A Publication brought to you by the members of Lower Sixth Medic, Vet and Dentist Society


A Publication brought to you by the members of Lower Sixth Medic, Vet and Dentist Society

Hello and welcome to the very first edition of LionMed, a magazine which has been produced by the members of L6 MVD (Medicine, veterinary and dentistry) Society over the last half term.
MVD Soc meets weekly to discuss the latest news in the medical world. From newly-discovered bacteria to revolutionary treatments for arthritic dogs, there is always stimulating conversation to be had – something I am sure will come across over the next few pages! Highlights from this edition include the role of telomeres in ageing and brachycephalic dogs – the latest fashion trend in the celebrity world.
This editor’s welcome would not be complete without a number of thanks. Firstly to Mr Langton, for allowing us to come together every Thursday, as well as for helping us to realise our vision for this magazine. Secondly, to Mr Cobb from Reprographics, for helping us commit LionMed to print. Finally, of course, I must thank all my fellow MVD Soc members for their brilliant articles and contributions to this issue.
I hope you will find something in LionMed which piques your interest, and all that’s left to say is enjoy!
Sam Govier, EditorOver 15 million people in England play sports at least once a week, with football at the forefront. But are the sports that we play and love damaging our brains? And what is being done to keep us safe? In this article, Sam Govier investigates…
Legal action by 19 claimants, including the son of 1966 World Cup winner Nobby Stiles, against several of football’s governing bodies reached the High Court in mid-January this year. As a result, head injuries in football seem like a more pertinent issue than ever.

NobbyStiles,whopassedaway in2020whilstsufferingfrom CTE
In recent years, more and more attention has been focused on the safety of players in football, especially with regard to head injuries. This came sharply into focus with the death of Stiles in 2020 from dementia linked to repeated heading of the ball – in all, he was estimated to have made between 70,000 and 100,000 headers in his career. In fact, five of the players who played in England’s 1966 victory have since been
diagnosed with or died from similar illnesses.
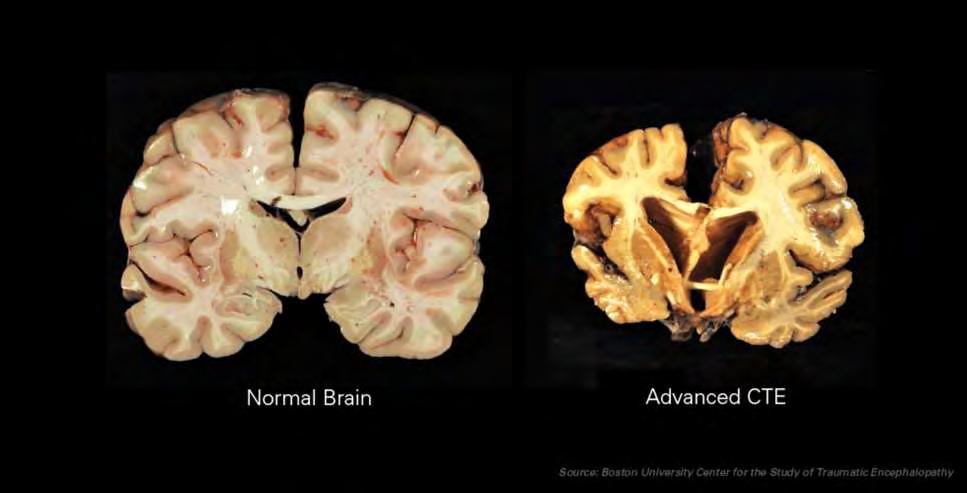
So why is this? The answer is a medical condition known as chronic traumatic encephalopathy – or CTE for short.
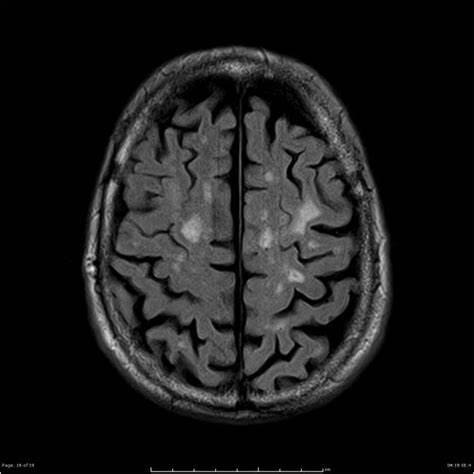
This is a degenerative condition – it causes brain tissue to die over a long period of time. This leads to dementia and, eventually, death as the brain loses healthy tissue and shrinks.
CTE has long been associated with combat sports such as boxing and MMA (it was originally calleddementiapugilista–boxer’s dementia) where participants often receive strong blows to the head, but has only relatively recently been linked to Britain’s most popular sport.
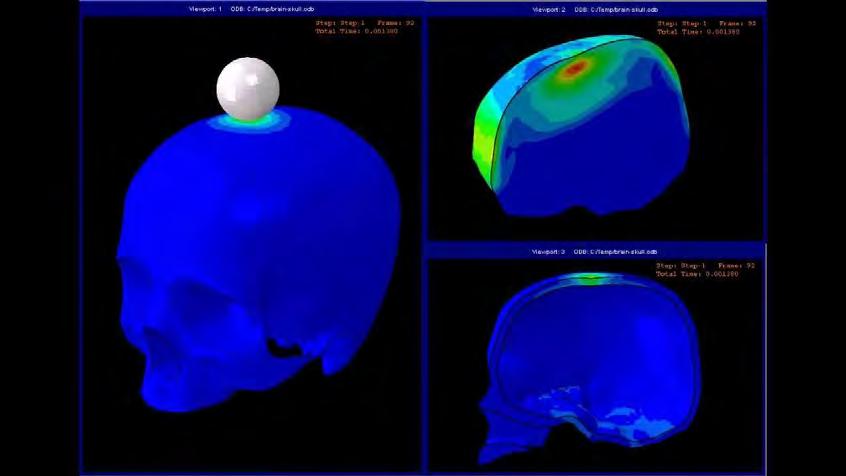
Whenever a player heads a ball, he or she not only risks a collision with the ball, but also potentially with another player – as has occasionally been seen at the top level, most recently between David Luiz and Raul Jimenez in 2020.
