

ON THE COVER - OCTOBER 2020
This past March, Robyn Kennedy survived emergency open heart surgery. Without the support of her family and friends, Robyn knows that things would not have gone as smoothly as they did. Her strengthened faith and steadfast reliance on God has helped her through this trying time, and she now has a much greater appreciation for life.
See “Blessed to be Alive” on page 8.

FEATURE STORIES

ALSO IN THIS ISSUE
27 • ISSUE 10 • OCTOBER 2020 INSIDE : ADVICE FROM LOCAL HEALTH PROFESSIONALS
advice
Women’s Health Issues.
14.
CONTENTS VOLUME
Local Physicians give
on
Beginning on page
Motherhood: A Beautiful and Challenging Time 14-15 Be Strong and Of Good Courage 16-20 Tips On Taking Care of The Skin You’re In 22-23 A Strong Finish 26-29 MRONJ Commonly Occurs in Women 30-31 Faith Bigger Than Fear 34-37 It’s Hard to Keep a Warrior Down 40-42 Diabetes Screening is Key to Early Detection 44 The Gift of Healing 46-50 Doctor, Do I Need a Hysterectomy? 52 Kicking Cancer to the Curb! 54-56 Right Where God Wants Her To Be 58-60
The Way I See It An op-ed piece from the publisher 6 Exquisite Interiors 62-64 Ask the Experts 66 Events 66 Raising My Tribe 68-69 The Road Less Traveled 72-73 The Friends List 74 Scene About Town 12, 24-25, 32, 38 5 OCTOBER 2020 fourstatesliving.com

The Way I See It...
PUBLISHER’S LETTER
Robin Rogers, Ed.D.
For the last 20 years, Four States Living has put out two issues in October. In addition to the monthly FSLM, we would produce an additional Four States for the Cure or a Women’s Health issue. We did this to shine a light on breast cancer, the cancer that kills the most women in America and to support the Komen Texarkana Race for the Cure®. Over the summer, and at a national level, Komen reorganized and decided that Texarkana didn’t need a Race for the Cure® anymore. Having worked so closely with two amazing executive directors of our local office for many years (Terrie Arnold and Amber Lawrence), I was really disappointed. I can’t tell you how many strong and beautiful women –daughters, mothers, and grandmothers – we interviewed in that 20 years. These were friends and friends of friends who had fought valiantly to live more life. The stories were real and raw, and occasionally, one of the women we had fallen in love with would succumb to a recurrence of her cancer. You might wonder why women who knew that their cancer could still kill them would share their personal, medical battles; they did so that maybe just one woman would gain awareness or inspiration to do self-breast checks or get a yearly mammogram. Survivors make up a club that nobody aspires to ever join, but the members are the most loving and supportive people I have ever known. They show up, show out, and faithfully pray for a cure. Over the years, I have covered many of the Races, and I will miss seeing the camaraderie of the women in the pink hats celebrating life, together with their families, friends, and supporters.
After the announcement was made that Texarkana lost our Race, we made a decision at Four States Living to continue our mission to promote women’s health awareness in October. Texarkana has wonderful physicians, hospitals,
Four St ates Living
and medical professionals who choose to live here because we are not Dallas or Shreveport or Little Rock, the schools are great, and the quality of life is terrific. I grew up here, but watching professionals move to Texarkana to plant roots reminds me of how nice the area is for raising families.
With a special needs daughter (Emily), I am particularly grateful for quality healthcare. Notice how I just mentioned my daughter’s care? Moms worry about their kids, their spouses, and their parents, and too often overlook their own health. That’s not good. One of my most espoused pieces of wisdom is “You can’t take care of anybody else if you don’t take care of yourself first.” For some of us, that’s as simple as getting an occasional massage or taking an Aleve when our head hurts. How many times have I complained about having a headache to not get up and take medicine and drink a glass of water? I’m not sure if that’s just laziness or some inborn stubbornness that “if I sit here long enough, it’ll go away?”
I have little appointment reminder cards all over my house for Emily’s doctors’ appointments. Just this week, she’s seen her eye doctor and a foot doctor. Cerebral palsy comes with all kinds of issues, but she handles them like a champ. But, getting myself to an appointment, well, that’s another story. Nobody asks me if I have had a mammogram or my annual checkup with the gynecologist (I have not yet). And now that I hit the big 5-0, I did get a card in the mail from the gastroenterologist about the joys of colonoscopies. Who knew that the only one on my tail to get my tail checked out would be the gastroenterologist. All kidding aside, I will get both of these appointments set up before the end of the year.
You know why I do it? It’s selfish. I love my three children so much, and I want to watch them live their lives. I want to
PUBLISHER
Dr. Robin Rogers
EDITOR
Suzy Turner
GRAPHIC DESIGNER
Kim McMurry
SALES REPRESENTATIVE
Lori Rochelle
EDITORIAL ASSISTANT
Sara Rothwell
PHOTOGRAPHER
Alamond Photography


