INDEPENDENT PRACTITIONER TODAY
The business journal for doctors in private practice



By Robin Stride
Private doctors face a huge defence cover shake-up under Government proposals advocating the merits of insurance rather than the discretionary cover provided by traditional medical defence organisations (MDOs).
Responses to the 51-page discussion document, reflecting widely different views, are being prepared by doctors’ representatives, private hospitals and interested parties.
The Department of Health and Social Care’s report, called ‘Appropriate clinical negligence cover – a consultation on appropriate clinical negligence cover for regulated healthcare professionals and strengthening patient recourse’, spells out two key observations:
‘At the heart of a contract of insurance is a legally enforceable obligation to provide some form of benefit – usually in the form of a
monetary payment – upon the occurrence of a certain event, which may be subject to specified caps and exclusions.
‘In contrast, MDOs offering discretionary indemnity do so on the basis that their discretion is absolute, that any assistance offered is at their sole discretion and they therefore are not obliged to pay out in any circumstances.
‘Consequently, regulated healthcare professionals have less visibility, certainty and assurance as to what incidents may or may not be covered under discretionary indemnity.’
The newly named Independent Healthcare Providers Network welcomed the consultation, saying private hospitals had long wanted fully comprehensive insurance indemnity cover to replace ‘simply not tenable’ discretionary cover.
It said it looked forward to working with the department, MDOs
and the insurance industry to ensure private patients got the same legal and financial protection as NHS patients.
A spokesperson added: ‘There is a lot of detail to work out, including how any risk-pool might work and what the cost will be. But looking at other industries that have moved from discretion to comprehensive cover, costs have not increased as some feared they might, with it also allowing for a greater level of risk adjustment.’
The Independent Doctors Federation has long voiced concern about discrepancies in indemnity cover for private doctors. It said all stakeholders had to have confidence in public and private arrangements, which were for the safety of doctor and patient.
Doctors and others have until 28 February to respond.
See more reaction at www.independent-practitioner-today.co.uk

We begin a major new series aimed at reducing human error in healthcare in a bid to improve patient outcomes See page 18
Patients are being advised to shop for the best prices as self-pay hits record levels.
The market rose 9% to £1.1bn for independent hospitals and clinics in 2017, according to market analysts LaingBuisson’s Private Healthcare Self Pay Report, in association with GoPrivate.com.
It said: ‘For patients seeking

prompt access to private treatment, it pays to shop around. There are wide price variations for fixed-price surgery across the UK.’
The report found prices for a total knee replacement vary from £9,559 to £15,202, while cataract surgery for one eye costs from £1,650 to £3,353 (average £2,464).
Providers are more actively pro-
moting their services and all major operators now publish ‘fixed-price surgery’ prices on their websites.
New types of service, such as direct access to GPs, diagnostics and consultants, are an increasingly important part of the market.
Cosmetic surgery accounts for around 25% of self-pay revenue.
Report author Liz Heath said bet-

ter marketing and payment plans were reaping rewards. ‘While the NHS is still highly valued and much loved, it demonstrates that people will use information to make informed healthcare choices, especially for more affordable procedures, and mix and match by selectively self-paying or choosing to wait for NHS-funded care.’


their views really count are you listening to your patients’ feedback? With more private doctors being subject to reviews, jane braithwaite gives some excellent advice on handling negative comments P14
be ‘time smart’ in the way you work the most successful private doctors ‘work smart’ and have been able to steal back time so they can focus on patients and developing their practice. Kingsley Hollis suggests five areas for suitable treatment P16

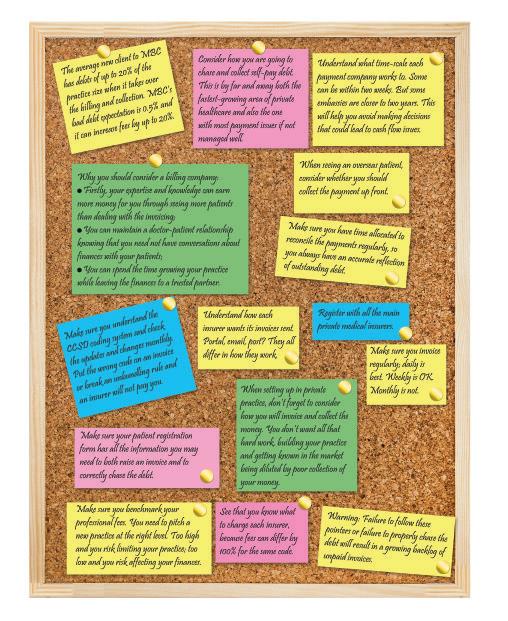
tips on getting the money in Heed these memos from Garry chapman to make your billing more efficient – and your bank account healthier P23
editorial comment
It is good to see independent practitioners enjoying positive results from private hospitals’ efforts to bring more fee transparency to patients.
Our front-page story shows operators are promoting their services much better than in the past and this has helped self-pay surgery and treatments flourish.
The market saw a 9% increase in self-pay in 2017 and analysts expect growth to continue. And that is not only where the alternative is a long and possibly painful wait; it is also for services that bring peace of mind, such as an earlier, more convenient GP appointment or diagnostic tests.
It is becoming much easier for patients to see prices for fixed-price surgery, as all the major providers now show these on their websites.
So if your hospital or clinic is lagging behind, then have a
word and do check just how easy it is for patients to find this information and understand it.
Sadly, as we reported six months ago, consultants are often missing out on the selfpay boom because their private hospitals have not geared up to make the most of it.
Complex websites and unclear pricing structures do not help, especially perhaps for many non-tech savvy older people –and be aware that market analysts LaingBuisson found the biggest growth in self-pay is among people over 60 who have greater disposable income.
There is much more price transparency to come this year when consultants’ fees are published by the Private Healthcare Information Network (PHIN). Achieving satisfying results with this for consultants and patients will be a much tougher task.
impress with an ‘a’ team competition among independent practitioners and private practices can be fierce, so making a good first impression with customers is vital. Stephanie Vaughan-jones discusses how you can do just that P24

chaperones’ vital role a chaperone should always be offered where any intimate examination is proposed, particularly if a patient has been sedated – says the mpS’s dr Gabrielle pendlebury P32

look after your entire family
What should you be asking your financial planner? Financial adviser dr benjamin Holdsworth shows what questions independent practitioners can ask to ensure they have the right help in place P38
Start a Private Practice: Self-assessment is getting trickier accountant ian tongue looks at the key considerations of the self-assessment scheme for income tax P44
doctor on the road: new breed with a famous pedigree motoring correspondent dr tony rimmer takes a new, premium, French brand for a spin P46
Profits focus: eyeing a healthy future our unique benchmarking series looks at the financial fortunes of ophthalmologists P48

tell US yoUr newS Editorial director Robin Stride at robin@ip-today.co.uk Phone: 07909 997340 @robinstride to advertiSe Contact advertising manager Margaret Floate at margifloate@btinternet.com Phone: 01483 824094
SUbScriPtion rateS £90 independent practitioners. £90 GPs and practice managers (private & NHS). £210 organisations. Save £15 paying by direct debit: individuals £75 (organisations £180). to SUbScribe – USe SUbScriPtion form on Page 28 or email: lisa@marketingcentre.co.uk Or phone 01752 312140 Or go to the ‘Subscribe’ page of our website www.independent-practitioner-today.co.uk chief sub-editor: Vincent Dawe Head of design: Jonathan Anstee Publisher: Gillian Nineham at gill@ip-today.co.uk Phone: 07767 353897
by edie bourne
Doctors are being urged to consider their position carefully in 2019 before following the rising number of medics opting out of the NHS Pension Scheme.
Financial experts blame the trend on harsh new tax rules which punish senior doctors for saving ‘too much’ in the pension scheme.
But specialist financial planners urged Independent Practitioner Today readers to proceed with caution.
Cavendish Medical technical director Patrick Convey said: ‘Doctors in the NHS who also run their own private practice may be caught by punitive new limits to their yearly and total pension contributions.
‘You will also undoubtedly have colleagues who are leaving the scheme and telling you to do the same. The truth is that it is not that simple.
‘Despite the challenges with the NHS scheme, there are too many advantages to ignore. The pension is Government-backed and indexlinked in retirement and also provides benefits for a surviving spouse.
‘It should also be remembered that if you opt out, you will lose other benefits such as death in service and may also face reduced ill-health retirement options.
250,000 workers chose to opt out of the nHS Pension Scheme between 2015-17, with 102,755 doing so in 2016 – up 78% on the previous year. new figures show those aged 46-55 represented the highest number of scheme leavers – up 94% in 2016.
the government introduced the ‘tapered annual allowance’ in 2016, drastically reducing the standard yearly pensions savings cap from the general £40,000 to as low as £10,000 for higher-earning doctors. excess savings above this rate are taxed at the marginal income tax rate. a significant cut to the lifetime allowance, which governs total pension savings overall, also hit doctors. from a 2011-12 peak of £1.8m, the limit is now £1.08m, but is due to rise in line with inflation.
compiled by Philip Housden
Regional PPU group hopes to be kernel for national forum
A self-help forum for private patient units (PPUs) aims to be part of a future national network to increase their influence.
Mandy Simpson, new chairman of the South West NHS Trusts regional group of private patient managers, said PPUs needed to work together.
She told Independent Practitioner Today: ‘We need to work collaboratively and to mobilise our collec-
‘In truth, opting out of the NHS scheme is a financially sound move for a limited number of individuals. Before making any decision to leave, you should look at detailed financial modelling which can pinpoint whether this is the best move for you and, if so, when would be the best time to leave,’ Mr Convey added.
tive resource to be at least competitive with the chains of private providers. We aim to be recognised as a positive force and to be heard centrally in the same way independent providers are.’
Ms Simpson, head of operations and quality for the Bournemouth Private Clinic at Royal Bournemouth and Christchurch Hospitals NHS Foundation Trust, said PPUs represented under 10% of insurers’ activity and, as such, were not considered important clients.
But, together, they could have a louder voice and explore ways to work jointly to share resource and maximise impact.
‘While you could face additional tax charges by staying in the scheme, if you leave, you will
She said PPUs wished to work with insurers to establish what they wanted for their members and to deliver this without compromise. But that was a tough message in NHS trusts that were pushed to the limits and looked to PPUs to help out with beds and staff when under real pressure.
NHS PPU managers needed support to keep fighting to ring-fence resources for private patients.
The forum is the only regional group meeting regularly and attracts support from a wide area.
Philip Housden is a director of Housden Group. Read his feature article on p46
Consultants of The London Orthopaedic Clinic (TLOC) have left Wimpole Street to join forces with nearby King Edward VII’s Hospital. TLOC has grown to include 15 hand-selected consultants covering six subspecialities since launching
ten years ago as one of the first independent, multidisciplinary, musculoskeletal clinics in the capital.
Consultant orthopaedic surgeon Mr Brian Cohen said the move presented exciting opportunities for 2019, enabling the group to
continue its clinical and organisational development.
King Edward VII’s boss Lindsey Condron said TLOC would reinforce the unit’s renowned orthopaedic service following unprecedented investment in facilities.
miss out on valuable pension and ancillary benefits, which can be much higher than the possible tax charges. Each individual will require specific advice. The decision to opt out is not one that should be taken lightly.’
Around 150 existing and wouldbe independent practitioners are expected at the BMA’s private practice conference at its London headquarters on Friday 5 April.
Topics include indemnity, the changing landscape of private practice, and Care Quality Commission registration.
The annual event is an opportunity for doctors to discuss issues affecting them in their day-to-day work.
The conference is targeted at all doctors – including GPs – who are engaged wholly or partly in private practice, as well as those looking to establish a private practice – including juniors. Register your interest at confunit@ bma.org.uk.
By Robin Stride
The voice of private hospitals in the UK finally has a name doctors and others can easily recognise.
Following a long-awaited rebranding exercise, it is now the Independent Healthcare Providers Network.
Things got confusing for independent practitioners and others after the previous private hospitals’ trade body and pressure group, the Association of Independent Healthcare Organisations (AIHO), was absorbed into the NHS Partners Network last Spring.
But the latter title with its NHS tag was continued and Independent Practitioner Today criticised this
last March when we suggested a new name was needed because many private consultants and GPs had never heard of it.
We wrote: ‘The NHS Partners Network? Really? Starting with the first word, it is an unlikely name for a private healthcare voice. How it will take over AIHO’s work and truly speak for this sector’s interests, we can’t wait to see.’
The renamed body said it had changed its name to ensure its brand identity fully reflected the wider remit in representing the entire independent health sector, including in Scotland and Wales. It will stay a member of the NHS Confederation.
Network boss David Hare said:
Private health insurers, and the intermediary companies who sell policies, have been urged to continue to campaign ‘vocally and vigorously’ to protect the industry from unaffordable prices.
The chairman of the Association of Medical Insurance Intermediaries (AMII) urged them to work to convince the Government to review how it treats health insurance and cash plans.
Stuart Scullion told the body’s Health and Wellbeing Summit that they should be treated in the fiscal system in line with other zero-rated insurance products such as life or critical illness.
‘We strongly believe spending on healthcare should be zerorated,’ he told the meeting.
Health insurance escaped a fur-
Independent healthcare Providers network (IhPn) – formerly the nhS Partners network – is the representative body for independent sector healthcare providers. Members deliver a diverse range of services to nhS and private patients, including acute care, primary care, community care, clinical home healthcare, diagnostics and dentistry.
Independent healthcare Providers network wales – formerly The welsh Independent hospitals Association – is a voluntary association of independent acute, mental health and learning disability hospitals in wales and is the welsh representation of the IhPn
It aims to represent the individual and collective interests of member healthcare organisations and to make ‘a positive contribution to the development and review of public policy regarding healthcare in wales’.
Independent healthcare Providers network Scotland – formerly the Scottish Independent hospitals Association – is a voluntary association of independent hospitals, both acute and mental health, and is recognised as the main point of contact for independent healthcare providers by regulators and the Scottish Government and is the Scottish representation of the IhPn
It has ten acute hospitals and eight mental health/addiction treatment centres in membership and has the same aims for its country as wales.
‘With people rightly becoming ever more demanding about the quality and timeliness of the care they receive, our new name puts us in an ideal position to build on our work in representing the sec-

tor and speaking up for its members, ensuring that the safety, quality and efficacy of the work delivered by independent healthcare organisations can be accessed by as many people as possible.’
ther damaging rise in October’s Budget after the Chancellor kept the insurance premium tax element at 12%.
This followed strong lobbying and research by Bupa and economics consultancy Cebr showing previous hikes in the tax had driven thousands of people to cancel or downgrade their health cover, costing the NHS £126m a year.
Mr Scullion reported that intermediaries regularly express frustration about the frequency with which scheme benefits change, and how difficult that makes it to keep up, while others complain about a lack of innovation.
But he felt there was innovation in the healthcare sector, with GP apps and improved clinical path-

ways for cancer, musculoskeletal and mental health being examples where there had been significant improvements over the last few years.
He said: ‘Other examples include increased focus on wellbeing, as well as initiatives which enable individuals to take responsibility for their own health and wellness.’
Albion Capital has invested £5m in a new centre in Harley Street dedicated to caring for and protecting all aspects of fertility and gynaecological health.
The Evewell is led by medical director Mr Colin Davis, a surgeon in laparoscopic and endoscopic treatments, and the team includes fertility and gynaecology consultants Dr Dimitri Psaroudakis and Dr Moses Batwala and Dr Christian Ottolini, laboratory director.
Albion’s head of healthcare Dr Andrew Elder said: ‘The Evewell is capitalising on an exciting opportunity to build a position as the leader in reproductive and gynaecological healthcare.’
By Olive Carterton
HCA’s The Wellington Hospital is the first London centre to install the Icon Gamma Knife and offer fractionated treatments via mask immobilisation to treat private and NHS patients.
The machine, seen as the most innovative and accurate brain and skull radiation therapy, treats patients with brain tumours, vascular and functional disorders.
HCA said the technology will provide more tailored and accurate treatment plans, meaning patients did not have to stay overnight, and shorter recovery times.

