
Annual Icahn School of Medicine Mount Sinai Morningside/West Internal Medicine Residency Research Week PROGRAM AND ABSTRACTS May 9-10, 2023 1
Table of Contents 3 4 7 20 121 132 196 205 Introduction Selection Committee and Oral Presentations List of Abstracts with Posters Abstracts with Posters List of Abstracts 2022-2023 Abstracts 2022-2023 List of Publications 2022-2023 Index of Posters Index of Resident Authors 210 2
Mount Sinai Morningside/West Internal Medicine Residency
Annual Virtual Research Week
May 9-10, 2023
Georgina Osorio, MD, MPH
John A. Andrilli, MD, FACP Program Director Internal Medicine Residency


Mount
Sinai Morningside/West
3
Mount Sinai Morningside/West Internal Medicine Residency Research Week Selection Committee 2022-2023
Selection committee members did not participate in the discussion or voting for abstracts in which they were involved or with which they had any additional conflict of interest.

Presenters were selected using a double-blind review process.
COMMITTEE MEMBERS
Georgina Osorio, MD, MPH, Chair
John Andrilli, MD
Ruchika Batwara, MD
Gabriela Bernal, MD
Abel Casso Dominguez, MD
Ashish Correa, MD
Deborah Edelman, MD
Karim El Hachem, MD
Lindsey Fox, MD
Jennifer Fung, MD
Tamara Goldberg, MD
Katherine Hawkins, MD
Krystle Hernandez, MD
Yasmin Herrera, MD
Daniela Jodorkovsky, MD
Michael Kaplan, MD
Kiran Mahmood, MD
Alejandro Prigollini, MD
Adam Rothman, MD
James Salonia, MD
Ashwin Sawant, MD

Nicholas Sells, MD
Shantheri Shenoy, MD
Priya Simoes, MD
Vasundhara Singh, MD
Melissa Wiener, MD
Sanaa Zafar, MD
Petra Zubin Maslov, MD
4
Abstracts selected to be oral presentations on Wednesday, May 10, 2023 at 8AM.
BASIC SCIENCE
Jonas Maximillian Marx, PGY2

ABSTRACT #44: IDENTIFICATION OF AN OPTIMAL METHOD FOR ECHOCARDIOGRAPHIC RIGHT VENTRICULAR MASS ESTIMATION IN A SWINE MODEL OF PULMONARY HYPERTENSION
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
Norah Sadek, PGY1



ABSTRACT #58: A CASE OF LAUGHING HER WAY TO VITAMIN B12 DEFICIENCY
CLINICAL RESEARCH
Brissete Mancero, PGY3
ABSTRACT #41: PROGNOSTIC SIGNIFICANCE OF EXERCISEINDUCED MYOCARDIAL ISCHEMIA IN PATIENTS WITH ANGIOGRAPHICALLY NORMAL CORONARIES COMPARED TO PATIENTS WITH NORMAL EXERCISE ECHOCARDIOGRAPHY
MEDICAL EDUCATION
Maxwell Horowitz, PGY3

ABSTRACT #31: RESIDENT EDUCATION FOR IMPROVED QUALITY AND CONFIDENCE IN INPATIENT HYPERGLYCEMIA
QUALITY IMPROVEMENT
Sharel Sadud Armaza, PGY2
ABSTRACT #59: IMPROVING RESIDENT CONTINUITY OF CARE AT AN URBAN FEDERALLY QUALIFIED HEALTH CENTER
5
Annual Icahn School of Medicine at Mount Sinai Morningside/West Internal Medicine Residency Research Week













Research Day Judges


May 9, 2023
 Valida Bajrovic Fernando Carnavali Natalie Cedeno
Maya Fakhoury
Katherine Hawkins
Sara Huda
Brian Markoff
Joseph Mathew
Doreen Mensah Argelis Rivera Samuel Seward Nirav Shah
Aakanksha Sharma Christine Stavropoulos
David Steiger
Kevin Yan
Valida Bajrovic Fernando Carnavali Natalie Cedeno
Maya Fakhoury
Katherine Hawkins
Sara Huda
Brian Markoff
Joseph Mathew
Doreen Mensah Argelis Rivera Samuel Seward Nirav Shah
Aakanksha Sharma Christine Stavropoulos
David Steiger
Kevin Yan
List of


Abstracts with Posters
7
LIST OF ABSTRACTS WITH POSTERS
1
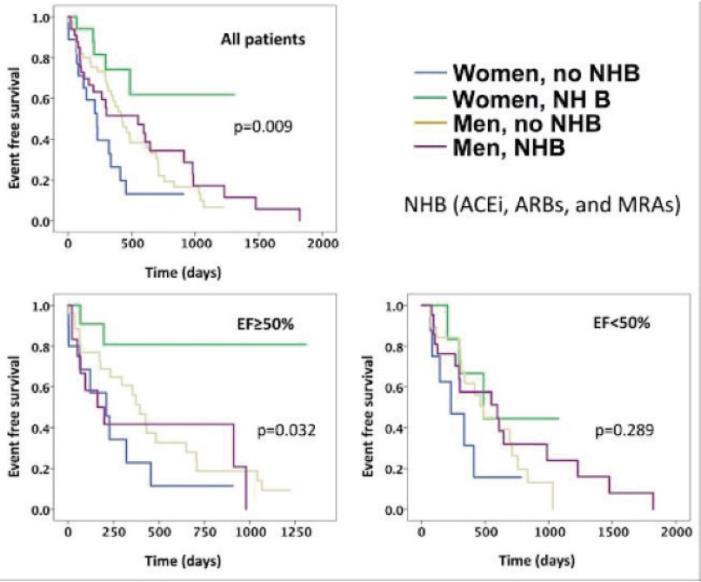
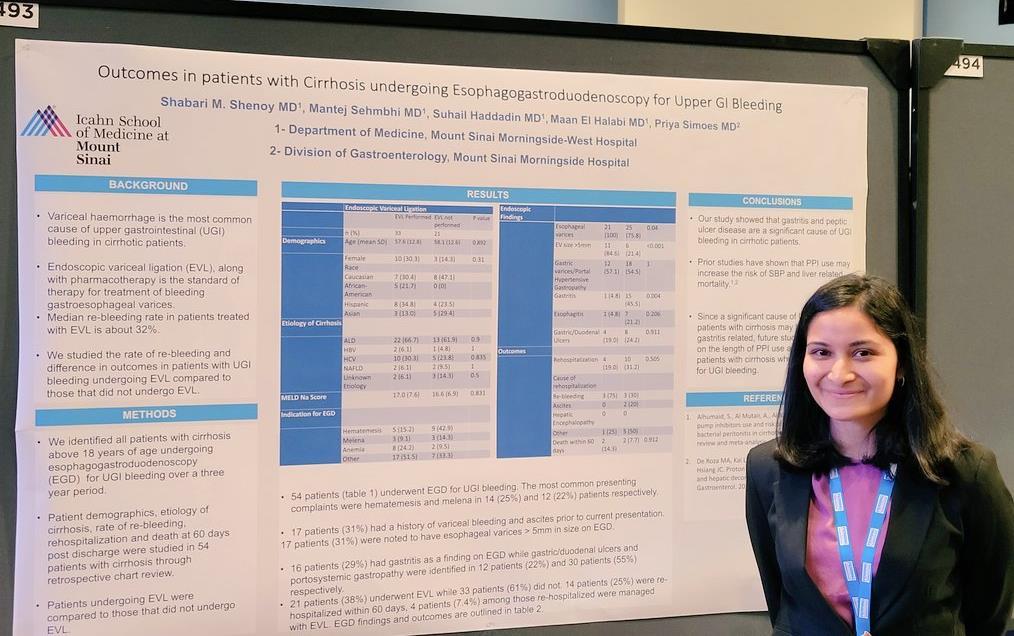
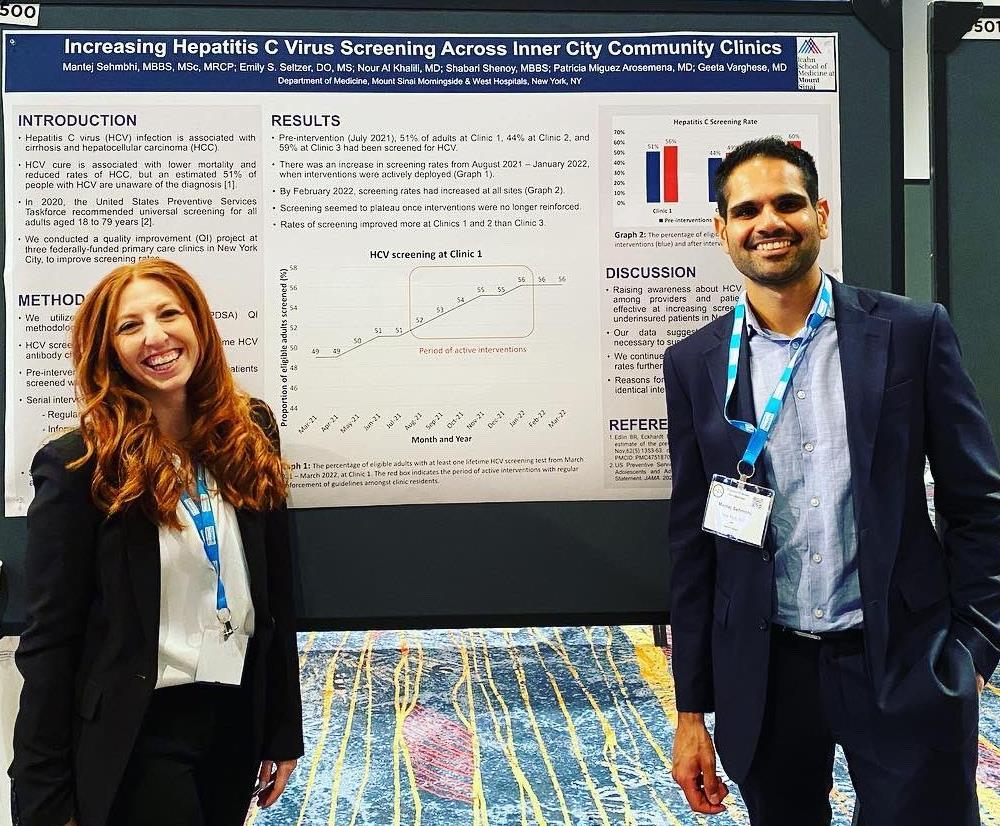
SEVERE OBESITY AND HEART FAILURE
José S. Aguilar-Gallardo1 , Francisco J. Romeo1, Kirtipal Bhatia1, Ashish Correa1 , Jeffrey Ian Mechanick2, Johanna P. Contreras2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in American Journal of Cardiology, 2022. PMID: 35705429 2
EVALUATING SERUM FREE LIGHT CHAIN RATIO AS A BIOMARKER FOR MULTIPLE MYELOMA
Theresia Akhlaghi1 , Kylee Maclachlan2, Neha Korde2 , Sham Mailankody2, Alexander
Lesokhin2 , Hani Hassoun2 , Sydney X. Lu2, Dhwani Patel2 , Urvi Shah2, Carlyn Tan2 ,
Andriy Derkach2 , Oscar Lahoud2, Heather J. Landau2, Gunjan Shah2 , Michael Scordo2 , David J. Chung2, Sergio A. Giralt2 , Saad Z. Usmani2, Ola Landgren3, Malin Hultcrantz2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Memorial Sloan Kettering Cancer Center, New York, NY, United States; 3University of Miami, Miami, FL, United States
Presented at the American Society of Clinical Oncology Annual Meeting (ASCO) that was held both virtually and in Chicago, Illinois, United States from June 3-7, 2022. 3
PROTON PUMP INHIBITOR USE DOES NOT AFFECT MANOMETRIC PARAMETERS IN PATIENTS WITH GASTRO-ESOPHAGEAL REFLUX CONFIRMED ON QUANTITATIVE TESTING
Nour Al Khalili1 , Mantej Sembhi1, Patricia Miguez Arosemena1, Kimberly Cavaliere1 , Daniela Jodorkovsky1 , Michael S. Smith1
THE EFFECTS OF COVID-19 ON PULMONARY PROCEDURES IN A NEW YORK CITY HOSPITAL SYSTEM
Matthew Alexander1 , Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 4
FACTORS INFLUENCING LEUCONOSTOC INFECTION – A SYSTEMATIC REVIEW
Yosef Joseph Rene Amel-Riazat-kesh1 , Samantha Jacobs2
Presented at the American Thoracic Society (ATS) Annual Meeting that was held in San Francisco, California, United States from May 13-18, 2022. 5
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States 6
ACUTE MYOPERICARDITIS IN A YOUNG MALE WITH UNDIAGNOSED GRAVES’ THYROTOXICOSIS
Michel Skaf1 , Juan Arango1 , Loba Alam1, Marni Wilkoff1, Raul Benavides1, Daniel Slack1 , Robert Bernstein1, Vikram Agarwal1, Abel Casso Dominguez1 , Arieh Fox1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
8
LIST OF ABSTRACTS WITH POSTERS
CLINICAL OUTCOMES OF TRACHEOSTOMIZED PATIENTS: COVID-19 VERSUS NON COVID-19
7
Jeeyune Bahk1 , Venus Sharma1 , Bridget Dolan2, Mantej Sembhi1, Jennifer Fung1 , Young Im Lee2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in Washington, DC, United States from May 19-24, 2023.
META-ANALYSIS EVALUATING THE CLINICAL OUTCOMES OF BETA-BLOCKER THERAPY IN PATIENTS WITH HEART FAILURE AND CONCOMITANT COCAINE USE
8
Yoni Balboul1 , Devika Aggarwal2, Arpanjeet Kaur1, Kirtipal Bhatia1, Arshdeep S Dhaliwal3 , Persio D. Lopez3, Basera Sabharwal1, Harsimran Kaur Bhatia4, Ashish Correa1 , Kiran Mahmood1 , Arieh Fox1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Beaumont Hospital, Royal Oak, MI, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Kasturba Medical College, Manipal, India 9
PANCREATIC NEUROENDOCRINE TUMOR PRESENTING AS AN ABDOMINAL PAIN FOLLOWING SUCCESSFUL HELICOBACTER PYLORI ERADICATION
Omar Belfaqeeh1, FrederickRozenshteyn1, Bruce Gelman1
OUTCOMES IN PREMENOPAUSAL PATIENTS WITH HR+/HER2- BREAST CANCER AND LYMPH NODE MICRO-METASTASIS BASED ON THE 21-GENE RECURRENCE SCORE
Nadeem Bilani1 , Rima Patel2, Amy Tiersten2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 10
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that will be held in Chicago, Illinois, United States from June 2-6, 2023 11
TUMOR LYSIS SYNDROME
Conor Buckley1
EXTENSIVE SPLANCHNIC VEIN THROMBOSIS ASSOCIATED WITH COMBINED ORAL CONTRACEPTIVE USE
Salvador Caceros Diaz1 , Jonas Marx1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 12
To be presented at the New York American College of Physician (NYACP) Chapter Resident/Fellow and Medical Student Forum that will be held in Albany, New York, United States on May 12, 2023
9
LIST OF ABSTRACTS WITH POSTERS
ISOLATED THROMBOCYTOPENIA AS AN INITIAL PRESENTATION OF HIV INFECTION IN A PREVIOUSLY HEALTHY MALE
Adrian Chernyk1 , Khalid Dar1
SEVERE GASTROINTESTINAL BLEEDING FOLLOWING TRANSESOPHAGEAL ECHOCARDIOGRAPHY AND ABLATION FOR ATRIAL FIBRILLATION
Christy Chon1 , Frederick Rozenshteyn1, Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 14
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022 15
A RARE CASE OF ESOPHAGEAL SCC WITH APPENDICULAR SKELETAL METASTASIS
Nobel Chowdhury1 , Tabitha Goring2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Memorial Sloan Kettering Cancer Center, New York, NY, United States 16
LATER ONSET OF NRAS-MUTANT METASTATIC MELANOMA IN A PATIENT WITH A PARTIALLY-EXCISED GIANT CONGENITAL MELANOCYTIC NEVUS
Bruno A. Costa1 , Victor Zibara1, Vasundhara Singh1, Omid Hamid2, Sonal Gandhi1 , Andrea P. Moy3, AllisonS. Betof-Warner3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Cedars-Sinai Medical Center, Los Angeles, CA, United States; 3Memorial Sloan Kettering Cancer Center, New York, NY, United States
Published in Frontiers in Medicine, 2022. PMID: 36569151 17
A RARE CASE OF ACUTE INFLAMMATORY DEMYELINATING POLYRADICULOPATHY FOLLOWING PFIZER COVID-19 VACCINE
Vincent Courant1 , Murilo Silva1, Satwant Grewal1, Margrit Wiesendanger2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
ADHERENCE TO NCCN GENETIC TESTING GUIDELINES IN PANCREATIC CANCER AND IMPACT ON TREATMENT
Fionnuala Crowley1 , Sonal Gandhi1, Michelle Rudshteyn2 , Mantej Sembhi1 , Deirdre Cohen2
Presented at the New York State Rheumatology Society (NYSRS) Spring Meeting that was held in New York, New York, United States from May 20-21, 2022. 18
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at American Society of Clinical Oncology (ASCO) Annual Meeting which was held virtually and in person in Chicago, Illinois, United States from June 3-7, 2022.
13
10
LIST OF ABSTRACTS WITH POSTERS
MANAGEMENT OF REFRACTORY HYPOGLYCEMIA IN DOEGE-POTTER SYNDROME WITHOUT AN OPTION FOR CURATIVE SURGERY
19
Katherine Cuan1 , Jeeyune Bahk1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
DIFFERENTIAL DIAGNOSIS OF EAR PAIN AND SWELLING IN AN ELDERLY WOMAN
Doreen Mensah1 ,Lady Njemeh Danso1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in Washington DC, United States from May 19-May 24, 2023 20
Presented at the Society of General Internal Medicine (SGIM) Annual Meeting that was held in Orlando, Florida, United States from April 6-9, 2022. 21
22
IMPROVING ASTHMA DOCUMENTATION AND MANAGEMENT AT A COMMUNITYHEALTH CENTER IN CENTRAL HARLEM
Juan Vasquez Mendez1 , Dalgis J. Dunker1 , Anne Socorro Corrales1, Erick Kawegere1 , Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of General Internal Medicine (SGIM) Annual Meeting that was held in Orlando, Florida, United States from April 6-9, 2022.
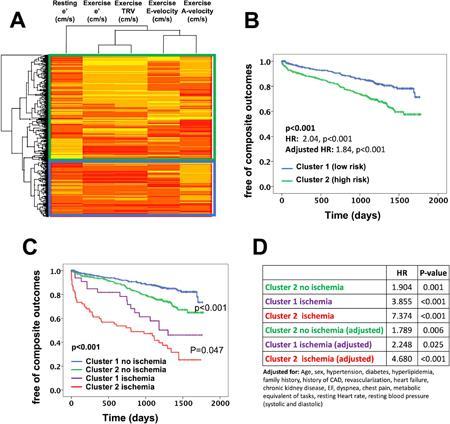
PROGNOSTIC UTILITY OF EXERCISE STRESS ECHOCARDIOGRAPHY IN PATIENTS WITH INDETERMINATE RESTING DIASTOLIC FUNCTION
Joseph Elias1 , Alaa Omar1, Ga Hee Kim1, Swiri Konje1, Loba Alam1, Elizabeth Zipf1 , David Meister1, Christopher Perez Lizardo1, Maria K. Peña1, Brissete Mancero1, Errol Moras1, Kruti Dhaval Gandhi1, Arpanjeet Kaur1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023
REPORT OF INDOOR MOLD EXPOSURE AND RHINITIS IN PRESCHOOL CHILDREN ATTENDING HEAD START CENTERS IN NEW YORK CITY
23
Jin Feng1, Adnan Divjan 2, Luis Acosta2, Andrew Rundle2, Maxine Ashby Thompson2 , Judith S. Jacobson2, Matthew S. Perzanowski2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
Presented at the American Academy of Allergy Asthma and Immunology (AAAAI) Annual Meeting that was held in San Antonio, Texas, United States from February 24-27, 2023.
COST OF CARE AWARENESS AMONG INTERNAL MEDICINE HOUSE STAFF
Madelin Fenianos1 , Alexandria Markley1, Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
24
11
LIST OF ABSTRACTS WITH POSTERS
25
MERCURY INDUCED MEMBRANOUS NEPHROPATHY IN A YOUNG FEMALE
Debbie Marie Fermin1 , Tamara Goldberg1, Karim El Hachem1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Will be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Aurora, Colorado, United States from May 10-13, 2023. 26
PROGNOSTIC VALUE OF EXERCISE ASSOCIATED DIASTOLIC ABNORMALITIES IN PATIENTS WITH ELEVATED RESTING SYSTOLIC BLOOD PRESSURE
Kruti Dhaval Gandhi1, Alaa Omar1, Swiri Konje1, Loba Alam1, Errol C. Moras1, Brissete Mancero1, Elizabeth A. Zipf1 , David Meister1, Arpanjeet Kaur1, Maria K. Peña1, Christopher Perez Lizardo1, Ga Hee Kim1, Joseph Elias1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023
27
IMPACTS OF SOCIAL DETERMINANTS OF HEALTH ON DUAL ANTIPLATELET THERAPY FOR ACUTE CORONARY SYNDROME
Christopher Gold1 , Dipal Patel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Society of General Internal Medicine (SGIM) Annual Meeting that was held virtually from April 21-April 24, 2021.
PREDICTORS OF MORTALITY AFTER TRANS-JUGALAR INTRAHEPATIC PORTOSYSTEMIC SHUNT PROCEDURE
28
Suhail Haddadin1 , Patricia Miguez Arosemena1, Farah Haddadin2 , Rand Fram2 , Samuel J. Daniel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Faculty of Medicine at Jordan University of Science and Technology, Amman, Jordan
Presented at the American Association for the Study of Liver Diseases (AASLD) Annual Meeting held in Washington DC, United States from November 4-8, 2022. 29
SEVERE HYPOPHOSPHATEMIA OCCURRING AFTER RELATED EXPOSURE TO A PARENTERAL IRON FORMULATION
Keerthana Haridas1 , Alice Yau1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Published in Case Reports in Endocrinology, 2022. PMID: 36248222 30
EARLY CONSULTATION TO PALLIATIVE CARE IN THE INTENSIVE CARE UNIT DECREASES LENGTH OF STAY
Ariela Hazan1 , Jeeyune Bahk1, Ariel Gordon1, Mantej Sehmbhi1, Jennifer Fung1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the European Association for Palliative Care Congress (EAPC) that will be held in Rotterdam, Netherlands from June 15-17, 2023.
12
LIST OF ABSTRACTS WITH POSTERS
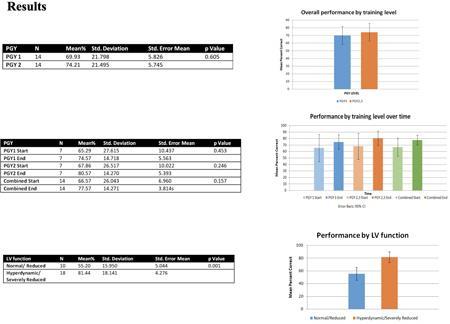
RESIDENT EDUCATION FOR IMPROVED QUALITY AND CONFIDENCE IN INPATIENT HYPERGLYCEMIA
Maxwell E. Horowitz1, Keerthana Haridas1, Sananda Moctezuma1, Rahul Agarwal1
31
1Mount Sinai Morningside-West Hospital Center, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 26, 2022 and at the Endocrine Society Annual Meeting that was held in Atlanta, Georgia, United States from June 11-14, 2022.
SARS-COV-2 INFECTIONS IN INBORN ERRORS OF IMMUNITY: A SINGLE CENTER STUDY
32
Kimberley Cousins1, Nicholas DeFelice1, Stephanie Jeong1, Jin Feng2, Ashley Sang Eun Lee1, Karina Rotella1 , David Sanchez1 , Faris Jaber2, Shradha Agarwal1, Hsi-en Ho1 , Charlotte Cunningham-Rundles1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in Frontier’s Immunology, 2022. PMID: 36479106
A NOVEL SIMULATION BASED APPROACH TO IMPROVE INTERNAL MEDICINE RESIDENTS’ CONFIDENCE AND KNOWLEDGE IN PERFORMING BEDSIDE CARDIAC POINT-OF-CARE ULTRASOUND
33
Arpanjeet Kaur1 , Arshdeep Dhaliwal2, Yoni Balboul1, Barbara Karagiannis1, Harrindra
Seepersaud1, Priscilla Loanzon1, Susannah Kurtz1, Adam Rothman1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Mount Sinai Institute of Medical Education Annual Research Day in New York, New York, United States on April 27, 2023. 34
ATYPICAL PRESENTATION AND DIAGNOSIS OF AIDS-RELATED CMV ENCEPHALITIS
Erick Kawegere1, Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in BMJ Case Reports, 2022. PMID: 36041775 35
PREVALENCE AND IMPACT OF TWILIGHT CRITERIA IN ALL-COMER PATIENTS UNDERGOING PERCUTANEOUS CORONARY INTERVENTION
Alessandro Spirito1 , Won Joon Koh2, Sartori Samantha1, Clayton Snyder1, Johny
Nicholas1, Davide Cao1, Birgit Vogel1, Vahid Rezvanizadeh1, Usman Baber3 , Joseph
Sweeny1 , Samin K. Sharma1 , Annapoorna Kini1, George Dangas1 , Roxana Mehran1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3University of Oklahoma Health Sciences Center, Oklahoma City, OK, Unites States
Presented at the European Society of Cardiology (ESC) Congress Meeting that was held in Barcelona, Spain from August 27-30, 2022.
13
LIST OF ABSTRACTS WITH POSTERS
36
A CASE OF PLASMODIUM FALCIPARUM MALARIA
Sanam Lama1 , Anjali Ajit1,2 , Vani Gandhi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
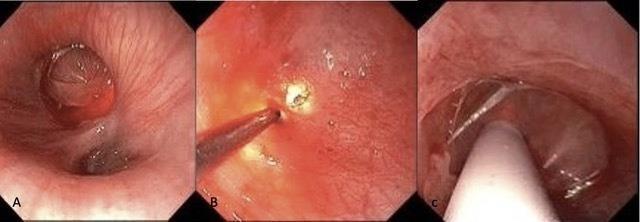
LIQUID NITROGEN SPRAY CRYOTHERAPY IN THE ESOPHAGUS PERFORMED WITH MINIMAL BLEEDING RISK REGARDLESS OF CONCURRENT ANTITHROMBOTIC THERAPY
37
Neil R. Sharma1, Abhilash Perisetti1 , Randy M. Leibowitz2, Mantej Sehmbhi 2, Erica Park2 , Zubair A. Malik3 , Kamran R. Mushtaq1, Christina M. Zelt1, Nicholas J. Talabiska3 , Jeremy Klein3, Carolyn T. Hogan3 , Michael S. Smith2
1Parkview Regional Medical Center Fort Wayne, IN, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 3Temple University Hospital, Philadelphia, PA, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in San Diego, California, United States from May 21-24, 2022.
38
IN-HOSPITAL OUTCOMES OF TAVR IN PATIENTS WITH CHRONIC KIDNEY DISEASE
Marta Lorente-Ros1, Subrat K Das1, José S. Aguilar-Gallardo1, Francisco J. Romeo1 , Amisha Patel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Transcatheter Cardiovascular Therapeutics (TCT) Annual Meeting that was held in Boston, Massachusetts, United States from September 16-19, 2022. 39
DELAYED DIAGNOSIS OF PULMONARY VEIN OCCLUSION AFTER ATRIAL FIBRILLATION ABLATION
Sara Luby1 , Jonathan M Oxman1 , Deepanjali Nair1, Alba Muñoz Estrella1 , Javier J Zulueta1
DETERMINANTS OF COVID-19 VACCINE HESITANCY IN A PREDOMINANTLY BLACK POPULATION WITH CUTANEOUS LUPUS ERYTHEMATOSUS
Sophia Lutgen1, S. Sam Lim2, Laura D. Aspey2, Gaobin Bao2, Charmayne DunlopThomas2, Jessica N. Williams2, Cristina Drenkard2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 40
2Emory University, Atlanta, GA, United States
Presented at the American College of Rheumatology Convergence Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 10-14, 2022. 41
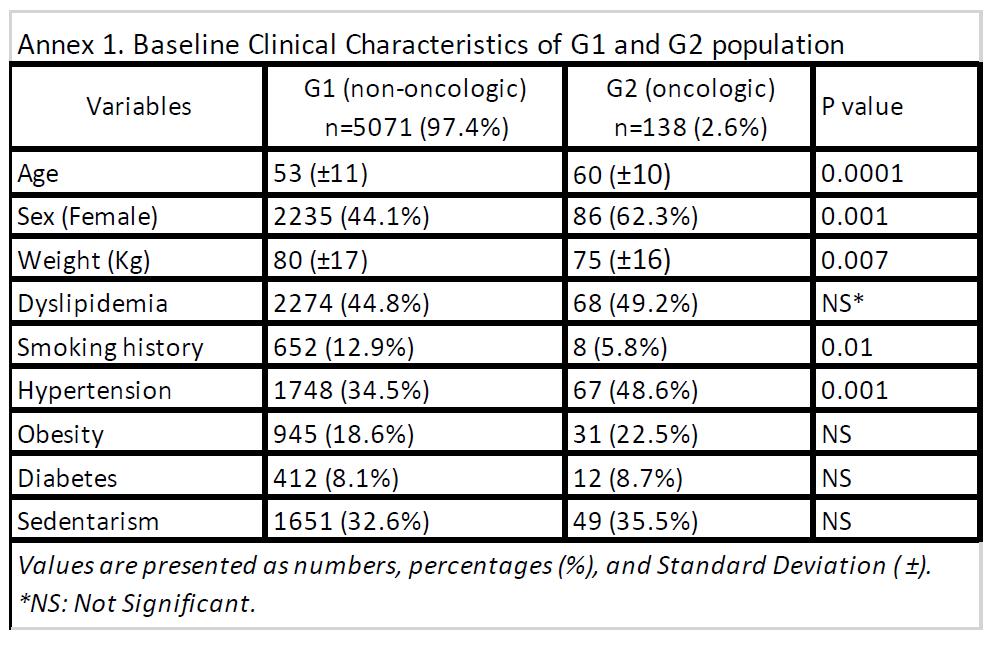
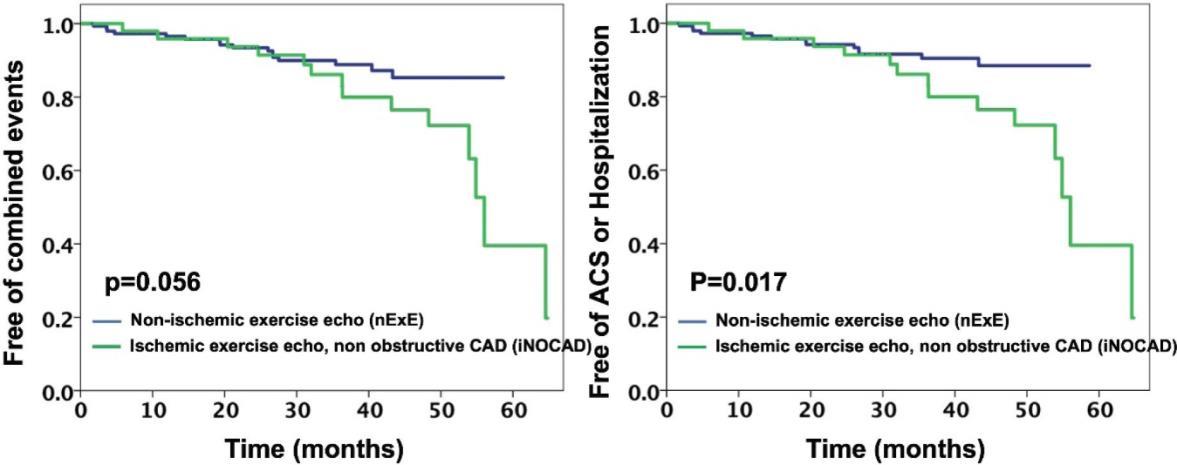
PROGNOSTIC SIGNIFICANCE OF EXERCISE-INDUCED MYOCARDIAL ISCHEMIA IN PATIENTS WITH ANGIOGRAPHICALLY NORMAL CORONARIES COMPARED TO PATIENTS WITH NORMAL EXERCISE ECHOCARDIOGRAPHY
Brissete Mancero1, Alaa Omar1, Ga Hee Kim1, Elizabeth A. Zipf1, Joseph Elias1 , David Meister1, Maria K. Peña1, Christopher Perez1, Kruti Dhaval Gandhi1 , Arpanjeet Kaur1, Errol C. Moras1, Robert Leber1, Nitin Barman1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
14
LIST OF ABSTRACTS WITH POSTERS
PATIENTS WITH ELEVATED UPPER ESOPHAGEAL SPHINCTER PRESSURES ARE LESS LIKELY TO PRESENT WITH ATYPICAL SYMPTOMS OF GASTROESOPHAGEAL REFLUX DISEASE
42
Alexandria Markley1, Nour Al Khalili1, Emily Seltzer1, Mantej Sehmbhi1 , Kimberly Cavaliere1, Daniela Jodorkovsky1, Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023.
IMPROVEMENT OF PERIMENSTRUAL ACNE WITH CLINDAMYCIN PHOSPHATE
43
1.2% AND BENZOYL PEROXIDE 3.75% COMBINATION GEL: AN INTERVENTIONAL PILOT STUDY
Olga Marushchak1, Matthew Gagliotti2, Anjali S. Vekaria2, Gary Goldenberg2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
IDENTIFICATION OF AN OPTIMAL METHOD FOR ECHOCARDIOGRAPHIC RIGHT VENTRICULAR MASS ESTIMATION IN A SWINE MODEL OF PULMONARY HYPERTENSION
Jonas Marx1 , Tomoki Sakata2, Renata Mazurek2, Anjali Ravichandran2 , Spyros
Mavropoulos2 , Taro Kariya2, Kiyotake Ishikawa2
Published in Journal of Clinical and Aesthetic Dermatology, 2022. PMID: 36381180 44
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Society of Echocardiography Annual Scientific Sessions that will be held in National Harbor, Maryland, United States from June 23-26, 2023.
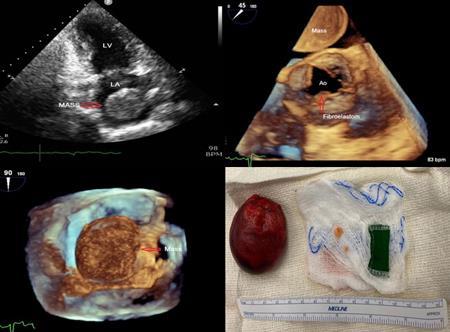
LARYNGEAL SYNOVIAL SARCOMA THAT METASTASIZED TO THE HEART
Christopher N. Matthews1 , Syed Farrukh Mustafa1 , Sidra Salman1 , Akshaya
Gopalakrishnan1, James Salonia1 , Deepika Misra1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
DIASTOLIC STRESS ECHOCARDIOGRAPHY IN PATIENTS WITH NORMAL RESTING DIASTOLIC FUNCTION: PROGNOSTIC UTILITY IN PRESENCE AND ABSENCE OF MYOCARDIAL ISCHEMIA
46
Loba Alam1, Alaa M. Omar1, Swiri Konje1, Kruti Gandhi1, Errol Moras1 , David Meister1 , Maria Peña1, Christopher Perez Lizardo1, Brisette Mancero1, Elizaebth Zipf1, Ga Hee Kim1 , Joseph Elias1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Barcelona, Spain from August 27-30, 2022.
45
15
LIST OF ABSTRACTS WITH POSTERS
47
CLINICAL SYMPTOMS NOT CONGRUENT WITH DIAGNOSTIC TESTING: A PERIPHERAL ARTERIAL DISEASE CASE
Jiaxi Miao1, Christopher N. Matthews1 , Doreen Mensah1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 48
COMPARISON BETWEEN MEN AND WOMEN WITH SEVERE OBESITY FOR RISK OF ADVERSE OUTCOMES OF MYOCARDIAL ISCHEMIA: AN EXERCISE STRESS ECHOCARDIOGRAPHIC STUDY
Errol Moras1, Kruti Gandhi1, Joseph Elias1, David Meister1, Maria Peña1, Christopher Perez Lizardo1, Brissete Mancero1, Ga Hee Kim1, Elizabeth Zipf1, Loba Alam1, Swiri
Konje1, Alaa M. Omar1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
49
CHECKPOINT IMMUNOTHERAPY-INDUCED MYOCARDITIS REQUIRING MECHANICAL CIRCULARLY SUPPORT: A CASE REPORT AND FUTURE OUTLOOK
Anna Sophie Mueller 1 , Ashish Correa1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
UNIVERSAL PROTOCOLIZED ALCOHOL BIOMARKER SCREENING IS EFFECTIVE IN DETECTING HIGH RATES OF ALCOHOL-RELATED CONTRAINDICATIONS TO LIVER TRANSPLANTATION
50
Rohit Nathani1, Adam Winters2, Chip Bowman- Zamora2, Jonathan Nahas3, Sander S. Florman2, Thomas D. Schiano2 , Gene Y. Im2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3University of Pennsylvania, Philadelphia, PA, United States
Presented at the American Association for the Study of Liver Diseases (AASLD) Annual Meeting held in Washington DC, United States from November 4-8, 2022.
THE UTILITY OF HEREDITARY THROMBOPHILIA TESTING AMONG PATIENTS WITH UNPROVOKED VENOUS THROMBOEMBOLISM
51
Cristina Olivo Freites1 , Leonard Naymagon2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in the International Journal of Laboratory Hematology, 2022.
PMID: 34749438
MEDICAL EDUCATION IN THE POST-COVID ERA: ATTITUDES AND PERCEPTIONS OF VIRTUAL VESUS IN-PERSON EDUCATION IN INTERNAL MEDICINE RESIDENTS AND FACULTY
52
Ricardo J. Ortiz1 , Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
16
LIST OF ABSTRACTS WITH POSTERS
53
CANDIDA PARAPSILOSIS PROSTHETIC VALVE ENDOCARDITIS
Maria Peña1 , Mudita Patel1, Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
A CASE OF ANAPHYLAXIS FOLLOWING ULTRASOUND CONTRAST AGENT
54
Christopher Perez Lizardo1 , Foram Parikh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
EVALUATION OF THE AGREEMENT AND PREDICTIVE PERFORMANCE OF CARBAPENEM RESISTANT ENTEROBACTERALES RISK PREDICTION MODELS IN HOSPITALIZED PATIENTS
55
Hendrik Sy1 , Carlos Plazola1, Arsheena Yassin2 ,, Kristy Huang1 , Mukti Patel1, Lina Loaiza1, Samuel Acquah3, Sara Radparvar3, Christine Stavropoulos1, Joseph Mathew1 , Andras Farkas1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Bon Secours Charity Health System, Suffern, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the 32nd European Congress of Clinical Microbiology and Infectious Diseases that was held Lisbon, Portugal from April 23-26, 2022.
EFFECT OF INHALED EPOPROSTENOL ON OXYGENATION IN COVID-19 PATIENTS WITH ACUTE HYPOXEMIC RESPIRATORY FAILURE
56
Maria Athena Riego1, Natasha Garg2, Omar Mahmoud3, Elizabeth Zipf1 , Dishant Shah4 , Edith Robin1, Abhinav Hoskote5, Arpanjeet Kaur1, Sara Luby1, Venus Sharma1 , Raymonde Jean1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Jamaica Hospital Medical Center, Jamaica, NY, United States; 3University of Maryland Medical Center, Baltimore, MD, United States;
4Westchester Medical Center, Valhalla, NY, United States; 5Holy Spirit Medical Center, Camp Hill, PA, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Nashville, Tennessee, United States from October 16-19, 2022
OUTCOMES OF CHRONIC TOTAL OCCLUSION RECANALIZATION IN PATIENTS WITH PRIOR BYPASS SURGERY: AN UPDATED SYSTEMATIC REVIEW AND METAANALYSIS OF REAL WORLD REGISTRIES
57
Francisco José Romeo1, Francesco Moroni2, Marco Giuseppe Del Buono3,4, Juan Ignacio Damonte5, Juan Guido Chiabrando5
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2University of Virginia, Charlottesville, Virginia, United States; 3Catholic University of the Sacred Heart, Rome, Italy;
4Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; 5Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
A CASE OF LAUGHING HER WAY TO VITAMIN B12 DEFICIENCY
58
Norah Sadek1, Bharat Monga1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
17
LIST OF ABSTRACTS WITH POSTERS
IMPROVING RESIDENT CONTINUITY OF CARE AT AN URBAN FEDERALLY QUALIFIED HEALTH CENTER
59
Salvador Caceros1 , Sharel Sadud-Armaza1 , Errol Morras1 , Bailey Perry1 , Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Will be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Aurora, Colorado, United States from May 10-13, 2023.
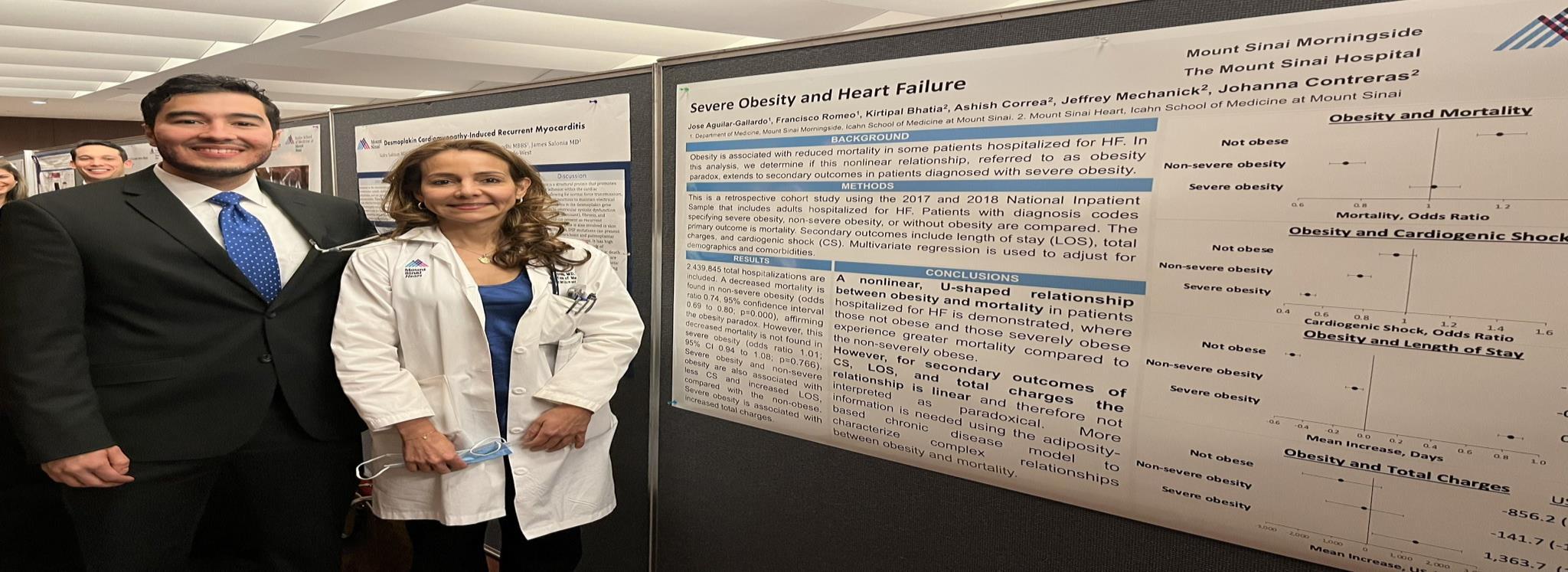
INCREASING HEPATITIS C VIRUS SCREENING ACROSS INNER CITY COMMUNITY CLINICS
60
Mantej Sehmbhi1 , Emily S. Seltzer1, Nour Al Khalili1 , Shabari Shenoy1 , Patricia Miguez
Arosemena1 , Geeta Varghese1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022
PRODUCING PAINLESS PEG CONSULTS: A PILOT QUALITY OF CARE STUDY TO IMPROVE PERCUTANEOUS ENDOSCOPIC GASTROSTOMY TUBE PLACEMENT WORKFLOW AND OUTCOMES
61
Emily S. Seltzer1 , Erica Park1,2, Patricia Miguez Arosemena1, Omar Belfaqeeh1 , Michael S. Smith1, Janet M. Shapiro1, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023.
62
VALACYCLOVIR ASSOCIATED NEUROTOXICITY IN A PATIENT WITH END STAGE RENAL DISEASE
Venus Sharma1 , Rohit Rajesh Nathani1 , Ayush Gandhi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
TRENDS IN SCREENING AND PREVENTION OF ANORECTAL AND COLON CANCER IN TRANSGENDER PEOPLE
63
Shabari Mangalore Shenoy1, Shanique Wilson Noack1,2, Emily Seltzer1 , Omar Belfaqeeh1, Patricia Miguez Arosemena1, Emilia Bagiella3, Amreen Dinani3 , Ilan Weisberg2, Joshua D. Safer3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States 64 A RARE CASE OF A MIDDLE MEDIASTINAL NEUROENDOCRINE TUMOR
Connor Smith1, Galit Balayla Rosemberg1, Krystle Hernandez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
18
LIST OF ABSTRACTS WITH POSTERS
65
CONCOMITANT GOUTY AND GONOCOCCAL POLYARTHRITIS IN A TRAVELER. Anne Socorro Corrales1, Yousef Ali1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
GLUCOCORTICOID THERAPY FOR MANAGEMENT OF HYPOGLYCEMIA IN THE CONTEXT OF NON-ISLET CELL TUMOR-INDUCED HYPOGLYCEMIA
66
Juan Vasquez Mendez1 , Rahul Agarwal1 , Susel Rodriguez Ortega1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Endocrine Society Annual Meeting that was held in Atlanta, Georgia, United States from June 11-14, 2022.
COMPARISON OF CHARACTERISTICS OF VACCINATED VERSUS UNVACCINATED PATIENTS ADMITTED WITH COVID-19 IN THE MOUNT SINAI HEALTH SYSTEM
67
Vani George1, Chi Doan Huynh2, Jordan Ehni1 , Kristine Rabii1, Alan Weinberg1 , Aarohi Vora3 , Marie Moss1, Waleed Javaid1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Ryan Health, New York, NY, United States; 3Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BURKITT LYMPHOMA INDUCED PSEUDOACHALASIA WITH DRAMATIC SYMPTOMATIC IMPROVEMENT POST-CHEMOTHERAPY
68
Marni H. Wilkoff1 , Emily S. Seltzer1 , Allison E. Wang1,2 , Bruno Almeida Costa1 , Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States 69
CANNABIS TOXICITY FROM STREET PERCOCET TREATED WITH NALOXONE
Eelin Wilson1 , Mohammed Khan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 70
COMPARISON OF THREE-YEAR OUTCOMES OF DRUG-COATED BALLOON ANGIOPLASTY IN TOTALLY OCCLUSIVE VERSUS NON-OCCLUSIVE IN-STENT RESTENOSIS OF DRUG-ELUTING STENTS
Zhuoran Yang1, Jiasheng Yin2, Yaqi Zhang3, Nirupama Krishnamurthi1, Lingling Wu4 , Jacqueline E. Tamis-Holland1, Junbo Ge2 ,
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
SUCCESSFUL BRENTUXIMAB VEDOTIN AND NIVOLUMAB THERAPY OF MULTIPLY REFRACTORY DIFFUSE LARGE B-CELL LYMPHOMA WITH HODGKIN FEATURES
Victor Zibara1, Filiz Sen2, Michael Scordo2, Lorenzo Falchi2
2Zhongshan Hospital, Fudan University, Shanghai Institute of Cardiovascular Diseases, Shanghai, China; 3John H. Stroger Jr. Hospital of Cook County, Chicago, IL, United States; 4University of Alabama Birmingham, Birmingham, AL, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023. 71
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Memorial Sloan-Kettering Cancer Center, New York, NY, United States
Published in Leukemia and Lymphoma, 2022. PMID: 36120859
19
Abstracts with Posters
ABSTRACT #1
CLINICAL RESEARCH CARDIOLOGY
SEVERE OBESITY AND HEART FAILURE
José S. Aguilar-Gallardo1 , Francisco J. Romeo1, Kirtipal Bhatia1, Ashish Correa1, Jeffrey Ian Mechanick2 , Johanna P. Contreras2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in American Journal of Cardiology. 2022. PMID: 35705429
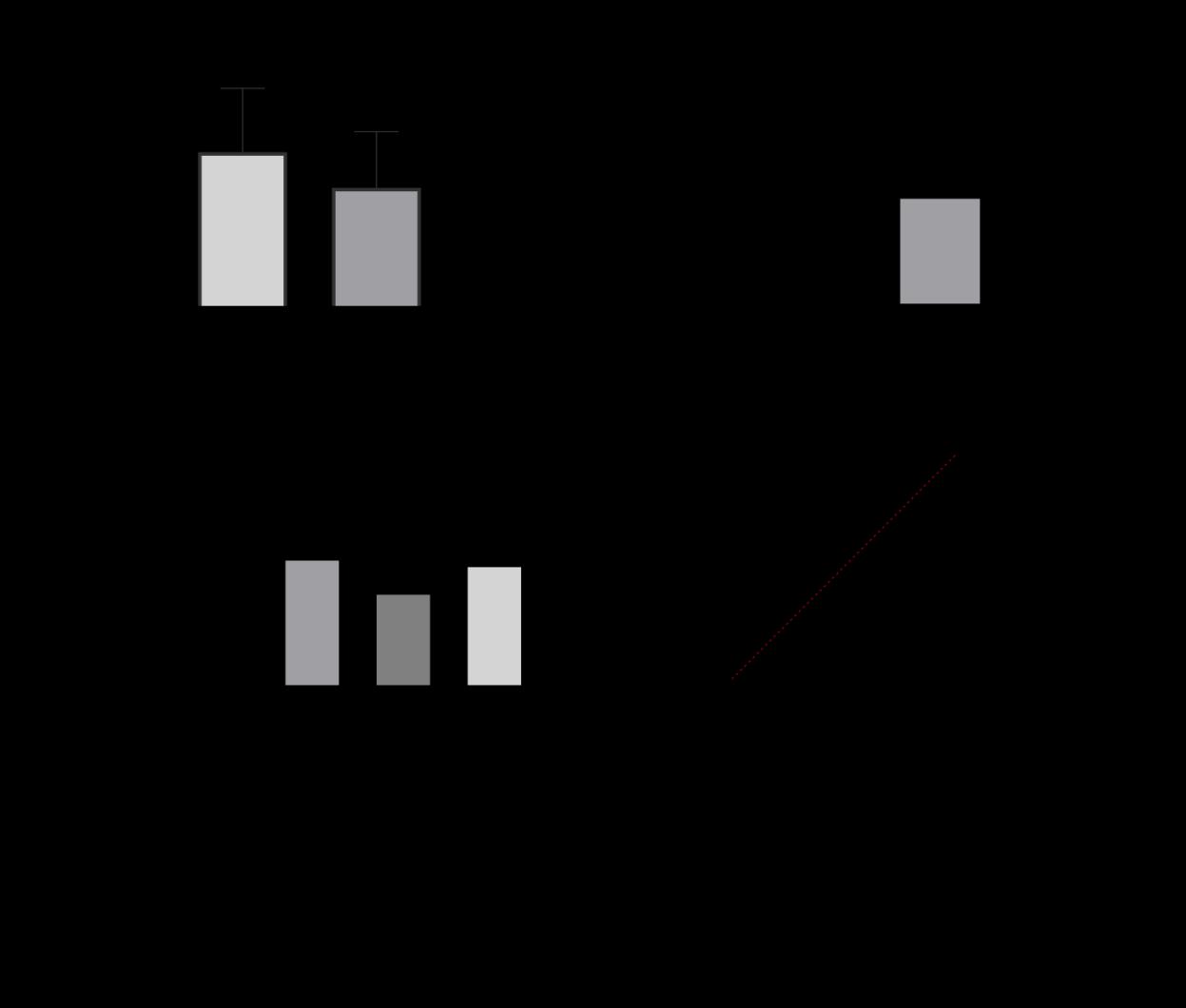
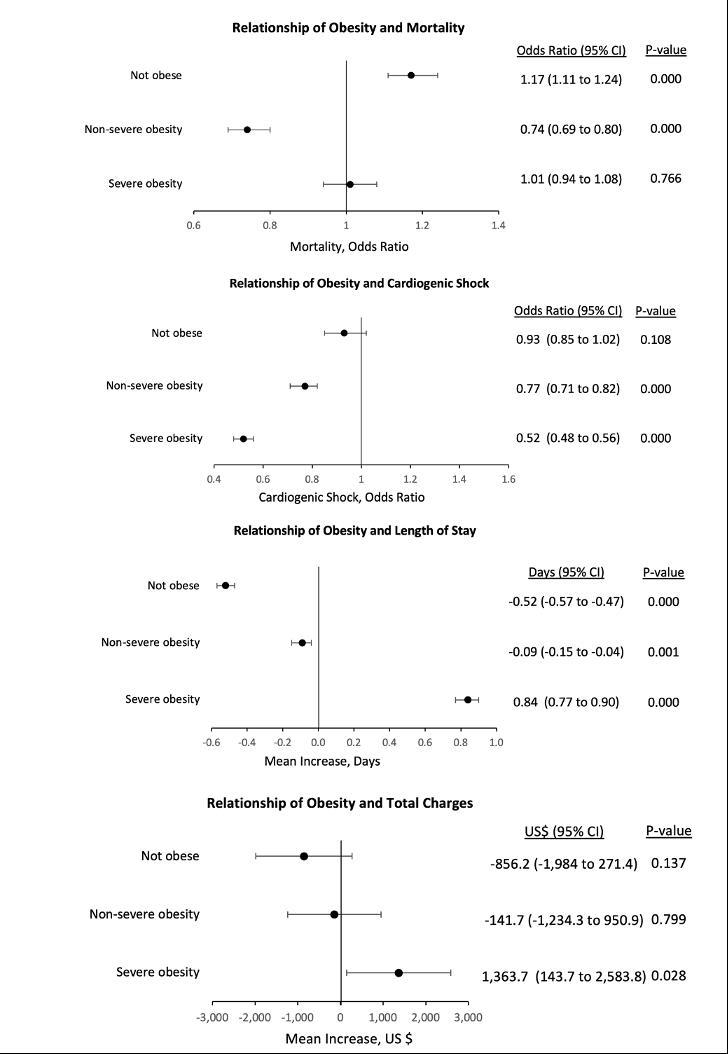
BACKGROUND/INTRODUCTION: Obesity is associated with reduced mortality in some patients hospitalized for heart failure (HF). In this analysis, we determine if this nonlinear relationship, referred to as obesity paradox, extends to secondary outcomes in patients diagnosed with severe obesity.
METHODS: This is a retrospective cohort study using the 2017 and 2018 National Inpatient Sample that includes adults hospitalized for HF. Patients with diagnosis codes specifying severe obesity, non-severe obesity, or without obesity are compared. The primary outcome is mortality. Secondary outcomes include length of stay (LOS), total charges, and cardiogenic shock (CS). Multivariate regression is used to adjust for demographics and comorbidities.
RESULTS: A total of 2,439,845 hospitalizations are included. A decreased mortality is found in non-severe obesity [odds ratio (OR), 0.74; 95% CI, 0.69-0.80; p=0.000], affirming the obesity paradox. However, this decreased mortality is not found in severe obesity (OR, 1.01; 95%CI, 0.94 - 1.08; p=0.766). Severe obesity and non-severe obesity are also associated with less cardiogenic shock and increased length of stay, compared with the non-obese. Severe obesity is associated with increased total charges.
CONCLUSION: A nonlinear, U-shaped relationship between obesity and mortality in patients hospitalized for HF is demonstrated, where those not obese and those severely obese experience greater mortality compared to the non-severely obese. However, for secondary outcomes of cardiogenic shock, length of stay, and total charges the relationship is linear and therefore not interpreted as paradoxical. More information is needed using the adiposity-based chronic disease model to characterize complex relationships between obesity and mortality.
21
Figure 1: Relationship of Obesity and Hospital Outcomes in Heart Failure
22
ABSTRACT #2
CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
EVALUATING SERUM FREE LIGHT CHAIN RATIO AS A BIOMARKER FOR MULTIPLE MYELOMA
Theresia Akhlaghi1 , Kylee Maclachlan2, Neha Korde2 , Sham Mailankody2, Alexander Lesokhin2 , Hani Hassoun2 , Sydney X. Lu2, Dhwani Patel2 , Urvi Shah2, Carlyn Tan2, Andriy Derkach2 , Oscar Lahoud2 , Heather J. Landau2, Gunjan L. Shah2 , Michael Scordo2, David J. Chung2, Sergio A. Giralt2 , Saad Z. Usmani2 , Ola Landgren3, Malin Hultcrantz2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Memorial Sloan Kettering Cancer Center, New York, NY, United States; 3University of Miami, Miami, FL, United States Presented at the American Society of Clinical Oncology Annual Meeting (ASCO) that was held both virtually and in Chicago, Illinois, United States from June 3-7, 2022
BACKGROUND/INTRODUCTION: In 2014, the definition of multiple myeloma (MM) was updated to include serum free light chain ratio (FLCr) 100 as a myeloma defining biomarker, based on retrospective data indicating a 2-year progression rate of 80% and a median time to progression (TTP) of 12 months associated with this marker. However, more recent studies have reported lower 2-year progression rates, 30-44%, and a longer median TTP of 40 months in patients with FLCr 100. Because of the disparity in risk prediction by FLCr across studies, we aimed to assess the risk of progression in patients with smoldering multiple myeloma (SMM) and FLCr 100.
METHODS: We performed a retrospective analysis of patients with SMM diagnosed between 2002 to 2019. Diagnosis of SMM and progression to MM requiring therapy was defined according to the International Myeloma Working Group (IMWG) criteria at the time of diagnosis. Only patients with available free light chains (FLCs) at diagnosis of SMM were included in the study and only patients with an involved FLC level >100 mg/L were included in the FLCr 100 group. Chi-square test was used to compare categorical values and Mann-Whitney U test to compare continuous variables between the < 100 and 100 FLCr group. Kaplan-Meier method was used to determine TTP and generate survival curves, with log-rank tests for comparison between groups.
RESULTS: A total of 466 patients were included in the study, of which 65 patients (14%) had a FLCr 100. Light chain MM was more prevalent in the FLCr 100 group (14% versus 2.8% among patients with FLCr < 100, p<0.001). Patients with FLCr 100 had overall higher Mayo-2018 risk, where 14% had 3 risk factors compared to 4% in patients with FLCr<100, 39% had 2 risk factors compared to 19% with FLCr<100, and 48% had 1 risk factor compared to 29% with FLCr<100 (p<0.001). In the FLCr 100 group, the median TTP was 32 months compared to 108 months in patients with FLCr <100 (p<0.001). At 2 years, 38% of patients with FLCr 100 had progressed. To identify patients in the FLCr 100 group with a higher risk of progression, we stratified the patients based on number of Mayo-2018 risk factors. Patients with 2 risk factors in addition to FLCr (BMPC >20% and M-spike >2g/dL) had a median TTP of 17 months and 2-year progression rate of 89%, compared to a median TTP of 31 months and 59 months, and 2-year progression rate of 45% and 24%, in patients with 1 and no additional risk factors, respectively (p=0.0024).
CONCLUSION: To conclude, we found that FLCr 100 is not an independent risk factor of imminent progression from smoldering multiple myeloma to active multiple myeloma. On the contrary, patients with FLC 100 were a heterogenous group with varying disease risk, where those with both BMPC >20% and M-spike >2g/dL indeed progressed within 2 years, while those with no other risk factors had a median TTP of 5 years before progressing. These findings suggest that patients with FLCr 100 as the sole myeloma defining event and otherwise lowintermediate risk disease may be considered for observation rather than early treatment.
23
ABSTRACT #3
CLINICAL RESEARCH GASTROENTEROLOGY
PROTON PUMP INHIBITOR USE DOES NOT AFFECT MANOMETRIC PARAMETERS IN PATIENTS WITH GASTRO-ESOPHAGEAL REFLUX CONFIRMED ON QUANTITATIVE TESTING
Nour Al Khalili1 , Mantej Sembhi1, Patricia Miguez Arosemena1 , Kimberly Cavaliere1, Daniela Jodorkovsky1 , Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: High Resolution Esophageal Manometry (HRM) provides qualitative and quantitative assessment of both peristalsis and sphincter function. Gastroesophageal reflux disease (GERD) may adversely affect peristaltic function, though proton pump inhibitor (PPI) use may mitigate changes. Accurate assessment of contractility is important in the selection of anti-reflux surgery approach. Recent guidelines suggest testing for GERD off PPI, a shift from prior recommended testing on PPI for patients with high suspicion of GERD. The aim of this study was to evaluate whether performing GERD evaluations off PPI alters HRM contractility findings and thus surgical approach.
METHODS: All patients undergoing HRM and multichannel intraluminal impedance-pH testing (MII-pH) for suspected GERD at a high-volume center between 2020 and 2022 were reviewed. Patients with prior foregut endoscopic or surgical interventions, eosinophilic esophagitis, or achalasia were excluded. Those with an abnormal MII-pH were included, defined as at least 80 reflux events, a distal acid exposure time (AET) of ≥2%, or a DeMeester score >14.72 on twice daily PPI, and at least 80 reflux events or AET ≥6% off PPI. Statistical analysis to compare both groups was performed, including adjustments for age, gender, and body mass index
RESULTS: Of 520 MII-pH cases, 102 patients met inclusion criteria (61 off PPI, 41 on PPI). All patients on twice daily PPI had AET>2%, 34 (83%) had a DeMeester score >14.72, and only 8 (19.5%) had 80+ reflux episodes. There were no significant differences in gender, body mass index, age, or HRM hiatal hernia size between groups. Patients off PPI had significantly higher upright and postprandial AET and normalized acid reflux episodes, while increased total normalized reflux activity, DeMeester score, and total distal AET did not reach statistical significance. Manometric parameters including lower esophageal sphincter pressures, distal latency, percent ineffective swallows (defined as distal contractile integral less than 450 mmHg-cm-s), percent complete bolus clearance, and Chicago classification diagnosis also were not significantly different between groups. Of note, mean distal contractile integral tended to be higher in patients off PPI, though this also was not significant (p=0.997).
CONCLUSION: PPI use did not affect core manometric parameters in patients with excess gastroesophageal reflux on MII-pH determined by AET, DeMeester score or number of reflux events. Of interest, patients diagnosed with refractory GERD had a significantly greater reflux burden despite high dose PPI therapy. Such findings underscore the validity of recent changes in the recommended GERD diagnostic algorithm, as peristalsis appears unaffected by the absence of PPI from a patient’s regimen. It appears HRM results off PPI may therefore be reasonable to use when selecting an approach to anti-reflux surgery.
24
Table 1: Demographics and MII-pH Findings for Patients with Reflux off and on PPI
Table 2: Manometric Findings for Patients with Reflux Off and On PPI
Off PPI Group On BID PPI Group p-Value N 61 41 Gender = Male (%) 27 (44.3) 15 (36.6) 0.539 Age (mean (SD)) 50.08 (16.18) 47.27 (16.60) 0.396 BMI (mean (SD)) 28.65 (6.79) 27.89 (6.96) 0.586 pH-Impedance parameters DeMeester Score (mean (SD)) 51.23 (46.24) 48.86 (44.75) 0.797 Distal AET% (total, mean (SD)) 12.99 (12.94) 11.38 (10.98) 0.514 Distal AET% (upright, mean (SD)) 26.29 (31.71) 14.54 (16.71) 0.032* Distal AET% [post prandial, mean (SD)] 27.71 (29.82) 16.70 (19.07) 0.039* Distal AET% [supine, mean (SD)] 27.52 (35.58) 19.17 (21.55) 0.186 Normalized All Reflux [mean (SD)] 58.73 (35.09) 51.22 (34.35) 0.291 Normalized Acid Reflux [mean (SD)] 38.73 (21.45) 21.24 (21.31) <0.001* Normalized weakly acid reflux [mean (SD)] 20.00 (24.45) 29.88 (26.40) 0.057 Normalized nonacid reflux [mean (SD)] 0.22 (1.20) 0.07 (0.35) 0.449 BMI: body mass index, AET: Acid exposure time.
Off PPI Group On BID PPI Group p-Value N 61 41 Manometric parameters LES respiratory pressure, mean (SD) 23.26 (15.30) 20.92 (13.68) 0.433 IRP (median [IQR]) 9.70 (4.90, 14.00) 8.50 (4.30, 13.00) 0.311 Hiatal hernia = Yes (%) 49 (80.3) 35 (85.4) 0.697 Hiatal hernia size, mean (SD) 2.44 (1.43) 2.15 (1.19) 0.333 % Peristaltic, [median (IQR)] 85.00 (50.00, 100.00) 70.00 (40.00, 100.00) 0.576 % Incomplete bolus clearance, [median (IQR)] 60.00 (40.00, 100.00) 70.00 (20.00, 90.00) 0.885 Distal latency ([median (IQR)] 6.40 (5.45, 7.50) 6.30 (5.80, 6.85) 0.655 DCI (mean) [median (IQR)] 972.10 (475.55, 1522.50) 884.40 (453.75, 1608.00) 0.997 DCI (highest) {median (IQR)] 1451.75 (886.20, 2527.38) 1429.10 (731.80, 2615.10) 0.763 Chicago Classification (%) 0.75 Absent contractility 2 (3.3) 2 (4.9) Distal esophageal spasm 1 (1.6) 2 (4.9) EGJ outflow obstruction 13 (21.3) 7 (17.1) Ineffective esophageal motility 21 (34.4) 17 (41.5) No Chicago classification abnormality 24 (39.3) 13 (31.7) LES: lower esophageal sphincter, IRP: integrated relaxation pressure, DCI: Distal contractile integral, EGJ: Esophagogastric junction. 25
ABSTRACT #4 CLINICAL RESEARCH INFECTIOUS DISEASES/PULMONARY/CRITICAL CARE
THE EFFECTS OF COVID-19 ON PULMONARY PROCEDURES IN A NEW YORK CITY HOSPITAL SYSTEM
Matthew
Alexander1 , Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Thoracic Society(ATS) Annual Meeting that was held in San Francisco, California, United States from May 13-18, 2022.
BACKGROUND/INTRODUCTION: While it is clear that the COVID-19 pandemic has wreaked havoc on the healthcare system in the United States, it is less certain how it has impacted the medical training of residents and fellows. This retrospective study aimed to analyze how the pandemic has affected the procedural numbers performed by pulmonary and critical care fellows in a New York City hospital system.
METHODS: Procedural data performed by pulmonary and critical care fellows at three New York City hospitals from March 15, 2019 through March 15, 2021 were retrospectively obtained. There were 1090 procedures included, divided among bronchoscopy, small-bore chest tube placement, thoracentesis, and endobronchial ultrasound (EBUS). March 2020 was selected as the midway point for the data collection, as this was when the outpatient procedure suites were closed at the height of the pandemic.
RESULTS: The average number of bronchoscopies performed per month pre-COVID-19 was 19. Following the procedure suite closures, this number dropped to 5 in April and 8 in May, increased to 12 in June, and returned to pre-COVID numbers by July. The monthly average for chest tube placement pre-COVID was 5. This number interestingly increased to 13 in April, decreased to 3 in May and 2 in June, and then returned to pre-COVID levels in July. The average monthly number of endobronchial ultrasounds performed pre-COVID-19 was 8. This dropped to 0 from March to May, increased to 2 in June (after the suites were reopened), and increased to an above-baseline value of 10 in July. The monthly average for thoracenteses pre-COVID was 11. This number decreased to just 3 in April and 4 in May, but subsequently returned to 11 in June and 12 in July. This data is summarized in Figure 1.
CONCLUSION: During the initial wave of the COVID-19 pandemic (March to May 2020), there was a decrease in the number of procedures performed by pulmonary and critical care fellows with the exception of small-bore chest tubes, which transiently increased in frequency. As the number of procedures that fellows perform can directly affect their competency, reliability, and confidence in completing these procedures, it is likely that these transient changes in numbers have impacted their training. Further studies are needed to assess the impact of COVID-19 on fellowship training, and plans should be implemented to minimize these suspected effects.
26

