

MY WEIGHT WAS SLOWLY KILLING ME... LOSING IT



MY WEIGHT WAS SLOWLY KILLING ME... LOSING IT

An eating plan that helps promote health and manage your weight includes a variety of healthy foods.
The US Centers for Disease Control offers a number of tips on healthy eating in its Dietary Guidelines for Americans 20202025, even adding a recommendation that households consider “an array of colors” in the diet that represent “eating the rainbow,” in reference to the many fresh foods that contain vital nutrients.

Dark, leafy greens, oranges, and tomatoes - even fresh herbs - are loaded with vitamins, fiber, and minerals, the CDC says, and adding frozen peppers, broccoli, or onions to stews and omelets gives them a quick and convenient boost of color and nutrients.

The CDC reports that meals should emphasize fruits, vegetables, whole grains, and fatfree or low-fat milk and milk products. Furthermore, meals should include a variety of protein foods such as seafood, lean meats and poultry, eggs, legumes (beans and peas), soy products, nuts, and seeds.
A healthy diet is low in
added sugars, sodium, saturated fats, trans fats, and cholesterol and stays within your daily calorie needs, according to the CDC.
The US Department of Agriculture’s ‘MyPlate Plan’ can help households identify what and how much to eat from the different food groups while staying within the recommended calorie allowance. A ‘My Food Diary’ can also be downloaded to help track meals.
Foods are grouped in a range of categories with the following tips from the CDC:

FRUIT
Fresh, frozen, or canned fruits are great choices. Try fruits beyond apples and bananas such as mango, pineapple or kiwi fruit. When fresh fruit is not in season, try a frozen, canned, or dried variety. Be aware that dried and canned fruit may contain added sugars or syrups. Choose canned varieties of fruit packed in water or in its own juice.
Meal prep containers with broccoli, carrots, rice or soba noodles.
Add variety to grilled or steamed vegetables with an
herb such as rosemary. You can also sauté (pan fry) vegetables in a non-stick pan with a small amount of cooking spray. Or try frozen or canned vegetables for a quick side dish - just microwave and serve. Look for canned vegetables without added salt, butter, or cream sauces. For variety, try a new vegetable each week.
In addition to fat-free and low-fat milk, consider low-fat and fat-free yogurts without added sugars. These come in a variety of flavors and can be a great dessert substitute.
If your favorite recipe calls for frying fish or breaded chicken, try healthier variations by baking or grilling. Maybe even try dry beans in place of meats. Ask friends and search the internet and magazines for recipes with fewer caloriesyou might be surprised to find you have a new favorite dish.
You can still enjoy your favorite foods, even if they are high in calories, fat or added sugars. The key is eating them only once in a while.

We have all seen plenty of advertisements on television and especially on social media for electronic devices that claim to develop abdominal muscles and create what is commonly known as a six-pack.
Testimonials and video give the impression that attaching pads to the abdomen and pulsing electricity through them will create a cut and toned figure with noticeable muscle tone and will promote dramatic changes to the waistline.
Whether these devices are effective at producing the results demonstrated is the question.

The short answer is no.
While electronic pulses to the muscles will cause them to tense and gradually strengthen, there is no evidence that the stimulation will reduce body fat, slim the waistline or in any way burn fat.

In fact, there is no substitute for healthy diet and exercise to reduce weight and develop athleticism.
(See SIX-PACK, Next Page)
Some general tips for comfort foods include eating them less often. If you normally eat these foods every day, cut back to once a week or once a month; and eat smaller amounts. If your favorite higher-calorie food is a chocolate bar, have a smaller size or only half a bar. Alternatively, try a lower-calorie version. Use lower-calorie ingredients or prepare food differently. For example, if your macaroni
and cheese recipe includes whole milk, butter, and fullfat cheese, try remaking it with non-fat milk, less butter, low-fat cheese, fresh spinach and tomatoes. Just remember not to increase your portion size.
The CDC says households can gradually adapt their meal plans to a healthier diet while still enjoying a wide variety of foods whose freshness, taste and color make them appealing to all.

