
Annual Icahn School of Medicine
Mount Sinai Morningside/West Internal Medicine Residency Research Week


Annual Icahn School of Medicine
Mount Sinai Morningside/West Internal Medicine Residency Research Week
May 14-15, 2024

Introduction
Selection Committee and Oral Presentations
List of Abstracts with Posters
Abstracts with Posters
List of Abstracts 2023-2024
Abstracts 2023-2024
List of Publications 2023-2024
Index of Posters
Mount Sinai Morningside/West Internal Medicine Residency
Annual Virtual Research Week
May 14-15, 2024
 Osorio, MD, MPH
Osorio, MD, MPH
 John A. Andrilli, MD, FACP
John A. Andrilli, MD, FACP
Program
DirectorInternal Medicine Residency
Mount Sinai Morningside/West
Mount Sinai Morningside/West Internal Medicine Residency Research Week
Georgina Osorio, MD, MPH, Chair
Selection Committee 2023-2024
Selection committee members did not participate in the discussion or voting for abstracts in which they were involved or with which they had any additional conflict of interest.
Presenters were selected using a double-blind review process.


John Andrilli, MD
Ruchika Batwara, MD
Laura Bock, MD
Abel Casso Dominguez, MD
Natalie Cedeno, MD
Ashish Correa, MD
Deborah Edelman, MD
Joseph Elias, MD
Lindsey Fox, MD
Jennifer Fung, MD
Tamara Goldberg, MD
Katherine Hawkins, MD
Ariela Hazan, MD
Krystle Hernandez, MD
Mariam Khandaker, MD
Zoe Lawrence, MD
Yuying Luo, MD
Rohit Nathani, MD
Alejandro Prigollini, MD
Adam Rothman, MD
Ashwin Sawant, MD
Matthew Seplowe, DO
Claire Schretlen, MD
Shabari Shenoy, MD
Avinash Singh, MD
Vasundhara Singh, MD
Christine Stavropoulos, MD
Melissa Wiener, MD
Kevin Yan, MD
Abstracts selected to be oral presentations on Wednesday, May 15, 2024 at 8AM.







BASIC SCIENCE
Jonas Maximillian Marx, PGY3
ABSTRACT #52: ALTERATION OF LEFT VENTRICULAR LOAD IMPACTS EXOSOMAL AND MYOCARDIAL MICRORNA EXPRESSION IN A PORCINE MODEL OF MYOCARDIAL ISCHEMIA
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
Connor Smith, PGY2
ABSTRACT #68:MEDIASTINAL ANGIOLIPOMAS: AN EXCEEDINGLY RARE PATHOLOGY
CLINICAL RESEARCH
Raphael De Oliveira Bertasi, PGY3
ABSTRACT #13: THE ASSOCIATION OF SOCIODEMOGRAPHIC FACTORS AND TYPE OF CANCER WITH END-OF-LIFE PALLIATIVE CARE UTILIZATION IN PATIENTS WITH METASTATIC CANCER
CLINICAL RESEARCH
Jin Feng, PGY3
ABSTRACT #30: TEMPORAL ASSOCIATION BETWEEN BREAST CANCER AND SYSTEMIC SCLEROSIS: A CROSS-SECTIONAL ANALYSIS IN AN URBAN INSTITUTION
MEDICAL EDUCATION
Raul Benavides Leon, PGY2
ABSTRACT #12: ENGAGING PHYSICIAN TRAINEES THROUGH BEDSIDE INTENSIVE CARE UNIT NARRATIVES: A MIXED METHODS STUDY
QUALITY IMPROVEMENT
Adrian Chernyk, PGY3 &
Sharel Sadud Armaza, PGY3
ABSTRACT #18: STOP THE LABS: A JOURNEY TO REDUCE RECURRING LABS HROUGHOUT A HEALTHCARE SYSTEM

















Annual Icahn School of Medicine at Mount Sinai Morningside/West Internal Medicine Residency Research Week
Research Day Judges May 15, 2024
Laura Bock Bernard Camins Fernando Carnavali Abel Casso Dominguez Ashish Correa Maya Fakhoury Peter Goulden Forough Hakimzada Sara Huda Raymonde Jean Theresa Mack Brian Markoff Ashwin Sawant Avinash Singh David Steiger Kevin Yan Javier J. Zulueta





Annual Icahn School of Medicine at Mount Sinai Morningside/West Internal Medicine Residency Research Week Resident Planning Committee 2023-2024
Alexandria Markley Patricia Miguez Arosemena Swati Patel


1
2
DAPSONE-INDUCED METHEMOGLOBINEMIA IN CHRONIC LYME DISEASE
Ayele Agboglo1 and Haoxu Ouyang1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BLOOD PRESSURE CONTROL IN THE PRIMARY CARE SETTING
Shirin Ahmed1, Mushmoom Khan2, Ana Manzar3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Dover Family Physicians PA, Rodney Village, Delaware, United States; 3St. George’s School of Medicine, St. George’s University of London, London, United Kingdom
TROPICAL TRIPLE THREAT
3
4
Oladayo Ajisafe1 and Christine Stavropoulos1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
CARDIOGENIC EDEMA PRESENTED AS UNILATERAL BREAST SWELLING
Alexander Nagourney1* , Mohammed Isam Alsaud1* , Laura Bock1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
*These authors contributed equally to this work.
AN OVERLOOKED MIMIC? AUTOIMMUNE MYELOFIBROSIS
Yosef Joseph Rene Amel Riazat-Kesh1, Alexander Maraveyas1, Lily Martin2 , Douglas Tremblay3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
5
6
2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the European Hematology Association (EHA) 2023 Congress Annual Meeting that was held in Frankfurt, Germany from June 8-11, 2023 and published in European Journal of Hematology, 2023. PMID: 37515415
MTORC2-NDRG1-CDC42 AXIS COUPLES FASTING TO MITOCHONDRIAL FISSION
Nuria Martinez-Lopez1,2, Pamela Mattar1,2, Miriam Toledo2,3, Henrietta Bais2, Manu Kalyani2 , Marie Louise Aoun4, Mridul Sharma1,2, Laura Beth J. McIntire5 , Leslie Gunther-Cummins2 , Frank P. Macaluso2, Jennifer T. Aguilan2, Simone Sidoli2, Mathieu Bourdenx6,7 , Rajat Singh1,2
1University of California Los Angeles, Los Angeles, CA, United States; 2Albert Einstein College of Medicine, Bronx, NY, United States; 3Institut d’Investigacions Biomediques August Pi i Sunyer (IDIBAPS), Barcelona, Spain; 4Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 5Weill Cornell School of Medicine, New York, NY, United States; 6United Kingdom Dementia Research Institute, London, United Kingdom; 7UCL Queen Square Institute of Neurology, London, United Kingdom
Published in Nature Cell Biology, 2023. PMID: 37386153
JUNGLE JUICE INDUCED MYOCARDIAL INJURY
Matthew Baer1, James Choi1, Vahid Namdarizandi1, Sandra Maria Soler3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
7
2James J. Peters Department of Veterans Affairs, United States Department of Veteran Affairs, Bronx, NY, United States
Presented at both the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024 and the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
THE RESIDENT EDUCATOR
Galit Balayla Rosemberg1, Julia Ferreira de Carvalho1 , Foram Parikh1
8
9
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
ANALYSIS OF DATA FROM THE PALOMA-3 TRIAL CONFIRMS THE EFFICACY OF PALBOCICLIB AND OFFERS ALTERNATIVES FOR NOVEL ASSESSMENT OF CLINICAL TRIALS
Celine Yeh1, Mengxi Zhou1 , Neil Bapodra2, Dawn Hershman1, Edward Espinal3, Marina Moran3, Maria Rivero3, Antonio Tito Fojo1,4, Susan E. Bates1,4
1Columbia University College of Physicians and Surgeons, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Pfizer España, Madrid, Spain;
4James J. Peters Veteran Affairs Medical Center, Bronx, NY, United States
Published in Breast Cancer Research and Treatment, 2024. PMID: 37955764
EARLY RECOGNITION OF MDA5 DERMATOMYOSITIS
10
Murilo Bastos1, Kristine Lou Gargaritano1, Michael Kaplan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York American College of Physicians Annual Scientific Meeting that was held in Tarrytown, New York, United States on November 5, 2022. 11
ELSBERG SYNDROME IN HSV-2 INFECTION
Omar Belfaqeeh1, Alexandria Markley1, Mudita Patel1,2, Brian Markoff1, Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in IDCases, 2023. PMID: 36875152 12
ENGAGING PHYSICIAN TRAINEES THROUGH BEDSIDE INTENSIVE CARE UNIT
NARRATIVES: A MULTISITE EXPANSION STUDY
Raul Benavides1,Maria Athena Riego1,2,Edith Robin1,2,Valeria Santibanez3,Hailey Gupta2 , Kathryn Bass1, Usha Govindarajulu4, Samantha Ortiz1, Gabriela Bernal4, Alexander Davidovich1, Edwardine Mirna Mohanraj1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Emory School of Medicine, Atlanta, GA, United States
Presented both at the Accreditation Council for Graduate Medical Education (ACGME) Annual Educational Conference that was held in Orlando, Florida, United States from March 7-9,2024 and the Institute for MedicalEducation (IME),Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16. 2024.
13
THE ASSOCIATION OF SOCIODEMOGRAPHIC FACTORS AND TYPE OF CANCER WITH END-OF-LIFE PALLIATIVE CARE UTILIZATION IN PATIENTS WITH METASTATIC CANCER
Raphael Bertasi1, Tais Bertasi1, Nadeem Bilani1, Alaina Kessler2, Nicholas Rohs2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
14
THE IMPACT OF CARDIOVASCULAR COMORBIDITIES ON MORTALITY IN PATIENTS RECEIVING INPATIENT CHEMOTHERAPY
Tais Bertasi1, Raphael Bertasi1, Nadeem Bilani1, Alaina Kessler2, Nicholas Rohs2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States 15
EVALUATION OF A DATA ANALYSIS VIDEO CURRICULUM CREATED FOR RESIDENTS AND FELLOWS
Nadeem Bilani1 , Mantej Sehmbhi1,2, Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16. 2024.
THE PERFECT STORM: TORSADES DE POINTES IN PATIENT WITH LIVER CIRRHOSIS PRESENTING WITH VARICEAL BLEEDING
16
17
Salvador Caceros Diaz1*, Jonas Marx1*, Juan Arango Morales1*, Gopal Narayanswami1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
*These authors contributed equally to this work
SINGLE LEAFLET DEVICE ATTACHMENT AFTER MITRACLIP IMPLANTATION
Kristen Carter1, Souyma Gupta1, Kirtipal Bhatia1, Marija Petrovic1, Stamatios Lerakis1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, New York, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
STOP THE LABS: A JOURNEY TO REDUCE RECURRING LABS THROUGHOUT A HEALTHCARE SYSTEM
18
19
Adrian Chernyk1* , Sharel Sadud1*, Krystle Hernandez1, Shantheri Shenoy1, Foram Parikh1, Vasundhara Singh1, Nikta Athari1, Philip Chen1, Julie Pearson1, Benjamin Dempsey1 , Faye Reiff-Pasarew1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of Hospital Medicine (SHM) Annual Meeting that was held in San Diego, California, United States from April 12-15, 2024 and will be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024
*These authors contributed equally to this work.
IN-HOSPITAL OUTCOMES AND USE OF MECHANICAL CIRCULATORY SUPPORT IN PATIENTS WITHOUT STANDARD MODIFIDABLE RISK FACTORS AND CARDIOGENIC SHOCK
James Choi1, Sara Diaz1, Christopher N. Matthews1, Francisco José Romeo2 , Ashish Correa1, Arieh Fox1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2University of Miami Miller School of Medicine/Jackson Memorial Hospital, Miami, FL, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
MICROSATELLITE INSTABILITY HIGH: A DEFINITIVE PREDICTIVE BIOMARKER FOR IMMUNE CHECKPOINT INHIBITORS YET UNDERSTUDIED IN UNDERREPRESENTED MINORITIES WITH GASTROINTESTINAL CANCERS
20
21
Nobel Chowdhury1 , Fiyinfolu Balogun2 , Mirella Altoe2, Catherine O'Connor2 , Francisco Sanchez-Vega2, Debyani Chakravarty2, Wungki Park2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Memorial Sloan Kettering Cancer Center, New York, NY, United States
Presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that was held in Chicago, Illinois, United States from June 2-6, 2023.
THROMBOEMBOLIC RISK OF CARFILZOMIB OR BORTEZOMIB IN COMBINATION WITH LENALIDOMIDE/DEXAMETHASONE FOR NEWLY-DIAGNOSED MULTIPLE MYELOMA: A COMPARATIVE META-ANALYSIS INVOLVING 2,304 PATIENTS
Bruno Almeida Costa1, Thomaz Alexandre Costa2, Sara Diaz Saravia1, Nicole Felix3 , Carlyn Rose Tan4, Neha Korde4, Joshua Richter5
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Federal University of Ceará, Fortaleza, Brazil; 3Federal University of Campina Grande, Campina Grande, Brazil; 4Memorial Sloan Kettering Cancer Center, New York, NY, United States; 5Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in American Journal of Hematology, 2024. PMID: 38488702
HNF1A-ASSOCIATED MONOGENIC DIABETES TREATED SUCCESSFULLY WITH REPAGLINIDE MONOTHERAPY
22
23
Katherine Cuan1 and Ilana R. Bass1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in the American Association of Clinical Endocrinology (AACE) Clinical Case Reports, 2023. https://doi.org/10.1016/j.aace.2023.12.003
A CASE OF SUSPECTED VIRAL ENCEPHALITIS WITH NEGATIVE CEREBROSPINAL FLUID POLYMERASE CHAIN REACTION STUDIES
Tyler Czaniecki1 and Lance Maresky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS, A RARE COMPLICATION OF BABESIOSIS
24
25
Mrittika Deb1, Rebecca Pietro2, Olga Marushchak1, Chrisanna Dobrowlski1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
SYSTEMATIC REVIEW AND META-ANALYSIS OF PLASMA AND URINE BIOMARKERS FOR CHRONIC KIDNEY DISEASE OUTCOMES
Caroline Liu1 , Neha Debnath2, Gohar Mosoyan2, Kinsuk Chauhan2, George Vasquez-Rios2 , Celine Soudant4, Steve Menez5, Chirag R. Parikh5, Steven G. Coca3
1Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, New York, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, New York, United States; 4Memorial Sloan Kettering Cancer Center, New York, New York, United States; 5Johns Hopkins University of Medicine, Baltimore, Maryland, United States
Published in the Journal of the American Society of Nephrology, 2022. PMID: 35858701
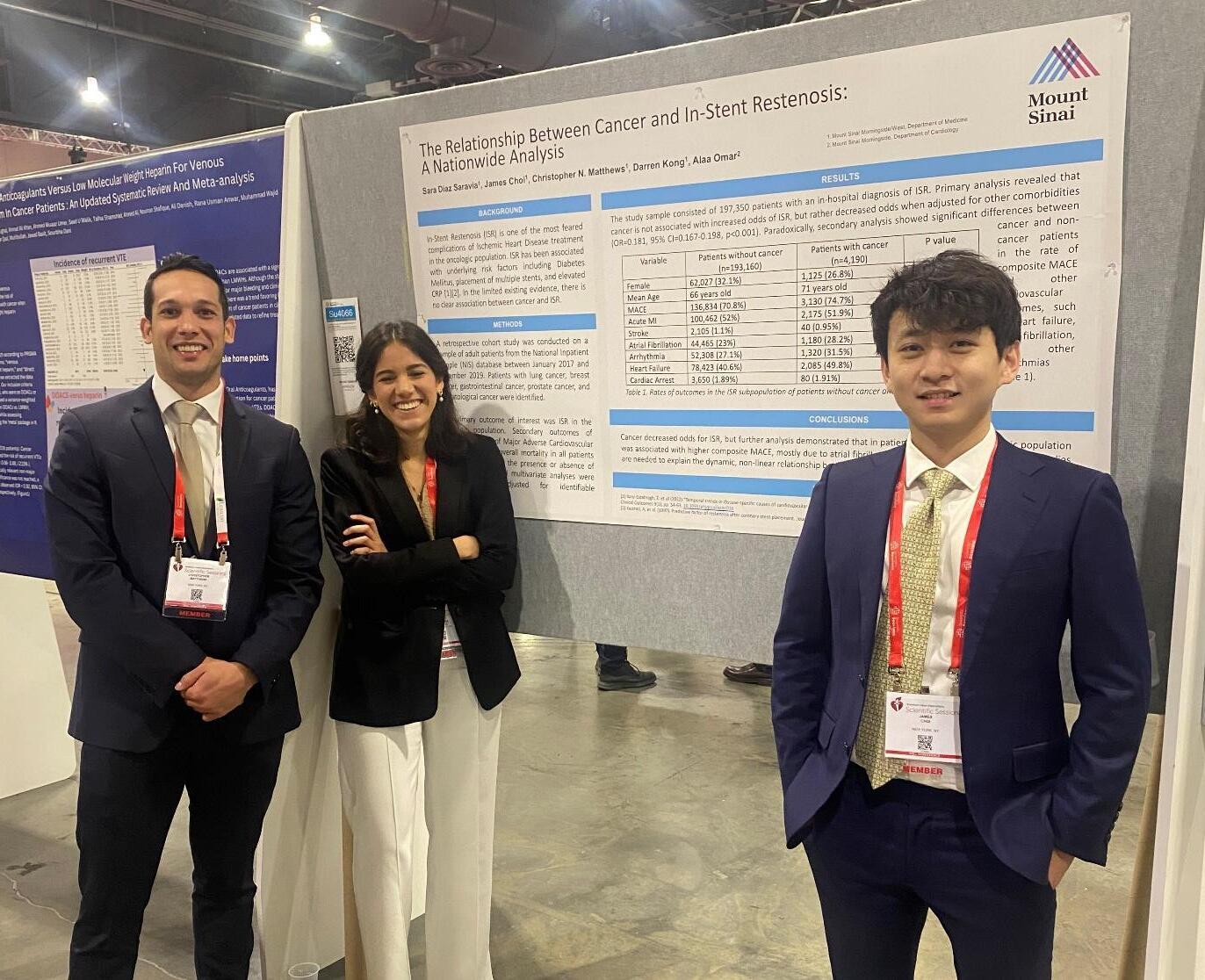
CANCER AS A NEW RISK FACTOR FOR MAJOR ADVERSE CARDIOVASCULAR EVENTS IN SECONDARY PREVENTION
26
27
Renzo Melchiori1 , Sara Diaz Saravia2, Lucas Szlaien1, Pablo Rubio1, Sergio Baratta1 , Alejandro Hita1, Romina Mouriño1, Manglio M. Rizzo1
1Hospital Universitario Austral, Buenos Aries, Argentina; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
SUPRAVENTRICULAR ARRHYTHMIA IN CARDIAC SARCOIDOSIS
Carlos G. Diola1 , Samuel Johnson1 , Loba Alam1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
IS TIMING EVERYTHING? ASSESSING DEMOGRAPHIC AND CLINICAL FACTORS IN TIMING OF PERCUTANEOUS TRACHEOSTOMY IN MEDICAL INTESIVE CARE UNIT PATIENTS
28
Keshav Dixit1, Yoshiko Ishisaka2, Shasha Chen2, Lina Miyakawa2, Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024. 29
30
SUCCESSFUL TREATMENT OF EOSINOPHILIC GRANULOMATOSIS WITH POLYANGIITIS WITH BENRALIZUMAB
Andrew Eng1 and Eugene Choo2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
TEMPORAL ASSOCIATION BETWEEN BREAST CANCER AND SYSTEMIC SCLEROSIS
Jin Feng1, Celestine He2, Hannah Verma2, Roshan Vasoya2, Daniel Qian2 , Ezequiel Olumuyide2, Alicia Leong2, Joseph Menand1, Murilo Roberto Bastos Silva1, Vincent Courant3, Sophia Lutgen1 , Chrisanna Dobrowolski3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the European Alliance of Association for Rheumatology (EULAR) Annual Meeting to be held in Vienna, Austria from June 12-15, 2024.
MORE THAN SKIN DEEP – SKIN MANIFESTATION OF ALK NEGATIVE LARGE CELL LYMPHOMA IN A POST-TRANSPLANT PATIENT
31
Debbie Marie Fermin1, Forough Hakimzada1, Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
OPTIC NERVE CHLOROMA IN ACUTE MYELOID LEUKEMIA
32
Thomas F. Fusillo1, Scott Millman2, Eytan M. Stein2,Varun Narendra2, Kamal Menghrajani3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Memorial Sloan Kettering Cancer Center, New York, NY, United States; 3White House Office of Science and Technology Policy, Washington, D.C., United States
PERCUTANEOUS CORONARY INTERVENTION VERSUS OPTIMAL MEDICAL THERAPY FOR CHRONIC TOTAL OCCLUSION
33
34
Kruti Gandhi1, Errol Moras1, Ameesh Isath2, Ashish Correa1, Kiran Mahmood1, Abel Casso Dominguez1, Jacqueline Tamis-Holland3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Medical College, New York, NY, United States; 3Cleveland Clinic, Cleveland, OH, United States
Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
ASSESSING THE UTILIZATION OF PALLIATIVE CARE SERVICES IN THE MANAGEMENT OF PATIENTSWITH METASTATIC PANCREATIC ADENOCARCINOMA
Sonal Gandhi1, Drew Moss1, Richard Sheppard2, Ibrahim Omore2, Linda Wu3, Deirdre Cohen2, Cardinale B. Smith2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Columbia University Irving Medical Center, New York, New York, United States
Presented at the American Society of Clinical Oncology (ASCO) Quality Care Symposium that was held in Boston, Massachusetts, United States from October 27-28, 2023.
35
37
“IT’S IN THE DIET’ - A CASE OF HEMATOCHEZIA SECONDARY TO SCURVY IN A SCHIZOPHRENIC PATIENT
Martin Emmanuel Garcia1, Debbie Marie Fermin1, Sanaa Zafar1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
RAPID PROGRESSION OF ACUTE HEART FAILURE RELATED TO TAKOTSUBO CARDIOMYOPATHY IN A YOUNG ANOREXIC FEMALE PATIENT
Justin Goodfarb1, Mohammad Ishrak Khan1, Samantha Shetty1, Jaskirat K. Gill1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
STATUS ASTHMATICUS COMPLICATED BY RHABDOMYOLYSIS
Satwant Grewal1, Tal Shachi1,2, Pavan Paka3, Sara Luby1, Arpanjeet Kaur1, Patrick TobinSchnittger1, Vincent Courant1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
3Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Nashville, Tennessee, United States from October 16-19, 2022.
38
39
NATIONWIDE ANALYSIS OF THE RISK OF MYOCARDIAL INFARCTION IN PATIENTS WITH ATRIAL FIBRILLATION: A RETROSPECTIVE OBSERVATIONAL STUDY
Soumya Gupta1, James Choi1, Kristen Carter1, Sara Diaz Saravia1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
CARDIAC SARCOIDOSIS WITH PREDOMINANT RIGHT VENTRICLE INVOLVEMENT
Hannah Hart1, Devika Aggarwal1, Soumya Gupta1, Vikram Agarwal1, Isha Ranadive1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at both the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024 and the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
INCREASING COLORECTAL CANCER SCREENING RATES AMONG PATIENTS AT A FEDERALLY QUALIFIED HEALTH CENTER
40
41
Marni Wilkoff1 , Allison E. Wang1 , Alexandria Markley1 , Swati Patel1 , Rama Hussein1 , Nicholas Piniella2 , Kevin Yan3 , Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Institute of Technology College of Osteopathic Medicine, Old Westbury, New York, NY, United States;
3Ryan Chelsea-Clinton Health Center, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
ECHOCARDIOGRAPHIC HEMODYNAMIC ASSESSMENT IN PATIENTS UNDERGOING AORTIC BALLOON VALVULOPLASTY
Joseph E. Karpenos1, Marija Petrovic1, Juan Arango Morales1, Joseph Elias1, Hannah Hart1 ,Samantha Shetty1,Soumya Gupta1,James Choi1,Sara Diaz Saravia1,Kristen Carter1 , Nnedindu Asogwa2, Eyadeh Mdanat3, Ga Hee Kim1, Robert Leber1, Alaa M. Omar1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Staten Island University Hospital, Staten Island, NY, United States; 3Cayuga Medical Center, Ithaca, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
IN-STENT THROMBOSIS THRICE IN 30 DAYS
42
43
Luka Katic1, Hammad Sheikh1, Alexander Silverman1 , Ankita Gore1, Nitin Barman1 , Amir Ahmadi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Fuster Heart Research Forum that was held in New York, New York, United States on March 15, 2024.
DESIGN AND IMPLEMENTATION OF BLENDED TELEMETRY CURRICULUM FOR INTERNAL MEDICINE RESIDENTS
Arpanjeet Kaur1, Joseph Elias1, Forough Hakimzada1, Kiran Mahmood1, Edgar Argulian1 , Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
IRINOTECAN-INDUCED DIFFUSE ALVEOLAR HEMORRHAGE IN A PATIENT WITH METASTATIC OVARIAN CANCER
44
Madison Kennedy1 , Abha Kulkarni2, Elina Tsyvkin3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Weill Cornell Medical Center, New York, NY, United States; 3Memorial Sloan Kettering Cancer Center, New York, NY, United States
IMPACT OF BIVALIRUDIN VERSUS HEPARIN ON MAJOR BLEEDING DURING PERCUTANEOUS CORONARY INTERVENTIONS: AN UPDATED META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS
45
Mohammad Ishrak Khan1, Errol Moras1, Raisa Subaita Zahir 2, Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Wayne State University School of Medicine, Detroit, MI, United States
Presented at the Society for Cardiovascular Angiography and Interventions Annual Meeting that was held in Long Beach, California, United States from May 2-4, 2024.
PROGNOSTIC SIGNIFICANCE OF RAAS INHIBITION IN HEART FAILURE PATIENTS WITH CO-EXISTING END STAGE RENAL DISEASE ON HEMODIALYSIS
46
47
Won Joon Koh1,Alaa M. Omar1,Anna Sophie Mueller1, Christopher N. Matthews1, Joseph Marinelli1, Justin Goodfarb1, Mohammad I. Khan1, Muhammad Ghallab1, Ashish Correa1 , Kiran Mahmood1,Arieh Fox1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Heart Failure Society of America (HFSA) Annual Scientific Meeting that was held in Cleveland, Ohio, United States from October 6-9, 2023.
TEMPORAL TRENDS AND CARDIOVASCULAR OUTCOMES IN HOSPITALIZED PATIENTS WITH FABRY DISEASE
Darren Kong1, James Choi1, Sara Diaz Saravia1, Benjamin Adegbite1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
48
49
OVER-THE-COUNTER OVERUSE: A CASE STUDY OF OVERDOSE ON MEDICATION BOUGHT ON AMAZON
Scott Low1 , Joseph Karpenos1, Matthew Baer1 , Rama Hussein1, Kyunghyun Lee1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
IMPACT OF PEER-TO-PEER TEACHING ON SEPSIS PATHWAY UTILIZATION AND OUTCOMES
Sara Luby1, Galit Balayla Rosemberg1 , Hammad Sheikh1 , Venus Sharma1 , Connor Smith1 , Rachael Schneider1 , Andrea Wood1 , Alvin Yang1 , Christiana Choi1 , Yoni Balboul2 , James Salonia1 , Raymonde Jean1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
YOU SHALL NOT PASS: RARE DUODENAL BULB ADENOCARCINOMA CAUSING GASTRIC OUTLET OBSTRUCTION
50
Randy Leibowitz1 , Alexander Maraveyas1, Frederick Rozenshteyn1, Tina Park1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 21-26, 2022.
LYMPHOMATOID PAPULOSIS AND METHOTREXATE-RELATED LYMPHOPROLIFERATIVE DISORDER IN A RHEUMATOID ARTHRITIS PATIENT TREATED WITH IMMUNOSUPPRESSIVE THERAPIES
51
52
Olga Marushchak1 , Patrick Brunner2 , Randie Kim2 , Chrisanna Dobrowolski1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Congress of Clinical Rheumatology Annual Meeting that was held in Destin, Florida, United States from May 9-12, 2024.
ALTERATION OF LEFT VENTRICULAR LOAD IMPACTS EXOSOMAL AND MYOCARDIAL MICRORNA EXPRESSION IN A PORCINE MODEL OF MYOCARDIAL ISCHEMIA
Jonas M. Marx1 , Renata Mazurek2, Olympia Bikou2, Tomoki Sakata2, Spyros A. Mavropoulos2, Kiyotake Ishikawa2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association Basic Cardiovascular Sciences (AHA BCVS) Scientific Sessions Annual Meeting that was held in Boston, Massachusetts, United States from July 31-August 3, 2023.
IN-HOSPITAL INFECTIVE ENDOCARDITIS FOLLOWING TRANSCATHETER MITRAL VALVE PROCEDURES
53
54
Christopher N. Matthews1, James Choi1, Sara Diaz Saravia1, Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Society of Cardiovascular Angiography and Interventions Scientific Sessions held in Long Beach, California from May 2-4, 2024.
DIGITAL RECTAL EXAMS ARE INFREQUENTLY PERFORMED PRIOR TO ANORECTAL MANOMETRY DESPITE HIGH SENSITIVITY FOR DYSSYNERGIA
Joseph A. Menand1, Robinderpal Sandhu1, Yonatan Israel2, Emma Reford2, Ahmun Zafar1 , Priyanka Singh1,3, Kimberly Cavaliere1,3, Jean Saleh1,3, Michael S. Smith1,3, Daniela Jodorkovsky1,3, Yuying Luo1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Center for GI Physiology and Motility, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week (DDW) Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023 and published in Digestive Diseases and Sciences, 2024. PMID: 38170338
SCHISTOSOMIASIS REACTIVE POLYARTHRITIS MASQUERADING AS SERONEGATIVE ARTHRITIS OF INFLAMMATORY BOWEL DISEASE
55
Jiaxi Miao1* , Aesha Patel1*, Elmarie Alexander1,2, Rahul Gaikwad1, George McKinley1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
*These authors contributed equally to this work.
ANAL CANCER SCREENING, ARE WE DOING ENOUGH IN FEDERALLY QUALIFIED HEALTH CENTERS?
56
57
Patricia Miguez Arosemena1 , Emily S. Seltzer1, Cristina Olivo Freites2, Sophia Nurani3 , Christian Olivo Freites3; John Anthony Andrilli1, Frank Nelson1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2University of Texas Health Science Center at Houston, Houston, TX, United States; 3Ryan Health, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
TRENDS AND OUTCOMES OF INTRAVASCULAR IMAGING IN PATIENTS UNDERGOING PERCUTANEOUS CORONARY INTERVENTION FOR CORONARY CHRONIC TOTAL OCCLUSION
Errol Moras1, Kruti Gandhi1, Abel Casso Dominguez1, Nitin Barman2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
AN ISOLATED CASE OF NOSOCOMIAL ACQUISITION OF INVASIVE NONTYPHOIDAL SALMONELLA
58
Jonathan M. Oxman1, Laura Rivera Boadla1,2 , Nicholas Sells1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Published in IDCases, 2023. PMID: 37645540
59 WHEN THEHEART'SCUREBECOMESTHESTOMACH'SCHALLENGE: A RARECASE OF POST-ABLATION GASTROPARESIS
Swati Patel1, Adam Tillowitz1, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
ADVOCATING COMMUNITY FOR HEALTHCARE ACCESS AND NETWORK FOR GROWTH AND EQUITY FOR THE MOST VULNERABLE BY OPPOSING THE 340B DRUG PRICING PROGRAM CARVE OUT
60
Bailey Perry1 , Debbie Fermin1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York American College of Physicians Annual Scientific Meeting that was held in Tarrytown, New York, United States on October 28, 2023
GASTROINTESTINAL BLEEDING SECONDARY TO IODODERMA
Sidra Salman1, Marni Wilkoff1, Kruti Gandhi1, James Salonia1
61
62
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
SHOULD GLUCAGON-LIKE PEPTIDE RECEPTOR AGONISTS BE HELD PRIOR TO AMBULATORY REFLUX TESTING?
Robinderpal Sandhu1, Alexandria Markley1, Emily S. Seltzer1, Joseph Abraham1 , Rama Hussein1, Binoy Desai1, James Choi1, Kimberly Cavaliere1,2, Yuying Luo1,2 , Michael S. Smith1,2, Daniela Jodorkovsky1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Center for GI Physiology and Motility, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
IMPROVING INPATIENT GASTROENTEROLOGY PERCUTANEOUS ENDOSCOPIC GASTROSTOMY TUBE REFERRALS AND OUTCOMES
63
64
Emily S. Seltzer 1, Erica Park 1, 2, Patricia Miguez Arosemena 1, Ines Varela Knorr1 , Anudeep Neelam1,2, Michael S. Smith2, Priya Simoes1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York Society for Gastroenterology and Endoscopy Annual Meeting that was held in New York, New York, United States from December 14-15, 2023.
NEWLY DIAGNOSED HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS IN AN ADULT PATIENT WITH MULTI-ORGAN FAILURE
Priya Shah1* , Christine Lenchur1* , Rayling Herrera1*, Ira Khanna1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
*These authors contributed equally to this work.
A CASE OF CRYPTOGENIC ORGANIZING PNEUMONIA - ULCERATIVE COLITIS OR INFLIXIMAB?
Venus Sharma1, Howard Freeman1,2, Mary O’Sullivan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
66 AN ATYPICAL PRESENTATION OF ARRHYTHMOGENIC RIGHT VENTRICULAR CARDIOMYOPATHY WITH CONCOMITANT STROKES
Samantha V.Shetty1,Chad Henry1,Justin Goodfarb1,Michael Bourne1,Basera Sabharwal1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
67
68
FRAILTY PREDICTS ADVERSE OUTCOMES IN OLDER PATIENTS WITH PULMONARY EMBOLISM
Jorge Sinclair De Frias1, Pablo Moreno Franco2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mayo Clinic, Jacksonville, Florida, United States
MEDIASTINAL ANGIOLIPOMAS: AN EXCEEDINGLY RARE PATHOLOGY
Connor Smith1 , Steven Lim1,2 , Daniel Nicastri1, Mary Beasley1, Daniel Chung1 , Boram Kim1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
RARE CASE OF ACUTE HYPOXIC RESPIRATORY FAILURE DUE TO TRAUMATIC TAPIA SYNDROME REQUIRING TRACHEOSTOMY
69
Vincent Torelli1 , Raymonde E. Jean1, Elena Tran2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Presbyterian Brooklyn Methodist Hospital, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
THE CASE OF THE PSEUDO-PSEUDO POLYP: FIRST REPORTED CASE OF A SPINDLE CELL SARCOMA AT AN ILEOCOLONIC ANASTOMOSIS
Ines Varela Knorr1, Jennifer Claytor2, James Marion2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
INTERHOSPITAL TRANSFER FOR ACUTE PULMONARY EMBOLISM: INVESTIGATION OF PROCESS METRICS, AND IMPACT OF TRANSFER TIMES IN DECISION MAKING AND OUTCOMES
71
72
Avinash Singh1 , Priyanka Sridhar2 , Hong Yu Wang2 , Agostina Velo1 , Destiny Nguyen2 , Madeline Ehrlich2, Abdul Rehman3, Robert Lookstein4, Samuel Acquah4, David Steiger1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Rutgers New Jersey Medical School, Newark, NJ, United States; 4Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
MARKERS OF COMMON VARIABLE IMMUNODEFICIENCY RELATED INTERSTITIAL LUNG DISEASE ACTIVITY
Brit Trogen1, Julia Jacob1, Code Demarco1, Adam Jacobi1 , Megha Verma2 , Hsi-En Ho1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
EVALUATING THE ACCURACY AND ACCEPTANCE OF AN ARTIFICIAL INTELLIGENCE-GENERATED COLONOSCOPY BOWEL PREPARATION PROMPT
Marni Wilkoff1, Nicholas Piniella2, Rashmi Advani3
73
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Institute of Technology College of Osteopathic Medicine, Old Westbury, NY, United States; 3Mount Sinai South Nassau Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting that will be held in Washington, D.C., United States from May 19-21, 2024.
PATIENT-LEVEL FACTORS DO NOT IMPACT THERAPEUTIC ESCALATION IN CHRONIC CONSTIPATION
74
75
Ahmun Zafar1, Joseph A. Menand1, Robinderpal Sandhu1, Yonatan Israel2 , Emma Reford2 , Kimberly Cavaliere1, Priyanka Singh1, Jean Saleh1,3, Michael S. Smith1,3, Yuying Luo1,3 , Daniela Jodorkovsky1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Center for GI Physiology and Motility, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
EVALUATING THE ROLE OF DAY 14 BONE MARROW BIOPSY AND EUROPEAN LEUKEMIA NET RISK CLASSIFICATION IN PREDICTING OVERALL AND RELAPSEFREE SURVIVAL IN ACUTE MYELOID LEUKEMIA
Franc Metodi Balev1 , Victor Zibara2 , Grace Van Hyfte1, Jonathan Feld1, Marina Kremyanskaya1,Michelle Becker1,Alla Keyzner1,Alan H. Shih1,Bridget Marcellino1, Hannah Levavi1, Lewis Silverman1, John Mascarenhas1, Douglas Tremblay1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States

ABSTRACT #1
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY/INFECTIOUS DISEASES
Ayele Agboglo1 and Haoxu Ouyang1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Methemoglobinemia, characterized by elevated methemoglobin levels impairing oxygen transport, presents diagnostic and management challenges, particularly in cases induced by dapsone therapy. This abstract explores such challenges in a 25-year-old female undergoing extensive dapsone treatment of chronic Lyme disease with elevated methemoglobinemia levels. Dapsone is traditionally used to treat conditions such as leprosy, Pneumocystis jiroveci pneumonia, and recently chronic Lyme disease (CLD). CLD itself is a controversial condition used to describe illness in patients with Lyme disease or symptoms in people who have no clinical or diagnostic evidence of current or past infection with B. burgdorferi. The National Institute of Allergy and Infectious Disease recommends the term "Post Treatment Lyme Disease Syndrome" (PTLDS) to portray patients' clinical presentation accurately. This case report details the diagnostic and therapeutic dilemmas encountered in managing methemoglobinemia in patients with CLD/PTLDS receiving dapsone therapy.
CASE PRESENTATION: Our patient is a 25-year-old female with a past medical history of chronic Lyme disease, depression, and anxiety who presented to the emergency department with complaints of shortness of breath and palpitations. Her treatment regimen for chronic Lyme disease included pyrazinamide, clarithromycin, rifabutin, dapsone, methylene blue, and leucovorin for at least four weeks. Upon examination, mucosal cyanosis was evident, and initial pulse oximetry revealed hypoxemia with an oxygen saturation of 85% on room air. Venous blood gas demonstrated elevated methemoglobin (MetHb) levels exceeding 30%, indicating severe methemoglobinemia. In the emergency department, the patient received 1 mg/kg methylene blue, leading to mild improvement of her symptoms of shortness of breath and hypoxia, with her O2 saturation increasing to 93% on 6L nasal cannula. The patient was admitted for monitoring, and poison control was consulted. They recommended the addition of ascorbic acid as well, but the patient refused ascorbic acid treatment due to prior instances of exacerbating her migraines. Additionally, given her extensive treatment course with methylene blue and selective serotonin reuptake inhibitors (SSRIs) for depression outpatient, there were concerns about potentially inducing serotonin syndrome. She received 1mg/kg of methylene blue once daily for three days with mild improvement in MetHb levels but minimal symptomatic improvement. Poison control recommended twice daily dosing of methylene blue as the patient had been off SSRI for a few days and the addition of famotidine 40 mg twice daily on hospital day 4. Her MetHb decreased to <15%, and discharge recommendations included continuing famotidine for a week, with no further methemoglobin testing needed. The patient was stable for discharge with close primary care physician follow-up.
CONCLUSION: Dapsone induces methemoglobinemia through hepatic metabolization. Its metabolites, dapsone hydroxylamine (DDS-NHOH) and mono-acetyl dapsone hydroxylamine (MADDS-NHOH), oxidize the Fe2+ to Fe3+ of hemoglobin, forming methemoglobin, a dangerous side effect. Additionally, due to its enterohepatic metabolization, dapsone has a half-life of 30 hours, making prolonged treatment hazardous Our patient's presentation included mucosal cyanosis, hypoxemia, and elevated methemoglobin levels exceeding 30%, indicating severe methemoglobinemia. Traditional management of methemoglobinemia involves one dose of 1‐2 mg/kg over 5 minutes, with a second dose rarely being needed. Our patient only showed mild improvement in symptoms, requiring alternative treatment options and considerations. One of those concerns is drug-drug interactions, notably with SSRIs for her depression and the risk of serotonin syndrome, and patient refusal of ascorbic acid supplemental treatment. Using an H2 blocker such as famotidine to treat dapsone-induced methemoglobinemia is elucidated through its reduction of hepatic oxidation of dapsone to the hydroxylamine, thereby limiting methemoglobinemia formation. One study found that long-term concurrent administration of
cimetidine with dapsone appeared to increase plasma dapsone levels and reduce methemoglobin levels in patients with chronic skin conditions such as dermatitis herpetiform. Consultation with poison control guided treatment adjustments, such as the addition of famotidine as a competitive inhibitor of dapsone metabolism and a modified dosing regimen for methylene blue. The complexities surrounding chronic Lyme disease diagnosis and treatment add a layer of complexity, necessitating a nuanced approach to managing associated complications. The National Institute of Allergy and Infectious Diseases (NIAID) has funded several placebocontrolled clinical trials to assess the efficacy of prolonged antibiotic therapy for treating PTLDS, and one clinical trial, which included two multicenter studies, provided no evidence that extended antibiotic treatment is beneficial. In those studies, physicians examined long term antibiotic therapy in patients with a well-documented history of previous Lyme disease but who reported persistent pain, fatigue, impaired cognitive function, or unexplained numbness. However, results showed no benefit from prolonged antibiotic therapy compared to placebo in treating those symptoms. In another study, people receiving antibiotics did report a more significant improvement in fatigue than those on placebo. However, no benefit to cognitive function was observed. Overall, the study authors concluded that the evidence did not support additional antibiotic therapy for PTLDS. In conclusion, the management of methemoglobinemia induced by dapsone therapy presents a complex clinical scenario, as highlighted by the case of our 25-year-old female patient with chronic Lyme disease. The extensive use of dapsone in treating conditions like chronic Lyme disease, coupled with its prolonged half-life and formation of methemoglobin-inducing metabolites, underscores the need for vigilance in monitoring patients for this potentially life-threatening complication.
ABSTRACT #2
CLINICAL RESEARCH
CARDIOLOGY/GENERAL INTERNAL MEDICINE
Shirin Ahmed1, Mushmoom Khan2, Ana Manzar3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Dover Family Physicians PA, Rodney Village, Delaware, United States; 3St. George’s School of Medicine, St. George’s University of London, London, United Kingdom
BACKGROUND/INTRODUCTION: Hypertension remains a significant public health challenge, with primary care practitioners at the forefront of management efforts. Effective blood pressure control is crucial in mitigating the risk of cardiovascular complications. However, discrepancies in blood pressure readings between clinical settings and home measurements, known as “white-coat” hypertension, complicate management. This study aims to retrospectively analyze outpatient blood pressure management practices to identify potential areas for improvement, with a specific focus on the prevalence of “white-coat” hypertension, the effectiveness of lifestyle modifications versus pharmacological interventions, and the comparative efficacy of different antihypertensive drug classes.
METHODS: This interim report outlines the initial six weeks of a comprehensive retrospective analysis. The methodology involves collating and examining electronic medical records from a primary care network. Data extraction focuses on systolic blood pressure readings (both in-office and reported home measurements), prescribed antihypertensive medications, and documented lifestyle modification recommendations. Preliminary statistical analyses aim to identify patterns in systolic blood pressure management and variance. The study also includes a sub-analysis to evaluate the initial impact of lifestyle changes versus medication on systolic blood pressure control, with a further breakdown by antihypertensive drug class.
RESULTS: As of this interim update, data from approximately 200 patient records have been extracted and are currently under analysis. Initial observations suggest a notable percentage of patients exhibit higher systolic blood pressure readings in the clinical setting compared to home measurements, indicative of potential 'whitecoat' hypertension. Preliminary data also indicate a wide variance in systolic blood pressure control across different antihypertensive classes, though detailed statistical analysis is pending to ascertain significance. A comparison between lifestyle modifications and pharmacological interventions has begun, with early trends suggesting a synergistic effect when both are employed concurrently.
CONCLUSION: Though results are still preliminary, this study underscores the complexity of blood pressure management in primary care and highlights the potential prevalence of “white-coat” hypertension in outpatient settings. The forthcoming analysis will provide deeper insights into the relative efficacy of lifestyle changes versus medication and elucidate any significant differences in SBP reduction by antihypertensive drug class. These findings could inform more nuanced and effective hypertension management strategies in primary care, contributing to improved patient outcomes. A potential future avenue of focus may be discrepancies in hypertension management outcomes in patients from different ethnic backgrounds.
ABSTRACT #3
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY/INFECTIOUS DISEASES
TROPICAL TRIPLE THREAT
Oladayo Ajisafe1 and Christine Stavropoulos1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Rocky Mountain Spotted Fever is a tick-borne disease affecting travelers to endemic regions, manifesting with nonspecific signs and symptoms. This case reports a young healthy 25-yearold female with no past medical history or medication use, whom shortly after returning from vacation in a tourist destination begins to suffer from headache, neck pain/stiffness, fever and photosensitivity. She went to urgent care, then presented to the hospital where she was admitted for further workup. She was started on doxycycline and monitored on telemetry while awaiting microbiology results. The most concerning findings included bicytopenia, elevated ferritin, and hepatosplenomegaly with the Rocky Mountain Spotted Fever serology result positive during her stay. Post-discharge serologies were also found to be positive for dengue fever and borderline Leptospirosis. When diagnosing tick and virus-borne illnesses, it is important to keep a wide differential and consider the possibility of co-infections.
Dengue Fever Arthralgia, Confusion Fever
Headaches
Leukopenia
Lymphadenopathy
Leptospirosis
Abdominal Pain
Fevers
Headaches
Myalgias Nausea Rigors
Vomiting
Rocky Mountain
Spotted Fever Fever
Headache Myalgias Nausea Rash
Hepatomegaly
Mucosal Bleeding
Severe Myalgia
Thrombocytopenia
Transaminitis
ARDS
Liver dysfunction
Renal Failure
Aseptic meningitis
Positive tourniquet test
Retro-orbital pain
Tri-phasic;
1. Febrile
2. Critical
3. Convalescent
Found in animal urine, usually seen post floods or camping
Bi-phasic;
1. Leptospiremic
2. Immune delayed
Cerebral Edema
Hyponatremia
Petechial Rash
Thrombocytopenia
Transaminitis
Rash around wrist and ankles found in 90% of patients, usually 2-5 days post symptoms
Popular tourist destinations; Central & South America, Caribbean, Pacific Islands, Southeast Asia
Found worldwide, more common in temperate and tropical climates
Multiple Ticks worldwide. High distribution in Southwest US and Mexico
CASE PRESENTATION: We report on a 25-year-old woman who first presented to an urgent care, then to the hospital for 3 days of headache, neck pain/stiffness, fever, and photosensitivity. The patient had no past medical history, and took no medications, but had been vacationing in Mexico for 5 days returning 9 days prior to presentation where she swam in the beach and local cenote. In triage, her blood pressure was 92/45 mmHg, heart rate: 50 bpm, respiratory rate: 15 breaths/min, temperature: 97.6F, and SpO2: 96% on room air. Initial electrocardiogram showed junctional bradycardia, and chest x-ray, CT-head, and CT-cervical spine revealed no acute abnormalities. Her initial labs showed serum white blood cells: 2.5 K/uL and platelets: 131 K/u/L with normal BMP and slight AST elevation to 40 U/L. Workup was continued to rule out meningitis and her blood work
continued to decline reaching troughs and peaks of AST: 537 U/L, AL: 593 U/L, White blood cell: 1.9 g/dL, platelets: 45 K/uL, Ferritin: 9,995 ng/mL. An ultrasound of her abdomen showed an enlarged liver and spleen. She was immediately started on doxycycline 100mg and the Infectious Disease team was consulted who recommended sending workup for multiple virus and tick-related diseases. The patients bicytopenia, elevated ferritin, and hepatosplenomegaly prompted concerns for other underlying processes so leading Hematology to be consulted who attributed the cause to acute phase reactants. She also had findings suggestive of Hepatitis B infection. The Gastroenterology team was consulted who suspected a probable resolved Hepatitis B infection within the last 6 months. Doxycycline was held due to rising transaminitis. On the sixth day of hospital admission, Rocky Mountain Spotted Fever IgM resulted positive. With clinical and laboratory improvement, the patient was discharged. Three days post-discharge, the patient’s dengue fever IgM serology resulted positive.
CONCLUSION: Rocky Mountain Spotted Fever can be a fatal disease if left untreated, and early diagnosis and treatment is vital. Due to timing for serology to come back, maintaining a wide differential, not anchoring on a certain diagnosis or symptoms, and providing early broad supportive care is important in patients who you suspect of having travel-related illnesses.
ABSTRACT #4
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/GENERAL INTERNAL MEDICINE
CARDIOGENIC EDEMA PRESENTED AS UNILATERAL
Mohammed Isam Alsaud1*, Alexander Nagourney1*, Laura Bock1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
*These authors contributed equally to this work.
BACKGROUND/INTRODUCTION: Invasive breast cancer is one of the most commonly diagnosed cancers in the United States with an annual incidence of 297,000. Cardiogenic edema leading to unilateral breast swelling is exceedingly rare but has been described in a case report
CASE PRESENTATION: This case involves an 85-year-old female with a past medical history of cirrhosis due to hepatitis C infection, primary sclerosing cholangitis, anemia, chronic kidney disease, and chronic heart failure who presented with acute changes to her left breast. Over the last month she noticed a gradual enlargement of the breast, with progressive skin changes and mild tenderness to palpation. She denied any recent changes in medication. No personal or family history of breast cancer. Her last mammogram was in 2014. Physical exam revealed a left breast that was significantly larger than the right breast. She had skin dimpling and a general firmness to palpation. There was no palpable mass or lymphadenopathy. The exam also showed mild lower extremity edema. Labs showed normal electrolytes and albumin, her kidney and liver function were at her baseline. Given the rapid onset of swelling and appearance of the breast there was concern for breast cancer and the patient was sent for breast imaging. Breast ultrasound revealed left sided skin and parenchymal thickening consistent with cardiogenic edema. Patient was started on torsemide with rapid resolution of asymmetric swelling.
DISCUSSION/CONCLUSION: The unilateral breast edema in our patient mimicked inflammatory breast carcinoma. Due to the rapid progression and peau d’orange cutaneous changes, it was challenging to overlook the possibility of malignancy. After her ultrasound revealed signs of fluid overload and the torsemide resulted in resolution of symptoms, it was confirmed that the patient’s presentation was cardiogenic. Given the patient had no significant signs of heart failure exacerbation other than breast swelling and mild lower extremity edema, a cardiogenic cause was not immediately obvious. Her breast swelling seemed out of proportion to the fluid status of the rest of her body however quickly improved with a diuretic. In hindsight, considering a diuretic while the patient awaited imaging would have resulted in faster resolution of symptoms as well as alleviated the patient's discomfort and anxiety regarding the symptoms. In counseling patients with newfound breast abnormalities, it is important to quickly rule out malignancy while not overlooking other possible explanations.
ABSTRACT #5
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY/RHEUMATOLOGY
AN OVERLOOKED MIMIC? AUTOIMMUNE MYELOFIBROSIS-A SCOPING REVIEW OF THE LITERATURE
Yosef Joseph Rene Amel Riazat-Kesh1, Alexander Maraveyas1, Lily Martin2, Douglas Tremblay3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the European Hematology Association (EHA) 2023 Congress Annual Meeting that was held in Frankfurt, Germany from June 8-11, 2023 and published in European Journal of Hematology, 2023. PMID: 37515415
BACKGROUND/INTRODUCTION: Autoimmune myelofibrosis (AIMF) is a rare cause of bone marrow fibrosis occurring in the presence or absence of a defined autoimmune disease (secondary or primary AIMF, sAIMF/pAIMF, respectively). Unlike primary myelofibrosis, autoimmune myelofibrosis responds well to immunosuppressive therapy with a benign clinical course. Diagnostic criteria for autoimmune myelofibrosis in opposition to primary myelofibrosis have been lacking, though recent work has helped better characterize molecular and pathological features of autoimmune myelofibrosis, improving diagnostic precision.
METHODS: Using a modern clinical and pathophysiological understanding of autoimmune myelofibrosis, we apply scoping review methodology and rigorous case-criteria to retrospectively analyze the case literature. We examine its patient-population, describing patient-associated factors, presentation, bone marrow pathology, genetics, treatment, and outcomes.
RESULTS: Fifty-five studies were identified, describing 139 autoimmune myelofibrosis patients. Patients were mostly young females (~4:1 ratio female:male, median age 40.8 years) and typically presented with cytopenias. Splenomegaly was rare. sAIMF was more common than pAIMF (~3:1 ratio), and most cases responded well to immunosuppressive therapy.
CONCLUSION: Our results strengthen the emerging picture of autoimmune myelofibrosis's patient population, natural history and response to treatment. Further work should continue to use reproducible diagnostic criteria, and explore autoimmune myelofibrosis's pathophysiology, response to different therapies, and sequelae over larger timescales, as well as differences between pAIMF, sAIMF and primary myelofibrosis.
ABSTRACT #6
BASIC SCIENCE
ENDOCRINOLOGY
MTORC2-NDRG1-CDC42 AXIS COUPLES FASTING TO MITOCHONDRIAL FISSION
Nuria Martinez-Lopez1,2, Pamela Mattar1,2, Miriam Toledo2,3, Henrietta Bais2, Manu Kalyani2 , Marie Louise Aoun4, Mridul Sharma1,2, Laura Beth J. McIntire5, Leslie Gunther-Cummins2, Frank P. Macaluso2, Jennifer T. Aguilan2, Simone Sidoli2, Mathieu Bourdenx6,7, Rajat Singh1,2
1University of California Los Angeles, Los Angeles, CA, United States; 2Albert Einstein College of Medicine, Bronx, NY, United States; 3Institut d’Investigacions Biomediques August Pi i Sunyer (IDIBAPS), Barcelona, Spain; 4Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 5Weill Cornell School of Medicine, New York, NY, United States; 6United Kingdom Dementia Research Institute, London, United Kingdom; 7UCL Queen Square Institute of Neurology, London, United Kingdom
Published in Nature Cell Biology, 2023. PMID: 37386153
BACKGROUND/INTRODUCTION: Fasting triggers diverse physiological adaptations including increases in circulating fatty acids and mitochondrial respiration to facilitate organismal survival. The mechanisms driving mitochondrial adaptations and respiratory sufficiency during fasting remain incompletely understood.
METHODS: We performed unbiased quantitative phosphoproteomics in livers of mice that were (1) basal fed; (2)overnight (14–16 h) fasted; or fasted overnight and then gavaged with (3) dietary triglycerides as corn oil; or (4)BODIPY FL C16/palmitic acid; or (5) refed a high-fat diet. Corn oil or BODIPY FL C16 groups served as models for exogenous lipid availability, while refeeding served as a control to simulate physiological feeding. Corn oil is absorbed as FFA and repackaged and secreted by enterocytes as lipoproteins and subsequently delivered to liver as FFA. Delivery of BODIPY FL C16 to livers was confirmed by direct fluorescence of liver slices.
RESULTS: Fasting or lipid availability stimulates mTORC2 activity. Activation of mTORC2 and phosphorylation of its downstream target NDRG1 at serine 336 sustains mitochondrial fission and respiratory sufficiency. Timelapse imaging shows that NDRG1, but not the phosphorylation-deficient NDRG1Ser336Ala mutant, engages with mitochondria to facilitate fission in control cells, as well as in those lacking DRP1. Using proteomics, a small interfering RNA screen, and epistasis experiments, we show that mTORC2-phosphorylated NDRG1 cooperates with small GTPase CDC42 and effectors and regulators of CDC42 to orchestrate fission. Accordingly, RictorKO , NDRG1Ser336Ala mutants and Cdc42-deficient cells each display mitochondrial phenotypes reminiscent of fission failure.
CONCLUSION: During nutrient surplus, mTOR complexes perform anabolic functions; however, paradoxical reactivation of mTORC2 during fasting unexpectedly drives mitochondrial fission and respiration.
ABSTRACT #7
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
JUNGLE JUICE INDUCED MYOCARDIAL INJURY: CHRONIC USE AND NEW VARIATIONS OF NITRITE PRODUCTS
Matthew Baer1, James Choi1, Vahid Namdarizandi1, Sandra Maria Soler3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2James J. Peters Department of Veterans Affairs, United States Department of Veteran Affairs, Bronx, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Jungle Juice is an alkyl nitrite derivative commonly purchased at supplement stores and used as an illegal inhalant. Limited case reports highlighting myocardial injury from chronic use have been published, along with recognizing newer variations of illegal nitrites.
CASE PRESENTATION: A 60-year-old male with hyperlipidemia presented after a syncopal episode. He presented multiple times prior for syncope, which was attributed to chronic, daily use of a nitrite supplement, Jungle Juice, and was treated with methylene blue each time. He now admitted to taking a different brand of Jungle Juice. Troponin 1300, blood pressure 195/91, and EKG unremarkable, with myocardial injury attributed to demand ischemia from rebound sympathetic response and coronary vasospasm from chronic Jungle Juice use. No percutaneous intervention was attempted, as he denied chest pain and was asymptomatic when seen by Cardiology. Myocardial perfusion scan showed minimal apical and anterolateral ischemia with reversible hypoperfusion; ejection fraction of 68%. Chronic and potentially lethal doses of nitrites from inhalants may lead to coronary artery vasospasm with increased sympathetic tone similar to the reaction seen with rebound angina from chronic nitrate tolerance. Although nitrite use usually presents with hypotension and syncope due to methemoglobinemia (current literature highlights cases after single episode use), this patient experienced rebound sympathetic response immediately after presentation leading to myocardial injury. This may be due to his daily use, leading to “withdrawal” and a depletion of nitric oxide availability. Further use by this patient and recurrent episodes of cessation, will likely lead to more myocardial demand ischemia and possible cardiac arrest. Newer variations in nitrites also contain more potent concentrations and novel compounds, with patients presenting “non-traditionally” after use.
CONCLUSION: Jungle Juice contains derivatives of nitrite inhalants that are becoming increasingly diverse in supplement stores. It is important to identify the frequency and type of use in patients to properly identify symptoms and order further cardiac workup.
ABSTRACT #8
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
THE RESIDENT EDUCATOR: CREATING RESIDENT-LED TEACHING CURRICULUM ON THE MEDICINE WARDS
Galit Balayla Rosemberg1, Julia Ferreira de Carvalho1, Foram Parikh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16. 2024.
BACKGROUND/INTRODUCTION: The fundamental goal of graduate medical training is education. Resident education is achieved through various modalities including formal academic lectures with Attending physicians and direct patient care. However, senior residents often serve as both learners and educators to junior faculty. The Accreditation Council for Graduate Medical Education considers resident teaching ability as a core competency and promotes resident preparation for this role. The importance of formal residents-as-teachers curricula has been established; nonetheless, many residency programs have not formalized such initiatives. Currently, senior residents provide most of the clinical wards' education without a dedicated curriculum within the Internal Medicine residency program at Mount Sinai West/Morningside. We recognize the importance of establishing a formal resident-led didactic session. The goal of this project is to improve the quality of clinical teaching by senior residents by creating infographic-based curricula.
METHODS: We selected a list of high yield medicine topics and created a concise infographics-based teaching guide. At the start of each two-week rotation, a topic was selected and emails with these teaching guides were provided to all residents rotating on the medical wards. Senior residents were instructed to provide a twentyminute lecture on the selected high yield topic to junior learners. All residents were asked to complete a satisfaction survey to assess both compliance and efficacy of senior-led teaching. Residents were requested to fill out pre- and post-surveys, including specific questions to evaluate knowledge improvement. We found that survey fatigue was a limiting factor and therefore, our evaluation plan was modified to a single retrospective post-teaching survey.
RESULTS: 24 responses were obtained from September 2023 to January 2024. Of those, 18 (75%) found the teaching and infographics helpful (selected 8 or above on a Likert scale from 1-10) and only 1 (4.2%) found it intermediate (between 5-7 out of 10). When asked about confidence level on the topic pre-teaching, survey results were highly variable. There was significant improvement in confidence (above 6) post-teaching (p=0.001).
CONCLUSION: Our results indicate that establishing a residents-as-teachers curriculum is an effective tool to improve overall teaching for junior learners. We found that establishing a standardized curriculum for senior residents fosters the necessary core competency skill of becoming a successful educator. While this initiative shows preliminary success, we encountered a few limitations, including allocation of dedicated teaching time and time to complete satisfaction surveys. Moving forward, we aim to create sustainability by establishing a formal curriculum as a standardized protocol for resident education on the medical wards. This is a low-cost initiative and easily reproducible at other institutions across the system.
ABSTRACT #9
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
ANALYSIS OF DATA FROM THE PALOMA-3 TRIAL CONFIRMS THE EFFICACY OF PALBOCICLIB AND OFFERS ALTERNATIVES FOR NOVEL ASSESSMENT OF CLINICAL TRIALS
Celine Yeh1, Mengxi Zhou1 , Neil Bapodra2, Dawn Hershman1, Edward Espinal3, Marina Moran3, Maria Rivero3 , Antonio Tito Fojo1,4, Susan E. Bates1,4
1Columbia University College of Physicians and Surgeons, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Pfizer España, Madrid, Spain; 4James J. Peters Veteran Affairs Medical Center, Bronx, NY, United States
Published in Breast Cancer Research and Treatment, 2024. PMID: 37955764
BACKGROUND/INTRODUCTION: There remains a need for novel therapies for patients with metastatic breast cancer. We explore the use of a novel biomarker of survival that could potentially expedite the testing of novel therapies.
METHODS: We applied a tumor regression-growth model to radiographic measurement data from 393 women with metastatic breast cancer enrolled in PALOMA-3 examining efficacy of palbociclib in disease that had progressed on previous endocrine therapy. 261 and 132 women were randomized to fulvestrant plus palbociclib or placebo, respectively. We estimated rates of regression (d) and growth (g) of the sensitive and resistant fractions of tumors, respectively. We compared the median growth of both arms. We examined the relationship between growth and progression-free and overall survival
RESULTS: As in other tumors, growth is a biomarker of overall survival. In PALOMA-3, we found significant differences in growth among patients with tumors sensitive to endocrine therapy but not amongst resistant tumors, emulating clinical trial results. Subgroup analysis found favorable growth values in visceral metastases treated with palbociclib. Palbociclib efficacy demonstrated by slower growth values was evident early in the trial, twelve weeks after the first 28 patients had been enrolled.
CONCLUSION: Values of growth, estimated using data collected while a patient is enrolled in a clinical trial is an excellent biomarker of overall survival. Our results correlate with the survival outcomes of PALOMA-3 and argue strongly for using growth as a clinical trial endpoint to help inform go/no-go decisions, improve trial efficiency, and deliver novel therapies to patients sooner.
ABSTRACT #10
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE PULMONARY/CRITICAL CARE/RHEUMATOLOGY
EARLY RECOGNITION OF MDA5 DERMATOMYOSITIS, A RARE AUTOIMMUNE DISEASE WITH RAPIDLY PROGRESSIVE LUNG DISEASE, BASED ON CLOSE OBSERVATION OF CLINICAL
Murilo Bastos1, Kristine Lou Gargaritano1, Michael Kaplan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York American College of Physicians Annual Scientific Meeting that was held in Tarrytown, New York, United States on November 5, 2022.
BACKGROUND/INTRODUCTION: The natural progression of interstitial lung disease in patients with dermatomyositis varies significantly. Some patients are asymptomatic or present with slowly progressive symptoms. A small minority of patients, however, present with an amyopathic (muscle-sparing) variant associated with rapidly progressive lung disease. This type of dermatomyositis is associated with the antimelanoma differentiation-associated gene 5 (MDA-5) autoantibody and is nearly uniformly fatal unless acted upon early and aggressively.
CASE PRESENTATION: We describe a case report of a 32-year-old male with no past medical history who presented to the hospital with a 2-month history of worsening dyspnea, cough, fatigue, involuntary weight loss, and myalgia. Prior to this presentation, he attended multiple emergency departments, urgent care, and outpatient visits for these symptoms. Hetested negative for COVID-19multiple times and initially treated for acute bronchitis and later for multifocal pneumonia during those encounters. His workup for pulmonary embolism was negative and computed tomography-chest showed diffuse patchy consolidations with lower lobe predominance. Pulmonary function tests demonstrated a restrictive pattern. The patient underwent extensive infectious and oncologic workup, all unrevealing. An initial myositis panel was negative. At the time of his exam with Rheumatology, a repeat myositis panel and skin biopsy were pending. On physical examination, the patient demonstrated diffuse inspiratory crackles bilaterally on auscultation, subtle violaceous plaques on his knees, and elbows, as well as nose, cheeks, and forehead. He had palmar erythema associated with fissuring and cracking of the skin of the palms, Gottron's papules on his fingers, and pronounced proximal muscular weakness characterized by limited neck flexion. Given the constellation of skin findings, myalgia, lung imaging, and rapidly progressive respiratory failure, a clinical diagnosis of melanoma differentiation-associated gene 5 (MDA5) dermatomyositis was made and later confirmed with a positive MDA5 test on the repeat myositis panel. Subsequently, he was aggressively treated with intravenous methylprednisolone, intravenous immunoglobulin (IVIG), and combination cyclophosphamide/tacrolimus therapy
CONCLUSION: Interstitial lung disease occurs in at least 30 percent of patients diagnosed with dermatomyositis. The presence of melanoma differentiation-associated gene 5 antibodies is linked to the elevated risk for interstitial lung disease progression, and for this reason, early recognition of cutaneous findings in the setting of myalgias and respiratory failure is crucial for early intervention and aggressive systemic treatment. This case report represents the importance of the physical examination for early diagnosis and management particularly relevant in the absence of available specific autoantibody tests.
ABSTRACT #11
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
ELSBERG SYNDROME IN HSV-2 INFECTION
Omar Belfaqeeh1, Alexandria Markley1, Mudita Patel1,2, Brian Markoff1, Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in IDCases, 2023. PMID: 36875152
BACKGROUND/INTRODUCTION: Elsberg syndrome is a neuroinflammatory disease that causes acute or subacute lumbosacral radiculitis, with or without myelitis. Elsberg syndrome typically presents as cauda equina syndrome, with symptoms of sensory impairment, lower extremity weakness, saddle anesthesia, and urinary and/or bowel incontinence. It is usually associated with infectious causes such as SARS-CoV-2, West Nile Virus, Varicella Zoster Virus (VZV), and Herpes Simplex Virus Type 2 (HSV-2), with HSV-2 being the predominate causative pathogen. Treatment with acyclovir, even in cases without a definitive viral cause, is considered beneficial in many cases. Duration of treatment varies and is typically between 10 and 21 days. The use of steroids in the treatment of Elsberg syndrome is debated. Oral steroid tapers or short course high dose intravenous steroids can be used to help shorten the duration of symptoms. Elsberg syndrome accounts for approximately 5–10% of cauda equina syndrome and myelitis and up to 30% of patients have a recurrence of symptoms within the first year. Below we present a unique case of HSV-2 lumbosacral radiculitis (Elsberg Syndrome) diagnosed at a large New York City Hospital Center.
CASE PRESENTATION: Our patient was a 51-year-old female with a past medical history significant for fibromyalgia, right-sided sciatica, right lower extremity deep venous thrombosis, asthma, nephrolithiasis, vertigo, and oral and genital herpes infection who recently returned from Dominican Republic. She presented to the emergency room with complaints of a 10-day history of progressive lower extremity sensory changes and weakness preceded by transient bilateral arm pain and neck and head pressure. Furthermore, she reported being unable to completely void for one day in duration. She described the weakness to be worse in the right leg compared to the left leg, describing it as “leg heaviness” which resulted in a fall at home a day prior to presentation. While she was sitting in the bathroom, she tried to stand but her knees ’buckled’ and she fell backward, hitting her head on the floor (denied any loss of consciousness). Her family carried her to the Emergency Department as she was unable to bear weight. Vital signs on presentation were within normal limits. Physical exam was most notable for reduced power of knee flexors and knee extensors (3/5), dysesthesia to touch and pinprick from mid-thigh distally in stocking distribution bilaterally, absent knee reflexes bilaterally, positive Babinski sign bilaterally, and no clonus. Given her weakness and urinary hesitancy, a magnetic resonance imaging (MRI) of the cervical, thoracic, and lumbar spine was done to assess for spinal cord pathology and a bladder scan was done to rule out urinary retention. Neurology evaluated the patient for acute progressive lower extremity neuropathic pain and weakness. A lumbar puncture was performed to rule out atypical Guillain Barre syndrome or multiple sclerosis.
Complete blood count showed a white blood cell count of 5.1 ×103 cells/mL, hemoglobin of 11.9 g/dL, platelet count of 371 × 103 cells/ mL, and eosinophils elevated to 5.7%. The basic metabolic panel was within normal limits. Vitamin B12 level came back low at 290 pg/mL, homocysteine of 11.2, erythrocyte sedimentation rate of 30.9 and c-reactive protein of 5.9. Other labs including creatine phosphokinase, aldolase, methylmalonic acid, Lyme titers, copper level, vitamin B12, SSA/SSB (Sjogren Antibodies), were unremarkable. The cerebrospinal fluid PCR cytology showed pleocytosis with a WBC count of 360 (100% lymphocytes), although no albumin cytologic dissociation was seen, and protein of 182 mg/dL. Cerebrospinal fluid PCR was positive for HSV-2.
Infectious disease was consulted and reviewed the MRI of the spine with radiology, which demonstrated a very faint enhancement of the L4–5 nerve roots. An MRI of the brain came back within normal limits. An initial
electromyography (EMG) study done during the first week of her admission was unremarkable. A repeat MRI of the whole spine 7 days later showed linear enhancement in the dorsal aspect of the thecal sac from L2 to L4 which may represent an abnormal enhancement of a nerve root in the cauda equina. A repeat EMG was indicative of bilateral L3/L4 radiculopathies. At this point, based on clinical, radiographic, and serological testing the patient was diagnosed with HSV2 lumbosacral radiculitis (Elsberg Syndrome).
The patient was started on acyclovir intravenous 10 mg/kg every 8 hours for 21 days along with adequate intravenous fluid hydration, 5 days of high dose methylprednisolone 1 gram intravenous daily, and B12 supplementation 1000 mcg daily. She needed an aggressive pain control regimen which included acetaminophen, Flexeril, lidocaine patch, duloxetine, Percocet®, and Dilaudid®. 10 days after the first lumbar puncture was performed a second lumbar puncture was done and came back positive for HSV-2 but with no significant improvement of the cerebrospinal fluid (CSF) analysis. 14 days later, a third lumbar puncture was remarkable for improved WBC count (360 down to 80) and protein level (182 down to 73). After being an inpatient for three weeks, the patient was discharged to acute inpatient rehabilitation to improve mobility and to maximize safety and functional independence. She remained in rehab for intensive physical and occupational therapy for one month before being discharged home. Her overall duration of symptoms may have also contributed to her symptom improvement. Although she made great progress while being in the acute rehabilitation unit, she was discharged from rehab with a walking cane as a main mode of ambulation.
CONCLUSION: Elsberg syndrome is a rare cause of infectious lumbosacral radiculitis with a wide variety of clinical presentations and diagnostic criteria. A proposed diagnostic criteria of Elsberg syndrome includes clinical signs and symptoms of caudal equina syndrome, such as urinary/ bowel retention, hesitancy, or incontinence, and MRI or electrophysiologic evidence of cauda equina involvement. Other features that may be suggestive of Elsberg syndrome include preceding genital herpes infection, herpes virus infection in the CSF, clinical or radiographic evidence of myelitis in the conus, acute/subacute onset, and CSF pleocytosis. Our patient met several of the proposed diagnostic criteria as she reported urinary retention, had CSF positive for HSV2, and had MRI evidence of cauda equina involvement as seen on the second MRI taken five days after admission. Additionally, the acute onset of her symptoms and CSF pleocytosis further supported her diagnosis. Antiviral treatment may affect symptom duration, but there is no evidence it helps with neurologic improvement in herpetic radiculomyelitis. Our patient was started on intravenous acyclovir for a total duration of 21 days and received 5 days of high dose corticosteroids. Steroids were initiated to reduce inflammation, and after receiving three days of steroids, the patient began to see improvement in her symptoms. Being cognizant of Elsberg syndrome while treating patients with signs and symptoms of lumbosacral radiculitis is crucial as initiating intravenous acyclovir for 10–14 days along with corticosteroids is regarded as a treatment of choice due to the possibility of shortening symptoms duration and improving overall morbidity.
ABSTRACT #12
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
ENGAGING PHYSICIAN TRAINEES THROUGH BEDSIDE INTENSIVE CARE UNIT NARRATIVES: A MULTISITE EXPANSION STUDY
Raul Benavides1 , Maria Athena Riego1,2 , Edith Robin1,2, Valeria Santibanez3 , Hailey Gupta2 , Kathryn Bass1 , Usha Govindarajulu4 , Samantha Ortiz1 , Gabriela Bernal4 , Alexander Davidovich1 , Edwardine Mirna Mohanraj1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Emory School of Medicine, Atlanta, GA, United States Presented at the Accreditation Council for Graduate Medical Education Annual Educational Conference that was held in Orlando, Florida, United States from March 7-9, 2024 and the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16. 2024.
BACKGROUND/INTRODUCTION: Intensive care unit (ICU) patients are at high-risk for dehumanization Barriers to providing empathic care include high workload, non-communicative patients, and provider burnout, which can also result in physician disengagement. In 2019, the authors implemented a novel narrative medicine intervention in the medical ICU to promote increased engagement with patients and increased fulfillment from work. Patient biographic and social information was elicited via questionnaire (Patient Bios), shared during ICU rounds, and posted in patients’ rooms (the intervention). Post-intervention, resident physicians spent more time at the patient’s bedside, developed easier rapport with surrogates, and derived more meaning from work. In this multisite expansion study, we hypothesize that eliciting and sharing Patient Bios with ICU physician trainees will increase interpersonal engagement and increase professional fulfillment irrespective of ICU type or geographic location.
METHODS: We designed a longitudinal, mixed-methods study to implement the intervention across ICUs in New York and New Jersey. To date, the study has been conducted for a 6-month period at Site 1 of 7 planned ICU sites. Qualitative and quantitative data was collected at the following intervals: pre-ICU rotation, end-rotation, and 3-months post-ICU rotation. At each data collection point, residents submitted prompted audio or written diaries and completed the Stanford Professional Fulfillment Index© (PFI), avalidated assessment of professional satisfaction and burnout in the workplace. Iterative thematic analysis of diary submissions was performed. Statistical analysis of PFI surveys were conducted using a within-subject design and analyzed with the Friedman test assessing statistical differences between the time points.
RESULTS: One hundred thirty-four Patient Bios were completed over 6-months at Site 1. Twenty-two physician subjects were enrolled. 46 end-rotation diary submission were submitted by 21 participants in total. 21 participants (95% response rate) completed the Professional Fulfillment Index Self-Assessment tool (PFI) before their ICU block, 16 (72% response rate) 2 weeks after and 8 (36% response rate) at the 3 months point. Thematic analysis of resident’s diaries before and after their ICU rotation, showed the following categories related to resident’s patient-care-experience: (i) Human Centered Care (HCC), (ii) Communication and Relationship Building (CRB), (iii) Effects on Personal Emotions (EOE), (iv) Impact on Patient Care (IPC), and (v) Impact on Personal Practice (IPP). Iterative analysis of core themes (ii, iii and iv) elicited the following subthemes: Successful or Unsuccessful, for CRB; Positive, Negative or Neutral, for EOE; and Positive, Negative or Neutral, for IPC. Fulfillment and burnout were identified as opposites on the spectrum of resident’s emotional experience. Quantitative analysis showed that before each resident's ICU block, 67% reported moderate and 33% reported high professional fulfillment (PF). At 2 weeks post-intervention, PF was high in 63% and moderate in 37%. By month 3, one participant (4.5%) reported low fulfillment, while 38% reported moderate PF and 50% reported high PF. Burnout scores were low in 43% and moderate in 57% of participants before their ICU block.
By week 2, burnout scores were low in 53% and moderate in 40%. At the 3-months post ICU, burnout scores were 43% low and 43% moderate. Only 1 participant (4.5%) scored high burnout at both 2 weeks and 3 months. Due to the potential non-normality of PFI and burnout scores and the multiple time points per participant, we utilized the Friedman test to evaluate for differences within each subject. The test revealed statistically significant differences among time points for Fulfillment (p<0.03) and for Burnout (p<0.002).
CONCLUSION: Implementation of this novel narrative medicine intervention is feasible and positively accepted by site-based implementation teams and physician subjects. Overall, residents enjoyed the intervention, noting its positive impacts on human-centered care, communication, and relationship-building. We hope to overcome limiting factors such as a declining response rate (95% before, 72% 2 weeks after and 36% at the 3-month point) by increasing the sample of participants once the rest of sites complete the intervention period. Site 1 quantitative analyses are promising with trends towards significant improvement in professional fulfillment and burnout. As additional multisite data is collected and analyzed, the authors anticipate similar and sustained improvements in primary and secondary outcomes irrespective of ICU type or geographic location.
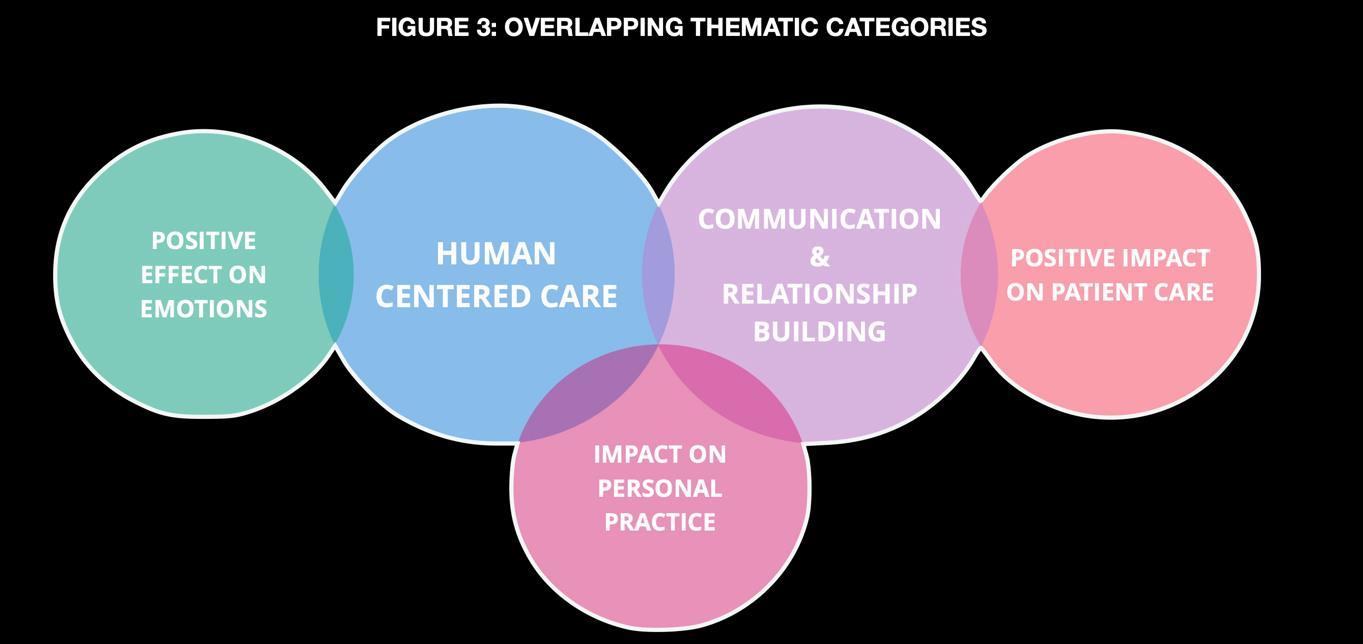
ABSTRACT #13
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY/PALLIATIVE CARE
THE ASSOCIATION OF SOCIODEMOGRAPHIC FACTORS AND TYPE OF CANCER WITH END-OF-LIFE PALLIATIVE CARE UTILIZATION IN PATIENTS WITH METASTATIC CANCER: A NATIONAL INPATIENT DATABASE ANALYSIS
Raphael Bertasi1 , Tais Bertasi1 , Nadeem Bilani1, Alaina Kessler2, Nicholas Rohs2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Early palliative care referrals are associated with improved quality of life, however, most referrals occur late in the disease process in the inpatient setting. We aimed to investigate sociodemographic barriers associated with palliative care utilization in the inpatient setting.
METHODS: Using the National Inpatient Sample (NIS) database from 2017 to 2020, we collected data of hospital admissions of patients with metastatic cancer that ended in inpatient death based on the ICD-10 code C77 to C79.9, and within this group, investigated the occurrence of palliative care utilization. We used univariate statistics to describe the sociodemographic characteristics and multivariate regression modeling to compute odds ratios (OR), 95% confidence intervals, and p-values to investigate the association of these characteristics with palliative care utilization. Each model was adjusted for age, race/ethnicity, type of cancer, income, disease severity by All-Patient Refined Diagnosis-Related Groups' (APR-DRG) Severity of Illness, insurance status, and Charlson comorbidity index. The analysis was performed using SPSS version 28.
RESULTS: There were 58,828 non-elective admissions of patients with metastatic cancer who died from 2017 to 2020, of which 61.5% received an inpatient palliative care consultation. During this time, there was an increase in palliative care consults from 60.2% to 61.7%. Overall, palliative care consults significantly decreased length of stay and total hospital charges by 8.9% and 19.6%, respectively (p<0.001). The most prevalent cancers in this cohort were lung (25.8%), breast (7.4%), and pancreas (6.7%). Central nervous system cancers were associated with higher palliative care utilization (OR, 1.75; 95%CI, 1.26-2.43; p<0.001), while hematologic malignancies were associated with lower odds of having a palliative care consult (OR, 0.83; 95%CI, 0.75-0.92; p<0.001). Females (OR, 1.14; 95%CI, 1.1-1.19; p<0.001), higher income (OR, 1.36, 95%CI, 1.29-1.43; p<0.001), and older age (OR, 1.28; 95%CI, 1.14-1.45; p<0.001) were associated with higher palliative care utilization. Black (OR, 0.77; 95%CI, 0.74-0.81; p<0.001), Hispanic (OR, 0.92; 95%CI, 0.86-0.98; p=0.013), and Asian (OR, 0.89; 95%CI, 0.82-0.97; p=0.007) patients had fewer palliative care consultations when compared to White patients. Fewer palliative care consultations were also significantly found in Medicare (OR, 0.83, 95%CI, 0.790.87; p<0.001) and Medicaid (OR, 0.91; 95%CI, 0.86-0.97; p=0.004) admissions when compared to private insurance or self-pay.
CONCLUSION: In recent years, there has been an increase in inpatient palliative care consults for patients with metastatic cancer associated with decreased length of stay and overall hospital expenses. However, there are still disparities in access to this care based on sociodemographic factors, including gender, race, income, and insurance status. Future studies should aim to address these disparities to reduce healthcare inequalities.
ABSTRACT #14
CLINICAL RESEARCH
CARDIOLOGY/HEMATOLOGY/ONCOLOGY
THE IMPACT OF CARDIOVASCULAR COMORBIDITIES ON MORTALITY IN PATIENTS RECEIVING INPATIENT CHEMOTHERAPY
Tais Bertasi1, Raphael Bertasi1, Nadeem Bilani1, Alaina Kessler2, Nicholas Rohs2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Cardiotoxicity is a common adverse effect of chemotherapy, which canresult in acute events such as arrhythmias, acute coronary syndrome, and myocarditis, as well as chronic conditions including cardiomyopathy and left ventricular dysfunction. Patients receiving chemotherapy who have underlying cardiovascular (CVS) risk factors are at increased risk of poor outcomes.
METHODS: Using the National Inpatient Sample dataset from 2017 to 2020, we collected data of hospital admissions for chemotherapy based on ICD-10 code. The primary outcome was the association of cardiovascular risk factors on all-cause mortality. We utilized univariate statistics to describe our cohort. We performed multivariable logistic regression modeling to compute hazard ratios, 95% confidence intervals, and pvalues depicting the adjusted impact of each covariate on hospital mortality. We adjusted for relevant confounders, including age, race/ethnicity, stage of disease (metastatic or not), and Charlson comorbidity index. The cardiovascular comorbidities included were a history of cerebrovascular accident (CVA), congestive heart failure (CHF), atrial fibrillation (Afib), coronary artery disease (CAD), peripheral vascular disease (PVD), metabolic syndrome, hypertension (HTN), smoking, and hyperlipidemia (HLD). The analysis was performed using SPSS version 28.
RESULTS: There were 107,425 hospital admissions for chemotherapy, among which 684 (0.64%) patients died during the admission. Median age was 47 years (IQR, 17-63) and 42.6% were females. There was no identified cardiovascular comorbidity in 56.5% of admissions, while there were 24% of admissions with one comorbidity, and 19.5% with more than one comorbidity. The cardiovascular covariate associated with all-cause mortality in patients receiving chemotherapy with the largest adjusted effect size was history of CVA (HR, 5.60; 95%CI, 4.137.61; p<0.001). A history of CHF (HR, 2.54; 95%CI, 1.96-3.29; p<0.001) and Afib (HR, 1.48; 95%CI, 1.08-2.03; p=0.014) were also significantly associated with increased mortality. A history of coronary artery disease, peripheral vascular disease, metabolic syndrome, hypertension, or smoking was not significantly associated with mortality (Table 1).
CONCLUSION: Among patients admitted for chemotherapy, cardiac disease is a significant cause of mortality. Patients with a history of cerebrovascular accident are at particularly high risk. With regards to congestive heart failure, patients receiving chemotherapy are more likely to receive fluids, which could explain the increased mortality in patients with heart failure. Moreover, management of atrial fibrillation can be challenging due to drug interactions, which could lead to high mortality in this group of patients. Therefore, a multidisciplinary approach including Cardiology and Oncology is important for patients with cardiovascular risk factors to help manage underlying comorbidities and improve patient outcomes.
Cardiovascular comorbidity (N=number of patients)
Table 1. Association of cardiovascular risk factors on all-cause mortality. Abbreviations: history of cerebrovascular accident (CVA), congestive heart failure (CHF), atrial fibrillation (Afib), coronary artery disease (CAD), peripheral vascular disease (PVD), metabolic syndrome, hypertension (HTN), and hyperlipidemia (HLD)
ABSTRACT #15
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
EVALUATION OF A DATA ANALYSIS VIDEO CURRICULUM CREATED FOR RESIDENTS AND FELLOWS Nadeem Bilani1 , Mantej Sehmbhi1,2 , Georgina Osorio1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16. 2024.
BACKGROUND/INTRODUCTION: In academic medicine, knowledge acquisition often occurs through asynchronous learning. In 2022, the Research and Scholarly Work Council, created an anthology of minuteslong video demonstrations in basic data analysis for clinical research using the Statistical Package for the Social Sciences (SPSS®) software. This curriculum delves into topics spanning data handling, cleaning, analysis, and interpretation, and was introduced to the Internal Medicine cohort in 3 once weekly workshops in May 2023 after being made available for access and independent viewing on the Mount Sinai shared drive.
METHODS: This abstract presents data from a 10-question survey, including both qualitative and quantitative measures, used to assess engagement of and perceptions towards this virtual statistics curriculum. Univariate statistics, including frequencies and percentages, are used to describe the quantitative results from this survey.
RESULTS: A total of n=23 Internal Medicine residents participated in this survey. The breakdown by postgraduate year level was n=5 (21.7%) first-year residents, followed by n=9 (39.1%) second-year, and n=9 (39.1%) third-year residents. On a 5-point Likert scale ranging from 1 ('Not Important') to 5 ('Extremely Important'), n=12 (50%) rated the importance of data analysis skills for residents and fellows as 5, while n=7 (29.2%) offered ratings of 4 and n=4 (16.7%) of 3. No responders (0%) provided a score of 1 ('Not Important') or 2 ('Somewhat Unimportant'). The majority of responders (n=10, 43.5%) first learned of this curriculum through residency didactics, while a minority reported discovering it in conversation with peers (n=6, 26.1%), or during research council meetings (n=3, 13.0%). When asked to describe their use of this curriculum, n=8 (34.8%) of responders reported "Successful" use, n=4 (17.4%) reported "Limited Success" in use, n=0 (0%) reported "Unsuccessful" use, while n=11 (47.8%) reported "No Use Yet". Despite this limited uptake, the majority reported being “Very Likely” (n=8, 34.8%) or “Somewhat Likely” (n=8, 34.8%) to use this SPSS curriculum in the future. Of those that reported use of this curriculum (n=12), n=6 (50%) reported using it “to independently run analysis on a research study”, while n=4 (30%) reporting using it “to assist in data analysis for a research study”. The rest (n=2, 16.7%) used this curriculum “for education purposes”. In recommendation for how to disseminate this curriculum further, n=14 (60.9%) responders suggested “incorporation into academic didactics”, n=7 (30.4%) suggested “as required curriculum during research electives”, while n=2 (8.7%) suggested moving the curriculum platform from the Mount Sinai shared drive to another location, such as YouTube.
CONCLUSION: This abstract corroborates a prior pre-intervention assessment by Sehmbhi et al. (2023) that highlighted a need for practical teaching in medical statistics and data science for resident physicians. It also shows that when given the opportunity for asynchronous learning, a significant proportion of trainees are able to apply this to independently run, or assist in running, analysis for research projects. Finally, this survey indicates that increased uptake of such a curriculum might be gained by implementation into required academic time for trainees, such as through didactics or dedicated electives, as well as through increased visibility and accessibility.
ABSTRACT #16
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/PULMONARY/CRITICAL CARE
THE PERFECT STORM: TORSADES DE POINTES IN PATIENT WITH LIVER CIRRHOSIS PRESENTING WITH VARICEAL BLEEDING
Salvador Caceros Diaz1*, Jonas Marx1*, Juan Arango Morales1*, Gopal Narayanswami1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States *These authors contributed equally to this work.
BACKGROUND/INTRODUCTION: Torsades de pointes is a rare but potentially lethal type of polymorphic ventricular tachycardia associated with congenital or acquired QT interval prolongation. Hospitalized patients are at an increased risk for developing the dreaded arrhythmia even in the absence of prior cardiac disease as they often present with multiple predisposing risk factors, such as advanced age, electrolyte abnormalities, exposure to QT-prolonging drugs, impaired drug metabolism, or bradycardia. One population known to be particularly prone to QT interval prolongation and subsequent development of torsades de pointes are patients with hepatic impairment and cirrhosis.
CASE PRESENTATION: A 63-year-old woman with a history of alcohol use disorder, type 2 diabetes mellitus, hypertension, and hypercholesterolemia was brought to the hospital with a 1-day history of hematemesis and melena. She experienced massive upper gastrointestinal bleeding during the initial assessment in the emergency department and became hemodynamically unstable requiring intubation for airway protection. The patient received a massive transfusion protocol with 5 units of packed red blood cells, 4 units of fresh frozen plasma, and 1 unit of platelets. Subsequently, she was admitted to the intensive care unit
The physical exam was notable for scleral icterus and palmar erythema. Remarkable laboratory findings included severe anemia with a hemoglobin of 5.5 g/dL, hypokalemia, borderline-low magnesium, elevated blood urea nitrogen, elevated lactate, and elevated troponin-I. Liver function testing with a Model for End-Stage Liver Disease-Sodium (MELD-Na) score of 23 was consistent with acute decompensated cirrhosis. Blood alcohol level, SARS-CoV-2 PCR, and urine toxicology were negative. Hypokalemia and borderline-low magnesium levels were actively repleted; the lowest levels of potassium and magnesium were 3.4 mEq/L and 1.6 mg/dL, respectively.
She also presented a myocardial injury with a troponin-I peak level of 3.4 ng/ml, T wave inversions in V2 and V3. A transthoracic echocardiogram showed an ejection fraction of 60%, left ventricular hypertrophy, right ventricle dilation, bi-atrial dilation, trivial aortic and mitral regurgitation, and trace pulmonic regurgitation. Normal right and left ventricular wall motion.
Approximately 2 hours after receiving massive transfusion protocol, the patient developed flash pulmonary edema with new-onset diffuse bilateral crackles and extensive opacities on chest radiograph, thought to be secondary to transfusion-associated circulatory overload. Significant improvement occurred with a single dose of furosemide 40 mg intravenously and fluid restriction. The case was evaluated by Gastroenterology. The upper gastrointestinal bleed was managed with pantoprazole and octreotide infusions, and endoscopic band ligation of 3 large esophageal varices was performed 14 hours after admission with no rebleeding.
Prolongation of QTc interval was noted on telemetry and serial electrocardiograms (ECG). The baseline QTc interval was 467 milliseconds (msec) 2 months prior to admission and 465 msec in the ED. QTc intervals on ECG were 569 msec and 634 msec, 10 hours and 28 hours after admission, respectively. After 29 hours of hospitalization, a 22-second polymorphic ventricular tachycardia was identified on telemetry, with a QTc of 682 msec immediately prior to event (Figure 1).
Defibrillator pads were placed preventively after recognizing torsades de pointes. Blood for laboratory analysis was collected before any intervention, magnesium sulfate 2 g intravenous in 15 min and potassium chloride 10 mEq/hr intravenous for 4 hours were administered. Cardiology was consulted, and after reviewing the case and the list of active medications, the only possible QT-prolonging agents identified were octreotide and pantoprazole (conditional torsades de pointes risk/to be avoided in congenital long QT syndrome). Octreotide was discontinued and isoproterenol infusion was started, to a goal heart rate above 100 bpm. Despite these interventions, the patient had 2 more episodes of torsades de pointes of 20 seconds and 5 seconds, 1 hour and 3 hours after initial torsades de pointes, respectively (Figure 2). An additional 1 gram of magnesium sulfate was administered after the second episode.
Over the next 48 hours the QTc interval decreased to 477 msec and isoproterenol was discontinued. Patient remained hemodynamically stable and was successfully extubated. No additional episodes of torsades de pointes were noted on telemetry monitoring in intensive care unit or medical floor.
After discharge, the patient stopped drinking alcohol and was referred to the liver transplant department. On follow-up appointmentsrepeat electrocardiogram showed QTc of 438-454msec. Unfortunately, 1 year after initial presentation, she died of urosepsis at another hospital before completing liver transplant process.
CONCLUSION: Torsades de pointes describes a spontaneously evolving polymorphic ventricular arrythmia most commonly triggered by a premature ventricular beat on a T wave in the setting of a prolonged QT interval. QT interval prolongation can be congenital, acquired, or a combination of both. This patient presented with a normal corrected QT interval, had no known prior QT interval prolongation and no family history of sudden cardiac death or personal history of unexplained syncope, rendering the presence of a congenital long-QT syndrome less likely.
Acquired QT interval prolongation often is the result of multiple contributing factors. While the patient did not suffer from any structural, ischemic, or arrhythmogenic cardiac disease, she presented with several risk factors predisposing for QT interval prolongation, including female sex, advanced age, and, importantly, hepatic impairment due to cirrhosis. Additionally, the patient was found to have hypomagnesemia and hypokalemia, electrolyte abnormalities known to favor QT interval prolongation. These electrolyte abnormalities may have been temporarily exacerbated by the massive transfusion of blood products. Massive transfusion protocol carries the risk of electrolyte abnormalities, particularly due to citrate compounds that prevent coagulation of fresh frozen plasma and platelets during storage. Citrate is metabolized to bicarbonate, which in turn causes hypocalcemia by binding to ionized calcium. Furthermore, alkalosis leads to hypokalemia as hydrogen ions exit the cell via H+/K+ cotransporter to offset alkalosis. Hypocalcemia and hypokalemia are known to prolong the QT, potentially leading to torsades de pointes. Furosemide is also to blame, being a drug classified as having conditional risk for torsades de pointes. Finally, intravenous injection of pantoprazole (conditional risk for torsades de pointes) and octreotide (not enough evidence to assign risk category) may have contributed to the observed QTc prolongation.
The case highlights the importance of close cardiac monitoring of cirrhotic patients admitted to the hospital for gastrointestinal bleeding given their increased risk of developing acquired QT interval prolongation. QT prolonging substances should be avoided in this patient population as best as possible, and electrolytes including magnesium, calcium and potassium should be monitored and repleted rigorously.
Figure 1: First episode of Torsades de pointes. QTc of 682 milliseconds preceding R on T phenomenon followed by polymorphic ventricular tachycardia episode lasting 22 seconds
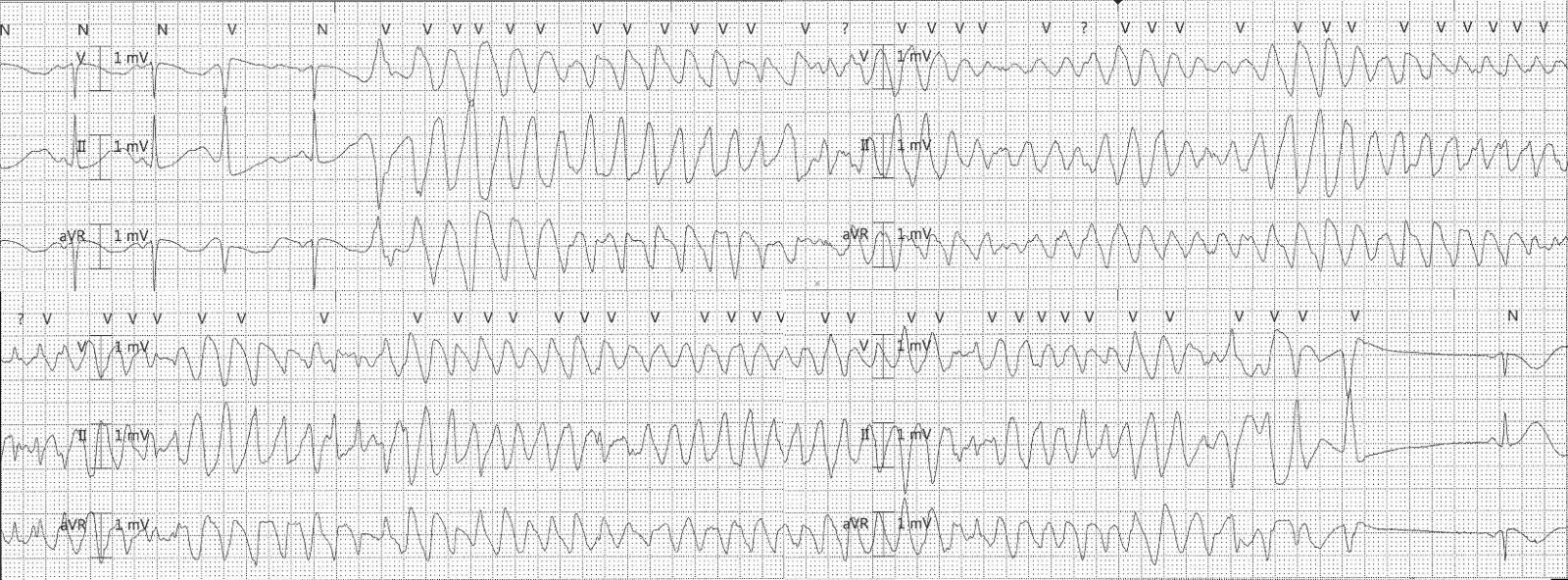
Figure 2: Recurring episodes of Torsades de pointes. Polymorphic ventricular tachycardia episodes lasting 20 seconds and 5 seconds