27
Figure 1: Number of Pulmonary Procedures by Date of Procedure
ABSTRACT #5
CLINICAL RESEARCH INFECTIOUS DISEASES
FACTORS INFLUENCING LEUCONOSTOC INFECTION – A SYSTEMATIC REVIEW
Yosef
Joseph Rene
Amel-Riazat-kesh1 , Samantha Jacobs2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Leuconostoc is a genus of vancomycin-resistant gram-positive cocci emerging as an opportunistic pathogen of immuno-compromised and critically unwell populations. While Leuconostoc species have been implicated in infection of multiple sites in adults and children, little work has focused on adult infection and associated factors.
METHODS: Here, we systematically analyze the adolescent/adult case literature around Leuconostoc infection, searching the Pubmed and Google Scholar databases to identify 58 studies meeting inclusion criteria, reviewing 74 cases (all aged 16 years or over), and examining patient characteristics. These include: location, age, gender, comorbidities, malignancy, surgical history, recent antibiotics, and presence of indwelling lines. Chi squared independence analysis was carried out for several factors against survival. Rates of co-infection, antimicrobial therapy, line removal, and survival were also collected.
RESULTS: Cases of Leuconostoc infection were reported on every inhabited continent, in patients aged 16 to 90 years, with a slight preponderance in the elderly. Fever and bacteremia were the most common presentation (44/74 cases); though infections also presented as respiratory infections (10/74); osteomyelitis or soft tissue infection (9/74); encephalo-meningism (4/74); focal peri-hepatic infection (4/74); endophthalmitis (2/74); and endocarditis (1/74).
30/74 patients were significantly immune compromised (14 on chemotherapy, 10 on high dose corticosteroids/high dose immunosuppressants, 4 with AIDS, 1 with severe burns), and 25/74 had an active cancer diagnosis. Only 4/74 patients had no comorbidities. 31/74 patients had an indwelling long line (26 with CVCs; 4 with a PICC, 1 with a port-a-cath); 2 had prostheses; 8 received TPN; and 1 had a PEG tube. 24/74 patients had recently undergone surgery. 33 patients had concomitant culture growth of other, non-Leuconostoc organisms.
42/74 patients had recently received antibiotics, though there was no clustering of infections after any specific antibiotic regimen. Of the 50/74 isolates with susceptibility data available, all were resistant to vancomycin; none tested were resistant to ampicillin, linezolid or daptomycin.
Overall, 52/74 patients survived acute infection, and no factor was associated with survival on chi squared analysis (including gender, age in decades, immunosuppression, cancer, recent surgery or recent antibiotics). In those with indwelling lines, there was a trend towards greater survival after line removal vs no removal (84.6%, 11/13, versus 60%, 6/10) though this was not statistically significant.
CONCLUSION: We show that Leuconostoc infection is rare, typically affecting the critically ill, with relatively high mortality. Potential contributing factors included immunosuppression, recent surgery, active cancer diagnosis +/chemotherapy, and indwelling central lines. Species are strongly resistant to vancomycin. If vancomycinresistant gram-positive cocci-infection is suspected, our data support empirical substitution of linezolid or daptomycin, or cautious addition of ampicillin, and removal of any indwelling central catheters.
28
ABSTRACT #6
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/ENDOCRINOLOGY
ACUTE MYOPERICARDITIS IN A YOUNG MALE WITH UNDIAGNOSED GRAVES’ THYROTOXICOSIS
Michel Skaf1 , Juan Arango1 , Loba Alam1, Marni Wilkoff1, Raul Benavides1 , Daniel Slack1 , Robert Bernstein1 , Vikram Agarwal1, Abel Casso Dominguez1, Arieh Fox1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
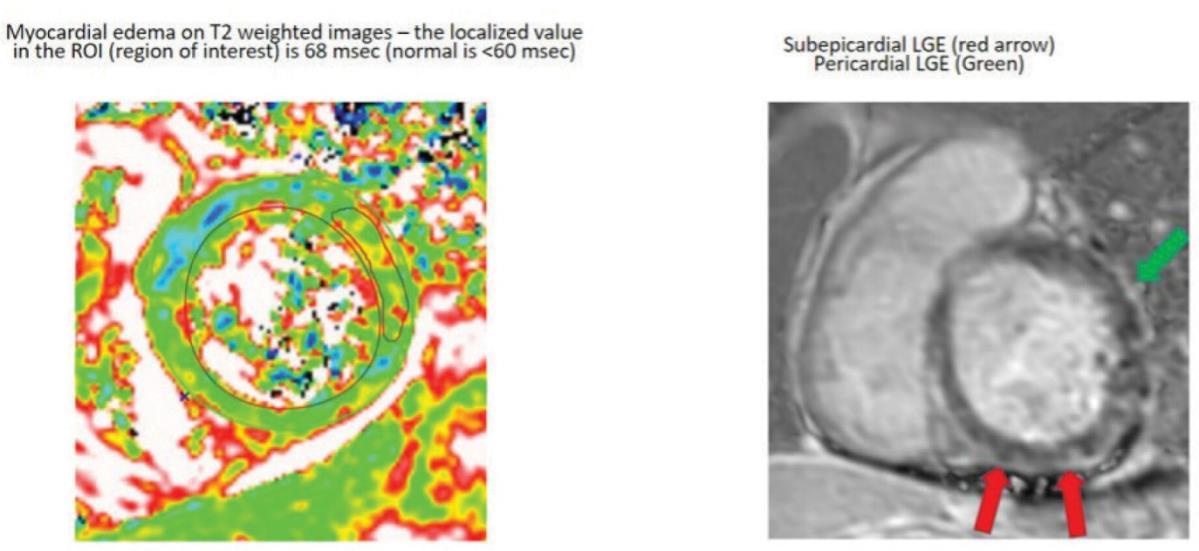
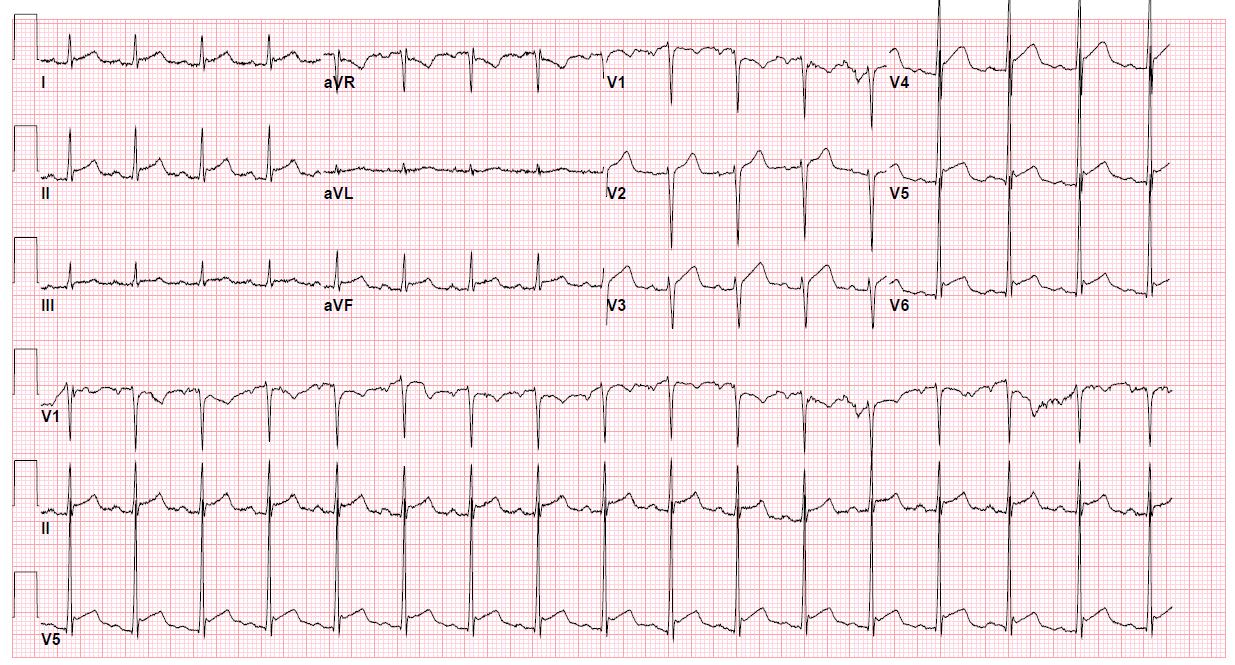
BACKGROUND/INTRODUCTION: Myopericarditis is an extension of inflammation from the pericardium to the myocardium. The incidence is hard to ascertain. It is estimated to occur in 1.1% of patients who present to the emergency department with chest pain. We describe the case of a healthy young male presenting with acute chest syndrome with electrocardiographic ST segment elevations and mild troponin elevation, found to have myopericarditis associated with Graves’ thyrotoxicosis.
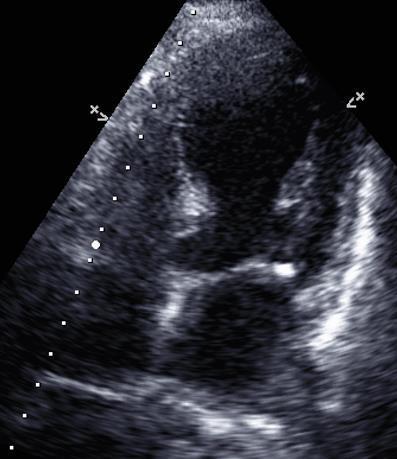
CASE PRESENTATION: A 32-year-old man presented to the emergency room following 12 hours of progressively worsening acute sharp right-sided chest pain that worsened with supine positioning and improved with seated or standing positioning. He was notably hypertensive (142/84 mmHg), tachycardic (108 beats/min), afebrile (99.4 F), and tachypneic (35 breaths/min). His electrocardiogram showed diffuse ST segment elevations in anterior, anterolateral, and inferior leads and diffuse PR segment depressions (Figure 1). The physical exam was remarkable for diaphoresis, tachypnea, temporal muscle wasting, symmetrically enlarged thyroid without palpable nodules, and tenderness in the subxiphoid area.
Initial labs showed an elevated WBC count of 17.8K [Normal Level (NL) 4.5–11.0 K/µL], troponin-I of 0.047 ng/mL (NL <0.031 ng/mL), and ALP of 140 U/L (NL 38–126 U/L). The patient had normal renal function and electrolytes. Repeat troponin-I was 37.5 ng/mL. CRP and ESR were 26.79 mg/L (NL < 5.1 mg/L) and 0 mm/hr, respectively. A chest X-ray showed a normal cardiac silhouette and bilateral lower lung volumes with increased vascular markings. Chest computed tomography (CT) with contrast showed presence of a prominent soft tissue mass within the anterior mediastinum suggestive of persistent thymus, and no evidence of acute aortic pathology or central pulmonary embolism. The patient’s cardiac magnetic resonance imaging (CMR) showed large amounts of transmural myocardial edema at the basal anterior, basal anteroseptal, mid inferior, mid inferoseptal, mid inferolateral, apical inferior, and apical inferoseptal segments (7/17 segments of the 17 segment ACC/AHA model). There was no evidence of concomitant late gadolinium enhancement (LGE) in these segments. There was a large amount of diffuse circumferential LGE of the pericardium, with a maximal pericardial wall thickness of 3.7 mm. Concomitant with LGE, there was a large amount of patchily-distributed pericardial edema.
The patient was started on ibuprofen 800 mg every 8 hours and colchicine 1.2 mg once as a loading dose, followed by colchicine 0.6 mg every 12 hours. The patient also received intravenous morphine for his chest pain and pantoprazole for gastric ulcer prophylaxis, and was started on metoprolol tartrate 25 mg every 12 hours. His TSH was found to be <0.008 μIU/mL (NL 0.4–4.2) with free thyroxin levels (T4) of 2.29 ng/dL (NL 0.8–1.5). Laboratory values were consistent with Graves’ thyrotoxicosis. On further examination, the patient reported unexplained weight loss despite an increased appetite and 3 months of persistent diarrhea. The patient also admitted to using cannabis and a stimulating supplement for strength training. The consulting Endocrinology team recommended methimazole 10 mg daily. Troponin I peaked at 37.5 ng/mL and subsequently decreased to 29.8 ng/mL. Repeat transthoracic echocardiogram two days after presentation revealed normal LV function and no pericardial effusion.
CONCLUSION: Graves’ disease is a well-known autoimmune thyroid disease associated with various systemic complications such as myxedema, ophthalmopathy, neuropathy, and enteropathies. Cardiovascular manifestations include supraventricular tachycardias (such as atrial fibrillation), non-ischemic cardiomyopathies (high output congestive heart failure or dilated cardiomyopathy), coronary vasospasms, and myxoid valve
29
degeneration. These systemic complications have been attributed to lymphocytic infiltration as part of an autoimmune-mediated process. TSH receptors have been isolated on cardiac myocytes in myocarditis patients with Graves’ disease without viral genomes, suggesting direct autoimmunity to this receptor as a possible pathophysiology. However, the exact mechanism by which Graves’ disease patients develop acute myopericarditis is still unclear. Other possible mechanisms include viral causes or direct changes in myocardial fat metabolism.
Up to 20% of patients with hyperthyroidism have cardiac symptoms. Although pericardial disease as a complication of thyrotoxicosis is rare, all patients presenting with signs of myocarditis/pericarditis should undergo screening for the extracardiac symptoms of hyperthyroidism that were present in our patient. Although most reported cases in the literature were confirmed by endomyocardial biopsy (EMB), CMR can offer the diagnostic yield without procedural risks. The presence or absence of myocardial LGE on CMR is important for risk stratification of myopericarditis, as patients showing LGE have a higher risk of major adverse cardiovascular events (MACE) (Hazard Ratio = 2.2), with the best outcomes predicted in patients with EF > 40% and no LGE. Although our patient showed no myocardial LGE and preserved EF, he had significant transmural myocardial edema. These findings are consistent with a very acute and early presentation, with a need for repeat CMR in the follow-up period to reassess for LGE. Ventricular arrhythmia risk secondary to lymphocytic infiltration in myocarditis is well reported but usually more commonly associated with Giant Cell Myocarditis (GCM) and cardiac sarcoidosis. Arrhythmias are less common in isolated pericarditis or minimal myocardial inflammation and are usually supraventricular (SV) in origin (<10%), with atrial fibrillation being the predominant SVT. However, despite the low incidence of sudden cardiac death (SCD), SVT, or VT, especially in the acute inflammatory phase, beta blockers have been recommended for risk reduction and treatment of hyperthyroidism symptoms. Our patient was started on metoprolol tartrate for both possible risks of arrhythmia and symptom treatment of hyper thyrotoxicosis.
30
Figure 1: Electrocardiogram showing diffuse ST segment elevations and PR segment depressions
ABSTRACT #7 CLINICAL RESEARCH INFECTIOUS DISEASES/PULMONARY/CRITICAL CARE
CLINICAL OUTCOMES OF TRACHEOSTOMIZED PATIENTS: COVID-19 VERSUS NON COVID-19
Jeeyune Bahk1 , Venus Sharma1, Bridget Dolan2, Mantej Sembhi1, Jennifer Fung1, Young Im Lee2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in Washington, DC, United States from May 19-24, 2023.
BACKGROUND/INTRODUCTION: Tracheostomies are commonly utilized to facilitate ventilation weaning in critically ill patients. There is currently limited data on tracheostomized patients with Coronavirus Disease 2019 (COVID-19) with conflicting guidelines. Our study aimed to compare outcomes of tracheostomized patients with and without COVID-19 infection in hopes of providing optimal management strategies for critically ill patients.
METHODS: We performed a retrospective observational case-control study of 604 consecutive tracheostomized patients hospitalized in an intensive care unit (ICU) of one of the Mount Sinai Health System hospitals between March, 2020 to September, 2021. We evaluated and compared clinical outcomes of length of stay (LOS), time to ventilator liberation, speech valve placement, decannulation, and mortality between patients with and without COVID-19 infection.
RESULTS: A total 398 COVID-19 negative (COVID-) and 206 COVID-19 positive (COVID+) patients were tracheostomized. Both groups had a similar mean age (62.08 years versus 61.55 years) and gender proportion (64.3% versus 63.6% male). COVID+ patients had fewer co-morbidities including coronary artery disease, congestive heart failure, malignancy, chronic kidney disease, liver disease, and human immunodeficiency virus (p<0.05).Total and ICU LOS were both shorter in COVID+ (60.14 days versus 54.29 days; 40.22 days versus 39.20 days), though not statistically significant. Time from tracheostomy to first pressure support and first tracheostomy collar placement were longer in COVID+ (2.87 days versus 1.80 days, p=0.005; 11.07 versus 4.46 days, p<0.001, respectively). Moreover, a longer period was observed until first speech valve placement and decannulation in COVID+ group, though not statistically significant (23.09 days versus 29.91 days; 49.2 versus 54.40 days, respectively). Similar proportion of patients eventually got decannulated: 28.1% from COVID(n=112), 30.6% from COVID+ (n=63). More COVID- patients were discharged to a rehabilitation center (41.2% versus 32.5%), whereas more COVID+ patients were discharged to a long-term acute care hospital (LTACH) (23.8% versus 13.6%) (p=0.015). Mortality within the same admission of tracheostomy was similar in both groups 36.4% (n=145) versus 35.9% (n=74). One-year mortality was significantly lower in COVID+ of 23.3% (n=48) compared to COVID- of 36.7% (n=146) with p-value of 0.001
CONCLUSION: Longer time from tracheostomy to ventilation weaning, speech valve placement, and decannulation were seen in COVID+ compared to COVID-. This may demonstrate initial clinical vulnerability of COVID-19 patients during an early to mid-phase of the disease process, followed by relative stability in recovery phase. Lower rate of mortality and increased rate of discharge to LTACH may imply better eventual outcome in tracheostomized COVID-19 patients. Patients with COVID-19 had less co-morbidities, implying a healthier population surviving tracheostomy. Intensivists should actively evaluate the suitability of tracheostomy for patients with COVID-19 with the aim to provide better opportunities of recovery
31
Note – except where indicated, data are number of patients, with percentages in parentheses. Continuous variables are presented as means and standard deviations for normally distributed data. Categorical variables are summarized as frequencies and percentages. Differences in distributions of characteristics of those with and those without COVID-19 were analyzed using Student t test or Mann-Whitney U test for continuous variables and Chi-square or Fisher’s exact test for categorical variables. Bold indicates statistical significance (p<0.05). COVID-19=coronavirus disease-2019; SNF=skilled nursing facility; LTACH=long-term acute care hospital; LOS=length of stay.
COVID-19 negative (n=398) COVID-19 positive (n=206) p-value Disposition Home SNF/Rehabilitation LTACH Expired Others Length of Stay (LOS) Hospital LOS (days) ICU LOS (days) Ventilation weaning Time from tracheostomy to first pressure support (days) Time from tracheostomy to first trach collar (days) Time from tracheostomy to speech valve (days) Time from tracheostomy to decannulation (days) Eventual decannulation Mortality Same admission One-year mortality 23 (5.8%) 164 (41.2%) 54 (13.6%) 145 (36.4%) 12 (3.0%) 60.14 (56.40) 40.22 (46.42) 1.80 (3.43) 4.46 (5.87) 23.09 (21.84) 49.32 (43.70) 112 (28.1) 145 (36.4) 146 (36.7) 14 (6.8%) 67 (32.5%) 49 (23.8%) 73 (35.4%) 3 (1.5%) 54.29 (38.61) 39.20 (24.27) 2.87 (5.28) 11.07 (14.29) 29.91 (22.08) 54.50 (46.11) 63 (30.6) 74 (35.9) 48 (23.3) 0.015 0.182 0.769 0.005 <0.001 0.062 0.474 0.594 0.973 0.001
Table 1: Comparison of Clinical Outcomes in Tracheostomized Patients with and without COVID-19
32
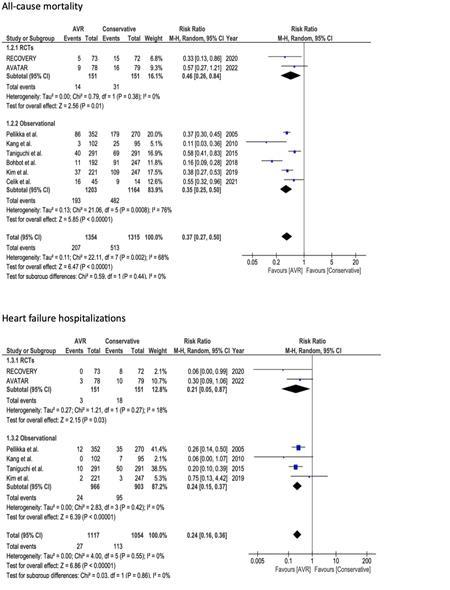
ABSTRACT #8
CLINICAL RESEARCH CARDIOLOGY
META-ANALYSIS EVALUATING THE CLINICAL OUTCOMES OF BETA-BLOCKER THERAPY IN PATIENTS WITH HEART FAILURE AND CONCOMITANT COCAINE USE
Yoni Balboul1 , Devika Aggarwal2, Arpanjeet Kaur1, Kirtipal Bhatia1, Arshdeep S Dhaliwal3, Persio D. Lopez3 , Basera Sabharwal1, Harsimran Kaur Bhatia4, Ashish Correa1, Kiran Mahmood1 , Arieh Fox1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Beaumont Hospital, Royal Oak, MI, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Kasturba Medical College, Manipal, India
BACKGROUND/INTRODUCTION: Current guidelines recommend beta-blockers for patients with heart failure and reduced ejection fraction (HFrEF) to reduce mortality. However, guidelines for beta-blockers in patients with HFrEF and concomitant cocaine use are unclear. Traditional teachings have dictated that beta-blockers should be avoided in cocaine users due to the theoretical risk of “unopposed” alpha-adrenergic stimulation potentially leading to acute coronary syndrome, hypertensive emergency, aortic dissection, and sudden death. We performed a meta-analysis to examine clinical outcomes and safety of beta-blockers in patients with HFrEF and concomitant cocaine use.
METHODS: We performed a systematic review of electronic databases (Embase, Medline, and Web of Science) from inception to June 20th, 2022, to identify studies that reported clinical outcomes among patients with HFrEF and cocaine use while on beta-blocker therapy. The primary outcome was major adverse cardiac events (MACE), a composite of mortality and heart failure readmission. Pooled risk ratios (RR) and 95% confidence interval (CI) were calculated using a random-effects model.
RESULTS: Of 600 citations, 4 retrospective cohort studies with a total of 703 patients were included in the final analysis. Carvedilol was the most prescribed beta-blocker across all studies. The analysis showed that the risk of having a MACE was significantly lower in patients receiving beta-blocker therapy versus not (RR, 0.58; 95%CI, -0.44 to 0.76, p<0.0001). Beta-blocker therapy was associated with a significantly lower risk of heart failure readmissions (RR, 0.52; 95%CI, -0.33 to 0.81; p=0.004). All-cause mortality, reported separately only in two studies, did not differ between patients who were given beta-blockers (RR, 0.76; 95%CI, -0.36 to 1.58; p=0.46). Heterogeneity between studies was low.
CONCLUSION: Our study suggests that beta-blocker therapy is associated with a reduced risk of mortality and heart failure related readmissions without increasing the risk of death in patients with HFrEF and concomitant cocaine use.
33
ABSTRACT #9
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
PANCREATIC NEUROENDOCRINE TUMOR PRESENTING AS AN ABDOMINAL PAIN FOLLOWING SUCCESSFUL HELICOBACTER PYLORI ERADICATION
Omar Belfaqeeh1 , Frederick
Rozenshteyn1
Bruce Gelman1
,
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
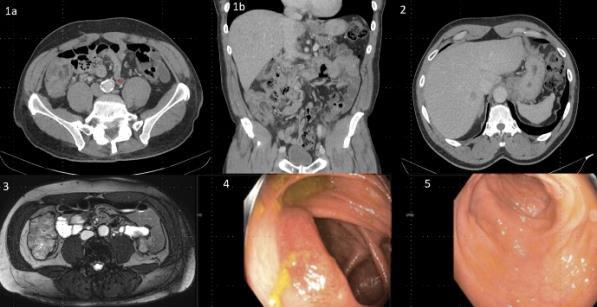
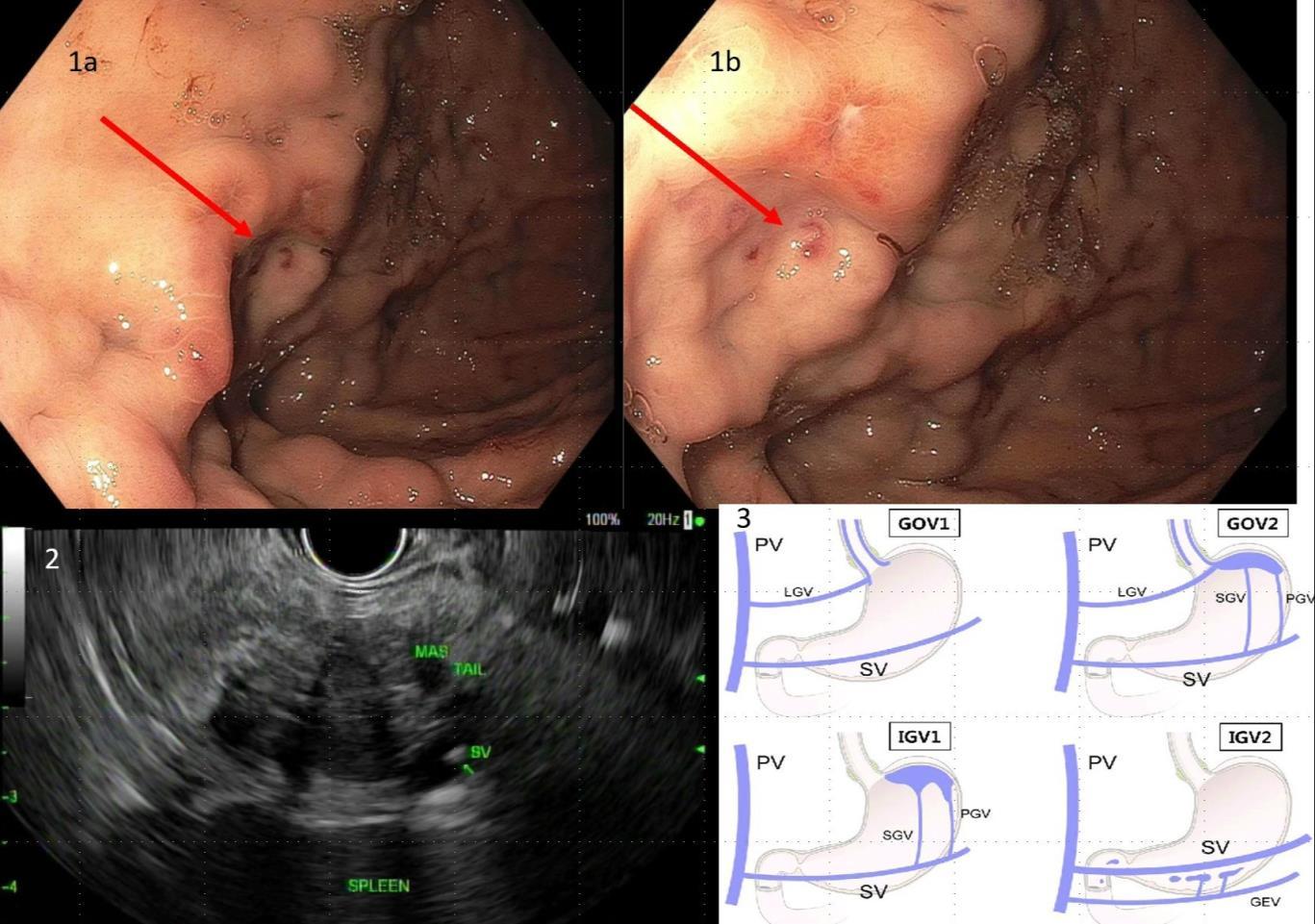
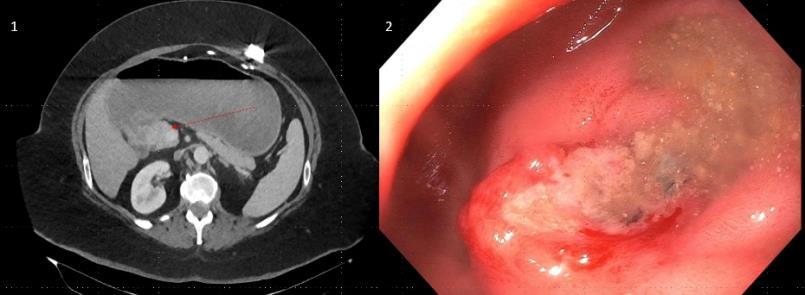
BACKGROUND/INTRODUCTION: Zollinger-Ellison syndrome (ZES) is caused by functional duodenal or pancreatic neuroendocrine tumors (NET) that secrete gastrin resulting in excess acid production causing peptic ulceration, reflux esophagitis and diarrhea. It is estimated that the annual incidence is one per million population, of which 20 to 30 percent are associated with multiple endocrine neoplasia type 1 (MEN1). Recent studies have demonstrated that 70-80% of gastrinomas arise in the duodenum.
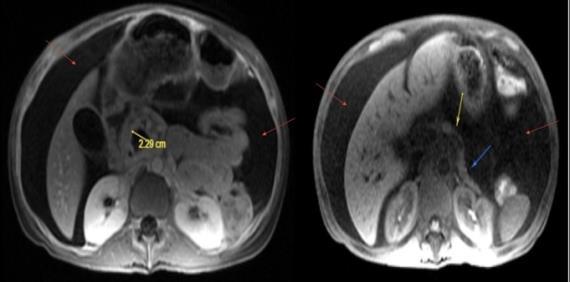
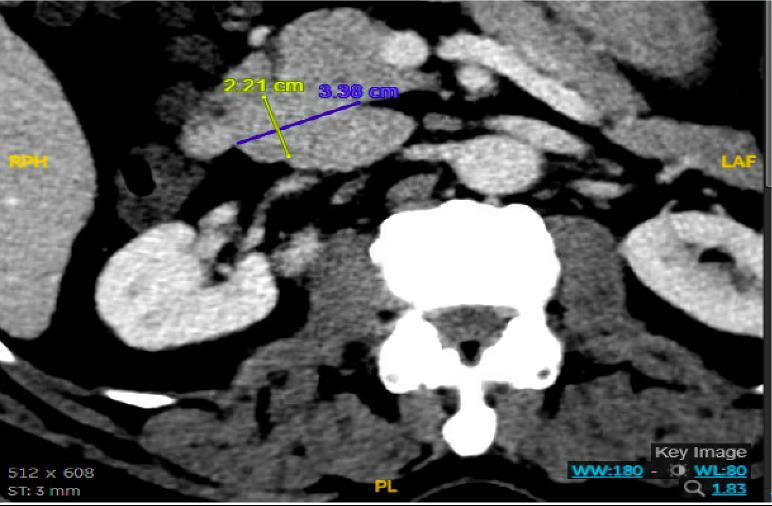
CASE PRESENTATION: A 67-year-old male with a history of partial liver resection, peptic ulcer disease, and Helicobacter pylori gastritis s/p quadruple therapy presented with acute on chronic abdominal pain despite being on a proton pump inhibitor (PPI). He had abdominal pain for the past 5 years associated with nausea, vomiting, diarrhea, and a 50-pound unintentional weight loss. An esophagogastroduodenoscopy (EGD) six months ago demonstrated peptic ulcer disease and Helicobacter pylori which was successfully eradicated.
He underwent a CT-abdomen/pelvis with intravenous contrast in the emergency department which revealed an enhancing 3.4 cm mass in the head of the pancreas with retroperitoneal lymphadenopathy. MRI of the abdomen confirmed the presence of a 3.2 cm enhancing pancreatic head mass with direct extension into the second portion of the duodenum and multiple enlarged retroperitoneal lymph nodes. EGD was remarkable for edema and granularity in the first portion of the duodenum. Endoscopic ultrasound (EUS) was notable for a hypoechoic and heterogeneous irregular mass in the pancreatic head measuring 25 mm by 23 mm in maximal crosssectional diameter with invasion into the serosa and muscularis mucosa of the duodenum. Fine needle aspiration of the pancreatic mass for cytology revealed a well-differentiated pancreatic neuroendocrine tumor (Ki-67 index <1%). Gastrin levels were ordered. He presented again to the hospital 3 weeks later with worsening epigastric abdominal pain and nausea despite adhering to PPI therapy. CT-abdomen revealed new proximal duodenal ulcerations. Gastrin level from the prior admission was noted to be 1988 pg/mL. He subsequently underwent a Whipple's procedure with no complications and was discharged home with a planned EGD surveillance in 6 months.
CONCLUSION: Establishing a diagnosis of ZE can be difficult due to the lack of consistent diagnostic criteria, the widespread use of PPIs that masks mask the symptoms and limited access to gastric pH testing. In our case, the diagnosis was based on a fasting serum gastrin level, FNA results, and imaging findings. Owing to its variable clinical presentation, high mortality, and challenging primary lesion identification, clinicians should consider ZE in the differential diagnosis of patients who are symptomatic despite taking PPI, having Helicobacter pylori successfully eradicated or having multiple duodenal and gastric ulcers that fail to respond to therapy.
34
35
Figure 1: CT Abdomen and Pelvis with contrast showing a suspicious mass in the second portion of the duodenum/pancreatic head.
ABSTRACT #10
CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
OUTCOMES IN PREMENOPAUSAL PATIENTS WITH HR+/HER2- BREAST CANCER AND LYMPH NODE MICRO-METASTASIS BASED ON THE 21-GENE RECURRENCE SCORE
Nadeem Bilani1 , Rima Patel2, Amy Tiersten2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that will be held in Chicago, Illinois, United States from June 2-6, 2023.
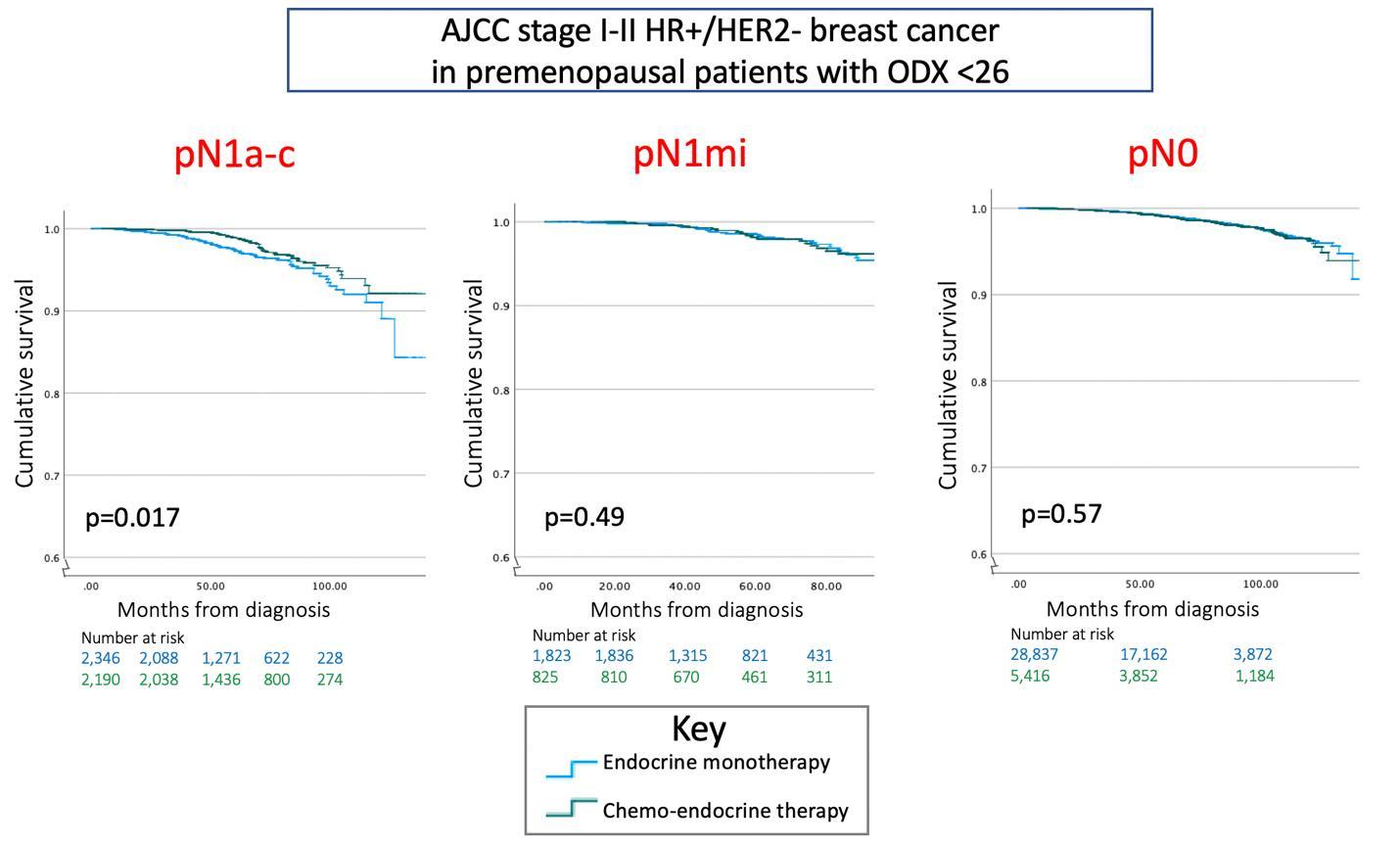
BACKGROUND/INTRODUCTION: Postmenopausal patients with hormone receptor positive, HER2-negative (HR+/HER2-) early breast cancer (EBC) and 21-gene OncotypeDX (ODX) recurrence scores (RS) <26 do not benefit from chemoendocrine therapy (‘CET’) compared to endocrine monotherapy (‘E’). The TAILORx and RxPONDER trials demonstrated this was consistent in node-negative and node-positive disease, respectively. In premenopausal patients, however, guidelines for those with low RS diverge between disease involving 0 (pN0) vs. 1-3 (pN1a-c) lymph nodes. Additionally, treatment decisions are less clear for patients with micro-metastasis (pN1mi), who comprised only about 10% of patients in RxPONDER. This study used the National Cancer Database (NCDB) to assess treatment patterns and survival outcomes in premenopausal patients with EBC and lymph node micro-metastasis.
METHODS: A cohort of patients aged <50 years, diagnosed between 2004-2019 with HR+/HER2- EBC, and who underwent ODX testing, was recruited from the NCDB. (A) Firstly, we described demographic and clinical characteristics of a sub-cohort with micro-metastasis using univariate statistics. (B) We confirmed the prognostic value of ODX in this sub-cohort with multivariate Cox regression analysis of overall survival (OS). (C) We explored patterns of practice amongst the total cohort with ODX <26 with chi-squared testing for differences in CET use by nodal status. (D) To elucidate the predictive value of this assay, we performed Kaplan-Meier models comparing OS for those with RS <26 receiving E versus CET, controlling granularly for nodal status: (i) pN1a-c, (ii)pN1mi, and (iii) pN0.
RESULTS: Of n=72,068 patients aged <50 years with HR+/HER2- EBC and ODX data, 6.1% (n=4,402) had micro-metastasis. (A) The median age of this subgroup was 45 (IQR 41-47) years. Most tumors were grade II (n=2,472, 57.7%) with ductal histology (n=3,500, 80.3%). 73.4% of pN1mi cases had RS <26, while 26.6% had RS ≥26. (B) Multivariate Cox regression – adjusting for comorbidity, race and chemotherapy use – confirmed significance in this pN1mi cohort of RS ≥26 prognosticating poorer OS compared to RS 0-15 (HR, 4.42; 95%CI, 2.35-8.31; p<0.001). (C) 29.0% (n=1,033) of patients with pN1mi and ODX <26 underwent CET, greater than 15.2% (n=6,568) with pN0 and less than 47.3% (n=2,884) with pN1a-c staging (p<0.001). (D) A benefit in OS (p=0.017) was observed in cases with RS<26 and pN1a-c using CET (5-year OS: 99%) versus E (5-year OS: 97.5%), but not in pN1mi (p=0.49) or pN0 (p=0.57) disease.
CONCLUSION: The management of premenopausal patients with HR+/HER2- EBC, isolated micro-metastasis, and ODX <26 is unclear. Our large registry analysis found the addition of chemotherapy to endocrine therapy was associated with improved survival in cases with ODX<26 involving 1-3 lymph nodes, but not in nodenegative or micro-metastatic disease. Prospective trials are needed to confirm these findings.
36
37
Figure 1: Kaplan-Meier modeling in patients aged <50 with RS<26
ABSTRACT #11
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
TUMOR LYSIS SYNDROME
Conor Buckley1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Tumor lysis syndrome (TLS) is an oncologic emergency characterized by massive tumor cell lysis, usually after commencing chemotherapy for hematological malignancy, causing the release of large amounts of intracellular potassium, phosphate and nucleic acids into the systemic circulation, resulting in elevated uric acid levels, secondary hypocalcemia, and potentially acute renal injury, cardiac arrhythmia or seizure. Patients with TLS have an in-hospital mortality rate of approximately 15%
DISCUSSION: Cairo-Bishop criteria (2004) provides specific laboratory criteria for the diagnosis of TLS both at presentation and within seven days of treatment. It also incorporates a grading system to help delineate the degree of severity of TLS.
1. Laboratory TLS: ≥2 criteria within 3 days before or 7 days after cytotoxic therapy: uric acid ≥8mg/dL, K ≥6mEq/L, phos ≥4.5mg/dL, or Ca ≤7mg/dL. Criteria also satisfied if 25% change from baseline.
2. Clinical diagnosis: laboratory diagnosis and ≥1 clinical criteria: Cr 1.5x ULN, arrhythmia, seizure A grading system for severity of TLS (on a scale from zero to five) in patients with laboratory TLS was based on the degree of elevation in serum creatinine, the presence and type of cardiac arrhythmia, and the presence and severity of seizures.
Pathophysiology: Breakdown of malignant cells causes massive release of intracellular potassium, phosphate and nucleic acids into the systemic circulation. Subsequently, the binding of phosphorus to calcium results in secondary hypocalcemia and catabolism of nucleic acids to uric acid leads to hyperuricemia. These electrolyte derangements can result in end organ dysfunction, which in severe cases can be life-threatening. Uric acid and calcium-phosphate crystal precipitation and deposition in the renal tubules causes acute uric acid nephropathy and acute kidney injury. Hyperkalemia increases the risk of cardiac arrhythmias. Secondary hypocalcemia predisposes patients to tetany or seizures.
Management of TLS: The anticipation of TLS, and initiation of preventative measures, is critical in reducing morbidity and mortality. Although no validated risk stratification system exists, patients at high risk (>5%) of TLS are typically those with ALL, AML, Burkitt's lymphoma or other malignancies with high tumor burden or grade in the setting of renal insufficiency or dehydration. The primary preventative measures are aggressive intravenous hydration and urate lowering therapies (allopurinol and rasburicase). Continuous cardiac monitoring is frequently recommended for patients at intermediate or high risk of TLS or have met criteria for a diagnosis of TLS. Monitoring of urine output, weight and every 6 hours laboratory testing is also recommended.
Aggressive intravenous (IV) hydration is the cornerstone of preventing TLS. Thegoal of IV hydration is to improve renal perfusion and glomerular filtration, minimizing the likelihood of uric acid or calcium phosphate precipitation in the tubules. The recommended rate is 2-3L/m2/day with an associated urine output goal of >100 mL/m2/hr. Loop diuretics such as furosemide may be used on an as needed basis to augment urine output. Patients should be monitored for signs of volume overload, particularly those with acute kidney injury or cardiac dysfunction. Allopurinol, a xanthine oxidase inhibitor, reduces the production of uric acid. Allopurinol dosed at 300-600 mg per day can be administered 24-48 hours before starting chemotherapy and continued until hyperuricemia has resolved. Renal dosing may be necessary and the reduced clearance of other meds (e.g. cyclophosphamide, MTX, 6-MP, azathioprine, ampicillin) should be noted.
38
Rasburicase is a recombinant urate oxidase that rapidly converts uric acid into allantoin, a more soluble compound that is excreted by the kidneys. Rasburicase is used for both prevention and treatment of TLS (in patients with hyperuricemia despite allopurinol). For prevention, rasburicase can be administered in high-risk patients with hematologic malignancies as a single 3 mg IV dose (off-label dosing). For treatment, dosing is typically 0.1 to 0.2 mg/kg once daily for 1-7 days (average of 2-3 days) with the dosing and duration of treatment dependent on plasma uric acid levels and clinical judgment. Rasburicase is contraindicated in G6PD deficiency (risk of hemolysis). Also risk of anaphylaxis and methemoglobinemia.
Electrolyte management: Hyperkalemia is managed with insulin and glucose, beta agonists, or ion exchange resins such as sodium polystyrene sulfonate according to local hospital protocol. Calcium gluconate 1000 mg IV is administered to patients with serum potassium >6.5 or EKG changes to reduce the risk of cardiac arrhythmias. Hypocalcemia in asymptomatic patients can be treated with oral calcium replacement. The associated hyperphosphatemia due to TLS should be treated first with phosphate binders, which in turn improves secondary hypocalcemia. Symptomatic patients should be treated with intravenous calcium replacement administered at the lowest possible dose required to relieve symptoms regardless of phosphate concentration. Renal consultation should be sought to assess the need for hemodialysis. Serum magnesium concentration should be checked and magnesium repletion provided as needed. Hyperphosphatemia can be managed with phosphate binders (calcium carbonate or aluminum hydroxide) along with aggressive continuous intravenous hydration at 2-3L/m2/day. However, persistent hyperphosphatemia, particularly with associated symptomatic secondary hypocalcemia, is an indication for hemodialysis. Indications for hemodialysis or continuous renal replacement therapy: 1. severe oliguria or anuria; 2. Intractable fluid overload; 3. persistent hyperkalemia; 4. hyperphosphatemia-induced symptomatic hypocalcemia; 5. calcium-phosphate product ≥70 mg/dL; 6. severe or refractory hyperphosphatemia in the setting of renal failure, hemodialysis may be required.
39
ABSTRACT #12
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
EXTENSIVE SPLANCHNIC VEIN THROMBOSIS ASSOCIATED WITH COMBINED ORAL CONTRACEPTIVE USE
Salvador Caceros Diaz1 , Jonas Marx1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the New York American College of Physician (NYACP) Chapter Resident/Fellow and Medical Student Forum that will be held in Albany, New York, United States on May 12, 2023
BACKGROUND/INTRODUCTION: Combined oral contraceptives (COCs) are a widely used form of hormonal contraception associated with an increased incidence of venous thrombosis. The individual risk is determined by the type and concentration of the contained estrogen, duration of use, age, and the presence of other thrombogenic factors, such as smoking or hereditary predisposition. While deep vein leg thrombosis, pulmonary embolism, and femoral vein thrombosis represent the most frequent sites of thrombotic events in connection with COCs, other venous systems can be affected.
CASE PRESENTATION: A 35-year-old woman presented to the emergency department with nine days of epigastric pain, exacerbated by food intake and associated with nausea and vomiting. The intensity of her abdominal pain gradually progressed to severe and constant on the day of admission. Past medical and surgical history were relevant for appendicitis with uncomplicated appendectomy, no prior pregnancy, never smoker, and occasional alcohol intake. The only active medication was a COC (norgestimate and ethinyl estradiol), which she had been taking for the past ten years without complications. No personal or family history of thromboembolic events was recognized. She was overweight with a BMI of 27 kg/m2 and had moderate generalized abdominal tenderness more pronounced over the right upper quadrant. Laboratory results, including hepatic function testing, were unremarkable, except for leukocytosis of 12,200 WBC per microliter. Abdominal ultrasound and computed tomography venogram of the abdomen revealed a main portal vein thrombus with extension to the right and left portal veins, splenic vein, and superior mesenteric vein. COCs were discontinued, and anticoagulation with apixaban was started with the eventual resolution of pain. Repeat imaging after three months of uninterrupted anticoagulation demonstrated chronic portal vein and superior mesenteric vein thrombosis with cavernous transformation and development of epigastric and mesenteric varices. She had an extensive thrombophilia evaluation that was negative, including antiphospholipid syndrome, paroxysmal nocturnal hemoglobinuria, JAK2V617F, and a negative genetic myeloid disorders panel.
CONCLUSION: This case highlights a rare case of extensive splanchnic vein thrombosis with long-term use of COCs as the only identified risk factor. Splanchnic veins, including porto-mesenteric and splenic veins, have been reported as unusual sites of thrombosis associated with COCs. The initial presentation is nonspecific, with nausea, vomiting, and abdominal pain as the most common symptoms, however, imaging studies are recommended in cases of worsening or unresolved abdominal pain in patients receiving COCs. Early recognition and subsequent anticoagulation are critical, as untreated thrombosis can result in mesenteric ischemia, development of portal hypertension, ascites, and variceal bleeding. In this case, progression to chronic portal vein thrombosis, superior mesenteric vein thrombosis, with development of epigastric and mesenteric varices occurred despite discontinuation of COCs and anticoagulation with apixaban.
40
ABSTRACT #13
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY/INFECTIOUS DISEASES
ISOLATED THROMBOCYTOPENIA AS AN INITIAL PRESENTATION OF HIV INFECTION IN A PREVIOUSLY HEALTHY MALE
Adrian Chernyk1 , Khalid Dar1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: An association between immune thrombocytopenia and the acquired immune deficiency syndrome (AIDS) or human immunodeficiency virus (HIV) infection was first recognized in 1982. Before highly active antiretroviral therapy (HAART), the incidence of HIV-associated thrombocytopenia was estimated at 10–30%, and thrombocytopenia was the initial manifestation of HIV in approximately 10% of cases. Although thrombocytopenia may occur at any time during the course of HIV infection the incidence generally correlates with the degree of immunosuppression and is more prevalent in clinical AIDS With the advent of ART the prevalence of HIV associated thrombocytopenia was found to be only 3.2% in one large study.
CASE PRESENTATION: The patient was an elderly male with no significant PMHx or family history of bleeding disorders or hematologic malignancies who presented to his primary medical doctor (PMD) for petechiae, epistaxis, and bruising over the past few months. The patient did not take any regular medications and did not have any recent illnesses. He was last sexually active 8 years prior and denied a history of intravenous drug use. He was found to have low platelets of 3000 K/uL at his PMD and sent to the ED for further work-up In the ED, the platelet count was 2000 K/uL Physical exam was notable for general petechiae. A broad work-up was sent for isolated thrombocytopenia while 2 units of platelets were transfused. Infectious work-up for EBV, CMV, and babesia were negative. Hepatitis panel was positive for Hepatitis A antibody and Hepatitis B surface antibody. Hepatitis C antibody was negative An autoimmune work up was sent. Patient was found to have HIV1 infection with a HIV viral load of 178K and CD4 count of 351. Toxoplasmosis and cryptococcus were negative. Hematology recommended for the patient to receive dexamethasone 40 mg intravenous daily for 4 days and IVIG 1g / kg for 2 days. Infectious disease was consulted and the patient was started on HAART therapy given the new HIV diagnosis.
CONCLUSION: It is important to do a broad work-up for thrombocytopenia of unclear etiology. HIV infection should always be on the differential diagnosis for individuals presenting with thrombocytopenia. Furthermore, the degree of platelet decline can be predictive for the later development of HIV induced CNS disease as well as being a strong independent predictor of mortality in untreated HIV. The recommended treatment is to treat with a short course of steroids and IVIG as the pathophysiology is immune mediated. Platelet improvement with immunosuppression is the best diagnostic test for HIV associated thrombocytopenia. However, the mainstay of treatment will be control of the HIV infection with ART.
41
ABSTRACT #14
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
SEVERE GASTROINTESTINAL BLEEDING FOLLOWING TRANSESOPHAGEAL ECHOCARDIOGRAPHY AND ABLATION FOR ATRIAL FIBRILLATION
Christy Chon1 , Frederick Rozenshteyn1 , Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Transesophageal echocardiograms (TEE) are performed to evaluate a variety of cardiac disorders. It involves blind intubation of the esophagus and carries a small risk of esophageal injury. This case describes a case of severe upper gastrointestinal bleeding (GIB) following TEE and ablation for atrial fibrillation.
CASE PRESENTATION: A 66-year-old male with a history of atrial fibrillation and upper GI bleeding underwent TEE with ablation with the intention of doing a Watchman procedure in the future. Anticoagulation had been resumed two weeks prior to the procedure. The patient underwent ablation and shortly afterwards had hematemesis followed by an episode of melena. The hemoglobin fell from 11.2g/dl to 8.7g/dl and the patient required vasopressor support and transfusion. EGD revealed many 2-3 mm non-actively bleeding erosions with clots at their bases throughout the entire esophagus, with a large blood clot found in the cardia and gastric body. Although no active bleeding was noted, the patient continued to have a hemoglobin drop so a CT angiogram was performed which was unrevealing. The patient was managed conservatively and stabilized with no further episodes of bleeding, and his anticoagulation was eventually resumed without further complications.
CONCLUSION: This case illustrates the occurrence of gastrointestinal erosions and bleeding following TEE and ablation. Severe gastrointestinal hemorrhage is a rare but known adverse event associated with TEE and ablation. The incidence of TEE-related hemorrhage has been estimated to be within 0.02% to 1.0% and is often due to direct mucosal trauma. Ablation may also induce thermal injury to the esophagus due to the proximity of the posterior left atrium and esophagus, causing esophageal ulcerations that can potentially lead to more serious complications such as atrioesophageal fistulae. Caution should be taken when evaluating patients planned for such procedures, especially those with history of prior GIB, and anticoagulation should be held if possible.
42
ABSTRACT #15
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
A RARE CASE OF ESOPHAGEAL SQUAMOUS CELL CARINCOMA WITH APPENDICULAR SKELETAL METASTASIS
Nobel Chowdhury1 , Tabitha Goring2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Memorial Sloan Kettering Cancer Center, New York, NY, United States
BACKGROUND/INTRODUCTION: Esophageal cancer is a highly lethal malignant cancer with 5-year overall survival rate of 20% in all stages combined and only 5% in metastatic esophageal cancer.Distant metastasis is present in approximately 50% of patients at initial diagnosis and in about one-third of patients it develops within 6 months of surgery or radiotherapy. Common metastatic sites of esophageal cancer are lymph nodes, liver, and lungs. Bone metastases are relatively uncommon in esophageal cancer, ranging from 5.2–7.7% in all-stage esophageal cancer patients.
CASE PRESENTATION: A 48-year-old male presented with dysphagia in 7/2022 after 1 year of reflux symptoms with a failed trial of a proton-pump inhibitor. At presentation, patient had a weight loss of 30lbs and dysphagia to solid food. Upper endoscopy performed in 8/2022 showed a distal esophageal mass and biopsy was positive for moderately differentiated invasive squamous cell carcinoma. PET scan in 11/2022 showed uptake in mid-distal esophagus, hyper metabolic thoracic and upper abdominal lymphadenopathy. The patient had a bronchoscopy with EBUS on 9/2022 with biopsy which showed no invasion in airway. The multidisciplinary tumor board decided on concurrent chemo radiation as initial therapy with the goal of R0 resection. Started on weekly chemotherapy (carboplatin and paclitaxel) and concurrent localized radiation to esophagus. Completed a total of 28 fractions (total of 5040 cgy) of radiation to the esophagus and 5 cycles of chemotherapy until end of 11/2022. During this time, chemotherapy was held for 3 weeks due to thrombocytopenia. He did not tolerate oral feeding and had a PEG tube placed in 11/2022 and decided to postpone further care until planned restaging PET scan in 11/2022. At the end of 12/2022, he presented with a severe headache, left arm weakness, rightward tongue deviation, and hospitalized MRI-brain showed a right occipital condyle lesion with involvement of right hypoglossal canal. CT-chest/abdomen/pelvis with contrast revealed increased peritoneal and retroperitoneal metastasis, new lesions in liver and right kidney, new lytic osseous metastases in the left glenoid with a nondisplaced fracture, new pathologic fracture of right third rib, and lytic metastasis of right humeral shaft with pathological fracture. He underwent surgery for insertion of intramedullary rod in right humerus and was started on radiation therapy (XRT) to base of skull, left shoulder, but developed side effects (nausea, vomiting) and did not complete the full course while inpatient. He then received XRT to right arm which was started 2 weeks post-surgery as an outpatient. Due to rapid metastasis to multiple organs including bones, the patient was planned to get FOLFOX and Nivolumab. The patient presented within 2 weeks of discharge with right groin pain and MRI-lower extremity revealed right femoral metastasis and lesser trochanteric fracture. He was again hospitalized and underwent right intramedullary rod insertion in the right femur and was started on cycle 1 FOLFOX at the end of 1/2023.
CONCLUSION: This case is an example of an uncommon finding of appendicular bone metastasis in a patient with esophageal squamous cell carcinoma. In esophageal cancer, bone metastases is rare and usually found in the adenocarcinoma subtype with involvement of axial, not the appendicular skeleton. One study noted that breast cancer patients with bone metastases have significantly better survival compared to those with metastases to other sites. Prognosis of esophageal cancer with bone metastases is poor with significantly worse overall survival (median OS 2-4 months) when compared to those with metastases to other sites. Management options include prompt surgical intervention (in case of pathological fracture or instability), radiotherapy, and chemotherapy. Early diagnosis and appropriate treatment is essential for esophageal cancer patients with bone metastases, as this could prevent skeletal-related events, maintain quality of life and performance status, allowing continuation of chemotherapy.
43
ABSTRACT #16
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
LATER ONSET OF NRAS-MUTANT METASTATIC MELANOMA IN A PATIENT WITH A PARTIALLYEXCISED GIANT CONGENITAL MELANOCYTIC NEVUS
Bruno A. Costa1 , Victor Zibara1 , Vasundhara Singh1 , Omid Hamid2 , Sonal Gandhi1 , Andrea P. Moy3 , Allison
S. Betof-Warner3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Cedars-Sinai Medical Center, Los Angeles, CA, United States; 3Memorial Sloan Kettering Cancer Center, New York, NY, United States
Published in Frontiers in Medicine, 2022. PMID: 36569151
BACKGROUND/INTRODUCTION: Despite recent advances in treatment and surveillance, metastatic melanoma still carries a poor prognosis. Large/giant congenital melanocytic nevi (CMNs) constitute a known risk factor for the condition, with the greatest risk for malignant transformation thought to be during childhood (50% of cases are diagnosed within the first 5 years of life). In a retrospective cohort of 379 large/giant CMN patients from 26 countries, the median and mean age at melanoma diagnosis were 3 and 8 years, respectively.
CASE PRESENTATION: A 30-year-old Caucasian male, previously healthy, presented with a new-onset upper back pain radiating to the right chest. The pain had an intermittent occurrence, stabbing quality, and moderate intensity, with no specific aggravating or alleviating factors. While denying other acute complaints, he described a 12-lb weight loss over 3 months and a slow-growing right axillary lump for the last 2 months. Past medical history was significant for a “birthmark” extending over his abdomen and lower back, for which multiple excision/grafting procedures were performed at 6 years of age. He denied any noticeable changes in the lesion's size, texture, color, or appearance for the last 20 years. The patient lived in South Africa during childhood and, when he was 10 years old, his father was treated for pulmonary tuberculosis. No other relevant family history was reported and he described a healthy lifestyle During bedside evaluation, the patient was found to have heterogeneous brown-to-black patches/plaques scattered on his torso, buttocks, and lower abdomen with satellite lesions, areas of hypertrichosis, and irregular borders, consistent with partially-excised giant CMN of bathing trunk distribution. The skin lesions were mostly flat except for a nodular border where grafting was previously done. In addition, a 2-cm subcutaneous nodule was palpated on the right axilla. Initial workup was remarkable for elevated serum LDH (350 U/L), elevated serum D-dimer (2.42 mcg/mL) and a left lower lobe density on chest radiography Chest computed tomography (CT) angiography was performed, showing multiple lung nodules (0.3-2.7 cm) Following admission for further diagnostic evaluation, other tests resulted negative (including additional tumor markers, viral serologies, and 3 sputum acid-fast bacillus smears). Abdominal CT demonstrated hypodense lesions in the liver, left inferior renal pole, and bilateral adrenal glands. Brain magnetic resonance imaging showed numerous parenchymal nodules (0.4–1.2 cm). Biopsy of the right mid-back nodular area showed no evidence of malignancy An incisional biopsy of the right axillary nodule was then performed, demonstrating malignant cells (S100+/Melan-A+/Tyrosinase+/PRAME+/BRAFV600E-) diffusely interspersed within fibroadipose tissue Next-generation sequencing found a somatic NRAS (exon 3) mutation. He was diagnosed with M1d(1) melanoma and started on ipilimumab/nivolumab immunotherapy plus brain stereotactic radiosurgery, but showed rapid disease progression. Response to subsequent treatment lines (cisplatin/vinblastine/temozolomide and nivolumab/relatlimab) was similarly poor, with his clinical course being complicated by small bowel intussusception, obstruction and ischemia secondary to intra- and extraluminal metastatic lesions.
CONCLUSION: This report highlights the importance of lifetime monitoring for progression to melanoma in large/giant CMN patients, regardless of whether partial or complete excision was performed earlier in life. Although previous cohorts suggest that most malignant transformations occur during childhood, adults with a history of large/giant CMNs remain at a significantly higher risk of developing melanoma than the general
44
population. As illustrated by the present case, melanomas associated with large/giant CMNs often harbor NRAS mutations, which represent a biomarker of disease aggressiveness and worse clinical outcomes. The ideal management for NRAS-mutant melanoma remains unknown and further clinical studies are urgently needed to improve the prognosis of patients with the condition