Although the US Food & Drug Administration has approved a type of over-thecounter abdominal stimulator, the Slendertone Flex, it has not indicated that the device replaces exercise as a means to remove body fat, lose weight or build muscle. In fact, the device is only approved for toning, firming and strengthening abdominal muscles.
Those who buy ab stimulators on the retail market will find that the packaging includes a disclaimer and a notice that recommends a healthy diet and regular exercise as the means to reduce weight, burn fat and develop a toned physique.
Reviews of so-called ab stimulators show that the devices will focus on the abdominal muscles when used correctly according to a recommended regimen (frequency of use and length of time vary between products) and can have an effect on the core muscles of the abdomen, but do not and cannot prove that electronic pulses burn body fat.
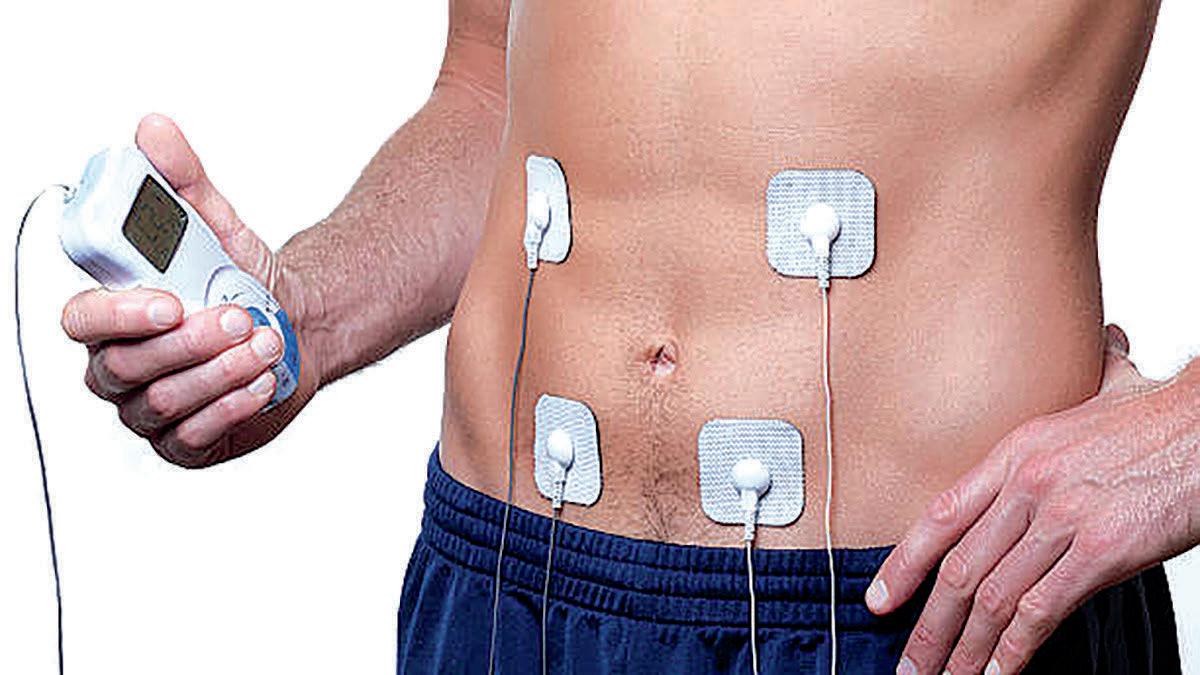
In a scathing review of the devices and their calorieburning claims, contributor Nick Nilsson wrote for TopEnd Sports that the advertising is not backed by research and that “in reality, the small muscle contractions produced by these belts burn about as many calories as the effort required to take the belt out of the box and put the batteries in.”
Nilsson’s review was published twenty years ago. Manufacturers continue offering the devices, however, despite Nilsson and others demonstrating that the actual effects are minimal.
In a recent review for the

Jacksonville Orthopaedic Institute, which is a member of the Baptist Health System, physical therapist Ehren Allen writes this year that while there is evidence to indicate abdominal stimulators help with strength, endurance, muscle size and function, they do not help with weight loss or fat burning.