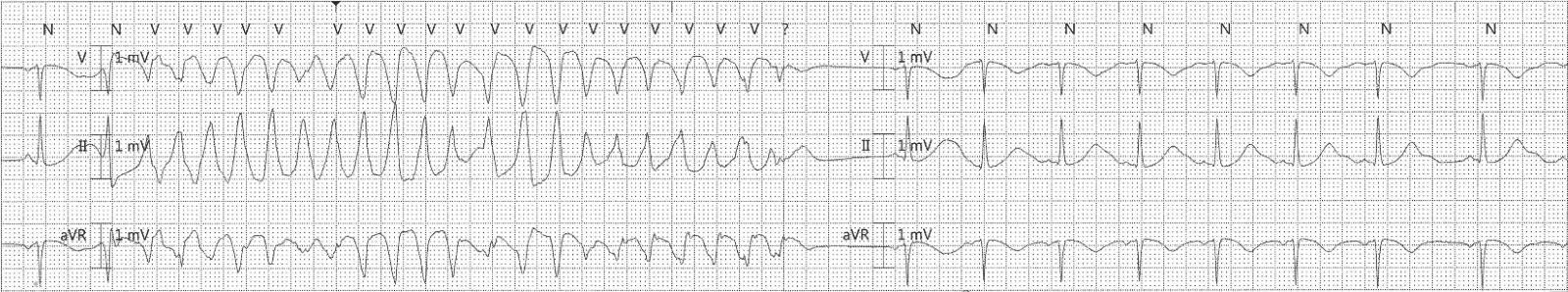
Supplemental material:
Electrocardiograms with dynamic QTc prolongation.
a. QTc approximately 634 milliseconds after 28 hours of admission.
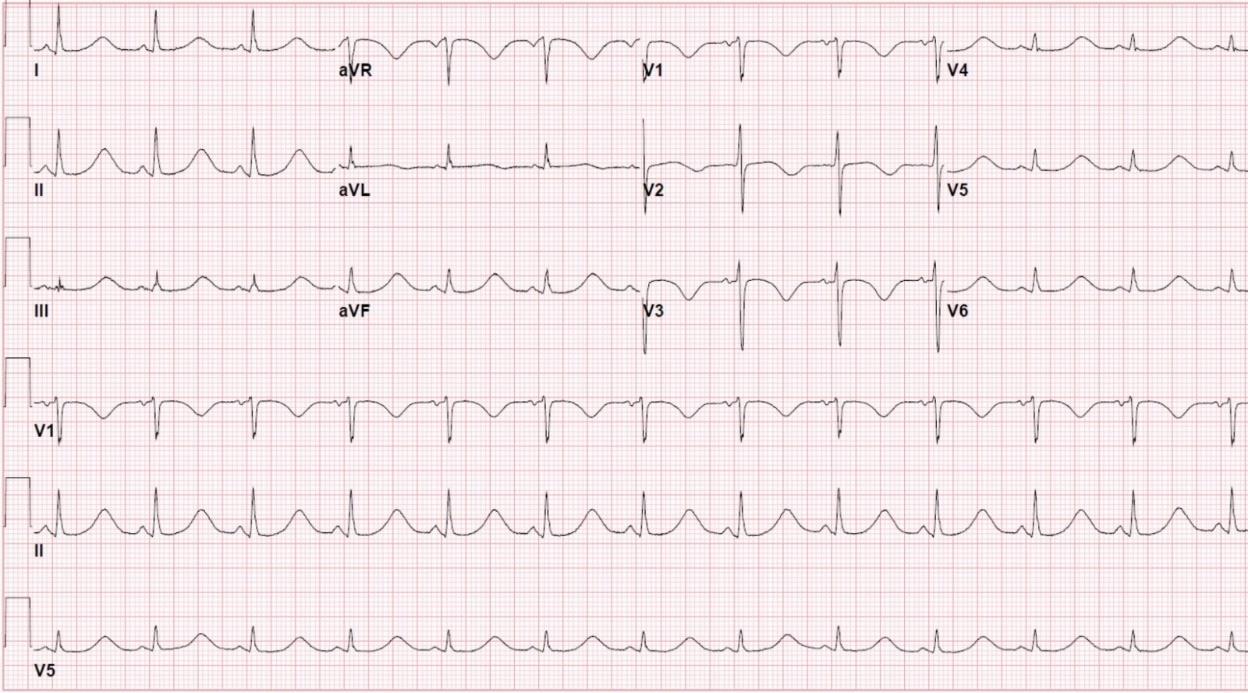
b. QTc approximately 477 milliseconds 77 hours after admission.
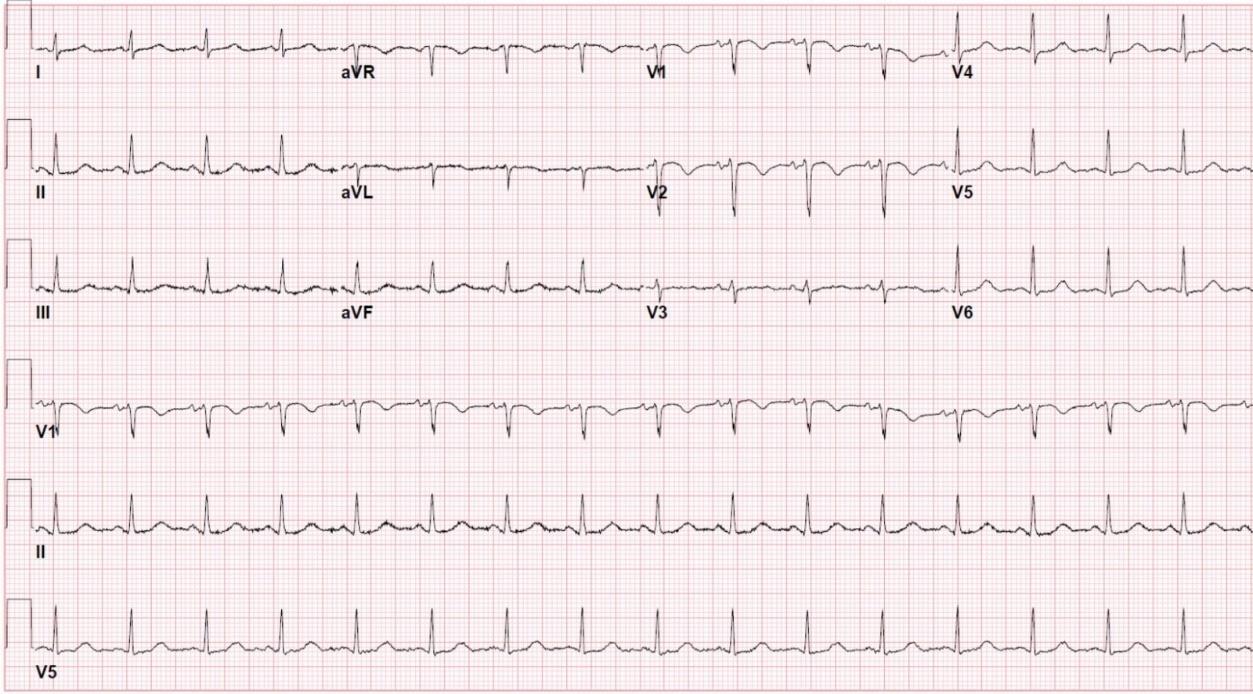
Table 1: Laboratory testing at different time points before and during hospitalization.
ALP = alkaline phosphatase; ALT = alanine transaminase; AST = aspartate transaminase; BUN = blood urea nitrogen; INR = international normalized ratio; BNP = brain natriuretic peptide; TP = massive transfusion protocol; PTT = partial thromboplastin time; TdP = Torsades de pointes; WBC = white blood cell.
Table 2: Pharmacologic agents administered before polymorphic ventricular tachycardia
Rocuronium Single dose
Ketamine Single dose
Midazolam Bolus and infusion
Fentanyl Bolus and infusion
Pantoprazole Bolus and infusion
Octreotide Infusion
Furosemide Single dose
Ceftriaxone Single dose
Thiamine Single dose
Phytonadione Single dose
ABSTRACT #17
CLINICAL RESEARCH
CARDIOLOGY
SINGLE LEAFLET DEVICE ATTACHMENT AFTER MITRACLIP IMPLANTATION: A SYSTEMATIC REVIEW AND META-ANALYSIS
Kristen Carter1, Souyma Gupta1, Kirtipal Bhatia1, Marija Petrovic1, Stamatios Lerakis1, Edgar Argulian1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, New York, United States
BACKGROUND/INTRODUCTION: This study aims to assess the incidence of single leaflet device attachment (SLDA) in patients undergoing percutaneous mitral transcatheter edge-to-edge repair (TEER) with the MitraClip device. Despite the success of mitral TEER in treating symptomatic moderate to severe mitral regurgitation, understanding the occurrence of SLDA is crucial. To evaluate influencing factors, we conducted a meta-analysis of examining the impact of various variables on single leaflet device attachment rates.
METHODS: A study-level random-effects meta-analysis, utilizing Freeman-Turkey transformation, estimated the pooled incidence of SLDA in patients undergoing TEER with the Mitraclip device. Subgroup analyses assessed the influence of variables, such as the underlying mechanism of mitral regurgitation (secondary versus primary), study size, publication date, and Mitraclip device generation. Meta-regression analyzed the effect ofsex on single leaflet attachment. The primary outcome was the incidence of single leaflet attachment during follow-up.
RESULTS: We included 41 studies with over 54,000 patients undergoing TEER with a Mitraclip. The pooled incidence of SLDA was 1.9% (95%CI, 1.5-2.3%; I2=81.7%). The rates of SLDA did not differ significantly among patients with primary or secondary mitral regurgitation. The Incidence of SLDA was significantly lower among more contemporary studies and among studies using a newer Mitraclip device generation for TEER (1.3%; 95%CI, 1.1-1.5%) compared to studies using a first-generation clip (2.7%; 95%CI, 2.0-3.5%).
CONCLUSION: Single leaflet attachment is a rare but important complication to identify among patients undergoing transcatheter edge-to-edge repair with a Mitraclip device. The incidence of single leaflet attachement has decreased over the past 5 years, particularly with the use of newer generation Mitraclip and improvement in procedural imaging.
ABSTRACT #18
QUALITY IMPROVEMENT
GENERAL INTERNAL MEDICINE
Adrian Chernyk1* , Sharel Sadud1, Krystle Hernandez1, Shantheri Shenoy1, Foram Parikh1, Vasundhara Singh1 , Nikta Athari1, Philip Chen1, Julie Pearson1, Benjamin Dempsey1 , Faye Reiff-Pasarew1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of Hospital Medicine (SHM) Annual Meeting that was held in San Diego, California, United States from April 12-15, 2024 and will be presented at theSociety of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024 *These authors contributed equally to this work.
BACKGROUND/INTRODUCTION: Laboratory testing is one of the highest volume medical activities in a health system. Despite their central role in driving clinical decision-making, laboratory diagnostics are highly variable and expensive. The annual cost estimate in the United States for low value screening, testing, or procedures range from 17.2 billion to 27.9 billion dollars. Excessive laboratory testing can be painful, disturb sleep, decrease satisfaction, increase length of stay, increase transfusions, lead to venipuncture complications, and is labor intensive. Physician trainees often order extraneous labs due to a lack of understanding of what is necessary and fear of supervisor criticism. Electronic medical systems have simplified the ordering of lab tests, which can lead to recurrent ordering without much consideration.
METHODS: Our primary endpoint was to reduce the number of common labs ordered on the inpatient medicine services per patient by 10% over six months. Our process measure was the percent of inpatients with recurrent lab orders (labs ordered for multiple days). We created a “recurrent labs” flag in the electronic health record (EHR), audited patient charts five times a week, and provided feedback to the teams. The EHR was queried for the total numbers of the most common venous blood studies (CBC, BMP, LFTs, PT/INR, PTT, magnesium, phosphorus, and type and screen). The study was divided into 3 phases. Phase 1 (January 3-20, 2023) established baseline data. Due to the low percentage of recurrent labs ordered on the non-teaching service, we focused on the teaching service, where rates were much higher. Phase 2 (1/20/2023-10/4/2023) combined chart audits, team feedback, and educational sessions for residents, advanced practice practitioners, and hospitalists to emphasize the principles of effective lab stewardship. We distributed mouse pads, chocolates, and handouts with a QR code linked to an intranet site outlining the initiative. During Phase 2 we also surveyed the house staff anonymously to assess barriers in reducing recurring lab orders. Phase 3 (starting from 10/9/2023) broadened the aforementioned interventions to a second site (Site B) and introduced incentives for the team with the fewest recurring lab orders over each two-week period.
RESULTS: Between 1/3/2023 and 11/17/2023, we audited 10,144 charts. The mean percentage of recurrent lab orders on the teaching service at Site A fell from 57% pre-implementation (phase 1) to 42.49% and 17.08% in phases 2 and 3, respectively. At Site B, the mean percentage of recurrent lab orders fell from 55% to 23.76% during phase 3. In the first 6 full months, the common lab orders per patient decreased by 14% at Site A over the prior year baseline, meeting our primary goal. Our House staff survey during phase 2 revealed that the most significant barrier to reducing recurring lab orders was the additional workload that is required to check lab orders daily (87%), coupled with the concern over missing information (52.2%). The most frequently recommended approach to reduce recurring labs was to take the time to discuss lab orders collectively as a team during rounds.
CONCLUSION: Successful strategies to improve lab stewardship included educating providers on the harms of unnecessary lab orders, understanding when to order labs, avoiding recurring lab orders, discontinuing unnecessary labs, and discussing labs on rounds. While education and constructive feedback improved the rate of recurrent labs, positive incentives were most effective.
ABSTRACT #19
CLINICAL RESEARCH
CARDIOLOGY
IN-HOSPITAL OUTCOMES AND USE OF MECHANICAL CIRCULATORY SUPPORT IN PATIENTS WITHOUT STANDARD MODIFIABLE RISK FACTORS AND CARDIOGENIC SHOCK
James Choi1, Sara Diaz1, Christopher N. Matthews1, Francisco José Romeo2, Ashish Correa1, Arieh Fox1 , Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2University of Miami Miller School of Medicine/Jackson Memorial Hospital, Miami, FL, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Recent studies have highlighted a rise in mortality rates and poorer outcomes among patients experiencing myocardial infarction with standard modifiable risk factors. Our objective was to investigate the outcomes in individuals presenting with heart failure and cardiogenic shock within this patient population.
METHODS: This is a retrospective study using the National Inpatient Sample for hospitalizations between 2017 - 2019. ICD-10 codes identified patients presenting with cardiogenic shock divided into those with and without standard modifiable risk factors (diabetes mellitus, hyperlipidemia, hypertension, and smoking). The outcomes of interest were mortality, in-hospital outcomes (acute kidney injury, arrest, and arrhythmias), and use of mechanical circulatory support. Multivariate logistic analysis was used to adjust for age, gender, race, location, and relevant co-morbidities with a p-value<0.2 in univariate screen.
RESULTS: A total of 520,225 patients were hospitalized with cardiogenic shock, of which 24.3% had no standard modifiable risk factors Standard modifiable risk factors less patients, compared to those with one or more standard modifiable risk factors, have increased adjusted odds of all-cause mortality (OR, 2.44; 95%CI, 2.392.49) and worse in-hospital outcomes including acute kidney injury (OR, 1.40; 95%CI, 1.24-1.58), cardiac arrest (OR, 1.10; 95%CI 1.03–1.18), and ventricular tachycardia (OR, 1.14; 95%CI, 1.08-1.19). There were increased use of extracorporeal membrane oxygenation (OR, 1.53; 95%CI, 1.32-1.77) and durable left ventricular assist device implantation (OR, 1.63; 95%CI, 1.41-1.88)
CONCLUSION: Considering the growing significance of identifying non-conventional risk factors for coronary artery disease and myocardial infarction, it is crucial to highlight that patients who present with acute heart failure and cardiogenic shock face heightened risks of mortality, adverse cardiovascular outcomes, and usage of mechanical circulatory support. There is a pressing need for additional research to delve into the root causes of this association, as it could play a pivotal role in mitigating and preventing unfavorable outcomes in these patients.
ABSTRACT #20
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
MICROSATELLITE INSTABILITY HIGH: A DEFINITIVE PREDICTIVE BIOMARKER FOR IMMUNE CHECKPOINT INHIBITORS YET UNDERSTUDIED IN UNDERREPRESENTED MINORITIES WITH GASTROINTESTINAL CANCERS
Nobel Chowdhury1 , Fiyinfolu Balogun2 , Mirella Altoe2, Catherine O'Connor2 , Francisco Sanchez-Vega2 , Debyani Chakravarty2, Wungki Park2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Memorial Sloan Kettering Cancer Center, New York, NY, United States Presented at the American Society of Clinical Oncology (ASCO) Annual Meeting that was held in Chicago, Illinois, United States from June 2-6, 2023.
BACKGROUND/INTRODUCTION: Mismatch repair deficiency (dMMR) results in microsatellite instability high (MSI-H) state and is the first tumor type-agnostic biomarker predictive of immune checkpoint inhibitors (ICI) response. Among gastrointestinal cancers, microsatellite instability high is most frequent in colorectal cancer (CRC 15%), gastroesophageal (GEC, 5%) and others (small bowel, hepatopancreatobiliary; 1%). For colorectal cancer, microsatellite instability high can be attributed to germline mutation (Lynch syndrome, 3%) or somatic inactivation (sporadic, 12%) of foundational MMR genes. Studies evaluating ICI efficacy in dMMR cancers focus primarily on non-Hispanic White(NHW) patients. We present prevalence, tumor genomic features, and outcomes in patients from a large cohort at Memorial Sloan Kettering (MSK).
METHODS: Retrospective analysis of MSI-H GI cancers from MSK-IMPACT database. Patients were grouped by self-reported race and ethnicity into 4 study arms: non-Hispanic White, Asian, non-Hispanic Black (NHB), and Hispanic. Age, tumor type, tumor mutation burden (TMB), and MMR genes were analyzed. Overall survival (OS) estimated with Kaplan-Meier.
RESULTS: Of 776 patients with microsatellite instability high gastrointestinal cancers, race/ethnicity: 623 (80.3%) non-Hispanic White, 60 (7.7%) Hispanic, 50 Asian (6.5%), and 43 (5.5%) non-Hispanic Black; tumor type: colorectal cancer (76%), gastroesophageal (14%), and other cancers (10%). We present initial evaluation of colorectal cancer and gastroesophageal: median age, tumor mutation burden, and most frequently altered MMR genes (MMR gene FA) are in Table 1. Median OS (mOS) in non-Hispanic White/underrepresented minorities by receipt of immune checkpoint inhibitors in microsatellite instability high colorectal cancer was 38.5m/25.3m (p=0.07) in no-immune checkpoint inhibitors group, 34.2m/28.7m (p=0.64) in +ICI group; microsatellite instability high gastroesophageal cancer was 43.4m/30m (p=0.44) in no-ICI group, 28.8m/26.7m in +ICI group.
CONCLUSION: Number of underrepresented minorities MSI-H CRC/GEC patients is 7 to 15-fold less than nonHispanic White, with no such difference in % MSI-H/MSS between groups; reflecting significant undertesting in underrepresented minorities patients. In MSI-H colorectal cancer, median age (m-Age) at sequencing was younger in underrepresented minorities compared to non-Hispanic White; pronounced in Asian and Hispanic patients, who were 10+ years younger than non-Hispanic White. No such age difference seen in GEC. No difference in mOS detected between non-Hispanic White and underrepresented minorities, however, a nonsignificant trend towards worse mOS in underrepresented minorities was observed in the no-ICI group. Next steps include validation of clinico-genomics of MSI-H GI cancers in other large cohorts, including TEMPUS (N=768) which is ongoing.
Table 1: Median age, tumor mutation burden, and most frequently altered MMR genes (MMR gene FA) in colorectal (CRC) and gastroesophageal cancers (GEC)
ABSTRACT #21
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
THROMBOEMBOLIC RISK OF CARFILZOMIB OR BORTEZOMIB IN COMBINATION WITH LENALIDOMIDE/DEXAMETHASONE FOR NEWLY-DIAGNOSED MULTIPLE MYELOMA: A COMPARATIVE META-ANALYSIS INVOLVING 2,304 PATIENTS
Bruno Almeida Costa1, Thomaz Alexandre Costa2 , Sara Diaz Saravia1 , Nicole Felix3, Carlyn Rose Tan4 , Neha Korde4, Joshua Richter5 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Federal University of Ceará, Fortaleza, Brazil; 3Federal University of Campina Grande, Campina Grande, Brazil; 4Memorial Sloan Kettering Cancer Center, New York, NY, United States; 5Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in American Journal of Hematology, 2024. PMID: 38488702
BACKGROUND/INTRODUCTION: Venous thromboembolism and arterial thromboembolism represent frequent and potentially severe complications among individuals with newly-diagnosed multiple myeloma. These adverse events can be driven by disease-related aspects, patient characteristics, and therapeutic factors. In current literature, the available evidence remains inconclusive about the differential thrombogenicity of carfilzomib/ lenalidomide/dexamethasone (KRd) and bortezomib/lenalidomide/dexamethasone (VRd). Hence, we performed a systematic review and meta-analysis aimed at comparing the thromboembolic risk associated with KRd versus VRd as frontline therapy for newly-diagnosed multiple myeloma.
METHODS: We systematically searched PubMed, Embase, and Cochrane databases from inception to July 2023 for clinical trials and observational studies that compared patients receiving either VRd induction or KRd induction for newly-diagnosed multiple myeloma. We excluded studies that (1) included patients with relapsed/refractory disease, other plasma cell dyscrasias, or non-plasma cell cancers; (2) lacked a VRd arm and/or a KRd arm; 4) did not report any outcome of interest; 5) had an overlapping population with a larger study eligible for the same analysis. The safety outcomes of interest included venous thromboembolism occurrence (defined as a diagnosis of deep venous thrombosis and/or pulmonary embolism during/after ≥1 cycles of VRd or KRd and before initiating a new therapy line) and arterial thromboembolism occurrence (defined as a diagnosis of ischemic stroke and/or myocardial infarction during/after ≥1 cycles of VRd or KRd and before initiating a new therapy line) We pooled the absolute number of events from each individual study to estimate odds ratios (ORs) and 95% confidence intervals (CIs) in binary endpoints. Due to a reasonable expectation of heterogeneity among included studies in terms of design and population characteristics, we employed a DerSimonian-Laird randomeffects model to provide a more cautious estimate of the overall effect size. RevMan v5.4.1 was used for all statistical analyses.
RESULTS: Out of 510 studies identified after deduplication, one randomized controlled trial and five retrospective cohort studies were deemed eligible (Figure 1). The comparative analysis for venous thromboembolism occurrence pooled data from 5 studies, encompassing 1,380 VRd-treated patients and 924 KRd-treated patients. Venous thromboembolism incidence in the former group (6.16%) was significantly lower than in the latter group (8.87%), with bortezomib-exposed subjects showing 47% lower odds of developing venous thromboembolism compared to carfilzomib-exposed subjects (OR, 0.53; 95%CI, 0.32-0.88; p=0.01; I2=44%; Figure 2). The comparative analysis for arterial thromboembolism occurrence pooled data from 4 studies, encompassing 1,314 VRd-treated patients and 865 KRd-treated patients. Arterial thromboembolism incidence was minimal in both treatment arms (VRd, 0.91%; KRd, 1.16%), with bortezomib-exposed subjects showing similar odds of developing arterial thromboembolism compared to carfilzomib-exposed subjects (OR, 1.01; 95%CI, 0.24-4.20; p=0.99; I2=37%; Figure 3).
CONCLUSION: Our meta-analysis suggests an increased risk of venous thromboembolism events among patients receiving KRd induction as compared to VRd induction for newly-diagnosed multiple myeloma management. Conversely, no significant difference in arterial thromboembolism risk was observed between these treatment groups.While the therapeutic arsenal for newly-diagnosed multiple myeloma continues to evolve and broaden, it remains essential to balance efficacy with safety in clinical practice, tailoring disease-directed interventions and employing prophylactic measures based on individual patient profiles as a way to pursue the best possible outcomes.


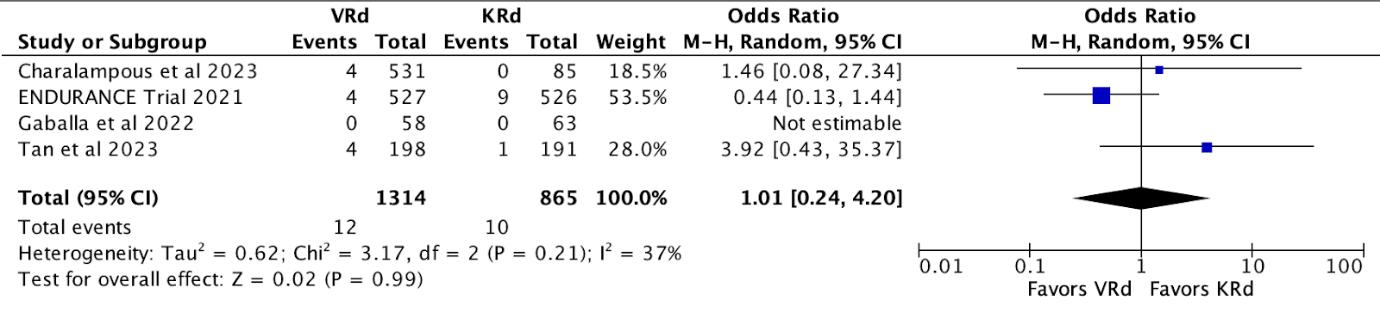 Figure 1: PRISMA flow diagram of study screening and selection.
Figure 2: Comparison of VTE rates between treatment arms.
Figure 1: PRISMA flow diagram of study screening and selection.
Figure 2: Comparison of VTE rates between treatment arms.
ABSTRACT #22
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE ENDOCRINOLOGY
HNF1A-ASSOCIATED MONOGENIC DIABETES TREATED SUCCESSFULLY WITH REPAGLINIDE MONOTHERAPY
Katherine Cuan1 and Ilana R. Bass1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Published in the American Association of Clinical Endocrinology (AACE) Clinical Case Reports, 2023. https://doi.org/10.1016/j.aace.2023.12.003
BACKGROUND/INTRODUCTION: Monogenic diabetes is a rare type of diabetes that is commonly misdiagnosed as type 1 or type 2 diabetes, which adversely impacts patient care. As the sole use of meglitinides, especially repaglinide, to treat HNF1A-associated monogenic diabetes has been rarely reported in a few other observational studies, we described our successful experience using repaglinide.
CASE PRESENTATION: A 38-year-old adopted woman with previously diagnosed type 1 diabetes, congenital deafness, chronic kidney disease, and retinopathy presented with difficulty controlling her blood glucose levels. Though initially treated with insulin, she had periods of non-compliance with insulin without experiencing diabetic ketoacidosis. While on insulin therapy, she experienced multiple episodes of hypoglycemia. Labs showed HbA1c 10.8%, c-peptide 2.7 ng/mL (1.1-4.4 ng/mL), glucose 192 mg/dL, creatinine 1.23 ng/dL, and an increased microalbumin-to-creatinine ratio (638, 0-29 mg/g). Pancreatic autoantibodies were negative. Given her congenital deafness, non-diabetic retinopathy, chronic kidney disease, preserved beta cell function and negative antibody testing, she was referred for genetic testing and was diagnosed with HNF1A-associated monogenic diabetes (c. 1340C>T (p.P447L)). She was ultimately treated with repaglinide after trials of sulfonylureas and DPP-4 inhibitors.
CONCLUSION: This case highlights the importance of correctly diagnosing monogenic diabetes and reports the successful use of repaglinide to treat HNF1A-associated monogenic diabetes. Such cases are particularly challenging given the heterogeneity in presentation and overlap with other types of diabetes.
ABSTRACT #23
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
A CASE OF SUSPECTED VIRAL ENCEPHALITIS WITH NEGATIVE CEREBROSPINAL
POLYMERASE CHAIN REACTION STUDIES
Tyler Czaniecki1 and Lance Maresky1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: HSV-1 is a common cause of viral encephalitis and a high clinical suspicion is advised due to ability to treat. HSV-1 PCR studies have a high sensitivity, but are fallible to false negative results in early testing and in the presence of RBCs.
CASE PRESENTATION: A 57-year-old female with a past medical history of cerebral palsy and superior vena cava/inferior vena cava thrombus secondary to heparin-induced thrombocytopenia presented to the emergency department for altered mental status. On arrival, patient was too somnolent to elicit a history. She was noted to be tachycardia, tachypneic, and febrile. The remaining physical exam was notable for peri-oral dried blood, inability to follow commands, but patient was withdrawing all extremities to pain. Initial lab findings revealed a WBC 16.3K/uL, lactate 2.74mmol/L, with urine toxicology, serum salicylate, and serum acetaminophen all negative. EKG showed sinus tachycardia, and both CT-head and chest X-ray were unremarkable. A CTabdomen/pelvis revealed a potential left lower lobe pulmonary consolidation. A lumbar puncture was performed notably traumatic with CSF revealing RBC 11,100/uL, total protein 103.8 mg/dL, glucose 84 mg/dL, with 84% lymphocytes; meningoencephalitis panel was negative. The patient was subsequently initiated on empiric antibiotic coverage for both community-acquired pneumonia, bacterial meningitis, and HSV encephalitis. Video EEG was concerning for underlying epilepsy with superimposed toxic-metabolic encephalopathy, although no seizures were seen. An MRI-brain was obtained and revealed edema and restricted diffusion in the left hippocampus, parahippocampal gyrus, and temporal cortex, concerning for encephalitis. CSF cultures grew S. hominis after 50 hours. Under advisement of neurology and infectious disease consultants, a repeat lumbar puncture was performed as suspicion was high for HSV encephalitis given MRI findings. Subsequent CSF findings were negative for HSV and other viral etiologies, as well as negative for autoimmune and paraneoplastic antibodies. The patient ultimately finished a course of antibiotics for communityacquired pneumonia, Staphylococcus meningitis although suspected to be a contaminate and acyclovir for a leading suspicion of HSV encephalitis given presentation and MRI brain findings. Prior to discharge, the patient had not returned to baseline cognition, however, became more alert, tracking with her eyes, but continued to be non-verbal and unable to follow commands.
CONCLUSION: HSV-1 is a common cause of viral encephalitis and a diagnostic lumbar puncture is integral to prevent delays in treatment. CSF analysis of viral encephalitis can reveal lymphocytic predominance and elevated protein, with viral PCR studies to identify causative viruses. Most laboratory HSV-1 PCR studies have a sensitivity greater than 95%, however, false negatives do occur when compared to brain biopsies with cultures. Early collection of CSF and the presence of RBCs can lead to an increase in false negative results. High clinical suspicion for HSV-1 encephalitis should remain even with a negative PCR and continued treatment with acyclovir should be considered. With regards to our case, the initial CSF was collected within 24 hours of admission and was a traumatic tap, leading to a high quantity of RBCs. Both the early testing and presence of RBCs may have contributed to a false negative HSV-1 PCR. Given the clinical presentation and MRI findings, the patient was empirically continued on acyclovir due to high suspicion for HSV-1 encephalitis. The patient ultimately underwent a second lumbar puncture, but the CSF was collected greater than 7 days after initiation of acyclovir which may have led to the second negative HSV-1 PCR. While a diagnosis was never confirmed, this case presents potential scenarios that increase the chance of false negative CSF studies. While the etiology of this patient’s encephalopathy remains unknown, here we present a case with a high clinical suspicion for HSV-1 encephalitis given presentation and imaging findings, regardless of negative HSV-1 PCR studies.
ABSTRACT #24
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES/RHEUMATOLOGY
HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS, A RARE COMPLICATION OF BABESIOSIS
Mrittika Deb1, Rebecca Pietro2, Olga Marushchak1, Chrisanna Dobrowlski1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Hemophagocytic lymphohistiocytosis (HLH) is a rare and potentially lifethreatening syndrome characterized by uninhibited immune activation and cytokine release, leading to tissue destruction and injury causing multi-organ dysfunction and failure. Early diagnosis and prompt treatment are crucial for survival, but HLH's nonspecific symptoms often pose diagnostic challenges. This case presentation highlights the importance of considering uncommon triggers like Babesiosis in HLH differential diagnosis.
HLH could be acquired genetically or could be triggered by a secondary cause like infection, immunosuppression, or autoimmune conditions. EBV is the leading cause of infectious HLH, however other infections like dengue infection were also reported as a potential trigger of HLH. Today we will present a rare case of Babesiosis leading to secondary HLH. The diagnostic criteria for HLH, determined by the HLH-2004 trial is either the confirmation of an HLH-associated genetic mutation, or the presence of five of the eight of the following features: fever ≥38.5°C, splenomegaly, peripheral blood cytopenia, hypertriglyceridemia, and/or hypofibrinogenemia, hemophagocytosis in bone marrow, spleen, lymph node, or liver, low or absent NK cell activity, ferritin >500 ng/mL, and elevated soluble CD25 (soluble IL-2 receptor alpha) two standard deviations above age-adjusted laboratory-specific norms.
CASE PRESENTATION: We present a case of a 75-year-old female with a past medical history of hypertension and chronic thoracolumbar pain who presented with cyclic fever and malaise, flank pain, and dark urine. She developed acute anemia requiring transfusions, transaminitis, and pancytopenia during the admission. Further workup revealed acute hemolytic anemia, markedly elevated ferritin, hypertriglyceridemia, oscillating fever, and elevated inflammatory markers with proteinuria, coagulopathy and liver dysfunction. Imaging was remarkable for hepatomegaly. These findings fulfilled the HLH-2004 diagnostic criteria. Infectious workup including Lyme disease, acid-fast bacillus, fungal infection, Anaplasma, Ehrlichia, and Histoplasma were negative. The patient eventually developed severe sepsis. Infectious Disease, Hematology, Rheumatology and Critical care team were on board. The patient’s blood smear later confirmed Babesiosis, establishing HLH secondary to this parasitic infection. Treatment with atovaquone and azithromycin led to a positive response with eventual resolution of parasitemia, pancytopenia, transaminitis, coagulopathy, and improvement of her symptoms.
CONCLUSION: This case underscores the importance of considering rare infectious triggers like Babesiosis in HLH diagnosis. With prompt diagnosis and specific treatment for underlying cause, even seemingly severe cases can have favorable outcomes.
ABSTRACT #25
CLINICAL RESEARCH
NEPHROLOGY
SYSTEMATIC REVIEW AND META-ANALYSIS OF PLASMA AND URINE BIOMARKERS FOR CHRONIC KIDNEY DISEASE OUTCOMES
Caroline Liu1 , Neha Debnath2, Gohar Mosoyan2, Kinsuk Chauhan2, George Vasquez-Rios2, Celine Soudant4 , Steve Menez5, Chirag R. Parikh5, Steven G. Coca3
1Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, New York, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, New York, United States; 4Memorial Sloan Kettering Cancer Center, New York, New York, United States; 5Johns Hopkins University of Medicine, Baltimore, Maryland, United States
Published in the Journal of the American Society of Nephrology, 2022. PMID: 35858701
BACKGROUND/INTRODUCTION: Sensitive and specific biomarkers are needed to provide better biologic insight into the risk of incident and progressive chronic kidney disease. However, studies have been limited by sample size and design heterogeneity.
METHODS: In this assessment of the prognostic value of preclinical plasma and urine biomarkers for chronic kidney disease outcomes, we searched Embase (Ovid), MEDLINE ALL (Ovid), and Scopus up to November 30, 2020, for studies exploring the association between baseline kidney biomarkers and chronic kidney disease outcomes (incident chronic kidney disease, chronic kidney disease progression, or incident end stage kidney disease). We used random-effects meta-analysis.
RESULTS: After screening 26,456 abstracts and 352 full-text articles, we included 129 studies in the metaanalysis for the most frequently studied plasma biomarkers (TNFR1, FGF23, TNFR2, KIM-1, suPAR, and others) and urine biomarkers (KIM-1, NGAL, and others). For the most frequently studied plasma biomarkers, pooled RRs for chronic kidney disease outcomes were 2.17 [95% confidence interval (95% CI), 1.91 to 2.47] for TNFR1 (31 studies); 1.21 (95%CI, 1.15 to 1.28) for FGF-23 (30 studies); 2.07 (95%CI, 1.82 to 2.34) for TNFR2 (23 studies); 1.51 (95%CI, 1.38 to 1.66) for KIM-1 (18 studies); and 1.42 (95%CI, 1.30 to 1.55) for suPAR (12 studies). For the most frequently studied urine biomarkers, pooled RRs were 1.10 (95%CI, 1.05 to 1.16) for KIM1 (19 studies) and 1.12 (95%CI, 1.06 to 1.19) for NGAL (19 studies).
CONCLUSION: Studies of preclinical biomarkers for chronic kidney disease outcomes have considerable heterogeneity across study cohorts and designs, limiting comparisons of prognostic performance across studies. Plasma TNFR1,FGF23, TNFR2, KIM-1, and suPAR were among the most frequently investigated in the setting of chronic kidney disease outcomes.
ABSTRACT #26
CLINICAL RESEARCH
CARDIOLOGY
CANCER AS A NEW RISK FACTOR FOR MAJOR ADVERSE CARDIOVASCULAR EVENTS IN SECONDARY PREVENTION
Renzo Melchiori1 , Sara Diaz Saravia2, Lucas Szlaien1, Pablo Rubio1, Sergio Baratta1, Alejandro Hita1, Romina Mouriño1, Manglio M. Rizzo1
1Hospital Universitario Austral, Buenos Aries, Argentina; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: The inflammatory mechanisms of cancer can be associated to the formation and progression of atherosclerosis. There is scarce evidence about the evolution of oncologic patients in secondary prevention after an acute coronary syndrome
METHODS: An observational retrospective study was done with 937 patients who underwent a percutaneous coronary intervention (PCI) for acute coronary syndrome from 2008 to 2022. Patients with a prior history or major cardiovascular events (MACE) were excluded, leaving a total of 787 patients. They were then divided into two subgroups according to the presence or absence of cancer: G1 (non-oncologic) and G2 (oncologic). The primary endpoint was a composite of MACE in secondary prevention within 3 years of STEMI.
RESULTS: G1 group consisted of 698 patients, and G2 of 89 patients. A total of 180 (22.9%) MACE were identified in the follow-up period in both groups combined, with a median follow-up time of 45 months [IQR= 1472]. The cumulative incidence of MACE for G1 was 22.2% (155/698) and 28.4% (25/88) for G2. The median follow-up time for G1 was 48 months (IQR=15-84), and for G2 was 36 months (IQR=11-48). G2 presented a density index of MACE significantly superior compared to G1 (0.78 MACE/100 patients/month 95%CI, 0.51-1.12 versus 0.48 MACE/100 patients/month 95%CI, 0.37-0.50; p=0.01). Kaplan-Meier analysis showed a significantly higher probability of MACE in G2 compared to G1 (p=0.0086). Multivariable Cox Hazard analysis showed that a history of cancer was an independent and significant predictor of MACE (HR, 1.66; 95%CI, 1.1-2.6, p=0.025) adjusted for other risk factors (hypertension, diabetes, smoking history, sedentarism, obesity, age, sex, and family history).
CONCLUSION: In our population, patients with cancer (G2) had a higher incidence of MACE during follow-up. History of cancer behaved as a significant and independent risk factor for MACE adjusted for other classical risk factors. Further studies are warranted to investigate this phenomenon.
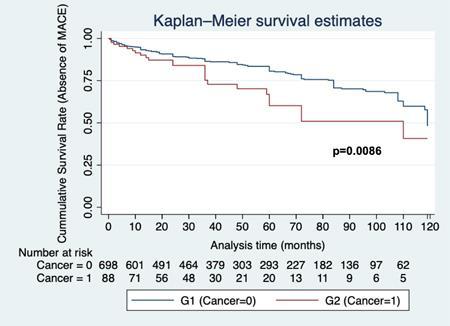
Figure 1: Kaplan-Meier analysis showed a significantly higher probability of MACE in G2 (oncologic; cancer=1) compared to G1 (non-oncologic; cancer=0).
ABSTRACT #27
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
1
Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at MountSinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Sarcoidosis is an inflammatory granulomatous condition that affects multiple organ systems. Established cardiac manifestations of sarcoidosis include tachyarrhythmias, heart failure, and conduction system abnormalities. Less well described in the literature are supraventricular arrhythmias. A previous Mount Sinai retrospective study of tachyarrhythmias in cardiac sarcoidosis patients demonstrated that atrial fibrillation was the most common arrhythmia (18%) followed by atrial tachycardias (7%), atrial flutter (5%), and other supraventricular tachycardias (2%). Understanding the mechanism of supraventricular arrhythmias is important to ameliorating disease progression.
CASE PRESENTATION: In this case, a 56-year-old man presented to Mount-Sinai Morningside Hospital with complaints of palpitations and shortness of breath and subsequently, was found to have a supraventricular tachycardia. He reported having episodes of palpitations monthly for the past year, which were exacerbated by inadequate sleep and anxiety surrounding changing medical insurers. The patient denied taking any medications the morning before the onset of symptoms and was in his usual state of health. A prior cardiac sarcoid positron emission tomography (PET) scan from 6 months prior showed a discrete foci of fluorodeoxyglucose (FDG) uptake involving the basal inferoseptal and apical septal wall as well as the anterolateral papillary muscle was consistent with cardiac sarcoidosis. The patient’s most recent transthoracic echocardiogram (TTE) showed a preserved ejection fraction (LVEF)= 55% with normal right ventricular function. He was immunosuppressed with mycophenolate acid (Myfortic®) after completing a steroids course for multisystem sarcoidosis. During the hospital admission, the patient was rate controlled with metoprolol tartrate and eventually underwent catheter ablation of the atrial foci with resolution symptoms and successfully discharged with plans for further FDG PET scans outpatient to evaluate for the progression of granulomatous inflammation within cardiac tissue.
CONCLUSION: This case displays the importance of recognizing supraventricular arrhythmias as being a significant complication in cardiac sarcoidosis. The initial presentation of dyspnea can be life threatening. Differentials for supraventricular arrhythmias in cardiac sarcoidosis should include atrial fibrillation, atrial tachycardia, and atrial ectopy. Early recognition of inflammatory changes on cardiac PET scan/MRI is critical to evaluate patients who may be predisposed to supraventricular arrhythmias. Multidisciplinary management will help to decrease morbidity associated with this cardiac sarcoid complication.
ABSTRACT #28
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
IS TIMING EVERYTHING? ASSESSING DEMOGRAPHIC AND CLINICAL FACTORS IN TIMING OF PERCUTANEOUS TRACHEOSTOMY IN MEDICAL INTENSIVE CARE UNIT PATIENTS
Keshav Dixit1, Yoshiko Ishisaka2, Shasha Chen2, Lina Miyakawa2, Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: Percutaneous tracheostomy is frequently performed in the intensive care unit for management of prolonged respiratory failure as it reduces duration of mechanical ventilation and length of intensive care unit stay, decreases sedation use, and improves patient comfort. Studies evaluating procedure timing, however, have demonstrated equivocal findings and suggest a nuanced and multifactorial decision. In this study, we aim to identify demographic and clinical factors that may impact tracheostomy timing and outcomes.
METHODS: Starting in October 2019, we performed a retrospective chart review on patients admitted to the medical intensive care units within a three-hospital health system in New York City, and who underwent percutaneous tracheostomy following a period of mechanical ventilation. Demographic, clinical, and laboratory data were recorded and analyzed.
RESULTS: Of the 139 patients included, 39 patients identified as White, 48 patients as Black, 7 patients as Asian, and 45 patients as Other. 27 patients identified as Hispanic. When assessing baseline functional status (Eastern Cooperative Oncology Group (ECOG) score), 119 patients scored 2 or less, 13 patients scored 3-4. 15 patients failed prior extubations. 20 patients had ahistory of coronary arterydisease, 9 patients had an underlying malignancy, and 14 patients were on hemodialysis. When separating the 139 patients into two groups based on number of intubation days prior to tracheostomy, the early group (<14 days mechanical ventilation) of 41 patients and late group (>14 days) of 98 patients were similar in age, Acute Physiology and Chronic Health Evaluation (APACHE) scores, and hospital/intensive care unit survival rates; there were also similar laboratory values on day of tracheostomy. Patients undergoing a delayed tracheostomy experienced a significantly longer intensive care unit stay, with no difference in hospital stay length.
CONCLUSION: Among the two groups, there were no statistically significant demographic differences. There may be an association between decreased baseline functional status and late tracheostomy, as well as prolonged intensive care unit stay. It is unclear, however, if this is due to an intrinsic patient characteristic or an extrinsic process, though a patient’s baseline debilitation may suggest a more complicated clinical course. A required multidisciplinary approach (often with input from palliative care) in caring for these patients may additionally prolong the decision-making process. Further analysis regarding long term follow-up to evaluate post-discharge outcomes (ventilator liberation, tracheostomy downsizing/decannulation) would be beneficial. Additional future research is needed to analyze whether other factors, such as palliative care involvement, socioeconomic status, optimal tracheostomy timing beyond 14 days, or other comorbidities, have overall effects on outcomes and mortality.
ABSTRACT #29
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE ALLERGY/IMMUNOLOGY/RHEUMATOLOGY
SUCCESSFUL TREATMENT OF EOSINOPHILIC GRANULOMATOSIS
Andrew Eng1 and Eugene Choo2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
BACKGROUND/INTRODUCTION: Benralizumab is not yet FDA-approved for eosinophilic granulomatosis with polyangiitis (EGPA).
CASE PRESENTATION: We present a 62-year-old female developed asthma and chronic sinusitis with nasal polyposis, both of which were severe and poorly controlled despite maximal medical therapy. She developed migratory pulmonary opacities and hypereosinophilia. This constellation of findings met the American College of Rheumatology (ACR) criteria for EGPA. She was started on benralizumab, which is not yet FDA-approved for EGPA, and was able to achieve significant improvement in both asthma and hypereosinophilia. She was a nonsmoker with past medical history significant for hypertension, hyperlipidemia, and asthma (diagnosed at the age of 56). Family history was remarkable for rheumatoid arthritis in her sister. Her asthma became poorly controlled despite aggressive inhaler pharmacotherapy, requiring multiple courses of oral corticosteroids per year. She had developed severe chronic pansinusitis with nasal polyposis which was refractory to maximal medical therapy. The patient was seen by multiple different specialists including Pulmonology, Otolaryngology, Rheumatology, and Allergy/Immunology. Initial pulmonary function testing demonstrated a mild, reversible obstructive pattern with fractional exhaled nitric oxide (FENO) elevated to 155 PPB. Absolute eosinophil count increased over several years to a peak of 2200 cells/uL (23%). Total IgE had increased over years to a peak of 1004 IU/mL. ANCA and parasite studies were negative. Serial CT-chest scans displayed numerous pulmonary nodules which changed in size, location, and surrounding ground-glass opacities over time. CT-sinus and nasal endoscopies revealed chronic pansinusitis with nasal polyposis; surgical biopsy of her polyps revealed <50 eosinophils/HPF The patient was ultimately diagnosed with EGPA due to her fulfilling four out of six ACR criteria (asthma, hypereosinophilia, paranasal sinus abnormality, and migratory/transient pulmonary nodules). Among the two ACR criteria that she did not fulfill, she never demonstrated mononeuropathy/polyneuropathy or had a biopsy containing a blood vessel with extravascular eosinophils. For asthma treatment, this patient was already on high dose ICS/LABA as well as LAMA; she had failed a prior trial of montelukast. She also received functional endoscopic sinus surgery for chronic pansinusitis with nasal polyposis, and postoperatively continued to use intranasal corticosteroids/antihistamines. Once diagnosed with EGPA, she was planned to be started on mepolizumab, as it is currently the only FDA-approved biologic for the treatment of EGPA. However, due to her insurance not being able to cover mepolizumab, she was instead started on benralizumab. Benralizumab is currently indicated for severe eosinophilic asthma, but was ultimately chosen due to insurance barrier and its powerful eosinophil-reducing effect. After starting benralizumab, the patient’s asthma symptoms dramatically improved, and FENO decreased from 155 to 72 PPB. Absolute eosinophil count dropped from 2200 to 0 cells/uL. Total IgE decreased from 1004 to 269 IU/mL. Repeat CT-chest to reevaluate pulmonary nodules is pending.
CONCLUSION: This case report demonstrates how benralizumab can be used to successfully treat patients with EGPA. Currently, mepolizumab is the only FDA-approved medication for the treatment of EGPA. However, given benralizumab’s powerful effect in depleting eosinophilia, as well as its proven efficacy in severe eosinophilic asthma, it is likely to be effective in EGPA as well (and is indeed currently undergoing clinical trials for this). In this case, benralizumab resulted in symptomatic and objective improvement in various aspects of EGPA, including asthma and hypereosinophilia.
ABSTRACT #30
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY/RHEUMATOLOGY
TEMPORAL ASSOCIATION BETWEEN BREAST CANCER AND SYSTEMIC SCLEROSIS: A CROSS-SECTIONAL ANALYSIS IN AN URBAN INSTITUTION
Jin Feng1 , Celestine He2, Hannah Verma2, Roshan Vasoya2, Daniel Qian2, Ezequiel Olumuyide2, Alicia Leong2 , Joseph Menand1, Murilo Roberto Bastos Silva1, Vincent Courant3, Sophia Lutgen1 , Chrisanna Dobrowolski3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the European Alliance of Association for Rheumatology (EULAR) Annual Meeting to be held in Vienna, Austria from June 12-15, 2024.
BACKGROUND/INTRODUCTION: Prior studies have demonstrated an increased risk of malignancy in patients with systemic sclerosis. Breast cancer is the most common subtype of malignancy observed in patients with systemic sclerosis in our cohort. The current study further investigates the association of systemic sclerosis with breast cancer, by examining the temporal relationship in incidence of these two conditions in order to elucidate a time period in which patients may be at highest risk. Given our previous study demonstrating a potential reduced incidence of malignancy in patients with systemic sclerosis utilizing mycophenolate, we also examined the association of mycophenolate use with onset of breast cancer.
METHODS: We used ICD codes to gather a retrospective cohort of patients with systemic sclerosis within a large, urban, tertiary center. Manual chart review was conducted to obtain the dates of diagnosis of breast cancer. Descriptive statistics were used to show the distribution of demographic characteristics in patients with and without a history of breast cancer. T-tests, Chi-square tests, and Fisher’s exact tests were used to study the differences in the distribution of patients’ characteristics. Patients’ timelines of breast cancer and systemic sclerosis diagnosis are presented individually. The intervals between the two diagnoses were calculated, the distribution of which is shown in a bar chart. Multivariable logistic regression analysis was conducted to study the association between breast cancer and patient characteristics. Propensity score matching was used to study the average treatment effect of mycophenolate in breast cancer. Stata, R, and Excel were used for data analysis and visualization.
RESULTS: We identified 32 (5.13%) breast cancer cases in a 625-patient cohort (81.6% female). All breast cancer patients were female. The breast cancer group was older (median age 74 versus 61, p<0.01). (Table 1) Non-mycophenolate immunosuppressant use was associated with a higher risk of breast cancer (OR, 2.36; 95%CI, 1.01, 5.52; p=0.047), in a multivariable logistic regression model adjusting for age, sex, race, health insurance, smoking, obesity, mycophenolate use, systemic sclerosis subtypes, and systemic sclerosis dates of diagnosis. Mycophenolate use was associated with reduced odds of breast cancer diagnosis. Through propensity score matching, we observed that mycophenolate use resulted in an average of 10.3% decrease in the odds of breast cancer. Of the 26 patients with complete documentation of both breast cancer and systemic sclerosis diagnosis dates, their individual timelines are presented in Figure 1. Five (19.2%) patients were diagnosed with both breast cancer and systemic sclerosis within 12 months. 13 (50%) patients were diagnosed with breast cancer within 3 years of their systemic sclerosis diagnosis. (Figure 2)
CONCLUSION: Our findings suggest a temporal association between onset of breast cancer and systemic sclerosis with most patients being diagnosed within three years of systemic sclerosis diagnosis. Prospective studies with larger cohorts are warranted to further investigate this temporal association.
Table 1: Demographic
Figure 1: The timeline of breast cancer diagnosis and systemic sclerosis (SSc) diagnosis in patients with both conditions (N = 26)
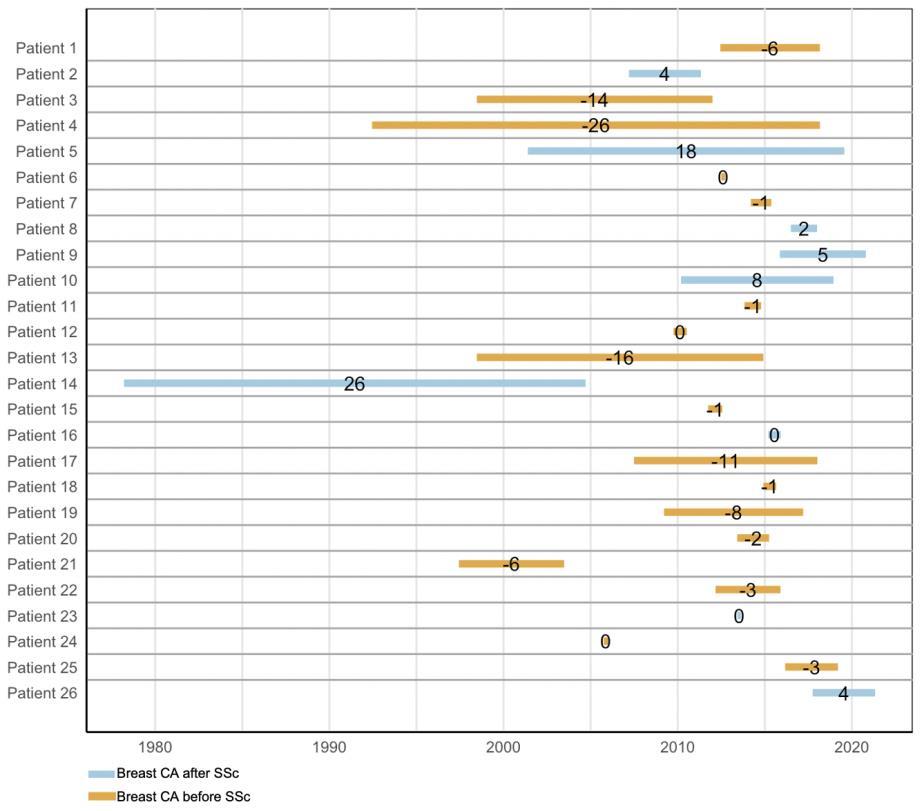
Figure 2: The distribution of patients by the interval between breast cancer diagnosis and systemic sclerosis (SSc) diagnosis (N = 26)
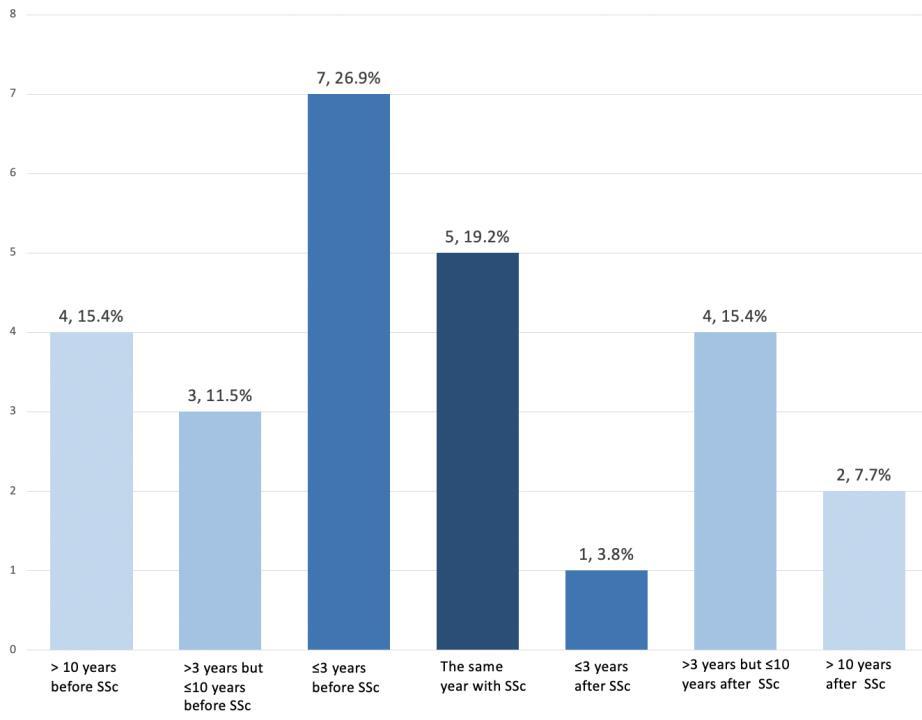
ABSTRACT #31
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
MORE THAN SKIN DEEP – SKIN MANIFESTATION OF ALK NEGATIVE LARGE CELL LYMPHOMA IN A POST-TRANSPLANT PATIENT
Debbie Marie Fermin1, Forough Hakimzada1, Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
BACKGROUND/INTRODUCTION: ALK-negative anaplastic large cell lymphoma (ALK-ALCL) is a rare subtype of CD30+ T-cell lymphoma which comprises only ∼5.5% of peripheral T-cell lymphomas. ALK-ALCL primarily impacts adults aged 40 to 65, with a 1.5:1 male-female ratio. Patients typically exhibit adenopathy and B symptoms. At diagnosis, 49% of cases involve the lymph nodes, while 20% are extra-nodal sites.
CASE PRESENTATION: A 57-year-old male with a history of end stage renal disease (ESRD) status post right kidney transplant in 2006 who was on immunosuppressive therapy presented to the hospital with three months of left leg swelling and mildly painful, round, raised, umbilicated, ulcerated skin lesions. The non-pruritic skin lesions initially started in the left inguinal area, then progressed in number and size with distal spread to the knee. He denied having fevers, chills, night sweats, or unintentional weight loss. Medications included tacrolimus, prednisone and nifedipine. He denied any recent travel, hiking, cave exploration, or animal exposure. Physical exam revealed numerous firm raised annular plaques, some with central crusting, with smooth rounded borders on the left thigh, 1 2 cm left inguinal lymphadenopathy and leg edema. Labs were remarkable for mild normocytic anemia. HIV-1 p24Ag and -1/2 antibody (4th generation HIV testing), AFB tissue culture and smear, EBV antigen and antibody, urine Histoplasma antigen, serum fungitell, galactomannan, Blastomyces antibody, and HTLV antibodies were all negative. Subsequently, patient underwent a skin biopsy, which was sent for histopathology and bacterial/fungal culture. Tissue culture revealed light growth of oxacillin-susceptible Staphylococcus aureus and coagulase negative Staphylococcus species. The patient completed a 7-day treatment course of doxycycline. Histopathologic findings were positive for CD30+ T-cell lymphoma, consistent with ALK-negative anaplastic large-cell lymphoma. Patient was referred to Oncology and was seen outpatient for staging and treatment.
CONCLUSION: This case highlights the importance of maintaining a broad differential for skin lesions, since although rare, ALK-negative anaplastic large cell lymphoma can manifest in diverse locations, including the skin. Insufficient data currently exists to establish a clear association between ALK-negative anaplastic large cell lymphoma and its occurrence in immunocompromised patients. No established optimal therapy exists for ALKnegative anaplastic large cell lymphoma due to its rarity, varied clinical presentations, and the absence of dedicated randomized trials. It often responds to doxorubicin-based chemotherapy, such as CHOP as the standard first-line treatment, however relapses are frequent. Patients with ALK-negative anaplastic large cell lymphoma have a 5-year overall survival rate of 49%. ALK-negative anaplastic large cell lymphoma typically manifests with adenopathy and B symptoms and can have extra-nodal site involvement such as the skin. There is insufficient data to establish an association between ALK-negative anaplastic large cell lymphoma and immunocompromised status. Further studies are needed to investigate for any correlation.
ABSTRACT #32
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
Thomas F. Fusillo1, Scott Millman2, Eytan M. Stein2, Varun Narendra2, Kamal Menghrajani3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Memorial Sloan Kettering Cancer Center, New York, NY, United States; 3White House Office of Science and Technology Policy, Washington, D.C., United States
BACKGROUND/INTRODUCTION: Acute myeloid leukemia (AML) is the most common form of leukemia and can present with a wide variety of signs and symptoms. A chloroma, also known as extramedullary disease and myeloid sarcoma, is a solid extramedullary tumor of neoplastic myeloid precursor cells and is a known rare sequela of AML. The incidence of extramedullary disease in AML is approximately 24%, with the lymph nodes and spleen being the most common locations and the central nervous system being one of the least common. The median overall survival in AML with extramedullary disease is 1.035 years but does differ with the cytogenetic profile.
CASE PRESENTATION: A 58-year-old woman with type II diabetes, hypertension, and refractory AML with FLT3-ITD, NPM1, DNMT3A, TET2/3, and HLA-B mutations was incidentally admitted to the hospital for euglycemic diabetic ketoacidosis due to SGLT-2 inhibitor use. She had previously undergone multiple lines of cancer therapy including 7 + 3 with midostaurin, high dose cytarabine, azacitidine and venetoclax, gilteritinib and decitabine, and a clinical trial. The patient was cytopenic on admission with a white blood cell count of 6.4 consisting of 8% blasts, an absolute neutrophil count of 0.1, hemoglobin of 8.9, and platelet count of 24. Her diabetic ketoacidosis resolved with conventional treatment. However, due to her neutropenic state she contracted multiple infections during the hospital stay including aspergillus pneumonia, bacteremia, a gluteal abscess, and cystitis. Appropriate antimicrobials and antifungals were started. Later during this admission, the patient suddenly reported blurry vision of the right eye and soon after became altered, being oriented only to person. A STAT non-contrast CT of the head was performed which showed a new mass surrounding a portion of the right optic nerve. A loading dose with continued scheduled administration of dexamethasone was given to reduce any possible mass effect on the optic nerve. Neurology was consulted and an MRI of the brain and orbits with and without contrast was performed which confirmed the mass was a chloroma and we made the diagnosis of extramedullary central-nervous system AML with mass effect on the optic nerve. The patient was transitioned to best supportive care and did not receive any further cancer directed therapies. She expired 1 week later.
CONCLUSION: This case illustrates the potential for extramedullary AML cells forming a solid tumor, known as a chloroma. Additionally, it emphasizes the severity and potential emergency of a chloroma in the central nervous system. There is debate over the modality required to diagnose extramedullary disease, with some recommending pathological examination. However, in scenarios where this is not feasible, such as surrounding the optic nerve, imaging can be sufficient. The same chemotherapy regimen is usually used, based on genetic and molecular markers, whether or not there is extramedullary disease present. The only exception is that extramedullary disease can warrant consideration of radiation therapy. Although overall prognosis of extramedullary AML is poor, there are recommendations on how to approach management and treatment.
ABSTRACT #33
CLINICAL RESEARCH
CARDIOLOGY
PERCUTANEOUS CORONARY INTERVENTION VERSUS OPTIMAL MEDICAL THERAPY FOR CHRONIC TOTAL OCCLUSION
Kruti Gandhi1 , Errol Moras1 , Ameesh Isath2, Ashish Correa1, Kiran Mahmood1 , Abel Casso Dominguez1 , Jacqueline Tamis-Holland3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2New York Medical College, New York, NY, United States; 3Cleveland Clinic, Cleveland, OH, United States Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
BACKGROUND/INTRODUCTION: The prevalence of coronary chronic total occlusion (CTO) varies widely from 18-52% in patients with stable ischemic heart disease. Despite recent advances in operator techniques and improving operator experience, percutaneous coronary intervention (PCI) for CTO still poses a major challenge. While several observational studies have demonstrated superior outcomes for CTO-PCI, the overall benefit of CTO intervention remains controversial. We aimed to compare the clinical endpoints and health status outcomes in all randomized controlled trials (RCT's) to evaluate safety and efficacy of PCI as compared to optimal medical therapy.
METHODS: We queried PubMed/MEDLINE, Cochrane Library and EMBASE for RCT’s that compared CTOPCI with optimal medical therapy. The primary endpoint was all-cause mortality. Secondary outcomes included cardiac mortality, major adverse cardiac and cerebrovascular events (MACCE), myocardial infarction (MI), target vessel revascularization (TLR), stent thrombosis, left ventricle ejection fraction (LVEF) changes and health status outcomes. Risk ratios (RR’s) and their corresponding 95% confidence intervals (CIs) were calculated using the random-effects model.
RESULTS: We included a total of 6 RCT’s (1890 total patients, mean age 61.8 ± 3.6 years, and 84.6% male) Follow-up ranged from 4 to 48 months. All-cause mortality and cardiac mortality were comparable between CTOPCI and optimal medical therapy groups (RR, 0.83; 95%CI, 0.47–1.48; p=0.53 and RR, 0.98; 95%CI, 0.24–4.07; p=0.98, respectively). There was no significant difference between percutaneous coronary intervention or medical therapy with regards to major adverse cardiac and cerebrovascular events (RR, 0.85; 95%CI, 0.50–1.45; p=0.55) and target vessel revascularization at follow-up (RR, 0.50; 95%CI, 0.24–1.06; p=0.07). Moreover, the risk for myocardial infarction (RR, 1.36; 95%CI, 0.91–2.-2; p=0.13), stent thrombosis (RR, 1.74; 95%CI, 0.36–8.40; p=0.49), and stroke at follow-up (RR, 0.57; 95%CI, 0.24–1.38; p=0.21) was comparable between the two groups. Health status outcomes such as angina frequency (RR, 4.05; 95%CI, –1.95–10.05; p=0.19), physical limitations (RR, 3.83; 95%CI, –0.75 – 8.41; p=0.10), quality of life (RR, 6.25; 95%CI, –1.54–14.03; p=0.12), and treatment satisfaction (RR, 2.60; 95%CI, –1.15 –6.35; p=0.17), were comparable between the two groups.
CONCLUSION: Pooled data from RCT does not support an advantage to coronary chronic total occlusion percutaneous coronary intervention in terms of a reduction in cardiovascular events or improved quality of life. Further adequately powered and long-term trials are required to identify the best management strategy for patients with coronary chronic total occlusion
ABSTRACT #34
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY/PALLIATIVE CARE
ASSESSING THE UTILIZATION OF PALLIATIVE CARE SERVICES IN THE MANAGEMENT OF PATIENTS WITH METASTATIC PANCREATIC ADENOCARCINOMA
Sonal Gandhi1, Drew Moss1, Richard Sheppard2, Ibrahim Omore2, Linda Wu3, Deirdre Cohen2, Cardinale B. Smith2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Columbia University Irving Medical Center, New York, New York, United States
Presented at the American Society of Clinical Oncology (ASCO) Quality Care Symposium that was held in Boston, Massachusetts, United States from October 27-28, 2023
BACKGROUND/INTRODUCTION: Pancreatic cancer is known to be associated with poor survival outcomes and high symptom burden. Integration of early palliative care has been associated with improved end of life care, including reduced hospitalizations and emergency room visits. We conducted a retrospective study to determine the utilization rates of specialist palliative care in patients diagnosed with metastatic pancreatic cancer at an academic teaching hospital and summarize the impact on end-of-life care.
METHODS: A database of patients diagnosed with metastatic pancreatic cancer on index presentation from 2011 and 2022 was analyzed for utilization of specialist palliative care. Patients who transitioned cancer care to other centers and those who were lost to follow-up were excluded. Data on patient demographics, treatment course, and end-of-life care were collected, and descriptive statistics were used to summarize the data.
RESULTS: In our study, 168 patients met the inclusion criteria. The average age of diagnosis was 66 years with a diverse ethnic composition, including White (35.7%), African American (26.8%), and Hispanic (15.5%) patients. Among the cohort, 126 out of 168 patients received palliative care, with 79 of them initially being seen during hospitalizations and 47 patients receiving outpatient palliative care. The median duration between pancreatic cancer diagnosis and first encounter with palliative care was 145 days. No significant differences were found in terms of age, race, sex, or ethnicity between patients who received palliative care and those who did not. The median time from consultation to death was 57 days and most patients (71.8%) received palliative care within one month of their death. Patients who received specialist palliative care were more likely to have a DNR code status (83.3% versus 44.5%, p<0.0001) and more likely to be referred to hospice (83.9% versus 35.9%, p<0.0001).
CONCLUSION: Early involvement of specialist palliative care in management of patients with metastatic pancreatic cancer may lead to optimization of health care services with earlier hospice referrals and comfort directed care at the end of life. Further research is warranted to explore the impact of palliative care on patient outcomes, quality of life, and the potential benefits of aligning treatment decisions with patients' end-of-life preferences.
ABSTRACT #35
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/GENERAL INTERNAL MEDICINE
Martin Emmanuel Garcia1, Debbie Marie Fermin1, Sanaa Zafar1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Scurvy is an ancient disease that was thought to be rare in the modern era. Recent data however have shown that scurvy can be as common as 7.1% in the United States and this can be more common in patients with psychiatric illness.
CASE PRESENTATION: A 57-year-old female with a history of schizophrenia presented to the emergency department with multiple complaints including generalized weakness, chest pain, nausea, and bright red blood per rectum that have been progressing over several weeks. She also claimed that her diet consisted mostly of bran and low-fat milk. She was disheveled on exam and had tangential thoughts on interview. Skin exam with multiple hematomas on the left side of the face and neck, and the left shin. Petechiae were present on bilateral legs. Gums were edematous and erythematous and with poor dentition. Heart, lung, and abdominal exams were normal. +1 bilateral peripheral edema was present up to the knees. No blood on digital rectal exam was noted upon rectal exam. Labs on the first day were significant for microcytic anemia of 7.5 mg/dl, INR 2.3, and negative troponin. EKG with normal sinus rhythm. Urine toxicology negative for any illicit substances. Iron found to be low. Vitamin levels were obtained: vitamin C: <0.1, B1, B12, MMA, and copper normal, The next day, hemoglobin down trended to 6.9 mg/dl necessitating transfusion with 1 pRBC. She was started on intravenous pantoprazole twice daily, multivitamins, vitamin C 1 gram for 3 days, and vitamin K for 3 days. She underwent endoscopy and colonoscopy with significant findings of erythematous mucosa in the stomach and a non-bleeding ulcer in the duodenum and scattered mucosal lesions in the colon suggestive of scurvy and a non-bleeding hemorrhoid. She was discharged with the instruction to continue multivitamins, oral pantoprazole daily, and oral iron every other day. She followed up after 2 months outpatient with Gastroenterology where her hemoglobin was at 12.7 mg/dl and had no recurrence of GI bleed.
CONCLUSION: Scurvy can be more common in patients with psychiatric illness, including schizophrenia. The poor dietary habits observed in individuals with schizophrenia are believed to stem from the dysregulation of the reward circuitry. This dysregulation is thought to be influenced by heightened dopamine activity in the mesolimbic pathway and in brain regions responsible for cognitive control. Clinical manifestations of scurvy include anemia, petechiae, gum disease, and poor wound healing. In advanced stages, the severity of symptoms escalates, posing life-threatening risks. Common manifestations during this late phase include widespread edema, jaundice, hemolysis, and instances of spontaneous and acute bleeding. Gastrointestinal bleeding in the form of melena and hematochezia have been reported due to friability of the gastrointestinal mucosa. Recommended management is 1 to 2 grams of vitamin C daily for the initial 2 to 3 days, followed by a 500 mg per day for the subsequent week and finally a maintenance phase with a daily intake of 100 mg of vitamin C for a period lasting 1 to 3 months.
ABSTRACT #36
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY/PULMONARY/CRITICAL CARE
PROGRESSION OF ACUTE HEART FAILURE RELATED TO TAKOTSUBO CARDIOMYOPATHY IN A YOUNG ANOREXIC FEMALE PATIENT
Justin Goodfarb1, Mohammad Ishrak Khan1 , Samantha Shetty1, Jaskirat K. Gill1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Takotsubo cardiomyopathy, a rare type of non-ischemic cardiomyopathy characterized by left ventricular dysfunction, can lead to severe complications like cardiogenic shock and acute heart failure despite being relatively uncommon. Its exact cause is not fully understood but is believed to involve various factors such as physical or emotional stress, hormonal imbalances, and inflammation. Excessive release of catecholamines plays a central role in its development, along with issues like impaired blood flow, electrolyte derangements, and inflammation in the heart muscle. Understanding these mechanisms is crucial for improving diagnostic and treatment approaches. Here, we describe a case of a 25-year-old woman with a history of anorexia nervosa who rapidly developed severe heart failure due to Takotsubo cardiomyopathy, ultimately leading to her death despite invasive interventions including mechanical circulatory support.
CASE PRESENTATION: A 25-year-old female with a history of anorexia nervosa was brought to the hospital by Emergency Medical Services after being found in a severely debilitated state. Upon arrival at the emergency department, she was noted to be hypotensive, bradycardic, emaciated (BMI of 10), with marked electrolyte imbalances, and coincidentally tested positive for COVID-19. Given her critical condition, the patient was promptly admitted to the medical intensive care unit (MICU).
In the MICU, she received aggressive fluid resuscitation, electrolyte repletion, and underwent an extensive infectious work-up. Initial laboratory findings revealed severe hypokalemia (K 2.0), hypomagnesemia (Mg 1.4), and anemia (Hgb 6.8). An ECG upon arrival in the MICU did not display any ischemic changes. While she had been empirically started on broad spectrum antibiotics, blood cultures eventually yielded gram-negative bacilli, later identified as Klebsiella oxytoca. A transthoracic echocardiogram (TTE) obtained early in her course demonstrated left ventricular ejection fraction (LVEF) of 65%, normal right ventricular function, no valvular disease.
While at first the patient did not exhibit any respiratory distress, she subsequently deteriorated and quickly progressed from non-invasive ventilatory support to requiring mechanical ventilation. Despite adherence to ARDSnet guidelines for ventilator management, the patient continued to become hypoxic. Concomitantly, she became progressively more tachycardic and hypotensive, requiring high doses of pressor support. Her clinical picture and labs were concerning for cardiogenic shock at this point, given her rising troponin and lactate. Cardiology was consulted, and a repeat TTE showed a diffusely hypokinetic LV with an acute drop in LVEF to 5-10%. A moderate sized pericardial effusion was also noted with diastolic collapse of the RV suggestive of cardiac tamponade. The patient was started on inotropes and transferred to the cardiac intensive care unit.
A multidisciplinary team, including Cardiology, Cardiothoracic Surgery, and Critical Care, was convened and a decision was made to take the patient to the cardiac catheterization lab to insert a Swan-Ganz catheter for ongoing hemodynamic monitoring, reappraisal of pericardial effusion, and pelvic angiography to determine the eligibility of peripheral veno-arterial extracorporeal membrane oxygenation (VA-ECMO). As suspected, the patient’s vessel size was too small and cannulation with adult ECMO cannulas was not a viable option. The patient’s LV dysfunction was thought to be reversible, and she was taken urgently to the operating room for initiation of central mechanical circulatory support. A median sternotomy was performed, and upon entry into the pericardium, a straw-colored effusion was encountered surrounding a virtually akinetic LV. A CentriMag left ventricular assistance device (LVAD) was placed, and the patient was admitted to the cardiothoracic intensive
care unit (CTICU). Unfortunately, in the subsequent days while the LVAD optimally offloaded the LV, the patient started to develop progressive RV dysfunction. The patient’s clinical status continued to deteriorate despite mechanical circulatory support of the LV and pharmacologic support of the RV. Her clinical condition continued to worsen, and she ultimately progressed to cardiac arrest.
CONCLUSION: In this case report, we present a compelling case of a young female with a history of anorexia nervosa, who experienced a severe and complex clinical course. Her condition was characterized by a florid progression of acute heart failure secondary to Takotsubo cardiomyopathy, compounded by septic shock with Klebsiella bacteremia, concurrent COVID-19 infection, and multiple electrolyte abnormalities. The patient's clinical course rapidly deteriorated, leading to cardiogenic shock and necessitating the implementation of advanced mechanical circulatory support with an LVAD. This case underscores the need for heightened awareness and vigilance in diagnosing and managing Takotsubo cardiomyopathy, particularly in patients with predisposing factors such as eating disorders. Additionally, it highlights the challenges encountered in delivering advanced therapies in cases where conventional interventions may be contraindicated or insufficient. Further research is warranted to halt the rapid clinical deterioration and to enhanceour understanding of pathophysiology and optimal management strategies for this complex condition.
ABSTRACT #37
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PULMONARY/CRITICAL CARE
STATUS ASTHMATICUS COMPLICATED BY RHABDOMYOLYSIS
Satwant Grewal1, Tal Shachi1,2, Pavan Paka3, Sara Luby1, Arpanjeet Kaur1, Patrick Tobin-Schnittger1 , Vincent Courant1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Columbia University Vagelos College of Physicians and Surgeons, New York, NY, United States Presented at the CHEST Annual Meeting that was held in Nashville, Tennessee, United States from October 16-19, 2022.
BACKGROUND/INTRODUCTION: Rhabdomyolysis in the setting of status asthmaticus is a rare but potentially fatal complication. The hallmark of rhabdomyolysis is an elevation in serum creatine phosphokinase (CPK) secondary to muscle necrosis, which may be categorized as: traumatic, nontraumatic exertional, and nontraumatic non-exertional. We report a case of a rhabdomyolysis in the setting of status asthmaticus, neuromuscular blockade, and steroid use.
CASE PRESENTATION: A 21-year-old male with a history of asthma presented with respiratory distress, tachypnea, and tachycardia. Physical exam revealed diffuse bilateral wheezing and accessory muscle use. Arterial blood gas revealed a pH of 7.11 and a PCO2 of 101.9 mmHg. Despite treatment with multiple nebulizers, systemic steroids, magnesium, and intramuscular epinephrine, he required tracheal intubation for acute hypercarbic respiratory failure due to status asthmaticus. He was sedated with fentanyl and midazolam. Due to ventilator dyssynchrony, continuous neuromuscular blockade with cisatracurium was initiated. High dose methylprednisolone and continuous albuterol nebulization was initiated in the intensive care unit. On day 3 of admission, the patient was found to have a CPK level of 20,123 U/L suggestive of rhabdomyolysis. There was no evidence of trauma or compartment syndrome. Due to concern for medication induced rhabdomyolysis, cisatracurium was discontinued and methylprednisolone was rapidly tapered, and CPK levels subsequently decreased after peaking at 20,253 U/L. Intravenous fluids were continued to maintain hydration. He continued to clinically improve and was successfully extubated on the 10th day of admission and eventually discharged with Pulmonary follow-up.
CONCLUSION: Rhabdomyolysis in the setting of status asthmaticus has several possible etiologies. Status asthmaticus leading to hypercapnia results in a respiratory acidosis while also preventing carbon dioxide and oxygen exchange within muscle tissue causing muscular hypoxia and necrosis. This may be further complicated by increased exertion of the respiratory muscles. Rhabdomyolysis resulting from the combination of corticosteroids and neuromuscular blocking agents is rare. Although steroid use may lead to glucocorticoid myopathy, it is uncommon to have elevations in CPK. However, when steroids are used concomitantly with neuromuscular blocking agents, patients are at increased risk of developing critical illness myopathy with elevations in CPK. The patient's subsequent decline in CPK after cisatracurium was discontinued and systemic steroids were significantly reduced leads us to believe that the combination of these medications was the likely precipitant to this patient's rhabdomyolysis. Our case highlights the importance of recognizing the development of rhabdomyolysis in patients presenting with status asthmaticus, especially when receiving a combination of neuromuscular blockade and high dose systemic steroids.
ABSTRACT #38
CLINICAL RESEARCH
CARDIOLOGY
NATIONWIDE ANALYSIS OF THE RISK OF MYOCARDIAL INFARCTION IN PATIENTS WITH ATRIAL FIBRILLATION: A RETROSPECTIVE OBSERVATIONAL STUDY
Soumya Gupta1, James Choi1, Kristen Carter1, Sara Diaz Saravia1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Apart from thromboembolism, atrial fibrillation is marked by a cluster of atherosclerotic risk factors, contributing to its complex clinical course. Atherosclerosis in coronary arteries, leading to acute coronary syndrome, can also be seen in patients with atrial fibrillation. Our study aims to evaluate if patients with atrial fibrillation are at a higher risk of acute myocardial infarction and also adjust for standard modifiable cardiovascular disease risk factors.
METHODS: A retrospective cross-sectional observational study on 21,348,997 patients with atrial fibrillation and 85,395,960 patients without atrial fibrillation was conducted using data from the Nationwide Inpatient Sample (NIS) files between January 2017 and December 2019. Statistical analyses utilized STATA logistic regression models for OR (Odds Ratio) and 95% CI estimation (p<0.05). Outcomes (acute myocardial infarction, death, cardiac arrest) in standard modifiable cardiovascular disease risk factors-less patients were compared to standard modifiable cardiovascular disease risk factors-positive patients.
RESULTS: Among 21,348,997 patients with atrial fibrillation, 3,478,360 patients developed acute myocardial infarction and the odds of acute myocardial infarction in these patients with atrial fibrillation was 1.2 times greater than the odds of acute myocardial infarction in patients without atrial fibrillation (95%CI, 1.26–1.28; p<0.0001). We also saw that the odds of death among standard modifiable cardiovascular disease risk factors negative atrial fibrillation patients was 1.19 times the odds of death in standard modifiable cardiovascular disease risk factors negative patients without atrial fibrillation.
CONCLUSION: Our finding suggests that atrial fibrillation is associated with a higher risk of acute myocardial infarction regardless of the presence of cardiovascular risk factors suggesting that it could also be secondary to thromboembolism. This finding opens doors for discussion regarding early screening for acute coronary syndrome among patients with atrial fibrillation
ABSTRACT #39
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
CARDIAC SARCOIDOSIS WITH PREDOMINANT RIGHT VENTRICLE INVOLVEMENT
Hannah Hart1, Devika Aggarwal1, Soumya Gupta1, Vikram Agarwal1, Isha Ranadive1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Cardiac sarcoidosis can have a variable clinical presentation. We present a case of cardiac sarcoidosis with rare predominant right ventricle (RV) involvement.
CASE PRESENTATION: A 31-year-old male with reported cutaneous sarcoidosis presented to the emergency department for shortness of breath. Vitals were stable except for bradycardia. Electrocardiogram showed complete heart block with junctional escape at 52 bpm. Chest X-ray showed bilateral patchy opacities in the upper lobes. Transthoracic echo demonstrated a normal left ventricle (LV) size and function (EF 55%) with RV dilation and hypokinesis.
Despite the lack of LV involvement on echocardiogram, the leading diagnosis was still cardiac sarcoidosis given the history of extracardiac sarcoidosis. We proceeded with cardiac MRI (CMR) to aid in the diagnosis and help decide between placement of a pacemaker versus defibrillator. CMR showed normal LV systolic function with severe RV dilatation and dysfunction. There was significant transmural late gadolinium enhancement (LGE) of the RV inferior and lateral wall. Additionally, mild subepicardial LGE with edema of the LV basal to mid inferoseptal wall was noted. Due to the presence of significant LGE, an implantable cardioverter defibrillator (ICD) was placed. The patient was started on oral steroids and outpatient PET was planned.
CONCLUSION: This case highlights the importance of cardiac MRI in patients with cardiac sarcoidosis, especially with isolated/ predominant RV involvement, for not only diagnosis but also guiding the management.
ABSTRACT #40
QUALITY IMPROVEMENT
GASTROENTEROLOGY
INCREASING COLORECTAL CANCER SCREENING RATES AMONG PATIENTS AT A FEDERALLY QUALIFIED HEALTH CENTER
Marni Wilkoff1 , Allison E. Wang1 , Alexandria Markley1 , Swati Patel1 , Rama Hussein1 , Nicholas Piniella2 , Kevin Yan3 , Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Institute of Technology College of Osteopathic Medicine, Old Westbury, New York, NY, United States;
3Ryan Chelsea-Clinton Health Center, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
BACKGROUND/INTRODUCTION: Colorectal cancer (CRC) screening rates remain low in vulnerable populations. In 2022, our New York City (NYC) Federal Qualified Health Center (FQHC)’s CRC screening rate was 35.9% - far below the 2020 national average of 69.7% and 40.1% in all FQHCs. More progress must be made to increase CRC screening in these historically underserved populations. In an attempt to raise CRC screening rates in our NYC FQHC, this quality improvement project focused on updating providers on screening guidelines and increasing patient understanding of screening options.
METHODS: Internal Medicine resident in-person visits for patients 45–75 years old between 8/14/2022 to 11/14/2023 at this single NYC FQHC were included. Demographic, social, and medical data were obtained. Exclusion criteria included patients with self-reported, unverified colon cancer screening and those who did not meet criteria for average risk CRC screening. Interventions to increase screening rates included a preintervention quiz, educational lectures with a follow-up knowledge assessment for residents, informational posters in patient rooms, daily pre-clinic resident reminders, and 2-minute educational videos for patients on appropriate stool test collection. We examined residents’ compliance with appropriate CRC screening guidelines and differences in average risk CRC screening rates pre- (8/14/2022-8/13/2023) and post-intervention (8/14/2023-11/14/2023).
RESULTS: Pre-intervention, 19% of patients were up to date on CRC screening, which increased to 25% in the 3-month post-intervention phase. Overall, there was a 3% increase in the screening test order rate (p=0.28). Vulnerable populations who had higher rates of screening tests ordered post-intervention included patients of Hispanic ethnicity (23% versus 14%, p=0.04), uninsured (24% versus 16%, p=0.28) and undomiciled (28% versus 16%, p=0.19). More colonoscopies were ordered post-intervention (56% versus 39%) compared to stool tests (44% versus 61%, p=0.03). Median time for stool test return improved from 18 days (IQR 37.8) to 4 days (IQR 7) post-intervention (p=0.06). Over 90% of residents reported feeling confident with CRC screening guidelines post-intervention, but their knowledge assessment demonstrated lack of understanding screening guidelines.
CONCLUSION: After an intervention to increase knowledge about CRC screening among physicians and patients, the overall rates of ordering appropriate screening tests increased, particularly in vulnerable, historically under-screened populations. In the post-intervention phase, colonoscopy was more likely to be ordered as the method of screening, possibly due to increased patient education. Test completion rates remained low but are anticipated to increase over time as this is an ongoing study. Continued low rates of screening highlight the importance of ongoing education at both provider and patient levels.
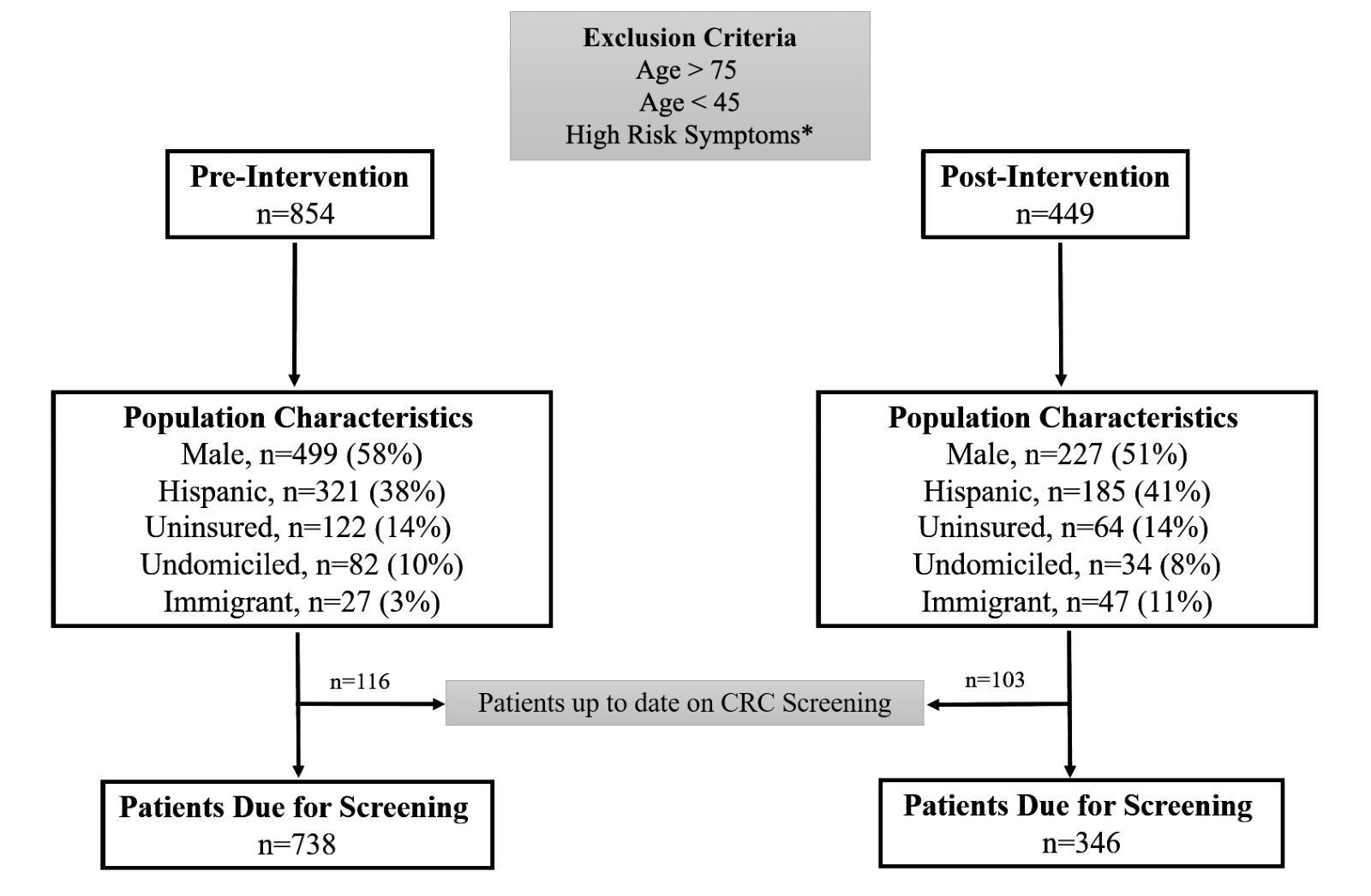
*Weight loss, rectal bleeding, altered bowel habits, personal or family history of CRC or advanced adenoma
Table 1: Changes in Average Risk CRC Screening Rates After Intervention Screening Test Characteristics – no. (%)
Hispanic Ethnicity
Undomiciled
Table 2: Resident Performance on Pre- and Post-Knowledge Assessment
CRC Screening Metrics – no. (%)
Knowledge Assessment Questions – no. (%)
(n=41, n=14)
ABSTRACT #41
CLINICAL RESEARCH
CARDIOLOGY
ECHOCARDIOGRAPHIC HEMODYNAMIC ASSESSMENT IN PATIENTS UNDERGOING AORTIC BALLOON VALVULOPLASTY
Joseph E. Karpenos1, Marija Petrovic1, Juan Arango Morales1, Joseph Elias1, Hannah Hart1, Samantha Shetty1 , Soumya Gupta1, James Choi1, Sara Diaz Saravia1, Kristen Carter1, Nnedindu Asogwa2, Eyadeh Mdanat3 , Ga Hee Kim1, Robert Leber1, Alaa M Omar1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Staten Island University Hospital, Staten Island, NY, United States; 3Cayuga Medical Center, Ithaca, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: We studied the anatomical and hemodynamic impact of balloon aortic valvuloplasty (BAV) using echocardiography in patients undergoing transcatheter aortic valve replacement (TAVR) or not.
METHODS: Retrospectively 22 patients referred for BAV were included [84 ± 7 years, 63% women, ejection fraction (EF): 55 ± 15%; EF≥50% in 16 patients]. Echocardiography was done at 3 time points: baseline, immediately after BAV, and either after TAVR or during follow-up if TAVR was not performed.
RESULTS: BAV indications were: 2 urgent non-cardiac surgery, 7 cardiogenic shock, 1 for palliation, and 13 bridged to TAVR. At baseline, the aortic valve area (AVA) was 0.7 ± 0.1 cm2, mean transaortic pressure gradient (PG) was 41 ± 11 mmHg, stroke volume index (SVi) was 33 ± 10 ml/m2, transvalvular flow rate (FR) was 197 ± 44 ml/s, and transvalvular resistance (TVR) was 118 ± 41 dyn.s.cm-5. Immediately after BAV, AVA significantly increased (0.9 ± 0.2 cm2 , p=0.002) and PG decreased (32 ± 8.7 mmHg, p=0.019), indicating favorable anatomic outcomes. Interestingly, SVi (36 ± 13, p=0.372), FR (209 ± 60 ml/s, p=0.112), and TVR (95 ± 49 dyn.s.cm-5, p=0.112) did not change immediately after BAV (Figure 1). During follow-up, TAVR patients exhibited near normalization of all valvular profiles, while non-TAVR did not show significant changes compared to post-BAV (Figure 1). After a median follow-up of 28 months, 7 patients died, 9 had cardiac hospitalizations, 2 had strokes, and 3 had acute coronary syndromes. As expected, TAVR had a significantly lower incidence of non-fatal composite outcomes compared to non-TAVR (1 versus 9, p=0.007).
CONCLUSION: Our findings indicate that BAV did not lead to substantial hemodynamic improvement in terms of transvalvular flow, flow rate, or valvular resistance, which appeared to improve only with TAVR. The modest anatomical effect of BAV did not seem to justify the high clinical risk associated with the procedure.
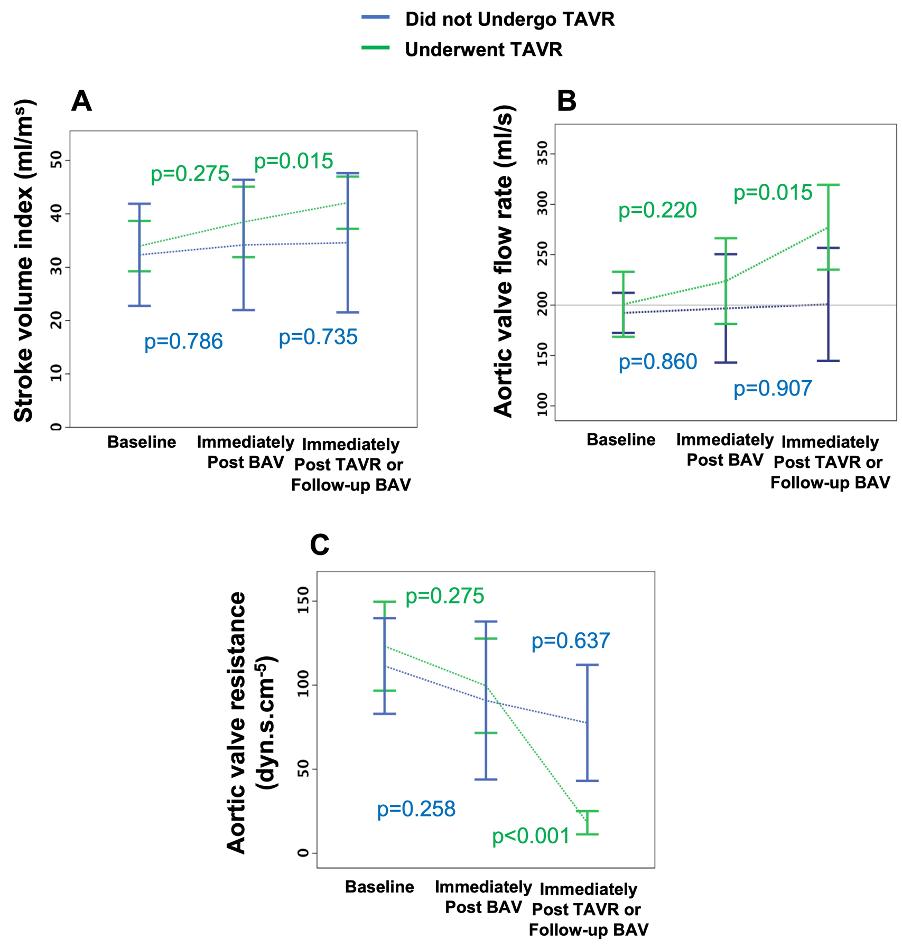
ABSTRACT #42
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
IN-STENT THROMBOSIS THRICE IN 30 DAYS
Luka Katic1 , Hammad Sheikh1, Alexander Silverman1, Ankita Gore1, Nitin Barman1, Amir Ahmadi1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Mount Sinai Fuster Heart Hospital Research Symposium that will be held in New York, New York, United States on March 15, 2023.
BACKGROUND/INTRODUCTION: In-stent thrombosis poses a multifaceted clinical challenge despite maximal antiplatelet therapy. Here we present a case of three episodes of in-stent thrombosis of the same stent within 30 days.
CASE PRESENTATION: A 80-year-old male with a complex cardiac history, including a three-vessel CABG and five percutaneous transluminal coronary angioplasties (PTCA) with stent placements, the most recent being a drug-eluting stent (DES) expanded over a previously stented and newly thrombosed distal left circumflex artery (dLCx) two days prior, presented with acute midsternal chest pain radiating to his left arm with ST depressions in leads V1-V4 in the setting of non-compliance with clopidogrel despite compliance with aspirin. Urgent left heart catheterization (LHC) showed total occlusion of the two-layered dLCx stent, concerning for stent under expansion, resolved via PTCA with atherotomy, intravascular lithotripsy, and thrombectomy with establishment of TIMI III flow. No additional stent was placed, and though consideration was given to starting triple therapy, the patient was started on aspirin and ticagrelor. 48 hours later the patient suffered a sudden episode of orthostatic hypotension and syncope with new EKG changes showing posterolateral STEMI. Urgent LHC revealed a second IST of the distal LCx, resolved again via PTCA with atherotomy and resultant TIMI III flow. No additional stent was placed once again. Following a brief cangrelor infusion post-procedure the patient was continued on aspirin and ticagrelor and discharged. P2Y12 Platelet reactivity assay drawn prior to discharge was low. Five days later, the patient was hospitalized due to dyspnea and during the subsequent admission suffered an episode of chest pain requiring a third urgent LHC showing another IST of the twice stented dLCx that was resolved via PTCA with Excimer laser atherectomy restoring TIMI III flow, a third DES was expanded within the distal LCx via IVUS guidance with still reduced minimal stent area, though improved from prior 2-layer stenting. The patient was placed on triple therapy with aspirin, ticagrelor, and rivaroxaban 2.5 mg twice daily, hypercoagulable workup during admission returned negative, and the patient was safely discharged home chest pain free thereafter and on follow up.
DISCUSSION/CONCLUSION: In-stent thrombosis is an adverse clinical event significantly less common of late due to advances in stent design, pharmacotherapy, and procedural techniques such as intravascular ultrasound guidance. We suspect three possible etiologies of in-stent thrombosis in this patient. First, the previous DES in the dLCx was under expanded due to the anatomy of the native LCx and/or malposition due to lack of intravascular ultrasound guidance. Second, episodic orthostasis may have produced transient stasis of blood within the LCx due to decreased coronary perfusion pressure. Third, an unknown thrombophilia or resistance to antiplatelet agents may have been present. This case highlights the critical role of intravascular ultrasound in ensuring ideal DES expansion and placement, preventing in-stent thrombosis and mitigating significant myocardial damage, and the crucial role of rapid clinical judgement and intervention.
A. ECG at presentation - ST depressions in leads V1-V4

