in Northern Ireland and Scotland.
State-backed indemnity also has its limits. It does not cover claims arising from private practice, for instance. Fee-paying work such as report writing, travel vaccinations, insurance forms, and private prescriptions are also not included.
The state won’t provide advice and legal representation at disciplinary hearings, support during inquests, help during a criminal investigation, or protection for Good Samaritan acts. Nor will the state always cover work commissioned privately by the NHS, such as under waiting list initiatives. This is where private insurers and medical defence organisations (MDOs) step in.
There are a number of insurance policies and indemnity schemes that can fill the gaps left by state indemnity. Some, such as Medical Protection, also offer additional services that help doctors reduce their risk of receiving a claim or complaint, and support them through the stress of an investigation.
The benefits offered by Medical Protection include:
• Indemnity for clinical negligence claims
• Support and representation in GMC investigations
• Help in disciplinary proceedings
• Assistance with criminal investigations arising from your clinical practice
• Representation and assistance in coroner inquests
• Help responding to patient complaints
• Medicolegal advice line, available 24/7 for emergencies
• Support for managing unwanted media attention
• Protection for Good Samaritan acts worldwide
• CPD courses and online learning
• Digital publications, factsheets, and case studies
• Confidential counselling and wellbeing advice
• HR and business support for practices Choosing the most appropriate protection can be confusing, so it is worth highlighting some of the key differences.
Insurance or indemnity: What’s the difference?
Medical malpractice insurance is usually bought as a stand-alone policy from an insurance company.
It provides cover within set limits and restrictions, set out in the terms of a legally binding contract. Insurance policies are usually ‘claims-based’, meaning they only cover claims for incidents that arise, and are reported while the policy is valid.
Medical indemnity – as provided by a mutually owned, non-profit organisation known as a medical defence organisation (MDO) – is typically part of a wider package of benefits, which are discretionary. There is no contract stipulating the circumstances under which a claim will be paid. This allows MDOs the flexibility to offer as much help as is needed, especially in unforeseen situations.
It also allows them to decline assistance, although this is extremely rare. The reason for declining assistance is usually due to a member deliberately withholding or providing false information about the scale or nature of their work. Of course, this would also affect an insurance policy.
Claims-based versus occurrence-based indemnity
Claims-based indemnity only provides protection against incidents that occur and are reported during the policy or membership period. Once the policy or membership expires, so does the protection. This means that if a claim arises outside of that period of membership, you would not be able to seek assistance unless you bought ‘run off’ cover. This can be expensive and limited to a set number of years, whereas claims can arise even decades after an event. This is worth

considering, given the average delay between an incident and the reporting of a claim is currently over five years [2]
Occurrence-based indemnity provides protection against incidents that happen during the membership or policy period, regardless of when the claim is made. Providing you were in membership and paying the correct subscription at the time of an incident, you are protected even if you’re retired or no longer a member. This means that you are protected for future claims arising from any year in which you were a member.
The choice is yours
The final choice of MDO membership or insurance policy will depend on the specific
circumstances of the doctor, their area of practice and career priorities.
For some, an off-the-peg policy may offer a sufficient safeguard in situations not covered by statebacked indemnity. Others may be looking for a more proactive and supportive solution.
At Medical Protection we have over 130 years of experience of dealing with medicolegal matters. This gives us a unique insight into why things go wrong and why complaints and claims arise.
The indemnity offered by Medical Protection is unlimited, with no financial caps on the legal fees we can incur or the compensation we can pay out. This allows us to protect and defend our
REFERENCES:
[1] Domain 4 Trust and professionalism - GMC (gmc-uk.org)
[2] MPS data; based on claims reported by UK medical members between 1 Jan 2019 and 31 Dec 2024.
members from legal, reputation, and financial consequences.
We are ready to intervene at every step of the process. By promoting best practice through our risk management resources, we help prevent problems from arising in the first place. We can nip emerging issues in the bud by helping doctors respond to patient complaints.
We offer legal representation and support to members throughout legal and disciplinary hearings. And our counselling and wellbeing services provide welcome relief from the stress that an investigation brings.
For more information or to get a quote visit: Medical Protectionthe world’s leading medical protection organisation.
THE RISKS OF AI TRANSCRIBING
THE USE of Artificial intelligence (AI) is rapidly transforming healthcare delivery, particularly in administrative and documentation tasks.
One area seeing accelerated adoption is AI-enabled ambient scribing - technology that captures and transcribes conversations between clinicians and patients, often in real-time. While the promise of these tools is substantial, the risks are equally critical, particularly regarding patient safety, data protection, regulatory compliance, and legal liability.
AI transcription tools and how they’re used
AI transcription tools such as Dragon Medical One, Amazon Transcribe Medical, Suki Assistant, Tali AI, and Dictate.IT are now embedded in clinical workflows. These systems often combine speech recognition, natural language processing (NLP), and generative AI to produce structured clinical notes or patient letters from spoken consultations.
On 27 April 2025, NHS England released updated guidance on the deployment of these technologies“Guidance on the use of AI-Enabled Ambient Scribing Products in Health and Care Settings” - which builds upon earlier initiatives to reduce documentation burden. The guidance supports innovation while reinforcing the principles of safety, transparency, professional oversight, and data privacy. Its principles apply equally to independent private healthcare providers.
Uses include:
• Generating outpatient letters automatically post-consultation
• Real-time transcription and summarisation of consultations
Neil Rowe, senior in-house counsel at THEMIS Clinical Defence, considers the potential pitfalls of relying on transcription tech.