be a grandmother. I want to travel. But more than anything else, I want to always be here to watch after Emily, love her, and keep her safe. That means being proactive with my own health, in addition to hers.
I’ve known people with good genes who have lived to be 100 and haven’t seen a doctor in decades. And, I’ve also known some super athletes who have dropped dead during a workout. A friend and I were visiting the other day about God having total control, and “when your number’s up, your number’s up.” But God also gave us good sense, and I believe He wants us to fulfill our life’s purpose staying as healthy as possible. So, if there is a way to prevent the trauma and turmoil of an illness by finding a defect in the heart or a cancer or something in the colon through early detection, I’m going to drag myself to the doctor each year for those inspections.
Life is so very precious. If we have not learned anything else from 2020, perhaps seeing what a random virus can do to so many humans has taught us to value living large.
This month, we celebrate women who have lived through strokes, cancers, heart attacks, mastectomies, and so much more. They are just like you and me, but they have been to hell and back. Some will bring you to tears, and others will make you pick up the phone and make some appointments. We also have some really great female physicians who are contributing writers this month; I believe you will love their messages about what they know best.
The Komen Race may be gone, but we are going to keep women’s health as a priority for our readers in October. If one person is helped or makes an appointment because of these stories, we have done our jobs. Hope you all have a good October, and as always, thanks for reading FSLM
FEATURED COLUMNISTS
Ali Deal
Nichole Holze
CONTRIBUTING WRITERS
Ly Gaylor, M.D.
Mary Laura Hastings, DMD
Jennifer Jordan
Lee Alison McCrary, AGNP-C
Lindsey McMillan
Vicki Melde
Ellen Orr
Jileen Platt
Sara Rothwell
Deborah Shuman, M.D.
Lisa Porterfield Thompson
Emily Williams, M.D.
Living Magazine is distributed free of charge. Direct mail subscriptions are $36.00 per year. Reader correspondence and editorial submissions are welcome. We reserve the right to edit or reject any material contributed.
Do You Have a Story or a Photo?
We welcome information regarding topics of interest for future publications. If you have a story or photos that in some way depicts living or visiting in the Four States area and would be of interest to our readers, we want to hear from you. Call 903-792 -2262 or write: Editorial Department, Four States Living Magazine, 4106 Summerhill Square, Texarkana, Texas 75503. Comments are also welcome at our e-mail address: info@fourstatesliving.com
Want to Advertise?
Advertising rates may be obtained by contacting the Sales Department at 903-7922262, writing to Four States Living Magazine, 4106 Summerhill Square, Texarkana, Texas 75503, visiting our website www.fourstatesliving.com or emailing our Sales Department at info@fourstatesliving.com
ELEVATE THE OPTIMIST STIR THE MIND ENTERTAIN THE SOUL Four States Living Magazine is published the first business day of every month. © Copyright 2020 by Four States Living Magazine. No part of this publication may be reproduced in any form without written permission of the publisher. Four States
INSPIRE THE PESSIMIST
FOUR STATES LIVING MAGAZINE
FOURSTATESLIVING WWW.FOURSTATESLIVING.COM
6 OCTOBER 2020 fourstatesliving.com

AFTER SURVIVING AN AORTIC ANEURYSM,
ROBYN KENNEDY LIVES LIFE TO ITS FULLEST

by
photo
ALAMOND PHOTOGRAPHY
TO BE ALIVE BLESSED
by JENNIFER JORDAN
“When hard things happen, I believe the true nature of our faith will show up.” Robyn Kennedy eloquently affirms God’s influence on a very hard thing—the emergency open heart surgery she survived this past March. A life changing experience for anyone, Robyn’s recovery only strengthened her faith and reliance on God. She is truly blessed to be alive.
March 2, 2020, began like an ordinary day for Robyn. She woke at 5 a.m. to enjoy her coffee and quiet time on the back porch swing before driving her 11-year-old daughter, Ivy, to school. “I felt great!,” Robyn remarks. “My husband, Shane, had flown out the day before to visit his oldest daughter and our new grandbaby in Florida. I began cleaning the house in preparation for guests that evening.” As Robyn bent over to change the mop head, she “felt a sensation (sort of like electricity) shoot through my body. Immediate cold sweat, the worst headache I can remember (right below my temples in front of my ears), and extremely weak arms. I knew it was bad!” Robyn called her sister, whose husband, Sam Nix, is her primary care provider, and happened to be off work that morning and within earshot of the conversation. They immediately came over to Robyn’s house. Sam could not find a pulse in her right arm. “He sprang into action and (carefully) got me to Wadley Regional Medical Center. Before I knew it, I was on the helicopter being flown to Baylor Scott & White Heart Hospital in Plano.”
When Robyn awoke in the hospital Tuesday morning, she learned that she had survived an aortic aneurysm over three inches in size and “one of the top 5 largest aortic aneurysms my surgeon, Dr.
Justin Schaffer, had ever seen.” She also suffered an ascending and descending aortic dissection, as well as a faulty aortic valve. Robyn’s case is highly unusual, as most patients presenting with these diagnoses are male and over age 65, with a genetic history. As Robyn explains, “I was age 40, female, and have no family history.”
Robyn’s journey of recovery has been daunting as well as inspiring for her. She comments, “Heart surgery is tough. Several times before I left the hospital, I was told to focus only on my physical recovery. ‘They’ say your body won’t allow for the mental and emotional healing until IT fully recuperates. I thought this was the dumbest thing I’d ever heard … but ‘they’ weren’t wrong!” Emergency open heart surgery is physically grueling. Robyn’s sternum was sawed in half and her chest clamped open while a machine kept her heart and lungs functioning throughout the surgery. Robyn elaborates about the physical recovery, “It’s a great deal of trauma on one’s body. In the beginning, a walk about three mailboxes down the street and a shower (administered by my saint of a husband) were enough to exhaust me. Using the bathroom alone was nearly impossible! But days turned to weeks and weeks to months, and I kept gaining strength every day.”
As her physical recovery progressed over this time period, Robyn’s mental and emotional recovery began. “Wham! The enormity of what just happened hit me,” she explains. “To say the mental and emotional healing has been a bit slow seems like an understatement to me. I am a moody little thing and I cry … a lot! There’s medicine for that, but I’m just