Either of these scenarios results in the head receiving a blow, though a much more significant one in a clash of heads. Such an impact can cause nerve cells to be damaged and die around the impact site. Repeated blows massively amplify the effect on the brain – over long periods, this damage can become so severe that large portions of the brain die, resulting in the development of CTE.
Football has also been linked with a higher likelihood of developing
Motor Neurone Disease –or MND – with a number of former professional footballers, such as Marcus Stewart and Steven Darby, developing the disease.
MND occurs when neurones in the brain begin to die, leading to a variety of symptoms around the body, such as muscle weakness and atrophy (loss of muscle tissue). Unfortunately, the condition is invariably fatal.
In July 2022, the Motor Neurone Disease Association released a statement in which they acknowledged a correlation between playing football and developing MND. They emphasised, however, that the research had not yet proven causation.
Although it appeared that footballers were more likely to develop MND, it could not be determined that football actually caused the onset of disease.
It is expected, however, that such a link will be made with future research – the limited number of studies performed so far is simply insufficient to prove anything beyond the increased likelihood.
So what is being done to protect those who play the beautiful game?
In 2022, the FA introduced a trial in which players at U12 level (year 7) and below were banned from heading the ball, with the trial expanded to more leagues across the country in 2023. This aims to reduce the exposure to head trauma at younger
ages, as well as encouraging players to find other ways to move the ball around, hopefully reducing heading in their future careers. While this won’t help players who have already been playing or have played for a long time, it is certainly a step towards making football a safer sport for newer players.
Some players at higher levels, most notably Petr Čech, choose to wear helmets designed to reduce the likelihood of suffering a serious head injury in a potential collision. Research into CTE and MND also continues in the hope that we will soon be able to better understand the condition and alleviate the risks somewhat at higher levels. Aseriesofheadscansshowingthedistributionofpressureafteraheadimpact
Mr Langton gives us the lowdown on applying to healthcare-related degrees…

The number of boys applying to medicine, dentistry and veterinary sciences from Hampton remains consistently high, despite the highly competitive nature of entry to these courses and then the demands of the degree course and jobs that follow.
But how hard is it to get into one of the 36 medical, 9 Vet or 14 dentistry schools in the UK?
The answer is that it IS hard, but every year the vast majority of the pupils from Hampton that apply (10 in each of the past 2 years), do gain entry to medical, dentistry or vet schools across the country.
The route to a successful application starts in your
GCSE years, particularly 4th and 5th. Deciding that you really want to pursue such a course will require great perseverance and drive, so only the most diligent are likely to be successful.
Attaining a very strong set of GCSEs forms part of the application for UCAS, combined with a minimum of three A grades at A level, but really strong candidates will have also completed work experience and hopefully some consistent volunteering in a care setting too.
But why is volunteering and work experience so important? Simply put, medical schools base their selection not just on academic credentials, but also on personal qualities that they consider will
make them good healthcare professionals. So, understanding the wide range of skills and attributes and, perhaps more importantly, nurturing these in yourself prior to an application, will significantly enhance your chances of success.
What attributes are needed to be a healthcare professional?
If you were to have a consultation with a doctor, dentist or vet you are likely to be in a vulnerable position and so clearly empathy is of paramount importance for anyone in a caring role. To show evidence that you do care and have cared for others is essential.
But there are so many ‘soft skills’ which any good healthcare professional
will have in spades; ability to work in a team, leadership, ability to listen, self-motivation, balance, decisiveness, problem solving, an ethical and moral perspective, calmness under pressure, approachability, adaptability and excellent time management.
All of us develop these skills as we grow up, but just like learning Biology or any other subject at school, we are able to nurture and build this skill-set over time, often by involvement in the cocurricular program at the school or beyond. Playing in an orchestra or sports team or gaining awards in D of E or volunteering on a regular basis will all help you to become more confident and able to interact effectively with others.
Have you got what it takes?
From my experience of helping pupils from Hampton apply to these roles over the past 23 years, successful applicants are easy to spot. They are the selfstarters – boys who do things for themselves rather than waiting to be told what to do. So, what are you waiting for? Get involved. Start reading one of the healthcare related books in the library, listen regularly to podcasts such as Just One Thing with Michael Mosley (https://www.bbc.co.uk/pr
ogrammes/p09by3yy/epis odes/downloads ) or set up some volunteering in your local community. Or join the Junior MVD Society (13:15 on Mondays in S43 – the biology lab next to the psychology and politics office). If you would like any additional advice please do contact me in the Biology department.
They’re the latest trend in the celebrity world –Tom Cahill shows us why brachycephalic dogs’ newfound popularity presents serious problems…
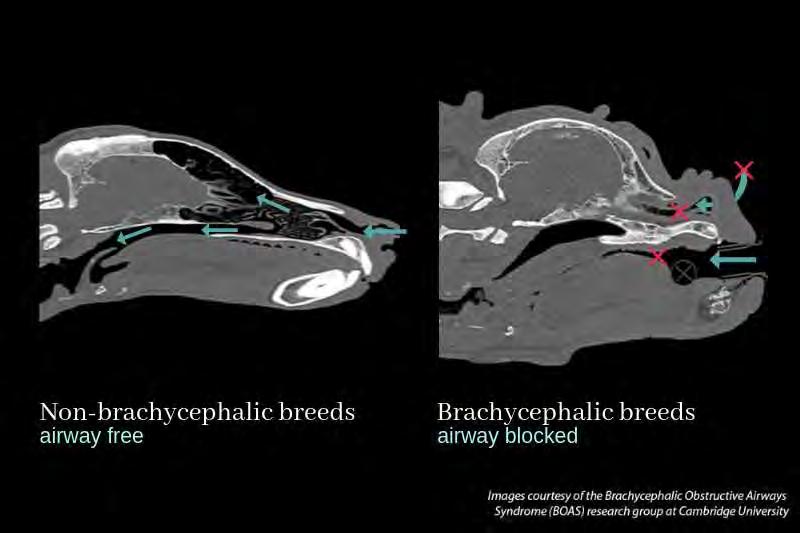
Brachycephalic literally means ‘short head’, but more specifically refers to animals with a skull at least 80% as wide as it is long. There are currently 24 different dog breeds listed as brachycephalic, all of which are easily recognisable due to their flat faces, short muzzles and big, bulging eyes.