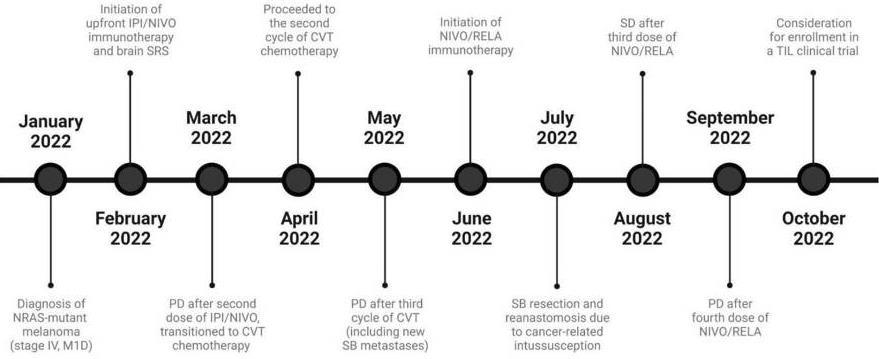 Figure 1: Clinical course timeline
Figure 1: Clinical course timeline
45
Figure 2: Skin lesions on physical exam
ABSTRACT #17
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES/RHEUMATOLOGY
A RARE CASE OF ACUTE INFLAMMATORY DEMYELINATING POLYRADICULOPATHY FOLLOWING PFIZER COVID-19 VACCINE
Vincent Courant1 , Murilo Silva1, Satwant Grewal1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York State Rheumatology Society (NYSRS) Spring Meeting that was held in New York, New York, United States from May 20-21, 2022.
BACKGROUND/INTRODUCTION: We present a case of a 36 year-old female who developed acute inflammatory demyelinating polyradiculopathy (AIDP) after receiving the second dose of Pfizer-BioNTech COVID-19 vaccine. We conducted a literature review on similar cases around the world with the following objectives: [1] To report a rare auto-immune complication of COVID-19 vaccination. [2] To educate and inform physicians about the approach to diagnosing AIDP and narrowing down its etiology.
CASE PRESENTATION: A 36 year-old female with no significant past medical history presented to the hospital with progressive bilateral paresthesia. She started to experience numbness and tingling sensation in her extremities 1 week after receiving the second dose of Pfizer-BioNTech COVID-19 vaccine. Following 5 days of symptoms onset, she was no longer able to hold onto objects and experienced difficulty ambulating without assistance. Physical exam was notable for decreased distal sensation to touch and pain in all 4 limbs, otherwise, the rest of her neurological and musculoskeletal evaluation was normal. MRI-head showed small scattered foci of increased FLAIR signal in the white matter, suggesting an underlying inflammatory process. Electromyography (EMG) was performed and showed evidence of acute diffuse sensorimotor neuropathy with mixed axonal and demyelinating features. These results along with the clinical features allowed us to diagnose our patient with Acute Immune-mediated Demyelinating Polyneuropathy (AIDP). Extensive autoimmune workup, including antiGM1, GD1b, Gq1b, ANA, DS-DNA, RF, CCP, and C/P ANCA were unremarkable. She had positive anti-Ro antibody but did not have any clinical or physical features that would suggest Sjogren’s Syndrome. Vitamin levels (B12, folate, thiamine) were found to be normal. Infectious workup of serum and CSF which included hepatitis, Campylobacter jejuni, Lyme, CMV, and EBV serologies were all negative. The etiology of her disease was attributed to Pfizer BioNTech COVID-19 vaccine given the temporal correlation. She was subsequently treated with 6 cycles of IVIG which resulted in moderate symptomatic improvement.
CONCLUSION: AIDP is an autoimmune-guided inflammatory neuropathy which result in axonal degeneration of myelinated nerves. In some extremely rare events, molecular mimicry following vaccination may lead to this disease. There have been reports of AIDP linked to Johnson & Johnson and AstraZeneca COVID-19 vaccines. Over the past year, a few cases have also been observed with Pfizer BioNTech COVID-19 vaccine. The majority of these cases occurred within 2 weeks following the first dose of the vaccine. Physicians should be made aware that AIDP is a potential complication of COVID-19 vaccination. Given the extreme rarity of these cases, it is also important to highlight that more common infectious and autoimmune etiologies of AIDP should be investigated before attributing any potential causal relationship to COVID-19 vaccines.
46
ABSTRACT #18
CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
ADHERENCE TO NCCN GENETIC TESTING GUIDELINES IN PANCREATIC CANCER AND IMPACT ON TREATMENT
Fionnuala Crowley1 , Sonal Gandhi1 , Michelle Rudshteyn2, Mantej Sembhi1, Deirdre Cohen2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at American Society of Clinical Oncology (ASCO) Annual Meeting which was held virtually and in person in Chicago, Illinois, United States from June 3-7, 2022.
BACKGROUND/INTRODUCTION: NCCN 2019 Guidelines recommend universal germline (GL) testing for pancreatic cancer (PC) patients given germline mutations (gMut) can occur at a similar rate irrespective of an individual’s family history of cancer. Molecular analysis of tumors in those with metastatic disease is also recommended. We aimed to determine rates of genetic testing at our institution, factors associated with testing, and outcomes of those tested.
METHODS: Frequency of GL and somatic testing was examined in patients diagnosed with non-endocrine PC, with >2 visits between June 2019 and June 2021 at the Mount Sinai Health System. The clinic-pathological variables and treatment outcomes were also recorded.
RESULTS: A total 149 patients met the inclusion criteria. 66 patients (44%) underwent GL testing: 42 (28%) at time of diagnosis with the remainder later in treatment. The rate of GL testing increased every year: 33% (2019), 44% (2020), 61% (2021). A family history of cancer was the only variable associated with decision to perform GL testing. 8 patients (12% of patients tested) had pathological gMut: BRCA1 (1), BRCA2 (1), ATM (2), PALB2 (2), NTHL1 (1), both CHEK2 and APC (1). Neither gBRCA patient received a PARP inhibitor, all except one received first line platinum. 98 patients (65.7%) had molecular tumor testing (66.7% of patients with metastases). Two patients with BRCA2 somatic mutations did not have GL testing. 3 patients received targeted therapies.
CONCLUSION: Genetic testing based on provider discretion results in low rates of GL testing. Early results of genetic testing can have an impact on treatment decisions and trajectory of disease. Initiatives to increase testing are needed but must be feasible in real world clinic settings.
47
ABSTRACT #19
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE ENDOCRINOLOGY/HEMATOLOGY/ONCOLOGY
MANAGEMENT OF REFRACTORY HYPOGLYCEMIA IN DOEGE-POTTER SYNDROME WITHOUT AN OPTION FOR CURATIVE SURGERY
Katherine Cuan1 , Jeeyune Bahk1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in Washington DC, United States from May 19-May 24, 2023.
BACKGROUND/INTRODUCTION: Doege-Potter syndrome (DPS) is a rare paraneoplastic syndrome of a solitary fibrous tumor that presents as a hypoinsulinemic hypoglycemia due to the ectopic secretion of prohormone insulin-like growth factor II (IGF-II). Diagnosis of DPS includes symptoms of hypoglycemia with secretion of IGF-II. Complete surgical resection of the underlying tumor is curative in most cases Where surgical resection is not a possibility, high-dose glucocorticoids reduce the frequency and severity of hypoglycemic episodes.
CASE PRESENTATION: A 69-year-old Chinese male with metastatic pelvic solitary fibrous tumor with peritoneal, hepatic, lung, and renal involvement complicated by DPS presented with acute onset dizziness, chills, weakness, abdominal pain, and diarrhea. He had been compliant with chronic steroid therapy at prednisone 30 mg/day. Presenting labs demonstrated hypoglycemia with a fingerstick glucose of 17 mg/dl, leukocytosis, metabolic acidosis, acute kidney injury, and a urinary tract infection. Computed tomography (CT) showed stable metastatic disease compared to a scan a month prior. He was admitted to the intensive care unit for persistent symptomatic hypoglycemia requiring steroids, dextrose-containing intravenous fluids, and frequent blood glucose monitoring. After achieving stable euglycemia with the goal range of 110-150 mg/dl as recommended by Endocrinology, he was downgraded to medical floors on a steroid taper without dextrose supplementation. Up-titration of steroids and re-initiation of dextrose supplementation were needed for multiple episodes of hypoglycemia. Eventually, given his overall poor prognosis with worsening tumor burden and refractory hypoglycemia, the patient was discharged to an inpatient hospice on prednisone 60 mg/day and dextrose supplementation.
CONCLUSION: Without a curative treatment directed at the underlying malignancy, Doege-Potter syndrome can be difficult to manage in patients with metastatic solitary fibrous tumor disease, with risks of hypoxic cerebral injury or death in the setting of severe hypoglycemia. Medical therapy with high-dose glucocorticoids helps reduce frequency and severity of hypoglycemic episodes. However, attaining stable euglycemia even on highdose steroids can be challenging when multifactorial causes for hypoglycemia exists. Our patient’s requirements to maintain euglycemia may have been higher in the setting of an underlying infection and secondary adrenal insufficiency from chronic steroid use. He also likely had an impaired IGF-II clearance given the pre-renal injury from intravascular volume depletion caused by diarrhea. Thus, focus of management should be placed on correcting potential reversible causes of hypoglycemia. Combination of high-dose glucocorticoids with dextrose supplementation is a reasonable medical therapy in such challenging cases where tumor burden and paraneoplastic hypoglycemic syndrome are expected to worsen.
48
ABSTRACT #20
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GENERAL INTERNAL MEDICINE/INFECTIOUS DISEASES
DIFFERENTIAL DIAGNOSIS OF EAR PAIN AND SWELLING IN AN ELDERLY WOMAN
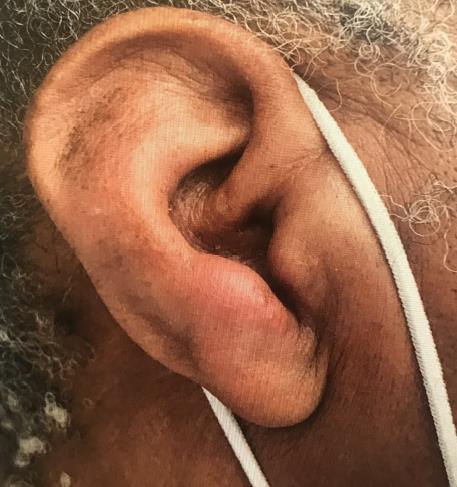
Doreen Mensah1 ,Lady Njemeh Danso1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of General Internal Medicine (SGIM) Annual Meeting that was held in Orlando, Florida, United States from April 6-9, 2022.
BACKGROUND/INTRODUCTION: The differential diagnosis of ear pain and swelling is broad. It can be the only presenting symptom of a serious underlying condition such as malignant otitis externa, other infectious causes or cancer in older patients; therefore, its etiology should be fully explored. Unfortunately, its workup is complex, and no simple algorithm exists. Early recognition, especially those of infectious etiology, is necessary to avoid severe complications such as brain abscess, osteomyelitis, and cranial nerve involvement. If there is a high index of suspicion of a serious but uncertain etiology, as in the case of my patient, early referral and specialty consultation are reasonable options and should not be delayed.
CASE PRESENTATION: A 79-year-old female with a past medical history of hypertension, dyslipidemia, prediabetes, asthma, fibromyalgia, and osteoporosis presented to the clinic with 2 days history of left ear pain extending to the lower jaw and neck, rated 10/10. It was associated with swelling, subjective fever, and chills. The patient denied trauma, ear discharge, itching or hearing loss. Physical exam was remarkable for severe tenderness on mild traction of the pinna, extensive swelling, and erythema of the peri-auricular area extending to the lower jaw with difficulty visualizing the auditory canal. The patient was immediately referred to the hospital due to severity of her symptoms and high index of suspicion for malignant otitis externa. She was hospitalized with an urgent ENT consultation. Initial vital signs were negative for fever and laboratory work-up revealed no leukocytosis. CT-head showed a polypoid lesion in the nasal cavity and soft tissue swelling. Despite the severity of her symptoms, the patient did not meet the diagnostic criteria for malignant otitis externa and other diagnosis such as cellulitis of the external ear was considered. She was treated with Piperacillin-Tazobactam for 2 days with improvement of her symptoms and was discharged on Cefalexin for an extra 8 days and ciprofloxacin ear drops. An ear wick was also placed. She was scheduled for a close ENT follow up due to concerns for potential infectious complications and further investigation of the polyploid lesion found in the nasal cavity.
CONCLUSION: The differential diagnosis of ear pain and swelling in the elderly, especially those with co-morbid conditions, is broad and can include infectious and non-infectious causes. Therefore, it is essential for clinicians to fully explore its etiology. Early diagnosis and treatment is warranted, especially those of infectious causes, to avoid severe complications. Assess thoroughly an older patient who presents with ear pain and swelling and be familiar with the differential diagnosis. Recognize the severity of symptoms that will warrant early hospital referral and specialty consultation.
49
ABSTRACT #21 QUALITY IMPROVEMENT GENERAL INTERNAL MEDICINE/PULMONARY/CRITICAL CARE
IMPROVING ASTHMA DOCUMENTATION AND MANAGEMENT AT A COMMUNITY-HEALTH CENTER IN CENTRAL HARLEM
Juan Vasquez Mendez1 , Dalgis J. Dunker1 , Anne Socorro Corrales1, Erick Kawegere1, Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of General Internal Medicine (SGIM) Annual Meeting that was held in Orlando, Florida, United States from April 6-9, 2022.
BACKGROUND: Without a standardized clinic-based process to capture disease status and risk factors, many patients with asthma will fail to achieve optimal management of their disease.
METHODS: To help standardize best practices for our patients with asthma, we 1. Collaborated with our IT Department to design a user-friendly EMR template to standardize documentation of symptom control and risk factors and 2. Developed a Provider Action Plan to improve adherence with GINA guidelines for medication management. Resident providers were informed of the template and Provider Action Plan during daily pre-clinic huddles over a 4-month period. We aimed to target completion of the asthma template for 40% of patients with asthma over a 6-month period and to improve adherence with GINA guidelines for medication management by 30% by tracking Long-Acting Beta Agonist (LABA)-Inhaled Corticosteroid (ICS) prescriptions.
RESULTS: This project is based at Ryan Health Adair, a Federally Qualified Health Center that serves as the primary care practice site for internal medicine residents. The patient population is approximately 45% Black and 30% Hispanic, with the vast majority of patients enrolled in Medicaid insurance. We retrospectively reviewed 299 patients with an asthma diagnosis from 9/14/19 to 9/14/20. We found that 69% of these patients were not receiving controller medication as per current GINA guidelines, 15.4% lacked an appropriate ICD code/asthma classification, and overall, we demonstrated poor documentation of symptom control. To date, our initiative resulted in budesonide-formoterol prescriptions for 34.13% of the patients with asthma since the integration of the EMR template and the Provider Action Plan. Rates of completion of the EMR template for our patients with asthma will be collected in February 2022 at the 6-month mark.
CONCLUSION: A streamlined EMR asthma template coupled with a Provider Action Plan shows promise in improving best practices for asthma management for our patients at a federally qualified health center. One limitation is that by only tracking budesonide-formoterol prescriptions we are likely underestimating appropriate prescribing patterns, since a significant number of patients were prescribed ICS + short-acting beta-agonists as an alternative when budesonide-formoterol was not covered by insurance.
50
ABSTRACT #22
CLINICAL RESEARCH CARDIOLOGY
PROGNOSTIC UTILITY OF EXERCISE STRESS ECHOCARDIOGRAPHY IN PATIENTS WITH INDETERMINATE RESTING DIASTOLIC FUNCTION
Joseph Elias1 , Alaa Omar1, Ga Hee Kim1, Swiri Konje1, Loba Alam1, Elizabeth Zipf1, David Meister1 , Christopher Perez Lizardo1, Maria K. Peña1, Brissete Mancero1, Errol Moras1, Kruti Dhaval Gandhi1, Arpanjeet Kaur1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
BACKGROUND/INTRODUCTION: The clinical significance of stress testing in symptomatic patients with indeterminate diastolic function has not been well studied. This study aims at evaluating the prognostic utility of exercise stress echocardiography in patients with baseline indeterminate diastolic function.
METHODS: Between 2017 and 2020, symptomatic patients referred for exercise stress echocardiography who had resting indeterminate diastolic function and had exercise stress echocardiography negative for ischemia were included. Patients were classified into those without traditional risk factors or cardiovascular co-morbidities (CR-) and those with any risk factor or co-morbidity (CR+). Abnormalities in the resting septal mitral annular early diastolic velocity (e’) or post-exercise E/e’ ratio were used to define diastolic abnormality. Patients were followed for a median of 2.6 years for the composite outcome of death, acute coronary syndrome, stroke, cardiac hospitalization, future ischemia testing, and revascularization.
RESULTS: We included 470 patients [age: 60 ± 12 years, 273 (58%) women, EF: 61 ± 6%, 100 (21%) CR-, and 370 (79%) CR+]. 196 patients had no diastolic abnormality (DA-) and 274 patients had diastolic abnormality (DA+). During the follow-up period, 7 patients died, 9 patients had acute coronary syndrome, 4 patients had stroke, 40 patients had cardiac hospitalization, 10 patients had revascularization, and 63 patients required repeat ischemia testing. The composite events occurred in 100 patients. The composite outcome was more frequent in CR+ compared to CR- patients [92 (25%) versus 8 (8%), p<0.001] as well as in DA+ compared to DA- patients [67 (24%) versus 33 (17%), p=0.047]. Among CR+ patients, DA+ patients had more events compared to DApatients [63 (25%) versus 29 (13%), p=0.001]. Importantly, compared to CR- patients, the events were significantly associated with CR+/DA+ (HR, 2.71; 95%CI, 1.3–5.6), but not CR+/DA- patients (HR, 1.9; 95%CI, 0.85–4.1).
CONCLUSION: Exercise stress echocardiography can unmask diastolic abnormality in patients with resting indeterminate diastolic function. In patients with elevated baseline clinical risk, exercise stress echocardiography can add significant prognostic information.
51
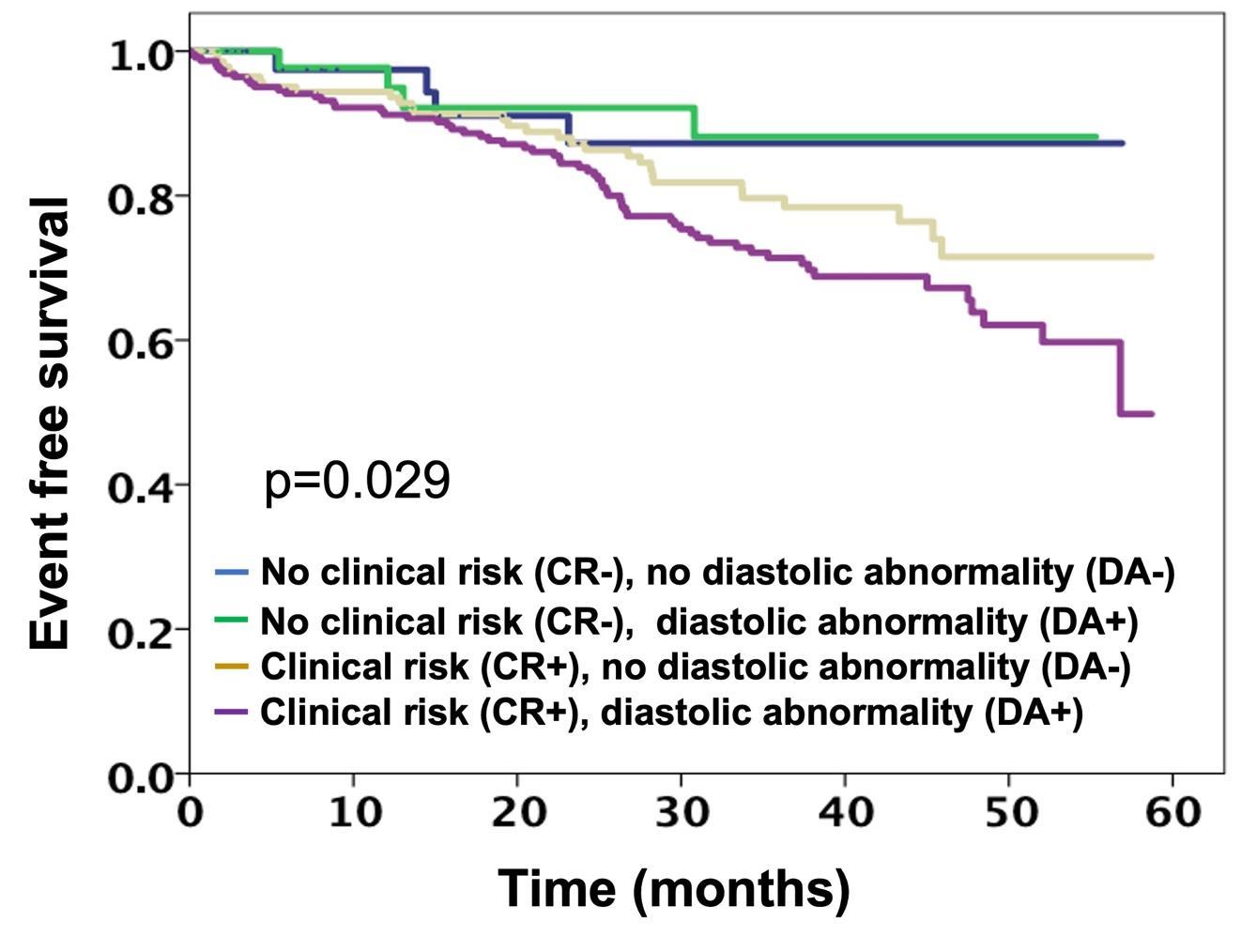
1: 52
Figure
ABSTRACT #23 CLINICAL RESEARCH ALLERGY/IMMUNOLOGY
REPORT OF INDOOR MOLD EXPOSURE AND RHINITIS IN PRESCHOOL CHILDREN ATTENDING HEAD START CENTERS IN NEW YORK CITY
Jin Feng1, Adnan Divjan 2, Luis Acosta2, Andrew Rundle2, Maxine Ashby Thompson2, Judith S. Jacobson2 , Matthew S.
Perzanowski2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
Presented at the American Academy of Allergy Asthma and Immunology (AAAAI) Annual Meeting that was held in San Antonio, Texas, United States from February 24-27, 2023.
BACKGROUND/INTRODUCTION: Although fungal exposure is known to cause rhinitis symptoms, few studies have focused on rhinitis among preschool children living in lower-income, urban neighborhoods. We hypothesized that mold exposure would be associated with rhinitis symptoms independent of pest exposure and that this risk would be modified by asthma symptoms.
METHODS: Children ages 2-5 years were recruited from Head Start Centers. Parents were queried about the child’s health, including rhinitis (runny nose in the absence of a cold) and environmental exposures, including mold or mildew on home surfaces in the past year. Prevalence ratios (PR) were calculated in models adjusted for sex, race, maternal education, maternal asthma, and reports of mice, rats, or cockroaches and were stratified by reported asthma symptoms in the past year.
RESULTS: Among children with complete data (n=973), rhinitis was common (46.5%), as were asthma symptoms (39.1%). Just over half (56.4%) of children with rhinitis also had asthma symptoms. Reports of mold were common (18.5%), most often in the bathroom (11.1%), followed by the kitchen (5.3%) and the parent’s (4.6%) and child’s (3.1%) bedrooms. In multivariable models, children exposed to mold were more likely to have rhinitis (PR=1.36, p=0.008). In stratified analyses, mold was associated with rhinitis only among children without and not among those with asthma symptoms (PR=1.55, p=0.014 versus PR=1.13, p=0.48, respectively; Pinteraction=0.15).
CONCLUSION: Among preschool children in lower-income NYC communities, report of domestic mold was associated with increased risk of rhinitis, specifically among children without asthma symptoms, children who may be at greater risk for future asthma incidence.
53
ABSTRACT #24
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
COST OF CARE AWARENESS AMONG INTERNAL MEDICINE HOUSE STAFF
Madelin Fenianos1 , Alexandria Markley1 , Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Residents starting their clinical training have limited knowledge of the complexity of healthcare cost. However, they face challenges early on with how to improve health care delivery and patient compliance as well as to ease patients’ financial healthcare burden without jeopardizing the bedside experience. This study aimed to assess the level of cost awareness among Internal Medicine residents in a large academic medical center.
METHODS: A cross-sectional survey was conducted among Internal Medicine residents using a questionnaire. The survey included questions on their knowledge of the costs of common inpatient lab tests and imaging, perceptions of their own cost awareness and their attitudes towards integrating cost into behavior of ordering tests. We then incorporated the cost of common labs and imaging into 4 interactive afternoon reports where a clinical case was discussed among internal medicine residents. During the session, residents were divided into groups and were encouraged to order the minimum tests needed to reach a diagnosis with those ordering the least number of tests to diagnose the disease won. Subsequently, the prices were shown next to each test ordered in a range value. The prices were obtained from the hospital’s standardized Medicare cost list and the online cost-estimator calculator from the hospital’s website that provided a price range depending on insurance coverage. A post-intervention survey was then conducted at the end of the afternoon report.
RESULTS: A total of 63 Internal Medicine residents participated in the survey, representing a response rate of 48%. Interestingly, 71% did not feel comfortable with their knowledge about the costs of common labs and imaging. For example, less than half of residents correctly estimated the cost of a chest x-ray or a complete blood count. 76.1% agreed that cost of a test would influence the frequency of ordering it. Furthermore, 81% of residents reported that they had inadequate access to information of the cost of these tests, and 70% felt that cost considerations were not adequately incorporated into clinical decision-making as they reported that they never or rarely factored in costs when ordering tests. While only 19 residents responded to the post-intervention survey, the results were overwhelmingly positive. A total of 95% felt that physicians should factor in costs in patient care, 100% agreed that these interactive reports improved their knowledge about cost of common tests, and 89% felt that knowing the cost influences their frequency of ordering them.
CONCLUSION: Although some residents had received a form of education on cost containment during their medical training, there were significant gaps in their knowledge of the costs of common medical tests. These findings suggest that while medical residents are aware of the importance of cost in healthcare, there is insufficient and difficult to obtain data regarding specific costs. Given the increasing focus on value-based care and the importance of containing healthcare costs to decrease the financial burden on patients and increase compliance, efforts to improve cost awareness among medical residents should be a priority for medical education and training programs. High value care teaching in an interactive and repetitive method to try to integrate cost awareness into physicians’ ordering behavior helped in closing that knowledge gap.
54
ABSTRACT #25
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE NEPHROLOGY
MERCURY INDUCED MEMBRANOUS NEPHROPATHY IN A YOUNG FEMALE
Debbie Marie Fermin1 , Tamara Goldberg1, Karim El Hachem1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Aurora, Colorado, United States from May 10-13, 2023.
CASE PRESENTATION: A 41-year-old female with no past medical history presented to her primary care physician with a 4-month history of bilateral leg swelling and fatigue as well as chronic rash on both hands. She denied fever, chest pain, shortness of breath, orthopnea, abdominal pain, or bowel or urinary symptoms. She recently came from Senegal and her only medication was a topical steroid as well as a cosmetic skin lightening cream that she used for years. Physical examination was pertinent for lichenified plaques on the dorsum of her hands, grade 3 bilateral pitting edema to the knees with normal cardiovascular and lung exams. Lab tests showed hypoalbuminemia (2.2 mg/dL), normal GFR, elevated total cholesterol (654 mg/dL) as well as proteinuria (1348 mg/dL). Given her edema, proteinuria, and severe hyperlipidemia she was referred to Nephrology for workup of nephrotic syndrome. A 24-hour urine protein yielded 9.936 g/24 hr. Other infectious, metabolic, and autoimmune labs were unremarkable. A kidney biopsy was consistent with secondary membranous nephropathy. Given prolonged exposure to a skin lightening product, blood and urine mercury levels were sent and were elevated (blood= 20.3 ug/L), (urine= 245 ug/L), and (mercury/creatinine ratio = 228 ug/g). She was advised to discontinue her lightening cream, started on furosemide and atorvastatin, and referred to Toxicology where she underwent chelation treatment with succimer. Over the next 6 months, the patient’s bilateral leg swelling, fatigue, and hypertension markedly improved. Lab markers revealed reduction in 24-hour urine mercury (30 ug/L) and mercury/creatinine ratio (38 ug/g creatinine), and reduced total cholesterol (242 mg/dL).
DISCUSSION/CONCLUSION: This case highlights the importance of mercury exposure as a potential cause of nephrotic syndrome. While mercury toxicity is rare, one method of potential exposure is through transdermal absorption from lightening creams. Mercury has a strong affinity for renal tissue deposition making the kidneys particularly susceptible to injury. The most common underlying pathology is membranous nephropathy, followed by minimal change disease. The diagnosis of chronic mercury-induced nephropathy should be suspected in patients with nephrotic syndrome, exposure to mercury containing products, and elevated 24-hour urine mercury. Therefore, including a history of transdermal cosmetic product use, particularly from outside the United States, is essential to help inform the diagnosis. The overall prognosis of membranous nephropathy secondary to mercury toxicity is generally good following immediate cessation of exposure and chelation treatment.
Mercury-associated renal damage commonly presents as nephrotic syndrome with membranous nephropathy and minimal change disease as major pathological features. Consider transdermal mercury-toxicity as a cause of nephrotic syndrome, particularly in women without other risk factors. Membranous nephropathy secondary to repeated exposure to mercury has an overall good prognosis. Chelation is the mainstay treatment.
55
ABSTRACT #26
CLINICAL RESEARCH CARDIOLOGY
PROGNOSTIC VALUE OF EXERCISE ASSOCIATED DIASTOLIC ABNORMALITIES IN PATIENTS WITH ELEVATED RESTING SYSTOLIC BLOOD PRESSURE
Kruti Dhaval Gandhi1, Alaa Omar1, Swiri Konje1, Loba Alam1, Errol C. Moras1, Brissete Mancero1, Elizabeth A. Zipf1, David Meister1, Arpanjeet Kaur1, Maria K. Peña1, Christopher Perez Lizardo1, Ga Hee Kim1, Joseph Elias1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
BACKGROUND/INTRODUCTION: We studied the prognostic value of exercise-associated diastolic abnormalities (DA) in patients with elevated resting systolic blood pressure (SBP) during exercise stress echocardiography
METHODS: Patients referred for exercise stress echocardiography (2017 – 2020) with resting SBP>140 mmHg were studied and followed for a median of 3.1 years for the combined outcome of death, acute coronary syndrome, stroke, or cardiac hospitalization. Diastolic abnormalities was defined as abnormalities in resting tissue doppler derived mitral annular velocity (e’) and post exercise E/e’ ratio.
RESULTS: We studied 651 patients (age: 62 ± 12 years, 371 (57%) women, EF: 60 ± 7%). 399 (61%) patients had DA, and 113 (17%) patients had an ischemic exercise stress echocardiography, which was more prevalent in DA+ patients [84 (21%) versus 29 (12%), p=0.002]. Compared to DA-, DA+ patients were older, had worse exercise capacity, and worse resting diastolic parameters. During follow-up, 10 patients died, there were 17 acute coronary syndromes, 4 strokes, and 55 hospitalizations. The combined events occurred in 86 patients. DA+ patients had higher rates of combined events [65 (16%) versus 21 (8%), p=0.003], which was also seen on univariate analysis (HR, 2.1; 95%CI, 1.3 to 3.4). Overall, the presence of DA stratified patients with and without ischemia to a higher risk for events, which was only statistically significant in the presence of ischemia (DA-: HR, 3.5; 95%CI, 1.3 to 9; DA+: HR, 6.8; 95%CI, 3.7 to 12.7). The findings persisted after multivariate adjustment and propensity score matching for covariates.
CONCLUSION: Exercise associated diastolic abnormalities are common among symptomatic patients referred for exercise stress echocardiography with elevated resting systolic blood pressures and have a prognostic value in the presence of myocardial ischemia.
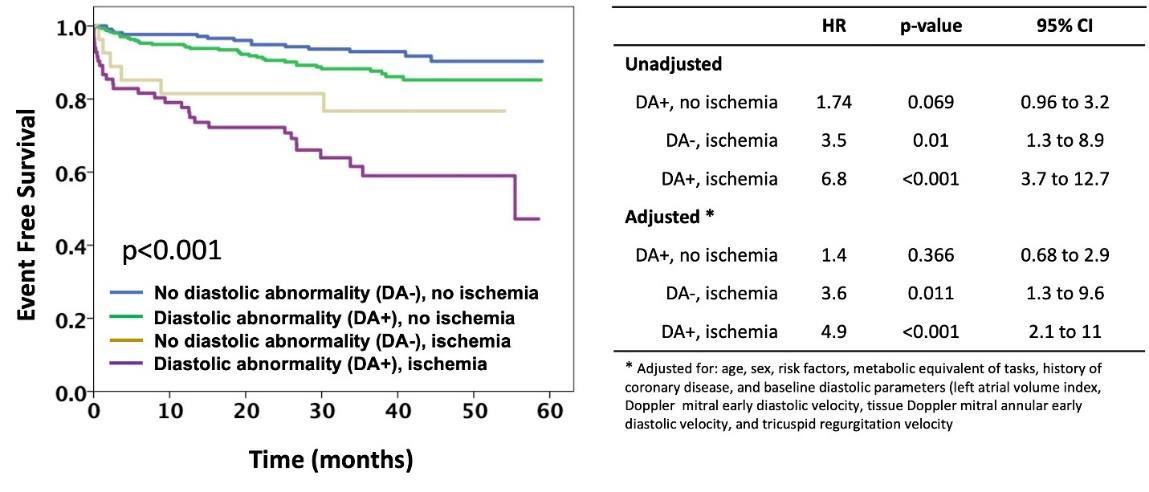
56
Figure 1: Kaplan-Meir Curve and Cox Regression Model highlighting time to event
ABSTRACT #27
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY
IMPACTS OF SOCIAL DETERMINANTS OF HEALTH ON DUAL ANTIPLATELET THERAPY FOR ACUTE CORONARY SYNDROME
Christopher Gold1 , Dipal Patel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of General Internal Medicine (SGIM) Annual Meeting that was held virtually from April 21-April 24, 2021.
CASE PRESENTATION: A 69-year-old female with unknown past medical history was brought into the Emergency Department after being found unconscious. ECG showed ST elevations in leads II, III and avF, reflecting myocardial infarction. After intubation for acute respiratory failure, she was loaded with ticagrelor and aspirin and rushed to emergent coronary angiogram and PCI of the RCA. Mechanical thrombectomy was performed, along with placement of a drug-eluting stent. After an extensive stay in the Cardiac Care Unit, she was discharged with prescriptions for aspirin, ticagrelor, lisinopril, atorvastatin, and metoprolol, along with a limited supply of ticagrelor. One week after discharge, the family contacted the hospital about medication costs. The patient was only taking ticagrelor. During a Cardiology follow up, she was given medication coupons. At her primary care follow up, she reported being unable to afford ticagrelor despite the coupons that reduced the outof-pocket monthly cost of $1,200 to $600. She had yet to start her other medications. After discussion with her Cardiologist, the regimen was changed to clopidogrel, available at the local 340B pharmacy for $30 per month.
DISCUSSION/CONCLUSION: This clinical vignette illustrates a complex but common example of myocardial infarction requiring PCI and DAPT. In the inpatient setting, evidence-based treatment was followed. According to the American Heart Association and American College of Cardiology, ticagrelor is a reasonably preferred antiplatelet agent to be administered with aspirin for acute coronary syndrome
However, when transitioning to an outpatient setting, other factors need to be considered. This patient had limited insurance coverage of her medications. Although this was somewhat addressed with the coupons, her socioeconomic status was not taken into consideration. Coupons reduced the cost of ticagrelor by half, but as this medication is needed at least 12 months, this was not a solution. Additionally, the other medications could not be obtained. Like ticagrelor, clopidogrel is effective in improving outcomes and reducing cardiovascular events. Moreover, it is available as a generic formulation with a much cheaper price. Although one can argue preference for ticagrelor, in situations where the more expensive drug cannot be obtained, clopidogrel is a practical alternative.
For STEMI treated with stent, DAPT with aspirin and a P2Y12 inhibitor (eg, ticagrelor, clopidogrel) should be administered for at least 12 months. While ticagrelor has been shown to result in fewer cardiovascular events and death, clopidogrel is an effective and cheaper option. It is imperative to assess social determinants of health when prescribing treatment options.
57
ABSTRACT #28
CLINICAL RESEARCH GASTROENTROLOGY
PREDICTORS OF MORTALITY AFTER TRANS-JUGALAR INTRAHEPATIC PORTOSYSTEMIC SHUNT PROCEDURE
Suhail Haddadin1 , Patricia Miguez Arosemena1, Farah Haddadin2 , Rand Fram2 , Samuel J. Daniel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Faculty of Medicine at Jordan University of Science and Technology, Amman, Jordan
Presented at the American Association for the Study of Liver Diseases (AASLD) Annual Meeting held in Washington DC, United States from November 4-8, 2022.
BACKGROUND/INTRODUCTION: Trans-jugular intrahepatic portosystemic shunt (TIPS) plays an important role in the management of complications of portal hypertension. Mortality prediction is important in these patients as they constitute a high-risk population. Therefore, the aim of our study was to identify risk factors related to higher mortality rates after TIPS.
METHODS: Using the National Inpatient Sample Database, we examined patient demographics, comorbidities predictors for in-hospital mortality after TIPS procedure during 2016. Our cohort included of all adults (≥18 years) using an ICD-10 diagnosis and procedure codes.
RESULTS: In our retrospective study, a total of 5415 patients underwent TIPS procedure in 2016. Mean age was 56 years old, 2,020 (37%) were males with a mean length of stay 9.6 days. The most common indication for TIPS was ascites (61%). Most frequent comorbidities were hypertension (32%), chronic kidney disease (14%), dyslipidemia (13%), and obesity (12%). On multivariate analysis, all-mortalities rates post TIPS were associated to hepatorenal syndrome (OR, 3.55; 95%CI, 2.02-6.24; p <0.001), hepatic encephalopathy (OR, 3.46; 95%CI, 1.05-11.38; p<0.040), end stage renal disease (OR, 2.95; 95%CI, 1.15-7.54; p<0.024) andprotein caloric malnutrition (OR= 1.82; 95% CI, 1.02-3.27; p<0.042). Higher all-cause mortality was also reported for admissions over the weekend (OR, 1.84; 95%CI, 1.05-3.24; p=0.033) and self-pay insurance (OR, 8.49; 95%CI, 1.62- 44.51; p<0.011), while TIPS performed as elective procedure was associated with lower all-cause mortality (OR, 0.27; 95%CI, 0.09-0.73; p=0.010). When varices were the primary indication for TIPS, patients had almost four times higher risk of mortality when compared to ascites as primary indication.
CONCLUSION: This study shows that complications states of liver cirrhosis and patients who underwent TIPS procedure due to varices rather than ascites have overall worse prognosis.
58
ABSTRACT #29
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE ENDOCRINOLOGY
SEVERE HYPOPHOSPHATEMIA OCCURRING AFTER REPEATED EXPOSURE TO A PARENTERAL IRON FORMULATION
Keerthana Haridas1 , Alice Yau1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in Case Reports in Endocrinology, 2022. PMID: 36248222
BACKGROUND/INTRODUCTION: Hypophosphatemia is a less known complication of parenteral iron use, particularly after the use of certain iron formulations.
CASE PRESENTATION: We report the case of a young male with inflammatory bowel disease and iron deficiency anemia, who developed severe symptomatic hypophosphatemia after his third exposure to iron carboxymaltose, with no evidence of the same occurring upon prior exposure to the compound. Investigations revealed serum phosphorous levels of 0.7 mg/dl, corrected serum calcium of 9-9.5 mg/dl, alkaline phosphatase of 50 U/L (38-126), 25-hydroxy vitamin D level of 40.2 ng/ml and intact parathyroid hormone (PTH) elevated to 207 pg/ml. Urine studies indicated renal phosphate wasting. Presentation was not in keeping with refeeding syndrome. Intact FGF 23 level, measured after the initiation of treatment was within the normal range at 179 RU/mL (44-215). 1,25-dihydroxy vitamin D level, also measured after the initiation of treatment, was normal at 26.3 pg/ml (19.9-79.3). The patient was treated with calcitriol and aggressive oral and intravenous phosphorous repletion. Symptoms then resolved and the patient was discharged on an oral regimen. This phenomenon is postulated to occur due to an increase in the level and activity of iFGF23 and decreased cleavage of the same due to anemia as well as use of the specific iron formulation.
CONCLUSION: This is the first instance, in our literature review, of this complication known to occur, not after initial exposure to an implicated iron formulation but occurring on subsequent exposure.
59
ABSTRACT #30
CLINICAL RESEARCH
PALLIATIVE CARE/PULMONARY/CRITICAL CARE
EARLY CONSULTATION TO PALLIATIVE CARE IN THE INTENSIVE CARE UNIT DECREASES LENGTH OF STAY
Ariela Hazan1 , Jeeyune Bahk1, Ariel Gordon1, Mantej Sehmbhi1, Jennifer Fung1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the European Association for Palliative Care Congress (EAPC) that will be held in Rotterdam, Netherlands from June 15-17, 2023.
BACKGROUND/INTRODUCTION: Use of intensive care unit resources at the end of life with low likelihood of survival is common. Studies have shown that use of specific criteria (“triggers”) which prompt proactive referral for Palliative Care consultation reduces intensive care unit (ICU) length of stay without a change in mortality. We aimed to analyze primary outcome measures of total and ICU lengths of stay, time from ICU admission to hospital discharge, with secondary measures of mortality rates and discharge disposition, in relation to time to Palliative Care consultation.
METHODS: We performed a descriptive retrospective cohort study identifying characteristics and analyzing outcomes of patients with Palliative Care consult during ICU stay at our institution from January to December 2021.
RESULTS: A total of 84 patients with mean age of 70 years, majority (n= 44, 52%) female patients, from home (n=60, 71%) were included. Most had at least two out of six co-morbidities (n=65, 77.4%). Mean hospital and ICU length of stay were 26.5 and 16.5 days, respectively. Mean number of days from ICU admission to initial Palliative Care consult was 8.6 days and the mean number of days from Palliative Care consult to discharge was 13.4 days. A total of 62 patients expired during the same admission (75.6%), 59.5% in an ICU. 47.6% (n=40) had a code status change with Palliative Care consult, with it resulting in hospital and ICU length of stay reduction by 11.4 days and 7.64 days respectively (p<0.05). Hospital and ICU length of stay were significantly associated with an increased duration from ICU admission to Palliative Care consult: β-coefficient 0.66, 0.79 for each day, p=0.015, p<001, respectively. No variables were identified to be predictors of earlier Palliative Care consult during ICU admission.
CONCLUSION: Earlier Palliative Care consult can lead to code status change and shorten length of stay in the intensive care unit. High risk patients (older age, >2 comorbidities, nursing home residents) did not lead clinicians to consult Palliative Care earlier but should be evaluated as triggers in future studies to facilitate earlier consults in order to optimize patient care and resource allocation.
60
ABSTRACT #31 MEDICAL EDUCATION ENDOCRINOLOGY
RESIDENT EDUCATION FOR IMPROVED QUALITY AND CONFIDENCE IN INPATIENT HYPERGLYCEMIA
Maxwell E. Horowitz1, Keerthana Haridas1, Sananda Moctezuma1, Rahul Agarwal1
1Mount Sinai Morningside-West Hospital Center, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 26, 2022 and at the Endocrine Society Annual Meeting that was held in Atlanta, Georgia, United States from June 11-14, 2022.
BACKGROUND/INTRODUCTION: Hyperglycemia is widely prevalent in hospitalized patients and has been associated with adverse outcomes and increased mortality. Guidelines for inpatient management of hyperglycemia in non-critically ill adults are inconsistently implemented within our hospital system in a large academic center in New York. Thus, we strove to develop a formal curriculum for our internal medicine program to improve the level of confidence in trainees when managing inpatient hyperglycemia and to promote appropriate subspecialty consultation.
METHODS: We designed a three-phase educational curriculum for internal medicine residents of all training levels. The first phase consisted of a pre-intervention questionnaire distributed online, examining the selfreported level of confidence and knowledge of hyperglycemia management in non-critically ill patients. The second phase consisted of a 50-minute lecture providing background on the prevalence and risk of inpatient hyperglycemia, standard guidelines for inpatient hyperglycemia management, appropriate insulin regimen initiation and adjustment and practice questions reviewed in real time. The third phase consisted of an online post-intervention questionnaire which, in addition to reassessing confidence and knowledge, examined change in individual confidence level in hyperglycemia management and the ability to recognize situations appropriate for endocrinology consultation. In the context of convenience sampling, all residents were eligible to participate in the second questionnaire independent of their participation in the first questionnaire or educational intervention.
RESULTS: There were 57 total respondents for the pre-intervention questionnaire and 54 total respondents for the post-intervention questionnaire. 26 (48%) of the post-intervention questionnaire respondents completed the initial questionnaire and 22 (41%) attended the lecture. In examining confidence in managing inpatient hyperglycemia on a four-level scale (“not comfortable” , “somewhat comfortable” , “comfortable”, and “very comfortable”), there was an overall increase in percentage of “comfortable” responses (26% to 52%) with a subsequent decrease in “somewhat comfortable” responses (65% to 37%) when comparing post- to preintervention questionnaires. In addition, there was a higher percentage of “comfortable” responses in those who attended the lecture versus those who did not (59% versus 47%). Furthermore, 21 of the 22 respondents who attended the lecture felt “more confident” in their ability to treat inpatient hyperglycemia. Lastly, those who attended the lecture were more likely to identify situations in which endocrinology should be consulted.
CONCLUSION: Currently, there is no formal longitudinal curriculum established for resident education in inpatient diabetes care and hyperglycemia management. The objective of this intervention was to identify and bridge the gap in practical knowledge and confidence level across all training levels. In a small sample size of residents, data revealed higher confidence in management and ability to recognize the necessity of endocrinology consults. Future research will focus on analyzing concrete data in a target unit to assess translation of the intervention to improved quality of inpatient glycemic control.
61
ABSTRACT #32
CLINICAL RESEARCH
ALLERGY AND IMMUNOLOGY/INFECTIOUS DISEASES
SARS-COV-2 INFECTIONS IN INBORN ERRORS OF IMMUNITY: A SINGLE CENTER STUDY
Kimberley Cousins1, Nicholas DeFelice1 , Stephanie Jeong1 , Jin Feng2 , Ashley Sang Eun Lee1, Karina Rotella1 , David Sanchez1 , Faris Jaber2 , Shradha Agarwal1, Hsi-en Ho1 , Charlotte Cunningham-Rundles1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in Frontier’s Immunology, 2022. PMID: 36479106
BACKGROUND/INTRODUCTION: Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a singlestranded RNA virus that causes coronavirus disease 2019 infection (COVID-19). An increased risk of death and severe disease was noted among elderly patients and those with preexisting medical conditions. Little has been reported on larger cohorts of patients with inborn errors of immunity diagnosed with COVID-19 infections. We set out to investigate if this population was particularly vulnerable to COVID-19 infection, and if vaccination altered their risk profile.
METHODS: We reviewed the data of COVID-19 infections in a single center cohort of 113 patients from the Mount Sinai Immunodeficiency program, who had 132 infections between January 2020 and June 2022. The cohort included 56 males and 57 females, age range 2 – 84 years (median=42 years).
RESULTS: The mortality rate in our cohort was 3%, compared to 1.1% in the general population. Comparison between admitted patients revealed a significantly increased risk of hospitalization amongst the unvaccinated patients, 4% vaccinated versus 40% unvaccinated (OR, 15.0; 95%CI, 4.2–53.4; p<0.00001). Although vaccination reduced the risk of hospitalization, there was no correlation between antibody level and need for hospitalization.
CONCLUSION: Our study shows that patients with inborn errors of immunity are at increased risk of death from COVID-19 infections compared to the general population. It also shows that vaccines are protective from severe disease Lastly, it shows that antibody titers are not predictive of disease severity in patients with inborn errors of immunity
62
ABSTRACT #33 MEDICAL EDUCATION CARDIOLOGY/PULMONARY/CRITICAL CARE
A NOVEL SIMULATION BASED APPROACH TO IMPROVE INTERNAL MEDICINE RESIDENTS’ CONFIDENCE AND KNOWLEDGE IN PERFORMING BEDSIDE CARDIAC POINT-OF-CARE ULTRASOUND Arpanjeet Kaur1, Arshdeep Dhaliwal2, Yoni Balboul1, Barbara Karagiannis1, Harrindra Seepersaud1 , Priscilla Loanzon1, Susannah Kurtz1, Adam Rothman1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Mount Sinai Institute of Medical Education Annual Research Day in New York, New York, United States on April 27, 2023.
BACKGROUND: Cardiac point-of-care ultrasound (POCUS) can complement traditional bedside physical examination and serve as an efficient and cost effective diagnostic tool. However, lack of dedicated training remains a major barrier to POCUS use as most internal medicine residency programs lack a standardized POCUS curriculum. We therefore developed a novel cardiac-focused POCUS curriculum for internal medicine residents, integrating simulation-based hands-on learning with didactics to increase trainee knowledge and confidence in using bedside cardiac POCUS.
METHODS: This was a prospective study assessing Internal Medicine residents’ knowledge and confidence of basic cardiac ultrasound knowledge using a pre and post-test design in the Center for Advanced Medical Simulation. All participants completed a pre-test questionnaire, followed by a didactic session, simulation case presentation, debrief and a post-test questionnaire. There was a total of 98 participants, of which 83 residents (PGY1: n=38; PGY2: n=23; PGY3: n=22) completed both the pre and post-test questionnaires used for analysis. The questionnaires evaluated both overall confidence level (7 questions using a four-point Likert scale) and knowledge (21 questions) and specifically assessed learners’ abilities to obtain basic cardiac POCUS views, analyze left and right ventricular function, and identify the presence and size of pericardial effusions. After completing the pre-test questionnaires, learners received a 20-minute didactic session covering these topics, followed by a case-based simulation session testing learner’s ability to utilize POCUS knowledge within a clinical context. This was then followed by a learner-centered debriefing session and a post-test questionnaire. For each PGY level, pre-test and post-test scores for every participant were calculated using SPSS, and a paired t-test analysis was completed to compare the mean difference in confidence levels and knowledge amongst the PGY levels.
RESULTS: A total of 83 residents (PGY1: n=38; PGY2: n=23; PGY3: n=22) completed both pre-and post-test questionnaires. The mean increase in knowledge score was 28% for PGY-1s (p<0.01), 20% for PGY-2s (p<0.01) and 16% for PGY-3s (p<0.01). For confidence assessment, there was statistically significant increase of 1.29 points, 0.79 points and 0.44 points on post-test surveys for PGY-1s, 2s, and 3s, respectively.
CONCLUSION: Our curriculum significantly improved trainee’s knowledge and confidence in POCUS image acquisition and interpretation, indicating that a multifaceted approach utilizing simulation-based training and traditional didactics is effective for POCUS training.
63
ABSTRACT #34
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
ATYPICAL PRESENTATION AND DIAGNOSIS OF AIDS-RELATED CMV ENCEPHALITIS
Erick Kawegere1 , Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in BMJ Case Reports, 2022. PMID: 36041775
BACKGROUND/INTRODUCTION: This case of a patient with AIDS-associated CMV encephalitis serves to highlight three main teaching points. First, thorough history-gathering to assess risk of immunocompromised status can broaden an initial differential, avoid anchoring bias, and facilitate prompt diagnosis when evaluating a patient with neurologic symptoms. Second, vigilance is needed in corroborating symptoms with radiographic findings. Our patient’s brain imaging was not consistent with toxic encephalopathy and in combination with persistent ataxic symptoms, lumbar puncture helped secure the diagnosis. Third, this case presents an example of atypical imaging findings in AIDS-associated CMV encephalitis. When CMV encephalitis is suspected, the utility of brain imaging is to support the diagnosis and exclude other intracranial processes, such as progressive multifocal encephalopathy and lymphoma. But in our case, CMV was not an initial consideration, and it was only through the brain MRI that we were pointed toward the diagnosis.
CASE PRESENTATION: A middle-aged right-handed man with past medical history significant for posttraumatic stress disorder, presented to the Emergency department (ED) with altered mental status, ataxia, blurred vision, headache, and dizziness. He was brought to the ED by police from a local hotel where the staff reported his erratic behavior. The patient reported feeling stressed living with his sister in the Bronx, and decided to spend few nights at a hotel, where he snorted amphetamines and mushrooms. He frequently used such drugs but denied injection drug use. The patient associated with moderate bitemporal headache and weight loss. He denied chest pain, SOB, cough, fever, seizures, upper respiratory tract symptoms, seizures, changes in bowel or urinary habits, night sweats or sick contacts.
On examination he was tachycardic (heartrate 110-130 bpm) and hypertensive (blood pressure was 160s/90s) in the ambulance, but normal throughout ED course. Patient was visibly anxious though not in distress. Neurologic exam revealed a non-cachectic, alert man, oriented to self and place, but not time, with non-bizarre delusions. Attention was intact, however, noted to have significant memory impairment, with 2 attempts needed for immediate recall and 1/5 on delayed recall: 3/5 with prompting. Speech was fluent, no dysarthria or aphasia. He followed multistep commands across midline. Gait was wide-based and unsteady, the rest of neurological examination, including strength, sensation, cranial nerve exam, and coordination, was intact.
Initial blood work was significant for mild leukopenia (WBC 3.2 K/L) and mild normocytic normochromic anemia (Hb 10.6g/dL, MCV 91.8fL, and MCH 28.8 pg). A comprehensive metabolic and lipid panel were both within normal limits. Urine toxicology was positive for methamphetamines. Twenty-four hours after presentation, the patient’s ataxia and dizziness failed to improve, and a CT head without contrast was performed revealing possible periventricular hypodensities. To further clarify these findings, an MRI brain without contrast was performed, which showed abnormal signal affecting the brainstem (Figure 1) extending into the cerebral white matter and cerebral volume loss (Figure 2). These findings prompted the possibility of immunocompromisedrelated leukomalacia. Based on these brain imaging findings and the persistent ataxia and dizziness, additional history was obtained to assess risks for immunocompromised status. The patient noted he was sexually active with multiple male partners and did not use protection. A subsequent HIV test was positive, with a viral load 96,800cp/mL, CD4 22 cells/L, with 22% CD4. Syphilis serology and RPR were also reactive, with quantitative RPR of 1:16. Serum CMV PCR was positive. CSF findings; no WBC’s, no RBC’s, normal glucose, elevated protein, and positive for CMV, (negative for VDRL, Toxoplasmosis, JC Virus, and EBV).
64
After his lumbar puncture results revealed CMV, the patient was transferredto the neurology service and followed closely by the infectious disease team. Ganciclovir 5mg/kg/dose intravenously was administered every 12 hours for three weeks. Ophthalmology services ruled out CMV retinitis since a strong association between CMV retinitis and encephalitis is apparent. In an autopsy series of 47 patients with AIDS, 75% of those with CMV retinitis involving the peripapillary area also had encephalitis. The patient was also treated for latent syphilis with Penicillin G 2.4MU intramuscular weekly for three doses. Additionally, he was placed on Azithromycin 1200 mg orally every week for Mycobacterium avium complex (MAC) prophylaxis and Bactrim double strength 1 tablet three times weekly for Pneumocystis jiroveci pneumonia (PJP) prophylaxis. While still in-patient, and after completing a course of intravenously Ganciclovir, he was started on bictegravir/emtricitabine/tenofovir alafenamide (Biktarvy®), one tablet daily, and switched to oral valganciclovir 900mg daily.
DISCUSSION/CONCLUSION: Traditionally, the diagnosis of CMV encephalitis is considered in patients who are severely immunocompromised, such as a history of AIDS and/or organ transplantation. In those with AIDS, CMV encephalitis occurs almost always in patients with CD4 + count of <50 cells/L, and often these patients present with confusion and impaired memory.
Most infections occur in the setting of prior CMV disease (seropositive), reactivation of latent CMV virus, or infection with a novel strain. Our patient presented with two of the most common symptoms, confusion, and memory impairment, which was confounded by his recent substance use.
Apart from the two most common clinical presentations (confusion and memory impairment), he also presented with profound ataxia, which is a rare presentation of CMV. CNS manifestations of CMV more commonly include encephalitis, ventriculitis, meningitis, myelitis, seizures, aphasia, and cranial nerve palsies.
The most common imaging finding of CMV encephalitis is nonspecific white matter T2/FLAIR hyperintensity. The CMV has ventricle tropism, which can present with periventricular diffusion restriction and contrast enhancement with/without hydrocephalus. Other reported MRI brain findings in confirmed cases of AIDS associated CMV encephalitis are cortical atrophy and diffuse white matter hyperintensity. Our patient’s MRI brain without contrast showed abnormal signal affecting the brainstem extending into the cerebral white matter. MRI brain with contrast revealed extensive confluent T2 hyperdense signal throughout the cerebral white matter, brainstem, and cerebellar white matter. The hyperdense signal in the brainstem and cerebellum likely explains our patient’s profound ataxia. Yet to our knowledge, abnormal brainstem imaging has not been reported in AIDS-associated CMV encephalitis.
The degree of cerebral volume loss observed in our patient was out of proportion for his age, indicating the chronicity of HIV and/or opportunistic infections. This case highlights the importance of primary care engagement for preventive screening for HIV. Undoubtedly, had the patient engaged in primary care, this would have dramatically reduced the chances of developing AIDS-related CMV encephalitis, given efficacy of today’s antiretroviral regimens, especially with early initiation.
Patients presenting with suspected toxic encephalopathy warrant re-evaluation if symptoms persist after sobriety is achieved. AIDS-related CMV encephalitis can have atypical imaging findings that have not been previously described, so it is important to corroborate imaging findings with symptoms. Inquiring about primary care engagement, or lack thereof, should prompt a clinician to investigate routine screening labs, which in this case would have uncovered his immunocompromised status and broadened the initial differential.
65