Patients can opt to use a custom face mask, as opposed to the traditional headframe used with previous Gamma Knife systems, which can cause discomfort.
Mr Ian Sabin, consultant neurosurgeon and medical director of The London Gamma Knife Centre said: ‘This new technology means
The London Clinic has announced it is the first UK private hospital to offer an innovative surgical service to above-the-knee amputees to improve limb function and reduce pain and skin-related complications.
Military veterans who have suffered serious injury are likely to be suitable candidates for surgery in London, when previously they have had to travel to Australia or the US for treatment.
Orthopaedic surgeon Mr Paul
Culpan, leading the service, said:
‘There’s robust clinical evidence that osseointegration, a pioneering operation for patients with amputations that removes the need for a socket prosthesis, significantly improves quality of life and long-term health.
The service also includes bespoke hip and knee replacement surgery using tailor made implants to fit the patient and complex trauma (fractures) and plastic reconstructive surgery.
Many patients are unaware of more minimally invasive techniques for hip replacements and so opt for standard surgery which can lead to longer recovery times, according to a consultant trauma and orthopaedic surgeon.
Mr Simon Mellor, who offers anterior hip replacement at Highgate Private Hospital, urged patients to shop around, as surgery options were more varied than ever.

we can offer patients the most accurate and precise radiosurgery completely tailored to them and their condition. Treatment times will be quicker, which means I will be able to treat more people within a day, and patients will be able to go back to their daily activities almost immediately after.’
The Wellington Hospital chief executive John Reay said: ‘We provide our consultants and clinicians with the most cutting-edge technology and equipment to provide patients with the very best care, and the acquisition of the Gamma Knife Icon furthers this promise and offering.’
Venous surgeon Prof Mark Whiteley, of the Whiteley Clinic, has launched a new book to ‘revolutionise’ leg ulcer care.
He says many patients and health professionals are unaware most venous leg ulcers can now be cured permanently or significantly improved using local anaesthetic endovenous surgery, provided the patient is able to walk. In venous centres, this is a ‘walk in, walk out’ procedure.
But most patients in the UK are not offered endovenous surgery, instead undergoing constant dressings and compression bandaging.
The cost of dressing and compressing a leg ulcer for one year is approximately the same as curing it with endovenous surgery.
Leg Ulcer Treatment Revolution is £6.99 from www.amazon.co.uk/ gp/product/1908586052
Specialist medical accountant Ray Stanbridge, of Stanbridge Associates, has joined the board of The Healthcare Property Group (HPG) to support a new focus on the development of private sector healthcare facilities.
The Healthcare Property Company, its main trading entity, has mostly worked with the NHS to developing a range of primary care facilities. It has also developed polyclinics in Germany.
Its move to working with the private sector was established four years ago when it partnered with IVF pioneer, Bourn Hall.
Highgate Private Hospital’s endoscopy department has been awarded JAG accreditation, the specialty’s gold standard of regulation and safety.
Lead consultant gastroenterologist Dr Deepak Suri paid tribute to the department for working hard over the last year to achieve the accolade.
Christine Etherington, clinical services and quality governance director, said: ‘For a new unit to receive this stamp of approval on first submission is quite simply amazing.’
Billing firm Medical Management Services Ltd, of Hemel Hempstead, has ceased trading, blaming EU General Data Protection legislation requiring it ‘to make very significant and costly operational changes’.
It said it would be unable to stay competitive on price for its customers while being a viable business.
The GMC full registration fee is going up from £390 to £399 on 1 April.
By a staff reporter
Breast surgeons must ensure women are aware of BIA-ALCL, a non-Hodgkin’s lymphoma associated with implants.
The warning was given to surgeons attending the London Breast Meeting, where they were told they must take more responsibility to diagnose and report cases.
Hundreds of breast specialists from around the world met at the Royal College of Physicians for the four-day conference, which heard that women receiving breast implants were not always being told of the risk of developing a cancer called Breast Implant Associated-Anaplastic Large Cell Lymphoma, or BIA-ALCL.
Consultant plastic surgeon Mr Nigel Mercer, who chairs the Plastic, Reconstructive and Aesthetic Surgery Expert Advisory
Group (PRASEAG) for the UK’s Medicines and Healthcare products Regulatory Agency’s (MHRA) committee looking at BIA-ALCL, said: ‘I know for certain, because I have seen patients who have not been warned there is a risk of BIAALCL by the clinic or surgeon they have seen.’
The conference urged surgeons to take the condition seriously. Mr Mercer, a past-president of the British Association of Plastic Reconstructive and Aesthetic Surgeons (BAPRAS), said all patients needed to be told from the outset about the risk and that for women who had already suffered from breast cancer, the implications of facing new cancer risk could be particularly devastating.
He said: ‘If you see a woman who has been one of the one in eight women unlucky enough to develop breast cancer and who is seeking an implant-based recon-
struction and then you say that type of reconstruction carries a 1 in 28,000 risk of developing another form of cancer that will need another form of cancer treatment – for that patient who has already undergone cancer treatment, that is pretty devastating news.’
The MHRA issued a joint statement with several of the UK’s leading surgeons’ associations last July, advising it was ‘essential’ that all patients considering a breast implant for reconstructive or cosmetic purposes are made fully aware of the potential risks by their surgeon.
Prof Jian Farhadi, co-chairman of the London Breast Meeting and former director of the Department of Plastic and Reconstructive Surgery at Guy’s and St. Thomas’ Hospital in London, said: ‘However small the risk may be, women must be made aware that

Mr Niger Mercer chairs the expert advisory group looking at the risk associated with breast implants
they could develop cancer associated with breast implants, and potentially even die.
‘Surgeons must do this before their patients agree to undergo procedures, although, in many cases, this does not appear to be happening.
‘Debate at the London Breast Meeting has highlighted the importance of greater investment in education, so that we can do more to identify cases of BIAALCL, better equip pathologists to support this mission, and better understand the state of the disease across the UK and the rest of the world.’
A leading light in the provision of private cancer services has called for a radical overhaul of the way the disease is diagnosed in Britain.
Prof Karol Sikora warned that the current system of incorporating diagnostic services within hospitals was simply not working and patients were facing drastic delays in getting crucial imaging and biopsies.
Prof Sikora, chief medical director of cancer services provider Proton Partners Inter national, said: ‘What we urgently need is for patients with certain symptoms to go straight to a non-hospital clinical environment where all relevant tests can be done at once and then referred to an appropriate specialist if necessary.
‘That would be a real gamechanger in cancer diagnostics in
the UK and more lives will be saved.’
He was commenting after a new Health Foundation report found that 10,000 deaths could be prevented each year with better diagnosis.
According to the report, at the heart of the problem is the ‘tight gate-keeping’ of the NHS: only GPs can refer patients for checkups and are pressured not to refer too many, while the NHS does not have enough equipment or staff to carry out the checks that it should.
Steve Powell, chief diagnostic officer at Proton subsidiary Rutherford Diagnostics, said: ‘At present, patients are having to wait at least six weeks for their diagnosis; that is not acceptable. We should be aiming to reduce those weeks of waiting to days and
ultimately be able to provide a 24-hour service.’
He said adding diagnostic equipment to hospitals would not solve the problem. They would simply be engulfed by the demand and patients would face the same structural obstacles of ‘tight gatekeeping’ highlighted by the report.
Added Mr Powell: ‘Patients with the relevant symptoms should be able to get all their tests in a pleasant specialised diagnostic environment, and then forwarded to the relevant specialist if diagnosed with cancer.
‘GPs need to be empowered to use CT, MRI and endoscopy services without having to make endless referrals. This will not only lead to quicker diagnoses but will prove hugely cost-efficient too.’

‘LifeBox’ introduces the safety bar much higher, which means patient risk will be reduced and that will lead to increased quality of care and better outcomes

By Leslie Berry
A team of Brighton-based consultants and technology specialists are saving time and money after creating ‘the first interactive digital patient assessment app’.
Instead of filling in pre-assessment forms with a nurse, patients who need a medical procedure or operation can now answer questions about their health via a hand-held computer in the comfort of their own home.
Called ‘LifeBox’, the assessment tool has been in development for the past two years and was launched at The Montefiore Hospital in Hove, Sussex. It is hoped that its success will help it be adopted nationally by NHS trusts. The answers they give will generate more patient-specific questions to fully identify their level of risk. All patients are then called by a nurse to discuss the findings.
Those with low or no risk may not need to come back into hospital for further tests before they
have their medical procedure. The app will also generate information and videos specific to the patient’s condition, so they can prepare for the procedure.
Mr Sandeep Chauhan, consultant orthopaedic surgeon at The Montefiore and lead consultant for LifeBox, said: ‘When a consultant has just told you that you need a medical procedure, your head is not often in the best place to be answering questions or taking on board information about your condition and the forthcoming operation.
‘With LifeBox, you can answer questions in your own home, when you feel calmer. You will have easier access to paperwork, medication or the help of family members to ensure questions are answered correctly.
‘Patients can elaborate on their health with guided questions to enable the medical teams to better assess risk. For instance, we may have several patients with angina coming in for a similar procedure
place, in one digital box, and stays with them for life. They can take the app with them wherever they go – on their phone, tablet or computer – which can be very useful if they fall ill away from home or on holiday, or in a situation where they need to give details of their medical condition and health history but are too stressed or anxious to do so.’
LifeBox is not just about preassessment and health history. It also allows the patient to do a post-op questionnaire, so they can compare how they felt before and after the procedure. And they can give satisfaction feedback. The app will direct any complaints straight to the hospital manager.
The LifeBox team predicts that soon every patient in every GP surgery will have access to the technology and be able to update their own health records as they go.
Hospitals will be able to use LifeBox to send group messages with information to people with similar conditions and, as well as physical health, LifeBox users will be able to upload details about their lifestyle and mental well-being.
Eventually there will be a communication portal, so a patient can have a video call with a nurse at a time that suits them.
but the answers they each give will be specific to them and means we can grade their angina and therefore assess individual risk.’
By reducing paperwork and unnecessary testing, LifeBox is expected to save around £215,000 per 5,000 patients.
And there are also significant time savings. On average, a patient spends around 3.2 hours coming back into The Montefiore for a pre-op assessment and tests, including travel time.
If they are fit and well and do not need those tests, they will not need to come into the hospital before their operation or need to take time off work or find childcare.
Each patient is given their own unique LifeBox login and they can decide who the information can be shared with. As their health changes in the future, their individual LifeBox can be updated.
JP Hamilton Savory, a member of the LifeBox technical team, said: ‘It is their health story in one
Mr Chauhan called LifeBox ‘a supplement’, not a replacement, for human intervention.
‘You could have a traditional pre-assessment with a junior nurse or one who has been on a long shift. They may not dig deep enough into the answers that you give about your health, which means something could be overlooked.
‘LifeBox overrides human error. It introduces the safety bar much higher, which means patient risk will be reduced and that will lead to increased quality of care and better outcomes.’
LifeBox was tested on patients on wards at The Montefiore and more than 100 patients are using the app. From now, every new surgical patient at the hospital will be signed up.
The hospital has also invested in five iPads for its reception area so a patient can be guided through the LifeBox programme by a nurse if they prefer.
Info: allan@lifeboxhealth.com


More than 1,000 people attended healthcare market analysts LaingBuisson’s annual awards ceremony to celebrate the best in health and social care.
Held in the ballroom at the Park Plaza Westminster Bridge, London, the event was hosted by actor, singer and writer Alexander Armstrong, who entertained guests before presenting the awards with LaingBuisson’s chairman Stephen Dorrell.
Finalists were chosen by an independent panel of judges from over 350 nominations.
LaingBuisson chief executive Henry Elphick said: ‘The LaingBuisson Awards offer providers and advisers the opportunity to recognise and celebrate the most inspiring and innovative work across healthcare and social care in the independent sector.
‘The nominations were hugely impressive and included many deserving projects, organisations and professionals who are dedicated to tremendous health and care causes, and I know that the judges’ decisions were not easy ones.’
The Nuffield Health team (left) walked away with the award for best private hospital group, while Royal Marsden Private Care (below) picked up two awards in the Clinical Services category: the Health Outcome accolade and the Nursing Practice prize




a look back through our journal’s archives of ten years ago reveals that although times change, some issues are not so
The recession was rife this time ten years ago and independent practitioners were warned they could not expect their earnings to escape the economic downturn


Ambitious plans to attract a new generation of consultants to stateoftheart rooms in Harley Street were unveiled by the area’s property company owners.
Bosses at Howard de Walden Estates said they wanted to see ‘independent consulting houses’ providing quality services and medical equipment for 30 to 50 doctors.
Private consultants were being urged to ensure tough data security for their mobile devices following concerns that thousands of patients’ records had been put at risk.
More than a third of health professionals in a survey failed to properly secure patient records, images, contact details and other sensitive data on laptops, handheld units and USB sticks.
The transatlantic study, which included UK independent specialists, sparked criticism of NHS standards rather than private sector failings. But private doctors were being advised to be alert.
Researchers in the survey found 35% of health practitioners here were using just a password to secure work laptops and devices.
A quarter of the doctors polled were anxious about patient details being held on mobile devices.
Chief executive Toby Shannon said: ‘The difficulty is we are in a conservation area, so we have to work in that framework. But we aim to get two to three buildings in a row and do a lateral conversion.
‘Doctors are asking for more independent consulting rooms. We are trying to fill a gap in the portfolio. It’s going to provide more variety. We want the area to be the place where medical practitioners want to come to practise.’
Property director Simon Baynham said the company had previously prioritised the space needs of the area’s ‘key stores’ private hospitals. But now it wanted independent buildings with no hospital affiliation.
£3.5k tax hike faced
The average consultant with an £85,000 NHS salary, £65,000 private practice income, a non
working spouse, and two children was set to be £442 better off in terms of gross income and benefit in 200910 than in 200809.
But from 201011, under Labour’s new National Insurance rates, a 45% income tax rate on earnings over £145,000 and cut in personal allowances for the higher paid, he or she would be £3,626 worse off.
Accountants said Chancellor Alistair Darling’s plans represented a 2.4% fall in gross income benefit.
Private health insurers were coming under renewed pressure to improve coding system clarity.
Insurance fraud investigators said they were committed to getting companies to act, something Independent Practitioner Today had called for two months previously.
The move followed further criticism from a surgeon at the first gathering of the Health Insurance Counter Fraud Group.
Patients who wanted to complain about their private or NHS doctor were now able to get support from a new online information centre from the GMC, called Patients’ Help.
It claimed to be the first website to help patients navigate the complaints system. The site was
SubScribe today don’t miss out on what we report and advise in the future. Sign up for a £75 subscription today –consultants, GPs and practice managers can save £15 with a direct debit.
See page 28
set up to provide case studies, a timeline for the life of a GMC complaint, and an interactive map with contact details for local help and advice centres.
A special report from communications specialist Neil Huband lifted the lid on the press’s tricks and showed what doctors could do when faced with a media circus wanting to know about the famous patient they were treating. He advised anonymous cars and ambulances should be used to take the patient to hospital – not the Bentley that everyone knows.
‘Choose an admission time when there are less likely to be a lot of people around. Patients are gossips and will often be the source of tipoffs about other patients.
‘There are plenty of things a good hospital can help you with. If your patient is very well known, discuss privacy and security with it at the outset.
‘Choose a “new” name for the admission – not an obvious one –and arrange that the hospital has a specific list of visitors and callers with a code name each caller must use to be identified as genuine.
‘And tell them not to accept flowers at reception. When trying to find out where a famous singer was having her baby, as a reporter for the Sunday tabloids, I used to send flowers to several hospitals and the one that accepted them was…well…more than likely to be the one.’