• Discharge summaries and follow-up documentation
• Integration with electronic patient record (EPR) systems
The new guidance stresses that ambient scribing tools must not replace clinician judgement, and that outputs should always be clinically reviewed and verified before being finalised.
Benefits of AI transcription in healthcare
• Efficiency gains: Clinicians save time previously spent on manual note-taking and typing, with overall cost gains.
• Enhanced patient interaction: Less screen time means more eye contact and better communication.
• Standardised documentation: Structured, templated output improves record clarity and auditing. Better accuracy enhances patient care.
• Real-time availability: Notes can be produced instantly, aiding continuity of care.
• Staff wellbeing: Reduced administrative workload contributes to lowering burnout rates.
• Scalability: Supports practices experiencing workforce shortages or high demand.
These benefits support the NHS’s broader digital transformation priorities publicised at the start of this month under the 10 Year Health Plan. However, the 2025 guidance makes clear that these tools are assistive, not autonomous.
Key risks and how things can go wrong
• Transcription errors: Speechto-text engines, while improving, still struggle with homophones, medical jargon, and accents. A misheard phrase can drastically change the clinical meaning. For example, a GP’s comment “No chest pain today” was transcribed as “Chest pain today” in the letter. The letter was not reviewed before sending, and the error led to an unnecessary cardiology referral.
• Clinician over-reliance or user error: Guidance warns against passive acceptance of AIgenerated documentation. Overtrusting output risks embedding serious errors into the patient record. Clinicians must also be wary of operating the product so that it generates output beyond its intended scope.
• Invisibility of errors: AIgenerated text often reads fluently and convincingly, what experts call “authoritative but incorrect”. Sometimes AI invents text i.e “hallucinations”. Subtle clinical misstatements may go unnoticed and potentially lead to errors like misdiagnosis unless carefully reviewed.
• Loss of clinical context: Ambient scribing tools might fail to capture key nuances such as facial expressions, body language, or hesitation, which are often crucial for safeguarding or differential diagnosis. Clinician observation and recording is critical.
TRANSCRIBING IN HEALTHCARE
• Confidentiality and cybersecurity risks: Ambient tools often store data temporarily. The 2025 NHS guidance mandates data minimisation, encryption, and compliance with UK GDPR, yet any lapse in supplier controls could result in a breach. For example, a transcription firm contracted by a Trust was found to have used subcontractors abroad, without informing the data controller, raising serious compliance concerns.
• Interoperability and record fragmentation: Without tight EPR integration, AI-generated documentation can result in duplicate or inconsistent records, undermining clinical handover and coordination.
Legal and regulatory liability
Responsibility for errors depends on the origin and nature of the failure:
• Clinicians: Remain personally accountable for checking the accuracy, completeness and proportionality of any record that bears their name. This is reinforced by GMC Good Medical Practice 2024.
• Healthcare organisations: Have a duty to ensure proper procurement, governance, training, and oversight of AI tools. Failure to do so could give rise to corporate liability.
• Vendors and developers: May be liable under product liability law, especially if faults arise from defective algorithms or insufficient limitation warning.
• Data processors: Third-party service providers who mishandle or unlawfully process patient data could face ICO action, civil claims, and reputational damage.
Claims could arise in negligence, contract, breach of statutory duty, breach of confidence, or under data protection laws, depending on the facts.
Practical risk mitigation strategies
The NHS England 2025 guidance recommends a governance-led approach to safe deployment. Practical steps for clinicians and managers include:
• Mandatory human review: No AI-generated document should be approved or sent without clinician verification.
• Ongoing training: Clinicians must be trained to understand how AI tools work, including common pitfalls and workarounds.
• Robust data governance: Ensure clear DPIAs, data flow maps, and supplier compliance with NHS DTAC (Digital Technology Assessment Criteria).
• Audit and oversight: Establish internal audit mechanisms to track discrepancies between AI drafts and finalised notes.
• Incident reporting: Errors should be captured through local risk systems and reported via PSIRF.
• Clear accountability: Local policies should specify responsibilities at each stagefrom capture to verification to storage.
• Robust contracting: Providers should ensure contracts with suppliers are clear on roles, responsibilities and liabilities.
The road ahead
The use of AI in clinical documentation is set to expand further, especially as large language models (LLMs) become more embedded in NHS infrastructure.
Emerging tools may not only transcribe but triage, code, and even generate clinical summaries or follow-up plans using broader patient data.
NHS England’s 2025 guidance will be reviewed again in six months as the picture quickly evolves and represents a timely intervention to shape this evolution responsibly. Regulators including the CQC, MHRA, and GMC are expected to increase scrutiny of how these tools affect clinical decision-making, patient experience, and service delivery.
The road ahead will likely be bumpy. Only three weeks ago, it was reported by Sky News that NHS England have written to hospitals in June, warning them to stop using AI transcribers from certain suppliers that do not comply with minimum standards, risking clinical standards, patient safety, data protection, and the wider digital strategy.
Conclusion
AI-enabled ambient scribing tools offer immense potential to reduce the documentation burden on healthcare staff, improve standardisation, and unlock new efficiencies in clinical care. However, their use introduces complex risks that can impact patient safety, clinician accountability, and institutional liability.
NHS England’s 2025 guidance serves as both a roadmap and a warning: use these tools well, but use them wisely. For healthcare providers, indemnifiers, and legal teams, this is a pivotal opportunity to embed safety, governance, appropriate cover and legal defensibility into how AI transcription is adopted across the entire sector.
THE DIGITAL PRESCRIBING DILEMMA