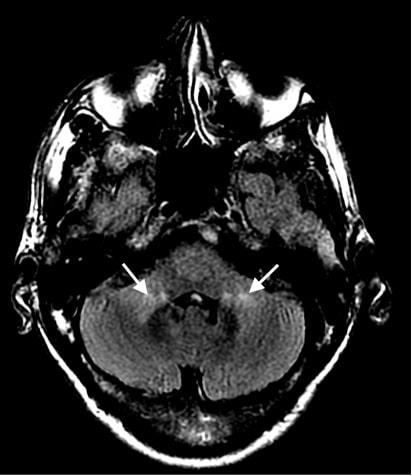 Figure 1: MRI Brain showing abnormal signal affecting the brainstem.
Figure 1: MRI Brain showing abnormal signal affecting the brainstem.
66
Figure 2: MRI Brain showing abnormal signal extending into the cerebral white matter, this figure also demonstrates cerebral volume loss.
ABSTRACT #35 CLINICAL RESEARCH CARDIOLOGY
PREVALENCE AND IMPACT OF TWILIGHT CRITERIA IN ALL-COMER PATIENTS UNDERGOING PERCUTANEOUS CORONARY INTERVENTION
Alessandro Spirito1 , Won Joon Koh2, Sartori Samantha1, Clayton Snyder1, Johny Nicholas1, Davide Cao1 , Birgit Vogel1, Vahid Rezvanizadeh1, Usman Baber3 , Joseph Sweeny1 , Samin K. Sharma1 , Annapoorna Kini1 , George Dangas1 , Roxana Mehran1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3University of Oklahoma Health Sciences Center, Oklahoma City, OK, Unites States
Presented at the European Society of Cardiology (ESC) Congress Meeting that was held in Barcelona, Spain from August 27-30, 2022.
BACKGROUND/INTRODUCTION: The Ticagrelor with Aspirin or Alone in High-Risk Patients after Coronary Intervention (TWILIGHT) randomized clinical trial demonstrated that in selected high risk patients who took ticagrelor and aspirin for 3 months after percutaneous coronary intervention (PCI), continuing ticagrelor alone was associated with significantly less bleeding events than ticagrelor plus aspirin and did not lead to ischemic harm over a period of 1 year. The prevalence and risk of adverse events of patients fulfilling the TWILIGHT inclusion criteria in real-world setting is unclear.
METHODS: Patients that received at least one drug eluting stent in a coronary artery at a large tertiary center (Mount Sinai Hospital, New York, United States) were considered for inclusion. As in the TWILIGHT trial, individuals on chronic oral anticoagulation treatment, with STEMI, cardiogenic shock, CKD on dialysis, prior stroke, or platelet count < 100,000 were excluded. Patients were stratified in two groups according to the presence of at least one clinical (age ≥65 years, female sex, established vascular disease, diabetes mellitus, estimated glomerular fraction rate <60 mL/min, acute coronary syndrome with troponin increase) and one angiographic (multivessel CAD, stent length >30 mm, thrombotic target lesion, bifurcation requiring 2 stents, left main or proximal LAD lesion, atherectomy device use, SYNTAX score ≥23) TWILIGHT inclusion criterion. The primary outcome was a composite of death, myocardial infarction, and stroke. Secondary outcomes included bleeding, components of the primary outcome, target vessel and target lesion revascularization, stent thrombosis. All events were assessed at 1 year after PCI.
RESULTS: Out of 30,470 patients undergoing PCI between 2012 and 2019, 13,236 were included in the current analysis. TWILIGHT criteria were met in 11,018 (83%) patients. Established vascular disease and multivessel coronary artery disease were the most frequently fulfilled criteria. At 1 year, TWILIGHT-like patients were at higher risk for the primary outcome (3.2% versus 1.1%; HR, 2.85; 95%CI,1.83-4.44), severe bleeding (3.3% versus 1.8%; HR, 1.86; 95%CI,1.32-2.62), all-cause death (1.4% versus 0.4%; HR, 3.63; 95%CI,1.70-7.77), myocardial infarction (1.8% versus 0.6%; HR, 2.81; 95%CI,1.56-5.04), TVR (7.8% versus 4.1%; HR, 1.94; 95%CI,1.53-2.47), TLR (5.1% versus 1.7%; HR, 2.98; 95%CI, 2.07-4.29). Stent thrombosis and stroke rate were generally low and did not differ between patients meeting or not the TWILIGHT inclusion criteria.
CONCLUSION: Among all-comer patients undergoing PCI, the fulfillment of the TWILIGHT inclusion criteria is frequent and is associated with a higher risk of death, ischemic and bleeding complications.
67
ABSTRACT #36
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
A CASE OF PLASMODIUM FALCIPARUM MALARIA
Sanam Lama1 , Anjali Ajit1,2 , Vani Gandhi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Malaria is an important cause of morbidity and mortality throughout tropical and temperate countries in the world and is endemic in about 85 countries. The World Health Organization (WHO) reported an increase of malaria cases and deaths from estimated 227 million cases and 558,000 deaths recorded in 2019 to 241 million cases and 627,000 deaths in 2020, respectively. This increase was most likely due to interruption of services due to the COVID-19 pandemic and revised method of computing the burden of malaria. Malaria accounts for 7.8 percent of the global disease burden with the revised WHO calculation (rather than 4.8 percent as reported previously).
CASE PRESENTATION: The patient is a 35 year old male with a history of hypertension presented to the Emergency Department (ED) reporting intermittent fever and body aches for the past 5 days. He had visited another hospital ED a week before for similar complaints where he was diagnosed with COVID19 infection and discharged with Paxlovid; however, he presented to our ED given he was having no improvement in his symptoms. On further history taking, he informed us of recent travel to Senegal and New Guinea. Physical exam was significantfor icteric sclera and mild rightupper quadrant tenderness but no hepatosplenomegaly. Laboratory results revealed a white blood cell count at 5.4K, hemoglobin 12.1 (normocytic), platelets 39K, and total bilirubin at 1.8. Serology for Dengue was negative. A parasite blood smear was sent which showed Plasmodium falciparum (2.3%) and was repeated every 12 hours until his parasitemia was <1%. He was given 3 days of Atovaquone-proguanil (Malarone 250/100mg) that resulted in undetectable parasitemia post treatment and improving thrombocytopenia. He was consequently discharged home.
CONCLUSION: The life cycle of Plasmodium species responsible for this condition is complex and thus, shown in figure 1. Patients can present with signs and symptoms concerning for severe malaria especially in Plasmodium falciparum. However, untreated malaria can lead to multiple complications including but not limited to liver failure with coagulopathy, disseminated intravascular coagulation, severe anemia, acute respiratory distress syndrome, cerebral malaria, and hypoglycemia. All patients who present with febrile illnesses, especially immigrants from the tropics must be approached with due diligence. Actual diagnoses may go missed given the similarities of how malaria, COVID-19, and other viral syndromes present. As malaria is a potentially lifethreatening condition, it should be diagnosed and treated quickly and this case report illustrates an example of the need for detailed history taking in any patient with a febrile illness so as not to miss a diagnosis.
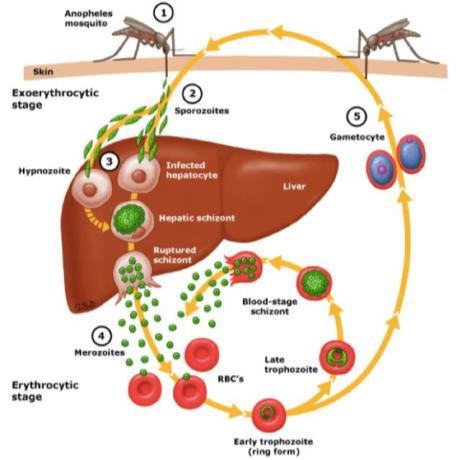
68
Figure 1: Plasmodium falciparum life cycle
ABSTRACT #37
CLINICAL RESEARCH
GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
LIQUID NITROGEN SPRAY CRYOTHERAPY IN THE ESOPHAGUS PERFORMED WITH MINIMAL BLEEDING RISK REGARDLESS OF CONCURRENT ANTITHROMBOTIC THERAPY
Neil R. Sharma1, Abhilash Perisetti1 , Randy M. Leibowitz2 , Mantej Sehmbhi2, Erica Park2, Zubair A. Malik3 , Kamran R. Mushtaq1, Christina M. Zelt 1, Nicholas J. Talabiska3, Jeremy Klein3, Carolyn T. Hogan3 , Michael S. Smith2
1Parkview Regional Medical Center Fort Wayne, IN, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Temple University Hospital, Philadelphia, PA, United States Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in San Diego, California, United States from May 21-24, 2022.
BACKGROUND/INTRODUCTION: Liquid nitrogen spray cryotherapy is a non-contact method of ablation used to treat Barrett’s esophagus and esophageal cancer. In the United States, there is increased utilization of antithrombotic therapy. Antithrombotic therapy often must be held for traditional modalities of thermal ablation leading to various clinical complexities. On the other hand, the risk of gastrointestinal bleeding events with use of liquid nitrogen spray cryotherapy with concurrent use of antithrombotic therapy is unclear.
METHODS: All adults who underwent esophageal liquid nitrogen spray cryotherapy from 2014-2021 at three high volume U.S. centers were identified. Demographic data, use and type of antithrombotic therapy during liquid nitrogen spray cryotherapy, and number of gastrointestinal bleeding events requiring treatment were collected. The primary outcome was to assess the overall risk and severity of gastrointestinal bleeding events within 30 days of liquid nitrogen spray cryotherapy. Secondary outcomes were to quantify the liquid nitrogen spray cryotherapy-associated gastrointestinal bleeding with concomitant antithrombotic therapy use. Data was analyzed in R (version 3.6.1) using generalized linear mixed effects models to account for intra-individual correlation in this repeated measure study.
RESULTS: A total of 695 liquid nitrogen spray cryotherapy cases among 183 patients met inclusion criteria. The mean age on presentation was 67.9 years (SD+10.8 years), 78% were male. Indications for liquid nitrogen spray cryotherapy were Barrett’s esophagus in 63% and esophageal cancer in 35.5% of cases. Among all liquid nitrogen spray cryotherapy procedures, five (0.007%) were associated with post-procedure bleeding, of which three cases required a blood transfusion. Of the five reported bleeding events, only one patient was taking antithrombotic therapy at the time of liquid nitrogen spray cryotherapy. No mortality was noted in the study.
CONCLUSION: In this multicenter retrospective study, the risk of gastrointestinal bleeding events with liquid nitrogen spray cryotherapy spray is rare and can be managed conservatively with blood products and endoscopic treatment. The risk of bleeding did not increase with concurrent use of antithrombotic therapy. These findings suggest that liquid nitrogen spray cryotherapy can be safely administered simultaneously with antithrombotic therapy in Barrett’s esophagus or esophageal cancer patients which may have significant clinical value.
69
ABSTRACT #38
CLINICAL RESEARCH CARDIOLOGY
IN-HOSPITAL OUTCOMES OF TAVR IN PATIENTS WITH CHRONIC KIDNEY DISEASE
Marta Lorente-Ros1, Subrat K Das1, José S. Aguilar-Gallardo1, Francisco J. Romeo1, Amisha Patel1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Transcatheter Cardiovascular Therapeutics (TCT) Annual Meeting that was held in Boston, Massachusetts, United States from September 16-19, 2022.
BACKGROUND/INTRODUCTION: Chronic kidney disease and end-stage renal disease have been associated with worse outcomes after transcatheter aortic valve replacement (TAVR). With TAVR indications extending to a wider range of patient populations, the implications of chronic kidney disease on outcomes are of increasing relevance and not well described. We aim to determine the association between chronic kidney disease and inhospital outcomes after TAVR.
METHODS: We queried the National Inpatient Sample for TAVR performed between 2016 and 2018 using ICD10 codes. We compared in-hospital outcomes between 3 groups: no chronic kidney disease, chronic kidney disease, and end-stage renal disease
RESULTS: 136,025 patients underwent TAVR in the study period (mean age 79.7 ± 0.1 years, 46.0% female) 64.4% of the patients had normal renal function, 32.0% had chronic kidney disease and 3.6% had end stage renal disease. Patients with chronic kidney disease or end stage renal disease had a higher prevalence of prior myocardial infarction, heart failure, atrial fibrillation and chronic obstructive pulmonary disease (all p<0.001). Both chronic kidney disease and end stage renal disease were associated with longer hospital stay (p<0.001) Patients with end stage renal disease had a higher incidence of vascular complications (4.9% versus 3.9% p=0.05), procedural myocardial infarction (6.0% versus 3.4% p=0.04) and cardiac arrest (0.8% versus 0.2% p=0.01). In-hospital mortality, conversion to open surgery, and the use of mechanical circulatory support did not differ between groups.
CONCLUSION: Patients with renal dysfunction undergoing transcatheter aortic valve replacement are at higher risk for cardiovascular complications, although this does not seem to result in increased in-hospital mortality or more frequent conversion to open surgery.
70
ABSTRACT #39
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/PULMONARY/CRITICAL CARE
DELAYED DIAGNOSIS OF PULMONARY VEIN OCCLUSION AFTER ATRIAL FIBRILLATION ABLATION
Sara Luby1 , Jonathan M Oxman1 , Deepanjali Nair1, Alba Muñoz Estrella1, Javier J Zulueta1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Pulmonary vein stenosis is a known, yet uncommonly diagnosed complication of pulmonary vein isolation ablation for atrial fibrillation. Advances in ablation have decreased rates of pulmonary vein stenosis, leading to a decline in post-procedural screening for this complication. Patients with pulmonary vein stenosis may be asymptomatic or develop non-specific symptoms including, chest pain, dyspnea, cough, or hemoptysis, often leading to extensive diagnostic workups without a correct diagnosis. Progression may ultimately lead to complete occlusion of the pulmonary vein, resulting in lung infarction and pulmonary hypertension. Computed tomography (CT) is the initial diagnostic modality of choice, however, invasive angiography or Doppler is more accurate at confirming the presence of total occlusion. Importantly, this guides the management strategy as complete occlusions are not always amenable to intervention. Despite high rates of restenosis, stenting is the pillar of therapy.
CASE PRESENTATION: The patient was a 51-year-old male with a history of atrial fibrillation, status-post two pulmonary vein ablations, who subsequently presented multiple times to both the inpatient and outpatient settings with chronic, non-exertional dyspnea and chest discomfort localized over the left upper chest over the course of one year. Multiple diagnostic evaluations during the year prior to this presentation were unrevealing. During the presenting admission, a chest CT showed diffuse ground glass attenuation of the left upper lobe and a peripheral consolidation in the same lobe compatible with pulmonary infarct secondary to a near complete occlusion of the left superior pulmonary vein. Transesophageal echocardiogram with Doppler confirmed these findings, demonstrating a trickle of flow through the pulmonary vein. The patient was discharged with planned stent placement.
CONCLUSION: We presented a case of symptomatic, near total occlusion of a pulmonary vein in the setting of atrial fibrillation ablation that had repeatedly been misdiagnosed. Although uncommon, pulmonary vein stenosis/occlusion should remain on the differential for symptomatic patients who have undergone pulmonary vein ablation to prevent progression of disease and provide symptom relief.
71
ABSTRACT #40 CLINICAL RESEARCH RHEUMATOLOGY
DETERMINANTS OF COVID-19 VACCINE HESITANCY IN A PREDOMINANTLY BLACK POPULATION WITH CUTANEOUS LUPUS ERYTHEMATOSUS
Sophia Lutgen1, S. Sam Lim2, Laura D. Aspey2, Gaobin Bao2, Charmayne Dunlop-Thomas2, Jessica N. Williams2, Cristina
Drenkard2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Emory University, Atlanta, GA, United States
Presented at the American College of Rheumatology Convergence Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 10-14, 2022.
BACKGROUND/INTRODUCTION: Due to demographic and disease-related factors, patients with lupus are deemed to be more vulnerable to COVID-19 infection than the general population, but they may be more hesitant to receive the COVID-19 vaccine. Black individuals have higher susceptibility to chronic cutaneous lupus erythematosus (CCLE); however, these patients are underrepresented in COVID-19 studies. We studied vaccination and patients’ perceptions during the early pandemic in a predominantly Black cohort of patients with CCLE.
METHODS: We studied patients with a validated diagnosis of CCLE enrolled in the population-based Georgians Organized Against Lupus (GOAL) Cohort. Participants were surveyed in early pandemic (1/15/21-8/16/21) after COVID-19 vaccination was available in the USA. We used validated tools to assess vaccination perceptions and ad hoc questions to assess COVID-19 concerns and vaccine status. We studied the relationship between vaccination status and trusted sources, concerns, beliefs, and vaccination attitudes.
RESULTS: Of 158 respondents (54% primary CCLE and 46% CCLE + SLE), 82% returned the survey by 3/15/21. Most participants were Black (81%) and female (89%), with a mean age of 54 years; 40% reported living below the poverty level and 42% were unemployed. 120 (76%) did not receive the vaccine, while 17% and 6% received 1 and 2 doses, respectively. The most frequent vaccination attitudes were unfound problems (79%), unknown effects of vaccine in the future (69%), unforeseen problems in children (50%), followed by reliability (49%), protection (48%) and safety (47%) (Fig. 1). Participants were highly concerned about COVID-19 infection consequences (Fig 2). The table shows that Black participants (p=0.01), those living in poverty (p=0.006), and unemployed (p<0.001) were less likely to be vaccinated. Doctors were a trusted source in 113 (71%) participants and 31% of them received the vaccine (p=0.001). Mistrust was significantly related to unvaccinated status (p<0.001). Participants who believed that lupus patients should get vaccinated, that vaccines protect against infection, or those that would get the vaccine regardless of a doctor’s advice were more likely to be vaccinated (p<0.001 for each association) whereas those that believed the vaccine will cause lupus to flare up (p=0.001), that the vaccine interacts with medications and causes harm (p=0.004), or is less effective in lupus patients than in the general population (p=0.007) were less likely to be vaccinated.
CONCLUSION: At early pandemic, only 23% patients with CCLE were COVID-19 vaccinated. Participants who were Black, living in poverty, or unemployed were less likely to be vaccinated. Concerns about COVID-19 infection were not associated with vaccine status, whereas mistrust and negative beliefs of vaccine benefits were more likely to occur among those unvaccinated. Despite that, 71% of participants trusted their doctors, 31% received the vaccine. Longitudinal studies are warranted to assess patients’ perceptions and vaccination rates as the pandemic progressed. Education interventions are critical to mitigate vaccine hesitancy in CCLE patients, particularly among those of Black race and those who are socioeconomically disadvantaged.
72
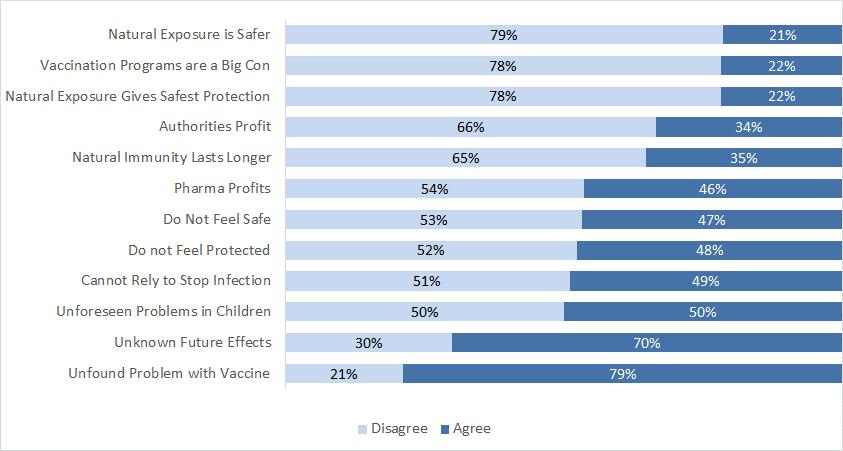
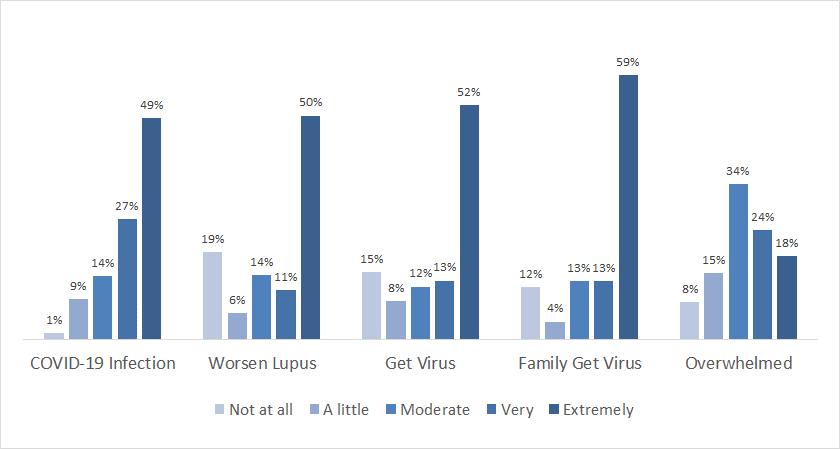 Figure 1: Vaccination Attitudes among 158 participants of a population-based cohort with a validated diagnosis of CCLE. Vaccination attitudes were measured with the Examination (VAX) Scale
Figure 1: Vaccination Attitudes among 158 participants of a population-based cohort with a validated diagnosis of CCLE. Vaccination attitudes were measured with the Examination (VAX) Scale
73
Figure 2: COVID-19 infection concerns reported by 158 participants of a population-based cohort with a validated diagnosis of CCLE
Table 1: Factors Associated with COVID-19 Vaccination among Patients with Chronic Cutaneous Lupus Erythematosus
Category Sub-Category Overall n = 158 COVID-19 Vaccine p-value Yes n=37 No n=120 Sociodemographic Sex Male 17 (10.7) 4 (10.8) 13 (10.8) 0.1 Female 141 (88.7) 33 (89.2) 108 (90.0) Race Black 129 (81.1) 25 (67.6) 104 (86.7) 0.01 Non-Black 29 (18.2) 12 (32.4) 17 (14.2) Age Group 18-34 20 (12.6) 3 (8.1) 17 (14.2) 0.07 34-54 56 (35.2) 9 (24.3) 47 (39.2) 55+ 83 (52.2) 26 (70.3) 57 (47.5) Below 100% Poverty level Yes 62 (39.0) 7 (18.9) 55 (45.8) 0.006 Current Work Status Employed 48 (30.2) 13 (35.1) 35 (29.2) <0.001 Off work force 43 (27.0) 18 (48.6) 25 (20.8) Unemployed 64 (40.3) 5 (13.5) 59 (49.2) Sources of trusted COVID-19 information Doctors 113 (71.1) 35 (94.6) 78 (65.0) 0.001 Government 72 (45.3) 23 (62.2) 49 (40.8) 0.03 News 72 (45.3) 26 (70.3) 46 (38.3) 0.001 Family/Friends 42 (26.4) 15 (40.5) 27 (22.5) 0.04 Church 19 (11.9) 2 (5.4) 17 (14.2) 0.15 Local Agency 22 (13.8) 4 (10.8) 18 (15.0) 0.5 Social Media 13 (8.2) 2 (5.4) 11 (9.2) 0.45 Lupus Advocacy or Support Groups 78 (49.1) 20 (54.1) 58 (48.3) 0.61 Concerns about COVID-19 COVID-19 in general 79 (49.7) 19 (51.4) 60 (50.0) 0.41 Lupus will worsen 79 (49.7) 18 (48.6) 61 (50.8) 0.21 Getting infected with COVID19 82 (51.6) 19 (51.4) 63 (52.5) 0.75 Someone in family getting infected 93 (58.5) 22 (59.5) 71 (59.2) 0.5 Feeling overwhelmed 30 (18.9) 4 (10.8) 26 (21.7) 0.48 74
Table 1: Factors Associated with COVID-19 Vaccination among Patients with Chronic Cutaneous Lupus
Erythematosus (continued)
Category Sub-Category Overall n = 158 COVID-19 Vaccine p-value Yes n=37 No n=120 Vaccination Attitudes Mistrust of vaccine benefit Do not feel safe 73 (45.9) 33 (89.2) 40 (33.3) <0.001 Cannot rely to stop serious infection 77 (48.4) 31 (83.8) 46 (38.3) <0.001 Do not feel protected 74 (46.5) 31 (83.8) 43 (35.8) <0.001 Worries about unforeseen future effects Unfound problem with vaccine 125 (78.6) 32 (86.5) 93 (77.5) 0.38 Unforeseen problems in children 79 (49.7) 18 (48.6) 61 (50.8) 0.69 Unknown future effects 110 (69.2) 25 (67.6) 85 (70.8) 0.56 Concerns about commercial profiteering Pharma profits 71 (44.7) 14 (37.8) 57 (47.5) 0.23 Authorities profit 51 (32.1) 9 (24.3) 42 (35.0) 0.18 Vaccination programs are a big con 35 (22.0) 2 (5.4) 33 (27.5) 0.004 Preference for natural immunity Natural immunity lasts longer 54 (34.0) 11 (29.7) 43 (35.8) 0.46 Natural exposure gives safest protection 36 (22.6) 7 (18.9) 29 (24.2) 0.45 Natural exposure is safer 35 (22.0) 4 (10.8) 31 (25.8) 0.05 COVID-19 Vaccine Beliefs Religious beliefs prevent from taking the vaccine agree 7 (4.4) 1 (2.7) 6 (5.0) 0.57 disagree 144 (90.6) 34 (91.9) 110 (91.7) People with Lupus should get vaccinated agree 76 (47.8) 34 (91.9) 42 (35.0) <0.001 neutral 55 (34.6) 2 (5.4) 53 (44.2) disagree 27 (17.0) 2 (5.4) 25 (20.8) Lupus patients have more side effects than general population agree 30 (18.9) 4 (10.8) 26 (21.7) 0.08 neutral 98 (61.6) 22 (59.5) 76 (63.3) disagree 87 (54.7) 11 (29.7) 76 (63.3) 75
Table 1. Factors Associated with COVID-19 Vaccination among Patients with Chronic Cutaneous Lupus Erythematosus (continued)
p-values were estimated using Chi-square test.
Category Sub-Category Overall n = 158 COVID-19 Vaccine p-value Yes n=37 No n=120 COVID-19 Vaccine Beliefs Vaccine will cause Lupus flare up agree 26 (16.4) 1 (2.7) 25 (20.8) 0.001 neutral 95 (59.7) 20 (54.1) 75 (62.5) disagree 35 (22.0) 15 (40.5) 20 (16.7) Vaccine will interact with Lupus meds and harm agree 18 (11.3) 0 (0.0) 18 (15.0) 0.004 neutral 99 (62.3) 21 (56.8) 78 (65.0) disagree 38 (23.9) 15 (40.5) 23 (19.2) Lupus medications will not affect vaccine agree 29 (18.2) 11 (29.7) 18 (15.0) 0.14 neutral 104 (65.4) 21 (56.8) 83 (69.2) disagree 22 (13.8) 5 (13.5) 17 (14.2) Vaccine not as effective in Lupus as in general population agree 12 (7.5) 0 (0.0) 12 (10.0) 0.007 neutral 101 (63.5) 20 (54.1) 81 (67.5) disagree 44 (27.7) 17 (45.9) 27 (22.5) Lupus patients are at higher risk of infection agree 73 (45.9) 16 (43.2) 57 (47.5) 0.3 neutral 55 (34.6) 11 (29.7) 44 (36.7) disagree 29 (18.2) 10 (27.0) 19 (15.8) Vaccine will protect from infection agree 44 (27.7) 21 (56.8) 23 (19.2) <0.001 neutral 76 (47.8) 12 (32.4) 64 (53.3) disagree 32 (20.1) 4 (10.8) 28 (23.3) Stop mask after vaccination agree 4 (2.5) 1 (2.7) 3 (2.5) 0.59 neutral 20 (12.6) 3 (8.1) 17 (14.2) disagree 133 (83.6) 34 (91.9) 99 (82.5) No need of vaccination because already infected agree 7 (4.4) 0 (0.0) 7 (5.8) 0.06 neutral 37 (23.3) 5 (13.5) 32 (26.7) disagree 109 (68.6) 31 (83.8) 78 (65.0) Will get vaccine only after Lupus doctor discussion agree 69 (43.4) 16 (43.2) 53 (44.2) 0.97 neutral 37 (23.3) 9 (24.3) 28 (23.3) disagree 156 (98.1) 36 (97.3) 120 (100.0) Will not get vaccine even after doctor recommendation agree 23 (14.5) 1 (2.7) 22 (18.3) <0.001 neutral 52 (32.7) 5 (13.5) 47 (39.2) disagree 82 (51.6) 31 (83.8) 51 (42.5) Will get vaccine regardless doctor recommendation agree 27 (17.0) 14 (37.8) 13 (10.8) <0.001 neutral 62 (39.0) 14 (37.8) 48 (40.0) disagree 67 (42.1) 9 (24.3) 58 (48.3)
76
ABSTRACT #41 CLINICAL RESEARCH CARDIOLOGY
PROGNOSTIC SIGNIFICANCE OF EXERCISE-INDUCED MYOCARDIAL ISCHEMIA IN PATIENTS WITH ANGIOGRAPHICALLY NORMAL CORONARIES COMPARED TO PATIENTS WITH NORMAL EXERCISE ECHOCARDIOGRAPHY
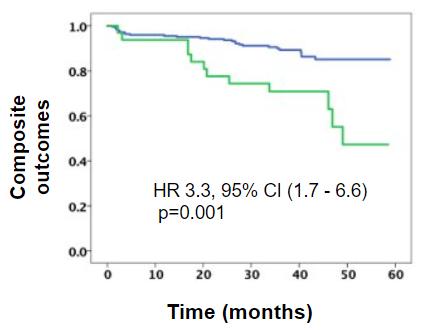
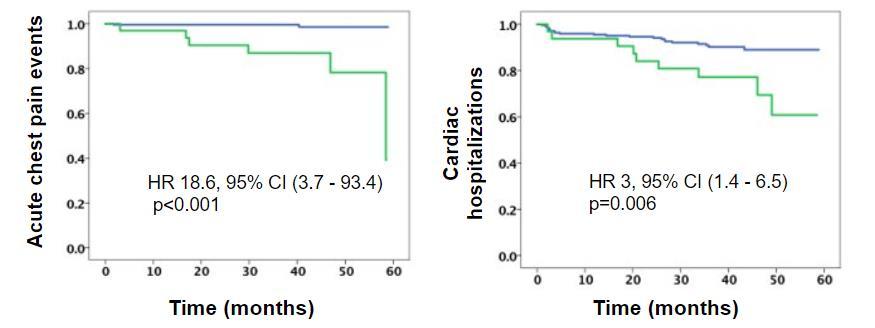
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023
BACKGROUND/INTRODUCTION: There is limited data regarding the prognostic significance of myocardial ischemia during exercise echocardiography in patients with normal coronaries. The following study assesses if differences in prognosis exist between this population and patients with non-ischemic exercise echocardiography.
METHODS: Symptomatic patients who underwent exercise echocardiography at Mount Sinai Morningside between 2017 and 2020 were analyzed. Patients with evidence of ischemia on exercise echocardiography and normal coronaries upon anatomic evaluation (iExE-NC), were matched through propensity score analysis to controls, defined as patients with non-ischemic exercise stress echocardiography, in a 1:3 ratio. Composite outcomes included acute chest pain events (defined as unstable angina and infarction with normal coronaries), strokes, and cardiac hospitalizations.
RESULTS: Thirty-four patients with iExE-NC were identified [age: 61±11 years, 26 (76%) women, EF: 58±7%]. Propensity scorematching yielded 102 controls with non-ischemic exercise stress echocardiography[age: 61±10 years, 77 (75%) women, EF: 57±9%]. For the analysis, adjustments for age, sex, risk factors, exercise tolerance, and ejection fraction were made. After a median follow-up of 3.1 years, patients with iExE- NC, when compared to those with non-ischemic exercise stress echocardiography, experienced more acute chest pain events [7 (21%) versus 1 (1%), p<0.001], strokes [2 (6%) versus 0 (0%), p=0.014] and cardiac-related hospitalizations [9 (26%) versus 9 (9%), p=0.011]. Ultimately, iExE-NC patients had a higher risk for developing acute chest pain events (HR, 19.0; 95%CI: 2.3 – 154) and composite outcomes (HR, 4.1; 95%CI: 1.78 – 9.7) compared to nonischemic exercise stress echocardiography patients.
CONCLUSION: In the present study, patients with ischemic exercise stress echocardiography had a higher incidence of adverse cardiac events when compared to patients with non-ischemic exercise stress echocardiography despite having normal coronaries. Non-atherosclerotic mechanisms, such as microvascular dysfunction, might explain these findings. Further studies are needed to understand the mechanisms involved.
Brissete Mancero1, Alaa Omar1, Ga Hee Kim1, Elizabeth A. Zipf1, Joseph Elias1, David Meister1, Maria K. Peña1 , Christopher Perez1, Kruti Dhaval Gandhi1, Arpanjeet Kaur1, Errol C. Moras1, Robert Leber1, Nitin Barman1 , Edgar Argulian1
77
Figure 1: Kaplan Meier Curves for acute chest pain events, cardiac hospitalizations, and composite outcomes
ABSTRACT #42 CLINICAL RESEARCH GASTROENTEROLOGY
PATIENTS WITH ELEVATED UPPER ESOPHAGEAL SPHINCTER PRESSURES ARE LESS LIKELY TO PRESENT WITH ATYPICAL SYMPTOMS OF GASTROESOPHAGEAL REFLUX DISEASE
Alexandria Markley 1 , Nour Al Khalili1 , Emily Seltzer1 , Mantej Sehmbhi1 , Kimberly Cavaliere1 , Daniela Jodorkovsky1 , Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Will be presented at the Digestive Disease Week (DDW) Annual Meeting that will be held in Chicago, Illinois, United States from May 6-9, 2023.
BACKGROUND/INTRODUCTION: High-resolution esophageal manometry (HREM) has made evaluation of the upper esophageal sphincter more readily available, including publication of normal values for both basal and residual (deglutitive) pressures. The association between upper esophageal sphincter dysfunction and oropharyngeal and esophageal symptoms and dysmotility remains poorly defined. The aim of this study was to identify associations between abnormal HREM upper esophageal sphincter findings and patient demographic and clinical parameters.
METHODS: All HREM studies at a high-volume motility center between 6/2021 and 11/2022 were reviewed. Patients with prior foregut endoscopic or surgical interventions were excluded. All patients with a basal upper esophageal sphincter pressure >104 mmHg or a mean residual pressure >12 mmHg were included in the elevated upper esophageal sphincter pressure group, whereas all other patients were placed in the normal group. Differences in demographic and clinical parameters between the groups were evaluated using t-tests, chi-square, or Fisher’s exact tests as appropriate.
RESULTS: Of the 363 HREM reports reviewed, 295 met criteria for inclusion in the analysis. There were no significant differences in gender, body mass index, age or race between the normal and abnormal upper esophageal sphincter pressure groups. Hypertension was present in significantly more patients with normal upper esophageal sphincter pressures (p=0.034); no other significant differences were observed in comorbidities including mood disorders, neurological or connective tissue diseases. The use of proton pump inhibitors, prokinetics, antidepressants, anticonvulsants, and muscle relaxants was not significantly different between groups. Heartburn was the most common presenting symptom in both abnormal and normal cohorts (64.5%, 66.5%). Patients with normal upper esophageal sphincter pressures had statistically higher rates of globus sensation (p=0.006), sore throat/throat clearing (p=0.039), and nausea/vomiting (p=0.01) compared to those with elevated upper esophageal sphincter pressures. Rates of other potential reflux symptoms were not statistically different between the groups. Chicago Classification v4.0 diagnoses were comparable as well.
CONCLUSION: Upper esophageal sphincter pressures do not receive the same attention as other parameters reported in high-resolution esophageal manometry studies, as their clinical significance has yet to be elucidated. This study demonstrates that patients with abnormally high upper esophageal sphincter values are less likely to present with atypical reflux symptoms, while many demographic and other clinical parameters are similar to patients with normal upper esophageal sphincter readings. These findings may be due to a compensatory upper esophageal sphincter mechanism to protect against reflux. Correlation of findings with manometric and quantitative reflux testing results will provide further insights into how upper esophageal sphincter readings could improve management of reflux in these patients.
78
ABSTRACT #43 CLINICAL RESEARCH DERMATOLOGY
IMPROVEMENT OF PERIMENSTRUAL ACNE WITH CLINDAMYCIN PHOSPHATE 1.2% AND BENZOYL PEROXIDE 3.75% COMBINATION GEL: AN INTERVENTIONAL PILOT STUDY
Olga Marushchak1, Matthew Gagliotti2, Anjali S. Vekaria2, Gary Goldenberg2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in Journal of Clinical and Aesthetic Dermatology, 2022. PMID: 36381180
BACKGROUND/INTRODUCTION: Acne is an extremely common dermatologic problem, affecting many individuals globally. It is a common belief among the public, as well as health care professionals, that women often experience perimenstrual flares of acne. Hormones, particularly androgens, such as testosterone and dihydrotestosterone, play a significant role in the pathophysiology of acne. Therefore, current mainstay treatment of perimenstrual acne consists of systemic hormonal therapies, which can be problematic due to their side effects, stigma, or pill burden. Topical treatments are often used as well; however, data on their efficacy in treating this type of hormonal acne are limited.
METHODS: The open-label, single-group interventional pilot study was performed on 22 adult female subjects with perimenstrual acne. The objective of the study was to evaluate the efficacy and tolerability of clindamycin phosphate and benzoyl peroxide 1.2%/3.75% combination gel in treating perimenstrual acne in adult women. The subjects applied the investigational drug daily and were assessed for inflammatory and non-inflammatory acne vulgaris every 14 days for a total of 99 days. Primary outcome was determined by treatment success, a static endpoint defined as a score of 0 (clear) to 1 (almost clear) on a scale of 0-5 on the physician global assessment (PGA) scoring system at the final study visit on day 99. Secondary outcome measures included assessment of PGA and lesion count changes at each visit and drug tolerability based on the subject-reported adverse events (AE) as well as physician-evaluated erythema, scaling, and dryness on a point scale from 0 (none) to 3 (severe).
RESULTS: The primary efficacy endpoint analysis showed that 52.9% of the patients reached a PGA score of 0 (clear) or 1 (almost clear) at the final visit on day 99, compared to 0% at the baseline. The mean percent change in PGA score showed gradual improvement throughout the study and reached 46.5% (SE, 9.04; p<0.0001) at day 99. The improvement in the lesion count reached 63.5% (SE, 6.74; p<0.0001) at day 99 Physician-evaluated local cutaneous reactions indicated that the highest percentage of patients with erythema (18.2%) and dryness (40.9%) were identified on day 29, while scaling was most prevalent on day 15 (13.6%). Erythema, scaling, and dryness gradually improved during subsequent visits and were detected in 13.6%, 9.1%, and 13.6% of the subjects, respectively, on day 99. For the duration of the study, majority of the reported cutaneous reactions were mild
CONCLUSION: The efficacy and tolerability of clindamycin phosphate 1.2% and benzoyl peroxide 3.75% combination gel in patients with perimenstrual acne suggests that this medication could provide an important, clinically effective topical treatment option and address the drawbacks of the oral medications currently recommended for this condition. Clinicians should be aware of this potential alternative therapy to offer an individualized therapeutic approach to their patients.
79
ABSTRACT #44 BASIC SCIENCE CARDIOLOGY
IDENTIFICATION OF AN OPTIMAL METHOD FOR ECHOCARDIOGRAPHIC RIGHT VENTRICULAR MASS ESTIMATION IN A SWINE MODEL OF PULMONARY HYPERTENSION
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Society of Echocardiography Annual Scientific Sessions that will be held in National Harbor, Maryland, United States from June 23-26, 2023.
BACKGROUND: Right ventricular mass and Fulton Index - ratio of right to left ventricular mass - are useful markers of right ventricular remodeling and predictors of mortality in pulmonary hypertension. Current echocardiography guidelines lack a standardized method for right ventricular mass determination. We compared the performance of four previously described echocardiographic models of right ventricular mass to estimate actual right ventricular weight measured post-mortem in a swine model of pulmonary hypertension
METHODS: Echocardiography was performed in a Yorkshire pig model of post-capillary pulmonary hypertension induced by pulmonary vein banding and healthy animals (n=70). Right ventricular mass was measured using the following models: (1) trapezoid method, (2) exact radius method, (3) longitudinal plane method, and (4) an algorithm proposed by Kochav, et al. A two-dimensional area-length method was applied to estimate left ventricular mass and Fulton Index was calculated. On the day of echocardiography, pigs were euthanized, hearts were explanted, and right ventricular and left ventricular weights were recorded. Pearson’s correlation, linear regression, and Bland-Altman analysis were employed to evaluate different methods compared to recorded weights and Fulton Index.
RESULTS: The mean right ventricular weight at necropsy was 41.2 ± 14.0 g (range: 11.1 g to 93.6 g). Fulton Index ranged from 0.29 to 3.60 with a mean of 0.70. All methods demonstrated a strong linear relationship with post-mortem right ventricular weight (r(1) = 0.88, r(2) = 0.88, r(3) = 0.84 r(4) = 0.82, p<0.0001). Bland-Altmann analysis revealed good agreement with recorded right ventricular mass for trapezoid, exact radius and longitudinal plane method (bias(1) = 4.5 ± 7.5g, bias(2) = -5.9 ± 6.6g, bias(3) = -2.7 ± 8.4g) while Kochav’s algorithm tended to underestimate right ventricular weights (bias(4) = -18.5 ± 8.7g). Measured left ventricular mass correlated strongly with post-mortem left ventricular weight and reached good agreement (r = 0.91, p<0.0001; bias = -4.0 ± 9.8 g). Fulton Index was best approximated by exact radius (bias = -0.04 ± 0.12) and longitudinal plane (bias = 0.01 ± 0.18) methods. The trapezoid model tended to overestimate Fulton Index (bias = 0.10 ± 0.11) and Kochav’s algorithm underestimated (bias = -0.23 ± 0.12).
CONCLUSION: Right ventricular mass and Fulton Index can be successfully approximated using echocardiography in a clinically relevant pulmonary hypertension model. Longitudinal plane and exact radius methods performed best and are suggested methods for evaluating right ventricular mass in clinical pulmonary hypertension patients.
Jonas Marx1 , Tomoki Sakata2, Renata Mazurek2, Anjali Ravichandran2 , Spyros Mavropoulos2 , Taro Kariya2 , Kiyotake Ishikawa2
80
ABSTRACT #45
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/HEMATOLOGY/ONCOLOGY
LARYNGEAL SYNOVIAL SARCOMA THAT METASTASIZED TO THE HEART
Christopher N. Matthews1 , Syed Farrukh Mustafa1 , Sidra Salman1 , Akshaya Gopalakrishnan1, James Salonia1 , Deepika Misra1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
BACKGROUND/INTRODUCTION: Synovial sarcomas have an age adjusted incidence of 1.42/1,000,000 in adults and 0.81/1,000,000 in children, while no more than 7% of synovial sarcomas reported are located at the head and neck. Laryngeal synovial sarcoma is a rare tumor.
CASE PRESENTATION: The patient was a 27-year-old male with history of laryngeal synovial sarcoma treated with total resection, chemotherapy, and radiation several years ago presented with dyspnea on exertion. He was found to have large right ventricular mass extending into the right atrium and pulmonary artery. He underwent surgical resection (>80% tumor removed), and tissue biopsy showed synovial sarcoma. One month postoperatively, he presented with heart failure symptoms and was found to have recurrence of the tumor occupying the bulk of the right ventricular cavity, bilateral pulmonary emboli, and worsening biventricular dysfunction. Bronchoscopy revealed complete extrinsic compression of the right main pulmonary artery. The patient was started on intravenous heparin for pulmonary emboli.
He was not deemed a candidate for redo surgery due to tumor adherence to the ventricular wall. Palliative chemotherapy with ifosfamide was started. He developed worsening respiratory distress followed by cardiogenic shock and multi-organ failure, resulting in death.
CONCLUSION: A 2021 review of laryngeal synovial sarcomas found 39 total cases in the literature from 2017 and prior, five of which had local disease recurrence, as with this case, and two of those had metastasis, none of which with cardiac metastasis Synovial sarcomas are known to be aggressive in nature, with the median overall survival of 138 months, which is longer than this patient’s course of about 110 months. The 5-year survival rate of head/neck synovial sarcomas was 70.5%, while it is less at 32.9% for thoracic synovial sarcomas. The overall 5-year survival rate of primary synovial sarcomas with metastasis is 19.6%.
We report the first case of laryngeal synovial sarcoma with cardiac metastasis. The aggressive nature of this tumor makes it difficult to treat, and hence, early diagnosis is crucial.
81
ABSTRACT #46
CLINICAL RESEARCH CARDIOLOGY
DIASTOLIC STRESS ECHOCARDIOGRAPHY IN PATIENTS WITH NORMAL RESTING DIASTOLIC FUNCTION: PROGNOSTIC UTILITY IN PRESENCE AND ABSENCE OF MYOCARDIAL ISCHEMIA
Loba Alam1, Alaa M. Omar1, Swiri Konje1, Kruti Gandhi1, Errol Moras1 , David Meister1, Maria Peña1 , Christopher Perez Lizardo1, Brisette Mancero1 , Elizaebth Zipf1, Ga Hee Kim1, Joseph Elias1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Barcelona, Spain from August 27-30, 2022.
BACKGROUND: Abnormal diastolic response to exercise is reportedly associated with worse cardiovascular events. However, this has not been well studied in patients with normal diastolic function at rest. We sought to study diastolic response to exercise in patients referred for exercise stress echocardiography and to explore its association with adverse outcomes in the presence and absence of exercise induced myocardial ischemia.
METHODS: In a retrospective study, patients referred for exercise stress echocardiography to assess myocardial ischemia between April 2017 and December 2018 were enrolled. Patients were included if they had guideline defined normal diastolic function at rest and availability of a full set of post exercise diastolic variables (post exercise tissue Doppler derived septal mitral annular early diastolic velocity (e’), ratio of pulsed Doppler derived mitral forward flow early diastolic velocity (E) over e’ (E/e’) and continuous wave Doppler derived maximum tricuspid regurgitation velocity (TRV)). The patients were followed for a median of 3.4 years for the occurrence of composite death, acute coronary syndrome, cardiac hospitalization, and need of follow-up ischemia testing. Abnormal exercise diastolic variables were defined as e’<7 cm/s, E/e’>15, and TRV>2.8 m/s.
RESULTS: We studied 492 patients [age: 55.7 ± 12.9 year, 268 (54%) women, EF: 61 ± 5.8%]. Mean achieved metabolic equivalents of tasks (METs) was 9.7 ± 3.1, and a total of 49 (10%) patients had evidence of exercise induced ischemia. At rest, mean left atrial volume index was 25.4 ± 12 ml, e’ was 8 ± 2 cm/s, E/e’ was 9.5 ± 2.4, and TRV was 2.1 ± 0.44 m/s. Post exercise e’ was 10 ± 3 cm/s [<7cm/s in 63 (13%)], E/e’ was 11.1 ± 3.9 [>15 in 95 (19%)], and TRV was 2.37±0.68 m/s [>2.8 m/s in 152 (31%)]. Ischemic ExE was found to be strongly associated with the outcome (HR, 4.46; 95%CI, 2.8 to 7.1; p<0.001). In addition, all diastolic variables predicted the outcome in isolation if they were abnormal (e’, 2.28; 95%CI, 1.4 to 3.7; p=0.001; E/e’, 1.81; 95%CI, 1.15 to 2.84; p=0.01; TRV, 1.58; 95%CI, 1.17 to 2.13; p=0.003).When combined, however, association with the outcome was seen only when 2 or 3 of these variables were abnormal simultaneously (Figure 1A). When patients were stratified by ischemia and abnormal diastolic variables (figure 1B), patients with 2 or 3 abnormal variables were more likely to experience the outcome compared to patients with 0 or 1 abnormal variables in both absence of ischemia (p<0.001) and presence of ischemia (p=0.016). The stratified groups were different in their clinical and exercise profiles, with worse profiles in patients with both ischemia and 2 or 3 abnormal variables, and best profiles in patients with no ischemia and 0 or 1 abnormal variables.
CONCLUSION: In patients referred for exercise stress echocardiography to assess ischemia with normal baseline diastolic function, exercise can unmask abnormal diastolic properties and stratify patients' risk regardless of the overt myocardial ischemia.
82
Figure 1: A) survival free of composite outcomes (percentage) over time (days) plotted by number of abnormal post exercise diastolic variables; B) survival free of composite outcomes (percentage) over time (days) plotted by number of abnormal exercise diastolic variables in both the presence and absence of exercise induced myocardial ischemia
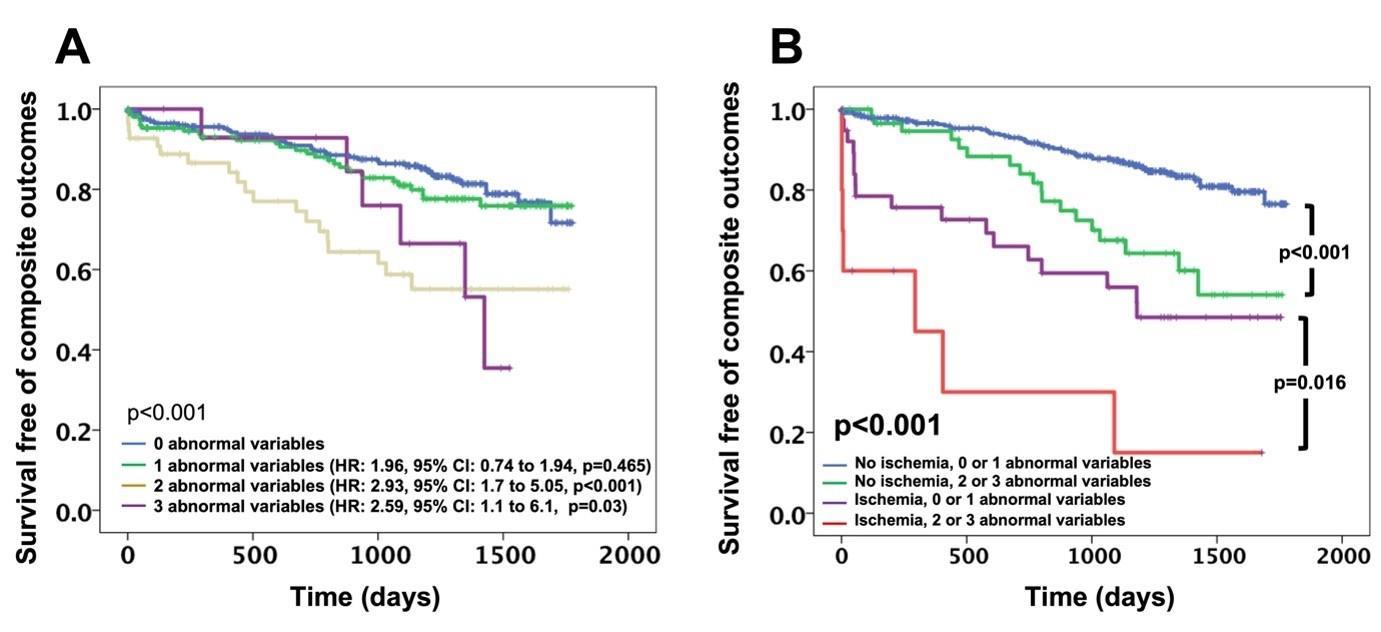
83
ABSTRACT #47
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/GENERAL INTERNAL MEDICINE
CLINICAL SYMPTOMS NOT CONGRUENT WITH DIAGNOSTIC TESTING: A PERIPHERAL ARTERIAL DISEASE CASE
Jiaxi Miao1 , Christopher N. Matthews1 , Doreen Mensah1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Lower extremity peripheral arterial disease (PAD) is a common cardiovascular disease estimated to affect 8.5 million Americans above the age of 40 years and is associated with significant morbidity, mortality, and quality of life impairment. Intermittent claudication, the classic presentation of PAD, is pain within a group of muscles induced by exercise and relieved with rest.
CASE PRESENTATION: The patient is a 56-year-old male with a past medical history of prediabetes, and tobacco use (>60 pack years), who presented to his primary care clinic endorsing right calf sharp pain after walking one block. The pain was alleviated after resting for about ten minutes. He has had similar complaints for over three years, but they were always constant in nature. Three years before the presentation, he was referred to the vascular surgery clinic for bilateral leg pain concerning for PAD. Non-Invasive Flow Studies showed normal ankle-brachial index (ABI) in the lower extremities. No exercise testing was performed afterwards. The pain was thought to be neurogenic in etiology, and he was put on Gabapentin 100 mg once daily and Tizanidine 2 mg three times a day, with only minimal relief. Physical examination revealed weak femoral pulses on palpation and 2+ right dorsalis pedis/1+ left dorsalis pedis /0 bilateral posterior tibial pulses. No evidence of skin ulcerations. There was no hair observed from the mid lower leg distally, on palpation his feet were warm with good capillary refill, bilateral lower extremity motor strength was 5/5, and bilateral light touch sensation was intact.
Given his symptoms, extensive smoking history, and physical exam findings, he was referred for an arterial Doppler ultrasound of the bilateral lower extremities to rule out PAD. The ultrasound showed remarkably highgrade stenosis and an occlusive lesion within the right common iliac (157.8 cm/s/monophasic flow/plaque) or external iliac artery. The left lower extremity demonstrates stenosis involving the common femoral artery (224.1 cm/s/monophasic flow/plaque) and peroneal artery. He was started on Aspirin 81 mg once daily, Atorvastatin 40 mg once daily, Cilostazol 100 mg twice daily, an exercise regimen, and referred to vascular surgery again one month after the presentation. The patient was in the contemplation phase of smoking cessation.
The patient underwent bilateral lower extremity angiogram with endovascular intervention two months after presentation. Post-operatively the posterior tibial pulses were palpable bilaterally. The patient quit smoking after over 30 years of consumption. At follow-up with his primary care physician three months afterwards, he reported that he could ambulate about 1.5 blocks before he experienced right lower extremity calf pain
DISCUSSION/CONCLUSION: When clinical symptoms and previous specialty workups are contradicted, who should we trust? Confirmation bias is the tendency to give greater weight to data that support a preliminary diagnosis while failing to seek or dismiss contradictory evidence. When pathognomonic intermittent claudication presented itself to the practice, it was almost intuitive to proceed with the next steps for PAD evaluation. Unfortunately, the symptoms were neglected during several visits over the course of 9 months. In this case, the voice of vascular specialty evaluation dominated the clinician's judgment in several primary care encounters. Admittedly, the initial vascular workup possessed strong evidence against the diagnosis of PAD. A low ABI (<0.9), which has a 90% sensitivity and 95% specificity for PAD. However, the patient’s ABI was normal. Much evidence suggests that post-exercise ABI has high diagnostic value in high-risk patients with normal ABI. Also, changes in the severity of symptoms during the following visits should always raise attention to rerevaluation.
84
ABSTRACT #48
CLINICAL RESEARCH CARDIOLOGY
COMPARISON BETWEEN MEN AND WOMEN WITH SEVERE OBESITY FOR RISK OF ADVERSE OUTCOMES OF MYOCARDIAL ISCHEMIA: AN EXERCISE STRESS ECHOCARDIOGRAPHIC STUDY
Errol Moras1, Kruti Gandhi1, Joseph Elias1, David Meister1 , Maria Peña1, Christopher Perez Lizardo1 , Brissete Mancero1, Ga Hee Kim1, Elizabeth Zipf1, Loba Alam1, Swiri Konje1, Alaa M Omar1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Obesity and sex have a complex relationship with myocardial ischemia. We explored the association of sex and severe obesity with adverse cardiovascular outcomes in patients with ischemic exercise stress echocardiography
METHODS: We retrospectively studied 142 patients with ischemic exercise stress echocardiography [Age: 65 ± 11 years, 70 (49%) women, EF: 57 ± 8%, body mass index (BMI): 28 ± 6 kg/m2]. Severe obesity (BMI>35 kg/m2) occurred in 48 (34%) patients. Patients were stratified based on obesity and sex (4 groups, women, and men with and without severe obesity), followed for median of 1.5 years, and compared for clinical, exercise variables and occurrence of composite outcomes (death, acute coronary syndrome, cardiac hospitalization, and repeat ischemia testing).
RESULTS: In our study, 28 (20%) women and 20 (14%) men had severe obesity, and 42 (29%) women and 52 (37%) men had no severe obesity. Groups were not different for age, risk factors, exercise characteristics, and resting LV function. Outcomes occurred in 85 (60%) patients and were more prevalent in women with severe obesity compared to women without or men with or without severe obesity [21 (75%), 17 (40%), 11 (55%), and 35 (67%), p=0.014]. Sex and severe obesity did not predict outcomes in isolation [HR, 1.13 (95%CI: 0.74 to 1.73), 1.48 (95%CI: 0.95 to 2.3), respectively, figure 1A, B]. Survival analysis showed that women without severe obesity were at lowest risk, men were at similarly elevated risk irrespective of severe obesity, and women with severe obesity were at highest risk for composite outcomes [p=0.037, figure 1C, HR, 2.5 (95%CI: 1.3 to 4.8)]. After adjusting for clinical, exercise, and echocardiographic variables, women with severe obesity remained at high-risk [HRm 2.2, (95%CI: 1.06 to 4.36)].
CONCLUSION: In patients with ischemic exercise stress echocardiography, women with severe obesity are at higher risk for adverse cardiac outcomes. Future studies are needed to understand the pathophysiologic mechanisms underlying this association.
85
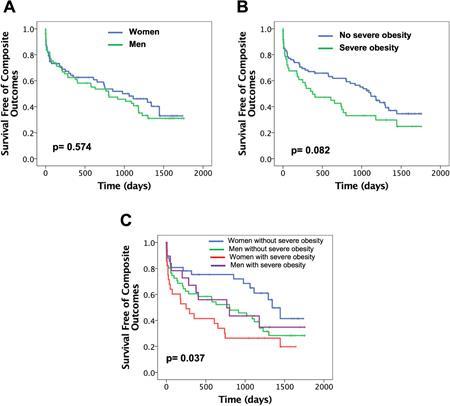
86
Figure 1: Kaplan Meier plot showing survival stratified by gender, sex and combined; p≤0.05 using the log-rank test for overall comparison among the groups
ABSTRACT #49
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/HEMATOLOGY/ONCOLOGY
CHECKPOINT IMMUNOTHERAPY-INDUCED MYOCARDITIS REQUIRING MECHANICAL CIRCULARLY SUPPORT: A CASE REPORT AND FUTURE OUTLOOK
Anna Sophie Mueller 1 , Ashish Correa1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Immune checkpoint inhibitors have been proven to be successful in management of many cancers. They work through re-activating tumor suppressed T-cells, stimulating an immune response. Checkpoint inhibitors, though effective, can offset severe immune related adverse events, including myocarditis. The incidence of immune checkpoint inhibitors-associated myocarditis is estimated to be up to 1.1%, with a mortality rate of up to 50%. However, the mechanisms leading to cardiac cell injury remain poorly understood and current guidelines do not recommend surveillance of cardiac injury for asymptomatic patients. The objective of this case report is to illustrate the challenges in managing patients who experience immune checkpoint inhibitor (ICI) related myocarditis.
CASE PRESENTATION: Our patient was a 53-year-old man who presented with acute pressure like, left chest pain. He had a history of metastatic melanoma for which he had undergone his first dose of immune checkpoint inhibitor treatment, namely Ipilimumab and Nivolumab, 10 days prior. At baseline the patient was not known to have any cardiac history. In the emergency department, he was found to have severe elevated cardiac markers, with a troponin of 79 ng/ml, CK: 4740 U/l, CKMB: 193 U/l, BNP: 250 ng/L. His initial EKG showed a right bundle branch block and multiple premature ventricular contractions. He underwent a left heart catheterization which found only minimal coronary artery disease, left ventricle (LV) gram showed mild LV dysfunction. He was admitted to the CICU for the management of presumed ICI-related myocarditis. Over the ensuing hours, the patient progressed into cardiogenic shock requiring multiple inotropes and pressors, and went into slow ventricular tachycardia (VT) that was refractory to antiarrhythmics. The patient was placed on peripheral VenoArterial Extracorporeal Membrane Oxygenation, alongside treatment with pulse steroids, as a potential bridge to recovery. The next day his LV was noted to be dilated, with elevated filling pressures, suggesting poor LV offloading. Therefore, an Impella was placed to help vent the LV. Additionally, the patient was intubated for increased work-of breathing. However, the patient continued to have rising troponins, frequent ventricular arrhythmias, persistent biventricular dysfunction and abnormal hemodynamics requiring pressor support After discussions with the cardio-oncology team we trialed Abatacept on day 3 of his hospitalization which led to a downtrend in his troponin and CPK levels. Despite all efforts, serial echocardiograms did not show significant improvement in myocardial function On day 8 the patient had a coughing spell, followed by AF with RVR and recurrent VT, requiring defibrillation and consistent low mean arterial pressure Extracorporeal Membrane Oxygenation (ECMO) and Impella flows were noted to be low with concerns for thrombosis, high dose heparin was given without any improvement, minimal tidal volumes were noted in the ventilator and bagging resulted in drops in ECMO flow, chest radiography showed a white-out of both lungs. Ultimately the decision was made to not further escalate treatment and the patient died that same day
CONCLUSION: The number of cancer patients being eligible for immune checkpoint inhibitors treatment is expected to be up to 1 million this year, as this number increases, the number of cases of myocarditis is expected to rise with it. Though current guidelines do not recommended surveillance of cardiac damage, its growing use and associated high mortality rate, may support some type of monitoring to safely continue this class of cancer medication. Further research identifying predictive biomarkers to recognize patients at risk is needed.
87
ABSTRACT #50 CLINICAL RESEARCH GASTROENTEROLOGY
UNIVERSAL PROTOCOLIZED ALCOHOL BIOMARKER SCREENING IS EFFECTIVE IN DETECTING HIGH RATES OF ALCOHOL-RELATED CONTRAINDICATIONS TO LIVER TRANSPLANTATION
Rohit Nathani1, Adam Winters2 , Chip Bowman-Zamora2 , Jonathan Nahas3, Sander S. Florman2, Thomas D. Schiano2 , Gene Y. Im2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3University of Pennsylvania, Philadelphia, PA, United States
Presented at the American Association for the Study of Liver Diseases (AASLD) Annual Meeting held in Washington DC, United States from November 4-8, 2022.
BACKGROUND/INTRODUCTION: The use of alcohol biomarkers, such as urine ethyl glucuronide (EtG)/ethyl sulfate (EtS) and serum phosphatidyl ethanol (PEth), to monitor alcohol use is increasing but has not been universally adopted by liver transplant centers. The aim of this study is to evaluate the impact of protocolized alcohol bio-marker screening in patients with alcohol-associated liver disease referred for liver transplant, specifically rates of psychosocial clearance and liver transplant.
METHODS: A center-wide electronic medical record protocol of alcohol biomarker screening (EtG/EtS and/or PEth) was initiated in 8/2018 for all new liver transplant evaluations. Using a prospectively maintained database from 8/2018 through 12/2020, consecutive new outpatient liver transplant referrals and those already under evaluation for alcohol-associated liver disease were retrospectively examined. Patients positive for EtG/EtS and/or PEth during the evaluation process were included. We measured the rate of psychosocial clearance for liver transplant and the rate of receipt of liver transplant. Follow-up was performed up to one year from the date of an index positive test.
RESULTS: Over a 16-month period, 455 patients were under liver transplant evaluation for alcohol-associated liver disease with near universal testing with alcohol biomarkers (447/455, 98%) as per protocol. Overall, 123 (27%) had a positive biomarker at some point during their evaluation. A majority (66/123, 53.7%) had positive tests at the initial liver transplant visit. Thirty-seven (30%) patients were positive for all three biomarkers. There was concordance between the same visit's positive biomarker and self-reported drinking in 74/123 (60.2%). Sixteen additional patients (32.6%) later admitted to recent alcohol use after positive biomarker discussion. At least one set of repeat biomarkers was obtained in 73 patients (59%). For those patients, whose positive test occurred after their initial visit, the median time to positive test from referral was 60 days (range: 0-254 days). Only 9 (7.3%) patients with positive biomarkers eventually received psychosocial clearance for liver transplant Only three patients (2.4%) underwent liver transplant. The median time from positive test to liver transplant was 287 days (range: 77- 370).
CONCLUSION: Protocolized alcohol bio-marker screening in liver transplant evaluations for alcohol-associated liver disease detects early and high rates of alcohol contraindications to liver transplant. This supports universal alcohol biomarker screening of alcohol-associated liver disease patients evaluated for liver transplant. If replicated at other liver transplant centers, alcohol biomarker screening may be an effective tool to help guide the decision to refer patients with alcohol-associated liver disease for transplant evaluation.
88
ABSTRACT #51
CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
THE UTILITY OF HEREDITARY THROMBOPHILIA TESTING AMONG PATIENTS WITH UNPROVOKED VENOUS THROMBOEMBOLISM
Cristina Olivo Freites1 , Leonard Naymagon2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in the International Journal of Laboratory Hematology, 2022. PMID: 34749438
BACKGROUND/INTRODUCTION: Hereditary-thrombophilia testing is often sent during the evaluation of patients with unprovoked venous thromboembolism (VTE). This remains a frequent practice even though the results of such testing are often of unclear practical significance.
METHODS: We conducted a multicenter retrospective study to assess whether hereditary-thrombophilia is associated with risk of recurrent VTE among patients who discontinue anticoagulation following an unprovoked VTE.
RESULTS: A total of 528 adult patients were included, 28% of whom (N = 110) tested positive for hereditarythrombophilia. Median follow-up was 55 months (IQR 40-66 months) following anticoagulation discontinuation. One hundred and twenty-four patients (23%) had a recurrent VTE during follow-up, including 29/110 with hereditary-thrombophilia (26%) and 95/418 without hereditary-thrombophilia (23%). Risk of recurrent VTE over time was similar between the two groups (logrank p=0.47). The Hazard Ratio (HR) for recurrence among patients withhereditary-thrombophilia was 1.17 (95%CI 0.76 to 1.81). On multivariable analysis, hereditary-thrombophilia was not associated with recurrence of VTE (HR with hereditary-thrombophilia, 1.07; 95%CI, 0.69 to 1.65; p=0.74). The only factor significantly associated with risk of VTE recurrence on multivariable analysis was presence of pulmonary embolism (as opposed to deep venous thrombosis alone) (HR, 1.54; 95%CI 1.02 to 2.30; p=0.035).
CONCLUSION: The presence of hereditary-thrombophilia was not associated with risk of recurrent venous thromboembolism in this cohort of patients. These findings underscore the questionable clinical utility of routine thrombophilia testing among patient with unprovoked venous thromboembolism and suggest that such testing should not be routinely pursued.
89
ABSTRACT #52
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
MEDICAL EDUCATION IN THE POST-COVID ERA: ATTITUDES AND PERCEPTIONS OF VIRTUAL VESUS IN-PERSON EDUCATION IN INTERNAL MEDICINE RESIDENTS AND FACULTY
Ricardo J. Ortiz1 , Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
BACKGROUND/INTRODUCTION: During the COVID-19 pandemic, graduate medical education underwent a paradigm shift due to the disruption of in-person didactics. Virtual tools and techniques provided an alternative to delivering medical education, which have their own advantages but also pose unique challenges. The purpose of this study is to describe perceptions and attitudes about in-person versus virtual medical education among Internal Medicine residents and faculty in a residency program.
METHODS: This was a cross-sectional study. Two different surveys, one for residents and one for faculty, adapted from Tsyrulnik et al, were distributed to all Internal Medicine residents and faculty at Mount Sinai Morningside and West Hospitals. A unique link was created for each subject and their responses were recorded using Microsoft FormsTM
RESULTS: Resident response rate was 30% and faculty response rate was (9%). Most of the participants in the resident group were PGY-1 (53%). At least 49% of the participants had prior experience with virtual didactics before starting residency. 46% were less likely to participate in virtual didactics. Both groups perceived virtual didactics as less conducive compared to in-person didactics (64% in both groups). 55% of residents reported less attention to virtual didactics. Engagement was perceived as lower by 56% of the faculty. Use of electronic devices for professional and non-professional activities was higher with virtual didactics (62% and 51% respectively) in the resident group. Engagement in unrelated professional activities was the most common activity reported by both groups (71.1% in the resident group and 76% in the faculty group). 40% of the faculty group would be more likely to volunteer to provide virtual lectures compared to in-person. 64% of residents felt that the change to virtual didactics had a positive impact on their quality of life. Both groups missed the social interactions related to in-person didactics (71% in the resident group and 76% in the faculty group).
CONCLUSION: Virtual didactics are perceived as equally effective but less engaging by residents and faculty. Both groups engage in professional activities during virtual didactics but miss the social interactions of in-person didactics. Virtual didactics have a positive impact on the perceived quality of life for residents.
90
ABSTRACT #53
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
CANDIDA PARAPSILOSIS PROSTHETIC VALVE ENDOCARDITIS
Maria Peña1 , Mudita Patel1 , Christine Stavropoulos1 , Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Disseminated fungal infections are rare, with fungal endocarditis encompassing 2-4% of infections, with Candida accounting for 1-2% of all cases of infectious endocarditis. Risk factors for fungemia are intravenous drug use, immunocompromised state, neutropenia, indwelling catheter use, prosthetic devices, renal failure, and hemodialysis. Candida and Aspergillus are the two most common organisms to cause invasive disease There are about 15 distinct candida species but C. albicans, C. glabrata, C. tropicalis, C. parapsilosis, and C. krusei are among the five common species that cause more than 90% of invasive disease. C. albicans is the most common
CASE PRESENTATION: The patient was 65 year-old female with past medical history of chronic obstructive pulmonary disease (on home oxygen 3L/min), severe pulmonary hypertension, obstructive sleep apnea, hypertension, hyperlipidemia, end-stage renal disease on hemodialysis via arteriovenous fistula (AVF), severe aortic stenosis (AS) requiring transvenous aortic valve replacement (TAVR) in 9/2021 (Sapien 3 ultra-valve replacement) with complication due to intra-operative complete heart block following post-valve deployment requiring transvenous pacer and ultimately dual chamber permanent pacemaker placement prior to discharge, presented 3 months later for worsening and persistent back pain and left lower extremity pain. The patient had been treated at an outside hospital for lower extremity weakness and paresthesia recently and reported to have Candida parapsilosis (C. parapsilosis) blood stream infection for which she was treated with Caspofungin for 2 weeks before leaving against medical advice on oral fluconazole prior to presenting for admission. On initial presentation to our hospital, she was afebrile and hemodynamically stable. No leukocytosis. She was monitored off of antimicrobials and antipyretics; remained afebrile. Initial and repeat blood cultures were positive with C. parapsilosis. Inflammatory markers were elevated (ESR 60 and CRP 106). Initial computed tomography (CT) lumbar spine (L-spine) was remarkable for a soft and well marginated soft tissue density eroding the inferior endplate of the L5 vertebral body and the superior endplate of the S1 vertebral body involving the anterior soft tissues and may represent amyloidosis, Magnetic resonance imaging (MRI) L-spine showed L5-S1 discitis/osteomyelitis without an epidural abscess. During her hospital course, Infectious Disease (ID) medicine was consulted for further management of her lumbar discitis/OM. She was then started on Caspofungin empirically. Repeat blood cultures grew C. parapsilosis while she remained afebrile and clinically stable. There was no evidence of eye involvement on ophthalmologic examination. Initial transthoracic echocardiography (TTE) was without vegetations. Transesophageal echocardiography (TEE) was without vegetations, intracardiac masses or abscesses. However, aortic prosthetic valve and PPM infection could not be excluded. The patient subsequently underwent permanent pacemaker with lead removal and temporary transvenous pacing (TVP) placement without complication on hospital admission day 9. She was then transferred to Coronary Care Unit (CCU) for close monitoring. Throughout the hospital course the patient had persistent candidemia. Repeat daily blood cultures were without Candida clearance. She then had a gallium scan of left upper arm which showed increased uptake radiotracer concerning for AVF infection. The patient was taken for TVP removal with the placement of a permanent leadless pacing device. Device placement was aborted as intra-operatively course was complicated by hypotension, hypoxia, and hypercapnia with cardiac arrest with return of spontaneous circulation (ROSC) achieved in thirty minutes. She was then transferred back to CCU and remained intubated with pressor support. With the patient’s failure to clear candidemia, the decision was made to continue with indefinite antifungal therapy in the setting of likely infected TAVR and AVF.
91
CONCLUSION: We report an unusual case of candidemia with many challenges regarding medical management. In our patient on hemodialysis (via arteriovenous fistula) with persistent candidemia in the setting of a permanent pacemaker with a recent transvenous aortic valve replacement, it was not entirely clear when the patient acquired fungemia. Although dialysis patients with AVF are less prone to infections when compared to those with arteriovenous graft, repeated access of AVF can be a possible cause of infection. Another possible source is her recent TAVR resulting in disseminated infection involving her AVF, intracardiac device, and discitis/OM of her lumbar/sacral spine. The inability to remove TAVR in this patient with prolonged and persistent candidemia required unique medical management for prosthetic valve fungal infection. The clinical decision making in this patient’s case required a multidisciplinary approach involving multiple subspecialties. Candida parapsilosis complex has become the second most common pathogen of candidiasis. C. parapsilosis is a colonizer of normal flora found within the oropharynx, gastrointestinal tract, and skin. Risk factors for invasive disease like general fungemia are: prosthetic valves (57.4%), IV drug use (IVDU; 20%), IV parenteral nutrition (6.9%), abdominal surgery (6.9%), immunosuppression (6.4%), broad-spectrum antibiotics (5.6%) and previous valvular disease (4.8%). Additionally, C. parapsilosis has also been linked to indwelling central venous catheters (CVC), long-term glucocorticoid therapy, transplant recipients, transcatheter aortic valve replacement (TAVR), and cardiac devices. Incidence of infection associated with pacemaker placement range from 0% to 12.6% with increasing rates ranging from 0.13% to 19.9% for permanent pacemakers and from 0.2% to 7.2% for ICDs. This case report outlines an unusual case of candidemia of C. parapsilosis with invasive disease presenting with many challenges regarding medical management which required a multidisciplinary team approach as FE is associated with high morbidity and mortality.
92
ABSTRACT #54
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY
A CASE OF ANAPHYLAXIS FOLLOWING ULTRASOUND CONTRAST AGENT
Christopher Perez Lizardo1 , Foram Parikh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Contrast agents are widely used in echocardiography to improve visualization of the left ventricular endocardium in patients with suboptimal windows. Hypersensitivity reactions are rare but have been described.
CASE PRESENTATION: We present a case of a 57-year-old male with a history of heart failure with recovered ejection fraction and alcohol use disorder who presented to the emergency room for alcohol withdrawal with complaints of worsening dyspnea on exertion prior to hospitalization. Given concerns of worsening cardiac function due to alcohol induced cardiomyopathy, he underwent a transthoracic echocardiogram. Patient developed sustained hemodynamic instability and hypoxia immediately after administration of Definity® contrast during routine echocardiogram. His vitals were: blood pressure 76/54 mmHg, heart rate 110 bpm, SaO2 82% on room air, and a respiratory rate of 30 breaths per minute. He received intramuscular epinephrine as well as intravenous methylprednisolone, diphenhydramine, and intravenous fluid resuscitation, with gradual improvement in symptoms. The patient was subsequently transferred to Intensive Care Unit for management of anaphylactic shock. This patient had no known drug allergies and had received iodinated contrast in the past but not lipid-based contrast.
DISCUSSION: Lipid emulsions are used in sonography due to increased echogenicity produced by the sonic waves interacting with the lipid molecules. In contrast, iodinated contrast agents are used in X-ray-based imaging as the high atomic number of iodine limits the ability of X-rays to pass through tissues where the iodinated contrast is present. In 2007, the FDA issued black box warning to Definity® contrast due to severe cardiopulmonary reactions. Restrictions were lifted in 2011, but allergic reactions continued to be reported. In 2021, the FDA warned physicians against using ultrasound contrast agents in patients with polyethylene glycol allergy. Studies for other adverse reactions are ongoing.
CONCLUSION: Although the risk of hypersensitivity reactions for lipid-based contrast agents is lower than that of iodinated agents, anaphylaxis has been described in patients with prior history of allergies and patients allergic to polyethylene glycol. Contrast agents improve diagnostic accuracy and help facilitate guidance in treatment and therefore their benefits outweigh their risk of adverse effects. With this case report we aim to raise physician awareness of the substantial risk of hypersensitivity reactions to these increasingly used lipid soluble contrasts for routine echocardiograms.
93
ABSTRACT #55 CLINICAL RESEARCH INFECTIOUS DISEASES
EVALUATION OF THE AGREEMENT AND PREDICTIVE PERFORMANCE OF CARBAPENEM RESISTANT ENTEROBACTERALES RISK PREDICTION MODELS IN HOSPITALIZED PATIENTS
Hendrik Sy1 , Carlos Plazola1, Arsheena Yassin2 , Kristy Huang1 , Mukti Patel1, Lina Loaiza1, Samuel Acquah3 , Sara Radparvar3, Christine Stavropoulos1, Joseph Mathew1, Andras Farkas1
1Mount Sinai Morningside and West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Bon Secours Charity Health System, Suffern, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the 32nd European Congress of Clinical Microbiology and Infectious Diseases that was held Lisbon, Portugal from April 23-26, 2022.
BACKGROUND/INTRODUCTION: Accurately predicting the presence of Carbapenem Resistant
Enterobacterales (CRE) in hospitalized patients would support timely initiation of CRE active agents. The aim of this study is to determine how reliably the risk prediction models identify patients likely to require empiric anti-CRE treatment, preliminary results of which are presented herein.
METHODS: A systematic search was conducted to identify all existing CRE risk prediction models for validation in our patient population. Data was gathered on model predictors, baseline demographics, clinical information, microbiology results, antibiotic utilization history and index infection with three teams of two raters collecting the same data points, retrospectively. Besides calculating a model averaged Area Under the Receiver Operating Characteristic (AUROC), we established optimal prediction score cutoffs and false positive rates (FPR) where corresponding model performance maintains a false negative rate (FNR) of <10%, <20%, and <30%, respectively. The intraclass correlation coefficient was calculated to establish rater agreement.
RESULTS: Eleven models were retained for validation. We identified 69 patients, 36 of which were treated for a CRE infection. Previous admission, organ transplantation, chronic kidney disease, infection type, and carbapenem use were baseline variables that significantly differed between the groups treated for a CRE versus non-CRE related infection. The models' ability to discriminate varied as evidenced by the AUROC range of 0.58 to 0.78, suggesting the Gao, et al model as the overall best. The model by Yang, et al produced the best FPR when evaluated at the pre-specified FNR interval of < 10%, while the model of Gao, et al performed best for intervals > 10% to < 30%.
CONCLUSION: Discriminative ability of the risk prediction models showed varying performance. The averaged model by Yang et al. appears to be most useful when a low risk level is deemed acceptable for failure rate, while at a moderate to high risk of missing a CRE case (20% and 30% FNR), the model by Gao et al. is most desirable as it minimizes the chance of over-treatment and it showed moderate to good agreement. Additional work to increase sample size is currently ongoing.
94
ABSTRACT #56
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
EFFECT OF INHALED EPOPROSTENOL ON OXYGENATION IN COVID-19 PATIENTS WITH ACUTE HYPOXEMIC RESPIRATORY FAILURE
Maria Athena Riego1, Natasha Garg2, Omar Mahmoud3, Elizabeth Zipf1 , Dishant Shah4, Edith Robin1 , Abhinav Hoskote5, Arpanjeet Kaur1, Sara Luby1, Venus Sharma1, Raymonde Jean1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Jamaica Hospital Medical Center, Jamaica, NY, United States; 3University of Maryland Medical Center, Baltimore, MD, United States; 4Westchester Medical Center, Valhalla, NY, United States; 5Holy Spirit Medical Center, Camp Hill, PA, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Nashville, Tennessee, United States from October 16-19, 2022.
BACKGROUND/INTRODUCTION: Inhaled pulmonary vasodilators such as Epoprostenol (iEPO) have been utilized in mechanically ventilated patients with ARDS and have shown to improve oxygenation. This is due to cAMP-mediated selective vasodilation of pulmonary vessels resulting in improvement in ventilation to perfusion matching. Additionally, a direct protective effect on the pulmonary vasculature has been postulated. We aimed to assess the physiological outcomes of iEPO on patients with acute hypoxemic respiratory failure due to COVID-19 pneumonia.
METHODS: An IRB-approved retrospective study was done on 105 COVID-19 patients. Indication for iEPO was refractory AHRF but ultimate decision for administration was at the discretion of the treating physician. There was no set cutoff for SpO2, PaO2, or P/F ratio when it was initiated. A subgroup analysis was performed on patients requiring high flow nasal cannula (HFNC), non-invasive ventilation (NIV), and invasive mechanical ventilation (IMV). Primary outcomes were change in oxygen saturation, FiO2 requirements, respiratory rate (RR), and pCO2.
RESULTS: iEPO significantly improved the PaO2 after 24 hours of administration [63 (53-72) versus 77 (61114), p<0.005] and SpO2 after 36-72 hours [92 (89-94) versus 94 (91-96), p=0.019]. FiO2 requirements decreased after 36-72 hours (94.65 ± 11.65 versus 87.39 ± 16.52, p<0.005). No changes in pCO2 levels or respiratory rate were observed. Subgroup analysis showed that among patients requiring HFNC, iEPO significantly increased PaO2 after 24 hours [62.05 (57-64.8) versus 78.5 (65-89), p=0.031] and decreased FiO2 requirements after 36-72 hours (94.64 ± 13.92 versus 82.42 ± 19.66, p=0.005). Among patients requiring NIV, there was no significant change in oxygenation or oxygen requirements. In patients on IMV, iEPO increased PaO2 within 24 hrs [64 (57-72.4) versus 79 (62-119.1), p=0.000] and SpO2 (90.05 +/- 6.08 versus 91.44 +/- 6.85, p=0.048). FiO2 requirements decreased after 36-72 hours (93.86 +/-11.03 versus 87.88 +/15.22, p=0.008). PCO2 significantly decreased at 24 hours and 36-72 hours [56.5 (46.5-70) versus 52.7 (4758)in 24 hours, p=0.010; and 47.3 (40.1-60), p=0.006 in 36-72hrs]
CONCLUSION: We present the largest study to date evaluating the effects of iEPO in patients with acute hypoxemic respiratory failure due to COVID-19 pneumonia. iEPO improved oxygenation within the first 72 hours. iEPO improved oxygenation and reduced oxygen requirements among patients on HFNC. Patients on NIV had no improvement in oxygenation and an apparent worsening of gas exchange, with 95% of the patients on NIV required intubation. These patients were possibly at a more advanced stage of acute hypoxemic respiratory failure and thus less likely to respond to iEPO. In patients on IMV, iEPO improved oxygenation and gas exchange. It should be noted that increased PEEP may have contributed to the improvement in oxygenation. iEPO should be considered in patients with AHRF due to COVID-19 requiring HFNC and IMV as it can significantly improve oxygenation.
95
ABSTRACT #57 CLINICAL RESEARCH CARDIOLOGY
OUTCOMES OF CHRONIC TOTAL OCCLUSION RECANALIZATION IN PATIENTS WITH PRIOR BYPASS
SURGERY: AN UPDATED SYSTEMATIC REVIEW AND META-ANALYSIS OF REAL WORLD REGISTRIES
Francisco José Romeo1, Francesco Moroni2 , Marco Giuseppe Del Buono3,4, Juan Ignacio Damonte5 , Juan Guido Chiabrando5
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2University of Virginia, Charlottesville, Virginia, United States; 3Catholic University of the Sacred Heart, Rome, Italy;
4Fondazione Policlinico Universitario A. Gemelli IRCCS, Rome, Italy; 5Hospital Italiano de Buenos Aires, Buenos Aires, Argentina
BACKGROUND/INTRODUCTION: Recanalization of chronic total occlusion coronary lesions by percutaneous coronary intervention (PCI) in patients with prior coronary artery bypass grafting (CABG) is still considered a challenging scenario due to the complexity of coronary lesions as well as the requirement of chronic total occlusion PCI advanced techniques. The aim of this study is to compare clinical outcomes of patients undergoing chronic total occlusion PCI with and without CABG surgery.
METHODS: We conducted a systematic review and meta-analysis of observational studies that compared inhospital outcomes of chronic total occlusion PCI in patients with versus without prior CABG published in Medline in English or Spanish from inception until December 2022. The results are synthesized in a quantitative manner with random effects models. Categorical variables were compared usingthe chi-square test, whereas continuous variables were compared using a 2-sample Student's t-test. Statistical heterogeneity was assessed by I2 statistics: I2 statistic >50% was considered substantial, and I2 >75% was considered considerable. The Review Manager Software version 5.3.5. (The Cochrane Collaboration, 2014) was used to calculate summary statistics [odds ratios (ORs) with 95% confidence intervals (CIs)]
RESULTS: In total, eleven observational studies with a total of 35,666 patients were included, of whom 7,005 patients had a history of CABG Prior CABG patients were older (68.08 ± 9.03 versus 64.06 ± 10.67 years of age; p<0.001) and had more complex coronary lesions (J-CTO score: 3.18 ± 1.37 versus 2.46 ± 1.43; p<0.001). Prior CABG was associated with lower technical success (66.6% versus 78.5%; OR, 0.53; 95%CI, 0.43 to 0.65; p<0.00001, I2 = 84%) as well as lower procedural success (80.5% versus 86.1%; OR, 0.64; 95%CI: 0.57 to 0.71; p<0.00001, I2 = 0%) as compared with patients with no prior CABG. Prior CABG patients had a higher incidence of in-hospital mortality (0.70% versus 0.38%; OR, 2.00; 95%CI, 1.32 to 3.05; p=0.001, I2 = 9%), coronary perforation (3.74% versus 2.27%; OR, 1.64; 95%CI, 1.15 to 2.33; p<0.006, I2 = 74%), and myocardial infarction (1.66% versus 0.74%; OR, 2.57; 95%CI, 1.73 to 3.81; p<0.00001, I2 = 12%), but a lower incidence of cardiac tamponade (0.19% versus 0.88%; OR, 0.36; 95%CI, 0.17 to 0.77; p=0.09, I2 = 0%) compared with those without prior CABG. Both groups had a similar incidence of acute cerebrovascular events (0.15% versus 0.10%; OR, 1.70; 95%CI, 0.75 to 3.88; p=0.21, I2 = 0%), major bleeding (1.39% versus 1.17%; OR, 1.24; 95%CI, 0.96 to 1.61; p=0.09, I2 = 0%),and vascular complications (1.42% versus 0.88%; OR, 1.50;95%CI, 0.93 to 2.41; p=0.10, I2 = 0%).
CONCLUSION: Prior CABG patients undergoing CTO PCI presented a higher chance of in-hospital mortality and perioperative procedural complications albeit a lower chance of cardiac tamponade.
96
Figure 1.
Technical Success
Procedural Success
In-Hospital Mortality
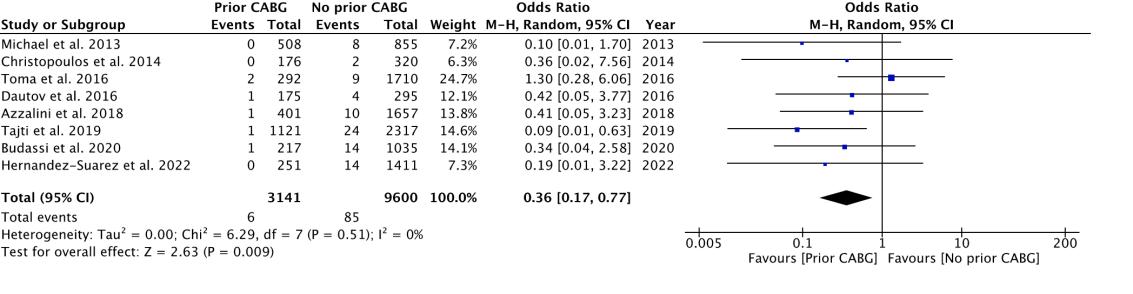
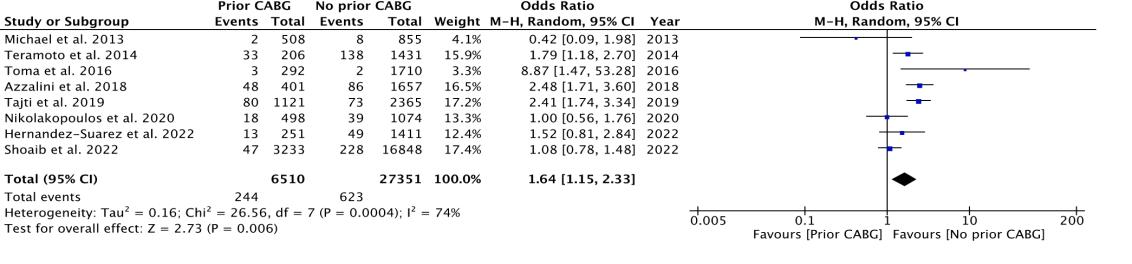
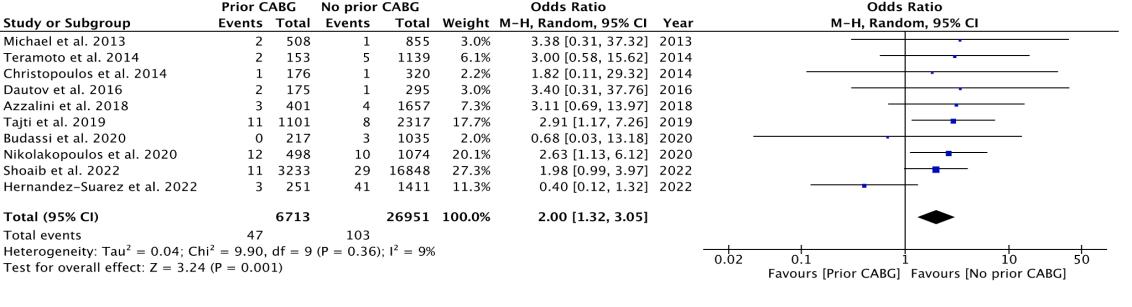
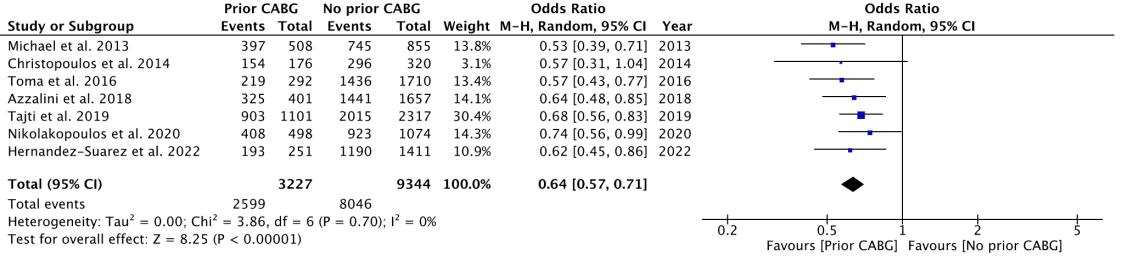
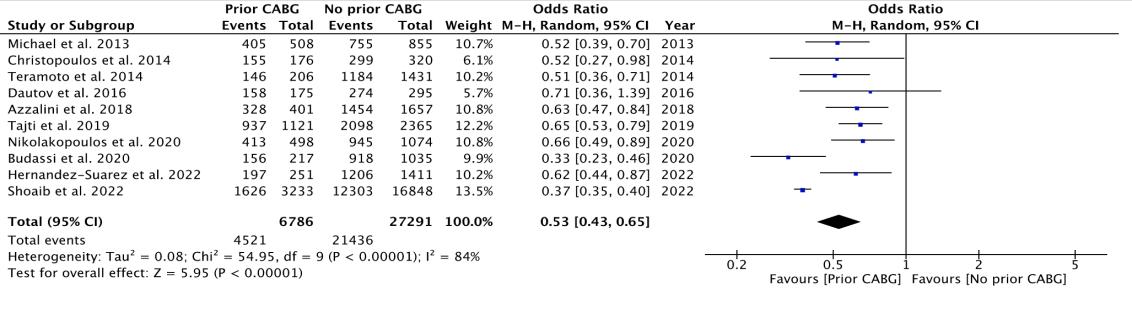
Coronary Perforation
Cardiac Tamponade
97
ABSTRACT #58
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GENERAL INTERNAL MEDICINE
A CASE OF LAUGHING HER WAY TO VITAMIN B12 DEFICIENCY
 Norah Sadek1 , Bharat Monga1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Norah Sadek1 , Bharat Monga1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Nitrous oxide has historically been used as an inhaled anesthetic in dentistry, as an anxiolytic in neuropsychiatry, and as a propellant in the food industry (whipped cream). Its use as a recreational drug by adolescents has become more prevalent in recent years as it is easy and legal to access via the Internet. The colorless, sweet-smelling gas is discharged from aerosol cartridges into latex balloons and inhaled for temporary analgesic, anxiolytic and euphoric effect (Image 1). The effects culminate in a few seconds, usually lasting less than a few minutes. Chronic use has been shown to cause Vitamin B12 deficiency through several mechanisms. Neurological symptoms are often the first to present followed by hematologic signs. We present a case of vitamin B12 deficiency as part of chronic nitrous oxide abuse.
CASE PRESENTATION: The patient is a 23-year-old female with no past medical history presented to the emergency department with chief complaint of persistent right knee pain. She stated that she fell three months ago when leaving the university library. She denied loss of consciousness or any other trauma. She was disheveled and cognitively impaired. She displayed poor eye contact and gave minimal history. She was able to respond to linear questions appropriately with a delay. Her judgement and insight were found to be poor. On physical examination, she was unable to dorsiflex her feet and had sensory ataxia with accentuated flexion at the hips and knees. She could not walk without visual cues. She had bilateral lower extremity numbness and upper extremity tremors. Her motor strength was intact in all extremities. She had no acute finding on the right knee examination. Laboratory data showed leukocytosis with macrocytic anemia (Hb-10.8 g/dL and MCV-110 fL). Lumbar puncture was performed. Cerebrospinal fluid analysis, chest X-ray, and computed tomography (CT) of head were unremarkable. Her urine toxicology screen was negative. Her vitamin B12 level was <146 pg/mL. Further inquiry revealed that she had inhaled "whipped cream" a few times a week for more than a year. She refused medical workup and chose to leave against medical advice. Drug cessation counseling was done. She was advised to supplement it with high dose vitamin B12.
DISCUSSION: There are several proposed mechanisms of nitrous oxide toxicity put forth in the literature. Nitrous oxide oxidizes the central cobalt moiety of vitamin B12, converting irreversibly from its monovalent to a divalent form. This form of methyl cobalamin cannot act as a cofactor in the synthesis of methionine. Similarly, it also cannot convert 5-methyltetrahydrofolate to tetrahydrofolate, a crucial step in DNA synthesis. Finally, the inactivation of vitamin B12, or cobalamin, leads to the production of methylmalonic acid instead of succinylCoA, leading to myelin inflammation. The interruption of these pathways leads to a concomitant increase in homocysteine and methylmalonic acid (Figure 1). Given the functional vitamin B12 deficiency, it is proposed
Image 1: N20 Aerosol cartridge 1
98
that increased homocysteine and methylmalonic acid can be a more sensitive marker of nitrous oxide toxicity, despite normal vitamin B12 levels. In this case the vitamin B12 levels were extremely low, although the research does not show a correlation between vitamin B12 levels and severity of neurologic impairment.
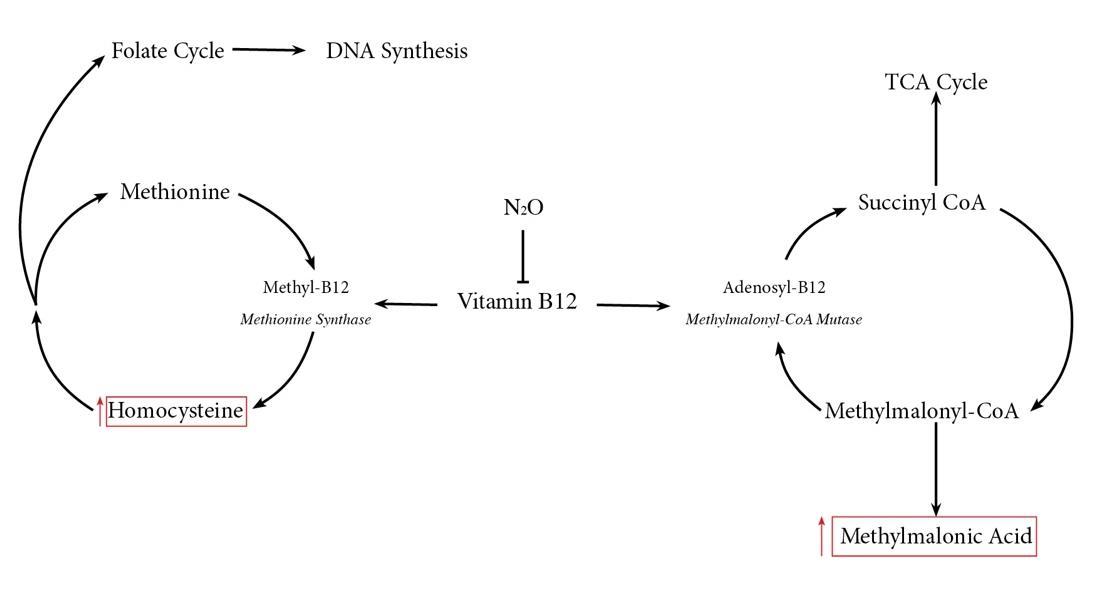
Figure 1: Vitamin B12 functions as cofactor in to methionine synthase and methylmalonyl-CoA Mutase enzymes. The functional deficiency of Vitamin B12 leads to interruption of the synthesis of Methionine and Succinyl CoA. Downstream effects include decreased folate and myelin synthesis.
Patients primarily present with neurologic symptoms including myeloneuropathy, peripheral neuropathy and subacute combined degeneration. Patients may develop neuropsychiatric symptoms, including thought disturbances, paranoia, and delusions. Evidence of macrocytic anemia is often a sign of late progression of the disease, in many instances there is no evidence of hematologic effects. Our patient exhibited a rare combination of all three, showing neurological, psychiatric, and hematological effects. Magnetic Resonance Imaging (MRI) is an important radiologic modality used to diagnose subacute combined degeneration, often seen as hyperintensity of the dorsal and lateral spinal column, noted as a “three-point sign”. Unfortunately, the patient left against medical advice prior to any further imaging.
Early diagnosis and treatment are crucial for improved outcomes among these patients. There is a common misconception perpetuated among some whippet users' diet or supplements can prevent these side effects. However, given the mechanism by which nitrous oxide renders vitamin B12 inactive, this is an ineffective prophylaxis. Drug cessation education must be emphasized to prevent further neurologic damage. In most cases, it is recommended to initiate parenteral vitamin B12 for the first week, followed by a prolonged course of oral supplementation.
CONCLUSION: Whippets is the most popular inhalant in the United States. 4.7% of people over age 12 and 5.2% of people over age 26 have used whippets at some point in their lives – amounting to millions of people. Young patients with symptoms of neurologic and mental impairment, it is important to consider nitrous oxide abuse despite a negative urine drug screen. Often, vitamin B12 levels can be normal. In these cases, levels of homocysteine and methylmalonic acid should be checked. MRI is the most sensitive radiologic modality to confirm subacute combined degeneration. Prompt cessation of nitrous oxide use plus high dose vitamin B12 supplementation is required to prevent irreversible neurological deficits.
99
ABSTRACT #59 QUALITY IMPROVEMENT GENERAL INTERNAL MEDICINE
IMPROVING RESIDENT CONTINUITY OF CARE AT AN URBAN FEDERALLY QUALIFIED HEALTH CENTER
Salvador Caceros1 , Sharel
Sadud-Armaza
1 , Errol Morras1 , Bailey Perry1 , Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Will be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Aurora, Colorado, United States from May 10-13, 2023.
BACKGROUND/INTRODUCTION: Continuity of care has been shown to increase patient satisfaction and trust, improve health outcomes, and reduce healthcare costs. However, our resident-based practice faces challenges in improving continuity of care due to the variability of resident schedules (X+Y schedule system), frequent resident turnover, and lack of standardized scheduling workflows. A resident pre-intervention survey (n=30) indicated that, while all participants considered continuity of care essential for their patients, 86.7% perceived that more than half (>50%) of their patients were unknown to them.
METHODS: To improve provider continuity, beginning in July 2022, we designed and implemented a standardized primary care giver algorithm to assign patients to their resident providers in the electronic medical record. In December 2022, we identified on-site scheduling workflow gaps and established priority areas for future interventions including; a focus on individual patient-physician continuity, an overbooking protocol, and proper documentation of follow-up instructions in progress notes.
Our main outcome will be the continuity of care Index measured at 0, 6, and 12 months among all adult patients seen by resident physicians. Process measures include; the percent of primary care giver assignment accuracy and appropriate documentation of follow-up instructions in the progress note. The impact of our interventions on resident perceptions of continuity will be assessed through post-intervention surveys.
RESULTS: Between July 2022 and December 2022, continuity of care index increased from 0.50 to 0.64 among adult patients seen by resident physicians. Accuracy of primary care giver assignments improved from 80% to 93% between December 2021 and October 2022, representing a 13% rise compared to the previous year. Upon review of scheduling data, the inclusion of a provider name in the follow-up section of the last encounter note improved continuity compared to no name listed (31% versus 13%).
CONCLUSION: Data to date suggests that implementing a provider assignment algorithm and standardizing scheduling procedures can improve continuity of care at a Federally Qualified Health Center (FQHC)-based residency practice. Challenges include accounting for patients who require short-term follow up, patient-based barriers to scheduling in advance, and standardizing practices at our centralized call center. Future directions include assessing patient perception regarding continuity of care and stratifying data by self-identified race/ethnicity to ensure we are not furthering scheduling disparities.
100
ABSTRACT #60 QUALITY IMPROVEMENT GASTROENTEROLOGY/INFECTIOUS DISEASES
INCREASING HEPATITIS C VIRUS SCREENING ACROSS INNER CITY COMMUNITY CLINICS
Mantej Sehmbhi1 , Emily S. Seltzer1, Nour Al Khalili1 , Shabari Shenoy1 , Patricia Miguez Arosemena1 , Geeta Varghese1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Hepatitis C virus (HCV) infection is a chronic infection in the majority of patients, with important sequelae including hepatic fibrosis, cirrhosis, and the development of hepatocellular carcinoma (HCC). HCV treatments are effective at reducing cirrhosis and HCC rates, but an estimated 51% of those infected with HCV are not aware of the diagnosis. The United States Preventive Services Task force (USPSTF) changed its HCV screening guidelines in 2020 to expand eligibility for screening to all those aged 18 to 79 years. We conducted a quality improvement project at three federally-funded primary care clinic sites in New York City, to raise awareness of the change in USPSTF guidelines and to improve screening rates in the adult population.
METHODS: We utilized the Plan-Do-Study-Act (PDSA) quality improvement methodology for this project. We gathered pre-intervention data on which patients had a HCV screening antibody test logged in the electronic medical record, stratified by clinic site. Surveys were sent out to residents to assess awareness of HCV presentation, treatment and screening guidelines. We deployed tailored interventions aimed at increasing awareness amongst both providers and patients at each site, including regular educational sessions for staff, informational posters in waiting areas, and reminders in consultation rooms. We then gathered post-intervention data at 3 and 6 months to examine the changes in HCV screening rates.
RESULTS: Prior to our interventions, we found that HCV screening rates were moderate at all sites: 51% of adults at Clinic 1, 44% of adults at Clinic 2, and 58.5% of adults at Clinic 3 had at least one HCV antibody screen on record as of July 2021. Of those who completed the pre-intervention survey, 55% of residents were not aware of the recent changes in USPSTF guidelines. We planned and implemented the interventions described above throughout the six-month period from August 2021 to January 2022. Our interventions were effective at achieving modest increases in screening rates at all sites. By February 2022, screening rates had increased to 56% at Clinic 1, 49% at Clinic 2 and 60% at Clinic 3.
CONCLUSION: Raising awareness about HCV screening guidelines amongst providers and patients was moderately effective at increasing screening rates at three primary care sites serving primarily underinsured patients in New York City. We are executing further PDSA cycles to continue to improve screening rates.
101
ABSTRACT #61 QUALITY IMPROVEMENT GASTROENTEROLOGY
PRODUCING PAINLESS PEG CONSULTS: A PILOT QUALITY OF CARE STUDY TO IMPROVE PERCUTANEOUS ENDOSCOPIC GASTROSTOMY TUBE PLACEMENT WORKFLOW AND OUTCOMES
Emily S. Seltzer1 , Erica Park1,2 , Patricia Miguez Arosemena1 , Omar Belfaqeeh1 , Michael S. Smith1 , Janet M. Shapiro1 , Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023.
BACKGROUND/INTRODUCTION: Appropriate utilization of percutaneous endoscopic gastrostomy (PEG) tubes requires careful evaluation of the patient by both the primary medical/surgical team and the endoscopic consultants Failure to appropriately select and evaluate patients prior to PEG consults may result in increased length of stay, procedure complications, and even mortality. The aim of this study was to develop a standardized workflow for appropriate consultation; we present initial results here.
METHODS: Implementation of a standardized pathway was completed in two phases from 8/1/22 to 10/31/22. The first part involved a comprehensive lecture on PEG tubes given to medicine residents and advanced practice providers. Covered topics included appropriate indications and contraindications, pre-procedure optimization, placement technique, and associated procedure risks. The second phase included rollout of a novel PEG-related checklist in the electronic medical record for primary teams to use before calling a PEG consult (Figure 1). The primary outcome measured was time between initial consult and PEG tube placement. Secondary outcomes included patient length of stay (LOS), 30-day complication rate after PEG, and 30-day mortality. Outcomes were compared to the pre-intervention period from 6/1/21 to 7/31/22 using descriptive statistics.
RESULTS: One hundred and seventy patients (144 pre- and 26 post-intervention) had PEG tubes placed during the two study periods (Table). Time between initial consult and PEG placement was 5.2 ± 6.2 days in the preintervention group, compared to 5.1 ± 5.3 days in the post-intervention group. LOS was 56 ± 63.28 days in the pre-intervention group compared to 47.8 ± 22.91 days in the post-intervention group. The post-procedure complication rate was lower in the post-intervention group compared to the pre-intervention group (15.4% versus 27.1%), as was the 30-day mortality rate (11.8% pre-intervention versus 11.5% post-intervention). Inpatient medicine teams used the checklist in 85% of the post-intervention cases compared to 45% among non-medicine teams.
CONCLUSION: These data suggest that implementation of PEG-related interventions including provider education and a standardized pre-procedure checklist facilitates shorter waiting times between consult to PEG placement and LOS, as well as decreased rates of 30-day post-PEG complications and mortality. This may be due to more appropriate patient selection and improved pre-procedure patient optimization. While this pilot study is limited by the small sample size of the post-intervention group, ongoing analysis hopefully will confirm if not strengthen these promising initial results.
102
Figure 1: Pre-percutaneous endoscopic gastrostomy (PEG) Checklist Pre-PEG Checklist:
A. Goals of Care/Ethical Concerns:
1. Has this patient been evaluated by the nutrition team and recommended for alternative means of nutrition? (Yes/No)
2. Has this patient been evaluated by the speech and language pathologist and are they being recommended for alternative means of nutrition? (Yes/No)
3. Who consents for the patient? (The Patient, Health Care Proxy/Surrogate, Two-Physician Consent)
4. What is the indication for PEG Tube? (Neurologic Dysphagia, Mechanical Obstruction, Acute/Chronic Disease Generating Catabolic State, Advanced Dementia, Pulmonary Aspiration Risk, Anoxic Brain Injury, Other)
B.Infection/Antibiotics Concerns:
1. Is there an active infection? (Yes/No)
i.If yes, what type of infection? (Bacteremia, Skin/Wound/Osteomyelitis, Peritonitis/Intrabdominal Infection, Other Gastrointestinal Related, Pneumonia/Respiratory Related Infection, Urinary Tract Infection) *
2. Are there any signs of sepsis currently? (Yes/No)
3. Has there been increasing oxygen requirements over the last 24 hours? (Yes/No)
4. Is the patient on antibiotics? (Yes/No)
If yes,
i. For what length of time?
ii. Is it for a known infection (as stated above), empiric treatment or prophylaxis?
C.Anticoagulation (AC)/Coagulopathies:
1. Is the patient currently on anticoagulation or anti-platelet therapy? (Yes/No)
If yes,
i. Can it be held safely for the procedure? (Yes/No)
ii.Which medication are they on?
iii.Have they been held for an adequate amount of time? **
2. Does the patient have any known coagulopathy? (Yes/No)
i.Is the INR < 1.5? (Yes/No)
ii.Are platelets reliably above 50,000? (Yes, No)
D.Critical Care Specific:
1. Is the patient pending tracheostomy placement? (Yes, No) ***
i. If yes, what is the date they are scheduled for?)
2. Is the patient currently on vasopressors/inotropes? (Yes, No) ****
* It is understood that every situation is unique, and patients/caregivers should understand what to expect in terms of recovery of current condition after PEG tube placement
** If possible, start holding AC appropriately prior to consulting GI, for possibility that PEG can occur in an expedited manner. For further information regarding duration to hold please see 2016 ASGE Guidelines. If there are questions regarding whether it is safe to hold AC in the patient, please consider reaching out to the cardiology/neurology team especially if patient had a recent acute coronary syndrome or stroke event or had stent placement within 12 months. *** Please note at our institution, typically PEG tubes are placed after tracheostomy is done if it is something that is needed in the patient
**** Please note at our institution PEGs are not routinely placed while a patient is on pressors (other than midodrine)
103
Table 1: Initial Data Pre- and Post-Intervention Pre-Intervention Post-Intervention N Characteristics N(%)/Mean(SD) 144 26 Days Between Initial PEG Consults and PEG Tube Placement 5.17 (± 6.20) 5.08 (± 5.30) Length of Stay 56.06 (± 63.28) 47.81 (± 22.91) 30-day Post-PEG Complications 29 (21.14) 4 (15.38) 30-Day Mortality 17 (11.81) 3 (11.54) Utilization of the Pre-Consult PEG Checklist N/A 18(69.23) Among Medicine Service Consults N/A 13(86.67) Among Non-Medicine Service Consults N/A 5 (45.45) 104
ABSTRACT #62
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES/NEPHROLOGY
VALACYCLOVIR ASSOCIATED NEUROTOXICITY IN A PATIENT WITH END STAGE RENAL DISEASE
Venus Sharma1 , Rohit Rajesh Nathani1 , Ayush Gandhi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Valacyclovir is a commonly used drug for the treatment of herpes zoster infections. Valacyclovir-associated neurotoxicity is a rare complication of valacyclovir treatment, especially in patients with end-stage renal disease (ESRD), if not renally dosed. Its presentation can be varied, including confusion, altered mental status, agitation, and dysarthria.
CASE PRESENTATION: The patient was 40-year-old transgender female patient who was brought to the Emergency Department by paramedics after being found behaving erratically. History was limited due to encephalopathy. Prior medical records revealed that the patient had ESRD and was undergoing hemodialysis (HD), with a missed session two days ago. On examination, she was noted to be hypertensive to 202/113 mmHg with otherwise stable vital signs. She was agitated and had slurred speech without any other localizing neurological signs. She was found to have scabbed superficial vesicular skin lesions on the left upper thoracic area. Computed Tomography (CT) scan of the head showed a small left subarachnoid hemorrhage (SAH). The patient was placed on a nicardipine drip in the Intensive Care Unit. The SAH was managed conservatively, and a repeat CT head showed a stable SAH. Despite improved blood pressure and stable SAH, the patient’s mental status deteriorated, with worsening agitation and hallucinations. A broad encephalopathy workup was performed which was unremarkable including a normal complete blood count, thyroid stimulating hormone, vitamin B1, B6, B12 levels, syphilis, human immunodeficiency virus, and blood toxicology screen. She was noted to have a blood urea nitrogen of 48, creatinine of 8. Aroutine electroencephalogram showed frequent left centro-parietal slowing and occasional sharp wave discharges. A subsequent magnetic resonance imaging (MRI) of the brain showed an interval decrease in size of the SAH but was otherwise unremarkable. Cerebrospinal fluid (CSF) was positive for varicella zoster virus (VZV). On medication reconciliation, it was discovered that the patient was recently prescribed valacyclovir 1 gram three times a day (non-renally adjusted dose) at an urgent care center. She had a rapid improvement in her symptoms with complete return to baseline in a few days after HD. Given the broadly negative workup and the rapid improvement after HD, a diagnosis of valacyclovir-associated neurotoxicity was made.
CONCLUSION: It is very challenging to differentiate VZV encephalopathy from valacyclovir-associated neurotoxicity clinically Valacylcovir-associated neurotoxicty will worsen if the medication is continued whereas VZV encephalopathy will improve. Dysarthria and visual hallucinations point more towards neurotoxicity. In order to assist diagnosis, MRI and CSF analysis are needed However, valacyclovir should be discontinued even in the presence of CSF PCR positive for VZV if the suspicion is high for valacyclovirassociated neurotoxicity in presence of ESRD.