B. ECG during witnessed stent thrombosis episode - ST elevation in leads V5 and V6, along with a new left bundle branch block (LBBB)
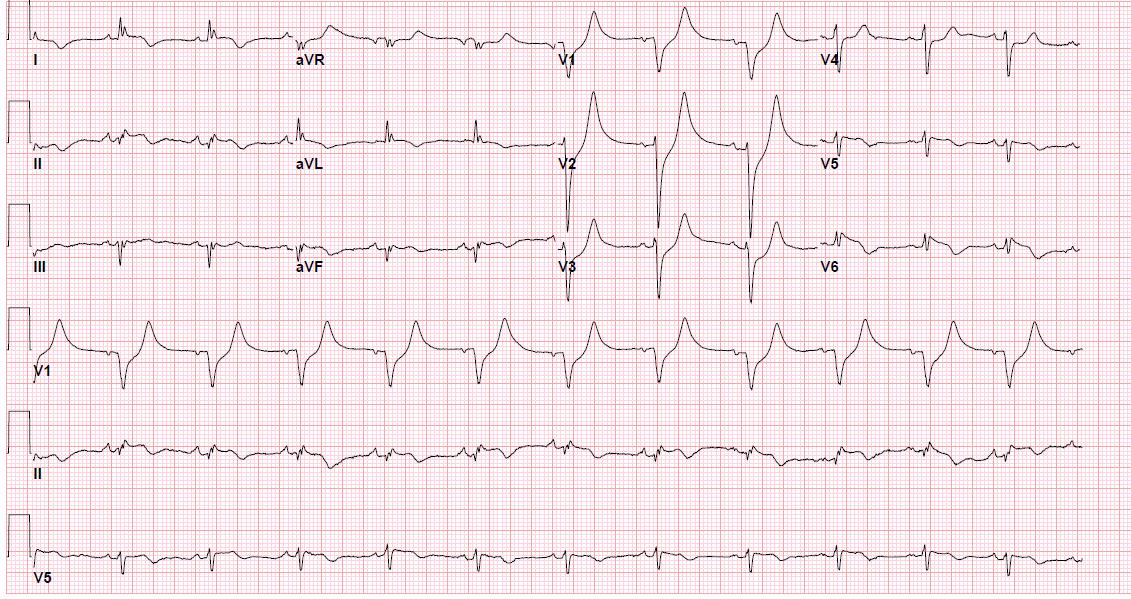
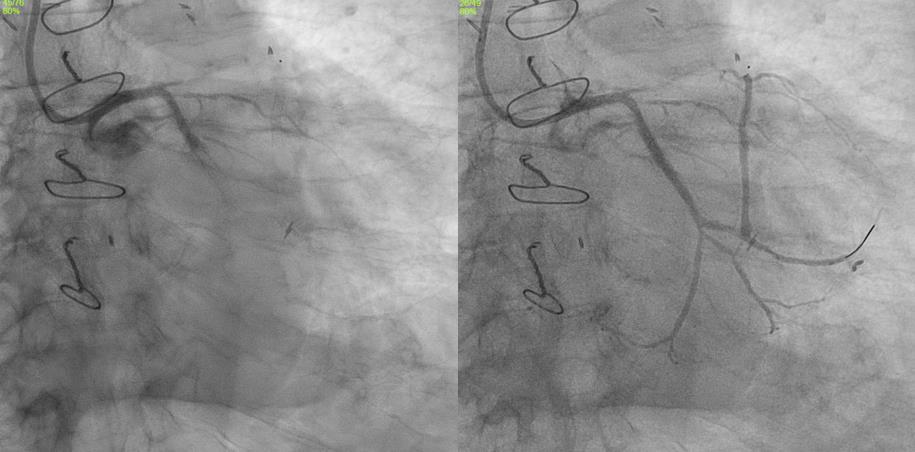
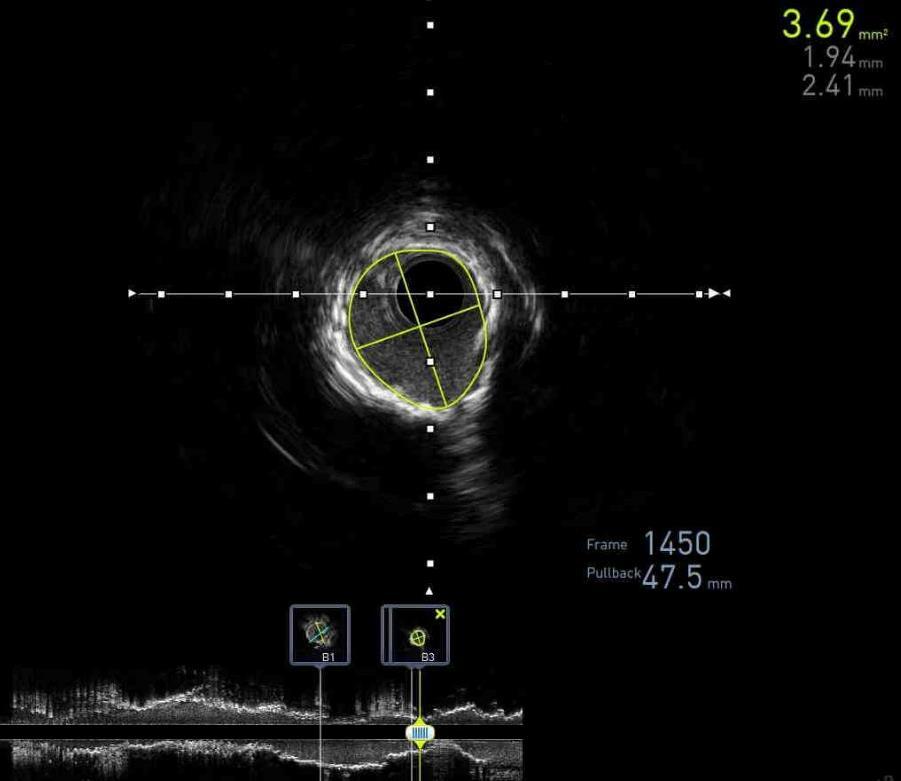 C. LCX before and after PCI
C. LCX before and after PCI
ABSTRACT #43
MEDICAL EDUCATION
CARDIOLOGY
Arpanjeet Kaur1, Joseph Elias1, Forough Hakimzada1, Kiran Mahmood1, Edgar Argulian1, Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: Inpatient telemetry monitoring is used to detect arrhythmias in patients deemed at a high risk for cardiac events. To deliver high value care it is crucial that physicians have knowledge of appropriate indications for telemetry monitoring, and have the skill set to effectively interpret and interrogate telemetry data. Misinterpretation leads to inappropriate treatment, adverse patient outcomes and overuse, which adds to healthcare cost, contributes to alarm fatigue and delays throughput. There are no widely accepted telemetry curricula for Internal Medicine residents. The goal of this study was to design and implement a multimodal curriculum to improve Internal Medicine residents’ knowledge and skills in telemetry interpretation via an education-based intervention involving: a. review of appropriate indications and b. step-by-step interpretation of telemetry monitors
METHODS: Based on the results of a targeted needs-assessment survey, a blended curriculum was designed consisting of brief online videos, case-based didactics and hands-on training. The curriculum was implemented during 2-week inpatient telemetry rotation at 1 of our 2 hospital sites. Thus, residents at this site were the intervention group and the residents rotating on inpatient telemetry floor at other site served as control cohort. The intervention group was provided with online videos before the start of the rotation to review key concepts of telemetry interpretation asynchronously. This was followed by 2 in-person small group weekly workshops, the first being a case based didactic session and the second a hands-on telemetry review session. At end of the rotation, participants at both sites were asked to complete a questionnaire testing participant’s knowledge and telemetry-interpretation skills. The questionnaire also had open-ended questions to gauge their experience with the curriculum
RESULTS: Out of total 72 residents included in the study, 34 in intervention group and 16 controls completed the questionnaire. The intervention group residents achieved better overall scores on the quiz (Mean score=5.2 versus controls=4.3, out of total 7 points, p<0.05). Further analysis of the data showed that intervention group had improved knowledge of basic telemetry concepts and indications (p<0.001), however there was no statistically significant difference in telemetry interpretation skills between two groups (p=0.72). Thematic analysis of qualitative comments showed that participants felt that the curriculum improved core knowledge, helped them become more comfortable in telemetry review and interpretation and impacted patient care management decisions.
CONCLUSION: Our curriculum significantly improved knowledge and had a positive impact on the participants' self-perception and attitude. The lack of improvement in skills may be due to short length of study, individual learning-style or small-sample size. This is an ongoing project, and we anticipate that inclusion of more residents in the future would provide additional meaningful data.
ABSTRACT #44
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
IRINOTECAN-INDUCED DIFFUSE ALVEOLAR HEMORRHAGE IN A PATIENT WITH METASTATIC OVARIAN CANCER
Madison Kennedy1 , Abha Kulkarni2, Elina Tsyvkin3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Weill Cornell Medical Center, New York, NY, United States; 3Memorial Sloan Kettering Cancer Center, New York, NY, United States
BACKGROUND/INTRODUCTION: Diffuse alveolar hemorrhage (“DAH”) is usually caused by autoimmune diseases, connective tissue diseases, drugs, anticoagulants, severe infections, transplantations, or toxins. This case report describes a less common and seldom documented etiology. Here, a patient likely developed DAH due to irinotecan, a topoisomerase inhibitor commonly used to treat colorectal, gastric, brain, and lung cancers. When deciding whether to prescribe irinotecan, physicians should consider the risk that it could cause DAH, as well as more common pulmonary toxicities, such as pneumonitis.
CASE PRESENTATION: A 37-year-old female with a medical history of recurrent mucinous adenocarcinoma with metastatic disease to the lungs, brain, osseous spine, and bone was initiated on irinotecan by her Oncologist. One month later, she presented to the hospital from her clinic with anemia and reported subacute hemoptysis. The hemoptysis began about 3 weeks before, during her second cycle of irinotecan. Of note, she was hospitalized for two weeks prior to this presentation for acute dyspnea after a plane flight. She was found to have a low-risk pulmonary embolism and was initiated on apixaban after a brief course of unfractionated heparin. Her hemoglobin on arrival was 4.8 g/dl (down from a baseline of 8.3 g/dl) with notable vital signs including a heart rate of 95 bpm, blood pressure of 107/54, and oxygen saturation of 93% on room air. The initial differential diagnosis included pneumonia, hemorrhagefrom the known bilateral lungmetastases, and upper gastrointestinal bleeding. She received two units of packed red blood cells with an appropriate increase in hemoglobin on posttransfusion CBC. Apixaban was discontinued on admission.
She was found to have guaiac-positive stool and underwent an upper gastrointestinal endoscopy to rule out an underlying source of blood loss. The endoscopy showed blood at the hypopharynx without a bleeding source in the esophagus, stomach, or duodenum. Computed tomography (“CT”) of the chest with angiography demonstrated unchanged to increased bilateral pulmonary metastasis along with new bilateral ground glass opacities sparing the left upper lobe, increased right middle lobe consolidation, and no active source of bleeding. Interventional pulmonologists performed a bronchoscopy, which demonstrated that blood was present throughout the tracheobronchial tree without an identified source. These findings suggested DAH was the cause of her hemoptysis. This CT-chest angiography was later repeated. Once again, it did not identify a source of bleeding. Cytology and cultures were obtained from bronchoalveolar lavage (“BAL”). BAL return was noted to be progressively bloodier on several aliquots of fluid. Cultures of BAL fluid detected methicillin-susceptible Staphylococcus aureus growth, which was treated with Cefazolin 2 grams every 8 hours for five days. C-reactive protein and erythrocyte sedimentation rate were elevated to 8.9mg/L and 60 mm/hr respectively. BAL cytology results were positive for “adenocarcinoma with mucinous features.”
Rheumatology was consulted with concern for a rheumatological etiology of DAH. Laboratory work-up for autoimmune etiologies were negative, including rheumatoid factor, ANCA, ANA, GBM antibody, lupus anticoagulant, CCP, beta 2 glycoprotein, cardiolipin, and complement 3 and 4. Coagulation studies were negative for coagulopathy. Given continued hemoptysis and recent segmental and subsegmental pulmonary embolism, the patient underwent inferior vena cava filter placement. She required an additional packed red blood cell blood transfusion of 1 unit during her hospitalization. She received inhaled tranexamic acid three times a
day for five days. Irinotecan treatment was stopped with a plan to initiate trastuzumab deruxtecan upon discharge.
DISCUSSION/CONCLUSION: The patient did not have any clinical signs of connective tissue disease and had a negative work-up for rheumatologic and autoimmune disease. Furthermore, she had no history of recreational drug use and, based on a chart review, she did not receive other pharmaceutical agents known to cause DAH. Moreover, while apixaban can cause DAH in rare instances, it did not do so in this case as the patient’s bleeding predated her course of apixaban. Given this context and the fact that her hemoptysis first presented during her second cycle of irinotecan, her DAH was likely induced by the irinotecan. Two notes of caution are warranted. First, the patient may not have had DAH, though this seems unlikely given her clinical presentation and findings on bronchoscopy. Ideally, to further support a diagnosis of DAH, BAL cell counts are obtained to test for further diagnostic indicators, such as hemosiderin-laden macrophages. This patient had limited cytology results that did not assess for cell counts, which could have provided further support for a DAH diagnosis. Moreover, the patient’s bleeding could have been caused by her pulmonary malignancy. However, this is unlikely. The patient’s two chest CT scans with angiography did not reveal any source of bleeding in the known locations of pulmonary metastasis, suggesting her metastasis was not the causal agent. Second, assuming the patient had DAH, her complex medical history injects some uncertainty as to the cause of her DAH. It is possible that her DAH could have been caused by her MSSA infection rather than by irinotecan. This too is unlikely as only a severe MSSA infection could cause DAH and the patient did not have clinical signs of a severe infection, such as fever, leukocytosis, or hypoxia requiring pressure or ventilatory support.While the benefits of irinotecan are well known, physicians should be cognizant of its risks, including that it can, in rare instances, cause DAH, a potentially lifethreatening condition. Further research is needed to explicate the mechanism of injury and the rate of incidence of irinotecan-induced DAH.
ABSTRACT #45
CLINICAL RESEARCH
CARDIOLOGY/HEMATOLOGY/ONCOLOGY
IMPACT OF BIVALIRUDIN VERSUS HEPARIN ON MAJOR BLEEDING DURING PERCUTANEOUS CORONARY INTERVENTIONS: AN UPDATED META-ANALYSIS OF RANDOMIZED CONTROLLED TRIALS
Mohammad Ishrak Khan1, Errol Moras1, Raisa Subaita Zahir 2, Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Wayne State University School of Medicine, Detroit, MI, United States
Presented at the Society for Cardiovascular Angiography and Interventions Annual Meeting that was held in Long Beach, California, United States from May 2-4, 2024.
BACKGROUND/INTRODUCTION: Bivalirudin gained ground against heparin in percutaneous coronary interventions (PCI) due to fewer bleeding risks; however, other safety outcomes are still debatable. We aim to compare such outcomes of bivalirudin and heparin in patients undergoing PCI for acute coronary syndrome
METHODS: We conducted a meta-analysis of the RCTs that randomized patients with myocardial infarction undergoing PCI to bivalirudin or heparin and assessed several safety outcomes. Primary endpoint was thirtyday major bleeding and secondary endpoints were thirty-day all-cause mortality, cardiovascular death (CVD), stent thrombosis, reinfarction, stroke and target vessel revascularization (TVR).
RESULTS: A total of 41,374 patients were randomized: 20,139 to bivalirudin and 21,235 to heparin. Thirty-day major bleeding was lower in the bivalirudin group when compared with heparin (RR, 0.63; 95%CI, 0.50-0.79; p<0.0001). Similarly, thirty-day CVD was lower in bivalirudin group compared to heparin (RR, 0.80; 95%CI, 0.680.94; p<0.006). Such differences between the groups were not observed in thirty-day all-cause mortality (p=0.09), stroke (p=0.36), stent thrombosis (p=0.75), reinfarction (p=0.39), and TVR (p=0.18).
CONCLUSION: Using the totality of the data available to date, procedural anticoagulation with bivalirudin reduced major bleeding and cardiovascular death when compared with heparin in patients undergoing PCI. Such statistically significant differences were not observed between the groups when examined all-cause mortality, stroke, stent thrombosis, reinfarction, and TVR. Bivalirudin should be considered as the first line anticoagulation method in patients undergoing PCI that are at high-risk for bleeding.
ABSTRACT #46
CLINICAL RESEARCH
CARDIOLOGY/NEPHROLOGY
PROGNOSTIC SIGNIFICANCE OF RAAS INHIBITION IN HEART FAILURE PATIENTS WITH CO-EXISTING END STAGE RENAL DISEASE ON HEMODIALYSIS
Won Joon Koh1, Alaa M. Omar1, Anna Sophie Mueller1, Christopher N. Matthews1, Joseph Marinelli1 , Justin Goodfarb1, Mohammad I. Khan1, Muhammad Ghallab1, Ashish Correa1, Kiran Mahmood1, Arieh Fox1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Heart Failure Society of America (HFSA) Annual Scientific Meeting that was held in Cleveland, Ohio, United States from October 6-9, 2023.
BACKGROUND/INTRODUCTION: Patients with end stage renal disease (ESRD) are largely excluded from clinical trials concerned with heart failure (HF) therapeutics, leading to a dearth of quality evidence of guideline directed medical therapy (GDMT) in this high-risk group. Furthermore, renin angiotensin aldosterone system inhibition (RAASi) is generally avoided in hemodialysis patients due to potential side effects including hypotension and hyperkalemia, possibly negating the known benefits of these medications. We studied the prognostic significance of RAASi in HF patients with ESRD on hemodialysis.
METHODS: In a retrospective study protocol, we studied patients followed in our HF clinic who had concomitant ESRD on hemodialysis. Individual and combined RAASi use was registered, and baseline clinical, hemodynamic, and echocardiographic data were assessed. Patients were followed for a median of 31.8 months for cardiac mortality and HF hospitalizations.
RESULTS: From 2014 to 2022, 89 patients were included for analysis [age: 62.4 ± 15 years, 43% women, EF: 46±15%, 39 (45%) reduced EF (HFrEF], and 60 (55%) preserved EF (HFpEF)]. During follow-up, 14 (16%) patients died and 61 (69%) patients had HF hospitalizations. 56 (63%) patients were on RAASi (ACEi, ARBs, ARNI), with no significant differences in baseline characteristics (e.g. age, sex, cause of cardiomyopathy, risk factors, device therapy, AHA/ACC class, BNP, baseline EF) (44.1 ± 14.7 versus 48.7 ± 15, p=0.167) or followup EF (44.7 ± 14 versus 50 ± 15.7, p=130) compared to those not on RAASi. Although RAASi patients had more hypotension (48% versus 20%, p=0.014), RAASi-related adverse events (cough, angioedema, hyperkalemia, intradialytic hypotension, intradialytic inotrope) were similar between both groups. Compared to patients not on RAASi, RAASi patients had statistically significant increase in HF hospitalizations [44 (79%) versus 17 (52%), p=0.004), but were associated with a trend towards fewer deaths [6 (11%) versus 8 (24%), p=0.09]. Both HFrEF patients and HFpEF patients had comparable RAASi use (55% versus 69%, p=0.162), and did not differ in outcomes of mortality (18% versus 14%, p=0.679) and rehospitalization (73% versus 65%, p=0.467). Moreover, on survival analysis, RAASi had significantly less risk for mortality (HR, 0.33; 95%CI, 0.11 to 0.97; Figure 1A, C) but no differences in hospitalization (HR, 1.72; 95%CI, 0.98 to 3.00; Figure 1B, C). Similar results were obtained after adjusting for co-variates.
CONCLUSION: In our study, although hypotension was more common in patients receiving RAASi, hyperkalemia and intradialytic hypotension were not associated with RAASi use. If tolerated, RAASi was associated with improved mortality, but not hospitalization.
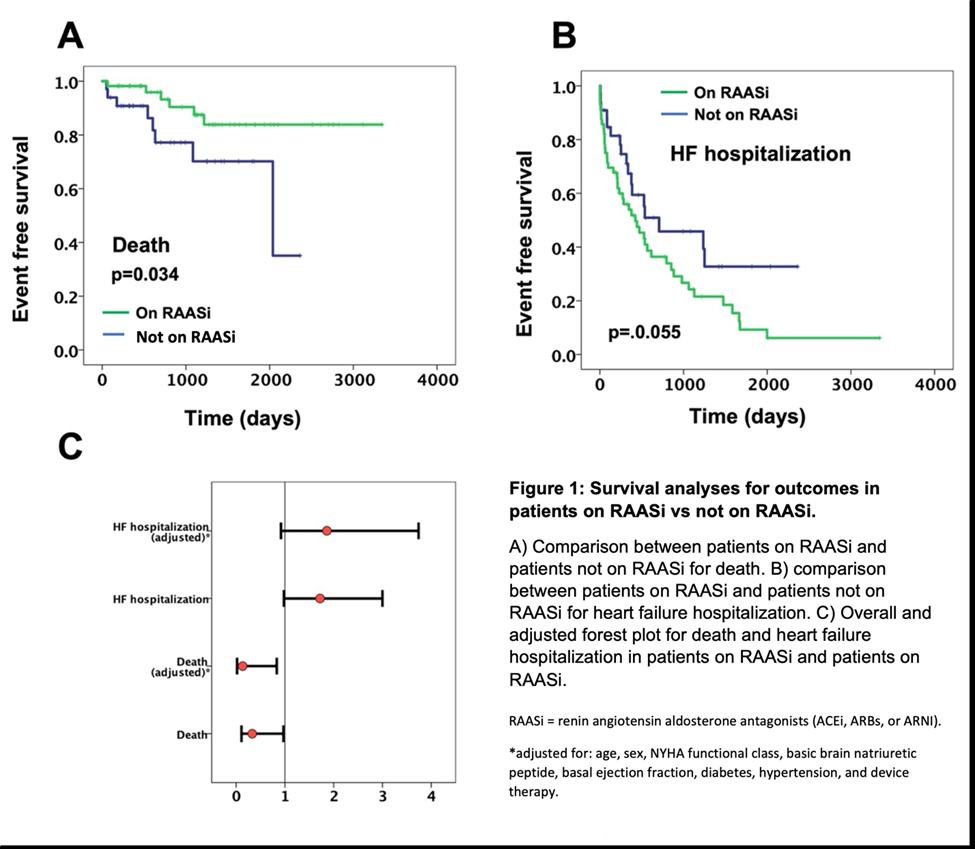
ABSTRACT #47
CLINICAL RESEARCH
CARDIOLOGY
TEMPORAL TRENDS AND CARDIOVASCULAR OUTCOMES IN HOSPITALIZED PATIENTS WITH FABRY DISEASE: INSIGHTS FROM THE NATIONAL INPATIENT SAMPLE
Darren Kong1, James Choi1, Sara Diaz Saravia1, Benjamin Adegbite1, Kiran Mahmood1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: Fabry disease, a lysosomal storage disease consisting of an alphagalactosidase-A deficiency, is associated with multi-organ disease including the liver, kidneys, and heart. New enzyme replacement and gene therapies have emerged in recent years to treat Fabry disease. We aim to study temporal trends and cardiovascular outcomes in hospitalized patients with Fabry disease.
METHODS: Using the National Inpatient Sample (NIS) database we collected major adverse cardiovascular events including arrhythmias, acute myocardial injury, stroke, cardiac arrest, and heart failure that occurred each year from 2017-2019. Appropriate ICD-10 codes were used for data collection. Proportions were calculated and adjusted odds ratios OR were determined using the Charlson Comorbidity Index.
RESULTS: Overall, there was an increase in total hospitalizations in patients with Fabry disease from 2017 to 2019. Fabry disease was associated with increased risk of major adverse cardiovascular events (OR, 2.88; 95%CI, 1.99-3.68; p<0.000) when compared with patients without Fabry disease. There was a significantly higher proportion of major adverse cardiovascular events in Fabry disease when compared to the general population from 2017-2019 (p-trend<0.000). Secondary outcomes showed an increased risk of arrhythmias (OR, 4.89; 95%CI, 3.22-7.08; p<0.000) and heart failure (OR, 4.34; 95%CI, 2.90-6.50; p<0.000), but no significantly increased risk of acute myocardial injury (OR, 3.11; 95%CI, 0.96-4.62; p=0.07) or stroke (OR, 1.79; 95%CI, 0.762.41; p=0.11).
CONCLUSION: Fabry disease is associated with worse inpatient cardiovascular outcomes when compared to patients without Fabry disease. Tissue injury from infiltrative deposits may cause subsequent myocardial fibrosis and conduction diseases, leading to heart failure and conduction diseases, respectively.
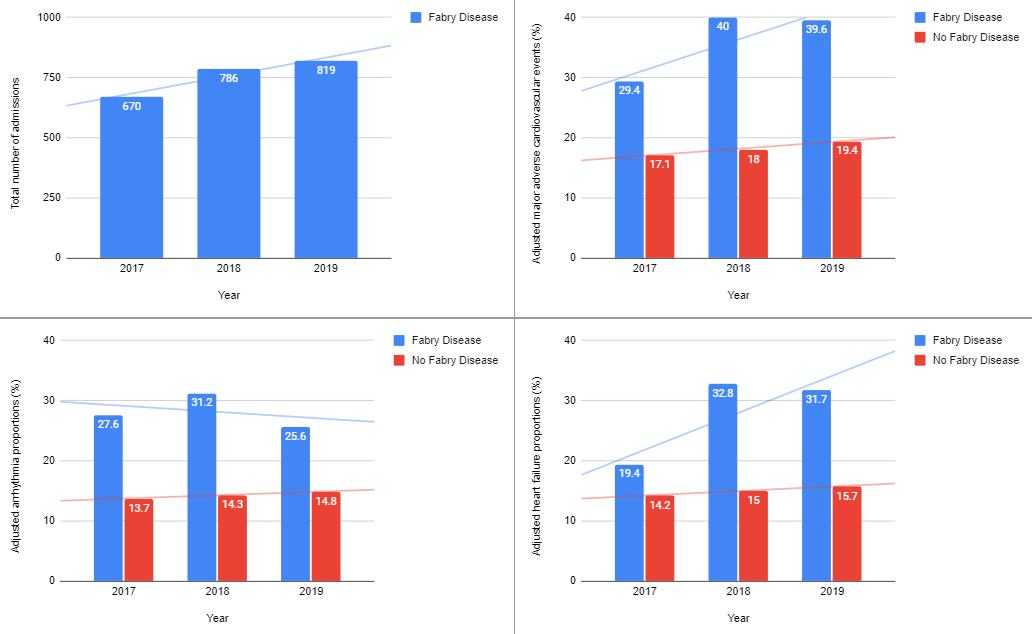
Figure 1: A. Total number of inpatient admissions with a diagnosis of Fabry disease; B. Proportion of major adverse cardiovascular events (MACE); C. Proportion of arrhythmias; D. proportion of heart failure.
ABSTRACT #48
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
OVER-THE-COUNTER OVERUSE: A CASE STUDY OF OVERDOSE ON MEDICATION BOUGHT ON AMAZON
Scott Low1 , Joseph Karpenos1, Matthew Baer1, Rama Hussein1, Kyunghyun Lee1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United StatesBACKGROUND/INTRODUCTION: Use of over-the-counter (OTC) medications is an enticing option for people experiencing health issues. These medications do not require an office visit with a health professional or diagnostic testing. Convenience of these medications has even increased in the past several years with OTC medications able to be delivered directly to a person’s front door overnight. There are many dangers to these medications including side effects, toxicity, drug interactions, and medication misuse.
CASE PRESENTATION: A middle aged female with a history of subclinical hypothyroidism and asthma presented to urgent care for shortness of breath after 3 days of sinus and chest congestion. When she became short of breath, she ordered an inhaler online which was epinephrine based. She had been using this inhaler over the two days prior to admission up to 10 times per day. She brought a document from urgent care which showed blood pressure (BP) readings as high as 247/128. She was told to go to the emergency department. On arrival she was given ipratropium-albuterol nebulizer and prednisone 60 mg for asthma exacerbation. Laboratory work was unremarkable, EKG showed sinus tachycardia, and chest x-ray showed no acute cardiopulmonary process. Poison control was called to discuss the treatment of sympathetic toxidrome secondary to inhaled epinephrine overuse. They had recommended benzodiazepines for BP control, so the patient initially received 5 mg of diazepam intravenously (IV). At the time of the admission interview, the patient's heart rate (HR) was 120s140s on a telemetry monitor with BP of 200/120. She complained only of the occasional feeling of her heart racing, restlessness, and tingling sensation in her thighs. On physical exam, she had constricted pupils, dry mucous membranes, diaphoresis, tachycardia, and intact neuro exam. With persistently elevated BP and HR, she was upgraded to the resuscitation room where she could be monitored closely for sedation while using more IV diazepam for BP control. The patient received diazepam 2.5 mg IV x 2 with minimal improvement of BP and HR. Intravenous hydralazine was chosen as the next line of therapy, but the patient’s BP remained elevated to 182/101. She was seen by the critical care team for further recommendations on management and to evaluate the need for continuous IV medication given the blood pressure was refractory to diazepam and hydralazine. IV labetalol was recommended due to the short half-life of epinephrine and absence of bronchospasm. Two doses of IV labetalol 10 mg were given two hours apart with no improvement in BP; however, there was improvement in HR from 130s to 100. As the epinephrine effect wore off, the patient's blood pressure stabilized around the 140-150s systolic range with HR within normal limits. She was discharged on oral labetalol 200 mg twice daily for likely underlying hypertension that had not been previously diagnosed.
DISCUSSION/CONCLUSION: Due to limited poison control recommendations and sparse information on epinephrine overdoses, literature on cocaine overdoses and pheochromocytomas guided blood pressure management. It was determined that oral phenoxybenzamine would not have a quick enough onset of action. Phentolamine was only available at our institution as an injection antidote for extravasation of vasopressor. Intravenous nitrates were only available in the form of titratable drips which would require ICU admission. As a result, hydralazine was chosen as a temporizing medication until it was believed to be safe to initiate beta blockade in view of consistently elevated heart rate. Beta-blockade was initially avoided due to the patient’s acute asthma exacerbation and concern for unopposed alpha adrenergic stimulation. This case illustrates the adverse effects of misuse of an easily obtainable over the counter medication. There is minimal literature on epinephrine overdose, usually in the setting of IV epinephrine used for anaphylaxis or as a vasopressor. While literature on inhaled epinephrine overdose is limited, the management approach underscores the importance of interdisciplinary collaboration and adaptation of existing protocols.
ABSTRACT #49
QUALITY IMPROVEMENT
PULMONARY/CRITICAL CARE
IMPACT OF PEER-TO-PEER TEACHING ON SEPSIS PATHWAY UTILIZATION AND OUTCOMES
Sara Luby1, Galit Balayla Rosemberg1 , Hammad Sheikh1 , Venus Sharma1 , Connor Smith1 , Rachael Schneider1 , Andrea Wood1 , Alvin Yang1 , Christiana Choi1 , Yoni Balboul2 , James Salonia1 , Raymonde Jean1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: The 2021 Surviving Sepsis Guidelines provide a strong recommendation that hospitals utilize screening tools to identify high risk patients and bundled programs to promote early treatment of sepsis.1 The recommendations hinge on the fact that timely intervention in early sepsis has resulted in reduced mortality.2 Some studies have shown that the use of EHR bundled sets promote guideline-directed interventions and reduce rates of mortality in all types of sepsis.3 We found that within our system (Mount Sinai Morningside/West) the sepsis pathway and order set were being underutilized.
METHODS: An educational lecture series was developed and presented to both Internal Medicine residents and hospitalists from November 2022 through July 2023. The lecture series was provided to the resident floor service teams in groups of 3-5 residents and reinforced at resident academic half-day and hospitalists meetings. A standard chi-squared analysis was used to assess the significance of increased pathway use pre- and postintervention as well as outcomes improvement (mortality and routine discharges home) in patients placed on the pathway.
RESULTS: The pathway utilization before intervention was 11.2% compared to 19.1% after intervention (chisquared p-value of <0.01) with a decreased overall mortality in patients diagnosed with sepsis from 18.2% preintervention to 12.7% post-intervention (chi-squared p<0.002). Before intervention the mortality on pathway patients was 21.2% compared to 16.9% post-intervention (chi-squared p=0.272) and routine discharges home on pathway patients, increased from 27.4% to 34.1% after intervention (chi-squared p=0.171).
CONCLUSION: The Mount Sinai Health System has created multiple bundle systems to improve overall patient outcomes. As seen in several studies, including this one, the use of the Sepsis Order set to provide early treatment of sepsis has shown overall benefits for patients. We saw a significant increase in pathway utilization with an overall decrease in mortality in septic patients after the intervention. Even though mortality and routine discharges were not statistically significant on pathway patients, the overall outcome improved. This can suggest that our innovative approach of teaching the house staff, in a more engaging environment, led to an overall increased awareness and better understanding of how to treat sepsis. Next steps for the project would be assessing if this intervention promotes long term consistency and to find ways of educating on how to use the Order Set in a more sustainable way.
ABSTRACT #50
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
YOU SHALL NOT PASS: RARE DUODENAL
Randy Leibowitz1 , Alexander Maraveyas1, Frederick Rozenshteyn1, Tina Park1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Charlotte, North Carolina, United States from October 21-26, 2022.
BACKGROUND/INTRODUCTION: Duodenal carcinoma accounts for only 1-2% of diagnosed gastrointestinal cancers in the United States. Due to its insidious onset, advanced disease is often established at the time of diagnosis resulting in poor outcomes for patients. Although duodenal adenocarcinomas have been found to comprise around half of all small bowel adenocarcinomas, disease arising from within the duodenal bulb in the D1 segment is a vanishingly rare phenomenon.
CASE PRESENTATION: A 52-year-old female with a past medical history of morbid obesity with placement of laparoscopic adjustable gastric band 14 years prior presented with frequent emesis, inability to tolerate oral diet and a 22 kg weight loss. Recent esophagogastroduodenoscopy during a previous admission revealed a cratered ulcer in the duodenal bulb. An upper GI series was obtained, showing a 2cm mass in the bulb apex which was confirmed by computed tomography. A repeat esophagogastroduodenoscopy was performed which identified a firm and friable ulcer with contact bleeding with complete obstruction of the duodenal bulb. Subsequent histopathology confirmed the presence of invasive, moderately differentiated adenocarcinoma.
CONCLUSION: Although it is difficult to distinguish the prevalence of duodenal bulb neoplasms, it has been clearly demonstrated that neoplasms arising from the D1 segment of the duodenum are extremely rare. By presenting this case, we hope to increase the index of suspicion for small bowel neoplasms as part of the differential for gastric outlet obstruction.
ABSTRACT #51
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE RHEUMATOLOGY
LYMPHOMATOID PAPULOSIS AND METHOTREXATE-RELATED LYMPHOPROLIFERATIVE DISORDER IN A RHEUMATOID ARTHRITIS PATIENT TREATED WITH IMMUNOSUPPRESSIVE THERAPIES
Olga Marushchak1 , Patrick Brunner2 , Randie Kim2 , Chrisanna Dobrowolski1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Congress of Clinical Rheumatology Annual Meeting that was held in Destin, Florida, United States from May 9-12, 2024.
BACKGROUND/INTRODUCTION: Lymphomatoid papulosis belongs to the group of cutaneous CD30+ lymphoproliferative disorders characterized by recurrent, self-healing papulonodular skin eruption with histologic features of a CD30+ lymphoid proliferation of atypical T cells. While pathophysiology is unknown, one study found that two allelic forms of the CD30 promoter were associated with the development of lymphomatoid papulosis, suggesting that allele-specific differences may have role. Mechanisms underlying the spontaneous regression is unknown; however, prevailing hypothesis is that the co-expression of CD30 and the death receptor CD95 (Fas) ligand may be responsible for the self-regression by enhanced apoptosis of proliferating cells. Although immunosuppressants have been reported to be associated with the disorder, there are cases of methotrexate used as successful treatment. Rheumatoid arthritis is associated with increased risk for lymphoproliferative disorders. Furthermore, the use of immunosuppressive drugs, most commonly methotrexate, is an independent risk factor. While the mechanism is unclear, in vitro model study suggested it to be mediated by adenosine through the adenosine A1 receptor. Spontaneous regression occurs in about 50% of cases with discontinuation of the medication; persistent cases and relapses require histology-adjusted chemotherapy.
CASE PRESENTATION: A 54-year-old female patient with medical history of seropositive, non-erosive rheumatoid arthritis and eosinophilic fasciitis controlled with adalimumab, methotrexate, and low-dose prednisone presented to a rheumatology outpatient office for a follow-up visit with a complaint of red and tender cutaneous lesions. Past medical history included glaucoma and hypertension. The review of systems was negative, except for mild morning stiffness and the rash. Social and family history were unremarkable. On the physical exam, diffuse erythematous, tender, non-pruritic subcutaneous nodules were noted over the trunk and upper and lower extremities. Labs were within normal limits except for elevated erythrocyte sedimentation rate. Initial biopsy came back with necrosis of adipose tissue with interspersed neutrophils, consistent with druginduced panniculitis. Patient was further referred to dermatology, and two additional biopsies were obtained. The biopsies showed lymphocytic infiltrates with increased numbers of CD20+ and CD30+ cells, representing lymphomatoid papulosis as a unique form of iatrogenic T-cell lymphoproliferative disease with CD20+ lineage infidelity in the setting of methotrexate therapy. As several cases of lymphoproliferative disorders have been reported in association with TNF-alpha inhibitors, both methotrexate and adalimumab were stopped. Rituximab was chosen as an alternative treatment due to its efficacy in treating rheumatoid arthritis and low risk of tumorigenesis. The patient reported no recurrent lesions on the new regimen.
CONCLUSION: This case highlights the importance of recognizing lymphoproliferative disorders associated with immunosuppressive therapies, particularly in patients with rheumatoid arthritis, and underscores the need for vigilant dermatopathological evaluation and consideration of alternative treatment strategies.
ABSTRACT #52
BASIC SCIENCE
CARDIOLOGY
ALTERATION OF LEFT VENTRICULAR LOAD IMPACTS EXOSOMAL AND MYOCARDIAL MICRORNA EXPRESSION IN A PORCINE MODEL OF MYOCARDIAL ISCHEMIA
Jonas M. Marx1 , Renata Mazurek2, Olympia Bikou2, Tomoki Sakata2, Spyros A. Mavropoulos2, Kiyotake Ishikawa2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association Basic Cardiovascular Sciences (AHA BCVS) Scientific Sessions Annual Meeting that was held in Boston, Massachusetts, United States from July 31-August 3, 2023.
BACKGROUND/INTRODUCTION: Mechanical unloading of the left ventricle (LV) in the setting of myocardial infarction (MI) exhibits cardioprotective effects and reduces infarct size. The underlying molecular mechanisms of these benefits have not been fully elucidated. MicroRNAs modify post-transcriptional gene expression and are regulators of cellular processes. When released into circulation within exosomes, they also participate in intraand interorgan communication. We hypothesized that alteration of LV load influences exosomal and myocardial microRNA expression.
METHODS: Anterior MI was induced in Yorkshire pigs using percutaneous coronary artery balloon occlusion. After one week, animals were subjected to either mechanical LV unloading with a catheter-based LV assist device or LV overloading using a model of aortic regurgitation generated by percutaneous aortic valve destruction. Two hours after manipulation of cardiac load, coronary sinus blood was collected, animals were euthanized and tissue from the infarct border zone was preserved. Exosomes were isolated from blood samples and microRNA patterns were studied using next-generation sequencing. Expression of select differentially regulated exosomal microRNAs was assessed in myocardial tissue employing quantitative polymerase chain reaction.
RESULTS: Change of LV load induced distinct exosomal microRNA signatures in coronary sinus blood. In LV unloaded animals, exosomal microRNAs such as mir-19b, mir-20a, mir-21, mir-144, and mir-146b were higher expressed compared to LV overloaded pigs (log2 FC = 3.47, 2.64, 1.86, 2.62, 1.58; p<0.05). Interestingly, opposite relationships were observed in myocardial tissue collected from the infarct border zone. Mir-19b and mir-20a were lower expressed in LV unloaded compared to overloaded animals (FC = 0.36 ± 0.11 and 0.37 ± 0.12, p<0.05). A similar trend was observed for expression of mir-21, mir-144, and miR-146b.
CONCLUSION: Exosomal miRNAs in coronary sinus blood are affected by changes in LV load. Inverse expression patterns in myocardial tissue suggest increased cardiac release or decreased uptake of exosomes as a possible mechanism.
ABSTRACT #53
CLINICAL RESEARCH
CARDIOLOGY/INFECTIOUS DISEASES
IN-HOSPITAL INFECTIVE ENDOCARDITIS FOLLOWING TRANSCATHETER MITRAL VALVE PROCEDURES
Christopher N. Matthews1, James Choi1, Sara Diaz Saravia1, Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of Cardiovascular Angiography and Interventions Scientific Sessions held in Long Beach, California from May 2-4, 2024.
BACKGROUND/INTRODUCTION: In this study, we examined infective endocarditis following transcatheter mitral valve procedures in a large database, as few cases exist in the literature.
METHODS: Patients recorded in the National Inpatient Sample database who underwent transcatheter mitral valve procedures between January 2017 to December 2019 were analyzed. The outcomes of in-hospital infective endocarditis following transcatheter mitral valve procedures were identified using chi-squared and multivariate logistic regression.
RESULTS: We identified 27,005 patients who underwent transcatheter mitral valve procedures, of which 120 (0.44%) developed in-hospital infective endocarditis. The most frequent causative organism for in-hospital infective endocarditis was viridans group Streptococci (12.5%), followed by other Staphylococci (8.33%), and group C Streptococci (8.33%). Those that developed infective endocarditis were younger and had higher rates of stroke, septic shock, and surgical heart valve replacement compared to patients without infective endocarditis (Table 1). On the multivariate analysis, those with infective endocarditis had higher odds of stroke (Table 2).
CONCLUSION: This study shows that infective endocarditis after transcatheter mitral valve procedures is significantly associated with stroke occurrence


ABSTRACT #54
CLINICAL RESEARCH
GASTROENTEROLOGY
DIGITAL RECTAL EXAMS ARE INFREQUENTLY PERFORMED PRIOR TO ANORECTAL MANOMETRY DESPITE HIGH SENSITIVITY FOR DYSSYNERGIA
Joseph A. Menand1, Robinderpal Sandhu1, Yonatan Israel2, Emma Reford2, Ahmun Zafar1 , Priyanka Singh1,3 , Kimberly Cavaliere1,3, Jean Saleh1,3, Michael S. Smith1,3, Daniela Jodorkovsky1,3, Yuying Luo1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Center for GI Physiology and Motility, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Digestive Disease Week Annual Meeting that was held in Chicago, Illinois, United States from May 6-9, 2023 and published in Digestive Diseases and Sciences, 2024. PMID: 38170338
BACKGROUND/INTRODUCTION: Digital rectal examination should be performed prior to anorectal manometry; however, real-world data is lacking. To better understand real world rates of digital rectal and their sensitivity for detecting dyssynergia compared to the gold standard, anorectal manometry.
METHODS: A retrospective single-center study was conducted to examine all patients who underwent anorectal manometry for chronic constipation or abdominal pain between 2021-2022 at one tertiary center with motility expertise. Primary analysis consisted of the rate of digital rectal exam prior to anorectal manometry; and secondary outcomes included the sensitivity of digital rectal exam for dyssynergic defecation.
RESULTS: Only 42.3% of 142 patients had digital rectal examinations prior to anorectal manometry. Overall sensitivity for detecting dyssynergic defecation was 46.4%, but significantly higher for Gastroenterology providers (2(1,57) = 8.32, p=0.004), and highest for Gastroenterology Attendings (82.6%).
CONCLUSION: Digital rectal examination is infrequently performed when indicated for chronic constipation. Sensitivity for detecting dyssynergic defecation may be impacted by discipline and level of training.
ABSTRACT #55
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASE/RHEUMATOLOGY
SCHISTOSOMIASIS REACTIVE POLYARTHRITIS MASQUERADING AS SERONEGATIVE ARTHRITIS OF INFLAMMATORY BOWEL DISEASE
Jiaxi Miao1* , Aesha Patel1*, Elmarie Alexander1,2 , Rahul Gaikwad1, George McKinley1 , Mark Alon1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States *These authors contributed equally to this work.
BACKGROUND/INTRODUCTION: Schistosomiasis is a parasitic infection caused by waterborne trematodes, which consists of three main species that infect humans: S. mansoni, S. haematobium, and S. japonicum, all prevalent in different regions of the world, but most common to sub-Saharan Africa, South America, East Asia and the Middle East. It is one of the most prevalent parasitic diseases across the globe, however, infections are often subclinical, later progressing to chronic schistosomiasis if untreated in its acute stages. Schistosomiasis presents as separate time specific manifestations. Acute infection manifests nonspecifically with intermittent fever, generalized rash, an intermittent cough, and gastrointestinal complaints. Chronic infection, however, ranges from asymptomatic to fulminant disease and can manifest as liver disease, pulmonary fibrosis, bladder calcification, gastrointestinal disease, neuroschistosomiasis, and more. Although the aforementioned symptoms from schistosomiasis are well documented, arthropathy remains to be seldom reported. Thus far, very few studies have reported reactive arthritis after parasitic infections, of which Schistosomiasis is least documented.
CASE PRESENTATION: This case presents an 18-year-old male with past medical history of Hepatitis B infection presenting to the emergency department for 1 month of low grade subjective fevers, bilateral lower extremity arthralgias, specifically in bilateral knees, hips, and lumbar spine, and new onset rectal bleeding of five days. The patient is originally from Guinea, however, he recently emigrated from Nicaragua, where he lived for four months prior to his arrival to New York. The patient was a resident in refugee housing and recently visited another emergency department for similar symptoms during which he was found to be positive for hepatitis B infection and discharged for follow up with Hematology/Oncology. The patient reported worsening joint pain in knees, hips and lower back, rated at 9/10 in intensity. He recalled the pain starting 1.5 months prior to his presentation, beginning in his left foot and traveling up both lower extremities, hips, and then lumbar spine. The patient endorsed that the pain was associated with intermittent subjective fevers and denied inciting trauma or insult. The patient denied nausea, vomiting, or diarrhea, or history of hemorrhoids, colitis or family history of colorectal cancer, however, he endorsed dark colored, red-streaked stool for 5 days prior to presentation. The physical examination revealed tenderness and edema in the knees and hips bilaterally with limited range of motion, and redness on the soles of both feet. The abdominal exam was benign without hepatomegaly or tenderness. Initial pertinent labs included iron deficiency anemia with hemoglobin of 8.1, hematocrit of 29.1, MCV of 60.3, iron of 16, transferrin of 4.36. CMP remarkable for creatinine 0.53, and alkaline phosphatase 134. He also had abnormal inflammatory markers (ESR 28, CRP 6.9; Negative: ANA, ANCA, CCP, Ro/La, and DSDNA). Imaging studies revealed erosive changes in the SI joints consistent with seronegative spondyloarthropathy. Lyme serologies returned positive. The presentation of new onset active hematochezia prompted colonoscopy, post-op diagnosis (before pathology) was consistent with pancolitis ulcerative colitis with inflammation. The patient was treated with appropriate pain regimen, initially started on intravenous methylprednisolone due to concern for ulcerative colitis and given intravenous iron supplementation for iron deficiency on labs. GI PCR returned positive for E. histolytica and the patient was appropriately started on a 7 day course of metronidazole. Steroids were stopped at this time given infection. Further, biopsy results from colonoscopy returned positive for parasitic ova indicating schistosomiasis instead of ulcerative colitis The patient was appropriately started on praziquantel. Lyme serologies were likely false positive as molecular mimicry. HLA- B27 was also found to be positive, which is associated with a higher risk of reactive polyarthritis.
On discharge, paromomycin was recommended for intraluminal coverage, and the patient was set up to have outpatient follow up with Hematology, Infectious Diseases, and Gastroenterology.
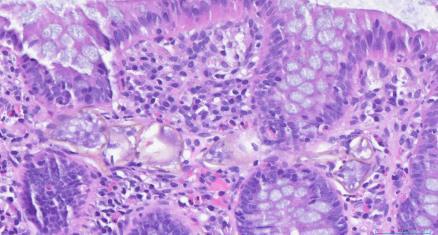
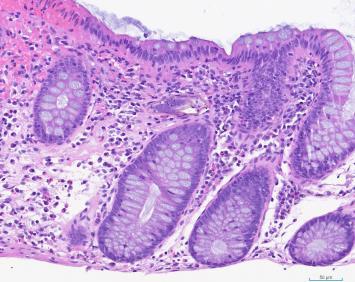


Image1-4: Biopsy results of the colonoscopy indicating rare parasitic like ova within lamina (eosinophils, lymphocytes, plasma cells and histiocytes) consistent with parasitic ova of schistosomiasis
CONCLUSION: In a patient with migrating joint pain and new onset hematochezia, IBD has been the prevailing diagnosis among teams. Furthermore, bilateral sacroiliac joint X-rays showed patterns of seronegative spondyloarthropathy, as well as colonoscopy patterns consistent with ulcerative colitis making the pretest probability of IBD even higher. However, recognizing infectious causes in immigrant patients is vital to come to the right diagnosis. Shortly after the colonoscopy, GI PCR came back revealing Entamoeba histolytica, which prevented initiation of empirical steroid, also casting doubts for UC and leading towards infectious causes. Eventually, biopsy, the pathology gold standard result came back showing parasitic-like ova indicating schistosoma within lamina propria with surrounding mild inflammation. Therefore, the seronegative spondyloarthropathy is indicating reactive arthritis, more confluent with the clinical picture.
ABSTRACT #56
CLINICAL RESEARCH
GASTROENTEROLOGY
ANAL CANCER SCREENING, ARE WE DOING ENOUGH IN FEDERALLY QUALIFIED HEALTH CENTERS?
Patricia Miguez Arosemena1 , Emily S. Seltzer1, Cristina Olivo Freites2, Sophia Nurani3, Christian Olivo Freites3 , John Anthony Andrilli1, Frank Nelson1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2University of Texas Health Science Center at Houston, Houston, TX, United States; 3Ryan Health, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
BACKGROUND/INTRODUCTION: The incidence of anal cancer has significantly increased over the last several years, along with a rise in advanced-stage diagnosis and mortality. This is particularly pronounced in people living with HIV (PLWH), as it is considered a significant risk factor for anal cancer. Similar to cervical cancer, a high-grade squamous intraepithelial lesion (HSIL) precedes anal cancer and is associated with human papillomavirus (HPV) infection. Current recommendations endorse anal cancer screening in high-risk populations. A randomized clinic trial showed a significantly lower likelihood of progressing to anal cancer when patients with HSIL received treatment compared to active monitoring. This study aims to evaluate the current baseline screening rates of anal cancer screening in three federally qualified health centers (FQHC) in New York City.
METHODS: This retrospective multicenter study includes PLWH over 35 years of age who were seen in 3 FQHC in New York City between January 2021 and January 2023. Subsequently, demographic and laboratory results were analyzed using descriptive statistics.
RESULTS: Out of the 485 patients identified, 17 were excluded due to lost to follow-up, or history of anal cancer. Therefore, we identified 468 patients 35 years and older with HIV between January 2021 and January 2023. The median age was 54 years, and 81% were men, of which 72.8% were men who reported having sex with men. The majority of patients were Black or White (45.7% and 32.5%, respectively), and 41.5% identified as Hispanic. Only 12% of patients tested positive for rectal chlamydia or gonorrhea. Most patients were immune to hepatitis B either through vaccination (44.9%) or previous infection (34%), and 88.5% were negative for hepatitis C. Nearly all patients were on HIV treatment (98.3%) with a median absolute CD4 count of 701. Only 7.7% of patients were vaccinated against HPV, with a median age of 38. Finally, only 31.5% of patients had an anal Pap smear in 2 years. Normal results were seen in 74.7%, and only 3.4% exhibited LSIL and 2.1% HSIL.
CONCLUSION: Despite current evidence highlighting the importance of anal cancer screening, our study found low screening rates across three FQHCs in a 2-year period. Limiting factors to successful screening, such as lack of awareness among physicians and patients, insufficient time during visits, and insurance coverage barriers, have been described. Overcoming these limitations requires comprehensive multidisciplinary efforts from Primary Care, Colorectal Surgery, Infectious Diseases, and Gastroenterology. Rising awareness among primary care providers, along with enhancing their proficiency in conducting anal pap tests, could serve as a crucial foundation.
Table 1: Patient Demographics, Medical History, and Anal Cancer Screening
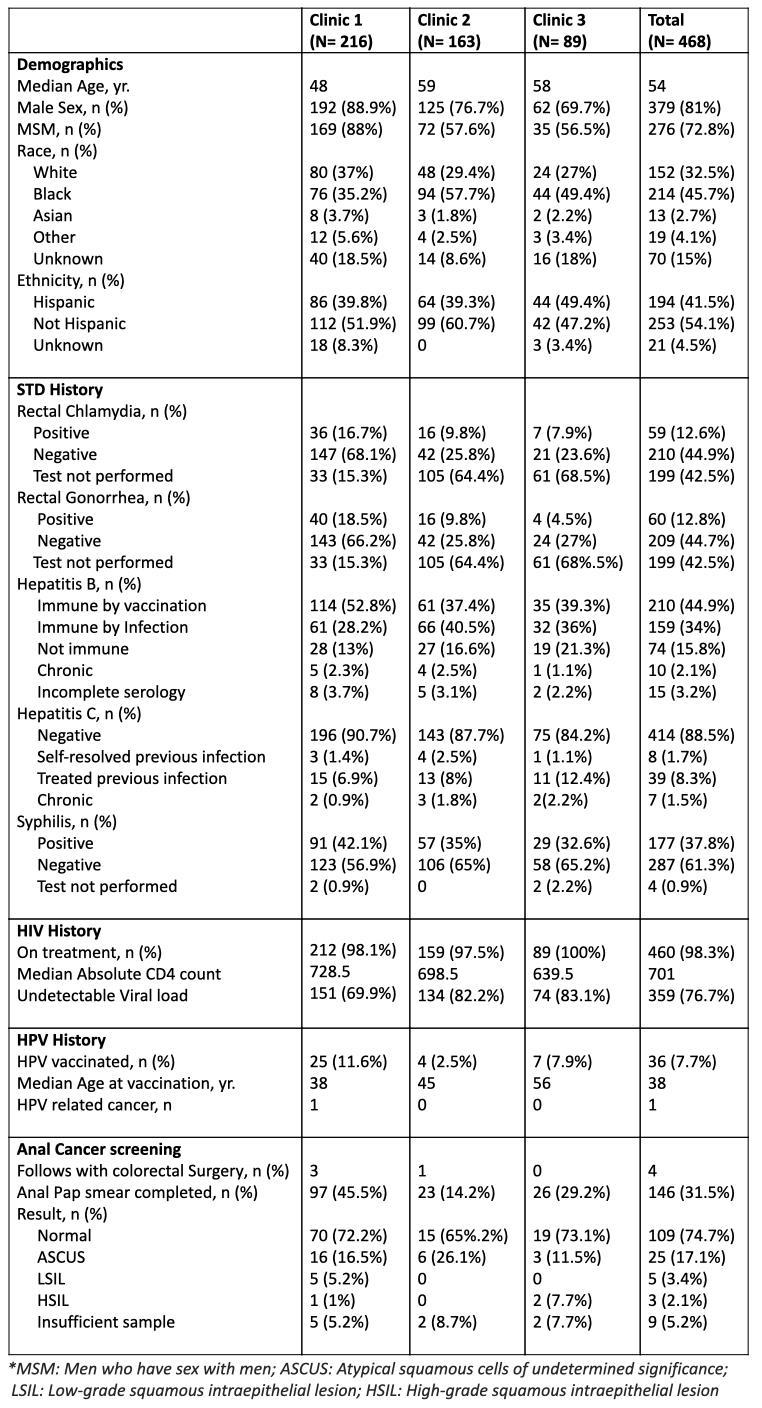
ABSTRACT #57
CLINICAL RESEARCH
CARDIOLOGY
TRENDS AND OUTCOMES OF INTRAVASCULAR IMAGING IN PATIENTS UNDERGOING PERCUTANEOUS CORONARY INTERVENTION FOR CORONARY CHRONIC TOTAL OCCLUSION
Errol Moras1 , Kruti Gandhi1, Abel Casso Dominguez1, Nitin Barman2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
BACKGROUND/INTRODUCTION: Elderly patients with coronary chronic total occlusions (CTO) represent a vulnerable population with comorbid conditions and complex coronary anatomy. Intracoronary imaging has become an important tool in the treatment of complex lesions with percutaneous coronary intervention (PCI). There is limited data on its impact in patients undergoing percutaneous coronary intervention (PCI) for coronary CTO. We aimed to identify the trends in utilization of intravascular ultrasound (IVUS) and optical coherence tomography (OCT) in patients undergoing single vessel (SV) - CTO PCI and its impact on clinical outcomes.
METHODS: We queried the Nationwide Inpatient Sample database to identify hospitalizations for single vessel PCI between 2016 – 2020. Patients with CTO were identified using the ICD-10 diagnosis code. The use of IVUS and OCT was identified using the ICD-10 codes. We compared utilization of IVUS-OCT for SV-CTO PCI to those without and studied the impact of their utilization on clinical outcomes. The primary outcome was major adverse cardiovascular and cerebrovascular events (MACCE). Secondary outcomes included in-hospital mortality, reinfarction, stroke, and post-procedural AKI. Outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: A total of 135,745 weighted hospitalizations for SV CTO-PCI were identified of which 13,610 (10%) utilized IVUS/OCT (mean age 66+/-12, 26.5% females). Hospitalizations were stratified by patient age into a younger cohort <75 years (mean age 61 ± 9 years) and an older cohort ≥ 75 years (mean age: 81 + 4 years). Male sex, Caucasians, and admissions to a large urban hospital were associated with higher IVUS/OCT use in both cohorts (p<0.001). The use of IVUS/OCT was associated with significantly lower MACCE (aOR, 0.73; 95%CI, 0.6-0.8; p<0.001) and lower incidence of re-infarction in both cohorts (OR, 0.6; 95%CI, 0.5-0.6; p<0.001 for both cohorts). In-hospital mortality was significantly lower in both cohorts utilizing intravascular imaging (OR 0.8; 95%CI, 0.7-1.0; p<0.05 for age ≥75 years and OR, 0.6; 95%CI, 0.5-0.7; p<0.001 for age < 75 years). Overall, the rates of stroke and length of stay (4 + 5 days) were comparable but associated with higher hospitalization costs ($153K-$170K versus $110K-$120K, p<0.001). In patients undergoing CTO-PCI, there was an increasing trend towards the utilization of IVUS and OCT over the study period.
CONCLUSION: The use of IVUS/OCT guidance for CTO-PCI was associated with a significant reduction in MACCE, re-infarction and in hospital mortality regardless of age. There was a significant increase in the utilization of IVUS and OCT for the study period in all groups.
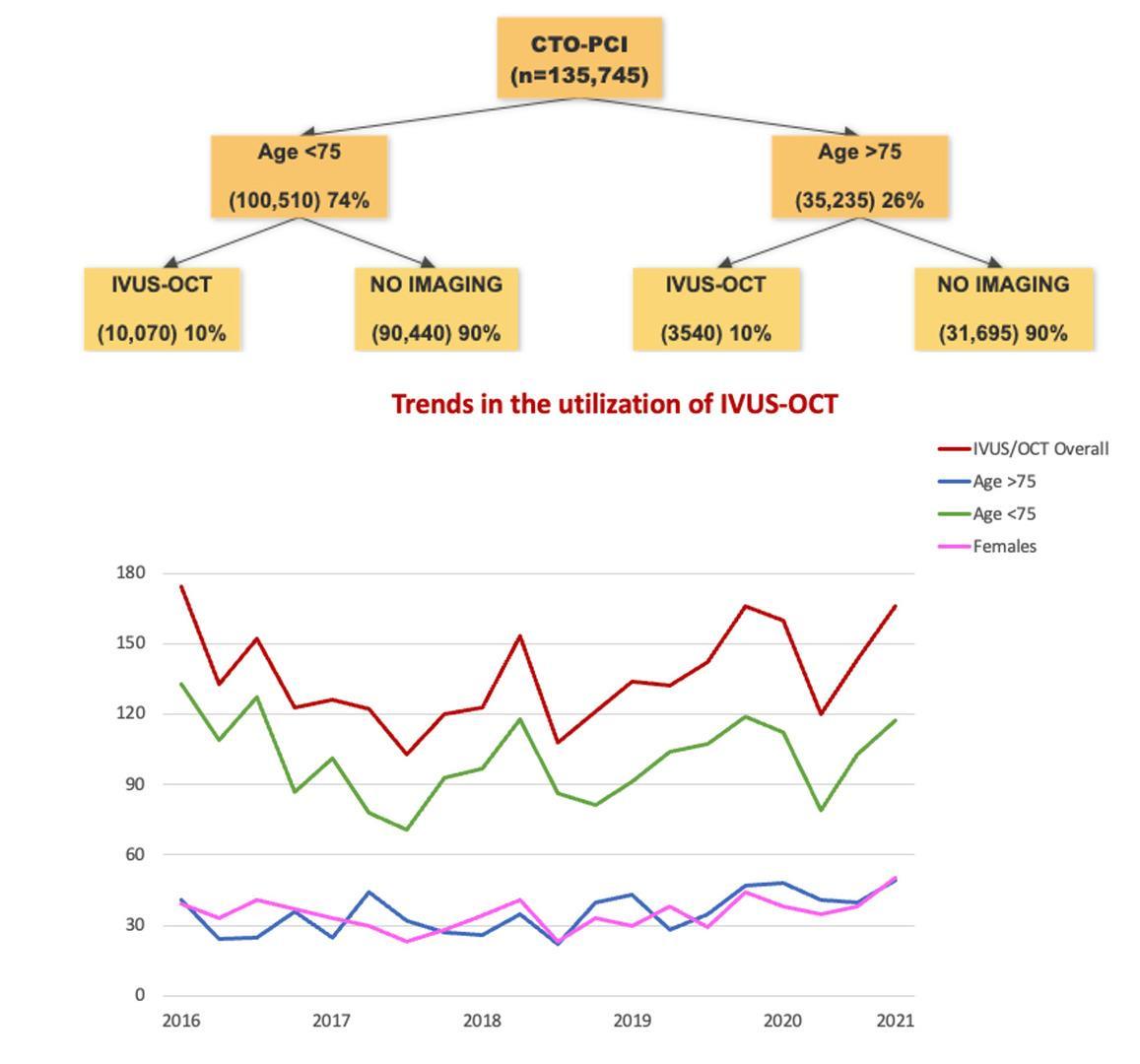

