8 minute read
How Covid-19 has aff ected Irish respiratory care
How Covid-19 has affected respiratory care
Dr Sarah O’Beirne, Consultant Respiratory Physician, speaks to Niamh Cahill, while Irish Thoracic Society President Dr Aidan O’Brien speaks to Paul Mulholland about how the sudden shifts in Irish respiratory services caused by Covid-19 could have a lasting impact
One of the most significant outcomes of the Covid-19 pandemic to date has been the immense changes it has wrought on the delivery of our healthcare services.
Given the nature of the coronavirus and its impact on the lungs, respiratory services have been particularly affected.
Dr Sarah O’Beirne, Consultant Respiratory Physician at St Michael’s and St Vincent’s University Hospitals, Dublin, spent much of her time during the first wave of the pandemic looking after hospitalised Covid-19 patients, and speaking to Update said that without doubt the pandemic has had a huge impact.
“The service has changed so much in the last six months. Like everything else in medicine we’ve all had to completely reorganise our practice. If anything, it’s shown us how we can adapt and adapt quickly. People have worked well together in these challenging times.”
She added that following the ‘first wave’ and the initial shutdown of all ‘non acute’ health services, the focus remains on keeping services up and running as much as possible and to try to stop waiting lists climbing further. “Since July services regular have become more normalised and I think a big push at the moment is to provide as much routine care as possible, despite the pandemic, provided it’s safe, to avoid increased morbidity and mortality in the future.”
Amid the upheaval and efforts to continue regular care, completely new services for patients suffering from postCovid respiratory symptoms are being developed to offer continuing care to those still affected by the virus.
Going virtual
One of the biggest shifts since Covid-19 emerged has been the move to virtual Dr Sarah O’Beirne Dr Aidan O’Brien
pulmonary rehabilitation outpatient classes for patients with chronic lung disease, a development that will have a long-lasting impact on the structure of healthcare, Dr O’Beirne believes.
Pulmonary rehabilitation is the standard care for patients with chronic lung disease, ongoing symptoms and limitations despite maximised medical treatment. It is a vital component of care, as rehabilitation reduces hospitalisations.
A 2018 report found that Ireland has the highest rate of hospital admission with COPD of any country in the OECD. A study, published in JAMA earlier this year, showed that pulmonary rehabilitation within 90 days of a COPD exacerbation reduces mortality.
Typically, pulmonary rehabilitation is provided in an outpatient setting with patients participating in a class run over six-to-12 weeks, depending on the programme. It includes an exercise component, as well as a focus on education and behavioural change.
But group classes for patients with chronic lung disease are not feasible during the pandemic, according to Dr O’Beirne. “So, the standard outpatient pulmonary rehabilitation programme we provided has been on hold since the pandemic began in earnest in March in this country.
“That’s led, as with other services, to a shift towards more virtual pulmonary rehabilitation. We’ve been running a virtual pulmonary rehab programme, which began during the pandemic.
“We’ve had several groups complete the programme already and have seen good results with it. This is a programme people do from home where they log into live sessions and complete an exercise component. We also have the educational parts. It’s all done virtually apart from the pre- and post-rehab assessments, which are done in the hospital. It’s a much safer way from an infection control perspective for patients and for staff.”
There have been definite improvements in symptoms, quality-of-life scores and walk distance scores in patients who took part in the virtual programme.
Dr O’Beirne said the virtual nature of the clinic has helped increase numbers among those who may not have been able to travel to clinics.
Despite this, it is evident that virtual clinics are not suitable for all patients, she acknowledged. “The downside is it’s not suitable for everyone. We know from contacting people on our waiting list for the regular rehab programme that only 50 or 60 per cent of them would be suitable to partake in the programme, due to a combination of access to technology, technological literacy and disease severity.
“Then there’s also the aspect that for some patients, depending on their condition, it may not be safe for them to exercise at home in a less supervised fashion.
“It’s about recognising the limitations of virtual care, while recognising its definite role, particularly when we are in the throes of a pandemic. I think in the long-term it will be a mix of virtual and standard care that we provide people.”
For those who cannot access virtual clinics, some severally ill patients have been offered inpatient rehabilitation, but the remainder are waiting for the outpatient programme to resume.
In March, the service had 60-70 people on a waiting list. Since then, this has increased and there have seen more referrals, said Dr O’Beirne. It is not yet known when standard outpatient rehabilitation services will resume.
Post-Covid rehabilitation
Another major development is the introduction of rehabilitation classes for patients suffering from post-Covid symptoms. The classes operate just like that of a pulmonary rehabilitation programme and are focused on people with respiratory symptoms, Dr O’Beirne explained.
“We’ve had nearly 20 people through so far. The groups are smaller because of infection control risk and it is provided in person rather than virtually.”
The programme runs for eight weeks and individuals attend twice weekly in person, similar to a standard pulmonary rehabilitation programme for exercise. There is a separate educational component and an occupational therapist works with patients on relaxation techniques, to help ease anxiety, thus providing a holistic service for patients.
“Initially we had thought that it would be predominantly beneficial for hospitalised patients that had more severe illness, but we are seeing more and more referrals from the community from people who weren’t hospitalised but who have persistent exercise limitation and ongoing symptoms,” said Dr O’Beirne.
“Outpatient services we were using for outpatient rehabilitation have been redeployed to this because we are not running the in-person outpatient pulmonary rehabilitation programme.”
Dr O’Beirne believes that post-Covid rehabilitation programmes will be required countrywide in the future. However, it remains unknown how long such services will be needed and how great the demand will be.
“Yes, this is something that will be needed around the country. It’s such a new condition, but we know that a high percentage of people have more prolonged symptoms, so you would anticipate that more of these structured programmes will be required.
“We don’t know how long this will go on for and we also don’t have long-term follow-up. We don’t know yet how great the need might be. It certainly looks like it will be required at least in the medium-term.”
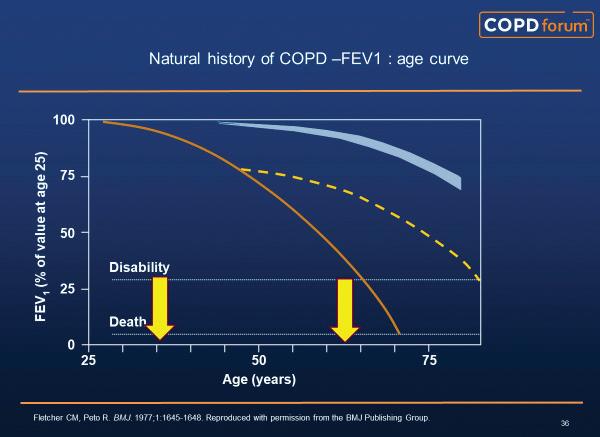
COPD
While spirometry is a crucial part of any COPD diagnosis, because of the infection risks involved non-essential pulmonary function testing (PF) ceased for a time during the first wave of the pandemic in spring. Testing has since resumed, but not at the same rate, as more guidance is awaited on how spirometry could be facilitated once again in the community.
Another impact of Covid-19 for COPD patients has been the reduction in hospital admissions related to the disease to date this year. While official figures have yet to be revealed, there is anecdotal evidence to suggest that there have been fewer hospital admissions related to COPD in 2020, according to Dr O’Beirne.
“This is probably because people were cocooning more because of the pandemic… because of that I think people contracted less viral illnesses overall. I would imagine we will see a slight reduction in COPD admissions over the last six months when the data is reported.”
ITS virtual 2020 Annual Scientific Meeting
Meanwhile, in a separate interview, Dr Aidan O’Brien, Irish Thoracic Society (ITS) President and Consultant Respiratory Physician, University Hospital Limerick, said respiratory services, not ICU services, are most affected by Covid-19.
“Most Covid-19 admissions are for respiratory problems,” Dr O’Brien told Update, speaking in advance of the ITS’s Annual Scientific Meeting, which will take place virtually on 3-4 December.
“Also, people with long-term symptoms as a result of Covid is quite a significant percentage. And a lot of those symptoms are respiratory. So a lot of the follow-up that is needed is going to be done by respiratory services.”
This has had a resulting impact on non-Covid-19 services. “All the ongoing management of existing respiratory services have been affected. Patients also have avoided coming in for follow-up, which has led to the problems of prolonged waiting lists, delayed diagnosis, and more advanced stages of disease.”
Dr O’Brien said the ITS “very much welcomes” the additional investment in respiratory services outlined in the HSE’s recently published Winter Plan, but noted that the funding is mainly for the community sector, and more support is still required for the acute sector.
As a result of its significance, the first session of the ITS meeting will be dedicated to Covid-19, and will include a presentation by Prof Stefano Nava, Professor of Respiratory Medicine, University of Bologna, Italy. As well as being a world expert on non-invasive ventilation for respiratory failure, Prof Nava also has first-hand experience of the pandemic in Italy, which was one of the most badly affected countries in the first wave of Covid-19. Dr O’Brien added that a “significant number” of research studies submitted to the Society for the meeting are related to Covid-19.
However, the coronavirus will not dominate proceedings, and the meeting will also feature expert presentations on a wide range of respiratory and sleep disorders, from interstitial lung disease to COPD and asthma.
Extensive, exclusive coverage of the meeting will be published in an upcoming issue of the Medical Independent. For further information on the meeting programme and speakers visit irishthoracicsociety.com.