These breeds have seen a surge in popularity over recent years, with French Bulldogs in particular becoming America’s most popular dog breed in 2022.
Celebrity ownership, an over-representation in marketing and an influx of social media posts has led to these dogs becoming very much the ‘it girl’ of the canine world, but unbeknownst to most owners, the aesthetics of these dogs come at a cost, and they are born with a plethora of health

conditions that make their lives a constant struggle.
The abnormalities which brachycephalic dogs are born with are a result of selective breeding to comply with pedigree breed standards, focusing on physical traits to enhance appearance, rather than those that would benefit the animals’ welfare. The most notable of these issues is BOAS (Brachycephalic Obstructive Airway Syndrome).
Due to these dogs being bred to have flatter faces, many have excessive tissues in the mouth and throat that cause major respiratory issues, as well as a narrower windpipe and nostrils, as shown in Figure 1. Symptoms of BOAS includes heavy breathing, snoring, and regurgitating – some of which are seen as ‘cute’ or ‘appealing’ by owners.
These abnormal behaviours are often then
posted onto social media, gathering hundreds of thousands of likes and boosting the popularity of these dogs even further.
BOAS is currently said to affect around two thirdsof Pugs, and over a half of all Bulldogs, and whilst it can be partially corrected by surgeries, these do come with their own risks and major complications.
It is commonly reported amongst vets that brachycephalic dogs take longer to recover from general anaesthesia, irrespective of the procedure they have undergone. This is believed to be due to the endotracheal tubes used allowing the dogs to breathe properly without obstruction for the very first time.
As well as BOAS, there are a number of other problems present in brachycephalic dogs. These include ongoing skin infections due to
excess skin folds harbouring bacteria, eye ulcers due to the protruding nature of their eyeballs, and spinal defects (shown in one study to occur in up to 83% of brachycephalic dogs).
The British Veterinary Association (BVA) has made it very clear that they stand against the breeding of brachycephalic dogs stating:
‘’BVAisconcernedthat therapidriseinthe numberofbrachycephalic dogsintheUKisleading toapopulation-based increaseofillhealthand compromisedwelfarein thesebreedtypes.’’
Whilst it goes without saying that owners of brachycephalic dogs are not cruel people and provide as much love and care towards their pets as anyone else, the misconception that the abnormal behaviour displayed by these breeds is desirable or ‘cute’ has to change.
Currently, only 10% of brachycephalic dog owners are said to be aware of their pets’ breedrelated problems, whilst 56% of the brachycephalic dogs brought through vets’ doors are in need of treatment.
Through raising awareness, and implementing educational initiatives targeted at owners and breeders, this animal welfare crisis can hopefully be averted. Brachycephalic dogs need to be taken out of the limelight, and thankfully campaigns have already started, such as the RSPCA’s #SaveOurBreath movement and the BVA’s #BreatheNotBreed movement, a sign we are moving in the right direction.
By acting now, we can reduce the suffering of future generations of brachycephalic dogs and prevent our pets from paying the price – simply for being cute.

Independent Vetcare, the UK’s largest veterinary services provider, operates over 500 sites across the country
There’s no doubting the veterinary industry is big money these days; in the UK alone the market is now worth over £2 billion pounds, but this isn’t what one initially expects.
If I were to ask you what you imagined when picturing veterinary practice, I’d imagine your answer would generally describe a small humble independent small animal practice, and if this were 2013, that wouldn’t be far off from reality (amongst small animal practices at least).
These days however over 53% of veterinary surgeons working with/for corporations, a far cry of the measly 11% of 2013. As it can be very easy to
jump on the anticorporatisation bandwagon, I decided to take a look into this ongoing trend of corporatisation in the veterinary industry to see what the real impacts would be for both vets and customers. It doesn’t paint the most hopeful view of the future.
While the idea of being employed by a corporation may seem appealing to many vets (especially newly qualified vets) with the significantly higher wages and much of finances being take care of by head office, most vets seem to become disenchanted pretty fast.
Veterinary surgeons working for conglomerates
are reported 13% more likely to experience burnout, compassion fatigue and other mental issues. With depression and suicide rates amongst veterinarians already regularly landing amongst the highest of all professions, this doesn’t bode well.
Many of these corporate practices are also markedly more understaffed than independent practices. In addition, given the higher proportion of new graduates being employed by chains (in some cases as the sole veterinary surgeon) the standard of care provided, despite the best efforts of employees
just can’t reach the same levels as a well-staffed practice.
Although it may seem at first to the consumer that many vet chains can provide more competitive pricing and accessibility, this comes at the detriment of the quality of care the veterinarians are able to provide for your animals. After all, a happy worker is almost always a better worker, for the sake of our animals and of our veterinarians, corporate chains are a poor choice.
Now, this is not to say that this is a model that can’t be done successfully, it just generally isn’t at the moment.
For example, many vet practices that work as a part of a small group with only a handful of branches report better statistics on the above issues than both independent and corporation owned practices.