Electronic pulses to a muscle group prompt contraction, much as the muscles may flex when tensed, but the therapist reminds his readers that the stimulator does not actually promote as much muscle contraction as if someone were to do the related exercise that focuses on the internal obliques, the external obliques and the transverse abdominals.
Again, in short, actual physical exercise is more effective than stimulating the muscles.
Allen also writes that “there is no significant scientific evidence to show that electronic stimulation helps with weight loss.”
He acknowledges, however, that the electronic stimulation to the abdominals “may decrease waist size but it does not translate to losing weight.”
Allen and other health care professionals agree that any change in waist size from electronic stimulation may in fact be due to the device’s effect on the transverse abdominal muscles.
Ab stimulators and related devices are sometimes marketed as transcutaneous electric nerve stimulation, or TENS, which is a therapy originally developed as part of a pain management program. The theory behind the procedure is that the electronic pulses affect the nerve fibers that send pain signals to the brain, thereby helping remove the sensation of pain but not the cause.
Electrical muscle stimulation works in a similar way but focuses on muscle contraction rather than nerve

endings. That contraction alone, however, is not adequate for actually building the muscles.
The electric stimulation procedure is also used by therapists for patients recovering from surgery or who have had to immobilize a limb. By stimulating the muscles during recovery, a therapist may help prevent atrophy and complete loss of muscle strength, essentially by keeping the muscle alive through routine contraction in a controlled environment. The procedure, however, is focused only on a targeted area and does not replace the physical exercise that must come later during recovery.
Exercising the abdominal muscles in a fitness regimen involves performing sit-ups or crunches that employ many more muscles than the abdominals. Legs, upper and lower back, arms and neck are involved in those exercises and are not at all affected by electric stimulation to the abdomen.
“The quick answer is that ab stimulators are not worth getting,” Allen writes. “If you’re looking for a way to get thin or in shape, there is no replacement for discipline and hard work.”


“There is no replacement for discipline and hard work”
Babies born with fetal alcohol syndrome are regarded as part of an overlooked vulnerable population.
There are stigmas and shame associated with drinking while pregnant, and most expectant mothers would not consume alcohol while pregnant in order to harm a baby intentionally.
Most women, however, do not know they are expecting until they are in week six of their pregnancy.
Recent research by the Cleveland Clinic shows that one in twenty babies may be diagnosed with fetal alcohol syndrome disorder (FASD), a number higher than those for Down syndrome, muscular dystrophy and spina bifida combined.

Drinking alcohol is dangerous during pregnancy due to a baby’s inability to metabolize the alcohol in the same way an adult does. The alcohol an expectant mother consumes is passed through her bloodstream to the fetus through the umbilical cord. The result is that by constricting blood vessels,


alcohol slows the blood flow to the placenta, causing a shortage of oxygen and nutrients to the fetus.

A child born with FAS may have formed a fundamentally different brain from a child not poisoned by alcohol as a fetus. Effects of alcohol on the fetus are contingent on when the alcohol is consumed by a woman carrying a developing baby, and for how long she continues to drink.
Studies show middle-class Caucasian women will continue to drink while pregnant.
Furthermore, half of pregnancies are reported as not
having been planned, and society often disparages expectant mothers who drink alcohol.
FASD is a spectrum disorder with primary and secondary characteristics. Primary indicators are organic brain changes that occur while the baby is still in the womb. Abnormalities include sensory issues, poor motor skills, decreased memory, an inability to focus, poor academic skills, impaired cognition, an inability to develop social adaptive skills, and the overall structure of the brain.



Drinking alcohol while pregnant can cause serious developmental disorders in your baby
“There is no safe limit; it is never worth the risk,” Christian Hancock, MS CCC-SLP says of a woman’s choice to drink alcohol while pregnant and the effect that choice has on a fetus. “Brain function is consistently inconsistent. It is like living in a home with faulty wiring.”
Children with fetal alcohol syndrome may have emotional regulation difficulties that cause mood swings. However, medical professionals describe the extreme mood swings as an “always scared brain, never a mean brain.”
In the United States, 13 is the average age at which a child has his or her first interaction with law enforcement. For a child born with fetal alcohol syndrome, that average age is five. Some health care professionals argue that such early evidence of mischief is due to a lack of impulsivity control.




“We fail these kids when we think they can link consequences to behavior,” Hancock says.
Decades of study have shown that fetal alcohol syndrome has a significant

impact on child development, including language and social skills, cognition, executive function and the ability to participate fully in society. The developmental immaturity level results in nearly 80 percent of fetal alcohol syndrome individuals being dependent in adulthood and unable to live independently. They are unable to predict outcomes and do not learn from their mistakes.
Although facial features of a baby born with fetal alcohol syndrome may be indicative of the disorder, they are not considered primary. However, a child must have abnormalities such as a smooth philtrum (the dimple between
the nose and upper lip) and thin reddish-orange or small palpebral fissures (the outer corners of the eyes) indicating a defect in forebrain development to be diagnosed with FASD.
A baby begins to develop facial features during week seven of the pregnancy.



