INDEPENDENT PRACTITIONER
THE BUSINESS MAGAZINE FOR DOCTORS WITH A PRIVATE PRACTICE
In this 60-page issue

No avoiding defence costs

A grip on staff illness
What can doctors do to manage sickness absence at their practice?




What can doctors do to manage sickness absence at their practice?

By Robin Stride
Ambitious plans to enable hundreds of consultants to see and treat their private patients in The Shard have been unveiled by HCA International.
The hospital group has applied for planning permission to relocate outpatient services from the neighbouring London Bridge Hospital onto three floors of the 1,016 foot ‘vertical city’ now dominating the capital’s skyline.
If approved, the multi-million pound development – covering 70,000 square feet on the fourth, fifth and sixth floors of Europe’s tallest and most iconic building –would be an international beacon for the private hospital sector.
Hospital chief executive John Reay told Independent Practitioner Today the decision to apply to develop The Shard was hugely influenced by customer demand.
He said: ‘There has been growing pressure on us to provide new and additional ultra-modern facilities for people living and working in the area. And if we get the goahead from the planners, we will also be able to expand our inpatient facilities at London Bridge Hospital itself.’
The outpatient centre, which would have a dedicated entrance, would represent the biggest expansion of any private hospital in London for many years.
It is envisaged there would ini tially be 80-100 consulting rooms for use by around 300 consultants from a wide range of specialties. They would have access to a huge range of state-of-the-art diagnos tic equipment and minor ill ness treatment rooms.
London Bridge Hospital, with 140 beds, is thought to have the highest number of MRI scanners of any in the UK. It has invested extensively in diagnostic treatment technology and has seen doubledigit revenue growth over the last decade.
An ambitious move to The Shard would release con siderable space for it to work with consult ants to expand the unit as a



centre of excellence for cardiac care, where there is demand for increasingly complex medical procedures. A planners’ goahead would also bring a boost to other specialties and free up room for 26 new inpatient rooms plus 30 new day patient beds. HCA declined to elaborate on the potential cost of the project other than to say it would be ‘very considerable – in the region of many millions’.
But HCA International president Michael Neeb is on record as saying the group has earmarked another £300m for development over the next two to three years. The London Bridge project, considered by some observers to be valued in the order of £60m, would represent a large chunk of that.
For the last five years, HCA has taken no profit out of its UK ventures, putting 100% back into investment. In the last three years, it has already spent £150m. It said 30% of its income was from abroad and increasing.
A spokesman said: ‘The facilities would be out of this world – one of the most dramatic and cheerful medical places to work in Europe.’
Units from other HCA hospitals could also have a presence in the complex along with new specialties.
The Shard is ideally placed to benefit from the area’s international transport hub status, which will see an estimated 54m people passing annually through the recently redeveloped London Bridge Station.
Towering above the London Bridge Quarter, The Shard so far comprises offices, three world-class restaurants, the five-star Shangri-La Hotel, exclusive apartments and a public viewing gallery.
Its website describes it as ‘a timeless reminder of the power of imagination to inspire change’.


December 2013-January 2014
www.independent-practitioner-today.co.uk



your bright ideas need protecting advice to doctors on how to get a patent to shield their ideas from plagiarism P14
your practice in the clouds
Graphic designer jonathan anstee reveals the principles of good website design P26
open up to new ways of reaching you Don’t just rely on old referral routes; open up to the magic of multiple doorways P32
Pressure on billing continue to build Big changes have affected doctors’ billing in recent years; what of the future? P42
don’t be bedazzled by lump sums planning to spend your pension lump sum may be exciting, but be very careful P46
solving your ethical dilemmas our medico-legal experts answers your questions about CCtV and abortions P50
Plus our regular columns starting a private practice planning ahead for tax P52 Doctor on the road Volkswagen Golf Gti P54 Profits Focus: ophthalmologists

ediTorial commenT
It’s certainly no time for ostriches in the costly and ever more complex realm of medical defence – as our feature on page 36 makes clear.
Keeping your head down makes sense to many in private practice, but as we enter 2014, there awaits an army of big issues facing private doctors.
And each one – there is no room here to name them all –demands doctors very much keep their heads up and watch carefully.
The Competition Commission inquiry will have a huge impact. We face a fastchanging landscape. Maintaining and
improving profitability will be a major challenge for many.
Then there are massive income implications from a raft of pension issues to deal with, changing requirements from HMRC and other bodies, and revised NHS contract considerations. If you are also an employer, then a raft of staff employment issues awaits too.
And you still have the main job to do! So we will do our best in the year ahead, as ever, to be your eyes and ears, alerting you to what is coming and providing expert advice to deal with it. Thank you for all your support in 2013.
Tell us your news Editorial director Robin Stride at robin@ip-today.co.uk
Phone: 07909 997340 @robinstride
To adverTise Contact advertising manager Margaret Floate at margifloate@btinternet.com Phone: 01483 824094
To subscribe lisa@marketingcentre.co.uk Phone 01752 312140

Publisher: Gillian Nineham at gill@ip-today.co.uk Phone: 07767 353897
Head of design: Jonathan Anstee chief sub-editor: Vincent Dawe Circulation figures verified by the Audit Bureau of Circulations
by leslie berry
Large numbers of senior doctors have started the New Year still unprepared for potentially massive cash hits due to the pension tax changes coming into force in April, warn financial planning experts.
Following a series of eleventhhour seminars with independent practitioners, specialist advisers revealed that many could face extra tax charges on their pension savings amounting to tens or even hundreds of thousands of pounds.
Experts from Cavendish Medical have been holding teachins to help doctors understand the severity of the Government’s changes.
They told Independent Practitioner Today that during the sessions, many doctors revealed they did not realise the extent of the issue or the potentially huge impact on their own retirement funds.
Cavendish Medical chairman Dr Mark Martin said: ‘Many of the doctors we spoke to have read the news reports about these changes but either haven’t had the time to act or don’t think the figures apply to them. They are shocked when we spell things out.’
To recap, the lifetime allowance for taxfree pension savings will fall from £1.5m to £1.25m.
Many high achieving doctors will be affected by this rate change. If they exceed it, then it could hit them with a 55% tax charge.
Both their NHS pension and any accumulated private pensions will be tested against this limit.
To increase the agony, at the same time, the annual allowance for taxrelievable pension contributions will drop from £50,000 to £40,000.
As reported in Independent Practitioner Today last October, many doctors have received notices for inadvertently exceeding the annual allowance when it fell from £255,000 to £50,000 in 2012.
But the fear is that many more could now be caught out by the next cut in April.
Dr Martin continued: ‘The bottom line is that if you breach one of these limits, you will be looking at a harsh tax penalty.
‘We are trying to help people now while they still have options available to minimise their liabilities. Unfortunately, there is little we can do after the event.’
He advised doctors to check their tax position without delay.
Advisers at the Medical and Dental Defence Union of Scotland (MDDUS) have revealed a 400% rise between 2010 and 2012 in doctors seeking guidance on the use of social media sites such as Facebook and Twitter.
Medical adviser Dr Naeem Nazem said: ‘Patients interacting with their doctors on social media may inadvertently create an uncomfortable and awkward situation.
‘It also risks blurring the boundaries in the doctor patient relationship, which could impact on the quality of care they receive.
‘Doctors must keep their relationship with patients professional or they risk becoming too close, which can cloud their judgement and affect their objectivity and clinical decisionmaking.’
Doctors on Twitter – see pages 18 to 24
by a staff reporter
King Edward VII’s Hospital Sister Agnes has got off to a very happy new year after being given an early Christmas present – its biggest ever gift, worth up to £30m.
Delighted bosses said they would use the money for expansion. Now they are working on plans to grow the facility by more than 25%.
Consultants are being promised additional facilities including operating theatres, extra wards and consulting rooms.
One possibility being pursued is to build a tunnel to link the hospital with new premises opposite at Macintosh House, Beaumont Street, Marylebone.
King Edward VII’s massive financial boost comes from The Michael Uren Foundation, which aims to advance any charitable purpose as the trustees at their discretion think fit.
The benefactor has given £5m to the hospital and said it was committed to providing such help and support as needed up to a maximum of £30m in the next decade.
Governors’ chairman Robin Broadhurst said: ‘This is the most generous gift the hospital has ever received. We are all extremely grateful to the Michael Uren Foundation for securing the longterm and independent future of the hospital.’
Michael Uren, chairman of the Michael Uren Foundation, said: ‘King Edward VII’s Hospital is very dear to my heart and I wanted to do all I could to ensure it has a long, successful and independent future. I hope this gift will secure that outcome.’
What’s a doctor worth? is the banner title of a programme of BMA events planned this year to engage consultants in discussions that could feed into a new contract for their NHS work.
Delivered in partnership with research company BritainThinks, the programme taking place in England and Northern Ireland aims to use the latest technology to draw out doctors’ views and ideas.
The events are part of a campaign, also using online resources
and discussion forums, to keep doctors informed and involved in the consultant contract negotiations now underway and the wider issues affecting their working lives.
BMA’s Consultants Committee chair Dr Paul Flynn said: ‘The NHS is facing a number of pressures, from rising patient demand and an ageing population to the increased costs of new technology and the impact of Government cuts.
‘These challenges are driving massive shifts in health care and changing doctors’ working lives. In meeting them, we must ensure the results are good for patients and fair to doctors, and by engaging in this way, we can ensure that we hear firsthand the experiences of doctors on the ground.’
Negotiations do not apply to consultants in Scotland and Wales. Doctors’ leaders there think a UKwide approach is not in consultants’ best interests.

King Edward VII’s Hospital, Sister Agnes’s boss John Lofthouse is leaving at the end of next month to start a new job in March as hospital director of the Leeds Nuffield Hospital.
He told Independent Practitioner Today: ‘I will be sad to leave here, as it is a truly exceptional hospital, now in good shape for the future with the £30m gift having been agreed (see story to the right).
‘However, I have spent the last five years – nearly – travelling up and down every weekend from my home in the north and the offer to manage Nuffield’s largest hospital, in commuting distance from home, proved very attractive.’
The hospital paid tribute to the ‘extraordinarily good job’ he had done and said he had guided it through ‘huge challenges’ following the well publicised tragic suicide of a nurse who took a hoax call about the Duchess of Cambridge in December 2012.
Clearer pricing is set to benefit patients in 2014, according to Fiona Booth, chief executive of the Association of Independent Healthcare Organisations (AIHO). Answering criticism about wrong invoices being sent by private units, she told Independent Practi tioner Today: ‘All independent providers work hard to ensure that invoice charges are accurate and clearly laid out. Where mistakes occur, they should act swiftly to update invoices and charge accurately.
‘Through transparent pricing, as published on providers’ websites, it is becoming easier for patients to understand the fees that apply for different services.
‘We anticipate that this transparency will be adopted by a broader range of providers, and across more treatments, in the future.’
Treatment sourcing specialists Medical Care Direct (MCD) had voiced concern about the number of wrong invoices being received
from private hospitals or clinics, with either overcharging or erroneous charges being most common.
Chairman Jan Lawson said: ‘We have been tracking this in detail for the last three months. During August, 11% of invoices received were wrong; in September it was 15% and October 14%.
‘Most of these relate to fixedprice procedures rather than normal itemised bills, so you would think that the scope for error is small. But they are totalling over
£20,000 each month – a significant sum.
‘Our worry is if we as experts in treatment sourcing are experiencing these error rates, what hope is there for an individual who arranges their treatment directly.’
She claimed her firm’s experience suggested there was a good probability of people being charged more than expected and/or getting a confusing bundle of bills.
See Fiona Booth’s vision of AIHO’s future, p12
By Leslie Berry
Doctors’ employment law advisers are drawing attention to changes from April 2015 when parents will be able to share the statutory maternity leave and pay currently only available to mothers.
New mums will have to use the first two weeks after birth but could transfer the remaining time off to their partner. So dads can tell employers they potentially
want as much as 50 weeks off work.
Parents could alternatively each take 25 weeks to run concurrently – taking the leave in turns, in different blocks, or at the same time.
Chris Inson, a partner at commercial law firm Capital Law, warned that private practice managers should be ready to ask relevant questions and assess how the changes could affect their business. They would need to know how they would manage patients’
All independent practitioners who have set up their business as a limited liability company are being advised to look carefully at new antitax avoidance legislation in the wake of The Chan cellor’s Autumn Statement.
Medical accountant
Susan Hutter, a partner with Shelley Stock Hutter, said doctors would need to find out if it was still tax efficient for them to have a corporate structure.

Today: ‘This will be particularly relevant where partnerships have been established which have limited company partners.
expectations and how they would ensure they had adequate cover for absent staff.
He said: ‘Many people have criticised the new laws as bringing an unnecessary level of complication to an already complex scenario. However, it is my belief that if communication lines are kept open between employers and employees, administrative headaches can be avoided and all parties could potentially benefit from
the new flexible parental leave arrangements.’
The overhaul is part of a Government drive to refute assumptions that women should stay at home to look after children.
Deputy Prime Minister and fatherofthree Mr Nick Clegg said the change was long overdue: ‘Women deserve the right to pursue their goals and not feel they have to choose between having a successful career or having a baby.’
Interest in facial rejuvenation has risen by 23% in the past 12 months, according to healthcare search engine WhatClinic.com
gical treatments are worth 75% of this market.
She told Independent Practitioner
‘This will be fertile ground for HMRC because of the disparity between corporate tax rates at 20% and income tax rates which could be as high as 45% – so even the most innocent commercial structures could be perceived to be tax avoidance, which is extremely worrying.’
Inquiries into laser skin tightening have gone up by 78% in the last year, while the average treatment price has dropped by almost a fifth (18%) during the same period.
Laser skin resurfacing has seen an increase of 70% over the same period with a 34% rise in the average price of treatments.
The value of the UK cosmetic surgery market in the UK is estimated to rise to £3.6bn by 2015, while it is estimated that nonsur
According to WhatClinic.com, pricing for facial rejuvenation laser treatment can start from £131 for laser skin tightening up to a £3,780 for four sessions of laser skin resurfacing at one Londonbased clinic.
Its CEO Caelen King is urging patients to research their practitioner and not be swayed by special offers or timesensitive pricing. She said a good question to ask practitioners was how many patients they had performed a treatment on and how often they did the treatment.
The Information Commissioner’s Office (ICO) is warning doctor employers about the importance of making sure temporary staff who regularly handle personal information receive adequate data protection training.
It said the problem was highlighted following four data breaches at the Great Ormond Street Hospital for Children NHS Trust. All occurred between 28
January 2012 and 18 June 2013 and were caused by letters being sent to the wrong address. The letters included information about the treatment of five patients.
The ICO’s investigation found that three of the incidents related to the work of temporary staff who had not received adequate data protection training, despite their role involving the handling of personal information. The trust also
had no measures to check whether letters were being addressed to the correct recipient before sending.
ICO enforcement group manager Sally Anne Poole said: ‘This time of year often coincides with a rise in the number of temporary workers being employed across the UK. However, the temporary nature of their employment doesn’t absolve employers of their legal responsibilities for making
sure people’s information is being looked after correctly.
‘If organisations are employing temporary or agency workers into positions that involve the handling and sending out of personal information, then they must make sure these staff have received adequate data protection training.’ Great Ormond Street was required to sign an undertaking with the ICO to improve its practices.