ABBC undercover investigation conducted in June 2025 revealed a troubling truth: online pharmacies were able to issue prescriptions for potent GLP-1 weight-loss medications, such as Wegovy and Mounjaro, simply by using falsified patient data submitted via questionnaires and photos without any video consultation, verified medical records, or clinical engagement.
GLP-1 agonists, which mimic the hunger-reducing hormone, are classified as high-risk medications by the General Pharmaceutical Council (GPhC).
Following the BBC’s tests, the GPhC reiterated that online services must verify a patient’s height, weight, BMI, and access relevant records and conduct either a video or in-person consultation before prescribing. Despite this, prescriptions were issued within days based on incomplete, and in some cases manipulated, submissions.
TMLEP’s lead healthcare investigator Nina Vegad asks why safeguards must catch Up with innovation

Why this matters: The risks of questionnaire-only prescribing
Online prescribing services offer clear advantages including greater accessibility, shorter wait times, and discretion for patients.
However, the risks of removing meaningful clinical verification are significant, particularly with high-risk drugs like GLP-1s, which have serious potential side effects, including gastrointestinal issues, allergic reactions, and psychological complications such as disordered eating.
The investigation revealed:
• Patients could easily alter their weight data to qualify for treatment.
• Hair loss after receiving Mounjaro from an online provider using inaccurate information.
• There were no safeguards in place to screen for eating disorders or confirm medical histories via GP records or direct consultation.
As the demand for these medications continues to grow, the pressure on digital providers to supply fast solutions must not override the principles of patient safety.
The role of independent clinical investigation
At TMLEP, our experience in clinical investigations highlights why independent reviews are essential when safety concerns arise, especially in evolving care models like digital health.