If there is something you are unsure about regarding your business accounting, never be afraid to ask your accountant. In this month’s column,
Susan Hutter (right) answers more of the most frequent questions she receives from doctors
Qi am going to be filing my tax return – could you advise me what the taxman will accept as legitimate expenses against my practice income?
ARemember you can only claim expenses that are wholly and exclusively for the purpose of the trade.
Typical expenses that can be claimed are:
➲ Motor/travelling expenses –except from your home to your place of work. If you have more than one clinic/surgery, travelling between them would be allowable, as would travelling for workrelated meetings, work-related training and conferences.
For motor expenses, for the first 10,000 ‘business miles’ a year, you can claim 45p per mile. However, you will need to keep a record in case you are challenged by HM Revenue and Customs (HMRC). For rail and air fares, it is advisable to keep the receipt.
➲ Subscriptions to professional bodies, such as the BMA, and also subscriptions to any medical journals such as Independent Practitioner Today
➲ Internet charges where you use your computer for work –nowadays that is nearly every -
body! Also computer-related expenses such as hardware and software updates for business purposes can be claimed along with any professional courses and training including continuous professional development.
➲ If you travel for work-related conferences , the accommodation, subsistence and air fares can be claimed.
But if your stay is extended for a holiday, the ‘holiday part’ should be disallowed and so you should apportion the expenses accordingly.
➲ Accountancy fees for preparation of your practice accounts, although not your personal tax return.
➲ Professional indemnity insurance
➲ Use of home as office – this is an expense that is often challenged by HMRC and therefore it is important that you calculate it correctly.
For many, it is not worth the trouble. But if you do carry out a lot of work from home, such as report-writing and, say, have a

dedicated office that you use for no other purpose, the best way of claiming is to work out the square footage of the office compared to the total space of the dwelling and apportion certain household bills accordingly, such as electricity and gas.
The above is not an exhaustive list and there are grey areas. So if you have specific expenses you are unsure about, be sure to check with your accountant.
QA family member has asked me to invest £25,000 in their new business. in return, i will receive 25% of the share capital. Are there any tax advantages?
AIf the business is a start-up and you are among the first investors, then as long as you and connected parties hold less than 30% of the share capital, you may be able to benefit from the Seed Enterprise Invest ment Scheme (SEIS).
This is available to initial investors in a start-up, as long as the company meets the requirements for a qualifying trading business. The maximum that a company can raise under SEIS is £100,000 in total (not per person).
Also, the company must have been trading for less than two years. As long as everything stacks up, then you as the investor will get 50% tax relief on the amount invested.
Provided you hold the investment for three years and then sell the investment, there is no capital gains tax if you make a gain.
If the company fails, then you as the investor will have made a loss of £12,500 (50% of £25,000). You are eligible for Share Loss Relief against income tax for the £12,500.
This means that if you are a 45% tax-payer, you would have received total tax relief of 78% on the £25,000.
By the nature of the investment – a start-up – it is considered a high-risk investment. However, given all the relief and tax benefits, it is a more manageable risk due to the tax relief.
If SEIS isn’t available because the firm has already exceeded the limit and/or is out of the timeframe, investors could qualify for the Enterprise Investment Scheme (EIS) instead. Under EIS, they get 30% income tax relief on the amount invested.
Qi have heard that HMRc is making far more tax investigations. What is the likelihood i could be investigated and what is the process if i am?
AHMRC regularly conducts tax investigations, but, in my opinion, it is not the case that it is necessarily making more or indeed targeting a specific industry or profession.
You should definitely protect yourself by making sure that you do not bring yourself to the HMRC’s attention for the wrong reasons.
Therefore, ensure your tax returns and accounts are always filed on time and your tax payments are made on time.
If there are certain figures in your tax return that look very unusual compared to previous years, there is a box in the tax return for ‘notes’ which you should use to explain to HMRC why the differences arose.
If HMRC is satisfied with the notes, then it may not raise an inquiry.
If you do get an inquiry, it is advisable to enlist the services of your accountant to assist with the replies.
Be completely open and honest and reply within the time limit requested by HMRC. If the time limit is too tight, then contact HMRC and ask for an extension.
As long as you do this on a timely basis, it is normally very accommodating.
Ask your accountant about professional fee protection insurance. Generally, this costs no more than £500 a year and will cover your practice accounts and your personal tax return in most cases.
If you take out this insurance, the accountancy fees charged in dealing with the enquiry will be paid by the insurance company. This is a wise move, as accountancy fees for this type of work can be quite expensive.
Qi don’t have enough money to pay my tax bill, what is your advice?
AThere is no point in sugarcoating this. HMRC expects all taxpayers to put aside money from their earnings to pay their tax.
If you have not, you will need to have a good reason.
Either way, the best way of dealing with this is to call HMRC yourself and explain the situation.
Before you make the call, speak to your accountant about your particular circumstances so that he or she can advise you on the best way to tackle HMRC.
However, in recent years, HMRC has tended to do better deals with taxpayers directly than if they ask their accountants to intervene. The deal will not be a reduction in tax. But you may be given time to pay.
The time period will need to be negotiated. Be aware that HMRC will ask what private funds you have available and whether you can take out a loan.
Susan Hutter is a partner at Blick Rothenberg and part of the team that advises medical practitioners

more private doctors being subject to reviews, Jane Braithwaite gives some excellent tips and advice on handling negative comments
Most practices will be receiving patient feedback on a regular basis.
this can range from the quiet chat with the receptionist or medical secretary, to the hand-delivered box of chocolates or the – hopefully infrequent – irate phone call or email.
But how are you collecting these reviews, measuring your patients’ satisfaction and dealing with complaints?
Measuring patient satisfaction and assessing areas for improvement is an important aspect of the care Quality commission assessment process, but it should also give you the opportunity to
involve all your team members in taking responsibility for improving the patients’ experience.
Feedback sources
p articularly popular forums for online patient feedback can be your practice’s Facebook page or Google My Business account.
positive reviews here can boost search results, they are easy to request and receive and they give potential patients good insights into your services.
Great reviews can be shared on your website or in articles, but you must ask for the patient’s express permission first.
on these public channels, there

measuring patient satisfaction is an important aspect of the care Quality commission assessment process
1 establish an open team culture encouraging all feedback to be shared
2 encourage patients to share their reviews on your Facebook page, google and other social media accounts
3 send patients links to relevant medical websites where reviews are encouraged
4 share great reviews on your website (having asked the patient’s permission)
5 set up a monthly or quarterly programme of feedback requests from patients
6 decide on the best way to collect ad hoc patient feedback from team members
7 put in place a detailed complaints process
8 communicate your complaints process openly with your patients
9 respond to complaints and online negative reviews promptly and professionally
10 collate all your feedback regularly from all sources, to inform your improvement plan

is the danger that a negative review can be widely seen but, if this complaint is handled promptly and professionally, it can often result in a positive outcome.
Many of our clients at Designated Medical request patient reviews on specific medical sector websites such as Doctify, where feedback can be anonymous and complaints can be addressed.
p atients are sent a link to the website’s reviews page, or an ipad app is used to collect reviews at the practice. similar review options are available on iwantgreatcare.org and My Health specialist.
clinics and doctors may choose to set up and implement their own in-house patient satisfaction survey, perhaps on a monthly or quarterly basis.
Websites such as smart survey or typeform offer various options for customising questions and compiling responses. the results can be summarised into a report giving a focus for practice improvements. t hese could be reviewed at the monthly practice meeting and an action plan agreed to address any issues. t he ad hoc face-to-face or emailed feedback should also be consolidated to form the basis of your improvement plan, which can be used as evidence of listening to patients and demonstrates a strong focus on patient satisfaction. it’s important that an open and
understanding culture be fostered within the team, with no fear of blame being apportioned, so that all feedback is actively shared and acted upon.
positive reviews should be celebrated as a team, too.
➤ all clinics should have in place a complaints process that is openly communicated to patients and closely followed by the team
➤ that process should clearly define who will have the responsibility for managing the complaint
➤ complaints should be dealt with in a timely manner and it is important that the patient be made fully aware of the process details and given time-scales for responses to be provided
➤ good communication at every stage is vital. the gmc’s advice on complaints handling is clear: ‘You must respond promptly, fully and honestly to complaints and apologise when appropriate’
➤ when handling online negative reviews, your aim is to address the issues raised in the complaint, without going into personal details, and offer to contact the patient directly to help resolve the problem

Jane Braithwaite (below) is managing director of Designated Medical, which offers business services for private consultants, including medical secretary support, book-keeping and digital marketing

➤ You will also want to make sure that the way you publicly answer the complaint is seen as professional and helpful to anyone reading the review in the future
➤ if a complaint is handled well, the patient may refrain from sharing any negativity with other potential patients and, in the best-case scenario, it may actually generate increased loyalty
➤ in the case of serious medical complaints, these should, of course, be escalated to the appropriate professional body

The most successful independent practitioners ‘work smart’ and have been able to steal back time so they can focus more on patients and developing their practice. Kingsley Hollis suggests five areas for suitable treatment
Time is a precious resource in medicine and most doctors quickly become adept at managing their clinical workload and prioritising tasks according to patient need.
Understandably, doctors see starting their own practice as an opportunity to spend longer with their patients, so it can be a shock
to discover how much time is taken up by day-to-day administrative and business tasks.
Time-consuming tasks
On top of managing the caseload generated by each patient, independent practitioners need to oversee their appointments diary, be their own marketing, human
resources and iT director, and stay on top of their finances.
in my experience, every practice has time-consuming tasks that could be managed more effectively, often by making better use of technology.
Here are five of the most common administrative ‘bottlenecks’ to address:
m edical secretaries tell me they can spend up to 75% of their time typing, printing and dispatching letters to keep patients and their GPs informed about appointments, investigations and treatments.
While a letter is often their preferred form of communication, the process can be streamlined by using letter templates for common subjects which can be completed with the relevant patient details.
i would also recommend using software which allows you to select and batch-print multiple documents at a time, rather than laboriously opening each one and clicking on print.
Check whether your practice management system allows you to do this.
Practices regularly have to call around hospitals or insurance companies to confirm a patient’s insurance details, but this can be a time-consuming – and sometimes frustrating – exercise.
in response, Healthcode developed the online membership inquiry feature within ePractice which enables users to instantly check patients’ insurance policy numbers and address details against the insurers’ database.
Healthcode estimates that automating the invoice process can save £2.15 per invoice by eliminating printing, postage and manpower costs.
Creating and submitting bills to private medical insurers online takes a fraction of the time, improves accuracy and ensures the invoice is validated against the relevant insurer rules so it is ready for processing and payment. Plus, you have the reassurance of knowing that the invoice has been received by the insurer. All practices can reap the business benefits of e-billing, whether they use Healthcode’s own ePractice solution or through our validation and clearing system, which is compatible with most practice management software.
When payments arrive, every practice needs a system in place to record exactly what invoices are being paid and identify shortfalls, which then need to be queried with the insurer or charged to the patient.
This can be time-consuming with a manual system and, in some cases, practices have been obliged to write off outstanding debts because payments have not been reconciled against the correct invoice.
Before investing in practice management or invoicing software, check how easy it is to manage payments and shortfalls, as this feature could make all the difference to your credit control process.
Without access to accurate information, it is impossible to steer your business effectively. However, manual book-keeping and accounting systems require expertise and time to prepare even basic reports such as an aged debtor analysis, so an automated system is a must.
Before investing in a practice management system, check that it provides a range of real-time financial reports so you can measure your performance, analyse your strengths and weaknesses and make informed decisions.
Few doctors have experience of running a business. However, the most successful independent practitioners i know are those who draw on the time management skills they learned early in their professional career.
By identifying ways to work smarter and making the most of the latest practice management technology, they have been able to ‘steal back’ time to focus on patients and on developing their practice.
next month: common practice management errors and how to avoid them
Kingsley Hollis (right) is head of business development (ePractice) at Healthcode











HMRC tax investigations and disputes create difficult and stressful times.
As an award winning firm of tax experts, our highly experienced partners specialise in resolving problems relating to tax investigations and disputes with HMRC.
To find out, in confidence, how we can help call 0800 734 3333.
‘Here to help. Not to judge.’

Our trio of writers – two doctors and an airline pilot – are co-founders of a business on a mission to improve patient outcomes by helping healthcare professionals understand why errors occur.
John Reynard, Tim Kane and Peter Stevenson’s major new series for Independent Practitioner Today gives a startling insight into attitudes and aims to inspire you with a wealth of practical patient safety solutions

Human beings are prone to a number of potentially disastrous failings when working in an environment where error can cause harm.
We forget things, we misunderstand each other and we sometimes fail to hear people speaking.
and we fail to notice important but unexpected developments happening right in front of our eyes. so it seems that any system containing a human element must eventually fail – and in ‘high-hazard’ environments, these failures can be catastrophic.
While errors will probably never be entirely eliminated where the ‘system’ relies on humans, it is noteworthy that in the last three decades there has been an impressive reduction in the number of fatal accidents occurring in a number of different ‘safetycritical’ industries: notably airlines, railways and chemical and petrochemical processing. organisations have sometimes actually managed to achieve the goal of ‘zero fatal accidents’ and sustain that achievement for many consecutive years.
some – but only some – of this improvement in safety has undoubtedly resulted from the use of more reliable hardware; for example, better designed aircraft and computer systems.
psychologists who studied how this safety improvement was achieved have shown that organisations that have also managed to change certain behaviours of their staff have reduced accidents to very low levels. these organisations have come to be known as highly reliable – High reliability organisations (Hros).
Hros provide their staff with ‘human factors’ training in the psychology of error and in simple techniques to mitigate or prevent mistakes.
problems with human memory can, for example, be largely mitigated through the use of check-lists and the practice of repeating back messages to their sender. other human failings can also be effectively managed through the use of other simple strategies.
Hros have come to realise that focusing on safety training not only enhances an organisation’s reputation, but also makes the organisation more efficient.
a major factor in this has been the improvement in the reliability of verbal communication between staff. not only does better communication enhance safety but it minimises confusion, wasted effort and delays.
these improvements in efficiency have resulted in the rise of the ‘low cost’ airlines in the last two decades, without compromising safety. budget airlines are therefore just as safe as the ‘high-end’ airlines and they are every bit as highly reliable.
in this series of articles for independent practitioner today, we discuss:
the scale and effects of healthcare error;
the High reliability organisation approach to error reduction and the development of a safety culture;
communication failure and simple tools to reduce communication errors in your practice;
crisis management and mismanagement.
Yes, there are great differences in the day-to-day operations of healthcare when compared to aviation and the railways, for example.
but much can be learnt about and much can be done to reduce error in healthcare by focusing on the psychology of human error in a way that Hros have done.
‘The medical profession has become a major threat to health’
Ivan Illich, Limits of Medicine
The landmark h arvard m edical Practice Study ( hm PS) quantified the scale of an age-old observation – that patients are harmed by their doctors and nurses [Brennan 1991, l eape 1991].
It was published in the New England Medical Journal in 1991 using data from 30,121 randomly selected records from 51 randomly selected acute care, nonpsychiatric hospitals in new York State, US.
The proportion of hospital admissions experiencing an adverse event, defined as injuries caused by medical management, was 3.7%. The percentage of these adverse events which were due to negligence was estimated to be 27.6%.
While most adverse events caused only minor harm – with complete recovery in one month – 13.7 % led to disabilities that lasted up to six months, 2.6 % caused permanent total disability and 13.6% caused death.
Of note is that the hm PS was originally conceived to determine the number of injuries that could lead to litigation and require compensation.
It was not conceived simply to quantify the scale or error, but rather it was driven by concerns over the cost of litigation and so was motivated and funded by the medical malpractice insurance industry.
a lmost as a by-product, but what became its legacy, was that it revealed a major issue with the scale of preventable harm.
Of course, there was nothing new in all of that; every doctor and nurse is aware of the concept of iatrogenic disease – doctor generated harm.
as far back as 1857, Semmelweis had observed that women delivered of their babies by medical students who had failed to wash their hands after dissecting cadavers had a substantial risk of death from streptococcal infection. Simple handwashing dramatically reduced the risk of such infection [Semmelweis 1860].