Hypersensitivity in a young child may lead to a misdiagnosis of autism, resulting in only five percent of children receiving a diagnosis of FASD by the age of five. However, 72 percent of children with FASD are also diagnosed with autism.


Health care professionals are at pains to educate the public on the long-term implications of the disorder, and remove preconceived notions, stigma and other obstacles to a FASD child’s development and acceptance in society.
“We cannot adapt to an environment until we build the skill,” Hancock says. “We have to fill in the gaps for the brain. Individuals with FASD are not inherently dangerous.”

“There is no safe limit”
With gastric bypass surgery never under consideration, two Pearsall men found the motivation they needed to lose weight through a local health and wellness program.
When the coronavirus pandemic hit in early 2020, 32-year-old AJ Frausto, who was already obese, gained 50 pounds immediately.
“I had started a Crossfit program in town, but when COVID restrictions shut it down I found myself gaining weight quickly,” Frausto says.
While he found motivation to improve his health through a desire to keep up with his niece, Frausto was suffering from high blood pressure, sleep apnea, joint pain and frequent headaches. In 2020,
he was referred and qualified for a health and wellness program through South Texas Rural Health Services (STRHS).
“Since I qualified every three months I paid five dollars, got a check-up and had blood work,” he says.

His 450-pound frame led to self-esteem issues which became a road block for AJ when he began the program.
“I mean, I had lost 58 pounds on my own but it was really hard at the beginning because I was self-conscious and didn’t want to embar-
rass myself in front of the trainers,” he admits. “They were all women.”
Scared and nervous, Frausto fought through self-doubt, fought for his pride and reminded himself why he started in the first place – to better himself.
By September 2021, a year after starting his weight loss journey, he had lost 100 pounds and, due to his success in the program, was offered a job as a trainer.
He continues to maintain his weight loss journey and has lost a total of 208

pounds.

Frausto says he continues to have high blood pressure, which he attributes to stress, but his primary care doctor has decreased his dosage significantly.
“I still use my machine for sleep apnea but I really don’t need it,” he says. “It is a comfort thing for me.”
He describes his life then and now as ‘two different worlds.’
“I am not that person anymore,” he says. “I couldn’t even get a job because my weight was a risk.”
Today, Frausto is employed with an oil field company as a generator technician. When he isn’t working, he can be found on the baseball field. For as long as he can remember, he has had a passion for the game, not just playing but sharing his sports knowledge with children.
(See WEIGHT, Next Page)
“Back then, I had to tell them what to do,” he says. “Now I can demonstrate. Weight loss has made me such a better coach.”
Dropping the pounds now allows the coach to be on the field for 12 to 14 hours at a time.

“Before, I had joint pain constantly, especially in my knees and ankles,” he says. “I would go and do those tournaments and I was unable to even walk the next day.”
Frausto shared his weight-loss journey on social media and earned support from families and friends. His success also inspired others, including Frio County Clerk Aaron Ibarra.





“There was a ‘spotlight on health’ thing that featured AJ,” Ibarra says. “It inspired me to start my journey.”