105
Figure 1: Computed Tomography (CT) of the head with small left subarachnoid hemorrhage
ABSTRACT #63
CLINICAL RESEARCH
GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
TRENDS IN SCREENING AND PREVENTION OF ANORECTAL AND COLON CANCER IN TRANSGENDER PEOPLE
Shabari Mangalore Shenoy1, Shanique Wilson Noack1,2, Emily Seltzer1, Omar Belfaqeeh1, Patricia Miguez Arosemena1, Emilia Bagiella3, Amreen Dinani3, Ilan Weisberg2, Joshua D. Safer3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Cancer screening rates overall are lower among transgender people compared to cisgender people. Individual barriers to cancer screening include factors such as gender identity, gender expression, socioeconomic status, race/ethnicity along with provider-specific barriers including perceived lack of cultural sensitivity. In addition, the lack of screening guidelines specific to transgender people may contribute to decreased screening rates. The aim of our study was to describe the rates of colorectal cancer and anal cancer screening in transgender people. Rates of human papilloma (HPV) vaccination were also assessed. Factors contributing to reduced screening rates such as gender affirming medical and/or surgical treatment, insurance status and race/ethnicity were assessed.
METHODS: A retrospective chart review was performed, including 769 transgender people over 50 years of age between January 2017 and January 2022 at a large academic medical center with expertise in transgender medicine in New York City. Individuals with a personal history of colon cancer were excluded. Information on demographic data, gender identity, gender expression, treatment(s), and insurance status were recorded. Colon cancer screening, anal pap smear rates and HPV vaccination status were recorded. A descriptive analysis, covariate analysis calculated by ANOVA and chi-square testing for numerical and categorical variates were performed.
RESULTS: Colorectal cancer screening was offered to under half of the study population (358/769, 46.6%) (Table 1). Of those offered evaluation, only 272 (35.5%) completed a screening test, a value significantly lower than the New York State general population screening rate (72%). The average age of individuals offered colorectal cancer screening was 54.5 years (SD, range +/- 6.8 years). HPV vaccination rate was 1%. One in ten (10.6%) individuals had a history of anal pap smears, of whom 7.4% had abnormal results. Family history of colon cancer and having health insurance was associated with increased colorectal cancer screening (p<0.001). Whereas social determinants of health such as financial resource strain and food/housing insecurity were associated with reduced screening (p<0.001) (Table 2). No correlation between gender affirming medical and/or surgical treatment and colorectal cancer screening rates was found.
CONCLUSION: Colorectal cancer screening among transgender people is profoundly lower than the general population. Several factors were identified that could potentially contribute to decreased screening rates. There is a need to develop comprehensive initiatives aimed at increasing awareness and screening for colorectal cancer for transgender people.
106
Table 1: Demographic data including gender identity and sexual orientation
n (%) Age 58 (SD, range +/- 7) Sex recorded on birth certificate Male 625 (81.3) Female 144 (18.7) Race White 343 (44.6) African-American 136 (17.7) Asian 0 (0) American Indian/Alaskan native 1 (0.13) Native Hawaiian 0 (0) Other 190 (24.7) Unknown 99 (12.8) Gender identity Male 125 (16.2) Female 612 (79.5) Non binary 17 (2.2) Gender non-confirming 5 (0.6) Other 6 (0.7) Unknown 4 (0.5) Sexual Orientation Straight 259 (33.6) Lesbian/Gay 105 (13.6) Bisexual 57 (7.4) Queer 23 (3.0) Don’t know 45 (5.8) Unknown 280 (36.4) 107
Table 2: Descriptive and co-variate analysis performed identifying factors contributing to screening rates
N (%) CRC screening offered (>50years) 358 (46.5) CRC Screening completed (>50 years) 272 (35.5) CRC screening performed Yes (%) No (%) p-value Age at which CRC first offered 54.1 55.9 0.037 Family history <0.001 Yes 32 (11.7) 14 (2.8) No 240 (88.2) 480 (97.1) Insurance Status <0.001 Medicaid 81 (29.7) 147 (29.8) Medicare 76 (27.9) 85 (17.2) Commercial 108 (39.7) 222 (45.0) Uninsured/selfpay 7 (2.5) 39 (7.9) Social determinants of health index <0.001 Yes 97 (35.9) 111 (22.6) No 173 (64.0) 380 (77.4) Gender affirming treatment Medical 96 (35.29) 188 (38) 0.449 Surgical 6 (2.21) 9 (1.82) 0.714 Medical + surgical 159 (58.4) 281 (56.8) 0.673 108
ABSTRACT #64
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE ENDOCRINOLOGY/HEMATOLOGY/ONCOLOGY
A RARE CASE OF A MIDDLE MEDIASTINAL NEUROENDOCRINE TUMOR
Connor Smith1, Galit Balayla Rosemberg1, Krystle Hernandez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Neuroendocrine neoplasms (NENs) are a rare group of heterogeneous malignancies that arise from neuroendocrine cells and are known to have rapid disease progression. Recently, the World Health Organization (WHO) re-classified NENs into well-differentiated neuroendocrine tumors (NETs) and poorly differentiated neuroendocrine carcinomas (NECs) for a better understanding of the disease. Mediastinal NENs, initially classified as thymic carcinomas, were assigned to a new category of thymic tumors in the 2015 WHO classification. The incidence of NENs increased to 6.98/100,000 in 2012 while mediastinal NENs have an annual incidence of only 0.02 per 100,000 accounting for 2–5% of all anterior mediastinal neoplasms making it an even more unfamiliar disease. NENs often times present with nonspecific symptoms that can delay diagnosis and treatment.
CASE PRESENTATION: We present a 59-year-old female who presented to the hospital with one month of nausea, vomiting and poor oral intake with a 50 lb. involuntary weight loss. She denied dysphagia and odynophagia. She was hemodynamically stable with a benign physical exam. Computed tomography (CT) of the abdomen and pelvis revealed bilateral heterogeneously enhancing adrenal lesions. Follow up CT of the chest revealed a 10 x 6.5 x 9.4 cm middle mediastinal mass with mass effect on mainstem bronchi bilaterally. Bronchoscopy revealed extrinsic compression of bilateral mainstem bronchi with >75% airway lumen compression. Biopsies were sent. The patient was discharged on day 6 of initial admission with close follow up with Pulmonology, Hematology/Oncology, and Gastroenterology clinics pending pathology results. Two days later, she presented to the hospital once again with continued nausea/vomiting and shortness of breath. CT of the chest showed re-demonstration of the mediastinal mass but no acute findings. Given her respiratory distress and concern for complete obstruction of the bronchi, she was transferred to the Intensive Care Unit (ICU) for advanced bronchoscopic rigid stent placement to the mainstem bronchi bilaterally. Her hypoxia initially improved substantially after stenting. On Day 5 of this second hospitalization, she was found to be hypoxic with copious secretions and was intubated. Respiratory cultures grew methicillin-sensitive Staphylococcus aureus and broad spectrum antibiotics were started. Cytology revealed poorly differentiated carcinoma with tumor cells positive for synaptophysin. Oncology recommended initiating carboplatin and etoposide. On Day 19, she had profound decompensation of mental status and CT head revealed multiple hemorrhagic metastatic lesions. On Day 24, she unfortunately expired from respiratory failure secondary to her tumor burden and brain metastases.
CONCLUSION: Neuroendocrine neoplasms are a rare type of malignancy with high morbidity and mortality. They are often misdiagnosed due to being both rare and nonspecific in their presentation. Nonetheless, a higher incidence of NENs has been reported in recent years, in correlation with better screening methods for detecting tumors in their most common target tissues, such as the gastrointestinal tract. NENs found in the mediastinum are uncommon, with thymomas accounting for only 0.4% of NENs. This makes early recognition and management particularly challenging for physicians. There are currently only a small handful of cases reporting carcinoid tumors of the middle mediastinum. Contrary to NENs of more typical sites such as the GI tract or lungs, mediastinal NENs are characterized by highly aggressive local invasion as well as distant metastasis. As seen in this case, most mediastinal NENs remain asymptomatic for a long period and frequently grow to a size difficult to treat before they are discovered. As such, they typically have poor prognoses, although one case report demonstrated a good response to surgical resection. The cytology of the tumor in this case indicated a good response to chemotherapy but unfortunately, the disease progressed before a response could be seen. Overall, this case demonstrates the need for further epidemiological study into the screening, diagnosis, and treatment of these aggressive tumors to prevent patient mortality.
109
ABSTRACT #65
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES/RHEUMATOLOGY
CONCOMITANT GOUTY AND GONOCOCCAL POLYARTHRITIS IN A TRAVELER
Anne Socorro Corrales1, Yousef Ali1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Gout [monosodium urate (MSU) crystal deposition disease] is characterized biochemically by extracellular fluid urate saturation. The clinical manifestations of gout may include recurrent flares of inflammatory arthritis, chronic arthropathy and tophaceous deposits. The possibility of disseminated gonococcal infection should be considered in sexually active individuals who present with arthralgias or joint pain concerning for septic arthritis. We present a rare case of concomitant flare of gout and gonococcal arthritis in a recent traveler.
CASE PRESENTATION: The patient is a 43-year-old male with history of gout and alcohol use disorder who presented to the emergency room with pain in multiple joints for four days. The pain started in his left first metatarsophalangeal (MTP) joint on day one, then spreading to multiple MTP joints bilaterally, ankles, knees, and elbows. It was accompanied by burning sensation over joints and it worsened with movement. It was described as moderate to severe and caused subjective, progressive weakness in lower and upper extremities to the point that he was unable to stand up by himself. He had self-medicated with Ibuprofen and Colchicine without achieving any improvement. He had returned from Mexico 6 days before his presentation. On review of systems, he endorsed having non-bloody, watery diarrhea for 3 days after returning from his trip. He denied having had fever, chills, abdominal pain, nausea, or vomiting.
Physical examination revealed synovitis of his right ankle, both knees, wrists, and right elbow. He also had an erythematous, macular, blanching rash over the dorsum of his hands and feet. No palms were spared. No tophi were seen. Initial laboratory tests showed mild thrombocytopenia and liver injury. Erythro-sedimentation rate (ESR) and C-reactive protein (CRP) were elevated. Uric acid levels were normal. Serologies for Lyme disease, Human Immunodeficiency Virus (HIV), Zika, Dengue, and Chikungunya virus were negative. Blood cultures, as well as Chlamydia/Neisseria Gonorrhea nucleic acid amplification tests (NAA) in urine were negative. A battery of myositis-specific antibodies was negative. A left knee arthrocentesis was performed. Analysis of synovial fluid showed 60,300 white blood cells per milliliter. Needle-shaped crystals with negative birefringence were seen under the light microscope.
The patient was diagnosed with a flare of gout affecting multiple joints and was treated with oral corticosteroids that resulted in a dramatic improvement of his symptoms. He was discharged home on day 8. After his discharge, the team was notified that his synovial fluid cultures were growing Neisseria gonorrhea. A diagnosis of polyarthritis-dermatitis syndrome due to gonococcal infection co-existing with a flare of gouty arthritis was made. The patient was contacted, and a shared decision was made to pursue appropriate antibiotic therapy in the outpatient setting.
DISCUSSION: The association between inflammatory arthritis and septic arthritis has been well described in the literature, especially for rheumatoid arthritis. Concomitant gout and septic arthritis have also been described. In a prior study (K.H. Yu, et al. Rheumatology, 2003), thirty cases of concomitant gout and septic arthritis are described. Causative organisms identified included Staphylococcus, Streptococcus, and Gram-negative bacilli. In another study by C. H. Lee and colleagues, 43.5% of 29 patients diagnosed with septic arthritis of the ankle also had gout arthritis. In none of the cases included in these two studies, did synovial cultures or NAA tests identify Neisseria gonorrhea
110
A gout flare is typically monoarticular and intensely inflammatory, occurring in the lower extremities. A polyarticular pattern is the initial manifestation in less than 20% of patients with gout, but occurs with increasing frequency in later flares. Polyarticular symptoms are particularly common late in untreated gout, when multiple recurrences, short or absent symptom-free intervals, and palpable tophaceous deposits are common.
Patients with disseminated gonococcal infection typically present with abrupt onset of mono or oligo-arthritis, with pain and swelling in one or more joints. Gonococcal arthritis involves distal joints, with knees, wrists, and ankles the most involved joints.
Concomitant gout and gonococcal arthritis have been reported but seems to be extremely rare. For instance, Smith E. L., et al reported two cases in recent travelers from the Philippines. Both patients reported unhealthy alcohol use and unprotected sex prior to the diagnosis. Interestingly, these cases had more severe manifestations with soft tissue abscesses and severe purulent arthritis that required multiple washouts and prolonged intravenous antibiotics. Another solitary case was reported in The Lancet Infectious Diseases by Tze Shien Lo, et al. This latter patient had a course like our patient, with his symptoms rapidly improving after receiving treatment with corticosteroids and a 7-day course of Ceftriaxone.
CONCLUSION: In conclusion, disseminated gonococcal infection can occur with polyarticular gout and delays in recognition and treatment, can lead to severe disease from both. Including disseminated gonococcal infection in the differential diagnosis of polyarticular gout is important.
111
ABSTRACT #66
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE ENDOCRINOLOGY
GLUCOCORTICOID THERAPY FOR MANAGEMENT OF HYPOGLYCEMIA IN THE CONTEXT OF NON-ISLET CELL TUMOR-INDUCED HYPOGLYCEMIA
Rahul Agarwal1 , Susel Rodriguez Ortega1 , Juan Vasquez Mendez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Endocrine Society Annual Meeting that was held in Atlanta, Georgia, United States from June 11-14, 2022.
BACKGROUND/INTRODUCTION: Non-islet cell tumor-induced hypoglycemia is a rare paraneoplastic syndrome which can cause recurrent hypoglycemia. There is no clear standard of care for management of hypoglycemia. Often, these patients have high morbidity, therefore, surgical tumor resection is not always possible.
CASE PRESENTATION: This is the case of a 69-year-old male presenting with altered mental status in the context of hypoglycemia without clear etiology with an initial serum glucose level of 32 mg/dL (normal range 60100 mg/dL) which quickly corrected after administration of intravenous glucose. He was found to have a large bowel obstruction with Computed Tomography (CT) abdomen revealing an underlying neoplasm. Biopsy of suspected lesion on colonoscopy revealed colorectal adenocarcinoma. Repeated episodes of hypoglycemia complicated by seizures required inpatient management.
Workup included serum insulin level which was suppressed (<1.0 uU/mL, normal range 1.9-23.0 uU/mL), low cpeptide level (0.1 ng/mL, normal range 1.1-4.4 ng/mL), low beta hydroxybutyrate level (0.07 mmol/L, normal level <0.3 mmol/L), cortisol level of 43.7 mcg/dL, undetectable insulin like growth factor-1 (IGF-1) level (<10 ng/mL, normal range 59-230 ng/mL) and low insulin like growth factor-2 (IGF-2) level (66 ng/mL, normal range 333 - 967 ng/mL). IGF2:IGF1 ratio was 66 (ratio >10 is indicative for diagnosis of non-islet cell tumor hypoglycemia).
Due to extremely poor oral intake and recurrent episodes of hypoglycemia despite continuous dextrose infusion, the patient was started on prednisone 20 mg daily. Eventually, intravenous methylprednisolone (40 mg) in addition to dextrose infusion was needed as maintenance therapy effectively preventing hypoglycemia. Given his poor functional status, the Surgical and Oncology team decided he was no longer a surgical or chemotherapy candidate. Eventually, Palliative Medicine was consulted and the patient was transitioned to comfort care with a plan for outpatient hospice.
CONCLUSION: Non-islet cell tumor-induced hypoglycemia should be suspected in any patient with hypoglycemia without clear etiology, especially if there is a known malignancy or newly diagnosed mass. Once non-islet cell tumor-induced hypoglycemia is identified and a primary tumor is found, complete tumor resection represents ideal management, however, it is not always attainable. In such cases, dextrose infusion might be insufficient to prevent hypoglycemia and is not always the preferred option given the required long-term venous access. In these circumstances, early high dose glucocorticoids are safe and appear to successfully prevent hypoglycemic events.
112
ABSTRACT #67 CLINICAL RESEARCH INFECTIOUS DISEASE
COMPARISON OF CHARACTERISTICS OF VACCINATED VERSUS UNVACCINATED PATIENTS ADMITTED WITH COVID-19 IN THE MOUNT SINAI HEALTH SYSTEM
Vani George1, Chi Doan Huynh2, Jordan Ehni1, Kristine Rabii1, Alan Weinberg1 , Aarohi Vora3 , Marie Moss1 , Waleed Javaid1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Ryan Health, New York, NY, United States; 3Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: In 7/2021, there was a spike of COVID-19 cases due to the B.1.617.2 Delta variant in New York City (NYC). By mid-December, the B.1.1.529 Omicron variant surpassed the Delta variant. The focus of this research was to investigate whether vaccination played a role in the clinical outcomes of patients hospitalized with COVID-19 in the Mount Sinai Health System (MSHS) in NYC between 7/2021 through 12/2021. Specifically, we examined the demographic and clinical characteristics of vaccinated and unvaccinated patients admitted with COVID-19 and associations with the outcomes of length of hospital stay (LOS), time spent in intensive care unit (ICU days),and in-hospital mortality.
METHODS: We conducted a retrospective study of all COVID-19 admissions from 7/1/2021 to 12/31/2021 in six MSHS hospitals. Demographic and clinical data such as age, sex, race/ethnicity, zip code, insurance provider, and comorbidities were obtained through hospital billing systems (TSI, ePSI) for all patients admitted and discharged with a primary or secondary diagnosis of COVID-19 based on ICD code UO7.1. The billing system was used to obtain the three primary outcomes studied: LOS, ICU days, and in-hospital mortality. Vaccination data was obtained from reviewing the electronic medical record (EMR) and manual reconciliation of vaccination status through review of the New York State Immunization Information System (NYSIIS) for patients vaccinated outside MSHS. Inclusion criteria was defined to include all patients ≥18 years of age admitted with COVID-19 diagnosis or positive COVID-19 PCR test result from 7/1/2021 to 12/31/2021. Patients were excluded if they had an unknown vaccination status or were vaccinated with non-FDA approved vaccines. Patients who were unvaccinated with documentation of unvaccinated status were included in the study. Patients who had received ≥1 dose of any authorized COVID-19 vaccine were considered vaccinated. Fully vaccinated patients were those who had received either two doses of the Moderna or Pfizer vaccine or one dose of the Jannsen vaccine prior to the date of admission. Patients who had received a booster dose of either the Moderna or Pfizer vaccine after the primary vaccination series were boosted patients. Partially vaccinated patients had received only one dose of the Moderna or Pfizer vaccine at the time of admission. Unvaccinated patients had received no vaccine at the time of their admission.
RESULTS: We identified 1472 hospitalized patients with COVID-19, of whom 548 (37.2%) were fully vaccinated, 72 (4.9%) were partially vaccinated, and 71 (4.8%) patients were fully vaccinated and had received a booster dose. A total of 781 (53.1%) patients were unvaccinated. The mean number of ICU LOS was 8.9 days in the fully vaccinated group versus 15.5 days in the unvaccinated group. Mortality was higher in unvaccinated patients versus fully vaccinated patients with an odds ratio of 1.9 (95%CI, 1.27 to 2.68; p=0.0009).
CONCLUSION: COVID-19 vaccination was associated with significant decreases in the length of hospital stay, ICU stay, and in-hospital mortality in hospitalized patients with positive SARS-COV-2 in a major NYC health system from 7/2021-12/2021. Comorbidities including liver disease, BMI >30, chronic kidney disease, and cardiovascular disease were associated with higher in-hospital mortality for all patients admitted with COVID-19. Vaccination against COVID-19 should continue to be emphasized as an important preventive intervention people, health care systems and jurisdictions can implement to prevent severe disease, prolonged hospitalization and death.
113
ABSTRACT #68
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
BURKITT LYMPHOMA INDUCED PSEUDOACHALASIA WITH DRAMATIC SYMPTOMATIC IMPROVEMENT POST-CHEMOTHERAPY
Marni H. Wilkoff1 , Emily S. Seltzer1 , Allison E. Wang1,2 , Bruno Almeida Costa1 , Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
INTRODUCTION: Primary achalasia is due to loss of inhibitory neurons leading to poor relaxation of the lower esophageal sphincter and abnormal peristalsis. In pseudo-achalasia, a similar radiographic pattern derives from a secondary etiology, most commonly a gastroesophageal junction (GEJ) adenocarcinoma, though cases of lymphoma-induced pseudo-achalasia have been reported. Here we present the second known case of Burkitt lymphoma (BL)-induced pseudo-achalasia.
CASE PRESENTATION: A 45-year-old female with a history of scleroderma, hypertension, gastroesophageal reflux disease, and prior H. pylori infection presented to the Emergency Department for 15 episodes of diarrhea associated with fecal urgency, one episode of melena, poor oral intake due to decreased appetite, lightheadedness, and weakness. She denied fever, chills, weight loss, sick contacts, or bleeding from other sites. Initial labs were notable for microcytic anemia (hemoglobin 5.5 g/dL from an unknown baseline) and thrombocytopenia (platelet count of 28 K/uL). Upper endoscopy revealed a large, fungating, and ulcerated mass with spontaneous oozing in the cardia, fundus, and body of the stomach (Figure 1). Histology was consistent with BL (CD20, CD10, MYC and BCL6 positive; Ki67 index 95%).
Upon discharge, the patient followed up with Oncology, but her scheduled positron emission tomography scan was delayed because of a readmission for a seizure. The patient was discharged and re-hospitalized 7 days later for four days of vomiting and acute dysphagia to both solids and liquids. She reported associated symptoms of substernal globus sensation, food regurgitation within 2 minutes of consumption, and a 28lb unintentional weight loss in one month. Barium esophagram demonstrated an aperistaltic esophagus with marked narrowing at the GEJ mimicking achalasia (Figure 2). Given the rapidly progressive and obstructive nature of the tumor, chemotherapy with rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (REPOCH) was promptly initiated. Prior to chemotherapy, the patient was only able to tolerate a pureed diet, but upon completion of the first cycle of R-EPOCH, she was tolerating a regular diet.
CONCLUSION: Accurate diagnosis and treatment of pseudo-achalasia is crucial for both symptomatic relief and patient survival. While adenocarcinomas of the GEJ or cardia are the predominant types of underlying cancer, lymphoma-induced pseudo-achalasia is also well-recognized. Low-grade B-cell lymphomas account for most cases, and aggressive histologic subtypes have been rarely reported. To the best of our knowledge, this is the second case of BL-induced pseudo-achalasia reported in the literature. This case highlights the importance of accurate diagnosis and prompt treatment of BL-induced pseudo-achalasia, with R-EPOCH being an effective regimen for inducing rapid and deep responses.
114





