5 minute read
References
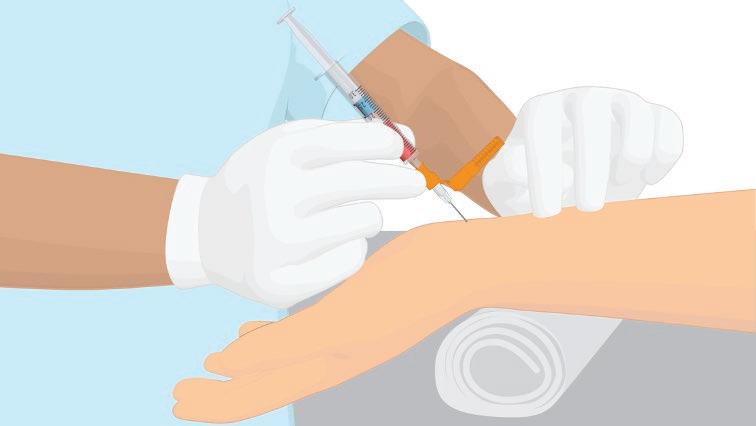
from Improving the Diagnosis and Monitoring of Critically ill Patients and the Role of Blood Gas Testing
Worldometer. COVID-19 Pandemic. 21st July 2020; Available from: https://www.worldometers.info/coronavirus/. Wu, Z. and McGoogan, J.M. Characteristics of and Important Lessons From the Coronavirus Disease 2019 (COVID-19) Outbreak in China: Summary of a Report of 72 314 Cases From the Chinese Center for Disease Control and Prevention. Jama, 2020. Remuzzi, A. and Remuzzi, G. COVID-19 and Italy: what next? The Lancet, 2020. 395(10231): p. 1225-1228. Bhatraju, P.K., et al., Covid-19 in Critically Ill Patients in the Seattle Region – Case Series. New England Journal of Medicine, 2020. 382(21): p. 2012-2022. Intensive Care National Audit and Research Centre. COVID 19 Report. https://www.icnarc.org/Our-Audit/Audits/Cmp/Reports. 21st May 2020 Berlin, D.A., Gulick, R.M. and Martinez, F.J. Severe Covid-19. N Engl J Med, 2020. Wong, H.Y.F., et al., Frequency and Distribution of Chest Radiographic Findings in Patients Positive for COVID-19. Radiology, 2020. 296(2): p. E72-e78. Tobin, M.J., Respiratory monitoring. Jama, 1990. 264(2): p. 244-51. Definition Task Force ARDS. Ranieri, V.M., et al., Acute respiratory distress syndrome: the Berlin Definition. Jama, 2012. 307(23): p. 2526-33. Radovanovic, D., et al., Helmet CPAP to Treat Acute Hypoxemic Respiratory Failure in Patients with COVID-19: A Management Strategy Proposal. J Clin Med, 2020. 9(4). NIH NHLBI, ARDS Clinical Network Mechanical Ventilation Protocol Summary 1st May 2020; Available from: http://www.ardsnet.org/files/ventilator_protocol_2008-07.pdf. Gattinoni, L., et al., COVID-19 Does Not Lead to a “Typical” Acute Respiratory Distress Syndrome. Am J Respir Crit Care Med, 2020. 201(10): p. 1299-1300. Modrykamien, A., Chatburn, R.L. and Ashton, R.W. Airway pressure release ventilation: an alternative mode of mechanical ventilation in acute respiratory distress syndrome. Cleve Clin J Med, 2011. 78(2): p. 101-10. Docherty, A.B, et al., Features of 16,749 hospitalised UK patients with COVID-19 using the ISARIC WHO Clinical Characterisation Protocol. 2020, medRxiv. Casserly, B., et al., Lactate measurements in sepsis-induced tissue hypoperfusion: results from the Surviving Sepsis Campaign database. Crit Care Med, 2015. 43(3): p. 567-73. Haddad, M. and S. Sharma, Physiology, Lung, in StatPearls. 2020, StatPearls Publishing StatPearls Publishing LLC.: Treasure Island (FL). Castro, H.J., J.M. Oropello, and N. Halpern, Point-of-care testing in the intensive care unit. The intensive care physician’s perspective. Am J Clin Pathol, 1995. 104(4 Suppl 1): p. S95-9. Brun-Buisson, C., et al., Epidemiology and outcome of acute lung injury in European intensive care units. Results from the ALIVE study. Intensive Care Med, 2004. 30(1): p. 51-61. Pandya, N.K. and S. Sharma, Capnography And Pulse Oximetry, in StatPearls. 2020, StatPearls Publishing StatPearls Publishing LLC.: Treasure Island (FL). Sweeney, R.M. and D.F. McAuley, Acute respiratory distress syndrome. Lancet, 2016. 388(10058): p. 2416-2430. Dellinger, R.P., et al., Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med, 2013. 39(2): p. 165-228. Godignon, M., et al., A support to biological validation of oxygenation parameters. Ann Biol Clin (Paris), 2017. 75(6): p. 653-663. Flower, L. and D. Martin, Management of hypoxaemia in the critically ill patient. British Journal of Hospital Medicine, 2020. 81(1): p. 1-10. Simpson, H., Interpretation of arterial blood gases: a clinical guide for nurses. Br J Nurs, 2004. 13(9): p. 522-8. Bullen, B. and R. Rollins, Blood gas testing: a brief history and new regulatory developments. MLO Med Lab Obs, 2015. 47(11): p. 46. West, J.B., A lifetime of pulmonary gas exchange. Physiol Rep, 2018. 