Three specialists have got together to transform an old railway station house into private medical consulting rooms in a prime spot on a major route to Belfast. Consultants Mr Sean McGovern (emergency medicine), Dr Brian Mangan (psychiatry) and Mr Niall Eames (spinal surgery) realised the building’s potential for them as Musgrave House Associates when it came on the market in 2012. Their centre boasts modern conference facilities, described as ‘excellent’ by Dr Martin Shields, director of postgraduate medical education in Northern Ireland. A wide range of courses are planned.
Mr McGovern told Independent Practitioner Today: ‘The vision was of a quality private medical facility for consultants and patients
offering state of the art medical consulting rooms with office facilities for medical secretaries in a building which could also accommodate educational facilities.’
Dr Mangan called it ‘a great site’ for patients and consultants because it was close to the main northsouth railway line, Belfast City George Best airport, the motorway and bus routes.
Mr McGovern said it had been a huge undertaking, but they were very proud of the finished article.
He added: ‘The house offers a beautiful reception area with modern fully equipped consulting rooms and offices upstairs for consultants to house secretarial staff. Disabled access and parking is excellent with on site parking for staff and patients as well.’
Prof Roger Williams, consultant physician and joint clinical director of The London Clinic Liver Centre, has been awarded the ‘Distinguished Achievement Award’ by the American Association of Liver Diseases. His career in hepatology began in 1959 when he was appointed as
Lecturer in Medicine at the Royal Free Hospital by the late Prof Dame Sheila Sherlock. He worked at King’s College London from 1966 to 1996, where he established the Institute of Liver Studies and served as its first director. In 1968, he was involved in the UK’s first liver transplant.
By Robin Stride
Independent practitioners claim Care Quality Commission (CQC) plans for registration fee increases are unfair compared to proposed charges for colleagues in the NHS.
The Independent Doctors Federation (IDF) says although the watchdog claims to be fair and consistent and to promote equality, there is ‘clear financial bias and discrimination against doctors working outside the NHS’.
According to the group, whose membership has just broken 1,200, it has seen no evidence to support differential fee structures.
The IDF noted that, taking into account the current charges and a proposed 2.5% fee increase across all providers, the fee structure is disproportionally geared against independent medical providers.
It said: ‘We have noted that as from 2014, the proposed fee for an independent medical provider at one location will be £1,540 compared with £565 for an NHS GP practice in one location with up to 5,000 patients.’
The IDF objections, in a formal
response to the CQC’s fees consultation document, are:
NHS GPs are independent contractors who provide services to the NHS. They are no different to independent doctors in nonNHS practices;
NHS practices are larger and more complex than non NHS practices, so will be more expensive to inspect and regulate. The IDF does not accept that the CQC does not yet know if it will cost more or take longer to inspect a larger establishment;
Most independent medical practices are not dissimilar to dental practices – they are generally in one location and may or may not grant practising privileges compared to the dental provider with a number of chairs. Yet dental practices are charged far less.
A CQC spokesman told Independent Practitioner Today: ‘We are encouraging as many people to put their views as possible. We try our best to listen to comments that come in and where possible modify our approaches.’
The CQC’s verdict is expected in March.
A new website being launched as we went to press – www.theconsultantforum.co.uk – is offering registration and a basic listing free of charge to all UKbased consultants working privately.
Director Gillian Zahir told Independent Practitioner Today the online directory would give consultants an independent platform to publish their private practice details for patients and GPs.
By Robin Stride
Consultants starting in private practice, or considering it, have been promised a new series of seminars in 2014 to help them make the most of their business.
The Medical Defence Union pledged to continue giving independent practitioners support following the success of a conference featuring wide-ranging advice from orthopaedic surgeon Mr Rob Ashford.
In a ‘warts ’n’ all’ talk, he pinpointed a number of reasons why doctors might decide against becoming independent practitioners. He said private practice could mean hassle on a number of fronts and, with so much pressure on their time, they might want to spend more with a young family.
Another big consideration now was the ongoing Competition Commission investigation into private healthcare, which was likely to result in huge changes for consultants and private hospitals.
Mr Ashford told the MDU ‘Setting Up In Private Practice’ seminar, organised in association with Healthcare Performance Ltd: ‘There are likely to be huge implications with this. If you haven’t established a private practice, it’s something worth keeping a close eye on.’
But there were good reasons to enter private practice too, as well
as income generation. Practitioners could benefit from different surroundings, new challenges and meeting different people. And everything was less rushed. Everyone else around them might be doing it and there could be pressure to go private from patients too.
His advice for those taking the plunge was to ensure there was a clear difference between their
NHS and private work. And he believed this extended to secretaries: ‘If you use the same secretary and the same environment, you are likely to run into trouble.’.
Mr Ashford, who practises in Leicester, said getting theatre time could be difficult, particularly at the beginning. He advised that with patients having access to more information in future, then
the independent practitioner’s choice of secretarial support is one of their most important decisions, said Mr Ashford. ‘the success of your business is down to them as well as you.’
Billing can be very stressful. it is complex, time-consuming and better done by somebody else – but not your private hospital.
check what your private hospitals and other promoters of your profile are actually saying about you on their websites. ‘Strange things’ can happen.
Have at least one website page saying who you are and where you are. ‘these days, you should probably put your fees on it.’
Do be nice to people behind the scenes in your private hospital, such as bookings. if you are not, then don’t expect those patients who are looking for a particular specialty doctor to be sent in your direction.
if you are doing GP visits or seminars, then find out first what it is they want to know about.
Be flexible on patients’ availability times. For example, be prepared to see just one patient in the evening if they cannot do it another time.
if you employ people, then be sure to keep everything above board.
it may be difficult to get operating time when you start out, but if you bring in work, then hospitals will want to give you better slots.
Get accountancy advice before you start. Ask colleagues whom they use. you need somebody with medical experience.
the outcomes of the work would be more important.
Doctors should identify their strengths and market them, but they should always remember they were now running a business and if they did not grasp that, then they would struggle. Billing properly was vital or they would not get paid.
As well as the well-known personal attributes of affability, ability and availability, independent practitioners now needed adaptability. But Mr Ashford, who has been in private practice for six years, warned doctors to stick to what they knew and not to be tempted to take on work they did not do in the health service.
If something went wrong, they would get ‘crucified’ by lawyers and colleagues, and lose goodwill. It was wise to take a considered approach to advice from colleagues and patients. Doctors would respect the consultant who sent someone on for treatment by a colleague. Consultants might even reciprocate.
He said doctors should make sure they were seen to be open and honest about their private work by putting it in their NHS job plan, even if it was an evening commitment.
And they would need to ensure they had got cover for their patients when they were going away.
A new 30-bed hospital opened by Nuffield Health in Bristol says it will be a centre of excellence for minimally invasive keyhole surgery and the first fully digital hospital in the South-west.
Opened on the former Chesterfield site in Clifton Village, the hospital represents a £20m investment, has created 50 new jobs and offers three digital operating theatres plus a diagnostic centre including MRI, CT,
digital mammography and high-definition endoscopy.
Treatments on offer include orthopaedics, neurospinal surgery, sports injury, weight loss surgery, endoscopy, cosmetic surgery, ENT, urology, pain management and dentistry.
The Grade II listed Georgian villa which fronts the hospital site was home to Nuffield Health’s first hospital in Bristol from 1961.


BMI Beardwood Hospital, Blackburn, hit a high note when singer and actress Linda Nolan – part of the sibling girl group The Nolans – brought some sparkle to the launch of its new MRI and CT scanning centre.
The scanners are part of the hospital’s £2.3m scheme to revamp its imaging and diagnostic centre and reduce diagnosis and treatment times.
Hospital bosses said the investment at the new imaging centre was made possible through a joint partnership with Alliance Medical. Executive director Sam Sheehan said: ‘The investment being made at the hospital will improve the patient pathway, speeding up the time between consultation, scan and diagnosis.’
David Loasby, business development director at Alliance Medical, said the company was delighted to be working with BMI The Beardwood Hospital to bring a much needed service to Lancashire and Cumbria.
‘Patients needing vital cardiac scans will no longer have to travel outside the area for a diagnosis, so it really helps in caring for the community,’ he said.
By Robin Stride
An independent practitioner has confessed surprise that she must conform to National Minimum Wage policies if she employs staff.
She told an MDU ‘Setting up in private practice’ seminar she thought she could pay what she wanted because, after all, she was the boss.
But advisers and other doctors at the meeting informed her that she would have to comply with the National Minimum Wage rules.
The misunderstanding surfaced as HM Revenue and Customs warned of tough action against employers following the cases of 2,400 care sector workers who are in line for nearly £340,000 in back-pay as a result of tax probes.
In the last two years, HMRC has investigated 224 employers in the sector. Some investigations are ongoing, but 88 cases have been found to be non-compliant.
These investigations identified nearly £340,000 in arrears for more than 2,400 workers and also over £110,000 in penalties to employers for breaking the law.
Employment Relations Minister Jo Swinson said: ‘Anyone entitled to the National Minimum Wage should receive it. Paying anything less than this is illegal and unacceptable. Government will take tough action on employers who break the law, as we can see through HMRC’s investigation into the care sector.
‘As well as financial penalties, employers who don’t play by the rules can be publically named and shamed and may even be prosecuted.’
Richard Summersgill, director for local compliance at HMRC, said: ‘Our investigations found that the reasons for not paying the legal wage varied from unpaid working time spent training or travelling between care appointments to making deductions from workers’ pay that brought their pay below the minimum wage.’
On 1 October 2013, the adult minimum wage rate increased by 12p to £6.31 an hour and for 18to 20-year-olds it rose by 5p to £5.03 an hour.
www.gov.uk/national-minimum-wage-rates
Radium-233 dichloride, a new radiotherapy treatment that treats the later stages of prostate cancer, is now available at The London Clinic.
Ashley Richmond, chief medical physicist at the hospital, said: ‘The demand for this treatment will be huge, due to the fact this is the first time a drug has offered the possibility of prolonged life expectancy for patients with such developed cancer, as opposed to the pain relief drugs currently on offer.’
Consultant oncologist Dr Stephen Mangar said improvement in the overall survival and quality of life with little side-effects, combined with the drug’s ease of administration, meant the treatment would be an attractive option for those chosing not to, or unable to have, systemic chemotherapy.
‘I believe this treatment will make a significant difference to the lives of many patients with prostate cancer and will form a valuable addition in the treatments and techniques available to medical staff at The London Clinic,’ he said.
BMI The Blackheath Hospital is spending £3.8m on modernising its theatre department and upgrading critical care provision.
It said the two-phase upgrade would improve facilities for consultants and clinical teams, while also increasing the level of complex care and procedures available to patients.
Phase one will deliver a new theatre department with a six-bed recovery unit, nursing station and upgrades to the hospital’s three theatres.
The development will also improve the theatre department’s staff areas, including offices,

changing rooms, corridors and a rest room. The infrastructure and support for the air handling units, which filter air coming into the operating theatres, and the medical
gas infrastructure will be upgraded. Two specialist orthopaedic theatres, which have air supplied through an ultra-clean ventilation system, will also be improved.
Accountant Susan Hutter shows how bigger private practices can ensure their ‘back-office’ procedures cope with the new methods of doing business
The working life of a specialist has changed over the last five years and many more are now working as part of a team and running fully fledged businesses.
Some have also broadened the scope of their business to include complementary therapists and online shops.
Are standard procedures in place?
if your administrative procedures are not keeping pace with the growth in the business, then you are likely to encounter serious problems, particularly in the areas of ‘patient’ service and finances, leading to cash flow issues.
You will need to look at all your standard procedures and update them where necessary. This includes:
Staff structuring;
how you use your professional accountants;
The trading vehicle – for example, should you incorporate or at least trade as a limited liability partnership (LLP);
e nsuring that your practice software keeps up with reporting and accounting requirements;
ensuring that your practice has a robust cash flow.
Don’t cut corners on recruiting your support team
Your in-house team is crucial and it is important to have strong personal assistant/secretarial back up. You may need more than one employee in this category
depending on the size of your business.
You will also need to look at your in-house accounting staff. Depending on the number of transactions that need to be processed, you may need a full-time book-keeper.
if not, you can start with a parttimer, who can attend on a weekly, monthly or quarterly basis. You will also need to ensure that the employees work together as a team to see that invoices are raised correctly – and on a timely basis – and that outstanding money is chased.
All businesses need to take control of their cash flow – and doctors are no exception. Be aware of when the business liabilities are going to arise so that you can manage your cash accordingly.
You do not need to have a complex system for this. Usually, it is sufficient to have a monthly bank reconciliation and then a simple spreadsheet showing the approximate liabilities, together with payment dates over, say the next six months or 12 months.
You will need to plan for such items as:
Corporation tax or personal tax if you trade as an LLP or sole trader;
PAYe on staff and directors’ salaries;
Payment of suppliers and freelancers.
in order to plan the above, you will need to be able to make some estimate of income on a monthly basis. The forecast is usually best based on the previous year, unless your business has expanded or contracted materially since then.
The document should be updated on a monthly basis, when you have more accurate figures.
Keep on top of all money owed to the business

Shortfalls and slow payment can be a problem. You will need to review your agreements with all the main suppliers.
i t is recommended that you have procedures in place regarding your schedule of fees, particularly to ensure that your invoicing is in line with the published schedules, using the correct insurance company’s code for each procedure or operation.
A uniform policy is the best way forward so that all employees are certain of the procedures. This should make debt collection quicker and easier and also ensure that any disputes are dealt with in the most efficient manner.
i f different specialists within the practice have different procedures, this can prove divisive and confusing for staff.
For those private consultants or gPs who still remain in the more ‘traditional mould’, it is still crucial to have good back-office procedures.
You will probably not require
the complexity that is necessary for a larger business, but it is important that you keep up to date and ensure that your accounting procedures and practice software can cope.
You may have a PA who can cope with all the book-keeping. o therwise consider taking on a part-time book-keeper who, once again, can work with your PA to ensure that your practice runs efficiently.
i n many cases, your external accountant can provide advice in this connection and it is worth looking at this to make sure that your practice is running smoothly and the patient-facing side is all you need to worry about.
Susan Hutter (right) is a partner with Shelley Stock Hutter LLP. She provides specialist accounting, taxation and business advice to the medical and healthcare industry

















Recording, editing and sending dictation files from your phone
The Olympus Dictation Delivery Service (ODDS)
EFFICIENT Dictate on the go, download, network or email your files back for typing
OPTIMISING Attach photos to your audio files for increased data accuracy
SECURE File encryption for maximum security
EASY Easy-to-use touch screen control for intuitive operation
For further information please email dictation@olympus.co.uk or visit www.olympus.co.uk/voice
Pioneer Prof Graham Hughes is calling for a new screening programme for women who miscarry.
It’s 30 years since Graham Hughes’s ‘eureka moment’: the day he discovered ‘sticky blood’ syndrome – a condition subsequently named after him, the Hughes syndrome.
Prof Graham Hughes, director of the London Lupus Centre at London Bridge Hospital, has helped revolutionise care for lupus patients over three decades, but in this anniversary year, he’s calling for automatic screening for women who miscarry.
Hughes s yndrome, an autoimmune condition which affects the blood and its ability to clot, is now in all the medical text books and if you Google it, you’ll find there’s more than 16,000 articles on the condition.
Prof Hughes, a pioneer in the modern treatment of lupus, set up the country’s first dedicated lupus clinic in 1971 at Hammersmith Hospital and, for many years, he has been recognised as one of the world’s leading authorities on this potentially devastating autoimmune condition.
He practises at the London Lupus Centre, where he works with seven other consultant physicians who all trained with him at s t t homas’ Hospital, and all specialise in lupus.
‘Patients tell us when they come here that they’ve finally reached a place where their condition is understood,’ says the professor. ‘the team have helped transform lupus from a dreaded, often fatal, disease to one where patients can look forward to living a normal life.’
The Hughes syndrome story
Prof Hughes, a consultant rheumatologist, is famous for his discovery of ‘sticky blood syndrome’ in
1983. realising that an overactive immune system produces antiphospholipid antibodies (aPL) which causes the blood to clot too quickly both in the veins and the arteries, Hughes identified a new medical syndrome.
the clotting can affect any vein, artery or organ in the body and the consequences may include potentially fatal conditions such as heart attacks, strokes and deep vein thrombosis (DVt).
In pregnancy, the antibodies can cause miscarriage, preeclampsia, small babies and still birth. a lthough Hughes s yndrome can be present in lupus, it can also exist independently on its own.
‘subsequently, we have discovered Hughes syndrome is probably more common than lupus and it has even wider implications for health,’explains Prof Hughes.
‘For example, oneinfive DVt cases test positive for Hughes syndrome, as do oneinfive cases of stroke in the under 45s, and oneinfive women with recurrent miscarriage.
‘Hughes syndrome is also internationally recognised as the commonest treatable cause of recurrent miscarriage.’

Eureka moment
Prof Hughes had his eureka moment when he was sent out to Jamaica for a year ‘on loan’ from the Hammersmith Hospital in the mid 1970s. With colleagues, he began to investigate female lupus patients, particularly those who had neurological symptoms.
‘It didn’t take us long to focus on Jamaican neuropathy, a devastating spinal cord paralysis affecting young women – the cause of this was subsequently found to be a virus – many of whom were to become wheelchair bound,’ he recalls.
‘We analysed their blood and found they had antibodies to

Thrombosis in a vein in the arm caused by ‘sticky blood’
phospholipids – these are delicate sausage skinlike structures which surround cells and platelets. In normal blood, platelets swim like salmon without touching, as they are negatively charged. But if you have aPL antibodies, the surfaces of platelets are damaged and they become sticky and clot.’
On his return to London, Prof Hughes began investigating more subsets of lupus patients. ‘In no time at all, a very clear picture had built up: this was a distinct syndrome – frequent in lupus and yet distinct from lupus,’ he remembers. In the late autumn of 1983, the team published their research in the British Medical Journal and the Lancet
‘We didn’t get much of a reaction at first – lots of people didn’t believe it,’ says Prof Hughes. ‘But, over the next two years, we published more on the other features of the syndrome, which included recurrent foetal loss, kidney thrombosis, stroke, liver thrombosis, chorea ( s t Vitus’s dance), low platelets, pulmonary hypertension, migraine, epilepsy, heart valve disease and even dementia.
‘In summary, we described a complex bloodclotting syndrome which clearly had the capacity to affect any organ in the body.
‘Just as when the petrol mix in a car is too rich, the car stutters, so in the human body “sticky blood” limits the supply of vital oxygen to any and every organ in the body.’
The human stories
Prof Hughes and his team have won many accolades for their research, including the International League a gainst r heumatism’s prize, but what matters most to him are the patients he has helped with treatment.
Blood platelets: their surfaces are damaged in patients with Hughes Syndrome due to the presence of aPL antibodies

t hey include the paralysed woman in a wheelchair – wrongly believed to have multiple sclerosis – now diagnosed with Hughes syndrome and being treated with the bloodthinning drug warfarin and living a normal life, and the patient who suffered ten miscarriages, but is now the mother of two healthy children. then there’s the teacher whose memory loss was wrongly attributed to depression, who was only
correctly diagnosed after she suffered a stroke – her brain returned to normal when anticoagulant treatment was started.
so what of the future?
Prof Hughes says the care of lupus has been transformed over the last 30 years mainly due to the introduction of newer diagnostic blood tests – ‘a real breakthrough’ – and also the introduction of more effective treatments, includ
ing lower dose steroids with far fewer sideeffects and the newer targeted biologic drugs which attack Bcells.
‘there are many more of these drugs on the way, which is good news,’ Prof Hughes says. ‘For lupus patients, this has made a huge difference; old high dose steroid treatments meant weight gain, infertility and hair loss and other unpleasant side effects. Now they can live normal lives.
‘In the past, women with lupus were advised not to have children – but now, thanks to the discovery of Hughes syndrome and anticoagulant therapies, these women can have healthy babies.
‘We can also help prevent strokes and damage to internal organs and other potentially fatal complications if patients are diagnosed early enough and given the right treatment.
‘the challenge that lies ahead is spreading greater awareness of both lupus and Hughes syndrome – women are still waiting too long for a diagnosis, sometimes more than two years. there’s so much we can do if these patients are diagnosed in the early days.
‘I also think that all women who have suffered a miscarriage should be screened for Hughes syndrome – it could save so much heartache.’
go to www.londonlupuscentre.co.uk If not, please join us for one of our FREE tax and NHS pension seminars.
DATE:
VENUE: TIME:
Tuesday 14 January or Thursday 16 January 2014
Royal Society of Medicine, 1 Wimpole Street, London, W1G 0AE 18:15 for 18:30
To register contact Nena Blake on 020 8457 1812 or email medical@mninsure.com. Places are limited so book early.