 Ben Tice (Robyn’s brother), Katy Nix (Robyn’s sister) and Rick Tice (Robyn’s father) celebrated Katy’s birthday while Robyn was in the hospital with Macaroni Grill and a bota box. (No wine for Robyn, of course.)
Ben Tice (Robyn’s brother), Katy Nix (Robyn’s sister) and Rick Tice (Robyn’s father) celebrated Katy’s birthday while Robyn was in the hospital with Macaroni Grill and a bota box. (No wine for Robyn, of course.)
9 OCTOBER 2020 fourstatesliving.com
Katy (Robyn’s sister) accompanied Robyn to Plano in the helicopter. Katy kept Robyn calm even though she hated riding in the chopper.
enough stubborn to try and get through it on my own. My spiritual growth has benefited tremendously, and I think Shane would agree that his has, too!” Robyn sees how God has played a hand in her recovery. “I in no way believe that God CAUSED this to happen to me and my family, but He has certainly USED it to make us stronger. His handy work was and is evident in the most minute details. We continue to give Him all the glory for bringing me through such a miraculous recovery and for all the wonderful blessings along the way.”
Robyn continues healing, noting that her aorta is “pretty much all manmade now.” Her surgeon inserted two Dacron grafts, a stent graft, and a mechanical valve that “sounds like a cheap Timex watch,” Robyn laughs. These new devices should last the rest of her life. Although Robyn has to take a daily blood thinner and undergo frequent testing of her INR value (blood clotting time), she acknowledges that these somewhat annoying doctor visits are a “small price to pay.” Robyn has also experienced some hypersensitivity due to the wires that held together her sternum during the healing process. “I’ve studied up on having them removed and will discuss it with my surgeon when I have my bi-yearly checkup this month,” she states. “It’s a quick day-surgery that would hopefully give me much relief! All in all, I have been released to ‘live my life’ which I intend to do to the fullest.”
That is exactly what Robyn is doing, and she could not do it without the support of her family and friends. “My husband Shane is a saint! He was patient beyond belief while nursing me back to health. He showered me and helped me use the bathroom, he dressed me and changed my compression socks (which is no easy feat), he walked and talked and prayed with me, he took me for drives when I couldn’t stand being at home one more second, he ran for popsicles and prescriptions, and he stayed positive all the while. Shane never allowed me to feel sorry for myself which would have been easy to do! He remained the rock that Ivy and I have always known.”
Robyn also credits Ivy as a tremendous help. Robyn feels that motherhood is the greatest reward of her life and adores being a mother to Ivy. In turn, Ivy “is an absolute soldier. She took over the role of ‘sitter’ when Shane had to leave for work. She kept the house clean and took great care of herself and me.”
>>> Without the support of her husband, Shane, and daughter, Ivy, Robyn admits that her recovery would have been so much harder.


 Robyn (right) with her sisters Katy Nix and Stacy Proctor, and mother, Brenda Jones, during a girls’ weekend in Houston, Texas, last November.
Robyn (right) with her sisters Katy Nix and Stacy Proctor, and mother, Brenda Jones, during a girls’ weekend in Houston, Texas, last November.
10 OCTOBER 2020 fourstatesliving.com
Robyn is grateful as well to her parents and siblings who provided daily FaceTime visits and funny COVID-related text messages. “My dad was great about coming and rubbing my back and shoulders when I thought I couldn’t take the pain any longer. My best girlfriends and church family kept us fed and were available at all hours for whatever we needed. The ‘Meal Train’ my dearest friend, Mendy, set up for my family during recovery was a huge blessing. It made me realize how important it is to feed others in their time of need. If you are looking for a fun and easy way to volunteer or just love on people check out ‘Meal Train’! You will be blessed in return.”
Robyn’s support team would not be complete without her brother-in-law. She avers, ”I would be remiss to not mention my brother-in-law, Sam, who I fully believe saved my life with his knowledge, quick thinking, and professional connections that sped up the process of getting me to Plano in time. He hates being called ‘hero,’ but he is … and I am forever grateful that he was available.”
According to Robyn, her main takeaway from her surgery and recovery is that “my faith in humanity is restored. I have never felt such an outpouring of love, kindness, and selflessness as I did in the midst of my episode. While it’s easy to allow our hearts and minds to be inundated with the ugliness of the world, we mustn’t forget that ultimately people are good and lovely and agreeable.”
Robyn also hopes and prays that her story serves as a “beacon to anyone going through a tough time.” In fact, Robyn credits her pastor, Matt Graves, with helping her understand the idea of post-traumatic growth. “I have come through something major that easily could have beaten me down. Instead, because my hope is in the Lord, I can shout from the rooftop that I am loved, blessed, highly favored, and healed! I have a new and much greater appreciation for life, and I am so grateful for all of the lessons I am taking away from this experience.”


11 OCTOBER 2020 fourstatesliving.com
Robyn’s brother-in-law, Sam, literally saved her life ... and she says she still owes him dinner!




SCENE ABOUT TOWN
TRAHC PRESENTS THE MUSES’ OPERA CLASSICS PLUS The Texarkana Regional Arts and Humanities Council presented The Muses’ Opera Classics Plus on September 12 in Cabe Hall in the Regional Arts Center. A classic music lovers dream, the concert featured the talents of the Muses Professional Troupe, performing arias, duets, and ensembles from some of the world’s most beloved operas and musical theatre standards.







 Kim Fowler and Kaye Baxter
John and Susie Stanley
Laney Bassham and Dr. Charles Fortenberry
Steve Brown and Jeff Brown
Debbie Gilliam, Tiffani Whitehead and Kelly Burkhalter
Judge Josh and Diana Morriss
Phyllis Carter, June Owen and Charles Carter
Dr. Beverly Rowe, Dr. Alyce Bunting and Brandy Aaron
Brian Goesl, Noah Crissman and Randal Conry
Kim Fowler and Kaye Baxter
John and Susie Stanley
Laney Bassham and Dr. Charles Fortenberry
Steve Brown and Jeff Brown
Debbie Gilliam, Tiffani Whitehead and Kelly Burkhalter
Judge Josh and Diana Morriss
Phyllis Carter, June Owen and Charles Carter
Dr. Beverly Rowe, Dr. Alyce Bunting and Brandy Aaron
Brian Goesl, Noah Crissman and Randal Conry
12 OCTOBER 2020 fourstatesliving.com
Betty Jo Hays, June Owen, Lucille Cook and Patti Goesl

by

A Beautiful and Challenging Time Motherhood
by EMILY WILLIAMS, M.D.
The time has come: your sweet bundle of joy is finally here! After the marathon workout of the delivery and a revolving door of doctors, nurses, techs, etc., you sleepily pack up your nursing bras and oversized pads and head home with your tiny human, one who is fully dependent on you for every want and need. I know firsthand how hard this can be. When my little family arrived home this past June, I was completely exhausted after a weeklong hospital stay, complications for me, and a NICU admission for my son. Professionally, I had the knowledge from medical books and journals of the “fourth trimester,” but I admit I didn’t fully grasp the mental and emotional aspects until recently. These last few months have simultaneously been the most beautiful and challenging time I’ve ever experienced.
During pregnancy, a woman’s body gradually undergoes hormonal changes to adapt physically, supply nutrients to the baby, and prepare the body for labor. Then the little one makes his debut, and in a matter of days, the body changes drastically. Estrogen and progesterone levels plummet, making a woman more sensitive to stress. While I am fortunate that my lows could be treated with a good cry session and a hug from my husband, this isn’t the case for many women. In the clinic, I’ve talked to new moms with tears in their eyes as they finally opened up about their feelings. There often is a stigma with mental health concerns, and for moms of newborns, there is an added guilt. After all, you love your baby. You prayed for this baby. Your best friend is struggling with infertility, so you should constantly feel grateful, right? But we are human.