6(20): p. e13903. Rubenfeld, G.D., et al., Incidence and outcomes of acute lung injury. N Engl J Med, 2005. 353(16): p. 1685-93. Villar, J., et al., The ALIEN study: incidence and outcome of acute respiratory distress syndrome in the era of lung protective ventilation. Intensive Care Med, 2011. 37(12): p. 1932-41. Riviello, E.D., et al., Hospital Incidence and Outcomes of the Acute Respiratory Distress Syndrome Using the Kigali Modification of the Berlin Definition. Am J Respir Crit Care Med, 2016. 193(1): p. 52-9. Merlani, P., et al., Quality improvement report: Linking guideline to regular feedback to increase appropriate requests for clinical tests: blood gas analysis in intensive care. BMJ (Clinical research ed.), 2001. 323(7313): p. 620-624. Noseworthy, T.W., et al., Cost accounting of adult intensive care: methods and human and capital inputs. Crit Care Med, 1996. 24(7): p. 1168-72. Singer, M., et al., The cost of intensive care: a comparison on one unit between 1988 and 1991. Intensive Care Med, 1994. 20(8): p. 542-9. Muakkassa, F.F., et al., ABGs and arterial lines: the relationship to unnecessarily drawn arterial blood gas samples. J Trauma, 1990. 30(9): p. 1087-93; discussion 1093-5. Melanson, S.E., et al., Utilization of arterial blood gas measurements in a large tertiary care hospital. Am J Clin Pathol, 2007. 127(4): p. 604-9. Ferreira, C.E.S., et al., Point-of-Care Testing: General Aspects. Clin Lab, 2018. 64(1): p. 1-9. Florkowski, C., et al., Point-of-care testing (POCT) and evidence-based laboratory medicine (EBLM) - does it leverage any advantage in clinical decision making? Crit Rev Clin Lab Sci, 2017. 54(7-8): p. 471-494. Sumita, N.M., et al., Clinical Applications of Point-of-Care Testing in Different Conditions. Clin Lab, 2018. 64(7): p. 1105-1112. Tang, R., et al., Capillary blood for point-of-care testing. Crit Rev Clin Lab Sci, 2017. 54(5): p. 294-308. Fries, D. and W. Streif, Point-of-care testing in critically ill patients. Semin Thromb Hemost, 2015. 41(1): p. 75-83. Toffaletti, J.G. and C.R. Rackley, Monitoring Oxygen Status. Adv Clin Chem, 2016. 77: p. 103-124. Ronquillo, J.G. and D.M. Zuckerman, Software-Related Recalls of Health Information Technology and Other Medical Devices: Implications for FDA Regulation of Digital Health. Milbank Q, 2017. 95(3): p. 535-553. Stern, A.D., et al., Cybersecurity features of digital medical devices: an analysis of FDA product summaries. BMJ Open, 2019. 9(6): p. e025374. ZingBox. IoT guardian for the healthcare industry [Internet]. 2016 July 2020]; Available from: http://www.zingbox.com/wp-content/uploads/2017/02/ZingBox_WP_IoT-Guardian-for-the-Healthcare-Industry.pdf Murad, M.H., Clinical Practice Guidelines: A Primer on Development and Dissemination. Mayo Clin Proc, 2017. 92(3): p. 423-433. Pompey, J. and B. Abraham-Settles, Clarifying the Confusion of Arterial Blood Gas Analysis: Is it Compensation or Combination? Am J Nurs, 2019. 119(3): p. 52-56. Lopez, J., Carl A. Burtis and David E. Bruns: Tietz Fundamentals of Clinical Chemistry and Molecular Diagnostics, 7th ed. Indian Journal of Clinical Biochemistry, 2015. 30(2): p. 243-243. Davis, M.D., et al., AARC clinical practice guideline: blood gas analysis and hemoximetry: 2013. Respir Care, 2013. 58(10): p. 1694-703. Albert, T.J. and E.R. Swenson, Circumstances When Arterial Blood Gas Analysis Can Lead Us Astray. Respir Care, 2016. 61(1): p. 119-21. Ferguson, N.D., et al., Screening of ARDS patients using standardized ventilator settings: influence on enrollment in a clinical trial. Intensive Care Med, 2004. 30(6): p. 1111-6. Gowda, M.S. and R.A. Klocke, Variability of indices of hypoxemia in adult respiratory distress syndrome. Crit Care Med, 1997. 25(1): p. 41-5. Seeley, E., et al., Predictors of mortality in acute lung injury during the era of lung protective ventilation. Thorax, 2008. 63(11): p. 994-8.