Although J A nu A ry is traditionally a month to look forward to the year ahead, we are also spending some time at the Association of Independent healthcare organisations (AIho) reflecting on what we achieved during 2013 and how our work is preparing us for 2014.
As I have been in the role for a year now, it also seems like the right moment to consider what we have achieved together so far, and what we need to do in the coming 12 months.
AIho’s goal is to widen understanding of how independent healthcare providers contribute to improving the nation’s health.
We want to challenge perceptions about independent healthcare and the role it plays in this country.
our membership encompasses a range of independent healthcare institutions, so we have a very broad view of how we can complement the work of the nh S and deliver healthcare for everyone.
We decided to discontinue the use of the ‘Private h ospitals Alliance’ name early in 2013 because we wanted to accurately reflect the breadth of our membership, and we devised the AIho brand as a better replacement.
We also merged with the Independent h ealthcare Advisory Services (IhAS) in April and, as a united organisation, we are now able to represent the industry more fully.
We have been working hard to raise the profile of the independent sector and give it a voice in the media, in g overnment and

across the broader healthcare sector this year. that has involved building up relationships across a variety of outlets and increasing our visibility with stakeholders through our attendance at all three party conferences in the autumn last year.
We are also looking to inform decision makers across the healthcare sector in order to help them understand the contribution that independent healthcare plays. And we intend to continue this profile raising and engagement work into 2014 and beyond.
As part of that work, we plan to have a formal launch event in 2014. We will be inviting a range of stakeholders including government, nhS, commentators, regulators, patient groups, journalists and others who have an interest in the healthcare debate in this country.
We will also substantially redevelop our website to reflect our goals and our membership. We want to become a powerful voice for the sector among these communities, and ensure they understand how our members contribute not only to delivering healthcare, but to the economy more broadly – both in terms of investment and growth.

We also want to showcase some of the excellent research and development work being done by the sector – research which becomes the newest and best treatments for a broad base of patients.
to that end, we are in the initial stages of exploring a partnership with Itn Productions to create an hour long news programme on the independent sector.
As we continue to raise our public profile, we will look to inform opinion in the lead up to the 2015 general election.
We want to make sure the independent sector is represented as the main parties start to prepare their manifestos, and we want to feed into the thinking around healthcare policy for the period of the next government.
We will also continue to engage in issues which we have been working on. We want to continue alleviating pressure on the nhS, especially as the population ages, and diseases such as diabetes become more prevalent.
We can do this both in partnership with the nhS and through private provision, and we want to ensure the public understand our critical role.
to do that, it is crucial that we challenge perceptions about our place in the healthcare system, and ensure that the broader pub lic understand the role that we play in shortening waiting lists and providing high quality, safe care at a cost defined by the nhS.
We will continue to support the sector as the Competition Commission looks to conclude its findings on the private healthcare market come April.
We strongly believe that, through price transparency and the provision of appropriate data, we can help patients make the right choices about their health care.
We will continue our partner ship with the Private healthcare Information n etwork (P h I n ) to raise awareness of the outcomes data being published by the sector as a whole.
2013 was a very busy year at AIho, and we are satisfied with what we achieved.
now we are looking forward to broadening and deepening rela tionships throughout 2014, rais ing the profile of the sector and further engaging in the ongoing debate about care delivery in the future.

Consultants and GPs in private practice are well known for their inventiveness to improve patients’ lives. But how do you take those ideas to the wider world without others claiming your idea is their own? The answer is to get a patent. Kate Lees explains when your invention may – or may not –be patentable
Patents have been around for centuries to encourage innovation and reward inventors.
the grant of a patent provides a monopoly for a limited time period – generally 20 years – in exchange for the publication of details of the invention. t his information is then readily available and can be freely used following expiry of the monopoly.
Despite the fact that patents have always been available in the modern world, they remain a mystery to a large proportion of professionals and the public.

Many inventors – and indeed businesses – have, at most, a brief knowledge of the patent system, placing them in a weak position when it comes to protecting any new or improved products or processes.

been made available to the public by any means anywhere in the world;
Involve an inventive step – is not an obvious modification of what has been done before; Be capable of industrial application.
t he healthcare industry provides a huge source of potentially patentable material, with many doctors and surgeons arriving at an invention after seeking and researching a solution to a problem they have encountered during patient care.
It is important to know what to do in these circumstances to
ensure that their invention is adequately protected. so which inventions are patentable and how do you obtain one?
Are all inventions patentable?
a wide range of inventions are patentable. to be so, the invention must:
Be novel – meaning it has not
Products, such as orthopaedic devices, surgical instruments, dosage regimes and compositions may be patentable, as may improved processes for manufacturing a product, novel uses for a known product, such as a drug, and kits containing several items that may be used together.
But some inventions may fall within one of a number of exclusions from patentability. t he most relevant exclusions to the medical industry are as follows:
➱ p16
Book your place at the UK’s largest medical aesthetics meeting today.
Aesthetics is one of the fastest growing medical sectors in the UK today. Sales of aesthetic treatments totalled £2.3 billion in 2010 and are forecast to rise to £3.6 billion by 2015. However, it is estimated that only 15% of demand is being met.
Designed by leaders in the field of medical aesthetics, The Aesthetic Conference and Exhibition 2014 offers a comprehensive programme combining business and academia addressing the key topics relevant to all professionals interested in the practice of aesthetic medicine.
The two-day event also includes FREE exhibition access, showcasing leading suppliers and service providers, workshops and live demonstrations.

Visit ACE 2014 and find out how your practice can benefit from providing medical aesthetic services.
• Free exhibition entry
• Learn from leading industry experts
• Dedicated Business Track workshop programme
• Gain CPD accredited education (Up to 24 points available)
• Engage in workshops and live demonstrations





• Evening Question Time with a panel of leading experts

8th-9th MARCH 2014
THE BUSINESS DESIGN CENTRE, LONDON




Inventions contrary to ‘ordre public’ or morality;
Plant or animal varieties or essentially biological processes for the production of plants or animals – although this provision does not apply to microbiological processes or the products thereof;
Methods for the treatment of the human or animal body by surgery or therapy and diagnostic methods practised on the human or animal body – although this provision does not apply to products, in particular substances or compositions, for use in any of these methods.
Clearly, these exclusions particularly apply to healthcare inventions. however, while methods of treatment may be excluded, the products for use in these methods are not.
t herefore, what at first sight appears to severely limit an inventor’s ability to obtain a patent in this field is not, in fact, the case. so, while a method for surgically joining two organs together may be excluded, the surgical stapling apparatus for implementing that procedure may be patentable.
interpretation required the boundaries set by the above exclusions require interpretation using available guidelines, directives and case law. It is therefore always appropriate to seek professional advice as to whether a new invention may fall within the exceptions to patentability.
For example, certain subject matter is considered to fall within the ‘contrary to morality’ exception, such as cloning human beings or the use of human embryos for industrial or commercial purposes.
h owever, an element isolated from the human body, such as Dna, may constitute a patentable invention provided that a plausible industrial application is disclosed for that isolated element.
Methods of treatment by surgery have also been interpreted differently over the years. In recent years, the european Patents Office’s enlarged Board of appeal has held that methods which were ‘neither clearly suitable nor potentially suitable for maintaining or restoring the health, the physical integrity, or the physical well-being of human beings or

While methods of medical treatment are excluded from getting a patent, products for use in these methods are not
What at first sight appears to severely limit an inventor’s ability to obtain a patent in this field is not, in fact, the case
animals’ fell outside the legal exclusion. therefore, ‘cosmetic’ surgeries may be patentable. although they may involve a non-intentional physical intervention which may be regarded as a surgical operation, they are not ‘potentially suitable for maintaining or restoring the health, physical integrity, or physical well-being of a person or animal’.
In contrast, methods relating to breast enlargement or nose reconstructions which were meant to restore the physical integrity of the body following, for example, breast cancer or a car accident, were held to be non-patentable.
so the invention may be patentable, what then?
The invention must remain secret until the filing of a patent application if you are to obtain a valid patent
invention into effect and to cover all envisaged variations.
t his will also enhance any searching that is carried out prior to filing to assess the novelty of the invention.
a patent application can be filed in the inventor’s home territory that will provide provisional worldwide protection for a 12month priority period.
the pending application is generally subject to a search and examination procedure over a number of years prior to any patent being granted. If protection is required outside of the inventor’s home territory, it is necessary to submit separate national applications before the expiry of the priority period.

Crucially, the invention must remain secret until the filing of a patent application if you are to obtain a valid patent. s o it is important to seek professional advice early in the development of an invention prior to any public disclosure, including any testing of the device or publication in a trade journal.
a full and frank disclosure should be provided to the professional representative to ensure a patent application contains enough information to put the

Be aware, however, that some regional patent systems exist, such as in europe, and it is possible to file an international application to delay the major expense of filing in numerous separate territories until 30 months from the original filing date.
next time: patent litigation – 10 tips for private doctors
Kate Lees (left), an expert in intellectual property law including medical, chemical and biochemical inventions, is European patent attorney Harrison Clark Rickerbys
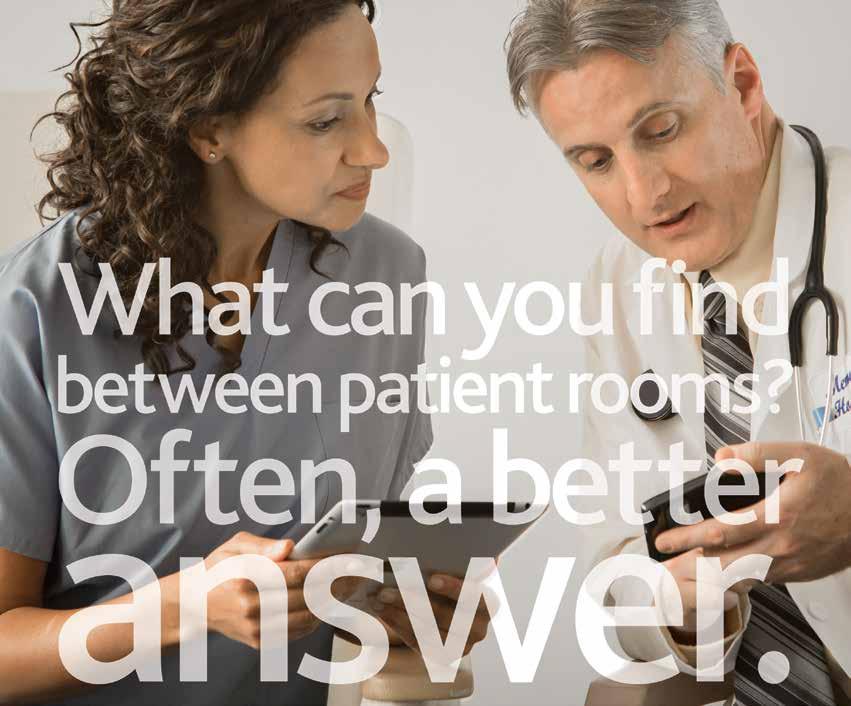
To learn more or to subscribe risk-free, visit learn.uptodate.com/UKanswer Or call 1-888-525-1299 (US and Canada) or +1-781-392-2000 (all other countries).
Patients don’t just expect you to have all the right answers. They expect you to have them right now. Fortunately, there’s UpToDate, the only reliable clinical resource that anticipates your questions, then helps you find accurate answers quickly – often in the time it takes to go from one patient to another. Over 700,000 clinicians worldwide rely on UpToDate for FAST clinical answers they trust. Shouldn’t you? Join your colleagues and subscribe to UpToDate risk-free today!


It is vaunted by some as the cheap, easy and effective answer to all our marketing woes, and dismissed by others as a time-wasting, hard-to-measure approach to building patient loyalty. In his series looking at the different media and communications options open to independent practitioners, Steve Bustin turns the spotlight on social media
S O c I al med I a is inescapable these days. Newspapers and broadcasters are regularly referencing Twitter as a news source.
Shop windows exhort us to ‘like’ highstreet brands on social networks. Teenagers are abandoning email in favour of online chat and no performance seems to be ‘live’ until it’s been snapped or videoed and shared online.
Twitter, Facebook and the like are now firmly embedded in people’s lives and are an intrinsic part of the online experience for many people, to a point where if they can’t find you on social media, they’ll assume you don’t exist or you’ve gone out of business.
Not having a social media presence is now akin to saying you don’t have a website, which is unthinkable to any growing business (see feature on page 26).
There are two usual comments I hear from doctors when talking to them about social media. The first is that ‘my patients don’t use it –it’s only for teenagers’.
But did you know that the fastest growing audience group on Facebook is middleaged women? many parents and even grandparents are now using social media to communicate with their teenage and grownup children.
If you think your patients don’t use social media, have you actually asked them? You might be surprised.
The other comment I often hear from practitioners is that ‘it’s just people telling me what they had for breakfast’ and so they see no relevance to their practice marketing strategy.
people open up
There is certainly a lot of ‘noise’ on social media and a very few strange people who insist on discussing and even photographing their latest meal – and imagine the openings that offers if you’re a nutritionist. But the majority of people are using social media to engage; to discuss and to share important aspects of their lives –such as their health – as well as the seemingly trivial.
One of the upsides of this is that it means people are very open on social media, sometimes too much so, which also makes them receptive, and this is where it can be useful to businesses looking to reach new patients.
Having said that, let’s get one thing clear: social media platforms such as Twitter and Facebook are not sales environments. People will ‘unfollow’ you very
quickly if they think they’re being sold to.
Social media platforms such as Twitter and Facebook are not sales environments. People will ‘unfollow’ you very quickly if they think they’re being sold to
Rather than seeing it as one big advert, you should view social media as a space for engaging, sharing and even generosity, not sales messages. Think of it as building a relationship and rapport, just as you do when you have a patient in front of you.
Before you get to the stage of engaging with other users, however, you’ve got to get yourself set up. I strongly suggest you aim to use one or two social networks well, rather than spread yourself too thinly across multiple networks. The most popular and – for most businesses – successful are Facebook and Twitter.
The process of setting up a profile is straightforward: just go to the homepage and simply follow the instructions. But it’s worth taking the time to complete your profile fully, upload an image –ideally a person rather than a logo, as people prefer to connect to other people rather than brands – and find a user name that will be instantly recognisable as you to other users.
Once you’re up and running, however, you’ve got to have something to say – so what can you tweet/post/update about?
The trick is to come up with a good mix of posts that reflects all aspects of your expertise and also your practice and its offerings. Have you just had a great meeting, been to a conference or seen a new product?
Talk about how what you’ve just seen or heard could potentially benefit your patients. Seen something in the paper that you thought was spot on – or vehe➱ p20

“MidexPro thinks like a doctor, not a computer expert”
All you need to run your private practice including document management, diary, clinical data, even test ordering and lab reports from TDL.
From paper billing (incl. VAT) to electronic billing (EDI) to management of bulk purchase contracts.
Grow seamlessly from a small solo practice through to a large group practice, remote access network system.
MidexPro is the cost effective practice management system with support second to none.
Free download of the full working package (30 day limited) from www.midexpro.com or call for a CD.
Try it for yourself with no sales pressure.
“MidexPro has revolutionised our lives; it is just so easy”
0845 505 0369
www.midexpro.com
sales@midexpro.com
mently disagreed with? Post a link to it and ask your followers what they think.
Just got a new qualification, taken on a new practitioner or started offering a new treatment? They’re all good topics for posts –although just as statements, not sales messages – as are comments about relevant TV programmes or celebrities, links to your blog posts or images of you or your practice, but not patients.
The more interesting, varied and relevant your postings are, the quicker you’ll start picking up followers on Twitter or ‘likes’ on Facebook.
Engage – don’t broadcast
One of the most common mistakes is to only ever post links to your blog or only ever plug your latest piece of kit, which comes across as dull and selfobsessed.
The maxim I encourage people to follow is ‘engage – don’t broadcast’, by which I mean you should set out to encourage and foster dialogue with people – whether they’re patients or not – as it’s an opportunity to prove you are (a) an expert and (b) an approachable human being.
The best way to engage is to ask a question. This could be as simple as ‘I’ve just blogged about an important topic – what’s your view?’ or ‘did you see dr X interviewed on This Morning earlier today? What did you think?’ ask people for their top tips on relevant health topics and, if necessary, use this as an opportunity to bust some myths that may come up. Or ask for their questions to you on a certain topic –
How about filming some short videos of you answering some of the frequently asked questions you get from patients?
although avoid getting into a situation where you are dealing with individuals’ problems and basically diagnosing or consulting online.
Keep it general, as this will keep it relevant to the widest number of people and keep you on the right side of any patient confidentiality issues.
On the topic of confidentiality and your responsibilities as a medic using social media, I can’t urge you strongly enough to read the G mc guidelines on http:// tinyurl.com/d3zkwcl and to make sure you follow common sense on what you do and don’t post, especially around sales messages and promotions and information about patients. It should also be needless to say, but alcohol and social media don’t mix.
images and video

a nother way of making your social media presence more engaging is to use ‘rich content’: more than just text and links in your posts. Images and video are popular and regularly and easily shared, so how about filming some short videos of you answering some of the frequently asked questions you get from patients? They don’t need to be huge production numbers; a smartphone is fine initially, and when posted on YouTube – itself now the secondlargest search engine in the world – not only does it give you great content to share on social media, it will help boost your search engine rankings, too. a lot of practitioners tell me they don’t have time to add social
The more interesting, varied and relevant your postings are, the quicker you’ll start picking up followers on Twitter or ‘likes’ on Facebook
Quarter page vertical 137 x93