LYNDSEY SULLIVAN PHOTOGRAPHY
photo
14 OCTOBER 2020 fourstatesliving.com
I’ll say it: motherhood is hard. The expectation is snuggles, smiles, and beautiful memories, but the less glamorous reality is spit-up covered nursing tanks, loads of laundry from blowouts, and loud cries that start the moment your head hits the much-needed pillow. I think my baby is the cutest thing in the world, and I love him deeply, but his passion for awakeness kicks my butt sometimes. Even our dog walked into the wall the other day because she’s so sleep deprived.
Considering the sleep deprivation, pile of new responsibilities, and lack of time to yourself, it’s no wonder mood disorders are one of the most common medical conditions in the postpartum period. While 15-20% of women will experience postpartum depression or anxiety, unfortunately, these disorders are often underdiagnosed, underreported, stigmatized and shamed. Untreated depression and anxiety can have devastating effects. (Maternal suicide is one of the leading causes of maternal mortality!) This needs to change.
Recognition is one of the first steps. Risk factors include life stress and lack of social support – and who hasn’t had a little bit of each in 2020 –so it’s no surprise there’s been an increase in these medical conditions this year in particular. Many of the symptoms of depression and anxiety can be normal postpartum, so often moms don’t realize when the scale has tipped into something more. “Postpartum blues” may occur in the first several days (and up to two weeks) after delivery and are milder depressive symptoms and crying spells. It can affect 50-70% of women but is transient and does not require treatment. Postpartum depression (PPD), on the other hand, will be more intense and persist for greater than two weeks. Symptoms can vary, as women may experience change in sleep and appetite (increased or decreased), low energy, difficulty concentrating, loss of joy, feelings of guilt/ worthlessness, irritability/anger, difficulty bonding with her infant, and/or
have thoughts of self-harm. Postpartum anxiety (PPA) can occur alongside depression or on its own and is more intense and persistent than typical new parent anxiety. It may present as a constant sense of worry, sleeplessness, decreased appetite, or OCD.
Good social support, whether family, friends, or a therapist, is key in helping prevent and treat PPD and PPA. Sleep and exercise (even in small amounts) can help with symptoms as well. Most important, however, is talking to your provider. Only about 20% of women talk to their ob-gyn about what they are experiencing, missing the opportunity for diagnoses and referrals to a counselor or initiation of medications if needed.
To my fellow moms, if you think you might be suffering from anxiety or depression, please hear me ... asking for help doesn’t mean you are “weak” or “less fit” for your postpartum struggles. If anything, it’s a demonstration of how you value your role as a mom and love your little one, proving you are striving to be your best by getting the assistance needed. For friends and family of new moms, know that depression and anxiety are diseases of isolation, so it’s important to help new mothers feel supported. Remind them they aren’t alone, even in the midst of a pandemic. Delivering a meal, dropping off some diapers, or sending an encouraging text can make a huge difference. Remember to ask Mom how she is doing, not just how the baby is doing.
Having a baby is a stressful, emotional mix of tears and moments where you feel your heart may explode with joy. Some days I long for my sweet boy to go to sleep, but as soon as he does, I miss him! Our babies are worth every second of lost sleep, every missed workout, and every reheating of the coffee … all five times of reheating the coffee. And Mom, you are worth getting the help you need as well.
Dr. Emily Williams is an OB-GYN currently serving as a laborist for OB Hospitalist Group at CHRISTUS St. Michael Health System in Texarkana. Her husband, Ben, partners with her as they learn about their son, Lucas, who was born this summer.

15 OCTOBER 2020 fourstatesliving.com
 photo by ALAMOND PHOTOGRAPHY
photo by ALAMOND PHOTOGRAPHY
STRONG Courage Be and of Good
by VICKI MELDE
Somehow, there is a prevailing thought that those who serve in healthcare are immune from the health challenges and diseases for which they treat their patients. They are knowledgeable about preventive medicine and proactive about living a healthy lifestyle. Unfortunately, life-changing health events do not spare those who dedicate their lives to healing others. Such is the case with an amazing nurse practitioner – Amy Kennemore.
Amy was born in Lafayette, Louisiana, and spent her first years in a small town near Natchitoches, Louisiana. She moved to Ashdown, Arkansas, where she was raised and graduated from Ashdown High School. With encouragement from her mother, Amy decided to pursue a career in nursing. An excellent student, she attended Texarkana College full-time during her senior year of high school. At that time, her high school didn’t allow dual credit classes, so Amy attended high school for English and Color Guard and spent the remainder of her days at the college.
STROKE
AMY KENNEMORE SHARES HER STORY OF FIGHTING HER WAY BACK AFTER A MAJOR

Amy in outpatient surgery waiting at Wadley Regional Medical Center on March 8, 2017. Initially, the abdominal surgery was thought to just be an outpatient procedure so Amy was FaceTiming with her daughter, Braylee, while waiting to be taken back to surgery.

17 OCTOBER 2020 fourstatesliving.com
After completing the basic courses for the nursing program, Amy had a couple of semesters before she could begin the program. She decided it might be useful to complete the EMT program and obtain certification as an EMT and become nationally registered, which she did. Next, she earned a bachelor’s degree in nursing from the University of Arkansas for Medical Sciences (UAMS) and entered the Family Nurse Practitioner program. “When my Dad had a heart attack and was admitted to the ICU, I had a desire to know more,” Amy explained. “It was then that I decided to specialize in Acute Care and transferred to St. Louis University.”
Fortunately, Amy was able to do most of her clinical training in Texarkana – with physicians such as Dr. Khalid Malik and Dr. Christopher Bailey.
As a nurse practitioner in neurology, Amy likens the field to “looking at a 1,000 piece puzzle and trying to figure out how to put it together.” “I