ABSTRACT #58
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES
AN ISOLATED CASE OF NOSOCOMIAL ACQUISITION OF INVASIVE
Jonathan M. Oxman1, Laura Rivera Boadla1,2 , Nicholas Sells1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Published in IDCases, 2023. PMID: 37645540
BACKGROUND/INTRODUCTION: Non-typhoidal Salmonella spreads to humans via contact with animals or consumption of contaminated animal products, often causing outbreaks of a self-resolving gastroenteritis. Less commonly, it can lead to bacteremia and invasive disease. Nosocomial, person-to-person, and asymptomatic carrier transmission are uncommon in the United States. Reactivation of latent Salmonella in immunocompromised patients is also a known phenomenon. Here, we report a case of an isolated Salmonella bacteremia that developed in an intubated patient with a prolonged hospital course and no clear outbreak or focus of infection.
CASE PRESENTATION: An 85-year-old male with a past medical history of hypertension, hyperlipidemia, diabetes, coronary artery disease, prostate cancer, stage five chronic kidney disease, peripheral arterial disease status-post left superficial femoral artery atherectomy with stenting, and a recent small right sided subdural hemorrhage, presented to the hospital after being found unconscious by a family member.
At his initial presentation, the patient was afebrile, with a blood pressure of 130/49, and a heart rate of 48. His oxygen saturation was 100% on room air. Initial physical exam was notable for bradycardia and a neuro exam remarkable for the patient being awake but not oriented and unable to follow commands. At baseline, he was alert and oriented to person, place, and time. No focal neurologic deficits were noted. His lung and abdominal exams were unremarkable.
Initial CBC was notable for a chronic anemia with hemoglobin 8.9 g/dL, WBC 5.9 K/uL and platelets 122 K/uL. Coagulation studies were unremarkable. His glucose was 260 mg/dL, Na 134 mmol/L, potassium 5.8 mmol/L, HCO3 16 mmol/L, BUN 120 mg/dL and creatinine 8.13 mg/dL, which was above his baseline creatinine of about 5 mg/dL. Liver function tests were unremarkable. His pH was 7.28 with pco2=56 mmHg and a normal lactate. His creatine kinase and troponins were unremarkable. Subsequent urinalysis was positive with small leukocyte esterase and 19 WBCs/HPF. No urine culture was obtained at that time.
A head CT revealed an acute on chronic right subdural hemorrhage with a 0.4 cm midline shift. The patient was admitted to the surgical ICU for close observation and surgical management. Given concern for uremia, continuous veno-venous hemofiltration was initiated. A dialysis catheter and arterial line were placed on the day of admission. On day 2, the patient was oriented to person and able to follow commands. He underwent a right sided craniotomy with evacuation of the subdural hemorrhage the following morning. On day 3 of admission the patient’s mental status declined. On day 4, seizures were observed, and the patient was intubated for airway protection. On day 7, enteral nutrition was started along with free water flushes. He was transitioned from continuous veno-venous hemofiltration to hemodialysis on day 9.
He continued to be encephalopathic with no evidence of seizures on EEG. Due to a poorly functioning dialysis catheter, a new one was placed in the in the right internal jugular vein on day and dialysis was resumed. Until this point, he remained afebrile with no concern for infection. On hospital day 12, he was noted to be febrile to 100.5 degrees Fahrenheit that resolved with acetaminophen. Subsequently, he remained afebrile for the following several days.
Given his persistent encephalopathy, palliative care was consulted, and the anti-epileptic medications were tapered. By hospital day 13, his mental status began to mildly improve with spontaneous movements of all extremities, withdrawal to pain, and eye opening. Up until this time, the patient intermittently required red blood cell transfusions, was still receiving enteral nutrition, and remained on a ventilator. On day 15, a midline catheter was inserted given poor peripheral access. An MRI brain on day 15 demonstrated chronic bilateral thalamic and cerebellar infarcts, as well as subacute subdural hematomas without midline shift or hydrocephalous.
On day 16, he had new onset, loose stools and became febrile with a maximum temperature of 102.4 Fahrenheit. He developed a leukocytosis with WBCs increasing from 7.7 K/uL to 11.3 K/uL with 86% neutrophils. Cultures were sent and he was started on piperacillin-tazobactam. On the following day, he remained intermittently febrile with a worsening leukocytosis. Respiratory gram stain and culture showed normal oropharyngeal flora. Gram stain from blood cultures returned positive for gram negative bacilli in one anaerobic bottle after 12 hours of growth. No urinalysis was obtained given his anuria. Due to the bacteremia, the dialysis catheter was removed. On day 18, the patient’s fever improved, and his WBCs fell from 17.5 K/uL to 14.6 K/uL, however, his loose stools persisted. Blood cultures speciated Salmonella species susceptible to Ceftriaxone which was started.
Given the unclear source of Salmonella, a gastrointestinal PCR, stool culture, repeat blood cultures, an HIV antigen/antibody test and CT abdomen pelvis were obtained. Further history obtained from the patient’s relatives revealed that no one in the family or any recent visitors had recent gastrointestinal symptoms. There were no known exposures to pets, reptiles, or any recent travel. The HIV test was negative. The patient had been NPO and receiving enteral nutrition up until this point. On day 20, despite improvement in the patient’s fever curve, he became hypotensive with MAPs below 60. He was started on multiple vasopressors. His abdomen was noted to be rigid. Metronidazole and tigecycline were started. The GI PCR resulted negative for pathogens. The repeat blood culture from day 20 was no longer positive for Salmonella. On day 21, a CT abdomen and pelvis did not demonstrate any pathology, however, it showed a left external iliac artery pseudoaneurysm with active extravasation into a 12 cm retroperitoneal hematoma. Shortly thereafter, the patient went into cardiac arrest and, despite efforts to resuscitate him, he passed away on day 22 of hospitalization.
DISCUSSION/CONCLUSION: While nosocomial transmission needs to be considered here, the literature describes cases of reactivation of latent Salmonella among colonized patients with several conditions, including malaria, sickle cell disease, lupus, cancer patients undergoing chemotherapy, HIV infection, and after major surgery. Although this patient did not have the typical conditions associated with reactivation, his age, multiple comorbidities, acute illness, and recent surgery, perhaps, all put him at risk for latent Salmonella reactivation. Hence, reactivation needs to be considered as a plausible explanation for his bacteremia. As mentioned prior, localized, extraintestinal Salmonellosis can often occur in the setting of bacteremia. Intravascular Salmonella infections involving the aorta, coronaries, peripheral arteries, arteriovenous fistulas, and bypass grafts are known phenomena. In particular, aneurysms, including of the aorta and femoral arteries are prone to infection after a bacteremia, with atherosclerosis being a risk factor for infection. Other sources of abdominal Salmonellosis outside of the gastrointestinal tract have involved the biliary tree, liver and spleen. The CT scan of his abdomen and pelvis was not suggestive of an abdominal focus of infection. Notably, this patient had prior percutaneous interventions of both the left popliteal and left superficial femoral arteries due to significant atherosclerotic disease. He ultimately expired from a left external iliac artery pseudoaneurysm rupture, possibly in the setting of prior instrumentation. His significant atherosclerotic disease and prior angioplasty, raises the possibility that the focus of his Salmonella infection was endovascular. However, the quick clearance of blood cultures poses a challenge to this hypothesis. Unfortunately, the patient expired, and no additional workup was undertaken to elucidate the source of his Salmonella bacteremia. Here we report an unusual case of a Salmonella bacteremia that developed in the hospital in the absence of a known outbreak. No other Salmonella infections or specimens were reported at the hospital throughout the course of his hospitalization. Whether this was nosocomial acquisition or reactivation of a latent infection will never be known. Given the high mortality rate of invasive, nontyphoidal Salmonella, prompt recognition and treatment are required regardless of the etiology
ABSTRACT #59
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE CARDIOLOGY/GASTROENTEROLOGY
BACKGROUND/INTRODUCTION: Atrial fibrillation is the most prevalent cardiac arrythmias. Multiple studies have demonstrated that cryo-balloon ablation, which delivers targeted cryotherapy to the pulmonary vein, successfully treats atrial fibrillation, reduces the rate of arrhythmia recurrence, and has a lower incidence of clinically significant adverse events when compared to antiarrhythmic medication. The overall rate of upper gastrointestinal complications following atrial fibrillation ablation procedures has been reported to be as low as 0.74%, with gastroparesis being an especially infrequent complication with an incidence of only 0.2%.
CASE PRESENTATION: A 45-year-old male with a past medical history of paroxysmal atrial fibrillation underwent cryo-balloon ablation. The following day, he began experiencing early satiety, vomiting, and abdominal distention, which progressed to an inability to tolerate any oral intake and was admitted to the hospital three days post procedure. An upper gastrointestinal series done seven days after the procedure showed no evidence of gastric or duodenal obstruction, but there was significant distention of the stomach with a large amount of retained contents. Within the first ten days after the procedure, the patient had lost 17 pounds. He was started on oral erythromycin 250 mg four times a day, for presumed gastroparesis with some improvement in his symptoms. Four weeks after starting erythromycin therapy, a gastric emptying study showed 74% retention after four hours. Two months post-ablation, the patient’s vomiting had resolved, and he had gained 8 pounds, but he continued to experience nausea and early satiety. An upper endoscopy was relatively unremarkable with no evidence of pyloric pathology.
CONCLUSION: Atrial fibrillation ablation is generally a well-tolerated procedure with a low risk profile but does have the propensity to cause gastrointestinal complications. Common problems include nausea, vomiting, and gastroesophageal reflux, while more serious complications such as esophageal injury and gastroparesis can also occur. Notably, lower periprocedural temperatures in the inferior pulmonary veins during cryo-balloon ablation and a smaller left atrium size are associated with an increased risk of gastroparesis. Given that the esophagus is near the posterior left atrium, endocardial ablation can cause direct thermal injury to the esophagus, ischemia from anterior esophageal artery damage, and esophageal dysmotility from periesophageal vagal plexus injury. Resolution of gastrointestinal symptoms generally occurs within two to six months with conservative management and prokinetic agents. This case demonstrates acute and severe onset of upper gastrointestinal symptoms with rapid weight loss immediately following routine cryo-balloon ablation and emphasizes how crucial it is for providers to be aware of the procedure’s ability to cause gastrointestinal complications.
ABSTRACT #60
CLINICAL RESEARCH
GENERAL INTERNAL MEDICINE
ADVOCATING COMMUNITY FOR HEALTHCARE ACCESS AND NETWORK FOR GROWTH AND EQUITY FOR THE MOST VULNERABLE BY OPPOSING THE 340B DRUG PRICING PROGRAM CARVE OUT
Bailey Perry1 , Debbie Fermin1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York American College of Physicians Annual Scientific Meeting that was held in Tarrytown, New York, United States on October 28, 2023
BACKGROUND/INTRODUCTION: Safety net providers and safety net health care centers are an essential part of the healthcare framework. They serve a predominantly Medicaid insured population along with underinsured and uninsured patients. These health centers offer a wide variety of services spanning from preventive medicine, mental health, BHI, Women’s Health, HIV/AIDs Treatment and care and social services, among many others. This allows for the centers to target specific community needs, especially the vulnerable populations. The 340b Drug Pricing Program protects the community through federal funding given to safety net health care centers to provide resources that are site specific. Other than the services mentioned above, 340b drug pricing program helps fund community-based vaccination drives, mammogram screenings, discounted medications, mental health treatments, and care coordination. In chapter 56 of the 2020 laws, there was a distinct transition to be made which gave the Department of Health (DOH) power to authorize transition of the pharmacy benefit from a managed care to fee-for-service. However, in doing so this would divert much needed funding away from safety net providers and health centers which would in turn cut crucial services as mentioned above. Over 50% of health centers across New York (NY) will have to scale back on or eliminate diabetes education programs, care management for critically ill patients and community outreach to expand access. Through C.H.A.N.G.E (Community for Healthcare Access and Network for Growth and Equity) two resident physicians in NYC are able to use social media as a platform to advocate for increased access to care for medically underserved and vulnerable patient populations by opposing the 340B carve out that is currently pending initiation amid the 2023 NYS Budget
METHODS: To enhance the reach and improve health awareness for our audience, we relaunched our Instagram account (@nycdoctors4change) on April 10, 2023. This relaunching consisted of 4 phases of posting Instagram posts, stories and reels in a span of 4 weeks. During phase 1, we rebranded with a new logo and reintroduced the mission and vision of our advocacy page. During phase 2 and 3, we shared information regarding access to care such as Health Insurance basics, Federally Qualified Health Centers (FQHCs) services and locations in New York City, as well as introduced the residents behind the project. During phase 4, we gathered data through a story poll with a 24-hour availability for response to better understand our audience’s awareness on FQHCs, 340b Drug Discount Program and 340b carve out. We also gathered data from 3 FQHCs located in Midtown, Upper West Side and Central Harlem through the Azara database. The data showed the number of insured patients and HIV/AIDs treatment and care services that were funded by the 340b Drug Discount Program. We also created reels explaining the 340b Drug Discount Program and how the 340b carve-out will negatively impact access to care for the underserved communities in New York City (NYC). We used the Instagram Algorithm insights to determine the number of accounts we have reached, as well as likes and follows.
RESULTS: Between April 10, 2023 and May 5, 2023, we reached a total of 7,105 Instagram users. The majority (52.1%) of our audience is from the United States and 25.1% of which are from New York City. With the reels we posted, we garnered a total of more than 15,000 views. The poll questions results are as follows: a. “Are you aware of federally qualified health centers?: Yes, 47% (17) and No, 53% (19)]; b. “Do you know that FQHCs offer services such as preventive health, mental health, women’s health, HIV/AIDS treatment and care, and social services?”: Yes, 48% (16) and No, 52% (17); c. “Do you think it is important for New Yorkers to have access to health care?”: Yes ,95% (37) and No, 5% (2); d. “Are you aware of the 340b carve out?”: Yes, 14% (5)
and No, 86% (31) and lastly, e. “Did you know that FQHC services are in jeopardy of getting defunded through the 340b carve out?”: Yes 3% (1), No, 97% (31). The data mentioned above showed how our online audience had no awareness of the 34, 0b Drug Discount Program and Carve-out. The data from the Azara database showed a total of 940 HIV/AIDS patients across three federally qualified health center sites in NYC will be in jeopardy of losing benefits. Therefore, increasing the risk of unnecessary hospitalizations, medication nonadherence and care coordination. A total of 2,018uninsured patients will also lose the sliding-fee per visit benefits from the 340b drug discount program and therefore will intensify the financial disparity further.
CONCLUSION: The data that we have collected over the past 4 weeks demonstrates the lack of public knowledge about the available valuable resources provided by safety net healthcare centers for the most vulnerable and medically underserved patient populations throughout New York City. Nearly 100% of our followers that took part in our poll had no knowledge of the potential financial impact of the 340B Drug Pricing Program carveout on safety net clinics in New York state. Safety net providers in New York State will be defunded of providing essential services to the community and eventually create more healthy disparities for the underinsured and uninsured patients. By implementing weekly Instagram posts to educate our followers, we have reached a total 7,000 accounts in a span of 4 weeks. We hope to keep posting on a weekly basis to expand our following and reach more accounts. Our posts and reels will hopefully spread awareness to the general public through education on current and relevant access to healthcare issues. Challenges that we have faced during this project include lack of time as we have collected our data within 4 weeks. We also struggled to obtain standardized data across all safety net health centers and data from Medicaid to further educate ourselves on the potential threat the carve out has on NYC as a whole. Although social media is an excellent avenue to educate the general public with short video clips, our content reached a majority of users (83.3%) who identify as female within the 25-34 age range (66.4%). In the future, we plan to produce posts and reels that will reach men too. Another challenge that we have faced while researching the 340B carveout is the lack of legitimate resources. A lot of our information was obtained through resources on the Community Health Care Association of New York State's Website and subsidized that information with the Department of Health website.
ABSTRACT #61
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE NEPHROLOGY/PULMONARY/CRITICAL CARE
GASTROINTESTINAL
Sidra Salman1, Marni Wilkoff1, Kruti Gandhi1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Iododerma is a rare, life-threatening dermatological eruption to iodine exposure in the setting of reduced renal clearance and accumulation of iodine. Iododerma commonly presents as acneiform, bullous, or hemorrhagic lesions. In rare cases, extra-dermal manifestations including mucosal involvement with gastrointestinal bleeding are seen. We report the first case demonstrating the propensity for mucosal involvement, and direct visualization of iododerma-induced gastrointestinal bullae. Given rarity of disease, lack of pathognomonic laboratory/histopathologic features, and overlap with other inflammatory and infectious etiologies, diagnosis can prove challenging, but critical. As iododerma can progress rapidly leading to fatal outcomes with significant morbidity and mortality.
CASE PRESENTATION: A 78-year-old female was admitted for acute on chronic kidney injury and pyelonephritis requiring a diagnostic CT-abdomen/pelvis with contrast. Three days later, diffuse flesh-colored umbilicated papules on the arms, face, and chest appeared, quickly progressing to large hemorrhagic bullae with mucosal involvement. Lab work including HSV-1/HSV-2, monkeypox PCR, and varicella antigen were all unremarkable, however, urine iodine was elevated. Shave biopsy showed diffuse dermatitis with neutrophils and histiocytes, with negative direct immunofluorescence. Given histopathology, differential diagnosis included iododerma, sweet syndrome, or infection. Diagnosis favored iododerma given clinical presentation with exposure in the setting of renal insufficiency and elevated urine iodine. She was treated with prednisone 1 mg/kg and her lesions began to crust over and ulcerate, though did not significantly improve. She developed recurrent melena requiring transfusions. Endoscopy revealed friable protruding bullous lesions secondary to iododerma. Her course was quickly complicated by septic shock with multi-organ failure, and recurrent gastrointestinal hemorrhage with hemodynamic instability and disseminated intravascular coagulation, leading to cardiac arrest.
CONCLUSION: Iododerma is a rare, life-threatening dermatological eruption to iodine exposure, commonly seen in renal insufficiency due to decreased clearance and accumulation of iodine. Although rare, iododerma can have extra-dermal manifestations and mucosal involvement leading to gastrointestinal bleeding. If suspected, patients should be evaluated with diagnostic endoscopy or colonoscopy. There is a lack of pathognomonic laboratory or histopathologic features, although elevated urine iodine and polymorphonuclear infiltrate with few eosinophils are supportive. Clinical features often overlap with other infectious and autoimmune etiologies including HSV, varicella, monkeypox, and bullous pemphigoid. This makes diagnosis challenging but critical, as iododerma can progress rapidly with fatal adverse outcomes including increased risk of infection in the setting of skin and mucosal barrier disruption, sepsis, multiorgan failure, gastrointestinal hemorrhage, and shock. Given the rarity of disease, there is limited data concerning the clinical features and diagnostic approach of iododerma. Furthermore, published data on the extra-dermal manifestations including mucosal involvement and risk of gastrointestinal bleeding is even more limited. Given the diagnostic challenge, the rapidly progressive nature, and significant morbidity and mortality of iododerma, there is great need for further scholarly review.
ABSTRACT #62
CLINICAL RESEARCH
GASTROENTEROLOGY
SHOULD GLUCAGON-LIKE PEPTIDE RECEPTOR AGONISTS BE HELD PRIOR TO AMBULATORY REFLUX TESTING? A RETROSPECTIVE COMPARISON OF QUANTITATIVE REFLUX TESTING RESULTS
Robinderpal Sandhu1, Alexandria Markley1, Emily S. Seltzer1, Joseph Abraham1 , Rama Hussein1, Binoy Desai1, James Choi1, Kimberly Cavaliere1,2, Yuying Luo1,2 , Michael S. Smith1,2, Daniela Jodorkovsky1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Center for GI Physiology and Motility, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
BACKGROUND/INTRODUCTION: There is great interest in use of glucagon-like peptide-1 receptor agonists (GLP-1 RAs) for weight loss, which are thought to increase satiation through delayed gastric emptying. As delayed gastric emptying is considered a risk factor for development of gastro-esophageal reflux disease (GERD), this study aims to determine whether GLP-1 RA use increases the detection of GERD on quantitative testing.
METHODS: Patients presenting to a single high-volume motility center for ambulatory reflux testing and upper endoscopy (EGD) between 1/2020 and 10/2023 were considered for inclusion. Patients taking GLP-1 RAs were identified, along with a control cohort of patients not on these medications. Patients with prior foregut endoscopic or surgical interventions were excluded. Chart review was performed to obtain demographic data, comorbidities, and medications. Positive studies for GERD were defined as having Los Angeles Grade B, Grade C, Grade D esophagitis, or Barrett’s metaplasia on EGD, and/or positive pH testing with cutoff values derived from the Lyon Consensus. Differences in demographic and clinical parameters between patients on and off GLP-1 RAs were evaluated using logistic regression, t-tests, chi-square, or Fisher’s exact tests as appropriate.
RESULTS: A total of 374 patients met inclusion criteria, of which 50 patients were on a GLP-1 RA. Patients on GLP-1 RAs had a higher body mass index (BMI), hemoglobin A1c, and were more likely to have diabetes (Table 1). GLP-1 RA users were less likely to have a hiatal hernia detected on manometry (64% versus 85%; p=0.003) GLP-1 RA use was not associated with an increase in either esophagitis (OR=1.12; 95%CI, 0.42-2.99; p=0.819), or a positive pH study (OR=1.20; 95%CI, 0.61-2.37; p=0.59) after adjusting for age, BMI, gender, and the presence of a hiatal hernia (Table 2).
CONCLUSION: In this study cohort, patients taking GLP-1 RAs were more likely to have two clinical risk factors associated with GERD, a higher BMI and diabetes. Despite these associations, patients on GLP-1 RAs were not more likely to have definitive endoscopic features for GERD, or an abnormal quantitative reflux study when compared to patients not on these medications. Increased utilization of GLP-1 RAs has brought the discussion about peri-procedure preparation to the forefront. These findings suggest there is no need to stop GLP-1 RAs in all patients prior to ambulatory reflex testing. Further analysis in larger study cohorts is essential to assess whether GLP-1 RAs affect reflux test results in specific subgroups.

Table 1: Patient Characteristics (BMI: body mass index; GLP1: glucagon-like peptide 1; EGD: Esophagogastroduodenoscopy; GERD: gastroesophageal reflux disease
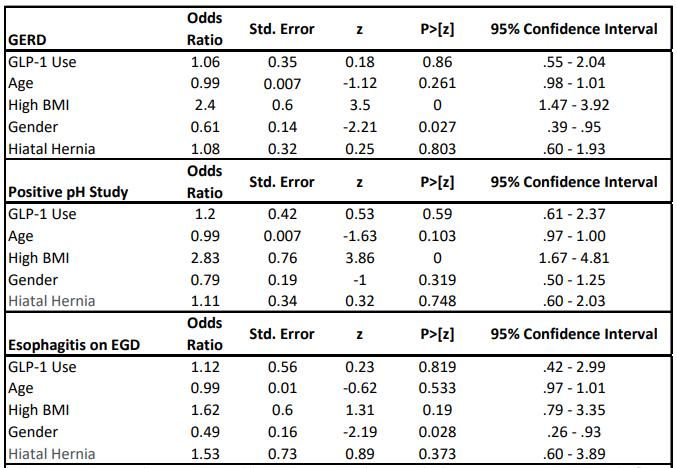
Table 2: GLP1 and association with GERD, positive pH study, and esophagitis on EGD (BMI: body mass index; GLP1: glucagon-like peptide 1; EGD: Esophagogastroduodenoscopy; GERD: gastroesophageal reflux disease
ABSTRACT #63
QUALITY IMPROVEMENT
GASTROENTEROLOGY
IMPROVING INPATIENT GASTROENTEROLOGY PERCUTANEOUS ENDOSCOPIC GASTROSTOMY TUBE REFERRALS AND OUTCOMES
Emily S. Seltzer 1, Erica Park 1, 2, Patricia Miguez Arosemena 1, Ines Varela Knorr1, Anudeep Neelam1,2 , Michael S. Smith2 , Priya Simoes1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the New York Society for Gastroenterology and Endoscopy Annual Meeting that was held in New York, New York, United States from December 14-15, 2023
BACKGROUND/INTRODUCTION: To ensure optimal outcomes and patient safety, healthcare providers must possess a comprehensive understanding of the indications and contraindications for percutaneous endoscopic gastrostomy (PEG) tube placement. Achieving appropriate patient selection necessitates interdisciplinary collaboration and engaging in patient-centered decision-making conversations centered on their goals of care. The European Society of Gastrointestinal Endoscopy recommends the implementation of pre-procedural checklists to facilitate meticulous case-by-case evaluation for enteral feeding. This quality improvement initiative sought to establish a standardized workflow utilizing a novel checklist to ensure the proper consultation with gastroenterology specialists for PEG tube placement.
METHODS: This quality improvement initiative utilized two interventions taking place from 9/1/22 to 8/30/23. Comprehensive lectures and infographics were distributed to medical residents and advanced practice providers describing indications, contraindications, techniques, and risks of PEG tube placement. An electronic medical record-based checklist was launched to guide primary care teams in patient optimization prior to consulting gastroenterology for PEG tubes. To assess improvement in PEG tubes placed by the inpatient gastroenterology service pre-intervention (6/1/2021-7/31/22) outcomes including time from consult to procedure, length of stay (LOS), 30-day mortality and PEG related complications were compared to the post-intervention group.
RESULTS: A total of 227 patients (116 pre- and 111 post-intervention) underwent PEG tube placement. Postintervention, the checklist was utilized in 69.4% of cases. Compared to pre-intervention, time between consult and placement slightly decreased in those where the checklist was used (5.30 versus 4.69 days). The most common reasons for delay occurred less frequently post-intervention (infection: 17.2% versus 9.1%, goals of care issues: 8.6% versus 5.2%, and anticoagulation: 6.0% versus 5.2%). Similarly, average LOS decreased from 57.33 days to 47.62 days. In post-intervention checklist-utilized patients, PEG tube complications occurred less frequently (17.2% versus 9.1%) and fewer patients died from any cause 30-days post procedure (11.2% versus 10.4%).
CONCLUSION: The findings of this quality-of-care study provides compelling evidence that introducing a preconsult checklist, complemented by education initiatives, enhances patient selection and optimization for PEG tube placement. The implementation resulted in a notable reduction in time from consult to procedure, LOS, in addition to the complication and mortality rates 30-day post procedure. Future endeavors involve expanding educational initiatives and optimizing patient care across other departments and institutions.
ABSTRACT #64
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE PULMONARY/CRITICAL CARE/RHEUMATOLOGY
NEWLY DIAGNOSED HEMOPHAGOCYTIC LYMPHOHISTIOCYTOSIS IN AN ADULT PATIENT WITH MULTI-ORGAN FAILURE
Priya Shah1* , Christine Lenchur1* , Rayling Herrera1*, Ira Khanna1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
*These authors contributed equally to this work.
BACKGROUND/INTRODUCTION: Hemophagocytic lymphohistiocytosis (HLH) is a multisystemic condition characterized by widespread immune system activation, leading to excessive inflammation and tissue destruction. While it commonly manifests in children, there is an increasing recognition of HLH in adults. This rare clinical syndrome is characterized by fever, hepatosplenomegaly, cytopenia, and progressive multiorgan failure. HLH is often associated with or can occur as a result of previously existing autoimmune conditions, malignancies, or infection.
CASE PRESENTATION: A 56-year-old male patient with HIV/AIDS (CD4=24), mixed connective tissue disorder, and Diffuse Large B Cell Lymphoma, presented with left-sided chest pain, cough and shortness of breath requiring oxygen. Physical exam was remarkable for bilateral axillary lymphadenopathy, confluent petechiae on trunk, diffuse edema and purpura on bilateral legs. Initial workup revealed pancytopenia, acute kidney injury, elevated CPK, INR, PTT, LDH, ferritin and transaminases (ALT 83, AST 550). CT chest showed bilateral subsegmental pulmonary embolism with possible superimposed pneumonia. He was admitted for anticoagulation, antibiotic therapy, and further infectious workup. Hospital course was complicated by spiking fevers despite broad spectrum antimicrobials, melena secondary to anticoagulation for PE and altered mental status requiring ICU level of care. The patient had ongoing pancytopenia (hemoglobin 7.7g/dL, platelets 84K/uL; ANC 1.1k/uL), ferritin 33500ng/mL, CPK 1058, and hypertriglyceridemia of 357mg/dL. Blood cultures were without growth and PCR was positive for Epstein-Barr virus (EBV). Given his fever >38.5, cytopenia with hemoglobin <9g/dL, platelets <100,000/microL; absolute neutrophil count <1000/microL, hypertriglyceridemia (fasting triglycerides >265 mg/dL) and ferritin >500 ng/mL, hemophagocytic lymphohistiocytosis was suspected. To meet 5 out of 9 diagnostic criteria, bone marrow biopsy was performed, showing hemophagocytosis, confirming HLH. Treatment was initiated with dexamethasone, but given lack of clinical response, escalated to pulse dose steroids for 5 days. Anakinra was added to dexamethasone. After an IVC filter was placed, IVIG was given for 3 days. However, the patient passed away from multi-organ failure leading to cardiac arrest.
CONCLUSION: Due to the diverse nature of HLH in terms of organ involvement and laboratory findings, it is imperative to consider the combination of predisposing medical history, clinical features, and lab findings to prevent diagnostic delays and initiate treatment since the mortality rate is 50-60%. In this case, our patient had multifactorial etiologies, including autoimmune conditions, malignancy, and viral infections such as EBV and HIV. A comprehensive physical examination is crucial, with a focus on identifying key indicators like fever, rashes, bleeding, and lymphadenopathy. Data supports the use of steroids, IVIG and Anakinra for patients with HLH. More evidence is needed about the role of plasmapheresis and Emapalumab in treating this multi-systemic disorder.
ABSTRACT #65
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/PULMONARY/CRITICAL CARE
A CASE OF CRYPTOGENIC ORGANIZING PNEUMONIA - ULCERATIVE COLITIS OR INFLIXIMAB? Venus Sharma1 , Howard Freeman1,2, Mary O’Sullivan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Infliximab is an anti-tumor necrosis factor-alpha agent approved for the treatment of moderate to severe active ulcerative colitis. This type of biological therapy has been associated with an increased risk of developing a variety of pulmonary complications, including cryptogenic organizing pneumonia. Ulcerative colitis can also lead to pulmonary complications, although this rarely manifests as cryptogenic organizing pneumonia. As such, it can be challenging to differentiate between the biological agent and the underlying inflammatory condition as the culprit for cryptogenic organizing pneumonia. Here, we present the case of a 24-year-old young patient who was started on infliximab for treatment of ulcerative colitis and subsequently developed cryptogenic organizing pneumonia
CASE PRESENTATION: A 24-year-old male presented to the emergency department with progressively worsening dyspnea. His past medical history was significant for ulcerative colitis that had been diagnosed seven years prior and Budd-Chiari syndrome treated with a transjugular intrahepatic portosystemic shunt. His medications included infliximab and rivaroxaban. Of note, the patient was admitted to an outside hospital several months prior with acute hypoxic respiratory failure, which was approximately one month after starting infliximab. Imaging at that time, demonstrated dense, bibasilar ground glass opacities. Results of a bronchoscopy with biopsy showed non-specific reactive inflammation. Stains for fungi and acid-fast bacilli were negative. Respiratory bacterial and fungal cultures were negative. The patient had low-level ANA and ANCA with no corresponding rheumatologic symptoms. He was treated with prednisone with gradual improvement in both symptoms and imaging and was tapered off the steroids. He continued to take infliximab at that time. On initial evaluation to our emergency room, he was in respiratory distress with evidence of accessory muscle use requiring nasal oxygen. A complete blood count and comprehensive metabolic profile were unremarkable. Respiratory viral panel and bacterial culture were negative. ESR and CRP were elevated. CT-chest demonstrated symmetric, multifocal, basilar predominant ground glass and consolidative opacities, concerning for recurrence of cryptogenic organizing pneumonia. He was again started on oral steroids and experienced rapid clinical improvement. The case was discussed with the patient’s outpatient gastroenterologist, and it was determined that the best course of action would be to discontinue infliximab. He was subsequently switched to vedolizumab instead.
The patient’s episode of cryptogenic organizing pneumonia was suspected to be related to infliximab given the temporal association between the initiation of infliximab and development of cryptogenic organizing pneumonia It is possible that this was instead related to his underlying ulcerative colitis, although this had been diagnosed seven years prior and he had been without any pulmonary manifestations up to this point. Since the change in therapy from infliximab to vedolizumab, he has had no evidence of disease recurrence and his respiratory status has remained stable off steroids. Vedolizumab works exclusively in the gut, suggesting that removal of the systemically active infliximab and substitution with a gut-specific biologic therapy allowed for sustained resolution of the cryptogenic organizing pneumonia and further supports the theory that the infliximab was the inciting agent.
CONCLUSION: Anti-tumor necrosis factor-alpha agents are novel biologic therapies that are currently used for a wide range of disease processes. Awareness and recognition of their potential adverse effects is vital to timely diagnosis and treatment of these complications. It is an ongoing challenge to distinguish ulcerative colitis manifesting with pulmonary involvement from infliximab toxicity. This case highlights the potential for pulmonary toxicity with the use of infliximab as well as the option of using vedolizumab under these circumstances.

 A. CT-chest at the time of infliximab initiation
A. CT-chest at the time of infliximab initiation
ABSTRACT #66
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
AN ATYPICAL PRESENTATION OF ARRHYTHMOGENIC RIGHT VENTRICULAR CARDIOMYOPATHY WITH CONCOMITANT STROKES
1
Samantha V. Shetty1
, Chad Henry1, Justin Goodfarb1, Michael Bourne1, Basera Sabharwal1 Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United StatesBACKGROUND/INTRODUCTION: Arrhythmogenic right ventricular cardiomyopathy (ARVC) is a rare inherited cardiomyopathy characterized by the deposition of fibroadipose tissue within the walls of the right ventricle (RV). Initially considered to be a RV dominant cardiomyopathy, there has been increased work which suggests that ARVC likely has biventricular involvement. Now considered to fall within a spectrum of arrhythmogenic cardiomyopathies, ARVC is primarily inherited in an autosomal dominant fashion, however, there have been rare instances in which ARVC has been inherited in an autosomal recessive fashion as well. Most commonly the pathophysiology of ARVC affects the cardiac desmosome protein. Given the role of cardiac desmosome proteins in cell-to-cell adhesion, the pathogenesis of ARVC is mediated by deficits in cell adhesion which subsequently predispose cardiac cells to injury and cell death, particularly in times of increased cardiac stress such as intensive exercise. Ultimately, cardiac cell death leads to loss of myocardium and enables fibroadipose tissue deposition, providing the substrate for ventricular arrhythmias and in some cases, sudden cardiac death. Given the manifestation of ARVC in predominantly healthy patients and its varying nonspecific manifestations, it is important for clinicians to not just appropriately identify, but also manage the care of patients with ARVC. In this case presentation, we share a unique case in which a young male presented after sustaining two witnessed cardiac arrests and was found to have ARVC with RV phenotype and concomitant small acute right thalamic and right cerebellar infarcts in the setting of patent foramen ovale (PFO).
CASE PRESENTATION: A 22-year-old male presented to the Emergency Department (ED) after a witnessed collapse while he was playing a game of basketball. Cardiopulmonary resuscitation (CPR) was initiated in the field by a bystander, who was reportedly a physician. Upon the arrival of emergency medical services (EMS) on the scene, the initial rhythm was identified as ventricular fibrillation and the patient received 2 shocks, intravenous Amiodarone 300 mg, and 2 doses of epinephrine. Shortly thereafter, the patient went into pulseless ventricular tachycardia and CPR was continued for 15minutes until return of spontaneous circulation (ROSC) was achieved. Given concerns regarding the patient’s ability to secure his airway, the patient was intubated in the field and sent to the ED. Upon arrival to the ED, the patient suffered another cardiac arrest at which time CPR was initiated and ROSC was achieved with 1 round of CPR and 1 dose of epinephrine. An initial bedside point-of-care ultrasound was notable for left ventricular ejection fraction of 40% and diffuse hypokinesis with a notable hypokinetic right ventricle. Given his collapse, a non-contrast CT-head without contrast was completed and did not show any signs of acute pathology including intracranial hemorrhage or acute territorial infarction. A CTchest without contrast was notable for dense bilateral lower lobe opacities and right lung ground glass opacities. His initial electrocardiogram (EKG) on arrival was notable for ST elevations across anterior wall leads (V1-V3). A high-sensitivity troponin collected on arrival was 193 and ultimately peaked at 27,138 throughout the course of his admission. The patient was then emergently taken to the cardiac catheterization lab for a left heart catheterization which demonstrated normal coronary arteries, normal left ventricular end diastolic pressure, and mild left ventricular systolic dysfunction. He was then transferred to the coronary care unit (CCU) for post cardiac arrest management. A formal transthoracic echocardiogram was notable for an ejection fraction of 50%, paradoxical septal motion, lateral wall hypokinesis, and right ventricular dilation and hypokinesis. The patient’s CCU admission was further complicated by episodes of acute onset confusion and retrograde amnesia. Given concerns for underlying neurological pathology, an MRI-brain was ordered and demonstrated recent small infarcts in the right thalamus and right cerebellum/vermis. To rule out a cardioembolic source of these infarcts, a transesophageal echocardiogram was performed and was significant for small patent foramen ovale (PFO). A cardiac MRI was then performed and demonstrated moderate right ventricle dilatation, moderate right ventricular
systolic dysfunction, akinesis of the right ventricular free wall, and microaneurysms on the mid to apical RV free wall. Additionally, there was a large amount of transmural late gadolinium enhancement of the right ventricular free wall and free lateral wall. These findings met two of the major criteria for the 2023 Padua Criteria for arrhythmogenic cardiomyopathy; namely: 1) low right ventricle ejection fraction with associated regional wall motion abnormalities of the right ventricle and 2) late gadolinium enhancement of the right ventricle. The patient opted for the elective placement of subcutaneous implantable cardioverter defibrillator (ICD) for secondary prevention of cardiac death. The patient was then subsequently transferred to the general medicine floor, where he was ultimately discharged home with a beta blocker, instructed to follow up with the inherited cardiomyopathy specialist and genetic counselor, and arranged for PFO closure given his young age. Upon further exploration of the patient’s family history, the patient stated that his sister, age 23, had a recent hospitalization for cardiac symptoms and a younger brother, aged 16, who experienced at least one syncopal episode while playing basketball himself. The patient was recommended for genetic testing through a comprehensive arrythmia and cardiomyopathy panel. His genetic testing identified a pathogenic variant of the PKP2 gene, which is associated with an autosomal dominant ARVC. The patient was extensively counseled on the adverse role of exercise in ARVC, particularly in ARVC mediated by a PKP2 mutation, and the importance of beta blocker use.
CONCLUSION: In this case presentation, we share the presentation of a seemingly healthy young male with an insignificant past medical history who was ultimately found to have a rare inheritable arrhythmogenic cardiomyopathy that was further complicated by the presence of small thalamic and cerebellar strokes in the setting of a PFO. Given that ARVC is the second most common cause of sudden cardiac death in young people under the age of 35, it is incumbent on clinicians to consider ARVC in their differential diagnosis for patients who present with arrythmias. Lastly, this case underscores the importance of appropriate genetic testing and routine counseling ARVC patients to avoid rigorous exercise.
ABSTRACT #67
CLINICAL RESEARCH
GENERAL INTERNAL MEDICINE
Jorge Sinclair De Frias1 , Pablo Moreno Franco2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mayo Clinic, Jacksonville, Florida, United States
BACKGROUND/INTRODUCTION: Frailty, an indicator of unsuccessful aging, is a geriatric syndrome characterized by deficits in multiple domains such as mobility, strength, and cognition, which increases the risk of hospitalization, and longer hospital stays. Previous studies have established a connection between frailty and an increased risk of thrombotic events. Despite this known correlation, focused research on outcomes postpulmonary embolism in frail patients is lacking. Our study aims to address this knowledge gap by investigating outcomes of frailty following pulmonary embolism. Our findings are positioned to improve patient care by guiding healthcare professionals in customizing their management strategies for this vulnerable population.
METHODS: Using the National Inpatient Sample database, we analyzed PE hospitalizations during the years 2017-2019 and categorized patients by frailty risk based on the Hospital Frailty Risk Score (HFRS) and using the ICD-10. Multivariate logistic regression was conducted to determine adjusted odds ratios (aOR) for all outcomes.
RESULTS: A total of 288,070 patients diagnosed with pulmonary embolism were analyzed in this study. These patients were stratified into low-risk (57.5%, n=165,820), medium-risk (39.9%, n=114,965), and high-risk (2.5%, n=7,285) categories. High frailty risk patients were characterized by advanced age, female gender, African American ethnicity, and a higher mean Charlson comorbidity index. Additionally, they were more likely to reside in areas with lower median household incomes and were less frequently admitted to smaller hospitals and nonteaching institutions. In comparison to patients with low frailty risk, those with medium and high frailty risk have increased odds of in-hospital mortality (Table 1). The discriminating ability of HFRS in predicting mortality using a receiver-operator curve (ROC) showed an area under the curve (AUC) of 0.7796 (Figure 1). Multivariate analysis also revealed that both medium and high frailty risk were significantly associated with increased odds for systemic thrombolysis, catheter-direct therapies, inferior vena cava filter, invasive mechanical ventilation, vasopressor use, intensive care unit admission, sudden cardiac death, acute kidney injury, cardiogenic shock, and prolonged hospital length of stay. Notably, individuals with a median frailty risk, rather than those with a high frailty risk, exhibited increased odds of undergoing mechanical thrombectomy.
CONCLUSION: In conclusion, the association between frailty and higher in-hospital mortality rates, coupled with a worsened clinical course, highlights the relevance of frailty as a crucial factor in pulmonary embolism outcomes. The Hospital Frailty Risk Score emerges as a potential predictor of mortality in this patient population. Our findings stress the necessity for more granular studies that delve deeper into the intricacies of frailty in guiding care strategies, ultimately aiming to enhance outcomes for individuals with frailty and pulmonary embolism.

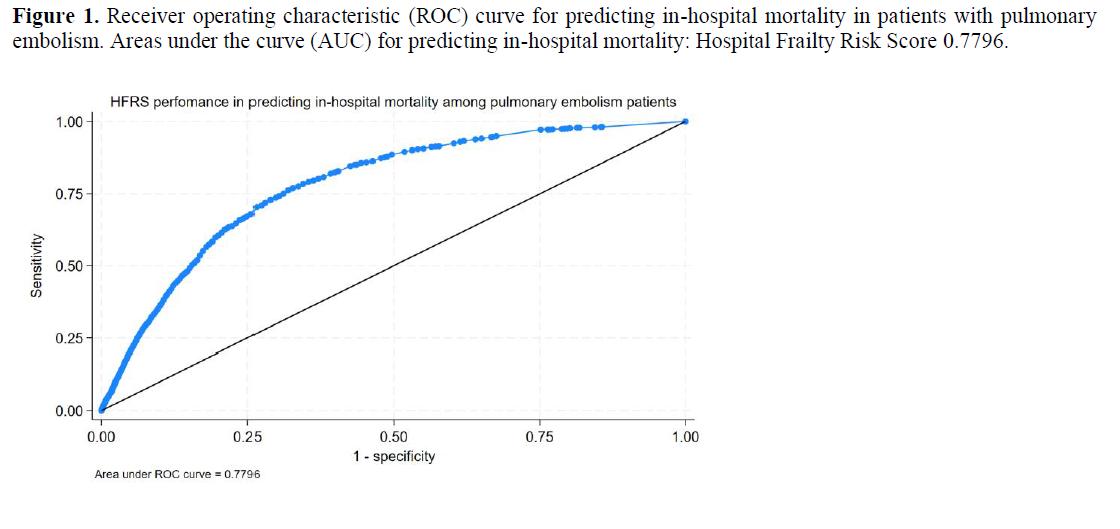
ABSTRACT #68
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
MEDIASTINAL ANGIOLIPOMAS: AN EXCEEDINGLY RARE PATHOLOGY
Connor Smith1 , Steven Lim1,2 , Daniel Nicastri1, Mary Beasley1, Daniel Chung1, Boram Kim1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: Angiolipomas are a class of rare benign neoplasm most often arising from subcutaneous tissue and muscles of the extremities or superficial trunk. Only 5 to 17% of all lipomas are angiolipomas. Angiolipomas are most common in males between the ages of 20 and 30. Primary mediastinal angiolipomas are exceedingly rare, with only 10 documented in the literature worldwide, nine of which were described in the posterior mediastinum. To the best of our knowledge, ours is the first reported case of angiolipoma with central necrosis. Here we present the 11th reported case of a mediastinal angiolipoma.
CASE PRESENTATION: A 60-year-old female with chronic glaucoma, a prior transient ischemic attack, obstructive sleep apnea on BIPAP, and a history of parathyroidectomy for hypercalcemia, presented to the emergency department with two weeks of intermittent heart palpitations and chest pressure. Initial chest radiography showed a small left-sided pleural effusion and focal consolidation. Follow-up CTA showed a pulmonary embolism in the upper lobar branches of the right pulmonary artery without evidence of right heart strain. Unexpectedly, the scan also revealed an incidental 3.4 x 3.1 cm posterior mediastinal mass that was further imaged with MRI, which showed central necrosis. The patient was admitted to the hospital for management of the pulmonary embolism and treated with an intravenous infusion of heparin that was later transitioned to low-molecular-weight heparin injections and eventually a direct oral anticoagulant on discharge. A CT-guided biopsy of the incidental mass was performed by the Interventional Radiology team. Pathology revealed an adipocytic neoplasm with prominent vasculature, consistent with angiolipoma. A multidisciplinary tumor board discussion was held, with the initial recommendation being surveillance imaging. However, on repeat assessment with physicians from Thoracic Surgery and Radiology, the decision was made to resect the mass due to three concerning factors: the central necrosis, the paucity of lipid seen on MRI, and the pleural effusion. The board agreed that each of these features imparted a higher risk of malignancy. The mass was successfully resected in a combined procedure with the Thoracic and Vascular Surgery teams. Pathology confirmed the diagnosis of a benign angiolipoma and pleural fluid studies showed benign cells.
DISCUSSION/CONCLUSION: Patients with mediastinal angiolipomas are extremely rare and the presenting complaint can be varied. The limited literature shows that mediastinal angiolipomas mostly arise paraspinally within the posterior mediastinum for reasons that are unclear. The most common tumors in this space are neurogenic tumors such as schwannomas and less commonly chordomas, paragangliomas or neurofibromas, all of which should remain on the differential diagnosis until a tissue sample can be obtained. If a mediastinal angiolipoma is pathologically diagnosed via biopsy prior to proceeding with resection, optimal management and need or urgency for resection is difficult to establish due to the lack of published literature to provide guidance. Due to the three alarm features of the mass as described above, our case was discussed in a multidisciplinary group consisting of a broad range of specialists: Thoracic Surgery, Pathology, Thoracic Radiology, Pulmonology, and Interventional Radiology. There are significant benefits to this form of discussion as different specialties may offer their own distinct perspectives on the details of the case. Angiolipomas are known to be benign masses, but if they grow large enough to cause significant symptoms it may be reasonable to resect them. The benefits of treatment, however, must always be weighed against the significant risk these resections pose when the tumor is nestled within the richly vascular mediastinum. In our case, the extensive quantity of feeder arteries arising from the aorta prompted the inclusion of a vascular surgeon in the operating room to advise on a secure plane of resection to prevent significant bleeding. This interdisciplinary approach led to minimal blood loss and zero complications during the procedure, In summary, this case adds to the sparse literature of mediastinal
angiolipomas and offers potential guidance for future cases. The choice of resection versus surveillance should be based on the tumor size, location, symptom burden and high-risk features. Based on our review and experience, we recommend a multidisciplinary discussion surrounding the location, radiological anatomy, pathology and high-risk features.
ABSTRACT #69
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PULMONARY/CRITICAL CARE
RARE CASE OF ACUTE HYPOXIC RESPIRATORY FAILURE DUE TO TRAUMATIC TAPIA SYNDROME REQUIRING TRACHEOSTOMY
Vincent Torelli1 , Raymonde E. Jean1, Elena Tran2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2New York Presbyterian Brooklyn Methodist Hospital, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: Tapia syndrome is a rare disease characterized by a lesion outside the central nervous system that causes cranial nerve symptoms. Typically, a complication of airway manipulation during orotracheal intubation, Tapia syndrome manifests as unilateral vocal cord paresis, tongue deviation, and dysphagia, resulting from paralysis of the hypoglossal and the recurrent laryngeal branch of the vagus nerve. We present the first case of Tapia syndrome secondary to trauma of the cervical spine.
CASE PRESENTATION: An 80-year-old female with hypertension presented with neck pain following a mechanical fall without loss of consciousness. Patient reported that she tripped and fell, landing anteriorly on her forehead, hyperextending her cervical spine. Vital signs were stable on admission, physical exam revealing for large hematoma on forehead, right sided tongue deviation, negative for peripheral weakness or sensation loss. At this time, patient did not require supplemental oxygen. CT-spine revealed a type II dens fracture, C1 posterior arch fracture with minimal subluxation of left atlanto-occipital joint, multiple rib fractures. CT-head was without acute intracranial abnormality. CT-angio neck revealed medialization of right vocal cord. MRI-brain unrevealing for infarct, intracranial mass or hydrocephalus. MRI-C-spine unrevealing for spinal cord compression, disc herniation, stenosis, spinal cord edema or myelomalacia. MRA-head and neck without evidence of significant stenosis affecting cranial vasculature. Neurosurgery opted for conservative management of spinal fracture with cervical collar, however patient’s hospital course complicated by hypophonia and dysphagia requiring percutaneous endoscopic gastrostomy (PEG) tube placement. Following PEG procedure, patient was extubated, however oxygen saturation maintained <70%, and was immediately re-intubated. She repeatedly passed spontaneous breathing trials while on ventilator support, however, upon extubation, again experienced acute hypoxic respiratory failure requiring re-intubation. Chart review revealed that the patient had never been intubated before and had no prior history of lung pathology. Patient underwent tracheostomy and received a steroid taper for Tapia syndrome.
CONCLUSION: Given lack of prior history of lung pathology and extensive neuroimaging unrevealing for other causes of vocal cord paresis, acute hypoxic respiratory failure was attributed to Tapia syndrome sustained from fall. Peripheral stretch of her cranial nerves resulted in the inability to ventilate adequately due to her paralyzed vocal cord, however shewas able to respirate when the vocal cord wasmechanically opened by the endotracheal tube. Both tongue deviation and vocal cord paresis was noted on imaging prior to initial intubation during the PEG procedure, ruling out any damage during intubation.
ABSTRACT #70
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
THE CASE OF THE PSEUDO-PSEUDO POLYP: FIRST REPORTED CASE OF A SPINDLE CELL SARCOMA AT AN ILEOCOLONIC ANASTOMOSIS
Ines Varela Knorr1, Jennifer Claytor2 , James Marion2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
BACKGROUND/INTRODUCTION: Anastomotic inflammatory polyps are an uncommon source of gastrointestinal bleeding in patients who have undergone bowel resection, but a malignant anastomotic source of chronic anemia has never been reported. We present the case of a patient with occult gastrointestinal bleeding six years after an ileo-colic resection for an incarcerated hernia.
CASE PRESENTATION: A 58-year-old female was admitted to the hospital for symptomatic anemia, primarily fatigue, without overt bleeding. Six years prior, she underwent hysterectomy for fibroids, which was complicated by a perforated, incarcerated incisional hernia requiring an ileocolic resection with lysis of adhesions. At the time of admission, she was hemodynamically stable and was found to have had an 8-point decrease in hemoglobin over 6 months. Inpatient colonoscopy revealed a white, nodular, semi-pedunculated 35mm polyp at the ileocolonic anastomosis (Figure 1). The polyp was presumed to be inflammatory and was removed using hot snare polypectomy which revealed a pigmented spot at the base. Unexpectedly, pathology revealed a spindle cell sarcoma with myogenic differentiation, suspicious for myxoid leiomyosarcoma, FNCLCC grade 2 (Figure 2). Metastasis from a uterine primary tumor could not be excluded given her reported surgical history. Computerized tomography scans excluded distant metastasis, and she underwent secondary ileocolic resection. The pathology of the resected bowel showed no residual spindle cell sarcoma and negative lymph nodes, stage T1N0Mx. At follow-up, she felt well with no recurrence of anemia. Given her low grade and absent metastatic disease, we elected to repeat cross-sectional imaging at 6 months after her initial resection.


CONCLUSION: Post-surgical polyp growth at an anastomotic site is an uncommon complication of bowel resection. This is the first case of spindle cell sarcoma with myogenic differentiation reported in the colon. We can only extrapolate from the existing literature on this rare entity which has compared the clinical courses of non-gynecologic leiomyosarcomas and sarcomas with myogenic differentiation, which are similar and driven by grade of tumor regardless of initial site. Notably, 14% of patients with low-grade tumors had no recurrence or progression at 8 years. In medium-to-high grade tumors, 38% had distant metastasis at 8 years, with a 66% overall survival rate. Chemotherapy is recommended for recurrent uterine leiomyosarcoma and has sometimes been used for colonic leiomyosarcoma, although these tumors are often rapidly progressive and poorly responsive.
Figure 1. Figure 2.ABSTRACT #71
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
INTERHOSPITAL TRANSFER FOR ACUTE PULMONARY EMBOLISM: INVESTIGATION OF PROCESS METRICS, AND IMPACT OF TRANSFER TIMES IN DECISION MAKING AND OUTCOMES
Avinash Singh1 , Priyanka Sridhar2 , Hong Yu Wang2 , Agostina Velo1 , Destiny Nguyen2 , Madeline Ehrlich2 , Abdul Rehman3, Robert Lookstein4, Samuel Acquah4, David Steiger1,2
1Mount Sinai Morningside-West Hospitals, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Rutgers New Jersey Medical School, Newark, NJ, United States; 4Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: Interhospital transfer (IHT) for patients with acute life-threatening pulmonary embolism (PE) is increasingly performed to facilitate expert care and provide access to potential advanced reperfusion therapies. IHT has previously been studied for acute trauma, ST-elevation myocardial infarction, and stroke patients. Qualitative studies have noted that transfer delays may compromise patient safety. Data supporting optimal transfer times that are associated with improved outcomes has not been identified
METHODS: We performed a retrospective review of consecutive patients who underwent IHT for acute PE management, facilitated by a multidisciplinary Pulmonary Embolism Response Team (PERT) serving a multicenter tertiary hospital system, from September 2021 through June 2023. Transfers from referring “out-ofsystem" hospitals were included, if admission records were complete. Total Length of Stay (LOS) comprised of ER arrival-to-diagnosis of acute PE, IHT evaluation time (pretransfer), IHT time, and time-to-procedure. Using these variables, we calculated diagnostic Chest CTA-to-Procedure, ER arrival “Door-to-PERT", and ER arrival “Door-to-Procedure" related procedure times.
RESULTS: 139 patients were included in our study. Nine (6.5%) patients were out-of-system transfers. The majority (88.4%) of patients requiring IHT were classified as Intermediate Risk (IR) according to the European Society of Cardiology (ESC) guidelines. Mean time to diagnosis for acute PE was six hours (SD, 7h 46m). Average time for PERT consultation and preparation for IHT was 4 hours (SD, 8h 28m), with time required for IHT being eight-and-half hours (SD, 12h 51m). For patients who received advanced reperfusion therapies (Catheter Directed Embolectomy or Thrombolysis, Surgical Embolectomy, n=34), average time from diagnosis of acute PE and intervention for PE was 29 hours (SD, 1d 19h). On subgroup analysis, out-of-system transfers had longer wait times to PE diagnosis, longer IHT preparation, longer IHT travel time, and time-to-intervention. The time taken to achieve transfer was not associated with either the patients receiving advanced therapies, or mortality. The most common IHT complication was worsening hypoxemia (n=30, 21.6%), followed by worsening shock (n=1, 0.7%). Patients who had worsening hypoxemia during transfer (n=30, 21.6%), were more likely to receive advanced therapies (OR, 1.22; p=0.03).
CONCLUSION: Interhospital transfers are safe; time from evaluation in the ER to intervention can be variable; and out-of-system referrals for IHT transfers were associated with longer IHT travel time. The timing of transfer did not impact the decision to perform advanced therapy and/or mortality. Further studies are required to determine whether reducing the total time taken to transfer patients following acute PE may result in improved outcomes.
ABSTRACT #72
CLINICAL RESEARCH
ALLERGY/IMMUNOLOGY/PULMONARY/CRITICAL CARE
MARKERS OF COMMON VARIABLE IMMUNODEFICIENCY RELATED INTERSTITIAL LUNG DISEASE ACTIVITY
Brit Trogen1 , Julia Jacob1, Code Demarco1, Adam Jacobi1 , Megha Verma2, Hsi-En Ho1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024
BACKGROUND/INTRODUCTION: Common variable immunodeficiency related interstitial lung disease (CVIDILD) and granulomatous and lymphocytic interstitial lung diseases (GLILD) are severe non-infectious complication of CVID, believed to result from systemic immune dysregulation. Despite extensive morbidity and mortality associated with CV-ILD/GLILD, best practices for screening and evaluation are under investigation.
METHODS: In this retrospective cross-sectional study, 42 adult patients with CVID and radiologic features of ILD were enrolled. Available high-resolution chest CTs (n=23) were scored by a Radiologist using a validated scoring metric. CTs were evaluated based on pathologic findings in the airway and lung interstitium. Pulmonary function test (PFT) results and pertinent clinical findings were assessed for correlation with imaging severity.
RESULTS: The percentage of patients with predominant disease findings in the airways and interstitium were 52% (n=12) and 43% (n=10), respectively. Common radiographic findings included bronchial wall thickening (91.3%), mucus plugging (91.3%), and bronchiectasis (73.9%). Interstitial findings included lung nodules (91.3%), linear/irregular opacities (95.6%), and groundglass opacities (73.9%). Patients in this study also demonstrated high prevalence of splenomegaly (83%), autoimmune cytopenias (54%), and low IgA serum levels at CVID diagnosis (100%). Spearman’s rank correlation was performed which found that CT-derived scores of disease severity had no statistically significant correlation with PFT results (FEV1, FVC, FEV1/FVC, or DLCO), presence of autoimmunity, IgG at diagnosis, or GLILD diagnosis.
CONCLUSION: Radiographic severity of ILD in this sample of adult CVID patients did not correlate with other clinical measures, including recent performance on PFTs. Results were limited by small sample size, and additional data collection is underway.
ABSTRACT #73
CLINICAL RESEARCH
GASTROENTEROLOGY
EVALUATING THE ACCURACY AND ACCEPTANCE OF AN ARTIFICIAL INTELLIGENCE-GENERATED COLONOSCOPY BOWEL PREPARATION PROMPT
Marni Wilkoff1, Nicholas Piniella2, Rashmi Advani3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Institute of Technology College of Osteopathic Medicine, Old Westbury, NY, United States; 3Mount Sinai South Nassau Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting that will be held in Washington, D.C., United States from May 19-21, 2024.
BACKGROUND/INTRODUCTION: Colorectal cancer (CRC) is the third most common cancer in the United States, with colonoscopy being the preferred screening method. Adequate bowel preparation is crucial for a successful colonoscopy, though up to 25% of colonoscopies are associated with poor preparation, leading to prolonged procedure time, repeat colonoscopies and decreased adenoma detection. ChatGPT has been used to answer patient questions about colonoscopy and for post-colonoscopy management, but this is the first study assessing the accuracy of a ChatGPT-generated pre-colonoscopy preparation prompt.
METHODS: We used ChatGPT to generate a response to the following prompt: “explain colonoscopy preparation to a patient using split dose preparation.” A REDCap survey was emailed to 208 gastroenterologists to rate the prompt for the following indicators on a 4-point Likert scale: comprehensibility, scientific accuracy, and agreement with the prompt. Reviewers were asked to interpret if the prompt was generated by artificial intelligence (AI) or a human. The reading level of the prompt was measured using the Flesch-Kincaid Grade Level and Gunning Fog Index obtained from an online readability tool (readable.com).
RESULTS: Forty four of 208 gastroenterologists completed the survey (21%). Most participants determined that the prompt was easy to understand (91%), scientifically accurate (95%), and were comfortable giving the prompt to their patients (66%) (Table 1). Most reviewers (68%) felt the prompt was better or about the same as the prompt currently used in their practice. Nineteen reviewers had at least one issue with the prompt (43%), of which most common issues were the prompt being too generic and long, no mention of NPO status or dietary and medication recommendations (Figure 1). The prompt scored 9.0 on the Flesch-Kincaid Grade Level and 15.7 on the Gunning Fog Index. Reviewers demonstrated 64% accuracy in identifying the AI-generated answer, but most (68%) were not confident in their answer.
CONCLUSION: This study demonstrated the ability of ChatGPT to create a pre-colonoscopy preparation prompt that most gastroenterologists were comfortable giving to patients. All fellows felt the prompt was easy to understand and scientifically accurate, while sixteen attending Gastroenterologists disagreed with several aspects of the prompt. These findings can be due to attending Gastroenterologists having more experience and ability to detect smaller inaccuracies than fellows. While most reviewers felt the prompt was easy to understand, the reading level was more advanced than the recommended 6th grade reading level by the American Gastroenterology Association, a possible reason patients may have poor bowel preparation. In the future, we will use similar scales to compare this AI-generated prompt to a prompt that is regularly distributed to patients in our hospital system with the goal of creating a standardized and easy to understand prompt.
Table 1: Assessment of Quality Indicators
Participants who agreed with the following statements – no. (%)
Characteristics
“The prompt is easy to understand” “The prompt is scientifically accurate” “I am comfortable giving this prompt to my patients”
1: Reasons for Disagreement with the Prompt

Table 2: Participants Who Believed the Prompt was Created by Artificial Intelligence versus Human
ABSTRACT #74
CLINICAL RESEARCH
GASTROENTEROLOGY
PATIENT-LEVEL FACTORS DO NOT IMPACT THERAPEUTIC ESCALATION IN CHRONIC CONSTIPATION
Ahmun Zafar1 , Joseph A. Menand1, Robinderpal Sandhu1, Yonatan Israel2, Emma Reford2, Kimberly Cavaliere1 , Priyanka Singh1, Jean Saleh1,3, Michael S. Smith1,3, Yuying Luo1,3, Daniela Jodorkovsky1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Center for GI Physiology and Motility, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Dyssynergic defecation is the inability to coordinate the abdominal and pelvic floor muscles to evacuate stools. Dyssynergic defecation affects up to half of patients suffering from chronic constipation. Anorectal manometry (ARM) is essential for the diagnosis of dyssynergic defecation, as it assesses the coordination of pelvic floor and anal sphincter muscles during bowel movements. Prior to undergoing ARM for chronic constipation, treatment guidelines for patients initially recommend lifestyle modifications, followed by over the counter (OTC) medications and then prescription medications. It has not previously been studied whether patient-level factors correlate with who is escalated on therapies. It is also unclear if there are higher rates of dyssynergic defecation in patients who require further escalation of care to prescription laxatives prior to being referred for ARM.
METHODS: A retrospective study of all consecutive patients who underwent ARM between 2021-2022 at one tertiary center with motility expertise was performed. Baseline patient characteristics (age, race/ethnicity, body mass index, English as a primary language, and insurance status) were compared with Chi-squared and Fischer’s Exact Test. Our primary outcomes were patient-level differences in those who were laxative-naïve or offered lifestyle modifications only, OTC only, and prescription medications. Secondary analysis included differences in ARM findings between these groups.
RESULTS: We included 130 patients with documented medication use prior to ARM for chronic constipation or difficulty evacuating. Of this cohort, 90% were offered some form of lifestyle modification prior to ARM, specifically 80.8% were recommended fiber. There were no significant differences in patient characteristics between laxative-naïve patients (n=19), those trialed on OTC (n=43) and prescription medications (n=68) (Table 1). There were no differences between the groups for presence of dyssynergia on ARM; however, the laxativenaïve group had significantly higher rates of rectal hyposensitivity (p=0.003) compared to the OTC and Rx group.
CONCLUSION: Biofeedback therapy remains the mainstay treatment of dyssinergic defecation, and studies have shown that biofeedback is superior to laxatives in the treatment of pelvic floor dyssinergia. However, laxatives can be effective and be used as an adjunctive treatment. Newer prescription medications for constipation, such as linaclotide, lubiprostone, and prucalopride, which are approved for the treatment of both IBS-C and chronic idiopathic constipation, have not been assessed in dyssinergic defecation. As there were no differences in the presence of dyssynergia on ARM between laxative-naive patients and those on prescription laxatives in our study, if there is clinical suspicion for an evacuation disorder, perhaps providers should not feel obligated to escalate patients to prescription laxatives before referring for ARM. Reassuringly, our study did not find any patient-level differences between patients based on whether they had been on OTC or escalated to prescription treatments, suggesting that socioeconomic level differences do not guide pharmacologic decisions in managing chronic constipation. While patients on OTC laxatives may be self-medicating rather than following a provider’s recommendations, it is still unclear why certain patients are offered prescription laxatives prior to
undergoing ARM while others are immediately recommended for ARM. However, this may be multifactorial and due to severity and duration of symptoms, or if patients have symptoms that are reminiscent of IBS-C. Limitations of our study include the relatively small sample size and the inherent limitations in retrospective data.
Table 1: Demographics of patients between laxative naïve, OTC laxative and RX laxative groups.
Table 2: ARM findings of patients across laxative naïve, OTC laxative and RX laxative groups.
Findings
ABSTRACT #75
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
EVALUATING THE ROLE OF DAY 14 BONE MARROW BIOPSY AND EUROPEAN LEUKEMIA NET RISK CLASSIFICATION IN PREDICTING OVERALL AND RELAPSE-FREE SURVIVAL IN ACUTE MYELOID LEUKEMIA
Franc Metodi Balev1 , Victor Zibara2 , Grace Van Hyfte1, Jonathan Feld1, Marina Kremyanskaya1, Michelle Becker1, Alla Keyzner1, Alan H. Shih1, Bridget Marcellino1, Hannah Levavi1, Lewis Silverman1 , John Mascarenhas1, Douglas Tremblay1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai MorningsideWest Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
BACKGROUND/INTRODUCTION: The most recent National Comprehensive Cancer Network (NCCN) guidelines for acute myeloid leukemia (AML) patients undergoing cytarabine-based induction therapy recommend the performance of a bone marrow biopsy 14 – 21 days after the initiation of therapy. These “day 14” bone marrow biopsies (D14 BM Bx) are routinely performed to assess early response to induction therapy. The presence of residual disease (RD), defined as an elevated marrow cellularity >20% and/or blast counts >5%, has been shown in several studies to be associated with a decreased rate of complete remission (CR) at day 28.This lower likelihood of CR with RD on D14 BM Bx has been utilized to justify the pursuit of prompt reinduction therapy for many AML patients. These efforts have been galvanized by prior studies that suggest similar long-term outcomes for AML patients regardless of whether they achieve CR with one or two induction cycles. However, in recent years, both the prognostic value of D14 BM Bx and the clinical utility of reinduction decisions based on its findings have been called into question. Several studies have suggested that up to onethird of patients with RD at D14 can go on to achieve CR without reinduction therapy. Although prospective trials have been conducted in which reinduction therapy is selectively administered to patients with higher blast counts on D14 BM Bx, there is still a paucity of randomized clinical trial data to indicate whether reinduction for D14 RD confers any benefit to major clinical endpoints such as overall survival (OS) or relapse-free survival (RFS). The prognostic limitations of D14 BM Bx underscore the concern that patients with delayed response who would have otherwise achieved CR without reinduction therapy may be unnecessarily exposed to additional chemotherapy and its associated risks; however, it remains one of the few post-treatment variables currently available to guide decisions regarding the course of induction therapy. Although its limitations in isolation are well appreciated, it remains unclear whether the degree of chemoresistance reflected in D14 RD may be able to independently inform the clinical heterogeneity that is still observed in other widely validated prognostic criteria such as European Leukemia Net (ELN) risk classification. To explore this question, we performed a retrospective review of AML patients who received induction chemotherapy and determined the prognostic impact of D14 BM Bx results stratified by ELN risk group and receipt of reinduction therapy on CR, OS, and RFS.
METHODS: This study was approved by the Program for Protection of Human Subjects (PPHS) at the Icahn School of Medicine at Mount Sinai. We retrospectively identified adult patients with AML who received intensive induction therapy with a “7 + 3” (cytarabine and an anthracycline) regimen and D14 BM Bx (performed 14-21 days after initiation of induction therapy) at Mount Sinai Hospital from January 2009 to July 2022. Relevant clinical, pathological, and laboratory data were gathered via review of electronic health records, and patients were retrospectively classified according to the 2022 ELN risk stratification guidelines using available cytogenetic and molecular characteristics. Characteristics for patients with residual disease, defined as either ≥ 20% cellularity and/or ≥ 5% blasts, and no evidence of disease (NED) on D14 BM Bx were compared using MannWhitney test for continuous variables and the chi-square test for categorical variables. The Kaplan-Meier method was used to estimate the median times to the NED vs RD at D14 BM Bx and additionally among the ELN risk classification groups at outcomes for OS and RFS, with corresponding 95% confidence intervals (CI) using the method of Brookmeyer and Crowley. Comparisons of time to event distributions between groups were made with the log-rank test. Comparisons were made between baseline. Univariable and multivariable Cox proportional
hazard regression models were used to estimate the hazard ratios (HRs) and corresponding 95% CIs for mortality and relapse. The univariable models were used to determine which covariates should be kept in the multivariable models. The p-value was set at 0.05 for significance. For all survival analyses, patients were censored at last follow-up, date of death, or time of hematopoietic stem cell transplantation (HSCT), whichever occurred first. All statistical analyses were done using SAS v9.4 (SAS Institute, Cary, NC).
RESULTS: Among those with RD at D14, 56 patients (64%) received reinduction therapy. 42 patients (75%) were treated with an intensive regimen and 14 patients (25%) were treated with a non-intensive regimen (azacitidine/decitabine monotherapy or in combination with venetoclax). When comparing baseline characteristics of patients with RD, those who received reinduction had higher rates of intermediate/adverse risk AML (p=0.01) and higher median D14 blast percentage (36% versus 6%, p<0.01) and cellularity (30 versus 20%, p=0.04) compared to those who did not. Those who received reinduction therapy were more likely to achieve a CR (86 versus 63% without; p=0.02). There was no statistically significant difference in median OS between patients with NED and RD at D14 (3.8 versus 1.4 years; p=0.28). Among patients who achieved CR, those with NED had an increased median RFS (2.6 versus 0.8 years; p=0.01). Within individual ELN risk classes, we did not observe a difference in OS when stratified by D14 disease status. Among patients with intermediate risk disease, those with NED at D14 had a longer RFS (2.6 versus 0.5 years with RD; p=0.03). Neither of the aforementioned RFS differences remained statistically significant when censoring at time of stem cell transplantation (SCT) was not performed (p=0.24 and 0.22 respectively). There was no difference in RFS among patients with favorable or adverse risk disease when stratified by D14 disease status regardless of censoring. Among patients with RD at D14, those who received reinduction therapy trended towards decreased OS [1.2 years versus Non-Estimable (NE); p=0.15] and had decreased RFS (0.4 versus 1.2 years; p=0.02) relative to those who did not. When not censoring at time of SCT, this difference in RFS was no longer statistically significant (1.0 years versus NE; p=0.13). When comparing those with NED and those with RD who did not receive reinduction therapy, there was no difference in OS (p=0.55) or RFS (p=0.73). In the unadjusted Cox regression model, OS was not significantly affected by D14 BM status (HR, 1.3; p=0.28). In those with RD at D14, reinduction was associated with an increased hazard of all-cause mortality (HR, 2.2; p=0.0004). The multivariable OS model (Table 1) showed no evidence of higher mortality risk among patients with RD at D14 (versus NED, HR, 0.98; p=0.97) or those with RD who received reinduction therapy (versus RD without reinduction; HR, 1.9; p=0.18). In the unadjusted Cox regression model, hazard of relapse was significantly increased among patients with RD at D14 (versus NED; HR, 1.9; p=0.02). In those with RD, reinduction was also associated with an increased hazard of relapse (versus no reinduction; HR, 2.8; p< 0.01). The multivariable RFS model showed no difference in hazard of relapse regardless of D14 disease or, amongst those with RD, receipt of reinduction.
CONCLUSION: The prognostic value and clinical utility of D14 BM Bx remains unclear, and these NED showed decrease hazard of relapse on univariable analysis, this relationship was findings further question this routine practice by showing similar clinical outcomes irrespective of D14 disease status.
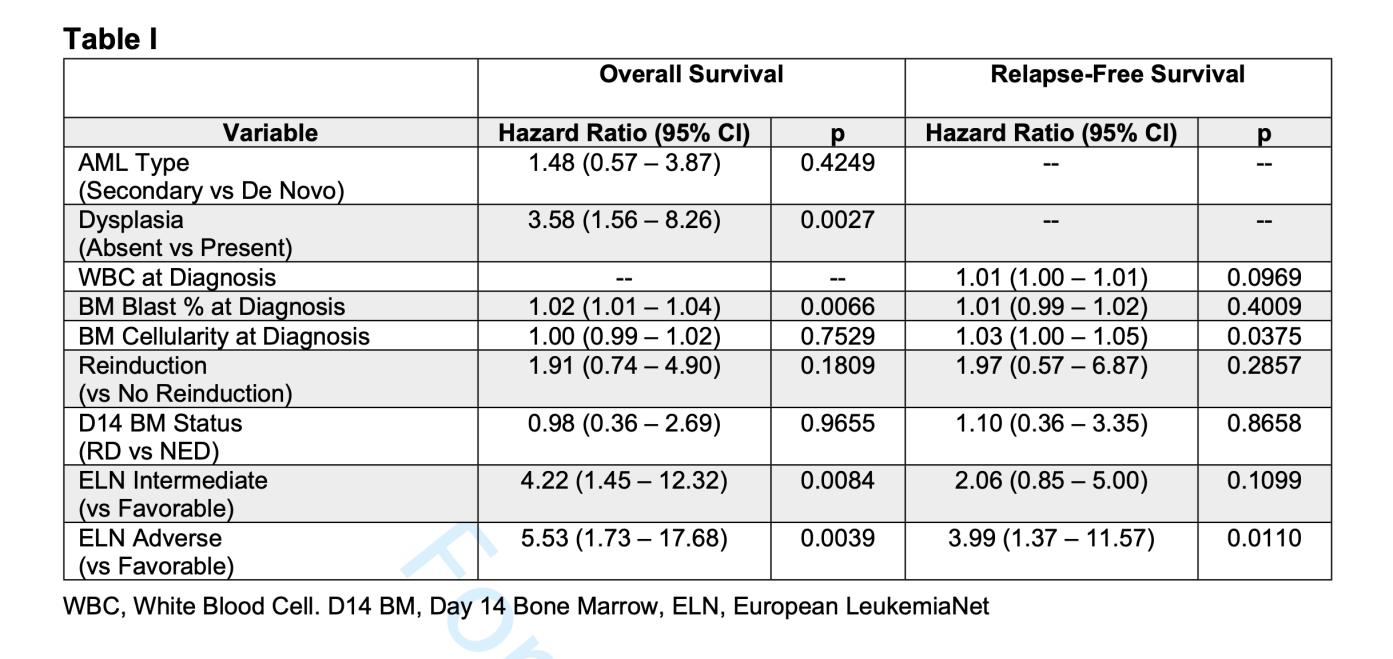