Facebook pages are driving to your website. a sk new patients how they heard of you and make sure social media is added as an option to new patient forms. don’t, however, get too hungup on numbers of followers or ‘likes’. e ven though your competitor may have thousands of followers, it’s all about quality not quantity. Better to have a couple of hundred really engaged followers who are potential new or repeat patients than thousands who really couldn’t care less about your latest treatments and who just followed you because you followed them.
Want to get started but not sure who to follow? Find me on Twitter at @medmediaTrain and say hello. I’ll be happy to answer any queries you may have.
Steve Bustin (left) is founder of Medical Media Training, which offers training courses in PR skills, media, presentation skills and social media



Today are attracted by our ability to reach 13,000 doctors with a private practice and their managers/administrators every month. But now the whole world can see your advert 24 hours a day, every day of the year when you advertise on our website.
Email Margaret Floate at margifloate@btinternet.com or phone her on 01483 824094 www.independent-practitioner-today.co.uk


OccasiOnal and sessiOnal cOnsulting ROOms
Monday to Friday 9am to 9pm
Saturday and Sunday 9am to 5.30pm FLEXIBLE, COST-EFFECTIVE, FULLY AIR-CONDITIONED
CONSULTING ROOM SOLUTIONS
SERVICED SUITES AVAILABLE
HIGH-SPEED WIRELESS INTERNET
PERSONALISED TELEPHONE ANSWERING AND VOICEMAIL
FULL SECRETARIAL SUPPORT
telephone 020 7467 8301
email: info@tenharleystreet.co.uk www.tenharleystreet.co.uk
Social media and Twitter use among plastic surgeons, in particular, is on the rise. Reza Nassab reports on a recent survey while Tingy Simoes has some timely advice

Social media, such as Facebook and Twitter, has become increasingly more popular. a survey of 500 american Society of Plastics Surgeons’ members has revealed that just over half used social media.
This study highlighted some positive and negative feedback about social media use in clinical practice which is summarised in the box on the right.
Twitter is a social media network that allows users to ‘tweet’ messages of 140 characters that are then visible to their followers and the public, unless you decide to keep your messages private. a staggering 500m tweets are sent daily.
We reviewed Twitter use among plastic surgeons and cosmetic surgery clinics in the UK. our study revealed 53 plastic surgeons that were BaPRaS (British association of Plastic, Reconstructive and a esth etic Surgeons) or B aa PS (British association of aesthetic Plastic Surgeons) members and ten major clinic groups.
The plastic surgeons had significantly fewer followers and tweeted less frequently than the clinics. all of the clinics utilised Twitter for marketing purposes, compared to 60% of plastic surgeons. all clinics were using Twitter on a regular basis, while 40% of plastic surgeons had not tweeted in the last three months.
o ur study revealed that 25% of plastic surgeons and 50% of clinics used Twitter to interact with patients. clinics were also significantly more likely to use Twitter to promote discounts on their services, with half utilising their tweets in this manner compared to only 2% of plastic surgeons.
i n fact, UK plastic surgeons have been late to adopt Twitter with the exception of a few early trend-setters. clinics are already actively using this platform for their marketing campaigns.
The US survey has shown potential benefits of social media, but using it may also have some negative consequences.
Below we review some useful tips for those considering developing their social media presence. in march 2013, the Gmc produced some guidance for doctors’ use of social media.1 Some recom-
This study highlighted some positive and negative feedback about social media use in clinical practice
Increased exposure of practice
Low-cost means of advertising New referrals
Effective as a patient educator
Improved efficiency with patient communication
Positive patient feedback on social media sites

Negative patient feedback
Time spent on social media away from patient care
Unwanted solicitations from advertisers
Compromise of patient privacy
Cost
mendations include creating separate accounts for personal and professional use.
it is important to monitor your social media presence and be aware of your online image. and it is crucial to maintain patient confidentiality at all costs. if there is contact with patients, then maintain appropriate boundaries.

Twitter etiquette
Research from 2011 shows that nine out of ten doctors in the US use social media for personal purposes. online physician communities came up as the most popular sites, followed by l inked i n, with Facebook and Twitter trailing behind. (See www. ➱ p24


Your sterile single-use solution, without compromise
+44 (0)1792 797910 www.dtrmedical.com
Whether you choose to participate in social media or not, you probably have a presence there already or are being talked about, even if you’re not aware of it
ama-assn.org/amednews/ 2011/09/26/bil20926.htm).
i t would be absurd to ignore these possible and very direct channels of communication. They can function as tremendous PR tools and enhance your credibility and make you – your practice, clinic or hospital – seem connected, interactive and responsive.
There are guidelines about doctors and social media regarding the separation of their personal and professional lives and we entreat you to follow those official, common-sense guidance.
There are published policies by the US2 and British medical associations,3 but the general gist is:
maintain patient confidentiality at all costs;
m onitor your own internet presence and be aware of your online image;
if there is contact with patients, maintain appropriate boundaries;
Keep personal and professional profiles separate;
libel laws apply in either case. Twitter, Facebook’s younger, ‘cooler’ and rather more anarchic sibling, should be cautiously treated like an ongoing, water cooler-side conversation which you can dip in and dip out of. it does allow you to connect with people from areas you find of interest: from celebrities and sports figures to industry peers and relevant organisations.

You can’t ignore it
The web as a whole terrifies many doctors and that’s no surprise. But it’s worth repeating the marketing adage: if you do not seek to position yourself, the public and your competitors will do it for you. Whether you choose to participate in social media or not, you probably have a presence there already or are being talked about, even if you’re not aware of it. There are thousands of review sites and forums where – whether you like it or not – you, your clinic or services will be discussed.
Just because you’re not on Twitter and Facebook, doesn’t mean you’re not on Twitter and Facebook, if you get our drift. Use them and linkedin, if it is appropriate with your brand image. every point of contact reflects on your brand – whether it’s your

Make it part of your routine. One of the main complaints of doctors who don’t want to engage in social media is ‘they don’t have the time’. Incorporate it into your daily schedule
Make liberal use of the mobile apps. Facebook, Twitter and Linked In are all available on your smartphone
The key word here is engagement. Constantly posting special offers and discounts without conversing with people will simply make you look like a spammer
Personalise and brand each of your sites. Use your logo or even better a photo of yourself; don’t just leave the anonymous Twitter ‘egg’ logo!
Monitor your sites. Empty pages and feeds are magnets for spammers who will post their own competitions or inappropriate messages
Respond to people. If someone comes to you with a question or an observation, interact with them. Otherwise they’ll think your practice or clinic may be equally unresponsive. If the comment is negative, thank them for their feedback and offer to tackle the issue
Don’t criticise peers. This should be obvious! There’s no such thing as ‘deleting’ something entirely from the Internet
Don’t re-tweet or re-publish others’ negative statements. By posting them, you are as responsible for what is being said as the person saying it
Don’t get overwhelmed. There are free (yes, free!) tools that will help you manage your social media presence and post to Linked In, Facebook and Twitter, such as HootSuite and TweetDeck.
linkedin profile, your website or even the front door of your premises. ensure all elements are in line with the image you wish to project.
We are not going to lie here; social media can be, on occasion, one big, nasty school playground where bullies abound. But to stress the point about media as a whole: you cannot ignore its existence and power.
dealing with negativity
i f you manage these feeds efficiently, negative experiences should be extremely rare. a courteous response and an offer of help via phone or email make you look good and detractors are the ones that could appear rude.
While we are speaking of negativity, we can’t ignore internet trolls: people who post inflammatory, inappropriate or even outright insulting or devious comments on webpages, forums and discussions. Their objective is mainly to cause disruption. The best way to deal with them is with one courteous reply before leaving well alone.
These people thrive on negativity, so don’t allow them the opportunity of engaging you in a public spat. in a similar vein, disgruntled patients may feel the need to post negative experiences for the world to see.
d on’t be tempted to criticise peers: this should be obvious.
There’s no such thing as ‘deleting’ something entirely from the internet, and that also applies for retweets and re-publishing. don’t re-tweet or re-publish others’ negative statements. By posting them, you are equally responsible for what is being said. and, finally, don’t foget to have fun with it. The thing about social media is it’s meant to be less formal. i t’s about conversations –how else could you find yourself chatting with a magazine editor in the UK, a company chief executive in australia and a Hollywood movie star all over the course of a ten-minute break or cab ride?
1. www.gmc-uk.org/guidance/ethical_ guidance/21186.asp
2. www.ama-assn.org/ama/pub/ physician-resources/medical-ethics/ code-medical-ethics/opinion9124.page
3. www.bma.org.uk/-/media/Files/PDFs/ Practical advice at work/Ethics/ socialmediaguidance.pdf
Co-written by Dr Reza Nassab, plastic surgery registrar and author of Applying MBA Knowledge and Skills to Healthcare , and Tingy Simoes, managing director of Wavelength Marketing Communications and author of How to Cut it in the Media: A PR Manual for Plastic Surgeons and Professionals in Cosmetic Medicine


www.medbc.co.uk
Come and join the hundreds of other consultants that use MBC and experience the following benefits:
• Bad debts of less than 0.5%
• Increase in net income by up to 25%
• Freedom for the consultant and secretary to just focus on the medical side of the practice
• 24/7 access on line for both your financial and practice management data
• Having a service tailored to your needs with your own Account Manager
To Celebrate our 20th consecutive year of growth we are, for a limited time offering all new clients an Introductory Discount of up to 20%*
For further information:
Please visit www.medbc.co.uk and fill in the form quoting 2020 or call: Garry Chapman on 01494 763999 for a free, no obligation chat in order to establish how we may assist your practice.

With the Competition Commission’s provisional findings into the private healthcare market last year recommending private doctors’ fees should be displayed on websites, there is no time like the present to get your business online if you have not done so already.
Independent Practitioner Today’s head of design, Jonathan Anstee, explains why the smart way forward now is to think ‘real world’ when planning your website

Whatever the final outcome of the Competition Commission’s investigation into private healthcare, the bottom line is that if you don’t already have a website, then you surely now need one in 2014.
Think of it as an opportunity. While it might initially seem like a headache and an expense, this really could be a great marketing opportunity for you.
It will give your business an identity that can find its footing in the marketplace. No matter how niche your specialty, the chances are you will get – or already have – competition. You need to stand out from the others. This is your opportunity to be seen and remembered.
The primary purpose of your website is to engage potential customers.
The challenge you have is that those customers do not tend to hang around long. Research from Microsoft Reasearch shows that the first ten seconds when a customer lands on your page are crucial to their decision to stay and explore.
The key for you in designing your website is to stand fully in your customers’ shoes and imagine what they would want to know about you. Do not think from your perspective. Think from theirs.
There is often a big difference between what you might want to tell them about, as a passionate independent practitioner and an expert in your field, and what they want to find out.
Start by thinking how your website might be experienced by a potential patient. What meets and greets them when they ‘walk in the door’? What impressions might they get?
Remember, you have ten seconds to persuade them to stay and take a longer look around.
Think of your future website like a shop front. It is an online place to communicate what you do and who you are; a place to do business. You might think of it as your practice in the clouds.
what do they want to know?
They want to know who you are, what you do and how you can help them. They want to feel safe and reassured that you are professional and get results.
Put a lot of thought into the images you use on your website. Don’t use cheesy pictures like the one on the right.
The photographic portrait below is less formal, yet more interesting and engaging than the usual passport mugshot.


The key for you in designing your website is to stand fully in your customers’ shoes and imagine what they would want to know about you
The colours and imagery will either enhance or detract from the customer experience. Humans think in pictures. Visuals and information graphics can capture what we would use hundreds of words to express.
And videos are a great way to describe services and can show the customer experience in ways that capture imagination and provide reassurance.
Stock photos and traditional images portray conventionality. If your practice is innovative, you want it to look and feel fresh. Try images with an edge, something unconventional. To use a well known corporate metaphor, ‘think outside the box’.
Much like the pictures you might choose for your real life practice, think carefully about the images used on your site.
friendly greeting, clear and well written information and an explicit menu pointing to other pages on the site.
Think of your services and ‘about’ page as your consulting room. It’s the place where the visitor can find out more detail on what you do and how you can help them. Case studies and testimonials with real clients will create a storyboard and a great impression for them.
An ‘about’ page might have a biography listing your professional achievements and qualifications, professional organisations you are a member of and bodies you belong to.
Using cheesy, poor-quality images on your site will give a negative, shabby impression to your visitor – as might a faded, tasteless picture hanging on your clinic’s wall.
If your potential customer stays on your site/s and decides to click through to the other pages, you want to ensure that the journey is smooth and flows in a natural continuum for them.
The structure and navigation of your site should be easy and logical, because users quickly make decisions to stay or leave a page.
It is important that the website is not unnecessarily complicated and has a simple yet effective navigation system.
The reception
As your page loads, think of it as a door opening. What’s inside?
You’ll have a home page: a front-facing first stop where visitors get an initial impression of you and your work as they would standing in a reception area.
Visitors will want to be greeted, to find generic information and then get a grasp of the navigation of the site. Give directions to where they need to go in your ‘practice in the clouds’.
So plan your home page as you would your reception. Have a
It might also provide an insight into your life outside your profession. Let them know your personal interests and achievements. Climbing Mount Kilimanjaro or running the London marathon might have little do with your skills as a consultant, but it will command the respect and interest of your visitors.
An information or resources page can be thought of as an online library. You might store a collection of PDFs, links to articles, papers you have written – anything relevant and useful that adds weight and credibility. You might have a collection of medical images or diagrams for potential patients to refer to.
The ‘contact’ page
A contact page with a form to fill in is your online receptionist, taking messages and passing on details. It’s important to let clients know what your response times are so that they are confident in your customer focus.
Thinking ‘real world’ when planning your website should help to make the planning and implementing more fun. What’s great is that you won’t need an architect, a builder, a plumber or a carpenter. All you need is a web designer who will listen to your ideas, and make your practice in the clouds a reality.
Jonathan Anstee is a freelance graphic designer whose Surrey-based business is called AnsteeCreative
Dear Reader,
Subscribing to Independent Practitioner Today is the only way you can be sure you will see every issue. Don’t risk missing out. Our personal subscription for doctors and managers is only £60 a year and £200 for organisations. But you can reduce these figures to just £50 (only £30 after tax for higher-rate payers) and £175 respectively if you pay by direct debit. So take advantage of this offer now for this unique business magazine dedicated to supporting you in your private practice. We’re confident your subscription will repay itself many times over!
Editorial director
Instructions to your Bank or Building Society to pay Direct Debits Name and full address of your bank/Building Society
a cheque


Name(s) of account holders
Branch sort code Account No
banks and building Societies may not accept direct debit instructions for some types of account
post your application (no postage required – uK only) to: independent practitioner today Subscriptions dept., FreepoSt, po box 36, plymouth, pL1 1br
Banks and Building Societies may not accept Direct Debit instructions for some types of account To: The Manager Bank/Building Society Address Postcode Ref. No. (Do
Please post to: Proact Ltd Subscriptions Dept., 12 Mary Seacole Road, The Millfields, PLYMOUTH
subscribe online at www.independent-practitioner-today.co.uk if you want to pay by card

copy of your letter to us.
Consultants working in the NHS’s private patient units (PPUs) are wondering what the Competition Commission’s private healthcare market investigation is going to mean for them. Philip Housden thinks it could be good news
Is the Competition Commission’s ongoing investigation into private healthcare going to be an irrelevance, a threat or an opportunity for private patient units (PPUs)?
the Nhs in england is a minority supplier of privately funded healthcare services, but with increasing market share.
the health and social Care Act 2012 that removed the private patient income cap on Nhs facilities in e ngland has enabled expansion of Nhs PPUs. And the new commercial freedoms are already having an impact, as private patient income across Nhs hospitals rose by 2% from £482m in 2011 to £504m in 2012, with a further 10% rise forecast for the next 12 months.
On one level, the Competition Commission’s private healthcare industry review has little relevance to the N hs t he issues reviewed and disagreements exposed are, in my view, principally an in house fraternal fallout between the five major insurers and the five principal hospital operators over who has most power in the value chain. t he Department of h ealth claims that private revenues approaching £500m would be less than 0.5% of the Nhs budget for
201314. the ‘closed shop’ of private healthcare in england would appear to go on as now in parallel with the 99%+ of Nhs core business, also unaffected.
But the wider picture is of a private healthcare industry with longterm challenges related to the affordability of private insurance and the rising costs of provision in a low growth economy.
the increasing demands of care quality regulators require investment and better performance management in an ageing private hospital estate portfolio. s o if action by the commission squeezes out the excess profits of £173£193m a year from operators, then the sector becomes less attractive for private equity investors.

our front page in September
t he commission’s review is a reminder that healthcare insurers and private hospitals are essentially in a symbiotic relationship – each has fundamentally required the other’s geographical and service coverage to have an offering to patients. A shift in the industry dynamic, as envisaged by the commission, therefore poses major commercial risks for insurers and hospital operators alike. ➱ p30
Private hospitals have long since worked to derisk their core insurance funded business by having ‘top up’ N hs activity. the programme of independent sector treatment centres has been replaced with ‘Choice’ referrals that now make up around 25% of all discharges in some groups. Further, Nhs trusts still outsource activity to their local private hospital to help with capacity and access challenges.
By contrast, health insurers have been generally slower to stimulate Nhs PPUs to offer alternatives to private hospitals. Not all N hs trusts provide private patient care, and of those that do, far from all are recognised by the major insurers.
t he commission’s competitive assess ment of hospitals’ catchment areas has found that there is a real deterrent to new entrants in
the setting up of a PPu requires relatively little additional capital, as the PPu can leverage economies of scale out of the host trust estate
most markets, and this is the necessity of incurring high levels of sunk capital costs. the significant capital costs of building and equipping a full service hospital means that many local markets are only large enough to support a small number of efficientlysized hospitals. this, of course, is why the Nhs has a long term trend towards centralising secondary care on fewer, larger campuses. t he setting up – or refreshing – of a PPU requires relatively little additional capital, as the PPU can leverage economies of scale out of the host trust estate. this places trusts in an advantageous position to offer increased local competition.
More N hs trusts are viewing investing in private patient provision as a way of raising revenue to subsidise their core public provision of care.
Most, but not all, PPUs remain managed in house rather than licensed to a partner, but the higher the ambition of the trust and the greater the costs of capital for a newbuild, the more likely a trust is to seek a partner.
As PPUs are co located with Nhs hospitals and have access to their infrastructure and support facilities, partnering with a trust may offer a low risk means of market entry for private hospital operators.
the commission proposes that the owner of a private hospital in a lowcompetition catchment – a socalled single or duopoly area –would be barred from partnering with an Nhs trust to operate a PPU. this may well impact on highprofile recent examples such as at UCL and Guy’s and st thomas’, both partnerships with hCA. Will this reduce the likelihood of new PPUs? Probably not, as either a commercial case stacks up
No up-front fees
Unlike other debt companies, we only work for doctors and allied health professionals.
Invoice recovery, using a sensitive and collaborative approach. Professional reputation maintained.
Medico-legal invoice collection included.
Full legal service available.