 Tylan, Amy and Braylee in downtown Texarkana before getting Braylee’s senior photos taken during March 2019.
Braylee took this photo of her mom’s surgical incision after Amy’s skull had been put back in and the drains were removed. She was still in ICU at this point but was discharged to go to rehab shortly thereafter.
Tylan, Amy and Braylee in downtown Texarkana before getting Braylee’s senior photos taken during March 2019.
Braylee took this photo of her mom’s surgical incision after Amy’s skull had been put back in and the drains were removed. She was still in ICU at this point but was discharged to go to rehab shortly thereafter.
18 OCTOBER 2020 fourstatesliving.com
This photo was taken after Amy had surgery to remove her skull to help reduce the pressure on her brain from swelling. Part of her skull was removed for four weeks and stored in a freezer at Wadley during that time. She had to wear a helmet during that month to help prevent any type of brain trauma.

love neurology because it never gets boring – no matter how much you know, there is always more to learn – and every patient is different,” she shared. “My favorite part of being a nurse practitioner is the patients. They are not only your patients, they also become your friends. It is such a blessing if you get the opportunity to make someone ‘better.’ There is probably nothing better than someone telling you that you made a positive difference in their life!”
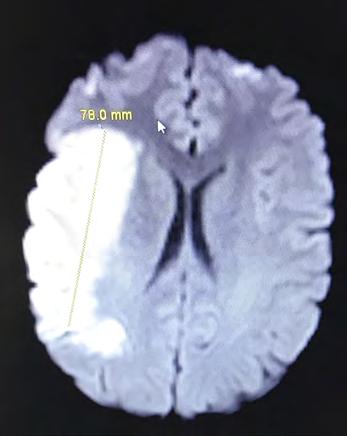
All of the positive things Amy has done for others certainly came back to her a thousand-fold when it was she who needed care and encouragement after suffering a major stroke following surgery. “When I was not waking up following surgery, the nurses called the vascular neurologist who evaluated me and felt that I was having a stroke,” Amy explained. “Fortunately, Wadley has 24/7 MRI coverage and CT perfusion abilities. I was taken for an MRI which revealed a large stroke and a blocked right middle cerebral artery, which basically supplies the part of the brain responsible for most of the movement and feeling sensations on the left side of the body.”
A CT perfusion revealed some of the brain to be salvageable so Amy was given tPA – the “clot buster,” despite the recent surgery, and a blood transfusion. It was decided that the benefits from receiving the clot buster outweighed the bleeding risk because if it was not given, Amy would most likely have died or been confined to a wheelchair, paralyzed on the left side.
The magnitude of the stroke became even clearer when the Texas Stroke Institute was consulted but they found the stroke to be too large for a mechanical thrombectomy (clot extraction). “I was kept at Wadley, in the ICU, cooled down to 96 degrees, with a cooling blanket, to help reduce the brain swelling that occurs with a stroke this large. I was given medications to raise my blood pressure, and then surgically had my skull removed the following day to help reduce the pressure that my skull would put on my swollen brain and to help prevent further brain injury,” Amy recalled. “My skull was stored in a freezer, at the hospital, because I had an abdominal infection, and my skull couldn’t be stored in my abdomen as is normally done following skull removal. I was on the ventilator for two weeks and had multiple other lines, drains, and a chest tube.”
On Easter Sunday, one month after the surgery to
remove it, Amy’s skull was replaced. She stayed in the ICU for 37 days, was then sent to TIRR Memorial Hermann for inpatient rehab in Houston, Texas, and finally had local outpatient rehabilitation. Botox injections are still required every 3-6 months in her left upper extremity to help reduce the spasticity. She also takes many medications – including one for seizures – that make her very tired.
Amazingly, when asked how her recovery has gone, Amy responded that it has gone well. This is definitely where one of Amy’s favorite scriptures played a crucial role. “Have I not commanded thee? Be strong and of good courage; be not afraid neither be thou dismayed: for the Lord thy God is with thee whithersoever thou goest.” (Joshua 1:9) “From working in Neurology for so many years, I know that without God’s miracles, the excellent care I received, and a wonderful support system that my outcome would have likely been very devastating, if I had lived,” Amy shared.
Amy lives with a spirit of gratitude to God and toward all who played a role in her survival and recovery. “I could never thank Dr. Malik, Dr. Bailey, Whitney White, all the wonderful nurses, radiologist, radiology techs, therapists, the entire Wadley staff and administration for all they did for me,” Amy declared. “I had worked at Wadley for about 10 years, and they took care of me and my family as if we were their family. They went above and beyond in their care for me and are largely responsible for the positive outcome that I have had.”
Following an event such as a major stroke, having a strong support system is crucial. Amy admitted she couldn’t begin to name everyone who has supported her along this journey. She is, however, very quick to express her appreciation to her children for caring for her and continuing to help her. Daughter Braylee, her “responsible child” is 19, attends Texas A&M University-Texarkana, and recently became engaged to her boyfriend of five years, Luke. Her 17-year-old son, Tylan, is smart and witty, loves baseball, and is the child who makes them laugh. His girlfriend, Tatum (“Tater Bug”) is also very special to Amy. Three fur babies, Mug-Z (considered Amy’s ‘therapy dog’), Bougie, and Big Moochie complete the family she adores.
Amy’s children, parents, Dr. Malik, Whitney, brothers
19 OCTOBER 2020 fourstatesliving.com
One of the initial images from Amy’s stroke taken in March 2017. It shows a very large right middle cerebral artery infarct.
and sisters-in law, and close friends and family spent many hours at her bedside and came to Houston during her rehabilitation. “My parents stayed in Houston in their motor home while I was in inpatient rehab and cared for my children during my hospitalization,” she gratefully recalled. “And my brothers did everything they could to help me. My eldest brother, Ernie, and his wife, Kim, even had a Sweet 16 party for Braylee when I couldn’t be with her on this special occasion. My brother, Mark, has taken me to countless doctor’s appointments in various states and even stayed with me following my hospital discharge when I wasn’t able to stay alone.”
It was Amy’s love for her family that kept her going and their love that motivated her. “On the days I felt like giving up, I couldn’t stand the thought of hurting the people that love me,” Amy admitted. “Parents always want the best for their children. I knew my parents would be devastated if I didn’t get better. And, I knew no one else would ever love my children the way that I love them!”
Though Amy struggles with simple things that she used to take for granted such as tying shoelaces, fastening buttons, and zipping coat zippers, her main challenge is stamina. She isn’t able to work the 12-16hour days that were common prior to the stroke. She hasn’t returned to work yet, but her goal is to obtain her doctorate in the near future and return to work in the field she so loves – neurology. No doubt, Amy’s experience with her stroke will make her an even more knowledgeable and compassionate healthcare provider.
Whatever the future holds, Amy’s outlook on life is inspiring. “I realize how blessed I am, not only to be here, but also to have so many people who love and support me!” When asked about any words she lives by, her response was so meaningful – and so appropriate. “Seek a miracle. Nothing is impossible with God!”