LOWER SEVERE CONSTIPATION, FECALITH, AND GIANT FECOLOMA IN PATIENT WITH SEVERE INTELLECTUAL DISABILITY
76
77
Matthew Baer1 , Dana Poloni2, CJ Quach1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Eisenhower Army Medical Center, United States Department of Veterans Affairs, Augusta, Georgia, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
LOWER SENSITIVITY AND SPECIFICITY OF CURRENTLY AVAILABLE ESOPHAGEAL PH TESTS
Bo Hyung Yoon1, Patricia Miguez Arosemena1 , Omar Belfaqeeh1, Marni Wilkoff1 , Samantha Shetty1 , Daniela Jodorkovsky1, Michael Smith1, Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
PANCREATIC NEUROENDOCRINE TUMOR PRESENTING AS AN ABDOMINAL PAIN FOLLOWING SUCCESSFUL HELICOBACTER PYLORI ERADICATION
78
79
Omar Belfaqeeh1, Frederick Rozenshteyn1, Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
AN UNEXPLAINED DIAGNOSIS OF HEART FAILURE THAT BEGAN WITH VIRAL PERIMYOCARDITIS AND ENDED WITH HEREDITARY TRANSTHYRETIN AMYLOID CARDIOMYOPATHY
Kristen Carter1, Soumya Gupta1, Ashish Correa1, Kiran Mahmood1, Arieh Fox1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
LEFT VENTRICULAR GEOMETRY AND EXERCISE DIASTOLIC STRESS TEST COMPLEMENT THE PROGNOSTIC VALUE OF H2FPEF SCORE IN ELDERLY WITH NON-ISCHEMIC EXERCISE ECHOCARDIOGRAPHY
80
81
Kristen Carter1, Alaa Omar1, Arpanjeet Kaur1, Kruti Gandhi1, Errol Moras1, Soumya Gupta1 , Joseph Elias1, Ga Hee Kim1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
ANEMIA IS NOT ASSOCIATED WITH INCREASED MORTALITY RISK FOR PATIENTS UNDERGOING LEFT VENTRICULAR ASSIST DEVICE IMPLANTATION
James Choi1, Benjamin Adegbite1, Darren Kong1 , Sara Diaz1, Jose Aguilar Gallardo1 , Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Heart Failure Society of America (HFSA) Annual Scientific Meeting that was held in Cleveland, Ohio, United States from October 6-9, 2023.
COMPARATIVE ANALYSIS OF INFECTIOUS COMPLICATIONS IN PATIENTS WITH MULTIPLE MYELOMA TREATED WITH BCMA-TARGETED BISPECIFIC ANTIBODIES AND CAR T-CELL THERAPY
82
83
Karthik Nath1 , Tala Shekarkhand1 , Bruno A. Costa2, David Nemirovsky1 , Andriy Derkach1, Noriko Nishimura1, Tasmin Farzana1, Colin Rueda1, David Chung1,3 , Heather Landau1,3, Oscar Boutros Lahoud1,3, Michael Scordo1,3, Gunjan L. Shah1 , Hani Hassoun1,3, Kylee H. Maclachlan1,3, Neha Korde1,3, Urvi A. Shah1,3, Carlyn Rose Tan1 , Malin Hultcrantz1,3, Sergio A. Giralt1,3, Saad Z. Usmani1,3, Zainab Shahid1 , Sham Mailankody1,3, Alexander Lesokhin1
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Weill Cornell Medicine, New York, NY, United States
Presented at the American Society of Hematology (ASH) Annual Meeting that was held in San Diego, California, United States from December 9-12, 2023.
DEMOGRAPHIC DISPARITIES IN CLINICAL TRIAL ENROLLMENT OF UNITED STATES PATIENTS WITH NEWLY DIAGNOSED MULTIPLE MYELOMA
Bruno A. Costa1, Neha Debnath1, Thomaz Alexandre Costa2, Raphael Bertasi1, Tarek H. Mouhieddine3, Karthik Nath4, Adriana C. Rossi3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Federal University of Ceará, Fortaleza, Brazil; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Memorial Sloan Kettering Cancer Center, New York, NY, United States Presented at the American Society of Hematology (ASH) Annual Meeting that was held in San Diego, California, United States from December 9-12, 2023.
COMPREHENSIVE SPATIAL, TRANSCRIPTOMIC, AND GENOMIC ANALYSIS OF IMMUNOGENIC BILIARY TRACT CANCER
84
Wungki Park1,2, Fergus Keane1, Hulya Sahin Ozkan1, Allison Richards1, Vasilisa Rudneva1 , Danny Khalil1,2, Kevin Soares1,2 , Bruno A. Costa3, Darren Cowzer1, Zeyneb Tarcan1, James Harding1,2, Olca Basturk2, Dae Won Kim4, William Jarnagin1,2, Ghassan Abou-Alfa1,2 , Mark Donoghue1, Eileen M O’Reilly1,2
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Weill Cornell Medical College, New York, NY, United States; 3Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Moffitt Cancer Center, Tampa, FL, United States
Presented at the Society for Immunotherapy of Cancer’s (SITC) Annual Meeting that was held in San Diego, California, United States from November 1-5, 2023.
IMPACT OF ABSOLUTE LYMPHOCYTE COUNT AT PRE APHERESIS AND PRE LYMPHODEPLETION ON CHIMERIC ANTIGEN RECEPTOR T THERAPY OUTCOMES IN RELAPSED REFRACTORY MULTIPLE MYELOMA
Noriko Nishimura1, Jessica Flynn1 , Bruno A. Costa2, Sean Devlin1, Tasmin Farzana1 , Karthik Nath1, David Chung1, Heather Landau1, Oscar Lahoud1, Michael Scordo1, Gunjan Shah1, Hani Hassoun1, Kylee Maclachlan1, Malin Hultcrantz1, Neha Korde1, Alexander Lesokhin1, Urvi Shah1, Carlyn Rose Tan1, Sergio Giralt1, Saad Usmani1, Sham Mailankody1
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the International Myeloma Society (IMS) Annual Meeting that was held in Athens, Greece from September 27-30, 2023.
PROGNOSTIC IMPACT OF CORTICOSTEROID AND TOCILIZUMAB USE ON THE EFFICACY OF CHIMERIC ANTIGEN RECEPTOR T CELL THERAPY FOR RELAPSED/REFRACTORY MULTIPLE MYELOMA
86
87
Bruno A. Costa1, Jessica Flynn2, Karthik Nath2, Noriko Nishimura2, Sean Devlin2 , Tasmin Farzana2, David Chung2 , Heather Landau2, Oscar Lahoud2, Michael Scordo2 , Gunjan Shah2, Hani Hassoun2, Kylee Maclachlan2, Malin Hultcrantz2, Neha Korde2 , Alexander Lesokhin2, Urvi Shah2, Carlyn Rose Tan2, Sergio Giralt2, Saad Usmani2 , Sham Mailankody2
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the International Myeloma Society (IMS) Annual Meeting that was held in Athens, Greece from September 27-30, 2023.
VITAMIN D DEFICIENCY AND CLINICAL OUTCOMES WITH CHIMERIC ANTIGEN RECEPTOR T CELL THERAPY IN RELAPSED/REFRACTORY MULTIPLE MYELOMA
Noriko Nishimura1, Jessica Flynn1 , Bruno A. Costa2 , Sean Devlin1, Tasmin Farzana1, David Chung1, Heather Landau1, Oscar Lahoud1, Michael Scordo1, Gunjan Shah1, Hani Hassoun1 , Kylee Maclachlan1, Malin Hultcrantz1, Neha Korde1, Alexander Lesokhin1 , Urvi Shah1 , Carlyn Rose Tan1, Sergio Giralt1, Saad Usmani1, Sham Mailankody1, Karthik Nath1
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the International Myeloma Society (IMS) Annual Meeting that was held in Athens, Greece from September 27-30, 2023.
A UNIQUE CASE OF COCAINE INDUCED ANCA NEGATIVE DIFFUSE INTRAABDOMINAL VASCULITIS
88
89
Neha Debnath1 and James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
CAN MANOMETRIC BOLUS CLEARANCE BE USED TO CONFIRM ESOPHAGOGASTRIC JUNCTION OUTLET OBSTRUCTION?
Binoy V. Desai1 , Emily Seltzer1, Michael S. Smith1, Kimberly Cavaliere1 , Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
90 A CASE OF TAKOTSUBO CARDIOMYOPATHY ASSOCIATED WITH TRASTUZUMABPACLITAXEL CHEMOTHERAPY
Sara Diaz Saravia1, James Choi1, Soumya Gupta1 , Shelly Brejt2 , Susan Lin1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York University Langone Health, New York, NY, United States
Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
CANCER AND SHORT-TERM COMPLICATIONS OF ACUTE MYOCARDIAL INFARCTION
91
92
Sara Diaz Saravia1, James Choi1, Christopher N. Matthews1, Darren Kong1 , Souyma Gupta1, Sakul Sakul1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented atthe Transcatheter CardiovascularTherapeutics (TCT) AnnualMeeting that was held in San Francisco, California, United States from October 23-26, 2023
MORTALITY AND OUTCOMES OF PATIENTS WITHOUT STANDARD MODIFIABLE RISK FACTORS UNDERGOING CORONARY REVASCULARIZATION
Sara Diaz Saravia1, James Choi1, Christopher N. Matthews1, Serdar Farhan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
PRESENCE AND SEVERITY OF SUBCLINICAL ATHEROSCLEROTIC DISEASE IN THE PRIMARY PREVENTION OF THE ONCOLOGIC POPULATION
93
94
Sara Diaz Saravia1 , Sergio Gonzalez, María Brenzoni2, Pamela Alarcón2, Fabián Ferroni2 , Carlos Castellaro2, Jorge A. Chiabaut2, Renzo Melchiori2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Hospital Universitario Austral, Buenos Aries, Argentina
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
THE RELATIONSHIP BETWEEN CANCER AND IN-STENT RESTENOSIS
Sara Diaz Saravia1, James Choi1, Darren Kong1, Christopher Matthews1, Alaa Omar1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
AN UNUSUAL CASE OF STROKE DUE TO CRYPTOCOCCAL MENINGITIS WITH IDIOPATHIC CD4 LYMPHOCYTOPENIA
95
96
Jin Feng1, Tal Shachi1,2, Jennifer Fung1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
ATYPICAL GOUT FLARE AFTER TOTAL KNEE ARTHROPLASTY COMPLICATED BY PROSTHETIC JOINT INFECTION
Jin Feng1, Shu Min Lao2, Olivia Ghaw2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Congress of Clinical Rheumatology Annual Meeting that was held in San Diego, California, United States from September 7-10, 2023.
DECREASED ODDS OF MALIGNANCY WITH MYCOPHENOLATE USE IN A SINGLECENTER SCLERODERMA COHORT
97
98
Jin Feng1, Chrisanna Dobrowolski1,2, Celestine He2, Hannah Verma3, Roshan Vasoya3 , Daniel Qian3, Ezequiel Olumuyide3, Alicia Leong3, Joseph Menand1, Murilo Roberto Bastos Silva1, Vincent Courant2, Sophia Lutgen1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Rheumatology (ACR) Annual Meeting that was held in San Diego, California, United States from November 14-19, 2023.
INCREASE SHINGRIX VACCINATION RATE IN PATIENTS ON JAK INHIBITORS
Jin Feng1 and Kristaq Koci1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Rheumatology (ACR) Annual Meeting that was held in San Diego, California, United States from November 14-19, 2023.
PHENOTYPIC CHARACTERIZATION OF NOD2 MUTATIONS IN PATIENTS WITH ANTIBODY DEFICIENCIES
99
100
Ashley Sang Eun Lee1 , Jin Feng1, Hsi-En Ho1 , Charlotte Cunningham-Rundles1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
SUMMERTIME ASSOCIATIONS BETWEEN MOLD EXPOSURE AND RHINITIS SYMPTOMS AMONG PRESCHOOL CHILDREN ATTENDING HEAD START IN NEW YORK CITY
Jin Feng1, Adnan Divjan2, Luis Acosta2, Andrew Rundle2, Maxine Ashby-Thompson2 , Judith Jacobson2, Matthew Perzanowski2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mailman School of Public Health at Columbia University, New York, NY, United States
Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
TEMPORAL ASSOCIATION BETWEEN BREAST CANCER AND SYSTEMIC SCLEROSIS: A CROSS-SECTIONAL ANALYSIS IN AN URBAN INSTITUTION
101
Jin Feng1, Celestine He2, Hannah Verma3, Roshan Vasoya3, Daniel Qian3, Ezequiel Olumuyide3, Alicia Leong3, Joseph Menand1, Murilo Roberto Bastos Silva1, Vincent Courant2, Sophia Lutgen1, Chrisanna Dobrowolski2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the European Alliance of Associations for Rheumatology (EULAR) Annual Meeting that will be held in Vienna, Austria from June 12-15, 2024.
A RARE HEMIBALLISMUS WITH ANTIPHOSPHOLIPID SYNDROME
Andreas Lau1 , Thomas Fusillo2, Dennis Kulp3, Mariam Rangwala3
102
1Western University of Health Science, Pomona, CA, United States; 2Mount Sinai Morningside-West Hospitals, New York, NY, United States; 3Community Memorial Hospitals and Healthcare, Ventura, CA, United States
Presented at the American College of Physicians Southern California Scientific Meeting that was held in Los Angeles, California, United States on October 7, 2023.
SALT, SEIZURES AND SIADH: PITUITARY (MACRO)ADENOMA AND SYMPTOMATIC HYPONATREMIA
103
104
Archana Pattupara1,2 , Kristine Lou Gargaritano1, Alyson Meyer1, Mrittika Deb1 , Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
CLINICAL OUTCOMES OF COVID-19 IN PATIENTS WITH HEART FAILURE WITH REDUCED EJECTION FRACTION
Kruti D. Gandhi1, Errol Moras1 , Adylin Moras2, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
DEVICE-RELATED ENDOCARDITIS IN CARDIAC RESYNCHRONIZATION THERAPY RECIPIENT COMPLICATED BY PULMONARY EMBOLI, CEREBRAL INFARCT, AND CRITICAL HYPOXIA
105
106
Kruti D. Gandhi1, Errol Moras1, Sidra Salman1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
EVALUATING THE EFFECTIVENESS OF VIRTUAL DIDACTIC SESSIONS VERSUS SMALL GROUP SIMULATION SESSIONS FOR RIGHT VENTRICULAR FUNCTION ASSESSMENT: A POINT-OF-CARE ULTRASOUND CURRICULUM
Kruti D. Gandhi1, Errol Moras1, Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States 2Mount Sinai
Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
PROGNOSTIC COMPARISON BETWEEN COMPUTER MODELLING-DERIVED VERSUS CONVENTIONAL H2FPEF SCORES
107
Swiri Konje1, Alaa M. Omar1, Alba Munoz2, Ga Hee Kim1, Joseph Elias1, Arun Mahtani3 , Kruti Gandhi1, Errol Moras1, Christopher Perez Lizardo1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Methodist Hospital, Houston, TX, United States; 3Richmond University Medical Center, Staten Island, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
PROGNOSTIC VALUE OF EXERCISE TOLERANCE AND EXERCISE-ASSOCIATED DIASTOLIC DYSFUNCTION IN ELDERLY PATIENTS REFERRED FOR EXERCISE STRESS ECHOCARDIOGRAPHY
108
Joseph Elias1, Swiri Konje1, Alba Munoz2 , Ga Hee Kim1 , Kruti Gandhi1, Errol Moras1 , Christopher Perez Lizardo1 , Arpanjeet Kaur1, Alaa M. Omar1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Methodist Hospital, Houston, TX, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
PROGNOSTIC VALUE OF H2FPEF SCORE AMONG SYMPTOMATIC PATIENTS REFERRED FOR EXERCISE ECHOCARDIOGRAPHY
109
110
Ga Hee Kim1, Swiri Konje1, Alba Munoz2 , Kruti Gandhi1 , Errol Moras1, Christopher Perez Lizardo1 , Joseph Elias1, Arpanjeet Kaur1, Alaa M. Omar1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
TEMPORAL TRENDS AND OUTCOMES OF HEART FAILURE PATIENTS BETWEEN LIGHT-CHAIN CARDIAC AMYLOIDOSIS AND TRANSTHYRETIN CARDIAC AMYLOIDOSIS
Kruti D. Gandhi1, Errol Moras1, Ashish Correa1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
TRENDS AND OUTCOMES OF ENDOBRONCHIAL VALVE IMPLANTATION IN PATIENTS WITH PERSISTENT AIR LEAK
111
112
Kruti D. Gandhi1, Errol Moras1, Adlyn Moras2, Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
DIFFICULT CONVERSATIONS AND EFFECTIVE COMMUNICATION TRAINING FOR INTERNAL MEDICINE RESIDENTS UTILIZING HIGH-FIDELITY SIMULATION
Ariela Hazan1, Jeeyune Bahk1 , Ariel Gordon1, Neha Debnath1, Priscilla V. Loanzon1 , Harrindra Seepersaud1, Donna Gormley1 , Adam Rothman1,2, James Salonia1, Susannah Kurtz1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
USE OF KETAMINE AND AN INTERDISCIPLINARY TEAM APPROACH TO RAPIDLY TAPER A PATIENT’S ULTRA-HIGH OPIOID REGIMEN
113
114
Ariel Gordon1, Evan L. Zazula2, Joseph D. Elder2, Estelle Jungah Hong2, Jordan NickelDubin2, Yu Shindo2, Ayla Pelleg2, Laura Belland2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Assembly of Hospice and Palliative Care that was held in Phoenix, Arizona, United States from March 20-23, 2024.
ASSESSING RESIDENT COMFORT IN ADVANCE CARE PLANNING AND HEALTHCARE PROXY DISCUSSIONS IN CHRONIC OBSTRUCTIVE PULMONARY DISEASE AND HEART FAILURE PATIENTS
Soumya Gupta1 , Christopher Matthews1, Kristen Carter1, Salvador Caceros Diaz1, Emily Seltzer1, Rebecca Shafer1, Deborah Edelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
CREATING A NOVEL CURRICULUM ON CARDIAC DEVICES FOR INTERNAL MEDICINE RESIDENTS
115
116
Soumya Gupta1, Priya Shah1 , Kristen Carter1, Ashish Correa1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
PREDICTORS OF IN-HOSPITAL MORTALITY AMONG HEART TRANSPLANT RECIPIENTS IN THE UNITED STATES
Soumya Gupta1, Kristen Carter1, Hannah Hart1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
PATIENT EDUCATION FOR CORONARY ARTERY DISEASE PREVENTION
117
118
Hannah Hart1, Brandon Rafison1, Anna Mueller1, Juan Arango Morales1, Petra Maslov1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
EFFECTS OF HIGH INTENSITY INTERVAL TRAINING ON CARDIORESPIRATORY FITNESSAND LEFT VENTRICULAR FUNCTION IN PATIENTSENROLLED IN CARDIAC REHABILITATION AFTER RECENT MYOCARDIAL INFARCTION
Arpanjeet Kaur1, Sakul Sakul2, Arshdeep Dhaliwal1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2University of Nebraska Medical Center, Omaha, NE, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
ECHOCARDIOGRAPHIC CHANGES OF TRANSTHYRETIN CARDIOMYOPATHY PATIENTS TREATED WITH TAFAMIDIS
119
120
Darren Kong1, Arpanjeet Kaur1, Kruti Gandhi1, James Choi1, Ashish Correa1 , Arieh Fox1 , Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
ENHANCING THE INTERN YEAR TRANSITION FOR INTERNATIONAL MEDICAL GRADUATES IN INPATIENT SETTINGS
Jiaxi Miao1 and Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
INITIATION OF TAKE HOME NALOXONE KIT DISPENSING ON THE INPATIENT MEDICINE SERVICE AT MOUNT SINAI WEST
121
Jiaxi Miao1, Scott Low1, Kristy Huang1, Modesta Asante1, Jood Ani1, Caroline McBrien1 , Annalisa Monahan1, Abdel Abada1, Beth Raucher2, Irina Zaretsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
GASTRIC LIPOMA: A RARE CAUSE OF MELENA*
Alexandria Markley1, Rohit Nathani1, Erica Park1 , Mohamed Rabie2, Armand Cacciarelli1,2
122
123
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
*ACG Outstanding Poster Presentation
ATRIAL FIBRILLATION AS AN INDEPENDENT PREDICTOR FOR MAJOR ADVERSE CARDIOVASCULAR EVENTS IN PATIENTS WHO UNDERWENT TRANSCATHETER TRICUSPID VALVE PROCEDURES
Christopher N. Matthews1, Sara Diaz Saravia1 , James Choi1 , Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Society of Hospital Medicine (SHM) Annual Meeting that will be held in San Diego, California, United States from April 12-15, 2024.
REVERSE TAKOTSUBO CARDIOMYOPATHY AFTER CESAREAN DELIVERY COMPLICATED BY MASSIVE POST-PARTUM HEMORRHAGE IN A CASE OF PLACENTA ACCRETA
124
125
Christopher N. Matthews1 , Yesha Rana2, Brandon Berman1, Joseph D. Marinelli1 , Krysthel Engstrom2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
TRANSCATHETER MITRAL VALVE PROCEDURE OUTCOMES IN PATIENTS WITH HYPERTROPHIC OBSTRUCTIVE CARDIOMYOPATHY
Christopher N. Matthews1 , Sara Diaz Saravia1 , James Choi1 , Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Society of Hospital Medicine (SHM) Annual Meeting that will be held in San Diego, California, United States from April 12-15, 2024.
A MINORITY OF PATIENTS IN NEED OF PELVIC FLOOR BIOFEEDBACK TRAINING ACTUALLY ATTEND SCHEDULED THERAPY SESSIONS
Joseph A. Menand1 , Yonatan Israel2 , Emma Reford2 , Robinderpal Sandhu1 , Ahmun Zafar1 ,
Kimberly Cavaliere1,3 , Priyanka Singh1,3, Jean Saleh1,3 , Michael S. Smith1,3, Yuying Luo3 ,
126
127
Daniela Jodorkovsky1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
IMPAIRED MOBILITY DOES NOT IMPACT ANORECTAL MANOMETRY FINDINGS AND BIOFEEDBACK UTILIZATION
Yonatan Israel1 , Joseph A. Menand2 , Emma Reford1 , Ahmun Zafar2 , Robinderpal Sandhu2 , Kimberly Cavaliere2,3 , Priyanka Singh3 , Jean Saleh2,3 , Michael S. Smith2,3 , Yuying Luo3 , Daniela Jodorkovsky2
1Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
WHERE IS THE DRE? DIGITAL RECTAL EXAMS ARE INFREQUENTLY PERFORMED PRIOR TO ANORECTAL MANOMETRY EXAMS
128
Joseph A. Menand1 , Robinderpal Sandhu1 , Yonatan Israel2 , Emma Reford2 , Ahmun Zafar1 , Kimberly Cavaliere1,3 , Priyanka Singh3 , Jean Saleh1,3 , Michael S. Smith1,3 , Daniela Jodorkovsky1,3, Yuying Luo3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
A DELAYED DIAGNOSIS OF AUTOIMMUNE PANCREATITIS IN A PATIENT WITH ALCOHOL USE DISORDER
129
130
Andre Khazak1 , Patricia Miguez Arosemena2, Jake Debroff1, Violetta Laskova1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
ENDOSCOPIC PALLIATIVE IN-STENT LIQUID NITROGEN SPRAY CRYOTHERAPYFOR ESOPHAGEAL ADENOCARCINOMA*
Patricia Miguez Arosemena1 , Andre Khazak2, Angad Uberoi1,2 , Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
*ACG Award-Winning Abstract
GASTROINTESTINAL TRACT COMPLICATIONS FROM IODODERMA
131
132
Patricia Miguez Arosemena1, Andre Khazak2, Angad Uberoi1,2, Shanique Wilson Noack1,2 , Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
RECURRENT CANDIDA ESOPHAGITIS IN A PATIENT WITH PSORIATIC ARTHRITIS TRANSITIONING IMMUNOLOGIC AGENTS
Andre Khazak1 , Patricia Miguez Arosemena2, Jake Debroff1, Alain Kameni1, Svetlana Chernyavsky1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
TUBERCULOSIS OR NOT TUBERCULOSIS?
Jenny Dave1,2 , Patricia Miguez Arosemena2, Priya Simoes1
133
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BRIDGING ASSESSING THE EFFICACY OF A POINT-OF-CARE ULTRASOUND CURRICULUM DELVIVERED VIA A TWO-WEEK ELECTIVE
Errol C. Moras1 , Keshav Dixit1, Kruti D. Gandhi1, Adam Rothman1,2
134
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
IMPACT OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE ON OUTCOMES IN PATIENTS WITH TAKOTSUBO CARDIOMYOPATHY
135
136
Errol Moras1, Kruti D. Gandhi1, Adlyn Moras2, Sidra Salman1, Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
INCIDENCE AND PREDICTORS OF NEW-ONSET ATRIAL FIBRILLATION IN PATIENTS HOSPITALIZED WITH COVID19 INFECTION
Errol Moras1, Kruti D. Gandhi1, Adlyn Moras2, Dave Mehta1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
TRENDS AND OUTCOMES OF PATIENTS WITH SYSTEMIC SCLEROSIS AND ATRIAL FIBRILLATION
Errol Moras1, Kruti D. Gandhi1, Adlyn Moras2, Sidra Salman1, Adam Rothman1,3
137
138
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Father Muller’s College, Karnataka, India; 3Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BRIDGING THE GAP IN LGBTQ+ HEALTH TRAINING FOR INTERNAL MEDICINE RESIDENTS: A NEEDS ASSESSMENT OF A CURRICULUM DEVELOPMENT STUDY
Lenisse Reyes Reyes1, Sharel Sadud1, Tamar Reisman2, Helene Hedian3 , Tamara Goldberg1, Joel Grimaldo Ochoa1, Brent Arcayan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Weill Cornell Medical Center, New York, NY, United States; 3John Hopkins University School of Medicine, Baltimore, MD, United States
Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024 and to be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
DESMOPLAKIN CARDIOMYOPATHY-INDUCED RECURRENT PERIMYOCARDITIS
Sidra Salman1, Marni Wilkoff1, Kruti D. Gandhi1, Errol Moras1, James Salonia1
139
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
FACTORS AFFECTING HOSPITAL LENGTH OF STAY AMONG PATIENTS HOSPITALIZED WITH ACUTE PULMONARY EMBOLISM
140
141
Jeeyune Bahk1, Abdul Rehman2 , Sidra Salman1, Venus Sharma1, Avinash Singh1, Hafiza Noor Ul Ain Baloch1,3, David J. Steiger1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Rutgers New Jersey Medical School, Newark, NJ, United States; 3Mount Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
IMPLEMENTATION OF A LONGITUDINAL PROCEDURAL CURRICULUM: WHAT EDUCATIONAL TOOLS IMPROVE PROCEDURAL PROFICIENCY WITHIN INTERNAL MEDICINE RESIDENCY PROGRAMS
Sidra Salman1 and James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
RURAL SETTING NOT ASSOCIATED WITH HIGHER RISK OF ADVANCED STAGE AT DIAGNOSIS IN NON-SMALL CELL LUNG CANCER
142
143
Sidra Salman1, Nadeem Bilani1, Rafael Arteta-Bulos2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Cleveland Clinic, Weston, FL, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
THE ASSOCIATION OF TEACHING STATUS ON INPATIENT MORTALITY AMONG CRITICALLY ILL PATIENTS WITH SEPSIS
Lorenzo Leys1,2 , Sidra Salman1, Sara Luby1, Deepanjali Radhkrishnan Nair1,2, Raymond A. Jean3, Raymonde Jean1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3University of Michigan Health, Ann Arbor, MI, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
144 A RARE CASE OF BACTRIM-INDUCED LIVER INJURY DUE TO DRESS SYNDROME
Ramnik K. Gill1, Ezana Bekele1 , Robinderpal Sandhu2, Meghaben Kothari1
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
145 A RARE CASE OF CHECKPOINT INHIBITOR MEDIATED HEPATITIS IN A PATIENT WITH MELANOMA
Ramnik K. Gill1 , Robinderpal Sandhu2, Ezana Bekele1, Meghaben Kothari1
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
DEFINING A CLINICAL PHENOTYPE: A RETROSPECTIVE COMPARATIVE ANALYSIS OF PATIENTS WITH DISTAL ESOPHAGEAL SPASM AND NORMAL HIGHRESOLUTION ESOPHAGEAL MANOMETRY
146
147
Emily S. Seltzer1, Kimberly Cavaliere1, Robinderpal Sandhu1, Mantej Sehmbhi1,2 , Kimberly Cavaliere1, Michael S. Smith1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
SAVING THE ESOPHAGUS FROM CAUSTIC INJURY: HOW SHOULD WE DO IT?
Jenny Dave1,2 , Emily S. Seltzer1, Kimberly Cavaliere2
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
WHAT’S GERD GOT TO DO WITH DES: COMPARING CHARACTERISTICS OF REFLUX AND NON-REFLUX PHENOTYPES OF DISTAL ESOPHAGEAL SPASM
148
Emily S. Seltzer1, Kimberly Cavaliere1, Robinderpal Sandhu1, Mantej Sehmbhi1,2, Kimberly Cavaliere1, Michael S. Smith1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
COMPARISON OF OUTCOMES IN PATIENTS TRACHEOSTOMIZED AT DIFFERENT FIO2 SETTINGS
149
150
Jeeyune Bahk1, Bridget Dolan2 , Venus Sharma1, Mantej Sehmbhi1,2, Jennifer Y. Fung1 , Young Im Lee2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
IMPACT OF DIFFERENT ANTICOAGULATION STRATEGIES ON OUTCOMES IN PATIENTS HOSPITALIZED WITH ACUTE PULMONARY EMBOLISM
Jeeyune Bahk1, Abdul Rehman2 , Venus Sharma1, Sidra Salman1, Avinash Singh1, Hafiza Noor Ulain Baloch1,3, David J. Steiger1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Rutgers New Jersey Medical School, Newark, NJ, United States; 3Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023
INPATIENT UTILIZATION OF SEPSIS PATHWAY AND ITS IMPACT ON THE LENGTH OF STAY AMONG THE PATIENTS DIAGNOSED WITH SEPSIS, SEVERE SEPSIS, AND SEPTIC SHOCK
Venus Sharma1, Harrindra Seepersaud1, Galit Balayla Rosemberg1, Sara Luby1, Hammad
151
152
Sheikh1, Connor Smith1 , Lorenzo Leys1,2, James Salonia1, Rachael Schneider1, Raymonde
Jean1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
INPATIENT UTILIZATION OF SEPSIS PATHWAY AND ITS IMPACT ON THE MORTALITY AMONG THE PATIENTS WITH SEPTIC SHOCK
Venus Sharma1, Harrindra Seepersaud1, Galit Balayla Rosemberg1, Sara Luby1, Hammad
Sheikh1, Connor Smith1 , Lorenzo Leys1,2, James Salonia1, Rachael Schneider1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
SYMPTOMATIC PRESENTATION OF MYCOBACTERIUM XENOPI IN A PATIENT WITH SCHAMBERG DISEASE
Venus Sharma1, Andrea Monfasani2, David J. Steiger1,2, Christian D. Becker3, Nkechi
153
Nwaoha3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BRIDGING THE GAP BETWEEN SEPSIS AND POST SEPSIS SYNDROME
Hammad Sheikh, James Salonia1, Susannah Kurtz1, Jacob Bell, Ahmed Shaikh1, Nikita Desai1, Priscilla Loanzon1, Harrindra Seepersaud1, Amit Pradhan1, Adam Rothman1,2
154
155
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented both at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
ANTIBIOTIC TERHAPY AT A TERTIARY MEDICAL CENTER IN NEW YORK CITY
Carolina Moreira Sarmiento1,2 , Connor Smith1, Galit Rosemberg1, Valida Bajrovic1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
A NOVEL SIMULATION-BASED THORACIC POINT-OF-CARE ULTRASOUND CURRICULUM FOR INTERNAL MEDICINE RESIDENTS
Hua Hsin Tai1 , Harrinda Seepersaud1, Adam Rothman1,2
156
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented both at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
ACUTE HYPOXIC RESPIRATORY FAILURE FROM DAPTOMYCIN INDUCED EOSINOPHILIC PNEUMONIA
157
158
Vincent Torelli1, Raymonde E Jean1, Elena Tran2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Presbyterian Brooklyn Methodist Hospital, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
RAPIDLY PROGRESSIVE INTERSTITIAL LUNG DISEASE DUE TO SILICOSIS IN AN OTHERWISE HEALTHY JEWELER
Vincent Torelli1, Raymonde E Jean1, Elena Tran2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2New York Presbyterian Brooklyn Methodist Hospital, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BURKITT LYMPHOMA INDUCED PSEUDOACHALASIA WITH DRAMATIC SYMPTOMATIC IMPROVEMENT POST-CHEMOTHERAPY*
159
160
Marni Wilkoff1, Emily Seltzer1, Allison Wang1,2, Bruno Costa1 , Mohamed Rabie1 , Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
*ACG Outstanding Poster Presentation
DEVELOPMENT OF FREE, OPEN-ACCESS EDUCATIONAL TOOL TO FACILITATE NUTRITION LEARNING USING TAILORED CASE-BASED SCENARIOS
Marni Wilkoff1, Samira Farouk2, David Thomas2, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
THE EFFECTS OF ENDOSCOPY SIMULATION ON RESIDENT PHYSICIANS' CONFIDENCE AND KNOWLEDGE IN TREATING COMMON GASTROINTESTINAL CONDITIONS
161
Marni Wilkoff1, Emily Seltzer1, Shabari Shenoy1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented both at the New York Society for Gastroenterology and Endoscopy Annual Meeting that was held in New York, New York, United States from December 14-15, 2023 and the Institute for Medical Education (IME), Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
USING QR CODE TECHNOLOGY TO IMPROVE GUIDELINE-DIRECTED CARE FOR ADMITTED PATIENTS WITH DECOMPENSATED CIRRHOSIS*
Randy Leibowitz1 , Marni Wilkoff1**, Swati Patel1**, Alexandria Markley1** , Ines Varela Knorr1**, Steven Rodriguez1,2, Frank Nelson1
162
163
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
*Selected for ACG Moderated Poster Session ***These authors contributed equally to this work.
DAPTOMYCIN-INDUCED EOSINOPHILIC PNEUMONIA
Agostina Velo1, Ilana Bandle1, Connor Welsh1, Idayat Brimah1,2, Edwardine Mirna Mohanraj1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Mount Sinai Health System’s Department of Medicine Annual Research Day that was held in New York, New York, United States from May 6-7, 2024.
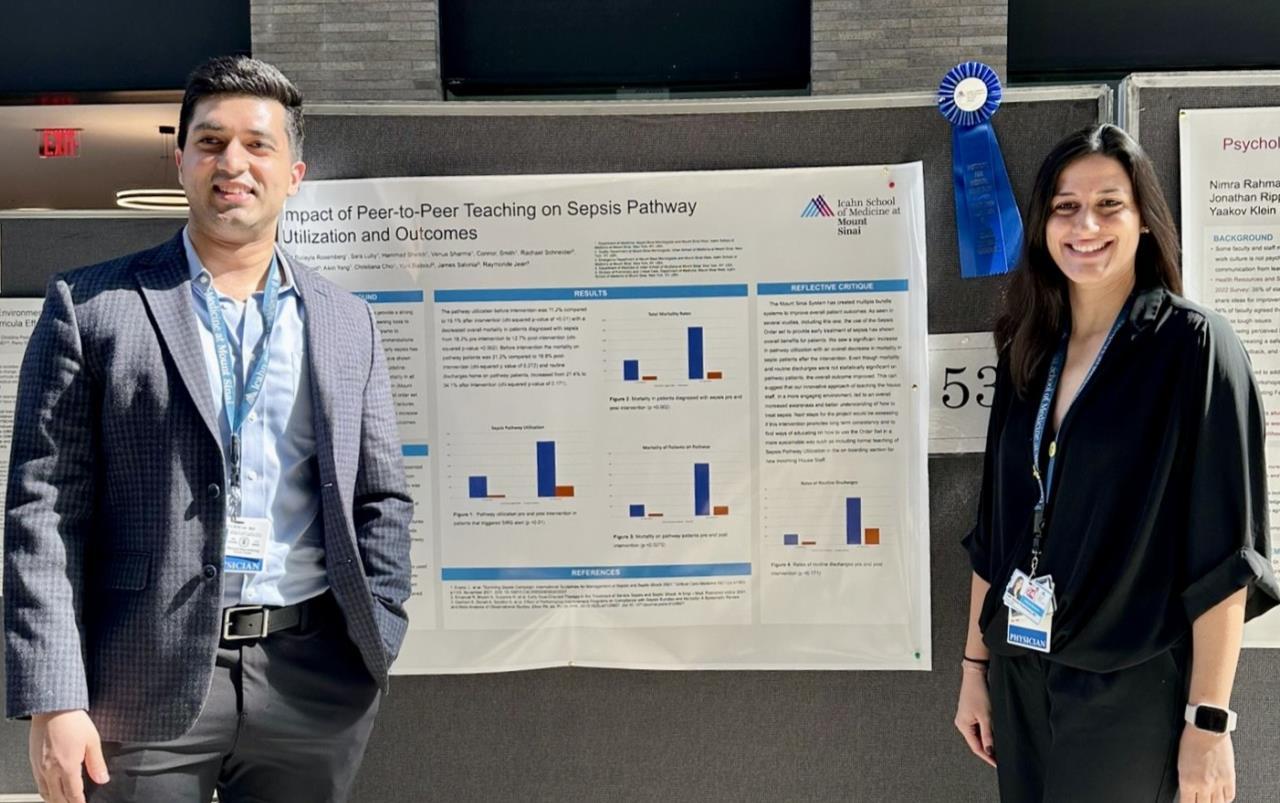
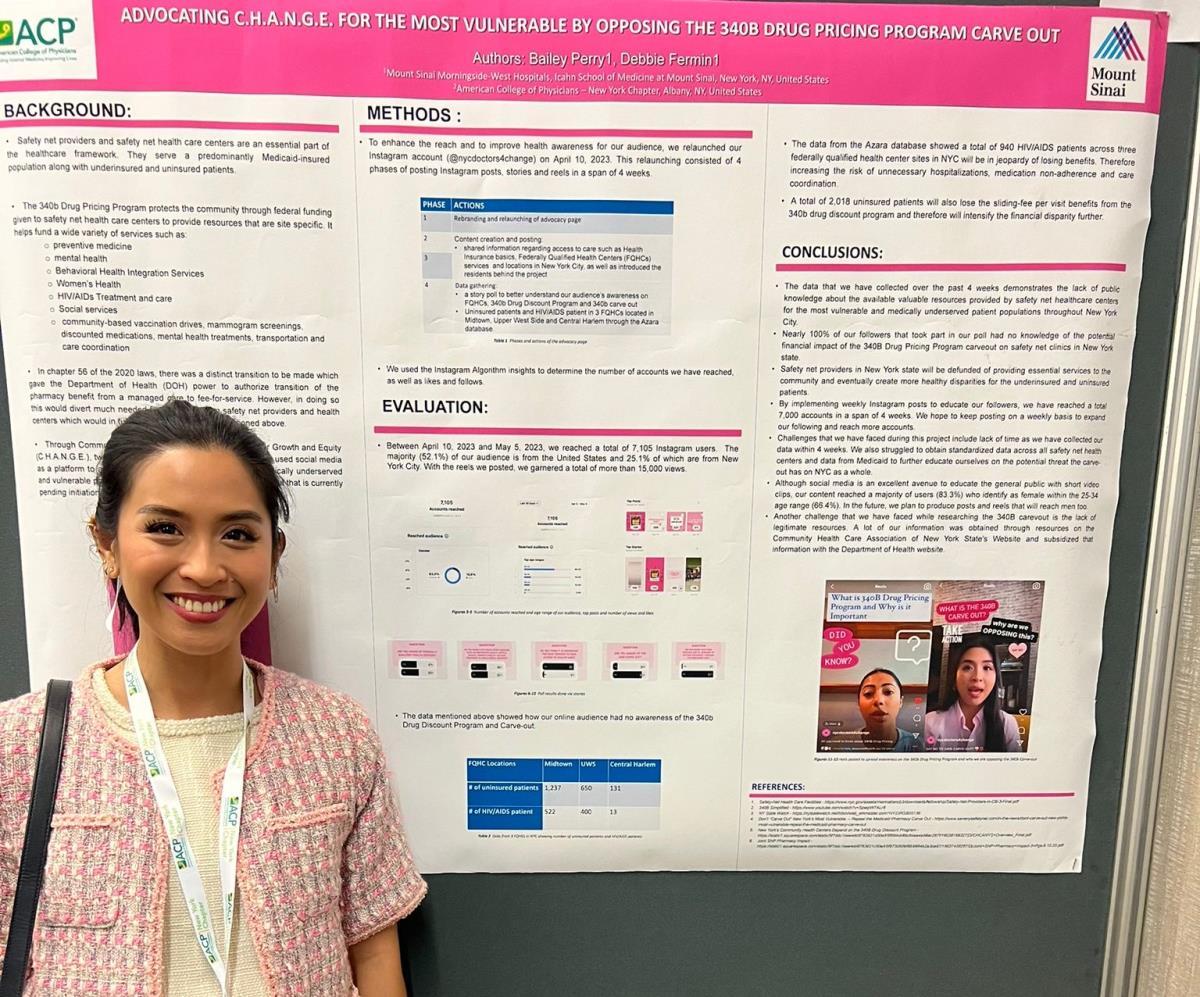
ABSTRACT #76
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
LOWER SEVERE CONSTIPATION, FECALITH, AND GIANT FECOLOMA IN PATIENT WITH SEVERE INTELLECTUAL DISABILITY
Matthew Baer1, Dana Poloni2, CJ Quach1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Eisenhower Army Medical Center, United States Department of Veterans Affairs, Augusta, Georgia, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
CASE PRESENTATION: A 52-year-old male with a history of severe intellectual disability and chronic constipation presented for constipation of two weeks. Patient was non-verbal at baseline but had been eating and drinking normally. He had no bowel movements in the last two weeks and his abdomen was severely distended. Physical examination revealed active bowel sounds and no pain to palpation of abdomen.
Previous imaging showed an impacted stool mass expanding the sigmoid colon to 21 cm and significant mass effect on internal organs, with an 8.0 cm diameter fecalith in the rectum starting to form five years prior to current presentation. No prior images were positive for bowel obstruction, pneumoperitoneum, pseudo-obstruction, or adult Hirschsprung’s disease. Patient had never seen General Surgery or Gastroenterology for management of constipation. He had a state-appointed health care proxy.
The patient was given senna, miralax, tap water enema, and manual disimpaction with only a minimal bowel movement elicited. New abdominal x-ray and CT showed extremely large, chronic stool burden, again with sigmoid colon measuring 21 cm, and an 8 cm calcified stool ball in the rectum. The calcified fecalith had partially blocked the rectum and prevented significant evacuation of his bowels for years. Chronic buildup of stool led to a massive fecaloma that spanned the entire sigmoid and descending colon. Given that the situation was nonemergent, and patient could not consent to surgical procedures, he was subsequently admitted to Internal Medicine for conservative management of constipation. Patient was discharged from the hospital with no issues. Imaging at follow-up showed movement of fecalith up into the left colic flexure. Abdominal distention had not improved, due to most of the stool burden being contained within the large fecaloma in the sigmoid and descending colon.
CONCLUSION: Patients with severe intellectual disability have frequent exacerbations of chronic constipation with inherent challenges. These individuals often experience difficulties in effectively communicating pain, making it hard to identify and address constipation in its early stages. Their cognitive and physical limitations can lead to poor dietary choices, limited fluid intake, and reduced physical activity, all of which contribute to worsening constipation. The administration of medications, dietary interventions, or possible surgeries require special considerations, as these patients may have difficulty understanding, consenting, and adhering to treatment regimens.

ABSTRACT #77
CLINICAL RESEARCH
GASTROENTEROLOGY
Bo Hyung Yoon1, Patricia Miguez Arosemena1 , Omar Belfaqeeh1, Marni Wilkoff1, Samantha Shetty1, Daniela Jodorkovsky1 , Michael Smith1, Kimberly Cavaliere1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
BACKGROUND/INTRODUCTION: Endoscopic findings of Los Angeles (LA) Classification Grade B, C, D esophagitis, Barrett’s metaplasia and peptic stricture are definitive evidence of gastroesophageal reflux disease (GERD). Transnasal catheter-based and wireless pH testing are used to quantify distal acid exposure time (AET). Using definitive endoscopic findings of GERD as the gold standard, studies from the 1980s and 1990s found that catheter-based pH testing had a sensitivity and specificity of 77–100% and 85–100% respectively. Repeat assessment in the setting of innovations including higher definition endoscopes and refinement in endoscopic grading of esophagitis has not been performed. This study aimed to compare both conventional methods of pH testing with the currently accepted endoscopic markers of GERD to assess the sensitivity and specificity of these procedures in current practice.
METHODS: A retrospective review of all reflux tests completed in a single high-volume motility center between March 1, 2018 and July 31, 2022 was performed. Patients were included in the analysis if complete test results were available in the patient record. Medical records were reviewed to obtain the following information: baseline demographics, DeMeester score, AET, and upper endoscopy (EGD) results within one year of the pH tests.
RESULTS: Of 970 total reflux procedures, 518 were performed off proton pump inhibitors and H2 receptor blockers. There were 267 catheter-based pH tests and 201 wireless pH tests with available EGD reports included in the analysis. Of 267 patients who underwent conventional esophageal pH tests, 62% were females with mean age of 49 years (range, 20–81) and mean body mass index (BMI) of 28 (range, 14–72). For catheter-based pH tests, the sensitivity and specificity of DeMeester score for GERD defined by esophagitis (LA grade B-D) were 64.5% and 55.1% respectively; the sensitivity and specificity for GERD defined by esophagitis (LA grade B-D) of an AET above 6% were 45.2% and 43.0% respectively. Of 201 patients who underwent wireless pH testing, 62 % were females with mean age of 50 years (range, 18–83) and mean BMI of 25 (range, 16–50). For these patients, the sensitivity for GERD defined by esophagitis (LA grade B-D) of the DeMeester score was 80% and the specificity was 51.1%; the sensitivity and specificity for GERD defined by esophagitis (LA grade B-D) of AET above 6 % were 73.3% and 67.7%, respectively.
CONCLUSION: In this study cohort, both the sensitivity and specificity for GERD using transnasal catheterbased and wireless capsule pH testing were much lower than in previously reported data. These results highlight the potential value of a future prospective study to evaluate the sensitivity and specificity of these tests in modern clinical practice. If these tests continue to demonstrate lower than expected accuracy, a search for a more accurate pH test should be explored.
ABSTRACT #78
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
THE PANCREATIC NEUROENDOCRINE TUMOR PRESENTING AS AN ABDOMINAL PAIN FOLLOWING SUCCESSFUL HELICOBACTER PYLORI ERADICATION
Omar Belfaqeeh1, Frederick Rozenshteyn1, Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
BACKGROUND/INTRODUCTION: Zollinger-Ellison syndrome (ZES) is caused by functional duodenal or pancreatic neuroendocrine tumors (NET) that secrete gastrin resulting in excess acid production causing peptic ulceration, reflux esophagitis and diarrhea. It is estimated that the annual incidence is one per million population, of which 20 to 30 percent are associated with multiple endocrine neoplasia type 1 (MEN1). Recent studies have demonstrated that 70-80% of gastrinomas arise in the duodenum. Establishing a diagnosis of ZE can be difficult due to the lack of consistent diagnostic criteria, the widespread use of PPIs that masks mask the symptoms and limited access to gastric pH testing.
CASE PRESENTATION: A 67-year-old male with a history of partial liver resection, peptic ulcer disease, and H. pylori gastritis status post quadruple therapy presented with acute on chronic abdominal pain despite being on a PPI. He had abdominal pain for the past 5 years associated with nausea, vomiting, diarrhea, and a 50-pound unintentional weight loss. An EGD six months ago demonstrated PUD and H. pylori which was successfully eradicated. He underwent a CT-abdomen/pelvis with intravenous contrast in the emergency department which revealed an enhancing 3.4 cm mass in the head of the pancreas with retroperitoneal lymphadenopathy. MRI of the abdomen confirmed the presence of a 3.2 cm enhancing pancreatic head mass with direct extension into the second portion of the duodenum and multiple enlarged retroperitoneal lymph nodes. EGD was remarkable for edema and granularity in the first portion of the duodenum. EUS was notable for a hypoechoic and heterogeneous irregular mass in the pancreatic head measuring 25 mm by 23 mm in maximal cross-sectional diameter with invasion into the serosa and muscularis mucosa of the duodenum. FNA of the pancreatic mass for cytology revealed a well-differentiated pancreatic neuroendocrine tumor (Ki-67 index <1%). Gastrin levels were ordered. He presented again to the hospital in 3 weeks with worsening epigastric abdominal pain and nausea despite adhering to PPI therapy. CT abdomen revealed new proximal duodenal ulcerations. Gastrin level from the prior admission was noted to be 1988 pg/mL. He subsequently underwent a Whipple's procedure with no complications and was discharged home with a planned EGD surveillance in 6 months.
CONCLUSION: This In our case, the diagnosis was based on a fasting serum gastrin level, FNA results, and imaging findings. Owing to its variable clinical presentation, high mortality, and challenging primary lesion identification, clinicians should consider Zollinger-Ellison syndrome in the differential diagnosis of patients who are symptomatic despite taking PPI, having Helicobacter pylori successfully eradicated or having multiple duodenal and gastric ulcers that fail to respond to therapy.
ABSTRACT #79
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
AN UNEXPLAINED DIAGNOSIS OF HEART FAILURE THAT BEGAN WITH VIRAL PERIMYOCARDITIS AND ENDED WITH HEREDITARY TRANSTHYRETIN AMYLOID CARDIOMYOPATHY
Kristen Carter1, Soumya Gupta1 , Ashish Correa1, Kiran Mahmood1, Arieh Fox1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
CASE PRESENTATION: A 63-year-old male presented to the ED for chest pain radiating to the right shoulder and dyspnea on exertion for one week. He had a medical history of HTN, hyperlipidemia, and bilateral carpal tunnel syndrome. His exam was unremarkable. He was tachycardic but his other vitals were normal. Troponin was mildly elevated, and BNP was normal. He was also found to be COVID-19 positive. The patient had a transthoracic echocardiogram (TTE) which showed a reduced EF of 35%, diffuse left ventricular hypokinesis, and mild concentric LVH without any valvular abnormalities. Coronary CTA showed a calcium score of 0. Cardiac MRI showed mild biventricular dysfunction with basal to mid inferoseptal, inferior, and inferolateral late gadolinium enhancement, involving full myocardial thickness with pericardial enhancement, suggesting perimyocarditis versus sarcoidosis. Viral perimyocarditis was high on the differential given the myocardial inflammation on cardiac MRI, the temporal association with COVID-19, and the lack of extra-cardiac findings consistent with sarcoidosis. He had a FDG PET scan, which showed focal glucose uptake with associated mismatch perfusion abnormalities in the basal inferoseptal region, with the perfusion defect extending beyond the region of glucose uptake suggesting a combination of active myocardial inflammation and chronic scar. The cardiac findings were attributed to resolving myocarditis. Since viral myocarditis is self-limiting, no immediate anti-inflammatory treatment was pursued. Genetic testing was positive for a pathogenic variant of hereditary transthyretin (hATTR) amyloidosis Val142Ile. He then underwent a pyrophosphate PYP scan which demonstrated moderate radiotracer uptake with a visual grade of 2 and a heart to contralateral lung ratio was greater than 1.5, suggestive of cardiac amyloidosis. The patient had a serum kappa/lambda free light chain ratio, serum protein immunofixation, and urine protein immunofixation drawn to rule out immunoglobulin light chain amyloidosis, which were all normal. He was started on tafamidis for hereditary transthyretin amyloid cardiomyopathy (hATTR-CM). The patient’s initial clinical symptoms, positive COVID-19 test, reduced EF on TTE, active pericardial and myocardial inflammation on cardiac MRI, and FDG PET CT suggested perimyocarditis, which resolved over time. However, genetic testing, PYP scan, and bilateral carpal tunnel syndrome suggested the patient also had hATTR-CM. He had a repeat TTE after treatment for several months which showed improvement in his EF to 50% but decreased global longitudinal strain in a characteristic apical sparing pattern that was indicative of early cardiac amyloidosis.
CONCLUSION: This is an interesting case of perimyocarditis secondary to COVID-19 and hATTR-CM. Perimyocarditis after viral infections is common and treatment is often conservative, since it is usually selflimiting. hATTR amyloidosis however is an underdiagnosed cause of nonischemic cardiomyopathy and is easily treatable with tafamidis.
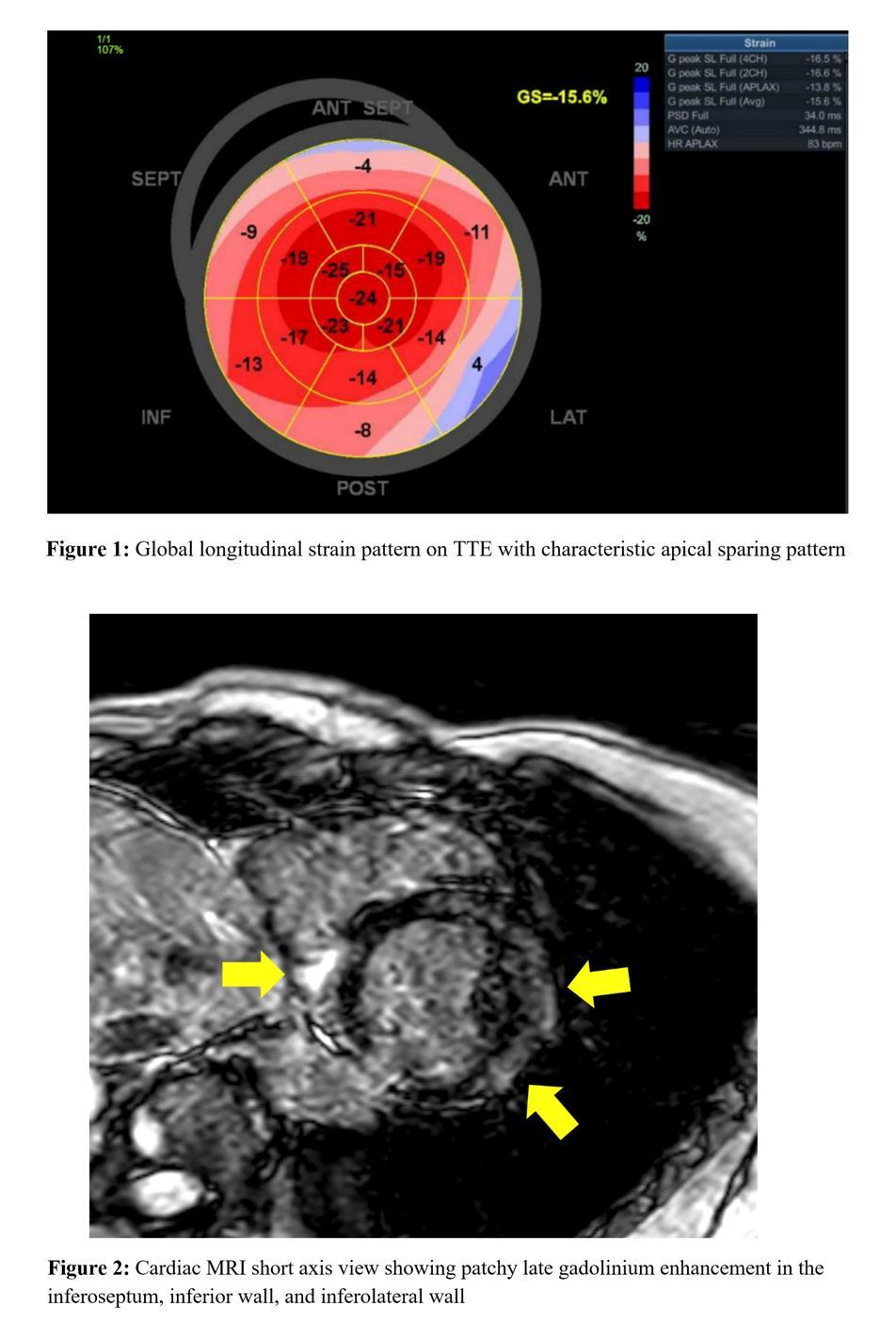
ABSTRACT #80
CLINICAL RESEARCH
CARDIOLOGY
LEFT VENTRICULAR GEOMETRY AND EXERCISE DIASTOLIC STRESS TEST COMPLEMENT THE PROGNOSTIC VALUE OF H2FPEF SCORE IN ELDERLY WITH NON-ISCHEMIC EXERCISE ECHOCARDIOGRAPHY
Kristen Carter1, Alaa Omar1, Arpanjeet Kaur1 , Kruti Gandhi1, Errol Moras1, Soumya Gupta1, Joseph Elias1 , Ga Hee Kim1 , Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: We studied left ventricular mass index (LVMi), exercise induced diastolic abnormality (ExDD) to H2FPEF score in predicting cardiovascular outcomes in elderly with preserved ejection fraction (EF).
METHODS: Retrospectively, we studied 578 patients with non-ischemic exercise echocardiography (ExE) (Age: 69 ± 6.2 years, 57% women, EF: 61±5%). LVMi abnormality was defined as >115 g/m2 in men and >95 g/m2 in women. ExDD was defined as post exercise E/e’>15. Patients were followed for a median of 3.7 years for death or heart failure hospitalizations (HFH).
RESULTS: During follow-up, 13 patients died, 27 had HFH and 39 had both outcomes. LVMi was 76.1 ± 24 g/m2 and H2FPEF score was 3±1.5. During ExE, patients achieved 8.5±2.7 METs, and 229 had ExDD. Abnormal LVMi (HR, 2.3; 95%CI, 1.1-4.9), H2FPEF>5 (HR, 3.6; 95%CI, 1.9-6.9), and ExDD (HR, 2; 95%CI, 1.1-3.8) were associated with outcomes. A score of the 3 variables was made ranging from 0 when all were normal to 3 when all were abnormal. Increasing score was associated with increased LV filling pressures post exercise, suggested by delta E/e’. A score of 2 (HR, 5.2; 95%CI, 2.3-12.1) and 3 (HR, 9.5; 95%CI, 2.6-34.6) were associated with increased combined outcomes which was preserved after adjusting for covariates.
CONCLUSION: In symptomatic elderly with preserved EF and non-ischemic ExE, H2FPEF score, LVMi, and ExDD are complementary in prediction of HF related outcomes. A majority of abnormalities among these domains put patients at special increased risk.
ABSTRACT #81
CLINICAL RESEARCH
CARDIOLOGY
ANEMIA IS NOT ASSOCIATED WITH INCREASED MORTALITY RISK FOR PATIENTS UNDERGOING LEFT VENTRICULAR ASSIST DEVICE IMPLANTATION
James Choi1, Benjamin Adegbite1, Darren Kong1, Sara Diaz1, Jose Aguilar Gallardo1 , Kiran Mahmood1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Heart Failure Society of America (HFSA) Annual Scientific Meeting that was held in Cleveland, Ohio, United States from October 6-9, 2023.
BACKGROUND/INTRODUCTION: Left ventricular assist devices (LVADs) are becoming more commonly used in patients with advanced heart failure, either as a temporary bridge to heart transplantation or as destination therapy, due to their ability to extend survival and improve quality of life. However, the impact of some co-morbid conditions, such as anemia, on outcomes after LVAD implantation warrants further investigation. In this study, we sought to evaluate anemia as an independent predictor of mortality and complications in those undergoing LVAD implantation for heart failure.
METHODS: This is a retrospective cohort study studying hospitalizations in the National Inpatient Sample (NIS) involving LVAD implantation between January 2017 and December 2019 in patients with and without anemia. The primary outcome was measurement of mortality risk in those with and without anemia undergoing LVAD implantation. Secondary outcomes focused on complications in hospitalization including cardiac arrest, cardiogenic shock, acute respiratory failure, acute kidney injury and ventricular arrythmia. Multivariate logistic analysis was used to adjust for age, gender, race, income quartile, Charlson Comorbidity Index, and other relevant comorbidities with a p-value<0.20 in univariate screen.
RESULTS: There were 12,855 hospitalizations involving implantation of an LVAD, of which 9,127 (71%) had anemia as a co-morbidity. Analysis revealed that anemia is not associated with increased odds of mortality in patients undergoing LVAD implantation (OR, 0.93; 95%CI, 0.64-1.33; p=0.695). The secondary outcomes of cardiac arrest, cardiogenic shock, ventricular arrythmia, and acute respiratory failure were also unchanged after adjusted analysis. There is, however, an increase in acute kidney injury with an OR=1.57 (95%CI, 1.20-2.05; p=0.001).
CONCLUSION: In this study, anemia has not been shown to be associated with increased mortality in patients undergoing LVAD implantation. However, there is a positive association with acute kidney injury highlighting the need to further investigate this increased risk in anemic patients.
ABSTRACT #82
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
COMPARATIVE ANALYSIS OF INFECTIOUS COMPLICATIONS IN PATIENTS WITH MULTIPLE MYELOMA TREATED WITH BCMA-TARGETED BISPECIFIC ANTIBODIES AND CAR T-CELL THERAPY
Karthik Nath1, Tala Shekarkhand1 , Bruno A. Costa2, David Nemirovsky1 , Andriy Derkach1, Noriko Nishimura1 , Tasmin Farzana1, Colin Rueda1, David Chung1,3 , Heather Landau1,3, Oscar Boutros Lahoud1,3, Michael Scordo1,3 , Gunjan L. Shah1, Hani Hassoun1,3 , Kylee H Maclachlan1,3, Neha Korde1,3, Urvi A Shah1,3, Carlyn Rose Tan1 , Malin Hultcrantz1,3, Sergio A. Giralt1,3, Saad Z Usmani1,3, Zainab Shahid1 , Sham Mailankody1,3, Alexander Lesokhin1
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Weill Cornell Medicine, New York, NY, United States Presented at the American Society of Hematology Annual Meeting that was held in San Diego, California, United States from December 9-12, 2023.
BACKGROUND/INTRODUCTION: There is limited data comparing infectious toxicities in patients with relapsed/refractory multiple myeloma (RRMM) treated with T-cell engaging therapies, which include chimeric antigen receptor T-cell therapy (CAR-T) and bispecific antibodies (BsAb). There are now three US FDA approved B-cell maturation antigen (BCMA)-targeting T-cell engagers, and several more in ongoing clinical development. Awareness regarding their infectious toxicities may inform treatment selection and mitigation strategies.
METHODS: We conducted a single-center, observational study in patients with RRMM comparing infectious complications in patients treated with a commercial or investigational autologous BCMA-targeting CAR-T versus patients treated with a commercial or investigational BCMA-targeting BsAb. The date of CAR infusion (day 0) was between 03/22/2017 02/27/2023 for the CAR-T patients. For the BsAb cohort, the date of treatment initiation (day 0) was between 01/21/2020-02/07/2023. All infection-specific variables were collected from day 0 until the date of next line of therapy or last follow-up, with a data cut-off of 06/01/23. Infectious events were graded according to CTCAE version 5.0. Prophylactic antimicrobials were administered according to institutional and protocol guidelines. The primary endpoint was the incidence of severe (grade 3) infections. Secondary objectives included the time to 1st infection, infection rate over time, infectious organisms, the impact of prolonged cytopenias, and the utility of intravenous immunoglobulin (IVIG) administration in preventing infections.
RESULTS: Of the total 147 patients, there were 92 CAR-T and 55 BsAb treated patients. The median age of the CAR-T and BsAb cohort was 62 years versus 65 years, respectively (p=0.043). CAR-T patients had a median of 6.5 prior lines of therapy (IQR, 5-8) versus 6.0 (IQR, 4-9) in the BsAb cohort (p=0.7); 97% of CAR-T patients had a prior autologous transplant compared to 75% in the BsAb cohort (p<0.001). In keeping with current clinical practice, 18 patients (33%) in the BsAb cohort had prior exposure to CAR-T whilst no patients in the CAR-T cohort had prior BsAb exposure. The median follow-up duration for infectious events was similar in both groups at 5.8 months (IQR, 3.8-9.2) for CAR-T and 4.3 months (IQR, 3.2-9.8) for the BsAb cohort. A total of 209 infections were reported: 115 with CAR-T and 94 with BsAb. In the CAR-T cohort 24/92 patients (26%) experienced1 severe infection, all of which were grade 3 and there were no grade 4 or 5 events. A numerically higher incidence was seen in the BsAb cohort with 21/55 BsAb patients (38%) experiencing 1 severe infection (p=0.14). Nineteen BsAb patients (35%) experienced grade 3 infections, 2 (3.6%) had grade 4 infections and 4 (7.3%) had grade 5 infections. Six CAR-T (6.5%) and 10 BsAb patients (18.2%) had >1 grade 3 infection. The incidence of 1 severe infection remained high in the BsAb cohort at 16/37 (43%) even after excluding the 18 BsAb patients with prior CAR-T exposure. The median time from treatment initiation to the first infection of anygrade was 2.5 months (95%CI, 1.2-NR) with CAR-T compared to 3.4 months (95%CI, 1.6-6.8) with BsAb (p=0.6). The rate of any-grade infections was similar between the two groups early post-therapy (before day 100). However, there was a significantly higher infection rate of any-grade after day 100 with BsAb compared to CART with a median of 0.24 (IQR, 0.18-0.34) versus 0.13 (IQR, 0.08-0.17) infections per 30 days,
respectively (p<0.001) (Figure 1A). Regarding the time to the first grade 3 infection, 79% occurred within day 100 for CAR-T patients compared to only 48% in the BsAb cohort (Figure 1B). The proportion of bacterial, viral, fungal, and parasitic infections in the CAR-T group was 49% (n=56), 48% (n=55), 4.3% (n=5) and 0.9% (n=1) respectively, and in the BsAb group was 51% (n=48), 44% (n=41), 3.2% (n=3), and 0.0% respectively.
CONCLUSION: Infectious complications were common early after BCMA-targeting BsAb and BCMA CAR-T and declined over time. In this real-world comparison, distinct from their CAR-T counterparts, BsAb recipients appeared to have a more persistent infection risk and higher incidence of severe infections, which included four patients having a grade 5 infection. Further analysis, including the impact of prolonged cytopenias and the utility of IVIG administration will be presented at the meeting.
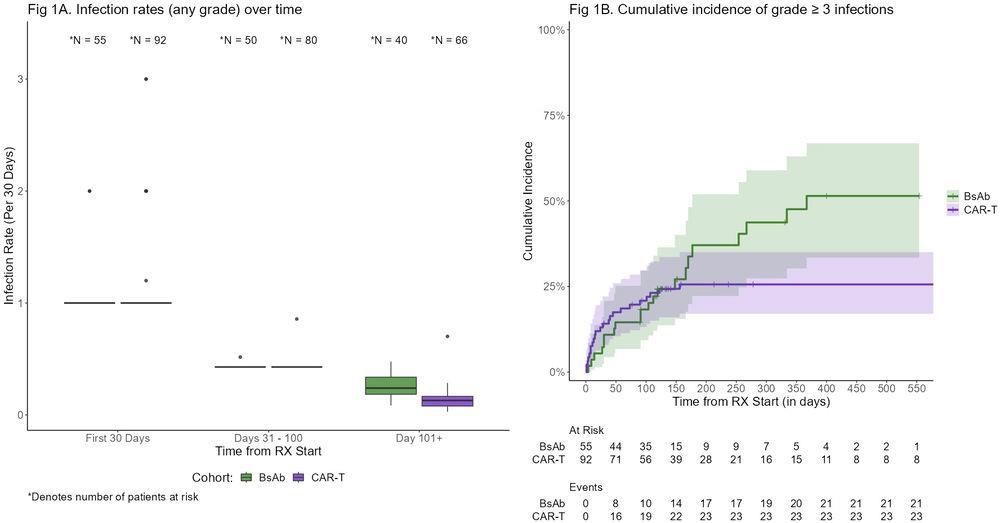
ABSTRACT #83
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
DEMOGRAPHIC DISPARITIES IN CLINICAL
ENROLLMENT OF UNITED
PATIENTS WITH NEWLY DIAGNOSED MULTIPLE
Bruno A. Costa1, Neha Debnath1, Thomaz Alexandre Costa2, Raphael Bertasi1, Tarek H. Mouhieddine3, Karthik Nath4, Adriana C. Rossi3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Federal University of Ceará, Fortaleza, Brazil; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Memorial Sloan Kettering Cancer Center, New York, NY, United States Presented at the American Society of Hematology Annual Meeting that was held in San Diego, California, United States from December 9-12, 2023.
BACKGROUND/INTRODUCTION: Racial, ethnic and gender disparities impact the real-world reproducibility of clinical trials leading to drug approvals for hematologic malignancies. Interestingly, a prior abstract (Boisclair et al., 2022) has shown an equitable enrollment between United States demographic groups in frontline trials for newly-diagnosed non-Hodgkin lymphoma. Although disparities in multiple myeloma (MM) trial participation have been oftentimes demonstrated, prior studies (Kanapuru et al., 2022; Alqazaqi et al., 2022) predominantly involved patients with relapsed/refractory MM (RRMM). To further assess this gap, we conducted a crosssectional analysis of United States demographic representation in phase II or III trials for newly-diagnosed MM (NDMM).
METHODS: Clinicaltrials.gov was searched for completed NDMM trials with a recruitment period between 01/01/2007-12/31/2020. Studies limited to phase I data (n=10), enrolling <30 patients (n=35), including RRMM or other malignancies (n=18), and/or recruiting outside the US (n=93) were excluded. We subdivided patients according to gender, race, and ethnicity. For each subgroup, total new cases of multiple myeloma from 20072020 were identified via the Surveillance, Epidemiology and End Results (SEER) Cancer Statistics Explorer Network, with subsequent calculation of a trial enrollment fraction (TEF; number of trial enrollees divided by incident United States cases). Pearson’s chi-square test was used to compare TEF between subgroups, yielding odds ratio (OR) and 95% confidence interval (95%CI) values, with p<0.05 deemed significant.
RESULTS: Among the 194 trials found on initial review, 25 met the established criteria for inclusion (Figure 1). All studies (n=3,559) described the participants’ gender, while only 18 (72%; n=3,129) reported race and 9 (36%; n=2,319) reported ethnicity. Overall, women showed a significantly lower TEF compared to men (OR, 0.88; 95%CI, 0.82-0.94; p<0.001). When compared to White Americans, TEF was significantly lower for African Americans (OR, 0.71; 95%CI, 0.64-0.78; p<0.001) and Asian Americans/Pacific Islanders (AAPIs; OR, 0.64; 95%CI, 0.22-0.41; p<0.001). In studies reporting ethnicity, TEF was significantly lower for Hispanics compared to non-Hispanics (OR, 0.18; 95%CI, 0.14-0.24; p<0.001).
CONCLUSION: Our cross-sectional analysis reveals an underrepresentation of women, African Americans, AAPIs, and Hispanics in NDMM trials conducted around the US. These findings are complementary to the enrollment disparities previously shown in RRMM trials. Through the implementation of a comprehensive diversity plan, multiple myeloma trials must include a more inclusive representation of the United States population affected by this blood cancer. Such an approach will not only enhance the external validity of these trials but also mitigate the impact of ascertainment bias and promote healthcare equity.
ABSTRACT #84
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
COMPREHENSIVE SPATIAL, TRANSCRIPTOMIC, AND GENOMIC ANALYSIS OF IMMUNOGENIC BILIARY TRACT CANCER
Wungki Park1,2 , Fergus Keane1, Hulya Sahin Ozkan1, Allison Richards1, Vasilisa Rudneva1 , Danny Khalil1,2 , Kevin Soares1,2 , Bruno A. Costa3, Darren Cowzer1, Zeyneb Tarcan1 , James Harding1,2, Olca Basturk2 , Dae Won Kim4, William Jarnagin1,2, Ghassan Abou-Alfa1,2, Mark Donoghue1, Eileen M O’Reilly1,2
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Weill Cornell Medical College, New York, NY, United States; 3Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 4Moffitt Cancer Center, Tampa, FL, United States
Presented at the Society for Immunotherapy of Cancer’s (SITC) Annual Meeting that was held in San Diego, California, United States from November 1-5, 2023.
BACKGROUND/INTRODUCTION: Biliary tract cancers (BTC) represent an uncommon and heterogeneous group of tumors of bile duct and the patients have poor prognosis. The TOPAZ-1 study led the approval of frontline durvalumab (D) in combination (GCD) with cisplatin and gemcitabine (GC) in advanced BTC. Modest durable responses with immune checkpoint inhibitor monotherapy (ICI) have also been reported in a subgroup among refractory BTC. To date, traditional ICI biomarkers (high tumor mutational burden [TMB], and PD-L1) have not shown a strong association with the response or outcomes. A paucity of comprehensive datasets with clinically annotated biospecimens has limited our ability to understand the impact of heterogenous biology (e.g. different etiology, driver mutations, and anatomic location) BTC outcomes on ICI, Herein, we report the initial analysis of comprehensive clinical, pathologic, genomic, and spatial transcriptomic analyses from large real-world and clinical trial datasets to describe the immunogenic BTC subgroup (iBTC).
METHODS: Patients with BTC treated at Memorial Sloan Kettering (MSK) and Moffitt, who received an ICI (> 2 cycles), GCD, GC between July 2017 and June 2023, were identified (IRB 19–006). Progression Free Survival (PFS) comparison was analyzed by the Kaplan Meier method. We included genomics using targeted gene sequencing and pathologic analyses of available tissues. Further bulk and spatial transcriptomic and exome analyses are ongoing.
RESULTS: During n=208 pts with BTCs who received either GCD (n=35), GC (n=128) and ICI (n=45) were identified at MSK. Across the whole group (n=208), median age 63 years (32–81 years), female (n=95; 45%), intrahepatic cholangiocarcinoma (IHCC) (n=144; 69%), extrahepatic cholangiocarcinoma (EHCC) (n=40; 19%), GBC (n=24; 12%). Hematoxylin and eosin (H&E) stains of n=45 samples were evaluated by a pathologist for tumor infiltrating (TI) and peritumoral (PT) lymphocytes (Lym), macrophages (Mac), and polymorphonuclear cells (PMN). No statistically significant differences were observed, but numerically higher peritumoral infiltration of lymphocytes and macrophages were observed in PT-Lym (p=0.13) and PTMac (p=0.16) when groups of PFS <6m and PFS>6m were compared. Deeper evaluation of the tumor immune contexture and their gene programming using spatial and bulk transcriptomic and genomic analyses (n=29 ICI, n=16 GCD) together with n=11 ICI from Moffitt are ongoing.
CONCLUSION: Durable responses (PFS>6M) to immunotherapy were seen in a subgroup of BTC. Currently available biomarkers have not predicted the response, but ongoing deeper analysis of spatial immune, tumor, and stromal microenvironment analysis will be presented.
ABSTRACT #85
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
IMPACT OF ABSOLUTE LYMPHOCYTE COUNT AT PRE‑APHERESIS AND PRE‑LYMPHODEPLETION ON CHIMERIC ANTIGEN RECEPTOR T THERAPY OUTCOMES IN RELAPSED REFRACTORY MULTIPLE MYELOMA
Noriko Nishimura1, Jessica Flynn1 , Bruno A. Costa2, Sean Devlin1, Tasmin Farzana1, Karthik Nath1, David Chung1, Heather Landau1, Oscar Lahoud1, Michael Scordo1, Gunjan Shah1, Hani Hassoun1, Kylee Maclachlan1 , Malin Hultcrantz1, Neha Korde1, Alexander Lesokhin1, Urvi Shah1, Carlyn Rose Tan1 , Sergio Giralt1, Saad Usmani1, Sham Mailankody1
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the International Myeloma Society Annual Meeting that was held in Athens, Greece from September 27-30, 2023.
BACKGROUND/INTRODUCTION: Biliary CAR-T cell therapy has been approved for patients with RRMM and 4 or more prior lines of therapy. Due to multiple prior treatments, some patients have a low absolute lymphocyte count (ALC) and data on the prognostic impact of pre-therapy ALC is conflicting. This real-world analysis investigated pre-apheresis (A) and pre-lymphodepletion (LD) ALC, and the ALC reduction between A and LD, on survival outcomes post CAR-T for RRMM.
METHODS: This was a single center, retrospective analysis of 88 patients with RRMM who received CAR-T cell therapy between March 2017 and December 2022. Both commercial (n=22) (BCMA-directed), and investigational (n=66) (BCMA- or GPRC5D-directed) CAR-T were included. We assessed the impact of Pre-A and Pre-LD ALC as well as the reduction in ALC (measured as the difference between pre-LD and pre-A ALC) on the progression-free survival (PFS) and overall survival (OS) using the Cox proportional hazard models.
RESULTS: The median age was 60 years (range, 37–79 years), of whom 52% were male. The median number of prior lines of therapy was 7 (range, 2–20). Extramedullary disease (EMD) was present in 51%, and 52% of patients received bridging therapy. The median pre-A and pre-LD ALC was 0.7Å~109/L (range, 0.1–3.4) and 0.7x109/L (range, 0.1–3.1), respectively. The median absolute reduction in ALC was 0.0 (range, -2.7 to 2.3). Using the lowest quartiles, low pre-A ALC and low pre-LD ALC were defined as ≤0.5x109/L and 0.4x109/L, respectively. A high reduction was set ≥0.27x109/L, as described in a prior study. The median follow-up duration post CAR-T infusion was 24 months. There was no significant difference in PFS with either a low versus high pre-A ALC (HR, 1.52; 95%CI, 0.92–2.50; p=0.11), low versus high pre-LD ALC (HR, 1.57; 95%CI, 0.93–2.68; p=0.10), or a high absolute reduction in ALC between these timepoints (HR 1.39; 95%CI, 0.82–2.36; p=0.24). On multivariate analysis, only EMD, high-risk cytogenetics, and ECOG-score of 1/2 were independently associated with a significantly inferior PFS. Regarding OS, on univariate analysis, low pre-LD ALC was significantly associated with a shorter OS (median OS, 13 versus 29 months; HR, 0.47; 95%CI, 0.24–0.92; p=0.032), as was presence of EMD, double refractory status, and Revised-International Staging System (R-ISS) of 2/3. Low pre-A ALC and a high absolute reduction in ALC between A and LD (≥0.27) had no significant impact on OS. On multivariate analysis, only EMD was associated with a significantly shorter OS (HR, 4.17; 95%CI, 1.96–8.87; p<0.001).
CONCLUSION: On multivariate analysis, the pre-A, -pre-LD, and the absolute reduction in ALC prior to CAR-T administration had no significant impact on either PFS or OS. Inferior survival outcomes post-CAR-T appear to be driven by previously recognized factors like the presence of EMD, high-risk cytogenetics, and reduced baseline performance status. Of note, all patients had an ALC > 0.1x109/L and the impact of pretreatment ALC below this level cannot be assessed from this analysis.
ABSTRACT #86
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
PROGNOSTIC IMPACT OF CORTICOSTEROID AND TOCILIZUMAB USE ON THE EFFICACY OF CHIMERIC ANTIGEN RECEPTOR T‑CELL THERAPY FOR RELAPSED/REFRACTORY MULTIPLE MYELOMA
Bruno A. Costa1, Jessica Flynn2 , Karthik Nath2, Noriko Nishimura2, Sean Devlin2, Tasmin Farzana2, David Chung2, Heather Landau2, Oscar Lahoud2, Michael Scordo2, Gunjan Shah2, Hani Hassoun2, Kylee Maclachlan2 , Malin Hultcrantz2, Neha Korde2, Alexander Lesokhin2, Urvi Shah2, Carlyn Rose Tan2, Sergio Giralt2, Saad Usmani2, Sham Mailankody2
1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the International Myeloma Society Annual Meeting that was held in Athens, Greece from September 27-30, 2023.
BACKGROUND/INTRODUCTION: Chimeric antigen receptor T-cell (CAR-T) therapy targeting B-cell maturation antigen (BCMA) or G proteincoupled receptor, class C, group 5, member D (GPRC5D) has shown unprecedented efficacy in patients (pts) with relapsed/refractory multiple myeloma (RRMM). Immune-related adverse events (irAEs) such as cytokine release syndrome (CRS) and neurotoxicity may occur early in treatment. Whilst immune-suppressive agents such as tocilizumab (TCZ) and corticosteroids (CS) are used to manage irAEs, a potential concern is a negative effect on CAR-T efficacy and survival outcomes. Here, we evaluated the prognostic impact of TCZ and CS use within 30 days of CAR-T infusion.
METHODS: This was a single-center, retrospective cohort study involving RRMM patients aged≥18 years and treated with commercial/investigational anti-BCMA or anti-GPRC5D CAR-T therapy from April 2017 to September 2022. Fisher’s exact test was used to determine whether CS use influenced the overall response rate (ORR; ≥PR as per IMWG Criteria). We also performed a 30-day landmark analysis using multivariable Cox proportional hazards models to evaluate the impact of TCZ administration and CS administration/dosing on progression-free survival (PFS) and overall survival (OS).
RESULTS: Among the 102 patients included (46% female), the median age was 62 years (range, 37-79 years) and median number of prior lines of therapy was 6 (range, 2-20). Triple-class refractoriness (TCR), extramedullary disease (EMD), and high-risk cytogenetics were present in 83%, 49%, and 70% of patients, respectively. Anti-BCMA CAR-T was used in 93 patients (91%), and anti-GPRC5D CAR-T in 9 patients (9%). After CAR-T infusion, 77% of patients developed CRS (35% grade 1; 34% grade 2; 8% grade 3) and 14% developed neurotoxicity (8% grade 1; 4% grade 2; 2% grade 3). A total of 42 patients (41%) and 29 patients (28%) received TCZ and CS within 30 days post-infusion, respectively. No significant difference in ORR was observed between patients who received CS and those that did not (66% versus 83%; p=0.089). Following a 30day landmark analysis, both PFS and OS were significantly inferior in patients with EMD with hazard ratio (HR) of 1.86 (95% confidence interval [CI], 1.05-3.29; p=0.034) and 3.88 (95%CI, 1.71-8.76; P20 mg versus ≤20 mg). Similarly, there was no significant difference in either PFS (HR, 1.06; 95%CI, 0.55-2.04; p=0.87) or OS (HR, 1.03; 95%CI, 0.40-2.68; p=0.95) in patients who received TCZ versus those that did not.
CONCLUSION: CS and TCZ treatment for irAEs does not appear to compromise CAR-T efficacy or survival outcomes in RRMM patients. These results support the timely and appropriate use of these drugs for attenuating CAR-T-related toxicities. CAR-T cell therapy has been approved for patients with RRMM and 4 or more prior lines of therapy. Due to multiple prior treatments, some patients have a low absolute lymphocyte count (ALC) and data on the prognostic impact of pre-therapy ALC is conflicting. This real-world analysis investigated preapheresis (A) and pre-lymphodepletion (LD) ALC, and the ALC reduction between A and LD, on survival outcomes post CAR-T for RRMM.
ABSTRACT #87
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY
VITAMIN D DEFICIENCY AND CLINICAL OUTCOMES WITH CHIMERIC ANTIGEN RECEPTOR T CELL THERAPY IN RELAPSED/REFRACTORY MULTIPLE MYELOMA
Noriko Nishimura1, Jessica Flynn1 , Bruno A. Costa2, Sean Devlin1 , Tasmin Farzana1, David Chung1, Heather Landau1, Oscar Lahoud1, Michael Scordo1, Gunjan Shah1, Hani Hassoun1, Kylee Maclachlan1, Malin Hultcrantz1 , Neha Korde1, Alexander Lesokhin1,Urvi Shah1, Carlyn Rose Tan1, Sergio Giralt1, Saad Usmani1 , Sham Mailankody1, Karthik Nath1 1Memorial Sloan Kettering Cancer Center, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the International Myeloma Society Annual Meeting that was held in Athens, Greece from September 27-30, 2023.
BACKGROUND/INTRODUCTION: Vitamin D deficiency is a potentially modifiable risk factor for poor outcomes in relapsed/refractory multiple myeloma (RRMM). Recent studies demonstrated that vitamin D deficiency may be associated with inferior survival in recipients of autologous stem-cell transplant (ASCT) (Eicher, Hem Onc, 2020). Additionally, we previously demonstrated that vitamin D insufficiency is associated with inferior clinical outcomes in patients with B-cell lymphoma treated with CD19-directed chimeric antigen receptor T-cell therapy (CAR-T) (Nath, TCT, 2022). The role of circulating vitamin D in patients with RRMM treated with CAR-T is currently unknown. Here, we evaluated the impact of vitamin D status on clinical outcomes in this patient population.
METHODS: We performed a single-center, retrospective analysis of adult patients with RRMM who received commercial or investigational CAR-T between 04/2017–09/2022 and had a serum vitamin D (25[OH]D) measured pre-CAR-infusion. Vitamin D deficiency was defined as <20ng/mL as per the Endocrine Society guidelines. Cox proportional hazards models were used to assess the impact of pre-CAR-T vitamin D status on progression-free survival (PFS) and overall survival (OS).
RESULTS: Of the 102 patients with RRMM who received CAR-T, 61 patients had a pre-CAR infusion vitamin D level available. The median age of the 61 patients was 62 years (range, 38-79), with 57% males. Patients were heavily pretreated with a median 6 prior lines of therapy (range, 2–14), and 97% had a prior ASCT. Triple-class refractoriness (TCR), extramedullary disease (EMD), and high-risk cytogenetics (HRC) were observed in 80%, 52%, and 70% of patients, respectively. Baseline characteristics were overall comparable between vitamin D deficient (<20ng/mL; n=11) and vitamin D replete (≥20ng/mL; n=50) patients. On univariate analysis, vitamin D deficient compared to replete patients had a significantly inferior PFS (median PFS, 3.5 months versus 6.5months, HR of 2.24, 95% Confidence Interval [CI] 1.09-4.59; p=0.041). These differences maintained significance in a multivariate analysis adjusting for baseline characteristics (age, gender, ECOG performance status, HRC, EMD, penta-refractory status) (HR of 2.53; 95%CI, 1.14–5.66; p=0.032). There was no significant difference in OS based on vitamin D status in both the univariate and multivariate analysis. Only EMD and decreased performance status (ECOG 1 or 2) was an independently significant poor prognostic factor for OS.
CONCLUSION: In this modest cohort of patients with RRMM, vitamin D deficiency (<20ng/mL) prior to CAR-T cell therapy was potentially associated with inferior PFS. However, the small sample size and the possibility of residual confounding precludes concrete conclusions. Future studies with larger cohorts of patients will be needed to confirm these findings.
ABSTRACT #88
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PULMONARY/CRITICAL CARE
UNIQUE CASE OF
Neha Debnath1 and James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Cocaine is a popular recreational drug in the United States. Up to 70% of seized Cocaine contains levamisole, an anti-helminthic that can cause cutaneous vasculitis with positive antineutrophil cytoplasmic antibodies. We report a unique case of ANCA negative diffuse intra-abdominal vasculitis following cocaine ingestion.
CASE PRESENTATION: A 57-year-old man with a medical history of alcohol and cocaine abuse presented with complaints of abdominal pain and vomiting. He reported excessive alcohol and cocaine use over the previous 3 days. On initial presentation, he was hypotensive with a blood pressure of 80/54 mmHg and his exam was significant for diffuse abdominal tenderness. Labs were significant for a potassium 6.1 mmol/L, creatinine 5.18 mg/dl, AST 20,940 U/L, ALT 4050 U/L, lactate 11 mmol/L, and Trop 16. He was admitted to the ICU for circulatory shock requiring multiple vasopressors, severe metabolic acidosis and severe rhabdomyolysis with CPK of 141,300. Urine toxicology was positive for cocaine. CT of the abdomen showed a circumferential wall thickening of the SMA, celiac artery, proximal splenic artery, and common hepatic artery compatible with vasculitis and bilateral renal infarcts. His ICU course was complicated by hypoxic respiratory failure requiring intubation, severe ARDS, AKI requiring renal replacement therapy and shock liver. A thorough autoimmune workup including ANA, Anti-Smith antibodies, Anti-dsDNA antibody, ANCA antibodies (MPO), C3 and C4 levels were negative. Despite aggressive critical care interventions, the patient clinically deteriorated and ultimately expired.
CONCLUSION: Cocaine induces 2 forms of vasculitis: ANCA associated vasculitis due to levamisole and a vasculitis due to direct cocaine toxicity. It is increasingly seen that direct cocaine toxicity may trigger a vasculitis which mimics true idiopathic ANCA-associated vasculitis. Patients may be positive for PR3-ANCA or MPOANCA. Determining whether cocaine exposure induces ANCA or whether patients develop unrelated idiopathic small/medium vessel vasculitis is often challenging. Our case is one of the few ANCA negative intra-abdominal vasculitis without any skin findings. This case highlights the importance of recognizing atypical presentations of cocaine-induced vasculitis, given its life-threatening complications.
ABSTRACT #89
CLINICAL RESEARCH
GASTROENTEROLOGY
CAN MANOMETRIC BOLUS CLEARANCE BE USED TO CONFIRM ESOPHAGOGASTRIC JUNCTION OUTLET OBSTRUCTION?
Binoy V. Desai1 , Emily Seltzer1, Michael S. Smith1, Kimberly Cavaliere1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the Digestive Disease Week (DDW) Annual Meeting to be held in Washington, D.C., United States from May 18-21, 2024.
BACKGROUND/INTRODUCTION: Under Chicago Classification v4.0, Esophagogastric Junction Outlet Obstruction (EGJOO) suspected on high-resolution manometry (HRM) must be accompanied by appropriate symptoms and confirmed with either timed barium esophagram (TBE) or upper endoscopy with impedance planimetry (FLIP). The aim of this study was to determine if the HRM parameter of incomplete bolus clearance (IBC) could also play a role in confirming EGJOO.
METHODS: A total of 120 patients with EGJOO suspected on HRM performed at a single high-volume motility center between 3/2020 and 9/2023 were considered for inclusion, with 72 patients excluded due to a history of prior foregut surgery, achalasia, or lack of confirmatory testing. HRM studies were manually reviewed to determine percent total IBC and percent distal esophageal IBC during supine swallows. HRM studies were defined as having IBC if at least 30% of swallows demonstrated bolus retention. EGJOO was considered confirmed if FLIP showed reduced distensibility index (DI) or if TBE showed either delayed contrast or tablet clearance. When an 8 cm long FLIP bag was used, DI measurements were recorded during distention to 40 mL and 50 mL. With a 16 cm long FLIP bag, DI measurements were recorded at volumes of 60 mL and 70 mL. Pearson correlation was used to determine the relationship between IBC and DI on FLIP. Independent t-test, Fisher’s exact test, and Mann-Whitney U test were used to compare patients with confirmed and unconfirmed EGJOO.
RESULTS: Patients with confirmed EGJOO were more likely to be male (p=0.007) than those with unconfirmed EGJOO, whereas there was no difference among groups when it came to age, body mass index, or hiatal hernia (Table 1). Patients with confirmed EGJOO tended to have more IBC (total: 93.3% versus 66.7%, p=0.073; distal: 73.3% versus 51.5%, p=0.212). Neither total nor distal IBC on HRM correlated with DI at smaller (total: r= -0.317, p=0.067; distal: r= -0.144, p=0.415) or larger FLIP bag volumes (total: r= - 0.115, p=0.537; distal: r= 0.024, p=0.896, respectively) (Table 2).
CONCLUSION: IBC during supine swallows did not significantly correlate with established confirmatory tests for EGJOO, suggesting that percent bolus clearance on HRM cannot be used at this time as a predictive parameter for EGJOO confirmation. However, given the relatively small sample size and a trend toward increased IBC in EGJOO-confirmed patients, additional evaluation with a larger cohort should be performed.

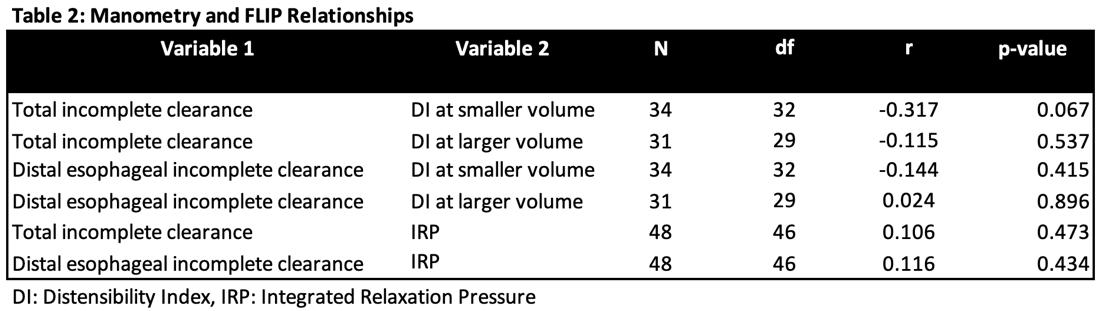
ABSTRACT #90
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
A CASE OF TAKOTSUBO CARDIOMYOPATHY ASSOCIATED WITH TRASTUZUMAB-PACLITAXEL CHEMOTHERAPY
Sara Diaz Saravia1, James Choi1, Soumya Gupta1, Shelly Brejt2, Susan Lin1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2New York University Langone Health, New York, NY, United States
Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
BACKGROUND/INTRODUCTION: The use of trastuzumab has been associated with heart failure and loss of left ventricular contractile function. Paclitaxel is also associated with cardiotoxicity and especially in combination with anthracyclines. Trastuzumab-induced Takotsubo cardiomyopathy (TCM) has been rarely reported and even less so in combination with Paclitaxel. We describe a rare case of TCM in a patient receiving trastuzumabpaclitaxel chemotherapy.
CASE PRESENTATION: A 76-year-old woman with a history of stage IIIB breast cancer, hypertension, hyperlipidemia, and non-insulin dependent diabetes mellitus type II presented to the Emergency Department with fatigue and poor oral intake of five days of onset. She had started her second cycle of neoadjuvant trastuzumab-paclitaxel one week before presentation. Initial vital signs were remarkable for HR 97 and BP of 163/72. Physical exam showed bilateral lower extremity edema, and fine tremors on bilateral upper extremities at rest and with movement. Initial laboratory work-up was remarkable for a mildly elevated troponin I of 0.225 ng/ml, with a peak troponin of 1.552 ng/ml five hours after presentation. Blood results were also notable for hypomagnesemia (<0.7 mg/dl), hypophosphatemia (1.7 mg/dl), and hypokalemia (2.8 mg/dl). Chest x-ray was unremarkable. EKG and telemetry showed paroxysmal Atrial Fibrillation (AF). Follow-up EKG three days after presentation showed QTc prolongation, diffuse T-wave inversions, Q waves in DII, DIII and aVF (Figure 1). Given the acute troponin elevation, new-onset AF, evidence of lateral lead ischemic changes on EKG, and physical exam findings, the differential diagnosis included NSTEMI, atrial fibrillation with myocardial injury secondary to severe electrolyte abnormalities in the setting of poor oral intake, and cardiotoxicity secondary to trastuzumabpaclitaxel. A transthoracic echocardiogram (TTE) showed severe new onset left ventricular systolic dysfunction. There was akinesis of all mid and apical segments with preserved function of basal segments (Figure 2, see Sup.1 for TTE clip). Left ventricular (LV) ejection fraction was estimated at 15%. Her findings were compatible with TCM. Prior to the initiation of chemotherapy in December, the patient had a TTE which demonstrated LV ejection fraction of 60-65%, no wall motion abnormalities and no valve abnormalities. Coronary angiography was performed and revealed non-obstructive coronary artery disease across all segments of the left main, left anterior descending, and lateral circumflex arteries. (Figure 3). Ventriculogram confirmed severe hypokinesis of all left ventricular segments with basal sparing. The patient was then started on a beta-blocker and angiotensin II receptor blocker during hospital admission, with further cardiology follow-up in the outpatient setting.
CONCLUSION: In this case report, we present a rare case of TCM associated with trastuzumab-paclitaxel therapy. It is essential to recognize that whilst many studies demonstrate the potentially harmful effects of trastuzumab and, to a lesser extent, paclitaxel on left ventricular function, acute heart failure secondary to TCM has also been described with these therapies and may well be underreported. Whether these chemotherapy agents can directly induce TCM or, rather, a result of psychological and physical stress remains unanswered. The clinical and pathogenic difference between trastuzumab or paclitaxel-induced ventricular dysfunction and TCM is unclear; the approach to these cases will have to be considered on an individual basis until more data is available.

Figure 1. Follow-up EKG with QTc prolongation, diffuse T wave inversions, Q waves in DII, DIII, aVF, and poor R wave progression
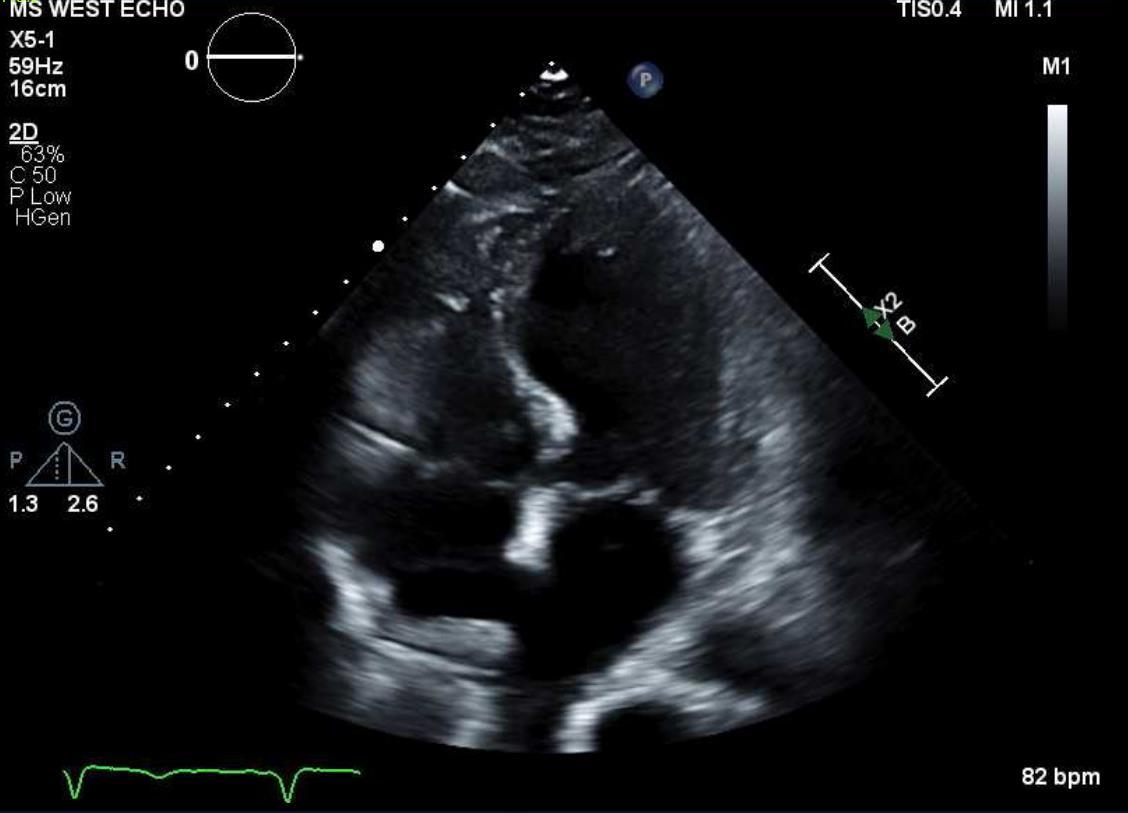

ABSTRACT #91
CLINICAL RESEARCH
CARDIOLOGY/HEMATOLOGY/ONCOLOGY
CANCER AND SHORT-TERM
Sara Diaz Saravia1, James Choi1, Christopher N. Matthews1, Darren Kong1, Souyma Gupta1, Sakul Sakul1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Transcatheter Cardiovascular Therapeutics (TCT) Annual Meeting that was held in San Francisco, California, United States from October 23-26, 2023.
BACKGROUND/INTRODUCTION: Cancer has been associated in the past with worsening cardiovascular outcomes like heart failure and ischemic heart disease. However, the prevalence and risk of acute myocardial infarction (AMI) complications in the oncologic population are unclear.
METHODS: A retrospective cohort study was carried out using the National Inpatient Sample database from January 2017 to December 2019. The population was then divided according to history of cancer using the International Classification of Diseases coding system. A total of 6 major cancers were included: lung, colorectal, breast, renal, prostate, and hematological cancer. Baseline population characteristics were defined. The main outcome was a composite of AMI complications by overall cancer and cancer site. This included intracardiac thrombosis, chordae tendineae rupture, wall rupture, papillary muscle rupture, atrial-septal defect, and ventricular septal defect. Univariate and multivariate analysis were done adjusting for age, race, income quartile, and Charlson comorbidity score.
RESULTS: Atotal of 3,478,360 cases ofAMI were identified of which 4.62% had a history of cancer.At baseline, AMI patients with cancer were significantly older (age 73 years versus 68 years; p<0.01) and mostly men (38.47% versus 41.25%; p<0.01). The rate of AMI complications was higher in the non-oncologic group (0.32% versus 0.26%; p=0.059) albeit nonsignificant. Overall cancer was not associated with higher odds of AMI complications (OR, 0.90; 95%CI, 0.67-1.21; p=0.503). However, there was a statistically significant association between breast cancer and AMI complications (OR, 2.23; 95%CI, 1.05-4.81; p=0.036) adjusting for confounding factors. The rest of the results are detailed in Table 1.
CONCLUSION: While overall cancer was not associated with increased AMI complications, certain cancer sites might be a significant risk factor for them. Breast cancer and renal cancer seem be at higher risk for AMI complications. Further prospective studies are needed to clarify the real risk of cancer patients, by cancer site, for AMI complications.