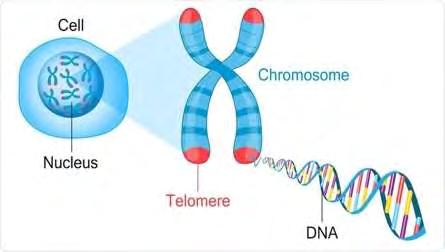
Telomeres are a region at the end of chromosomes made of DNA sequences. They cap the end of chromosomes which can serve as protection for the chromosomes like aglets on a shoelace. This prevents the genetic material (chromosomes) from becoming frayed or tangled.
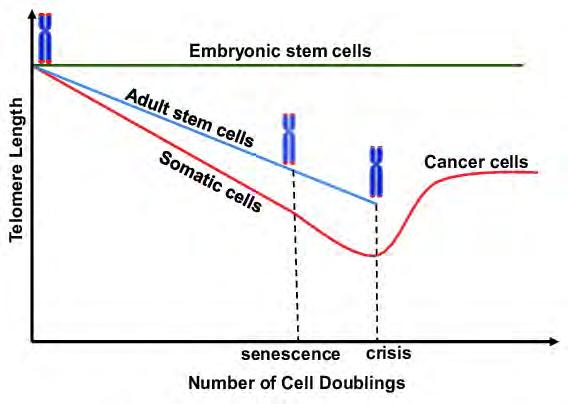
As shown by the graph on the top right, each time a cell divides, the telomeres shorten in length. This process happens until the cell can no longer divide, meaning the telomeres are too short and the cell e ectively dies. In certain cell types an enzyme called telomerase adds one-o parts of the telomere preventing the telomeres from becoming too short and extending its life.
Ageing has many e ects –some are harmless, such as greying hair, while others are more harmful, such as reduced cognitive function and increased chance of developing diseases, including cancer.
Current research aims to slow down the e ect of ageing. This will be not only be desirable for many people, but also economically beneficial as the amount of money spent on pensions and healthcare does not have to increase.
An enzyme called telomerase has recently been suggested as a‘cure’ for ageing. This is because the enzyme helps prevent cells from dying sooner as telomeres do not shorten as quickly.

However, people may object to the continuation and further development of this research on ethical grounds.
Telomeres could also be a contributing factor to cancer –the longer we live, the more chance we have of our DNA mutating and possibly developing cancers. Since these theories may take a long time to come into practice or testing people want to know what else we can do to influence telomere length.
Activities such as mindfulness meditation and cardiovascular fitness have been proven to be very beneficial for telomere health as they both proven to increase telomerase levels.
However current studies from a genetic learning centre in Utah has stated that many cancers themselves haves shortened telomeres (e.g. pancreatic, bone, prostate, and bladder). Since cancer could be detected by measuring telomeres, being able to inhibit telomerase activity may be able to fight cancer.
This can be done by decreasing telomerase levels, shortening the telomeres and causing the cancerous cells to die. Research has already been done in this with breast and prostate cancer cells in a lab.
Researchers blocked the activity of telomerase which caused the cancerous cells to die suggesting that inhibiting telomerase levels could help fight cancer. However, this comes with its own complications such as impairing immune system cells and fertility.

Glossary
-chromosomes: a structure found in the nucleus that contains DNA.
-enzyme: a protein that helps speed up chemical reactions in our body (metabolism)
-SEM: scanning electron microscope
-senescence: a cellular response of stable growth arrest
-cardiovascular: the system that consists of the heart, blood, and blood vessels.
Ishan Patel examines the latest use of AI in the medical world…
(*1=definitionavailableinglossary;attheendofthearticle)
It is undeniable that organ transplants are transformative and even lifesaving. Considerable strides have been made, however organ transplantations are not without its challenges. Issues ranging from organ shortages and rejection, to the complexities of immunosuppressive therapies, implies that there must be a closer examination. This article delves into the many hurdles involved in organ transplantations and how AI may play a role in the future in assisting with these challenges.
Kidney transplantation challenges
Within the National Health Service (NHS), organ transplantation consists of a number of different challenges that collectively impact the efficiency and accessibility of this tough medical procedure.
According to NHS Blood and Transplant (NHSBT) data, the UK has witnessed a gradual increase in the number of deceased organ donors in recent years, reaching a record high in 2020. Worryingly, the demand for organs
continue to outgrow the supply. As of 2020, there were approximately 5,800 people on the waiting list for an organ transplant in the UK. Shortages like these not only increase waiting times, but unfortunately lead to otherwise avoidable deaths.
Among the organs in high demand, kidneys holds a central position due to their critical role in the body's regulatory functions. Kidney transplantations are the most common type of organ transplantation globally. Kidney transplantations represents the treatment for end-stage renal disease*1. Data from NHSBT indicates that waiting times for kidney transplantations range from many months to even years which could very well take a toll on patients’ physical and psychological strength. As the web of challenges regarding kidney transplantations becomes increasingly intricate, it is evident that these issues be faced with the utmost importance.
Immunosuppressant*2 challenges
Immunosuppressive medications are needed in

order to prevent the body from rejecting the transplanted organ (in this case the kidney), therefore allowing the transplanted kidney to successfully integrate into the recipient’s body. As with any foreign substance being injected into the body, the long-term uses of immunosuppressive medications can pose serious complexities and a range of problems. One of the main concerns would be how to balance the immunosuppressive regimen*3 to prevent rejection while minimizing the risk of infection and other side effects. The immunosuppressive drugs dampen the immune response, increasing the recipient's susceptibility to infections that can pose serious threats. Achieving this balance requires close monitoring and adjustment of medication dosages based on individual patient
factors, including immunological status, comorbidities*4, and medication tolerability.
Furthermore,thelong-term use of these medications may lead to many medical complications such as diabetes, hypertensions and gastrointestinal issues.