The study indicated that at least 44,000 and perhaps as many as 98,000 Americans die in hospital each year as a result of medical errors
So, there was nothing really new in the hmPS other than that it established the scale of an ageold phenomenon. nor was there anything new in the scepticism that greeted the authors of the hmPS.
a s a retort to Semmelweis, meigs stated: ‘doctors are gentlemen and a gentleman’s hands are clean’. Semmelweis was ridiculed by a medical community unable to accept the idea that they might be a cause of patient harm and he ended his days in an asylum. a nd that scepticism arose because the scale of the problem identified in the hm PS was almost too great to be believable.
Critics argued that those individuals who died at the hands of their doctors and nurses were sick anyway and that their primary pathology was likely to have been the cause of death rather than a ‘medical’ error – you only come into hospital if you are sick, after all.
That belied the truth. d eaths followed routine and elective surgery in fit individuals – ‘Betsy lehman, died from an overdose during chemotherapy. Willie king had the wrong leg amputated. Ben k olb was eight years old when he died during “minor” surgery due to a drug mix-up’. It was the errors that killed them [kohn 1999].
Uncomfortable reading a ll of this could have made uncomfortable reading for the medical and nursing professions, but it seemed to have little initial impact [leape 2000].
It was only with the publication in late 1999 of the Institute of
This report acknowledged that adverse events occur in around 10% of hospital admissions and that the cost in picking up the pieces was an estimated £2bn in extra bed days
m edicine (IO m ) report, To Err is Human , that the penny finally dropped – at least in the US Congress, which now cast the spotlight on quality and safety in healthcare – that we might have a really big problem on our hands. This report estimated the numbers of americans who die in hospitals as a result of potentially preventable adverse events based on extrapolations from the hmPS and the more recent UtahColorado study [Gawande 1999]. This was the bottom line: when extrapolated to the 34m admissions to US hospitals in 1997, the results of the hmPS and the UtahColorado study indicated that at least 44,000 and perhaps as many as 98,000 americans die in hospital each year as a result of medical errors.
d eaths due to preventable adverse events exceeded deaths attributable to motor vehicle accidents (43,458), breast cancer (42,297) or a I d S (16,516) [C d C 1999].
nonetheless, in a survey of doctors in the US published after the 1999 Institute of medicine report, only 13.8% of doctors agreed with the statement ‘a recent estimate that medical errors kill 44,000 to 98,000 americans yearly is accurate’ and 79% of doctors thought healthcare matched the safety records of other organisations [robinson 2002].
little insight
This latter finding is all the more interesting when one considers that since the kegworth air crash in leicestershire in 1989, almost 30 years ago, not a single death has occurred on a Uk airliner, at
the time of writing. d o doctors really think that healthcare even approaches the safety record of the aviation industry? have they so little insight?
That such a state of affairs could exist in a country as sophisticated and wealthy as the US galvanised other countries into investigating their own scale of medical errorinduced harm.
The result was that studies in a ustralia [Wilson 1995], n ew Zealand [ d avis 2001], France [michel 2004], denmark [Schioler 2001], the Uk [Vincent 2001] and Canada [Baker 2004], using the well-established methodology of the hmPS, demonstrated a stark set of statistics. n amely that roughly 10% of hospital admissions world-wide are associated with an adverse event that causes harm, and 5% of that 10% of harms (0.5% of all hospital admissions) led to death.
It has been estimated that half of these errors could have been prevented with, among other things, although not exclusively:
Better clinician-to-clinician communications;
Better standards of checking;
Better standard procedures.
These studies not only established the scale of the problem in a variety of different countries, they also indicated that the problem was even more prevalent than had been thought from the hmPS.
Furthermore, they also emphasised that error leading to harm in healthcare was a global phenomenon occurring irrespective of the way in which healthcare was funded – private or public, state or insurance.
From the Uk’s perspective, it has been estimated [Vincent 2001] that each year about 40,000 patients die following a potentially preventable adverse event. Vincent’s study followed within a year of the department of health report An Organisation with a Memory, published by e ngland’s Chief m edical Officer Sir l iam donaldson [2000].
This latter report acknowledged that adverse events occur in around 10% of hospital admissions and that the cost in picking up the pieces was an estimated £2bn in extra bed days. This, at a time of austerity. how can we be so profligate? Can we not do something to avoid such waste?
But the disease of error goes beyond just the cost to patients, their families and the taxpayer.
Below the tip of this iceberg of serious harm and extra bed days lies a mass of second victims of error: the doctors and nurses at the coal face of care and the harm caused to the reputation of hospitals and the medical and nursing professions – the third victims of error – through their alleged complacency.
The second victims must at the very least struggle with the psychological harm from having harmed someone and, for some, the weight of the law is called to bear on them.
impressive reduction
While errors will probably never be entirely eliminated where the system relies on humans, it is noteworthy then that, in the last three decades, there has been an

impressive reduction in the number of fatal accidents occurring in a number of different safety-critical industries, notably the airlines, the railways and the chemical and petrochemical processing industries.
as a consequence, these industries have come to be known as high reliability Organisations –hrOs. Some have actually managed to achieve the goal of ‘zero fatal accidents’ and sustain that achievement for many consecutive years. remember, at the time of writing, there has been no fatality on a Uk-registered jet airliner since the 1989 k egworth plane crash, when a British m idland a irways’ Boeing 737 crashed on the embankment of the m1 motorway.
d enial from the medical and nursing professions, cultural inertia and learned helplessness in healthcare organisations (‘I’m just an individual in a huge machine – what can I do to make the system safer?’) have limited the translation of hrO safety training techniques into the healthcare environment.
These factors are also likely to play at least some role in the absence of any substantial reduction in avoidable error reported in a 2010 study of patient safety carried out over six years in ten north Carolina hospitals in the US.
The rate of avoidable serious harm to patients remains at approximately the same rate as the 1991 study; the authors of the study concluding that there was ‘little evidence of widespread improvement’ in patient safety [landrigan 2010].
Since 2011, I have used CPS exclusively for all my histopathology. Altogether an excellent service that I recommend to all my consultant colleagues.
Mr George Fowlis – Consultant Urological Surgeon
Psychology of error h owever, there is hope on the horizon, because some healthcare organisations have woken up to the problem of error in healthcare and are taking initial steps to move towards hrO status.
One component required for any organisation to become highly reliable is staff training in the psychology of error.
We have argued for many years that there is no need to re-invent the wheel [reynard 2006] in this regard. Tried and tested training techniques for pilots and train drivers in the psychology of error as a means of reducing mistakes in those domains are equally applicable to healthcare.
although the scale of training required is probably greater in the healthcare setting, because there are many more healthcare workers relative to patients than there are air and cabin crew to flying passengers, the types of errors committed by pilots and train drivers share a remarkable similarity to those committed by doctors and nurses.
The reason of course is simple –we are all human and we share the same psychology, a psychology which at times makes us prone to error.
Next month: The hRo approach to error reduction and the development of a safety culture
John Reynard, Tim Kane, and Peter Stevenson are co-founders of Practical Patient Safety Solutions
see their biographies overleaf

John Reynard (left) is a consultant urological surgeon and honorary senior lecturer in the Nuffield Department of Surgical Sciences at the Univer sity of Oxford. He is an honorary consultant urologist to The National Spinal Injuries Centre at Stoke Mandeville Hospital. He holds a masters degree in Medical Law and Ethics.

Peter Stevenson (left) has been an airline pilot and human factors instructor for more than 30 years. He flies Airbus A330 airliners on intercontinental routes for a major UK airline.
Tim Kane (left) is a consultant trauma and orthopaedic surgeon at Spire Portsmouth Hospital and the city’s Queen Alexandra Hospital
References

Ivan Illich, Limits of Medicine. Medical nemesis: the expropriation of health. Pelican Books, London
Brennan TA, Leape LL, Laird NM et al. Incidence of adverse events and negligence in hospitalized patients: results of the Harvard Medical Practice Study I. NEJM 1991;324:370-7
Leape LL, Brennan TA, Laird NM et al. The nature of adverse events in hospitalized patients: results of the Harvard Medical Practice Study II. NEJM 1991;324:377-84
Leape LL. Institute of Medicine medical error figures are not exaggerated. JAMA 2000;284:95-97
Semmelweiss I. The Etiology, the Concept and the Prophylaxis of Puerperal Fever, 1860
Kohn L, Corrigan J, Donaldson ME. Institute of Medicine report: To Err is Human. Building a Safer Health System, 1999, National Academy Press, Washington DC, p1
Incidence and Types of Adverse Events and Negligent Care in Utah and Colorado. Med Care 2000
Gawande A, Thomas EJ, Zinner MJ et al. The incidence and nature of surgical adverse events in Utah and Colorado in 1992. Surgery 1999;126:66-75
Institute of Medicine (IOM) report, To Err is Human Building a Safer Health System 1999 www.nap.edu/catalog/9728.html
Centers for Disease Control and Prevention (National Center for Health Statistics). Births and Deaths: Preliminary Data for 1998. National Vital Statistics Reports. 47(25):6, 1999
Robinson AR, Hohmann KB, Rifkin JI et al. Physician and public opinions on quality of health care and the problem of medical errors. Archives of Internal Medicine 2002;162:2186-90
Wilson RM, Runciman WB, Gibberd RW, et al. The Quality in Australia Health Care Study. Med J Aust 1995;163:458-76
Vincent C, Neale G, Woloshynowych M. Adverse events in British hospitals: preliminary retrospective record review. BMJ 2001;322:517-9
Davis P, Lay-Yee R, Schug S, et al. Adverse events regional feasibility study: indicative findings. NZ Med J 2001; 114:203-5
Davis P, Lay-Yee R, Schug S, et al. Adverse events regional feasibility study: methodological results. NZ Med J 2001;114:200-2
Schioler T, Lipczal H, Pedersen BL et al. Danish adverse events study: Incidence of adverse events in hospitals. A retrospective study of medical records. Ugeskr Laeger 2001;163:1585-86
Michel P, Quenon JL, de Sarasqueta AM, et al. Comparison of three methods for estimating rates of adverse events and rates of preventable adverse events in acute care hospitals. BMJ 2004;328:199-200
Baker GR, Norton PG, Flintoff V et al. The Canadian adverse events study: the incidence of adverse events among hospital patients in Canada. Canadian Medical Association Journal 2004;170:1678-86
Department of Health (DoH). An organisation with a memory: learning from adverse events in the NHS. The Stationary Office, London 2000
Landrigan CP, Parry GJ, Bones CB et al Temporal Trends in Rates of Patient Harm Resulting from Medical Care. NEJM 2010;363:2124-34
Reynard J, Reynolds J, Stevenson P. Practical Patient Safety, Oxford Uni Press, 2006

Heed these memos from Garry Chapman (below) to make your billing more efficient –and your bank account healthier

Garry Chapman is executive chairman of Medical Billing and Collection
Competition among independent practitioners and private practices can be fierce, so making a good first impression with customers is vital. Stephanie Vaughan-Jones discusses how you can do just that
According to research, a mere seven seconds is all we have to win someone over when we first meet them.
it’s a small but magical window in which we can make a fantastic first impression. i n business terms, this means we have to be the best possible version of ourselves at all times.
i was reminded of the importance of this when i heard two friends talk about their recent experiences with private healthcare practices.
one created a brilliant impression and the other – well, it wasn’t quite so brilliant.
the first of these happened at a private clinic a few months ago. From the minute my friend walked through their front door, she was bowled over.
t he reception area was calm and tranquil, the staff were warm and caring and, within minutes of arriving, she was shown to a comfortable waiting area and offered a fresh cup of coffee.
t he whole experience was seamless and she left feeling like she was their most important patient, not just a visitor.
But the second encounter shared by another friend was very different. Arriving at the practice, she couldn’t see a sign for the main entrance, so rang the reception phone number to ask for directions.
t he person who answered, though, sounded less than happy to help and her abrupt instruc -
➱ p26
tions left my friend feeling like a nuisance. t he waiting area did nothing to improve matters either, with phones constantly ringing and bright lights creating a busy and slightly hectic atmosphere. the contrast in these two experiences couldn’t have been starker. Yet they are both private practices that would be competing for the same clients. And if i was a prospective patient, i certainly know which one i’d have chosen to use. So, how can healthcare practices make an unforgettable first impression? Here are ten simple things every practice can do.
1 the quest for making a fantastic first impression and offering excellent customer service starts with hiring the right people
When we choose our receptionists, we do so based on attitude, not just aptitude and we handpick each one to work with our healthcare clients. Why?
We’ve learned that a positive, can-do approach, a desire to provide amazing service and the right personality is far more important than a dazzling cV when it comes to recruiting staff. take time to explain why customer service and first impressions are so important to your team too. We consistently tell our receptionists how important they are to the success of our company, and how much we value the wonderful job that they do. recognition is essential. As well as making your team happy, it will boost productivity and motivate them to do a fantastic job.
2
At Moneypenny we talk about being a ‘GOFI’: a god/ goddess of first impressions it’s the term we use to describe the impression we want to create every time we answer the phone or a live chat inquiry. Why? We know that first impressions can be make or break when it comes to winning a prospective client.
our mystery shop of 300 businesses found that customers who were greeted with a curt ‘hello’, for example, thought the business was unprofessional, off-putting and even rude. that’s three adjectives that no private practice or clinic wants to be associated with. And, over the phone, this can be especially important, according to
the UK c ustomer Satis faction index 2018, which found the way calls were handled was one of the key differentiating factors between the top businesses and their competition.
3
next, simply be available. it may sound easy – and in theory it is – but at a busy practice with support staff juggling the needs of patients walking through the door and calling on the phone, as well as medical staff working at capacity, it’s all too common for online inquiries to be missed. the phones don’t get answered and visitors fail to receive the attention they deserve.
Have a plan or provision in place to make sure you’re covered during busy periods or when staff are on holiday.
think about who answers your phone calls and where they are located too. it could, for example, be worth creating one team of receptionists who are dedicated to seeing to the needs of patients in person and one to answer phone calls and/or live chats and emails in a separate office.
Each one can then do what they do best and give every client the attention they deserve.
4 Always remember to wear your customers’ shoes Experience your business as a new client would, looking at each touch point they could come into contact with.
Sit with someone as you watch them send an email and see how long it takes them to get a reply. get them to ask a question via live chat and call your reception team too to see how each element performs – particularly at lunchtime, during your busy periods or once the clinic is closed.
Would you have been impressed if you were a client or prospective client? Be honest and ask yourself if there is anything you can do to improve the first impression you’re currently creating.
5 remember, your clients’ experience begins before they even call or set foot in your practice.
What impression does your website give, for instance? does it look professional and reflect your high levels of service or is it looking a little tired and outdated?
A survey by Minewhat.com
found that 81% of consumers conduct online research prior to committing to a purchase and deciding which company to use. this means you could be losing out on clients before you even know it. think about your clinic environment too. What does it say to a new client?
How tidy is the parking area? is the entrance well signposted? i s the reception calm and welcoming? All of these elements will help your clients form an overall impression of your practice.
6
give each client your undivided attention. Forget everything else for the time you’re talking to them.
d on’t look at your computer, don’t look at your watch and don’t talk to colleagues.
We’ve all been served in shops where the person at the counter hasn’t even broken eye contact with the friend she is chatting to; and it doesn’t feel good.
n ot only does giving clients your full focus help to establish an instant connection, but it is an incredibly powerful way to demonstrate you value them.
So when a client calls or walks through your door, give them the gift of your full attention.
7 Smile . When we smile, it changes the chemistry in our brain, as well as the tone of our voice and can be seen or heard whether in person or over the phone.
think about your overall body language too; how it may unconsciously affect your mood and what you are ‘saying’ to your clients.
We don’t always remember what a business says to us, but we will undoubtedly remember how they made us feel.
8
How you speak is equally important, so talk clearly and confidently clients want to know whether they can trust the person they are speaking to and whether they will be able to provide a professional and reliable service.
they need reassurance that the person on the other end of phone, or a live chat enquiry or at the reception desk is listening to their needs, taking their request seriously and knows how to assist them.
do this well and it will help you
build rapport and trust, ultimately leading to better long-term relationships between you and your clients.
9
remember that it’s OK not to always have the answers there will undoubtedly be times when a client asks a question you won’t have the answer to or is upset about a situation you aren’t aware of.
What is important is that you show them you care. clients want to feel valued and looked after, especially if they are getting in touch because a family member or themselves have a health concern. i t’s your job to hold their hand through the process.
And if you don’t know how to help immediately, explain what you can do, give them a clear outline of what will happen next and stick to the promises you have made.
10
Finally, ask yourself what you can do to wow your clients – i mean really wow. We were recently lucky enough to have customer service and marketing expert geoff ramm visit our team to discuss this, and he asked us the question: what are you doing for customers that your competition isn’t?
it’s this gap which will mean you outperform competitors and blow the socks off your clients. it could, for example, be placing a handwritten note and a pair of slippers on their pillow when they arrive, or it might be following up their appointment with a card. t hey really don’t have to be big things. As so often in life, it’s the little touches that mean the most. t hink about the ways in which you could do this, with the aim of impressing every client so much they can’t wait to go away and tell a friend how brilliant you are.
See ‘Using social media to come out ahead’, page 29
Stephanie Vaughan-Jones is commercial manager at leading outsourced communications specialist, Moneypenny, which delivers phone answering, live chat, switchboard and multichannel customer services to doctors and other businesses in the UK






having served healthcare professionals since its inception in 1993, tax-link, chartered tax advisers and accountants in wimbledon, has built a wealth of knowledge and experience in dealing with taxation issues faced by doctors in private practice. our focus is on tax planning and compliance.
l tax structuring to suit personal circumstances (llp, limited companies)
l Solvent liquidations
l consultant groups and consortia
l Assessment of pension contributions in light of tapering annual allowances
l Ad hoc assistance with hmrc investigations and reviews. For more information and tax-efficient advice, please:
phone: 020 8540 1920
email: rakesh@tax-link.com
Address: the long lodge, 265-269 Kingston road, wimbledon, Sw19 3nw
Dear Reader,
Subscribing to Independent Practitioner Today is the only way you can be sure you will see every issue and have the option of reading us online using our special page-turnable edition. Don’t risk missing out. Our personal subscription for doctors and managers is only £90 a year and £210 for organisations. But you can cut this to just £75 and £180 respectively if you pay by direct debit. So take advantage of this offer now for our unique business journal dedicated to supporting you in your private practice. We’re confident your subscription will repay itself many times over!