The 35-year-old dad of two says Frausto’s success coupled with his desire to see his daughters grow up gave him the wake-up call he needed.
When Ibarra was 14, his dad died of a heart attack. Ibarra says he didn’t want his daughters growing up without him. He attempted to start losing weight on his own by counting calories and eating better, but after a couple of months he realized he needed help.
Without realizing it, Ibarra was channeling his negative emotions through overindulging and then trying to justify his actions.
things needed to be cut out of their diets, to increase their water intake, decrease sugar and carbohydrate intake, and how intermittent fasting is good for the body.
Now the pair eat as healthily as they can, and both practice intermittent fasting.
“It is hard, living in a Hispanic community,” both say. “Everything is so fatty, and holidays are tough. But once you get past the hardest part of cutting all of that out and sticking with it, your stomach shrinks and it becomes easier.”
Frausto says a vital step is meal prepping, a task for which he has help from Hannah Gandara.
“It is the easiest way to go,” he says. “You get the portions you need and you do not overeat.”
Ibarra chooses to cook at home and hopes to instill good eating habits in his children. He says he has learned to prepare healthy meals.
“My weight was slowly killing me,” Ibarra says. “Carbs are the devil. My sleep apnea was so bad that I had developed sleep paralysis.”
ITALIAN SALAD
Ingredients:
Salami
Pepperoni
Black olives
Green olives
Italian shredded cheese
Purple onion
Bag of shredded lettuce
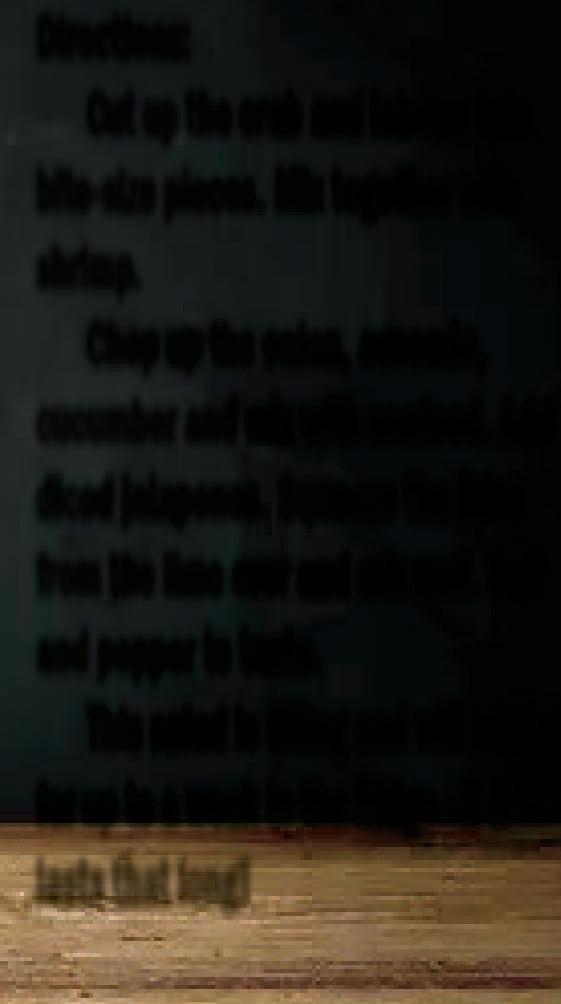
Directions:
As you see there are no measurements – just add how much of each ingredient you like.
Trainers at the STRHS Wellness Center are not nutritionists, but their knowledge of weight loss has enabled them to give suggestions and guidance for healthier eating. Both Frausto and Ibarra credit the resource with having helped them develop their new, healthier lifestyle.
Both men agree the staff taught them what
Fifteen months later and down 143 pounds, Ibarra no longer needs his CPAP machine. He has no intentions of stopping the program in the near future and has turned his focus into strength training to tighten his loose skin.
Empty the bag (I use the small bag) into a bowl, chop up the salami and pepperoni into bite-size pieces. Add the meat to the lettuce.
Chop up about a quarter of the purple onion and add to the mix. Add a small can of sliced black olives and however many green onions you would like. Mix in some shredded cheese. Mix together and season with salt and pepper. You can eat it dry or top with your favorite salad dressing. (Eating it dry saves on calories!)
AVOCADO SEAFOOD SALAD
1 bag of imitation crab legs
1 bag of imitation lobster
½ bag of salad shrimp
1 cucumber
½ purple onion

1 lime
¼ cup diced jalapenos
1 large avocado
Salt and pepper to taste
Directions:
Cut up the crab and lobster into bite-size pieces. Mix together with shrimp.
Chop up the onion, avocado, cucumber and mix with seafood. Add diced jalapenos. Squeeze the juice from the lime over and mix well. Salt and pepper to taste.
This salad is filling and will hold for up to a week in the fridge - if it lasts that long!
With summer right around the
corner,the
following two tasty salads standout and offer a light, refreshing, fulfilling meal. They are easy to prepare and are low calorie.BEFORE AND AFTER - (Photos from top) Aaron Ibarra and AJ Frausto of Pearsall took part in the South Texas Rural Health Services’ Wellness Program and share their success stories of better living, condfidence and self-esteem.