When incidents occur, a thorough investigation:
• Reconstructs the clinical journey, identifying not just what went wrong, but why, highlighting system gaps, training issues, or misaligned protocols.
• Provides clarity and accountability, ensuring that patients, providers, and organisations understand the facts behind adverse events.
• Drives change, informing policy updates, improving governance frameworks, and ultimately helping to prevent recurrence.
As a national leader in healthcare investigations, TMLEP is uniquely positioned to support providers and regulators in embedding evidencebased safety measures into their models before harm occurs.
Strengthening the framework: What needs to happen next
To ensure online prescribing evolves
responsibly, we must embed safeguards that mirror the rigour of in-person care. This includes:
• Mandatory audit trails within digital systems to track prescribing rationale and safeguard against misuse.
• Routine oversight and mystery shopper-testing by regulators to assess compliance in real time.
• Cross-sector collaboration between independent investigators, digital health developers, and prescribers to design safer, more accountable systems.
• Clear escalation pathways for when prescribing protocols are bypassed, so that patient concerns lead to action.
The GPhC has taken commendable steps in tightening guidance and committing to enforcement, but as the digital landscape rapidly evolves, so must our mechanisms for learning, review, and prevention.
Conclusion: Innovation demands integrity
Digital prescribing holds tremendous potential. But innovation without scrutiny leads to blind spots, and ultimately, to preventable harm.
At TMLEP, we believe that every healthcare model, traditional or digital, must be built on a foundation of safety, transparency, and learning.
Independent clinical investigation is not just about identifying errors; it’s about enabling better systems, empowering patients, and informing future models of care.
As the healthcare sector embraces new tools and technologies, the imperative remains the same: to do no harm, and to hold ourselves accountable when harm occurs.
For more information on TMLEP’s services, click here.

tenharleystreet.co.uk 020 7467 8300 Liverpool eightyeightrodneystreet.co.uk 0151 709 7066 Providing first class medical consulting and therapy rooms at prime locations in Central London and Liverpool
PRIVATE HEALTHCARE MARKETERS: GENERATE MORE ENQUIRIES FOR YOUR CLINIC WITH MEDIAHAWK
With NHS pressures, long waiting lists, and limited access to care, more patients are turning to private healthcare. That shift brings growing pressure for marketers in the sector.

HERE’S how Mediahawk helps you reach the right patients and drive more enquiries – enabling faster treatment and a more profitable, competitive service.
Understand diverse patient journeys
Patient needs and behaviours vary greatly. According to the Private Healthcare Information Network, factors like condition type, urgency, emotional state, confidence, and prior experience with private care all influence how patients research their options.
Call tracking helps you make sense of these varied journeys by revealing common entry points and engagement triggers. “With that information, you can focus on the channels and activities that drive more enquiries,” says Faye Thomassen, Head of Marketing at Mediahawk.
Track every call and link them to revenue
Mediahawk connects every enquiry to its source - online or offline. Static numbers reveal which calls come from print ads, billboards, or brochures, while dynamic numbers