Editorial director

Doctors, please give GMC No.
(See rates listed above)
i enclose a cheque for £ ........... made payable to the independent practitioner Ltd please debit my mastercard/Visa/amex/diners
I encose a cheque made payable to The Independent Practitioner Ltd
Please debit my Mastercard/Visa/
manager* r * indicates this item must be filled
i would like to pay by direct debit (please complete all details in box below). Don’t forget, it’s £15 cheaper to pay by direct debit; £30 less for organisations.

the manager
Instructions to your Bank or Building Society to pay Direct Debits Name and full address of your bank/Building Society
Name(s) of account holders
name(s) of account holders branch sort code
post your application (no postage required – uK only) to: independent practitioner today Subscriptions department, FreepoSt, po box 36, plymouth, pL1 1br
Please post to: Proact Ltd Subscriptions Dept., 12 Mary Seacole Road, The Millfields, PLYMOUTH PL1 3JY Or email to: jackie@marketingcentre.co.uk Or
Banks and Building Societies may not accept Direct Debit instructions for some
banks and building Societies may not accept direct debit instructions for some types of account Signature(s) date ___________ phone: 01752 312140 Fax: 01752 313162 email: lisa@marketingcentre.co.uk or subscribe online at www.independent-practitioner-today.co.uk if you want to pay by card

Debit at any time, by writing to your Bank or Building Society. Please also send a copy of your letter to us.
ATTRAcTing pATiEnTs: 2

Will this be the year you get ‘out there’? Grant Brookes (below) presents an independent practitioner’s guide to the dos and don’ts of social media

We cannot ignore the way social media has become ingrained in society.
People look to their social channels for answers for almost every kind of problem, as well as to engage and build relationships with others.
Social media is also a costeffective marketing method for private practitioners. It plays a huge part in many people’s lives and can be tapped into as a source for growing your practice and gaining interest from
potential patients as well as business connections and networking with colleagues and influencers.
o f course, there are contentious issues to keep in mind as a professional practitioner when communicating through social media. You can quickly and easily get started on social media, but you need to keep professional boundaries in place and abide by official guidelines provided by industry bodies.
t he GM c sets out its own
guidelines for social media use by doctors and practitioners which should be kept in mind at all times.
Before looking at some of the key social media channels private practitioners can benefit from, here are some key reminders to keep in mind whatever social platform you are using:
1
Confidentiality: the GMc guidelines state all doctors must be honest in communica-
tions with patients, as well as clients and colleagues. o n social media, almost all communications are public, so confidentiality is key.
2 Professionalism: You are representing yourself and your practice on social media. You must remain true to your professional practice and also maintain a level of integrity throughout your online communications.
3Understanding: Do you know why you are using a particular social media channel? It is essential you understand any social media channel before you start using it, so you can get the most out of it and not use it in an inappropriate or ineffective way.
Let’s look at three key social media channels, how to use them and how they can benefit your practice and your patients.
LinkedIn is a professional network designed for connecting and communicating with colleagues and others in your sector. It’s a chance to share expert content and opinion with other likeminded professionals.
There are more than 467 million users on LinkedIn and more than 130,000 posts are shared on a weekly basis, many in the medical field. Below is a closer look at how to succeed on LinkedIn.
On LinkedIn, there is the opportunity to share a great deal of information about yourself. The site allows for different sections to be created and each one is an opportunity to concisely share a little more information about you and your experience.
The summary section, for example, should always be as simple and to the point as possible. You need to keep it concise but engaging.
you or for you to share exactly how they feel about their experiences.
You don’t have to give recommendations to receive them, but it’s all part and parcel of the LinkedIn experience. Be sure to comment on the skills and qualities of anyone you recommend and provide detail as to how they offered a positive impact on your time working together.
The largest social media platform is a great place for providing a wealth of relevant information for your patients and potential patients.
Your practice or professional page is a place where patients will naturally gravitate towards, as Facebook is so popular and actively used by many to search for services.
There are more than 1.47 billion people daily active users on Facebook, showing just how integral the platform is to many people’s lives. Doctors can actively use Facebook to grow their practice by keeping the following points in mind:
➲ Know your audience
As mentioned, the people liking or following your professional or practice page on Facebook are likely to be patients or those considering becoming patients.

• Completely open scanner that is well tolerated by claustrophobic patients
• Weight-bearing scans for spine and joints enable a more precise diagnosis
• Patients who are large or cannot lie down can be accommodated

Don’t just write your specialty; write what makes your particular line of interest and work unique and interesting. Treat this section like your elevator pitch and really show exactly what makes you stand out in your field.
The ‘Skills and Endorsements’ section is your opportunity to list all of your key medical skills. Don’t forget those outside of medicine, though. Highlighting your additional skills is once again a way of standing out from others in your field who have put less time and energy into their profile.
Recommendations are like mini testimonials of your work and practice on LinkedIn. It’s a chance for those who have worked with
You need to know what they want to see in terms of content and what they expect your page to offer them. There needs to be close relevance in what you share and what they are looking for or they will quickly disengage.
➲ be clever with content
People visiting your Facebook page don’t just want generic posts thrown out there or random shares of others content. They want to know who is writing to them and why.
Are you actively going to be the ‘face’ of your page or do you plan to allow the voice to come from others in your practice such as receptionists or other professionals?
The content you produce and share needs to resonate with your audience, so use names, images and more to create a sense of belonging for your patients on the page.
Being able to offer something new and unheard is the lifeblood of successful Twitter accounts, so if you have something interesting and unknown to share, tweet it

Getting noticed can be tricky, but, with the right approach, you can find your place and engage with the right followers to attract interest and eventually growth in your practice. Below is some advice on how to do this:
➲ inject personality into your posts
Professionalism is key, but your tweets are an opportunity to create a unique voice for your practice.
It needs to reflect the feel of your practice and injecting a little personality will definitely be more engaging and interesting to your followers. People want to know the personal side of everyone they follow and while you have boundaries to keep, you can still offer this in your tweets and content.
➲ break news
OK, you’re unlikely to have any world-changing news to share, but even small changes in your practice or local area news is what people want to hear.
Being able to offer something new and unheard is the lifeblood of successful Twitter accounts, so if you have something interesting and unknown to share, tweet it.
➲ promote your best content
Paying for Facebook posts may seem like a waste, but you can hone your adverts so closely to your desired target audience that it’s often worth trying.
You can fully localise your adverts to ensure they only appear in the feeds of those local to your practice, showing them your best, most relevant content and potentially piquing their interest in your practice.

Twitter is an online news and social networking site where people communicate in short messages called tweets.
It moves at an extremely fast pace and as you send a tweet, anyone who follows you will see it and hopefully be engaged and interested in what you have to say. There are more than 330 million globally active users on Twitter.
➲ be consistent
It is very easy to get sucked into constantly tweeting absolutely everything. This is very rarely successful and won’t work in the long term.
Sticking to a content calendar or scheduling your tweets consistently throughout the day is effective for ensuring you are consistently seen but not noticeably ‘always there’.
You can schedule in time to follow up on any replies or messages, too, to ensure your followers know you are engaged and interested.
Social media can enhance your online profile and, in turn, bring more people to your practice door.
Effective social media marketing requires time and effort, but it can be worth it and is a very costeffective method of attracting more attention to your practice.
Grant Brookes is managing director of The Web Surgery www.thewebsurgery.com
Investing in a Practice Management System is a huge commitment. That’s why we offer you a FREE 30 day trial to see if our software is right tor you.
The Cost Effective, Secure & Private Practice Management System.
Support is FREE throughout your trial via telephone, online chat or email.
Thinking of moving from your current Practice Management supplier?
• Access anytime, 24/7, on any device
Changing your software may seem daunting and time consuming, but it doesn’t need to be.
• Data backed up in ‘real time’ on the Microsoft Azure Platform
• Clear, user friendly interface
• Go Paperless by typing & importing documents
Talk to our Support team today on 0330 999 3399 and ask how moving to MidexPro can give you a more cost-effective alternative and hear how we can minimise the impact to your practice whilst you move.
One Touch eBilling
•
• Advanced analytical Practice Data available
• Encrypted software to IS027001 standards with Optional 2-Factor Authentication
•
Outstanding UK support via Email, Phone & Live Chat
For a FREE 30 day trial of the system, Please call 0330 999 3399 or email support@midexpro.com
E: support@midexpro.com
T: 0330 999 3399
W: midexpro.com
A chaperone should always be offered where any intimate examination is proposed, particularly if a patient has been sedated – even if the doctor and patient are of the same sex, says Dr Gabrielle Pendlebury (left)

An A lleg Ation of sexual misconduct involving patients can be potentially devastating for a doctor, impacting negatively on their career and reputation.
So it is essential that doctors do not become complacent and overlook the use of chaperones, when faced with multiple clinical commitments.
these allegations can often arise when least expected, especially at times of high clinical demand,

when the search for a chaperone may seem like an unnecessary hindrance to the efficient use of time.
gMC guidance1 states: ‘intimate examinations can be embarrassing or distressing for patients and whenever you examine a patient you should be sensitive to what they may think of as intimate.
‘this is likely to include examinations of breasts, genitalia and rectum, but could also include any examination where it is necessary
Make everyone aware of the chaperone policy in your place of work and the procedure for accessing chaperones
be prepared to defer examination if the patient is uncomfortable or a chaperone is not available
communication is key. explain clearly what the examination will entail and the clinical rationale behind it
Document carefully that a chaperone was offered, if no chaperone is available or the patient declines. outline the reasons why examination was necessary at that time and details of the examination undertaken
to touch or even be close to the patient.’
good communication
Doctors should consider what the patient would deem to be an intimate examination. Allegations of assault have arisen in relation to the placing of eCg leads, fundoscopy or inadvertent touching of the patient in what is a legitimate clinical examination.
intimate examinations include
examination of the breasts, as well as the genitalia and rectum. t herefore, clear and comprehensive communication of the nature of the examination is essential to prevent the possibility of misunderstanding, but also to allow the patient to decline the examination, if they choose.
Doctors need to ensure that their actions are above reproach. and that they have clear written documentation to support their actions.
A S triking nu M ber of allegations of sexual assault or inappropriate sexual behaviour arise in connection with the administration of general anaesthetics or sedation.
in these situations, it is important that a doctor is never left alone with an unconscious or sedated patient.
i n relation to anaesthesia and sedation, sexual hallucinations are more common with newer agents
such as midazolam and propofol. it is not uncommon for doctors to be accused of inappropriate and potentially criminal behaviour as a result of the hallucinogenic effects of these drugs.
Any allegations of this nature should be taken seriously, even if the patient was never alone with the doctor, as the patient is likely to be distressed and fearful, completely believing the veracity of their accusation.
Doctors should make sure that the consent process outlines details of the procedure to reduce the possibility of the patient misinterpreting clinically indicated procedures.
in the event of an allegation, a full explanation of the cause must be offered, along with reassurance that there was a chaperone present. Allegations have arisen even when the patient was in theatre with numerous others present. the nature of these hallucinations can mean that it may be difficult for the patient to accept the explanation and prolonged counselling might be necessary.
Doctors should be prepared and accurate in their response to an accusation of this nature. Any discussions around the event should be witnessed and documented and hopefully the records of events while under sedation or anaesthesia will corroborate the explanation.
it is not uncommon for doctors to be accused of inappropriate and potentially criminal behaviour as a result of the hallucinogenic effects of these drugs
Mrs smith underwent a colonoscopy under sedation. The procedure was unremarkable, but, post recovery, Mrs smith indicated to her husband that she had been assaulted in recovery. she indicated that the surgeon had placed his penis in her hand.
Mr smith immediately called the police, and the doctor called the advice line, as the police were requesting that he attend the police station for an interview under caution.
The doctor had made meticulous notes. he had reviewed Mrs smith in recovery in the presence of a nurse.
Medical Protection suggest dealing with complaints of this nature promptly, as this will help the patient process the matter, thus relieving their distress and preventing matters escalating, potentially to the regulator or the police. e ven if the events are later exposed as sexual hallucinations, this scrutiny can damage both the patient and the doctor.
Mrs smith was groggy from the sedation. The doctor had placed two of his fingers in the palm of her hand and asked her to squeeze them. Mrs smith had misinterpreted this stimulus due to the hallucinatory effect of the sedation.
Medical Protection was able to support the doctor by instructing a solicitor to attend the police interview with him. During this interview, supported by the medical notes, the doctor was able to explain the clinical rationale for all the actions he took in respect of this patient.
The presence of a chaperone protected the doctor, as the nurse was able to give a witness statement, supporting the doctor’s position. as a result of this and a full explanation to the patient, the matter did not progress further.
Dr Gabrielle Pendlebury is a medicolegal consultant at Medical Protection reFerence 1. GMC (2013), Intimate Examinations and Chaperones, London, GMC
years’

Where we are today in private healthcare owes much to the development of the NHS. Dr Ellen Welch (right) presents some of the key milestones down its 70 years
The first decade of the NHS was not without its problems, but it was successful enough to cement it into an institution.
A free, universal service was a huge cultural change from what had preceded it and, only three years into the NHS, financial challenges became evident, resulting in the introduction of charges for prescriptions, dental and optical services by the end of 1952.
The 50s saw a post-war baby boom and the introduction of technologies such as the microwave oven, plastics, nylon stockings and computers.
Medical technology also thrived. Ultrasound was adapted for use in foetal monitoring and the success of antibiotics in the 1940s was followed by a rash of new drugs.
1950 The link between smoking and lung cancer is proven. Richard Doll had been studying lung cancer patients since the 1940s, expecting to find it was caused by fumes from coal fires or cars, but instead found that smokers are more likely to die of lung cancer than non-smokers.
He also found an increased risk of heart disease. Doll quit smoking during his study and lived to the age of 92.
The Collings Report – the first major report on quality in general practice – found poor standards of care, poor working conditions and isolation from other professionals. GPs had remained outside of the NHS as independent contractors rather than salaried employees.
The 1948 NHS Act had intended that GPs would move away from being single-handed and would be
rehoused with other GPs inside health centres, but this proved unaffordable.
1951 Charges for dental and optical appliances imposed.
1952 Prescription charges of one shilling are introduced and a flat rate of £1 for ordinary dental treatment.
Watson and Crick discover structure of the DNA.
1954 Children are granted daily visits from their families while in hospital. Until this time, visiting was only permitted for an hour at the weekend.
Children were often placed alone in adult wards, with little explanation as to what was happening to them. Paediatricians realised that this separation was traumatic and instituted family visiting.
Rationing ends.
The Percy Commission is established by Winston Churchill’s government to review the care given to people with mental health problems. They recommend that treatment should be given in the community, where possible, rather than in large psychiatric institutions.
This is supported by the 1959 Mental Health Act, which also states that mentally ill patients should not be differentiated from physically sick patients.
1956 The Guillebaud Report on the cost of the NHS is published. It reports that the cost of the NHS in relative terms is falling and that capital spending is 33% of pre-war levels and that future costs would be met by economic growth.