or it doesn’t. It’s clearly a commercial risk for a private hospital operator to invest in a joint venture with a trust, but this can be mitigated by length of contract, the treatment of the rewards over the contract life and whether the hospital chain is the funding source.
Alongside this, the majority of trusts have the potential to enable enhanced internal ‘armslength’ commercial entities within their own organisations without recourse to a formal long term partnership with a third party. the creation and maintenance of a vibrant, empowered inhouse PPU management team – often supplemented by specialist consultancy support – has been the route followed by the majority of the highearning Nhs trusts. the evidence is that it is these trusts that are driving higher than average PPU growth, according to health market analysts LaingBuisson.
this scrutiny of the private hospital market is a further opportunity for trusts
pricing
the commission’s analysis demonstrated to its satisfaction that there is a causal relationship between selfpay prices and local competition, with private hospital operators, on average, charging higher prices where they face less competition to both insurance firms and to selfpay patients.
t he potential decoupling of national pricing contracts between insurers and hospital chains in favour of more local agreements should lead to a review and freeing up of access to insurance company networks.
Recognition within insurers’ networks has been a challenge for PPUs, even if offering attractive tariffs. this is an opportunity for PPUs to gain market share in return for robust governance, improved customer service quality and better value pricing.
s imilarly, PPUs can usually charge lower self pay prices

than incumbent private hospital operators.
so, this scrutiny of the private hospital market is a further opportunity for trusts, particularly as access times remain strained and commissioners increasingly revise referral criteria and treatment thresholds.
Warrington and halton, southampton, Chelsea and Westminster and James Paget, are just some of the trusts reported to be offering self funding patients the treatment at standard Nhs prices. taken together, perhaps it is the Nhs, largely unmentioned in the Competition Commission’s Private healthcare Market Review’s provisional findings, that could be the main winner from the proposed remedies, if enacted.
Philip Housden (left) is a director of Housden Group management consultancy specialising in commercial support across the healthcare sector
An independent firm offering one to one meetings anywhere in the UK giving advice and help with:
• how to start in private practice
• how to maximise private practice income
• ways to reduce tax payments
• setting up in Chambers/Groups
• limited companies and LLP’s
• financial planning
• record keeping

• computer software
• tax and financial advice re: car purchases
• pensions: NHS, personal and employee schemes
• purchase of consulting rooms and surgeries
• inheritance tax and capital gains tax planning
• VAT
For more information please contact us by:
Phone: 01625 527351
Fax: 01625 539315 Harley Street
Phone: 020 7307 8759
Fax: 01625 539315
Email: info@sandisoneasson.co.uk
Website: www.sandisoneasson.co.uk
In 2014, your private practice business has the chance to benefit like never before from the ‘magic of multiple doorways’. Surgeon Dev Lall shows how
Many consultants are very dubious of the whole ‘marketing thing’. their suspicions reside at many levels, from simple unfamiliarity to fear of looking unprofessional.
s ome are worried about what their colleagues might think. all these fears are understandable. I once thought the same way.
the key thing, though, is to get over your preconceptions and the stigma of the term ‘marketing’ and look through to the underlying reality. a fter all, what does
marketing mean? simply connecting the people in need of your services with your expertise. that’s it.
In my monthly series of Independent Practitioner Today articles, I have talked about some of the very many different ways to bring patients in to your private practice.
now I suggest it’s time to make a new year’s resolution to pull all these strands together and show how you can use this information to build a stunningly successful practice.
The traditional model up until recently, perhaps five to ten years ago, the traditional model for running a private medical practice looked something like in figure 2 in the box on the right.
t he ‘doorways’ patients could enter a consultant’s private practice were:
Via their GP;
Via a referral from a consultant colleague;
after stumbling upon the consultant’s web page by chance on the website of the local private hospital;
Depending upon specialty, patients might get referred from certain paramedical specialties –such as optometrists to ophthalmologists or physiotherapists to orthopaedic surgeons.
and that was about it. a maximum of four doorways and usually less than three.

t hat model was effective, but inefficient and slow. It was a product of its time. a nd times have changed. n ow look at the 21st century model of private practice in 2014 in figure 1 on the right.
this illustrates just some – 29 in fact – of the very many doorways it is possible to construct to allow
patients in to your private practice. some of these – such as PR, media presence and print advertising – existed before the dawn of the internet but were very seldom used by consultants.
Many others are a function of the internet and their use has only recently entered the mainstream, such as video advertising on youtube.
any and all of these doorways will be of value in growing any type of private medical practice – or any other business, for that matter.
However, the relative importance of each of these will vary with specialty. s o, for example, social media and blogging can work very well in orthopaedics, but forum posts and print advertising work better for allergies, paediatrics, gynaecology and plastic surgery.
t he reasons for this are pretty clear when you consider the demographics of the people you are trying to target for conditions relevant to those specialties, of course. and joint ventures work very well for almost all specialties – you just have to ask yourself the question: Who else sees patients that I would like to see too?
t here are obvious overlaps between rheumatologists and orthopods, for example, or care of the elderly/diabetologists and ophthalmologists.
t he box overleaf summarises the pros and cons of the two approaches to running a private practice.
your perceived pre-eminence and celebrity
Everyone likes to deal with an expert, but even more than that, people like to rub shoulders with celebrity. yet expertise in the eyes of the patients comes not from academic qualifications or tute
lage under former royal college presidents; rather, it comes from being found in many places.
s o if when people search for information about c rohn’s disease, your name comes up everywhere, that makes you the expert, even in the absence of a teaching hospital post or any relevant research papers.
s imilarly, seeing your name, photo or videos come up repeatedly on the internet or in the media makes you a celebrity in the eye of the public and this further increases your attraction to patients.


Pros cons
TraDiTionaL You don’t have to face the fear of marketing
moDeL
21st cenTurY rapid practice growth
slow practice growth (may be very slow)
Difficult to compete with incumbent consultants
‘Dead men’s boots’ may severely restrict practice growth for many years
Delay until practice becomes profitable
it takes work
moDeL Potential for much larger practice than Possible to get swamped with work (nice problem to have) otherwise
insurance against closure of any one ‘doorway’
Perceived pre-eminence and celebrity status in your field
ability to compete with and overtake incumbent consultants
no need to worry about ‘dead men’s boots’
Total of marketing efforts greater than the sum of its parts
now, clearly, this is all a load of nonsense, but it works very powerfully to attract patients and the wonderful thing is that it is very easy to do.
Reducing your vulnerability to the ‘one’
If you have ‘one’ of anything, you are vulnerable. If one GP is responsible for the majority of your private referrals, suppose he or she changes his referral pattern, gets sick or retires? t hat could see a significant proportion of your private practice disappear – literally overnight.
yet if there are many doorways patients can walk through to reach you, that is less of a problem. If one or two of those doorways were to close, you would only be minimally affected.
Ability to compete with incumbent consultants o ne of the commonest complaints I get from consultants is the difficulty they have in competing with senior, more established colleagues.
t his is particularly true for newly appointed specialists, but is also true of senior specialists who have never really made much impact with their private practices and find that they cannot compete with certain of their colleagues.
once again, the benefit of having multiple doorways to your
practice is evident. the practices of senior, established clinicians almost always conform to the 20th century model, and a major reason for their success is pre-eminence in the minds of GPs who always think to refer patients privately to those consultants not others.
yet this pattern can be broken, because power no longer resides with GPs but with their patients. If a patient attends a GP’s practice asking to be referred to see you specifically, the GP will almost always comply simply to keep them happy and to get rid of them.
the trick, of course, lies in getting patients to ask for you specifically in the first place, and the way to do that is by having huge visibility when people are searching for help with conditions you treat.
a s before, if your name keeps cropping up, then they will see you as an expert and celebrity and they will want to see you in preference to someone else.
this is one of the most powerful tools at your disposal when starting out in private practice. success requires sharp elbows at the table or you will be left with the crumbs, as many, many newly appointed consultants have found out.
Effectiveness of the total marketing efforts is greater than the sum of its parts.
this is not as daft as it sounds and, once again, comes back to being found everywhere patients look, so that it is your name and your face that crops up time after time in place after place.
It is as if there is a tipping point, or critical mass after which disproportionate numbers of patients start requesting to see you compared to the marketing efforts you put in.
so how do you build a 21st century private practice?
the answer is ‘one brick at a time’. you simply cannot jump from having only three or four patient doorways to having 30, 40 or more. some are quick and easy to implement – such as PR – but others take longer and require more work.
none of these tactics is hugely difficult, but some are quite technical – such as Google and adWords. certainly, all require a willingness to learn and to overcome your reluctance and fear to implement them.
the best approach is to decide which conditions you would most like to target in the first instance. t his will reflect your expertise, interests and, of course, the profitability of looking after such patients privately.
once you have done that, you need to consider their demographics. Where may such patients be found? online or offline?
your understanding and knowledge of both the condition as well as the patients will be vitally important here, because once you can accurately describe ‘who’ you are looking for, you will be far better placed to decide how best to reach out to them.
Promoting your services on websites like mumsnet would be a good idea if you wanted to target young mothers or their children’s health problems, but probably of little value if you wanted to reach the older generation – for example, with cataract surgery. yet even this is an assumption and one worthy of testing. young mums have older parents, of course, some of whom will have cataracts…
Invariably, there will be many ways you will be able to identify that would allow you to reach your chosen target group. all you have to do is pick one way and try it out.
and once you have found one approach that is working effectively, you continue doing that in the background but also try out something else.
In this way, brick by brick, you will create multiple doorways for patients to find you and for your practice to succeed.
Dev Lall is an upper-GI surgeon and runs a specialist private practice consultancy. He is the owner and director of www.PrivatePracticeExpert.co.uk

With
the increasing cost of defence for many specialists – and more choice of provider – it is no time to be an ostrich in the medical malpractice indemnity market. Defence expert Kevin McCluskie gives a personal overview of how he sees the current arena
In november 2011, the Federation of Independent Practitioner o rganisations (FIP o ) published my report, On the Market for Medical Malpractice Indemnity, for consultants practising in the independent sector.
The document 1 set out to explain why:
medical malpractice indemnity was needed;
Its cost was dramatically rising;
Some specialties faced particular difficulties in getting cover.
It also aimed to throw light upon the differences between the traditional offering of the medical defence organisations ( m D o s) and the emerging new, discounted products, offered by the insurance industry.
In the two years since the publication of that report, there have been some significant developments which I now discuss here. but let me make it clear from the start, I believe mDos are not for everybody. Yet neither are insurers for everybody.
Doctors have seen the introduction of some innovative new products, genuine price competi
tion, and a major rethink from the m edical Defence Union ( m DU) on how it offers indemnity to its members.
costs inflation
but what has not changed is the rate of medical malpractice claims inflation. It is currently generally accepted to be approximately 10% year on year.
Some key reasons for this are:
The high cost of care packages; Courts that award damages for loss of earnings on top of pain; Suffering and loss of amenity assessments;
Patients being more willing to sue and who are supported by ‘no win, no fee’ lawyers.
There are also special features that will influence the cost of indemnity. The ministry of Justice is reviewing the ‘discount rate’ currently set at 2.5%. This rate directly impacts on damages paid as a lump sum because it is used as the multiplier applied to factor in the return on investment a claimant might achieve if his or her damages were put into low risk investment products.
If the discount rate goes down, then the lump sum needs to be higher. And if the rate goes up, it will decrease. Indemnifiers need to set aside provisions for these future losses, so any variation will have a significant effect on their reserves.
An alternative to a lump sum award is a Periodic Payment order (PP o ). This allows a court to impose a ‘rest of life’ structured payment to provide for longterm care.
PPos pass all the financial risks onto indemnifiers that a traditional lump sum would move onto a claimant, such as the risk of low investment returns on payouts and also inflation.
Also, if the patient lives longer than expected, then the burden of the extra cost falls upon the indemnifier. PPos are becoming increasing popular. At 31 march 2012, there were 1,116 PP o s against the n HS Litigation Authority.
This evidence suggests that rising claims costs will remain unabated. Therefore, the cost of buying malpractice indemnity must inevitably rise even further. but there is an alternative view.
The insurance industry accepts that any financial product will be subject to price increases, but asserts that, by dint of them entering this market, they can offer competition that will stabilise prices, if not reduce them. b y being careful in the risks they accept, they contend that they can reduce the risk of large claims.
Fundamental principles
It is important that we understand some fundamental principles on how indemnity for clinical negligence is offered and by whom. This determines the financial modelling used by an m D o or an insurance company and helps explain how the price of the indemnity is decided.
e xplained below are the key definitions and who uses mainly what.
‘Contractual indemnity’ on a ‘claims made’ basis are the terms used by insurance companies. Contractual means that there is a legally binding insurance contract in force where terms and conditions are set out in print at the outset.
‘Claims made’ means the policy in force at the time the clinician becomes aware of the (alleged) negligent procedure is the one that pays, not the policy in force when the procedure took place.
The alternative system used by the m D o s is ‘discretionary indemnity’ on a ‘claims occurring’ basis. Discretionary means that when a claim is reported, the member asks his or her mDo for rights of assistance.
These rights are granted or declined at the discretion of a membership committee. There are no guarantees or legal entitlement to indemnity. ‘ Claims occurring’ means that, if a doctors was a member of an mDo at the time of an (alleged) negligent procedure, assistance can be asked for any time in the future, regardless when the claim is reported.










HMRC tax investigations and disputes create difficult and stressful times.
As an award winning firm of tax experts, our highly experienced partners specialise in resolving problems relating to tax investigations and disputes with HMRC.
To find out, in confidence, how we can help call 0800 734 3333.
It is useful to understand why they adopt such different approaches. A feature of medical indemnity claims is the time lag between the date a procedure took place and the date a claim is
The mDos say this is not possible because claims are too randomly spread and even the best doctors can face an adverse event regardless of the skill employed. So who is right and what is happening? ➱ p38
‘Here
to help. Not to judge.’
actually made. negligence claims are rarely made soon after an adverse procedure.
Statistics from the m edical Protection Society (mPS) showing the period of the delay between the date the incident occurred and the date the claim is made are illustrated in the box at the bottom of this page.
This delay is called Incurred But Not Reported (Ibnr), which means inevitable claims are in the pipeline but they have not been declared to indemnifiers.
However, indemnifiers must make a provision and allocate reserves to fund these unknown claims that will eventually result in payments.
This is where the mDos and the insurance industry take radically different positions and it goes a long way to explaining why they offer their products in the way they do.
With occurrencebased indemnity offered by the m D o s, they reason that, in any one year, they can predict the total number of claims generated within that year, regardless of when they are presented to them in the future, and collect the necessary subscription accordingly.
The insurance industry used to adopt this approach but decided it was financially unsustainable and largely abandoned it in the 1980s. The occurrence based indemnity means liabilities will always remain unknown and a merely a best guess based on actuarial predictions.
This is not a financial model insurers are prepared to accept, as they are required to deal in greater certainty. Insurance companies adopt the ‘claims made’ model.
This means once a policy year is closed, then all known incidents have been declared and are therefore fully funded within the insurer’s accounts. Future Ibnr claims are still covered but will be dealt with in future policy years, as cover is triggered by the date the claim is made, not when it occurs. both systems work, but I would
argue there are pitfalls that need to be considered.
With an occurrence indemnity model used by the mDos, the predictive costs of claims has to be accurate. It must predict rates of inflation, care costs, legal trends, changes in legislation and financial climates.
Insurers say it is impossible to calculate these numbers, as there as just too many uncontrollable variable factors. If the calculations are wrong, two things must happen. Firstly, prices must rise to take account of past mistakes and, secondly, prices must rise to take account of future provisions. A doublewhammy price increase!
After retirement
one issue with ‘claims made’ contracts offered by insurance companies is what happens when you stop buying insurance policies –for example, on retirement? How is the Ibnr catered for, since, on retirement, a doctor will stop buying the insurance policy but unknown liabilities will still exist?
The solution offered is for insurers to offer an Extended Reporting Period, commonly known as a ‘run off’.
From April 2013, the MDU said it was no longer offering a contractual indemnity on subscription renewals and was reverting to offering a discretionary indemnity on an occurrence basis
This extends the period a claim can be made for many years after the final insurance policy was purchased to respond to any Ibnr issues. This period needs to reflect the risk and insurers have responded to criticism that their past offerings have been too short.
Recent changes in the market one recent significant change we have witnessed is the shift in position of the mDU and how it offers part of its indemnity.
The mDU was the biggest supporter of offering an insurance contract for clinical negligence. From 2000 to April 2013, it offered an insurance contract with a £10m indemnity limit for clinical negligence claims.
In December 2010, the m DU issued a statement responding to a Government ministerial announcement on compulsory indem nity requirements. The mDU said: ‘most patients do not realise that around 70% of doctors and 70% of dentists are not insured and rely only on discretionary indemnity.
‘This means there is no contract or a guarantee and they will only know if they are indemnified for a claim at the time they notify that claim. They have no right to an indemnity, only a right to ask. The providers of discretionary indemnity can give no guarantee and their past record in assisting doctors and dentists cannot be taken as a guide to the future.’
It went on to say: ‘You are not allowed to insure your house or your car with discretionary indemnity and it is unthinkable that discretionary indemnity remains acceptable for clinical negligence.’
However, from April 2013, the m DU ( Independent Practitioner Today, April 2013) announced a 180° aboutface. It said it was no longer offering a contractual indemnity on subscription renewals and was reverting to offering a discretionary indemnity on an occurrence basis – of which it was so critical in 2010.
Discretionary indemnity on a ‘claims occurring’ basis has been
around since the formation of the mDos. It is a system that works provided it is properly funded and there are adequate reserves to meet all future claims.
The criticism of the current mDos is that they are – save some minor affiliates – not subject to regulation by the Financial Conduct Authority (FCA), the body that regulates the insurance and banking industry in the UK.
This is important because although we know the income and the reserves of the mDos, we do not fully understand the extent of their I bnr liabilities. These figures are known to them, yet they steadfastly refuse to advise their members.
Legally, they are compliant with accounting rules, as a claim not notified is technically not a liability. but to defend this system by saying it has worked well for a 100+ years is really not good enough in the turbulent financial
environment of 2013 and the backdrop of significant medical claims inflation.
Insurers have been around for 400 years and would argue their strength lies in their transparency and the ability to adapt to changing commercial environments. Until either the m D o s come under FCA regulation or Ibnr figures are declared which are independently audited, we will never know the true financial position of the mDos.
Unlimited indemnity
o ne feature of the indemnity offered by the mDos is that the limit of indemnity – that is to say, how much they will pay out on any one claim – is, in theory, unlimited. Insurance contracts do not have this feature and they impose a limit.
So extreme care needs to be taken, as large claims are becoming more common. Insurers and
some advisers have argued that certain specialties do not need high limits of indemnity. b ut I believe such advice should be ignored.
The probability of some specialties having fewer claims is proven, but it is possible for any specialty to have a catastrophic incident. Claim values of £5m to £7m are becoming more frequent and that is at today’s valuations. Some claims are even higher.
Any significant incident notified today may well not be settled for several years. Add claims inflation into that equation and, for example, a £4m claim at today’s value will be a more likely £6m in four years’ time.
The level limit of indemnity has a direct bearing on the cost of the insurance and, in the past, there has been a temptation by some consultants to keep this limit low to – illadvisedly – save premiums.