 Breyana Segura Frio-Nueces Current
Breyana Segura Frio-Nueces Current
It was never a question of whether Alex would be going to college; it was where.
Graduating from Dilley High School in May 2022, Alex Alvarez was accepted into a cohort program through the University of Texas at Austin, the E4, designed for students with disabilities, educating and empowering them to find their voice after high school.
Alex has autism, a speech impairment, and is classified as intellectually disabled.
“We knew something was wrong because when he was a baby, Alex did not like to be patted on his back or rocked,” his mom Nora says. “He would get frustrated when there was a lot of noise and nervous if we had company.”
Alex would often flap his hands, cover his ears, and cry incessantly.
“I just knew something was different,” Nora says. “The
pediatrician just kept saying that all kids were different.”
When Alex was 18 months old, he completely stopped talking for nearly six months.
Nora’s maternal instincts were strong, and a year later Alex’s parents learned the boy was developmentally delayed.
Because of his delay, Alex was able to start public school at the age of three, where he began to excel. Nora points to Alex’s drive to prove himself to earlyeducation teacher Judy Wilmeth as evidence of his determination.

Nora agrees that early intervention is the best intervention.
There are few opportunities for children growing up with disabilities in a small South Texas community. Alex did not let this stop him. He has always advocated for things he is passionate about, and in high school he pushed himself to remain in regular classroom education and participated in a number of extracurricular activities that included clubs, band, athletics and even academic competition.

(See ALEX, Next Page)



Attending a university was always a dream of Alex’s. He refused to let obstacles such as his disability stand in the way of his aspirations to pursue higher education. He had the same wants and desires as his peers in high school.

Furthermore, he did not allow his disability to affect his ability to perform successfully in daily life.
Recently, Alex learned that only three states require disability history to be taught in public school. He found such a glaring lack of inclusion unacceptable and began working on a legislative bill that would require such history be taught in Texas. It signaled the creation of Texas Senate Bill 670.
“I hope this bill will spark other states to do the same,” Alex says. “We need to edu-

cate society. We always learn Roman history, gay history, even ‘black lives matter’ history, but one history we are learning now is disability history. Why don’t we have disability history?”
Alex skipped his Christmas vacation last year and opted to attend meetings at the Texas Capitol, fighting for his bill to be passed.
“He has always been so smart but the way he talks just impresses me,” his mother says.
When he is not at the
Capitol doing research, interning at an Austin high school or studying for classes, Alex volunteers at the school for the blind. He has also learned how to use public transportation to navigate through busy Austin.
“I am learning to ride buses and get employment,” Alex says. “I mean, I lived in a small town, so riding the buses is... Wow!”
Alex is set to graduate on May 13 with an associate’s degree to become a paraprofessional, a job he hopes to pick up at his alma mater.
According to the US Census’ American Community Survey (ACS) in 2021, of the 36 million people who reported having a disability only 13 percent attended a post-secondary institution.

Students with intellectual disabilities have difficulty understanding new information, communicating appropriately, have slow cognitive processing time and sequencing information, and comprehending abstract concepts. These are often the principal barriers to leaving home and attending a university.
“Not only is he graduating from college, he is determined to be valedictorian,” his mom says. “He has far exceeded all our expectations of him. We always wanted him to become a productive member of society, even with his disabilities.”


 Marc Robertson Frio-Nueces Current
Marc Robertson Frio-Nueces Current
Anew report from the Texas Department of Health and Human Services outlines a number of serious health risks to children and adolescents who choose to use e-cigarettes.


Recent surveys of teens vaping with the electronic devices indicates that most are unaware of what the e-cigarettes contain, and even fewer understand the short- and long-term effects of vaping.
The National Institute on Drug Abuse published a report in 2018 – the year in which the popularity of vaping by teenagers reached a highpoint from its origins as an emerging fashion – indicating that more than half – at least 66 percent - who vaped e-cigarettes believed the devices contained only flavoring.
The remainder included nearly six percent who mistakenly believed the e-cigarettes contain marijuana; nearly 14 percent who didn’t know what was in the devices; but more than 13 percent who acknowledged that e-cigarettes
contain nicotine.
In fact, a single e-cigarette pod contains the nicotine equivalent of 20 tobacco cigarettes.