20 OCTOBER 2020 fourstatesliving.com
Amy with her family during a family reunion in Lake Charles, Louisiana. With her are her brother, Ernie Kennemore; father, Ray Kennemore; mother, Joan Kennemore; and brother, Mark Kennemore.


How often should I get a skin exam?
Tips On Taking Care of The Skin You’re In
by LY GAYLOR, M.D.
photo by SARA ROTHWELL
In general, a yearly skin examination is an important part of a good health maintenance program. However, individuals who have a personal or family history of skin cancer may need to be seen more often. I strongly encourage those who spend a lot of time outdoors or who have a history of tanning to be seen at least annually.
When should I worry about a mole or spot on my skin?
When performing a skin exam, I look for the “uglyduckling moles” or the moles that don’t look like your other moles. I also emphasize to my patients to come see me if an odd-looking spot suddenly arises, especially if the spot bleeds or becomes painful.
Be concerned if any of your spots have the following features:
“A” stands for Asymmetry: melanoma lesions are often irregular; one half looks different than the other half.
“B” stands for Border: melanoma lesions usually have irregular borders.
“C” is for Color: the presence of more than one color or the uneven distribution of color on a skin spot can sometimes be a warning sign.
“D” refers to Diameter: melanoma lesions are often greater than 6 mm in diameter (approximately the size of a pencil eraser). Although this is a good rule of thumb, I do often diagnose melanomas less than 6 mm.
“E” stands for Evolution: If a mole is changing in color and/or size, have a dermatologist examine it.
How can I protect my skin from skin cancer? I often stress to my patients: there is no such thing as a healthy tan! One in five Americans will develop skin cancer in their lifetime. Most skin cancers are the result of UV exposure from the sun or from tanning beds. Skin cancer prevention should start at a young age since much of the damage to your skin starts in your youth or early adulthood. The following are

helpful tips for proper sun protection:
1. Choose a sunscreen that has these 3 features: SPF of 30 or higher, is water resistant, and provides broad-spectrum coverage (UVB and UVA coverage).
2. Try to avoid peak hours of sun between 10 a.m. to 4 p.m.
3. Apply sunscreen before going outdoors. It takes approximately 15 minutes for your skin to absorb the sunscreen and protect you. Apply sunscreen even on cloudy days.
4. Apply enough sunscreen. Most adults need about 1 ounce — or enough to fill a shot glass — to fully cover their body. Rub the sunscreen thoroughly into your skin.
5. Apply sunscreen to all skin not covered by clothing. Cover-up with long-sleeved clothing, a broad-brimmed hat and sunglasses with UV protection. Protect your lips by applying a lip balm with at least SPF of 15.
6. Reapply sunscreen every two hours, or immediately after swimming or sweating.

22 OCTOBER 2020 fourstatesliving.com
7. Avoid sunburns and tanning beds. I personally prefer physical sunscreens (vs. chemical sunscreens) which contain mainly zinc oxide and titanium dioxide. These physical blockers are also the recommended sunscreen for children and for those individuals with sensitive skin.
What products should I use to prevent aging?
I realize that it can be quite overwhelming to pick a product with so many skin care options to choose from. My advice is to start simple. Oftentimes, a patient will bring in a bag full of products they are using, and I find that some of the products may actually be aggravating their skin. First, start with the two most effective products to combat aging –a good sunscreen and moisturizer. No matter your skin type (normal, oily, or dry), I recommend a daily moisturizer. Also, find a gentle, facial cleanser to use twice a day to remove dirt and oil off your skin. Retinols found in many anti-aging products will help with fine lines and wrinkles and help brighten dull skin by increasing cell turnover. In addition, products containing anti-oxidants (such as Vitamin C) can reduce inflammation and help the skin repair itself.
Can certain types of food make my acne worse?
I often hear from my patients, “Every time I
eat chocolate or drink a soda, my face breaks out.” Actually, there is evidence to support this. Studies show that low-glycemic foods (such as fruits, vegetables, beans, and oats) can lower your risk of acne breakouts. On the other hand, high-glycemic foods (such as white bread and rice, corn flakes, potato chips, fries, doughnuts and sugary drinks) can worsen acne. High-glycemic foods can cause spikes in your blood sugar that can lead to inflammation throughout the body. This inflammation can cause an increase in the production of sebum, an oily substance in your skin. Both inflammation and excess sebum can lead to acne. Some studies have also suggested that cow’s milk (whole, low-fat, and skim) may be linked to acne.
Can I be breaking out to my face mask?
Yes! “Maskne” is caused by pores being blocked by sweat, oil, and makeup from wearing a mask. And for those who wear a mask for several hours a day, the humidity created within the mask from breathing or talking creates an ideal environment for bacteria and yeast to grow. This along with friction from the mask can promote acne flares around the cheeks and mouth.
Some tips for reducing “maskne” include: 1. Skip the makeup when wearing a mask. If
makeup is necessary, use products labeled “noncomedogenic” or “oil free.”
2. Use a daily cleanser. This will keep your skin clean and calm. Look for products with salicylic acid or benzoyl peroxide for acne-prone skin. Be aware that benzoyl peroxide products may bleach or stain the fabric of your mask.
3. Wear a cotton-lined mask. Avoid synthetic fabrics such as nylon, polyester, and rayon. These are more likely to irritate your skin and cause breakouts. Also, it is very important to wash masks regularly to kill the germs on the inside and outside of your masks.
And lastly, when should I worry about a skin condition?
With so much information available at our fingertips, it’s natural to want to diagnose our skin problems over the internet. Although the internet can be very informative, it’s best to seek professional medical advice to verify your findings. The problem is that people often misdiagnose their conditions. This may lead to worsening of a problem that could have been addressed sooner or delaying necessary treatment. My best advice is if you are concerned at all, go see a dermatologist. This will help to relieve a great deal of stress and worry and possibly even save your life!
Dr. Ly Gaylor has been a dermatologist at Collom & Carney Clinic since 2008. When she is not working, she enjoys spending time with her husband of 23 years, Aaron, and their three children.

23 OCTOBER 2020 fourstatesliving.com

SCENE ABOUT TOWN


OPPORTUNITIES, INC. INVITATIONAL GOLF TOURNAMENT
The 31st annual Opportunities, Inc. Invitational Golf Tournament was held on Monday, September 14, at Texarkana Country Club. This year’s guest speaker was Dajha Smith. Dajha is currently a sophomore at Texas A&M University-Texarkana where she double majors in child psychology and business administration. Dajha attended the day therapy children’s program at Opportunities when she was little, and her journey has inspired her to be a psychologist for children with disabilities. She also dreams of opening a boys and girls club. In her spare time, she reads and writes stories. She is also active on TAMUT’s Campus Activities Board and the university’s PATH program. The tournament was sponsored by nearly 40 local businesses and partners, led by Platinum Sponsor, Eagle Dental Center. To date, the Opportunities, Inc. Invitational Golf Tournament has raised over $2.5 million for children and adults with developmental disabilities.





 Mayor Allen Brown and FaEllen Yates
Dajha Smith and Miss Texarkana Twin Rivers Outstanding Teen Gracie Britton
Katrena Goodwin and Mieashia Lindsey Sherry Young, Rebekah Drennon and Clay Roberts Dan Edmonds and Hershel Flanagan
Billy Power and Bruce Hornbuckle
Mayor Allen Brown and FaEllen Yates
Dajha Smith and Miss Texarkana Twin Rivers Outstanding Teen Gracie Britton
Katrena Goodwin and Mieashia Lindsey Sherry Young, Rebekah Drennon and Clay Roberts Dan Edmonds and Hershel Flanagan
Billy Power and Bruce Hornbuckle
24 OCTOBER 2020 fourstatesliving.com
Landry Gibbs and Drew Mims










 David Rolf and Bob Hubbard John Flippo, Chris Richards, Ryan Morgan and Jon Sheppard
Dan Edmonds, Ron Copeland, Corey Jerry and Jeff Butler
Dr. Hesham Hazin, Brandon Rampy, Dr. Chad Patterson and Tim Asimos
Katie Andrus and Lyndsey Craig
Rebekah Dannar, Mieashia Lindsey, Treston Osby and Jeremiah Stacks
Mike Rogers, Jason Ross, Matt Keil and Brock McCorkle
Mayor Allen Brown, David Hickerson, Sonny Brainerd and Calvin Williams David Rolf, Dr. Tom Hunley, FaEllen Yates and Bob Hubbard
David Rolf and Bob Hubbard John Flippo, Chris Richards, Ryan Morgan and Jon Sheppard
Dan Edmonds, Ron Copeland, Corey Jerry and Jeff Butler
Dr. Hesham Hazin, Brandon Rampy, Dr. Chad Patterson and Tim Asimos
Katie Andrus and Lyndsey Craig
Rebekah Dannar, Mieashia Lindsey, Treston Osby and Jeremiah Stacks
Mike Rogers, Jason Ross, Matt Keil and Brock McCorkle
Mayor Allen Brown, David Hickerson, Sonny Brainerd and Calvin Williams David Rolf, Dr. Tom Hunley, FaEllen Yates and Bob Hubbard
25 OCTOBER 2020 fourstatesliving.com
Philip Mobley, Paul Knowles, Cory Venable and Levi Ponder
SEVENTEENYEAR-OLD EMILY MEUNIER SHARES
HER TOUCHING STORY OF STRUGGLING WITH ANOREXIA NERVOSA

by
photo
ALAMOND PHOTOGRAPHY
A STRONG FINISH
by LINDSEY MCMILLAN

Emily Meunier is a senior at Texas High School with long blonde hair and lovely blue eyes. She’s soft-spoken but full of energy for life, enjoys sports, and loves being with her family and friends. She excitedly talks about the future and is looking forward to attending the University of Central Arkansas in Conway next year where she has already been accepted and plans to major in Psychology. This is a strong finish for a young lady whose start to high school wasn’t the case. Emily has overcome an obstacle many others like her face and has a positive outlook to share with others. This obstacle is the eating disorder, anorexia nervosa.
At the start of her freshman year in 2017, Emily began school like everyone else, enjoying herself by playing volleyball and spending time with friends. Shortly after Homecoming that Fall, she just wanted to lose some weight. Peer pressure and constant influence on social media began to affect the image of how she “should” look so she began dieting. That diet escalated months later into a very restrictive one where she was eating no more than 400 calories per day while also running three miles. She always enjoyed going running with her mom but began to use the exercise as a way of burning off every single calorie she ate. She says that it became almost like an obsession, wanting to restrict