The Clean Air Act is passed, aimed at reducing the air pollution created by burning coal.
In 1952, the ‘Great Smog’ had descended upon London, exacerbating the health problems of those with heart and lung conditions, resulting in a dramatic increase in mortality rates. The act allowed local authorities to control emissions from industrial premises and improved death rates.
1957 The Willick Report suggests a 12% reduction in the number of doctors being trained, due to the increasing numbers of specialist registrars unable to secure consultant posts.
This is later considered a misjudgement and training numbers are increased in 1961. The report is later believed to be responsible for the severe shortages of junior doctors throughout the 1960s.
1958 Polio and diptheria vaccination programme launched
ensuring everyone under 15 is vaccinated, leading to a dramatic reduction in cases.
The Opticians Act allows opticians to become regulated professionals.
The buoyant economy of the technicolour 60s brought low unemployment rates and increasing affluence. UK families bought their first cars, kitchen appliances and televisions, and mass communication became a reality.
Sixties’ teenagers were the first generation free from conscription and the decade saw laws regarding divorce, homosexuality and abortion become more liberalised. Feminism gained credibility, meaning women could broaden their dreams beyond motherhood and marriage.
In 1968 , 850 female factory workers in Dagenham went on strike, fighting for equal pay to
their male co-workers – and the Equal Pay Act was passed in 1970 as a result.
The newly introduced contraceptive pill created a sexual revolution, while a boom in pharmaceuticals saw the development of drugs of abuse.
Immigration also bolstered the workforce of the NHS. The Caribbean and Ireland had been a primary source of nurses since the 1940s; in the 1960s, more than 18,000 doctors came from Indian and Pakistan in response to an appeal.
1960 Male nurses are admitted to the Royal College of Nursing for the first time.
Surgical Firsts. The first UK kidney transplant is performed by Michael Woodruff in Edinburgh. The 49-year-old twins both survive for six years, before dying of an unrelated illness.
In the same year, the first full hip replacement is carried out at the Wrightington Hospital, Lancashire, by Prof John Charnley. He asks patients if they mind returning their hips to him post mortem, and the majority agree, allowing him to check for wear and tear and research improved future models.
1961 The oral contraceptive pill is launched.
1962 The Hospital Plan approved development of district general hospitals for populations of around 125,000 in an attempt to unify the tripartite system of hospitals, GPs and local authorities and make hospitals accessible to the populations they served.
The Porritt Review is published the same year, led by old-school surgeon Sir Arthur Porritt. He was initially sceptical about the NHS and had been a critic in the 1940s, but had been convinced that it had to continue. He suggested the system was fragmented and that Area Health Boards should be established to bring together hospital, GP and community services.
1964 Fluoridation is introduced to the water supply with the intention to cut tooth decay.
1965 Prescription charges abolished.
Abolition of the death penalty.
1966 A new contract improved pay and conditions for GPs, instituting a maximum list size of 2,000 patients, improving resources available for professional education and improvement in premises and hiring support staff. Following this, group practices became the norm.
1967 The Salmon Report makes recommendations for developing the nursing staff structure and the status of the profession in hospital management.
The Cogwheel Report considers the organisation of doctors within hospitals and proposes specialty groupings.
The Abortion Act is introduced by the Liberal MP David Steel and becomes law in 1968, allowing termination of pregnancy by a registered physician up to 28 weeks’ gestation, if two other doctors agree that it is in the best mental and physical interests of the woman. In 1990, this is reduced to 24 weeks. In 2019, the Act still does not extend to Northern Ireland.
1968 Britain’s first heart transplant is carried out in May 1968 by South African-born surgeon Donald Ross in London. A team of 18 spend seven hours on the procedure, on what is the tenth procedure of its kind carried out since it was pioneered by Christiaan Barnard in Cape Town, a year earlier. The patient dies after 46 days from an associated infection.
Prescription charges re-introduced
The NHS saw real advances in medical progress. CT scans and transplants became available and the first computers found their way into NHS hospitals.
In the mid-1970s, then Health Secretary Barbara Castle tried to phase out private patients being treated in NHS facilities.
1972 CT scans introduced. Computer tomography scans were invented in the late 1960s by Sir Godfrey Hounsfield and became commercially viable in 1972.
The Cochrane Report sets out the vital importance of randomised controlled trials in assessing the effectiveness of treatments,
leading the way for evidencebased medicine.
The Royal College of General Practitioners is established, giving GPs an official representative body.
1975 The Merrison Report extends the functions of the GMC in relation to medical education to make the body more accountable. Disciplinary processes are separated so those whose performances are impaired by ill health are recognised.
It is suggested that doctors might undertake some sort of periodic ‘relicensure’, but the committee decided this was beyond its remit. Revalidation is eventually implemented in 2012 after a series of high-profile medical scandals.
Endorphins are discovered by John Hughes and Hans Kosterlitz at the University of Aberdeen.
Three-year postgraduate training programmes for GPs become mandatory.
1978 The world’s first IVF baby is born. Gynaecologist Patrick Steptoe and physiologist Robert Edwards develop in-vitro fertilisation. Louise Brown is the first ‘test tube baby’ to be born using this technique. Since then, more than a million children have been born this way worldwide.
The Winter of Discontent caused by the oil crisis sees a worsening of the NHS’s financial problems.
1979 First bone marrow transplant is performed on a child with primary immunodeficiency at Great Ormond Street Hospital by Prof Roland Levinsky.
Wearing seat belts is made compulsory for drivers and front-seat passengers in a car.
The 80s saw a rise in drug resistance. Widespread use of antibiotics since the 1940s had allowed infectious organisms to adapt to become resistant, meaning the drugs used to kill them were no longer effective.
There was a focus on preventative medicine in the 80s and a notion that individuals were responsible for their own health and lifestyle choices and breast and cervical screening programmes were introduced to the NHS.
Privatisation took off in the 80s – and the NHS looked like it would follow suit when Prime Minister Margaret Thatcher announced plans to reform the service and introduce an internal market.
More next month
☛ Adapted from The NHS At 70 – A Living History, by Dr Ellen Welch, a cruise ship doctor and GP in West London. £12.99 from www.pen-and-sword.co.uk

Independent Practitioner Today readers can get 25% off 'The NHS at 70', plus free UK p&p.
Quote NHS70 at www. pen-and-sword.co.uk
the outset, may come as a surprise and mean that a contract lasts much longer than you expected.
In particular, these queries arise in relation to what may be called ‘rolling contracts’ or ‘auto renewing contracts’, also known as contracts with ‘evergreen’ clauses.
These contracts are typically entered into for a fixed period. For example, you may wish to contract with a supplier for the provision of advertising services for two years. You may forget about this contract over the next 24 months, but decide to try a new supplier at the end of the two years.
Stuck in a contract

Watch out for the rolling contract. Terms and conditions apply, but many doctors get caught out, warns Michael Rourke (pictured opposite)
ALCHEMISTS SOUGHT to turn base metal into gold, but their searches and efforts proved fruitless.
Physicists have studied the cosmos and determined there can be no perpetual motion due to the laws of thermodynamics.
But lawyers have worked out how to turn base letters into gold, through the perpetual – or at least rolling – contract.
A typical complaint made by non-lawyers when reading contract terms will be that they are
all ‘small print’ and written in ‘legalese’.
Contracts are typically drafted by lawyers, to be understood by lawyers with legal certainty in mind, rather than with the aim of being usable or understandable by those who read or sign them.
Despite this, it is essential that anyone in private practice does not sign without reading and understanding or they may fall into various traps.
This article is concerned with one trap for the unwary, concerning how long the contract is going to last. This is sometimes called the ‘term’ or ‘duration’ of the contract.
A query which can arise from doctor clients concerns contract renewal clauses, whereby they have found suppliers informing them that they are stuck with contracts that they no longer want or require for a further period.
Buried in the contract may be terms which, if not appreciated at
But if the original contract contained a provision which provides for it to automatically renew for a further period, you may – unless notice has been given in the right way – be stuck with the old supplier. In the worst case, you may be stuck with the old supplier, and have entered into a contract with the new supplier.
These clauses are found in a huge variety of contracts and can catch out practitioners whether acting as single consultant, or in contractual groups or corporate structures.
The precise terms of such clauses vary from contract to contract. Typically, they provide that if no notice is given by a specified time before the expiry of the first term – for example, three months before the expiry date – then the contract shall automatically roll on for a period.
These clauses provide for certainty of ongoing terms without the need for new contracts to be entered each year and provide certainty for the supplier and provider on which they may plan for the next years business – provided no notice has been given. While these are the basic justifications for such terms most of us
will have some experience of such contracts (and their potential pitfalls) from the perspective of a consumer, for whom they have not always proved popular.
Unfair contract terms are what they say on the tin; terms, or clauses, in contracts which are deemed to be unfair, and so are unenforceable in the courts.
When such terms arise in the business-to-consumer relationship, protection for the consumer can be found in legislation. The latest guidance on consumer protection indicates that, for consumers, automatically rolling over contracts may be unfair, unless the contracts contain protections.
But when businesses contract between themselves, the law largely takes the view that they are ‘the best judge of the commercial fairness of the agreement which they have made, including the
fairness of each of the terms of that agreement’.
The view of the law is that commercial parties should be sufficiently prudent to either read and understand what they were signing up to, or have sought advice. Unfortunately, too few people necessarily read the terms they sign or seek legal advice.
Despite this, the position remains that if a business did not take steps to understand the terms of the contract, they should have, and the terms and conditions will therefore apply, with very few exceptions.
When a small business contracts with a much larger business, they can feel powerless to negotiate the terms of the contract. For consumers, this would attract legislative protection, but for small businesses no such protection is available. While other jurisdictions have sought to address this imbalance in business-to-business (B2B) con-
tracts, the UK is yet to adopt such an approach.
Limited protection against some unfair terms between businesses is found in legislation. This is available where businesses have not negotiated the terms of the contract and instead have contracted on one business’ standard terms.
In these circumstances, provisions of contracts limiting liability, or permitting a defaulting supplier to either perform no or different services to that contracted for, will be subject to a test of ‘reasonableness’. However, an auto-renewal clause would not be caught by this requirement.
Research by the Federation of Small Businesses (FSB) in 2016, found that 24% of respondents had suffered from rolling contracts, resulting in businesses either being tied into lengthy notice periods (22%), or having to
pay high early termination fees (20%) to end the contract.
The FSB’s research found that, on average, B2B ‘unfair’ contract terms had cost the UK’s small business community an estimated £1.3bn a year annum.
It is important that independent practitioners’ businesses review the contracts they sign up to, as businesses are generally held to the contracts that they make.
Clauses providing for automatic renewal are just one of the potential traps which can be buried in the text of contracts. In practice, such traps, once noted, are easily avoided simply by the giving of notice in the right way.
Unfortunately, those who do not read the small print, or fail to take action having read articles such as this, may find themselves in difficulty.
Michael Rourke is an associate solicitor at Hempsons
Independent Practitioner Today has joined forces with leading healthcare lawyers Hempsons to offer readers a free legal advice service.
We aim to help you navigate the ever more complex legal and regulatory issues involved in running and developing your private practice – and your lives.
Hempsons’ specialist lawyers have a long track-record of advising doctors – and an unrivalled understanding of the healthcare system as a whole.
Call Hempsons on 020 7839 0278 between 9am and 5pm Monday to Friday for your ten minutes’ of free legal advice.

Advice is available on:
Business structures (including partnerships)
Commercial contracts Disputes and litigation HR/employment
Premises
Regulatory requirements and investigations


YOU MAY be deciding whether now is the time to engage some help with your finances, as the scale of your work is growing, your income streams are becoming more complex and your tax affairs seem confusing.
Alternatively, you may have stayed with the same financial planner for a decade but never been entirely convinced that they understand every aspect of your financial affairs.
Whatever your current situation, it can be worth asking a few key questions to ensure the needs of you and your family – both now and in the future – are being met.
Do they have experience of medical income streams? You may have NHS work, a private practice, an academic post or a combination of all three. Understanding the complexity of your remuneration package is a skill that comes with experience in the medical arena.
Doctors’ pay scales are complicated, the pay slip is convoluted and mistakes can be easily missed by busy medical professionals getting on with the day job or financial advisers not well versed in NHS pay regulations.
We see many new clients who have pay slips which we find to be incorrect. One consultant had been on the wrong pay level for over eight years leading to an arrears payment claim of £75,000.
What should you be asking your financial planner?
Dr Benjamin Holdsworth (right) shows how independent practitioners can ensure they have the right help in place

As well as the substantial salary rebate, the consultant’s pension income in retirement will increase by more than £4,000 per year, plus the capital value of his or her NHS pension will be increased by £100,000.
These types of mistakes can lead to grave consequences with pension contributions. There are harsh penalties for excess annual and lifetime pension savings.
If you are on the wrong pay scale, your pension will be greater than projected and could lead to
breaches of the taxfree savings limits. Any repayment paid as a lump sum could also trigger a tax charge.
Do they understand the nuances of the NHS pension?
The three separate NHS pension schemes affect the benefits you will receive when you retire and depend on when you joined.
Each one has a different structure, operating criteria, retirement age and repayment level. Whereas the 1995 and 2008 options are definedbenefit schemes, the 2015 pension is based on average career earnings.
Comprehending every facet of your scheme will have a direct impact on giving the best advice possible.
Do they understand how the annual and lifetime allowances work for doctors? There are strict limits to pensions’ savings known as the annual and lifetime allowance. These govern how much you can put into your pension free of tax each year and overall.
There are many doctors who walk blindly into these tax traps. Since ‘pension simplification’ in 2006, total annual allowance tax charges have netted the Treasury more than £1,200m and lifetime allowance breaches have generated a revenue of £335m.
Calculations for the annual allowance are particularly complicated because HM Revenue and Customs determines the contributions for a defined benefit scheme such as the NHS very differently to that of a private pension.
Figures are based on the deemed ‘growth’ of the pension in that year with an allowance made for inflation.
The new ‘tapered’ annual allowance means senior doctors earning over £150,000 from all sources –and this includes their pension growth itself, which is a point often missed – face a substantially lower
taxfree savings limit, down to just £10,000 a year in some cases.
Excess pensions’ savings above the annual allowance which is relevant to you are charged at your marginal rate of income tax. Breaches to the lifetime allowance are charged at up to 55% on anything taken as a lump sum and 25% if taken as income.
Do they work together with your accountant?
There is a perception that your accountant and financial planner have very different roles to play in organising your finances. To some extent this is true; an accountant will be looking specifically at tax compliance and efficiency, while the financial planner will be proposing how you can achieve your overall wealth objectives.
However, there is a greater need than ever before to have a united source of advice. Unless you have twoway communication between both parties, essential information can be missed or you can receive conflicting advice that leads to poor decisionmaking.
An accountant will have an accurate record of the income of the client from every source –which is usually quite complex at senior consultant level.
This indepth information can be extremely useful to the financial adviser meticulously planning how to make the client’s assets work together to generate future income.
Are they versed in clinical practice trading structures?
You may well have considered the advantages of trading as a partnership or limited company, but are you really maximising the efficiencies that these can provide?
The tax landscape has changed significantly over the last few years and there are now more implications to consider when selecting the best structure for your business.
Your trading structure will have an impact on your pension contributions and pension tax. A limited company can contribute ‘pretaxed’ company income to a pension.
Higher rate taxpayers can put profit straight into a personal pension rather than taking the income as a dividend. This applies to any director, so it can be particularly useful to contribute to a spouse’s pension if their lower salary means a higher annual allowance or they do not already have NHS pension contributions to consider.
Do they understand your attitude to risk?
If you have a retirement plan, is it still an accurate reflection of your objectives? Your plan will need to keep pace with your current standard of living. If you sought advice ten years ago but have not reviewed your financial status recently, it is imperative to check your savings and investments are fit for purpose.
It should also reflect your present attitude to risk. For example, we helped a new client who, at 59, had been previously working with just a stockbroker with many of his assets tied up in high risk investment products that were completely unsuitable for his situation.
Can they advise on different types of medical retirement options?
Some doctors are retiring later –no longer clocking off permanently at aged 60 and often phasing their retirement over several years. Lifestyle choices, which might include ‘retire and return’ or ‘24hour retirement’ bring an extra facet to the finance discussion.
With a clear idea of a client’s entire financial scene, we can conduct very specific modelling, which could show that it might be advantageous to retire after, say, 36 years rather than continuing to contribute for more years of service.
Can they plan your exit strategy from your practice?
You will want to ensure you and your adviser have unified thinking over your income require
ments now and your future exit strategy, considering carefully whether to opt for formal liquidation – hoping that Entrepreneur’s Relief will apply – or to maintain the company and extract dividends for a number of years post retirement.
Will they look after your family across generations?
The finances of each member of your family need to be working constructively together to maximise wealth and ensure the security of future generations.
For example, ISAs have become significantly more useful as a savings vehicle, particularly if different generations are taking advantage of their allowances.
The introduction of pension freedoms now gives universal access to pension funds from age 55. Furthermore, the ability to pass on pensions tax efficiently on death to family members and other beneficiaries makes pension funding attractive – particularly for some spouses of consultants or where the lifetime allowance and annual allowances are less of a concern.
Individuals should also maximise their annual capital gains allowance, which can provide great scope to reap investment gains every year free of tax. With proper stewardship, you and your partner can both build a goodsized portfolio before you need to worry about capital gains tax.
Make sure you have the right professional in place to help you achieve your own financial and lifestyle objectives.
The content of this article is for information only and must not be considered as financial advice. Cavendish Medical always recommends that you seek independent financial advice before making any financial decisions. Levels, bases of and reliefs from taxation may be subject to change and their value depends on the individual circumstances of the investor. The value of investments and the income from them can fluctuate and investors may get back less than the amount invested.
Dr Benjamin Holdsworth is a doctor and director of Cavendish Medical, specialist financial planners helping consultants in private practice and the NHS
Dr Ellie Mein (right) responds to two more medico-legal dilemmas that independent practitioners have had to confront