Table 1. Predictors of acute myocardial infarction.
ABSTRACT #92
CLINICAL RESEARCH
CARDIOLOGY
MORTALITY AND OUTCOMES OF PATIENTS WITHOUT STANDARD MODIFIABLE RISK FACTORS UNDERGOING CORONARY REVASCULARIZATION
Sara Diaz Saravia1, James Choi1, Christopher N. Matthews1, Serdar Farhan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Lifestyle modifications and reduction of Standard Modifiable Risk Factors (SMuRFs) have been the forefront of Primary and Secondary Prevention in Cardiology, long with optimal medical therapy. However, recent studies have demonstrated a higher risk of 30-day mortality in patients without Standard Modifiable Risk Factors (SMuRF-less) presenting with STEMI and NSTEMI. It is unclear if there is a higher risk of Mortality and MACE in SMuRF-less patients undergoing coronary revascularization.
METHODS: A retrospective cohort study was carried out using the National Inpatient Sample (NIS) database from January 2017 to December 2019, with patients who had undergone either a PCI or CABG. The population was then divided according to the presence or absence of SMuRFs into two groups (SMuRF versus SMuRF-less) using the International Classification of Disease (ICD) coding system. Baseline population characteristics were designed. Main outcome was defined as overall mortality and Major Adverse Cardiovascular Events (MACE). Univariate and multivariate analysis were done adjusting for age, race, and Charlson comorbidity score.
RESULTS: A total of 1,887,800 patients underwent Coronary Revascularization, of which 1,698,650 had SMuRFs. SMuRF-less patients were significantly younger compared to patients with SMuRFs (48 versus 65 years, p<0.001) and mostly female (30.96% versus 39.24%, p<0.001). Multivariate analysis showed that SMuRF-less patients had a significantly high odds of mortality (OR, 4.57; 95%CI, 4.28-4.87; p<0.001), adjusted for confounders. Additionally, SMuRF-less patients also had increased odds for MACE, although to a lesser degree (OR, 1.33; 95%CI, 1.27-1.39; p<0.001).
CONCLUSION: The absence of SMuRFs is a significant predictor for increased odds of mortality and MACE. It is unclear if this is result of under-recognition of risk factors or underestimation of baseline risks. Further studies are needed to elucidate the factor behind the cardiovascular risk of SMuRF-less patients.
ABSTRACT #93
CLINICAL RESEARCH
CARDIOLOGY
PRESENCE AND SEVERITY OF SUBCLINICAL ATHEROSCLEROTIC DISEASE IN THE PRIMARY PREVENTION OF THE ONCOLOGIC POPULATION
Sara Diaz Saravia1, Sergio Gonzalez, María Brenzoni2, Pamela Alarcón2, Fabián Ferroni2 , Carlos Castellaro2 , Jorge A. Chiabaut2, Renzo Melchiori2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Hospital Universitario Austral, Buenos Aries, Argentina
Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: There is scant evidence regarding endothelial dysfunction and damage in patients with a history of cancer in primary prevention and its impact on the development of subclinical atherosclerotic disease (SCASD).
METHODS: A cross-sectional study was done using a registry of patients enrolled in primary prevention who underwent a Doppler ultrasound (D-US) screening for SCASD in the carotid and ileo-femoral territory, from September 2020 to April 2023. Patients older than 18 years old without a previous cardiovascular and/or cerebrovascular event were included. History of cancer was defined as active or remitted cancer, excluding squamous and basal cell carcinoma. The population was then divided in two according to this last criterion: G1: non-oncologic group, and G2: oncologic group. SCASD was defined as the presence of ≥1 atherosclerotic plaque in the carotid and/or ileo-femoral territory according to the Mannheim Consensus. Univariate and bivariate analyses were performed to establish population characteristics. Several adjustment models were done comparing oncological history and the presence and distribution of SCASD.
RESULTS: A total of 7920 patients were included: 7694 in G1 and 226 in G2 (97.15% versus 2.85%). G2 patients were older, mostly women, and had a higher prevalence of hypertension and dyslipidemia. A linear regression analysis was done to assess the total plaque area by history of cancer, adjusted for age, sex, smoking history, dyslipidemia, sedentarism, diabetes mellitus, and hypertension. The result shows that a history of cancer significantly increases the total plaque area by an average of 8 mm [Coeff 8.2 p0.045; 95%CI, 0.2-16, adjusted R2=0.32]. Multivariate analysis was made to determine whether cancer behaved as a predictor for SCASD. In our cohort, oncologic disease behaved as an independent predictor of SCASD (OR, 1.43; 95%CI, 1.06-1.95; p=0.021). The model was tested for adequacy and was deemed to have adequate calibration and prediction power, with ROC=0.75 (95%CI, 71-78) and H&L=0.78.
CONCLUSION: The prevalence of oncologic disease in our population enrolled in primary prevention was of 2.85%. Patients with a history of cancer presented more SCASD, behaving as an independent risk factor for an increase in total plaque area adjusted for classic risk factors. These findings raise the need for more intensive control of SCASD in cancer patients. More studies are needed to verify these findings and clarify the pathophysiological mechanisms.
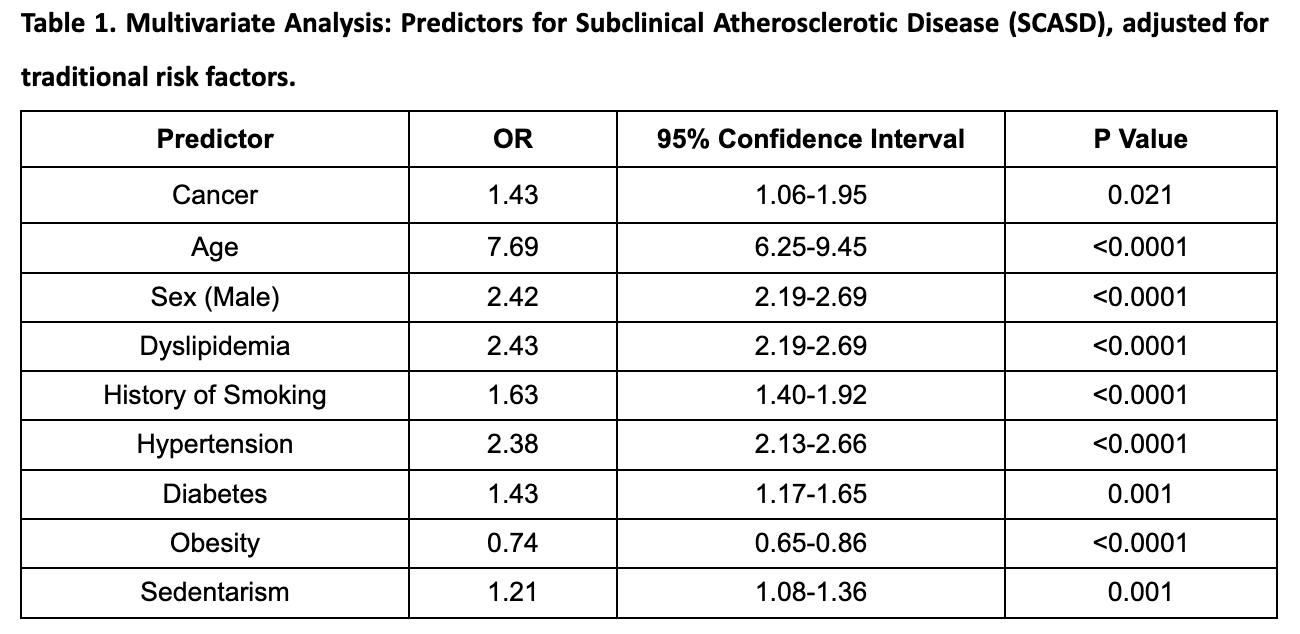
ABSTRACT #94
CLINICAL RESEARCH
CARDIOLOGY
Sara Diaz Saravia1, James Choi1, Christopher N. Matthews1, Serdar Farhan1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Cardiovascular disease and Cancer are the leading causes of mortality worldwide. There is growing evidence that patients with active cancer and cancer survivors are at increased risk for acute cardiovascular events. The inflammatory mechanisms of cancer and its treatment can be associated to the pathophysiological conditions that favor the progression of atherosclerosis. However, despite these speculations, there is scant information about the evolution of oncologic patients in secondary prevention after an Acute Coronary Syndrome.
METHODS: Single center observational retrospective study with patients presenting with ACS from 2008 to 2022. Primary endpoint: Composite of MACE in the secondary prevention within 3 years of ACS. Secondary endpoint: stratified analysis for MACE in secondary prevention for patients without Radiotherapy and Chemotherapy.
RESULTS: A total of 90,900,000 adults were identified, of which 4,888,734 had cancer. From the adult population, 197350 patients with an in-hospital diagnosis of ISR were identified. Primary analysis revealed that cancer is not associated with increased odds of ISR but rather decreased adjusted for other comorbidities, with an (OR, 0.181; 95%CI, 0.167-0.198; p<0.001). Paradoxically, secondary analysis of the ISR subpopulation showed statistically significant differences between cancer and non-cancer patients in the rate of composite MACE, and other cardiovascular outcomes such as Heart Failure, Atrial Fibrillation, and other arrhythmias (Table 1).
CONCLUSION: In the present study it is demonstrated that cancer had decreased odds for ISR, but further analysis demonstrated that in patients with ISR, the oncologic population was associated with higher composite MACE, mostly due to Atrial Fibrillation and other arrhythmias. Further studies are needed to explain the dynamic and non-linear relationship between cancer and cardiovascular outcomes.

ABSTRACT #95
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
INFECTIOUS DISEASES
AN UNUSUAL CASE OF STROKE DUE TO CRYPTOCOCCAL MENINGITIS WITH IDIOPATHIC CD4 LYMPHOCYTOPENIA
Jin Feng1, Tal Shachi1,2, Jennifer Fung1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
BACKGROUND/INTRODUCTION: Cryptococcal meningitis can present with stroke. Here, we discuss a case of stroke caused by disseminated cryptococcal infection with incidental findings of Idiopathic CD4 Lymphocytopenia (ICL).
CASE PRESENTATION: A 59-year-old male with a history of coronary artery disease was admitted after syncope with headaches, blurry vision, and hearing loss. MRI brain showed subacute infarcts in right cerebellum and multiple punctate recent infarcts in bilateral fronto-parietal areas. MRA head revealed bilateral small arterial stenoses. TTE showed no emboli. ANCA screen was negative. Patient's mental status waxed and waned, complicated by hyponatremia. EEG showed generalized slowing without seizures. He developed altered mental status requiring intubation. CT Head revealed subacute left cingulate gyrus infarct with repeat CT showing diffuse cerebral edema. The patient progressed to brain death. Labs revealed positive cryptococcal antigen, for which he underwent lumbar puncture with subsequent Cryptococcus neoformans growth in the CSF culture. HIV-1/2 and HTLV-1/2 were negative. With further chart review, he had persistent lymphopenia. CD4 count was 35 (13%). Autopsy revealed the cause of death to be disseminated cryptococcal infection in his lungs, kidneys, liver, and CNS, with depleted lymph nodes secondary to ICL.
CONCLUSION: Stroke, caused by infectious vasculitis, is an uncommon manifestation of Cryptococcal meningitis (4%). ICL, first described in 1992, is extremely rare (<0.2% of immunodeficiency). Diagnosis requires CD4+T cell < 300 (20%) on separate occasions without other underlying causes. When the patient had disseminated cryptococcus without HIV infection, malignancy, COVID, autoimmune disorders, or immunosuppressive treatments, and with confirmed CD4 lymphopenia of 35, T-cell immunodeficiency likely ICL was suspected.

Figure 1. The trend of WBCs, lymphocytes, and neutrophils during the patient’s hospitalization.
ABSTRACT #96
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE RHEUMATOLOGY
ATYPICAL GOUT FLARE AFTERTOTAL KNEE ARTHROPLASTY COMPLICATED BY PROSTHETIC JOINT INFECTION
Jin Feng1 , Shin Min Lao2, Oliva Ghaw2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Congress of Clinical Rheumatology Annual Meeting that was held in San Diego, California, United States from September 7-10, 2023.
BACKGROUND/INTRODUCTION: Gout affects millions in the US but is rare in post-operative joints. There is scarce data on gout in the post-total knee arthroplasty (TKA) subpopulation. Here we discuss a case of acute gout flare in a patient with bilateral TKA who was later found to have prosthetic joint infection (PJI).
CASE PRESENTATION: A 78-year-old female with a medical history of gout, CKD, and bilateral TKA (1990s) presented with worsening atraumatic left knee pain for one week. She was afebrile and the exam revealed a hot tender left knee with a large effusion. She also had synovitis in her right ankle, left third PIP joint, and bilateral MTP joints. Blood tests showed a WBC count of 18.4K, uric acid 13.3 mg/dL, CRP 174.6 mg/L, and ESR 108 mm/hr. X-ray of the left knee ruled out fractures, and CT of the left knee revealed joint effusion. Left knee arthrocentesis was performed, and synovial fluid analysis showed 550 WBCs and intracellular negatively birefringent needle-shaped monosodium urate (MSU) crystals. Gram stain was negative. Thus, she was diagnosed with a polyarticular gout flare and was started on methylprednisolone 24 mg. She also received empiric ceftriaxone for cellulitis of the lower leg. While most of her joint pain improved with steroids, the patient's left knee pain worsened. It was attributed to a large joint effusion. Methylprednisolone was then increased to 40 mg and allopurinol was also started. The synovial fluid culture subsequently grew Propionibacterium acnes after seven days. Repeat CT of the left knee with contrast showed a rim-enhancing left knee effusion, not excluding infection. A repeat left knee arthrocentesis showed WBCs of 16.6K (70% PMNs). Given the rising synovial WBCs, CT findings, and positive synovial culture, PJI was diagnosed. She underwent left knee two-stage revision arthroplasty and articular purulence with a large soft tissue abscess found in the left knee joint. Left knee synovial biopsy revealed a gouty tophus. The patient received an antibiotic spacer during the operation, was started on a 6-week course of ceftriaxone, and continued allopurinol.
CONCLUSION: Gout is rarely reported in prosthetic knees and there is no prevalence data. There are several case reports but no cohort study on this topic. This patient had an atypical gout flare in the setting of a prosthetic knee with initially relatively low synovial WBCs of 550. The measure of intracellular MSU though, was the key to diagnosis. She had multiple risk factors for gout flares, such as CKD, diuretic use, and lack of allopurinol. Her presentation was initially atypical for PJI, a condition with a prevalence of < 3%. P. acnes, a slow-growing pathogen, is involved in 10% of PJI, mostly delayed and low-grade infection. When she did not improve clinically with steroids, we were forced to revisit our diagnosis. This was confirmed by a subsequent late culture growth. In a retrospective study, gout is found to increase PJI risk (OR 1.62). This case offers insights to differentiate gouty arthritis and PJI within the post-TKA population. Early recognition of these two distinctive conditions is crucial. It also highlights the importance of maintaining an open differential if a patient’s clinical presentation does not respond as expected. Further studies are warranted to shed light on the association between gout and PJI.
ABSTRACT #97
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY/RHEUMATOLOGY
DECREASED ODDS OF MALIGNANCY WITH MYCOPHENOLATE USE IN A SINGLE-CENTER SCLERODERMA COHORT
Jin Feng1, Chrisanna Dobrowolski1,2, Celestine He2, Hannah Verma3, Roshan Vasoya3, Daniel Qian3 , Ezequiel Olumuyide3, Alicia Leong3, Joseph Menand1, Murilo Roberto Bastos Silva1, Vincent Courant2, Sophia Lutgen1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Rheumatology (ACR) Annual Meeting that was held in San Diego, California, United States from November 14-19, 2023.
BACKGROUND/INTRODUCTION: Prior studies have shown an increased risk of malignancy in patients with systemic sclerosis (SSc). The reasons for this increased risk may be multifactorial, including effects of chronic inflammation, genetics, shared environmental risk factors, use of immunosuppressive medications, among others. The aim of this study is to identify and characterize malignancy risk factors in a diverse SSc cohort.
METHODS: A retrospective cohort was assembled of all patients with SSc followed within a large, urban, tertiary care center. Validated ICD codes were used to identify cases. Descriptive statistics were used to study the crosssectional distribution of patient characteristics, including age, sex, race/ethnicity, health insurance status, smoking status, scleroderma subtype, mycophenolate (MMF) use and other immunosuppressant use. Student t-test was performed to compare variations in age. Chi-square test and Fisher exact test were used to examine the difference in other categorical characteristics of patients with and without malignancy. The prevalence of specific types of cancers was calculated. Odds ratios (OR) of cancer diagnosis with respect to patient characteristics were calculated with multivariable logistic regression.
RESULTS: A total of 625 patients met inclusion criteria. The distribution of participant characteristics was calculated and stratified by cancer diagnosis. 93 (14.9%) patients were found to have a history of cancer. Breast cancer (N=32, 5.1%) was the most prevalent cancer in our cohort; distribution of each specific malignancy is outlined in Figure 1. Patients with a malignancy history were older than those without malignancy (median age 69 versus 61years, p< 0.01). Lack of medical insurance was associated with increased odds of malignancy (OR, 2.13; 95%CI, 1.07-4.24; p=0.03). Participants taking MMF were significantly less likely to be diagnosed with malignancy (OR, 0.58; 95%CI, 0.36-0.94; p=0.03), whereas other immunosuppressant use was associated with higher prevalence of malignancy (OR, 2.16; 95%CI, 1.36-3.43; p=0.001). The multivariable logistic regression showed cancer had statistically significant associations with public insurance (p=0.01), lack of insurance (p= 0.01), MMF (p<0.01), and other immunosuppressants (p<0.01), but not with SSc’s time of diagnosis, SSc subtypes, or smoking.
CONCLUSION: While MMF has been associated with increased malignancy risk in prior studies, this analysis showed a reduced odds of malignancy in participants with SSc treated with mycophenolate. The reason for this unexpected finding is unclear and further studies are warranted to determine if a relationship exists beyond correlation. Lack of health insurance, increasing age and non-MMF immunosuppressant use are associated with increased malignancy risk in this urban, single-center multiethnic SSc cohort. The cancer prevalence in our cohort is similar to prior SSc studies, and higher than the general population.

Table 1. Characteristics of patients with systemic sclerosis with and without history of malignancy (N=625)
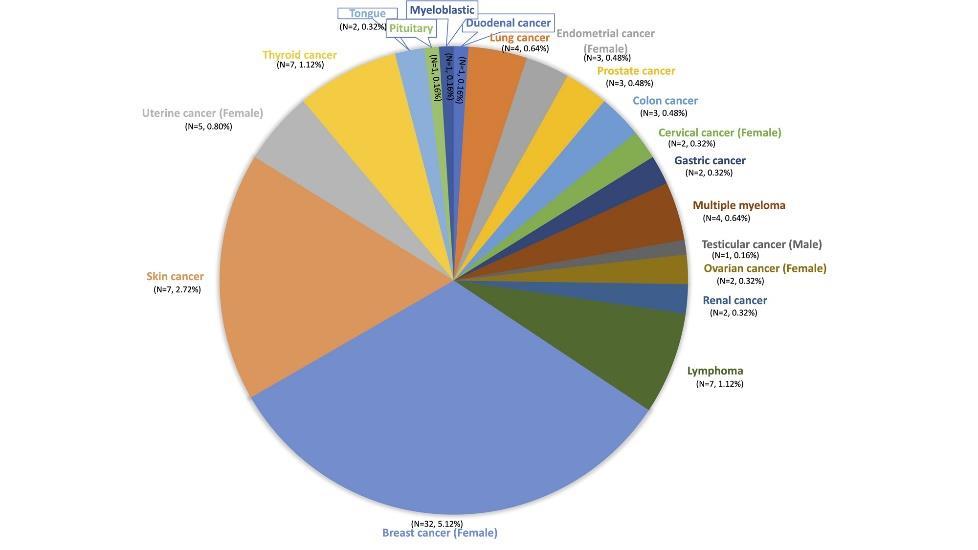
Figure 1. Prevalence of specific malignancies in patients with scleroderma, distributed in a pie chart
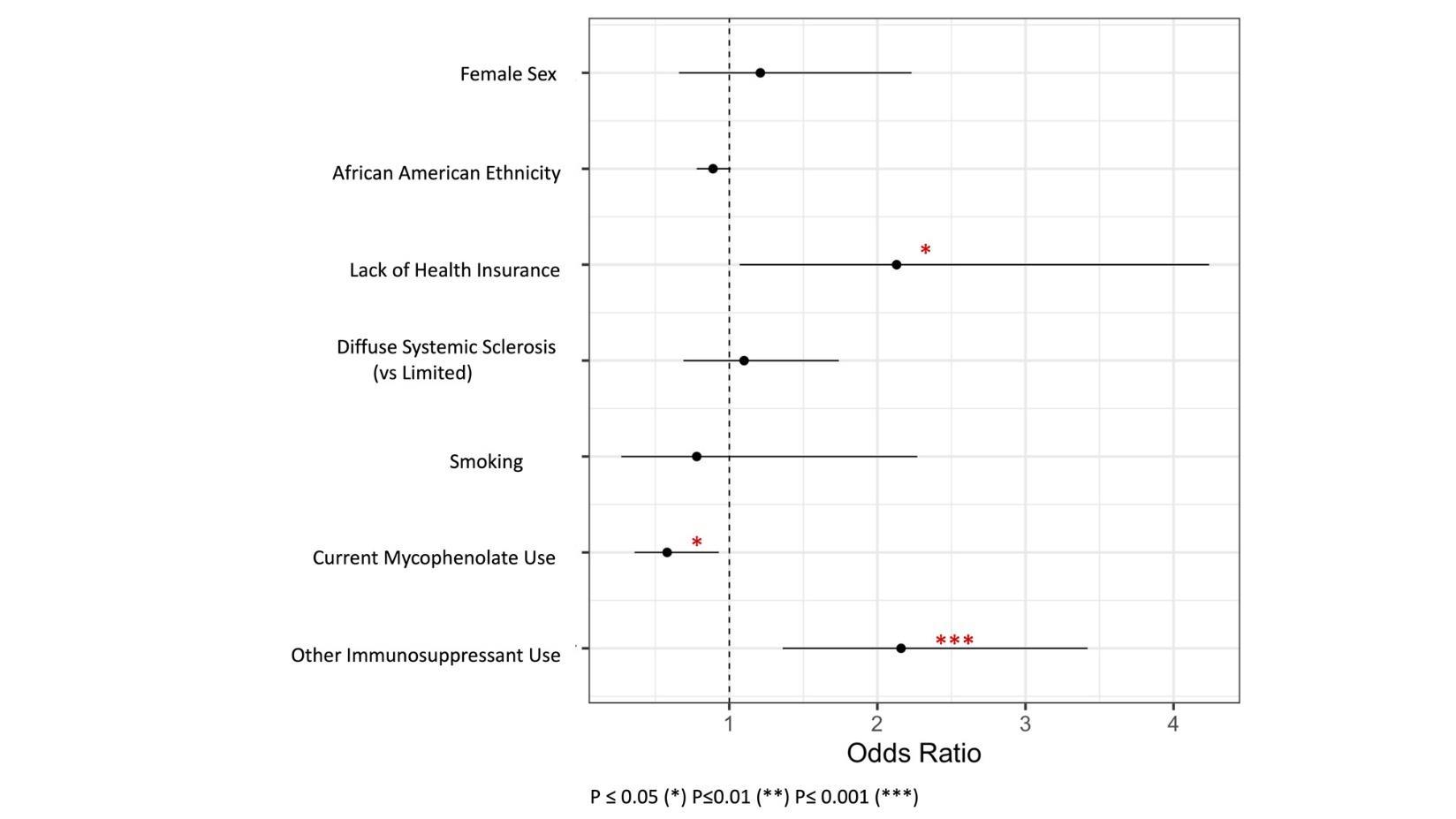
2. Adjusted odds ratios for patient characteristics versus malignancy
ABSTRACT #98
CLINICAL RESEARCH
INFECTIOUS DISEASES/RHEUMATOLOGY
INCREASE SHINGRIX
Jin Feng1 and Kristaq Koci1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Rheumatology (ACR) Annual Meeting that was held in San Diego, California, United States from November 14-19, 2023.
BACKGROUND/INTRODUCTION: The 2022 ACR guidelines for vaccination strongly recommend recombinant VZV vaccination for all patients >18 years old who are taking immunosuppressive medication. Studies have shown that there is a higher risk of shingles in patients on JAK inhibitors. To assess the Shingrix vaccination rate at the rheumatology outpatient practice of an urban academic institution and improve adherence, we initiated a quality improvement project in patients who are on JAK inhibitors.
METHODS: The primary aim of our QI project was to increase the Shingrix vaccination rate by 10%. We also attempted to identify the risk factors for eligible patients not receiving Shingrix despite guideline recommendations. We acquired data quarterly from electronic health records, including patients’ MRN, age, sex, race, Shingrix vaccination status, and last visit dates. Vaccination status was further validated with manual chart review. Data obtained from 4/1/2022 to 6/30/2022 were considered the baseline. We implemented interventions via Plan-Do-Study-Act (PDSA) method: 1) provide posters at clinics to improve awareness, 2) remind eligible patients during the encounter 3) notify patients’ primary rheumatologists quarterly. Data were obtained from 9/1/2022-11/30/2022 and 12/1/2022-2/28/2023 respectively. We used descriptive statistics and analyzed the data via Stata/SE 17.0, stratified by Shingrix vaccination status. We also studied the trend of the Shingrix vaccination rate.
RESULTS: From 4/1/2022 to 2/28/2023, the Shingrix vaccination rate raised from 22.22% (14/63) to 39.19% (29/74) after two cycles of PDSA, meeting our goal of a 10% increase. (Figure 1) After PDSA #1 in 9/2022, the overall vaccination rate slightly declined to 19.67%. After PDSA #2 in 12/2022, it significantly improved. Among all the patients (N=198) seen from 4/1/2022 – 2/28/2023, 55.56% (110) of them were ≥50 years old while 44.44% (88) were <50 years old. 14.14% (28) were male, while 85.86% (170) were female. 41.41% (82) of the patients were Caucasian, 10.61% (21) were African American, and 9.09% (18) of the patients identified as AAPI. Patients ≥50 years old had higher vaccination rate than patients <50 years old. (Figure 1) From 4/1/2022 to 2/28/2023, patients ≥ 50 years old had a significant increase in vaccination rate from 29.73% to 56.41%. Male and female patients had similar vaccination rates, with 41.67% male and 38.71% female vaccinated. Despite the improvement in the 12/2022 TO 2/2023 period, patients who identified as African American had a lower vaccination rate than their Caucasian counterparts. 25% (2/8) African American patients were vaccinated compared to 46.97% (15/32) Caucasian patients. (Figure 2).
CONCLUSION: Our interventions improved the Shingrix vaccination rate. Congress’s new bill eliminating the cost of vaccines covered by Medicare Part D may have also played a role. Besides achieving our goal of a 10% increase, we identified the risk factors for lower vaccination rates: patients < 50 years old and African American patients. As the PDSA cycle continues, targeted interventions will be implemented to address disparities and improve adherence to Shingrix vaccination.
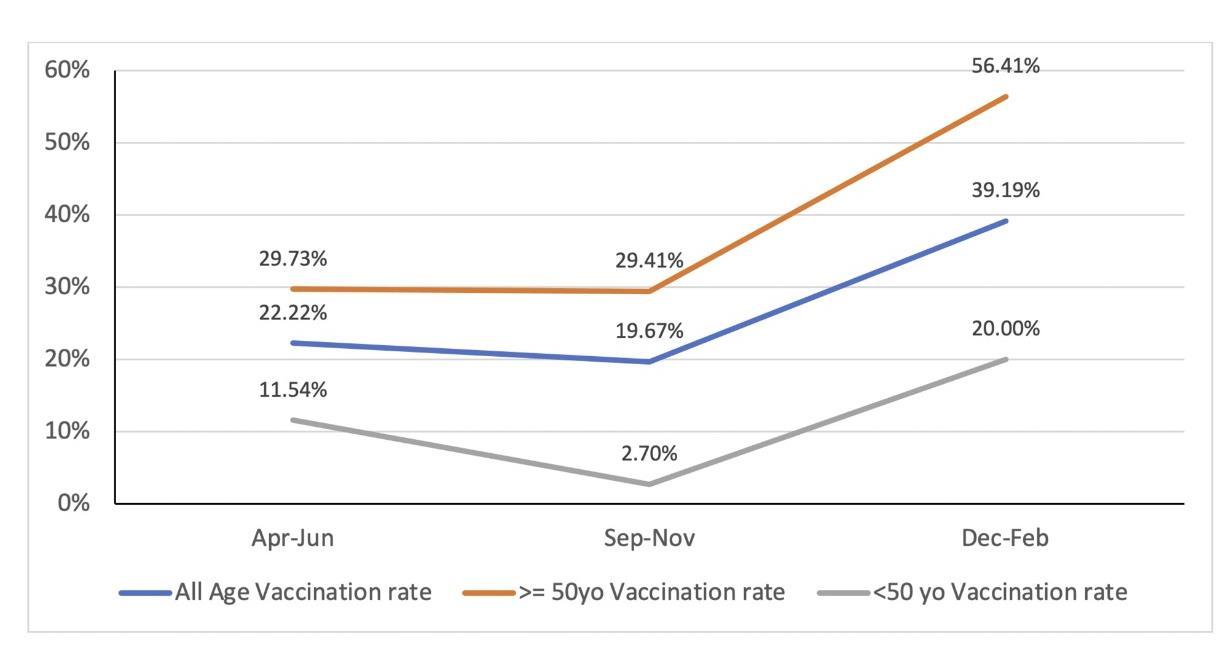
Figure 1. The trend of Shingrix vaccination rate stratified by age

2. Shingrix vaccination rates by race/ethnicity in PDSA #2 (12/2022 – 2/2023)
ABSTRACT #99
CLINICAL RESEARCH
INFECTIOUS DISEASES
PHENOTYPIC CHARACTERIZATION OF NOD2 MUTATIONS IN PATIENTS WITH ANTIBODY DEFICIENCIES
Ashley Sang Eun Lee1 , Jin Feng1, Hsi-En Ho1, Charlotte Cunningham-Rundles1
1Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
BACKGROUND/INTRODUCTION: Mutations in the NOD2 (Nucleotide Binding Oligomerization Domain Containing Protein 2) in antibody-deficient patients.
METHODS: Patients followed in the Mount Sinai Primary Immunodeficiency Clinic were examined by targeted gene sequencing for deleterious mutations. NOD2 mutations, associated with Crohn’s disease and Blau syndrome (p.Arg702Trp, p.Leu1007Profs*2, p.Gly908arg, p.Asn852Ser), were noted in some. We screened these subjects for their clinical phenotypes: bronchiectasis, autoimmunity, granuloma, interstitial lung disease, splenomegaly, and enteropathy.
RESULTS: Of the 325 patients from our Primary Immunodeficiency Clinic, 31 antibody-deficiency patients had one or more of the polymorphisms in the NOD2 gene (9.5%). Patients were 58% female, with a median age of 45 (range 13-68). 65% were white (35% unknown), and 87% were non-Hispanic with 6% identifying as Hispanic, and 6% as “other.” 68% had common variable immunodeficiency (CVID), with other defects including IgG deficiency and hypogammaglobulinemia. Clinical complications included autoimmunity (65%), splenomegaly (48%), granulomatous disease (32%), interstitial lung disease (29%), enteropathy (23%), and/or bronchiectasis (16%). 33% of these patients had other monogenic mutations including NFKB1, TNFRSF13B/TACI, C2/3, DCLRE1C, and RMRP. Within our antibody-deficient cohort with monogenic mutations excluding NOD2, 47% had autoimmunity, 16% enteropathy, and 17.6% granulomas.
CONCLUSION: 9.5% of our antibody-deficient patients had NOD2 mutations with medical complications. Additional analyses are required to determine if there is a phenotype-genotype association, since some of these patients also had other monogenic mutations, which are likely to contribute to their clinical phenotype.
ABSTRACT #100
CLINICAL RESEARCH
ALLERGY/IMMUNOLOGY
SUMMERTIME ASSOCIATIONS BETWEEN MOLD EXPOSURE AND RHINITIS SYMPTOMS AMONG PRESCHOOL CHILDREN ATTENDING HEAD START IN NEW YORK CITY
Jin Feng1, Adnan Divjan2, Luis Acosta2, Andrew Rundle2, Maxine Ashby-Thompson2, Judith Jacobson2 , Matthew Perzanowski2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mailman School of Public Health at Columbia University, New York, NY, United States Presented at the American Academy of Allergy and Immunology (AAAI) Annual Meeting that was held in Washington, D.C., United States from February 23-26, 2024.
BACKGROUND/INTRODUCTION: Previously, we demonstrated associations between reports of domestic mold and rhinitis symptoms among children attending Head Start in NYC. In a recent study, we observed seasonal variability in domestic fungal exposure in NYC homes (Cochran et al. Building and Environment, 2022;226:109711). We hypothesized that the association between domestic mold and rhinitis would vary by season.
METHODS: Children ages 2-5 were recruited from Head Start Centers. Parents were queried about rhinitis symptoms (runny nose in the absence of a cold) and visible mold or mildew at home in the past year. Prevalence ratios (PR) with 95% confidence intervals (CIs) were computed with adjustments for sex, race, maternal education, maternal asthma, and reports of mice, rats, and cockroaches.
RESULTS: Rhinitis symptoms were reported more frequently in fall, winter, and spring (highest, January=20.8%) than in summer (lowest, August = 6.9%) months (n=986). Reports of mold were associated (p<0.05) with rhinitis symptoms in all months except March, April, September, and December. However, the associations between mold and rhinitis symptoms were stronger in the summer months (highest, July PR=2.6; 95%CI, 1.6-4.3; p<0.001) than in other months (lowest, April 1.2; 95%CI, 0.83-1.8; p=0.30).
CONCLUSION: 9.5% of our antibody-deficient patients had NOD2 mutations with medical complications. Additional analyses are required to determine if there is a phenotype-genotype association, since some of these patients also had other monogenic mutations, which are likely to contribute to their clinical phenotype.
ABSTRACT #101
CLINICAL RESEARCH
HEMATOLOGY/ONCOLOGY/RHEUMATOLOGY
TEMPORAL ASSOCIATION BETWEEN BREAST CANCER AND SYSTEMIC SCLEROSIS: A CROSSSECTIONAL ANALYSIS IN AN URBAN INSTITUTION
Jin Feng1, Celestine He2, Hannah Verma3, Roshan Vasoya3, Daniel Qian3, Ezequiel Olumuyide3, Alicia Leong3 , Joseph Menand1, Murilo Roberto Bastos Silva1, Vincent Courant2, Sophia Lutgen1, Chrisanna Dobrowolski2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the European Alliance of Associations for Rheumatology (EULAR) Annual Meeting that will be held in Vienna, Austria from June 12-15, 2024.
BACKGROUND/INTRODUCTION: Prior studies have demonstrated an increased risk of malignancy in patients with Systemic Sclerosis (SSc). Breast cancer was found to be among the most prevalent malignancies in patients with SSc by several studies, while a meta-analysis did not show an increased risk of breast cancer in such population. Our study investigates the temporal relationship between breast cancer and SSc to elucidate the time period in which patients may be at highest risk.
METHODS: We used ICD codes to gather a retrospective cohort of patients with SSc within a large, urban, tertiary center. Manual chart review was conducted to obtain the dates of diagnosis of breast cancer. Descriptive statistics were used to show the distribution of demographic characteristics in patients with and without a history of breast cancer. T-tests, Chi-square tests, and Fisher’s exact tests were used to study the differences in the distribution of patients’ characteristics. Patients’ timelines of breast cancer and SSc diagnosis are presented individually. The intervals between the two diagnoses were calculated, the distribution of which is shown in a bar chart. Multivariable logistic regression analysis was conducted to study the association between breast cancer and patient characteristics. Propensity score matching was used to study the average treatment effect of MMF in breast cancer. Stata, R, and Excel were used for data analysis and visualization.
RESULTS: We identified 32 (5.13%) breast cancer cases in a 625-patient cohort (81.6% female). All breast cancer patients were female. The breast cancer group was older (median age 74 versus 61 years, p<0.01) (Table 1). NonMMF immunosuppressant use was associated with a higher risk of breast cancer (OR, 2.36; 95%CI, 1.01-5.52; p=0.047), in a multivariable logistic regression model. MMF use was associated with reduced odds of breast cancer diagnosis. Through propensity score matching, we observed that MMF use resulted in an average of 10.3% decrease in the odds of breast cancer. Of the 26 patients with complete documentation of both breast cancer and SSc diagnosis dates, their individual timelines are presented in Figure 1. Five (19.2%) patients were diagnosed with both breast cancer and SSc within 12 months. 13 (50%) patients were diagnosed with breast cancer within 3 years of their SSc diagnosis. Seven (26.9%)patients were diagnosed with breastcancer ≤3 years before SSc diagnosiswhile one (3.8%) patient was diagnosed with breast cancer ≤3 years after SSc diagnosis. In addition, seven (26.9%) patients were diagnosed with breast cancer >3 years before SSc diagnosis while six (23.1%) patient was diagnosed with breast cancer >3 years after SSc diagnosis.
CONCLUSION: Our findings suggest a temporal association between onset of breast cancer and SSc, with most patients being diagnosed within three years of SSc diagnosis. Interestingly, more patients were diagnosed with breast cancer before than after SSc diagnosis. Prospective studies with larger cohorts are warranted to further investigate this temporal association.

Table 1. Demographic characteristics of SSc patients with demographic characteristics (N = 32).
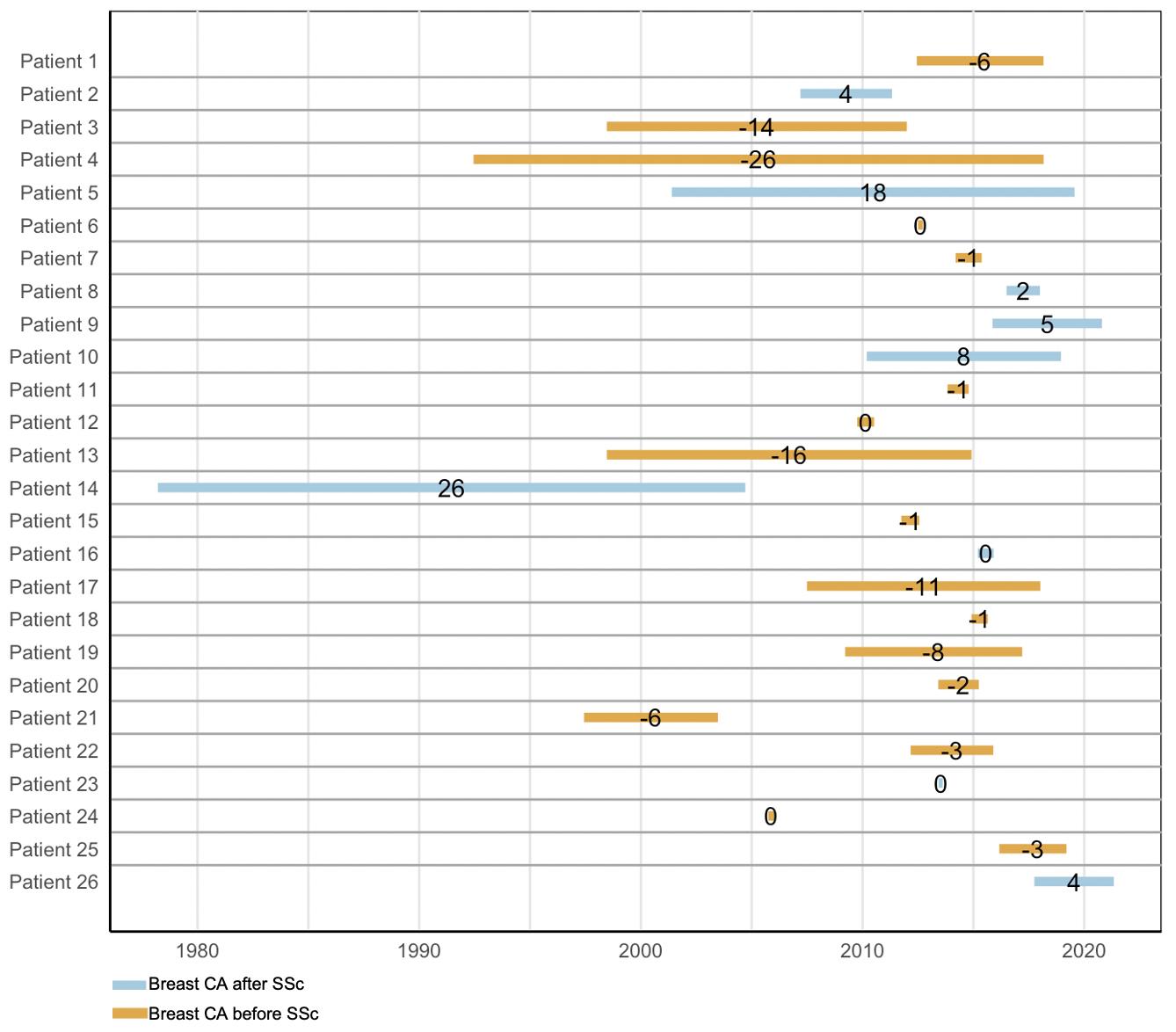
1. The timeline of breast cancer diagnosis and SSc diagnosis in patients with both conditions (N = 26).
ABSTRACT #102
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE HEMATOLOGY/ONCOLOGY
A RARE HEMIBALLISMUS WITH ANTIPHOSPHOLIPID SYNDROME: A CASE REPORT AND LITERATURE REVIEW
Andreas Lau1 , Thomas Fusillo2, Dennis Kulp3, Mariam Rangwala3
1Western University of Health Science, Pomona, CA, United States; 2Mount Sinai Morningside-West Hospitals, New York, NY, United States; 3Community Memorial Hospitals and Healthcare, Ventura, CA, United States
Presented at the American College of Physicians Southern California Scientific Meeting that was held in Los Angeles, California, United States on October 7, 2023.
CASE PRESENTATION: We report a case of an 84-year-old male with history of atrial fibrillation on anticoagulation and prior transient ischemic attacks without residual deficits who presented with an acute onset of right-sided hemichorea-hemiballism of the upper and lower extremity in setting of antiphospholipid syndrome. Symptomatic control of his movements was achieved with haloperidol. Anticoagulation was changed from apixaban to warfarin in the outpatient setting.
CONCLUSION: Antiphospholipid syndrome can present with a variety of hematologic, renal, cardiac, dermatologic, and neurologic symptoms. Diagnosis of APS is governed by the revised Sapporo criteria and requires satisfaction of at least one clinical and one laboratory criteria. Clinical criteria include vascular thrombosis and pregnancy morbidity. Laboratory criteria include detection of one or more of the following: lupus anticoagulant, anticardiolipin antibodies, and anti-beta2 glycoprotein antibodies. The mainstay treatment for APS is anticoagulation with vitamin K antagonists. Several case studies describe APS presenting with neurologic manifestations including chorea.
ABSTRACT #103
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PULMONARY/CRITICAL CARE
SALT, SEIZURES AND SIADH: PITUITARY (MACRO)ADENOMA AND SYMPTOMATIC HYPONATREMIA
Archana Pattupara1,2 , Kristine Lou Gargaritano1, Alyson Meyer1, Mrittika Deb1, Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: Hyponatremia is a common condition encountered in the intensive care unit. Common etiologies described in the elderly include drugs (diuretics, antidepressants) and “tea and toast” syndrome, with many other factors often contributing. Neurological symptoms vary based on the severity and the acuity of the hyponatremia, and can manifest as headaches, altered mental status, lethargy, seizures, and coma. Here, we present a case of severe symptomatic hyponatremia in a patient ultimately diagnosed with a pituitary macroadenoma.
CASE PRESENTATION: A 71-year-old gentleman with a history of hypertension presented to the hospital following a witnessed seizure in a taxicab. On arrival to the emergency department, the patient was hemodynamically stable on room air and conversant, and he endorsed feeling fatigued Further assessment showed the patient to be confused, oriented only to himself, with exam otherwise unremarkable and without focal neurological deficits. Initial laboratory studies were significant for white blood cell count of 16.3K/microL and a serum sodium of 115 mmol/L that worsened to 110 mmol/L after intravenous fluids. A CT head was negative for an acute intracranial process, and an infectious workup was unrevealing. The patient was then admitted to the medical ICU for further management. Urine sodium and potassium were 112 mmol/L and 25 mmol/L respectively, and urine osmolality was 556 mOsm/kg, consistent with syndrome of inappropriate antidiuretic hormone (SIADH). The patient was treated with repeated boluses of 3% hypertonic saline and over the next few days, his sodium level gradually improved to 131. Further workup was significant for low random cortisol of 3.3 mcg/dL, with subsequent cosyntropin stimulation test consistent with central adrenal insufficiency. Thyroid function tests including free T3, free T4, and insulin growth factor-1 were low. MRI brain revealed a pituitary adenoma measuring >1 cm. He was treated with hydrocortisone and thyroid replacement. FSH, LH, and prolactin levels were normal. Neurosurgery and ophthalmology recommended further outpatient evaluation. The patient’s mental status returned to baseline, and the patient was discharged home with close follow-up.
CONCLUSION: COVID-19 Elucidating the true etiology to severe hyponatremia can be challenging. Even though pituitary adenoma is a known cause of hyponatremia, it is rarely encountered in clinical practice. This case report highlights a severe acute presentation without other neurohormonal symptoms and serves as a reminder to this uncommon etiology. This also emphasizes the need for thorough workup and continued comanagement involving specialists including endocrinology, ophthalmology, and neurosurgery to prevent further complications.
ABSTRACT #104
CLINICAL RESEARCH
CARDIOLOGY
CLINICAL OUTCOMES OF COVID-19 IN PATIENTS WITH HEART FAILURE WITH REDUCED EJECTION FRACTION
Kruti D. Gandhi1, Errol Moras1 , Adylin Moras2, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: The rate of infections in patients with cardiac implantable electronic devices (CIED) in the United States ranges from 0.8 to 6.2%. CIED-related infections are associated with right-sided endocarditis, which may cause TV aneurysms or pulmonary embolisms. Embolic strokes are frequently associated with left-sided infective endocarditis. We present a case highlighting a complex diagnostic and management approach of a patient with a cardiac resynchronization therapy-defibrillator (CRT-D) related endocarditis with a complicated hospital course.
METHODS: Data from National Inpatient Sample database from 2020 was used to identify HFrEF hospitalizations with and without a diagnosis of COVID. Independent t-tests were used to compare continuous variables and chi square tests were used to determine associations between categorical variables. Clinical outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: A weighted total of 1,474,835 patients hospitalized with HFrEF were identified of which 68540 patients (4.6%) had a concomitant diagnosis of COVID-19. Patients with COVID-19 were older, more Hispanic (14.3% versus 8.3%, p<0.001) and black population (23.8% versus 20.1%, p<0.001), and had a higher incidence of urgent admissions. HFrEF patients with COVID-19 had higher rates of in-hospital mortality (22.6% versus 5.5%, p<0.001), longer length of stay (10 ± 10 days versus 6 ± 8 days, p<0.001), higher hospitalization costs ($121K versus $96K, p<0.001), and increased incidence of outcomes such as sepsis, thromboembolism, vasopressor requirements, mechanical ventilation, and blood transfusion. During hospitalizations for HFrEF, COVID-19 was also found to be an independent predictor of mortality (aOR 5.0; 95%CI, 4.8-5.3; p<0.001). Further, increasing age (aOR 1.2, p<0.001), atrial arrythmias (aOR 1.1, p<0.001), chronic kidney disease (aOR 1.2, p<0.001), chronic liver disease (aOR 3.7, p<0.001), and bleeding complications (aOR 2.8, p<0.001) were independent predictors of mortality in HFrEF patients with COVID-19.
CONCLUSION: COVID-19 is associated with increased in-hospital mortality, longer hospital stays, higher cost of hospitalization and increased risk of adverse outcomes in patients admitted with HFrEF. During hospitalizations for HFrEF, COVID-19 was also found to be an independent predictor of mortality. Increasing age, atrial arrythmias, chronic kidney disease, chronic liver disease, and bleeding complications were independent predictors of mortality in HFrEF patients with COVID-19.
ABSTRACT #105
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
DEVICE-RELATED ENDOCARDITIS IN CARDIAC RESYNCHRONIZATION THERAPY RECIPIENT COMPLICATED BY PULMONARY EMBOLI, CEREBRAL INFARCT, AND CRITICAL HYPOXIA
Kruti D. Gandhi1, Errol Moras1 , Sidra Salman1, Kiran Mahmood1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: The rate of infections in patients with cardiac implantable electronic devices (CIED) in the United States ranges from 0.8 to 6.2%. CIED-related infections are associated with right-sided endocarditis, which may cause TV aneurysms or pulmonary embolisms. Embolic strokes are frequently associated with left-sided infective endocarditis. We present a case highlighting a complex diagnostic and management approach of a patient with a cardiac resynchronization therapy-defibrillator (CRT-D) related endocarditis with a complicated hospital course.
CASE PRESENTATION: A 70-year-old-male with non-ischemic cardiomyopathy s/p CRT-D (2018) presented with 5 days of fever, chills, and dysuria. On further evaluation, he was found to have a new onset atrial flutter (AF) and elevated d-dimer. Computer Tomography (CT) chest was notable for multiple small pulmonary emboli without evidence of right heart strain. Transthoracic echocardiography (TTE) initially showed mobile echodensities on the right atrial and ventricular leads. Blood culture resulted positive for Group B Streptococcus agalactiae. The patient was started on intravenous antibiotics and anticoagulation. However, his hypoxia worsened rapidly despite non-invasive ventilation and the patient was emergently intubated. A repeat CT chest was notable for persistent showering of septic pulmonary emboli. A transesophageal echocardiogram (TEE) showed a 1cm patent foramen ovale (PFO) with right to left predominant shunt, severe tricuspid regurgitation (TR) and tricuspid valve (TV) endocarditis, elevated pulmonary pressures and multiple vegetations on the pacemaker leads. A CT head showed evidence of a large subacute middle cerebral artery infarct with a small region of hemorrhagic conversion. Given he was pacemaker dependent, extraction alone of the CIED was high risk. Hence, an emergent extraction of the CRT-D was undertaken and a transvenous pacemaker was simultaneously implanted. His course was further complicated by worsening hypoxia despite maximum ventilator settings. The sudden increase in pulmonary and right heart pressures secondary to persistent showering of septic pulmonary emboli was contributing to predominant right to left shunting through PFO, leading to critical hypoxia. The strategy employed here was to allow permissive systemic hypertension through increased pressor support and nitric oxide for vasodilation, thus reducing right to left shunting and improving hypoxia, which was successful. The patient was subsequently found to have hemorrhagic conversion of a large embolic stroke. The patient was not a candidate for thrombolytic therapy or mechanical thrombectomy due to the unknown duration of large artery occlusion. PFO closure, a definite approach for worsening hypoxia was considered, but was deferred in the setting of a large subacute infarct, torrential TR and extensive tricuspid valve vegetations due to high risk of embolization and worsening neurological outcomes. He was eventually transitioned to comfort care.
CONCLUSION: Cardiac implantable electronic devices endocarditis remains a therapeutic challenge despite early diagnosis and requires a multidisciplinary approach. Embolic events are a major cause of morbidity and mortality in patients with cardiac implantable electronic devices endocarditis. This case highlights permissive systemic hypertension as a management strategy for refractory hypoxemia in ventilated patients with significant right to left intracardiac shunting. Technological advances with the leadless pacemaker defibrillator system could potentially benefit a much larger patient population with a decrease in the incidence of lead-related complications.
ABSTRACT #106
CLINICAL RESEARCH
CARDIOLOGY/PULMONARY/CRITICAL CARE
EVALUATING THE EFFECTIVENESS OF VIRTUAL DIDACTIC SESSIONS VERSUS SMALL GROUP SIMULATION SESSIONS FOR RIGHT VENTRICULAR FUNCTION ASSESSMENT: A POINT-OF-CARE ULTRASOUND CURRICULUM
Errol Moras1 , Kruti D. Gandhi1 , Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Point-of-Care Ultrasound (POCUS) is an invaluable tool for rapidly assessing patients in a variety of bedside clinical situations. The aim of the study is to determine whether a virtually delivered didactic POCUS session can be as effective as a small-group in-person simulation centerbased session for improving learner competency in assessing and mastering right ventricular (RV) function.
METHODS: The virtual didactic sessions were 2 hour-long zoom sessions for interns and residents and included pretest and posttest questionnaires. The in-person simulation sessions occurred twice weekly over eight weeks consisting of pretest and posttest surveys, a didactic lecture, case-based simulation scenario, and a debrief discussion. The survey questions consisted of cardiac US clips evaluated by 3 POCUS experts. Effect size as the percent of correct responses was calculated. Data was analyzed using SPSS with a level of statistical significance as p≤0.05.
RESULTS: For the small group simulation sessions, 40 interns and 45 residents were included. 44.4% of residents had attended an ultrasound elective compared to 10% of interns. 40% of interns and 68.9% of residents correctly identified the RV pre-lecture, improving to 95% and 95.6% respectively, afterward. 57.5% of interns and 91.1% of residents correctly identified the etiology of shock pre-lecture, improving to 85% and 97.8% respectively afterward. 62.5% of interns and 75.6% of residents correctly described normal RV characteristics pre-lecture, improving to 77.5% and 82.2% respectively, afterward. 17.5% of interns and 48.9% of residents answered all 3 questions correctly in the pretest, improving to 62.5% and 78% respectively, afterward. These trends were found to be statistically significant (p<0.05). The majority of interns pre-session reported no RV assessment knowledge (88.9%), and by the end of the session, 77.7% reported good knowledge. The majority of residents reported some familiarity with RV assessment pre-session (65.9%), and by the end of the session, 78% reported good knowledge. For the virtual sessions, 11 interns and 30 residents were included. 54.5% of interns and 60% of residents correctly sized the RV pre-lecture, improving to 90.9% and 93.3% respectively, afterward. 18.2% of interns and 63.3% of residents correctly described RV function pre-lecture, improving to 63.6% and 80% respectively afterward. 36.4% of interns and 40% of residents accurately described McConnell’s sign pre-lecture, improving to 90.9% and 90% respectively, afterward. 9.1% of interns and 25% of residents answered all three questions correctly pre-lecture, improving to 63.6% and 71.9% respectively afterward. These trends were not statistically significant.
CONCLUSION: This study showed similar trends for both educational strategies, with impressive and comparable results in the assessment of RV function among interns and residents in both styles of training sessions. This highlights the potential for virtual didactic sessions to at least partially replace and obviate the need for small-group in-person sessions for basic POCUS training and comprehension. Future studies are needed to see the continued effectiveness of these methods longitudinally.
ABSTRACT #107
CLINICAL RESEARCH
CARDIOLOGY
PROGNOSTIC COMPARISON BETWEEN COMPUTER MODELLING-DERIVED VERSUS CONVENTIONAL H2FPEF SCORES
Swiri Konje1, Alaa M. Omar1, Alba Munoz2, Ga Hee Kim1, Joseph Elias1, Arun Mahtani3 , Kruti Gandhi1, Errol Moras1 , Christopher Perez Lizardo1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Houston Methodist, Houston, TX, United States; 3Richmond University Medical Center, Staten Island, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: H2FPEF score of 0-1 and ≥6 indicate low and high risks of HFpEF, while scores of 2-5 may require additional testing. We compared the prognostic abilities of unsupervised cluster modeling (USCM) and the conventional H2FPEF score.
METHODS: Respectively, 532 patients with suspected heart failure (HF) symptoms were included (69±6 years, 57% females, EF: 61±5%, all>50%). H2FPEF score was calculated as recommended: BMI (>30: 2 points), atrial fibrillation (3 points), and 1 point each for age>60 years, ≥2 hypertension drugs, E/e' ratio >9, and pulmonary systolic pressure >35 mmHg. Using these variables, a 2-step USCM was done and compared to the H2FPEF score for death and cardiac hospitalization
RESULTS: The mean H2FPEF score was 3.2±1.5. During a median follow-up of 3.8 years, 13 patients died, 66 hospitalized (35 HF and 51 non-HF causes), and 76 had the composite outcome. H2FPEF scores of 0-1 and ≥6 had the lowest and highest frequencies of individual and combined outcomes, respectively, while scores of 2-5 was intermediate (Figure 1A). Compared to scores of 0-1, scores of 2-5 (HR, 11; 95%CI, 1.5-78) and ≥6 (HR, 29; 95%CI, 4-219) had a higher risk of outcomes. USCM (Figure 1B) identified three clusters with varying risks: (low: 145 patients, intermediate: 333 patients, and high: 54 patients) (Figure 1C). The mean H2FPEF scores differed significantly between clusters (1±0, 3.3±1.1, 6.6±1, p<0.001). Compared to the low-risk cluster, the intermediate-risk (HR, 3.4; 95%CI, 1.5-8), and high-risk clusters (HR, 7.3; 95%CI, 3-18) had a higher risk of outcomes. Clusters significantly reclassified H2FPEF scores (Figure 1D), particularly those with scores of 2-5 (23% reclassified as low risk, 7% as high risk). Among the reclassified patients with H2FPEF scores of 2-5, there was significant discrimination in outcomes (p=0.02, Figure 1A)
CONCLUSION: Machine learning techniques, can enhance the prognostic accuracy of the H2PEF score, particularly for intermediate scores.
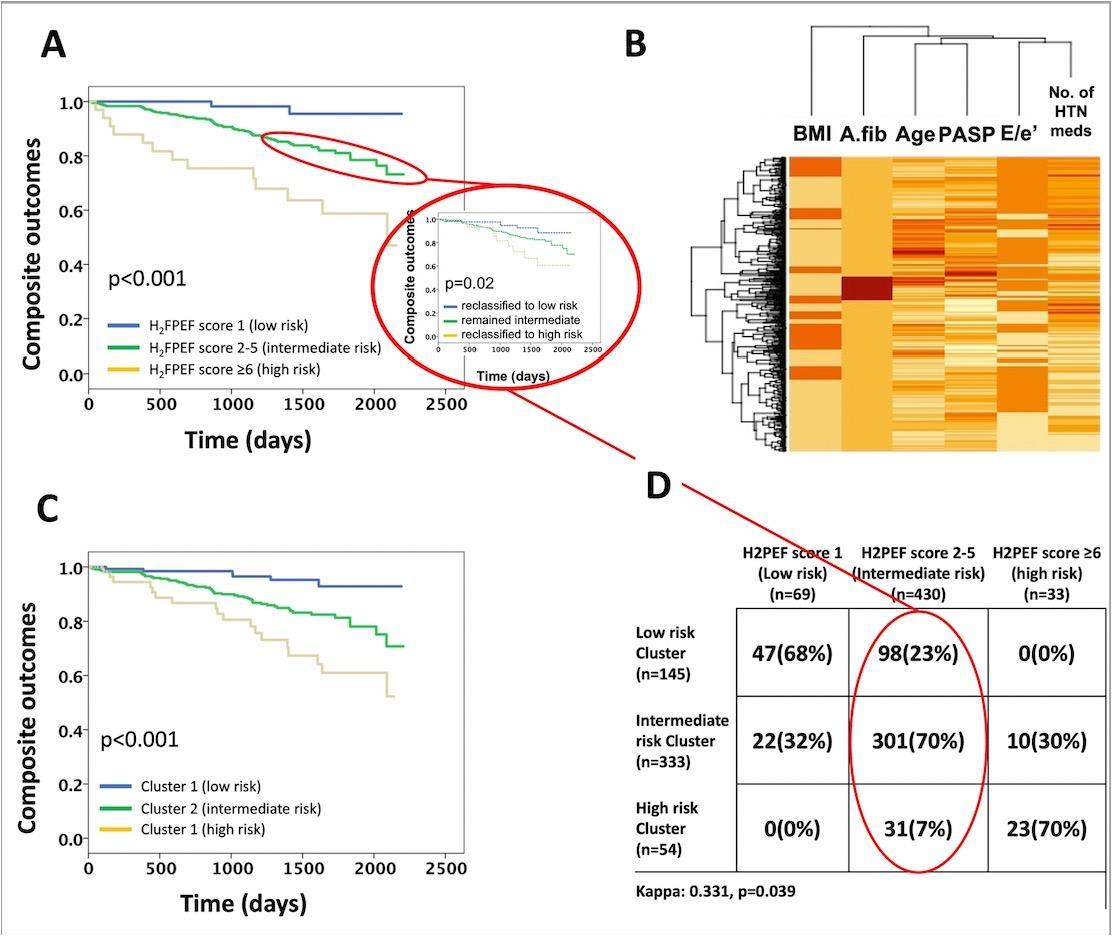
ABSTRACT #108
CLINICAL RESEARCH
CARDIOLOGY
PROGNOSTIC VALUE OF EXERCISE TOLERANCE AND EXERCISE-ASSOCIATED DIASTOLIC DYSFUNCITON IN ELDERLY PATIENTS REFERRED FOR EXERCISE STRESS ECHOCARDIOGRAPY
Joseph Elias1, Swiri Konje1, Alba Munoz2, Ga Hee Kim1 , Kruti Gandhi1, Errol Moras1, Christopher Perez Lizardo1, Arpanjeet Kaur1, Alaa M. Omar1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Houston Methodist Hospital, Houston, TX, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: We studied the prognostic value of exercise tolerance, measured in metabolic equivalents of tasks (METs), and exercise-associated diastolic dysfunction (Ex-DD) in elderly patients referred for exercise stress echocardiography (ExE).
METHODS: Retrospectively, 583 patients (70 ± 6 years, 57% women, EF: 61±5%) who underwent ExE using the Bruce protocol and were ≥60 years of age were included and followed for death or cardiac hospitalization. Ex-DD was defined as the presence of abnormal resting tissue Doppler mitral annular velocity (e') and post-exercise E/e' ratio.
RESULTS: During a median follow-up period of 3.7 years, 13 patients died, 70 were hospitalized, and 77 had combined outcome. 151 (26%) patients had Ex-DD and had more combined outcome compared to no Ex-DD [29 (19%) versus 48 (11%), p=0.01]. The average workload during ExE was 8.3±2.8 METs. Receiver operating characteristic curve identified that METs <8.5 best predicts the combined outcome. As such, patients were classified into 260 with METs ≥8.5 and 323 with METs <8.5. Patients with METs <8.5 were older, had worse risk profiles, poorer resting and post-exercise diastolic variables, more Ex-DD (32% versus 19%, p<0.001), and more outcomes [55 (17%) versus 22 (9%), p=0.002) compared to METs ≥ 8.5. Both Ex-DD (HR: 1.9, 95% CI: 1.2-2.9) and METs <8.5 (HR, 1.9; 95%CI, 1.1-3.1) independently predicted the combined outcome. The presence of both METs <8.5 and Ex-DD conferred the highest risk (HR, 2.9; 95%CI, 1.5-5.6) and remained significant after adjustment and propensity score matching, while the presence of either alone carried an intermediate risk (HR, 1.9; 95%CI, 1.1-3.5), which became non-significant after adjustment and matching.
CONCLUSION: Poor exercise capacity is associated with an adverse prognosis, irrespective of resting or Ex-DD. METs<8.5 had particularly poor prognosis when combined with Ex-DD, while either alone did not predict outcomes.
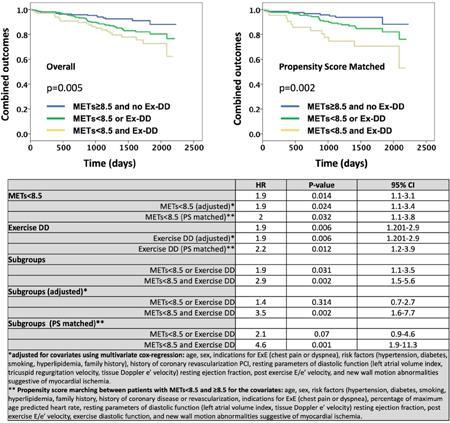
ABSTRACT #109
CLINICAL RESEARCH
CARDIOLOGY
PROGNOSTIC VALUE OF H2FPEF SCORE AMONG SYMPTOMATIC PATIENTS REFERRED FOR EXERCISE ECHOCARDIOGRAPHY
Ga Hee Kim1, Swiri Konje1, Alba Munoz2 , Kruti Gandhi1, Errol Moras1, Christopher Perez Lizardo1, Joseph Elias1, Arpanjeet Kaur1, Alaa M. Omar1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: The H2FPEF score is a recommended tool for estimating the likelihood of heart failure with preserved ejection fraction (HFpEF) in cases of unexplained dyspnea. Limited data is available regarding its prognostic ability. This retrospective study aimed to assess the prognostic value of the H2FPEF score for adverse cardiovascular outcomes.
METHODS: 532 patients [age 69±6 years, 57% female, and ejection fraction 61±5% (all >50%)] with suspected symptoms of heart failure (HF) referred for exercise echocardiography were included. H2FPEF score was calculated based on: BMI >30 kg/m2 (2 points), atrial fibrillation (3 points), age >60 years (1 point), use of ≥2 hypertension drugs (1 point), E/e’ ratio >9 (1 point), and pulmonary systolic pressure >35 mmHg (1 point). Comparisons were made for death and HF hospitalization.
RESULTS: During a median follow-up of 3.8 years, 13 patients died, 35 had HF hospitalizations, and 48 experienced the composite outcome. The score distribution was as follows: 0-1 in 69 (13%) patients, 2-5 in 430 (81%) patients, and ≥6 in 33 (6%) patients. The H2FPEF score averaged 3.2±1.5 and showed a progressive increase in the risk of adverse outcomes. A score of 0-1 was associated with the lowest risk, ≥6 with the highest risk, and 2-5 with an intermediate risk (Figure 1A-C). Compared to a score of 0-1, increased risk for combined outcomes occurred with a score of 2-5 (HR, 3.4; 95%CI, 1.5-8) and ≥6 (HR, 9.6; 95%CI, 3.6-26). Similar risk patterns were observed for death and HF hospitalization. Importantly, during exercise echocardiography, new wall motion abnormalities occurred in 105 (20%) patients and did not differ significantly among the different H2FPEF score groups (p=0.403). A H2FPEF score >1 was associated with an increased risk regardless of the presence or absence of myocardial ischemia (Figure 1D).
CONCLUSION: H2FPEF score is a useful prognostic tool in suspected HFpEF, regardless of echocardiographic presence or absence of ischemia.
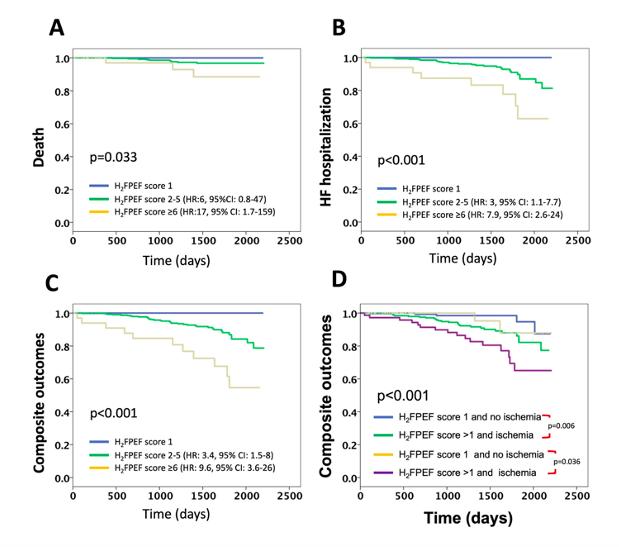
Figure 1A-D. Associations of H2FPEF score with death (A), HF hospitalization (B), and composite outcomes (C). Association of composite outcomes and H2FPEF score and with or without ischemia (C).
ABSTRACT #110
CLINICAL RESEARCH
CARDIOLOGY
TEMPORAL TRENDS AND OUTCOMES OF HEART FAILURE PATIENTS BETWEEN LIGHT-CHAIN CARDIAC AMYLOIDOSIS AND TRANSTHYRETIN CARDIAC AMYLOIDOSIS
Kruti D. Gandhi1, Errol Moras1, Ashish Correa1, Kiran Mahmood1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the European Society of Cardiology (ESC) Congress Annual Meeting that was held in Amsterdam, Netherlands from August 23-28, 2023.
BACKGROUND/INTRODUCTION: Systemic amyloidosis comprises a family of diseases caused by deposition of misfolded fibrillar proteins in the extracellular space. Cardiac involvement is the leading cause of morbidity and mortality in systemic amyloidosis and a major determinant of survival, regardless of the underlying pathogenesis of amyloid production. Data regarding the clinical outcomes in immunoglobulin light-chain (AL) va amyloid transthyretin (ATTR) cardiac amyloidosis (CA) is scarce. We aimed to investigate the trends, baseline clinical characteristics, and clinical outcomes of AL CA vs ATTR CA in heart failure (HF) patients.
METHODS: Data from United States National Inpatient Sample database from 2017-2020 was used to identify hospitalizations for CA with concurrent cardiomyopathy in HF patients and were further subclassified into AL versus ATTR CA. Outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: During 2017-2020, there were 12430 hospitalizations of CA of which 96.3% were ATTR CA and 3.7% were AL CA. Patients with ATTR-CA when compared to AL-CA were older, predominantly male, more blacks, and had a higher prevalence of co-morbidities including atrial arrythmias, sick sinus syndrome, and aortic stenosis. Patients with AL CA had significantly increased in-hospital mortality, length of stay, total charges, acute heart failure exacerbations, and cardiopulmonary resuscitation. After adjustment for baseline characteristics, AL CA patients had significantly increased odds of in-hospital mortality and HF hospitalizations when compared to ATTR CA cohort. There is an increasing trend in hospitalizations in AL CA from 2017-2019.
CONCLUSION: AL cardiac amyloidosis had significantly higher odds of in-hospital mortality and HF hospitalizations in comparison to ATTR cardiac amyloidosis cohort. AL CA had lower incidence of stroke, thromboembolism and major bleeding with similar need for cardiac device implantation.
ABSTRACT #111
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
TRENDS AND OUTCOMES OF ENDOBRONCHIAL VALVE IMPLANTATION IN PATIENTS WITH PERSISTENT AIR LEAK
Kruti D. Gandhi1, Errol Moras1 , Adlyn Moras2, Sidra Salman1 , Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Endobronchial valves (EBV) have been considered an innovation in the management of persistent air leak (PAL) as they offer a minimally invasive alternative to the traditional approach of pleurodesis and surgical intervention. There has been a paucity of data on the trends of its use and associated complications. We aim to describe the trend of utilization of EBV in PAL and evaluate the outcomes over a 5year period.
METHODS: We reviewed the National Inpatient Sample (NIS) database from 2016-2020 to identify patients who underwent EBV implantation exclusively for PAL, using ICD-10 procedure codes. We analyzed patient characteristics, pre-procedural co-morbidities, and outcomes such as in-hospital mortality, hemoptysis, pneumonia and sepsis. Outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: We identified a total of 5,570 EBVs (weighted sample) implanted for PAL from 2016-2020. The mean age of patients who underwent EBV implantation for PAL was 64 ± 12 years and 62.9% were male. 64.6% of the patients had chronic obstructive pulmonary disease, 54.1% had hypertension, 12.1% had congestive heart failure, 7.6% had chronic kidney disease and 9% had diabetes mellitus. 31.4% had acute hypoxic respiratory failure (AHRF) and 9.5% had AHRF requiring mechanical intubation. Overall, in-hospital mortality after EBV implantation for PAL was 6%. 12% of the patients had pneumonia, 5% of patients developed hemoptysis and 4.2% progressed to sepsis while in the hospital. The mean length of stay (LOS) in patients who received EBV for PAL was 13 ± 15 days. The absolute numbers of EBV’s implanted in patients with PAL increased over time from 495 in 2016 to 2220 in 2020.
CONCLUSION: We found that there has been an increase in the number of endobronchial valve implantations for persistent air leak. The associated in-hospital mortality rate after EBV implantation for PAL was 6% and complications included pneumonia (12%), hemoptysis (5%) and sepsis (4.2%). Further studies are needed to evaluate the safety and efficacy of the procedure and the factors associated with the complications.
ABSTRACT #112
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
DIFFICULT CONVERSATIONS AND EFFECTIVE COMMUNICATION TRAINING FOR INTERNAL MEDICINE RESIDENTS UTILIZING HIGH-FIDELITY SIMULATION
Ariela Hazan1, Jeeyune Bahk1 , Ariel Gordon1, Neha Debnath1 , Priscilla V. Loanzon1 , Harrindra Seepersaud1 , Donna Gormley1 , Adam Rothman1,2, James Salonia1, Susannah Kurtz1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Given the lack of formal training surrounding difficult conversations, a simulation-based educational curriculum was designed to address this educational gap. The goal was to improve effective communication skills among Internal Medicine (IM) residents using high fidelity simulation (SIM).
METHODS: A pre-session informative graphics of the SPIKES protocol and NURSE statements and a video of a simulated doctor-patient conversation was provided to the learners prior to the SIM session. The SIM session consisted of a didactic component on the SPIKES protocol and NURSE statements as well as a high-fidelity simulation component in which the learners engaged in difficult conversation training surrounding end of life discussions. Each learner was assigned a role within the SPIKES protocol which they handled during the SIM session. A debrief and feedback session was held after the SIM, with the learners, SIM faculty and Chaplain. Learners completed a pre-session and a post-session survey, evaluating a change in subjective comfort and objective knowledge on the SPIKES protocol and NURSE statements.
RESULTS: 115 and 104 internal medicine residents participated in a pre-session and post-session survey, respectively. Most reported never receiving formal training in difficult conversations (n=69, 60%). The majority reported less than ten difficult conversations with patients (n=83, 72.2%). Only 18.3% (n=21) felt that they had adequate training in delivering bad news to patients and most requested additional training in the topic (n=76, 66.7%). Half of the learners felt that the biggest hurdle in these conversations is when patient/family members exhibit difficulty understanding limitations/complications of life-sustaining therapies and the prognosis (n=57, 49.6%). Only 40.9% (n=47) reported feeling comfortable communicating the prognosis to patients pre-session, which improved to 73.8% (n=76) post-session. Similarly, only 34.8% (n=40) felt comfortable discussing death with a terminally ill patient, which improved to 66.7% (n=68) post-session. The subjective comfort surrounding code status discussion was reported by 67.0% (n=77) of learners, which improved to 85.6% (n=89). Overall, 88.3% (n=91) learners reported feeling comfortable holding a goals of care conversation after the SIM session. Evaluation of resident knowledge on SPIKES and NURSE statements revealed that 97.4% (n=111) and 93.9% (n=108) knew the components of each, which improved to close to 100% post-session.
CONCLUSION: Pre-session surveys demonstrated learners’ discomfort with difficult conversations mostly surrounding the prognosis and death. Post-session surveys held after a didactic and high-fidelity SIM session demonstrated significant improvement in comfort and knowledge.
ABSTRACT #113
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PALLIATIVE CARE
USE OF KETAMINE AND AN INTERDISCIPLINARY TEAM APPROACH TO RAPIDLY TAPER A PATIENT’S ULTRA-HIGH OPIOID REGIMEN
Ariel Gordon1, Evan L. Zazula2 , Joseph D Elder2, Estelle Jungah Hong2, Jordan Nickel-Dubin2 , Yu Shindo2, Ayla Pelleg2, Laura Belland2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Assembly of Hospice and Palliative Care that was held in Phoenix, Arizona, United States from March 20-23, 2024.
BACKGROUND/INTRODUCTION: Subanesthetic intravenous ketamine in palliative care patients can control pain that is poorly responsive to escalating doses of opioids, especially when ultra-high opioid (>1000 oral morphine equivalents (OME) daily) regimens are required. Analgesic titration of intravenous ketamine is established, but it is less clear how to concurrently down-titrate ultra-high opioid doses. Here, intravenous ketamine was effective in controlling a patient’s intractable pain while we rapidly deescalated her ultra-high opioid requirements. Additionally, we highlight the special role the palliative care interdisciplinary team (IDT) plays in supporting patients on intravenous ketamine who experience mild side effects.
CASE PRESENTATION: A 39-year-old woman with hereditary thrombophilia complicated by recurrent venous thrombosis with chronic left lower leg pain on methadone presented with acute right leg pain due to a new deep vein thrombosis. Ineligible for thrombectomy or stenting, she was started on a hydromorphone patient-controlled analgesia (PCA). Her pain was intractable requiring upwards of 8,000 OME including methadone up-titration. Opioid-induced hyperalgesia was suspected, so the continuous dose of hydromorphone was rotated to morphine, however her pain remained uncontrolled on 5,000 OME. While administering a continuous infusion of intravenous ketamine over 36hrs, we tapered her opioid regimen by 25-30% every 4 to 8 hours with an 80% reduction in total OME. She reported good pain control and showed no signs of withdrawal. Ketamine-induced anxiety and mild dissociation were mitigated by IDT members at bedside including chaplaincy, expressive arts therapy, and massage therapy who utilized non-pharmacological techniques to create a supportive environment and strengthen her therapeutic alliance with the entire team.
CONCLUSION: This case illustrates that intravenous ketamine is especially useful for intractable pain and high opioid requirements allowing for quick de-escalation of total opioid needs. Side effects from ketamine can be ameliorated by the support and expertise of a comprehensive interdisciplinary team.
ABSTRACT #114
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
RESIDENT COMFORT IN ADVANCE CARE PLANNING AND HEALTHCARE PROXY DISCUSSIONS IN CHRONIC OBSTRUCTIVE PULMONARY DISEASE AND HEART FAILURE PATIENTS
Soumya Gupta1, Christopher Matthews1, Kristen Carter1, Salvador Caceros Diaz1, Emily Seltzer1, Rebecca Shafer1, Deborah Edelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
BACKGROUND/INTRODUCTION: In patients with chronic obstructive pulmonary disease (COPD) and heart failure, acute exacerbations often require invasive interventions, yet outpatient discussions on advance care planning (ACP) are scarce, leading to poor end-of-life communication. Our paper aims to assess resident familiarity and comfort in ACP and healthcare proxy (HCP) discussions in this group of patients.
METHODS: A needs assessment was conducted among Internal medicine residents at Ryan Health Center to evaluate their familiarity with ACP documentation and their comfort levels in completing HCP forms. Descriptive statistics were utilized to analyze the survey responses, including percentages to quantify resident familiarity, engagement, and comfort levels in ACP documentation and HCP discussions.
RESULTS: A total of 28 internal medicine residents participated in the needs-assessment questionnaire. Among them, 46.4% were in PGY-1, 35.7% were PGY-2, and 17.9% were PGY-3. The analysis revealed that a significant majority, 82.1%, had never documented ACP or completed a HCP form with patients at Ryan Health center. Only a small fraction, 7.1%, had engaged in such documentation. Among those who had documented ACP, only 20% had done so for patients with CHF and COPD, while the remaining 80% had documented it for other causes excluding these two conditions. Furthermore, a considerable portion of the residents (39.3%) expressed discomfortin documentingACPor completingHCPforms, while 21.4% reported beinguncomfortable. These results underscore the imperative for the implementation of our quality improvement initiative within this vulnerable patient population. The findings highlight the necessity for targeted educational interventions and emphasize specific areas requiring focused attention in our curriculum.
CONCLUSION: Our study highlights a significant gap in ACP documentation and HCP discussions among internal medicine residents, particularly concerning patients with COPD and heart failure. The findings underscore the urgent need for targeted educational interventions and improved training in end-of-life communication skills. Implementing a quality improvement initiative tailored to this patient population is crucial, focusing on enhancing resident education and resources for effective ACP documentation. By addressing these challenges, we can ensure that patients receive comprehensive, patient-centered care aligned with their values and preferences.