This has been a concern to some hospital groups and so there has been the introduction of the requirement for consultants to have a minimum level of indemnity, usually £3 or £5m depending on specialty.
Such is the pressure of claims inflation, it is very probable that these limits will be raised to perhaps £10m, regardless of specialty, in the foreseeable future ( Independent Practitioner Today, november 2013).
The insurance market has anticipated this and responded to low limits of indemnity and now routinely offers limits of £10m and more if requested. Also, run off periods, that in some cases were as low as two or five years, have now been extended to ten or even 20 years and are freely available.
insurance is cheaper
In the main, insurance contracts are proving to be cheaper than discretionary indemnity even with the higher limits of indemnity. At first glance, this may seem odd, as the risk to the clinician over the course of a career is exactly the same no matter what system of indemnity is selected.
mDos say that a ‘claims made’ contract is artificially cheaper in the first few years and will increase in price over time and will, in fact, get more expensive as retirement approaches because the runoff has to be funded.
The difference is accounted for, according to the insurance companies, by how they select risk. m D o s have traditionally priced risk by banding specialties into groups – not individually. This is known as ‘population underwriting’.
The group specialty is set against an income band and a subscription is determined. o f course, some applicants have special terms imposed or are rejected, but, in percentage terms, this is low.
Conversely, insurers look at the risk by individual assessment, taking many more factors into account, and they can reject up to 20% of applicants. The net effect is that insurers claim they avoid poor risk, have fewer claims and can pass the savings onto policyholders
The m D o s say claims are too
The wrong thing consultants can do right now about clinical negligence indemnity is to bury their heads in the sand and ignore what is happening
random and any doctor, regardless of their level of expertise, can have an adverse event. b ut the current evidence seems to favour the insurances companies.
o ne insurer has claimed that, over the past five years, its premiums have remained the same and, in some instances, it has actually reduced premiums with the introduction of noclaim discounts.
Compared to a steady increase on membership subscriptions from the mDos, that represents a considerable saving.
mDos say they are tightening up their underwriting criterion, which, to me, appears contrary to their position that claims are too random and that this has little effect on total payments. To get a true picture, we perhaps need at least another five years of data. Insurers may have some of their own Ibnr claims to pay.
The biggest innovation since the FIPo report is the introduction of the medica Insure affinity scheme introduced by Spire Healthcare in April this year, for which I was an adviser. This is an insurance contract for clinical negligence offered to those 6,000 consultants who have practising privileges at Spire ( Independent Practitioner Today, november 2013).
It has a £10m limit of indemnity, 20year runoff and, as part of the package, has innovative features not found elsewhere, such as public liability and loss of reputation insurance.
The product has been supplemented with a specialist product for consultants who treat sportsmen and women. And it deals with potentially complicated contractual relationships consultants may enter into that the mDos are unwilling to offer indemnity for. by adopting stringent risk management techniques within its hospitals, Spire can demonstrate a declining claim trend. This data gives insurers an insight into Spire’s clinical quality and allows them to give extra discounts to consultants who do work at their hospitals.
It is taking the idea of risk assessment one step further by combining the risk profile of the hospital with that of the doctor. Furthermore, the risk analysis in
this scheme takes into account not only the income of the doctor but the type number of procedures undertaken, making the product truly bespoke to the individual clinician.
Spire recognises that rising indemnity costs are a threat to its business. If consultants cannot afford to buy clinical negligence cover, they cannot work in the independent sector. Some consultants have already given up independent practice due to high costs.
e qually worrying is that such costs are a barrier for new entrants. many may not want to start an independent practice where, in some cases, 100% of income is paid out on malpractice indemnity costs.
Explore, do not ignore
The wrong thing consultants can do right now about clinical negligence indemnity is to bury their heads in the sand and ignore what is happening.
We have seen more changes in the past two years than in the last 100. This issue will affect income and, perhaps for some, the affordability for them to be able to continue to practise in the independent sector.
The G m C has, I think, been wrong in not providing any form of institutional leadership or guidance on the issue. effectively it says it is the responsibility of the individual to ensure adequate indemnity is in place.
While consultants are currently seeing real competition available in the market, they need to be aware that there are pitfalls which need to be understood.
The message must be to review your current indemnity arrangements and seek professional independent advice where necessary. Like I said, mDos are not for everybody and insurers are not for everybody.

1. The report, which featured in Independent Practitioner Today’s Decem ber 2011January 2012 issue, is available at www.fipo.org.
Kevin McCluskie (left) is a chartered insurance broker, independent medical malpractice consultant and adviser




changes have affected consultants’ billing and incomes in the last five years. Garry Chapman provides a round-up and looks ahead – with a note of optimism – to 2014
2008 to 2013 was probably the most difficult period consultants have ever encountered.
They had to contend with an ever-changing landscape of the private healthcare market, a huge growth in unemployment numbers shrinking the size of the market considerably and some major changes in the way they could bill the private medical insurers (pMIs).
Depending upon the specialty and the type of practice they had, the changes implemented within the sector in conjunction with the worst recession on record reduced many doctors’ incomes between 5% and 35% with no corresponding decrease in costs.
we have seen very few consultants substantially grow their income during this time. They may well have grown their practice volume of patients, but due to fee reductions imposed upon them, they ended up doing a lot more work for the same amount of income or, in many cases, less. and where the consultant was unaware of the changing rules and continued to bill incorrectly, the risk of being derecognised by insurers grew substantially. below, I outline the major market changes affecting consultants:
This was the single biggest change, as it affected the way consultants could bill all insurance companies. rule changes starting during 2010 affected the rules regarding the way CCsD codes are used together when billing for operations.
w hat codes could be billed together was limited and, in many cases, this resulted in only being able to bill for a single code, whereas, in the past, consultants

would have been allowed to bill two or even three codes.
a n example of this is where they would have been able to bill the codes M4430 (endoscopic removal of foreign body from bladder), M4510 (diagnostic endoscopic examination of bladder) and M7920 (dilation of urethra) together. Now they could only bill for a M4430. For those billing within insurance guidelines – which most consultants do – this obviously reduced the amount of income earnable for doing the same work as before.
There are many examples of these changes and the case above represents approximately a 30% drop in income for doing the same operation. During the rest of this period, more changes were implemented affecting most, if not all, specialties.
another fundamental change was that, in 2008 and 2010, the two biggest p MIs introduced a new recognition system, meaning that any consultant wishing to see their patients had to sign a contract.
They had to agree to a fixed fee schedule as well as a fixed consultation fee, which was typically lower than what was being charged in the market. The new process meant that, irrespective of where their practice was based, they were limited to what they could charge.
Then, in early 2011, an insurer changed the way procedures could be charged at the same time as a follow-up consultation. It limited which CCsD codes could be charged in conjunction with a follow-up visit. For example, a consultant carrying out a D0702 (aural toilet) was only allowed to charge for the consultation or procedure code and not both as previously allowed.
Depending on the specialty, this also had a major impact on income. In some cases, doing the same work before the change compared to afterwards represented a 50% income reduction. The above example is one of many.
In 2010, a major pMI also started writing to consultants asking them to either reduce their consultation fees or substantiate the rationale for their pricing structure. The fee reduction requested varied and could have been anywhere between 10% and 35%.
This process has continued apace with some consultants being threatened with derecognition if they did not comply with
the suggested fee reduction. In some cases, the consultant has been derecognised.
During 2011, there were a number of different changes from multiple insurance companies where they stopped or limited the practice on what exactly could be billed in the area of diagnostic tests, pathology and procedures. one example of this was unless the practice could prove it owned the machine on which the test was carried out and had a service agreement, then some insurers would not allow it to charge for the procedure. s ome insurance companies have stopped all charges for pathology, insisting this must go through the recognised laboratory/hospital.
since January 2012, a new system for referring some patients was introduced, shifting the emphasis from the Gp to the pMI to decide whom the patient should go to see. other insurers have since followed similar schemes. Unless you are on the special designated lists of the pMIs, it is unlikely you will see patients referred to you who are on these policies.
In 2012, there was another major push to reduce the fee schedules for CCsD codes. This was particularly brutal for some specialties, as a large proportion of these cuts were for the most common codes used.
o n top of this, some of codes were restricted even further as consultants were not allowed to charge for a local anaesthetic. an example of this would have been
for the s0633 (Excision of lesion of skin or subcutaneous tissue).
These price reductions varied and were, in some cases, in excess of 50%, which meant consultants ended up doing twice the amount of work for the same income.
Examples of some of the most common codes reductions are as follows: one insurer used to allow £548 for a w8200 (arthroscopic meniscectomy), whereas now the amount has been reduced to £289. That same pMI would allow £589 for a w 8500 (multiple arthroscopic operation on knee) and now that has been cut to £335.
Keeping abreast of so many changes is extremely difficult and if you are unaware of them, you may be losing income but not understand why.
To understand the impact of all the above, the consultant needs to review where they are in terms
of their finances. If that has not been done, then the start of 2014 is certainly a sensible time to start the review.
Do your own billing review:
Establish if you are billing to the new rules and what the impact has been;
Check if your treatments are being coded correctly – not unbundling;
see if your codes are being accurately billed per insurer – follow the rules;
If your procedures have been affected, establish what the difference is per procedure;
Find out which patients owe you money you cannot collect due to incorrect billing;
o nce you know all that, you need to decide what action to take to gain control of your finances and to stop losing money.
Garry Chapman is managing director at Medical Billing and Collection
taking into account all of the changes in the private healthcare sector, it is clear consultants now work in a totally different landscape compared to 2008.
they need to embrace this and decide the best way to move their practice forward.
on a much brighter note, looking at all the economic indicators during the second half of 2013, we can see for the first time since 2008 some sustained improvement in the economy. and if this rate of growth continues, the economy may well get back to the same level it was before the recession by the end of 2014/early 2015.
the Competition Commission is due to finish its investigation into this sector during 2014, so it will be important to make sure you are aware of any changes you may have to make to your practice in order to comply with any recommendations.
as unemployment continues to drop, the number of people with PMI will continue to rise.
self-pay patients are also forecasted to grow. so consultants need to ensure they are in the best possible situation to take advantage of this growth.
that means it becomes even more vital that you know exactly what is happening on the financial side of your practice from both a billing and collection perspective.

The year just gone signalled more huge change for independent practitioners, financial concerns from different quarters, and then a welcome tonic of optimism too. Leslie Berry reports
January 2013
Doctors were offered the chance to completely escape a mounting debt plague by one firm offering a guaranteed 100% recovery of invoices raised.
Accountants estimated that independent practitioners’ businesses lost an estimated average of £28m in uncollected fees over the previous year.
Experts said billing problems were costing private doctors an estimated average 2% of due income each year.
A drop in private consultants’ incomes was reflected in record applications to pay less tax to HM Revenue and Customs (HMRC) at the end of the month.
Independent Practitioner Today – the fastest growing medical magazine – again froze its subscription rate at the level they were when we published our first edition four-and-a-half years previously.
Senior doctors were warned they would be hard hit by tax relief cuts to their pensions, under plans announced by The Chancellor of the Exchequer.
Bupa kicked off the new year with a further major restructure heralding the splitting up of its insurance arm, Bupa Health and Wellbeing, into two separate business units: Bupa Health Funding and Bupa Health Clinics.
The British Association of Aesthetic Plastic Surgeons (BAAPS) stepped up its fight against ‘cosmetic cowboys’.
Consultants were warned they must pay the taxman back thousands of pounds in expense claims following a judge’s ruling in the long-running doctor’s mileage test case. The long-awaited judgment, affecting most independent practitioners, means the miles they drive between a home office to consulting rooms or operating theatres are not allowable against tax.
As many as 4,000 private consultants were owed at least £200m in uncollected fees, according to ‘conservative’ estimates from a billing company.
Independent practitioners were advised to get individual patient consent if planning to store patient records on virtual ‘cloud’ servers.
A consultant bariatric surgeon’s operation at a private hospital was claimed to be the first in the UK to be ‘tweeted’ live.’
Independent Practitioner Today gave away two free guides to readers – a directory of companies providing goods and services to independent practitioners and private hospitals, plus a consultant’s guide to forming and running a limited liability company.
Independent Practitioner Today gave away a free mileage logbook to every subscriber to help them keep track of their legitimate expense claims and avoid unnecessary hassle with the taxman.
Meanwhile advisers to Dr Samad Samadian – the consultant at the centre of the mileage claims case with the HMRC – followed our call to appeal against the judgment. They warned it could be a year or more before a final decision.
Shocked doctors found they faced huge extra pension tax charges after breaching lower annual allowance limits in 201112. Financial planning experts said several new clients had been unaware of stringent new limits of subsequent punitive tax charges.
our landmark 50th issue
With some accountants giving doctors the wrong advice, Independent Practitioner Today launched a new website service exclusively for its subscribers to keep them fully briefed on important developments in the ongoing car mileage claims test case.
They were given the option of being notified by email when there were developments in the case that they needed to be aware of.
We urged readers to give their views to the ongoing Competition Commission inquiry into private healthcare.
Consultants and providers were promised faster payment with new ‘intelligent validation’ technology from private healthcare online solutions firm Healthcode.
The Private Hospitals Association changed its name to the Association of Independent Healthcare Organ isations and absorbed the