QI have been called to give evidence at the inquest of a private patient who collapsed and died at home ten days after I carried out a hip replacement procedure.
I don’t believe my report would have given any cause for concern, but the coroner has named me as an interested party.
Does this mean I need legal representation?
AThe coroner has wide scope to name interested persons in line with the categories set out in section 47 of the Coroner’s and Justice Act 2009.
These include family members and life insurance policy beneficiaries but also anyone whose action or failure to act may, in the Coroner’s view, have contributed to the death.
Being named as an interested party also gives you certain rights. As well as being informed of the date, time and place of an inquest, you can see reports of the witnesses whose evidence is to be used and you or your legal repre-

sentatives can ask questions of other witnesses.
While legal representation is not usually necessary for doctors who are called to give evidence and attending the inquest with a solicitor can appear overly defensive, you should definitely contact your medical defence organisation (MDO) in this case. Your MDO will be able to advise you and appoint a solicitor as necessary, bearing in mind factors such as whether there is any known or anticipated criticism of your care; whether the family or other parties are to be legally represented and whether the coroner is sitting with a jury.
At the inquest itself, it helps to know what to expect as a witness and be prepared. It’s likely that you will be asked to read all or part of your report and then be asked questions by the coroner. You may then be questioned by other interested persons or their legal representatives and your own solicitor and members of the jury, if applicable.
The coroner is obliged to exclude any inappropriate questions not relevant to the limited scope of the inquiry, and no witness is obliged to answer questions that could incriminate them.
If you think your professional conduct or competence is being called into question while you are giving evidence, you can ask the coroner for an adjournment of the inquest. However, this is highly unusual, and it is better to seek legal advice in advance if you have concerns.
When giving evidence, it’s important to listen to the question carefully rather than answer the question you want or expect to hear.
It is better to ask for clarification than try and interpret what the questioner intended.
Answer as clearly, honestly and succinctly as you can, avoiding medical jargon and don’t be afraid to say that you do not know the answer or that it is outside your area of expertise, rather than speculate.
While it might be unnerving to be given the status of interested person, this does not mean that you are certain to be criticised or aggressively questioned at the inquest.
It may be reassuring to know that in an audit on MDU inquest files from 2013 and 2014 that had a solicitor instructed, less than 1% of those members were criticised by the coroner to the extent that they needed to inform the GMC and only the same tiny proportion were associated with any form of criminal investigation.
Claims were initiated by the estate in approximately 14% of cases, while a complaint was raised with the GMC in 8%.
Given that these were inquest cases where legal representation had been thought prudent, the statistics for all inquest cases in total are likely to be even lower.
QThe parents of one of my young private patients are going through an acrimonious split and the mother now wants her daughter to have her surname – rather than her father’s. She has asked me to change my medical records, but I am not sure if I can do this without agreement from the child’s father?
If you know that both mother and father have parental responsibility, acceding to the mother’s request would be difficult to justify and is likely to lead to a complaint
AWhile adults are entitled to change their name as they wish, changing the name of a child requires the consent of all those with parental responsibility or a court order.
And the child’s father will have parental responsibility if he is married to the child’s mother or named on the birth certificate.
However, this depends on when and where the child was born. In England and Wales, this applies to any child born on or after 1 December 2003; in Scotland, any child born on or after 4 May 2006 and in Northern Ireland any child born on or after 15 April 2002. For more information, go to the website www.gov.uk/parentalrights-responsibilities/who-hasparental-responsibility.
Unmarried fathers who are not named on the birth certificate can also acquire parental responsibility if they obtain a Parental Responsibility Agreement from the mother or a Parental Responsibility Order from the court.
If you know that both mother and father have parental responsibility, acceding to the mother’s request would be difficult to justify and is likely to lead to a complaint.
You could also invite criticism for failing in your ethical duty to ensure that your records are accurate.
In these circumstances, you have no choice but to tell the patient’s mother that you cannot change her daughter’s name on her medical records and explain the legal reasons.
You could also direct her to the relevant Government guidance for more information: www.gov. uk/change-name-deed-poll/ change-a-childs-name.
Dr Ellie Mein is a medico-legal adviser with the MDU
Tug of love: Her mother wants to change her daughter’s surname due to a divorce




Anaesthesia, Critical Care & Pain
Dermatology • General Practice
Plastic Surgery • Radiology
Trauma & Orthopaedics
Hands-on workshops
Multidisciplinary lectures
Satellite and joint sessions
Bedside ultrasound course
Contribution from allied specialities
Keynote lectures by invited speakers
Our tour of NHS private patient units continues with Philip Housden (right) analysing private patient revenue growth for 27 NHS acute trusts across the North-west region. This covers the conurbations of Greater Manchester and Liverpool, and counties of Cheshire, Lancashire and Cumbria
FOR THIS regional group of trusts, the accounts show that total private patient revenues increased in 2017-18, albeit not fully making up the reduction experienced the year before.
Total revenues are stated at £30.0m in 2017-18, up approximately 2.5% from £29.3m in 2016-17 ( Figure 1 ). This level of income represents a small decline from 0.36 to 0.35% of these trusts’ total patient-related activity revenues. This remains below the combined national average outside of London of 0.5%.
These 27 acute trusts vary significantly by private patient revenues (Figure 2 on opposite page). For this analysis, the trusts have been grouped together, where relevant, according to whether or not they have a dedicated private patient unit or not and present turnover (Figure 3). Only 18 of the trusts are shown, as the remaining nine have revenues below £250k a year.
The regional top earner is The Christie Hospital at £6.09m, up £247k year on year (4.1%).
This places the trust sixth in the top ten-earning trusts outside of London by revenue – and 18th overall in England. This is now 2.8% of the trust’s revenues, a gradually declining figure from 2.92% in 2016-17 and 3.51% in 2013-14. The trust achieves the majority
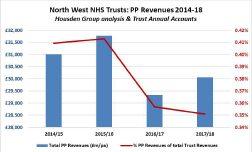
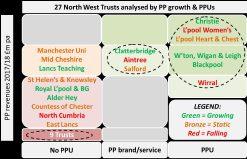
of these earnings through a partnership with HCA Healthcare UK located within the Christie Private Clinic. HCA entered into a joint venture with the trust in 2009, which led to investment in the formation of the clinic.
There are 34 inpatient beds in
single rooms and the clinic specialises in the diagnosis, management and treatment of all cancers.
Across Liverpool, there are a number of trusts with small PPU wards and services and these enable

these trusts to achieve higher than the regional averages for private patient revenues and overall trust income contributions.
The highest grossing of these is the Liverpool Heart and Chest’s six-bed Maple Suite, which enables the trust to achieve over £3m a year in private patient revenues. Last year’s income of £3.25m (£3.36m 2016-17) was 2.46% of total trust revenues, a gradually declining figure from the peak of 3.27% three years ago.
Liverpool Women’s Hospital shows a similar pattern, with £2.9m revenues last year, down over £700k on two years ago, and representing a slide to 2.81% of revenues, down from 4% in recent years.
The trust’s seven-bed Catharine Suite, located on the Crown Street site, supports a range of private gynaecology and cosmetic surgery procedures plus a range of non-surgical cosmetic procedures.
In north Liverpool, Aintree’s Sefton Suite is a 19-bed unit that, uncommonly for an inhouse NHS PPU, has a dedicated theatre and Resident Medical Officer. Despite this, the service earned £1.62m –0.46% of total trust revenues – last year, down nearly 4% on the year before and well down on the peak of £2.2m in 2014-15.
The Royal Liverpool and Broadgreen University Hospital has enjoyed growth of over 45% last year, albeit to a modest £511k of
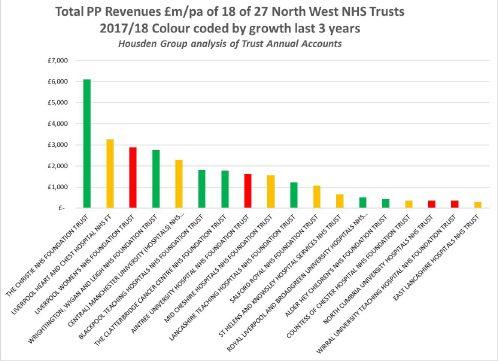
total private patient revenues. The trust may be enabled to increase future earnings following the long-awaited move to the new hospital campus.
To complete the city’s NHS providers, the region’s specialist children’s hospital, Alder Hey, offers a service to international patients, including remote clinical consultation and multidisciplinary patient reviews and this has enabled the trust to grow private patient revenues form a modest £90k (0.05% of turnover) in 201516 to £434k last year (0.19%).
The Clatterbridge Cancer Centre opened the Clatterbridge Private Clinic in 2013 – a joint venture with the Mater Private Hospital.
Clatterbridge is one of the largest networked cancer centres in the UK, operating in ten sites across Merseyside and Cheshire, providing chemo- and radiotherapy and highly specialised treatments, including proton Papillion therapies, to local, regional and international patients.
The trust reported revenues of £1.8m last year – 1.41% of trust totals – down a little on 2016-17, but well up on the £1.25m two years ago and the less than £0.5m a year prior to the joint venture.
Manchester hospitals
In Manchester, the highest-earning trust is the conglomerate Manchester University Hospitals, which has no dedicated private patient beds and so achieves a modest 0.19% of turnover from this source, which, given the size of the trust, still delivered £2.3m last year.
These earnings are mainly achieved through the Private Patient Centre at the Manchester Royal Eye Hospital and also paediatrics and, to a lesser extent, dental.
Wrightington, Wigan and Leigh have grown their private patient revenues to nearly £2.8m last year, a high point of 1.0% of total revenues, mainly through the specialist orthopaedic John Charnley Wing, which offers outpatient consultation rooms and 16 private rooms.
Completing the city’s NHS private patient services are St Helen’s and Knowsley, and Salford Royal. The former has virtually doubled revenues from £375k two years ago to £660k last year – up from 0.14% to 0.21% of turnover –without a PPU. The latter delivered £1.07m in 2017-18, down on the £1.5m two years earlier, with the growth coinciding with the opening of the Salford Clinic to
provide outpatient and ambulatory services for private patients.
In Cheshire, the Countess of Chester, Mid Cheshire and Wirral University Hospitals have differing performance. In Chester, drawing on the private medical insurance hot spot south of Manchester, revenues have increased to £358k last year, without a PPU, but these remain down on previous earnings of over £0.5m a few years ago.
In Macclesfield, Mid Cheshire Hospital is steady at £1.5m revenues a year. On the Wirral, the trust has provided services from an eight-bed PPU, Park Suite, but the trust accounts show a continued decline in private patient revenues, down to a new low of £339k last year – 0.12% of turnover –when in 2011-12 the revenues were £1.3m at 0.52% of the total.
On the coast, Blackpool has a relatively high-level retirement population driving insured and self-pay activity. The trust provides the Lancashire Suite, a sixbed private patient suite within Blackpool Victoria Hospital, where earnings were £1.8m last year; at 0.46% of the trust total, up £384k on the previous year.
Of the remaining trusts, none have a dedicated PPU and only
Lancashire Teaching trust has revenues over £500k a year.
The majority are delivering NHS services within a catchment that has low private insurance take-up, but others have perhaps not developed private patient services due to local independent sector competition and other NHS priorities.
Within this latter group are Stockport and the Walton Centre in Liverpool. Stockport is well located within the ‘Golden Triangle’, which offers 24/7 backup and specialist care that even the BMI Alexandra cannot. The Walton Centre looks capable of reversing the recent years’ decline in private patient activity through its range of specialist services.
Private patient earnings provide a useful additional source of income for a number of NHS trusts in the North-west. Unsurprisingly, those with a dedicated PPU are doing best, as are those teaching hospitals with specialist services. The region is second only to the South-east in terms of prosperity and it is likely that the potential for private patient growth is far from exhausted.
Philip Housden is a director of Housden Group

With the much talk of HM Revenue and Customs’ move to a digitised tax system over the coming years, it is easy to overlook the current system which is still relevant for all.
Ian Tongue looks at the self-assessment tax system for individuals and explains some of the key considerations, particularly for those who may have recently started their private work and have not felt the full effect of the self-assessment tax system

THE SELF-ASSESSMENT tax system for individuals has been around since 1996 and is just that: self-assessment. Each year, you self-certify your relevant tax information to HM Revenue and Customs (HMRC) by submitting a tax return.
For those that have not previously submitted a tax return, you have until 5 October following the tax year in question to register for self-assessment.
The tax return needs to be submitted by the 31 January following the tax year which always ends on the 5 April for an individual.
For example, the tax return for the year ended 5 April 2018 needs to be submitted by 31 January 2019. Nowadays, almost everyone submits their tax return electronically, but for those wanting to submit their return manually, the deadline for paper returns is 31 October each year.
The tax return pulls together all of your sources of taxable income net of allowable expenditure and any other relevant items that are required to be disclosed for tax.
For those who prepare the tax return themselves, the Government gateway system allows you to complete your tax return using HMRC’s web-based software.
For those using an accountant to submit their return, the accountant will use specialist software. For all taxpayers who are required to submit a tax return annually, it is a good idea for doctors to use the services of an accountant with specialist knowledge of the sector.
It is relatively easily to get to grips with the submission deadlines, but the most common area of misunderstanding is the tax payment system. This can be confusing. Most doctors will be used to paying their tax each month under the pay-as-you-earn system (PAYE). This generally works well to collect the right amount of tax on salaried employment earnings, provided that an individual’s tax coding is reviewed regularly. However, typical problem areas where the PAYE can under collect tax are:
Moving job between employers;
Not providing a new employer with your P45;
Multiple salaried positions;
Working abroad for a relatively short period;
Earnings exceeding £100,000 for the first time.
As a result of the above, it is a good idea to consider having an accountant well in advance of engaging in private work to avoid any nasty surprises on your salaried earnings.
The self-assessment system creates a long delay from the time you incur a tax liability to when you actually pay it over to HMRC.
The payment dates for paying tax under self-assessment are 31 January and 31 July each year, with the January payment being the one where catch-up payments are made.
Falling just after an expensive period for many, it can be the date to hate!
The area that can catch out someone new to self-assessment is the ‘payment on account’ system. This requires you to make a payment within the tax year as well as after the tax year once you earn sufficient untaxed income.
It can be painful the first time you breach the requirement to make a payment on account, as the tax charge is effectively 1.5 x the tax due for the previous year.
An example is as follows:
Tax liability for the year ended 5 April 2018
£20,000
Payment by 31 January 2019
It has been well publicised in Independent Practitioner Today that a fundamental change to the way your tax affairs will be reported to HMRC is coming. This new system is known as ‘Making Tax Digital’ – or MTD as the taxman calls it (See our September issue, page 46)
For doctors who are VAT-registered, the start of the changes commence in April 2019. And for almost everyone else, it will be from April 2020 at the time of writing.
It remains to be seen whether the implementation for VAT-registered taxpayers is successful, but the general feeling is that there could be further delays for non VAT-registered taxpayers.
The new system will require quarterly reporting of your financial affairs and is generally expected to be a burden to small businesses.
HMRC believes this will increase tax revenues through more accurate returns, but, in reality, this system is likely to result in additional compliance costs for small businesses who submitted their affairs accurately historically.
HMRC has indicated that it has no intention of changing the payment system under MTD, but this remains to be seen.
A move to electronic record-keeping will be required and the main providers of practice management software have been working hard to ensure their systems are compliant with the new digital tax regime.
representative of that year’s liability.
In the early stages of your private practice, the payments on account made do not keep pace with the increasing tax liability and therefore the January payments catch up the shortfall.
out if you are not aware of the payment system.
Ensuring you engage a medical specialist accountant prior to or at the commencement of your private work is the best way to ensure there are no surprises later on and your affairs are managed effectively.
Amount due in respect of the year ended 5 April 2018
£20,000
If you are in a position where the payments of 50% of the prior year would be too high, there is a system to allow you to reduce the payments on account.
£10,000
1st payment on account for the year 2018-19
The self-assessment tax system can be confusing and catch you
Ian Tongue (right) is a partner with Sandison Easson accountants

£30,000
Total payment by 31 January 2019
Payment by 31 July 2019
2nd payment on account for the year 2018-19
£10,000
As can be seen from the example, a £20,000 tax liability results in a £30,000 payment the first time that you have to pay on account.
The payments on account always represent 50% of the previous year tax liability, which is why the payments in the example above are £10,000 each.
This figure may or may not be

CHENIES MEWS IMAGING CENTRE SPECIALIST MRI IN THE HEART OF LONDON
• Advanced Cardiac MRI
• 3T Neuro MRI
• MRI for patients with cardiac pacemakers
T: 0203 887 0566
E: referrals@cheniesmews.com
W: www.cheniesmews.com

Our motoring correspondent Dr Tony Rimmer (below) takes a new, premium, French brand for a spin. Can it recapture the magic of years past?