How can AI (Artificial Intelligence) help ?
Despite the many obstacles associated with immunosuppressive therapy, AI holds promise for the future. AI-driven technologieswillbeableto boost patient monitoring, optimise regimens and predict a patient response to immunosuppressive therapy, by using details such as a patient’s medical history, resulting in the outcomes of this type of therapy vastly improving. Immunosuppressive therapy plays a critical role in preventing organ rejection, but achieving the right balance between too many and too little immunosuppressive drugs can be challenging. AIdriven approaches can analyse patient-specific factors to develop personalised medication regimens tailored to the unique needs and characteristics of each transplant recipient. By optimising medication dosages and schedules, AI systems can minimize the risk of rejection and medication-related complications while maximising long-term survival and patient life.
An example of this would beAIalgorithmsbeingable to analyse patient data, which would include laboratory results and medication adherence patterns*5, to identify and suggest a personalised style of treatment for a patient. AI systems can predict the chances of rejection and other serious side effects that could occur and thereby help healthcare professionals change medication regimens regularly if needed.
In addition to all this, AIpowered machines can optimise organ allocations and improve waitlist management thereby enhancing transplant efficiency and reducing waiting times for patients in need. Organ allocation is a process which involves prioritising patients, based on factors such as medical urgency and geographical proximity to the donor. AI algorithmscananalysevast amount of patient data to develop more accurate organ allocation models. These systems can identify patterns and trends that may not be apparent to human observers, thereby optimisingorganallocation decisions and maximising transplant success rates.
Additionally, AI-driven predictive analytics can enhance patient monitoring. Transplant recipients require lifelong surveillance to detect early signs of organ rejection, infection, and medicationrelated complications. AI algorithms can analyse patient data, such as vital
signs, laboratory results, and medication adherence patterns, to identify subtle changes which are an indicatoroflife-threatening events. By predicting individual patient responses to immunosuppressive therapy and other interventions, AI systems can enable healthcare providers to intervene and prevent complications before they escalate, therefore improving transplant outcomes and reducing healthcare costs.
In conclusion, AI is a powerful tool that can be used to transform the process of immunosuppressive therapies after kidney transplantation. By making use of AI-driven approaches to procedures like organ allocation, patient monitoring and medication adherence patterns, we can pave the way for a future where kidney transplantation is a much more effective and efficient type of organ transplantation. Although, bearing all this in mind, it is important to make sure that the use of AI technologies are deployed ethically and evaluated veryrigorouslytomaximise its potential benefits and minimisethepotentialrisks and unintended consequences.
*1 Renal disease refers to any condition that a ects the kidney being able to filter wastefromtheblood.Commoncausesincludediabetes,highbloodpressure.
*2Immunosuppressantsincludeanysubstanceormedicinethatreducestheactivity of the immune system. These drugs are most commonly used to prevent the body rejectingtransplantedorgansortomanageautoimmunedisease(e.g.Diabetestype 1,multiplesclerosisandinflammatoryboweldisease).
*3 Immunosuppressiveregimenreferstoatreatmentplaninvolvingtheuseofoneor more immunosuppressive drugs to reduce/supress the activity of the immune system. These regimens are typically prescribed by qualified healthcare professionals and vary on many factors ranging from the patient’s medical history, the type of organ transplant and the presence of other medical conditions. For a kidneytransplantrecipient, this might include a combination of drugs such as a calcineurin inhibitor, an antimetabolite and corticosteroids.
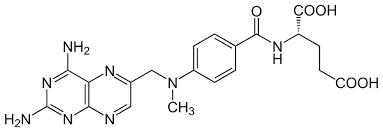
Methotrexate (image shown)isonetypeofantimetabolite.
*4Comorbiditiesrefertothepresenceoftwoormoreco-existingmedicalconditions or diseases in an individual. These conditions may occur simultaneously but are distinct from each other. Comorbidities can complicate medical management, influencetreatmentdecisions,andimpactoverallhealthoutcomes.
*5Medication adherence patterns are various ways in which individuals adhere to prescribed medication regimens over time. Adherence patterns can vary widely amongpatientsandareinfluencemostlybyapatient’sindividualcharacteristics.
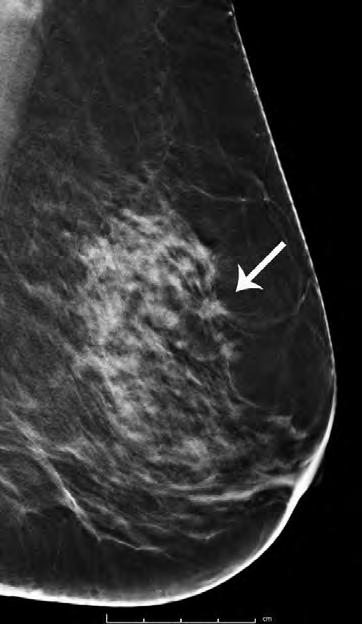
The conscientious process begins with the patient arriving in the clinic, with a complaint that they have found either a lump or abnormal feeling on their body – all of which are common signs of cancer. For example, in a breast cancer clinic, after the patient has reported an issue they have found in their breast, either near their armpit or in the main chest cavity, the doctor conducts a test to deduce whether A) a tumour is present and B) the tumour is malignant and dangerous to the patient.
Before conducting such a test, the doctor re-checks the patient’s medical and physical history, using the NHS Database, and also by a few simple questions to the patient.
This is to check if the patient’s poor health habits may contribute to the severity of the tumour – for example, if the patient is an avid smoker, or has a history of cancer in their family, they are more at risk to develop cancerous tumours within their body. In the end, this is a crucial step that the
doctor must take during cancer diagnosis.
If the doctor finds signs of a potential malignant tumour, they immediately ask the patient to have either an MRI, PET or CT scan, depending on the size and severity of the tumour that the doctor has detected.