ABSTRACT #115
MEDICAL EDUCATION
CARDIOLOGY
Soumya Gupta1, Priya Shah1, Kristen Carter1, Ashish Correa1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: The aim of teaching residents about cardiac devices is to equip them with knowledge for evidence-based care, thereby enhancing patient outcomes and safety. We are creating a focused curriculum covering pacemakers, cardiac monitoring devices, and mechanical circulatory support devices. Using infographics, we’ll break down key aspects to efficiently convey crucial information and empower residents in clinical practice.
METHODS: Following the Kern method of curriculum development, we performed a needs assessment of Internal Medicine residents via an electronic survey to assess current knowledge of cardiac devices and identify the areas of gaps in knowledge. The needs assessment survey identified knowledge gaps, paving the way for a targeted intervention. Subsequently, a didactic session will be conducted to familiarize residents with the key concepts. Within this session, residents will be introduced to three infographics, each dedicated to a key topicPacemakers, Cardiac Event Monitors, and Mechanical Circulatory Support Devices. To reinforce understanding, a post-session questionnaire will be administered. Additionally, the infographics will be distributed for easy review, promoting sustained comprehension. Supplementary learning resources, including videos, podcasts, and articles, will be accessible on the Chiefs website, ensuring residents have comprehensive materials at their disposal for continuous education.
RESULTS: Among the 27 internal medicine residents who participated in the needs-assessment questionnaire, results revealed varying levels of knowledge. Notably, only 33.3% demonstrated understanding of lead placement in different types of pacemakers, while 59.3% showed proficiency in identifying a defibrillator on a chest x- ray. The lowest knowledge was observed in criteria for CRT-D implantation in heart failure patients, with a mere 18.5% accuracy. In terms of cardiac event monitoring, 44.4% correctly identified the appropriate device. Understanding the mechanism of action of intra-aortic balloon pumps was demonstrated by 61.5%, yet only 29.6% could identify contraindications. On a positive note, a majority (81.5%) exhibited knowledge of the mechanism of action of Impella®. These findings underscore the need for targeted education and emphasize areas requiring focused attention in our curriculum.
CONCLUSION: While we do feel this needs assessment identified a knowledge gap in cardiac device education, it did have some limitations. The response rate was lower than expected, which could be due to the fact that the survey contained multiple complex questions and the residents were experiencing survey fatigue. Additionally, the results may not be representative of the entire residency program as residents who are interested in cardiology and have done multiple elective rotations on cardiology may have been more interested in completing the survey which would result in a higher knowledge of cardiac devices than residents not as familiar with cardiology topics.
ABSTRACT #116
CLINICAL RESEARCH
CARDIOLOGY
Soumya Gupta1, Kristen Carter1, Hannah Hart1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
BACKGROUND/INTRODUCTION: A remarkable increase in the rate of heart transplant has occurred in recent years. In our study, we determine the in-hospital predictors of mortality in patients with heart transplant.
METHODS: Data was obtained from the Nationwide Inpatient Sample database from January 2016 to December 2020. The study included all adult patients who had received a heart transplant. The primary outcome was inpatient mortality. Information about demographics, insurance, year of admission, and hospital characteristics, comorbidities and acute in hospital complications were abstracted. Using in-hospital death as our outcome, variables that achieved statistical significance (p<0.05) using Chi square testing were included in a multivariable regression analysis.
RESULTS: A total of 15,664 patients had heart transplants. 63.5% of the patients were Caucasian and more than half of the patients (65%) were on Medicare insurance. The overall mortality rate was 2.2%. The use of mechanical ventilation was associated with the highest risk of in-hospital death (aOR, 40.07; 95%CI, 31.5750.86; p<0.001). Other predictors of mortality included older age (age >85 years) (aOR, 5.54; 95%CI, 1.7317.79; p=0.004), African-American race (aOR, 0.58; 95%CI, 0.42-0.80; p<0.001), end stage renal disease (ESRD) (aOR, 2.16; 95%CI, 1.71-2.72; p<0.001), DIC (aOR, 34.57; 95%CI, 14.80-80.72; p<0.001), pulmonary embolism (aOR 3.84; 95%CI, 2.30-6.42; p<0.001), mechanical ventilation (aOR, 40.07; 95%CI, 31.57-50.86; p<0.001), and gastro-intestinal bleeding (GIB) (aOR, 2.4; 95%CI, 1.19-5.19; p=0.01).
CONCLUSION: In this nationwide analysis, overall in-hospital mortality occurred in 2.2% of the patients following heart transplant. The presence of older age, ESRD, GIB, pulmonary embolism, mechanical ventilation and DIC are associated with worse outcomes following heart transplant.
ABSTRACT #117
CLINICAL RESEARCH
CARDIOLOGY
Hannah Hart1, Brandon Rafison1, Anna Mueller1, Juan Arango Morales1, Petra Maslov1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
BACKGROUND/INTRODUCTION: Coronary artery disease is the most common manifestation of cardiovascular disease related morbidity and mortality. Although billions of dollars have been spent on diagnostic and therapeutic innovations over the last two decades, it remains the number one cause of morbidity and mortality. While most coronary artery disease is entirely preventable, only a small fraction of our healthcare dollars is spent on prevention of coronary artery disease and the lifestyle and environmental factors that cause it. Guidelines now explicitly recommend doctors to provide educational resources to optimize heart health, yet finding sufficient time and resources for effective patient education remains a challenge. In this study, we perform a comprehensive review of the published literature involving patient education-based interventions intended to prevent coronary artery disease. We hypothesize that media-based education on coronary artery disease may improve clinical outcomes compared to more traditional forms of education.
METHODS: We conducted a review of the currently published manuscripts dating up to July 2023 using Pubmed and Google Scholar. The search phrases used were “Patient Education,” “Educational Intervention,” and “Coronary Artery Disease Prevention”. The results were sorted by title and date. We compiled data from these studies with information about demographics, type of intervention, and results of the interventions. We discuss our major findings from the review as well as the limitations and future studies that may arise as a result of our findings.
RESULTS: A total of eight studies were included in the review. On average, the study population was 61% male and 56 years old. The studies consisted of a variety of different educational interventions such as video-based, phone call-based, smartphone-based, or pamphlet-based. The majority of patient education-based interventions regarding coronary artery disease lead to significant changes in behavior, knowledge, or in some cases, significant improvement in clinical outcomes. Overall, this did not depend on the specific type of intervention, nor the setting in which the intervention was studied. When comparing the media-based interventions to the more traditional text-based or usual care groups, there was a trend toward more significant improvement in knowledge about coronary artery disease as well as improvement in modifiable risk factors such as body mass index, blood pressure, or cholesterol.
CONCLUSION: Patient education is an important and effective means of not only improving patient quality of life and satisfaction, but also a means to improve clinical outcomes. This review of the literature demonstrates that patient education involving coronary artery disease may have significant implications to improve the individual and societal burden of coronary artery disease. With advancements in technology and a greater role of digital and social media in society, video-based interventions will be essential to invest in to advance the field of preventive cardiology.
ABSTRACT #118
CLINICAL RESEARCH
CARDIOLOGY
EFFECTS OF HIGH INTENSITY INTERVAL TRAINING ON CARDIORESPIRATORY FITNESS AND LEFT VENTRICULAR FUNCTION IN PATIENTS ENROLLED IN CARDIAC REHABILITATION AFTER RECENT MYOCARDIAL INFARCTION
Arpanjeet Kaur1 , Sakul Sakul2, Arshdeep Dhaliwal1, Edgar Argulian1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2University of Nebraska Medical Center, Omaha, NE, United States
Presented at the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Aerobic exercise based cardiac rehabilitation protocols have been shown to potentially reverse cardiac remodeling and decrease morbidity and mortality after recent myocardial infarction (MI). Traditionally, these structured exercise protocols consist of low to moderate intensity continuous training (MICT). Recently, high-intensity interval training (HIIT) have been shown to be superior to MICT in patients with chronic heart failure and coronary artery disease (CAD), however there is limited clinical data assessing its effectiveness in post-MI patients. Hence, we performed a meta-analysis to evaluate the effects of HIIT on cardiorespiratory fitness and left ventricular function in post-MI patients.
METHODS: A comprehensive review of electronic databases (PubMed, Embase, Scopus, Cochrane) was performed from inception through September 2023 to identify randomized controlled trials (RCTs) which evaluated effects of HIIT versus control (MICT or regular physical activity) on cardiorespiratory fitness using cardiopulmonary exercise testing (CPET) and/or left ventricular systolic and diastolic performance on echocardiography in patients enrolled in cardiac rehabilitation post-MI. A random-effects analysis was used to estimate the mean difference, with a 95% confidence interval (CI) using Revman 5.4.1. Heterogeneity was assessed using the Higgins I2 statistic.
RESULTS: 7 eligible RCTs were identified, including 342 patients (HIIT, n=166; Control, n=176). The mean age was 57.4 +/- 1.4 years. Mean training duration was 11.5 +/- 3.7 weeks. HIIT significantly improved peak oxygen uptake (peak VO2) (MD= 2.60 mL/kg/min; 95%CI, 0.19-5.01; p<0.05; I2=76%). No significant difference for change in ventilator efficiency (VE/VCO2 slope) (MD=0.02; 95%CI, -1.55-1.60; p>0.05; I2= 53%). HIIT group showed significant gain in global longitudinal strain (GLS) (MD= 0.52; 95%CI: 0.04-0.99; p<0.05; I2= 0%), however, no significant improvement in LVEF (MD= -0.58; 95%CI, -4.4-3.2; p>0.05; I2=78%). Compared to control, LV diastolic function was better in HIIT group (Change in E/e’ MD= -0.04; 95%CI: -0.14-0.06; p>0.05; I2= 0%) however this did not reach statistical significance.
CONCLUSION: In post MI patients, HIIT significantly improves exercising capacity and global longitudinal strain.
ABSTRACT #119
CLINICAL RESEARCH
CARDIOLOGY
ECHOCARDIOGRAPHIC CHANGES
TAFAMIDIS
Darren Kong1, Arpanjeet Kaur1, Kruti Gandhi1, James Choi1, Ashish Correa1, Arieh Fox1, Kiran Mahmood1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American Heart Association (AHA) Annual Meeting that was held in Philadelphia, Pennsylvania, United States from November 11-13, 2023.
BACKGROUND/INTRODUCTION: Tafamidis, a transthyretin stabilizer, has been shown to have improved survival benefits in patients with transthyretin cardiomyopathy (TTR-CM). However, the echocardiographic effects of tafamidis in TTR-CM patients have not been well studied. We aim to summarize the echocardiographic effects of patients with TTR-CM treated with tafamidis.
METHODS: We performed a meta-analysis using searches on PubMed, Cochrane, and Web of Science between 2018 to 2023 according to Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines. We included retrospective studies involving TTR-CM patients treated with tafamidis 61mg daily and untreated TTR-CM patients over a 12-month period. Our primary outcome was changes in echocardiographic parameters over a 12-month period including left ventricular ejection fraction (LVEF), global longitudinal strain (GLS), and interventricular septal thickness (IVS).
RESULTS: Three different publications were included in our study, with 153 TTR-CM patients in the tafamidis treatment group and 94 TTR-CM patients in the untreated group. The combined average age was 79 ± 6.9 years, and the total number of males in the tafamidis group was 139 (90%) and 80 (85%) in the untreated group. When compared with untreated TTR-CM patients, tafamidis was associated with a decreased decline of GLS by an average of 0.89% (95%CI, -1.32 to -0.46; p<0.0001). However, no differences were found in IVS (mean -0.78, 95%CI, -1.60 to 0.04; p=0.06) or LVEF (mean 1.72; 95%CI, -0.50 to 3.95; p=0.13).
CONCLUSION: Tafamidis decreases the decline in GLS but does not have an association with other echocardiographic parameters. While tafamidis's effects on strain are promising, further studies are needed to characterize its echocardiographic effects.
ABSTRACT #120
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
Jiaxi Miao1 and Vasundhara Singh1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: This project aims to support International Medical Graduates (IMGs) during their critical transition into the intern year, focusing particularly on inpatient rotations. The project envisions a consortium designed to address the unique educational needs of IMGs through a multifaceted approach that includes education, cultural adaptation, mentorship, and wellness support. Project supported by Harvard-Macy institute, and collaborating with University of Wisconsin as a multi-center project launch
METHODS: The project involves a series of targeted interventions, which includes an online video series that offers introduction to the United States healthcare system, covering insurance systems, pharmacy protocols, referral processes, social work dynamics, and interdisciplinary team collaboration. Utilizing simulation labs, IMGs engage in discussions exploring ethical dilemmas within the US healthcare context, addressing cultural nuances. Interactive peer-to-peer workshops focus on honing language proficiency and presentation skills, specifically on the SOAP format for case presentations. Additionally, a podcast series featuring senior IMG residents sharing experiences and strategies to combat imposter syndrome provides valuable emotional support. The initiative also prioritizes community-building by offering mentorship opportunities and group therapy sessions, fostering a supportive environment for IMGs as they navigate the challenges of their intern year. Project evaluation strategies are crucial to ensure the effectiveness of the initiative. Surveys and questionnaires tailored to IMGs’ needs, focus groups, interviews, observations by mentors and senior residents, defined performance indicators, and longitudinal tracking mechanisms constitute the evaluation framework. These methods will gauge participant satisfaction, gather qualitative insights, monitor progress, and assess the project’s overall impact on IMGs’ integration into the intern year. This comprehensive approach aims not only to facilitate a smoother transition for IMGs but also to acknowledge and harness the valuable skills and perspectives they bring to the medical field. By providing tailored support, educational resources, and fostering a supportive community, this initiative seeks to nurture IMGs, enabling them to excel in their residency training and contribute significantly to the healthcare system’s diversity and excellence.
RESULTS: The anticipated positive impact encompasses enhanced learning experiences for IMGs, improved patient care, and a more inclusive medical workforce. By addressing language barriers, cultural differences, and educational disparities, this initiative aims to empower IMGs to leverage their diverse perspectives, ultimately contributing to higher-quality patient care delivery.
CONCLUSION: The project’s scalability should be taken into account, especially if it proves successful. Ensuring that the initiative can be replicated or adapted for different institutions will contribute to its wider applicability.
ABSTRACT #121
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
INITIATION OF TAKE HOME NALOXONE KIT DISPENSING ON THE INPATIENT MEDICINE SERVICE AT MOUNT SINAI WEST
Jiaxi Miao1, Scott Low1, Kristy Huang1, Modesta Asante1, Jood Ani1, Caroline McBrien1, Annalisa Monahan1 , Abdel Abada1, Beth Raucher2, Irina Zaretsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: The opioid crisis continues to be a growing problem nationwide. In NYC, there were 3,026 deaths attributed to drug overdose in 2022, an increase of 12% from 2021, with fentanyl being present in 81% of the cases. To help combat the rise in opioid overdose, our institution became a registered Opioid Overdose Prevention Program (OOPP) in 2020 and began the distribution of take-home naloxone kits from the Emergency Department in 2021 which we are now expanding to the inpatient units. Our aim is to increase take home naloxone kit dispensing to 20% among at-risk patients discharged from the medicine service from September 2023 to March 2024.
METHODS: A take-home naloxone kit dispensing algorithm was created through a collaborative effort between providers, pharmacy and nursing. Naloxone dispensing criteria was established using guidance from the CDC and the NYC DOH and include patients with illicit substance use, on treatment for opiate use disorder, on high dose opioids, or on concurrent CNS depressants. Internal medicine residents, advanced practice practitioners, and attending physicians became certified dispensers of naloxone through the OOPP training. A SmartPhrase was developed to ensure that proper patient education on naloxone use was provided at the bedside. Lectures were conducted on the process of kit dispensing. Posters outlining prescribing protocols were displayed in charting areas. Ongoing chart reviews are being conducted and reminder notifications are sent to providers in real time via secure Epic Chat. A raffle was created to further engage providers in kit dispensing. A patient database with take-home naloxone orders and the order administration record is generated via an Epic report biweekly. A manual review of unadministered orders is conducted to confirm documentation of dispensed kits outside of the medication administration record. A separate report is generated via Epic using the provider dispensing SmartPhrase to determine the number of patients that were offered a kit but declined.
RESULTS: Baseline data was obtained using ICD10 codes and prescription reports from January through March 2023. This data indicated an average of 70 at-risk patients per month discharged from the medicine service. The number of patients at the start of our project in September 2023 who were offered a take home kit was 8. This number increased to 19 in November and 17 in December.
CONCLUSION: While the dramatic increase in kit distribution so far is encouraging, we believe sustainability of our project will be an issue given the high reliance on provider education and ongoing real time reminders sent out by our team. We hypothesize creating a best practice advisory alert within the EMR to prompt providers to dispense naloxone on discharge to at-risk individuals would offer a more sustainable solution.
ABSTRACT #122
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
GASTRIC LIPOMA: A RARE CAUSE OF MELENA*
Alexandria Markley1, Rohit Nathani1, Erica Park1, Mohamed Rabie2, Armand Cacciarelli1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
*ACG Outstanding Poster Presentation
BACKGROUND/INTRODUCTION: Gastric lipomas (GL) are rare benign tumors, accounting for less than 1% of all gastric tumors arising from adipose tissue within the stomach. They are often asymptomatic and slow growing but can cause symptoms and complications such as gastric outlet obstruction and gastrointestinal (GI) bleeding. We present a case of a GL incidentally discovered during an esophagogastroduodenoscopy (EGD) for melena.
CASE PRESENTATION: A 66-year-old male with a medical history of hypertension, benign prostate hyperplasia, and obesity presented with dark stools. Physical examination was unremarkable and initial laboratory studies revealed iron deficiency anemia with a Hb of 9.8 mg/dl. The differential diagnosis was broad for causes of upper GI bleeding and the patient underwent EGD. EGD revealed a medium-sized, noncircumferential, ulcerated mass in the gastric antrum without active bleeding. Histology confirmed a gastric hyperplastic polyp with no malignancy. Further evaluation with endoscopic ultrasound (EUS) identified an intramural, hyperechoic lesion originating from the submucosa. Pathology showed fibroadipose tissue with reactive features consistent with an ulcerated lipoma. Due to its large size, the patient was referred for surgical evaluation. Computed Tomography (CT) scan showed a 9.1 x 4.5 cm fat density lesion. The patient underwent diagnostic laparoscopy, robotic subtotal gastrectomy with removal of perigastric lymph nodes, longitudinal gastrotomy, and excision of intragastric mass. The mass was confirmed to be a well differentiated lipoma on excisional biopsy. The patient had complete resolution of symptoms.
CONCLUSION: Gastric lipomas are often asymptomatic; however, in some instances, as described above, gastric lipomas can cause symptoms such as abdominal pain, bloating, nausea, vomiting, or gastrointestinal bleeding if it is associated with ulceration or necrosis. Initial evaluation with EGD allows direct visualization of the lesion. Imaging techniques such as EUS, CT, or magnetic resonance imaging can further provide valuable information about its size, location, and appearance. Small asymptomatic GL can be managed conservatively with regular surveillance EGDs. GL under 4 cm can typically be removed endoscopically. However, larger lipomas or symptomatic cases, particularly those with concerns of ulceration, bleeding, or diagnostic uncertainty, may require surgical removal. Recurrence is rare post-removal, and long-term follow-up is generally unnecessary.
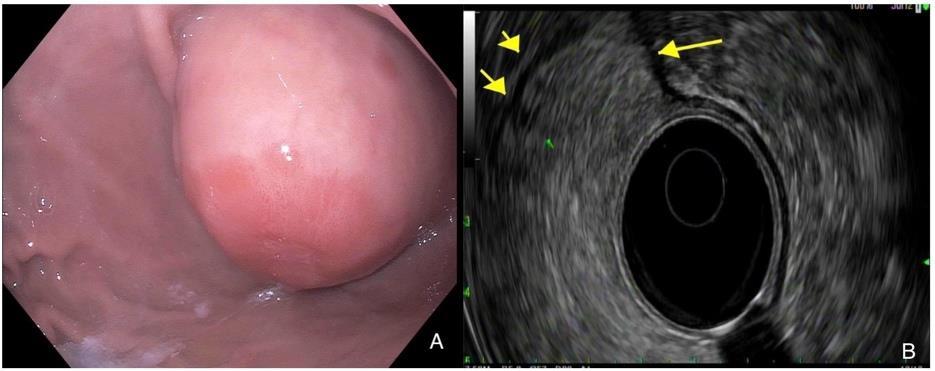
Figure 1: A. Upper Gastrointestinal Endoscopy image showing large subepithelial gastric antrum mass with ulceration. B. Endoscopic Ultrasound image demonstrating an intramural lesion in the antrum of the stomach.
ABSTRACT #123
CLINICAL RESEARCH
CARDIOLOGY
ATRIAL FIBRILLATION AS AN INDEPENDENT PREDICTOR FOR MAJOR ADVERSE CARDIOVASCULAR EVENTS IN PATIENTS WHO UNDERWENT TRANSCATHETER TRICUSPID VALVE PROCEDURES
Christopher N. Matthews1, Sara Diaz Saravia1 , James Choi1 , Abel Casso Dominguez1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of Hospital Medicine (SHM) Annual Meeting that will be held in San Diego, California, United States from April 12-15, 2024.
BACKGROUND/INTRODUCTION: Transcatheter tricuspid valve procedures (TTVP) are used to manage tricuspid regurgitation, however these procedures are less common than other transcatheter valve procedures. Limited literature on TTVP exists, especially with regards to predictors of major outcomes. Atrial fibrillation is associated with increased mortality, stroke, cardiogenic shock, need for permanent pacemaker, AKI, major bleeding in those that underwent transcatheter aortic valve replacement (TAVR). Atrial fibrillation is also associated with increased mortality, major bleeding, heart failure hospitalization, stroke, and major adverse cardiovascular events (MACE) in those that underwent transcatheter mitral valve repair. This study will investigate the effect of concomitant atrial fibrillation on outcomes of those undergoing TTVP.
METHODS: A retrospective cross-sectional design was implemented using the National Inpatient Sample, a database of U.S. hospitalizations between January 2017 and December 2019. Within this population, adults who had undergone TTVP were selected. Pearson chi-squared analysis was used to compare prevalence of baseline characteristics. Atrial fibrillation was used to predict major adverse cardiovascular event (MACE). Multivariate logistic regression analysis was performed adjusted for age, gender, and race, with a p-value <0.2 in univariate screen.
RESULTS: A total of 1380 patients underwent TTVP, and 1095 (79.35%) had atrial fibrillation. Patients with atrial fibrillation were older with mean age of 76.37 years compared to the non-atrial fibrillation group with mean age of 61.59 years, p<0.05 (Table 1). Both the atrial fibrillation group and non-atrial fibrillation group were made up of slightly more females. There was no significant difference in the atrial fibrillation and non-atrial fibrillation group when it came to race composition. With regards to Charlson comorbidity index score, the two groups were statistically different, p=0.003. Those with atrial fibrillation had a higher prevalence of MACE than those without, p<0.0001. For those that underwent TTVP, having atrial fibrillation increased the odds of MACE by 3.29 compared to those without atrial fibrillation (OR, 3.29; 95%CI, 1.65-6.57; p=0.001) (Table 2). For individual outcomes that comprise MACE having atrial fibrillation increased the odds of heart failure by 3.05 compared to those without atrial fibrillation (OR, 3.05; 95%CI, 1.54-6.05; p=0.001) in those that underwent TTVP. Mortality was not statistically significant between those with atrial fibrillation (2.74%) and those without atrial fibrillation (3.51%).
CONCLUSION: This study shows that in patients who underwent TTVP, atrial fibrillation was associated with increased MACE, specifically heart failure. Predictors of outcomes after TTVP in patients with atrial fibrillation should be evaluated in future studies. This may help to develop a risk score similar to ENVISAGE for those with atrial fibrillation that may undergo TAVR.Outcomes that comprise the ENVISAGE include excessive alcohol use, older age, renal failure, liver disease, peripheral artery disease, major/ predisposition bleeding, and NYHA III/IV.
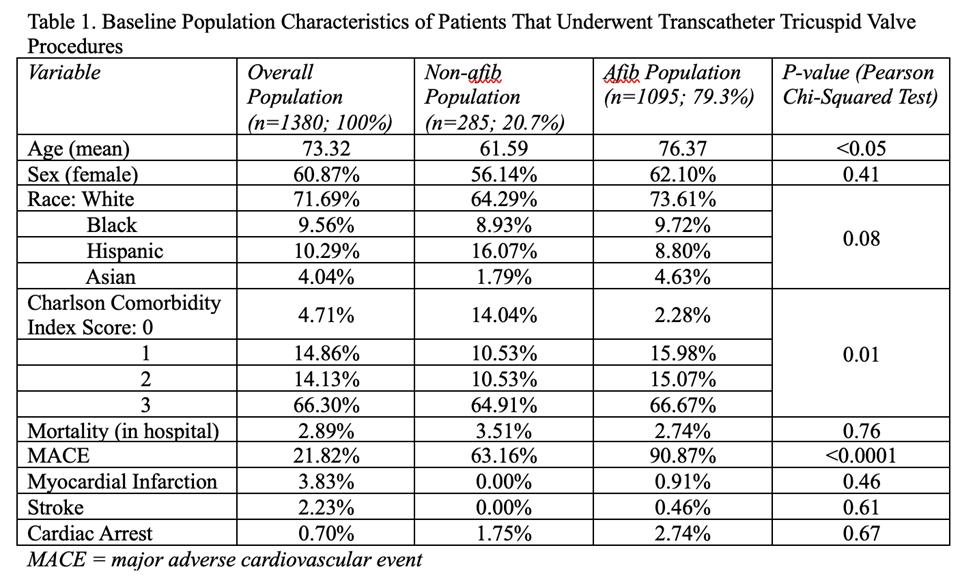

ABSTRACT #124
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
REVERSE TAKOTSUBO CARDIOMYOPATHY AFTER CESAREAN DELIVERY COMPLICATED BY MASSIVE POST-PARTUM HEMORRHAGE IN A CASE OF PLACENTA ACCRETA
Christopher N. Matthews1, Yesha Rana2 , Brandon Berman1, Joseph D. Marinelli1, Krysthel Engstrom2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at both the Annual Mount Sinai Fuster Heart Research Forum that was held in New York, New York, United States on March 15, 2024 and the American College of Cardiology (ACC) Annual Meeting that was held in Atlanta, Georgia, United States from April 6-8, 2024.
BACKGROUND/INTRODUCTION: Reverse takotsubo cardiomyopathy (CM) is a less common variant of takotsubo CM associated with younger age and a smaller decline in left ventricular ejection fraction.
CASE PRESENTATION: A 31-year-old pregnant female presented with active vaginal bleeding in hemorrhagic shock at 32-weeks gestation. She underwent emergent c-section for placenta accrete that was complicated by bladder laceration with an estimated total blood loss of 10L. Consequently, she underwent hysterectomy and bilateral salpingectomy, followed by embolization of five intra-abdominopelvic arteries and cystorrhaphy. Despite fluid and blood product resuscitation with 18 units of pRBC, 7 units FFP, 4 units of cryoprecipitate, 3 units of platelets, she required vasopressor support to maintain blood pressure. Emergent TTE revealed severely reduced LVEF 30% with hypokinesis of all basal segments (Figure 1). Post operative day 2, she was successfully weaned off vasopressors and beta blocker were initiated for heart failure with reduced ejection fraction. Repeat TTE 1 week after showed normal LVEF with no wall motion abnormalities (Figure 2). CTA coronaries revealed calcium score of 0 and patent coronary arteries, most consistent with reverse stress cardiomyopathy or peripartum cardiomyopathy.
CONCLUSION: Our patient had two etiologies that could explain her cardiomyopathy: peripartum as well as stress-induced. It is difficult to distinguish between peripartum cardiomyopathy and stress cardiomyopathy in this case as both are diagnoses of exclusion. Stress cardiomyopathy and peripartum cardiomyopathy can have similar features; however, complete recovery of systolic function is more characteristic of stress cardiomyopathy, as found with this patient.
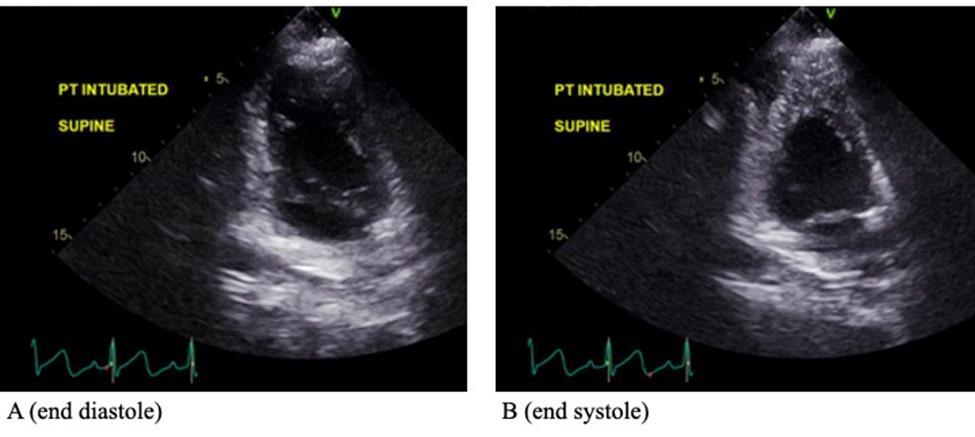
1. TTE POD0 showing LV basal-mid anteroseptal and basal-mid inferoseptal dyskinesis, basal-mid inferior wall akinesis and basal anterolateral and basal inferolateral hypokinesis.
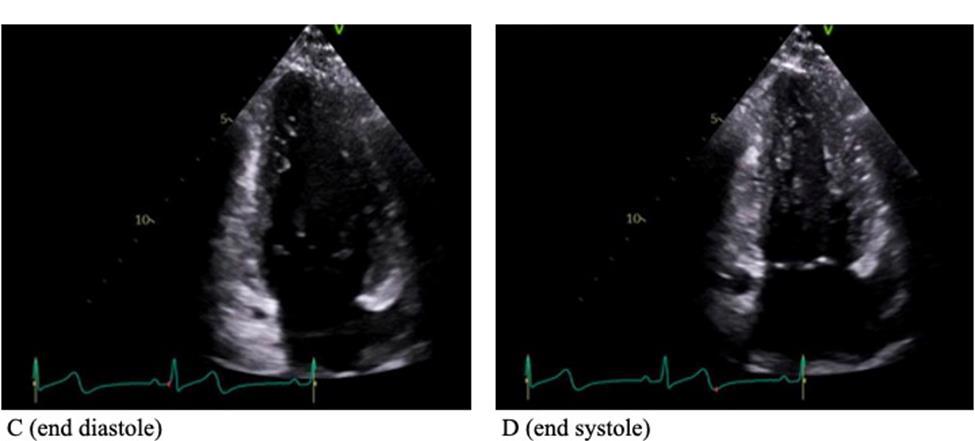 Figure
Figure
ABSTRACT #125
CLINICAL RESEARCH
CARDIOLOGY
TRANSCATHETER MITRAL VALVE PROCEDURE OUTCOMES IN PATIENTS WITH HYPERTROPHIC OBSTRUCTIVE CARDIOMYOPATHY
Christopher N. Matthews1, Sara Diaz Saravia1, James Choi1, Abel Casso Dominguez1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Society of Hospital Medicine (SHM) Annual Meeting that will be held in San Diego, California, United States from April 12-15, 2024.
BACKGROUND/INTRODUCTION: Several case reports and case series have found that transcatheter mitral valve procedures (TMVP) improve hemodynamics and reduce symptoms in patients with mitral valve disease and concomitant hypertrophic obstructive cardiomyopathy (HOCM). There is a lack of evidence regarding the outcomes of patients that undergo TMVP with HOCM, however several studies have evaluated the outcomes of transcatheter aortic valve replacement (TAVR) in patients with HOCM. These studies have shown a higher incidence of in hospital mortality, net adverse cardiovascular events, acute kidney injury (AKI) and hemodialysis, vascular complications, permanent pacemaker requirement, aortic dissection, cardiogenic shock, and mechanical ventilation requirement. The present study examined a large nationally representative cohort to evaluate clinical outcomes of patients with HOCM after TMVP.
METHODS: Patients (age ≥18 years) from the National Inpatient Sample database who underwent transcatheter mitral valve repair and replacement between January 2017 to December 2019 were selected and a retrospective, cross-sectional design was utilized. Pearson chi-squared analysis was used to compare prevalence of characteristics listed in Table 1. Outcomes of those with and without HOCM that underwent TMVP were analyzed using multivariate logistic regression adjusted for age, sex, race, income, Charlson comorbidity index, hospital teaching status, hospital region and hospital bedsize. For both analyses, p-values of less than 0.05 were considered significant.
RESULTS: We identified 27,005 patients who underwent TMVP during the study period, and 125 (0.46%) had concomitant HOCM. Demographic characteristics were similar in patients that had a TMVP with HOCM vs without HOCM (Table 1). There was a significant difference in the rates of AKI (4.00% versus 0.15%, p<0.0001) and cardiac arrest (4.00% versus 0.56%, p=0.02) in patients with HOCM vs those without HOCM, respectively. There were no significant differences in rates of in-hospital mortality (0.00% versus 2.33%, p=0.43), stroke (0.00% versus 0.89%, p=0.64), cardiogenic shock (8.00% versus 5.13%, p=0.52) or bleeding (4.00% versus 1.60%, p=0.34) in patients with HOCM vs without HOCM, respectively (Table 1). Patients with HOCM had higher adjusted odds of acute kidney injury (AKI) (OR, 17.53; 95%CI, 1.42 – 216; p=0.03) (Table 2).
CONCLUSION: Patients who underwent TMVP with concomitant HOCM had similar rates of in-hospital mortality, stroke, cardiogenic shock and bleeding as patients without HOCM, however there was a higher rate of AKI after TMVP in patients with HOCM. We only identified one other large study in the literature on TMVP patients with HOCM, which utilized the national readmission database. This study found that patients with HOCM had higher odds of in-hospital mortality, stroke, and length of stay compared to those without HOCM that underwent MitraClip®, and presence of AKI was not statistically significant between patients with HOCM (22%) and without HOCM (15%), which does not align with our results. Further research in this population is needed to understand prognostic significance and to prevent AKI occurrence in patients undergoing TMVP.
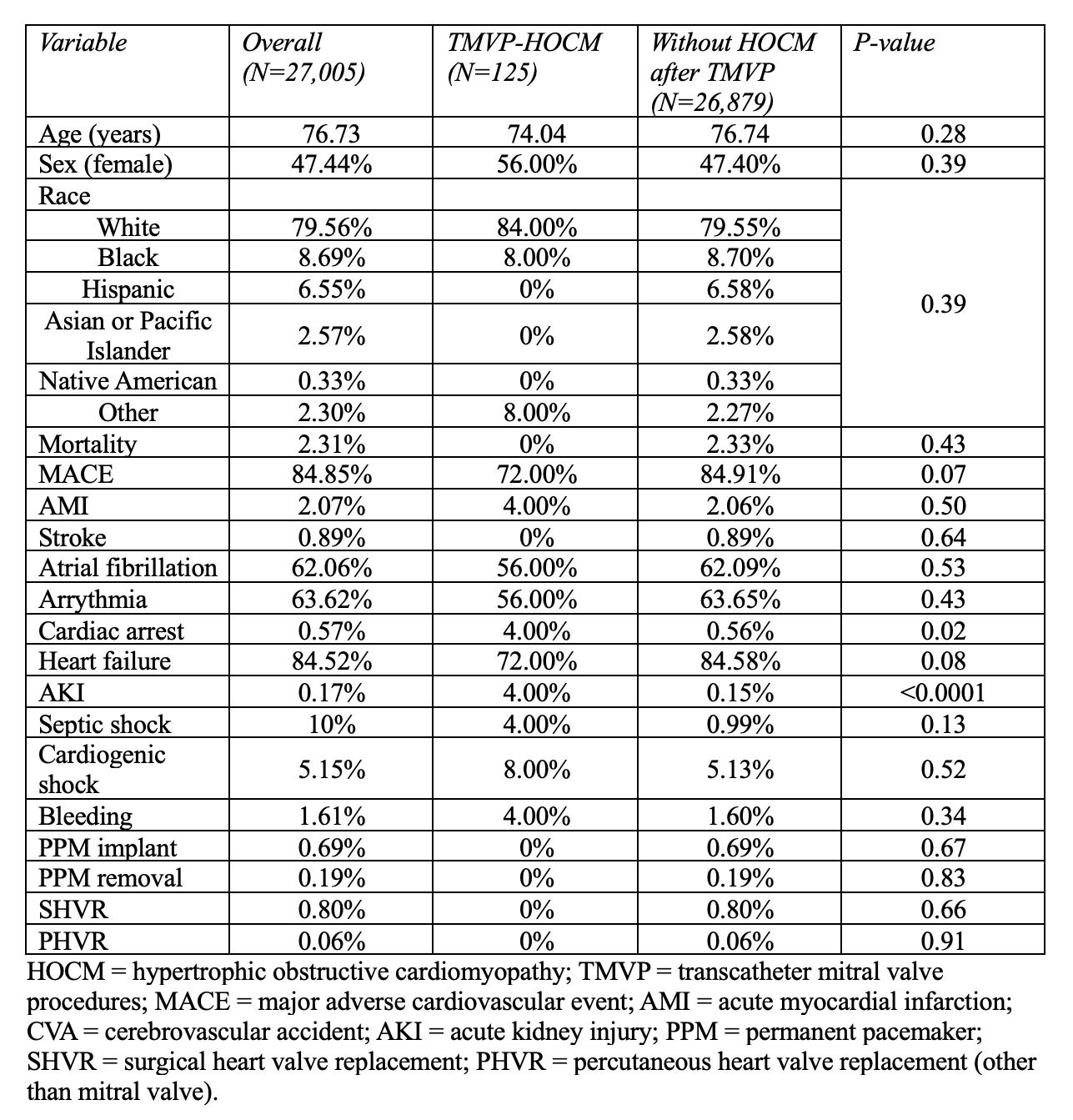
1. Characteristics of patients with and without HOCM that underwent TMVP

Table 2. Multi-variate logistic regression of outcomes of patients with HOCM after TMVP
ABSTRACT #126
CLINICAL RESEARCH
GASTROENTEROLOGY
A MINORITY OF PATIENTS IN NEED OF PELVIC FLOOR BIOFEEDBACK TRAINING ACTUALLY ATTEND SCHEDULED THERAPY SESSIONS
Joseph A. Menand1, Yonatan Israel2, Emma Reford2, Robinderpal Sandhu1, Ahmun Zafar1 , Kimberly Cavaliere1,3, Priyanka Singh1,3, Jean Saleh1,3, Michael S. Smith1,3, Yuying Luo3, Daniela Jodorkovsky1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023
BACKGROUND/INTRODUCTION: Pelvic Floor Biofeedback Therapy (BFT) is the gold standard treatment for dyssynergic defecation (DD), but access to this intervention remains a significant barrier. We aim to characterize whether socioeconomic and demographic factors impact access to and completion of BFT sessions.
METHODS: All patients who underwent anorectal manometry (ARM) between 2021-2022 at a single highvolume center with motility expertise were considered. Patients were included in the analysis if BFT was recommended based on ARM. Baseline patient characteristics were compared using Chi-squared analysis and one-way ANOVA. Primary outcomes were attendance of at least one BFT session and completion of a sixsession regimen, if recommended. Secondary outcomes included differences in socioeconomic and demographic characteristics based on whether BFT was attended and completed.
RESULTS: A total of 148 patients who underwent ARM were recommended for BFT. Only 54 of 148 patients (36.5%) participated in BFT at the home site, attending an average of six sessions. A full six session regimen was completed by 48.1% of patients. There were no significant differences in patient-level factors between patients who attended BFT and those who did not. There were also no significant differences in patient-level factors between patients who attended at least 1-5 BFT sessions compared to those who completed a minimum set of six sessions.
CONCLUSION: In this cohort, less than 40% of patients recommended for BFT to treat dyssynergic defecation participated in at least one session. Additionally, a minority of those who attended at least one session completed the standard set of six visits. Interestingly, more than 75% of those who completed six sessions continued with regular BFT. There were no socio-demographic factors that were found to impact BFT attendance. Study limitations include the quality and availability of retrospectively collected data. This study should prompt further prospective research to qualitatively assess patient and healthcare system barriers to pelvic floor biofeedback therapy attendance and completion, to develop patient-centered interventions to improve show rates.
ABSTRACT #127
CLINICAL RESEARCH
GASTROENTEROLOGY
IMPAIRED MOBILITY DOES NOT IMPACT ANORECTAL MANOMETRY FINDINGS AND BIOFEEDBACK UTILIZATION
Yonatan Israel1 , Joseph A. Menand2 , Emma Reford1 , Ahmun Zafar2 , Robinderpal Sandhu2 , Kimberly Cavaliere2,3 , Priyanka Singh3 , Jean Saleh2,3 , Michael S. Smith2,3 , Yuying Luo3 , Daniela Jodorkovsky2
1Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Anorectal Manometry (ARM) is a key diagnostic test used to evaluate patients with constipation or fecal incontinence not responding to first-line interventions. Previous research shows that level of physical mobility can impact anorectal dysfunction through pre-existing underlying comorbidities as well as impaired anorectal sensation. However, the effects of impaired mobility on anorectal manometry findings have not been studied.
METHODS: This is a retrospective study of all patients who underwent ARM between 2021-2022 at a tertiary care center with expertise in motility disorders. Baseline patient characteristics were compared using Chi-Square analysis or Fisher's Exact Test. Outcome variables from ARM studies, as well as biofeedback referrals and attendance were compared between patients with independent versus impaired mobility (defined as use of assistive device, wheelchair or bedbound).
RESULTS: The study included 166 patients (73% female) with a mean age of 51.4 ± 19.0 years; the majority were independently mobile (83.1%). There was no statistical difference between the independent and impaired mobility groups in terms of indication for ARM referral, the presence of dyssynergic defecation, rectal sensory abnormalities, presence of the recto-anal inhibitory reflex or balloon expulsion testing. There also was no difference in the recommendation for biofeedback training and the proportion of patients who attended biofeedback.
CONCLUSION: We found no difference in ARM results according to mobility status, suggesting mobility status should not be a barrier to referring a patient to ARM if appropriate. Reassuringly, attendance at biofeedback sessions if recommended did not differ between the two groups. This study was limited by a small number of subjects in the impaired mobility group which may reflect a bias in those who were initially referred to ARM. Future research should focus on identifying barriers to appropriate anorectal testing in patients with impaired mobility status.
ABSTRACT #128
CLINICAL RESEARCH
GASTROENTEROLOGY
WHERE IS THE DRE? DIGITAL RECTAL EXAMS ARE INFREQUENTLY PERFORMED PRIOR TO ANORECTAL MANOMETRY EXAMS
Joseph A. Menand1, Robinderpal Sandhu1, Yonatan Israel2, Emma Reford2, Ahmun Zafar1, Kimberly Cavaliere1,3, Priyanka Singh3, Jean Saleh1,3, Michael S. Smith1,3, Daniela Jodorkovsky1,3, Yuying Luo3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Dyssynergic defecation (DD) is a common cause of constipation in patients not responding to pharmacologic therapy. A diagnostic digital rectal examination (DRE) should be performed prior to referral for anorectal manometry (ARM) as studies have shown that DRE has similar sensitivity and specificity in diagnosing DD when performed by a skilled provider. It is unclear how frequently DRE is performed prior to ARM, and whether DRE findings can predict a diagnosis of DD on ARM in a real-world setting with a range of providers.
METHODS: A retrospective study of all consecutive patients who underwent ARM between 2021-2022 at one tertiary center with motility expertise was performed. Baseline patient characteristics were compared using Chisquared and Fischer’s Exact Tests. Our primary outcome was the proportion of patients who had a DRE prior to ARM; secondary outcomes included the concordance between DRE findings and diagnosis of DD.
RESULTS: Our study included 166 patients, with 67 (40.3%) having a documented DRE prior to ARM (Table 1). There were no significant differences in age, gender, race, BMI and English as primary language between patients who did and did not receive a DRE. The majority (58.2%) of DREs were performed by gastroenterology providers (attendings, fellows or nurse practitioners). Patients with a DRE were more likely to have a dyssynergic pattern on ARM (p=0.030); however, there were no significant differences in the proportion of patients with rectal hyper- or hyposensitivity, present recto-anal inhibitory reflex, or abnormal balloon expulsion test. Of the DREs performed by gastroenterology providers, 57.9% had findings concordant with ARM results, which was significantly higher than for DREs by non-GI providers (30.8%, p=0.007).
CONCLUSION: In our study, only 40% of patients referred for ARM had a DRE prior to additional diagnostic testing. The majority of DREs were administered by gastroenterology providers, yet these examinations were only 57.9% concordant with ARM findings. While concordance was lower than previously reported, it was significantly higher than non-GI providers. Given access barriers to ARM in many clinical settings, as well as previous reports ofhigh concordance between DREand ARM, trainingin a skilled DREshould be re-emphasized for all levels of clinical providers.
ABSTRACT #129
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
Andre Khazak1 , Patricia Miguez Arosemena2, Jake Debroff1, Violetta Laskova1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Autoimmune pancreatitis (AIP) is a rare etiology of pancreatic inflammation that can have presentations ranging from asymptomatic jaundice to severe abdominal pain. Type 2 AIP has a younger age of onset, often without significant elevation in immunoglobulin G4 (IgG4) positive cells and a lack of systemic involvement as compared to type 1 AIP. Diagnosis is based on imaging, histology, and IgG4 levels with consideration for response to glucocorticoids. We present a case of a 28-year-old male with 7 emergency department (ED) visits for abdominal pain thought to be secondary to alcohol related pancreatitis found to have repeat imaging concerning for AIP.
CASE PRESENTATION: A 28-year-old male with a history of alcohol use disorder presented to the ED for recurrent abdominal pain, his 7th ED visit over a 2-week interval. He had elevated lipase levels ranging from 609 U/L to 1,141 U/L on previous visits treated with fluids and nonsteroidal anti-inflammatory drugs without further work up given presumptive diagnosis of alcohol related pancreatitis. Initial CT scan obtained during his 5th ED visit showed haziness in the pancreatic head and body consistent with acute pancreatitis without necrosis. Ultrasound was negative for gallstones. The patient was again discharged following pain control. During his 7th and final ED visit, the patient endorsed additional symptoms of dark urine and clay colored stool. Labs were significant for an elevated lipase to 344 U/L with new transaminitis with AST 339 U/L, ALT 699 U/L, direct bilirubin 5.6 mg/dl, and total bilirubin 7.4 mg/dl. Repeat CT revealed acute pancreatitis with new hyperenhancement of the pancreatic tail with intra and extra hepatic bile duct dilatation with abrupt tapering of the common bile duct (CBD). MRCP revealed a diffusely boggy, enlarged sausage-shaped pancreas and distal CBD narrowing with upstream CBD dilatation suspicious for autoimmune pancreatitis. IgG4 levels returned elevated to 101 mg/dl after the patient had left against medical advice and subsequently lost to follow up.
CONCLUSION: AIP is a rare and often missed diagnosis. Lack of suspicion for AIP in this patient with alcohol use disorder resulted in delayed diagnosis and failure to administer steroids leading to recurrent ED visits. Physicians need to be diligent in considering an immunologic component of pancreatitis in young patients as early diagnosis will provide prompt initiation of appropriate serologic and radiologic work up with timely initiation of steroids.
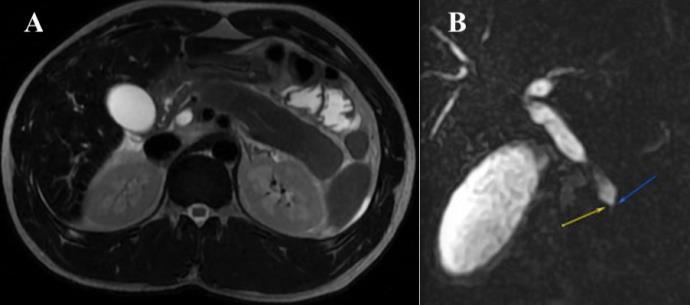
Figure 1: Left (A): Magnetic Resonance Cholangiopancreatography (MRCP) with diffusely boggy, enlarged sausage-shaped-pancreas with diffuse T1 hypointense signal. Right (B): MRCP with narrowing of the distal common bile duct (CBD) with upstream CBD dilatation secondary to the edematous pancreas.
ABSTRACT #130
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
ENDOSCOPIC PALLIATIVE IN-STENT LIQUID NITROGEN SPRAY CRYOTHERAPYFOR ESOPHAGEAL ADENOCARCINOMA*
Patricia Miguez Arosemena1 , Andre Khazak2, Angad Uberoi1,2, Michael S. Smith1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023. *ACG Award-Winning Abstract
BACKGROUND/INTRODUCTION: Conventional esophageal adenocarcinoma (EAC) treatments include surgery, chemotherapy, and radiation. Patients with unresectable disease often are plagued by dysphagia, which can result in poor nutrition and aspiration. Endoscopic stent placement is the most commonly used palliative modality in these patients. Studies have demonstrated the benefit of liquid nitrogen spray cryotherapy (LNSCT) to eradicate persistent Barrett’s esophagus in patients previously treated with chemoradiotherapy for EAC, and more recently for dysphagia palliation. Here we present a case of LNSCT after stent placement for palliation of persistent dysphagia.
CASE PRESENTATION: An 84-year-old male with EAC previously treated with chemoradiotherapy presented with recurrent dysphagia and weight loss. Endoscopy revealed a mass at the esophago-gastric junction (EGJ), with biopsy confirming recurrent EAC. He underwent stent placement for dysphagia palliation, but had persistent symptoms. LNSCT was performed, with treatment directed through the stent to the adjacent tissue, along with the tissue distal to the stent near the EGJ. Each luminal hemi-circumference received three cycles of 30 seconds of LNSCT. The patient reported symptom improvement following treatment. Four weeks later, repeat endoscopy demonstrated decreased tissue bulk distal to the stent, and another round of LNSCT was performed. Unfortunately, the patient passed away before further his next endoscopy.
CONCLUSION: Stent placement is a preferred option for dysphagia palliation in EAC. However, stents are associated with adverse events including migration, perforation and development of chest pain. In Pulmonology, in vitro studies have shown LNSCT in conjunction with existing airway stents is feasible and does not cause stent damage. Based on similarity of stent composition, this seems highly applicable to the gastrointestinal field. Further in vivo studies are needed to confirm the efficacy of palliative combination therapy with both stent placement and LNSCT.g
ABSTRACT #131
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
GASTROENTEROLOGY
GASTROINTESTINAL TRACT COMPLICATIONS FROM IODODERMA
Patricia Miguez Arosemena1 , Andre Khazak2, Angad Uberoi1,2, Shanique Wilson Noack1,2, Kimberly Cavaliere1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Iododerma is a rare and potentially serious dermatosis that develops as a delayed hypersensitive reaction to iodinated compounds, often occurring in patients with renal insufficiency. Cutaneous presentation can vary but includes nodular eruption, acneiform, pustular, and hemorrhagic bullae. Symptoms typically start 2-3 days following exposure and resolve within 2-6 weeks. Extracutaneous manifestations include conjunctivitis, salivary gland swelling, vasculitis, and respiratory compromise. We present a case of a patient with iododerma and gastrointestinal manifestations.
CASE PRESENTATION: A 78-year-old female with chronic kidney disease and diverticulosis presented with hematuria and was found to have a urinary tract infection with acute kidney injury. Computed tomography (CT) of the abdomen and pelvis with iodinated contrast medium was performed. Three days later, the patient rapidly developed oral nodular lesions and multiple flesh-colored papules on her face, neck, upper chest, and arms that progressed to crusted erythematous papules and hemorrhagic bullae. Dermatology was consulted and a skin biopsy demonstrated diffuse dermatitis with histiocytes and neutrophils. Special stains for fungus and bacteria were negative. Laboratory tests for infections including Herpes Simplex Virus, Varicella Zoster, Monkeypox, HIV serology were negative in addition to negative blood cultures. Urinary levels of iodine were elevated, raising concern for iododerma and the patient was started on intravenous steroids. Four days later, the patient developed painless hematochezia for which the Gastroenterology service was consulted. An upper endoscopy was performed which showed friable nodular mucosa with dark deposits in the stomach and duodenum. Biopsy of these deposits showed non-specific acute and chronic inflammation with reactive changes. The patient developed multiorgan failure and passed away the next day. Autopsy showed dark pigment deposited in the superficial mucosa of the stomach, small intestine, and colon with ulcers in the ileum and frank blood in the colon.
CONCLUSION: Iododerma can progress rapidly and due to its heterogeneous clinical presentation, can represent a diagnostic challenge. Delayed reactions to iodinated contrast medium may be underdiagnosed as cutaneous symptoms may be attributed to medications, autoimmune or infectious processes. Here we contribute to the literature by describing some of the gastrointestinal manifestations of this rare condition.

Figure 1: A-D. Endoscopic photography of the lesser curvature of the stomach and incisura with nodules and dark discoloration of the mucosa. E. Flesh-colored papules in the neck (Three days after exposure). F. Hemorrhagic bullae in the neck (Five days after exposure). G. Oral ulcers and facial hemorrhagic papules (Five days after exposure). H. Facial hemorrhagic crusted lesions (Eight days after exposure).
ABSTRACT #132
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
RECURRENT CANDIDA ESOPHAGITIS IN A PATIENT WITH PSORIATIC ARTHRITIS TRANSITIONING IMMUNOLOGIC AGENTS
Andre Khazak1 , Patricia Miguez Arosemena2, Jake Debroff1, Alain Kameni1 , Svetlana Chernyavsky1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Candida esophagitis is often seen in immunocompromised patients, most commonly presenting as an acquired immunodeficiency syndrome (AIDS) defining illness in patients with poorly controlled human immunodeficiency virus (HIV) infection. It can also be seen in patients with hematologic or solid organ malignancies on cytotoxic treatment regimens and patients on chronic steroids. There have been no documented cases of Candida in patients undergoing biologic medication adjustment from interleukin 17 alpha (IL-17a) antagonists to tumor necrosis factor alpha (TNFa) inhibitors, requiring further investigation into practice guidelines and associated risks of bridging medications. We present a case of a 58-year-old female with poorly controlled psoriatic arthritis with recent biologic medication adjustment and significant dysphagia found to have recurrent Candida esophagitis.
CASE PRESENTATION: A 58-year-old female with a history of Candida esophagitis, gastric bypass with small bowel obstruction, multiple endocrine neoplasia 2b, and psoriatic arthritis presented with generalized weakness and a 15-pound weight loss over 1 month. She reported worsening dysphagia to solids with globus sensation and associated nausea and vomiting. She was initially planned for outpatient upper gastrointestinal series however presented to the hospital before completing the work up due to severe weakness. She was also recently transitioned from the IL-17a antagonist ixekizumab to the TNFa inhibitor etanercept for her poorly controlled psoriatic arthritis prior to admission, completing a total of 3 etanercept doses. Given her weight loss and dysphagia, she underwent an inpatient endoscopy that was significant for diffuse esophageal candidiasis. She was started on oral fluconazole and discharged with resolution of her dysphagia. Immunosuppressants were held with plan for close outpatient follow up.
CONCLUSION: Although Candida esophagitis has been documented in the setting of IL-17a antagonist use, Candida esophagitis secondary to etanercept is rare. There have been no reported studies of Candida esophagitis when transitioning immunosuppressants. Assessment of duration of action of IL-17a antagonists and risk for synergistic toxicity should be investigated to inform decisions on safe practices regarding medication bridging. Close monitoring and consideration for careful transition of immunosuppressants may be integral as switching from an IL17 antagonist to a TNF alpha inhibitor may increase the risk for Candida esophagitis.
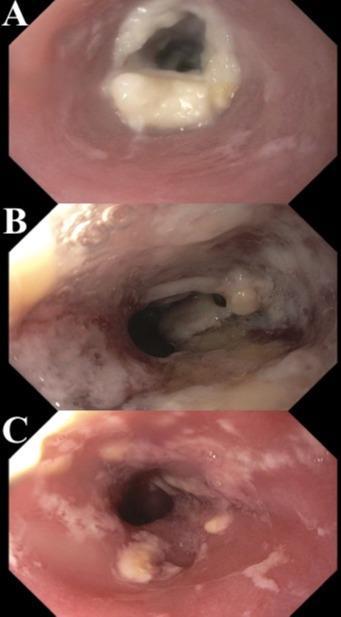
ABSTRACT #133
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
TUBERCULOSIS OR NOT TUBERCULOSIS?
Jenny Dave1,2 , Patricia Miguez Arosemena2, Priya Simoes1
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Gastrointestinal (GI) tuberculosis (TB) accounts for 1 to 3% of all TB cases worldwide (Chakinala, 2022). If left undiagnosed and untreated, it can cause significant morbidity with up to a 60% mortality (Chan, 2015). Most prevalent in Africa and Asia, western countries are seeing a rise in cases largely due to immunocompromising disease, biologic use and migration. However, given the low rate of cases in the U.S. and non-specific symptoms, Gastrointestinal tuberculsosis is not always on the clinician’s differential for patients with common risk factors which may lead to a delay in diagnosis and treatment. We present a case of ileal tuberculosis in an elderly female.
CASE PRESENTATION: An 82-year-old female who traveled to the Dominican Republic six months prior with a medical history of rheumatoid arthritis on methotrexate (MTX) and low dose prednisone presented to the hospital for three months of abdominal pain and one week of diarrhea with high grade fevers. Abdominal CT revealed wall thickening of the terminal ileum, ascending and transverse colon with inflammatory changes. GI PCR was positive for Enteroaggregative E. Coli. Despite three days of antibiotic treatment for infectious colitis she experienced fevers and continued diarrhea. MTX and prednisone were held and antibiotic coverage was broadened. A full infectious workup was performed including a normal transthoracic echocardiogram. A QuantiFERON gold was positive. CT Chest showed a right upper lobe opacity with one of three AFB sputum tests positive. Repeat CT showed resolution of colonic wall thickening but continued thickening of the terminal ileum. On day 17 of hospitalization colonoscopy revealed a severely inflamed and ulcerated ileum. Pathology showed granulomatous inflammation. It was debated if this could represent Crohn’s disease but was ultimately thought to be most consistent with TB. On day 30 she was started on anti-TB therapy with clinical improvement in symptoms.
CONCLUSION: Gastrointestinal tuberculosis can pose a diagnostic challenge and requires a high index of suspicion to diagnose. This case highlights a patient with common risk factors including recent travel to an endemic region and immunosuppression as well as typical presenting symptoms and imaging findings of gastrointestinal tuberculosis, however diagnosis was still delayed. While still rare, cases are becoming more common in the United States and timely diagnosis can improve prognosis and lower the risk of long-term hospitalization. Clinicians should familiarize themselves with common epidemiological risk factors, signs, and symptoms of gastrointestinal tuberculosis.
ABSTRACT #134
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
BRIDGING ASSESSING THE EFFICACY OF A POINT-OF-CARE ULTRASOUND CURRICULUM DELIVERED VIA A TWO-WEEK ELECTIVE
Errol C. Moras1, Keshav Dixit1, Kruti D. Gandhi1, Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: Point of care ultrasound (POCUS) is an invaluable tool that can facilitate rapid clinical decision- making, minimize costs, reduce procedural complications, and shorten hospital length of stay. Despite the benefits of POCUS, its use among internal medicine residents remains limited as there are no standardized methods for appropriate training within residency programs and there are few ultrasound experts able to oversee this education. This study aims to assess the efficacy of a POCUS elective within an Internal Medicine Residency Program.
METHODS: Starting in July 2023, we expanded and standardized a two-week POCUS elective based in a medical intensive care unit at a New York City hospital and offered it to any interested resident. Over the two weeks, resident learners completed pre-elective and post-elective surveys, a series of small group didactic sessions conducted by POCUS experts, extensive directly observed hands-on training, and image interpretation discussions. For the subsequent data analysis, we calculated effect size as the percentage of correct responses and used Statistical Package for the Social Sciences (SPSS), with a statistical significance level set at p≤0.05.
RESULTS: 28 residents participated in the elective over the first part of the academic year, with all of them completing the pre-elective survey, and 21 of them completing the post-elective survey. Resident learners reported increased comfortability with all variables assessed, with 100% of residents feeling comfortable with probe identification, adjustment of depth/gain, and lung views post-elective. The largest increase in comfortability was noted with abdominal views (7.4% pre-curriculum versus 95% post-curriculum), while deep vein thrombosis (DVT) assessment remained the most challenging. There were statistically significant improvements in many normal anatomical findings in basic cardiac, abdomen, and thoracic ultrasound. There were also statistically significant improvements in the identification of various pathologies: pericardial effusion (46% to 90%), right ventricular pressure overload (36% to 71%), absence of lung sliding via M-mode (7% to 76%), and presence of ascites (54% to 86%).
CONCLUSION: This study revealed that over the two-week elective, there were statistically significant improvements in comfortability of image acquisition and accurate interpretation of both normal and pathologic POCUS findings. This highlights the potential for a POCUS elective serving as foundational training for internal medicine residents interested in becoming POCUS experts. Additional studies are needed to see how well the resident learners retain these skills and information over time, and whether the implementation of a POCUS elective impacts clinical practice.
ABSTRACT #135
CLINICAL RESEARCH
CARDIOLOGY/PULMONARY/CRITICAL CARE
IMPACT OF CHRONIC OBSTRUCTIVE PULMONARY DISEASE ON OUTCOMES IN PATIENTS WITH TAKOTSUBO CARDIOMYOPATHY
Errol Moras1 , Kruti D. Gandhi1, Adlyn Moras2, Sidra Salman1 , Adam Rothman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Chronic obstructive pulmonary disease (COPD) is a known comorbidity of takotsubo cardiomyopathy (TCM). Many studies have found that TCM could be triggered by acute exacerbation of COPD, though the evidence of COPD affecting the outcomes of admitted TCM patients is lacking. We sought to assess the effect of COPD on hospitalized patients with a primary diagnosis of TCM.
METHODS: We conducted a retrospective cohort study in patients with a primary diagnosis of TCM with or without COPD using the latest National Inpatient Sample from 2016–2020. We analyzed patient characteristics, pre-procedural co-morbidities, and outcomes among the two groups. Outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: There were a total of 8138 hospitalizations for TCM, of which 21.4% had concurrent COPD. The COPD group had worse outcomes compared with the non-COPD group. This includes in-hospital mortality (2.4% versus 1.3%, p0.05), similar length of stay (LOS) (4 days versus 3 days, p=0.02), and higher hospitalization charges ($59,935 versus $52,595, p<0.001). Those with COPD had higher AKI (12.5% versus 10.5%), cardiogenic shock (6.1% versus 2.1%), and acute hypoxic respiratory failure (AHRF) (27.7% versus 9.4%). The rates of sudden cardiac death and ventricular arrythmias were similar between the two groups. Baseline comorbidities such as smoking, hypertension, diabetes, and chronic kidney disease were higher in those with COPD.
CONCLUSION: Patients with COPD who are hospitalized for TCM have higher rates of inpatient mortality, AHRF, cardiogenic shock, higher hospitalization costs but similar LOS as compared to those without COPD. Prospective studies are warranted to examine the effect of early intervention or treatment of COPD on shortand long-term outcomes of TCM.
ABSTRACT #136
CLINICAL RESEARCH
CARDIOLOGY/INFECTIOUS DISEASES
INCIDENCE AND PREDICTORS OF NEW-ONSET ATRIAL FIBRILLATION IN PATIENTS HOSPITALIZED WITH COVID19 INFECTION
Errol Moras1, Kruti D. Gandhi1, Adlyn Moras2 , Dave Mehta1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Father Muller’s College, Karnataka, India
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: COVID-19 infection has been associated with both an elevated incidence of myocardial injury, and an increased risk of thrombotic events such as venous thromboembolism and ischemic stroke. We performed a retrospective analysis of a large cohort of hospitalized patients afflicted with COVID-19 to assess the incidence, predictors, and outcomes of new onset atrial fibrillation (AF).
METHODS: This is a retrospective observational study involving index hospitalizations for COVID from the National Inpatient Sample (NIS), the largest all-payer public database of hospital care data in the United States. Our study sample included discharged adult patients (≥18 years) primarily hospitalized for COVID-19 using ICD10 codes. Confounders were adjusted using multivariable regression analysis.
RESULTS: A total of 331,808 patients were hospitalized with COVID-19 between March–December 2020. The incidence of AFib/AFL was 13.4% (n=44,292), among which 1.8% had developed new-onset Afib/AFL during the index hospitalization Overall Afib/AFL was associated with increased mortality (25.4% versus 14.6%, p<0.001), longer lengths of stay(10+3 days versus 7 days, p=0.005), higher hospitalisation costs (117k vs 99k, p<0.001) and higher odds of stroke (2.6% versus 1.3%; OR, 1.4; p<0.001). In a propensity matched sample multivariable logistic regression identified 3 factors significantly associated with increased incidence of new onset AF: presence of heart failure (OR, 2.2; p<0.001), valvular heart disease (OR, 4.3; p<0.001), HTN (OR, 1.6; p<0.001) and increased age >65 years. After adjusting for demographics, clinical comorbidities, and severity of disease, new onset AF was not significantly associated with higher in-hospital mortality (OR, 1.10; 95%CI, 0.99–1.23).
CONCLUSION: New-onset atrial fibrillation was common (1.7%) among patients hospitalized with COVID-19 infection. After multivariable adjustment for comorbidities and disease severity, new-onset atrial fibrillation was not statistically significantly associated with death, suggesting that new-onset atrial fibrillation in these patients may primarily be a marker of other adverse clinical factors rather than an independent driver of mortality
ABSTRACT #137
CLINICAL RESEARCH
CARDIOLOGY
TRENDS AND OUTCOMES
Errol Moras1 , Kruti D. Gandhi1, Adlyn Moras2, Sidra Salman1 , Adam Rothman1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Father Muller’s College, Karnataka, India; 3Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Systemic Sclerosis (SSc) is a chronic autoimmune disease characterized by vascular and immune dysfunction, leading to widespread fibrosis affecting multiple organ systems with cardiopulmonary complications being the most frequent cause of mortality. Arrythmias such as atrial fibrillation (AF) are the most frequent cardiac complications in patients with SSc, which is largely attributed to myocardial fibrosis. Although associated with high mortality and poor prognosis, there is limited data available on hospitalization outcomes for SSc patients with AF. We aim to determine the burden and outcomes of AF in patients with SSc
METHODS: We reviewed data from the National Inpatient Sample (NIS) database 2016-2020. ICD-10 codes were used to identify adult hospitalizations with AF as principal diagnosis, with and without SSc as secondary diagnosis. Outcomes were compared using univariate and multivariate logistic regression analysis.
RESULTS: From 2016-2020, a total of 4,253,349 hospitalizations were identified for AF, of which 5343 (0.1%) had SSc. The primary outcome of in-patient hospitality was 7.1% for those with SSc vs 4.9% for those without (p≤0.001). Atrial fibrillation with coexisting SSc hospitalizations had similar length of stay (LOS) (7 versus 6 days; p=0.34), but increased total hospitalization costs (THC) ($82,140 versus $71,698, p<0.005). Among patients hospitalized with AF with a secondary diagnosis of SSc, there was a significantly increased risk of congestive heart failure (OR, 1.2; 95%CI, 1.1-1.5; p<0.01), cardiogenic shock (OR, 1.4; 95%CI, 1.2-1.7; p<0.001), and venous thromboembolism (OR, 1.2; 95%CI, 1.1-1.3; p<0.001). The rates of stroke (OR, 1.2; 95%CI, 0.9-1.2; p=0.4) and cardiac arrest (OR, 1.0; 95%CI, 0.8-1.2; p=0.5) were similar among the two groups. While odds of undergoing catheter ablation (0.8% versus 0.7%) were similar among the two groups, there were higher odds of electrical cardioversion (OR, 2.3; p<0.001) in AF patients without SSc.
CONCLUSION: We found that patients hospitalized for AF with a secondary diagnosis of SSc have significantly increased inpatient mortality, congestive heart failure, cardiogenic shock, venous thromboembolism/blood clots, and THC. The rates of stroke and cardiac arrest were similar among the two groups. While odds of undergoing catheter ablation were similar among the two groups, there were higher odds of electrical cardioversion in AF patients without SSc
ABSTRACT #138
MEDICAL EDUCATION
GENERAL INTERNAL MEDICINE
BRIDGING THE GAP IN LGBTQ+ HEALTH TRAINING FOR INTERNAL MEDICINE RESIDENTS: A NEEDS ASSESSMENT OF A CURRICULUM DEVELOPMENT STUDY
Lenisse Reyes Reyes1, Sharel Sadud1, Tamar Reisman2, Helene Hedian3, Joel Grimaldo Ochoa1 , Brent Arcayan1, Tamara Goldberg1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Weill Cornell Medical Center, New York, NY, United States; 3Johns Hopkins University School of Medicine, Baltimore, MD, United States
Presented at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024 and to be presented at the Society of General Internal Medicine (SGIM) Annual Meeting that will be held in Boston, Massachusetts, United States from May 15-18, 2024.
BACKGROUND/INTRODUCTION: LGBTQ+ patients often experience significant health disparities due to various factors, including limited access to culturally competent care. Internal medicine residents play an essential role in delivering care to such patients; however, most feel unprepared [1-8]. While several initiatives have been introduced to address this gap over the last ten years, further research is needed to identify specific areas where such training should be focused. This study aims to analyze a needs assessment, as the initial phase in developing a comprehensive LGBTQ+ health curriculum for Internal Medicine residents. The second phase will implement and evaluate the curriculum, with results expected by Spring 2024.
METHODS: This anonymous online survey, developed and validated with LGBTQ+ health experts, assessed demographics, confidence levels, knowledge gaps, and preferred learning methods for multiple LGBTQ+ health topics.
RESULTS: During the initial phase, 39.8% (n=63) of residents completed the survey. 58.7% (n=37) were identified as senior residents. Among respondents, 50.8% (n=32) reported insufficient exposure to LGBTQ+ health education. Only 20.6% (n=13) of residents expressed high level of comfort in addressing the unique healthcare needs of LGBTQ+ patients. Remarkably, comfort scores did not differ across training levels (p>0.05). Participants reported greater comfort with general topics such as sexual health (68%) and pronoun use (54%) compared to more complex areas like gender-affirming hormone therapy (20%) and family/fertility planning (33%). The most frequently cited barriers to delivering optimal care to this population included; insufficient training (82.5%; n=52) and fear of appearing intrusive (61.9%; n=39). Furthermore, 73% (n=46) of residents cited online lectures as the preferred educational strategy for acquiring LGBTQ+ health knowledge.
CONCLUSION: Our survey analysis highlights a significant gap in self-reported comfort levels among internal medicine residents in delivering optimal LGBTQ+ care at a single program. Specific attention should be given to areas such as gender-affirming hormone therapy, fertility-related concerns, and promoting patient-centered communication training to address residents’ fear of appearing intrusive to LGBTQ+ patients. While we acknowledge the low survey response rate could be a potential confounder, our findings nevertheless support advocating for the integration of comprehensive LGBTQ+ health education into residency curricula.
ABSTRACT #139
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
CARDIOLOGY
DESMOPLAKIN CARDIOMYOPATHY-INDUCED RECURRENT PERIMYOCARDITIS
Sidra Salman1, Marni Wilkoff1, Kruti D. Gandhi1, Errol Moras1, James Salonia1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Mutations in the desmoplakin gene (DSP) result in bi-ventricular systolic dysfunction, fibrosis, arrhythmias, and can present as recurrent perimyocarditis. There is limited data available to guide effective therapy in preventing desmoplakin cardiomyopathy-induced recurrent perimyocarditis. We report the case of a young female with recurrent perimyocarditis and genetic testing concerning for desmoplakin cardiomyopathy.
CASE PRESENTATION: A 31-year-old female was diagnosed with recurrent perimyocarditis. She typically presented with chest pain, elevated troponins, and nonischemic EKGs showing QRS fractionation. Of note, her features were significant for woolly hair and calloused hands. Her family history was significant for a sister who was diagnosed with dilated bi-ventricular cardiomyopathy and ventricular arrhythmias with an EF of 40%, who passed from sudden cardiac death in her mid 30s. Genetic testing of the patient revealed desmoplakin variant of unknown significance, invoking concern for desmoplakin cardiomyopathy. Holter monitoring showed frequent PVCs. Cardiac MRI showed bi-ventricular dilation, circumferential subepicardial delayed gadolinium enhancement (LGE) with 13% scar burden, and an EF of 35%. She was treated intermittently with colchicine and pulse steroids. She received an implantable cardioverter-defibrillator (ICD) and was started on guideline directed medical therapy.
CONCLUSION: Desmoplakin is a structural protein that promotes intercellular adhesion within the cardiac myocardium allowing for normal force transmission, and regulates gap junctions to maintain electrical conduction. Mutations in the desmoplakin gene result in bi-ventricular systolic dysfunction (although often leftdominant), fibrosis, and arrhythmias, and can present as recurrent perimyocarditis. Desmoplakin gene is also involved in skin and hair integrity, thus, desmoplakin mutations can present classically with hypotrichosis and palmoplantar keratoderma, as seen in our patient. It has high clinical penetrance with significant risk of ventricular arrhythmias and sudden cardiac death. Left ventricular EF<55% and frequent PVCs are strong predictors of these adverse events. Majority of patients demonstrate late gadolinium enhancement of the left ventricular subepicardium. Although pulse steroids and immunosuppressants are often used, there is limited and conflicting data available to guide effective therapy in preventing recurrent perimyocarditis. Desmoplakin mutations can present with recurrent perimyocardial inflammation and subsequent fibrosis similar to other forms of myocarditis and inflammatory cardiomyopathies, presenting a diagnostic challenge. There is limited and conflicting data available to guide therapy, raising a need for further clinical studies.
ABSTRACT #140
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
FACTORS AFFECTING HOSPITAL LENGTH OF STAY AMONG PATIENTS HOSPITALIZED WITH ACUTE PULMONARY EMBOLISM
Jeeyune Bahk1, Abdul Rehman2 , Sidra Salman1, Venus Sharma1, Avinash Singh1, Hafiza Noor Ul Ain Baloch1,3 , David J. Steiger1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Rutgers New Jersey Medical School, Newark, NJ, United States; 3Mount Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Pulmonary embolism (PE) has an estimated population-based annual incidence of 70 per 100,000. Over the past two decades, hospitalizations for PE have steadily increased, accompanied by a commensurate rise in healthcare costs. We aimed to explore factors that influence the length of hospital stay (LOS) among patients hospitalized for acute PE.
METHODS: We performed a retrospective chart review of 209 patients with acute PE, who were admitted to one of three hospitals in the Mount Sinai Health System from 1/2020 to 9/2022, who were evaluated by the Pulmonary Embolism Response Team. Demographic, clinical, laboratory, and radiographic data were collected. Multivariate linear regression analysis was used to explore the effect of various factors on LOS.
RESULTS: Mean age of included patients was 62.9 (standard deviation [SD]: 16.8) years and 50.2% were women. White patients (55%) were more common than patients of other races (40.7% Black, 3.4% Asian, 0.9% others). PE was the admitting diagnosis in 90.4% of patients and was diagnosed in the emergency department in the majority (93.3%). PE was incidentally diagnosed in 4.3% of patients, while another 5.3% had hospitalacquired PE. The most common risk factors for PE were a prior history of venous thromboembolism (21.1%), active malignancy (18.2%), smoking (12%), and immobilization for >3 days (6.7%). The mean PESI score was 88.7 (SD: 30.2) points. Based on the European Society of Cardiology guidelines, 2.9%, 23.9%, 64.1% and 9.1% had low-risk, intermediate low-risk, intermediate high-risk, and high-risk PE respectively. Systemic thrombolysis was administered in6.2% of patients. Surgical embolectomyand catheter-directed embolectomy were performed in 18.7% and 8.1% of patients respectively. Median LOS was 6 (interquartile range: 3-10) days. The overall mortality rate was 11.5%. Based on multivariate regression analysis, an admission diagnosis of PE (regression coefficient: -89.8; p<0.001) and an incidental diagnosis of PE (regression coefficient: -79.1; p<0.001) were both strong negative predictors of LOS. Red cell distribution width at the time of diagnosis of PE (regression coefficient: +11.2; p<0.001) was a strong positive predictor of LOS. Moreover, the need for bridging anticoagulation (regression coefficient: +11.2; p<0.001) and surgicalembolectomy (regression coefficient: +18.8; p=0.02) were both weak positive predictors.
CONCLUSION: Red cell distribution width at the time of diagnosis of PE was found to be a strong positive predictor of LOS. Need for bridging anticoagulation and surgical embolectomy also were predictors of a longer LOS. Conversely, incidental diagnosis of PE or an admission diagnosis of PE were predictors of a shorter LOS.
ABSTRACT #141
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
IMPLEMENTATION OF A LONGITUDINAL PROCEDURAL CURRICULUM: WHAT EDUCATIONAL TOOLS IMPROVE PROCEDURAL PROFICIENCY WITHIN INTERNAL MEDICINE RESIDENCY PROGRAMS
Sidra Salman1 and James Salonia1 1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: We developed a procedure curriculum for Internal Medicine (IM) residents at the Mount Sinai Morningside-West Internal Medicine Residency Program, with the following objectives: familiarization with equipment, acquisition of required knowledge, and integration of skills through simulation and direct patient procedures. The purpose of this study is to assess which educational tools best improve procedural proficiency and whether learner-driven, website-based education followed by simulation would improve procedural training amongst trainees.
METHODS: For acquisition of knowledge, a website was developed which included modules for each core procedure: nasogastric intubation, arterial puncture, ultrasound-guided IV access, central and arterial line insertion, paracentesis, thoracentesis, and lumbar puncture. Each module contains an equipment checklist, and pertinent information including: indications, contraindications, complications, and instructional videos. For application of knowledge, residents were offered simulation sessions each dedicated to a different procedure, as well as a 2-week elective that offered direct patient procedures. A pre- and post-survey was utilized to measure the change in comfortability, certification rates, and knowledge level. Statistical significance was measured using chi-square analysis.
RESULTS: We received 35 responses (54.3% interns, 45.5% residents) on the pre-assessment and 32 responses (43.7% interns, 56.3% residents) on the post-assessment, with no statistical difference in ratio of interns to residents (p=0.38). 74.3% of housestaff felt the current procedure training at the program was insufficient, mostly due to lack of opportunities performing procedures (68.8%) and lack of knowledge (20%). 100% of housestaff felt the implemented curriculum improved procedural proficiency. Majority of housestaff felt the visual aids, step-by-step instruction, simulation practice, and diversity of educational tools specifically improved proficiency the most. Comfortability levels, measured using Likert-style scales, increased by 26.4% and 36% in procedural proficiency and sterile approach respectively. 42.9% of housestaff were not certified in any procedures pre-curriculum, whereas 100% of housestaff were certified in at least one procedure postcurriculum. Certification numbers increased by 53% in low skilled procedures (defined as nasogastric intubation, arterial puncture, and ultrasound-guided IV, with p<0.001), 47.9% in central lines (p<0.001), 31.4% in arterial lines (p<0.001), 32.3% in paracentesis (p<0.01), and 15.6% in lumbar puncture (p>0.01). On average 25.7%68.9% answered the procedural knowledge base questions correctly pre-curriculum, as compared to 42.9%89% post-curriculum with an average of 20-25% improvement in correct answers per question.
CONCLUSION: Given similar demographics with no statistical difference between the ratio of interns to residents,the increase in certification rates and knowledge level post-curriculum is independent of level of clinical experience. Our procedural curriculum resulted in significant improvement in comfort, knowledge, and certification rates among the various procedures expected during Internal Medicine Residency training.
ABSTRACT #142
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
RURAL SETTINGNOT ASSOCIATED WITH HIGHER RISK OF ADVANCED STAGEAT DIAGNOSISIN NONSMALL CELL LUNG CANCER
Sidra Salman1, Nadeem Bilani1, Rafael Arteta-Bulos2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Cleveland Clinic, Weston, FL, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Social determinants of health that have already been thoroughly investigated include race and insurance status. More work is still needed to understand what role, if any, geographic location plays in determining outcomes of patients with cancer. Current USPSTF guidelines recommend the use of an annual low-dose CT-scan to screen for lung cancer in patients older than 50 years of age with at least a 20 pack-year smoking history. We used a national registry to investigate for differences in stage at diagnosis in non-small cell lung cancer (NSCLC) by patient residential setting of urban versus rural.
METHODS: We retrospectively analyzed the National Cancer Database 2004-2016 dataset to identify factors associated with advanced stage at diagnosis in patients with non-small cell lung cancer usingmultivariate logistic regression modeling. ‘Early-stage’ NSCLC was defined as AJCC clinical staging of 0-II, while ‘advanced-stage’ NSCLC reflected diagnoses at AJCC clinical staging of III-IV. This model controlled for known social determinants of health, as well as clinical characteristics, significantly associated with stage at diagnosis, as identified by a review of literature.
RESULTS: This analysis included n=1,496,837 patients with NSCLC, of which 66.5% had been diagnosed at an advanced stage of disease. N=1,176,900 (81.6%) patients reside in metropolitan settings, versus n=232,736 (16.1%) and n=32,204 (2.2%) in urban and rural counties respectively. The majority of patients were White (n=1,279,086, 88.7%) while n=162,754 (11.3%) were Black. Significant predictors of a diagnosis at advanced stages of NSCLC included – but was not limited to – patient age, race, ethnicity, insurance status, histology, and tumor grade. Compared to patients diagnosed at ages <50 years, those diagnosed between 50-70 years (OR, 0.70; 95%CI, 0.68-0.72; p<0.001) and >70 years (OR, 0.65; 95%CI, 0.63-0.67; p<0.001) were less likely to have de novo advanced disease. Black patients were more likely to be diagnosed at advanced stages of NSCLC compared to White patients (OR, 1.37; 95%CI, 1.35-1.40; p<0.001). Residential setting (urban versus rural) was not a significant predictor of stage of diagnosis (p>0.05).
CONCLUSION: This retrospective analysis of a largeregistry showed that after controllingfor the effect of known confounders – including race, ethnicity, insurance status, tumor histology and grade – setting (urban versus rural) was not a significant predictor of diagnosis at advanced stages of non-small cell lung cancer
ABSTRACT #143
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
THE ASSOCIATION OF TEACHING STATUS ON INPATIENT MORTALITY AMONG CRITICALLY ILL PATIENTS WITH SEPSIS
Lorenzo Leys1,2 , Sidra Salman1, Sara Luby1, Deepanjali Radhkrishnan Nair1,2, Raymond A. Jean3 , Raymonde Jean1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3University of Michigan Health, Ann Arbor, MI, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: The organizational structure and operation of teaching hospitals differ from nonteaching hospitals, which leads to common differences to include, but are not limited to, cost, patient characteristics, resources and outcomes. This research aims to explore and understand the outcomes of sepsis, a common cause of in-hospital mortality, in critically ill patients, in teaching versus nonteaching hospital settings.
METHODS: The National Inpatient Sample between 2008 and 2017 was queried for all non-surgical discharges with a primary or secondary diagnosis of sepsis among patients aged 18 years or older, who were critically ill, requiring mechanical ventilation during their hospital stay. We compared inpatient mortality among patients who were treated at teaching hospitals to nonteaching hospitals. Adjusted logistic regressions were used to compare outcomes adjusting for age, sex, comorbidity, race, socioeconomic factors, and hospital factors.
RESULTS: There were 3,375,039 weighted discharges over the study period, of which 2,051,336 were admitted to teaching hospitals (60.8%). Overall, 46.4% of patients were female, and 62.5% were aged above 60 years old. Patient demographics and comorbidity profiles were similar between groups. Among all patients, the most common principal diagnoses were septicemia and respiratory failure (ICD-10 J96.X and ICD-9 518.X). There was a higher 2% unadjusted absolute mortality hospitals at teaching hospitals compared to nonteaching hospitals (41.0% versus 39.1%, p<0.0001). In the adjusted regression model, there was 17% increased odds of mortality at teaching hospitals (OR, 1.17; 95%CI, 1.15-1.19).
CONCLUSION: Although prior studies have shown a lower mortality for common conditions in teaching hospitals, our data demonstrate a consistently higher mortality at teaching hospitals among intubated, critically ill patients with sepsis. Though these differences may be mediated by higher severity of illness, these findings warrant further investigation to understand why these differences exist.
ABSTRACT #144
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
Ramnik K. Gill1, Ezana Bekele1 , Robinderpal Sandhu2, Meghaben Kothari1
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: DRESS syndrome is a systemic response to a drug, commonly leading to a rash, lymphocytosis and eosinophilia. We introduce the case of a patient, treated with a prolonged course of bactrim, who presented with gastrointestinal symptoms with associated transaminitis and eosinophilia with a negative hepatic work-up and the development of a rash with RegiSTAR score diagnostic for DRESS.
CASEPRESENTATION: The patient is a male who presented with nausea, abdominal pain, fever for onemonth, concerning for gastroenteritis. Initial labs pertinent for leukocytosis with elevated precursors, anemia, hepatocellular predominant transaminitis, direct hyperbilirubinemia. Upon further questioning, pt revealed that he recently finished a 21-day course of bactrim for a urinary tract infection. CTAP with no acute findings. Hospital course significant for development of diffuse papular rash, rising LFT and eosinophilia, which up-trended throughout his stay. Infectious and Hepatic work-up negative. HIDA scan negative for cystic duct obstruction. High concern for DILI (iso DRESS Syndrome) due to recent prolonged bactrim use and elevated eosinophils. RegiSCAR score 6. Pt started on high dose corticosteroids with significant improvement in labs and clinical symptoms, with eventual resolution of rash in less than 15 days.
CONCLUSION: DRESS syndrome is a severe drug reaction that involves organs, skin, lymph nodes often characterized by a rash, eosinophilia, and lymphocytosis. Oftentimes, there is a latency between symptom presentation and medication initiation, typically 2-8 weeks after the start of medication. DRESS occurs in .9 to 2 per 100,000 patients in a year. Antibiotics contribute to 74% cases of DRESS syndrome, 3% of which are caused by sulfonamides. Liver injury occurs in 53% of cases, often cholestatic abnormalities are seen (37%), then hepatocellular (19%), and lastly mixed. Skin findings are usually the first indication of a potential diagnosis, presenting as a maculopapular rash then progressing to coalescing erythema. Stopping the offending agent is often the first treatment modality, with systemic steroid administration as a subsequent treatment. Recovery can take up to 12 weeks. Our case described a patient who presented with nausea/abdominal pain, who recently completed a course of bactrim DS for a urinary tract infection and was found to have worsening transaminitis with labs pertinent for eosinophilia and late onset development of rash. Patient noted to have significant clinical and symptomatic improvement with the course of high dose steroids.
ABSTRACT #145
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
Ramnik K. Gill1 , Robinderpal Sandhu2 , Ezana Bekele1 , Meghaben Kothari1
1New York Presbyterian Brooklyn Methodist, Brooklyn, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: With the rise of immune checkpoint inhibitors in the treatment regimen of multiple malignancies, many lesser-known complications are unveiled, such as checkpoint inhibitor mediated hepatitis (3% incidence). Our case highlights the presentation, diagnosis and treatment of a patient with Nivolumab induced hepatitis.
CASE PRESENTATION: We present the case of a female with vulvar melanoma on nivolumab therapy (5 doses), admitted for elevated liver enzymes on outpatient labs. Hospital course was significant for fluctuating liver enzymes without the introduction of steroids. AST/ALT peaked at 531/369 respectively, Alk Phos peaked at 772 and Bilirubin peaked at 1.5. Hepatitis panel was negative, Immune panel positive for ANA IgG. RUQ US showed mild steatohepatitis. MRCP showed 2mm filling defect in the posterior wall of the gallbladder. Liver biopsy showed portal inflammation, bile duct injury/ductitis, lobular inflammation and scattered acidophil bodies thought to be due to drug mediated liver injury from checkpoint inhibitors. The patients hepatic function stabilized with cessation of checkpoint inhibitor, without the initiation of steroids.
CONCLUSION: Hepatotoxicity is a rare complication seen in ICI therapy. Nivolumab, a PD-1 inhibitor, is associated with a 3% incidence of LFT elevations in hepatocellular and/or cholestatic pattern. While many are asymptomatic, symptoms of nausea, cramping and diarrhea may occur. The diagnosis of ICI hepatotoxicity is clinical once other causes (infectious, autoimmune) have been excluded. Patients with Grade I hepatotoxicity (AST/ALT 1-3 x ULN, Bilirubin 1-1.5x ULN) require frequent monitoring of LFT while continuing the ICI. A liver biopsy can be considered in patients with Grade II hepatotoxicity (AST/ALT 3x - 5x ULN, Bilirubin 1.5x -3x ULN) or higher, who may require systemic glucocorticoid (prednisone 0.5 - 1 mg/kg/day with taper) or potential ICI discontinuation, with plans to resume once LFTs improve to Grade I Hepatitis. In addition, the initiation of glucocorticoid therapy is recommended in patients whose LFT do not resolve spontaneously or require a delay in ICI dosing. For Grade III and above, it is recommended to discontinue ICI and initiate 1-2mg/kg/day methylprednisolone with an eventual taper. If refractory to methylprednisolone, physicians can consider alternatives such as mycophenolate, tacrolimus, or azathioprine. Due to the increased use of ICI therapy, physicians should be aware of the diagnosis and management of ICI induced hepatotoxicity.
ABSTRACT #146
CLINICAL RESEARCH
GASTROENTEROLOGY
DEFINING A CLINICAL PHENOTYPE: A RETROSPECTIVE COMPARATIVE ANALYSIS OF PATIENTS WITH DISTAL ESOPHAGEAL SPASM AND NORMAL HIGH-RESOLUTION ESOPHAGEAL MANOMETRY
Emily S. Seltzer1, Kimberly Cavaliere1 , Robinderpal Sandhu1, Mantej Sehmbhi1,2, Kimberly Cavaliere1, Michael S. Smith1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Distal Esophageal Spasm (DES) is a rare and poorly understood disorder defined as at least 20% premature contractions on High Resolution esophageal Manometry (HRM) per Chicago Classification (CC). DES has a heterogeneous presentation and can be incidentally found on HRM. CC v4.0 stipulates that DES is clinically relevant only if patients present with dysphagia or chest pain. The association between DES and gastroesophageal reflux disease (GERD) is not fully established. This study aims to define a clinical phenotype of DES by examining clinical differences between DES and normal findings on HRM.
METHODS: A retrospective cohort study was conducted comparing subjects with DES, defined by CC v4.0, to subjects without any CC v3.0 or 4.0 motility disorder on HRM from 2/2020-12/2022. Patients with type III achalasia or prior foregut surgery were excluded. A diagnosis of GERD was defined as having Los Angeles Grade C/D esophagitis or Barrett’s on endoscopy, and/or a positive 24–48-hour reflux testing. To compare characteristics of DES to normal HRM subjects, descriptive and univariate analysis was used.
RESULTS: A total of 99 DES and 66 normal HRM subjects met inclusion criteria. DES patients were older (57.8 years, 52.2 years, p=0.023) and had a higher mean BMI (29.5, 26.3, p=0.001). Opiate use was similar between groups (8.6%, 6.1%, p=0.763). Proton Pump Inhibitors (PPIs) were commonly used in both groups (82%, 77%, p=0.49), though more patients with DES underwent reflux testing on PPIs (p<0.001). HRMs Among DES subjects, 75% underwent HRM as a prerequisite for GERD testing, and 14% had HRM to investigate dysphagia or chest pain. The presence of objectively diagnosed GERD did not differ among groups (47%, 56%, p=0.45). Normal HRM subjects more frequently had a positive symptom associated probability (42%, 21%, p=0.043). DES patients were not more likely to have hiatal hernias based on HRM, but when present, hernias were larger in size (2.5 cm, 1.8 cm, p=0.013).
CONCLUSION: A clinical phenotype for DES, distinct from that of patients with normal HRM, could not be identified. DES often is found incidentally in patients undergoing HRM for pre-GERD testing, though DES patients do not have a higher prevalence of GERD. The lack of a clear clinical phenotype validates CC v4.0 recommendations to consider an HRM DES diagnosis only in the context of clinical presentation. Prospective studies should be performed to elucidate the pathophysiology and treatment targets for DES patients.
ABSTRACT #147
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY
SAVING THE ESOPHAGUS FROM CAUSTIC INJURY: HOW SHOULD WE DO IT?
Jenny Dave1,2 , Emily S. Seltzer1, Kimberly Cavaliere2
1Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Caustic injury can cause significant damage to the upper gastrointestinal tract including stricture formation. Despite the severity of this condition, there are no comprehensive guidelines on acute and chronic stricture management. This leaves providers to trial and error, which may lead to further complications and need for an esophagectomy. We present a case of esophageal stricture formation and complications from caustic injury.
CASE PRESENTATION: A 24-year-old female presented to an outside hospital after ingesting paint stripper, bleach and Drano. CT-chest was without evidence of perforation. Within 24 hours she underwent EGD revealing Zargar classification Grade 2B/3A circumferential inflammation and focal necrosis of the esophagus and Grade 3A/3B necrosis and ulcerations in the stomach. A nasogastric tube (NGT) was placed and remained in place upon discharge for luminal patency. A J-tube was placed for nutrition. Her care was transferred to our institution three weeks later. She underwent repeat EGD 6 weeks after ingestion, revealing friable mucosa with two areas of benign-appearing stenosis in the mid and distal esophagus dilated with a Savary dilator to 35Fr, and removal of the NGT. Required serial dilations over the next four weeks with minimal improvement in stenosis. At 12 weeks, dilation was performed to 48Fr, resulting in an esophageal tear. CT-chest showed new pneumomediastinum and esophageal micro perforation. She was managed conservatively and repeat imaging showed resolution. She is planned for continued serial dilations.
CONCLUSION: This case highlights the challenges of stricture prevention and management from caustic injury. NGT placement may be helpful to ensure the patency of the esophageal lumen. However, it is also known to contribute to the development of long strictures and delay mucosal healing, thus it’s use is controversial. It is unclear if the NGT had help prevent or cause the refractory strictures in our patient. Additionally, the timing of when to perform repeat EGD to prevent and/or treat strictures is uncertain. It is thought that strictures typically develop 8 weeks after ingestion (De Lusong, 2013). Conversely, an expert review notes dilation is usually done at 3 weeks as scar tissue is completely formed after 8weeks (Methasate, 2018). There is a need for standardized guidelines to optimally manage caustic injury strictures. This may help prevent complications including perforation and possible esophagectomy when dilation outcomes are poor.
ABSTRACT #148
CLINICAL RESEARCH
GASTROENTEROLOGY
WHAT’S GERD GOT TO DO WITH DES: COMPARING CHARACTERISTICS OF REFLUX AND NONREFLUX PHENOTYPES OF DISTAL ESOPHAGEAL SPASM
Emily S. Seltzer1, Kimberly Cavaliere1, Robinderpal Sandhu1, Mantej Sehmbhi1,2 , Kimberly Cavaliere1, Michael S. Smith1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023.
BACKGROUND/INTRODUCTION: Distal esophageal spasm (DES) is a rare motility disorder characterized by ≥20% premature contractions (distal latency ≤ 4.5s) and a distal contractile integral of ≥450 mmHg·s·cm on highresolution manometry (HRM). Cardinal symptoms of DES include dysphagia and non-cardiac chest pain. Previous studies suggested a potential association between DES and gastroesophageal reflux disease (GERD) based on endoscopic findings or acid perfusion. However, the recommendation for DES management is to “optimize GERD treatment,” despite limited supporting data. This study aims to investigate symptomatic and manometric differences among DES patients with and without GERD on quantitative testing.
METHODS: A retrospective cohort study was conducted using HRM and reflux testing from 2/2020-12/2022. Exclusion criteria included type III achalasia or prior foregut surgery. Participants with DES on HRM were characterized by reflux testing results. The reflux DES group (R-DES) included individuals with endoscopic evidence of GERD (Los Angeles grade C/D esophagitis or Barrett’s) or elevated acid exposure on 24–48-hour pH testing. The non-reflux group (NR-DES) consisted of patients with normal 24–48-hour reflux testing. Descriptive and univariate analyses were performed comparing R-DES to NR-DES subjects.
RESULTS: A total of 99 eligible subjects with DES were identified, with 66 undergoing reflux testing and 2 with Barrett’s. The R-DES cohort included 32 subjects and NR-DES cohort had 36 subjects. Compared to NR-DES, R-DES subjects weighed more (mean BMI 30.33, 26.93, p=0.012). Both groups exhibited similar usage rates of proton pump inhibitors (78.1%, 91.7%, p=0.218) and chronic opioids (10%, 5.6%, p=0.652). No significant differences between groups were observed with respect to presenting symptoms (heartburn, regurgitation, abdominal pain, globus sensation, belching, nausea/vomiting, dysphagia, or chest pain) or HRM metrics (hiatal hernia size, basal LES pressure, residual LES pressure, or bolus clearance).
CONCLUSION: Despite the long-believed association between DES and GERD, this study demonstrates that DES patients with and without GERD do not exhibit phenotypic differences in symptom presentation or HRM metrics associated with GERD physiology. Based on this data, the role of GERD in DES has been overemphasized. To establish causation and assess the clinical significance of GERD, future studies should investigate potential differences in treatment response between DES patients with and without reflux.
ABSTRACT #149
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
COMPARISON OF OUTCOMES IN PATIENTS TRACHEOSTOMIZED AT DIFFERENT FIO2 SETTINGS
Jeeyune Bahk1, Bridget Dolan2 , Venus Sharma1, Mantej Sehmbhi1,2, Jennifer Y. Fung1, Young Im Lee2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023
BACKGROUND/INTRODUCTION: Current guidelines for the readiness for Spontaneous Breathing Trials (SBT) and the ability to be weaned off a ventilator includes oxygen saturation (SaO2)$89% on fraction of inspired oxygen (FiO2)40%. Our study compared outcomes of patients who underwent a tracheostomy at different FiO2 settings with the aim to facilitate optimal settings for a tracheostomy.
METHODS: We performed a retrospective observational cohort study of 604 consecutive tracheostomized patients hospitalized in an intensive care unit (ICU) within the Mount Sinai Health System between March 2020 to September 2021. We analyzed clinical characteristics and outcomes of patients who underwent a tracheostomy at FiO2 settings of 50% or <50%.
RESULTS: 221 patients were tracheostomized at FiO250% and 383 patients were tracheostomized at FiO2<50%. Both groups had a similar mean age (61.94 and 61.83 years), gender proportion (37.9% versus 32.6% females), and co-morbidities. At the time of tracheostomy, lower pH (7.41 versus 7.44, p<0.001), higher pCO2 (44.6 versus 38.3, p<0.001), and higher positive end-expiratory pressure (PEEP) (7.41 versus 5.48, p<0.001) were observed in the FiO250% group. Longer time from tracheostomy to first pressure support (3.03 days versus 1.67 days, p<0.001) and tracheostomy collar trials (9.37 days versus 5.11 days, p<0.001) were seen in the FiO250% group, but no difference were observed between time to speech valve placement and decannulation. There was no statistical difference in tracheostomy-associated complications between the two groups. Higher in-hospital mortality was seen in FiO250% group (46.6% versus 30.3%, p<0.001), but one-year mortality was similar between the two groups (29.9% versus 33.4%, p=0.417). More patients were discharged home from FiO2<50% group, compared to larger proportion of discharges to a longterm acute care hospital (LTACH) in the FiO250% group.
CONCLUSION: Despite tracheostomies being performed at higher ventilator settings than current guidelines, there was no observed difference in complication rates in the group tracheostomized at higher FiO2 settings compared to lower FiO2 settings. Patients tracheostomized at higher FiO2 settings demonstrated longer time to pressure support or tracheostomy collar trial and higher in-hospital mortality but had similar long-term outcomes of time to speech valve placement, decannulation, and lower one-year mortality.
ABSTRACT #150
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
IMPACT OF DIFFERENT ANTICOAGULATION STRATEGIES ON OUTCOMES IN PATIENTS HOSPITALIZED WITH ACUTE PULMONARY EMBOLISM
Jeeyune Bahk1, Abdul Rehman2 , Venus Sharma1, Sidra Salman1, Avinash Singh1 , Hafiza Noor Ulain Baloch1,3 , David J. Steiger1,3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Rutgers New Jersey Medical School, Newark, NJ, United States; 3Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Pulmonary embolism (PE) is the third most common acute cardiovascular disease with mortality rate of approximately 6.5%. Hospitalizations for PE represent a substantial cost burden with the mean cost per admission for acute PE approximating $37,000. We hypothesized that different anticoagulation (AC) strategies in acute PE may be associated with differences in overall patient outcomes. Our aim was to assess the impact of different AC strategies on length of stay (LOS), bleeding complications, and mortality.
METHODS: A retrospective chart review was performed of 209 patients with acute PE evaluated by the Pulmonary Embolism Response Team, admitted to one of three hospitals in the Mount Sinai Health System from 1/2020 to 9/2022. Demographic, clinical, laboratory, radiographic data, and AC therapies were collected. Linear and logistic regression models were applied to assess the impact of different variables on quantitative (LOS) and qualitative (mortality, bleeding and readmission) endpoints respectively.
RESULTS: 105 women and 104 men with a mean age of 62.9 years (standard deviation: 16.8) were included. The mean PESI score was 88.7 (SD: 30.2). Median LOS was 6 days (interquartile range: 3-10). Bleeding complications occurred in 17 (8.1%) patients, while the all-cause mortality rate was 11.5%. Most patients (n=158, 75.6%) were initially treated with intravenous unfractionated heparin (UFH). Of these, 70 were transitioned to low molecular weight heparin (LMWH), while another 69 were transitioned to a direct oral anticoagulant (DOAC). Among the 70 patients transitioned to LMWH from UFH, 42 were subsequently transitioned to a DOAC, 15 were transitioned to warfarin, while the remaining 13 patients were discharged on LMWH. Among patients treated with LMWH from the start (n=47), 37 were subsequently transitioned to a DOAC, while 2 were switched to warfarin. Another 5 patients were discharged on LMWH. In multivariate regression analysis, a strategy of UFH with transition to LMWH followed by warfarin was associated with a longer LOS (regression coefficient: 11.92; p=0.02). With respect to overall mortality, patients who were initially on UFH and subsequently discharged on LMWH (without being switched to oral anticoagulants) had increased 30-day mortality (odds ratio: 1.27, p=0.01). Risk of bleeding and readmission rates did not differ significantly among the various AC strategies.
CONCLUSION: Patients initially treated with UFH who were switched to LMWH followed by warfarin therapy had significantly longer LOS. The risk of bleeding complications or readmission rates were similar among the various AC strategies. However, patients who were started on UFH and discharged on LMWH had higher mortality.
ABSTRACT #151
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
INPATIENT UTILIZATION OF SEPSIS PATHWAY AND ITS IMPACT ON THE LENGTH OF STAY AMONG THE PATIENTS DIAGNOSED WITH SEPSIS, SEVERE SEPSIS, AND SEPTIC SHOCK
Venus Sharma1, Harrindra Seepersaud1 , Galit Balayla Rosemberg1, Sara Luby1, Hammad Sheikh1 , Connor Smith1, Lorenzo Leys1,2, James Salonia1, Rachael Schneider1, Raymonde Jean1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Sepsis affects 750,000 patients annually in the United States. It is a leading cause of death in critically ill patients in the hospital. This study explores the utilization/application of our sepsis pathway and its impact on in-hospital length of stay (LOS) among the patients diagnosed with sepsis, severe sepsis and septic shock.
METHODS: We performed a retrospective analysis of patients with sepsis, severe sepsis, and septic shock admitted to two major teaching hospitals in New York City from January 2022 to November 2022 comparing those that were placed on the Sepsis Pathway versus those not placed on the pathway. Multivariate binary logistic regression analysis was used to explore the association between the utilization of sepsis pathway and its impact on the LOS.
RESULTS: This cohort includes outcomes data on n=2,584 patients diagnosed with sepsis during their hospital stay. 1,520 of these patients were diagnosed with sepsis (58.8%), 554 patients were diagnosed with septic shock (21.4%), and 510 patients were diagnosed with severe sepsis (19.7%). Nearly half of the cohort was placed on the sepsis pathway during their admission (n=1,380; 53.4%). The severity of sepsis was significantly associated with the likelihood of being placed on the sepsis pathway (chi-squared p-value <0.001). 48.7% of patients with sepsis were placed on the pathway compared to 58.6% of patients with severe sepsis, and 61.6% of patients with septic shock. Patients with septic shock were 1.68 times more likely to be placed on the sepsis pathway compared to patients with sepsis (OR, 1.68; 95%CI, 1.38-2.06; p<0.001). There was a statistically significant association between placement on sepsis pathway and length of stay, with patients not placed on the pathway having longer LOS (mean length of stay 17.8 days compared to 14.9 days, independent t-test p-value <0.001).
CONCLUSION: The sepsis pathway is structured to act on sepsis alert in a timely manner and with appropriate reporting. This study concludes that placing patients on the sepsis pathway is associated with shorter hospital LOS. It was also concluded that patients with septic shock were more likely to be placed on the sepsis pathway compared to patients with sepsis.
ABSTRACT #152
CLINICAL RESEARCH
PULMONARY/CRITICAL CARE
INPATIENT UTILIZATION OF SEPSIS PATHWAY AND ITS IMPACT ON THE MORTALITY AMONG THE PATIENTS WITH SEPTIC SHOCK
Venus Sharma1, Harrindra Seepersaud1, Galit Balayla Rosemberg1, Sara Luby1, Hammad Sheikh1 , Connor Smith1, Lorenzo Leys1,2, James Salonia1, Rachael Schneider1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States
Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Sepsis remains the leading cause of mortality in critically ill patients. Nearly 750,000 patients are affected and 210,000 people die every year in the United States. Early identification along with prompt interventions improve outcomes. This study explores the application of sepsis pathway and its impact on mortality in septic shock patients.
METHODS: We performed a retrospective analysis of patients with septic shock admitted to two major teaching hospitals in New York City from January 2022 to November 2022, who were placed on sepsis pathway versus those who were not placed on sepsis pathway. Multivariate binary logistic regression analysis was used to explore the association between the utilization of sepsis pathway and its impact on mortality.
RESULTS: This cohort includes outcomes data on n=2584, patients diagnosed with sepsis during their hospital stay. 1,520 of these patients were diagnosed with sepsis (58.8%), followed by 554 patients who were diagnosed with septic shock (21.4%), followed by 510 patients who were diagnosed with severe sepsis (19.7%). Nearly half of the cohort was placed on the sepsis pathway during their admission (n=1,380; 53.4%). The severity of sepsis was significantly associated with the likelihood of being placed on the sepsis pathway (chi-squared p-value <0.001). 48.7% of patients with sepsis were placed on the pathway, compared to 58.6% of patients with severe sepsis, and 61.6% of patients with septic shock. Patients with septic shock were 1.68 times more likely to be placed on the sepsis pathway compared to patients with sepsis (OR, 1.68; 95%CI, 1.38-2.06; p<0.001). There is a statistical significance associated with placing the patients with septic shock on the sepsis pathway and mortality (46.8% versus 53.3%, independent t-test p=0.034).
CONCLUSION: The sepsis pathway is a structured tool that acts promptly on sepsis alert parameters, with appropriate reporting and tracking. Patients with septic shock are more likely to be placed on the sepsis pathway compared to patients with sepsis and severe sepsis. This study highlights the improved mortality benefits of this intervention tool in patients with sepsis. This outcome is likely the association with earlier intervention when this pathway is utilized.
ABSTRACT #153
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE INFECTIOUS DISEASES/PULMONARY/CRITICAL CARE
SYMPTOMATIC PRESENTATION OF MYCOBACTERIUM XENOPI IN A PATIENT WITH SCHAMBERG DISEASE
Venus Sharma1, Andrea Monfasani2, David J. Steiger1,2 , Christian D. Becker3, Nkechi Nwaoha3
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 3Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Chest Physicians (CHEST) Annual Meeting that was held in Honolulu, Hawaii, United States from October 8-11, 2023.
BACKGROUND/INTRODUCTION: Mycobacterium xenopi is a rare non-tuberculous Mycobacterium (NTM). Most patients infected with Mycobacterium xenopi have underlying lung disease, a history of immunosuppression or other co-morbidities. Here, we present a case of a 20-year-old female patient with Schamberg disease who presented for evaluation of lung nodules secondary to Mycobacterium xenopi.
CASE PRESENTATION: A 20-year-old female with a history of childhood asthma controlled on inhaled steroids, celiac disease and a recent diagnosis of Schamberg disease which manifested as purpura following a coronavirus vaccination, presented to Pulmonary clinic for the evaluation of lung nodules. She was initially evaluated at urgent care center three months prior for evaluation of chest pain and cough of one week duration. She was diagnosed with bronchitis and was treated with a short course of prednisone and azithromycin. A chest x-ray demonstrated lung nodules. Computed tomography (CT) scan revealed multiple bilateral parenchymal nodules, the largest measuring 1.3 x 1.8 centimeter in the left upper lobe with cavitation. Sputa were acid-fastbacilli (AFB) smear negative. Bronchoscopy was performed with bronchoalveolar lavage (BAL) in the left upper lobe and left lingula revealing macrophages with scattered lymphocytes and neutrophils. The BAL cultures were positive for Mycobacterium xenopi. She underwent video assisted thoracic surgery wedge resection of three left lung nodules. Biopsies revealed necrotizing granulomas without evidence of malignancy and fungal and AFB stains were negative. On her presentation to the Pulmonary clinic 3 months from the onset of illness, the patient reported daily clear phlegm production without fever, chills, cough, or hemoptysis. The patient described exposure to air from a home humidifying system and the use of a netti-pot with tap water. Physical examination was unremarkable, and there was no evidence of extra-pulmonary Mycobacterium xenopi infection. Sputum samples were sent, and a CT chest demonstrated stable scattered sub-centimeter solid pulmonary nodules. The patient was started on a three-drug regimen of moxifloxacin, rifampin, and ethambutol, and counselled on avoiding environmental sources of NTM. The patient is being evaluated for a possible underlying immunodeficient state.
CONCLUSION: Mycobacterium xenopi is a slow growing non-tuberculous mycobacterium. It can present as an acute infiltration in immunocompromised hosts, nodular disease in immunocompetent hosts and cavitary disease in the context of preexisting lung disease. The prognosis with drug treatment alone is unpredictable, and resection has been performed for focal disease refractory to medical treatment. We present a rare case of Mycobacterium xenopi which manifests as a nodular disease in immunocompetent patients. Decision was made to perform wedge resection as response with drug treatment is very unpredictable.
ABSTRACT #154
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
BRIDGING THE GAP BETWEEN SEPSIS AND POST SEPSIS SYNDROME
Hammad Sheikh1, James Salonia1, Susannah Kurtz1, Jacob Bell1, Ahmed Shaikh1, Nikita Desai1 , Priscilla Loanzon1 , Harrindra Seepersaud1, Amit Pradhan1 , Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented both at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024
BACKGROUND/INTRODUCTION: Sepsis is a global health problem and a major cause for hospital admission. Despite improvements in care, Sepsis cases and hospital admissions attributed to Sepsis continue to increase. Prompt recognition and delivery of high-quality care have improved Sepsis mortality but has resulted in a significant increase in Sepsis survivors who suffer from Post-Sepsis Syndrome. There are well established protocols and management strategies for Sepsis, but there is little information on how to minimize physical disability, cognitive impairment, or health deterioration after Sepsis and for Post-Sepsis Syndrome.
METHODS: The goal of our curriculum is to increase awareness of the diagnosis of Sepsis and Post-Sepsis management. Our curriculum will be composed of a didactic component focusing on basic physiology of Sepsis and Post-Sepsis Syndrome, a review of the Mount Sinai Health System Stop Sepsis Guidelines, and hands on training. These didactic sessions will be supervised by Critical Care faculty trained in the recognition and management of Sepsis. We will focus on major causes of Sepsis readmission, such as heart failure and pneumonia. Our upcoming novel simulation-based educational curriculum will improve recognition and management of patients with Sepsis and Post-Sepsis Syndrome. By incorporating a high-fidelity simulationbased case Residents will have a unique opportunity to practice and refine their skills. With our initial needs assessment, we recognized a gap in knowledge for Post Sepsis Care. Our project will have pre-assessment questions on Sepsis and Post-Sepsis Syndrome. We will then have focused objectives for education with didactics, implementing the Sepsis pathway, and a high-fidelity simulation training to improve Post-Sepsis management. Finally, administer post-assessments to evaluate the learners’ knowledge and behaviors.
RESULTS: Currently, we have completed a needs assessment. Our novel high-fidelity simulation-based case will begin in March at the Center for Advanced Medical Simulation (CAMS). Didactic lectures will be presented at Academic Half-Day this month. Pre and post assessments will include qualitative and quantitative metrics that will be presented during assigned CAMS session. Kirkpatrick model will be included when analyzing the effectiveness of our project. Finally, we plan to track metrics such as utilization of the Sepsis pathway, Sepsis length of stay, and Sepsis 30-day readmission.
CONCLUSION: Part of our goal as mentioned in Glassick’s criteria is to analyze and provide reflective critique. We recognize that we haven’t started our education and simulation case. We would like our outcomes to show that this project was not only feasible, but had a meaningful impact on education. Our limitations are we won’t be able to evaluate patient metrics at this time. But with our sessions quickly approaching we will hopefully evaluate the potential impact of our educational initiative with our defined metrics.
ABSTRACT #155
CLINICAL RESEARCH
INFECTIOUS DISEASES
CLINICAL OUTCOMES, EFFICACY, AND SAFETY OF OUTPATIENT PARENTERAL ANTIBIOTIC TERHAPY AT A TERTIARY MEDICAL CENTER IN NEW YORK CITY
Carolina Moreira Sarmiento1,2 , Connor Smith1, Galit Rosemberg1 , Valida Bajrovic1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Annual Mount Sinai Health System Department of Medicine Research Day that was held in New York, New York, United States on May 6-7, 2024.
BACKGROUND/INTRODUCTION: Outpatient Parenteral Antimicrobial Therapy (OPAT) was first described in 1974 in a pediatric cohort with cystic fibrosis for the treatment of bronchopulmonary infections; it has since become the standard of care for the administration of prolonged intravenous antibiotic therapy outside the hospital setting. The many benefits of OPAT include reducing hospital length of stay and nosocomial infections and improving patient comfort and satisfaction. Although OPAT programs are widely implemented, there is a paucity of data regarding OPAT outcomes in New York State. This study aims to determine the safety and efficacy of a NYC based OPAT program.
METHODS: A retrospective analysis was conducted using our electronic medical record system to identify all patients seen at the OPAT Clinic from May 1, 2018, to March 31, 2020. Filters included date and type of visit. Adults 18 years of age and older who received intravenous antibiotics as outpatients were included. This is a descriptive study that includes as primary outcomes: successful therapy completion, readmission rates, and complications related to antimicrobial therapy or vascular access. We also describe any secondary readmissions and the need to switch antibiotics. One limitation of this study is that it included only patients that attended their follow up appointment and were followed at the Mount Sinai System.
RESULTS: We collected preliminary data on 200 patients seen at the OPAT clinic. The most common infections were orthopedic infections 115 (57.5%) followed by skin and soft tissue infections 60 (30%), and bacteremia (30%) (Figure 1). Ceftriaxone was used in (38%), Vancomycin (27%) and Ertapenem (16%), however dual antibiotic therapy was also used in some cases. The main outcome was the successful completion of therapy in 195 (97.5%) cases. In total, 2.5% of patients did not complete treatment or were lost to follow-up. Only 10 (5%) of patients were readmitted within 60 days due to OPAT-related etiologies. Few patients experienced antibiotic related adverse events and the most common side effect was nephrotoxicity in 11 patients corresponding to 5.5% of this sample (Figure 3.) Vascular access related complications were rare and occurred in 6% of patients.
CONCLUSION: Our study shows that the implementation of OPAT in a NYC-based academic medical center was efficacious and safe with a similar rate of successful treatment compared to studies across the country. Most of our patients successfully completed treatment with few antibiotic- related adverse events or vascular access complications.
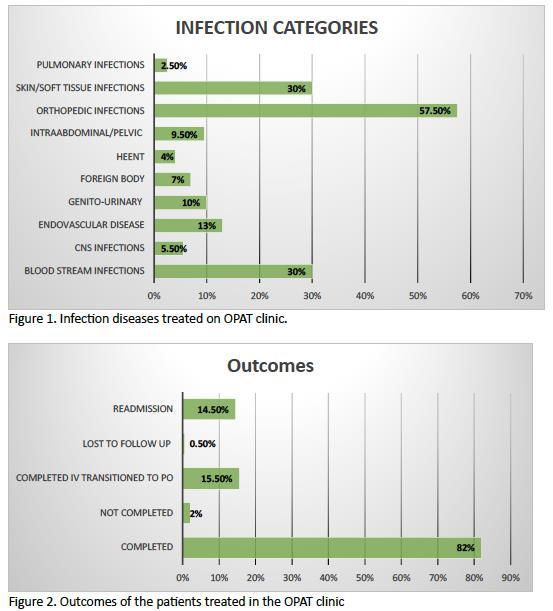