JUST OCCASIONALLY, in medicine, a revolutionary development comes along which takes us all by surprise and alters the way we practise.
It may take us a while to change, but if we do not take notice, we can be left behind. In the world of cars, this is what happened in 1955 when Citroën launched the legendary DS.
An aerodynamic and futuristic body clothed a chassis with an advanced hydro-pneumatic suspension and braking system.
The result was a car that possessed a magic carpet ride and cut through the air very efficiently.
All other car manufacturers were caught napping and could not understand how Citroën could sell this new technology to the mass market so cheaply.
The DS cemented Citroën’s reputation as being a forward-think-
ing, albeit quirky, producer of mainstream cars.
In 2010, to capitalise on this positive image, Citroën named all the top versions of each of its models, DS. Then, in 2014, to separate these cars from the basic Citroëns that they were based on, it created the standalone and premium DS brand.
The DS 7 Crossback is the first DS product that is all new and has no Citroën equivalent.
Premium SUV
It is a medium-sized premium SUV to compete with the Audi Q3, BMW X1, Mercedes GLA, Jaguar E-Pace and the Volvo XC40.
Three engine options include two turbo-diesel models of 1.5 and 2.0 litres producing 128bhp and 178bhp respectively and economy figures of 69mpg and 58mpg.
The petrol model uses a
1.6litre turbo-petrol unit producing 225bhp with an impressive 49mpg economy. All models are front-wheel drive, but in 2019 there will be an allwheel-drive plug-in hybrid model at the top of the range.
There are four trim levels: Elegance, Performance Line, Prestige and Ultra Prestige. All have excellent standard equipment, but the top models have some interesting and innovative features.
DS Active Scan Suspension uses an onboard camera to scan the road 20 metres ahead, identify any significant undulations and alter the dampers accordingly. Clever stuff if it works –more of that later.
DS Active LED Vision is another smart system to adapt the headlights to speed and terrain automatically.
From the outside, the DS 7 is



shaped like any other SUV, but had some nice design features that set it apart. When switched on, the front light units are bathed in a warm purple glow while three separate lighting modules rotate into place. The rear light clusters have a striking diamond shaped design that is quirky and very Citroënesque.
Step in to the driver’s seat and you definitely feel that you are in a premium product. Lots of leather trim, high-quality plastic and a large infotainment screen of 12.3 inches on top models, make you feel good about yourself before the car turns a wheel.
The central dashboard clock is made by French watchmaker B.R.M and rotates into view on start-up – a nice feature. The overall quality is not quite at Audi or BMW levels, but not far behind.
The cabin is roomy with plenty
of space for four or five and the boot is spacious enough for everyone’s luggage. I am not convinced by the hands-free boot opening, though. You wave a foot underneath the rear bumper to activate the door, but its erratic operation is more irritating than helpful.
I was keen to try the DS 7 on the road and assess the clever suspension. The 220bhp version is my favourite; it is smooth, powerful and quiet, whereas the 2.0litre diesel version is a bit noisy at slow speeds which spoils the premium experience.
The 1.5litre diesel is a bit too underpowered for a car of this size. The eight-speed automatic gearbox shifts smoothly and straight-line performance is swift. The ride, although no magic carpet, is soft and comfortable.
The rear light clusters have a striking diamond shaped design that is quirky and very Citroënesque


However, around corners, the body does lean a bit and keen drivers among you will not get much satisfaction from a dash along B-roads. The steering lacks some precision too, which does not help the situation. The Active Scan Suspension seems to help a bit but not as much as I would hope.
As long as you do not expect too much of the DS 7, it delivers a perfectly comfortable and refined ride and passengers will appreciate the relaxed progress.
As a brand to reflect other highend French couture products like Hermes and Chanel, this new DS is mainly successful.
If you are a medic who likes to be a bit different and is a bit fed up with the usual German brand offerings, then it will appeal.
Dr Tony Rimmer is a former GP practising in Guildford, Surrey
The hands-free boot opening is triggered by you waving a foot underneath the rear bumper
Body: Five-door SUV. Front-wheel drive
Engine: 1.0 litre four-cylinder turbo-petrol
Power: 220bhp
Torque: 300Nm
Top speed: 141mph
Acceleration: 0-62mph in 8.7 secs
Claimed economy: Combined 47.9mpg
CO2 emissions: 134g/km
On-the-road price: £38,990

All you need to know about accountancy for private practitioners

Growth in the self-pay market has given consultants in our latest benchmarking survey a profit boost. Ray Stanbridge reports
OUR HEADLINE figures show that, for a typical consultant ophthalmologist’s private practice, gross income has risen by 3.9% between 2016 and 2017, going up from £127,000 to £132,000.
Costs have increased by 3.6%, rising from £55,000 to £57,000, and, as a result, gross profit went up by 6.9% from £72,000 to £75,000.
The profit margin of 56.8% is virtually unchanged from that in 2016.
The last time I looked at this specialty – in Independent Practi
tioner Today , December 2017January 2018 – I commented: ‘My view is that ophthalmology continues to be an attractive option in private practice, although it is subject to the vagaries of Choose and Book.’
The evidence for 2017 tends to support this cautious view.
Choose and Book work continues to be a very significant part of the income of some consultants.
But things are volatile and there is some evidence, albeit very limited, to suggest that the NHS is trying to make savings here,
essentially by extending waiting times.
This may suggest a ‘boom’ in a year or two, when NHS chiefs are directed to reduce waiting lists.
The major growth sector seems to be in self-pay, and that won’t come as a surprise to regular readers.
Ophthalmology services appear to be one of those for which private patients are prepared to dip in to their savings and pay. There are significant signs that a percentage of insured work is slightly falling.
There have been some changes in costs, which have surprised us.
Staff costs have risen from £17,000 to £19,000 on average –this partially represents the Competition and Markets Auth ority (CMA) imposition of market rate charges to consultants.
Also, there is the effect of tracking the personal allowance when consultants employ spouses and partners.
Surprisingly, there has been a slight fall in consulting room charges. We are not sure of the reason for this.
Some, although not many, consultants have negotiated consultation agreements with private
All the evidence suggests that the bad debt rate is lower when consultants have employed professional billing services rather than trying to deal with matters on their own
hospitals. This has led to a net downward effect on room hire charges. The evidence is not clear; it may be this is just an anomaly. There has been a small growth in the use of home office costs –following the Samadian tax case – and in motor and travel and bad debts.
But all the evidence suggests that the bad debt rate is lower when consultants have employed professional billing services rather than trying to deal with matters on their own.
There has been a significant fall in ‘other’ costs, primarily marketing. Most ophthalmologists have now built their websites and the fall may be a corrective action, show-
Year ending 5 April. Figures rounded to nearest £1,000 (percentage is also rounded up)
Source: Stanbridge Associates Ltd.

Since
Since starting in the mid 1970’s Sandison Easson has continued to grow and is one of the largest independent medical specialist accountants in the UK.
Since starting in the mid 1970’s Sandison Easson has continued to grow and is one of the largest independent medical specialist accountants in the UK.
Sandison Easson
Sandison Easson acts for medical professionals throughout all stages of their career and has clients in almost every town in England, Scotland and Wales.
Sandison Easson acts for medical professionals throughout all stages of their career and has clients in almost every town in England, Scotland and Wales.
We provide the usual services you would expect from an accountant such as preparation of your accounts and tax declarations but offer so much more including advice
We provide the usual services you would expect from an accountant such as preparation of your accounts and tax declarations but offer so much more including advice on:
We provide the usual services you would expect from an accountant such as preparation of your accounts and tax declarations but offer so much more including advice on:
• Setting up in Private Practice
• Setting up in Private Practice
• Setting up in Private Practice
• Developing your Private Practice
• Developing your Private Practice
• Developing your Private Practice
• Tapering of the Annual Allowance
• Tapering of the Annual Allowance
• Tapering of the Annual Allowance
• Lifetime Allowance planning
• Lifetime Allowance planning
• Personal Allowance planning
• Personal Allowance planning
• Expenses that you can claim and those you cannot
• Reviewing your PAYE Coding Notices SPECIALIST
• Expenses that you can claim and those you cannot
• Minimising your tax bills
• Minimising your tax bills
• Reviewing your PAYE Coding Notices
ing they do not invest in expensive websites every year!
What then of the future?
There are signs that consultants with small private practices are looking at the options of being employed by private hospitals.
On paper, this seems to be an attractive option for some. Other consultants are looking at developing groups, and this business structure is increasingly attracting the interest of private medical insurers, as we have reported
before in Independent Practitioner Today
We expect incomes to continue to rise slowly, although many consultants are likely to earn the same income but will have to work harder.
But, in real terms, it does look as if all incomes from ophthalmologists will, on average, be stable over the next couple of years.
Our survey is not statistically significant, but is rather a reflection of how consultant ophthalmologists are typically performing in the market place.
Consultants who are included in our survey are those who:
Are not in full-time private practice;
Have at least five years of private practice experience;
Are seriously interested in private practice as a business;
Earn at least £5,000 a year gross in the private sector;
May not be a member of a group or have incorporated.
Next month: Gynaecologists
Ray Stanbridge is a partner with accountancy, finance and tax advisory medical specialists, Stanbridge Associates
Oncologists
Gynaecologists
Make sure you don’t miss our next issue, published on 14 February. You may not receive every issue if you have not yet subscribed to the journal. Don’t risk missing out on vital topics we tackle next time: We’ve dubbed our next issue the ‘February Fixer’ because there’s a lot of emphasis and advice on rectifying various aspects of things that can sadly go wrong in private practice:
1. Tackling the disease of error in healthcare – risks and opportunities in the private healthcare sector. Our trio of writers – two doctors and an airline pilot – continue their series with a look at the high-reliability organisation approach to error reduction and the development of a safety culture
2. Our Technology in Practice series by Kingsley Hollis examines management errors and how to avoid them
3. A review of many consultants’ incomes demonstrates it is time to find new ways of running their private practice because their business efficiency is no longer what it was
4. Intellectual property: our legal column warns of the potential mistakes you could make if you are considering the development of your own health technology
Business Dilemmas columnist Dr Kathryn Leask advises a private GP on how to end a professional relationship with a patient and responds to a private GP on what to do when a patient threatens violence
Surprise surprise! Consultant gynaecologists have just notched a 28% profits rise. Our Profits Focus examines the reasons
Published by The Independent Practitioner Ltd. Independent Practitioner
Today is editorially independent and thanks Bupa for its assistance with distribution. Printed by Pepper Communications Ltd Material is governed by copyright. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment. Editorial layout is the copyright of the publishers. If you wish to use it for promotional purposes on websites or for reprints, we would be happy to discuss licensing the copyright to you.
© The Independent Practitioner Ltd 2019
Registered office: 7 Lindum Terrace, Lincoln LN2 5RP
Write to Independent Practitioner Today PO Box 198, Cranleigh GU6 9BB
EDITORIAL INQUIRIES
Robin Stride, editorial director
Email: robin@ip-today.co.uk Phone: 07909 997340
@robinstride
What are you saving for? Cavendish Medical’s Patrick Convey explains why this decision will help shape your best course of action. The key to navigating difficult financial waters is ensuring your overall plan is fit for purpose and it should be able to weather any storm
Top Tips for Busy Doctors: Jane Braithwaite on how to ensure your practice answers all calls – and how to manage this effectively
Our ‘double-O doctor’ motoring correspondent has all the fun – and he’s still smiling after testing Aston Martin’s DB11 duo, the Volante and new Vantage
Tracing our roots. Where we are today in private healthcare owes much to the development of the NHS over 70 years. Dr Ellen Welch presents more of the key milestones since 1982


Accountants give their tips on spring cleaning your finances and turning over a new leaf
Our PPU series reviews private patient revenue growth for NHS acute trusts across the North-east region covering the conurbations of Tyne and Wear and counties of Durham and Northumbria
Ten years ago in Independent Practitioner Today
ADVERTISERS: The deadline for booking adverts in our February issue is 18 January

ADVERTISING INQUIRIES
Margaret Floate, advertising manager Email: margifloate@btinternet.com Phone: 01483 824094
SUBSCRIPTION RATES
£90 independent practitioners. £90 GPs and practice managers (private & NHS). £210 organisations. Save £15 paying by direct debit: individuals £75 (organisations £180).
TO SUBSCRIBE – USE SUBSCRIPTION FORM ON PAGE 28 or EMAIL: lisa@marketingcentre.co.uk or phone 01752 312140 or go to the ‘Subscribe’ page of our website www. independent-practitioner-today.co.uk
Publisher Gillian Nineham Phone: 07767 353897. Email: gill@ip-today.co.uk

SAVE £15 WITH DIRECT DEBIT!
Guarantee delivery of your next copy of Independent Practitioner Today. Take out a subscription and you will get full access to our news, features and previous issues on our website. See details on the left.
BACK ISSUES: £12.50 including post & packaging CHANGING ADDRESS OR SUBSCRIPTION DETAILS?
Phone 01752 312140 or Email lisa@marketingcentre.co.uk


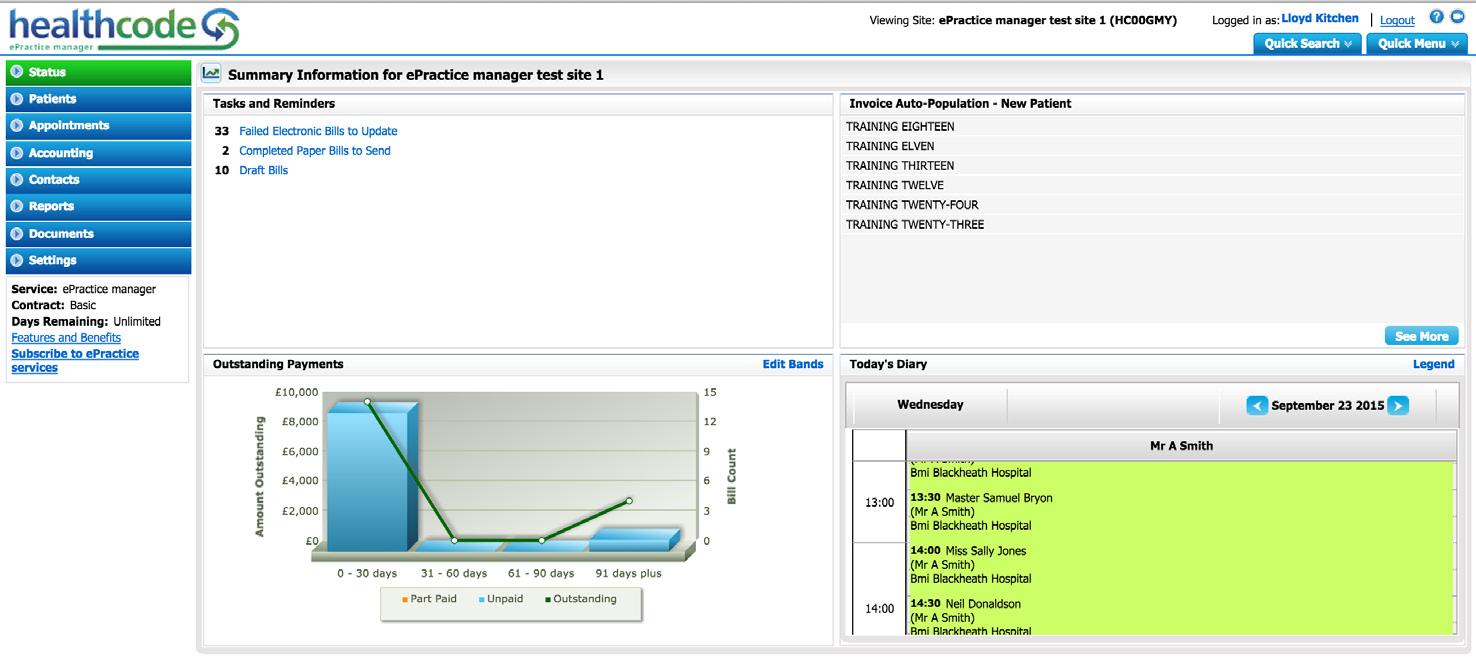
Electronic Billing
Remove printing, posting and admin costs
Payment Tracking
Ensure you have been paid for the bills you submit
Financial Reporting
Keep track of your practices’ performance
Complimentary App
Free Apple and Android app available
Appointments and Diary
Manage your schedule and send appointment letters
Membership Enquiry
Real-time online checks for patient membership number
Pre-populated Invoices
Which contain the information you require to submit bills
Shortfall Reminders and Letters
Automated prompts to keep you on top of any shortfalls