The patient then completes the scan, and the results are analysed during an MDT meeting, where a variety of specific specialists come together to discuss multiple cases, and they decide what next steps should be taken in order to improve the patient’s health.
In one circumstance, a PET scan detected lesions within the breast of a patient, and the conclusion during the MDT meeting was to conduct a biopsy to further analyse the tumour.
A biopsy is where specialist surgeons do their work, by precisely removing the affected area in the patient, without disturbing any healthy part of the patient at the same time, and the dissected
parts are sent off to the pathology unit, where they are dissected, sampled, tested, and observed by even more specialists – an extremely key process in the diagnosis of cancer.
The body parts that have been dissected during a biopsy are stored in buckets that contain formalin – a liquid containing a mixture of water and formaldehyde –that is used in ‘formalin fixation’ in order to maintain the structure and effectively preserve the specimen during transportation to the laboratory and storage within the laboratory itself.
Sometimes, part of the sample might be sent fresh (without any preservative) to the pathology department, so that certain tests that require fresh tissue – such as cytogenetics – can be done. The container with the specimen from the biopsy is labelled with the patient’s name and other information, and also the site of biopsy (where on the body it was taken from).
The next step during diagnosis of cancer is gross examination. This is where a pathologist (a doctor with special training in pathology) takes a look at the specimen without a microscope.
During this examination, the tissue sample’s size, colour, consistency, and other characteristics are recorded on the NHS database, with pictures being taken if necessary. Such an examination is key as the pathologist may see features that suggest a particular diagnosis, such as cancer, but it may also help the pathologist decide which parts of the large sample are most critical to look at under a microscope.
The biopsy tissue, after gross examination, is then dissected into smaller pieces, to be put into small containers called cassettes – to be sent off for microscopic examination. These pieces of the biopsy must be pieces that the pathologists are interested in finding more about, as they may indicate the presence of a malignant (or even benign) tumoursomething that has the potential to cause cancer or a build-up of uncontrolled cell division.
The tissue sample within the cassette is then sent off to the processing laboratory, where it is placed into a mould with
hot paraffin wax. This wax then cools to form a solid block that protects the tissue. This paraffin wax (containing embedded tissue from the biopsy) is then cut into very thin slices using an instrument called a microtome. These thin slices of the specimen are finally placed on glass slides and are dipped into a series of stains or dyes to change the colour of the tissue so that the distinct parts of the cell are more clearly visible under a microscope.
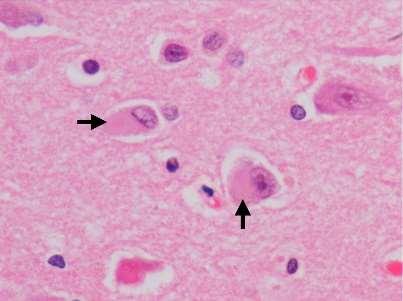
At this point (usually the day after the biopsy was done), the pathologist looks at the tissue under a microscope – called histopathology, which is the study of the structure of cells and tissues.
During histopathology, histopathologists use chemical stains, immunological procedures and increasingly molecular specialist techniques in a laboratory setting to help distinguish healthy tissue and identify abnormal tissue, cells, and infective agents.
Under microscopic examination, the tissue that has been placed on glass slides are carefully scrutinised, with histopathologists looking for signs of malignancy, such as irregular cell shapes, uncontrolled cell growth patterns or the presence of cancer-specific markers (such as ‘picketfence’ cell growth). The
histopathologist then diagnoses the patient with either a malignant tumour, which indicates cancer, or a benign tumour, which is a build-up of cells that do not have the potential to cause cancer.
The results of the diagnosis are then returned to the patient, and the next steps that are to be taken will be discussed once more in an MDT meeting, where patients that have a cancer diagnosis may be admitted to chemotherapy of surgery to remove the cancer from the body.
Advancements in imaging techniques, such as MRI, CT scans, and PET scans, have complemented traditional dissection methods by providing non-invasive ways to visualize and detect cancers within the body. These technologies have enhanced the accuracy and efficiency of cancer diagnosis.
In conclusion, dissecting body parts to find cancers plays a vital role in medical research, diagnosis, and understanding the nature of cancer. It allows for meticulous examination of tissues at a cellular level, contributing to early detection and improved treatment outcomes for patients. However, it is crucial to approach this process with the utmost respect for ethical considerations and the
individuals involved. The entire process of diagnosing cancer is extremely thorough and well thought-out, with multiple specialists being involved, during MDT meetings and during histopathology, ensuring that the patient receives the best possible care and consideration. From start to end, this massive operation takes only about 10 days to occur, in order to quickly deliver results to the patients in a considerate manner.
Cancer research is a vast and complex field with scientists and researchers working phenomenally hard to understand the disease and develop successful treatments.
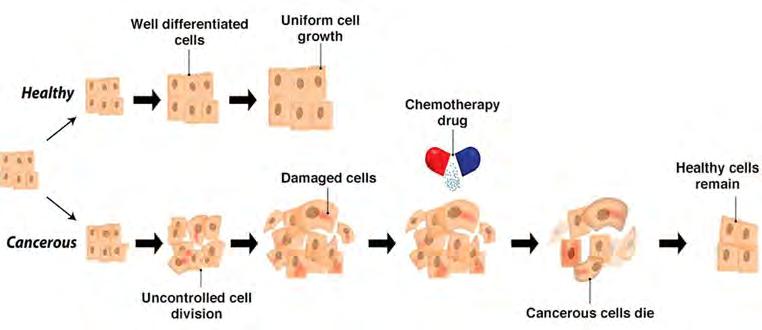
One of the vital areas of focus in cancer research is understanding the causes of cancer. Scientists have identified a multitude of risk factors, such as genetic mutations, exposure to certain chemicals or substances, and lifestyle factors like smoking, the intake of excessive alcohol and poor diet. By studying these factors, researchers hope to develop strategies for prevention and early detection.