Independent Healthcare Advisory Services as a division. It said it would be ‘dedicated to working with the NHS to improve Britain’s healthcare’ and would now provide a single voice for independent healthcare organisations.
Private doctors in the UK were warned they risked losing out on a medical tourism boom because they were not harnessing marketing opportunities.
In a major speech delivered at a Reform meeting, Bupa’s new insurance division boss Dr Damien Marmion spelled out three key challenges he believed faced the sector:
1. A continuous challenge on quality.
2. A recognition that commissioners with healthcare expertise had both a right and a responsibility to their customers to intervene in the market to deliver better quality and value treatment.
3. A need to be much more obsessive about improving value for money for customers.
Yet another watchdog? Independent Practitioner Today hit out at a recommendation from the team investigating cosmetic cock-ups for the whole of the private healthcare sector to come under the remit of the Parlia mentary and Health Service Ombudsman. We called instead for a beefingup of the existing Independent Sector Complaints Adjudication Services (ISCAS) and said it should be left to get on with the job.
A new public website set up by the evolving Private Healthcare Information Network (PHIN) enabled patients and GPs to directly compare nearly 200 independent hospitals on a range of quality of care indicators for the first time.
PHIN, a collaboration involving almost all independent hospital operators, said it would be publishing standardised and directly comparable information drawn from records of both private and NHS treatment.
One-in-five consultants doing private practice told the BMA their independent income had risen over the last year. Meanwhile troubled times for NHS GPs sparked a new surge of would-be private practitioners.
The UK’s first ever practice management app was unveiled, promising to transform the lives of independent practitioners by enabling them to efficiently manage their practices on the move.
Developer Healthcode said it was keen to reflect the changing way independent practitioners now wanted to access its online services.
With a growing number of NHS patients being treated in private hospitals, Independent Practitioner
Today called for the sector to tackle differentiation in a high-profile way. We warned that consultants were increasingly concerned at the problem of private patients wanting to know what they were getting for their money compared to the NHS patient next to them who was paying nothing.
High-earning independent practitioners who opted out of the NHS pension were shocked to find themselves unwittingly reenrolled thanks to the Government’s new push to encourage retirement saving.
Financial planning experts warned the move could invalidate precious fixed protection on their pension savings and leave some vulnerable to huge tax penalties.
Independent Practitioner Today gave away the first of two guides – ‘100 ways to grow your private practice’.
Care Quality Commission plans to beef up its inspections in the wake of severe criticism over wellpublicised previous failings were given a cautious welcome in the independent sector.
Independent Practitioner Today said training for inspectors needed to consist of a set of basic requirements to stop doctors coming under fire to deliver different standards in different practices.
HCA NHS Ventures won the 2013 HealthInvestor award for public/private partnership of the year.
The newborn Portland Hospital, London, reported receiving growing demand for its worldclass private paediatric medicine and huge interest from a new generation of specialists wanting to work there.
We reported that no private doctor’s business could now expect to escape the outcome of the Competition Commission’s ongoing investigation into the private healthcare market.
Provisional findings from the watchdog would force specialists to consider a raft of possibilities likely to affect their future incomes and working environment, we said.
We warned of a new competitive arena: ‘Incentives from private hospitals would be banned, practitioners would be forced to give patients a written list of proposed charges before treatment, and fees would have to be displayed on websites.
‘Potentially thousands of consultants could face upheaval as their private hospitals changed ownership and information about the result of their work would be accessible for patients to compare.’
Authors of an influential industry report said consultant innovators were set to be major drivers fuelling a predicted double-digit growth in self-pay over the next few years.
Shocked consultants were hit with tax penalties of up to £50k after inadvertently busting pension fund limits for 2011-12.
Independent Doctors Federation chairman Mr Ian Mackay strongly criticised threats to the future of private hospital incentives for consultants. He said the provision of consulting rooms or secretarial services – facing a ban under current Competition Commission proposals – were actually good for clinicians and the sector.
Accountants Stanbridge Associates said profits in private practice were on the up as many independent practitioners bounced back from two difficult years.
They reported that 2013 tax returns, currently being completed for the 30 January 2014 deadline, were showing a much healthier outlook than 2011 and 2012.
Members of the Federation of Independent Practitioner Organisations quizzed defence organisation bosses face to face at a lively meeting discussing the rising costs of indemnity.
The event heard that consultants who are covered for £5m indemnity insurance are likely to come under increasing pressure to at least double this limit in order to practise in some private hospitals.
See our five-page special feature on indemnity, starting on page 36
Planning how to spend your pension tax-free lump sum might be exciting, but Patrick Convey explains why you should proceed with caution
Colle C ting your pension lump sum upon retirement is seen as the worthy reward for a long, high-pressure career.
t he lump sums are normally paid free of tax, which is an added bonus and the stand-out feature that makes pensions so attractive.
But some doctors make hasty decisions about this golden pot of cash without realising the full consequences.
o ne of the biggest challenges we face is helping doctors who seek financial advice only after they have retired. it could be your first chance to look closely at your finances or you may have been swept along with the momentum of simply ‘getting out’ of the nHS.
As such, your first action is to take the lump sum from your nHS pension and use it to start all those well-considered retirement projects unaware of the financial disadvantages of doing so.
Unintended consequences
if you have more than one pension arrangement, you should be careful about the order in which you take your benefits. it may be beneficial to look at your private pension first.
you should be wary of the lifetime allowance (ltA) – the total pension savings you can build before attracting tax. the sum of your separate pension plans will be tested against ltA, with any excess heavily taxed. the current

ltA is £1.5m, but this will fall to £1.25m in April 2014. the lump sum cap that can be paid free of tax is 25% of the ltA, so you will be able to take £312,500 as cash. the amount of lump sum you take from your n HS pension should be well considered. there are various pros and cons of drawing the standard (if part of the 1995 scheme) or mandatory (2008 scheme) lump sum as opposed to drawing a higher
amount in return for a reduced pension.
t here is no right or wrong answer here and what works for one individual may be less beneficial for another. it should be noted that you will forgo an index-linked income, paid for life, in order to draw a higher lump sum.
i f you choose to retire after April and take the full n HS lump sum amount, this may not
If you have more than one pension arrangement, you should be careful about the order in which you take your benefits. It may be beneficial to look at your private pension first
leave any allowance for private pension lump sums. However, if you take the private pension lump sum first – say £50,000 –this would still allow £262,500 to take tax-free from your nHS fund.
Private pensions can also be accessed earlier than the n HS, from age 55. Modern flexible pensions allow you to draw your lump sum without needing to purchase a pension income ‘lifetime annuity’. the best route to take will vary by individual, so seek independent advice in this area.
Where lump sums are not otherwise required, you may opt to continue generating long-term tax-efficient growth through reinvesting these monies in an iSA or investment portfolio. i f you purchase an annuity or draw other pension income from your fund, note that the income is taxable at your highest rate.
Are you over the limit?
if you are facing a tax charge after breaching the ltA – a substantial 55% if taken as lump sum – the tax payment method differs depending on whether the charge arose from your private or n HS pension.
From your private pension, the 55% tax owed is collected when you draw benefits and the fund value is reduced accordingly to pay HM revenue and Customs.
However, if you had drawn benefits from your private scheme first and then followed with the nHS pension, your tax charge will be paid by the n HS Pension Agency on your behalf.
t he money is recovered by reducing your annual indexlinked pension income over the course of your remaining lifetime.
When considering how much of lump sum to draw from your pensions, it is also worth assessing your health as you near retirement.
While we cannot predict how long we might live, if you are in poor health, it could make sense to take a greater lump sum than if you expect to live for many years to come.
you will need to live for a number of years to make leaving your lump sum in your pension fund financially worthwhile and the longer you live, the more valuable the annual index-linked income. i n all scenarios, spouses’ and dependents’ benefits need to be taken into account.
i n the lead-up to every Budget Autumn Statement and general election there is extensive speculation that pension legislation will be changed (again) and the tax-free lump sum threshold will be threatened.
e arlier last year (2013), the Pensions Policy i nstitute asked the government to consider a cap
of just £36,000 on tax-free lump sum payouts.
i t recommended imposing restrictions on anyone with a pension pot of more than £144,000, which, after the lump sum payment is made, provides annual retirement income of only around £6,000.
i n a consultation published ahead of its conference in March, the liberal Democrats argued that the current lump sum allowance of 25% could be reduced.
t his unwelcome suggestion now seems to have been replaced with an equally unappealing proposal to cut the lifetime allowance further to £1m – before the latest cuts have even come into force. e very time the ltA is reduced, the overall lump sum limit is cut by default.
t he paper cited: ‘ i f we introduced such changes, we would propose to leave reliefs at these levels for some time, to allow a
period of certainty in pension planning.’ With change after change, cut after cut – the ltA was £1.8m just two years ago – savers might question if such certainty exists.
it may seem like a good idea to jump ship before further changes occur, but it would be unwise to take action purely on the basis of speculation and you might be penalised financially for doing so. in order to safeguard your hardearned retirement funds, you need to stick to the facts, seek expert help and consider the best order to take pension benefits before making any hasty decisions.
see more on pensions in ian Tongue’s tax tips feature on page 52
Patrick Convey is technical director of Cavendish Medical, an independent financial practice helping senior consultants in private practice and the NHS
What can independent practitioners do to actively manage sickness absence at their practice?
Chris Inson (below) offers some

The Office for National Statistics report ‘Sickness Absence in the Labour Market, April 2012’ recorded that 131 million days were lost due to sickness absence or injury in 2011.
With an estimated cost to UK businesses of £12bn a year, it is easy to see why employers are so keen to manage sickness absence in the workplace.
We all know that everyone has an important role to play in a busy, thriving private medical practice, with members of staff likely to struggle even if just one colleague is absent. So clear absence policies are a must for the private doctor who employs staff.
it is a good idea to have an effective policy in place to help you apply a consistent approach to sickness absence. A clear policy will also help employees understand what attendance standards are expected of them and how to report their sickness absence.
You may wish to indicate in your policy how many sick days an employee may take before you consider dismissal, and we comment on this further below.
monitoring is another must it is important that you have an accurate picture of the level and patterns of absence in your practice. With clear records, you can adopt a consistent approach to absenteeism, which is in line with your policies.
You should take care when analysing absence data and always consider whether an employee is off sick due to a disability, which should be recorded separately.
e mployees must know who to contact at your practice if they cannot attend work – and remember to choose the point of contact wisely. This person has an important role to play in asking sensitive and discreet questions of the absent employee.
i n most situations, it will be appropriate to ask the employee the reason for their absence and when they are likely to return to work.
for this reason, you may wish to provide training to the point of contact to ensure that they obtain sufficient information from the employee to recognise any issues which may require further inquiries or follow-up action.
The Office for National Statistics recorded that the most common reason for employee absence –with over 35m days lost in 2011 –was musculoskeletal problems. This was closely followed by minor illnesses such as coughs, colds and flu, which accounted for 27.4m days lost in 2011.
An employee’s evidence of incapacity can take two forms, depending on the length of absence. if a person is absent for seven calendar days or fewer, you may require the employee to selfcertify their absence. This is essentially a signed statement from the employee providing the dates and description of the incapacity.
Where the employee is absent for longer than seven calendar days, you may insist on receiving a statutory ‘fit note’ or other reasonable
evidence. i n cases of long-term sickness, it may be necessary to refer the employee to an independent occupational health specialist.
employers are required by law to provide employees with particulars of any ‘terms and conditions relating to incapacity for work due to sickness or injury, including any provision for sick pay’. Details are usually contained in the employee’s written statement of particulars, but it is also acceptable for the particulars to refer the employee to a sickness policy or staff handbook.
if you do not provide enhanced contractual sick pay, you are obliged to pay statutory sick pay (SSP) to employees who have been absent for four or more consecutive days at a minimum weekly payment – currently £86.70. This is subject to a cap of 28 weeks.
Keeping in touch
it is easy to get caught up in the running of a practice and forget about maintaining relationships with those off sick. A careful balance should be struck between showing concern and offering support, and keeping a sufficient distance so that employees do not feel that you are being overly intrusive.
Your contracts of employment or sickness policies may specify that medical reports should be obtained once an employee is absent for a specified period of time. Six weeks is likely to be an appropriate time-scale.

it would still be appropriate for employers to request an update on the employee’s medical condition before that time.
These interviews should not be treated as a mere formality to tick off your sickness absence procedure. f or those who have been absent for a long period, these interviews can form an important part of the integration process. Where the employee has taken regular periods of short-term sick leave, interviews can be an opportunity to discuss any issues and sensitively let the employee know that their absences are being monitored.
The cause of an employee’s absence may not be immediately obvious and it is important to consider whether there is an underlying health condition or even a problem with workloads or a colleague.
Getting to the root of the problem will help you establish whether any reasonable adjustments need to be made to discharge your duties under the equality Act 2010. if an employee is disabled, you may wish to discuss with the employee what reasonable adjustments may be made to help them return to work. Reasonable adjustments can take the form of a phased return to work, varied start and finish times, alteration or re-allocation of duties or purchasing certain equipment to assist the employee.
The employer-employee relationship is governed by contract, so if the employee is unable to carry out work owing to long-term sickness absence, the contract may be incapable of continuing. in spite of this, it would be most foolish for an employer to hastily dismiss an employee without considering the situation carefully. There may be other alternatives to explore rather than dismissal on capability grounds. e mployers should consult the employee and consider seven key things when faced with an employee on long-term sick leave (see box on the right).
it is essential that full and accurate records are kept of all discussions with the employee. Should you eventually dismiss the employee, a clear paper trail showing all efforts made to consult with them will be of vital importance should a tribunal claim be made.
in summary
Sickness absence is an incredibly delicate issue which is difficult for employers to handle, but, equipped with a clear policy, employers can work through the panic of what to do next. At each stage, try to communicate with the employee as far as possible.
There are a number of issues which could potentially give rise to a claim, so it is important to gain the full picture before any hasty decisions are made.
Chris Inson is a partner in the healthcare team at commercial law firm Capital Law LLP
1 the nature of the sickness absence, supported by an expert medical report that has been provided by an independent party
2 the prospect of the employee’s medical condition improving within the foreseeable future
3
4
5
Whether the employee is incapable of carrying out their job owing to their medical condition
Whether there are any reasonable adjustments which could be made to help the employee return to work
In terms of needs and resources, whether the practice can sustain the employee’s absence
6 Whether health insurance, a pension or sick pay scheme could help the practice sustain the employee’s absence for a longer period
7 Whether a suitable alternative position is available at the practice Independent Healthcare Marketing Consultant



Business development & marketing support for Consultants & General Practitioners in private practice
Are you considering developing your practice to increase your private referrals?
Medici Marketing is an independent business development consultancy providing the following services for sole practitioners and working groups of Consultants or General practitioners:
• Project management
• Development of business models for integration of new service lines

• Management of website build and SEO optimisation
• Event management
• Customised marketing strategy
• Network facilitation
• Branding and logos
• Business planning and market analysis


For further information or to arrange an informal meeting, please contact Sue O’Gorman, at: sue@medicimarketing.co.uk or call 07985 456487

www.medicimarketing.co.uk

Dr Carol Chu (left) answers some more tricky ethical questions from independent practitioners
QAs a private GP, I yesterday attended a consultation with a young woman who is 25 weeks pregnant and has decided she can no longer continue with the pregnancy, so she requested an abortion.
I gently explained that the legal limit for a termination is 24
weeks and she stated that if I would not help her, she would have to find someone who would, otherwise she might as well end her life.
She also stated that she has a history of self-harm. I am concerned for her safety. What should I do?
AInformation for Care. Everywhere.
Crosscare is the solution




The Abortion Act 1967 allows for abortion beyond 24 weeks if ‘it is necessary to prevent grave permanent injury to the physical or mental health of the pregnant woman or where the continuance of the pregnancy would involve risk to the life of the pregnant woman, greater than if the pregnancy were terminated’. (Section 1 [b] and [c]).
The Act requires two medical practitioners to form an opinion in good faith that the termination is necessary and an abortion must be undertaken by a registered medical practitioner.
You will need to discuss all the relevant options with the woman and, as the pregnancy is relatively far advanced, you may wish to refer the patient urgently to a pregnancy counselling service or local gynaecology department. Given her history of self-harm, you may also want to consider referring her urgently for a psychiatric assessment.
If you have a conscientious objection to abortion, the GMC’s guidance Personal Belief and Medical Practice (2013) says you must tell the patient about her right to see another doctor, provide her with enough information to exercise that right, and not seek to impose your views on her. In this context, you should try to ensure she can see a colleague without delay.
This is a difficult dilemma and you may wish to seek advice from your medical defence organisa
tion.
Q
I am a psychiatrist in the process of setting up my own private practice. At the moment, I am looking into the equipment I want for my practice and am considering installing CCTV.
However, I am concerned that there may be medico-legal implications to this. For example, what do I do if the police ask me to show them CCTV footage?
AYou are right to consider the medico-legal implications of installing CCTV. Although you are probably keen to install the equipment in order to ensure the safety of your staff and patients, the use of surveillance equipment in healthcare settings can be problematic due to the need to protect patients’ confidentiality. Although the GMC has not published specific guidance on the use of CCTV, any disclosure of footage must comply with the GMC’s guidance Confidentiality (2009)
This states that personal information may be disclosed in the public interest, without consent ‘if the benefits to an individual or to society of the disclosure outweigh both the public and the patient’s interest in keeping the information confidential. You must weigh the harms that are likely to arise from non-disclosure of information against the possible harm both to the patient, and to the overall trust between doctors and patients, arising from the release of that information’ (paragraph 37).
In general, you should seek consent ‘unless it is not practicable to do so’ because it would be ‘likely

to undermine the purpose of the disclosure – for example, by prejudicing the prevention or detection of serious crime’ (paragraph 38).
You may wish to place signs around the building to alert patients to the fact that CCTV is in operation The use of surveillance equipment in healthcare settings can be problematic due to the need to protect patients’ confidentiality
If, for example, a patient had been identified on a CCTV image following a serious assault, a doctor is unlikely to be criticised for disclosing to the police that they had attended the practice – but the doctor should not provide details of their medical history or reason for their attendance.
But each disclosure decision should be considered on its own merits and it’s a good idea to check with your medical defence body.
It is also important to comply with national guidance relating to CCTV. In June 2013, the Surveillance Camera Code of Practice was released as part of the Protection of Freedoms Act 2012. The code applies to all local authorities and the police.
However, other operators and users of CCTV in England and Wales are encouraged to make a public commitment to adopt it

voluntarily. The code sets out 12 principles for CCTV operators and users to make sure that its use is necessary, proportionate and that the appropriate safeguards are in place.
These include the requirement to document the purpose of the CCTV and the need for as much transparency in its use as possible with clear rules, procedures and a designated person who is accountable for its use.
You may wish to place signs around the building to alert patients to the fact that CCTV is in operation. A policy should be
created covering the installation of cameras, safe storage of images, retention periods, disclosure to police and subject access requests.
The Government’s code is intended to be used in conjunction with the CCTV Code of Practice published by the Information Commissioner’s Office (ICO) in January 2008.
This contains detailed information on what CCTV operators must do to comply with the Data Protection Act (DPA) 1998, which applies across the whole of the UK. It explains that CCTV should be installed for a specific purpose such as the prevention or detection of a crime. Signs should be displayed warning patients.
The ICO also states that the use of CCTV should be reviewed each year.
Dr Carol Chu is a medico-legal adviser with the Medical Defence Union
welcome both Private and NHS patients NHS patients by arrangement with the relevant Trust
Upright Positional MRI, a new concept providing real benefits to patients
• Weight-bearing and variable patient positioning enables a more precise diagnosis
• Truly open system enhances patient comfort for an anxiety-free examination
For more information or to book your scan go online at: www.mri-london.com or call us on: 020 7370 6003