track digital interactions like website visits and downloads.
“With Sales Matching, you can go a step further by linking those calls to booked appointments and revenue,” Faye explains.
“See which channels drive specific consultations, understand their value, and know exactly what’s generating high-value leadslike orthopaedic enquiries that lead to scans.”
Reach patients at the right point
Research from the Independent Healthcare Providers Network shows 43% of patients considering private care don’t know how to access it, and 63% aren’t sure about treatment costs.
Clinics must offer clear, helpful information on procedures, pricing, and next steps – not just to guide research, but to build trust.
“Effective marketing isn’t just about becoming a trusted source,” says Faye. “It’s about ensuring that once patients are ready, they choose your clinic – and become a source of revenue.”
The key is capturing engagement when they’ve done their research and are ready to talk
Summary
With Mediahawk, you’re not just driving more enquiries – you’re finding ways to engage high-intent patients who are ready to start their care journey. You’re unlocking insights into which channels and activities deliver value, and which need optimising. And if any of your strategies aren’t working out, you have the tools to refocus your efforts and budgets elsewhere.
Book a Mediahawk demo and see how you can get more enquiries.
WHY SIMPLICITY AND TRANSPARENCY MATTER IN MEDICAL BILLING
ONE OF the most common frustrations we hear from consultants is the lack of clarity when it comes to billing, both in the way fees are collected and in understanding what’s happening behind the scenes once invoices are sent.
When it comes to medical billing services, clarity and simplicity should be the baseline and not a bonus. Yet for many consultants, the process can feel anything but straightforward. Confusing fee structures, limited visibility into the status of invoices, and inconsistent communication with patients and insurers can lead to poor cash flow, administrative overload, and rising stress levels.
We believe private consultants deserve something better:
• A simple, transparent pricing structure with no surprises
• A live, 24/7 reporting dashboard that puts you in control
Here’s why these two elements (simplicity and transparency) are more than just conveniences. They’re critical tools for building a healthy, efficient, and profitable private practice.
The pitfall of complexity
Medical billing can be notoriously complex, especially when working with insurers, chasing excess payments, or managing large caseloads. Unfortunately, many
Clinical care is your priority but managing the business side of medicine is equally essential to maintaining a successful and sustainable practice, says Medserv’s Derek Kelly.
with confidence. Medserv offers consultants a simple and transparent fee structure, so you always know what you’re paying and why.
No hidden fees. No confusing breakdowns. Just a straightforward service aligned with your practice goals.
This simplicity helps you:
• Plan your overheads accurately
billing solutions make matters worse with:
• Hidden costs or unclear charging models
• Delays in communication
• Outdated reporting tools or static monthly summaries
• Limited support when questions arise
For a private consultant, this means:
• A disconnect between clinical activity and financial return
• Difficulty forecasting income
• Stress about unpaid invoices or missed patient charges
• A general feeling of “not knowing what’s going on”
Complexity in billing doesn’t just waste time, it impacts your income and undermines confidence in the financial side of your practice.
Why simple, transparent pricing matters
A clear pricing model from your billing partner allows you to plan
• Understand the value you’re getting from your billing provider
• Avoid surprises at the end of the month
• Have confidence in your partnership
Just as you’re transparent with your own patients about fees, your billing partner should provide you with that same level of respect and clarity.
Always-on insight with real-time reporting
Billing isn’t just about sending invoices, it’s about knowing what’s happening to them after they’re sent.
Who has paid? Who’s late? Are claims stuck with insurers? Are excesses being collected efficiently?
Medserv provides a secure, 24/7 online reporting dashboard that gives consultants access to live updates on:
• Invoice and claim status
• Patient and insurer payments
MATTER

• Outstanding balances (including excess payments)
• Average time to payment
• Monthly income trends
This level of transparency means:
• You don’t have to wait for end-of-month reports.
• You can check on your finances any time, from any device.
• You’ll know instantly when a payment is received, or a claim is delayed.
In short: you’re always in the loop without having to chase.
Improving financial performance without lifting a finger
By combining simple pricing with clear, real-time reporting, Medserv allows consultants to:
• Improve cash flow with timely follow-ups
• Reduce admin time by eliminating the need to manually track payments
• Gain strategic insight into how their practice is performing financially
• Make informed business decisions backed by real data
You stay in control — without needing to micromanage the process.
Supporting your patients, too
Clarity in billing doesn’t only benefit the consultant. It also improves the patient experience.
Medserv ensures that patients receive:
• Professional, timely invoices
• Clear explanations of charges and insurance excesses
• Friendly follow-up communications when needed
This helps preserve the clinical relationship, maintain trust, and reduce uncomfortable financial conversations between you and your patients, all while ensuring the practice gets paid.
The right billing partner can make all the difference
Private practice is hard work. You shouldn’t also have to be a finance expert, a credit controller, and an IT manager just to get paid for your time and expertise.
At Medserv, we believe the foundation of a successful billing partnership is clarity in pricing, in reporting, and in communication.
That’s why we offer:
• Straightforward billing with no surprises
• Live, transparent reporting accessible 24/7
• Support from a team who understands the private healthcare landscape
If you’re ready to remove the uncertainty from your billing and gain true control over your practice’s financial health, we’re here to help.
Discover more about Medserv here.
Published by Healthcare Today Media Ltd. Healthcare Today is editorially independent. Material is governed by copyright.
No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment.
© Healthcare Today Media Ltd 2025 Registered office: Connect 38, 1 Dover Place, Ashford, Kent, TN23 1FB

Tell us your news: Contact: Adrian Murdoch, Editorial Lead adrian.murdoch@healthcaretoday.com +44 (0)7983 407607
Advertise with us: Advertise with us: Contact: Andrew Schofield andrew@spotonmedia.co.uk +44 (0)7862 133912
To download a copy of our media pack, click here.