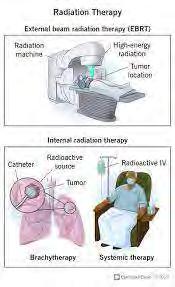
Another important aspect of cancer research is the development of new and more effective treatment methods. Traditional treatments like surgery, chemotherapy, and radiation therapy have been effective in many cases, but they can also have significant side effects (such as hair loss in chemotherapy, and extreme fatigue in radiation therapy). That's why scientists are exploring
innovative approaches like immunotherapy, targeted therapy, and gene therapy.
Immunotherapy aims to enhance the body's immune system to fight cancer cells. It involves using substances or treatments that stimulate the immune system (similar to the way in which vaccines work), helping it recognise and destroy cancer cells more effectively. This approach has shown promising results in some types of cancer, and ongoing research is expanding its potential applications and slowly improving its success rate.
within cancer cells. By targeting these specific changes, researchers aim to develop treatments that are more precise and effective, while minimising damage to healthy cells. This personalised approach has shown great promise in treating certain types of cancer, such as breast cancer and lung cancer.
Gene therapy is an emerging field that seeks to correct or modify faulty genes responsible for cancer development and growth. This approach involves introducing genes into a patient's cells to replace or repair the abnormal genes. While still in the early stages of development, gene therapy has great potential for treating many types of cancer.
Collaboration and sharing of research findings are ongoing and vital. Scientists from different institutions and countries work together to exchange knowledge and ideas, ‘fast-tracking’ progress. Also, clinical trials and experimentation play a vital role in testing the safety and effectiveness of new treatments, providing valuable data for many different scientists and doctors to work with.
While finding a definitive cure for cancer remains a complex challenge, the efforts of researchers worldwide give hope for the future. Each breakthrough brings us closer to better prevention, detection, and treatment options.
Neuralink is the latest sensation in the world of biomedical technology. But how does it actually work? And what does it mean for the future? Dimi Mikas has the answers…
What is Neuralink?
Neuralink, led by Elon Musk, is at the forefront of pioneering brain - computer interface (BCI) technology, aimed at redefining the relationship between humans and machines.
Neuralink is dedicated to facilitating direct communication between the human brain and computers. This visionary endeavour holds the potential to revolutionise healthcare, communication, and human augmentation, offering a glimpse into a future where individuals can seamlessly interact with technology using only their thoughts.
Through innovative developments in ultra-thin electrodes and implantable devices, Neuralink is posed to break new ground in neuroscience and technology.
ambitious vision of a world where the boundaries between humans and machines blur, opening up unprecedented possibilities for human machine integration and advancement.
How does Neuralink Work?
Neuralink works by implanting electrodes called threads into the brain’s neural tissue. These threads are finer than a human hair and are capable of recording and stimulating neural activity with high precision.
The implanted threads are connected to a small device, known as the “Link”, which sits behind the ear and communicates wirelessly with external devices.
Neuralink has already shown promising applications in medical research and treatment, particularly in the realm of neuroscience. Current uses of Neuralink technology include research endeavours aimed at better understanding neural activity and developing innovative treatments for neurological disorders.
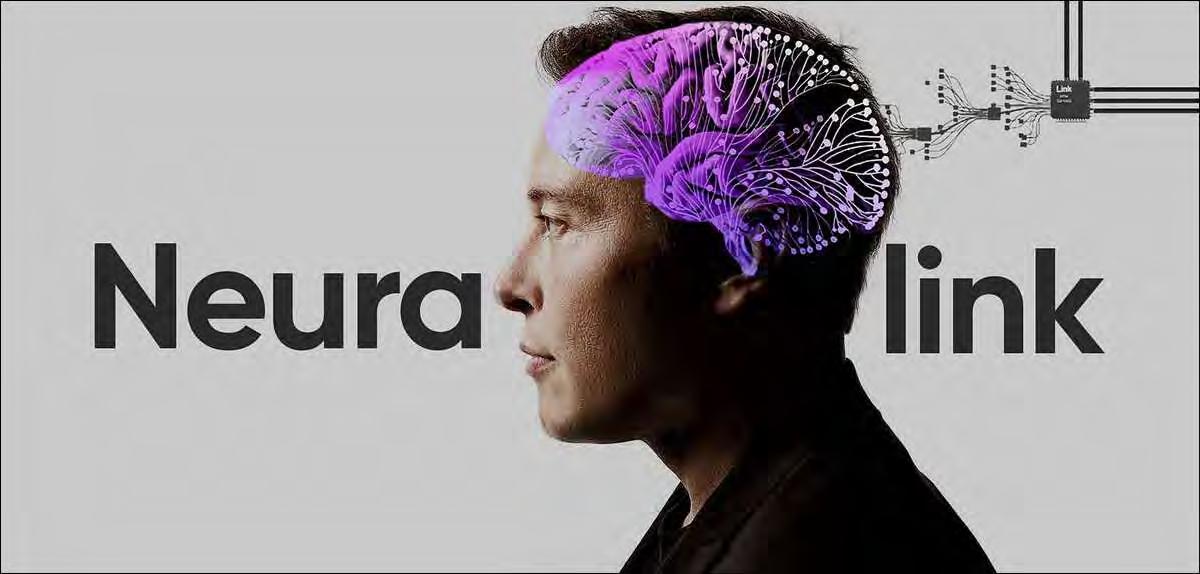
By enabling precise recording and simulation of neural activity, Neuralink’s advancements have the potential to address long standing challenges in treating neurological disorders. With each milestone, Neuralink edges closer to realising Elon Musk’s
This setup allows Neuralink to directly interface with the brain, enabling tasks such as recording neural signals for analysis, stimulating specific regions of the brain, and potentially even transmitting information between the brain and external devices.