With the new tax year coming up fast, it is time to consider whether you need to take any action before 5 April 2014. Ian Tongue shows what to do
Many allowances are per tax year and therefore it is important for you to utilise any that are available for you and, in some cases, your spouse as well.
This article explores some of the more common areas you should be considering before the 5 april 2014 and does not form investment advice. you should discuss your individual circumstances with your professional advisers.
certain tax-efficient savings products have annual allowances. The most common example of this is the Individual savings account or Isa
I sa s come in two forms: cash only and stocks and shares Isas. The amount that can be paid into a cash Isa for the tax year ending 5 april 2014 is £5,760.
For those looking to invest in a stocks and shares Isa, the limit is double at £11,520 and this also represents the overall limit for the tax year.
a s the I sa limits are per tax -

payer, you can double up your allowances with your spouse.
o ther funds held in savings accounts should also be reviewed regularly, as promotional interest rates can often apply only for short periods reverting to a lower rate later on.
certain investments provide you with tax relief and the most common are e nterprise Investment s chemes ( e I s ), s eed e nterprise Investment s chemes ( se I s ) or Venture capital Trusts (VcT).
Under all of the above, you are putting money into an area into which the Government would like investment and so tax relief is available to encourage this.
There are limits to how much can be paid into each per year to attract tax relief and various criteria that must be met for the tax relief to be valid. If you are considering such investments, discuss matters with your accountant and independent financial adviser (IFa).
Before entering into any such schemes, you should assess the risk with your advisers to ensure that you adequately understood the trade-off between risk and reward and timing of tax relief available.
Pensions are a hot topic at the moment, both in terms of the changes imposed on members of the nHs Pension scheme and the taxing of excess contributions and exceeding lifetime allowances.
your pension position should always be reviewed by an IFa who understands the scheme as well as the pensions market as a whole.
The annual allowance represents the maximum that can be paid into pension schemes/products collectively in a year. This is currently £50,000, but will be reduced to £40,000 a year from 6 april 2014. Unused relief can be carried forward for a maximum of three years.
It is worth noting that, under
the n H s Pension s cheme, the contributions you pay are not the figure relative to the annual allowance. your additional benefits from being in the scheme another year is the starting point for the calculations, and pay increments or merit awards can make a significant difference to the calculations.
Running alongside the annual allowance is the ‘lifetime allowance’, which is the maximum capital value of pension schemes that you can have without a tax charge arising on the excess. a gain, a reduction is scheduled for 6 april 2014 when the lifetime allowance is set to fall from £1.5m to £1.25m.
For many, a detailed review of their pensions is required to allow time for any action that may be required: for example, protection of lifetime allowance.
a further discussion of the pension annual allowance and lifetime allowance was covered in the november 2013 edition of Independent Practitioner Today
For those that employ their spouse, it may be that a pension contribution can be made from your private practice to provide both tax relief on the contributions and additional pension for your spouse on retirement. you should consider your position and discuss matters with an IFa well in advance of 5 a pril 2014.
For those considering disposing of capital assets, you currently have a capital gains tax annual allowance of £10,900 for the tax year ended 5 april 2014. Depending on your circumstances and future expected capital disposals, it may be worth
this is also a possible area of tax planning that may be considered. you should discuss your individual circumstances with your accountant.
Gifts to UK registered charities are normally made under the Gift aid scheme. The advantage of this scheme is that the charity can claim some additional money and the donating taxpayer is also given additional tax relief if they are a higher-rate taxpayer.
If you are considering making donations under the scheme, it may be worth making them before 5 april 2014 to obtain tax relief at the earliest opportunity. you can also give away £3,000 a
As there are certain provisions to transfer assets between spouses without capital gains tax arising, this is also a possible area of tax planning that may be considered is per donor and not receiver. There are other exemptions available for special occasions, such as marriage and a small gifts exemption of £250 per receiver.
Inheritance tax planning is a complex area and you should seek advice before making any donations in excess of this limit
dividends are paid and, therefore, it may be beneficial to pay dividends before – or after – 5 a pril 2014 depending on your circumstances.
For those in this position, contact your accountant annually around February/March to discuss this, as they will be able to review matters and the advice may change from one year to the next.
The above covers some of the more common areas to consider in advance of the new tax year commencing on 6 april 2014. If you are considering any of the above, speak with your professional advisers before committing to anything to allow consideration of all factors.
Next time: The importance
Stop the waste with ‘PPM’ – Private Practice Manager software and get complete administrative and financial control
Our easy-to-use software provides these benefits and more:
• Full support – no question too trivial
• Templates set up to your specification
• Pre-loaded CCSD and Bupa codes, categories and fees
• Full and speedy training and installation
• Optional secure e-mail and text messaging
• Optional integration with TDL (The Doctors Laboratory)!
For the consultant:
• Reduces losses due to invoicing mistakes and aged debtors
• Provides detailed medical analyses
• Pays for itself in months
For the secretary:
• Saves hours of administration time
• Gives access to data in seconds
• Produces year-end financial analysis in minutes

t: 01992 655 940
m: 07860 525 831
e: tomhunt@ppmsoftware.com www.ppmsoftware.com

Generations of top-end VW Golfs have been among doctors’ favourite cars. Now there’s a new one. Independent Practitioner Today’s Dr Tony Rimmer puts it to the test
There are times in private practice when you get a good idea and it starts something you did not expect.
an alteration to service type or delivery becomes more successful than you imagined. It may be that others copy your good idea – but you have a head start. There is a good example of this in the car industry.
In 1975, a group of Volkswagen development engineers, in their spare time, put a larger fuelinjected engine in the recently launched Golf Mark 1 and fettled the suspension to create what was to become the Golf GTI.
The company’s management took a risk and offered it on general sale. The first hot-hatch was born.
Combining sports car performance and handling in a practical user-friendly package, it spawned
a whole new market segment that became known as the hot-hatch sector.
Sales were slow at first, but really took off with the Mark 2 Golf that firmly established the iconic GTI label.
at this point, other manufacturers like Ford and Peugeot jumped on the bandwagon and competition became fierce. as in private practice, to keep ahead and remain the best requires constant refining and updating so that you remain the standard-setter.
Lost the plot
Unfortunately, Volkswagen lost the plot with the Mark 3 and Mark 4 Golf and it was only with the arrival of the Mark 5 GTI that it regained its crown of best in class.
The Mark 6 was basically an updated Mark 5 and only now
Combining sports car performance and handling in a practical userfriendly package, it spawned a whole new market segment that became known as the hot-hatch sector
230bhp and, more importantly, adds an electronically controlled differential lock and limited slip differential to improve traction and handling. This is important in a front-wheel drive car with so much power.
with the new Mark 7 do we have a totally new chassis and body.
So can the latest Golf, appearing nearly 40 years after the original, still appeal in the same sort of way and remain the best of its type?
I have been testing what will probably be the most popular version: a five door with the optional £980 Performance pack.
This boosts the already impressive 217bhp power output to
First impressions as you approach the car leave you in no doubt that this is a Golf. VW styling has always been evolutionary rather than revolutionary and they have been accused of being boring in doing so.
The lack of outlandish body trim and spoilers also keeps the whole package visually low-key. I actually like this understated approach and I think it a major factor in the car’s success.
The interior carries this theme forward. The new higher levels of build quality and materials in the

Golf Mark 7 extend to the GTI, which also has a high level of standard equipment.
Its sports seats are very supportive and are covered by the classic GTI tartan trim to go with the golfball gear knob. The latest sat-nav system has an impressive eightinch screen and, at last, accepts full post codes. Unfortunately, it remains a pricey option.
There is plenty of room in the rear for three passengers and the spacious boot has a very convenient flat floor. The Golf is a versatile car.
On the road, the first thing that comes as a relief is the ride quality. Despite standard 18-inch wheels, the suspension copes with our rough British roads impressively. a lthough firm, it never becomes harsh and, together with the improved sound insulation, makes the GTI feel more like an executive car than a family hatch.
Optional adaptive suspension (£800) allows even greater smoothness if you choose Comfort mode. h andling is predictably superb and with new, more direct, steering the GTI can be shuffled through a set of corners with great confidence and speed.
Performance is excellent. The latest cleaner version (47mpg) of the 2.0 litre turbo has a great linear power delivery and the meaty torque band minimises the constant need to change gear.
My test car had a manual gearbox, but a twin-clutch DSG auto box is available and maintains the sporty character. There is a certain
iron fist in velvet glove feel to the GTI and I really like the confidence this inspires when driving it. The only negative might be that the exhaust note is somewhat subdued for a sports car but your passengers will appreciate the quiet.
So the new GTI is an impressive hot hatch. It may not be the fastest or most stylish among competitors, but it is the one that you could live with on a daily basis as your only form of transport. It is more expensive than rivals and my advice would be to opt for the adaptive suspension but hold back from the Performance pack unless you are going to do some track days.
h ere we have a sophisticated and understated product with a desirable image that fulfills all the requirements of a busy professional who enjoys his or her driving. It can also deliver what only a hot hatch can: when pushed, it is fun to drive.
Dr Tony Rimmer is a GP practising in Guildford, Surrey
VoLkswaGen
GoLF GTI
Body: Five-seat hatchback. Three or five doors engine: 2.0 litre turbo petrol power: 217bhp (230bhp with performance pack)
Torque: 350nm acceleration: 0-60mph in 6.4 secs
Claimed economy: (Combined) 47.1mpg on the road price: £26,500 (£980 performance pack)

To guarantee your copy of Independent practitioner Today by taking out a subscription (at the rates shown on p59), phone 01752 312140 or send off a subscription form on page 28 or email lisa@marketingcentre.co.uk or go to the ‘about’ page of our website www.independent-practitioner-today.co.uk
If you pay by direct debit, individuals pay only £50 for a subscription – just £30 after tax. Just fill in the form on page 28 and send it to the Freepost address shown at the bottom of the form.
BaCk Issues: £10 including post & packaging CHanGInG aDDRess oR suBsCRIpTIon DeTaILs? phone 01752 312140 or email lisa@marketingcentre.co.uk

Ophthalmologists
have experienced a big drop in profits. Ray Stanbridge highlights the reasons in our unique benchmarking series. Additional data from Martin Murray
Just a year back in our last review of ophthalmologists’ profits, we anticipated a ‘steady as you go’ scenario. there were positive signs in the market place and also a number of negative ones.
We were therefore surprised to find that ophthalmologists’ private practice gross incomes, on average, have shown a fall between 2011 and 2012 of about 7.5%. t hey went down from £133,000 to £115,000.
adding to the disappointment was an above-inflation rise in
expenses. they went up, on average, by 8.6% from £46,000 to £50,000.
a s a result, taxable incomes have fallen by 25% from £87,000 in 2011 to £65,000 in 2012. this is a substantial fall.
Of course, as usual we must state that our sample is not statistically significant. rather, it represents an average of what a range of ophthalmologists in private practice are achieving.
We commented last year on the problems of trying to be consist-
aveRage iNCoMe aND eXpeNDituRe oF a CoNSultaNt ophthalMologiSt With aN eStaBliSheD pRivate pRaCtiCe
ent in our analysis. t his has proved a difficulty again, as we have had to adjust data where consultants have incorporated and gone into groups.
reasons for drop
What then are the reasons for the income fall? Firstly, we are starting to see the effect of fee reductions imposed by the insurers. younger consultants have had, effectively, to sign up for lower fees than their more experienced colleagues. Older consultants have been affected too; for example, by the open referral system. secondly, it seems that, for reasons we do not know, there was a loss of self-pay patients that generally generate higher margins. thirdly, some consultants seem to have increased the amount of ‘Choose and Book’ income, which is conducted at lower unit prices.
Others, meanwhile, have clearly lost ‘Choose and Book’ work. so all in all, there has not been one overwhelming factor in affecting the results.
Costs have shown increases. s taff costs have inevitably gone up again. However, there is a correlation between family member salaries and the annual personal allowance, which has been increasing in recent years as a result of Government policy. Professional indemnity costs have increased further, as nobody can fail to realise, although there is limited evidence to suggest that the rate of increase is slowing down.
Perhaps this is because of the increasing competition in the market particularly for those consultants with outstanding claims – or rather lack of claims – records.
our income survey is restricted to those consultant ophthalmologists
who are not full-time in private practice. they:
have had at least five years’ private practice experience
are seriously interested in pursuing private practice as a business
earn at least £5,000 in the private sector
hold either an ‘old-style’ or ‘new-style’ NhS contract
May or may not be a member of a group or have incorporated





Year ending 5 April. Figures rounded to nearest £1,000 (percentage is also rounded up)
Source: Stanbridge Associates Ltd. Additional information: Sandison Easson and Co















Courses and conference costs seem to have shown a modest increase, as consultants seek more exotic destinations to conduct their learning as part of their continuing professional development. Other costs have risen too. It is now increasingly common for ophthalmologists to spend money on websites, marketing and promotion. these costs seem to be an integral part of a successful practice.
future trends so what then of the future? Our review over the years probably shows ophthalmology private practice incomes to fluctuate far
pRoFitS FoCuS iS the iNDuStRy BeNChMaRK
Doctors and their specialist medical accountants use the statistics published in our ‘profits Focus’ series to look at how their earnings compare with others and see where they can cut costs and boost their income.
Now all this information is available on our website and is free when you take out a subscription. either fill in the subscription form on page 28 or phone 01752 312140 or email lisa@marketingcentre.co.uk. get a discount by paying by direct debit.
www.independentpractitioner-today.co.uk
more than other disciplines. Much of this is the result of the ‘on-off’ approach of the NH s in dealing with eye problems.
Group practices seem to be thriving, particularly where they are adding value. those practices who are marketing well seem to be prospering.
In addition, those consultants who have linked up with major chains, such as Optegra – who undertake their own marketing –seem to have survived the problems well.
However, as the older practitioners approach retirement to be replaced by younger practitioners,
eXpeNSeS SuBSCRiptioNS/pRoFeSSioNal
we would expect a fall, on average, in incomes.
younger consultants, in all disciplines are unlikely, on average, to achieve the earnings of their older colleagues over the past few years. t he key, however, seems to be marketing and promotion. those who do well here will continue to prosper.
Ray Stanbridge runs an accountancy, finance and tax advisory service specialising in the medical profession. Martin Murray is a partner at Sandison Easson & Co, specialist medical accountants
how arE You doiNg?
use these benchmarking statistics to help you compare your financial performance with other specialists in private practice. Subscribers can check out their specialty in full at www.independentpractitioner-today.co.uk
years ending 5 april Source: Stanbridge Associates Ltd
Don’t miss the next issue of the fastest-growing medical magazine, published on 20 February. only subscribers are guaranteed to get a copy. to be sure you receive it, and all future issues of independent practitioner today, why not take out a subscription – from as little as £50 a year? you can even offset much of the cost against your tax bill! See rates at the bottom of this page and signing-up details on page 55.
Coming free with your February edition of independent practitioner today is our product guide 2014. this handy directory of companies which provide goods and services to independent practitioners will give you contacts with a wide range of experts to help you in your growing business – from accountants and tax specialists to medical products and equipments
top ten marketing questions from consultants – answered!
lots of doctors have very complicated investments. But they could be a whole lot easier, Cavendish Medical reports
With more practices now diversifying and broadening services, it is vital that you are aware of the working capital requirements in your business. See Susan hutter’s accountant’s Clinic
published by The Independent Practitioner Ltd. Independent Practitioner Today is editorially independent and thanks Bupa for its assistance with distribution.
printed by Williams press
Material is governed by copyright. No part of this publication may be reproduced, stored in a retrieval system or transmitted in any form without permission, unless for the purposes of reference and comment.
Editorial layout is the copyright of the publishers. If you wish to use it for promotional purposes on websites or for reprints, we would be happy to discuss licensing the copyright to you.
© The Independent Practitioner Ltd 2014. Registered office: 7 Lindum Terrace, Lincoln LN2 5RP
twitter.com/robinstride
Circulation figures verified by the Audit Bureau of Circulations
Write to Independent Practitioner Today PO Box 198, Cranleigh GU6 9BB
eDitoRial iNquiRieS
Robin Stride, editorial director
Email: robin@ip-today.co.uk Tel: 07909 997340
aDveRtiSiNg iNquiRieS
Margaret Floate, advertising manager. Email: margifloate@btinternet.com Tel: 01483 824094
publisher Gillian Nineham Tel: 07767 353897.
Email: gill@ip-today.co.uk
SuBSCRiptioNS
£60 private practitioners. £60 GPs and practice managers (private & NHS).
£200 organisations.
But if you pay by direct debit, individuals pay only £50, and organisations £175. Call Proact Ltd on 01752 312140. Email: lisa@marketingcentre.co.uk
inventive independent practitioner? See our top tips for challenging an infringement to your patents
Bonus schemes for staff are becoming an increasingly fashionable means of rewarding strong performance. lawyer Chris inson considers the types of schemes available and some legal pitfalls to be wary of
the growth of health screening examined
Business Dilemmas – your ethical conundrums answered
accountants Ray Stanbridge and Martin Murray check out gynaecologists’ financial performance in their monthly profits Focus
our Doctor on the Road, tony Rimmer, gets behind the wheel of a doctors’ favourite – the volvo XC70
ian tongue’s monthly series for doctors starting a private practice looks at the importance of reviewing your private practice regularly
pluS all the latest news
aDveRtiSeRS: the deadline for booking advertising for our February issue is 24 January



Healthcode’s ePractice system is designed for private practices and is tailored to the needs of your practice. It delivers high quality, cost effective, online practice management solutions, providing you with the tools to take direct control to expand your practice and spend more time on patient care. Here’s what the professional’s say...
The diary management feature on ePractice manager means I can focus on treating patients, while my PA is able to coordinate my appointments remotely across the three practice locations. Healthcode’s ePractice manager provided the e-billing facility I needed at the right price. I would be happy to recommend Healthcode and ePractice manager to any independent practitioner.
Mr Barlow-Kearsley, Founder, Total Footcare Solutions
We use Healthcode’s ePractice manager system for all our invoicing which streamlines everything for us. Roughly 75% of our invoices are submitted electronically, payments are now made much more quickly, which is good for cash-flow. We have built our business based on the simple principle of delivering excellent service. Healthcode has allowed us to maintain these high standards while giving us the capacity we need for future growth.
John Morgan, Accounts Director, Jenny Morgan Secretariat
‘Code for Success…
…Take Direct Control
Access your patient details, appointments, bills and financial status from anywhere, anytime.
…Protect Your Practice
Healthcode systems are encrypted to the same standards as online banking.
…Long Term Partner
Ensuring that you have the right tools and support to grow your business and improve cash flow.
Call us today to arrange a demo and to discuss your requirements on 01784 263 150 quoting: 34AiP.
For further information visit:
