IMPROVING THE DIAGNOSIS AND MONITORING OF CRITICALLY ILL PATIENTS AND THE ROLE OF BLOOD GAS TESTING
The Role of Blood Gas Analysis in the Management of Patients with Severe COVID-19 Professor Daniel Martin OBE, Intensive Care Consultant, Royal Free Hospital, London, UK Advanced blood gas analysers can support the monitoring and management of COVID-19 patients.
Introduction Airborne infectious diseases are a constant threat to society. Transmissible via the air in droplet or aerosol form, and through contact with contaminated surfaces, they primarily affect the respiratory tract leading to a range of illnesses with varying severity. In 2019, a novel coronavirus named severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) emerged, spreading rapidly to cause coronavirus disease 2019 (COVID-19) and eventually resulted in a pandemic that changed the world. To date, 14.8 million people have tested positive for the virus, and over 600,000 are known to have died from COVID-1938. These figures are likely to be underestimates of the total disease burden and will have increased by the time this report is published. Approximately 80% of people who are affected by COVID-19 develop mild symptoms (most commonly a fever, persistent cough, and shortness of breath), which requires no specific treatment. Around 15% of those infected with the virus will develop severe acute respiratory failure with breathlessness and hypoxaemia, requiring hospital admission for the administration of oxygen1. If giving oxygen by simple measures such as a nasal cannula or face mask fails to correct the hypoxaemia then admission to an intensive care unit (ICU) may be required. This occurs in around 5% of those infected, and most will go on to require mechanical ventilation via an endotracheal tube2-4. Unfortunately, the mortality of those admitted to the ICU is approximately 50%5,6. Older people, males, and those with diabetes, obesity, and hypertension appear to be prone to a more severe form of the infection. In the absence of a definitive treatment for COVID-19, supporting respiratory function is the cornerstone of the current strategy to promote survival in
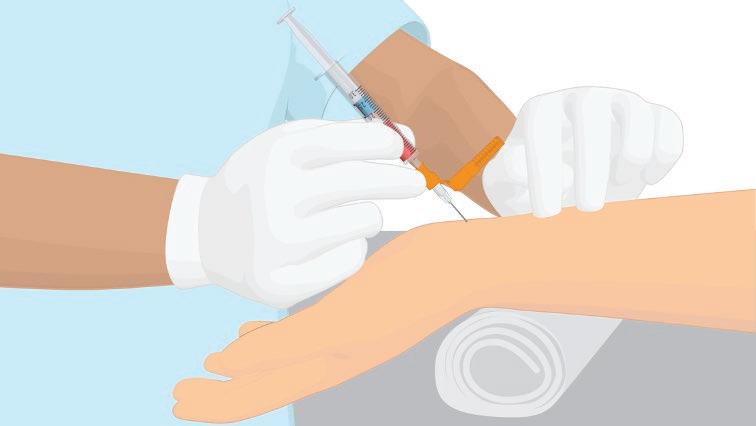
patients with COVID-19. Optimum application of all of the various modalities available to improve oxygenation in hospitalised patients relies on rapid, accurate, and reliable measurement of arterial oxygenation by point-of-care test (POCT) arterial blood gas (ABG) analysis to titrate to the required physiological target.
COVID-19 and Oxygenation At the cellular level, oxygen is essential for the preservation of energy production via oxidative phosphorylation. When oxygen is in short supply, normal cellular function deteriorates and ultimately fails altogether. A continuous supply of oxygen must be maintained along a pathway known as the oxygen cascade (Figure 1). The cascade describes the journey taken by oxygen from the air, along the respiratory tract, into the blood, and then via the circulatory system to the tissues that use it. Oxygen transport can be impaired by pathology at any point along this pathway. COVID-19 primarily affects gas exchange at the interface between the respiratory and cardiovascular systems, where gaseous oxygen and carbon dioxide are exchanged at the alveolar membrane. Of the five commonly described physiological causes of hypoxaemia (Table 1), ventilation-perfusion (VA/Q) mismatching is likely to be the dominant factor in COVID-19. Commonly, patients present to the hospital with rapid, shallow breathing, but often without the other classic signs of respiratory distress, such as increased work of breathing. The typical picture is a type-1 respiratory failure with severe hypoxaemia but a normal (or low) arterial partial pressure of carbon dioxide (PaCO2). Chest X-ray and computed tomography (CT) scanning of the lungs tends to show patchy areas of consolidation throughout both lungs and widespread ground-
Approximately 80% of people who are affected by COVID-19 develop mild symptoms (most commonly a fever, persistent cough, and shortness of breath), which requires no specific treatment
WWW.HOSPITALREPORTS.EU | 3