A typical vape pod contains between 1,500 and 2,500 “puffs.” Nicotine levels in vapes range from one brand to another, and those available for retail sale in the United States may contain nicotine levels as high as five percent. In other countries, nicotine percentage content is limited to no more than two percent in e-cigarettes, as health professionals have indicated a higher percentage content is dangerous.
“When teens vape, they inhale much more than flavored aerosol mist,” the Texas health agency reports in its clarification of what e-cigarettes actually contain. “They breathe in addictive nicotine and dozens of dangerous chemicals.”
The legal age for purchasing e-cigarettes in Texas is 21, and the devices are banned in schools and on school property such as stadiums in the same manner in which all tobacco and related products are banned. A number of school districts have reported continued

vaping by teens and are researching the installation of “vape detecting” devices on their campuses.
The TDHHS report includes results of surveys conducted last year that indicate teen vaping remains so common that it may be described as an epidemic.
“Five million middle and high school students vaped last year,” the state agency reports of its study of Texas teens’ habits. “About one fourth of high school students have vaped in the past 30 days. The popularity of vaping is growing rapidly each year.”
Data from 2018, shared by the TDHHS, indicates that over 20 percent of high schoolers across the United States had vaped in the 30 days preceding the study, and the percentage was only slightly lower for Texas, where 18.9 percent of students surveyed reported having vaped.
Nationwide, the numbers were lower for middle school students that year, with less than five percent reporting having vaped in the past 30 days. In Texas, however, that number of middle schoolers stood at six percent in 2018.
(See VAPE, Next Page)
Survey indicates many teens don’t know what they’re inhaling(Photo: Holland Hospital)
A 2019 survey by the National Institutes for Health reported that as many as 37 percent of high school 12th graders admitted to having vaped during the previous year.
The US Centers for Disease Control reported in 2019 that the national average for teen vaping had increased from 20.8 percent to 27.5 percent.
The TDHHS outlines its reasons for supporting a ban on teen vaping, not least of which are the serious potential health hazards of inhaling chemicals while the body is still in its developmental stage prior to full adulthood.

While some health care providers have suggested that e-cigarettes may be a safer alternative to smoking tobacco, such as a transition from smoking to quitting altogether, none have indicated that e-cigarettes are in any way healthy for the body at any age.
Research suggests that vaping may affect the way cells in the respiratory tract (nose, throat and lungs) react to germs and may increase the chance of disease and infection from bacterial and virus, like the virus that causes COVID-19.
Vaping may also make it harder to recover from infections and increase the possibility of complications, according to the state health department.
Vapes emit an aerosol that includes at least 31 chemicals and compounds that affect different parts of the body, the TDHHS reports, and the brain may be among the organs critically affected.
“The brain is still devel-
oping until about age 25,” the agency reports. “Using nicotine in adolescence can permanently harm the parts of the brain that control attention, learning, mood and impulse control.”
For those who choose e-cigarettes because of their flavor, the agency notes that flavoring chemicals such as diacetyl can permanently injure the lungs.
“Breathing in ultra-fine vapor particles can cause asthma attacks, coughing, wheezing and shortness of breath,” the TDHHS repots.
Brain, heart, kidneys, lungs and liver are also affected by other chemicals in e-cigarettes, as heavy metals in vapor can build up in the blood and organs and cause damage. Chemicals known as volatile organic compounds, or VOCs, cause eye, nose and throat irritation, severe headaches, nausea and organ damage. Formaldehyde irritates the eyes, nose, throat and skin and may cause lung and throat cancer over time.
“Nicotine is addictive and can harm adolescent brain development,” the TDHHS reports. “The brain continues developing into the mid-20s. Using nicotine in adolescence can harm the parts of the brain that control attention, learning, mood and impulse control. In addition, teens who use nicotine are more likely to experiment with other substances.

“Nicotine addiction is difficult to break,” the state agency concludes. “It takes determination, support and time to stop vaping for good.”
VAPING is not necessarily a safe alternative to smoking tobacco, and many users do not know what e-cigarettes contain.
The Texas Department of State Health Services has issued a health advisory notifying health care providers of reports that an animal tranquilizer called xylazine has been found mixed with illegal drugs distributed in Texas.

Law enforcement investigators have identified xylazine in the illegal fentanyl supply in West Texas, and it has been combined with other opioids, benzodiazepines like Xanax, and recreational drugs, leading to at least four reported xylazine-related deaths, according to the state agency.

Xylazine produces a strong sedative effect and can prolong the high of opioids and other drugs. It can cause unconsciousness, low blood pressure, a slowed heart rate and breathing, and may cause organ damage due to a loss of blood flow. Chronic use can cause
Did you know...
necrotic skin ulcers, severe sores that can kill skin tissue and lead to infection.
Law enforcement officers across Texas have reported that drug combinations with xylazine may be sold on the street under names like “Tranq,” “sleep cut,” or “Philly drug” or may be sold without the end user’s knowledge that they contain a tranquilizer.
Because xylazine is not an opioid, its effects cannot be reversed with the use of naloxone (Narcan). However, because of the prevalence of fentanyl and other opioids, the DSHS recommends that clinicians continue to treat suspected drug overdoses with naloxone. If the patient does not respond, health care clinicians should consider xylazine exposure and provide supportive care, according to the agency, and health care providers should also consider chronic xylazine exposure as a possible diagnosis for


patients with severe and unexplained necrotic skin ulcers.
The drug fentanyl is ranked by the US Centers for Disease Control as one of the most powerful sedatives on earth, fifty times stronger than heroin and a hundred times stronger than morphine. It is also ranked as highly addictive.

The CDC reported in 2021 that over 107,500 people had died from consumption of fentanyl. The narcotic is produced in Asia and imported by the United States, Canada and Mexico for medical use, although illegal trafficking has proven profitable for smugglers. The CDC estimates that one kilo of fentanyl equals a million doses and has a market value of approximately $400,000.
The US Drug Enforcement Administration reports that consumption of as little as two milligrams of fentanyl can represent a fatal overdose.
Vitamin D helps the body absorb and retain calcium and phosphorous, critical for building bone. It can also reduce cancer cell growth, help control infections and reduce inflammation.
There is a reason President George Washington looked uncomfortable in his portrait.
For the same reason, he looked a little swollen in the jaw.
He was wearing wooden teeth, because he had been afflicted by something that we all face over time. In his case, we are told, it was particularly difficult to manage.
As we age, the American Dental Association says we enter a second round of cavity-prone years. The first was when we were children. The second is all the more problematic because we have grown accustomed to taking care of our teeth and we don’t expect to have them riddled with cavities, causing us pain in our everyday lives.

We certainly don’t want to end up with wooden teeth as replacements.
Some of the reasons we could be experiencing more cavities late in life is dry mouth, which is a side effect
in more than 500 medications. We may also be more prone to gum disease and mouth cancers as we age, too.
Dry mouth is not a normal part of aging, but as we age, we tend to make more medications that can cause dry mouth. Some tips to fight dry mouth from the ADA include using oral moisturizers such as sprays and mouthwashes, drinking more water and not waiting until we’re thirsty to drink, using sugar-free gum or lozenges to stimulate saliva production, using a humidifier at home to keep moisture in the air; and avoiding foods and beverages that irritate dry mouths, including coffee, alcohol, carbonated soft drinks and acidic fruit juices.


Gum disease, also called periodontal disease, is caused by the bacteria in plaque. The bacteria irritate the gums, making them swollen, red and more likely to bleed. It can be difficult to catch gum disease in its ear-
lier stages, the ADA says, because it’s a painless condition until well advanced.

Untreated gum disease can cause the gums to pull away from the teeth and form pockets where food particles and plaque collect. Eventually, gum disease can destroy the gums, bone and ligaments supporting the teeth, leading to tooth loss.
The American Cancer Society says there are about 35,000 cases of mouth, throat and tongue cancer diagnosed each year. The average age of people diagnosed with the specific types of cancer is 62.

During regular dental visits, the dentist should check for signs of oral cancer, which include open sores, white or reddish patches, and changes in the mouth that last for more than two weeks.
Early detection of oral cancer saves lives, so it’s important to have regular dental checkups.






Medicare doesn’t cover routine dental care, the ADA says, so we should begin planning for dental expenses before retirement. Organizations like the AARP and others offer supplemental dental plans for their members. We can also look at discount dental plans that have a lower monthly fee than traditional insurance or look into low- or no-cost dental care locally through teaching clinics.
Deteriorating teeth and gums are a fact of life, but we don’t have to experience discomfort and loss if we take steps early to manage our dental health.
George Washington was a role model for many great leaders who followed, but in this one respect he may have set a different type of example from which we can learn.

Dental care is especially important in our senior years