How can Neuralink be applied?
Additionally, preliminary case studies suggest that Neuralink holds significant potential for improving the lives of individuals with conditions like Parkinson's disease and paralysis by providing more targeted and effective interventions.
Looking forward, Neuralink's future applications are even more groundbreaking, with the potential to enhance human cognition, communication, and sensory perception through direct brain-computer interfaces.
However, alongside these exciting advancements come important ethical considerations and societal implications that must be carefully addressed.
Privacy concerns, equitable access to technology, and the potential for unintended consequences all warrant
thoughtful consideration to ensure that Neuralink's transformative capabilities are harnessed responsibly and for
the collective benefit of humanity.

Many of us have heard about Dementia but there are many misconceptions about what dementia is. Although many assume dementia is simply memory loss, the definition given by the NHS is ‘a syndrome(agroupofrelated symptoms)associatedwith anongoingdeclineofbrain functioning.’Although memory loss is the easiest symptom of dementia to spot there are several others: communication/language impairments, apraxia (the inability to perform previously learned tasks) and agnosia (the inability to recognise objects).
acetylcholine, and help improve the brain functions, it is not a cure for Alzheimer’s disease.
What causes Dementia?
Dementia is not one disease, there are multiple diseases which can lead to dementia, and they are linked with an abnormal level of build-up of protein within the brain. This leads to the function of nerve cells to decline and even die causing the brain to shrink. It can also stem from injury to the cerebral cortex, which is a part of the brain, which is responsible for higher level processing such language, memory, reasoning and many more.
There are four main subtypes of dementia which are:
1. Alzheimer’s disease
2. Vascular dementia
3. Lewy body dementia
4. Frontotemporal dementia
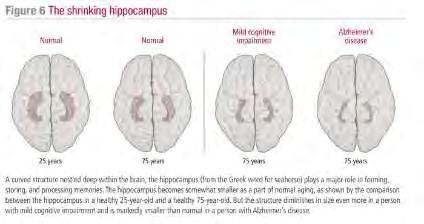
Alzheimer’s disease is the most common type of dementia, compromising 60% to 80% of cases. It is believed that it is caused by the build-up of two proteins amyloid and tau. Deposits of the protein amyloid are called plaques, and this occurs around the brain cells, but deposits of the protein tau ‘tangles’ occur within the brain cells. These both first occur in a part of the brain called the entorhinal cortex and hippocampus. Although research do not fully understand how the proteins amyloid and tau are involved in loss of brain cells, new research done last October suggests that there is a link between Alzheimer’s disease and gut microbiota (a wide variety of bacteria).
Their finding found that the symptoms of Alzheimer’s are transferable to a young healthy organism via the gut microbiota. As the brain cells become affected, there is also a decrease in neurotransmitters (chemical messengers), these are involved in sending signals between brain cells.
There are different levels of neurotransmitters, one called acetylcholine, which is low within the brains of Alzheimer’s patients.
Although medicines can increase the level of this neurotransmitter,
Genetics also plays a role in the development of Alzheimer’s, most patients are diagnosed after the age of 60, early onset Alzheimer’s (patients aged from 30 to 60) is related with gene mutation. Onset Alzheimer’s is almost impossible to detect short term memory loss is most commonly the first sign, and this is due to the hippocampus being affected early on. The hippocampus is responsible to setting new memories.
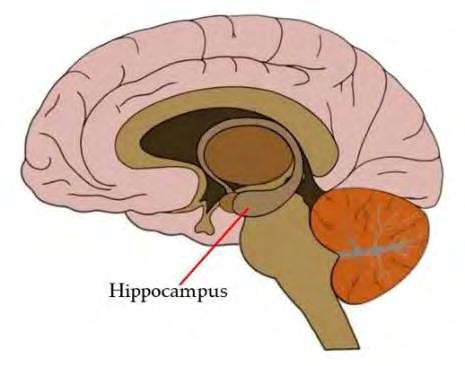
The enthral cortex is the gateway for information entering and leaving the hippocampus.
Vascular Dementia is the second most common subtype of dementia and is due to a lack of oxygen to
the brain normally due to reduced blood flow or a block. The most common cause of vascular dementia is strokes, after a major stroke the most prominent symptom would be mental confusion, however unlike Alzheimer’s memory might not be affected. If you were to also have multiple small strokes it could lead to a decrease in the executive functions (e.g. reasoning and thinking) as the damage accumulates.
A Lewy body is a tiny clump of protein, known as synuclein, that develops within brain cells. The most common feature of Lewy body Dementia (LBD) is confusion or memory loss that occurs in fluctuations and spontaneous Parkinsonism (an umbrella term, that includes Parkinson’s disease, used to describe symptoms where
the patient would have tremors and muscle rigidity).
Despite memory loss being more frequent in early Alzheimer’s it is more commonly seen in advanced LBD so being able to correctly diagnose the subtype of dementia can always be a struggle. More 80% of patients with LBD develop Parkinsonism. Patients who have LBD tend to have dementia occur 12 months prior to Parkinsonism but patients with Parkinson’s disease dementia (PDD) they tend to present parkinsonian symptoms at the same time as their dementia diagnosis. Another difference between
the two is that the tremors are more common in patients with PDD, but patients with LBD tend to have postural instability.
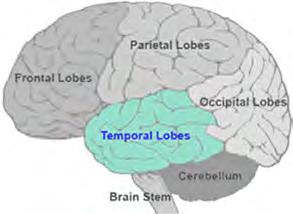
Frontotemporal Dementia (FTD) is a general term that describes multiple disorders such as Pick’s disease. It gets its name as it affects the frontal and temporal lobes of the brain, it tends to be more common in younger patients (40-75) than Alzheimer’s. The most common features of FTD are changes in personality and behaviour of the patient.