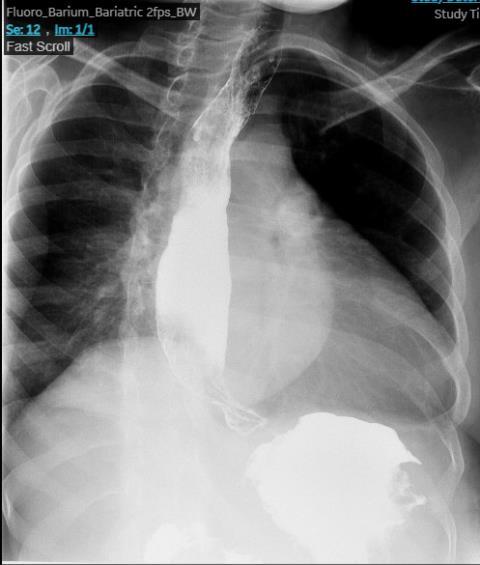
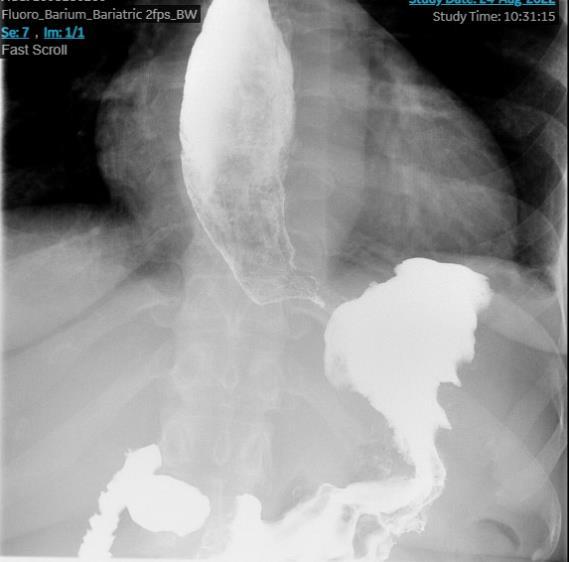 Figure 1: Upper endoscopy revealing a large, fungating mass in the lower third of the esophagus (A), gastric cardia (B), gastric body (C) and gastric fundus (D)
Figure 1: Upper endoscopy revealing a large, fungating mass in the lower third of the esophagus (A), gastric cardia (B), gastric body (C) and gastric fundus (D)
A B C D 115
Figure 2: Barium esophagram demonstrating an aperistaltic esophagus with marked narrowing of the gastroesophageal junction
ABSTRACT #68
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GENERAL INTERNAL MEDICINE
CANNABIS TOXICITY FROM STREET PERCOCET TREATED WITH NALOXONE
Eelin Wilson1 , Mohammed Khan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Over the past two decades, in the United States, driven by the legalization of cannabis use, cannabis use has doubled to approximately 10% of the adult population. Consequently, patients presenting to the emergency department (ED) with cannabis toxicity have become more prevalent The symptoms of acute cannabis toxicity are tachycardia, respiratory depression, and CNS depression. Cannabis may also cause pupillary constriction While the opioid receptor antagonist naloxone is administered to patients with suspected opioid overdose exhibiting hypoventilation and somnolence, there is currently no specific antidote for cannabis toxicity. We present a case of a young male with acute toxicity after unintentional cannabis use who was successfully treated in the field with naloxone injection.
CASE PRESENTATION: The patient is a 27 year-old man was brought in by ambulance, called by his girlfriend for encephalopathy, pinpoint pupils, and shallow breathing. The patient reported that he usually takes three oxycodone/acetaminophen (Percocet®) tablets per day for his headaches and had ran out of his medication. He bought one pill from the street which he was told was “Percocet® ” It was his first time taking street drugs. He lost consciousness for less than a minute, then awakened with encephalopathy and pinpoint pupils, and slow shallow breathing. He was found by first-responders to be tachycardic and hypoxic with oxygen saturation in the 70s and given a total of 3 mg naloxone injection in the field. In the ED he was awake, oriented but drowsy, with normal breathing rate with no respiratory distress. Initial vital signs were: blood pressure 124/78 mmHg, pulse rate 129 beats/min, respiratory rate 15 breaths/min, and pulse oximetry (SaO2) 92% on 6 liters nasal cannula. Rapid blood glucose was 183 mg/dL. The patient reported alcohol socially, smokes marijuana occasionally, and denied any other illicit drug use. He denied smoking tobacco. A single-view chest radiograph suggested pneumonia. Laboratory testing revealed an elevated white blood count of 21 K/uL, and normal basic metabolic panel. Venous blood gas drawn while the patient was on 6 L/min nasal cannula showed a mild respiratory acidosis consistent with hypoventilation, with PO2 56 mmHg (laboratory reference range 37–42 mmHg), 87% O2 saturation (laboratory reference range 70%–75%), PCO2 51 mmHg (laboratory reference range 42–48 mmHg), HCO3 22 mEq/L (laboratory reference range 20–26 mEq/L), and pH 7.25. A rapid qualitative urine toxicology screen for barbiturates, benzodiazepines, opiates, amphetamine, PCP, methadone, cannabinoids, and cocaine revealed the presence of only cannabinoids. Given the leukocytosis and tachycardia, there was concern for sepsis from aspiration pneumonia, the patient was started on cefepime and vancomycin. His heart rate was tachycardic between 108 and 129 for the 14 hours that he was admitted (he left against medical advice), and respiratory rate stabilized at 16 to 18 breaths/min. His oxygen saturation was between 92% and 98% on room air. His tachycardia was likely a side-effect of cannabis ingestion, and sepsis from aspiration pneumonia. We advised him to obtain a chest CT scan angiogram to rule out pulmonary embolism, but he declined. Troponin down trended from initial 0.206 ng/mL to 0.074. The D-dimer was slightly elevated at 1.06 ug/mL. The patient was admitted to the medicine floors from the ED. Over the course of the day, he looked comfortable, though still drowsy. After 14 hours of presentation, he felt well, and left against medical advice.
CONCLUSION: In summary, this case represents evidence that naloxone may play a role in the treatment of cannabinoid toxicity, which may be explained by overlap between the endocannabinoid and endogenous opioid systems. Physicians should not expect the marked reversal in hypoventilation and somnolence usually observed with naloxone treatment of opioid overdose. Multiple doses of naloxone may be required to achieve effect, and a continuous infusion may be needed given the long half-life of cannabinoids. Further research into the use of naloxone for acute cannabinoid intoxication may offer more insight into the varied human responses reported in prior controlled studies and case reports.
116
ABSTRACT #70 CLINICAL RESEARCH CARDIOLOGY
COMPARISON OF THREE-YEAR OUTCOMES OF DRUG-COATED BALLOON ANGIOPLASTY IN TOTALLY OCCLUSIVE VERSUS NON-OCCLUSIVE IN-STENT RESTENOSIS OF DRUG-ELUTING STENTS
Zhuoran Yang1, Jiasheng Yin2, Yaqi Zhang3, Nirupama Krishnamurthi1, Lingling Wu4, Jacqueline E. Tamis-Holland1, Junbo Ge2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Zhongshan Hospital, Fudan University, Shanghai Institute of Cardiovascular Diseases, Shanghai, China; 3John H. Stroger Jr. Hospital of Cook County, Chicago, IL, United States; 4University of Alabama Birmingham, Birmingham, AL, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023
BACKGROUND/INTRODUCTION: The long-term outcomes of drug-coated balloon angioplasty in totally occlusive in-stent restenosis (ISR) are largely unknown.
METHODS: Patients who underwent drug-coated balloon angioplasty for in-stent restenosis of prior drug-eluting stents (DES) were divided into totally occlusive and non-occlusive ISR groups by coronary angiography. Those who had bail-out stenting, in-stent restenosis of coronary artery bypass graft, in-stent thrombus, ADHF and ESRD were excluded. Patients were followed for 3 years. The primary endpoint was target vessel failure. The secondary endpoint was target vessel revascularization.
RESULTS: Forty-seven patients were included in the totally occlusive ISR group and 338 patients were included in the non-occlusive ISR group. Clinical characteristics were similar between the two groups. The totally occlusive in-stent restenosis group had more stent layers and greater post-dilation diameter stenosis than the non-occlusive in-stent restenosis group. There was no statistically significant difference in the three-year target vessel revascularization (31.1% versus 18.6%, p=0.11) and target vessel revascularization rates (28.9% versus 16.3%, p=0.11) between the two groups. However, late target vessel revascularization rate (>1 year) was significantly higher in the totally occlusive in-stent restenosis group than in the non-occlusive group (25.6% versus 9.1%, p<0.01) driven primarily by target vessel revascularization. The independent risk factors for late target vessel revascularization were totally occlusive ISR, stent layers and post-dilation diameter stenosis. Three-year TVMI and cardiac death rates were similar between the two groups.
CONCLUSION: Target vessel failure and target vessel revascularization were more often observed in totally occlusive DES-ISR than in non-occlusive DES-ISR treated by drug-coated balloon angioplasty
117
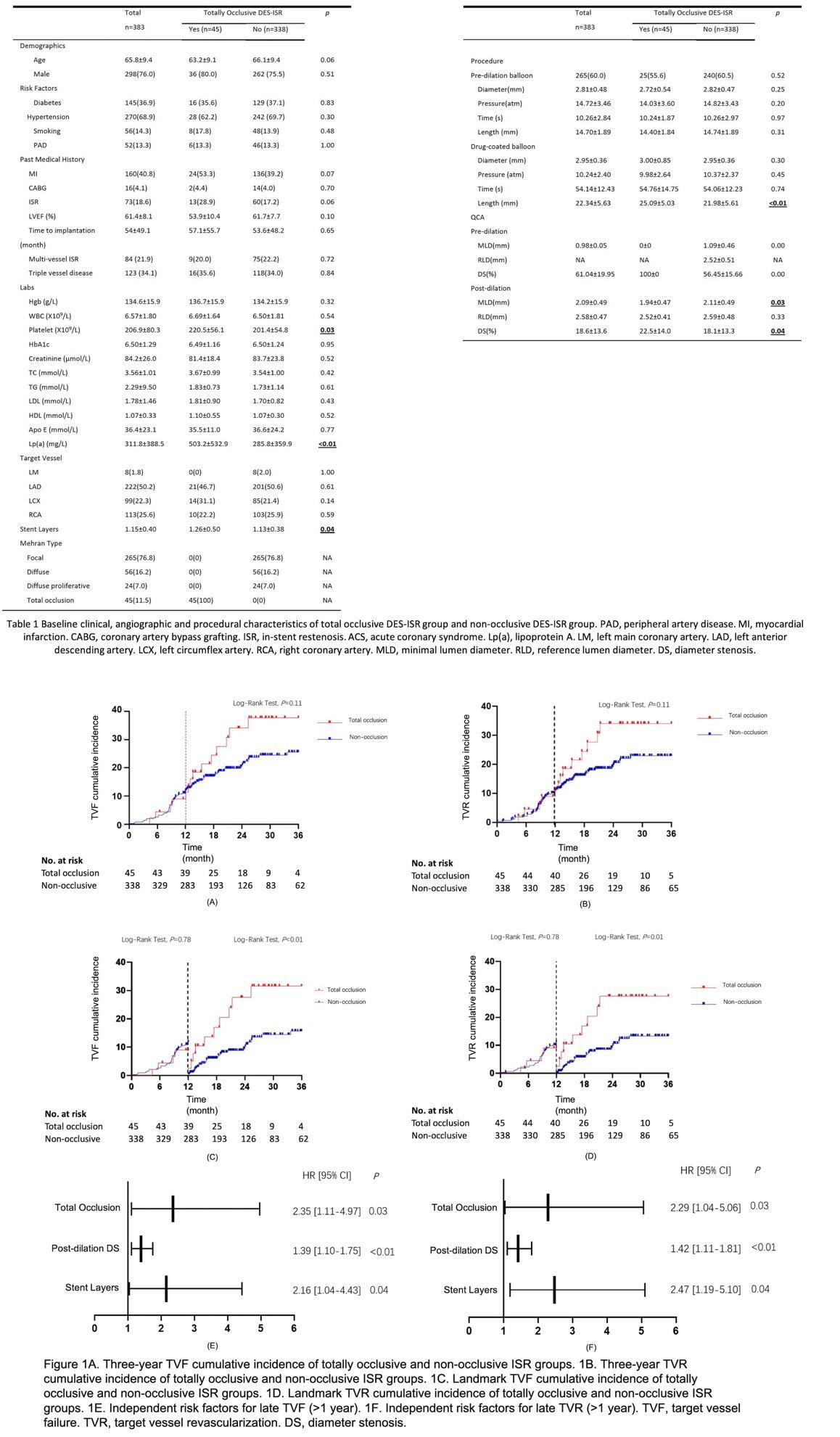
ABSTRACT #71
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
SUCCESSFUL BRENTUXIMAB VEDOTIN AND NIVOLUMAB THERAPY OF MULTIPLY REFRACTORY DIFFUSE LARGE B-CELL LYMPHOMA WITH HODGKIN FEATURES
Victor Zibara1, Filiz Sen2, Michael Scordo2 , Lorenzo Falchi2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Memorial Sloan-Kettering Cancer Center, New York, NY, United States
Published in Leukemia and Lymphoma, 2022. PMID: 36120859
BACKGROUND/INTRODUCTION: Diffuse large B-cell lymphoma (DLBCL) is the most com-mon subtype of non-Hodgkin lymphoma in the United States with high biological complexity and multiple discrete subtypes, identified by detailed gene expression and sequencing studies. Despite this heterogeneity, anthracycline-based chemoimmunotherapy, such as R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), remains the standard of care for most patients with newly diagnosed DLBCL. Patients with primary refractory DLBCL have limited treatment options and often-dismal prognosis and require newer, more effective treatment options. CD30, a diagnostic hallmark of classical Hodgkin lymphoma (cHL), is expressed in 14% of DLBCL cases. Brentuximab vedotin (BV), an anti CD30 monoclonal anti-body conjugated to the small-molecule microtubule disrupting agent monomethyl auristatin E (MMAE), is FDA approved for the treatment of cHL. While its biological and prognostic implications are unclear in DLBCL, CD30 may represent a viable therapeutic target for BV, in this disease, although data on this topic are extremely limited. Another potential target for DLBCL therapy is the programmed death (PD-)1/PD-ligand (L)1 axis. PD-L1 expression has been reported in almost all patients with cHL, but only a fraction of those with DLBCL. Nivolumab (NIVO), a human IgG4 anti-PD-1 monoclonal antibody, has shown remarkable results in patients with relapsed/refractory (R/R) cHL and it is currently approved (as are other PD-1 blockers) for this indication. It has, however, only modest activity in patients with R/R DLBCL, possibly due to the low frequency of alterations of 9p24.1 (where the PD-L1 and PDL2 genes reside) in this population. The term DLBCL with Hodgkin features refers to a distinctive subgroup of aggressive lymphomas with clinical and pathological features reminiscent of both DLBCL and cHL, thus BV and NIVO may represent attractive treatment options for this entity. Herein, we present the case of a patient with DLBCL with cHL-like features, primarily refractory to multiple lines of therapy, including chimeric antigen receptor (CAR)-T cells, who was success-fully treated with combined BV and NIVO.
CASE PRESENTATION: The patient is a 56-year-old man who presented to our clinic with persistent fatigue, bloating, lack of appetite, drenching night sweats, unintentional weight loss, and palpable lymphadenopathy. Lab work was notable for a hemoglobin of 8.5 g/dL. Biopsies of an inguinal enlarged lymph node and a rib lesion revealed large cells expressing CD20, PAX5 (strong), BCL6, MUM1, MYC, p53, CD30, and BCL2.FISH showed translocation ofBCL2, but no rearrangements of cMYC or BCL6. A PET scan revealed multiple FDG-avid lymph nodes above and below the diaphragm, bilateral subpleural nodules, bone lesions, and mildly FDG-avid splenomegaly. A staging bone marrow biopsy additionally showed a CD10-positive, t(14;18)-positive B-cell population, suggesting that the DLBCL had arisen in the context of underlying follicular lymphoma. The patient was diagnosed with stage IVDLBCL, germinal center B-cell subtype with an inter-national prognostic index of 2, and was treated with R-CHOP.
An interim positron emission tomography (PET)-computer tomography (CT) scan after four cycles suggested progression of disease in the right chest wall, subsequently confirmed by biopsy of the lesion. The patient began salvage therapy with rituximab, dexamethasone, cytarabine, and oxaliplatin (R-DHAX) and a post-cycle 2 PETCT scan showed further progression of diseae. The patient was treated with third-line axicabtagene ciloleucel, utilizing bendamustine, rituximab (BR) and polatuzumab as a bridging therapy. Of note, a PET-CT performed after one cycle of BR-polatuzumab showed further progression of disease. The post-CAR-T therapy course was complicated by grade 2 cytokine release syndrome treated with tocilizumab and grade 3 immune effector cell-
119
associated neurotoxicity syndrome requiring dexamethasone, anakinra, and a brief intensive care unit admission. A day 28 PET-CT again raised concern; therefore, the patient underwent biopsy of an FDG-avid axillary lymph node. Pathologic examination revealed atypical large lymphoid cells with irregular nuclei, vesicular chromatin, and conspicuous nucleoli, in a background of fibrosis, numerous eosinophils, and marked patchy necrosis. The large cells were arranged in sheets in portions of the biopsy and expressed PAX5 (weak), CD30 (bright), MUM1, BCL6,BCL2, c-MYC, and PD-L1, while being negative for OCT2,CD19, CD20, and LMP1. In light of the double CD30, PD-L1 positivity, pathologic features reminiscent of cHL, lack of viable treatment alternatives and the relatively young age, the patient was treated with combined BV and NIVO on a compassionate basis following the previously reported schedule. Treatment was only complicated by neutropenia requiring G-CSF support. A PET-CT scan performed after two cycles showed decreased size and complete resolution of metabolic activity of all sites of disease, consistent with complete metabolic response (CR). During cycle 4, NIVO was held to allow at least 6 weeks between the last dose of anti-PD-1 antibody and the planned allogeneic hematopoietic cell transplantation (allo-HCT) and minimize the risk of acute graft-versushost disease (GVHD) and associated complications. The patient received a non-myeloablative-conditioned matched related donor allo-HCT with post-transplantation cyclophosphamide-based GVHD prophylaxis and remains in clinical and radiographic CR without significant complications 4 months later
CONCLUSION: To our knowledge, this is the first reported case of cHL-like DLBCL treated with combined BVNIVO. In a phase II study of BV in patients with R/R DLBCL and variable CD30 expression. Jacobsen et al. reported an objective response rate (ORR) of 44% and CR 17% with a median response duration of 16.6 months (range 2.7 to 22.7 months). A CD30 expression level >5% by immunohistochemistry correlated with greater antitumor activity. NIVO, on the other hand, yielded disappointing results in patients with heavily pretreated DLBCL producing short-lived responses in only 10% of cases and a median progression-free survival (PFS) of less than 1.9 months. Combined BV and NIVO were studied as a first salvage in 91 patients with R/R cHL, where it was safe and effective with an ORR of 85% and CR 67%. The 3-year PFS rate of all patients on study was 77%. The combination was also studied in R/R primary mediastinal B-cell lymphoma, which is frequently both CD30 and PD-L1 positive, where the ORR was 73% and CR 37%. Although the median duration of response and overall survival were not established, BV-NIVO may exhibit curative potential and, potentially, avoid a more toxic allogeneic transplantation in some of these patients.
The story of our patient mirrors these encouraging results and suggests that cHL-like DLBCL may represent an ideal candidate for combined CD30 and PD-L1 blockade. More broadly, we advocate for systematic assessment of CD30 and PD-L1 expression in patients with R/R DLBCL and speculate that, in cases of concomitant CD30 and PD-L1 positivity, BV-NIVO may represent an effective therapy when no other viable options exist. Prospective clinical trials are warranted to validate this hypothesis and define the role of BV-NIVO, if any, in the management of patients with R/R DLBCL
120
List of Abstracts 2022-2023*
*Research/Scholarly Work presented in 2022-2023; does not include presentations already submitted as a poster
LIST OF ABSTRACTS 2022-2023
EARLY USE OF VASOPRESSORS IN THE RESUSCITATION OF HEMORRHAGIC SHOCK DUE TO GASTROINTESTINAL BLEEDING
72
Jeeyune Bahk1 , Adiac Espinosa Hernandez2, Patrick Maher2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in Washington, DC, United States from May 19-24, 2023.
NON-INVASIVE VENTILATION AND HIGH FLOW OXYGEN SYSTEM EDUCATION FOR INTERNAL MEDICINE RESIDENTS UTILIZING HIGH FIDELITY SIMULATION
73
Jeeyune Bahk1*, Matthew Alexander 1*, Harrindra Seepersaud1, Priscilla Loanzon1, Adam Rothman1, Susannah Kurtz1, Joseph Mathew1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
REMOTE ULTRASOUND TRAINING FOR BEDSIDE RIGHT VENTRICULAR DILATION AND DEEP VEIN THROMBOSIS IDENTIFICATION
74
Patrick Tobin-Schnittger1 , Yoni Balboul1, Adam Rothman1
ELSBERG SYNDROME IN HSV-2 INFECTION
Omar Belfaqeeh1, Alexandria Markley1, Mudita Patel1, Brian Markoff1, Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the CHEST Annual Meeting that was held in Nashville, TN, United States from October 16-19, 2022. 75
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Published in IDCases, 2023. PMID: 36875152 76
PREDICTORS OF RESPONSE TO NEOADJUVANT CHEMOTHERAPY IN BREAST CANCER: ONCOTYPEDX VERSUS MAMMAPRINT VERSUS LIQUID BIOPSY
Nadeem Bilani1, Mira Itani2 , Mohamed Mohanna3, Neha Debnath1, Barbara Dominguez2 , Hong Liang2, Zeina Nahleh3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Cleveland Clinic, Weston, FL, United States; 3Cleveland Clinic, Fort Lauderdale, FL, United States
Presented at the San Antonio Breast Cancer Symposium that was held in San Antonio, Texas, United States from December 6-10, 2022.
77
DEGREE OF INEFFECTIVE PERISTALSIS DOES NOT AFFECT FREQUENCY OF GASTROESOPHAGEAL REFLUX, BUT MAY FACILITATE MORE PROXIMAL REFLUX EVENTS
Christy Chon1, Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
122
LIST OF ABSTRACTS 2022-2023
DEMOGRAPHIC DISPARITIES IN CLINICAL TRIAL ENROLLMENT OF US PATIENTS WITH NEWLY-DIAGNOSED MULTIPLE MYELOMA
78
Bruno Almeida Costa1 , Raphael de Oliveira Bertasi1 , Neha Debnath1 , Adriana Rossi2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that will be held in Chicago, Illinois, United States from June 2-6, 2023.
NON-VITAMIN K ORAL ANTAGONISTS VERSUS ASPIRIN FOR PRIMARY THROMBOPROPHYLAXIS IN PATIENTS WITH MULTIPLE MYELOMA ON OUTPATIENT CHEMOTHERAPY: A SYSTEMATIC REVIEW AND META-ANALYSIS
79
Thomaz Alexandre Costa1 , Bruno Almeida Costa2, Nicole Felix4, Amanda Godoi5 , Alleh Nogueira6, Joshua Ryan Richter7, Adriana Rossi7
1Federal University of Ceará, Fortaleza, Brazil; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY; 4Federal University of Campina Grande, Campina Grande, Brazil; 5Cardiff University School of Medicine, Cardiff, United Kingdom; 6Bahia School of Medicine and Public Health, Salvador, Brazil; 7Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY
To be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that will be held in Chicago, Illinois, United States from June 2-6, 2023.
EVALUATING MEDICAL RESIDENT’S COMFORT AND KNOWLEDGE ON CARING FOR PATIENTS AT THE END OF THEIR LIFE
Fionnuala Crowley1, Neha Dabnath1, Sonal Gandhi1, Yosef Joseph Rene Amel Riazat
80
Kesh1, Jennifer Fung1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
UTILIZATION PRESENCE AND SEVERITY OF SUBCLINICAL ATHEROSCLEROTIC DISEASE IN THE PRIMARY PREVENTION OF THE ONCOLOGIC POPULATION
81
Sara Diaz Saravia1, Renzo Melchiori2, Szlaien Lucas2, Romina Mourino2, Pablo Rubio2 , Mateo Bivort2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Hospital Universitario Austral, Unidad Coronaria, Buenos Aires, Argentina
Presented at the New York American College of Cardiology Annual Meeting on December 9, 2022 and at the Inaugural Mount Sinai Heart Research Forum on February 22, 2023 that were both held in New York, NY, United States.
PROGNOSTIC SIGNIFICANCE OF MYOCARDIAL ISCHEMIA DURING EXERCISE IN PATIENTS WITH NON-OBSTRUCTIVE CORONARY DISEASE COMPARED TO PATIENTS WITH NORMAL EXERCISE ECHO
82
Ga Hee Kim1 , Alaa Omar1, Swiri Konje1, Loba Alam1 , Joseph Elias1, Elizabeth A. Zipf1 , Christopher Perez Lizardo1, Maria K. Peña1, David Miester1, Errol C. Moras1, Kruti Dhaval Gandhi1, Arpanjeet Kaur1, Brissete Mancero1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
123
LIST OF ABSTRACTS 2022-2023
83
EVALUATING THE EFFECTIVENESS OF VIRTUAL DIDACTIC SESSIONS VERSUS SMALL GROUP SIMULATION-BASED SESSIONS FOR MASTERING RIGHT VENTRICULAR FUNCTION ASSESSMENT WITHIN A POINT-OF-CARE ULTRASOUND CURRICULUM
Kruti Dhaval Gandhi1, Errol Moras1, Arpanjeet Kaur1, Yoni Balboul1, Adam Rothman1
85
IMPACT OF FRAILTY ON OUTCOMES OF PERCUTANEOUS CORONARY INTERVENTION: INSIGHTS FROM THE NATIONWIDE INPATIENT SAMPLE
Kruti Gandhi1 , Errol Moras1, Tais Bertasi1, Raphael Bertasi1, Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023. 84
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Society for Cardiovascular Angiography and Interventions (SCAI) Annual Meeting that will be held in Phoenix, Arizona, United States from May 18-20, 2023.
TEMPORAL TRENDS AND OUTCOMES OF HEART FAILURE PATIENTS BETWEEN LIGHT-CHAIN CARDIAC AMYLOIDOSIS AND TRANSTHYRETIN CARDIAC AMYLOIDOSIS: INSIGHTS FROM THE NATIONAL INPATIENT SAMPLE DATABASE
Kruti Gandhi1 , Errol Moras1 , Tais Bertasi1, Raphael Bertasi1, Nadeem Bilani1, Ashish Correa1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Technology and Heart Failure Therapeutics (THT) Annual Meeting that was held in Boston, Massachusetts, United States from March 20-22, 2023. 86
UNBIASED CLUSTER MODELLING FOR UNCOVERING NATURAL DISTRIBUTION OF DOPPLER DERIVED DIASTOLIC VARIABLE RESPONSE TO EXERCISE AMONG PATIENTS REFERRED TO EXERCISE ECHOCARDIOGRAPHY
Alaa Omar1, Swiri Konje1, Loba Alam1 , Kruti D. Gandhi1 , Errol Moras1, Brissete Mancero1 , Elizabeth Zipf1, David Meister1, Maria K. Peña1, Christopher Perez Lizardo1, Ga Hee Kim1 , Joseph Elias1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022. 87
COMMUNICATION SKILLS TRAINING CURRICULUM NEEDS ASSESSMENT FOR INTERNAL MEDICINE RESIDENTS
Sonal Gandhi1, Yosef Joseph Rene Amel Riazat-kesh1, Fionnuala Crowley1, Vasundhara Singh1, Noelle Javier1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
124
LIST OF ABSTRACTS 2022-2023
ASSESSMENT OF POST-PROCEDURAL COMPLICATIONS IN THE INPATIENT SETTING: IMPLEMENTATION OF A STANDARDIZED COMPREHENSIVE DOCUMENTATION TOOL
88
Kristine Lou Gargaritano1, Irina Zaretsky1, Shantheri Shenoy1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
STATUS ASTHMATICUS COMPLICATED BY RHABDOMYOLYSIS
Satwant Grewal1, Tal Shachi1,2, Pavan Paka3, Sara Luby1, Arpanjeet Kaur1 , Patrick Tobin-Schnittger1, Vincent Courant1, James Salonia1
89
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
3Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
Presented at the CHEST AnnualMeeting that was held in Nashville, TN, United States from October 16-19, 2022.
90
THE CORRELATION BETWEEN EARLY ENDOSCOPY AND IN-HOSPITAL OUTCOMES IN PATIENTS WITH UPPER GI MALIGNANCIES ADMITTED FOR UPPER GI BLEEDING
Suhail Haddadin1, Patricia Miguez Arosemena1, Farah Haddadin2, Rand Fram2 , Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2The University of Jordan, Amman, Jordan
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
CHANGES IN GLYCEMIC CONTROL AND BODY WEIGHT OVER THE COURSE OF THE COVID-19 PANDEMIC IN AN URBAN OUTPATIENT SETTING
91
Keerthana Haridas1, Deborah Edelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
DIFFICULT CONVERSATIONS AND EFFECTIVE COMMUNICATION TRAINING FOR INTERNAL MEDICINE RESIDENTS UTILIZING HIGH FIDELITY SIMULATION
Ariela Hazan1, Jeeyune Bahk1, Ariel Gordon1, Neha Debnath1, Harrindra Seepersaud1 , Donna Gormley1, Priscilla Loanzon1 , Adam Rothman1, James Salonia1, Susannah Kurtz1
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Aurora, Colorado, United States from May 10-13, 2023. 92
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
125
LIST OF ABSTRACTS 2022-2023
A GIANT FREE-FLOATING BALL THROMBUS OR A TINY FIBROELASTOMA: WHICH CAUSES MULTIPLE STROKES?
93
Swiri Konje1, Yeraz Khachatoorian1 , Arpanjeet Kaur1, Nirupama Krishnamurthi1 , Soheila Talebi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
A TARGETED NEEDS ASSESSMENT FOR THE DEVELOPMENT OF A TELEMETRY CURRICULUM FOR INTERNAL MEDICINE RESIDENTS
94
Arpanjeet Kaur1, Joseph Elias1, Neojsa Markovic1, Roberto O. Jimenez1, Michel Skaf1 , Robert Abed1 , Deepika Misra1, Edgar Argulian1, Kiran Mahmood1, Jacqueline TamisHolland1, Forough Hakimzada1, Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023 95
ROLE OF EARLY AORTIC VALVE REPLACEMENT VERSUS CONVENTIONAL MANAGEMENT IN ASYMPTOMATIC PATIENTS WITH SEVERE AORTIC STENOSIS: A META-ANALYSIS
Arpanjeet Kaur1 , Arshdeep Dhaliwal2, Sumit Sohal2, Yoni Balboul1, Jacqueline TamisHolland1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Newark Beth Israel Medical Center, Newark, NJ, United States
VIRTUAL CARDIAC POINT-OF-CARE ULTRASOUND CURRICULUM AMONG RESIDENTS: A MEDICAL EDUCATION PROJECT
Arpanjeet Kaur1 , Yoni Balboul1, Kruti Gandhi1, Adam Rothman1
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022. 96
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022. 97
CLINICAL BENEFIT OF NEUROHORMONAL BLOCKADE IN WOMEN WITH TRANSTHYRETIN CARDIAC AMYLOIDOSIS AND HEART FAILURE WITH PRESERVED EJECTION FRACTION
Darren Kong1, Alaa Omar1, Maria K. Peña, Arpanjeet Kaur1, Ashish Correa1, Edgar Argulian1, Johanna Paola Contreras2, Arieh L. Fox1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
126
LIST OF ABSTRACTS 2022-2023
98
DRESS SYNDROME-ASSOCIATED PERIMYOCARDITIS AFTER INITIATION OF RIPE THERAPY: A CASE REPORT
Darren Kong1, Keshav K. Dixit1 , Swiri Konje1, Vikram Agarwal1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
GASTRIC INTESTINAL METAPLASIA PREVALENCE AND APPROPRIATE FOLLOW UP: A QUALITY IMPROVEMENT STUDY
Frederick Rozenshteyn1, Emily Seltzer1 , Randy Leibowitz1, Marni Wilkoff1, Attila Molnar1 , Gabriel Levi1, Tina Park1
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023. 99
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023.
NOW YOU SEE ME, NOW YOU DON’T: A CASE OF CAMPYLOBACTER JEJUNI COLITIS PRESENTING AS A COLONIC MASS
Randy Leibowitz1 , Frederick Rozenshteyn1, Samuel Daniel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022. 101
THE MASTER OF DISGUISE: ISOLATED GASTRIC VARICEAL HEMORRHAGE AS A COMPLICATION OF ENDOSCOPIC GASTRIC BIOPSY
Randy Leibowitz1 , Frederick Rozenshteyn1, Edward Lung1, Abdallah Beano1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
YOU SHALL NOT PASS: RARE DUODENAL BULB ADENOCARCINOMA CAUSING GASTRIC OUTLET OBSTRUCTION
Randy Leibowitz1 , Alexander Maraveyas1, Frederick Rozenshteyn1, Tina Park1
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022. 102
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
WORKSHOPS TO TEACH INTERNAL MEDICINE RESIDENTS AND EVALUATE THEIR ABILITY TO TREAT GASTROINTESTINAL BLEEDING
Randy Leibowitz1, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022. 103
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
100
127
LIST OF ABSTRACTS 2022-2023
TAKOTSUBO CARDIOMYOPATHY AS A COMPLICATION OF SCALENE NERVE BLOCK
104
Christopher N. Matthews1, Syed Farrukh Mustafa1, Deepika Misra1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the New York American College of Cardiology Annual Meeting on December 9, 2022 and at the Inaugural Mount Sinai Heart Research Forum on February 22, 2023 that were both held in New York, NY, United States. 105
CLINICAL OUTCOMES OF CARDIAC DEVICES IN HEART FAILURE PATIENTS HOSPITALIZED WITH COVID-19: INSIGHTS FROM NATIONAL INPATIENT SAMPLE DATABASE
Errol Moras1 , Kruti D. Gandhi1 , Nadeem Bilani1, Tais Bertasi1, Raphael Bertasi1, Ashish Correa1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Technology and Heart Failure Therapeutics (THT) Annual Meeting that was held in Boston, Massachusetts, United States from March 20-22, 2023. 106
PATENT FORAMEN OVALE WITH PLATYPNEA-ORTHODEOXIA PRECIPITATED BY LARGE HEPATIC CYST REQUIRING CLOSURE: NOVEL APPROACH
Errol Moras1, Kruti D. Gandhi1, Apurva Sharma1, Francisco J. Romeo1, Parissa Tabirzian1 , Barry A. Love1 ,
Amirali Ahmadi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022. 107
THE EFFECT OF COVID-19 ON OUTCOMES OF NON-ST ELEVATION MYOCARDIAL INFARCTION (NSTEMI): RESULTS FROM THE NATIONAL INPATIENT SAMPLE DATABASE
Errol Moras1 , Kruti D. Gandhi1 , Tais Bertasi1, Raphael Bertasi1 , Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
COLONIC SCHWANNOMA: A CAUSE FOR NERVES?
Mantej Sehmbhi1, Sera Satoi2, Qingqing Liu3, Ilan Weisberg2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
To be presented at the Society for Cardiovascular Angiography and Interventions (SCAI) Annual Meeting that will be held in Phoenix, Arizona, United States from May 1820, 2023. 108
3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
128
LIST OF ABSTRACTS 2022-2023
DIAGNOSING VISCERAL KAPOSI SARCOMA: THE NECESSITY TO AVOID ANCHORING ON THE DIAGNOSIS OF A CROHN'S FLARE
109
Emily Seltzer1, Shabari M. Shenoy1, Bo Hyung Yoon1, Frederick Rozenshteyn1 , Kevin Mijares1, Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022 and published in Cureus, 2023. PMID: 36938235
SIMULATION CASE ON ABDOMINAL SEPSIS-APPLICATION OF THREE ESSENTIAL CLINICAL CONCEPTS-SEPSIS PROTOCOL, COGNITIVE BIASES ALONG WITH POINT-OF-CARE ULTRASOUND
110
Venus Sharma1, James Salonia1, Priscilla Loanzon1, Harrindra Seepersaud1
UNPLANNED EXTUBATION IN THE ICU: OPPORTUNITIES AND CHALLENGES
Yasmin I. Herrera1 , Venus Sharma1, Sara Luby1, James Salonia1, Adam Rothman1 , Raymonde Jean1, Joseph P. Mathew1, Susannah Kurtz1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023 111
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the CHEST Annual Meeting that was held in Nashville, TN, United States from October 16-19, 2022. 112
OUTCOMES IN PATIENTS WITH CIRRHOSIS UNDERGOING ESOPHAGOGASTRODUODENOSCOPY FOR UPPER GASTROINTESTINAL BLEEDING
Shabari M. Shenoy1, Mantej Sehmbi1, Suhail Haddadin1, Maan El Halabi1, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022. 113
RECURRENT PANCREATITIS SECONDARY TO ADDERALL USE WITH PANCREATIC ASCITES: A SIGHT TYPICALLY UNSEEN
Shabari M. Shenoy1 , Jenny Dave1,2, Edward Lung1 , Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
THE MARCHING BAND: PSEUDOACHALASIA SECONDARY TO GASTRIC BAND SLIPPAGE
Shabari M. Shenoy1 , Gres Karim2, Kimberly Cavaliere1
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022. 114
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
129
LIST OF ABSTRACTS 2022-2023
TIME FOR A RENDEZVOUS: MULTI-DISCIPLINARY MANAGEMENT OF COMPLETE ESOPHAGEAL OBSTRUCTION IN A PATIENT FOLLOWING RADIATION TO POSTSURGICAL ANATOMY
115
Shabari M. Shenoy1 , Gres Karim2, Kimberly Cavaliere1, Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022. 116
IMPLEMENTATION OF A LONGITUDINAL PROCEDURAL CURRICULUM: WHAT EDUCATIONAL TOOLS IMPROVE PROCEDURAL PROFICIENCY WITHIN INTERNAL MEDICINE RESIDENCY PROGRAMS
Sidra Salman1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
A NOVEL ENDOTHELIAL FUNCTION TEST IN PREDICTING LATE CORONARY INSTENT RESTENOSIS
Zhuroran Yang1 , Jiasheng Yin2, Yaqi Zhang3, Lingling Wu4, Jieyu Jiang2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023. 117
2Zhongshan Hospital, Fudan University, Shanghai, China; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; 4University of Alabama, Birmingham, AL, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
COMPLICATION AND READMISSION OUTCOME OF ATRIAL FIBRILLATION CATHETER ABLATION AMONG CANCER PATIENTS
Lingling Wu1, Bharat Narasimhan2 , Zhuoran Yang3, Kirtipal Bhatia3 , Pengyang Li4 , Arti Shah5, Bharat K. Kantharia5
118
1University of Alabama, Birmingham, AL, United States; 2Methodist Hospital, Houston, TX, United States; 3Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Virginia Commonwealth University, Richmond, VA, United States; 5Cardiovascular and Heart Rhythm Consult, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
THIRTY DAY READMISSION OUTCOMES OF PERCUTANEOUS LEFT ATRIAL APPENDAGE OCCLUSION IN PATIENTS WITH CANCER
Yaqi Zhang, Zhuoran Yang2 , Raquel Soon-Shiong1, Muhammad Usman Almani1 , Bolun Liu3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mayo Clinic Health System, Mankato, MN, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
119
130
LIST OF ABSTRACTS 2022-2023
UTILIZATION AND IN-HOSPITAL OUTCOMES OF PERCUTANEOUS LEFT ATRIAL APPENDAGE OCCLUSION IN PATIENTS WITH CANCER
Yaqi Zhang1 , Zhuroran Yang2 , Raquel Soon-Shiong1, Muhammad Usman Almani1 , Ufuk Vardar1, Sami Shoura1, Sadichhya Karki1, Bolun Liu3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mayo Clinic Health System, Mankato, MN, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
120
131
Abstracts 2022-2023*
*Research/Scholarly Work presented in 2022-2023; does not include presentations already submitted as a poster
ABSTRACT #72 CLINICAL RESEARCH
GASTROENTEROLOGY/PULMONARY/CRITICAL CARE
EARLY USE OF VASOPRESSORS IN THE RESUSCITATION OF HEMORRHAGIC SHOCK DUE TO GASTROINTESTINAL BLEEDING
Jeeyune Bahk1 , Adiac Espinosa Hernandez2, Patrick Maher2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in Washington, DC, United States from May 19-24, 2023.
BACKGROUND/INTRODUCTION: Although transfusion remains the cornerstone of treatment in traumatic hemorrhagic shock, recent data suggests a role for vasopressors in certain patients to reduce transfusion requirements and limit the duration of shock. Little is known about vasopressor use in early resuscitation of nontraumatic/medical hemorrhagic shock. Our study aimed to investigate benefits of early use of vasopressors in hemorrhagic shock due to gastrointestinal bleeding (GIB).
METHODS: We performed a retrospective cohort study on 113 patients hospitalized with hemorrhagic shock due to GIBin four MountSinai Hospitals identifiedusingthe Mount Sinai Data Warehouse. Clinical characteristics of patients who received vasopressors within the first six hours of shock were compared to those who did not. The primary outcome of interest was time to resolution of shock by Kaplan-Meier analysis. Secondary outcomes included mortality, volume of crystalloids and blood products at seven days.
RESULTS: 44 patients received vasopressors whilst 69 patients were treated without vasopressors. The mean ages were 68.2 years for vasopressor patients and 71.7 years without.Vasopressor patients included 70% males compared to 57% of those without vasopressors. Causes of GIB for both groups were similar with the majority being upper GIB (60.5% and 50.7%), followed by lower GIB and esophageal varices. Higher APACHE II score at 24 hours was seen in patients requiring vasopressors (22.3 versus 17.2, p=0.001). The receipt of anticoagulants at the time of shock were statistically similar. Patients placed on vasopressors were given more colloids in first 24 hours (182 ml versus 43 ml, p=0.0001), whilst statistically similar amounts of crystalloids were given. More total crystalloids, packed red cells, and fresh frozen plasma were administered within the first seven days of shock (2311 ml versus 1927 ml; 4.8 units versus 3.4 units; 2.2 units versus 0.7 units, respectively, p<0.005). ICU length of stay and mortality was not statistically different between the groups on multivariate logistic regression analysis. Time to resolution of shock was longer in patients given vasopressors than those without vasopressors (p=0.01).
CONCLUSION: Our study indicates that vasopressors did not improve outcomes in patients with hemorrhagic shock from GIB. Possible explanations include refractory vasoplegic state leading to multiple organ failure or differences in illness severity not captured by our current analysis. Limitations include retrospective design and small sample size. A larger cohort study with propensity score matching is planned for further investigation.
133
Table 1: Clinical characteristics comparing patients who received vasopressors first six hours of shock to those who did not
Note – Continuous variables are presented as means and standard deviations for normally distributed data. Categorical variables are summarized as frequencies and percentages. Differences in distributions of characteristics were analyzed using Student t test or Mann-Whitney U test for continuous variables and Chisquare or Fisher’s exact test for categorical variables. SBP=systolic blood pressure; APACHE II=Acute Physiology and Chronic Health Evaluation II; GIB=gastrointestinal bleeding; DOAC=direct oral anticoagulant; pRBC=packed red blood cells; FFP=fresh frozen plasma; ICU=intensive care unit; LOS=length of stay.
Vasopressors 0-6 hours No Vasopressors 0-6 hours p-value Age (yr) [mean (IQR)] 68.2 (36-97) 71.7 (29-101) 0.682 Males – [N (%))] 31 (70.1) 39 (56.5) 0.137 Females 13 (29.5) 30 (43.5) 0.137 Charlson Comorbidity Index (mean (SD)) 5.36 (2.3) 5.01 (2.9) 0.107 APACHE II score [mean (SD)] 22.3 (14.9) 17.2 (5.7) 0.001 Upper GIB NOS [N (%)] 26 (60.5) 35 (50.7) 0.416 Lower GIB [N (%)] 11 (25.6) 26 (37.7) 0.416 Esophageal varices bleeding [N (%)] 6 (14) 8 (11.6) 0.416 DOAC [N (%)] 4 (9.1) 12 (17.4) 0.217 Heparin [N (%)] 1 (2.3) 3 (4.3) 0.561 Warfarin [N (%)] 3 (6.8) 1 (1.4) 0.132 Antiplatelets [N (%)] 7 (15.9) 20 (29) 0.112 Volume of crystalloids-24 hours (ml) [mean (SD)] 1234 (1664.4) 1420 (1341.8) 0.203 Volume of colloids-24 hours (ml) [mean (SD)] 181.8 (404.7) 43.5 (135.3) 0.0001 PRBC –24 hours(unit) [mean (SD)] 3.8 (4.3) 2.6 (1.8) 0.001 FFP-24 hours (unit) [mean (SD)] 1.64 (2.7) 0.59 (1.2) 0.0001 Platelets-24 hours (unit) [mean (SD)] 2.89 (4.2) 1.3 (2.7) 0.0001 Volume of crystalloids-7 days (ml) [mean (SD)] 2311 (3962.7) 1926.8 (2139.5) 0.004 PRBC –7 days (unit) [mean (SD)] 4.8 (4.7) 3.4 (2.3) 0.001 FFP-7 days (unit) [mean (SD)] 2.2 (2.9) 0.7 (1.3) 0.0001 Platelets-7 days (unit) [mean (SD)] 3.3 (5.6) 2.4 (3.9) 0.152 ICU LOS [mean (SD)] 8.2 (9.3) 5.9 (5.7) 0.06 Mechanical ventilation first 48 hours [N (%)] 22 (52.4) 24 (35.3) 0.07
134
ABSTRACT #73 MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
NON-INVASIVE VENTILATION AND HIGH FLOW OXYGEN SYSTEM EDUCATION FOR INTERNAL MEDICINE RESIDENTS UTILIZING HIGH FIDELITY SIMULATION
Jeeyune Bahk1*, Matthew Alexander 1*, Harrindra Seepersaud1 , Priscilla Loanzon1, Adam Rothman1 , Susannah Kurtz1, Joseph Mathew1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
BACKGROUND/INTRODUCTION: Utilization of non-invasive ventilation (NIV) and high flow oxygen delivery system (HFNC) has substantially increased over time. A novel, simulation-based educational curriculum was designed to address the educational gap in resident education. Goals were to improve NIV/HFNC equipment familiarity and to enhance understanding of the physiology and application of NIV/HFNC.
METHODS: The curriculum included an initial didactic session discussing management of acute respiratory failure, physiology behind different oxygen modalities, and indications/contraindications of NIV/HFNC. After an opportunity to familiarize themselves with various NIV/HFNC machines, a simulated case-based scenario followed, incorporating high-fidelity simulation modalities aimed at training the learners in the clinical application of oxygen delivery systems. A short debrief and feedback session was held thereafter. Learners filled out a presession and a post-session survey, evaluating a change in subjective comfort and objective knowledge on NIV/HFNC management. P-values were calculated using independent two-sample t-tests and p≤0.05 was considered to indicate statistical significance.
RESULTS: There 79 Internal Medicine residents participated in a pre-session survey,including29 post-graduate year 1 (PGY1) (36.7%), 24 PGY2 (30.4%), and 26 PGY3 (32.9%). Most confirmed having never received a formal training in NIV/HFNC (n=67, 84.8%). Whilst 38% (n=30) reported equipment familiarity, 87.3% (n=69) admitted to having needed help for titration of the machines. Less than half reported feeling comfortable in utilizing HFNC (n=28, 35.4%) and NIV (n=21, 26.6%) on the Likert scale. This improved to 90% (n=58/64) postsession (p=0.045).
Evaluation of resident knowledge on NIV/HFNC revealed that only 2 (3.1%) knew how to correctly utilize CPAP (2.5%), which improved to 13 (20.3%) post-session (p=0.006). Initially, 48.1% (n=37) and 22.1% (n=17) incorrectly answered asthma and severe hypoxemia as one of the first-line indications of BiPAP, which improved to 9.4% (n=6) and 17.2% (n=11), respectively. Contraindications of BiPAP were correctly answered in 83.5%, which further improved to 95.3% (p=0.048). Only 31.6% (n=25) knew how to appropriately adjust NIV in worsening hypercarbic respiratory failure prior to the training, which drastically improved to 76.6% (n=49) (p=0.023). Correctly answered titration of HFNC also improved from 68.4% to 78.1% (p=0.001).
CONCLUSION: Pre-session surveys demonstrated learners’ unfamiliarity and discomfort as well as knowledge deficits with NIV/HFNC systems. Post-session surveys held after a didactic and high-fidelity simulation session demonstrated statistically significant improvement in comfort and knowledge. This novel simulation-based curriculum educated residents on the recognition of patients with acute respiratory failure and the management of these patients utilizing NIV and HFNC. High fidelity simulation can be utilized as a training modality to improve knowledge and skill among clinicians and thus improve clinical care.
135
ABSTRACT #74 MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
REMOTE ULTRASOUND TRAINING FOR BEDSIDE RIGHT VENTRICULAR DILATION AND DEEP VEIN THROMBOSIS IDENTIFICATION
Patrick Tobin-Schnittger1 , Yoni Balboul1, Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the CHEST Annual Meeting that was held in Nashville, TN, United States from October 16-19, 2022.
BACKGROUND/INTRODUCTION: Point-of-care ultrasound (POCUS) is an increasingly accessible tool allowing for earlier identification of VTE and treatment. POCUS has typically been taught in small groups with low instructor to participant ratios, making it time consuming and challenging to coordinate training for large numbers. It is our hope that virtual POCUS training may alleviate these shortcomings. We aim to show that short virtual didactic sessions, focused on deep vein thrombosis (DVT) and right ventricular (RV) size assessment can quickly improve competency amongst large groups of internal medicine house staff, and in the future reduce delays in diagnosis.
METHODS: Internal medicine housestaff at an academic teaching hospital completed an anonymous and voluntary REDCap survey before and after a one-hour remotely delivered didactic POCUS session focused on DVT and RV size. The pre- and posttest surveys were identical, consisting of multiple choice and closed-ended questions using Likert scales to ascertain participants’ confidence levels.
RESULTS: Of the 62 participating housestaff (26 interns, 36 residents), 54 completed the pre-test (18 interns, 36 residents), and 41 (11 interns, 30 residents) completed the post-test (76.5% response rate overall). 37% (23/62) had formal training in ultrasound. Both interns and residents reported weekly use of POCUS. SPSS software was used for paired t-test analysis of pre- and post-test results. There was a significant increase (p=0.003) in the percent of correct responses post lecture amongst all participants (pretest M 0.47, SD ± 0.17; post-test M 0.84, SD ± 0.09), amongst interns (p<0.001; pre-test M 0.40, SD ± 0.19; post-test M 0.86, SD ± 0.14), and amongst residents (p=0.009; pre-test M 0.50, SD ± 0.20; post-test M 0.79, SD ± 0.10). There was a significant increase in the percent of correct responses post lecture amongst participants with formal US training (p=0.007; pre-test M 0.56, SD ± 0.19; post-test M 0.84, SD ± 0.09) and amongst participants without formal US training (p=0.002; pre-test M 0.39, SD ± 0.17; post-test M 0.77, SD ± 0.11).
CONCLUSION: All groups studied demonstrated increased competency after a short didactic session. Need for in-person small group learning, a barrier to POCUS trainingen masse, may be overcome with this new approach. Study limitations include small sample size and discrepancies in group numbers pre- and post-test. As POCUS proficiency spreads amongst Internal Medicine housestaff, in part by these virtual didactic sessions, delays to timely VTE diagnosis and thereby treatment may be reduced.
136
Abstract #75
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
ELSBERG SYNDROME IN HSV-2 INFECTION
Omar Belfaqeeh1, Alexandria Markley1, Mudita Patel1, Brian Markoff1 , Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in IDCases, 2023. PMID: 36875152
BACKGROUND/INTRODUCTION: Elsberg syndrome (ES) is a neuroinflammatory disease that causes acute or subacute lumbosacral radiculitis, with or without myelitis. ES typically presents as cauda equina syndrome (CES), with symptoms of sensory impairment, lower extremity weakness, saddle anesthesia, and urinary and/or bowel incontinence. It is usually associated with infectious causes such as SARS-CoV-2, West Nile Virus, Varicella Zoster Virus (VZV), and Herpes Simplex Virus Type 2 (HSV-2), with HSV-2 being the predominate causative pathogen. HSV-2 is dormant in 40% of sacral dorsal root ganglia; when reactivated, virus can spread axonally into the spinal cord. Primary genital infection similarly causes neurologic dysfunction, most commonly in younger patients. Immunocompromised patients such as those with malignancy, HIV, or history of organ transplants are at a greater risk for herpes zoster infections, which is a cause of infectious lumbosacral radiculitis and myelitis. Additionally, ES related to VZV should be considered in the differential diagnosis of patients with prolonged poorly controlled T2DM. Treatment with acyclovir, even in cases without a definitive viral cause, is considered beneficial in many cases Duration of treatment varies and is typically between 10-21 days. The use of steroids in the treatment of ES is debated. Oral steroid tapers or short course high dose IV steroids can be used to help shorten the duration of symptoms. Elsberg syndrome accounts for approximately 5-10% of cauda equina syndrome and myelitis and up to 30% of patients have a recurrence of symptoms within the first year
CASE PRESENTATION: Our patient was a 51-year-old female with a past medical history significant for fibromyalgia, right-sided sciatica, right lower extremity deep venous thrombosis, asthma, nephrolithiasis, vertigo, and oral and genital herpes infection who recently returned from Dominican Republic. She presented to the emergency room with complaints of a 10-day history of progressive lower extremity sensory changes and weakness preceded by transient bilateral arm pain and neck and head pressure. Furthermore, she reported being unable to completely void for one day in duration. She described the weakness to be worse in the right leg compared to the left leg, describing it as “leg heaviness” which resulted in a fall at home a day prior to presentation. While she was sitting in the bathroom, she tried to stand but her knees 'buckled' and she fell backward, hitting her head on the floor (denied any loss of consciousness). Her family carried her to the Emergency Department as she was unable to bear weight.
Vital signs on presentation were within normal limits. Physical exam was most notable for reduced power of knee flexors and knee extensors (3/5), dysesthesia to touch and pinprick from mid-thigh distally in stocking distribution bilaterally, absent knee reflexes bilaterally, positive Babinski bilaterally, and no clonus. Given her weakness and urinary hesitancy, a magnetic resonance imaging (MRI) of the cervical, thoracic, and lumbar spine was done to assess for spinal cord pathology and a bladder scan was done to rule out urinary retention. Neurology evaluated the patient for acute progressive lower extremity neuropathic pain and weakness. A lumbar puncture was performed to rule out atypical Guillain Barre syndrome or multiple sclerosis.
Complete blood count showed a white blood cell count of 5.1 × 103 cells/mL, hemoglobin of 11.9 g/dL, platelet count of 371 × 103 cells/mL, and eosinophils elevated to 5.7%. The basic metabolic panel was within normal limits. Vitamin B12 level came back low at 290 pg/mL, homocysteine of 11.2, ESR 30.9, and CRP 5.9. Other labs including creatine phosphokinase, aldolase, methylmalonic acid, Lyme titers, copper level, vitamin B12, and SSA/SSB (Sjogren Antibodies) were unremarkable. The CSF PCR cytology showed pleocytosis with a WBC count of 360 (100% lymphocytes), although no albumin cytologic dissociation was seen, and protein of 182 mg/dL. CSF PCR was positive for HSV-2. Infectious disease (ID) was consulted and reviewed the MRI
137
spine with radiology, which demonstrated a very faint enhancement of the L4-5 nerve roots. An MRI brain came back within normal limits. An initial electromyography (EMG) study done during the first week of her admission was unremarkable. A repeat MRI of the whole spine 7 days later showed linear enhancement in the dorsal aspect of the thecal sac from L2 to L4 which may represent an abnormal enhancement of a nerve root in the cauda equina. A repeat EMG was indicative of bilateral L3/L4 radiculopathies. At this point, based on clinical, radiographic, and serological testing the patient was diagnosed with HSV2 lumbosacral radiculitis (Elsberg Syndrome).
The patient was started on Acyclovir IV 10mg/kg q8hr for 21 days along with adequate IV fluid hydration, 5 days of high dose methylprednisolone 1g IV daily, and B12 supplementation 1000 mcg daily. She needed an aggressive pain control regimen which included Tylenol, Flexeril, lidocaine patch, duloxetine, Percocet, and Dilaudid. 10 days after the first LP was performed a second lumbar puncture was done and came back positive for HSV-2 but with no significant improvement of the CSF fluid analysis. 14 days later, a third LP was remarkable for improved WBC count (360 down to 80) and protein level (182 down to 73).
After being an inpatient for three weeks, the patient was discharged to acute inpatient rehabilitation to improve mobility and to maximize safety and functional independence. She remained in rehab for intensive physical and occupational therapy for one month before being discharged home. Her overall duration of symptoms may have also contributed to her symptom improvement. Although she made great progress while being in the acute rehabilitation unit, she was discharged from rehab with a walking cane as a main mode of ambulation.
CONCLUSION: Elsberg syndrome is a rare cause of infectious lumbosacral radiculitis with a wide variety of clinical presentations and diagnostic criteria. A proposed diagnostic criteria of Elsberg syndrome includes clinical signs and symptoms of caudal equina syndrome, such as urinary/ bowel retention, hesitancy, or incontinence, and MRI or electrophysiologic evidence of cauda equina involvement. Other features that may be suggestive of Elsberg syndrome include preceding genital herpes infection, herpes virus infection in the CSF, clinical or radiographic evidence of myelitis in the conus, acute/subacute onset, and CSF pleocytosis. Our patient met several of the proposed diagnostic criteria as she reported urinary retention, had CSF positive for HSV2, and had MRI evidence of cauda equina involvement as seen on the second MRI taken five days after admission. Additionally, the acute onset of her symptoms and CSF pleocytosis further supported her diagnosis.
Antiviral treatment may affect symptom duration, but there is no evidence it helps with neurologic improvement in herpetic radiculomyelitis. Our patient was started on IV Acyclovir for a total duration of 21 days and received 5 days of high dose corticosteroids. Steroids were initiated to reduce inflammation, and after receiving three days of steroids, the patient began to see improvement in her symptoms. Being cognizant of Elsberg syndrome while treating patients with signs and symptoms of lumbosacral radiculitis is crucial as initiating IV acyclovir for 10-14 days along with corticosteroids is regarded as a treatment of choice due to the possibility of shortening symptoms duration and improving overall morbidity
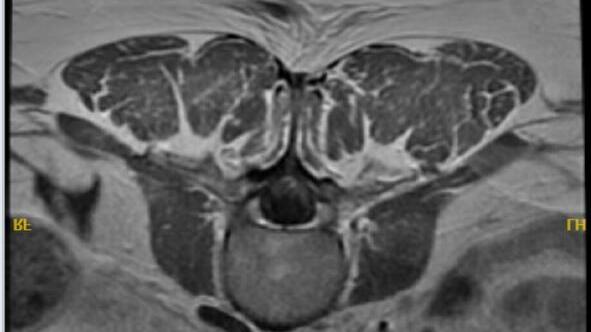 Figure 1: Repeat MRI whole spine w/wo contrast demonstrating a linear enhancement in the dorsal aspect of the thecal sac from L2 to L4
Figure 1: Repeat MRI whole spine w/wo contrast demonstrating a linear enhancement in the dorsal aspect of the thecal sac from L2 to L4
138
ABSTRACT #76 CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
PREDICTORS OF RESPONSE TO NEOADJUVANT CHEMOTHERAPY IN BREAST CANCER: ONCOTYPEDX VERSUS MAMMAPRINT VERSUS LIQUID BIOPSY
Nadeem Bilani1, Mira Itani2, Mohamed Mohanna3, Neha Debnath1, Barbara Dominguez2, Hong Liang2 , Zeina Nahleh3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Cleveland Clinic, Weston, FL, United States; 3Cleveland Clinic, Fort Lauderdale, FL, United States Presented at the San Antonio Breast Cancer Symposium that was held in San Antonio, Texas, United States from December 6-10, 2022
BACKGROUND/INTRODUCTION: OncotypeDX (ODX) is a 21-gene recurrence score (RS) assay that is predictive of the benefit of adjuvant chemotherapy in early-stage hormone receptor-positive and HER2-negative (HR+/HER2-) breast cancer. MammaPrint (MP) is a 70-gene signature validated to prognosticate distant metastasis and survival. We have previously presented data suggesting that the presence of circulating tumor cells (CTCs) evaluated via liquid biopsy may also have prognostic and predictive utility in HR+/HER2- breast cancer. In this study, we compare the value of ODX, MP and liquid biopsy evaluating CTCs and disseminated tumor cells (DTCs) in predicting pathologic complete response (pCR) following neoadjuvant chemotherapy (NAC).
METHODS: This retrospective analysis used the National Cancer Database (NCDB) 2004-2017 breast cancer dataset to identify a cohort of patients with HR+/HER2-, AJCC clinical stage I-III breast cancer who received NAC. A series of multiple logistic regression models were used to assess the value of a. ODX (RS < 26 versus ≥26), b. MP, c. the presence of CTCs, and d. the presence of DTCs in predicting pCR to NAC. Each model controlled for age, race, Charlson/Deyo comorbidity scoring, disease histology, grade, and nodal status.
RESULTS: A total of n=52,463 patients with stages I-III HR+/HER2- breast cancer received NAC. The patient characteristics of this cohort were as follows: the majority were White (n=42,826, 81.6%), between 50-70 years of age (n=27,683, 52.8%), and with invasive ductal carcinomas of the breast (n=40,197, 76.6%). N=6,111 (11.6%) had Grade I or well-differentiated disease, n=23,546 (44.9%) Grade II or moderately-differentiated disease, and n=2,605 (43.5%) had Grade III or poorly-differentiated disease. N=3,823 have documented recurrence scores based on ODX: with n=2,653 having RS < 26 (69.4%) and n=1,170 (30.6%) having RS ≥26. After controlling for age, race, comorbidity scoring, disease histology, grade and nodal status, RS ≥26 was found to be significantly associated with pCR to NAC (OR, 1.85; 95% CI, 1.46-2.35; p< 0.001). High-risk scoring per MP was also correlated with pCR but this relationship was not statistically-significant (OR, 1.68; 95% CI, 0.933.03; p=0.084), possibly due to the smaller size of this sample (n=828 patients underwent MP testing). Liquid biopsy data was also limited, with n=250 patients havingdocumented CTC status and n=211 havingdocumented DTC status. Neither the presence of CTCs (OR, 0.96; 95% CI, 0.44-2.09; p=0.908) nor DTCs (OR, 0.61; 95% CI, 0.25-1.50; p=0.279) was significantly associated with pCR to NAC.
CONCLUSION: ODX is found to be predictive of pCR to NAC in early-stage, HR+/HER2- breast cancer. Utility of MP and liquid biopsy data in this context appears less robust, however, data is limited. More research is needed to validate existing data in a prospective trial setting, and explore for novel biomarkers across breast cancer subtypes.
139
ABSTRACT #77 CLINICAL RESEARCH GASTROENTEROLOGY
DEGREE OF INEFFECTIVE PERISTALSIS DOES NOT AFFECT FREQUENCY OF GASTROESOPHAGEAL REFLUX, BUT MAY FACILITATE MORE PROXIMAL REFLUX EVENTS
Christy Chon1, Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Chicago Classification v4.0 (CC4) describes more stringent criteria for Ineffective Esophageal Motility (IEM), in order to identify patients with clinically significant dysmotility. IEM is a common finding in patients with gastroesophageal reflux disease (GERD). The aim of this study was to evaluate whether patients meeting CC4 IEM criteria also have more severe reflux, as defined by worse outcomes on 24hour multichannel intraluminal impedance-pH testing (MII-pH).
METHODS: A total of 684 patients undergoing GERD evaluation with MII-pH at a single high-volume center between 2019-22 were identified. Patients were included only if they had a diagnosis of either no CC4 abnormality or IEM based on either Chicago Classification v3.0 (CC3) or CC4. For the analysis, patients were divided into three groups: 50-69.9% ineffective swallows (CC3-only IEM), 70-100% ineffective swallows or at least 50% failed swallows (CC4 IEM), and no CC3/CC4 diagnosis (Controls). Demographic data and MII-pH results were collected and analyzed.
RESULTS: Of 153 patients that met criteria, 29 had CC3-only IEM, 98 had CC4 IEM, and 26 were Controls. Age, gender, body mass index and tobacco/alcohol use were similar among groups. The mean total number of normalized reflux events actually was higher in the CC3-only IEM group (66.9) than for CC4 IEM (49.5) and Controls (51.9), but this was not significant (p=0.61 between all groups, p=0.91 between CC3-only IEM versus CC4 IEM). The mean number of proximal reflux episodes was higher for CC4 IEM patients (18.9) than CC3-only IEM patients (9.3) and Controls (6.3), though this also did not reach significance (p=0.23). Both acid exposure times (AETs) and DeMeester scores were higher in IEM patients compared to controls, but the differences also were not significant.
CONCLUSION: The degree of ineffective peristalsis did not affect the overall number of reflux events seen on MII-pH. This finding is expected, as peristalsis is not thought to be involved in the generation of a reflux event. A trend toward more proximal reflux events in patients meeting CC4 criteria suggests a higher degree of esophageal dysmotility increases the likelihood reflux events are not cleared effectively, and therefore have a greater opportunity to move retrograde. Extended refluxate exposure may predispose to worsened symptoms. Future studies focusing on refluxate exposure times and symptom correlation may provide significant conclusions leading to improved care of these patients with dysmotility.
140
ABSTRACT #78 CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
DEMOGRAPHIC DISPARITIES IN CLINICAL TRIAL ENROLLMENT OF US PATIENTS WITH NEWLYDIAGNOSED MULTIPLE MYELOMA
Bruno Almeida Costa1 , Raphael de Oliveira Bertasi1 , Neha Debnath1 , Adriana Rossi2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that will be held in Chicago, Illinois, United States from June 2-6, 2023.
BACKGROUND/INTRODUCTION: By the time cancer therapies reach later stages of clinical development, study populations should ideally reflect the real-world disease population as much as possible. Enrollment disparities have been a limiting factor for the real-world reproducibility of multiple myeloma (MM) clinical trials, with prior analyses mostly focusing on patients with relapsed/refractory disease. To further assess this gap, we conducted a cross-sectional analysis of US demographic representation in newly-diagnosed MM (NDMM) trials.
METHODS: We systematically searched PubMed, Embase, and Cochrane library from January 1, 2010 to December 31, 2022 for completed phase 2 and 3 clinical trials involving NDMM patients and reporting an enrollmentperiod between January 2008 and December 2019. Studies includingrelapsed/refractory MM or other malignancies, with an intention-to-treat population <45 patients, or with patient recruitment outside of the US were excluded. Following determination of incident MM cases from 2008-2019 using SEER 22, an enrollment fraction (EF; number of trial participants divided by the estimated US cases) was calculated for each subgroup. EF was then compared between subgroups using odds ratios (OR), with a p-value<0.05 deemed significant. Statistical analysis was performed with SPSS version 19.
RESULTS: A total of 18 trials met criteria for inclusion (n=4,606). Women showed a significantly lower EF compared to men [OR, 1.12; 95% confidence interval (CI]) 1.05-1.19; p=0.0007]. Among the 12 (67%) trials reporting race data, EF was significantly lower for Black patients compared to White patients (OR, 1.39; 95% CI, 1.26-1.55; p<0.0001). Among the 4 (22%) trials reporting ethnicity data, EF was significantly lower for Hispanics (OR, 0.07; 95% CI, 0.05-0.09; p<0.0001) compared to non-Hispanics. Furthermore, phase 3 trials had similar odds of including race data (p=0.71) or ethnicity data (p=0.89) compared to phase 2 trials.
CONCLUSION: In conclusion, our study reveals an alarming underrepresentation of women, Hispanics, and African Americans in NDMM trials conducted in the US, similar to prior studies involving relapsed/refractory patients. In order to improve external validity and mitigate ascertainment bias, future phase 2 and 3 clinical trials of frontline anti-myeloma therapies must include a more representative sample of the US population affected by this hematologic malignancy.
141
ABSTRACT #79 CLINICAL RESEARCH HEMATOLOGY/ONCOLOGY
NON-VITAMIN K ORAL ANTAGONISTS VERSUS ASPIRIN FOR PRIMARY THROMBOPROPHYLAXIS IN PATIENTS WITH MULTIPLE MYELOMA ON OUTPATIENT CHEMOTHERAPY: A SYSTEMATIC REVIEW AND META-ANALYSIS
Thomaz Alexandre Costa1 , Bruno Almeida Costa2, Nicole Felix4, Amanda Godoi5, Alleh Nogueira6, Joshua Ryan Richter7, Adriana Rossi7
1Federal University of Ceará, Fortaleza, Brazil; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY; 4Federal University of Campina Grande, Campina Grande, Brazil; 5Cardiff University School of Medicine, Cardiff, United Kingdom; 6Bahia School of Medicine and Public Health, Salvador, Brazil; 7Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY
To be presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that will be held in Chicago, Illinois, United States from June 2-6, 2023.
BACKGROUND/INTRODUCTION: Patients with multiple myeloma (MM) are at an elevated risk of venous thromboembolism (VTE), which is further increased in patients receiving immunomodulatory drugs (IMiDs). Current guidelines suggest that non-vitamin K oral anticoagulants (NOACs) may be an alternative to low-dose aspirin (ASA) for primary thromboprophylaxis in this population. However, there is limited data comparing these two antithrombotic therapies among MM patients undergoing treatment with IMiDs.
METHODS: We performed a systematic review and meta-analysis to compare NOACs with ASA for primary thromboprophylaxis in individuals with newly-diagnosed or relapsed/refractory MM undergoing outpatient chemotherapy with an IMiD-based regimen. PubMed, Cochrane, and EMBASE were systematically searched from inception to January 2023. Observational studies and randomized controlled trials were included when comparing NOACs versus aspirin for thrombotic and hemorrhagic outcomes. Statistical analysis was performed with Review Manager 5.4.1.
RESULTS: We included 10 randomized controlled trials and observational studies comprising 1026 MM patients who underwentprimary thromboprophylaxis with NOACs (33%) or ASA(67%). Thromboprophylaxis with NOACs was associated with a significantly lower incidence of VTE compared with ASA (OR, 0.33; 95% CI,0.16-0.68; p< 0.001; I² = 0%). Each group had one major bleeding event, with no statistically significant difference between NOACs and ASA (OR, 1.35; 95% CI,0.05-35.51; p=0.86; I²=51%). Similarly, clinically relevant non-major bleeding (OR,0.56;95% CI, 0.12-2.70; p=0.47; I² = 0%) and minor bleeding(OR 1.48; 95%CI: 0.42-5.24; p=0.54; I² = 0%) event rates did not differ significantly between groups.
CONCLUSION: These findings suggest that NOACs may be superior to ASA for VTE prophylaxis among MM patients receiving IMiD-based chemotherapy, with no significant difference in the overall bleeding risk between the two groups.
142
ABSTRACT #80 MEDICAL EDUCATION
PALLIATIVE CARE MEDICINE
EVALUATINGMEDICAL RESIDENT’SCOMFORT AND KNOWLEDGEON CARING FOR PATIENTSAT THE END OF THEIR LIFE
Fionnuala Crowley1, Neha Dabnath1, Sonal Gandhi1, Yosef Joseph Rene Amel Riazat Kesh1 , Jennifer Fung1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
BACKGROUND/INTRODUCTION: A number of studies have highlighted that residents generally across a number of specialties are uncomfortable with end of life discussions. One study from a single institution found that 88.1% of 175 residents surveyed had no formal classroom training in conducting goals of care discussions despite having these conversations frequently. This needs assessment aims to identify knowledge and skills deficits when caring for patients at the end of life.
METHODS: Surveys were distributed to residents at the Mount Sinai Morningside/West Internal Medicine Residency program. Surveys were emailed, distributed by text, and also distributed to documentation rooms. Analysis was descriptive and was done using SPSS.
RESULTS: 36 residents completed the needs assessment (response rate 30%). 17 (47.2%) were PGY-1s, 6 (16.7%) were PGY-2s, 13 (36.1%) were PGY-3. When asked how much classroom teaching they had received during residency on EOL discussions the responses were as follows: “None” (10, 27.8%), “Very little” (1-2 lectures) (21, 58.3%), “Some” (1-2 week course or lecture series) (4, 11.1%), “A Lot” (>3 weeks) (0, 0.0%), “I don't know” (1, 2.8%). When asked how often they have had EOL discussions during residency 2 (5.7%) said “none”, 8 (22.9%) said “1-5 times” , 7 (20.0%) said “6-10 times”, 5 (14.3%) said “11-15 times”, 3 (8.6%) said “1625 times”, 6 (17.1%) “26-50 times” and 4 residents said “greater than 50 times.” Twenty residents (57%) responded that most of these conversations were unsupervised. 22.9% said they learned how to conduct these conversations through “trial and error’, 25.7% from watching attendings conduct conversations, 31.4% from sitting in on family meetings. When asked about their comfort levels having these conversations there was a lot of variation: “I feel very comfortable” (8,23.5%), “I feel mostly comfortable” (11, 32.4%), “Iam neither comfortable nor uncomfortable” (7, 20.6%), “I feel mostly uncomfortable” (6, 17.6%), “I feel very uncomfortable” (1, 2.9%), “I'm not sure” (1, 2.9%). 4 (11.8%) of respondents felt lack of adequate supervision or training for end-of-life discussions negatively impacted patients care often while 17 (50%) said it sometimes did. Discomfort with patient/ families’ reaction or emotions (17, 48.6%) was cited as the biggest barrier to being honest with families about the likely outcomes of CPR/trial of critical care. Teaching during rotations was the more preferred method of teaching delivery for this content (60%), followed by small group workshops (42.9%).
CONCLUSION: There needs to be additional teaching around conducting end of life discussions in the Internal Medicine curriculum. Over 50% of residents felt a lack of adequate supervision or training for end-of-life discussions negatively impacted patients care. In addition to knowledge and communication skills teaching residents would also benefit from teaching on managing emotional reaction to bad news and emotionally supporting patients and their families.
143
ABSTRACT #81 CLINICAL RESEARCH CARDIOLOGY
UTILIZATION PRESENCE AND SEVERITY OF SUBCLINICAL ATHEROSCLEROTIC DISEASE IN THE PRIMARY PREVENTION OF THE ONCOLOGIC POPULATION
Sara Diaz Saravia1, Renzo Melchiori2, Szlaien Lucas2, Romina Mourino2, Pablo Rubio2, Mateo Bivort2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Hospital Universitario Austral, Unidad Coronaria, Buenos Aires, Argentina
Presented at the New York American College of Cardiology Annual Meeting on December 9, 2022 and at the Inaugural Mount Sinai Heart Research Forum on February 22, 2023 that were both held in New York, NY, United States.
BACKGROUND/INTRODUCTION: There is scanty evidence regarding endothelial dysfunction and damage in patients with a history of cancer in cardiovascular primary prevention, and the impact in the development of subclinical atherosclerotic disease (SCASD).
METHODS: A cross-sectional study was carried out on a registry of patients enrolled in primary prevention who underwent a Doppler ultrasound (D-US) screening for SCASD in the carotid and ileo-femoral territory from September 2020 to April 2022. Inclusion criteria: Patients between 35- 75 years old. Exclusion criteria: Previous cardiovascular and/or cerebrovascular event. History of cancer was defined as active or remitted cancer excluding basal cell and squamous cell carcinoma. The population was divided in two according to this criteria, G1: non-oncologic group; G2 oncologic group. SCASD was defined as the presence of ≥1 atherosclerotic plaque in the carotid and/or ileofemoral territory according to the Mannheim Consensus. Univariate and bivariate analysis were performed to establish population characteristics.Several adjustment models were manually made comparing oncological history and the presence and distribution of the SCASD.
RESULTS: A number of 5209 patients were included: 5071 in G1 and 138 in G2 (97.4 versus 2.6%). G2 patients were older, mostly women, and had more prevalence of hypertension. The rest of the characteristics are detailed in Annex 1. A linear regression analysis was done to assess the total plaque area in relation to the oncological history, adjusted for age, sex, smoking history, dyslipidemia, diabetes, and hypertension. The result shows that history of cancer increases significantly the total plaque area by an average of 8 mm [Coeff 8.2; p=0.045; 95% CI, 0.2-16, adjusted R2 = 0.32].
CONCLUSION: In our population, the prevalence of oncologic disease in the cardiovascular primary prevention was 2.6%.Patients with history of cancer presentedmore SCASD with greater area, behavingas an independent risk factor for the increase in total plaque area adjusted for classic risk factors. These findings raise the need for more intensive control of SCASD in cancer patients. More studies are needed to verify these findings, as well as to clarify the pathophysiological mechanisms. The prevalence of oncologic disease in our cardiovascular primary prevention was 2.6%. Patients with history of cancer presented more SCASD, behaving as an independent risk factor for an increase in total plaque area adjusted for classic risk factors. These findings raise the need for more intensive control of SCASD in cancer patients. More studies are needed to verify these findings, and clarify the pathophysiological mechanisms.
144
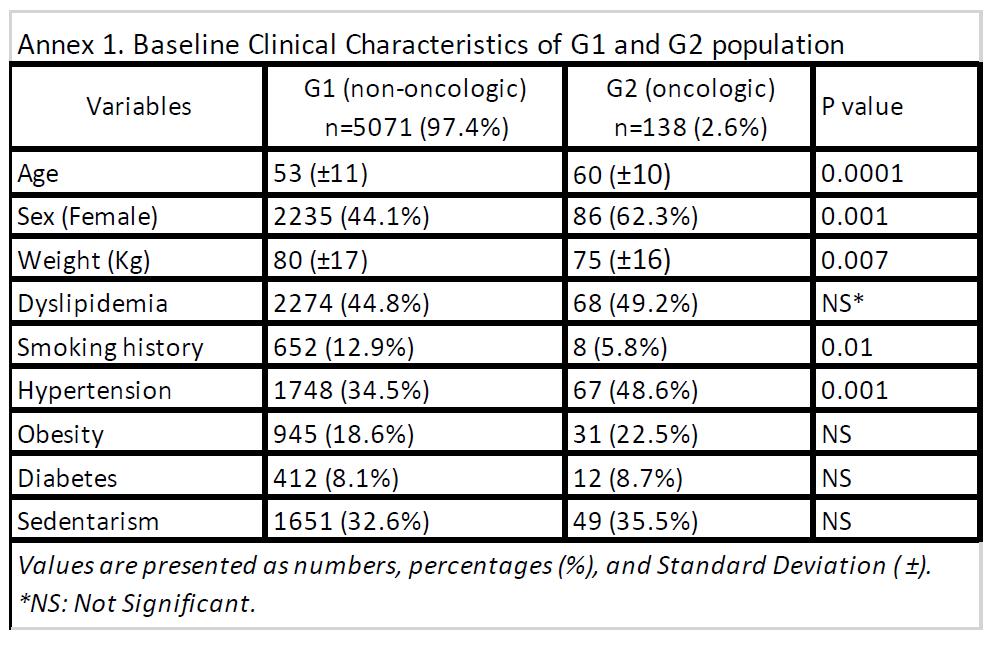
145
ABSTRACT #82
CLINICAL RESEARCH CARDIOLOGY
PROGNOSTIC SIGNIFICANCE OF MYOCARDIAL ISCHEMIA DURING EXERCISE IN PATIENTS WITH NON-OBSTRUCTIVE CORONARY DISEASE COMPARED TO PATIENTS WITH NORMAL EXERCISE ECHO
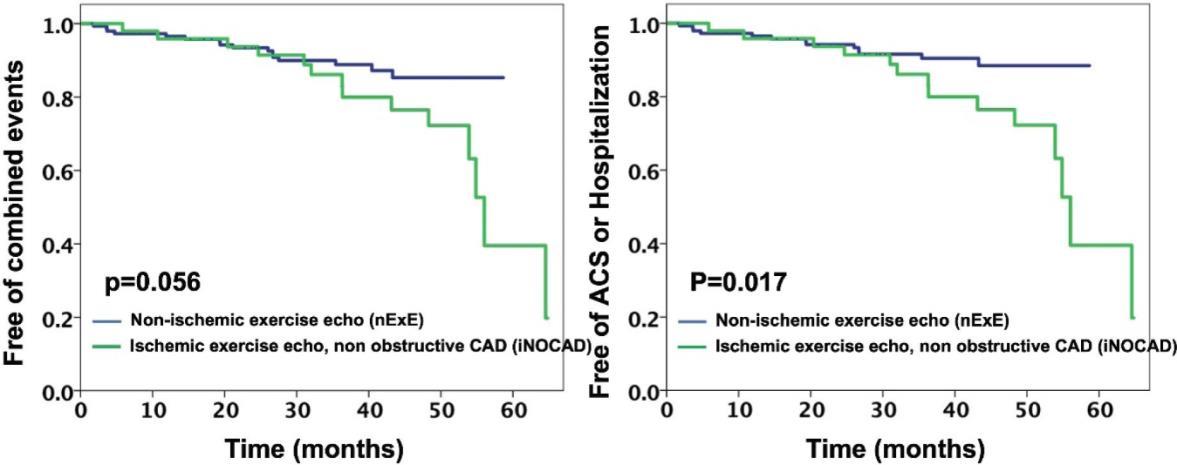
Ga Hee Kim1 , Alaa Omar1, Swiri Konje1, Loba Alam1 , Joseph Elias1, Elizabeth A. Zipf1, Christopher Perez Lizardo1, Maria K. Peña1, David Miester1, Errol C. Moras1, Kruti Dhaval Gandhi1, Arpanjeet Kaur1, Brissete Mancero1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
BACKGROUND/INTRODUCTION: Ischemic stress echocardiogram (ExE) in the absence of obstructive coronary disease (CAD) is controversial. We compared clinical risk between myocardial ischemia on ExE who had non-obstructive CAD with non-ischemic ExE.
METHODS: Between 2017 and 2020, symptomatic patients with ischemic ExE and invasive evidence of nonobstructive CAD (iNOCAD) and matched non-ischemic controls (nExE) were included and followed (median 3.3 years) for death, acute coronary syndrome (ACS), and non-ACS cardiac hospitalization.
RESULTS: We studied 50 iNOCAD patients [age: 68±9 year, 23(46%) women, EF: 56 ± 6%]. 1:3 propensity score matching was done for nExE and iNOCAD for age, sex, risk factors, exercise tolerance, LV functions, and medications, and yielded 150 nExE patients [age: 65 ± 12 year, 64 (43%) women, EF: 59 ± 6%]. iNOCAD and nExE were similar in death [1(2%) versus 3(2%), p=1.00], but, more iNOCAD had ACS [3 (6%) versus 1 (1), p=0.02] and hospitalizations [12 (24%) versus 12 (9%), p=0.003]. Compared to nExE, combined events [14 (28%) versus 16 (11%), p= 0.003] as well as combined ACS and non-ACS hospitalizations [13 (26%) versus 14 (9%), p=0.001] were more frequent in iNOCAD. Overall, iNOCAD was associated with elevated risk for combined events (HR, 2.0; 95% CI, 0.97 - 4.2) and combined ACS and cardiac hospitalizations (HR, 2.5; 95% CI, 1.15.4).
CONCLUSION: Myocardial ischemia despite non-obstructive CAD carries an elevated clinical risk necessitating medical optimization and close follow-up for disease progression.
146
ABSTRACT #83 MEDICAL EDUCATION CARDIOLOGY
EVALUATING THE EFFECTIVENESS OF VIRTUAL DIDACTIC SESSIONS VERSUS SMALL GROUP SIMULATION-BASED SESSIONS FOR MASTERING RIGHT VENTRICULAR FUNCTION ASSESSMENT WITHIN A POINT-OF-CARE ULTRASOUND CURRICULUM
Kruti Dhaval Gandhi1, Errol Moras1, Arpanjeet Kaur1, Yoni Balboul1, Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
BACKGROUND/INTRODUCTION: Point-of-care ultrasound (POCUS) is an invaluable tool for rapidly assessing patients in a variety of bedside clinical situations. The aim of the study is to determine whether a virtually delivered didactic POCUS session can be as effective as a small-group in-person simulation center-based session for improving learner competency in assessing right ventricular (RV) function.
METHODS: The virtual didactic sessions were 2 hour-long zoom sessions for interns and residents and included pretest and posttest questionnaires. The in-person simulation sessions occurred twice weekly over eight weeks consisting of pretest and posttest surveys, a didactic lecture, case-based simulation scenario, and a debrief discussion. The survey questions consisted of cardiac US clips evaluated by 3 POCUS experts. Effect size as the percent of correct responses was calculated. Data was analyzed using SPSS with a level of statistical significance as p≤0.05.
RESULTS: For the small group simulation sessions, 40 interns and 45 residents were included. 40% of interns and 68.9% of residents correctly identified the RV pre-lecture, improving to 95% and 95.6% respectively, afterward. 57.5% of interns and 91.1% of residents correctly identified etiology of shock pre-lecture, improving to 85% and 97.8% respectively afterward. 62.5% of interns and 75.6% of residents correctly described normal RV characteristics pre-lecture, improving to 77.5% and 82.2% respectively, afterward. 17.5% of interns and 48.9% of residents answered all 3 questions correctly in the pretest, improving to 62.5% and 78% respectively, afterward. These trends were statistically significant. The majority of interns pre-session reported no RV assessment knowledge (55.6%), and by the end of the session, 61.1% reported some knowledge. The majority of residents reported some familiarity with RV assessment pre-session (56.1%), and by the end of the session, 51.2% reported good knowledge. For the virtual sessions, 11 interns and 30 residents were included. 54.5% of interns and 60% of residents correctly sized the RV pre-lecture, improving to 90.9% and 93.3% respectively, afterward. 18.2% of interns and 63.3% of residents correctly described RV function pre-lecture, improving to 63.6% and 80% respectively afterward. 36.4% of interns and 40% of residents accurately described McConnell’s sign pre-lecture, improving to 90.9% and 90% respectively, afterward. 9.1% of interns and 25% of residents answered all three questions correctly pre-lecture, improvingto 63.6% and 71.9% respectively afterwards. These trends were not statistically significant.
CONCLUSION: This study showed similar trends with impressive and comparable results in the assessment of RVfunction amonginterns and residents in both styles of trainingsessions. This highlights the potential forvirtual didactic sessions to at least partially replace and obviate the need for small-group in-person sessions for basic POCUS training and comprehension. Future studies are needed to see the continued effectiveness of these methods longitudinally.
147
ABSTRACT #84 CLINICAL RESEARCH CARDIOLOGY
IMPACT OF FRAILTY ON OUTCOMES OF PERCUTANEOUS CORONARY INTERVENTION: INSIGHTS FROM THE NATIONWIDE INPATIENT SAMPLE
Kruti Gandhi1 , Errol Moras1 , Tais Bertasi1, Raphael Bertasi1, Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society for Cardiovascular Angiography and Interventions (SCAI) Annual Meeting that will be held in Phoenix, Arizona, United States from May 18-20, 2023.
BACKGROUND/INTRODUCTION: Patients with significant coronary artery disease require percutaneous coronary intervention (PCI). However, whether frailty has adverse outcomes in patients undergoing PCI has been controversial. We investigated the impact of frailty on the outcomes of patients who underwent PCI.
METHODS: We reviewed the National Inpatient Sample to identify patients that underwent PCI. Frailty was defined using the Johns Hopkins Adjusted Clinical Groups frailty-defining diagnoses indicator. Univariate and multivariate logistic regression analyses were performed to determine any association between frailty and the clinical outcomes.
RESULTS: From 2017-2020, 102,324 patients underwent PCI in the United States, and 7.3% met the criteria for frailty. We found that the frail group had longer lengths of stay (10 versus 4 days, p<0.001), and higher hospitalization costs ($266k versus $158k, p<0.001). After multivariate adjustment, we found that frailty was associated with increased in-hospital mortality, cardiogenic shock, increased vasopressor requirements, higher need for mechanical circulatory support, higher need for mechanical ventilation, increased incidence of postoperative stroke and post-operative sepsis, and increased risk of sudden cardiac death.
CONCLUSION: The presence of frailty in patients who underwent PCI was associated with significantly higher in-hospital mortality, longer lengths of stay, higher hospitalization costs, and worsening secondary outcomes. These findings may suggest the need for an alternative approach for frail patients who are indicated for revascularization.
148
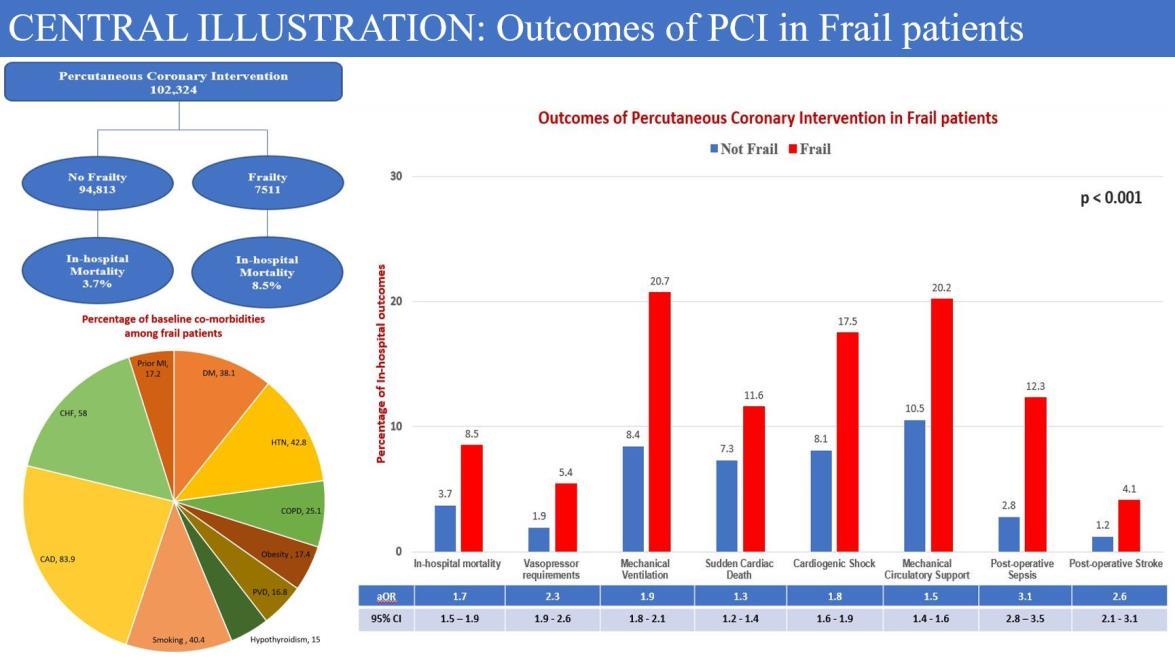
149
ABSTRACT #85
CLINICAL RESEARCH CARDIOLOGY
TEMPORAL TRENDS AND OUTCOMES OF HEART FAILURE PATIENTS BETWEEN LIGHT-CHAIN CARDIAC AMYLOIDOSIS AND TRANSTHYRETIN CARDIAC AMYLOIDOSIS: INSIGHTS FROM THE NATIONAL INPATIENT SAMPLE DATABASE
Kruti Gandhi1 , Errol Moras1 , Tais Bertasi1, Raphael Bertasi1, Nadeem Bilani1, Ashish Correa1, Kiran Mahmood1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Technology and Heart Failure Therapeutics (THT) Annual Meeting that was held in Boston, Massachusetts, United States from March 20-22, 2023.
BACKGROUND/INTRODUCTION: Data regarding the clinical outcomes in immunoglobulin light-chain (AL) versus amyloid transthyretin (ATTR) cardiac amyloidosis (CA) is scarce. We aimed to investigate the trends, baseline clinical characteristics, and clinical outcomes of AL CA versus ATTR CA in heart failure (HF) patients.
METHODS: Data from National Inpatient Sample database from 2017-2020 was used to identify hospitalizations for CA with concurrent cardiomyopathy in HF patients and were further subclassified into AL versus ATTR CA. Outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: During 2017-2020, there were 12430 hospitalizations of CA of which 96.3% were ATTR CA and 3.7% were AL CA. Patients with ATTR-CA when compared to AL-CA were older, predominantly male, more blacks, and had a higher prevalence of co-morbidities including atrial arrythmias, sick sinus syndrome, and aortic stenosis. Patients with AL CA had significantly increased in-hospital mortality, length of stay, total charges,acute heart failure exacerbations, and cardiopulmonary resuscitation. After adjustment for baseline characteristics, AL CA patients had significantly increased odds of in-hospital mortality and HF hospitalizations when compared to ATTR CA cohort. There is an increasing trend in hospitalizations in AL CA from 2017-2019.
CONCLUSION: AL cardiac amyloidosis had significantly higher odds of in-hospital mortality and HF hospitalizations in comparison to ATTR cardiac amyloidosis cohort. AL CA had lower incidence of stroke, thromboembolism and major bleeding with similar need for cardiac device implantation.
150
ABSTRACT #86 CLINICAL RESEARCH CARDIOLOGY
UNBIASED CLUSTER MODELLING FOR UNCOVERING NATURAL DISTRIBUTION OF DOPPLER DERIVED DIASTOLIC VARIABLE RESPONSE TO EXERCISE AMONG PATIENTS REFERRED TO EXERCISE ECHOCARDIOGRAPHY
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Exercise-induced diastolic dysfunction is associated with poor prognosis. We studied diastolic response to exercise based on the natural distribution of Doppler variables and its relationship to adverse outcomes.
METHODS: In a retrospective study, 813 patients referred for exercise echocardiography (ExE) for ischemia assessment were included (Age: 58 ± 13 years, 57% females, EF: 60 ± 7%). A 2-step unsupervised cluster model was constructed using resting and post-exercise tissue Doppler early diastolic mitral annular velocity, post-exercise pulsed Doppler-derived mitral inflow velocity in early and late diastole, and post-exercise tricuspid regurgitation velocity. Clusters were compared for a composite outcome (death, cardiac rehospitalization, acute coronary syndrome, and need for future ischemia testing).
RESULTS: Exercise-induced ischemia occurred in 116 (14%). The composite outcome occurred in 196 (24%) patients over a median follow-up of 3.2 years. The model yielded 2 clusters labelled low and high risk for the composite outcome, Figures 1A and 1B). Compared to the low risk cluster, patients in the high risk cluster were older, had more risk factors and comorbidities, worse exercise performance, worse resting and exercise diastolic variables, and more ischemic ExE. After stratification for ischemia, clusters resulted in significant separation of risk for the outcome, regardless of the presence or absence of ischemia (Figures 1C and 1D). These findings persisted after multivariate adjustment.
CONCLUSION: In patients referred to ExE for assessment of ischemia, diastolic response to exercise involves complex interactions among diastolic variables. Appreciation of such complexity seems to add prognostic value beyond ischemia, suggesting a need for novel approaches for characterization of the natural distribution of diastolic variables, such as computational unbiased clustering.
Alaa Omar1, Swiri Konje1, Loba Alam1 , Kruti D. Gandhi1 , Errol Moras1, Brissete Mancero1, Elizabeth Zipf1 , David Meister1, Maria K. Peña1, Christopher Perez Lizardo1, Ga Hee Kim1, Joseph Elias1, Edgar Argulian1
151
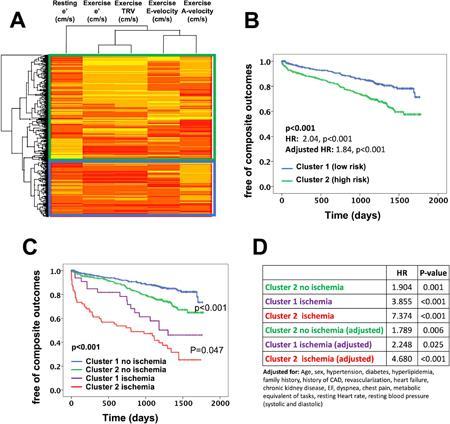
1: 152
Figure
ABSTRACT #87
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
COMMUNICATION SKILLS TRAINING CURRICULUM NEEDS ASSESSMENT FOR INTERNAL MEDICINE RESIDENTS
BACKGROUND/INTRODUCTION: ACGME recognizes interpersonal and communication skills as one of the six core competencies for Internal Medicine residency training. Studies have shown increased patient, family, and clinician satisfaction and better healthcare outcomes with effective communication. Despite compelling evidence suggesting the utility of a formal curriculum, it is often a hidden curriculum, acquired by observation and self-study. This project’s aim is to determine the perceived need for a formal curriculum by Internal Medicine residents and how to effectively address it.
METHODS: We created an anonymous survey for all Internal Medicine residents at various levels and assessed the following domains: prior training in communication skills for patients with serious illnesses, the frequency of difficult conversations, the level of perceived confidence in delivering serious news and complex goals of care discussion, and the importance of having a formal communication skills training.
RESULTS: There were 52 completed responses. The breakdown of responses are as follows: 48% PGY1; 25% PGY2; and 27% PGY3. Only a third (31%) of respondents reported any history of formal instruction in communication skills. The overwhelming majority (96%) reported having to deliver serious news and have complex goals of care and end-of-life discussions with patients at least once (the most common response being >10 times). Most respondents (62% and 73% respectively) reported having a confidence of 3/5 or lower (on a Likert scale with 5 as most confidence) in having both types of discussions. 93% of respondents agreed that communication skills training is essential. The most popular areas of further communication training included establishing goals of care and discussing grim or uncertain prognoses.
CONCLUSION: Our results demonstrate a clear unmet need for a formalized curriculum on difficult end-of-life conversations including prognostication. The next steps in the project will be recruiting and training volunteer communication champions and designing a series of case-based small-group teaching and simulation sessions for residents during academic half-days with a pre-test and post-test assessment.
Sonal Gandhi1, Yosef Joseph Rene Amel Riazat-kesh1, Fionnuala Crowley1, Vasundhara Singh1, Noelle Javier1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
153
ABSTRACT #88
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
ASSESSMENT OF POST-PROCEDURAL COMPLICATIONS IN THE INPATIENT SETTING: IMPLEMENTATION OF A STANDARDIZED COMPREHENSIVE DOCUMENTATION TOOL
Kristine Lou Gargaritano1, Irina Zaretsky1 , Shantheri Shenoy1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
BACKGROUND/INTRODUCTION: Bedside procedures such as paracentesis, lumbar puncture, and thoracentesis are commonly performed on the general medicine wards by house staff, advanced practice providers, and attending physicians. While such procedures are considered safe and cost effective, lack of prompt detection of serious complications can have life threatening implications. We aim to promote patient safety in the post procedural period by performing timely and comprehensive assessment of patients through a standardized approach. Our goal is to improve provider compliance with evaluation of patients at 4 to 6 hours post procedures. We plan to analyze the post procedure complication detection rate and the effects of medical interventions implemented on patient outcomes.
METHODS: Our team designed a standardized template note within our electronic medical record (EMR) system to guide comprehensive post procedure patient assessments. The template is available to all providers within the Department of Medicine. The template prompts providers to document the following: time of assessment procedure-related symptoms, a detailed physical examination, relevant labs and imaging, any post-procedural complications, a follow-up plan, and confirmation of the plan of care communication with nursing staff as well as the patient or the patient’s health care proxy. Educational sessions are currently being conducted within the Department of Medicine to promote provider awareness and compliance with the utilization of our template.
RESULTS: Patient charts are being reviewed following the formal educational interventions to assess for compliance with the post procedure template. Our initial analysis will include the following data (from March 2023): all patients who have a regular procedure note in their chart, all patients with post-procedure notes in their chart. We intend to analyze the frequency at which procedures performed, when these procedures were performed relative to the timing of provider assessments, which complications have been identified by house staff and any subsequent actions taken. This data analysis is set to take place starting in April 2023. While our research is still ongoing, we hypothesize that systematic post-procedure patient evaluations will allow for early detection of complications, prompt intervention, and improvement in patient outcomes.
CONCLUSION: We hypothesize that systematic post-procedure patient evaluations will allow for early detection of complications, prompt intervention, and improvement in patient safety and outcomes.
154
ABSTRACT #89
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE PULMONARY/CRITICAL CARE
STATUS ASTHMATICUS COMPLICATED BY RHABDOMYOLYSIS
Satwant Grewal1, Tal Shachi1,2, Pavan Paka3, Sara Luby1, Arpanjeet Kaur1, Patrick Tobin-Schnittger1 , Vincent Courant1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
3Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
Presented at the CHEST Annual Meeting that was held in Nashville, TN, United States from October 16-19, 2022.
BACKGROUND/INTRODUCTION: Rhabdomyolysis in the setting of status asthmaticus is a rare but potentially fatal complication. The hallmark of rhabdomyolysis is an elevation in serum creatine phosphokinase (CPK) secondary to muscle necrosis, which may be categorized as: traumatic, nontraumatic exertional, and nontraumatic non-exertional. We report a case of a rhabdomyolysis in the setting of status asthmaticus, neuromuscular blockade, and steroid use.
CASE PRESENTATION: A 21-year-old male with a history of asthma presented with respiratory distress, tachypnea, and tachycardia. Physical exam revealed diffuse bilateral wheezing and accessory muscle use. ABG revealed a pH of 7.11 and a PCO2 of 101.9 mmHg. Despite treatment with multiple nebulizers, systemic steroids, magnesium, and intramuscular epinephrine, he required tracheal intubation for acute hypercarbic respiratory failure due to status asthmaticus. He was sedated with fentanyl and midazolam. Due to ventilator dyssynchrony, continuous neuromuscular blockade with cisatracurium was initiated. High dose methylprednisolone and continuous albuterol nebulization was initiated in the ICU. On day 3 of admission, the patient was found to have a CPK level of 20,123 U/L suggestive of rhabdomyolysis. There was no evidence of trauma or compartment syndrome Due to concern for medication induced rhabdomyolysis, cisatracurium was discontinued and methylprednisolone was rapidly tapered, and CPK levels subsequently decreased after peaking at 20,253 U/L. Intravenous fluids were continued to maintain hydration. He continued to clinically improve and was successfully extubated on the 10th day of admission and eventually discharged with pulmonary follow-up.
DISCUSSION/CONCLUSION: Rhabdomyolysis in the setting of status asthmaticus has several possible etiologies. Status asthmaticus leading to hypercapnia results in a respiratory acidosis while also preventing carbon dioxide and oxygen exchange within muscle tissue causing muscular hypoxia and necrosis. This may be further complicated by increased exertion of the respiratory muscles. Rhabdomyolysis resulting from the combination of corticosteroids and neuromuscular blocking agents is rare. Although steroid use may lead to glucocorticoid myopathy, it is uncommon to have elevations in CPK. However, when steroids are concomitantly used with neuromuscular blocking agents, patients are at increased risk of developing critical illness myopathy and elevations in CPK. The patient's subsequent decline in CPK after cisatracurium was discontinued and systemic steroids were significantly reduced leads us to believe that the combination of these medications was the likely precipitant to this patient's rhabdomyolysis.
155
ABSTRACT #90 CLINICAL RESEARCH GASTROENTEROLOGY
THECORRELATION BETWEEN EARLY ENDOSCOPYAND IN-HOSPITAL OUTCOMESIN PATIENTS WITH UPPER GI MALIGNANCIES ADMITTED FOR UPPER GI BLEEDING
Suhail Haddadin1, Patricia Miguez Arosemena1, Farah Haddadin2 , Rand Fram2, Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2The University of Jordan, Amman, Jordan
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Upper gastrointestinal bleeding (UGIB) in the setting of UGI malignancies is challenging due to friable vasculature. Data on the role of esophagogastroduodenoscopy (EGD) remains limited on improving overall outcomes. New therapeutics are now available to achieve hemostasis during EGD such as Hemospray which prompts promising outcomes for early interventions. The goal of this report was to investigate whether early EGD in cancer related UGIB improves overall in-hospital outcome using a large representative database.
METHODS: Using the National Inpatient Sample, we examined patient characteristics and predictors for inhospital outcomes for patients with UGI malignancies (esophagus to stomach) admitted with UGIB stratified based on undergoing early EGD (≤ 24 hours) vs not during 2016. In-hospital outcomes of interest were all-cause mortality, need for blood transfusion, invasive mechanical ventilation, length of stay and total hospital charge. Multivariate analysis was used to predict in-hospital outcomes stratified based on undergoing early EGD after adjusting for baseline characteristics, Charlson comorbidity index, day of admission during the week and medical comorbidities.
RESULTS: In our retrospective study, a total of 1,935 patients with UGI malignancy were admitted for UGIB in 2016, of which 695 (35.9%) underwent early EGD. Patients who underwent early EGD when compared to patients who did not had similar demographic, racial and medical comorbidities baseline characteristics. On Multivariate analysis, Early EGD patients were more likely to require blood transfusion (OR, 1.77; 95% CI, 1.092.85; p=0.020). There was a trend towards lower all-cause mortality in patients undergoing early EGD, but it did not reach statistical significance (OR, 0.48; 95% CI, 0.12-1.91; p=0.304). There was no significant difference in the requirement of invasive ventilation (OR, 0.58; 95% CI, 0.05-6.23; p=0.654), length of stay (Coef., -0.41; 95% CI, -1.16-0.34) and total hospital charge (Coef., -2.38; 95% CI, -1.07-5.97; p=0.576).
CONCLUSION: Early EGD did not show improved all-cause mortality rate for patients with UGI cancer who have UGIB, but showed increased requirement for blood transfusion which possibly indicates more severe bleeding and more vigilant anticipation of complications. This study preceded the approval of new therapeutics such as Hemospray, which was approved in the US in 2018, and raises the question whether outcomes would improve after further utilization of newer therapeutic innovations.
156
ABSTRACT #91
CLINICAL RESEARCH ENDOCRINOLOGY/GENERAL INTERNAL MEDICINE
CHANGES IN GLYCEMIC CONTROL AND BODY WEIGHT OVER THE COURSE OF THE COVID-19 PANDEMIC IN AN URBAN OUTPATIENT SETTING
Keerthana Haridas1, Deborah Edelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Aurora, Colorado, United States from May 10-13, 2023.
BACKGROUND/INTRODUCTION: The COVID-19 pandemic has altered health outcomes in populations through a hostofdownstream social, economic, andpsychological changes, especially amongthose withchronic non-communicable diseases (NCDs). Some studies reveal worsened glycemic control and weight gain, while others indicate improved glycemic control and weight loss. Thus, evidence demonstrates conflicting results in this context. We aimed to conduct a study to explore changes in these metrics in an outpatient setting providing for an underserved population.
METHODS: We conducted a single-site observational study at a Federally Qualified Health Center (FQHC) in New York City to compare glycemic control and body weight, measured by Hemoglobin A1c (HbA1c) and body mass index (BMI) respectively, before and after the onset of the COVID-19 pandemic.
RESULTS: After the pandemic, there was a 103% increase in the annual change in average HbA1c from the years prior to the pandemic versus from early 2020 to2021 (p<0.005). Mean BMI increased duringthe pandemic, although this was not statistically significant. The slope for the change in BMI over five years prior to the pandemic is -0.09, while the slope of change in BMI before and after the onset of COVID-19 is 0.31. The difference between the two slopes is 0.48 (p=0.37).
CONCLUSION: Our study reveals that the COVID-19 pandemic may have led to a worsening in the status of metabolic disorders due to decreased physical activity, worsened dietary habits, psychosocial stressors, and reduced access to healthcare, emphasizing the need for enhanced medical, pharmaceutical and emotional support. Concurrently, many individuals practiced healthier lifestyles via dietary and activity modifications, with an improvement in cardio-metabolic parameters. Given the need for limited data of this type in the United States and conflicting data from other parts of the world, it can be concluded that there is a need to explore changes in healthcare outcomes in patients with non-communicable diseases occurring due to downstream effects of the pandemic.There is indeed a pressingrequirement to provide continued support to patients with chronic disorders through telemedicine, access to medications, improved access to laboratories or facilities for the collection of samples from home as well as continued emotional support during a pandemic to prevent acute and chronic complications and to decrease the burden on the healthcare system.
157
ABSTRACT #92
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
DIFFICULT CONVERSATIONS AND EFFECTIVE COMMUNICATION TRAINING FOR INTERNAL MEDICINE RESIDENTS UTILIZING HIGH FIDELITY SIMULATION
Ariela Hazan1 , Jeeyune Bahk1, Ariel Gordon1, Neha Debnath1, Harrindra Seepersaud1, Donna Gormley1 , Priscilla Loanzon1 , Adam Rothman1, James Salonia1, Susannah Kurtz1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
BACKGROUND/INTRODUCTION: Given the lack of formal training surrounding difficult conversations, a simulation-based educational curriculum was designed to address this educational gap. The goal was to improve effective communication skills among Internal Medicine (IM) residents using high fidelity simulation (SIM).
METHODS: A pre-session informative graphics of the SPIKES protocol and NURSE statements and a video of a simulated doctor-patient conversation was provided to the learners prior to the SIM session. The SIM session consisted of a didactic component on the SPIKES protocol and NURSE statements as well as a high-fidelity simulation component in which the learners engaged in difficult conversation training surrounding end of life discussions.. Each learner was assigned a role within the SPIKES protocol which they handled during the SIM session. A debrief and feedback session was held after the SIM, with the learners, SIM faculty and Chaplain. Learners completed a pre-session and a post-session survey, evaluating a change in subjective comfort and objective knowledge on the SPIKES protocol and NURSE statements.
RESULTS: 115 and 104 internal medicine residents participated in a pre-session and post-session survey, respectively. Most reported never receiving formal training in difficult conversations (n=69, 60%). The majority reported less than ten difficult conversations with patients (n=83, 72.2%). Only 18.3% (n=21) felt that they had adequate training in delivering bad news to patients and most requested additional training in the topic (n=76, 66.7%). Half of the learners felt that the biggest hurdle in these conversations is when patient/family members exhibit difficulty understanding limitations/complications of life-sustaining therapies and the prognosis (n=57, 49.6%). Only 40.9% (n=47) reported feeling comfortable communicating the prognosis to patients pre-session, which improved to 73.8% (n=76) post-session. Similarly, only 34.8% (n=40) felt comfortable discussing death with a terminally ill patient, which improved to 66.7% (n=68) post-session. The subjective comfort surrounding code status discussion was reported by 67% (n=77) of learners, which improved to 85.6% (n=89). Overall, 88.3% (n=91) learners reported feeling comfortable holding a goals of care conversation after the SIM session. Evaluation of resident knowledge on SPIKES and NURSE statements revealed that 97.4% (n=111) and 93.9% (n=108) knew the components of each, which improved to close to 100% post-session.
CONCLUSION: Pre-session surveys demonstrated learners’ discomfort with difficult conversations mostly surrounding the prognosis and death. Post-session surveys held after a didactic and high-fidelity SIM session demonstrated significant improvement in comfort and knowledge. This simulation-based curriculum increased IM resident comfort, knowledge and skill in utilizing the SPIKES protocol and NURSE statements during difficult conversations. High fidelity simulation should be incorporated into IM Residency Programs to improve communication skills among clinicians.
158
ABSTRACT #93
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY
A GIANT FREE-FLOATING BALL THROMBUS OR A TINY FIBROELASTOMA: WHICH CAUSES MULTIPLE STROKES?
Swiri Konje1, Yeraz Khachatoorian1 , Arpanjeet Kaur1, Nirupama Krishnamurthi1, Soheila Talebi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Left atrial (LA) thrombus is not rare in patients with mitral valve stenosis, but in patients with nonvalvular atrial fibrillation on anticoagulation, the formation of a "ball thrombus" in the LA is uncommon.
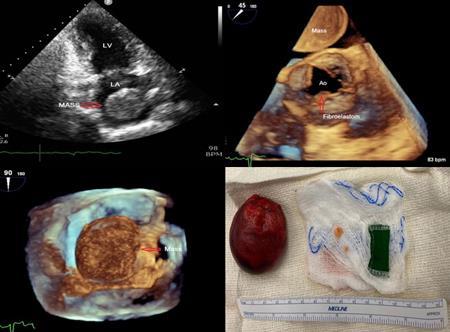
CLINICAL PRESENTATION: A 73-year-old man with nonvalvular atrial fibrillation on Eliquis® presented with frequent syncope and slurred speech. The appearance of the infarcts on brain MRI and involvement of different vascular territories suggests embolic phenomena as the cause. On transthoracic echo a large, highly mobile echo density in the left atrium was noted. Transesophageal echo revealed smoke in the left atrium and the left atrial appendage. A large round mobile echo density mass measuring 4.7 cm x 3.6 cm was seen in left atrium with no attachment to left atrium. A mobile round density measuring 0.7 x 0.7 cm was seen on the right coronary cusp. Absence ofperfusion,no enhancement, and high signal intensity on T1 and T2 weighted images oncardiac MRI was suggestive organized clot in left atrium. Both masses were removed successfully. Pathology confirmed a large intact spherical organized clot from the LA and a small fibroelastoma attached to the aortic leaflet.
CONCLUSION: This was a rare case of giant round-shaped left atrium thrombus, which occurred in a patient with nonvalvular atrial fibrillation on anticoagulation. An aortic fibroelastoma was also discovered by transesophegeal echo as another potential cause of stroke. The left atrial thrombus is thought to have developed from a small mural thrombus caused by prolonged blood stagnation, which gets rounded by the sculpting impact of multiple complex encounters with the atrial wall. This may then detach from the LAA and form a floating "ball thrombus.
159
Figure 1:
ABSTRACT #94 MEDICAL EDUCATION CARDIOLOGY
A TARGETED NEEDS ASSESSMENT FOR THE DEVELOPMENT OF A TELEMETRY CURRICULUM FOR INTERNAL MEDICINE RESIDENTS
Arpanjeet Kaur1, Joseph Elias1, Neojsa Markovic1, Roberto O. Jimenez1, Michel Skaf1, Robert Abed1 , Deepika Misra1, Edgar Argulian1,Kiran Mahmood1,Jacqueline Tamis-Holland1,Forough Hakimzada1,VasundharaSingh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023
BACKGROUND/INTRODUCTION: Telemetry monitoring is used to detect a wide range of arrhythmias in patients at high risk of cardiac events. Internal medicine residents should be able to interpret and interrogate telemetry to identify and characterize arrhythmias and differentiate these from artifacts. Misinterpretation can lead to adverse patient outcomes, increased hospitalization costs and inappropriate interventions. However, there are no widely accepted curricula for Internal Medicine residents on inpatient telemetry. To address this gap in graduate medical education, we hope to design telemetry curriculum for Internal Medicine residents. Following the Kern method of curriculum development, we performed a targeted needs assessment to guide our curriculum design
METHODS: A web-based survey was sent to current Internal Medicine residents at Mount Sinai Morningside/West., which collected data regarding residents’: (1) prior telemetry training; (2) preferred method of learning, (3) preferred learning environment. Using a Likert-type scale ranging from 1 (“no knowledge”) to 5 (“extremely knowledgeable”), residents were also asked to rate their knowledge for: indications of telemetry; reviewing telemetry alarms; navigation of telemetry-monitors, and identifying true arrhythmias versus artifacts.
RESULTS: Hands-on training alone or in combination with other options (i.e. didactics and/or self-paced videos) was the most popular choice, accounting for 84.9% of all the responses. Further analysis showed that 27.4% preferred hands-on training alone, 21.9% preferred hands-on training and didactics, and 19.1% preferred a combination of hands-on, didactics, and self-paced study. 72.6% of residents preferred the curriculum to be implemented during inpatient rotation alone or in combination with academic half days and/or simulation training (17.8% chose inpatient rotation only, 17.8% preferred inpatient rotation and simulation training, and 21.9% preferred inpatient rotation and academic half day). Analyzing residents’ self-assessment of telemetry skills, 40.4%thought they had slight knowledge across the four mentioned categories of telemetry review. When stratified by training year, 50% of PGY-1s felt having slight knowledge, 43.4% of PGY2 rated having moderate knowledge and 56.8% of PGY3 assessed themselves as being very knowledgeable.
CONCLUSION: This study highlights the need for a structured telemetry curriculum for Internal Medicine residents and provides data on residents’ baseline knowledge and preferred learning technique. This information can guide educators to develop a standardized curriculum to enhance learning of Internal Medicine residents on inpatient telemetry floors and to contribute to high-value patient care.
160
ABSTRACT #95 CLINICAL RESEARCH CARDIOLOGY
ROLE OF EARLY AORTIC VALVE REPLACEMENT VERSUS CONVENTIONAL MANAGEMENT IN ASYMPTOMATIC PATIENTS WITH SEVERE AORTIC STENOSIS: A META-ANALYSIS
Arpanjeet Kaur1 , Arshdeep Dhaliwal2, Sumit Sohal2, Yoni Balboul1 , Jacqueline Tamis-Holland1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Newark Beth Israel Medical Center, Newark, NJ, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Aortic-valve replacement (AVR) is an effective therapy for patients with severe symptomatic aortic stenosis (AS) but the appropriate timing of intervention for asymptomatic patients with severe AS remains controversial. Increased mortality associated with the onset of symptoms challenges the conventional “watchful waiting” strategy followed for this subset of patients. An early intervention may be warranted, however the data supporting this hypothesis is small. Our aim was to perform meta-analysis looking at outcomes of early surgical AVR (SAVR) in asymptomatic severe AS patients with preserved LVEF.
METHODS: Electronic databases were searched for studies comparing early SAVR and conventional treatment in patients with asymptomatic severe AS and normal LV function. The primary outcome of interest was all cause mortality. Secondary outcome was heart failure hospitalization. Random-effects model was used to estimate the pooled risk ratio (RR), and 95% confidence interval (CI) using Revman 5.4.1. Subgroup analysis stratified by study design was performed. Heterogeneity was assessed by Higgins I2 statistic.
RESULTS: We found total of 8 studies (2 RCTs; 6 observational) from which 2669 patients with asymptomatic severe AS were identified. 1354 underwent SAVR and 1315 were managed conservatively. The mean age was 68 years with mean follow up duration of 4.8±2 years. There was statistically significant reduction in all-cause mortality (RR, 0.37; 95%CI, 0.27-0.50; p<0.05; I2=68%) and heart failure hospitalization (RR,0.24; 95% CI: 0.160.36; p<0.05; I2= 0%) among patients who underwent AVR compared with conservative treatment with subgroup analysis by study design showing similar trends.
CONCLUSION: Our meta-analysis shows that compared with conventional treatment strategy, early SAVR in asymptomatic patients with severe AS is associated with improved long-term outcomes notably reduced all cause mortality and heart failure hospitalizations.
161
Figure 1: Pooled risk-ratios and 95% confidence intervals for outcomes of (a) all-cause mortality and (b) heart failure hospitalizations. CI: confidence interval; AVR: aortic valve replacement
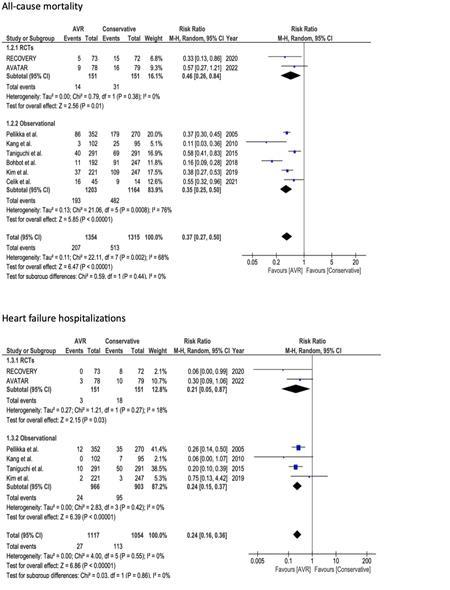
162
ABSTRACT #96 MEDICAL EDUCATION CARDIOLOGY
VIRTUAL CARDIAC POINT-OF-CARE ULTRASOUND CURRICULUM AMONG RESIDENTS: A MEDICAL EDUCATION PROJECT
Arpanjeet Kaur1 , Yoni Balboul1, Kruti Gandhi1, Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Point-of-care ultrasound (POCUS) is becoming increasingly important for rapid assessment and diagnosis in a variety of clinical situations. With the ongoing COVID-19 pandemic, the aim of this study is to determine whether a virtual POCUS session can improve learner competency in assessing left ventricular (LV) systolic function.
METHODS: An hour long session, involving a short lecture and fourteen practice questions was created. The questions consisted of cardiac ultrasound clips from real patients, evaluated by three POCUS experts. For each clip, LV systolic function was classified as hyperdynamic, normal, reduced, or severely reduced. The session was given separately to a group of interns (n1=30) and a group of senior residents (n2=39) virtually via Zoom. Series of clips were shown as the lecture progressed and participants recorded their answers as either hyperdynamic, normal, reduced, or severely reduced using the polling feature within the Zoom platform. Effect size as the percent of correct responses was calculated. Data was analyzed using SPSS software with independent t-test and paired t-test analysis with a level of statistical significance as p≤0.05.
RESULTS: The intern group had a mean score of 69.9% (SD 21.8%) and the resident group had a mean score of 74.2% (SD 21.5%). All participants achieved a mean score of 66.6% (SD 26.0%) during the first half of the lecture, which then improved to 77.6% (SD 14.2%) in the second half (p=0.547). Both groups showed similar overall trends, although these were not statistically significant. When combined, extremes of LV function (hyperdynamicand severely reduced) werebetter recognized than more subtle differences (reduced and normal) (81.4% ± 18.1 versus 55.2% ± 15.9; p=0.001] overall.
CONCLUSION: Compared to the conventional in-person approach, this study highlights the potential for virtual didactic sessions in POCUS training with impressive results when recognizing extreme cardiac findings.
163
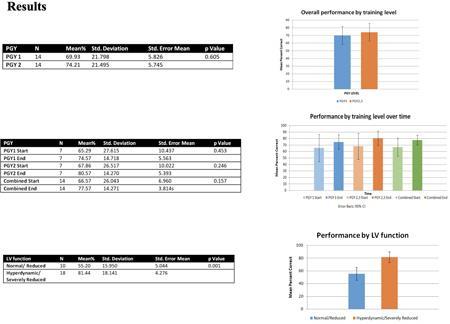
Figure 1: 164
ABSTRACT #97 CLINICAL RESEARCH CARDIOLOGY
CLINICAL BENEFIT OF NEUROHORMONAL BLOCKADE IN WOMEN WITH TRANSTHYRETIN CARDIAC AMYLOIDOSIS AND HEART FAILURE WITH PRESERVED EJECTION FRACTION
Darren Kong1, Alaa Omar1, Maria K. Peña, Arpanjeet Kaur1 , Ashish Correa1, Edgar Argulian1, Johanna Paola Contreras2, Arieh L. Fox1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
BACKGROUND/INTRODUCTION: Scarce data exists regarding guideline directed medical therapy (GDMT) in transthyretin amyloid cardiomyopathy (TTR-CM).
METHODS: TTR-CM patients seen in the cardiology department from 2017 to 2021 were retrospectively included. GDMT usage, echocardiography, and right heart catheterization (RHC) data was collected. Patients were followed for a median of 21 months for death, acute coronary syndrome (ACS), stroke, and cardiac hospitalization.
RESULTS: We included 115 patients [age=78 ± 12 years, 36 (31%) women, EF=47 ± 15%, 58 (50%) with EF ≥50%]. During follow-up, 20 patients died, 3 patients had ACS, 4 patients had stroke, and 78 patients were hospitalized, and the combined outcomes occurred in 81 patients. Overall, sex, EF, and GDMT use did not predictoutcomes,exceptfor theassociation of neurohormonal blockade (NHB: ACEI, ARB, and MRA) with better outcomes. Compared to men, women were older, had similar risk factors, comorbidities, LV systolic and diastolic function, and RHC pressures. NHB+ women were low-risk for outcomes; NHB- women had the worst outcome risk, while NHB+ or NHB- men were intermediate. In the subgroups, this NHB/sex association persisted only in HFpEF but not in HFrEF patients.
CONCLUSION: NHB can be beneficial in selected TTR-CM patient populations. In our study, women with preserved ejection fraction seem to be the group showing clinical benefit of NHB use.
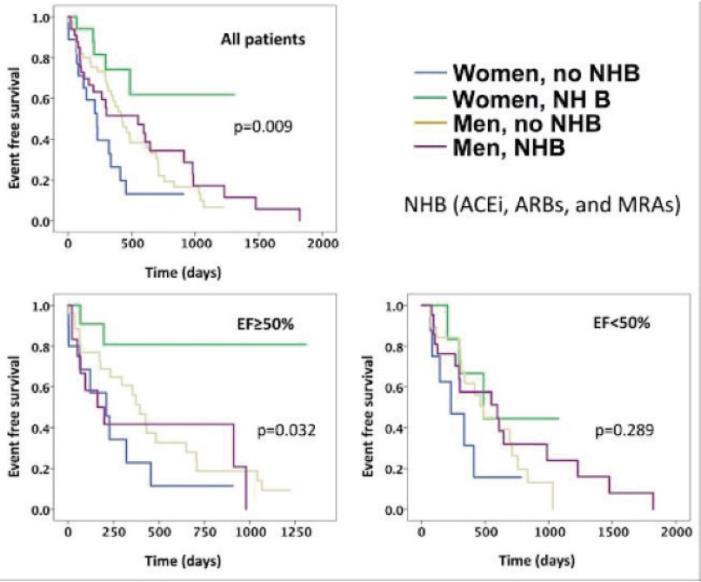
165
ABSTRACT #98
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY
DRESS SYNDROME-ASSOCIATED PERIMYOCARDITIS AFTER INITIATION OF RIPE THERAPY: A CASE REPORT
Darren Kong1, Keshav K. Dixit1, Swiri Konje1, Vikram Agarwal1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in New Orleans, Louisiana, United States from March 4-6, 2023.
BACKGROUND/INTRODUCTION: Cardiac involvement in DRESS Syndrome is rare and not well understood. We present a case ofperimyocarditis after initiation of RIPE therapy with improved ejection fraction after initiation of corticosteroids and cyclosporine.
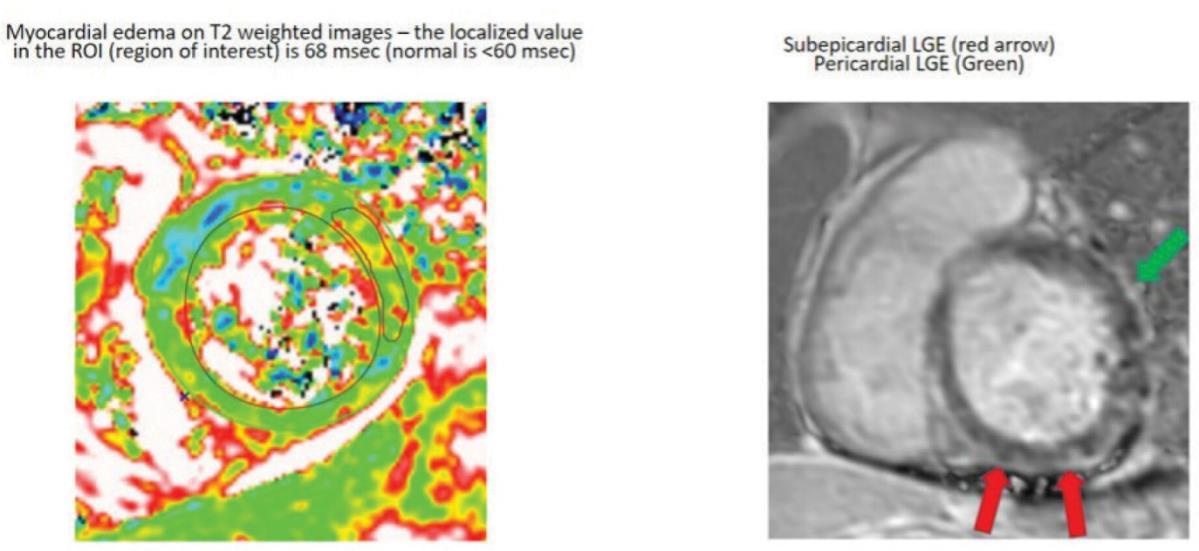
CLINICAL PRESENTATION: A 34-year-old female recently on RIPE therapy for suspected TB reinfection presented with fevers, rash, and generalized fatigue. Labs show signs of end organ damage with eosinophilia and leukocytosis. The patient became hypotensive with a worsening fever, and an ECG showed new diffuse ST segment elevations with an elevated troponin. ECHO showed a reduction in ejection fraction (EF) and diffuse hypokinesis; MRI obtained showed circumferential subepicardial LGE with associated myocardial edema and acute pericarditis. Prompt diagnosis of DRESS Syndrome using the RegiSCAR criteria and discontinuation of RIPE therapy was initiated. She was started on systemic corticosteroids and cyclosporine, with improvement of hemodynamics and rash. Skin biopsy revealed perivascular lymphocytic dermatitis, consistent with DRESS syndrome. She was discharged with oral corticosteroids, and a repeat ECHO showed full recovery of EF.
DISCUSSION/CONCLUSION: Early discontinuation of offending agents and initiation of corticosteroids are essential to improved clinical outcomes. Further research should be towards greater emphasis on cardiac evaluation in DRESS syndrome and multimodality imaging to confirm perimyocardial involvement and guide management strategies.
Figure 1:
166
ABSTRACT #99 QUALITY IMPROVEMENT GASTROENTEROLOGY
GASTRIC INTESTINAL METAPLASIA PREVALENCE AND APPROPRIATE FOLLOW UP: A QUALITY IMPROVEMENT STUDY
Frederick Rozenshteyn1, Emily Seltzer1 , Randy Leibowitz1, Marni Wilkoff1, Attila Molnar1, Gabriel Levi1 , Tina Park1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023.
BACKGROUND/INTRODUCTION: Gastric intestinal metaplasia (GIM) is often incidentally found during an endoscopy performed for other indications. Although it is thought to be a precursor to dysplasia and gastric cancer in correa’s cascade, there is a paucity of data on its prevalence and surveillance guidelines in the United States. Previous studies suggest low prevalence rates of 11%. Given the lack of consensus, surveillance rates after GIM diagnosis remain low in the US, while gastric cancer incidence is growing. The European Society of Gastrointestinal Endoscopy (ESGE) recommends eradication of H. Pylori and a surveillance endoscopy with gastric mapping biopsies in 3 years for patients with GIM without dysplasia. This study aims to better understand the prevalence of GIM at two diverse city hospitals and the rate of follow-up being recommended for GIM.
METHODS: Consecutive endoscopies performed for any indication at two academic hospitals in New York City between June 1, 2017 to June 1, 2022 were reviewed. Endoscopies with gastric biopsies with pathology reports demonstrating GIM were identified using Provation and Epic. Intestinal metaplasia found from the cardia or GE junction were excluded to avoid Barrett’s esophagus patients. Data on demographics, symptoms, Helicobacter pylori status and other classifiers were collected on the 644 cases included in the study.
RESULTS: A total of 3288 endoscopies with gastric biopsy were performed during the above time period. Of these,19.6% were found to have GIM. Dysplasia wasdocumented in 2.5%.The majority of GIM-positive biopsies occurred within the antrum (46.1%), with most biopsies showing focal IM (59.3%). Intestinal metaplasia subtypes were not specified in 91.6% of the pathology reports. H. pylori was found in 21.1% of patients with GIM with 61.8% treated. Further subgroup analyses were performed by age, gender, ethnicity, BMI, H. pylori status, and smoking/alcohol status. Appropriate discussion of follow-up endoscopy for mapping occurred in 36.5% of patients with GIM.
CONCLUSION: Despite a higher rate of gastric intestinal metaplasia identified on routine endoscopy withbiopsy, the appropriate follow-up rates for gastric mapping remained low. In order to improve our hospital systems’ management of gastric intestinal metaplasia, we plan to implement provider education via didactics on the risk of gastric intestinal metaplasia progression to gastric cancer, the importance of discussion of appropriate followup, and the role ethnic and gender disparities play in achieving improved surveillance. In addition, we will also work to standardize our hospital systems’ protocol in response to biopsies positive for gastric intestinal metaplasia. By implementing these practices into our standard of care, we hope to improve guideline-directed follow-up for patients with confirmed gastric intestinal metaplasia.
167
ABSTRACT #100
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
NOW YOU SEE ME, NOW YOU DON’T: A CASE OF CAMPYLOBACTER JEJUNI COLITIS PRESENTING AS A COLONIC MASS
Randy Leibowitz1 , Frederick Rozenshteyn1, Samuel Daniel1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Campylobacter jejuni (C. jejuni) is responsible for 3-6% of diarrheal illnesses in the United States. Inoculation follows ingestion of a contaminated source such as poultry, unpasteurized milk, or drinking water. The presentation of a C. jejuni infection may radiographically and endoscopically mimic other pathologies such as colonic malignancy and inflammatory bowel disease (IBD).
CLINICAL PRESENTATION: A 66-year old man with a past medical history of prostate cancer in remission and a 6 mm colonic polyp removed 5 years prior presented to the emergency department with 5 days of watery diarrhea. He complained of 6 watery bowel movements per day associated with colicky abdominal pain and bloating. He was hemodynamically stable with a physical exam notable for severe tenderness in the right lower quadrant. Serum chemistries did not reveal any abnormalities. Computed tomography revealed severe, focal bowel wall thickening in the ascending colon and a 1.7cm hypodense lesion in the right hepatic lobe which was confirmed on magnetic resonance of the abdomen. The radiologist’s interpretation emphasized concern for colonic malignancy with metastasis to the liver. Endoscopic evaluation revealed diffusely erythematous, granular and ulcerated mucosa throughout the colon with concern for infectious versus inflammatory colitis. Histologic evaluation of ascending colonic mucosal biopsy revealed moderately active chronic colitis with extensive cryptitis and cryptabscesses.Stool polymerase chain reaction was notable for C. jejuni infection and the patient achieved clinical and endoscopic remission without antimicrobial therapy.
DISCUSSION/CONCLUSION: In patients with C. jejuni enterocolitis, radiographic imaging may reveal signs of bowel wall edema or ulcerations which may resemble colonic malignancy or IBD. Endoscopic findings of campylobacter enterocolitis are non-specific, however, may reveal edematous, erythematous, and friable mucosa which may be associated with hemorrhage. Inflamed mucosa can be either isolated or discontinuous. Colonic ulcers may present as either aphthous or linear (may resemble cobblestoning as seen in Crohn's Disease). Histologic evaluation can reveal cryptitis and crypt abscess formation similar to findings of ulcerative colitis. This case highlights the range of radiographic and endoscopic presentations of C. jejuni colitis. Infectious colitis should remain on the differential for radiographic evidence of colonic edema in the right clinical setting.
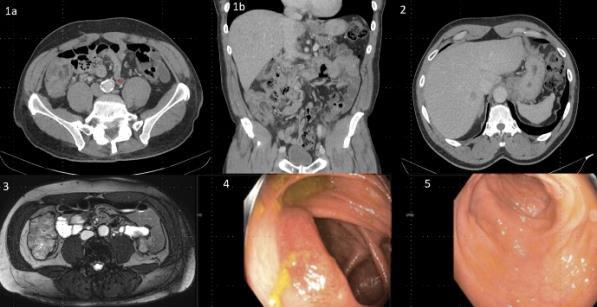
168
Figure 1a,1b: CT Abdomen/Pelvis showing ascending colon wall thickening resembling mass; Figure 2: CT of Hypoechoic liver mass; Figure 3: T2-weighted MRI Abdomen of ascending colon wall thickening resembling a mass; Figure 4: Colonoscopy image revealing inflamed mucosa of ascending colon; Figure 5: Ulcerated mucosa of the sigmoid colon
ABSTRACT #101
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
THE MASTER OF DISGUISE: ISOLATED GASTRIC VARICEAL HEMORRHAGE AS A COMPLICATION OF ENDOSCOPIC GASTRIC BIOPSY
Randy Leibowitz1 , Frederick Rozenshteyn1, Edward Lung1 , Abdallah Beano1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Splenic vein thrombosis (SVT) causes left-sided portal hypertension that can result in the formation of gastric varices. Gastric varices can be isolated or contiguous with esophageal varices. Isolated gastric varices may be difficult to distinguish from gastric rugae. They are responsible for 10-30% of all variceal bleeds.
CLINICAL PRESENTATION: A 61-year old male with a past medical history of coronary artery disease on aspirin and clopidogrel presented to the emergency department with 2 days of black tarry stools and associated dyspnea and palpitations. 3 weeks ago, he saw an outpatient gastroenterologist to evaluate new onset anemia (hemoglobin 10 mg/dL) and an unexplained 25-pound weight loss over 6 months. He underwent esophagogastroduodenoscopy (EGD) 2 days prior to presentation in which a protruding lesion in the gastric fundus was biopsied. On initial presentation, he was hemodynamically stable with epigastric tenderness on physical exam. Initially, his hemoglobin was 8.1 mg/dL, which further decreased to 6.6 mg/dL that evening requiring transfusion. Computed tomography of the abdomen with IV contrast showed a 4.6cm pancreatic tail lesion with associated splenic vein thrombosis. The patient underwent EGD with endoscopic ultrasound (EUS) which revealed a fundal isolated gastric varix with stigmata of recent bleeding. EUS guided biopsy results of the pancreatic tail lesion demonstrated a well-differentiated neuroendocrine tumor.
DISCUSSION/CONCLUSION: Gastric varices (GV) are categorized based on their location. Gastroesophageal varices (GOV) include GOV1, extending from the esophagus to the lesser curvature of the stomach, and GOV2, extending from the esophagus to the greater curvature. Isolated gastric varices (IGV) include IGV1 in the fundus, while IGV2 are located at ectopic gastric sites including the antrum, body, pylorus, incisura and duodenum. The most common gastric varix is GOV1 (74%). IGV1 comprises 8% of total GV and 78% of IGV. A prospective cohort study by Sarin et al. noted IGV1 to bleed at a much higher rate (78%) than IGV2 (9%). Gastric vein obliteration is the mostsuccessful modality in treatingacute bleeds and harbors the lowest rebleedingrate(22%). Gastric varices have a similar bleeding risk to esophageal varices (25%) and are more difficult to treat. For patients with risk factors for SVT (pancreatitis, cirrhosis and other prothrombotic states) who present with a GI bleed, IGV should be included in the differential.
169
Figure 1a and 1b: Endoscopic image of isolated gastric varix with stigmata of recent bleeding; Figure 2: EUS image of the pancreatic tail mass and the splenic vein with visible thrombosis; Figure 3: Anatomy of gastroesophageal varices and Isolated gastric varices. SV=Splenic vein, PV=Portal vein, LGV=Left gastric vein, GEV=Gastroepiploic vein, SGV= Short gastric vein, PGV=Posterior gastric vein
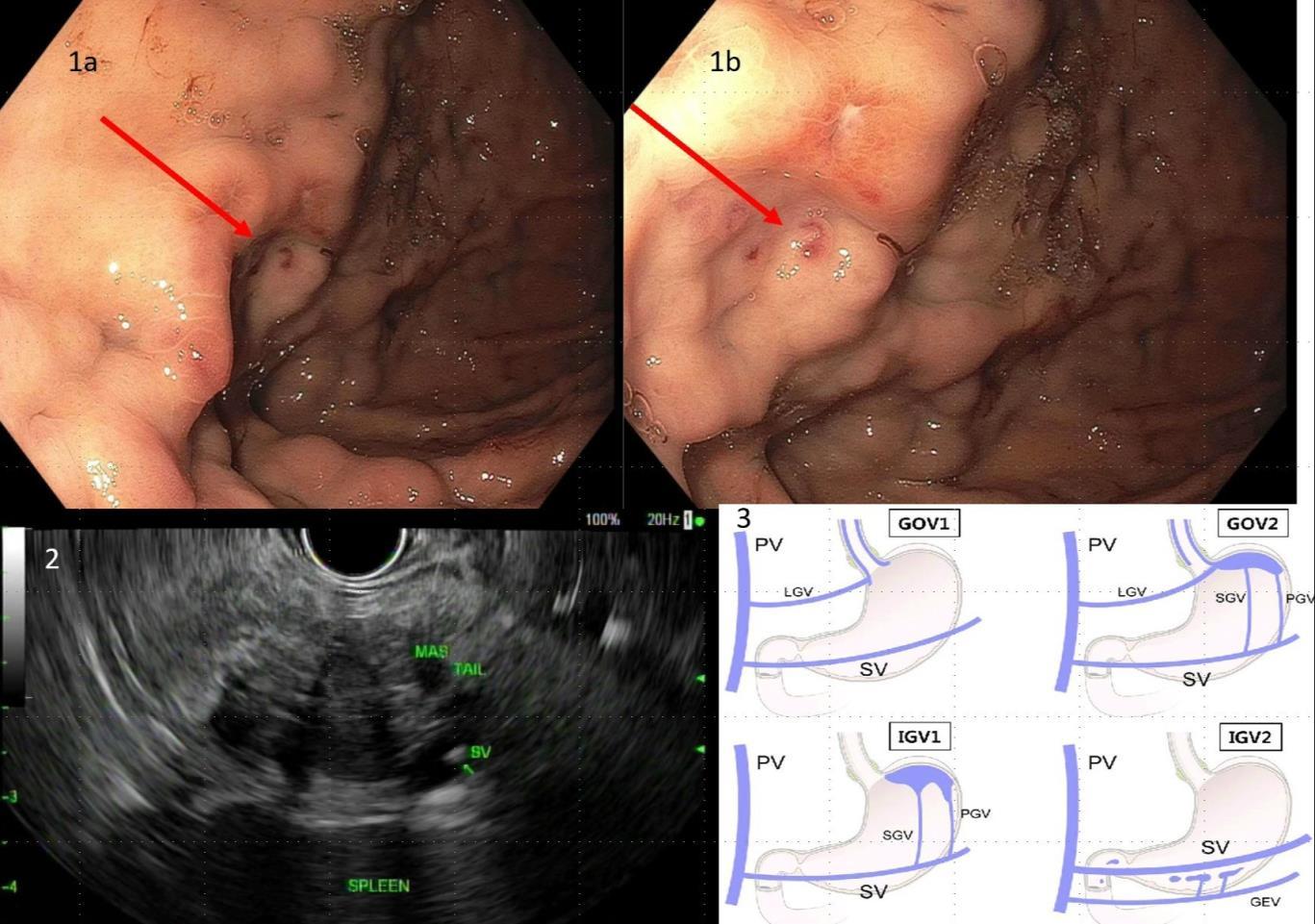
170
ABSTRACT #102
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
YOU SHALL NOT PASS: RARE DUODENAL BULB ADENOCARCINOMA CAUSING GASTRIC
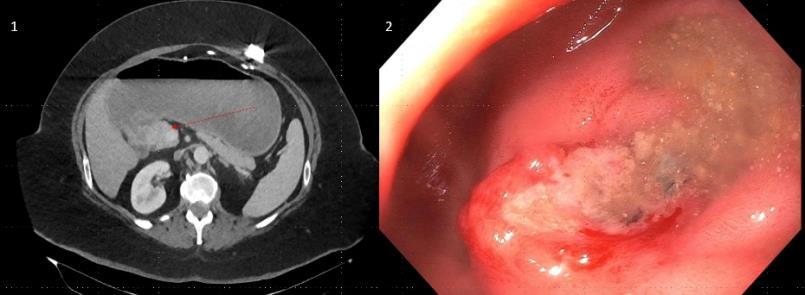
OUTLET OBSTRUCTION
Randy Leibowitz1 , Alexander Maraveyas1 , Frederick Rozenshteyn1, Tina Park1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Duodenal carcinoma accounts for only 1-2% of diagnosed gastrointestinal cancers in the United States. Due to its insidious onset, advanced disease is often established at the time of diagnosis resulting in poor outcomes for patients. Although duodenal adenocarcinomas have been found to comprise around half of all small bowel adenocarcinomas, disease arising from within the duodenal bulb in the D1 segment is a vanishingly rare phenomenon.
CLINICAL PRESENTATION: A 52-year old female with a past medical history of morbid obesity with placement of laparoscopic adjustable gastric band 14 years prior presented with frequent emesis, inability to tolerate oral diet and a 22 kg weight loss. Recent esophagogastroduodenoscopy during a previous admission revealed a cratered ulcer in the duodenal bulb. An upper GI series was obtained, showing a 2cm mass in the bulb apex which was confirmed by computed tomography. A repeat esophagogastroduodenoscopy was performed which identified a firm and friable ulcer with contact bleeding with complete obstruction of the duodenal bulb. Subsequent histopathology confirmed the presence of invasive, moderately differentiated adenocarcinoma.
DISCUSSION/CONCLUSION: Small bowel tumors comprise about 2% of all GI tumors. Adenocarcinoma accounts for about 30% of all small bowel tumors. The duodenum comprises 53% of all small bowel neoplasms. Of duodenal tumors, about 57% occur in the D2 segment of the duodenum. One 2014 meta-analysis of small bowel cancers between 1990-2012 from an institutional registry (excluding ampullary cancers arising from the bile duct mucosa) identified only 30 cases of primary duodenal adenocarcinoma with none arising from D1. A previous 1991 literature review cites 47 cases of primary duodenal adenocarcinoma arising from D1, however, anatomic distinction between the duodenal bulb and the distal D1 segments was not made. Although small bowel tumors are the third leading cause of gastric outlet obstruction, lesions are typically asymptomatic. In a study of 217 primary duodenal adenocarcinoma, the median survival was 20 months with 35% presenting with metastatic disease (39% present with stage III disease). Although it is difficult to distinguish the prevalence of duodenal bulb neoplasms, it has been clearly demonstrated that neoplasms arising from the D1 segment of the duodenum are extremely rare. By presenting this case, we hope to increase the index of suspicion for small bowel neoplasms as part of the differential for gastric outlet obstruction.
171
Figure 1: CT demonstration of duodenal bulb mass causing gastric outlet obstruction; Figure 2: Endoscopic image of duodenal bulb tumor
ABSTRACT #103 MEDICAL EDUCATION GASTROENTEROLOGY
WORKSHOPS TO TEACH INTERNAL MEDICINE RESIDENTS AND EVALUATE THEIR ABILITY TO TREAT GASTROINTESTINAL BLEEDING
Randy Leibowitz1, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
BACKGROUND/INTRODUCTION: Gastrointestinal (GI) bleeding is one of the most common chief complaints internal medicine residents will encounter during inpatient training. However, a 2015 study found residents (42%) were more likely to identify stool as melena on a digital rectal exam when compared to GI fellows (12%). In turn, residents were more likely to identify a GI consult as emergent (13%) compared to fellows (4%).
The Accreditation Council for Graduate Medical Education (ACGME) outlines milestones for residents on a Dryfus rating scale ranging from novice to expert. Residents are expected to progress from being able to develop a differential diagnosis of GI bleeding, to eventually being able to properly evaluate patients with GI bleeding and develop accurate treatment options based on severity and prognosis.
METHODS: The assessment of The GI bleeding workshops will be separated into two installments: lower GI and upper GI bleeding. The workshops will be performed with residents ranging from PGY-1 to PGY-3. Each installment will include a pre-survey and a post-survey one month after the workshop. Both workshop lectures contain an evidence-based outline of the American College of Gastroenterology (ACG) Clinical Guidelines for the managementofacute upper and lower GI bleeding. Within each section, data from the studies that influenced the guideline recommendations will be summarized and explained. Each section will conclude with a peerreviewed multiple choice question from the American College of Physicians Medical Education Division. At the end of each lecture an algorithmic diagram, either derived from or provided by the ACG Clinical Guidelines, will be administered.
RESULTS: Prior to the workshop and one month after, residents will be administered an identical comprehensive survey to assess their knowledge and attitudes towards treating GI bleeds. PGY-1 surveys will be evaluated separately from PGY-2 and PGY-3 to account for differences in experience level. Knowledge will be assessed by responses to the peer reviewed questions. Residents will also be assessed on their confidence in evaluating and treating GI bleeds, as well as measuring residents’ progress against the ACGME milestones.
CONCLUSION: The aim of administering these two workshops is to assess the knowledge and attitudes of internal medicine residents in evaluating and treating GI bleeds, as well as assist them in advancing in the milestones set forth by the ACGME.
172
ABSTRACT #104
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY
TAKOTSUBO CARDIOMYOPATHY AS A COMPLICATION OF SCALENE NERVE BLOCK
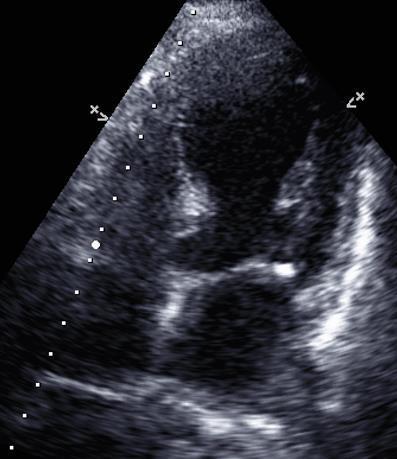
Christopher N. Matthews1, Syed Farrukh Mustafa1, Deepika Misra1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York American College of Cardiology Annual Meeting on December 9, 2022 and at the Inaugural Mount Sinai Heart Research Forum on February 22, 2023 that were both held in New York, NY, United States.
CLINICAL PRESENTATION: An 82-year-old female with history of coronary artery disease, heart failure with preserved ejection fraction, hypertension and prior rotator cuff surgery presented for an elective total shoulder arthroplasty. The patient received a right interscalene nerve block with bupivacaine. She subsequently reported neck pain, sensation of “throat closing”, shortness of breath and left sided crushing chest pain a few minutes after the block. Physical exam showed tachypnea, use of accessory muscles and bilateral rales in mid and lower lung zones. The patient was intubated for hypoxia and rapidly increasing work of breathing. ECG showed sinus tachycardia (150 bpm) with frequent premature ventricular contractions. Bedside echocardiogram showed left ventricular ejection fraction of 15-20% with basal hyperkinesis and mid to apical akinesis. Troponin-I was elevated to 0.101 ng/mL, up trended to 0.265 ng/mL and down trended within 24 hours. The patient was managed on heparin, aspirin, atorvastatin and started on low dose goal directed medical therapy with metoprolol and sacubitril-valsartan. The patient was extubated maintaining adequate oxygen saturation, but reported mild chest pain. Low dose goal directed medical therapy was initiated and transitioned. A left heart catheterization revealed non-obstructive coronary artery disease.
DISCUSSION/CONCLUSION: Takotsubo cardiomyopathy has been a rarely reported complication of nerve blockade, believed to be secondary to diaphragm paralysis from paravertebral cervical block in one case and pain secondary to insufficient analgesia from femoral nerve block in another case.
Conclusion: We report the first case of takotsubo cardiomyopathy believed to be induced by anesthesia with an interscalene nerve block.
173
Figure 1: Transthoracic echocardiogram. Apical 4-chamber view showing akinesis of mid and apical segments and hyperkinetic basal segments
ABSTRACT #105 CLINICAL RESEARCH CARDIOLOGY
CLINICAL OUTCOMES OF CARDIAC DEVICES IN HEART FAILURE PATIENTS HOSPITALIZED WITH COVID-19: INSIGHTS FROM NATIONAL INPATIENT SAMPLE DATABASE
Errol Moras1 , Kruti D. Gandhi1 , Nadeem Bilani1 , Tais Bertasi1 , Raphael Bertasi1, Ashish Correa1 , Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Technology and Heart Failure Therapeutics (THT) Annual Meeting that was held in Boston, Massachusetts, United States from March 20-22, 2023.
BACKGROUND/INTRODUCTION: Scarce date is available with respect to cardiac device (CD) implantations in patients with active COVID-19. We aimed to investigate the impact of COVID-19 on implantation rates and clinical outcomes in heart failure (HF) patients hospitalized for COVID-19.
METHODS: Data from National Inpatient Sample database from 2020 was used to identify hospitalizations for COVID in HF patients. Clinical outcomes of CD implantations were compared using univariate and multivariate logistic regression analysis.
RESULTS: From March-December 2020, a total of 20426 CD were performed in HF patients in the United States, of which 0.9 % were among those with active COVID-19 infection. Patients with COVID were younger, more Hispanic and Black population, and had a higher prevalence of comordities such as ventricular fibrillation and complete heart block when compared to patients without COVID. CD implantation in patients with COVID had significantly increased in-hospital mortality, longer lengths of stay, higher costs, and outcomes such as incidence ofacute stroke,thromboembolism, and sepsis. Device related complications and the need for revisions were comparable in the two cohorts. After adjustment for baseline characteristics, COVID cohort had increased odds of in-hospital mortality.
CONCLUSION: Patients with active COVID-19 infection who underwent device implantation had increased inhospital mortality, longer lengths of stay and higher hospitalization costs with comparable outcomes of device complications.
174
ABSTRACT #106
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY
PATENT FORAMEN OVALE WITH PLATYPNEA-ORTHODEOXIA PRECIPITATED BY LARGE HEPATIC CYST REQUIRING CLOSURE: NOVEL APPROACH
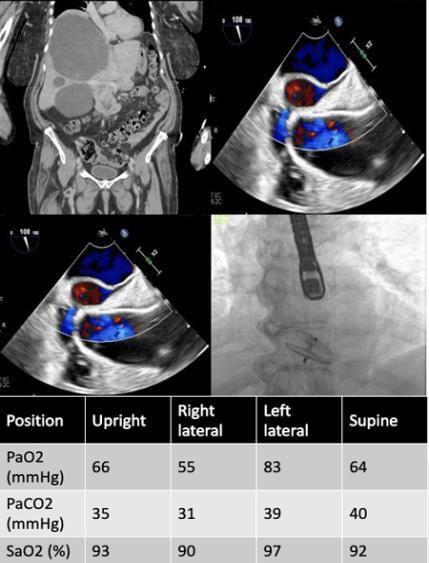
Errol Moras1, Kruti D. Gandhi1, Apurva Sharma1, Francisco J. Romeo1, Parissa Tabirzian1, Barry A. Love1 , Amirali Ahmadi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
CLINICAL PRESENTATION: A 71-year-old female with history of liver cyst presented with severe epigastric and RUQ pain. Abdominal CT demonstrated interval worsening of the liver cyst (largest cyst 18cm) causing right hemi-diaphragmatic elevation. She was hemodynamically stable, and plan was for elective surgical cyst fenestration in 2 weeks. However, her pain worsened, and was readmitted with severe dizziness and hypoxia. Chest CTA workup revealed subsegmental pulmonary emboli (PE) bilaterally and lower extremity dopplers showed deep vein thrombosis. She was started on anticoagulation, but her hypoxemia worsened, requiring maximum high flow oxygen. Persistent hypoxia disproportionate to the PE that worsened in the right lateral decubitus position led to repeat transthoracic echocardiogram with bubble study that demonstrated a largepatent foramen ovale (PFO) and a normal right ventricle. Mechanism of this severe hypoxemia was largely attributed to the shunting from the IVC directly across the PFO and couldn’t be explained by a small PE. Given the high risk for paradoxical emboli, the need for PFO closure versus debulking the liver cyst was discussed at the time. Aspiration of the cyst was attempted initially to avoid PFO closure, with temporary improvement in her hypoxemia. Hence a decision was made to close the PFO before further definitive management of the cyst. The PFO was closed with 30mm Amplatzer Talisman occlude device and post operatively her oxygen was weaned down to room air sating 95%. However, her abdominal fullness continued to be present, and she underwent successful fenestration of her cyst.
CONCLUSION: There have been cases where large hepatic cysts causing compression of the right atrium were treated either with surgical drainage or cyst resection. Rare cases have the need for a PFO closure with hemodynamic changes, as this one, where it was successfully done, leading to significant improvement.
175
Figure 1:
ABSTRACT #107 CLINICAL RESEARCH CARDIOLOGY
THE EFFECT OF COVID-19 ON OUTCOMES OF NON-ST ELEVATION MYOCARDIAL INFARCTION (NSTEMI): RESULTS FROM THE NATIONAL INPATIENT SAMPLE DATABASE
Errol Moras1 , Kruti D. Gandhi1 , Tais Bertasi1, Raphael Bertasi1 , Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society for Cardiovascular Angiography and Interventions (SCAI) Annual Meeting that will be held in Phoenix, Arizona, United States from May 18-20, 2023.
BACKGROUND/INTRODUCTION: The influence of the COVID-19 pandemic on the in-hospital outcomes in patients with NSTEMI showed conflicting results and are limited by single-center or limited regional datasets. We aimed at analyzing the clinical impact of Covid-19 infection on in-hospital outcomes in patients with Non-STelevation myocardial infarction (NSTEMI) from the nationwide dataset in the United States.
METHODS: We reviewed the National Inpatient Sample to identify hospitalizations with a primary diagnosis of NSTEMI. COVID-19 was used to segregate the population into 2 groups. Univariate and multivariate logistic regression analyses were performed to determine any association between NSTEMI and primary or secondary outcomes.
RESULTS: From March-December 2020, there were 626,420 NSTEMI hospitalizations in the United States, and 4.3% of which were found to be COVID positive. We found that NSTEMI patients with COVID-19 had increased in-hospital mortality (37.6% versus 7.3%, p<0.001),longer lengths ofstay (10 versus 6days, p<0.001) and higher hospitalization costs ($156k versus $114k, p<0.001). After multivariate adjustment, NSTEMI patients with COVID-19 showed a higher rate of inpatient mortality [adjusted odds ratio (aOR), 5.8; 95% CI: 5.4 -6.2; p< 0.001), and worse secondary outcomes that included increased vasopressor requirements (aOR, 2.0; 95% CI, 1.8-2.3; p<0.001), increased respiratory complications requiring mechanical ventilation (aOR, 3.5; 95% CI, 3.3.7; p< 0.001), and increased risk of sudden cardiac death (aOR, 1.7; 95% CI, 1.5-1.8; p<0.001). NSTEMI patients with COVID-19 also received less invasive cardiac procedures such percutaneous coronary intervention [PCI] (aOR, 0.23; 95% CI, 0.18-0.29; p<0.001), trans-venous pacing [TVP] (aOR, 0.4; 95% CI, 0.3-0.5; p<0.001) and had a lower need for MCS devices (aOR, 0.4; 95% CI, 0.3-0.5; p<0.001).
CONCLUSION: In conclusion, patients with COVID-19 had significantly higher in-hospital mortality, longer lengths of stay, higher hospitalization costs, and worsening secondary outcomes. Further studies are warranted to understand the mechanisms underlying the association between Covid-19 and mortality in this cohort.
176
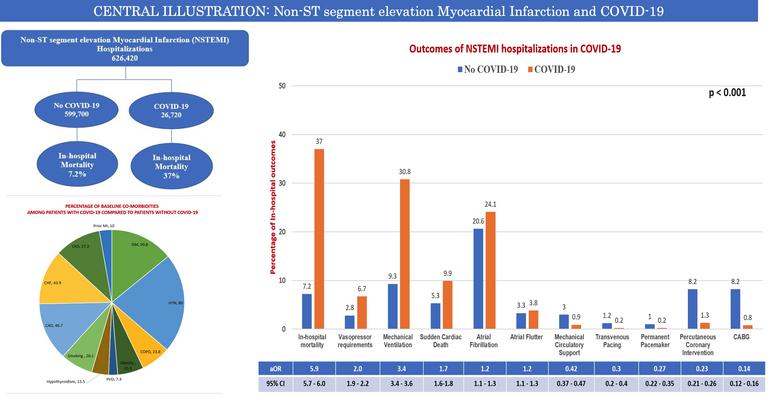
177
ABSTRACT #108
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
COLONIC SCHWANNOMA: A CAUSE FOR NERVES?
Mantej Sehmbhi1, Sera Satoi2, Qingqing Liu3, Ilan Weisberg2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Schwannomas arise from schwann cells, and though they are the commonest of all peripheral nerve tumors, it is exceedingly rare for them to be detected in the lower gastrointestinal (GI) tract. Here, we present the case of a submucosal colonic schwannoma detected incidentally as part of a routine colonoscopy for colorectal cancer (CRC) screening and discuss the clinical significance of such tumors.
CLINICAL PRESENTATION: A 59-year-old male patient with intermittent constipation presented for colonoscopy for CRC screening. A previous colonoscopy 7 years prior had been unremarkable. Family history was notable for CRC in several second-degree relatives. The patient’s past medical history was significant for non-alcoholic fatty liver disease, well-controlled human immunodeficiency virus infection and prediabetes. Physical examination was unremarkable. At colonoscopy, an 8 mm submucosal lesion was found in the cecum. This was sessile and firm,and did not demonstrate a pillow sign characteristic of lipoma. The lesion was resected using a saline injection-lift technique and hot snare. At histology, the lesion was described as tan-pink polypoid tissue, with negative margins. Immunohistochemically, the tumor cells were diffusely and strongly positive for S100 and negative for CD117, DOG1, SMA and desmin. This was consistent with a diagnosis of schwannoma.
DISCUSSION/CONCLUSION: When GI schwannomas arise, they are most commonly found in the upper GI tract, with 60-70% of GI cases found in the stomach and only 3% in the colon. There are no clear risk factors for their development other than advanced age. As in our patient’s case, colorectal schwannomas are typically detected incidentally on screening colonoscopies. They can be asymptomatic, or present with rectal bleeding (22.9%), abdominal pain (15.6%) or constipation (7.3%). The mass effect of large schwannomas can lead to colonic obstruction necessitating surgical resection of the tumor, but smaller lesions can typically be resected endoscopically. Schwannomas present as submucosal lesions and are almost always benign, with only atypical versions harboringany malignant potential. Numerous studies have demonstrated that recurrenceafter complete resection is rare, even after extended follow-up. There is no established guidance regarding follow-up intervals for patients with colorectal schwannomas, owing to their rarity. Based on the lack of malignant potential and the low risk of recurrence, we recommended a repeat colonoscopy in 5 years for our patient.