ABSTRACT #156
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
A NOVEL SIMULATION-BASED THORACIC POINT-OF-CARE ULTRASOUND CURRICULUM FOR INTERNAL MEDICINE RESIDENTS
Hua Hsin Tai1 , Harrinda Seepersaud1, Adam Rothman1,2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented both at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: To increase Internal Medicine residents’ confidence in recognizing common lung pathologies utilizing POCUS. In a small group setting, resident learners received a thirty-minute overview of thoracic ultrasound techniques and image recognition. They subsequently participated in a thirty-minute casebased simulation, where they evaluated a patient with sudden shortness of breath, and used POCUS to assist in formulating a diagnosis and treatment plan for the patient. The session was repeated over a six-week period in 2021, and then again over a six- week period in 2023.
METHODS: The study employed paired-sample t-tests and independent t-tests to analyze the pretest and posttest scores of 10 questions, assessing the alterations in learners’ POCUS identification. Residents (n=224) were asked to identify the following ultrasound findings: a-lines, air, b-lines, interstitial filling pattern, stratosphere sign, pneumothorax, pleural effusion, liver, diaphragm, and lung hepatization. The analysis was divided into two segments: one evaluating the overall effectiveness of the simulation session, and the other contrasting the 2023 and 2021 resident groups.
RESULTS: Across all years of training, and in both the 2021 and 2023 groups, there was a statistically significant difference when correctly identifying all ultrasound findings (p<0.05) following the intervention, suggesting an improvement in knowledge following the sessions. Subgroup analysis showed that the PGY-2 group improved in all test questions, while the PGY-3 group only improved in 3 of the 10 questions. The PGY-3 group overall had higher pretest scores, suggesting a higher baseline knowledge compared to other learners. Learners in 2023 overall had higher pretest scores compared to residents in 2021, with an overall mean pretest score of 0.7102 compared to 0.6878, and with further analysis specifically showing better recognition of pleural effusions (p<0.05). This suggests that the 2023 learners exhibited higher baseline thoracic ultrasound knowledge compared to their 2021 counterparts.
CONCLUSION: These findings highlight the immediate benefit that simulation-based POCUS curriculum has in improving resident learner knowledge on thoracic ultrasound. The higher pretest scores in 2023 suggests that the ongoing longitudinal curriculum has also resulted in improved long-term proficiency for POCUS topics among resident learners. Nevertheless, it is crucial to consider additional variables that might potentially impact these findings, such as distinct cohort characteristics or other modifications in the educational setting, and to conduct a more comprehensive statistical examination in order to arrive at a conclusive determination.
ABSTRACT #157
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PULMONARY/CRITICAL CARE
ACUTE HYPOXIC RESPIRATORY FAILURE FROM DAPTOMYCIN INDUCED EOSINOPHILIC
Vincent Torelli1, Raymonde E Jean1, Elena Tran2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2New York Presbyterian Brooklyn Methodist Hospital, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: With antibiotic resistance on the rise, daptomycin is being utilized with increasing frequency for treatment of methicillin-resistant Staphylococcus aureus (MRSA) infections thanks to its activity against gram-positive organisms. Acute eosinophilic pneumonia is a potentially serious yet rare adverse effect from daptomycin use, particularly in elderly adults receiving prolonged courses of daptomycin. We present a case of acute hypoxic respiratory failure due to daptomycin induced eosinophilic pneumonia requiring ICU admission.
CASE PRESENTATION: An 86-year-old female with hypertension, diabetes mellitus and history of left lower extremity cellulitis resulting in below the knee amputation was admitted for management of right lower extremity cellulitis complicated by septic joint arthritis. A 6-week course of daptomycin and ceftriaxone was recommended by Infectious Diseases consult team, followed by long-term suppressive therapy with trimethoprim and sulfamethoxazole. Following two weeks of the antibiotic regimen, a rapid response was called for worsening acute hypoxic respiratory failure with increasing high flow nasal cannula requirements despite aggressive diuresis. On physical examination, lung sounds were diminished bilaterally with diffuse crackles. Patient was newly disoriented from baseline, no longer following commands or conversational. Chest X-ray revealed worsening bilateral pulmonary opacifications most consistent with multifocal pneumonia. CT chest showed extensive bilateral pulmonary opacities, likely representing atypical pneumonia. She was admitted to the ICU with further increasing oxygen requirements on 45L HFNC FiO2 80%. Antibiotics were promptly changed to vancomycin and zosyn, and the patient was started on hydrocortisone 100mg twice daily for probable daptomycin-induced pulmonary toxicity. This patient was too unstable for bronchoscopy prior to starting steroids, however peripheral eosinophil count trended from 0.3% on admission to 7% prior to daptomycin cessation and steroid initiation. Following discontinuation of daptomycin, peripheral eosinophils trended down to 4.0% in the first 24 hours, and 0.25% within 48 hours. Patient’s symptoms almost immediately improved, with rapid improvement of mental status as well as oxygen requirement, and she was able to wean off HFNC to nasal cannula with eventual transfer to the general medical floors, where she completed her antibiotic course.
CONCLUSION: Given daptomycin’s efficacy towards MRSA infections, daptomycin-induced pulmonary toxicity will likely only become more prevalent. The average duration of daptomycin therapy upon onset of respiratory symptoms is roughly 3 weeks. With rapid identification and cessation, this patient was able to avoid further pulmonary complications. Clinicians should be aware of this complication and include daptomycin-induced eosinophilic pneumonia in their differential diagnosis in the appropriate clinical context.
ABSTRACT #158
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
PULMONARY/CRITICAL CARE
PROGRESSIVE
Vincent Torelli1, Raymonde E Jean1, Elena Tran2
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2New York Presbyterian Brooklyn Methodist Hospital, New York, NY, United States
To be presented at the American Thoracic Society (ATS) Annual Meeting that will be held in San Diego, California, United States from May 17-22, 2024.
BACKGROUND/INTRODUCTION: Silicosis is the most common occupational disease worldwide with an estimated 7,300 cases per year in the US from 1987-96. Presenting symptoms are non-specific including gradual onset dyspnea and mucus hypersecretion, most commonly following prolonged coal dust exposure. Treatment is limited to evidence from basic research given unavailability of diagnostic protocol despite clear, preventable etiology.
CASE PRESENTATION: An 83-year-old female presented following 5 days of dyspnea and exercise intolerance. Notably, she did not require oxygen prior to presentation. Vital signs notable for tachycardia, oxygen saturation (O2 sat) 91%, respiratory rate (RR) 19 breaths/min. Lung examination demonstrated bibasilar and diffuse right-sided crackles. Lab work notable for white blood cell count 16.9K, pH 7.35, pCO2 34, lactate 2.4. Chest X-ray revealed extensive accentuated markings in mid-lungs without pneumothorax/effusion. Upon transfer to ICU, she failed to improve despite aggressive diuresis and broad-spectrum antibiotics. Oxygen requirements rapidly progressed from 3 liters to 50 liters high flow nasal cannula (HFNC) over the next 24 hours. Patient developed new onset atrial fibrillation, O2 sat <89%, RR>35. On further questioning, she admitted to working as a jeweler since her early teens, filing diamonds for over 60 years. CT angiogram showed underlying pulmonary fibrosis, honeycombing of middle and superior lobes, however the patient was too unstable for bronchoscopy. Rheumatologic workup for autoimmune markers, respiratory and blood cultures, viral panel, and urine Legionella/Strep antigen were negative. She started solumedrol, ipratropium, and albuterol. Atrial fibrillation was controlled with beta-blockers, and an echocardiogram showed no evidence of underlying heart failure. Despite anti-inflammatory treatment, she continued to deteriorate, requiring HFNC 60L, FiO2 100% and eventually switched to BiPAP. The next steps included pulse dose steroids but the patient expired.
CONCLUSION: Interstitial lung disease due to silicosis currently lacks quality data on early diagnostic protocol and directed treatment, with in-hospital mortality estimated over 50% and median survival between 1-4 months. Data for treatment of interstitial lung disease is contained in cohort studies, lacking randomized controlled trials of substantial size and is mostly symptomatic. There are few large trials for bronchodilator or glucocorticoid use in silicosis, and the only data-proven management is to avoid exposure. When presentation of silicosis is nontypical, patients are offered limited treatment options. This patient lacked traditional insidious onset, and was healthy before admission. As other causes of acute hypoxic respiratory failure were ruled out, management of this case became difficult given lack of evidence-based options.
ABSTRACT #159
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE GASTROENTEROLOGY/HEMATOLOGY/ONCOLOGY
BURKITT LYMPHOMA INDUCED PSEUDOACHALASIA WITH DRAMATIC SYMPTOMATIC IMPROVEMENT POST-CHEMOTHERAPY*
Marni Wilkoff1, Emily Seltzer1, Allison Wang1,2, Bruno Costa1, Mohamed Rabie1, Bruce Gelman1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the American College of Gastroenterology (ACG) Annual Meeting that was held in Vancouver, British Columbia, Canada from October 20-25, 2023. *ACG Outstanding Poster Presentation
BACKGROUND/INTRODUCTION: Primary achalasia is due to loss of inhibitory neurons leading to poor relaxation of the lower esophageal sphincter and abnormal peristalsis. In pseudoachalasia, a similar radiographic pattern derives from a secondary etiology, most commonly a gastroesophageal junction (GEJ) adenocarcinoma, though cases of lymphoma-induced pseudoachalasia have been reported. Here we present the second known case of Burkitt lymphoma (BL)-induced pseudoachalasia.
CASE PRESENTATION: A 45-year-old African American female with a history of scleroderma, hypertension and gastroesophageal reflux disease presented to the Emergency Department for 15 episodes of diarrhea associated with fecal urgency, melena, poor oral intake, lightheadedness and weakness. She denied weight loss or bleeding from other sites. Initial labs were notable for microcytic anemia (hemoglobin 5.5 g/dL from an unknown baseline) and thrombocytopenia (platelet count 28 K/uL). Upper endoscopy revealed a large, fungating and ulcerated mass with spontaneous oozing in the esophagus, cardia, fundus and body of the stomach. Histology was consistent with BL (CD20, CD10, MYC and BCL6 positive; Ki67 index 95%). Upon discharge, the patient was scheduled to follow up with oncology, but was readmitted for a seizure. She was discharged and re-hospitalized for 4 days of vomiting and acute dysphagia to both solids and liquids. She had associated substernal globus sensation, food regurgitation within 2 minutes of consumption and a 28lb unintentional weight loss in 1 month. Barium esophagram demonstrated an aperistaltic esophagus with marked narrowing at the GEJ mimicking achalasia. Given the rapidly progressive and obstructive nature of the tumor, chemotherapy with rituximab, etoposide, prednisone, vincristine, cyclophosphamide, and doxorubicin (REPOCH) was promptly initiated. Prior to chemotherapy, the patient only tolerated a pureed diet, but upon completion of one cycle, tolerated a regular diet.
CONCLUSION: Accurate management of pseudoachalasia is crucial for symptomatic relief and patient survival. While adenocarcinomas of the gastroesophageal junction or cardia are the most common cause, lymphomainduced pseudoachalasia is well-recognized. Low-grade lymphomas account for most cases, and aggressive subtypes have been rarely reported. This is the second case of Burkitt lymphoma-induced pseudoachalasia reported in the literature and highlights the importance of accurate diagnosis and prompt treatment, with REPOCH being an effective regimen for inducing rapid responses.

Figure 1: Upper endoscopy revealing a large, fungating mass in the gastric cardia (A) and gastric fundus (B). Positive BCL6 (C) indicates germinal center origin, and c-Myc (D) demonstrates the presence of t(8;14) translocation which is hallmark of Burkitt Lymphoma. Barium esophagram demonstrates an aperistaltic esophagus with marked narrowing of the gastroesophageal junction (E).
ABSTRACT #160
MEDICAL EDUCATION
PULMONARY/CRITICAL CARE
DEVELOPMENT OF FREE, OPEN-ACCESS EDUCATIONAL TOOL TO FACILITATE NUTRITION LEARNING USING TAILORED CASE-BASED SCENARIOS: “NUTRI-BYTES”
Marni Wilkoff1, Samira Farouk2, David Thomas2, Priya Simoes1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented both at the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024
BACKGROUND/INTRODUCTION: Malnutrition and obesity are prevalent, however graduate and continuing medical education lack dedicated nutrition training. Case-based learning (CBL) tailors learning to specific scenarios and free open-access medical education (FOAMed) tools have revolutionized medical education. Online CBL modules are being used to supplement traditional didactics, but there are no open-access CBLs for nutrition training. “Nutri-Bytes” is an online case collection designed to teach pathophysiology and management of disease states with specialized nutritional requirements.
METHODS: We modeled Nutri-Bytes after NephSIM, an e-learning nephrology platform. We developed 10 interactive cases that teach nutrition assessment, pathophysiology, and specialized nutrition requirements. Each peer-reviewed case mimics a real patient encounter and includes a history, physical, diagnostic, and nutrition assessments, such as malnutrition screening and micro-nutrient deficiencies. Users build a differential diagnosis and are prompted to select the next best step with immediate feedback on response. A summary conclusion page describes steps to the final diagnosis and treatment plan, summarizes key take-away points, and highlights references, guidelines, and resources. Users are encouraged to complete a post-test and anonymous user survey upon completion. This curriculum is also linked to the Fellow’s Nutrition curriculum. Website usage including number of website views and case completion rate were analyzed. Two separate questionnaires including a post-test with 8 multiple choice questions assessing knowledge after completion of the modules, and an anonymous survey containing multiple-choice questions, Likert scale questions, and open comments to elicit users’ input on quality of infographics, explanations, and ease of use, were available on the website upon completion of the cases.
RESULTS: Since its launch one year ago, Nutri-Bytes has received 2,320 page views from 449 independent visitors (average of 5 views/visitor). Eleven users (11/449, 2.4% response rate) have taken the post-test, and the average number of questions correct was 6.5/8 (81%). 80% of users correctly answered all post-test questions and noted that the cases would change their clinical practice. Feedback was positive, with >90 % of users reporting that cases were interactive with appropriate level of difficulty and improved their knowledge.
CONCLUSION: Initial response is encouraging but 6/10 (60%) of respondents are gastroenterology fellows. While this is the intended audience, learners at all levels would benefit, thus a focus will be to improve reach at different levels. While there was increased engagement during the initial phase of launch, this has decreased in the last two months. We will proactively increase engagement on social media to increase the case completion rate and survey responses. Third, we have 10 cases and plan to release new cases monthly, with notifications to email subscribers and followers on social media.
ABSTRACT #161
MEDICAL EDUCATION
GASTROENTEROLOGY
THE EFFECTS OF ENDOSCOPY SIMULATION ON RESIDENT PHYSICIANS' CONFIDENCE AND KNOWLEDGE IN TREATING COMMON GASTROENTEROLOGY CONDITIONS
Marni Wilkoff1, Emily Seltzer1, Shabari Shenoy1, Daniela Jodorkovsky1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented both at the New York Society for Gastroenterology and Endoscopy Annual Meeting that was held in New York, New York, United States from December 14-15, 2023 and the Institute for Medical Education, Icahn School of Medicine at Mount Sinai Annual Meeting that was held in New York, New York, United States on April 16, 2024.
BACKGROUND/INTRODUCTION: Simulation has become a popular tool in medical education. As of 2011, 64 participating teaching hospitals utilized simulation for residents, and 61% used simulation for subspecialty training, with 31% of the hospitals having screen-based virtual reality simulation for gastroenterology (GI) endoscopic skills. The use of endoscopy simulation has been well studied in general surgery trainees and GI fellows, but there is limited data for its use in medical resident training. The purpose of this study is to determine if a hands-on high-fidelity. GI simulation improves internal medicine resident knowledge and confidence treating common GI conditions.
METHODS: Internal Medicine Residents at a single-site voluntarily participated in a didactic GI course which was offered in two formats: simulation plus lecture (SIM + lecture) or lecture-only. The 3D Systems GI MentorTM simulator was used to navigate virtual cases on colorectal cancer screening, esophagitis/Barrett’s esophagus, peptic ulcer disease (PUD), esophageal varices, and inflammatory bowel disease. Following each case, a brief didactic lecture was given to optimize retention of material. The lecture-only group received the same lecture via a 1-hour online video meeting. An identical post-intervention survey was distributed to all residents two weeks after completion of the session. A pre- and post-intervention REDCap survey was distributed. The survey captured post-graduate year (PGY), subjective confidence on a scale of 0-100, and nine objective multiple choice questions assessing knowledge in managing clinical scenarios. The pre- and post-intervention scores were analyzed using repeated measures ANOVA.
RESULTS: Eighteen residents signed up to participate in the study and 12 completed the intervention (66.7%). The overall mean confidence score significantly increased for participants in the SIM + lecture group (59.25 to 81.84) compared tothe lecture-only group (61.69 to 67.38, p=0.014). Therewas a statistically significant increase in confidence treating PUD in the SIM + lecture group (p-value=0.028). The average number of correct questions improved following both interventions, though was not statistically different between groups (p=0.196).
CONCLUSION: This pilot study demonstrated the feasibility of trainees to supplement their education using a GI virtual simulator. The use of simulation significantly increased trainee confidence managing common GI conditions over lecture format alone. All PGY-1s in the study chose the SIM + lecture group, potentially highlighting a target audience of this simulation-based education modality. Limitations include a small sample size, lack of randomization, and subjective nature of confidence scores. Results of this pilot study prompted development of a larger simulation curriculum, where all 150 residents in the residency program will learn to manage various conditions based on endoscopic findings.
ABSTRACT #162
CLINICAL RESEARCH
GASTROENTEROLOGY
USING QR CODE TECHNOLOGY TO IMPROVE GUIDELINE-DIRECTED CARE FOR ADMITTED PATIENTS WITH DECOMPENSATED CIRRHOSIS*
Randy Leibowitz1 , Marni Wilkoff1** , Swati Patel1**, Alexandria Markley1**, Ines Varela Knorr1**, Steven Rodriguez1,2, Frank Nelson1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States;
2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Digestive Disease Week Annual Meeting that will be held in Washington, D.C., United States from May 19-21, 2024.
*Selected for ACG Moderated Poster Session
**These authors contributed equally to this work.
BACKGROUND/INTRODUCTION: Current AASLD guidelines suggest all patients admitted with ascites should receive a diagnostic paracentesis within 24 hours of presentation to rule out spontaneous bacterial peritonitis (SBP). Early identification of SBP is imperative in preventing further clinical decompensation. The primary goal of our quality improvement study was to reduce the number of paracenteses not performed on admitted patients by 20% over a 3-month period.
METHODS: Medical records of patients admitted with decompensated cirrhosis were reviewed from two large metropolitan hospitals in New York City over 3 years. We designed a user-friendly workflow algorithm outlining the basic workup necessary for admitted patients presenting with ascites and discussed when to give prophylactic and empiric antibiotics for SBP. This algorithm was linked to a QR code and placed at multiple computer stations throughout both hospitals and was made accessible to Internal Medicine and Emergency Medicine providers (Image 1). Education sessions were provided to the house staff of Internal Medicine and Emergency Medicine to help emphasize how the workflow algorithm can aid in carrying out goal directed care. Emergency medicine engagement in our intervention began around the 3-month timepoint
RESULTS: Pre-intervention: A random sample of 342 patients admitted with ascites over a 3-year period was analyzed. Diagnostic paracentesis was not performed in 133/342 patients (38.80%). 129/342 patients (37.61%) had their paracentesis performed after 24 hours. The average time from admission to paracentesis was 1.44 days. Post-intervention: Following the implementation of our QR Code Algorithm, we reviewed charts of 40 patients admitted with ascites over a 3-month period Subsequently, 43 patients admitted with ascites between month’s 3-6 post-intervention were reviewed There was a 16.3% reduction in patients with paracentesis not performed at the 3-month point which was sustained through month 6 (Table 1) The amount of paracentesis which were delayed beyond 24 hours into admission saw its largest decrease (14.07%) between months 3 and 6 (Table 4). We saw a steady decrease in the average time from admission to paracentesis reaching 0.58 days between months 3-6. (Table 2). In total, the average time from admission to paracentesis over the 6-month study period decreased form 1.44 days to 0.81 days (Table 3).
CONCLUSION: Following the implementation of our QR code teaching algorithm, we saw a sustained improvement in each of our primary and secondary outcomes. Our hospitals average time from admission to paracentesis has improved to be within 24-hours following our intervention In effort to ensure we sustain this improvement, we are working on imbedding our algorithm into an order set accessible through our hospitals electronic medical record system.
Image 1: Example of educational flyer that was placed at Internal Medicine and Emergency Medicine provider computer stations. Follow QR code to see the ascites algorithm contained.

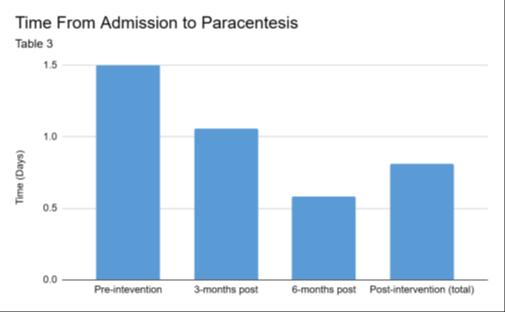
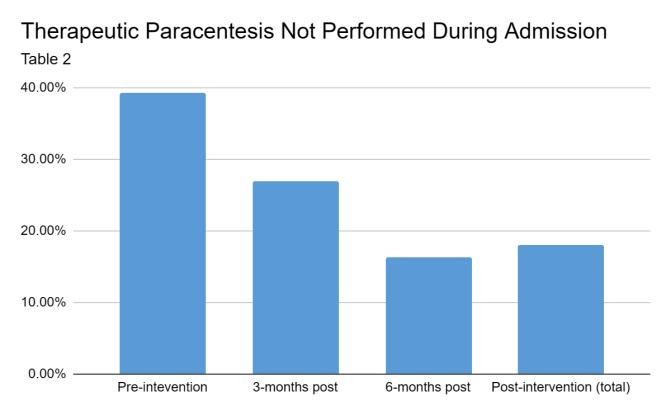

Tables 1-4 indicate our primary outcomes (Table 1) and our secondary outcomes (Tables 2-4) before implementing our QR Code, 3-months after our intervention, 6-months after our intervention and a combination of all admissions following initiation of our intervention.
ABSTRACT #163
CASE REPORT/CLINICAL REVIEW/CLINICAL VIGNETTE
INFECTIOUS DISEASES
DAPTOMYCIN-INDUCED EOSINOPHILIC PNEUMONIA
Agostina Velo1, Ilana Bandle1, Connor Welsh1, Idayat Brimah1,2, Edwardine Mirna Mohanraj1
1Mount Sinai Morningside-West Hospitals, Icahn School of Medicine at Mount Sinai, New York, NY, United States; 2Mount Sinai Beth Israel Hospital, Icahn School of Medicine at Mount Sinai, New York, NY, United States Presented at the Mount Sinai Health System’s Department of Medicine Annual Research Day that was held in New York, New York, United States from May 6-7, 2024.
BACKGROUND/INTRODUCTION: Daptomycin-induced eosinophilic pneumonia (DIEP) is a rare cause of acute hypoxic respiratory failure. Clinical presentation can be variable, making the diagnosis potentially elusive.
CASE PRESENTATION: A 70-year-old woman with diabetes mellitus, peripheral artery disease, and left calcaneal osteomyelitis on day thirty of treatment with daptomycin and cefepime, presented with confusion and fatigue. She had increased work of breathing, oxygen saturation of 88% on room air, bilateral basilar hypoventilation, and was febrile. Laboratory studies demonstrated eosinophilia (white blood count 16.4 K/uL, eosinophils 6%), and acute kidney injury. Chest x-ray revealed bilateral airspace opacities. Progression of respiratory distress, oliguric renal failure, and metabolic acidosis prompted escalation of care to the intensive care unit requiring high-flow nasal cannula (fraction of inspired oxygen 75%, flow of 40 liters/minute), a trial of diuresis with furosemide, and renal replacement therapy. Echocardiogram was normal. Despite therapy, pulmonary infiltrates progressed. This non-resolving, culture-negative pneumonia with eosinophilia raised suspicion of DIEP. Daptomycin had been stopped since admission. On day six, oral prednisone 40mg daily was started with rapid clinical improvement after one day (nasal cannula at 3 liters/minute), and resolution of eosinophilia and pulmonary infiltrates after three days.
CONCLUSION: DIEP is characterized by a combination of fever, dyspnea requiring oxygen supplementation or mechanical ventilation, new bilateral infiltrates, and BAL with >25% eosinophils in the setting of exposure to daptomycin, and with improvement after drug discontinuation. There are two notable features in this case. Often, discontinuing daptomycin may be sufficient, but therapy with steroids is often necessary for resolution. This was the case for our patient. Additionally, a bronchoalveolar lavage (BAL) was not obtained as the risk of empiric steroids was deemed less than the risk of bronchoscopy. In a review, 22 of 35 patients with reported DIEP had a BAL performed, and only 10 had a confirmatory eosinophilic count. Some authors propose that eosinophilia could be a surrogate. The mechanism of daptomycin-induced eosinophilic pneumonia remains unclear. The proposed pathophysiology suggests that antigens derived from the drug can activate alveolar macrophages, resulting in eotaxin and interleukin 5 release, causing eosinophils migration to the lungs. Daptomycin-induced eosinophilic pneumonia should be considered in the appropriate clinical setting, not necessitating a BAL for diagnosis, and should be treated with drug cessation and steroids.
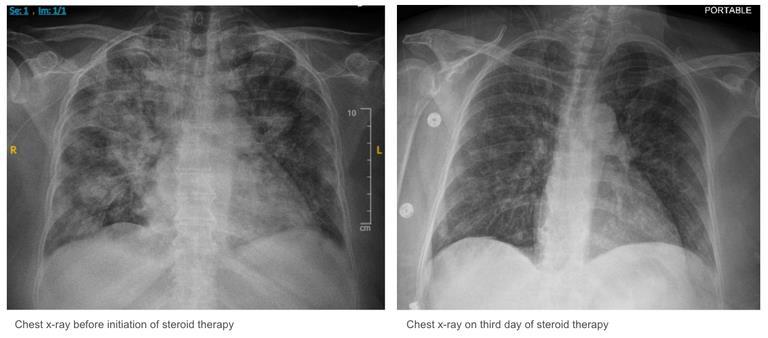
Figure 1. Chest x-rays with timeline of steroid therapy for daptomycin-induced eosinophilic pneumonia.
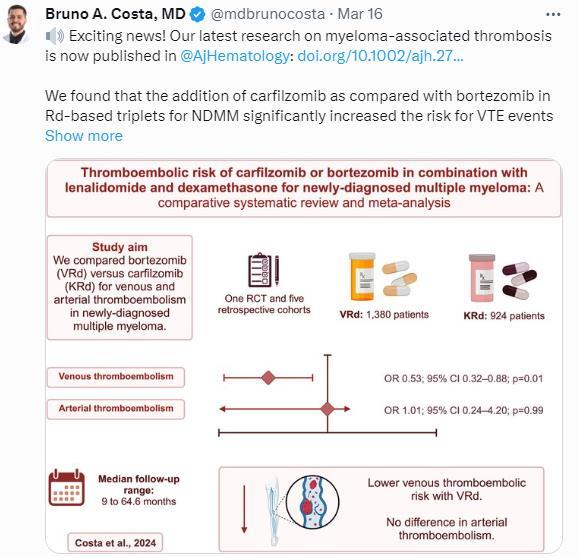
1
2
Jessica R. Leschied, Katherine E. Maturen, Maura Brown, Kate Hanneman, Julia H. Schoen, Beth Zigmund, Benjamin E. Northrup, Jonathan S. Gross, Priya Dave, Sean A. Woolen, Cameron Henry, Cody R. Quirk, Tarek A. Hijaz, Michael E. Zalis , John R. Scheel. “Letter to the Editor: Radiology Action for Climate Change.” Academic Radiology, 2023. PMID: 37230822
Beth Zigmund, Tarek Hijaz, Benjamin E Northrup, Julia H Schoen, Kate Hanneman, Maura Brown, Priya Dave, Jonathan S Gross, Cameron E Henry, Jessica R Leschied, Katherine E Maturen, Cody R Quirk, Sean A Woolen, Michael E Zalis, John R Scheel “Public Health Statement of the Association of University Radiologists Committee on Climate Change and Sustainability.” Academic Radiology, 2023. PMID: 37438160
3
4
Do Han Kim, Frank J. Lukens, Donghyun Ko, Paul T. Kröner, Miguel Salazar, Massimo Raimondo, Pedro Palacios Arguet. “Modified Bedside Index for severity in acute pancreatitis (BISAP) score validation in the national inpatient sample database.” Advances in Medical Sciences, 2023. PMID: 37329692
Ester Del Duca, Helen He, Ying Liu, Angel D. Pagan, Eden David, Julia Cheng, Britta Carroll, Yael Renert-Yuval, Jonathan Bar, Yeriel D Estrada, Catherine Maari, Etienne Saint-Cyr Proulx, James G Krueger, Robert Bissonnette, Emma Guttman-Yassky “Intrapatient comparison of atopic dermatitis skin transcriptome shows differences between tape-strips and biopsies.” Allergy, 2024. PMID: 37577841
5
6
Alessandro Spirito, Won-Joon Koh, Samantha Sartori, Birgit Vogel, Yihan Feng, Usman Baber, Johny Nicolas, Clayton Snyder, Karim Kamaleldin, Brunna Pileggi, Vahid Rezvanizadeh, Joseph Sweeny, Samin K Sharma, Annapoorna Kini, Stuart J Pocock, George Dangas, Roxana Mehran “Fatal, ischemic and bleeding risk of patients meeting the selection criteria of the TWILIGHT trial: Insights from a large PCI registry.” American Heart Journal, 2023. PMID: 37094668
Kruti D. Gandhi, Errol C. Moras, Shailesh Niroula, Persio D Lopez, Devika Aggarwal, Kirtipal Bhatia, Yoni Balboul, Joseph Daibes, Ashish Correa, Abel Casso Dominguez, Edo Y. Birati, David A. Baran, Gregory Serrao, Kiran Mahmood, Saraschandra Vallabhajosyula, Arieh Fox “Left Ventricular Unloading with Impella Versus IABP in Patients with VAECMO: A Systematic Review and Meta-Analysis ” American Journal of Cardiology, 2023 PMID: 37812867
7
8
Bruno Almeida Costa, Thomaz Alexandre Costa, Sara Diaz Saravia, Nicole Felix, Carlyn Rose Tan, Neha Korde, Joshua Richter. “Thromboembolic risk of carfilzomib or bortezomib in combination with lenalidomide and dexamethasone for newly diagnosed multiple myeloma: A comparative systematic review and meta-analysis.” American Journal of Hematology, 2024. PMID: 38488702
Bruno Almeida Costa, Ricardo J Ortiz, Alexander M Lesokhin, Joshua Richter. “Soluble B-cell maturation antigen in multiple myeloma.” American Journal of Hematology, 2024. PMID: 38270277
*Updated on April 28, 2024
Priya Dave, Olga R Brook, Alexander Brook, Ammar Sarwar, Bettina Siewert. “Moral Distress in Radiology: Frequency, Root Causes, and Countermeasures-Results of a National Survey.” American Journal of Roentgenology, 2023. PMID: 36946897
Errol C. Moras, J Dawn Abbott, Saraschandra Vallabhajosyula. “AABB recommends restrictive RBC transfusions for hospitalized adults and children.” Annals of Internal Medicine, 2024. PMID: 38316008
Maria Karim, Robert S Boikess, Robert A Schwartz, Philip J Cohen. “Dimethyl sulfoxide (DMSO): a solvent that may solve selected cutaneous clinical challenges.” Archives of Dermatological Research, 2023. PMID: 36459193
Luka Katic and Anamarija Priscan. “Multifaceted Roles of ALK Family Receptors and Augmentor Ligands in Health and Disease: A Comprehensive Review.” Biomolecules, 2023. PMID: 37892172
Yosef Joseph Rene Amel Riazat-Kesh, John Mascarenhas, Michal Bar-Natan. “Secondary acute lymphoblastic/lymphocytic leukemia done playing second fiddle.” Blood Review, 2023. PMID: 36894417
Thomaz Alexandre Costa, Nicole Felix, Bruno Almeida Costa, Amanda Godoi, Alleh Nogueira, Adriana Rossi. “Direct oral anticoagulants versus aspirin for primary thromboprophylaxis in patients with multiple myeloma undergoing outpatient therapy: A systematic review and updated meta-analysis.” British Journal of Hematology, 2024. PMID: 37533165
Christopher N. Matthews, Sidra Salman, Syed Farrukh Mustafa, Deepika Misra. “Cardiogenic and obstructive shock: Primary laryngeal synovial sarcoma with cardiac metastasis.” BMJ Case Reports, 2023. PMID: 38042527
Marita Yaghi, Nadeem Bilani, Barbara Dominguez, Maroun Bou Zerdan, Hong Li, Diana Saravia, Elizabeth Stone, Zeina Nahleh. “Efficacy of chemotherapy in patients with HR+/HER2-Invasive lobular breast cancer.” Cancer Treatment and Research Communications, 2023. PMID: 36525755
Errol C. Moras, Kruti D. Gandhi, Mohammad Khan, Adlyn Moras, James Choi, William H. Frishman, Wilbert S. Aronow. “Direct Oral Anticoagulants: An Overview of Indications, Pharmacokinetics, Comorbidities, and Perioperative Management.” Cardiology in Review, 2023. PMID: 37754756
Keshav Dixit and William H. Frishman. “Postural Tachycardia Syndrome and COVID-19: Focus on Ivabradine Therapy.” Cardiology in Review, 2024. PMID: 36729924
Ahmad Mustafa, Craig Basman, Michael P Cinelli, Ythan Goldberg, Denny Wang, Vidhi Patel, Arpanjeet Kaur, Priyanka Singh, Chapman Wei, Ethan Paliwoda, Arber Kodra, Luigi Pirelli, Shankar Thampi, Gregory Maniatis, Bruce Rutkin, Robert Kalimi, Elana Koss, Biana Trost, Azhar A Supariwala, Samuel Jacob Scheinerman, Chad A Kliger. “ Contemporary experience of mitral transcatheter edge-to-edge repair technology in patients with mitral annular calcification.” Catheterization and Cardiovascular Interventions, 2024.
PMID: 38436540
20
Errol Moras, Kruti Gandhi, Bharat Narasimhan, Ramon Brugada, Josep Brugada, Pedro Brugada, Chayakrit Krittanawong. “Genetic and Molecular Mechanisms in Brugada Syndrome.” Cells, 2023. PMID: 37443825
Benjamin O. Adegbite, Matthew H Abramson, Victoria Gutgarts, Florin M Musteata, Kinsuk Chauhan, Alecia N Muwonge, Kristin A Meliambro, Steven P Salvatore, Sebastian El Ghaity-Beckley, Marina Kremyanskaya, Bridget Marcellino, John O Mascarenhas, Kirk N Campbell, Lili Chan, Steven G Coca, Ellin M Berman, Edgar A Jaimes, Evren U Azeloglu. “Patient-Specific Pharmacokinetics and Dasatinib Nephrotoxicity.” Clinical Journal of the American Society of Nephrology, 2023.
PMID: 37382967
Nadeem Bilani, Mira Itani, Leah Soweid, Sindu Iska, Tais Bertasi, Raphael Bertasi, Marita Yaghi, Mohamed Mohanna, Barbara Dominguez, Diana Saravia, Evan Alley, Zeina Nahleh, Rafael Arteta-Bulos. “Geographic Origin may Affect Outcomes for Hispanic Patients with Non-Small Cell Lung Cancer in the United States.” Clinical Lung Cancer, 2023. PMID: 37271715
John Kiel, Andres I. Applewhite, Tais G. O. Bertasi, Raphael A. O. Bertasi, LaRae L. Seeman, Lorena M. C. Costa, Haytham Helmi, George G. A. Pujalte. “Ketorolac Injections for Musculoskeletal Conditions: A Narrative Review.” Clinical Medicine and Research, 2024. PMID: 38609144
Norah Layla Sadek, Bruno Almeida Costa, Karthik Nath, Sham Mailankody. “CAR T-Cell Therapy for Multiple Myeloma: A Clinical Practice-Oriented Review.” Clinical Pharmacology and Therapeutics, 2023. PMID: 37750399
Jeeyune Bahk, Bridget Dolan, Venus Sharma, Mantej Sehmbhi, Jennifer Y Fung, Young Im Lee. “Characteristics and Outcomes of Tracheostomized Patients with and without COVID-19.” Critical Care Explorations, 2023. PMID: 37546230
Bruno Almeida Costa, Tarek H. Mouhieddine, Ricardo J. Ortiz, Joshua Richter. “Revisiting the role of alkylating agents in multiple myeloma: Up-to-date evidence and future perspectives.” Critical Reviews in Oncology/Hematology, 2023. PMID: 37244325
*Updated on April 28, 2024
27
Harrison R Jordan, Sidharth Sahni, Mamun M, Ahmed, Joseph E Fares, Binoy V. Desai, Christine N. Lenchur, Richard T Jermyn.” A Comprehensive Literature Review of Digital Health Interventions in the Treatment of Substance Use Disorder with Special Focus on Mobile Applications.” Cureus, 2024. PMID: 38021738 28
Kevin Do, Alan A Zakaria, Tais Garcia de Oliveira Bertasi, Raphael Adroaldo de Oliveira Bertasi, Rock P Vomer, Jeffrey Nadwodny, George G A Pujalte. “A Schatzker Type III Tibial Plateau Fracture in a Soccer Player.” Cureus, 2024. PMID: 37593268
29
30
31
32
Thomas F. Fusillo, Scott Millman, Kamal Menghrajani. “Acute Myeloid Leukemia Presenting as Common Colds: An Uncommon Consideration.”Cureus, 2024. PMID: 38425594
Thomas F. Fusillo and Michael Nguyen, “Bilateral Avascular Necrosis of the Femoral Heads Secondary to Familial Hyperlipidemia.”Cureus, 2024. PMID: 37814725
Alexander Maraveyas, “Rare Gastric Diverticulum Mimicking Adrenal Abscess on Computed Tomography.” Cureus, 2024. PMID: 38586689
Artemii Lazarev, Sahil Nath, Christine Q Nguyen, Anna M Demian, Raphael Adroaldo de Oliveira Bertasi, Tais Garcia de Oliveira Bertasi, George G A Pujalte. “Sports and Weight Control in Children.” Cureus, 2024. PMID: 38455821
Matthew K. Lunser, Mark Friedrich Hurdle, Walter C. Taylor, Raphael Adroaldo de Oliveira Bertasi, Tais Garcia de Oliveira Bertasi, Svetlana Kurklinsky, George M Cooper, Hillary W. Garner, Haytham Helmi, George G A Pujalte. “Ultrasound Measurement of Femoral Articular Cartilage Thickness Before and After Marathon Running.” Cureus, 2024. PMID: 38406107
Errol Moras, Mohammad Ishrak Khan, David D. Song, Moinuddin Syed, Sivaguha Yadunath Prabhakaran, Kruti D. Gandhi, Carl J. Lavie, Mahboob Alam, Raman Sharma, Chayakrit Krittanawong. “Pharmacotherapy and revascularization strategies of peripheral artery disease.” Current problems in Cardiology, 2024. PMID: 38309544
Maria Karim, Elizabeth J. Klein, Ambika Nohria, Dolly Taiwo, Prince Adotama, David Cohen, Jerry Shapiro, Emily Milam, Kristen Lo Sicco. “Potential for Allergic Contact Dermatitis in Popular Hair Care Practices and Ingredients.” Dermatitis, 2023. PMID: 37339433
Catherine B. Stroud, Frances R. Chen, Erin E. Dunning, Julia Cheng, Carey Marr, Suzanne Vrshek-Schallhorn. “Early adversity and depressive symptoms among early adolescent girls: the mediating role of exposure to recent interpersonal acute stress.” Development and Psychopathology, 2023. PMID: 34743768
Joseph A. Menand, Robinderpal Sandhu, Yonatan Israel, Emma Reford, Ahmun Zafar, Priyanka Singh, Kimberly Cavaliere, Jean Saleh, Michael S Smith, Daniela Jodorkovsky, Yuying Luo. “Digital Rectal Exams Are Infrequently Performed Prior to Anorectal Manometry.” Digestive Diseases and Sciences, 2024. PMID: 38170338
Donghyun Ko, Frank J Lukens, Do Han Kim, Miguel Salazar, Paul T Kroner, Massimo Raimondo, Pedro Palacios Argueta. “Patients with chronic pancreatitis have increased mortality when admitted for vaccine preventable diseases.” Digestive and Liver Disease, 2023. PMID: 37098455 39
42
43
44
on April 28, 2024 37
Bharat Narasimhan, Kruti D. Gandhi, Errol C. Moras, Lingling Wu, Akanibo Da Wariboko, Wilbert Aronow. “Experimental drugs for supraventricular tachycardia: An analysis of early phase clinical trials.” Expert Opinion on Investigational Drugs, 2023. PMID: 37728554
Sruthi Ranganathan, Edward Christopher Dee, Neha Debnath, Tej A. Patel, Bhav Jain, Vedang Murthy. “Access and barriers to genomic classifiers for breast cancer and prostate cancer in India.” International Journal of Cancer, 2024. PMID: 37962056
Ariana Ringer, Andrea María Smichowski, Ramiro Gómez, Belén Virasoro, Liliana Martínez, Emmanuel Bertiller, Carlos Siegrist, Brian Abdala, Serenela Chulibert, German Grossi, Eduardo Rubín, Alex Kostianovsky, Sebastián Andrés Muñoz, Sophia Lutgen, Ignacio Javier Gandino; Study Working Group of Rheumatological Ocular Diseases, Argentinian Society of Rheumatology. “Ocular cicatricial pemphigoid: is there an association with autoimmune diseases?” International Ophthalmology, 2024.
PMID: 38376602
Aiden Lui, Eric Feldstein, Kevin Clare, Alis J. Dicpinigaitis, Medha Reddy, Farzana Khan, Rosa Semaan, Daniela Galluzzo, Steve Shapiro, Haris Kamal, Shadi Yaghi, Jared Pisapia, Carrie Muh, Rolla Nuoman, Philip Overby, Mill Etienne, Ji Chong, Stephan Mayer, Chirag D. Gandhi, Fawaz Al-Mufti. “Acute ischemic strokes in patients with developmental disabilities: A cross-sectional analysis.” Interventional Neuroradiology, 2023.
PMID: 35786031
David A. Sanchez, Ashley Sang Eun Lee, Karina Rotella, Andrew Eng, Charlotte Cunningham-Rundles. “Social Determinants of Health Impacting Diagnosis and Management of Primary Immunodeficiencies: A Case Series.” Journal of Allergy and Clinical Immunology, 2024. PMID: 38061547
Kirtipal Bhatia, Basera Sabharwal, Kartik Gupta, Persio D. Lopez, Arpanjeet Kaur, Harsimran K. Bhatia, Kruti D. Gandhi, Shailesh Niroula, Ashish Correa, Edo Y. Birati, Edgar Argulian, Arieh Fox, Kiran Mahmood. “Clinical outcomes of intravenous iron therapy in patients with heart failure and iron deficiency: Meta-analysis and trial sequential analysis of randomized clinical trials.” Journal of Cardiology, 2023. PMID: 37380069
45
46
Carli D Needle, Elizabeth J Klein, Jessica Gjonaj, Ambika Nohria, Maria Karim, Lynn Liu, Jinal Shah, Rebecca A Betensky, Michael Garshick, Kristen Lo Sicco, Theodora K Karagounis. “Comparison of comorbidities and adverse events in dermatology and rheumatology patients prescribed tofacitinib: A retrospective analysis.” Journal of the American Academy of Dermatology, 2024. PMID: 38008410
Dylan J Rust, Bradley D. Kwinta, Larisa J Geskin, Faramarz H Samie, Fabrizio Remotti, Sam S Yoon. “Surgical management of dermatofibrosarcoma protuberans.” Journal of Surgical Oncology, 2023. PMID: 36999599
47
48
Madeline Kim, Ester Del Duca, Julia Cheng, Britta Carroll, Paola Facheris, Yeriel Estrada, Amy Cha, John Werth, Robert Bissonnette, Karl Nocka, Chuanbo Zang, Ana B Pavel, Emma Guttman-Yassky. “Crisaborole reverses dysregulation of the mild to moderate atopic dermatitis proteome toward nonlesional and normal skin.” Journal of the American Academy of Dermatology, 2024. PMID: 37054814
Michael G Buontempo, Christina S Oh, Lina Alhanshali, Elizabeth J Klein, Maria Karim, Jerry Shapiro, Kristen Lo Sicco. “Evaluating subjective versus objective measures of changes in hair density using standardized scalp photography.” Journal of the American Academy of Dermatology, 2024. PMID: 37775047
49
Jacob L. Thomas, Kristina Navrazhina, Kalee Shah, Tzippy Shochat, Kira Minkis. “The anatomic region impacts the duration of action of ropivacaine during dermatologic surgery.” Journal of the American Academy of Dermatology, 2023. PMID: 37394141
50
51
Celine M. Schreidah, Lauren M. Fahmy, Brigit A. Lapolla, Emily R. Gordon, Bradley D. Kwinta, Larisa J. Geskin. “Accessibility and readability of online patient education on cutaneous lymphomas.” Journal of the American Academy of Dermatology International, 2024. PMID: 37727629
Errol C. Moras, Kruti D. Gandhi, Anoop N. Koshy, Kirtipal Bhatia, Chayakrit Krittanawong, Abel Casso Dominguez, Edgar Argulian, Gregg W. Stone. “Mitral Transcatheter Edge-to-Edge Repair in Patients with Atrial Functional Mitral Regurgitation.” Journal of the American College of Cardiology, 2024. PMID: 38538205
52
53
Arpanjeet Kaur, Arshdeep S. Dhaliwal, Sumit Sohal, Yeongjin Gwon, Soumya Gupta, Kirtipal Bhatia, Abel Casso Dominguez, Craig Basman, Jacqueline Tamis-Holland. “Role of Cerebral Embolic Protection Devices in Patients Undergoing Transcatheter Aortic Valve Replacement: An Updated Meta-Analysis.” Journal of the American Heart Association, 2024. PMID: 38240252
Vinay Rao, Ishaan Dharia, Jessica Gibilisco, Danielle Kirelik, Scott Baumgartner, Katherine Negreira, Karan Chawla, Jenny Dave, Samuel Kallus, Omar Ali Belfaqeeh, Marie L. Borum. “Delay in prior authorization of biologic therapy: Another possible cause of healthcare disparity in IBD patients.” Journal of the National Medical Association, 2024. PMID: 38036315
*Updated on April 28, 2024
54
Margaret Chou, Maria Karim, Joshua Josephs, Tamar Itzkowitz, Margaret R Dreker, Jessica G Labadie. “Pulsed dye laser and adjuvant topical therapies for the treatment of port-wine stains: A systematic review.” Lasers in Surgery and Medicine, 2024
PMID: 37431532
55
56
Emily R Gordon, Bradley D. Kwinta, Celine M Schreidah, Lauren M Fahmy, Oluwaseyi Adeuyan, Dawn Queen, Megan H Trager, Cynthia M Magro, Larisa J Geskin “Cutaneous lymphoproliferative disorders after COVID-19 vaccination: clinical presentation, histopathology, and outcomes.” Leukemia and Lymphoma, 2024. PMID: 37861685
Karthik Nath, Bruno Almeida Costa, Sham Mailankody. “GPRC5D as a novel immunotherapeutic target in multiple myeloma.” Nature Reviews. Clinical Oncology, 2023.
PMID: 36725915
57
58
Mariel L. Schroeder, Arefeh Sherafati, Rachel L. Ulbrich, Muriah D. Wheelock, Alexandra M Svoboda, Emma D. Klein, Tessa G George, Kalyan Tripathy, Joseph P Culver, Adam T Eggebrecht “Mapping cortical activations underlying covert and overt language production using high-density diffuse optical tomography.” Neuroimage, 2023.
PMID: 37245559
Nadeem Bilani, Rima Patel, Fionnuala Crowley, Amy Tiersten. “Outcomes in Premenopausal Patients with HR+/HER2- Breast Cancer and Lymph Node Micrometastasis Based on the 21-Gene Recurrence Score.” Oncologist, 2023.
PMID: 37682780
Bruno Almeida Costa, Paulino Tallón de Lara, Wungki Park, Fergus Keane, James J. Harding, Danny N. Khali. “Durable Response after Olaparib Treatment for Perihilar Cholangiocarcinoma with Germline BRCA2 Mutation.” Oncology Research and Treatment, 2023. PMID: 36882017
Sydney Katz, Iris Insogna, Courtney Tomblinson, Priya Dave, Shanna A. Matalon. “Supporting Physicians through Infertility and Assisted Reproductive Technology.” Radiographics, 2024. PMID: 38206832
61
62
Alexander Lesokhin, Karthik Nath, Tala Shekarkhand, David Nemirovsky, Andriy Derkach, Bruno Almeida Costa, Noriko Nishimura, Tasmin Farzana, Colin Rueda, David Chung, Heather Landau, Oscar Lahoud, Michael Scordo, Gunjan Shah, Hani Hassoun, Kylee Maclachlan, Neha Korde, Urvi Shah, Carlyn Rose Tan, Malin Hultcrantz, Sergio Giralt, Saad Usmani, Zainab Shahid, Sham Mailankody. “Comparison of Infectious Complications with BCMA-directed Therapies in Multiple Myeloma.” Research Square, 2024. 424897PMID: 38405866
Bertin D. Salguero, Sidra Salman, Abhinav Agrawal, Christian M. Lo Cascio, Greta Joy, Udit Chaddha. “Evaluating the safety of intraprocedural chest tube removal during medical thoracoscopy.” Respiratory Medicine, 2024. PMID: 38331227
*Updated on April 28, 2024
63
64
Austin M Looney, Aman Chopra, Seleem H Elkadi, Justin Chau, Daniel F Childers, Joon Chung, William F Postma Bertin. “Association of Symptomatic Venous Thromboembolism and BMI in Patients Undergoing Sports Medicine Knee Procedures: A Retrospective CaseControl Study.” Sports Health, 2024. PMID: 37114797
Alison Karasz, Samuel Nemiroff, Pablo Joo, Irene Blanco, Ariel Y Fishman, Mary S Kelly, Steven M Henick, Maryl Lambros, William B Burton. “A Sense of Belonging: Perceptions of the Medical School Learning Environment among URM and Non-URM Students.” Teaching and Learning in Medicine, 2024. PMID: 37450615
65
66
Celine M Schreidah, Lauren M Fahmy, Brigit A Lapolla, Bradley D. Kwinta, Cynthia M Magro, Larisa J Geskin. “Clinical Remission of Primary Cutaneous Marginal Zone B-Cell Lymphoma in a Patient with Crohn's Disease after Helicobacter pylori Quadruple Therapy and Vedolizumab.” The American Journal of Dermatopathology, 2023. PMID: 37377200
Emma D. Klein, Emily B Sonnenblick, Arielle L Sasson, David Anderson, Laurie R Margolies. “Breast MRI for Extent of Disease: Association of Demographic Factors and Biopsy Compliance on Surgical Decisions in Patients with BI-RADS 4 and 5 Findings.” The American Surgeon, 2023. PMID: 37311567
67
Sara Dehbozorgi, Nicole Ramsey, Ashley Sang Eun Lee, Amaziah Coleman, Pooja Varshney, Carla M. Davis. “Addressing Health Equity in Food Allergy.” The Journal of Allergy and Clinical Immunology, 2024. PMID: 38280451 68
Serene Z. Mirza, Yi Zhang, Huong T. Do, Bella Mehta, Susan M. Goodman, Anne R. Bass. “Black Patients are More Likely to Undergo Early Revision Total Knee Arthroplasty in a Matched Cohort Regardless of Surgeon Experience.” The Journal of Arthroplasty, 2023. PMID: 37295621
69
Samuel Nemiroff, Raymond Chai, Jun Fan, Ilana Ramer-Bass. “Ectopic Cervical Thymoma in a Patient Diagnosed with Graves Disease: A Systematic Literature Review.” The Journal of Clinical Endocrinology and Metabolism, 2023. PMID: 37897424
70
71
Tomoki Sakata, Spyros A. Mavropoulos, Renata Mazurek, Francisco J. Romeo, Anjali J. Ravichandran, Jonas M. Marx, Taro Kariya, Kiyotake Ishikawa. “Reduction of left ventricular diastolic pressure as a key regulator of infarct coronary flow under mechanical left ventricular support.” The Journal of Physiology, 2024. PMID: 38457313
George G. Pujati, Tais G. Bertasi, Raphael A. Bertasi, Ryan D. Frank, Sara E. Filmalter, Manisha Salinas, Ahmad Al Awadi, Renu Gautam, Walter C. Taylor. “Physician attitudes toward sports medicine coverage of mixed martial arts.” The Journal of Sports Medicine and Physical Fitness, 2023. PMID: 37158795
*Updated on April 28, 2024
72
73
Gloria Farber, Jonas Marx, Andre Scherag, Ibrahim Saqer, Mahmoud Diab, Christoph Sponholz, Torsten Doenst. “Risk stratification for isolated tricuspid valve surgery assisted the Model for End-Stage Liver Disease score.” The Journal of Thoracic and Cardiovascular Surgery, 2023. PMID: 35431033
Katie A O'Connell, Jacob L. Thomas, Fadi Murad, Guohai Zhou, Guru P Sonpavde, Matthew Mossanen, Timothy N Clinton, Antonio Ji-Xu, Kristina Alton, Philippe E Spiess, Anthony M Rossi, Chrysalyne D Schmults. “Total Margin Control Is Superior to Traditional Margin Assessment for Treatment of Low-Stage Penile Squamous Cell Carcinoma.” The Journal of Urology, 2024. PMID: 37788015
74
Parissa Tabrizian, Allen Yu, Neha Debnath, Bryan Myers, Thomas Marron. “Immunotherapy and Liver Transplantation: The Future or the Failure?” The Surgical Clinics of North America, 2024. PMID: 37953034
*Updated on April 28, 2024
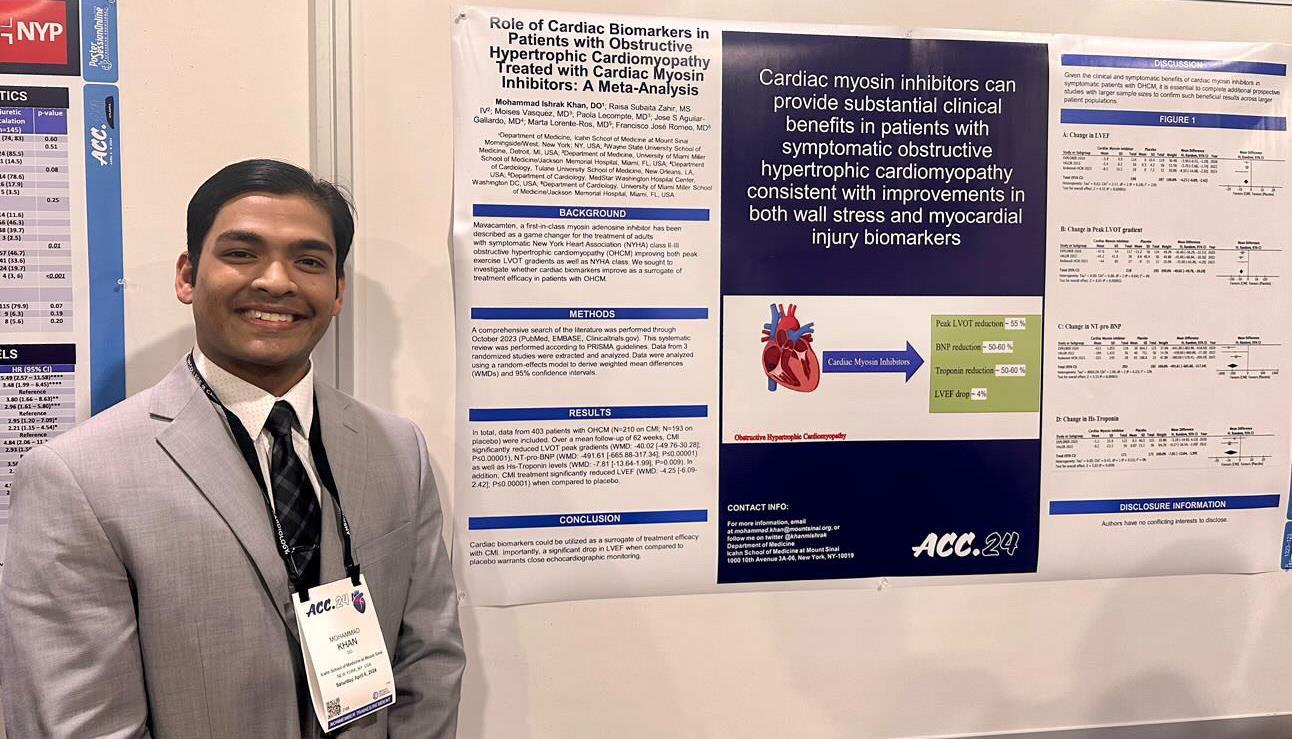
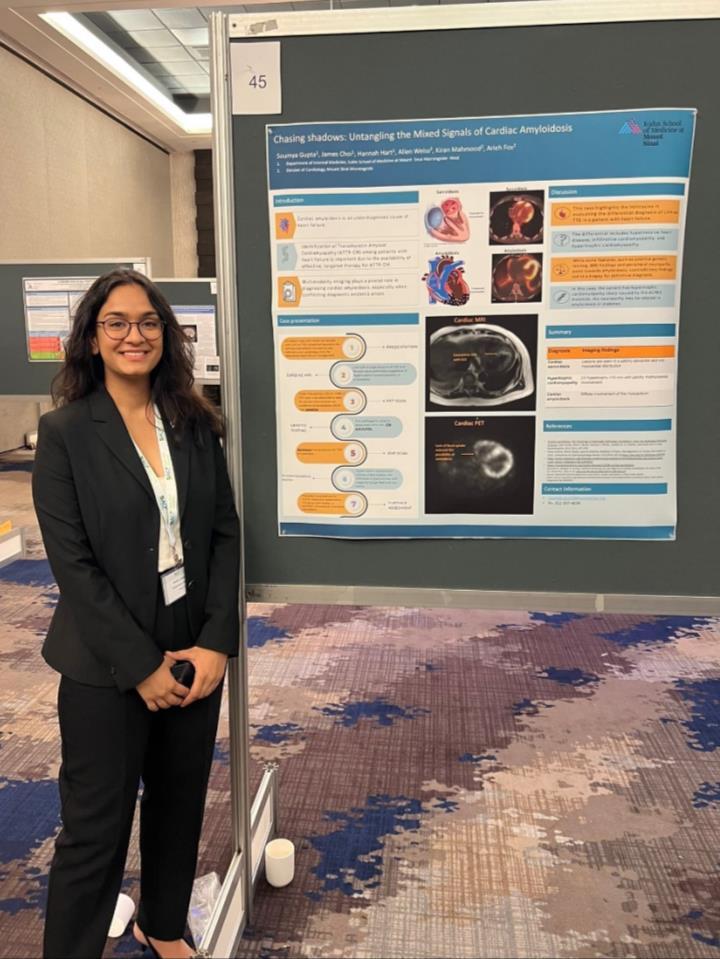

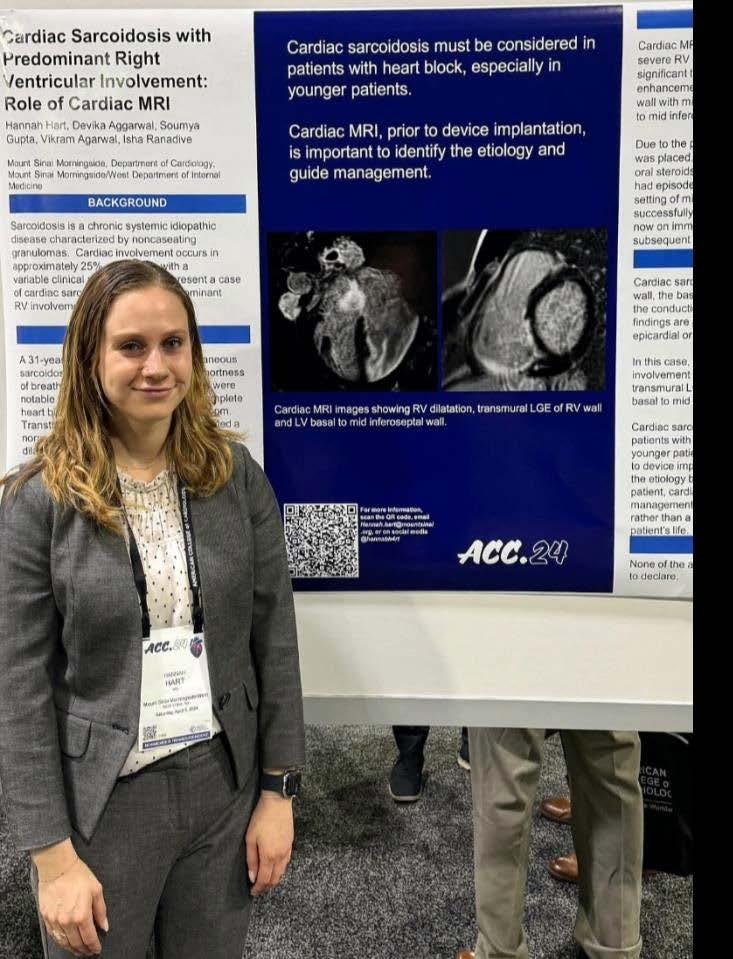

Abraham, Joseph: 118-120
Adegbite, Benjamin: 94-95, 169, 280
Agboglo, Ayele: 23-24
Ahmed, Shirin: 25
Ajisafe, Oladayo: 26-27
Alsaud, Mohammed: 28
Amel Riazat-Kesh, Yosef Joseph
Rene: 29, 279
Aoun, Marie Louise: 30
Arango Morales, Juan: 43-48, 83-84, 220
Arcayan, Brent: 247
Baer, Matthew: 31, 96, 162-163
Balayla Rosemberg, Galit: 32, 97, 260, 261, 264
Bapodra, Neil: 33
Bastos Silva, Murilo Roberto: 34, 66-68, 190-192, 197-199
Belfaqeeh, Omar: 35-36, 164, 165, 283
Benavides Leon, Raul: 37-38
Bilani, Nadeem: 39, 40-41, 42, 251, 279, 280, 284
Caceros Diaz, Salvador: 43-48, 215-217
Carter, Kristen: 49, 77, 83-84, 166-167, 168, 215-217, 218, 219
Chau, Justin: 285
Cheng, Julia: 278, 281, 283
Chernyk, Adrian: 50
Choi, Christiana: 97
Choi, James: 31, 51-52, 77, 83-84, 94-95, 101-103, 118-120, 169, 180-182, 183, 184, 187, 222, 226-227, 230-232
Chowdhury, Nobel: 53-54
Costa, Bruno: 55-56, 170-171, 172, 173, 174, 175, 176, 269-270, 278, 279, 280, 284
Cuan, Katherine: 57
Czaniecki, Tyler: 58
Dave, Priya: 278, 279, 284
De Oliveira Bertasi, Raphael: 39, 40-41, 172, 280, 281, 285
De Oliveira Bertasi, Tais: 39, 40-41, 280, 281, 285
Deb, Mrittika: 59, 201
Debnath, Neha: 60, 172, 177, 213, 282, 286
Dehbozorgi, Sara: 285
Desai, Binoy: 117-119, 178-179, 281
Dhaliwal, Arshdeep: 221, 283
Diaz Saravia, Sara: 51-52, 55-56, 61-62, 77, 83-84, 94-95, 101-103, 169, 180-182, 183, 184, 185-186, 187, 226-227, 230-232, 278
Diola, Carlos: 63
Dixit, Keshav: 64, 243, 279
Eng, Andrew: 65, 282
Feng, Jin: 66-68, 188, 189, 190-192, 193-194, 195, 196, 197-199
Fermin, Debbie Marie: 69, 73, 115-116
Ferreira de Carvalho, Julia: 32
Fusillo, Thomas: 70, 200, 281
Gandhi, Kruti: 71, 109-111, 117, 168, 202, 203, 204, 205-206, 207-208, 209-210, 211, 212, 222, 243, 244, 245, 246, 248, 278, 279, 280, 281, 282, 283
Gandhi, Sonal: 72
Garcia, Martin Emmanuel: 73
Gargaritano, Kristine Lou: 34, 201 Goodfarb, Justin: 74-75, 92-93, 125-126
Gordon, Ariel: 213, 214
Grewal, Satwant: 76
Grimaldo Ochoa, Joel: 247
Gupta, Soumya: 77, 78, 83-84, 166-167, 168, 180-182, 215-217, 218, 219, 283
Hart, Hannah: 78, 83-84, 219, 220
Henry, Chad: 125-126
Herrera, Rayling: 122
Hussein, Rama: 79-82, 96, 118-120
Johnson, Samuel: 63
Karim, Maria: 279, 281, 283, 284
Karpenos, Joseph: 83-84, 96
Katic, Luka: 85-87, 279
Kaur, Arpanjeet: 76, 88, 168, 207208, 209-210, 221, 222, 280, 282, 283
Kennedy, Madison: 89-90
Khan, Mohammad: 74-75, 91, 92, 279, 281
Kim, Do Han: 278, 282
Klein, Emma: 284, 285
Koh, Won Joon: 92-93, 278
Kong, Darren: 94-95, 169, 183, 222
Kwinta, Bradley: 283, 284, 285
Lenchur, Christine: 122, 281
Low, Scott: 96, 224
Luby, Sara: 76, 97, 252, 260, 261
Lutgen, Sophia: 66-68, 190-192, 197-199, 282
Maraveyas, Alexander: 29, 98, 281
Marinelli, Joseph: 92-93, 228-229
Markley, Alexandria: 35-26, 79-82, 118-120, 225, 273-379
Marushchak, Olga: 59, 99
Marx, Jonas Maximilian: 43-48, 100, 285, 286
Matthews, Christopher: 51-52, 9293, 101-103, 183, 184, 187, 215-
217, 226-227, 228-229, 230-232, 279
Menand, Joseph: 66-68, 104, 137-139, 190-192, 197-199, 233, 234, 235, 282
Meyer, Alyson: 201
Miao, Jiaxi: 105-106, 223, 224
Miguez Arosemena, Patricia: 107-108, 121, 164, 236, 237, 238239, 240-241, 242
Mirza, Serene: 285
Moras, Errol: 71, 91, 109-111,168, 202, 203, 204, 205-206, 207-208, 209-210, 211, 212, 243, 244, 245, 246, 248, 278, 279, 280, 281, 282, 283
Moss, Drew: 72
Mueller, Anna: 92-93, 220
Nagourney, Alexander: 28
Nemiroff, Samuel: 285
Oxman, Jonathan: 112-113
Patel, Aesha: 105-106
Patel, Swati: 79, 114, 273-274
Perry, Bailey: 115-116
Reyes Reyes, Lenisse: 247
Sadek, Norah: 280
Sadud Armaza, Sharel: 50, 247
Salman, Sidra: 117, 203, 212, 244, 246, 248, 249, 250, 251, 252, 253, 259, 279, 282, 284
Sandhu, Robinderpal: 104, 118-120, 137-139, 233, 234, 235, 254, 255, 257
Seltzer, Emily: 107-108, 118-120, 121, 178-179, 215-217, 255, 256, 257, 269-270, 272
Semaan, Rosa: 282
Shah, Priya: 122, 218
Sharma, Venus: 97, 123-124, 140, 249, 258, 259, 260, 261, 262, 280
Sheikh, Hammad: 85-87, 97, 260, 261, 263
Shetty, Samantha: 74-75, 83-84, 125-126, 164
Silverman, Alexander: 85-87
Sinclair De Frias, Jorge: 127-128
Smith, Connor: 97, 129-130, 260, 261, 264-265
Tai, Hua-Hsin: 266
Thomas, Jacob: 283, 286
Torelli, Vincent: 131, 267, 268
Varela Knorr, Ines: 121, 132, 273-274
Velo, Agostina: 133, 275-276
Verma, Megha: 134
Wilkoff, Marni: 79-82, 117, 135-136, 164, 248, 269-270, 271, 272, 273-274
Yang, Alvin: 97
Zafar, Ahmun: 104, 137-139, 233, 234, 235, 282
Zibara, Victor: 140-142

Residency Leadership
John A. Andrilli, MD, FACP
Georgina Osorio, MD, MPH
Mariah Soria
Angus Cheung
Eric Wu

Residency Contact Information
Email: msmwimresearch@mountsinai.org
Website: https://icahn.mssm.edu/education/residencies -fellowships/list/msw-msm-internal-medicineresidency
Twitter: @msm_msw

Georgina Osorio
Associate Editors
Jeeyune Bahk
Randy Leibowitz
Eric Wu
Angus Cheung
Bianka Delvarin
Mariah Soria
John Andrilli
Deborah Edelman
Joseph Elias
Lindsey Fox
Tamara Goldberg
Ariela Hazan
Krystle Hernandez
Rohit Nathani
Alejandro Prigollini
Adam Rothman
Vasundhara Singh