178
Figure 1: Cecal schwannoma in macroscopic (left) and microscopic (right) views
ABSTRACT #109
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
DIAGNOSING VISCERAL KAPOSI SARCOMA: THE NECESSITY TO AVOID ANCHORING ON THE DIAGNOSIS OF A CROHN'S FLARE
Emily Seltzer1, Shabari M. Shenoy1, Bo Hyung Yoon1, Frederick Rozenshteyn1, Kevin Mijares1 , Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022 and published in Cureus, 2023. PMID: 36938235
BACKGROUND/INTRODUCTION: Inflammatory bowel disease (IBD) and human immunodeficiency virus (HIV) affect the immune system in inverse means, IBD causes an overdrive of the immune system whereas HIV suppresses it. The decline in CD4+ count in HIV is believed to promote remission of IBD by decreasing inflammatory responses.
CLINICAL PRESENTATION: We present a 45-year-old male with a self-reported history of Crohn’s disease (CD) complaining of bloody diarrhea and weight loss that he presumed to be the result of a Crohn’s flair. He was afebrile and tachycardic with multiple violaceous plaques on his left leg and left lower quadrant abdominal tenderness on exam. Labs were significant for anemia, elevated C-reactive protein, erythrocyte sedimentation rate, and fecal calprotectin. Abdominal computed tomography angiography revealed mild mural thickening in the mid to distal esophagus, mesenteric adenopathy, and wall thickening of the ascending colon. To rule out infectious causes, Clostridium difficile and gastrointestinal pathogens panel were collected and resulted as negative. The patient’s course was complicated by sepsis of unknown etiology. Further investigation revealed his lower extremity lesions were recently biopsied establishing a diagnosis of Kaposi Sarcoma (KS). Initiation of high-dose glucocorticoids for possible Crohn’s flare was deferred in light of this. Despite previous negative results, HIV antigen was positive with a CD4+ count of 58 cells/mm3 and viral load >1,000,000 copies/mL.Upper endoscopy and colonoscopy demonstrated many 10 to 50 mm violaceous nodules in the esophagus, duodenum, and throughout the colon consistent with KS. This was confirmed immunohistochemistry positive for CD34 and HHV8. The KS was staged as Tumor 1 (visceral disease), Immune system 1 (CD4< 200), Systemic illness 1 (B symptoms). He was started on paclitaxel, with anti-retroviral therapy held due to increased risk of immune reconstitution inflammatory syndrome.
DISCUSSION/CONCLUSION: KS in patients with HIV and IBD is extremely rare with a prevalence of 0.4%, and, visceral KS is rarely present with initial diagnosis of HIV. We demonstrate the risks of anchoring on a CD diagnosis of CD, as it is possible HIV would have been missed and starting treatment of CD could have been very harmful as high-dose steroids have been shown to further progress KS. We share this truly rare case of visceral KS in a patient with newly diagnosed HIV masquerading as a CD flare to promote broadening the diagnostic arsenal where the picture of IBD is not clear cut.
179
ABSTRACT #110 MEDICAL EDUCATION
INFECTIOUS/DISEASES/PULMONARY/CRITICAL CARE
SIMULATION CASE ON ABDOMINAL SEPSIS-APPLICATION OF THREE ESSENTIAL CLINICAL CONCEPTS-SEPSIS PROTOCOL, COGNITIVE BIASES ALONG WITH POINT-OF-CARE ULTRASOUND
Venus Sharma1 , James Salonia1, Priscilla Loanzon1, Harrindra Seepersaud1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
BACKGROUND/INTRODUCTION: Sepsis is a life-threatening organ dysfunction that results from the body’s response to infection. It requires prompt recognition, appropriate antibiotics, careful hemodynamic support, and control of the source of infection. Through this simulation case, we aim to educate the residents regarding the rapid evaluation and management of patients with sepsis, recognizing the need to initiate sepsis protocol, avoiding cognitive biases, thinking about the differential diagnoses and using point-of-care ultrasounds for more clarity.
METHODS: To create awareness among the residents taking care of patients with sepsis, severe sepsis, and septic shock, we created a simulation case on abdominal sepsis. Through this case, we highlighted the importance of rapid evaluation and management of patients who triggered systemic inflammatory response syndrome (SIRS) alert in the epic, recognizing the need to initiate sepsis protocol, avoiding cognitive biases using the debiasing techniques and using point-of-care ultrasound (POCUS) for diagnostic or therapeutic purposes together with a traditional medical examination. Briefly, the simulation case started with the registered nurse calling the floor team to evaluate the patient (high-fidelity mannequin) who was admitted with chronic obstructed pulmonary disease (COPD) exacerbation, now complaining of shortness of breath and abdominal pain. The vital signs and the laboratory results were simulated to meet SIRS criteria. The team was evaluated based on the immediate evaluation and management of sepsis, maintaining a broad differential diagnosis based on the patient’s clinical presentation. The teams were also evaluated on the basis of performing at least three simple debiasing techniques – slow down, discuss aloud, consult (‘diagnostic timeout), “actively seek alternative hypotheses/diagnoses (“rule of 3),” and seek disconfirming evidence to avoid confirmation bias and premature closure (for example, ask to questions/look for data to disprove own hypothesis, and avoid pseudo-diagnostics). Performing POCUS for diagnostic or therapeutic purposes was also a part of this simulation case. The case simulation was followed by debriefing. It involved constructive feedback to the team regarding the case. We discussed the Mount Sinai Health System Sepsis Bundle and the importance of placing the patient on a stop sepsis pathway
RESULTS: The team was evaluated based on the immediate evaluation and management of sepsis,maintaining a broad differential diagnosis based on the patient’s clinical presentation using the debiasing techniques and performing POCUS for more clarification. Through this case, sepsis, severe sepsis & septic shock were discussed. The benefits of the stop sepsis order set were discussed in the debriefing session. Overall, it was emphasized that early identification and appropriate immediate management improve outcomes. There was an increased number of stop sepsis pathway utilization on the floors following this simulation session along with increased documentation following the SIRS alert. The primary learning objectives which were met at the end of simulation labs were: demonstrate immediate evaluation and management of sepsis; use POCUS for diagnostic and therapeutic purposes together with medical examination, history, and laboratory studies whenever required; and, maintain a broad differential diagnosis based on the patient’s clinical presentation.
180
CONCLUSION: Sepsis affects 750,000 patients annually in the United States. It is a leading cause of death in critically ill patients in the hospital. Through this case, we aimed to make residents more confident in evaluating and managing patients with sepsis, severe sepsis, and septic shock. It resulted in improved utilization of stop sepsis pathway.
181
ABSTRACT #111 CLINICAL RESEARCH PULMONARY/CRITICAL CARE
UNPLANNED EXTUBATION IN THE ICU: OPPORTUNITIES AND CHALLENGES
Yasmin I. Herrera1 , Venus Sharma1, Sara Luby1, James Salonia1, Adam Rothman1, Raymonde Jean1 , Joseph P. Mathew1, Susannah Kurtz1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the CHEST Annual Meeting that was held in Nashville, TN, United States from October 16-19, 2022.
BACKGROUND/INTRODUCTION: Unplanned Extubation (UE) in the Intensive Care Unit (ICU) is an indicator of quality of care and is associated with increased ventilator days and length of hospital stay. Its complications range from hypoxemia to hemodynamic compromise and death. We aimed to describe potential risk factors for UE among critically ill adults requiring mechanical ventilation in order to identify strategies to reduce the occurrence of this adverse event.
METHODS: We performed a retrospective review of all UE that took place in the Medical, Surgical, and Neurosciences ICU in an urban academic hospital, from January 1st, 2020 to December 31st, 2021. These events were identified by the institutional electronic adverse event reporting software system. We implemented a quality improvement (QI) cause analysis, and plan-do-act study (PDSA) cycle to create awareness amongst ICU staff and improve outcomes.
RESULTS: In the studied period, there were 34 UEs, representing 0.36 events per 100 mechanical ventilator days. The majority of patients were male (76%), with a median age of 62 years (range, 28 to 87 years), and admitted to the Medical ICU (70%). A history of polysubstance abuse was present in 35% of the cases. Most of the patients were on physical restraints (76%). Sedation was titrated within 4h prior to the event in 39% of the cases. UE occurred more frequently during day shifts (52%) than night shifts, and 24% of the UE happened around the time of nursing handoff. Re-intubation within 24h was required in 38% of the cases, and there was an 8% mortality rate within 24 h of the event.
CONCLUSION: Despite having an acceptable incidence rate compared to the national benchmark, many of our patients needed to be re-intubated. Therefore, interventions are necessary to improve the quality of care and patient safety. Male sex and a history of polysubstance abuse appear to be risk factors for UE. The majority of the UEevents occurred in the absenceofsedative titration, which suggests inadequate managementofsedation. Physical restraints did not appear to be effective in preventing UE. A QI initiative is being designed and implemented in our ICUs, focusing on staff education, early identification, and management of patients at increased risk of UE, with the ultimate goal of reducing UE.
182
ABSTRACT #112 CLINICAL RESEARCH GASTROENTEROLOGY
OUTCOMES IN PATIENTS WITH CIRRHOSIS UNDERGOING ESOPHAGOGASTRODUODENOSCOPY FOR UPPER GASTROINTESTINAL BLEEDING
Shabari M. Shenoy1, Mantej Sehmbi1, Suhail Haddadin1, Maan El Halabi1, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Variceal hemorrhage is the most common cause of upper gastrointestinal bleeding (UGIB) in patients with liver cirrhosis. Endoscopic variceal ligation (EVL), along with pharmacotherapy, is the standard of care for treatment of bleeding gastroesophageal varices. Median re-bleeding rate in patients treated with EVL is about 7.6% at 2 weeks. We studied the rate of re-bleeding and difference in outcomes such as re-hospitalization, mortality in patients undergoing EVL compared to those that did not undergo EVL.
METHODS: We identified adult patients with cirrhosis undergoing esophagogastroduodenoscopy (EGD) for UGIB, admitted over a 3-year period to a tertiary care center in New York City. Demographics, medical history, and rates of re-bleeding, rehospitalization and death at 60 days post-discharge were recorded. Patients undergoing EVL were compared to those who did not undergo EVL.
RESULTS: 54 patients (median age 57 years, 44% male) underwent EGD for acute UGIB. Etiologies of UGIB were portal hypertensive gastropathy (34%), esophageal varices (34%), gastritis (32%) and gastric or duodenal ulcers (24.5%). 21 (38%) patients underwent EVL and 33 (61%) did not. Reasons for not undergoing EVL included other etiology of UGIB, varices less than 5mm or other. Age, gender, race, etiology of cirrhosis, MELD Na score, proton pump inhibitor (PPI) use and prior decompensating event, were similar between the 2 groups. There was no difference in rates of re-bleeding, re-hospitalization due ascites, portosystemic encephalopathy, and infection and 60-day mortality between the 2 groups. Interestingly, gastritis or gastroduodenal ulcers were the likely cause of UGIB in 23 patients (42%).14 patients were re-hospitalized within 60 days of initial admission. The leading cause of rehospitalization was rebleeding (41%).
CONCLUSION: We found no differences in outcomes of cirrhotic patients hospitalized for UGIB based on etiology of UGIB and whether they underwent EVL. A significant proportion of patients rebled. Our study demonstrated that gastritis and gastric/duodenal ulcers were common etiologies of UGIB in cirrhotic patients. There is a higher risk of spontaneous bacterial peritonitis and liver-related mortality among cirrhotic patients on long term PPI. However, since a significant cause of UGIB in patients with cirrhosis may be peptic ulcer/gastritis related,future studies should focuson the length of PPI use after discharge inpatients with cirrhosis who undergo EGD for UGIB.
183
ABSTRACT #113
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
RECURRENT PANCREATITIS SECONDARY TO ADDERALL USE WITH PANCREATIC ASCITES: A SIGHT TYPICALLY UNSEEN
Shabari M. Shenoy1 , Jenny Dave1,2, Edward Lung1, Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Pancreatic ascites is a rare disease with a prevalence of 3.5% resulting from pancreatic duct injury. While small ascites resolves spontaneously, large volume, persistent ascites can cause significant morbidity and mortality. We present a case of pancreatic ascites in a patient with recurrent pancreatitis from Adderall use.
CLINICAL PRESENTATION: A 38-year-old female with attention deficit hyperactive disorder (ADHD), remote alcohol use, and recurrent pancreatitis complicated by pseudocyst and ascites presented with acute on chronic epigastric pain. Her last reported alcohol use was two years ago. Home medications included Adderall (amphetamine and dextroamphetamine) and benzodiazepines. Physical examination revealed normal vital signs, severe cachexia and peripheral edema. Abdomen was distended with epigastric tenderness. Pertinent labs included hemoglobin of 10.8g/dl, calcium 7.6mg/dl, albumin 1.7g/dl and a lipase of 462U/l. Bilirubin, transaminases, alkaline phosphatase and INR were normal. Quantitative immunoglobulins, IgG4, triglycerides and thyroid stimulating hormone were within normal limits. Blood alcohol and phosphatidylethanol (PETH) levels were negative. Previous CT scan demonstrated pancreatic head cyst (4.6cm), stable pseudocysts in the head and body, peripancreatic inflammation and large abdominal ascites. MRCP this admission revealed pancreatic head fluid collection decreased in size (2.3cm), consistent with walled off necrosis. Diagnostic paracentesis was significant for: WBC 93 cells/mm3, PMN 25%, RBC 2050 cells/mm3, protein 1.9g/dl, lactate dehydrogenase 102U/L, amylase 1496U/L and a serum ascites-albumin gradient (SAAG)<1.1. An endoscopic retrograde cholangiopancreatography (ERCP) was pursued due to suspicion for pancreatic ascites which showed abrupt cut off of the pancreatic duct in the head, without filling of the pancreatic duct in the body or tail likely due to stricture. A pancreatic stent was placed into the ventral pancreatic duct to maintain patency with plan for endoscopic ultrasound examination (EUS) to exclude obstructive pathology.
DISCUSSION/CONCLUSION: Pancreatic ascites is often seen with recurrent pancreatitis commonly ofalcoholic etiology. Our patient had recurrent pancreatitis and ascites due to chronic adderall use. While pancreatitis from adderall use is rare, presentation with ascites can pose a diagnostic challenge. Hence, clinicians should familiarize themselves with early diagnosis and endoscopic management which improves prognosis in this rare disease.
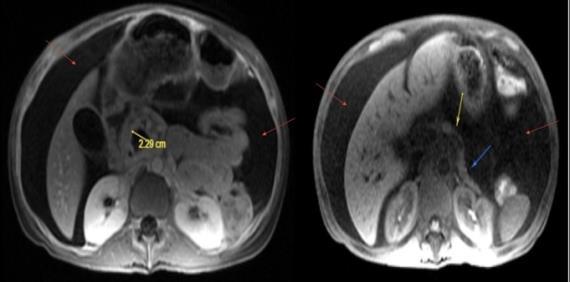
184
Figure 1: MRCP images revealing large volume ascites (red arrow), walled off necrosis in the pancreatic head (yellow arrow) and peripancreatic inflammation (blue arrow)
ABSTRACT #114
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
THE MARCHING BAND: PSEUDOACHALASIA SECONDARY TO GASTRIC BAND SLIPPAGE
Shabari M. Shenoy1 , Gres Karim2, Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Gastric band slippage is a late complication of laparoscopic adjustable gastric banding surgery (LAGBS) with an incidence of less than 5%. We present a case of pseudoachalasia caused by gastric band slippage in a patient with a history of LAGBS.

CLINICAL PRESENTATION: A 53-year-old female with a history of LAGBS for obesity ten years ago presented to our motility clinic with complaints of recurrent emesis for the last ten years. Episodes were associated with minimal retching,often self-induced to relieve chest discomfort. She appeared tearful while explainingthe debility from her symptoms, severely affecting her quality of life. Due to severe, progressive worsening of symptoms for three months prior to presentation, a gastric emptying study performed by her gastroenterologist did not reveal any pathology. A recent esophagogastroduodenoscopy showed mild esophagitis. Proton pump inhibitors provided no relief. Given the incongruence between symptoms and workup, we decided to obtain an upper gastrointestinal (UGI) series. UGI series revealed tilting of the laparoscopic band, collimation around the thoracic esophagus immediately on barium swallow followed by passage of short amount of contrast along the narrowed diameter at the location of the band. Over the course of the study, significant stasis was noted in the thoracic esophagus causing severe restriction of passage confirming the diagnosis of gastric band slippage. She was referred to bariatric surgery for adjustment of the gastric band.
DISCUSSION/CONCLUSION: The complication rate from LAGBS increases by 3-4% each year that the band is left in-vivo and rises to 40% at 10 years. Complications such as slippage and obstruction at the band site present with nonspecific symptoms such as vomiting and regurgitation. In our patient’s case, pseudoachalasia was one of the differential diagnoses given the long-standing dysphagia, regurgitation, and chest discomfort. Although majority of pseudoachalasia is cancer related, benign causes also exist. LAGB can lead to formation of scar tissue from tight fundic band can also cause pseudoachalasia by creating persistent high-pressure and low flow resistance, leading to impaired LES relaxation, weakening of the esophageal body. This case highlights the importance of primary care providers and gastroenterologists familiarizing themselves with presentation, diagnosis, and management of late complications of bariatric procedures as delayed diagnosis can severely affect quality of life as demonstrated by our case.
185
Figure 1: UGI series demonstrating tilting of the laparoscopic band, collimation around the thoracic esophagus immediately on barium swallow along the narrowed diameter at the location of the band.
ABSTRACT #115
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
TIME FOR A RENDEZVOUS: MULTI-DISCIPLINARY MANAGEMENT OF COMPLETE ESOPHAGEAL OBSTRUCTION IN A PATIENT FOLLOWING RADIATION TO POST-SURGICAL ANATOMY
Shabari M. Shenoy1 , Gres Karim2, Kimberly Cavaliere1, Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 24-26, 2022.
BACKGROUND/INTRODUCTION: Esophageal stricture is a common complication of radiation exposure. Balloon dilation restores luminal patency for partial narrowing, though complete obstruction can require recanalization through combined anterograde and retrograde endoscopic dilation (CARD), also known as the rendezvous technique. We describe a case of successful CARD recanalization following multimodal cancer treatment.
CLINICAL PRESENTATION: A 65-year-old male with right tonsillar cancer underwent resection of the right tonsil, tongue base and palate with pectoralis major reconstruction, followed by radiation. One year later, he reported progressive dysphagia to solids and liquids that required gastrostomy tube placement to maintain adequate nutrition. Laryngoscopy revealed radiation changes but no evidence of malignancy, and upper endoscopy revealed complete luminal obstruction. Retrograde endoscopy via gastrostomy initially was unsuccessful due to scarring, so wire-guided Savary dilation was performed until an ultra-thin endoscope could pass into the stomach. Retrograde inspection revealed a benign-appearing, complete stenosis in the proximal esophagus. Concurrent antegrade laryngoscopy visualized a thin tissue membrane with distal endoscopic illumination. The membrane was pierced retrograde under direct visualization with the sharp end of a Savary wire, after which it was advanced out the mouth. Stepwise antegrade Savary dilation then was performed over this wire to 45 French under visualization with the retrograde endoscope. Post-dilation inspection showed moderate mucosal disruption without luminal perforation, significant improvement in luminal narrowing, and minimal bleeding. A 12 French nasogastric tube was placed to maintain luminal patency, and the patient was discharged home. While he regained the ability to swallow liquids, a second dilation session was required to achieve complete dysphagia relief.
DISCUSSION/CONCLUSION: Most CARD procedures are performed by gastroenterologists to treat postradiation luminal obstruction. However, this case demonstrates CARD can be performed collaboratively with surgeons, which can be helpful in the setting of post-operative anatomy. CARD is effective, safe, and welltolerated, with a lower complication risk (esophageal perforation, pneumomediastinum) compared to blind antegrade dilation. High technical success rates (83%) and frequent dysphagia resolution (44%) make CARD a preferred approach to restore luminal patency in patients with severe radiation-induced dysphagia.
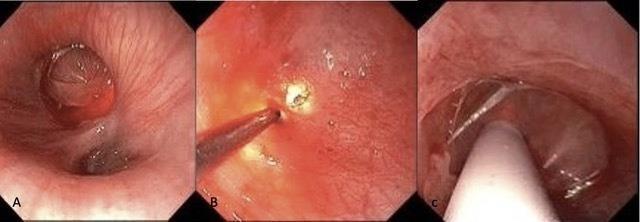
186
Figure 1: A- Stricture in the upper third of the esophagus; B- Piercing of the membrane in the upper third of the esophagus; C- Savary dilation of the upper third of the esophagus
ABSTRACT #116 MEDICAL EDUCATION GENERAL INTERNAL MEDICINE
IMPLEMENTATION OF A LONGITUDINAL PROCEDURAL CURRICULUM: WHAT EDUCATIONAL TOOLS IMPROVE PROCEDURAL PROFICIENCY WITHIN INTERNAL MEDICINE RESIDENCY PROGRAMS
Sidra Salman1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute of Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 27, 2023.
BACKGROUND/INTRODUCTION: We developed a procedure curriculum for Internal Medicine residents at the Mount Sinai Morningside/West Internal Medicine Residency program, with the following objectives: familiarization with equipment, acquisition of required knowledge, and integration of skills through simulation and direct patient procedures. The purpose of this study is to assess which educational tools best improve procedural proficiency and whether learner-driven, website-based education followed by simulation would improve procedural training amongst trainees.
METHODS: For acquisition of knowledge, a website was developed which included modules for each core procedure: nasogastric intubation, arterial puncture, ultrasound-guided intravenous access, central and arterial line insertion, paracentesis, thoracentesis, and lumbar puncture. Each module contains an equipment checklist, and pertinent information including: indications, contraindications, complications, and instructional videos. For application of knowledge, residents were offered simulation sessions each dedicated to a different procedure, as wellas a 2 week elective that offered direct patient procedures. Apre-and post-survey was utilized to measure the change in comfortability, certification rates, and knowledge level. Statistical significance was measured using chi-square analysis.
RESULTS: We received 35 responses (54.3% interns, 45.5% residents) on the pre-assessment and 32 responses (43.7% interns, 56.3% residents) on the post-assessment, with no statistical difference in ratio of interns to residents (p=0.38). 74.3% of housestaff felt the current procedure training at the program was insufficient, mostly due lack of opportunities performing procedures (68.8%) and lack of knowledge (20%). 100% of housestaff felt the implemented curriculum improved procedural proficiency. Majority of housestaff felt the visual aids, step-by-step instruction, simulation practice, and diversity of educational tools improved proficiency. Comfortability levels, measured using likert-style scales, increased by 26.4% and 36% in procedural proficiency and sterile approach respectively. 42.9% of housestaff were not certified in any procedures pre-curriculum, whereas 100% of housestaff were certified in at least one procedure post-curriculum. Certification numbers increased by 53% in low skilled procedures (defined as nasogastric intubation, arterial puncture, and ultrasoundguided IV, with p<0.001), 47.9% in central lines (p<0.001), 31.4% in arterial lines (p<0.001), 32.3% in paracentesis (p<0.01), and 15.6% in lumbar puncture (p>0.01). On average 25.7%-68.9% answered the procedural knowledge base questions correctly pre-curriculum, as compared to 42.9%-89% post-curriculum with an average of 20-25% improvement in correct answers per question.
CONCLUSION: Given similar demographics with no statistical difference between the ratio of interns to residents, the increase in certification rates and knowledge level post-curriculum is independent of level of clinical experience. Our procedural curriculum resulted in significant improvement in comfort, knowledge and certification rates among the various procedures expected during Internal Medicine residency training. Procedural proficiency is integral to internal medicine residency training, and greatly impacts patient care, correlating with the rate of hospital-acquired infections and patient outcomes. This study showed the positive impact our procedural curriculum had on proficiency amongst Internal Medicine Residents, while highlighting the importance of deliberate practice method and diversity of educational tools when formulating a procedural curriculum.
187
ABSTRACT #117 CLINICAL RESEARCH CARDIOLOGY
A NOVEL ENDOTHELIAL FUNCTION TEST IN PREDICTING LATE CORONARY IN-STENT RESTENOSIS
Zhuroran Yang1 , Jiasheng Yin2, Yaqi Zhang3, Lingling Wu4, Jieyu Jiang2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Zhongshan Hospital, Fudan University, Shanghai, China; 3John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; 4University of Alabama, Birmingham, AL, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Endothelial dysfunction is related with in-stent restenosis (ISR) of prior drugeluting stents (DES) implanted more than 1 year ago (late ISR). EndoPAT is a novel non-invasive test quantifying endothelial function as reactive hyperemia peripheral arterial tonometry index (RHI). EndoPAT is a potential predicting test for late ISR.
METHODS: We conducted a case control study on 186 patients with coronary DES implanted more than 1 year ago in a single medical center. Those who had contraindications to EndoPAT test, acute myocardial infarction, coronary artery bypass graft (CABG), chronic kidney disease (CKD) stage III and above, active infection and rheumatologic disease or acute decompensated heart failure were excluded. Patients were divided into ISR and non-ISR group based on coronary angiography. EndoPAT test was done at 24 to 48 hours prior to catherization. LnRHI is an index after natural log transformation of RHI. A receiver operative characteristic (ROC) curve analysis was used to determine the sensitivity and specificity of LnRHI for predicting late ISR.
RESULTS: ISR group had significantly more patients with history of ISR or triple-vessel disease, longer stent length and fewer totally occlusive lesions than non-ISR group. LnRHI was significantly lower in ISR group than in non-ISR group (0.66 versus 0.50, p<0.01). Patients with diffuse ISR had lower LnRHI than those with focal ISR (0.40 versus 0.55, p=0.03). Patients without ISR but undergoing revascularization had lower LnRHI than those with patent coronary arteries (0.56 versus 0.70, p=0.02). Endothelial function quantified by LnRHI was an independent risk factor for ISR (LnRHI/0.1; OR=0.79; 95% CI, 0.64-0.97; p=0.03). The ROC curve analysis showed LnRHI of 0.44 had a sensitivity of 81.7% and specificity of 53.8% for predicting late ISR.
CONCLUSION: Endothelial dysfunction measured by EndoPAT had a clinical potential for predicting the development of late ISR.
188
Total N=186 ISR P Yes (n=93) No (n=93) Age 65.6±9.5 65.4±9.3 65.7±9.6 0.95 Male 149 (75.6) 81 (87.1) 68 (73.1) 0.02 Diabetes 73 (39.2) 41 (44.1) 32 (34.4) 0.20 Hypertension 128 (65.0) 61 (65.6) 67(72.0) 0.33 Current Smoker 50(26.8) 23(24.7) 27(29.0) 0.48 PAD 18(9.7) 7(7.5) 11(11.8) 0.61 History MI 51(25.8) 27(29.0) 24(25.8) 0.38 ISR 11(5.6) 10(10.7) 1(1.1) <0.01 Triple vessel disease 42(22.6) 27(29.0) 15(16.1) 0.03 LVEF 61.5±8.1 60.2±8.4 62.8±7.5 0.03 Time from implantation (months)a 52.4 67.2 48.5 0.08 Medications ACEI 122(65.6) 61(65.6) 61(65.6) 0.92 β-blocker 152(81.7) 77(82.8) 75(80.6) 0.58 Anti-platelets 176(94.6) 87(93.5) 89(95.6) 0.69 Lipid-lowering 176(94.6) 89(95.6) 87(93.5) 0.44 Diagnosis Stable angina 71(38.2) 35(37.6) 36(38.7) 0.93 ACS 104(55.9) 52(55.9) 52(55.9) 0.93 189
ISR P Yes(n=93) No (n=93) Hemoglobin (g/L) 136.8±14.0 136.9±13.5 1.00 WBC 6.76±1.77 6.16±2.13 0.04 Platelet 199.2±62.4 189.4±49.6 0.24 Neutrophils(%) 61.5±8.5 59.1±9.6 0.10 Lymphocytes(%) 27.4±0.4 29.9±8.9 0.04 Monocytes(%) 7.5±2.1 8.0±2.1 0.07 Eosinophils(%) 2.49±1.98 2.79±1.81 0.30 NT-proBNP (pg/ml)a 397.8 222.4 <0.01 HbA1c (%) 6.69±1.06 6.48±1.07 0.28 Fibrinogen (mg/dl)a 289.4 251.3 <0.01 Creatinine (μmol/L) 88.2±36.2 84.1±34.1 0.42 Uric acid (mmol/L) 337.4±97.8 337.6±87.4 0.99 TC 3.9±4.3 3.9±3.1 0.95 TG 1.8±0.1 1.6±0.1 0.14 LDL 1.72±0.87 1.80±0.86 0.53 HDL 1.06±0.41 1.12±0.30 0.22 ApoE 37.5±17.0 38.1±15.2 0.79 Lp(a) 338.1±424.5 280.7±341.8 0.32 CRPa 3.48 2.35 0.04 190
ISR P Yes(n=93) No(n=93) Number of stents 1.65±0.65 1.34±0.61 <0.01 49.9±36.8 36.9±19.2 <0.01 Minimal diameter of stents (mm) 2.77±0.34 2.88±0.65 0.26 Strut thickness (μm) 100.5±19.4 103.3±17.8 0.43 Diseased vessels 1.98±0.81 1.68±0.77 <0.01 1 31(33.3) 46(49.4) 2 32(34.4) 28(30.1) 3 30(32.3) 17(18.3) Left main lesions 16(17.2) 7(7.5) 0.05 Totally occlusive lesions 19(20.4) 9(9.7) 0.03 Mehran Type Focal 46(49.5) 0(0) NA Diffuse In-stent Diffuse 8(8.6) 0(0) NA Proliferative 16(17.2) 0(0) NA Totally occlusive 23(24.7) 0(0) NA 191
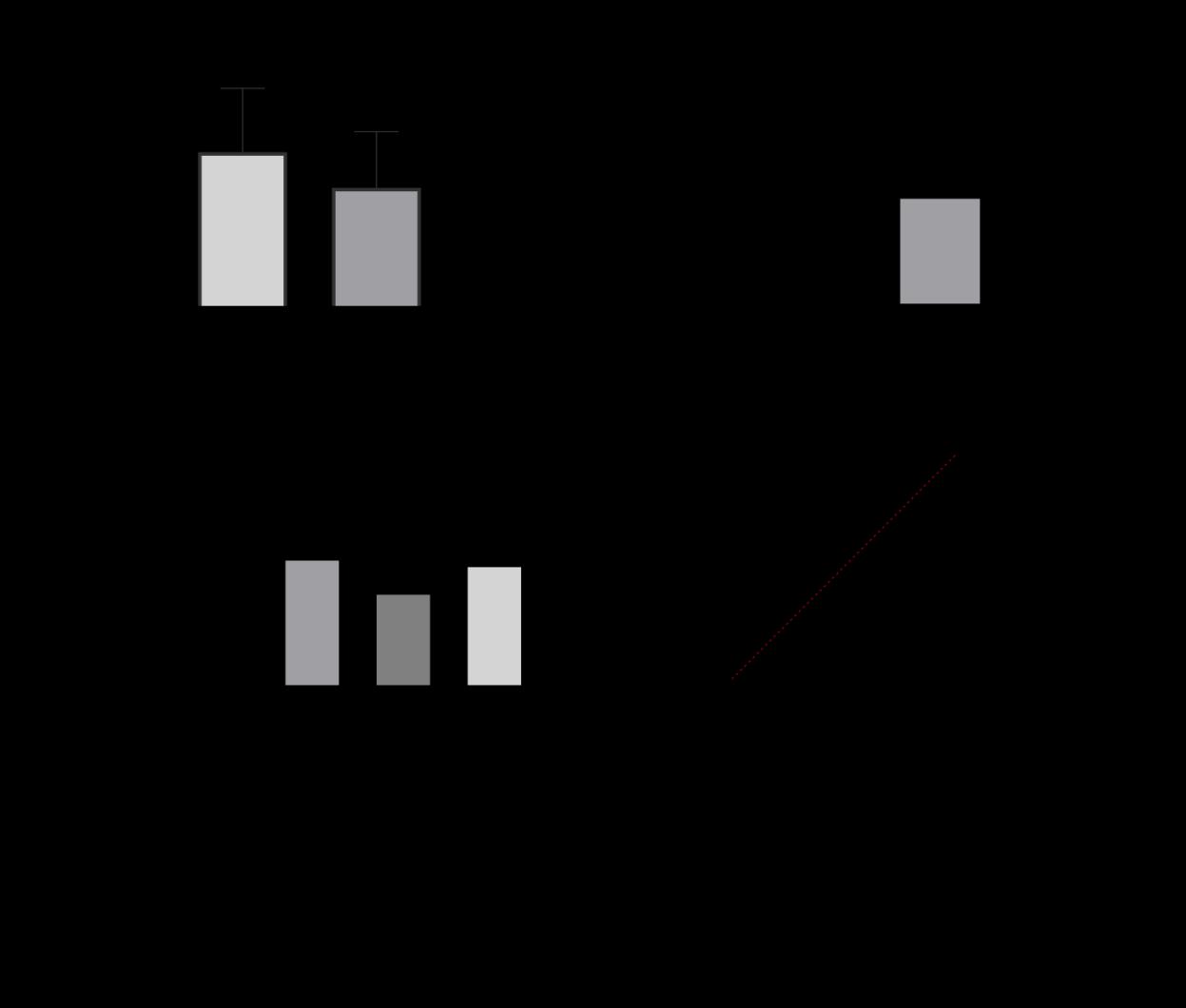
192
ABSTRACT #118
CLINICAL RESEARCH CARDIOLOGY
COMPLICATION AND READMISSION OUTCOME OF ATRIAL FIBRILLATION CATHETER ABLATION AMONG CANCER PATIENTS
Lingling Wu1, Bharat Narasimhan2 , Zhuoran Yang3, Kirtipal Bhatia3, Pengyang Li4, Arti Shah5, Bharat K. Kantharia5
1University of Alabama, Birmingham, AL, United States; 2Methodist Hospital, Houston, TX, United States; 3Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Virginia Commonwealth University, Richmond, VA, United States; 5Cardiovascular and Heart Rhythm Consult, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Catheter ablation (CA) has been increasingly utilized among patients with atrial fibrillation (AF) as a guideline-supported treatment. However, limited data is available regarding its safety among cancer patients. Patients with a cancer diagnosis has worse outcome following AF CA
METHODS: We queried the 2016 to 2019 United State Nationwide Readmission database to identify all patients with (active cancer or a history of cancer) or without cancer diagnosis who underwent AF CA. Hospital outcome and 30 days readmission rate were analyzed. Multivariate logistic regression or Cox proportional hazards regression analysis was employed when appropriate adjusting for comorbidities as well as patient and hospitallevel factors.
RESULTS: ISR A total of 46,461 AF CAs were included in the analysis, among which 800 (1.72%) patients were diagnosed with active cancer and 5,133 (11.04%) patients had a history of cancer. Compared to non-cancer patients, patients with a cancer diagnosis were older and more likely to be female. Patient with cancer diagnosis also has a higher burden of comorbidities, stroke risk, and bleeding risk as evidenced by Charlson Comorbidity Index, CHA2DS2-VASc score, and ATRIA score. As a result, patient with active cancer has higher inpatient hospital mortality, procedural complication rate, and all-cause readmission rate. After adjusting for confounders, active cancer diagnosis but not a history of cancer was associated with increased hospital mortality [Odds ratio, 2.72 (1.18-6.24); p=0.018 versus noncancer] In contrast, only a history of cancer was associated with a small increased risk of 30 days readmission following CA [Hazard ratio, 1.19 (1.04-1.37); p=0.009 versus noncancer]. There was no difference in procedural risk between cancer and non-cancer patients.
CONCLUSION: Active cancer, but not a history of cancer was associated with increased in-hospital mortality among AF patients who underwent CA.
193
ABSTRACT #119 CLINICAL RESEARCH CARDIOLOGY
THIRTY DAY READMISSION OUTCOMES OF PERCUTANEOUS LEFT ATRIAL APPENDAGE OCCLUSION IN PATIENTS WITH CANCER
Yaqi Zhang, Zhuoran Yang2 , Raquel Soon-Shiong1, Muhammad Usman Almani1, Bolun Liu3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mayo Clinic Health System, Mankato, MN, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Percutaneous left atrial appendage occlusion (LAAO) has been rapidly evolving since FDA’s approval in 2015, and has become more of a same-day-discharge procedure. Cancer patients who underwent LAAO are known to have more inpatient complications and longer hospital stay. Readmission data, however, were rarely studied in this patient population. Readmission burden is relatively high in cancer patients who received LAAO.
METHODS: Data were derived from the National Readmission Database from 2016 to 2019. Patients with primary diagnosis of atrial fibrillation or flutter admitted for percutaneous LAAO (ICD-10 code 02L73DK) were grouped by cancer as a secondary diagnosis. We assessed inpatient mortality, length of stay, total charges and procedure complications from index hospitalization. We also compared readmission rate and most common readmission reasons. Stata SE 17.0 was used for data analysis.
RESULTS: There were 49882 index hospitalizations for LAAO, among which 1545 (3.1%) patients had a secondary diagnosis of cancer. From index hospitalizations, patients with cancer had higher inpatient mortality (0.65% versus 0.14%, p=0.007), longer length of stay (1.54±0.08 versus 1.31 ± 0.01, p<0.001) and higher total charges (120.25 ± 3.44 versus 117.29 ± 2.40, p<0.001). There was no statistical significance of 30-day readmission rate between patients with cancer and patients without cancer (10.0% versus 9.1%, p=0.34). The most common readmission reason in cancer patients was gastrointestinal bleeding.
CONCLUSION: Readmission utilization is comparable between patients with cancer and patients without cancer who underwent LAAO.
194
ABSTRACT #120 CLINICAL RESEARCH CARDIOLOGY
UTILIZATION AND IN-HOSPITAL OUTCOMES OF PERCUTANEOUS LEFT ATRIAL APPENDAGE OCCLUSION IN PATIENTS WITH CANCER
Yaqi Zhang1 ,Zhuroran Yang1 ,Raquel Soon-Shiong1,Muhammad Usman Almani1,Ufuk Vardar1,Sami Shoura1 , Sadichhya Karki1, Bolun Liu3
1John H. Stroger, Jr. Hospital of Cook County, Chicago, IL, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mayo Clinic Health System, Mankato, MN, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Chicago, Illinois, United States from November 5-7, 2022.
BACKGROUND/INTRODUCTION: Percutaneous left atrial appendage occlusion (LAAO) has been increasingly utilized since the approval of the Watchman device in 2015, which is emerging as an alternative to anticoagulation in patients with atrial fibrillation or atrial flutter (AF/AFL). AF/AFL is a common comorbidity in cancer patient, who usually possess higher risk of ischemic or bleeding events. The objective of this study was to investigate the utilization of LAAO in cancer patients with AF/AFL and a sequence of in-hospital outcomes.
METHODS: Data were derived from the National Inpatient Sample database from 2016 to 2019. Patients with primary diagnosis of AF/AFL admitted for percutaneous LAAO (ICD-10 code 02L73DK) were grouped by cancer as a secondary diagnosis. We assessed primary outcomes including in-hospital mortality, length of stay, total hospital charges, and complications as secondary outcomes. Predictors of primary outcomes and complications were also analyzed.
RESULTS: Percutaneous LAAO was performed in 60,380 patients with AF/AFL, among which cancer patients accounted for 3%. Baseline characteristics showed cancer patients undergoing percutaneous LAAO were older, more male patients, and more cases with renal failure, anemia or coagulopathy as comorbidities. There were no differences in in-hospital mortality and total hospital charges; however, cancer patients tended to have longer hospital stay (1.59 ± 0.11 days versus 1.32 ± 0.02 days, p=0.013). As for complications, cancer patients carried high risk for open/percutaneous pericardial drainage [adjusted odds ratio (aOR), 2.38; 95% confidence interval (CI), 1.19-4.76] and major bleeding events (aOR, 7.07; 95% CI, 1.82-27.38).
CONCLUSION: Percutaneous LAAO is a promising procedure in cancer patients complicated by AF/AFL and contraindication to anticoagulation, but more cases and longer observation time need to be conducted to assist with balancing risks and benefits and minimizing complications in this specific patient population.
195
Publications 2022-2023 196
LIST OF PUBLICATIONS 2022-2023*
1
Arpanjeet Kaur, Davendra Mehta, Kiran Mahmood, Jacqueline Tamis-Holland. “A Rare Case of Blue-Gray Discoloration Induced by Low-Dose Amiodarone.” American Journal of Cardiology, 2023. PMID: 36527997 2
Kirtipal Bhatia, Vardhmaan Jain, Michael J. Hendrickson, Devika Aggarwal, Jose S. Aguilar-Gallardo, Persio D. Lopez, Bharat Narasimhan, Lingling Wu, Sameer Arora, Aditya Joshi, Matthew I. Tomey, Kiran Mahmood, Arman Qamar, Edo Y. Birati, Arieh Fox. “Meta-Analysis Comparing Venoarterial Extracorporeal Membrane Oxygenation with or Without Impella in Patients With Cardiogenic Shock.” American Journal of Cardiology, 2022. PMID: 3599070 3
Álvaro Lorente-Ros, Gonzalo L. Alonso-Salinas, Juan M. Monteagudo Ruiz, María Abellás-Sequeiros, José M. Vieítez-Florez, Diego Sánchez Vega, Jesús Álvarez-Garcia, Marcelo Sanmartín-Fernández, Marta Lorente-Ros, Susana Del Prado Díaz, Covadonga Fernández Golfín, José L. Zamorano Gómez. “Effect of Duration of Anticoagulation in the Incidence of Stroke in Patients With Left-Ventricular Thrombus.” American Journal of Cardiology, 2022. PMID: 36243566 4
Marta Lorente-Ros, Amisha Patel, José A. Lorente, Esteban López-de-Sá. “Temporal Trend of Sex-Related Differences in the Treatment of ST-segment elevation Myocardial Infarction in Young Patients.” American Journal of Cardiology, 2022. PMID: 35193766 5
Shahab Hajibandeh, Shahin Hajibandeh, Christina Intrator, Karim Hassan, Mantej Sehmbhi, Jigar Shah, Eshan Mazumdar, Ambareen Kausar, Thomas Satyadas. “Neoadjuvant chemoradiotherapy versus immediate surgery for resectable and borderline resectable pancreatic cancer: Meta-analysis and trial sequential analysis of randomized controlled trials.” Annals of Hepato-biliary-pancreatic surgery, 2023. PMID: 36536501 6
Aaron Burshtein, Joshua Burshtein, Sergey Rekhtman. “Extragenital lichen sclerosus: a comprehensive review of clinical features and treatment.” Archives of Dermatology Research, 2023. PMID: 36198917 7
Sabrina Pan, William Zheng, Lisa Q. Rong. “Gender representation on editorial boards of anaesthesiology journals from 2010 to 2020.” British Journal of Anaesthesia, 2022. PMID: 35778275 8
Fionnuala Crowley, Meredith Mihalopoulos, Simita Gaglani, Ashutosh K. Tewari, Che-Kai Tsao, Miroslav Djordjevic, Natasha Kyprianou, Rajveer S. Purohit, Dara J. Lundon. “Prostate cancer in transgender women: considerations for screening, diagnosis and management.” British Journal of Cancer, 2023. PMID: 36261584
*Updated on April 24, 2023.
197
LIST OF PUBLICATIONS 2022-2023*
9
Nadeem Bilani, Fionnuala Crowley, Mohamed Mohanna, Mira Itani, Marita Yaghi, Diana Saravia, Iktej Jabbal, Barbara Dominguez, Hong Liang, Zeina Nahleh. “Does the 21-gene recurrence score have clinical utility in HR+/HER2+ breast cancer?” Breast, 2022. PMID: 36137495 10
Marita Yaghi, Nadeem Bilani, Barbara Dominguez, Iktej Singh Jabbal, Carlos Rivera, Maroun Bou Zerdan, Hong Li, Diana Saravia, Elizabeth Stone, Zeina Nahleh. “Management of HR+/HER2+ lobular breast cancer and trends do not mirror better outcomes.” Breast, 2022. PMID: 3560346 11
Iktej S. Jabbal, Alok Dwivedi, Nadeem Bilani, Barbara Dominguez, Gehan Botrus, Zeina Nahleh. “Disparities in Metabolic Conditions and Cancer Characteristics among Hispanic Women with Breast Cancer: A Multi-Institutional Study.” Cancers (Basel), 2022. PMID: 35884473 12
Marita Yaghi, Nadeem Bilani, Barbara Dominguez, Maroun Bou Zerdan, Hong Li, Diana Saravia, Elizabeth Stone, Zeina Nahleh. “Efficacy of chemotherapy in patients with HR+/HER2-Invasive lobular breast cancer.” Cancer Treatment and Research Communications, 2023. PMID: 36525755 13
Keshav Dixit, William H. Frishman. “Postural Tachycardia Syndrome and COVID-19: Focus on Ivabradine Therapy.” Cardiology in Review, 2022. PMID: 36729924 14
Marta Lorente-Ros, Subrat Das, Joseph Elias, William H. Frishman, Wilbert S. Aronow. “Cardiovascular Manifestations of the Long COVID Syndrome.” Cardiology in Review, 2023. PMID: 37071080 15
Jiasheng Yin, Rui Wang, Han Chen, Hao Lu, Zhuoran Yang, Fei Xu, Tongtong Zang, Chengpeng Liu, Li Shen, Junbo Ge. “In vivo evaluation of intravascular lithotripsy in a healthy porcine coronary model.” Catheter and Cardiovascular Interventions, 2023.
PMID: 36934416 16
Arthur Y. Shou, Mary M. Salvatore. “CT predictors of outcomes in patients with connective tissue disease and progressive lung fibrosis.” Clinical Imaging, 2023.
PMID: 36493681 17
Marcia Lange, Priyanka Boddu, Ayushi Singh, Benjamin D. Gross, Xueyan Mei, Zelong Liu, Adam Bernheim, Michael Chung, Mingqian Huang, Joy Masseaux, Sakshi Dua, Samantha Platt, Ganesh Sivakumar, Cody DeMarco, Justine Lee, Zahi A. Fayad, Yang Yang, Maria Padilla, Adam Jacobi. “Influence of Thoracic Radiology training on classification of interstitial lung diseases.” Clinical Imaging, 2023. PMID: 36868033
*Updated on April 24, 2023.
LIST OF PUBLICATIONS 2022-2023*
18
Nikhila Chelikam, Vandit Vyas, Lavanya Dondapati, Beshoy Iskander, Ghanshyam Patel, Siddhant Jain, Tanvi Singla, Ali Bombaywala, Daniel Zarrate, Neha Debnath, Nitesh K. Jain, Appala Suman Peela, Urvish K. Patel, Amit Sharma. “Epidemiology, Burden, and Association of Substance Abuse Amongst Patients with Cardiovascular Disorders: National Cross-Sectional Survey Study.” Cureus, 2022. PMID: 35989848 19
Connor Smith, Olivia Mobarakai, Amber Bux, Ralph Kamel, Neville Mobarakai “Secondary Pneumothorax induced by a bronchopleural fistula in a patient with COVID-19 pneumonia.” Cureus, 2022. PMID: 35949739 20
Allen J. Weiss, Marta Lorente-Ros, Ashish Correa, Nitin Barman, Jacqueline E. TamisHolland. “Recent Advances in Stent Technology: Do They Reduce Cardiovascular Events?” Current atherosclerosis reports, 2023. PMID: 35821187 21
Sumit Sohal, Sheetal Vasundara Mathai, Kevin Lipat, Arpanjeet Kaur, Gautam Visveswaran, Marc Cohen, Sergio Waxman, Nidhish Tiwari, Esad Vucic. “Multimodality Imaging of Constrictive Pericarditis: Pathophysiology and New Concepts.” Current Cardiology Reports, 2023. PMID: 35917048 22
Ramesh Holla, Darshan Bhagawan, Bhaskaran Unnikrishnan, Durga Nandhini Masanamuthu, Srinjoy Bhattacharya, Arushi Kejriwal, Vetha Palani Chellakkannu, Nidhi Shreshtha, Errol Moras. “Risk Assessment for Diabetes Mellitus by Using Indian Diabetes Risk Score Among Office Workers of Health Institutions of South India.” Current Diabetes Review, 2022. PMID: 34823460
Sandipan Chakraborty, Subrat Kumar Das, Marta Lorente-Ros, Neelkumar Patel, Adrija Hajra, Dhrubajyoti Bandyopadhyay, Aaqib Malik, Akshay Goel, Sabyasachi Mukhopadhyay, Wilbert S. Aronow. “Impact of Pulmonary Hypertension in Patients With Hypertrophic Cardiomyopathy Presented With Cardiogenic Shock/Acute Decompensated Heart Failure.” Current problems in Cardiology, 2023.PMID: 35577078 24
Alaa Mabrouk Salem Omar, Swiri Konje, Alba Muñoz-Estrella, Loba Alam, Kruti Gandhi, Errol Moras, Brissete Mancero, Arpanjeet Kaur, Elizabeth Zipf, David Meister, Maria Peña, Christopher Perez-Lizardo, Ga Hee Kim, Joseph Elias, Edgar Argulian.
“Prognostic significance of incorporating exercise tissue doppler mitral annular early diastolic velocity in exercise diastolic dysfunction assessment.” Echocardiography, 2023.
PMID: 37076781 25
Keerthana Haridas. “Hypercalcemia in the setting of HTLV-1 infection and a normal PTHrP level.” Endocrinology, Diabetes, and Metabolism Case Reports, 2022.
PMID: 36137195
*Updated on April 24, 2023.
23
199
LIST OF PUBLICATIONS 2022-2023*
26
Bruno Almeida Costa, Fernando Barroso Duarte, João Vitor Araújo Duarte, Isabella Araújo Duarte, Karine Sampaio Nunes Barroso, Alexia Triandopolis Gonçalves. “Nontyphoidal Salmonellosis Leading to Fatal Outcome in an Allogeneic Hematopoietic Stem Cell Transplant Recipient from Northeastern Brazil.” Experimental and Clinical Transplantation, 2023. PMID: 37073996 27
Merav Koschitzky, Kristina Navrazhina, Michael S. Garshick, Juana Gonzalez, Joseph Han, Sandra Garcet, James G. Krueger. “Ustekinumab reduces serum protein levels associated with cardiovascular risk in psoriasis vulgaris.” Experimental Dermatology, 2022. PMID: 35474520 28
Marta Lorente-Ros, Jose S. Aguilar-Gallardo, Aayush Shah, Bharat Narasimhan, Wilbert S. Aronow. “An overview of mineralocorticoid receptor antagonists as a treatment option for patients with heart failure: the current state-of-the-art and future outlook.” Expert Opinion in Pharmacotherapy, 2022. PMID: 36262014 29
Anjali J. Ravichandran, Francisco J. Romeo, Renata Mazurek, Kiyotake Ishikawa. “Barriers in Heart Failure Gene Therapy and Approaches to Overcome Them.” Heart, Lung, and Circulation Journal, 2023. PMID: 37045653 30
Frank R. Chen, Theodore Quan, Sabrina Pan, Joseph E. Manzi, Melina Recarey, Amil R. Agarwal, Allen Nicholson, Zachary R. Zimmer, Lawrence Gulotta, Joshua S. Dines. “Anesthesia Type and Postoperative Outcomes for Patients Receiving Arthroscopic Rotator Cuff Repairs.” HSS Journal: The Musculoskeletal Journal of Hospital for Special Surgery, 2022. PMID: 36263279 31
Maan El Halabi, James Feghali, Jeeyune Bahk, Paulino Tallón de Lara, Bharat Narasimhan, Kam Ho, Mantej Sehmbhi, Joseph Saabiye, Judy Huang, Georgina Osorio, Joseph Mathew, Juan Wisnivesky, David Steiger. “A novel evidence-based predictor tool for hospitalization and length of stay: insights from COVID-19 patients in New York City.” Internal and Emergency Medicine, 2022. PMID: 35773370 32
Scott Stratman, Caralin Schneider, Daniela Sanchez, Hadar Lev-Tov. “Burden of food insecurity among people with cutaneous ulcers.” International Journal of Dermatology, 2022. PMID: 34748209 33
Iktej S. Jabbal, Nadeem Bilani, Marita Yaghi, Leah Elson, Hong Liang, Zeina A. Nahleh. “Geographical Disparities and Factors Associated With the Decision to Decline Chemotherapy in Breast Cancer.” JCO Oncology Practice, 2022. PMID: 35658495
*Updated on April 24, 2023.
LIST OF PUBLICATIONS 2022-2023*
34
Diana Khatib, Peter J. Neuburger, Sabrina Pan, Lisa Q. Rong. “Transcatheter Mitral Valve Interventions for Mitral Regurgitation: A Review of Mitral Annuloplasty, Valve Replacement, and Chordal Repair Devices.” Journal of Cardiothoracic and Vascular Anesthesia, 2022. PMID: 35871885 35
Sabrina Pan, Sasha Shillcutt, Daryl Oakes, Jochen D. Muehlschegel, Linda ShoreLesserson, Lisa Q. Rong. “Gender of Abstract Presenters at the Annual Meetings of the Society of Cardiovascular Anesthesiologists and American Society of Anesthesiologists: 2016 to 2020.” Journal of Cardiothoracic and Vascular Anesthesia, 2022.
PMID: 34916140 36
Subrat Das, Marta Lorente-Ros, Lingling Wu, Davendra Mehta, Ranjit Suri. “Safety of left atrial appendage closure in heart failure patients.” Journal of Cardiovascular Electrophysiology, 2022. PMID: 36125496 37
Renata Mazurek, Taro Kariya, Tomoki Sakata, Spyros A Mavropoulos, Anjali J Ravichandran, Francisco J. Romeo, Kelly P Yamada, Kiyotake Ishikawa “Negative Impact of Acute Reloading after Mechanical Left Ventricular Unloading.” Journal of Cardiovascular Translational Research, 2023. PMID: 37022610 38
Olga Marushchak, Matthew Gagliotti, Anjali S. Vekaria, Gary Goldenberg. “A Pilot Study of Clindamycin Phosphate 1.2% and Benzoyl Peroxide 3.75% Combination Gel in the Treatment of Perimenstrual Acne.” Journal of Clinical and Aesthetic Dermatology, 2023.
PMID: 36381180 39
Olga Marushchak, Rebecca Yakubov, Rose Yakubov, Gary Goldenberg. “New Technologies in Diagnosis and Prognosis of Melanocytic Lesions.” Journal of Clinical and Aesthetic Dermatology, 2023. PMID: 36909871 40
Joseph Han, Scott Stratman, Jade N. Young, Dina Poplausky, Shayan Owji, Yen Luu, Yeriel Estrada, Joel Correa de Rosa, James G. Krueger, Nicholas Gulati. “Unique protein signatures evolve during the course of a delayed-type hypersensitivity reaction in human skin.” Journal of Dermatology, 2022. PMID: 36578124 41
Sandhya Deverapalli, Jared Kahn, David Rosmarin. “A Potential Alternative Treatment for Vitiligo: An Observational Study on Tacrolimus 0.3% Lotion.” Journal of Drugs in Dermatology, 2022. PMID: 36468953 42
Shaun E. Gruenbaum, Federico Bilotta, Tais Garcia de Oliveira Bertasi, Raphael Adroaldo de Oliveira Bertasi, William E. Clifton, Benjamin F. Gruenbaum, Gaetano De Biase, Diogo M. Garcia, Elird Bojaxhi, Klaus D. Torp, Alfredo Quinones-Hinojosa. “Emergency Airway Management During Awake Craniotomy: Comparison of 5 Techniques in a Cadaveric Model.” Journal of Neurosurgical Anesthesiology, 2022.
PMID: 33060551
*Updated on April 24, 2023.
201
LIST OF PUBLICATIONS 2022-2023*
43
Mindy Kresch, Mark Weingarten, Sophie Guenin, Nancy Wei, Emily Elbogen, Joel Correa da Rosa, Mark Lebwohl. “Risk of rebound psoriasis flare from systemic corticosteroid use in patients with psoriasis: A retrospective cohort study.” Journal of the American Academy of Dermatology, 2023. PMID: 36538947 44
Francisco José Romeo, Renata Mazurek, Tomoki Sakata, Spyros A. Mavropoulos, Kiyotake Ishikawa. “Device-Based Approaches Targeting Cardioprotection in Myocardial Infarction: The Expanding Armamentarium of Innovative Strategies.” Journal of the American Heart Association, 2022. PMID: 36382949 45
Caroline Liu, Neha Debnath, Gohar Mosoyan, Kinsuk Chauhan, George Vasquez-Rios, Celine Soudant, Steve Menez, Chirag R. Parikh, Steven G. Coca. “Systematic Review and Meta-Analysis of Plasma and Urine Biomarkers for CKD Outcomes.” Journal of the American Society of Nephrology, 2023. PMID: 35858701 46
Rohit Nathani, Randy Leibowitz, Dewan Giri, Carolina Villarroel, Sidra Salman, Mantej Sehmbhi, Bo Hyung Yoon, Amreen Dinani, Ilan Weisberg. “The Delta Delta: Gaps in screening and patient assessment for hepatitis D virus infection.” Journal of Viral Hepatitis, 2023. PMID: 36458863
Victor Zibara, Filiz Sen, Michael Scordo, Lorenzo Falchi. “Successful brentuximab vedotin and nivolumab therapy of multiply refractory diffuse large B-cell lymphoma with Hodgkin features.” Leukemia and Lymphoma, 2022. PMID: 36120859
Keerthana Haridas, Michael A. Via, Jeffrey I. Mechanick. Chapter: “The New World: Endocrine Disruptors and Cardiometabolic Based Chronic Disease.” Lifestyle Medicine for Prediabetes, Diabetes and Cardiometabolic Disease: The Preventive Care Approach, 2022. Published, pending online release/print.
Jose S. Aguilar-Gallardo, Javier Arreaza, Alaa Omar, Glenmore Lasam, Johanna P. Contreras. “Successful treatment of cardiac sarcoidosis based on clinical suspicion and advanced cardiac imaging: A case report.” Medicine, 2022. PMID: 36042616
Francisco J. Romeo, Marco Del Buono, Jose S. Aguilar-Gallardo, Marta Lorente-Ros, Juan Damonte, Juan Chiabrando, Dave Dixon, Giuseppe Biondi-Zoccai, Antonio Abbate, Salvatore Carbone. “Letter to the Editor: Cardiac Remodeling with SGLT2 inhibitors in Heart Failure with Reduced Ejection Fraction.” Minerva Cardiology and Angiology, 2023. Accepted.
*Updated on April 24, 2023.
47
48
49
50
LIST OF PUBLICATIONS 2022-2023*
51 Francisco J. Romeo, Spyros A Mavropoulos, Kiyotake Ishikawa. “Progress in Clinical Gene Therapy for Cardiac Disorders.” Molecular Diagnosis & Therapy, 2023. PMID: 36641770
Xueyan Mei, Zelong Liu, Ayushi Singh, Marcia Lange, Priyanka Boddu, Jingqi Q. X. Gong, Justine Lee, Cody DeMarco, Chendi Cao, Samantha Platt, Ganesh Sivakumar, Benjamin Gross, Mingqian Huang, Joy Masseaux, Sakshi Dua, Adam Bernheim, Michael Chung, Timothy Deyer, Adam Jacobi, Maria Padilla, Zahi A. Fayad, Yang Yang. “Interstitial Lung Disease Diagnosis and Progrnosis’ using an AI system integrating longitudinal data.” Nature Communications, 2023. PMID: 37080956
Karthik Nath, Bruno Almeida Costa, Sham Mailankody. “GPRC5D as a novel immunotherapeutic target in multiple myeloma.” Nature Reviews. Clinical Oncology, 2023. PMID: 36725915
Fionnuala Crowley, Sonal Gandhi, Michelle Rudshteyn, Mantej Sehmbhi, Deirdre J. Cohen. “Adherence to NCCN Genetic Testing Guidelines in Pancreatic Cancer and Impact on Treatment.” Oncologist, 2023. PMID: 36933202
Bruno Almeida Costa, Paulino Tallón de Lara, Wungki Park, Fergus Keane, James J. Harding, Danny N. Khali. “Durable Response after Olaparib Treatment for Perihilar Cholangiocarcinoma with Germline BRCA2 Mutation.” Oncology Research and Treatment, 2023. PMID: 36882017
Laura E. Levin, Neha Kinariwalla, Gerald G. Behr, Kimberly D. Morel, Christine T. Lauren, Maria C. Garzon. “Lumps and bumps: What not to miss.” Pediatric Dermatology, 2022. PMID: 35918890 57
Olga Marushchak, Kathryn Jayne Tan, Maria Rosa noliza Encarnacion, Loren Clark, Alexandra Golant. “Acne Keloidalis Nuchae Successfully Treated with Halobetasol 0.01% and Tazarotene 0.045% Lotion.” SKIN. The Journal of Cutaneous Medicine, 2022.
https://jofskin.org/index.php/skin/article/view/1567/pdf 58
Raphael A O Bertasi, Tais G O Bertasi, Trisha E. Jethwa, George G A Pujalte. “Perioperative method of applying chlorhexidine and iodine as skin preparation solutions: does it matter? A literature review.” Surgical infections, 2022. PMID: 36067117
59
Bruno Almeida Costa, Tarek H. Mouhieddine, Joshua Richter. “What's Old is New: The Past, Present and Future Role of Thalidomide in the Modern-Day Management of Multiple Myeloma.” Targeted Oncology, 2022. PMID: 35771402
*Updated on April 24, 2023.
52
53
54
55
56
203
LIST OF PUBLICATIONS 2022-2023*
60
Elizabeth B. Elimimian, Leah Elson, Hong Li, Hong Liang, Nadeem Bilani, Emily C. Zabor, Abby Statler, Zeina Nahleh. “Male Breast Cancer: A Comparative Analysis from the National Cancer Database.” The World Journal of Men’s Health, 2021.
PMID: 33474851
61
Errol Moras, Basavaprabhu Achappa, B V Murlimanju, G M Naveen Raj, Ramesh Holla, Deepak Madi, Nikhil Victor D'Souza, Soundarya Mahalingam. “Early diagnostic markers in predicting the severity of dengue disease.” 3 Biotech, 2022. PMID: 36091089
62
Francisco J. Romeo, Spyros A. Marvopoulos and Kiyotake Ishikawa. Chapter 1: “Overview of cardiac gene therapy.” Updates on cardiac gene therapy research and methods, 2nd edition, 2022.
*Updated on April 24, 2023.
Index of Posters

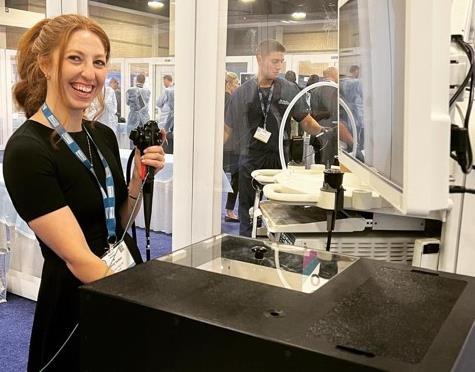
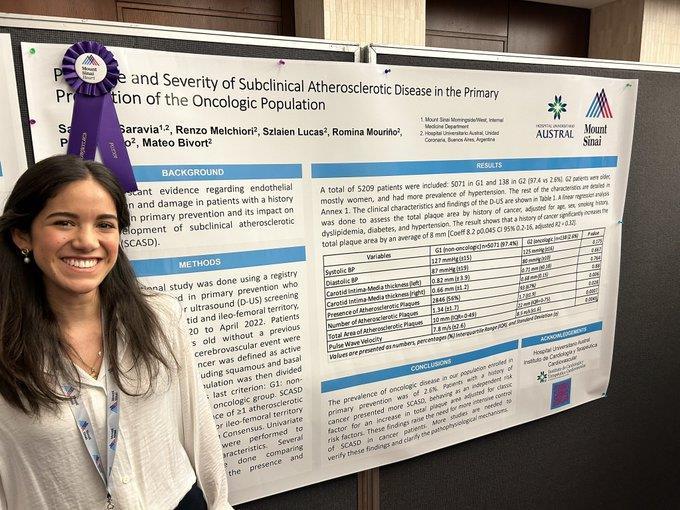
205
RESIDENT NAME POSTER CATEGORY POSTER Aguilar Gallardo, José Clinical Research 1 Akhlaghi, Marie Jasmin Theresia Clinical Research 2 Al khalili, Nour Clinical Research 3 Alexander, Matthew Clinical Research 4 Amel Riazat-Kesh, Yosef Joseph Rene Clinical Research 5 Arango Morales, Juan Case Report/Clinical Review/Clinical Vignette 6 Bahk, Jeeyune Clinical Research 7 Balboul, Yoni Clinical Research 8 Belfaqeeh, Omar Case Report/Clinical Review/Clinical Vignette 9 Bilani, Nadeem Clinical Research 10 Buckley, Conor Case Report/Clinical Review/Clinical Vignette 11 Caceros Diaz, Salvador Case Report/Clinical Review/Clinical Vignette 12 Chernyk, Adrian Case Report/Clinical Review/Clinical Vignette 13 Chon, Christy Case Report/Clinical Review/Clinical Vignette 14 Chowdhury, Nobel Case Report/Clinical Review/Clinical Vignette 15 Costa, Bruno Case Report/Clinical Review/Clinical Vignette 16 Courant, Vincent Case Report/Clinical Review/Clinical Vignette 17 Crowley, Fionnuala Clinical Research 18 Cuan, Katherine Case Report/Clinical Review/Clinical Vignette 19 Danso, Lady Njemeh Case Report/Clinical Review/Clinical Vignette 20 206
RESIDENT NAME POSTER CATEGORY POSTER Dunker del Rosario, Dalgis Quality Improvement 21 Elias, Joseph Clinical Research 22 Feng, Jin Clinical Research 23 Fenianos, Madelin Quality Improvement 24 Fermin, Debbie Marie Case Report/Clinical Review/Clinical Vignette 25 Gandhi, Kruti Clinical Research 26 Gold, Christopher Case Report/Clinical Review/Clinical Vignette 27 Haddadin, Suhail Clinical Research 28 Haridas, Keerthana Case Report/Clinical Review/Clinical Vignette 29 Hazan, Ariela Case Report/Clinical Review/Clinical Vignette 30 Horowitz, Maxwell Medical Education 31 Jaber, Faris Clinical Research 32 Kaur, Apranjeet Medical Education 33 Kawegere, Erick Case Report/Clinical Review/Clinical Vignette 34 Koh, Won Joon Clinical Research 35 Lama, Sanam Case Report/Clinical Review/Clinical Vignette 36 Leibowitz, Randy Clinical Research 37 Lorente Ros, Marta Clinical Research 38 Luby, Sara Case Report/Clinical Review/Clinical Vignette 39 Lutgen, Sophia Clinical Research 40 207
RESIDENT NAME POSTER CATEGORY POSTER Mancero, Brissete Clinical Research 41 Markley, Alexandria Clinical Research 42 Marushchak, Olga Clinical Research 43 Marx, Jonas Maximillian Basic Science 44 Matthews, Christopher Case Report/Clinical Review/Clinical Vignette 45 Meister, David Clinical Research 46 Miao, Jiaxi Case Report/Clinical Review/Clinical Vignette 47 Moras, Errol Clinical Research 48 Mueller, Anna Case Report/Clinical Review/Clinical Vignette 49 Nathani, Rohit Clinical Research 50 Olivo Freites, Cristina Clinical Research 51 Ortiz, Ricardo Medical Education 52 Pena, Maria Case Report/Clinical Review/Clinical Vignette 53 Perez Lizardo, Christopher Case Report/Clinical Review/Clinical Vignette 54 Plazola, Carlos Clinical Research 55 Riego, Maria Athena Clinical Research 56 Romeo, Francisco Clinical Research 57 Sadek, Norah Case Report/Clinical Review/Clinical Vignette 58 Sadud Armaza, Sharel Quality Improvement 59 Sehmbhi, Mantej Quality Improvement 60 208
RESIDENT NAME POSTER CATEGORY POSTER Seltzer, Emily Quality Improvement 61 Sharma, Venus Case Report/Clinical Review/Clinical Vignette 62 Shenoy, Shabari Clinical Research 63 Smith, Connor Case Report/Clinical Review/Clinical Vignette 64 Socorro Corrales, Anne Case Report/Clinical Review/Clinical Vignette 65 Vasquez Mendez, Juan Case Report/Clinical Review/Clinical Vignette 66 Vora, Aarohi Clinical Research 67 Wilkoff, Marni Case Report/Clinical Review/Clinical Vignette 68 Wilson, Eelin Case Report/Clinical Review/Clinical Vignette 69 Yang, Zhuoran Clinical Research 70 Zibara, Victor Case Report/Clinical Review/Clinical Vignette 71 209
Index of Authors


210
INDEX OF RESIDENT AUTHORS
Aguilar Gallardo, Jose: 21-22, 70, 197, 200, 202
Akhlaghi, Marie Jasmin Theresia: 23
Al Khalili, Nour: 24-25, 78, 101
Alexander, Matthew: 26-27, 135
Amel Riazat-Kesh, Yosef Joseph
Rene: 28, 143, 153
Arango, Juan: 29-30
Bahk, Jeeyune: 31-32, 48, 60, 133-134, 135, 158, 200
Balayla Rosemberg, Galit: 109
Balboul, Yoni: 33, 63, 136, 147, 161-162, 163-164
Bastos Silva, Murilo Roberto: 46
Belfaqeeh, Omar: 34-35, 102-104, 106-108, 137-138
Bilani, Nadeem: 36-37, 139, 150, 174, 198, 200, 204
Buckley, Conor: 38-39
Burshtein, Joshua: 197
Caceros Diaz, Salvador: 40, 100
Chernyk, Adrian: 41
Chon, Christy: 42, 140
Chowdhury, Nobel: 43
Costa, Bruno: 44-45, 114-115, 141, 142, 200, 203
Courant, Vincent: 46, 155
Crowley, Fionnuala: 47, 143, 153, 197, 198, 203
Cuan, Katherine: 48
Danso, Lady Njemeh: 49
De Oliveira Bertasi, Raphael: 141, 148-149, 150, 174, 176-177, 201, 203
De Oliveira Bertasi, Tais: 148-149, 150, 174, 176-177, 201, 203
Debnath, Neha: 139, 141, 143, 158, 199, 202
Diaz Saravia, Sara: 144-145
Dixit, Keshav: 166, 198
Dunker del Rosario, Dalgis: 50
Elias, Joseph: 51-52, 56, 77, 82-83, 85-86, 146, 151-152, 160, 198, 199
Feng, Jin: 53, 62
Fenianos, Madelin: 54
Fermin, Debbie Marie: 55
Gandhi, Kruti: 51-52, 56, 77, 82-83, 85-86, 146, 147, 148-149, 150, 151, 163-164, 174, 175, 176-177, 199
Gandhi, Sonal: 44-45, 47, 143, 153, 203
Gargaritano, Kristine Lou: 154
Gold, Christopher: 57
Gordon, Ariel: 60, 158
Grewal, Satwant: 46, 155
Haddadin, Suhail: 58, 156, 183
Haridas, Keerthana: 59, 61, 157
Hazan, Ariela: 60, 158
Horowitz, Maxwell: 61
Jaber, Faris: 62
Kahn, Jared: 201
Kaur, Arpanjeet: 33, 51-52, 56, 63, 77, 95, 146, 147, 155, 159, 160, 161-162, 163-164, 165, 197, 199
Kawegere, Erick: 50, 64-66
Kinariwalla, Neha: 203
Koh, Won Joon: 67
Kong, Darren: 165, 166
Koschitzky, Merav: 200
Lama, Sanam: 68
Leibowitz, Randy: 69, 167, 168, 169-170, 171, 172, 202
Lorente Ros, Marta: 70, 197, 198, 199, 200, 201, 202
Luby, Sara: 71, 95, 155, 182
Lutgen, Sophia: 72-76
Mancero, Brissete: 51-52, 56, 77, 82-83, 85-86, 146, 151-152, 199
211
INDEX OF RESIDENT AUTHORS
Maraveyas, Alexander: 171
Markley, Alexandria: 54, 78, 137-138
Marushchak, Olga: 79, 201, 203
Marx, Jonas Maximilian: 40, 80
Matthews, Christopher: 81, 84, 173
Meister, David: 51-52, 56, 77, 82-83, 85-86, 151-152, 199
Miao, Jiaxi: 84
Miguez Arosemena, Patricia: 24-25, 58, 101, 102-104, 106-108, 156
Moras, Errol; 51-52, 56, 77, 82-83, 85-86, 146, 147, 148-149, 150, 151, 174, 175, 176-177, 199, 204
Mueller, Anna: 87
Nathani, Rohit: 88, 105, 202
Olivo Freites, Cristina: 89
Ortiz, Ricardo: 90
Oxman, Jonathan: 71
Pan, Sabrina: 197, 200, 201
Peña, Maria: 51-52, 53, 77, 82-83, 85-86, 91-92, 146, 151-152, 165, 199
Perez Lizardo, Christopher: 51-52, 56, 82-83, 85-86, 93, 146, 151-152, 199
Perry, Bailey: 100
Plazola, Carlos: 94
Riego, Maria Athena: 95
Romeo, Francisco J.: 21, 70, 96-97, 106, 175, 200, 201, 202, 203, 204
Sadek, Norah: 98-99
Sadud Armaza, Sharel: 100
Salman, Sidra: 81, 187
Sehmbhi, Mantej: 60, 78, 101,
178, 197, 200, 202, 203
Seltzer, Emily: 78, 101, 102-104, 106-108, 114-115, 167, 179
Sharma, Venus: 31-32, 95, 105,
180-181, 182
Shenoy, Shabari: 101, 106-108,
179, 183, 184, 185, 186
Shou, Arthur: 198
Sivakumar, Ganesh: 198, 203
Smith, Connor: 109
Socorro Corrales, Anne: 50, 110-111
Stratman, Scott: 200, 201
Vasquez Mendez, Juan: 50, 112
Vora, Aarohi: 113
Wei, Nancy: 202
Wilkoff, Marni: 29-30, 114-115, 167
Wilson, Eelin: 116
Yang, Zhuoran: 117-118, 188-192, 193, 194, 195, 198
Zibara, Victor: 44-45, 119-120
212
John A. Andrilli, MD, FACP
Mariah Soria
Georgina Osorio, MD, MPH Eric Wu Angus Cheung
Email: msmwimresearch@mountsinai.org
Website:
https://icahn.mssm.edu/education/residencies -fellowships/list/msw-msm-internal-medicineresidency

Twitter: @msm_msw

Thank you for attending the Mount Sinai Morningside/West Internal Medicine Residency Annual Research Week!
Residency Leadership
Contact
Residency
Information
Editors
Georgina Osorio
Rebecca Pietro
Patrick Tobin-Schnittger
Eric Wu
Angus Cheung
Mariah Soria
Editorial Board
John Andrilli
Gabriela Bernal
Deborah Edelman
Lindsey Fox
Tamara Goldberg
Krystle Hernandez
Yasmin Herrera
Ga Hee Kim
Alejandro Prigollini
Adam Rothman
Vasundhara Singh
Official Publication of Annual Mount Sinai
West Internal Medicine
Morningside/
Residency Research Week


























 Valida Bajrovic Fernando Carnavali Natalie Cedeno
Maya Fakhoury
Katherine Hawkins
Sara Huda
Brian Markoff
Joseph Mathew
Doreen Mensah Argelis Rivera Samuel Seward Nirav Shah
Aakanksha Sharma Christine Stavropoulos
David Steiger
Kevin Yan
Valida Bajrovic Fernando Carnavali Natalie Cedeno
Maya Fakhoury
Katherine Hawkins
Sara Huda
Brian Markoff
Joseph Mathew
Doreen Mensah Argelis Rivera Samuel Seward Nirav Shah
Aakanksha Sharma Christine Stavropoulos
David Steiger
Kevin Yan


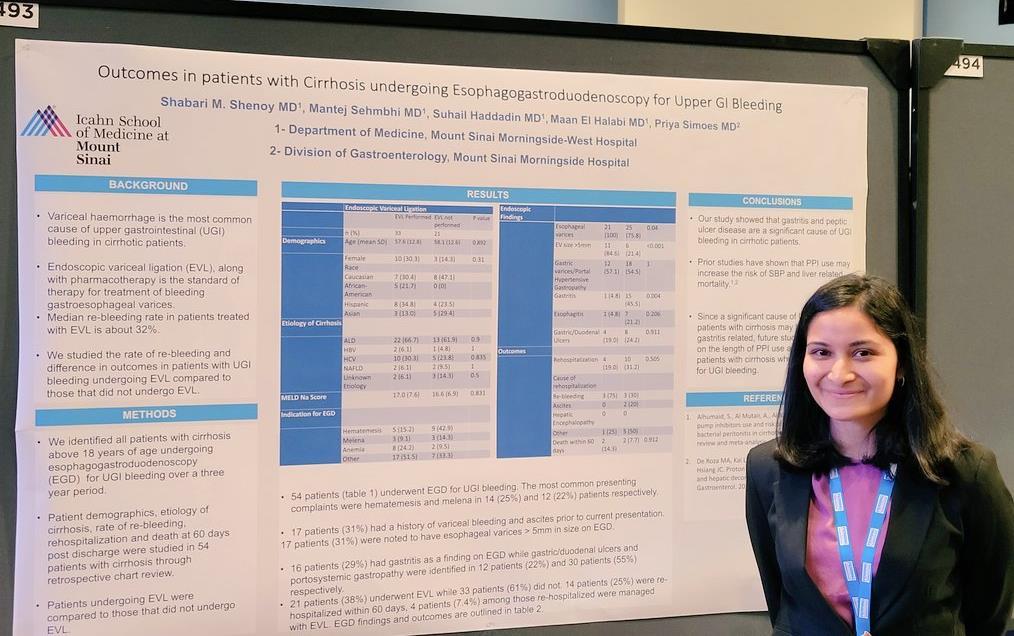

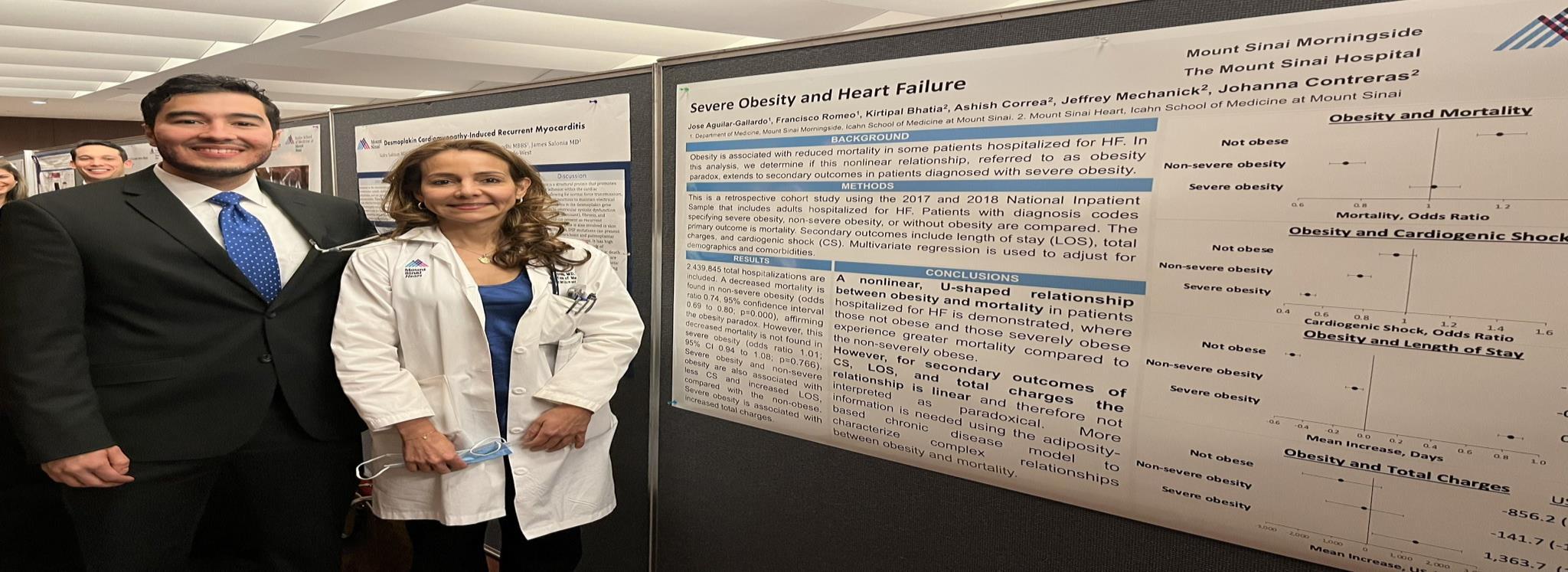
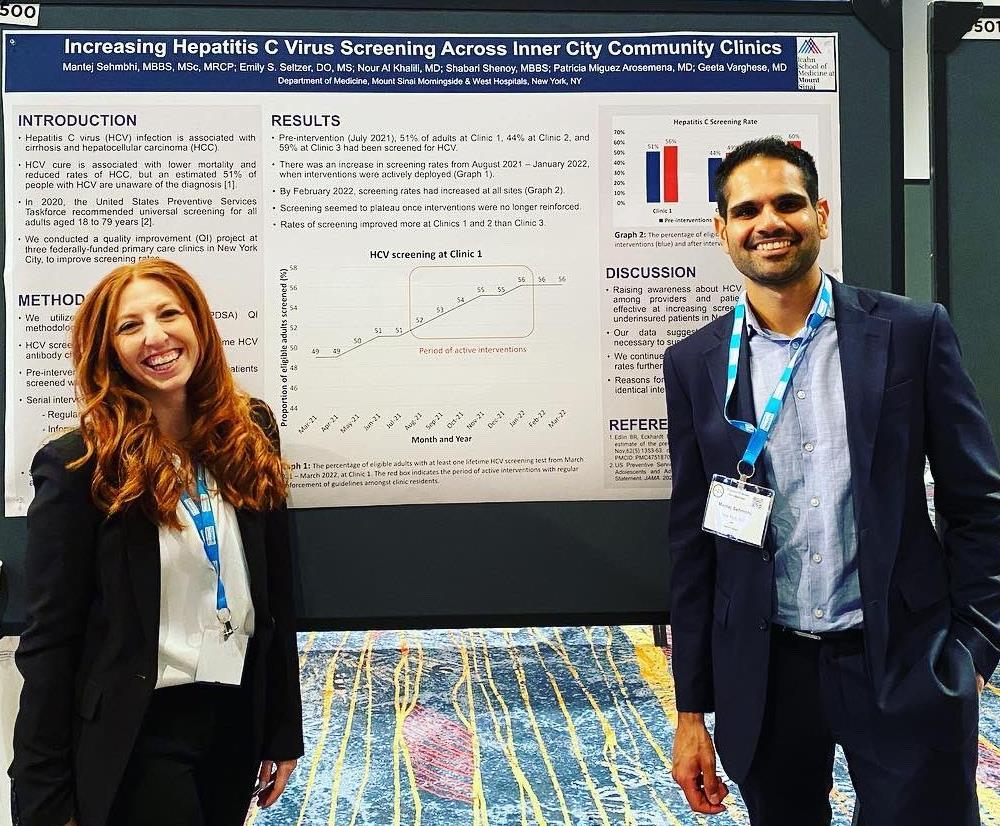
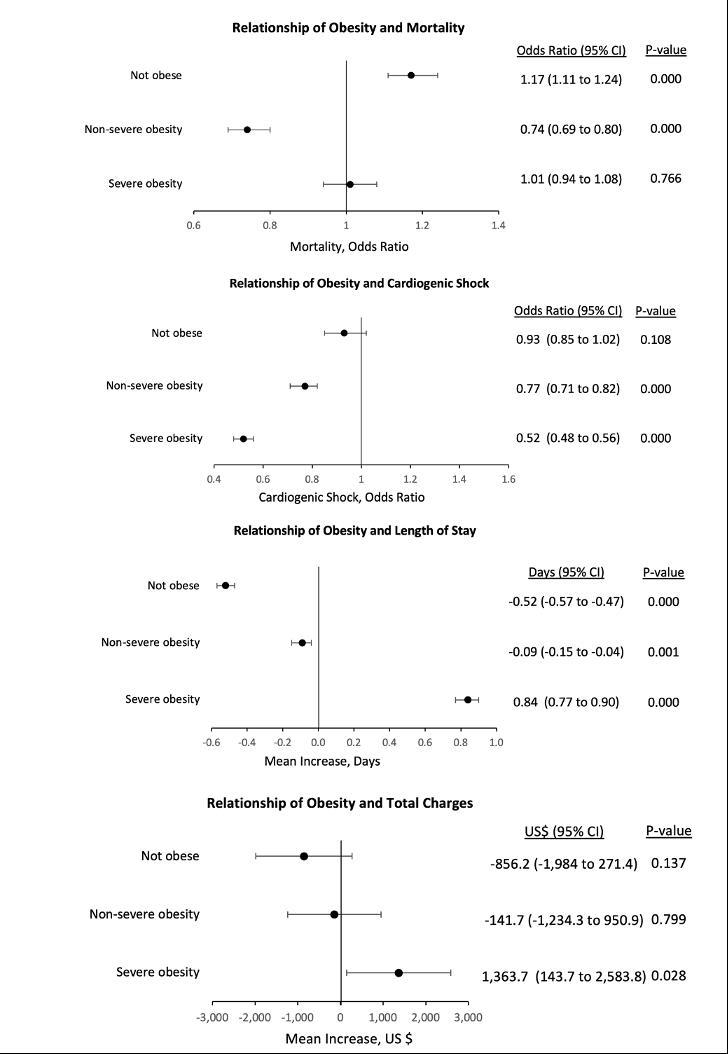

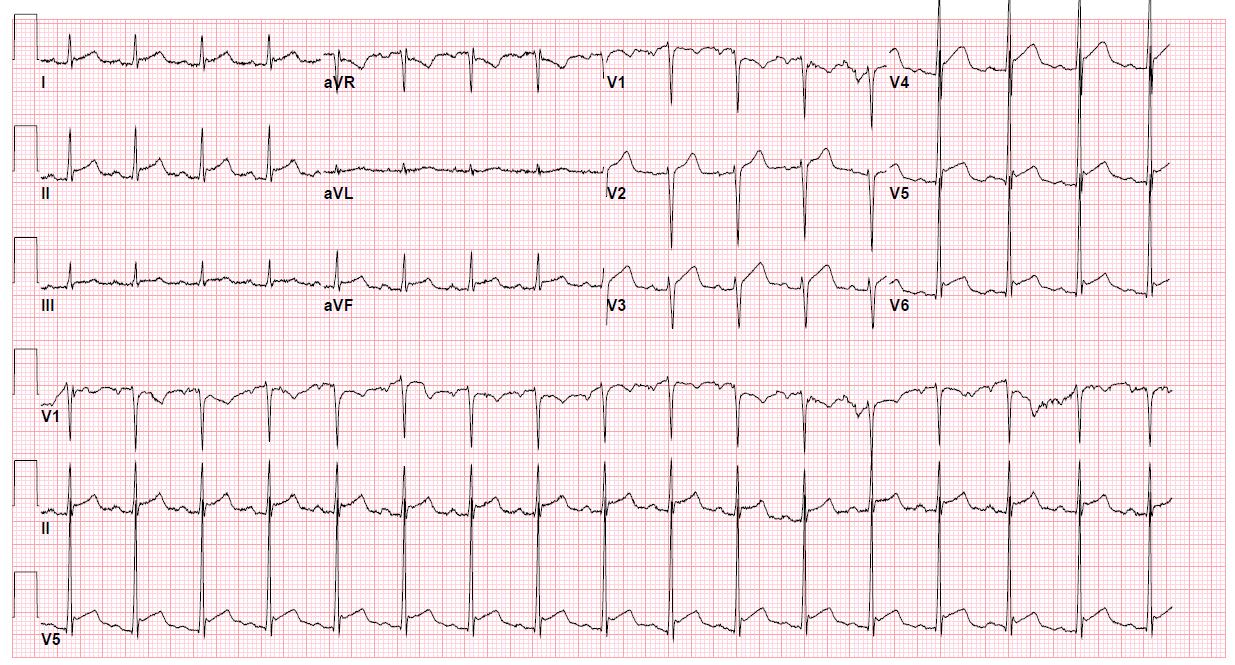
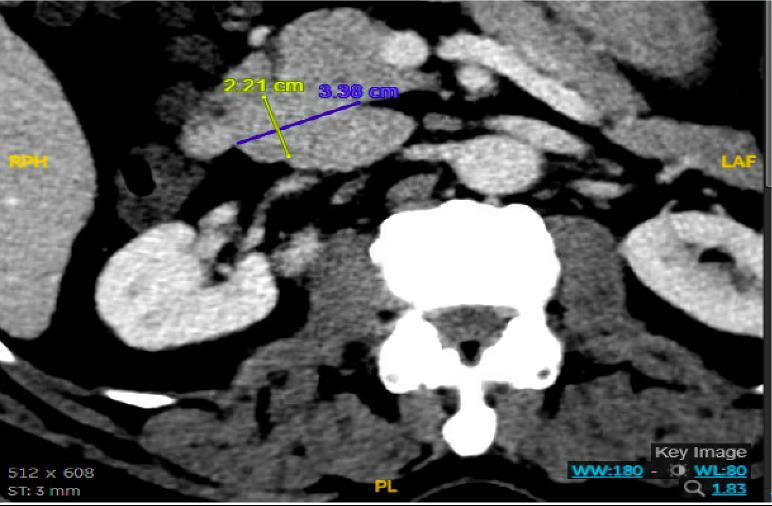
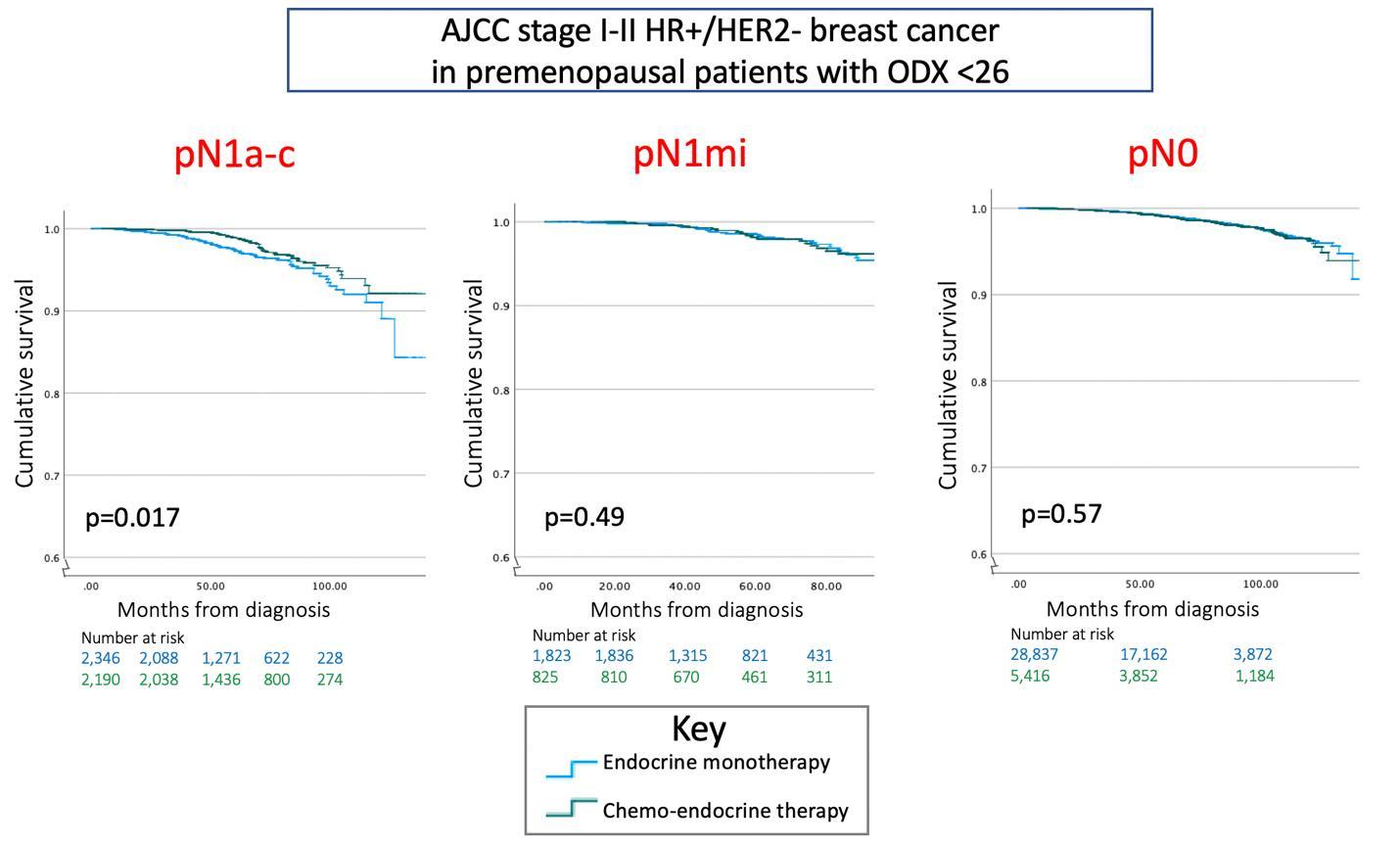

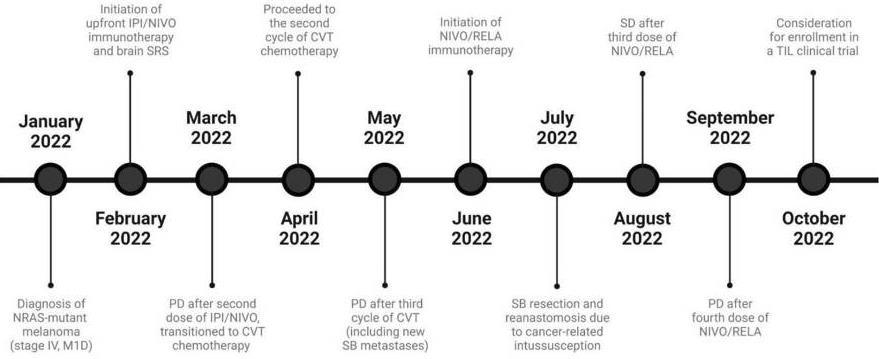 Figure 1: Clinical course timeline
Figure 1: Clinical course timeline
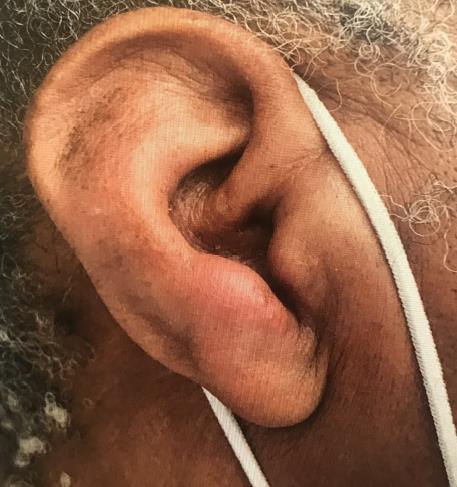
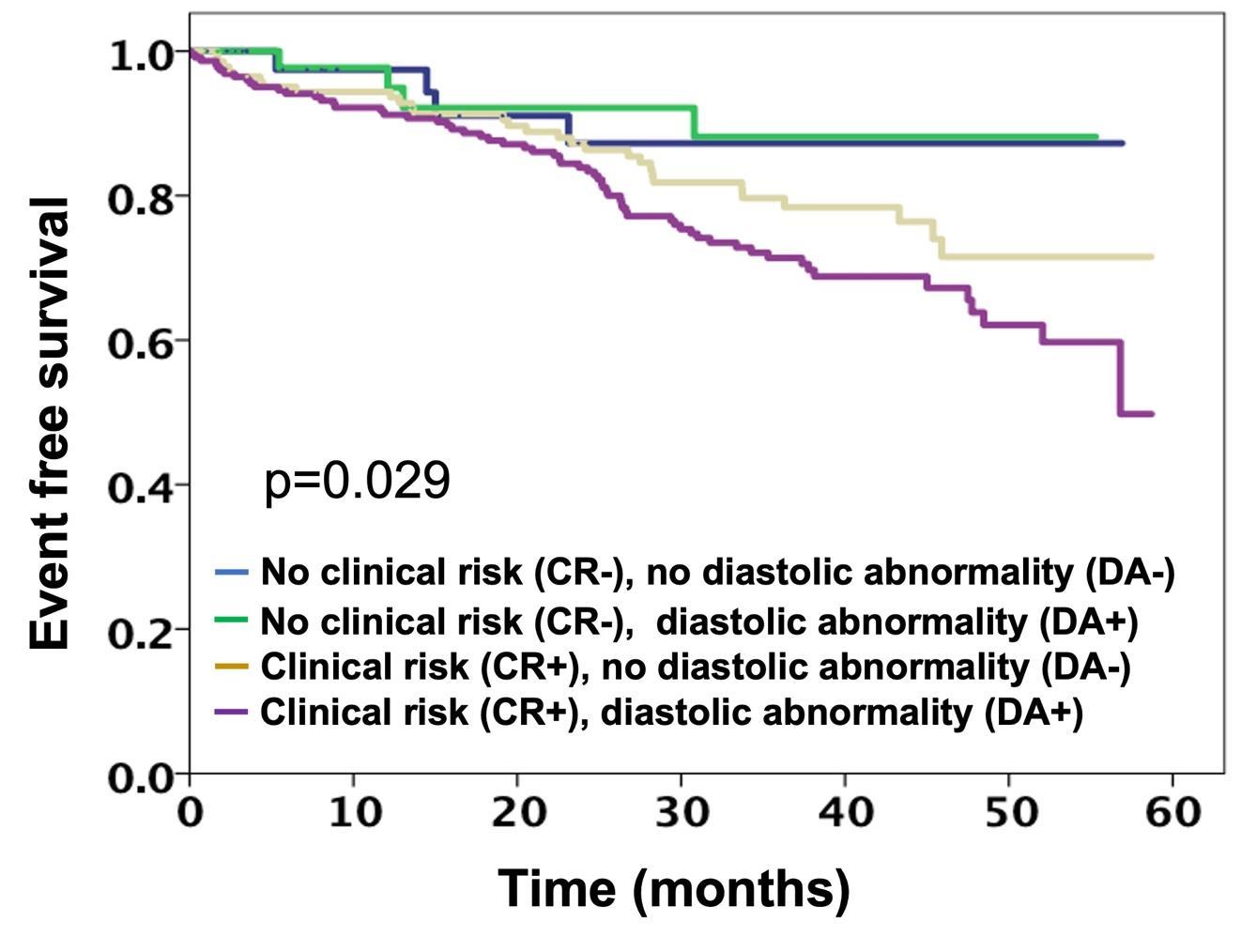
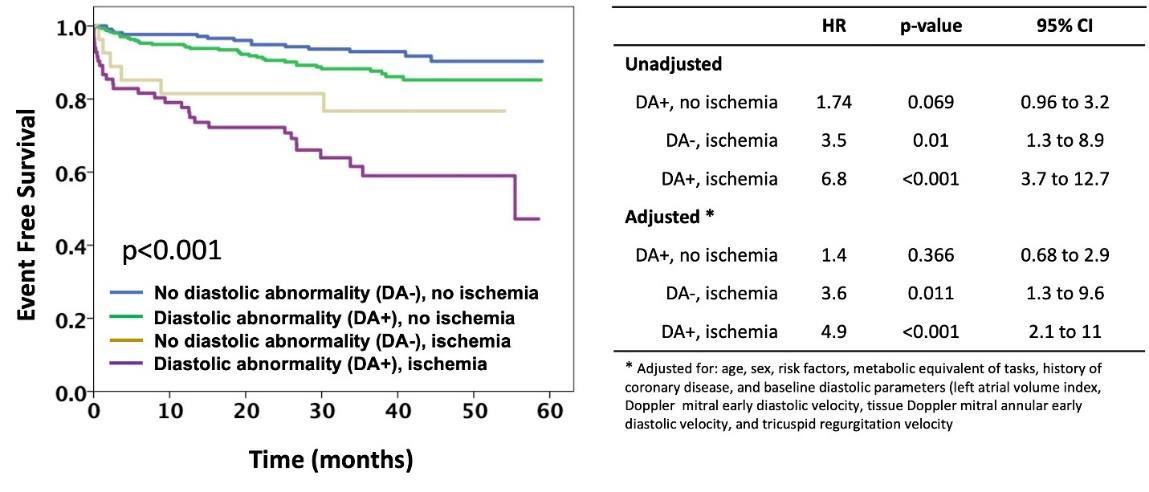

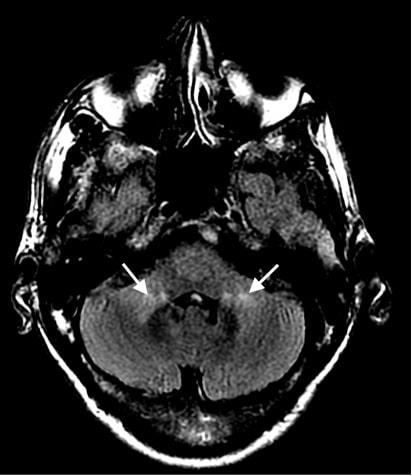 Figure 1: MRI Brain showing abnormal signal affecting the brainstem.
Figure 1: MRI Brain showing abnormal signal affecting the brainstem.
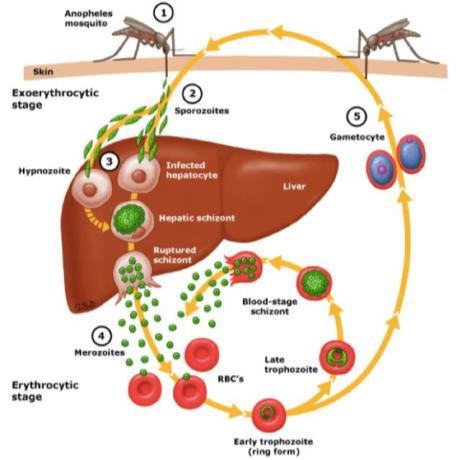
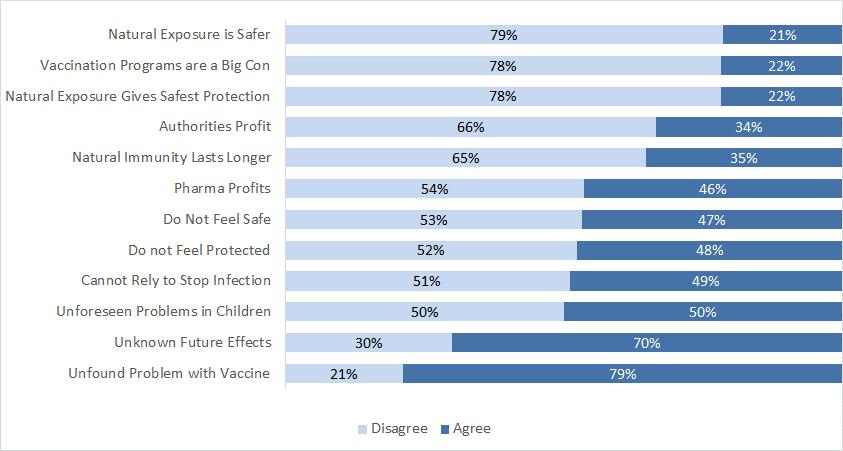
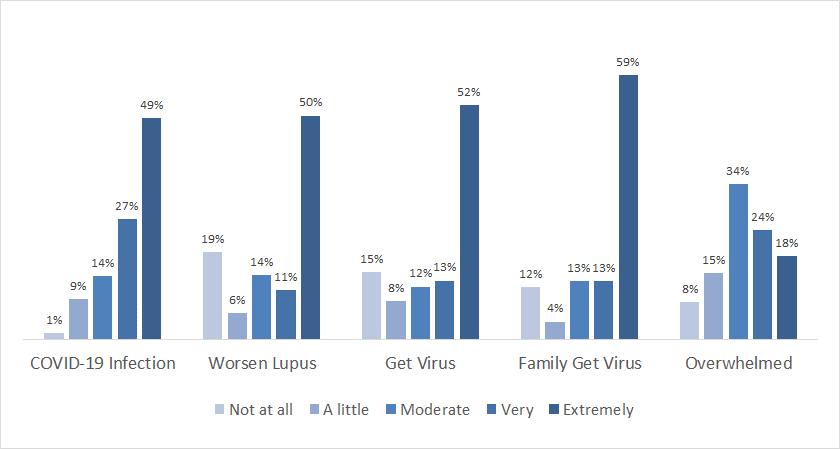 Figure 1: Vaccination Attitudes among 158 participants of a population-based cohort with a validated diagnosis of CCLE. Vaccination attitudes were measured with the Examination (VAX) Scale
Figure 1: Vaccination Attitudes among 158 participants of a population-based cohort with a validated diagnosis of CCLE. Vaccination attitudes were measured with the Examination (VAX) Scale
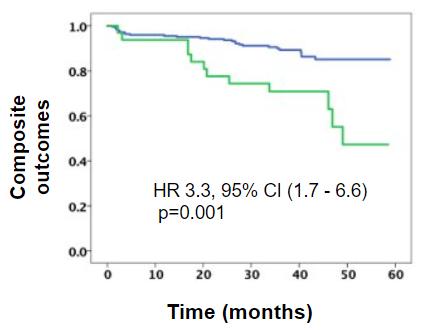
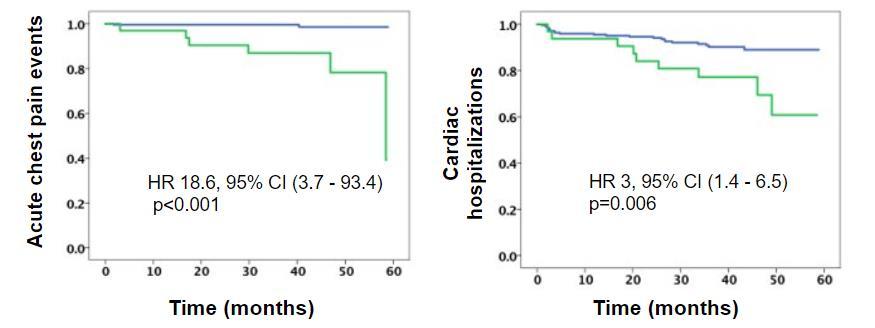
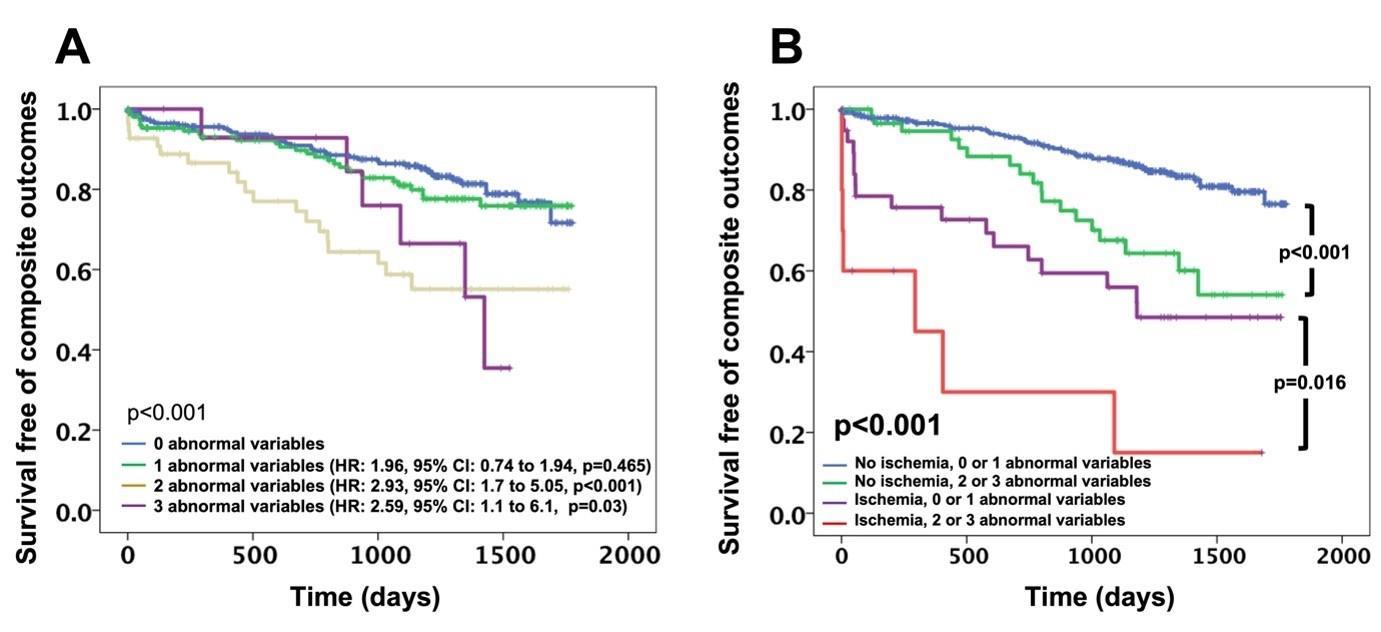
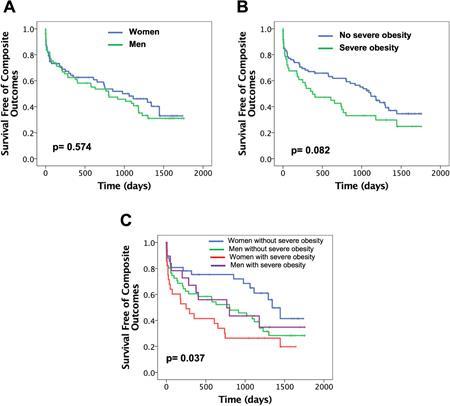
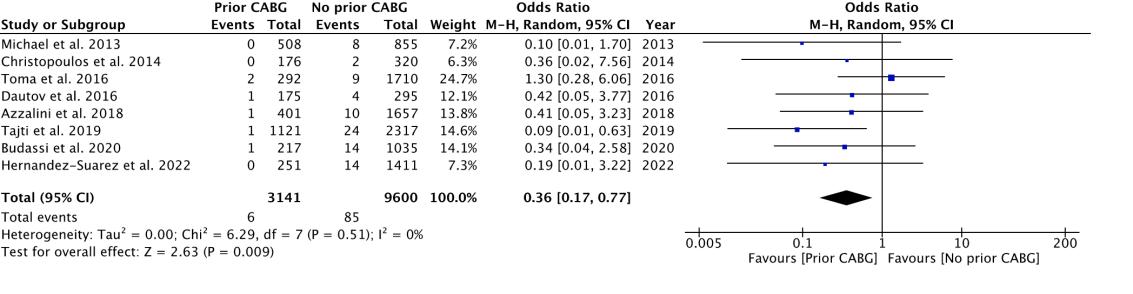
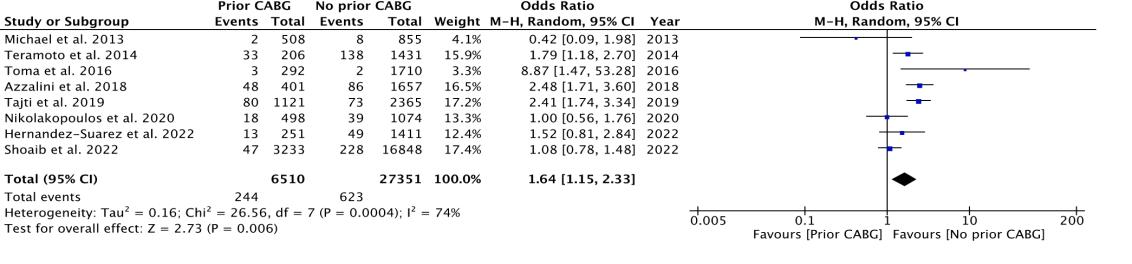
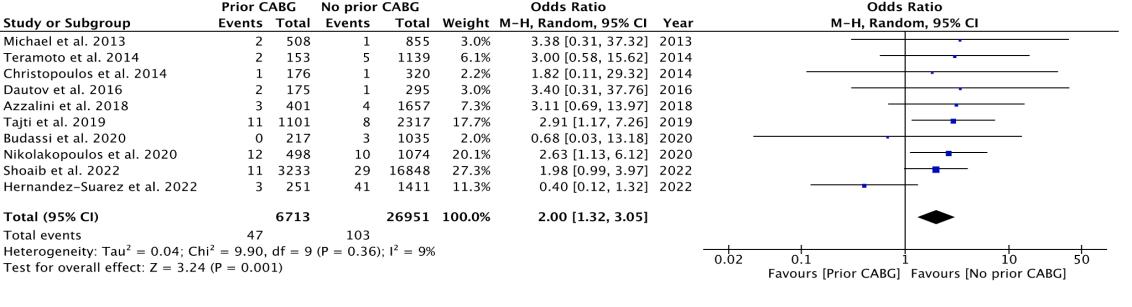
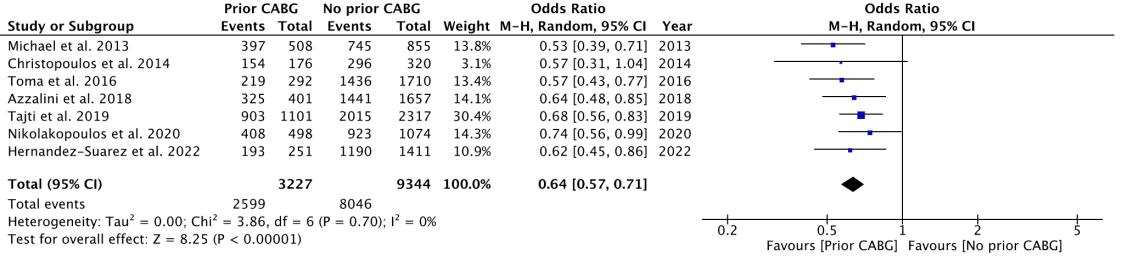
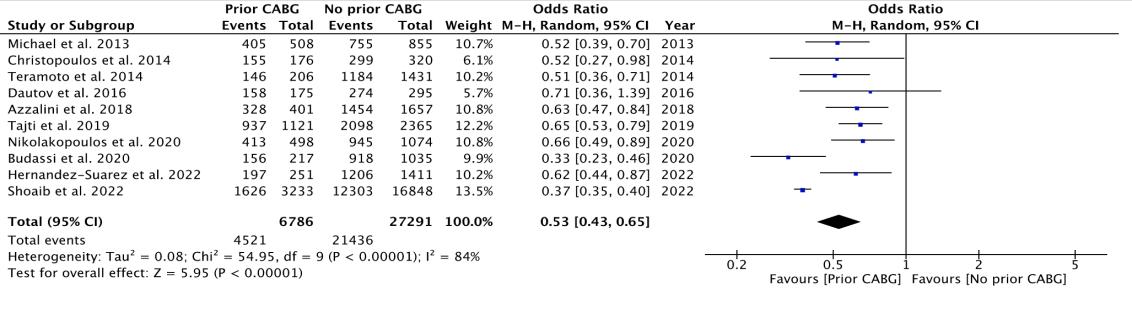
 Norah Sadek1 , Bharat Monga1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Norah Sadek1 , Bharat Monga1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
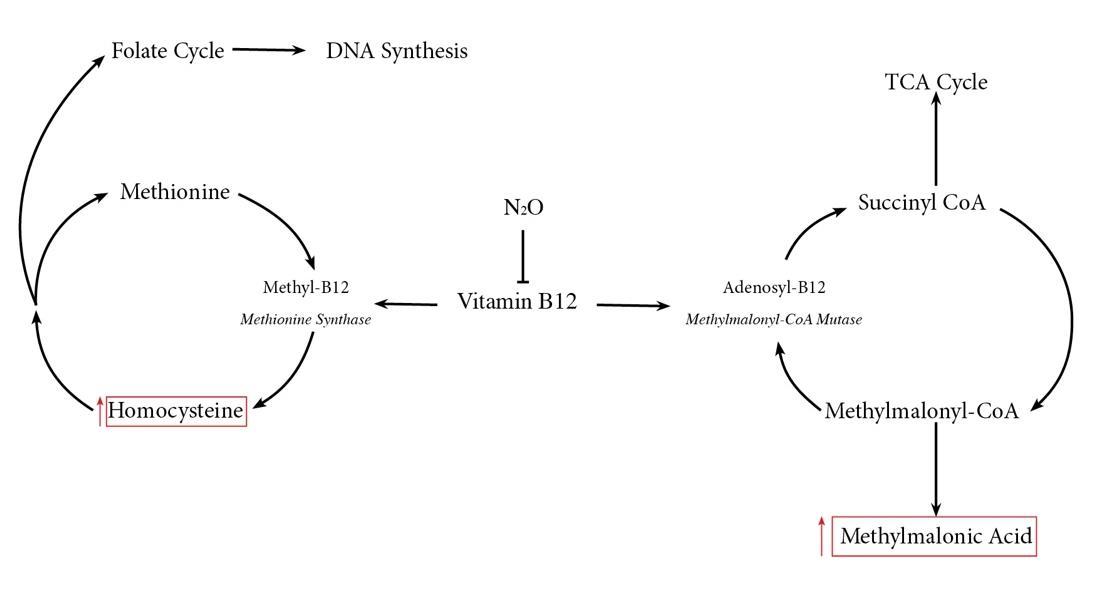



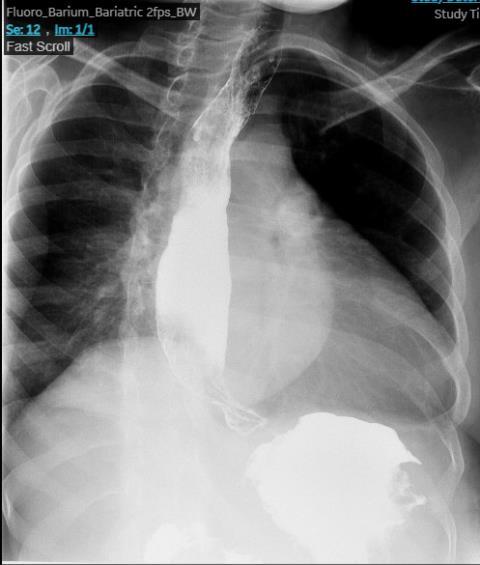
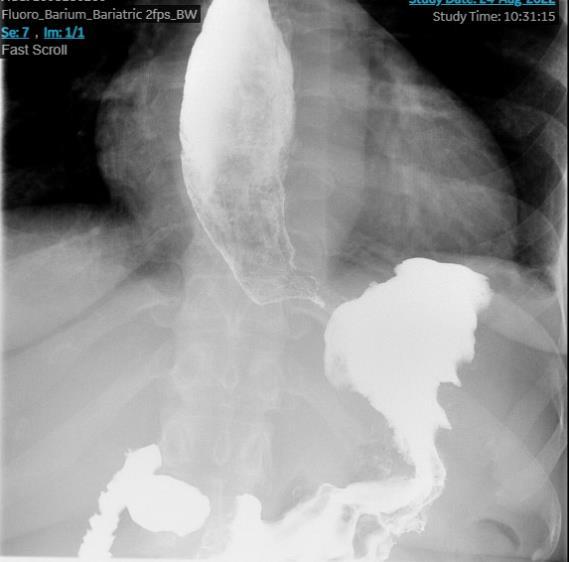 Figure 1: Upper endoscopy revealing a large, fungating mass in the lower third of the esophagus (A), gastric cardia (B), gastric body (C) and gastric fundus (D)
Figure 1: Upper endoscopy revealing a large, fungating mass in the lower third of the esophagus (A), gastric cardia (B), gastric body (C) and gastric fundus (D)
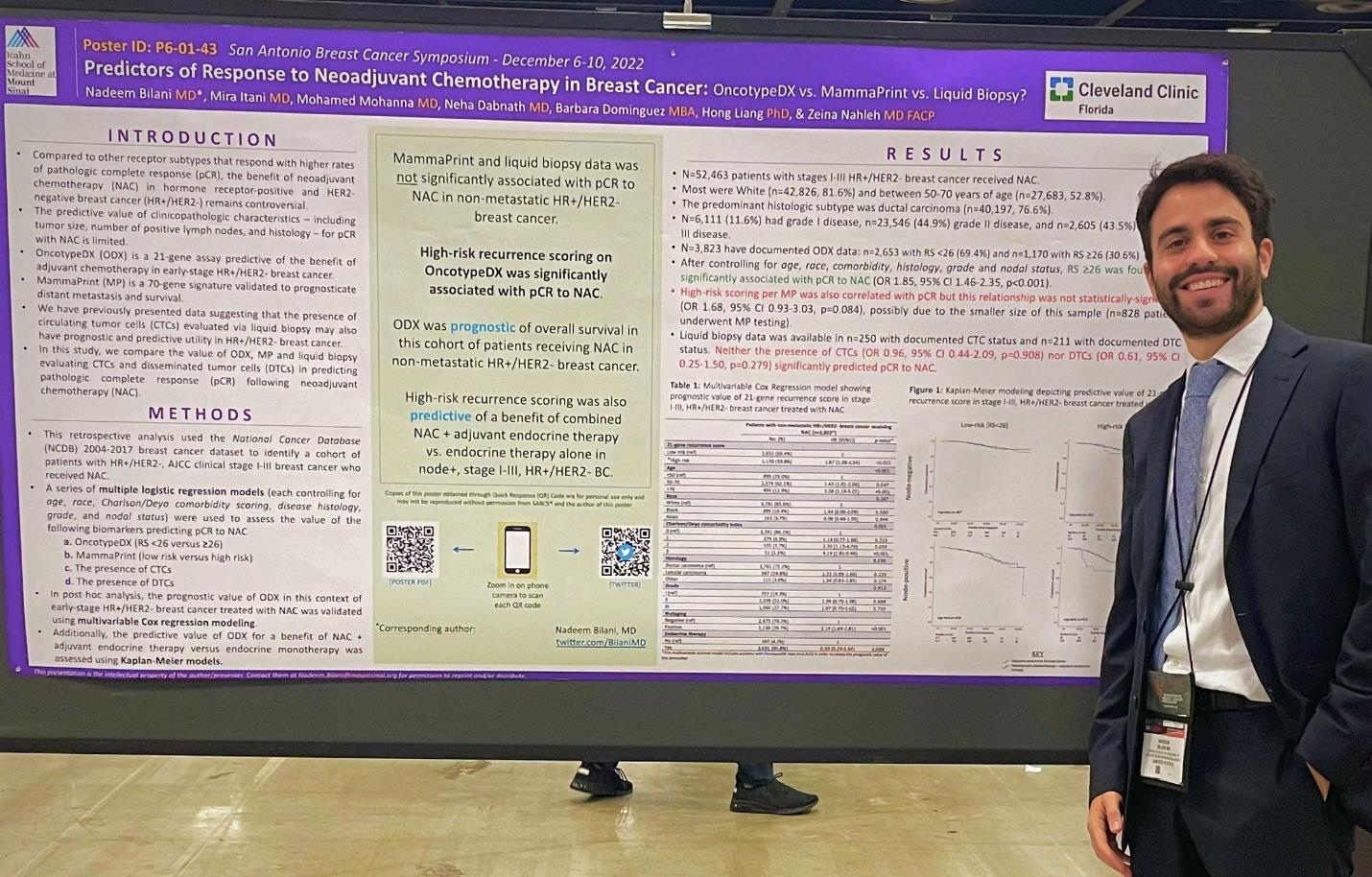
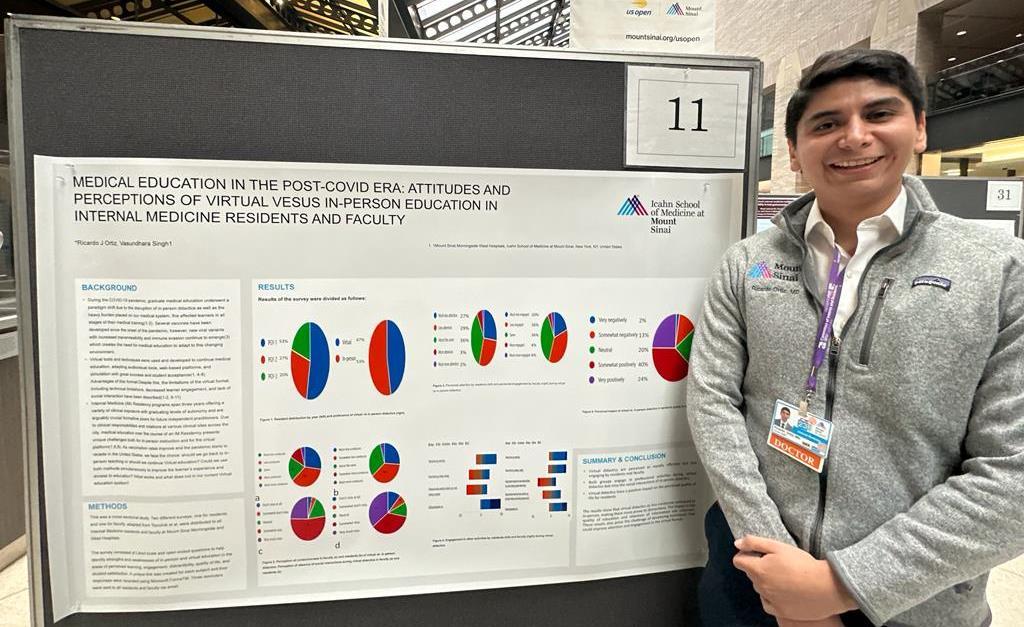
 Figure 1: Repeat MRI whole spine w/wo contrast demonstrating a linear enhancement in the dorsal aspect of the thecal sac from L2 to L4
Figure 1: Repeat MRI whole spine w/wo contrast demonstrating a linear enhancement in the dorsal aspect of the thecal sac from L2 to L4