herself in order to lose more and more weight. She was compulsive about her diet regimen and what she ate every day. She drank only water, had a very small breakfast, and a dinner of only one meat and a vegetable. She skipped lunch altogether.
Much like obsessive-compulsive disorder, anorexia nervosa is an illness which has serious psychological and physical consequences. Emily refers to her behavior at the time as being very ritualistic in what she ate and when. She constantly wanted to be moving to burn off calories. She suffered like many anorexics with body dysmorphia, or the inability to stop thinking about flaws in one’s appearance. Body dysmorphic disorder is directly tied to eating disorders as it focuses on flaws they see in themselves. Anorexics tend to view themselves as overweight even though they are not and become compulsive about weight loss. Shame, embarrassment, and anxiety are just a few emotions which result from this altered form of self-image.
Emily’s condition deteriorated in the time frame of five months where she was faithfully monitoring her calorie intake and exercising non-stop. She even recalled countless instances when she couldn’t sleep so she would just walk around the house. She was able to hide what was going on from others but only
On June 23, 2020, Emily and her friends, Lia Graham, Charli Hueter and Johnni Hueter, enjoyed taking senior photos together. (Photo by Rachel Alison)
Now happy and healthy, Emily prepared for her senior pictures this past June.
27 OCTOBER 2020 fourstatesliving.com
for so long. Symptoms emerged such as her feeling cold all of the time, loss of sleep, and a very low heart rate. She felt like she still needed to lose weight and had already lost 50 pounds. By the time the school year ended, Emily weighed 96 pounds and was urged by her pediatrician, Dr. Cindy Porter, to enter the hospital. She was told if she didn’t enter a program right away she would not have long to live. It was in May of 2018 when she left for Children’s Health in Plano for an inpatient program which lasted approximately two months.
At first Emily resisted going into treatment for her eating disorder, recalling she was in denial about her health and how sick she was becoming. But with the strong support of her family, she went to begin treatment. Emily’s mother, Stephanie Hawkins, and her father, Jeremy Meunier, were by her side, taking turns staying nearby at the Ronald McDonald House. A typical day in the hospital involved both group and individual therapy, routine meal and snack times, and visiting with dieticians and other nutrition specialists. Emily says that while being inpatient she learned so much, and not just about anorexia but other eating disorders as well. She was alongside other patients her age, as well as those who were older and younger. She made friends there who she still remains in touch with today. These peers were able to identify with her on the feelings and behaviors they dealt with and how to focus on healing and learning new ways of thinking.
Emily says that her time spent in the hospital was a very positive experience overall and one she learned from. Sometimes that isn’t the case with many patients, as others she met had been in the hospital several times and unsuccessful in recovery. Emily adjusted to the schedule which involved being busy throughout the day keeping record of her caloric intake and staying motivated to feel better. She could visit with family every evening, and they were able to visit on weekends. During the week her dad stayed nearby which was a big comfort to her. Her mom was there as well on weekends, and the three of them were able to learn about anorexia so they could continue to help Emily after treatment was completed. After her inpatient stay, Emily remained in Plano for an outpatient program which lasted another month and a half. Over the three-


This photo of Emily’s back, taken August 12, 2018, shows the toll that her eating disorder took on her body. Since she was obsessed with how her body looked, Emily would take body check photos often during her battle with anorexia.
After being released from the inpatient treatment program, Emily stayed at the Ronald McDonald House in Plano, Texas. Here, she weighed approximately 102 pounds.

<<<
>>>
28 OCTOBER 2020 fourstatesliving.com
month period, Emily learned all about her condition, specifically focusing on the emotions and struggles which accompany anorexia.
She admits it was hard adjusting to life back at home after treatment but she relied on help from family and friends for support. For the first six weeks of her sophomore year, she was homeschooled and did not feel ready to return to school. She also was in touch weekly with a dietician via virtual conference call. By the middle of that year, she felt stronger and more established with her eating habits. She shares that it was hard at first, as she struggled with changing her mentality, particularly when it came to food, exercise, and feeling better about herself. Many with this condition can relapse fairly easily. What helped Emily was changing the way she thought about herself since self-image is the driving factor in anorexia. She remembers being very hungry for a long time, experiencing “extreme hunger,” common for those in recovery. Also during this time her body was trying to rebalance her hormones. Being undernourished for so long wreaks havoc on the body overall, so she experienced some trouble with acne and facial bloating. An important lesson she first learned in recovery is that of eating and exercising wisely. Emily says, “I realized it’s okay to gain weight and get healthy. I changed my thinking to where I exercised for health and enjoyment not to burn off what I ate.”
Emily began to gain weight and feel confident with the changes her body was undergoing. The strong urge to control what she ate and overcome hunger before involved an inner voice (referred by inpatients as a persona named “Ed”). Emily shares that those suffering with eating disorders have to learn to understand and quiet the voice which previously dominated their selfimage and desire to keep losing weight. She also learned how the illness is a process of learning to love and accept one’s self. The lack of self-love and body dysmorphia results in the obsession with physical appearance and strict control of eating habits. Emily adds, “You are more than your physical appearance. Don’t put your idea of self-worth on other people and their opinions of you.” Various resources were helpful as she has moved forward in her journey. Emily recalls watching YouTube videos like those of Jen Brett who documented their own recovery with eating disorders and share with others. Another book she recommends is “Life Without Ed” by Jenni Schaefer.
Now Emily is healthy, strong, and optimistic about what lies ahead. She remains encouraged and looks forward to her senior year and college to follow. She knows that her struggle is one she will always have to deal with, and her past experience inspires her to help others. She hopes to become a psychologist or therapist working with teenagers afflicted with mental illness. When asked what she could share with other girls her age going through what she experienced she responds with, “What you see on social media is not real. It doesn’t matter what your body type is. Don’t try to change yourself to please others. Just love yourself for who you are.” With an empathetic and warm demeanor this is wise advice from a young lady who is confident and happy with who she is and who she wants to be.
>>>

 Emily (center) with her aunt, Lori Rochelle; cousin, Olivia Rochelle; grandmother, Paula Hawkins; and mother, Stephanie Hawkins, during the Pleasant Grove Academic Award ceremony when Emily was right in the middle of battling her eating disorder.
Emily (center) with her aunt, Lori Rochelle; cousin, Olivia Rochelle; grandmother, Paula Hawkins; and mother, Stephanie Hawkins, during the Pleasant Grove Academic Award ceremony when Emily was right in the middle of battling her eating disorder.
29 OCTOBER 2020 fourstatesliving.com

Medication-Related Osteonecrosis of the Jaw (MRONJ) Commonly Occurs In Women
by MARY LAURA HASTINGS, DMD
I feel honored to write this article for the Women’s Health and Wellness Issue in order to share information about the Oral and Maxillofacial Surgery specialty concerning women’s health. I went back and forth regarding what topic to discuss, especially one that would be pertinent to women’s health. Most of you reading this article are probably wondering how there could even be an oral surgery topic that could be specific to women’s health. There is a disease process that manifests far more commonly in women than men, and that is medication-related osteonecrosis of the jaw (MRONJ). This is because MRONJ is most commonly associated with medications that are used to treat osteoporosis, a disease which commonly occurs in women.
MRONJ has very specific diagnostic characteristics although it can be confused with other clinical conditions that cause delayed healing. Therefore, it is important to properly identify and diagnose this condition.
MRONJ is characterized by three findings:
(1) Exposed bone in the mouth lasting for greater than 8 weeks;
(2) In a patient who is either on or has received antiresorptive or antiangiogenic medications and who
(3) has never had radiation therapy to the jaws or metastatic disease to the jaws.
To clarify, these medications are used most commonly to treat osteoporosis, but they are also used to treat certain types of cancer. You may be more familiar with the common names of these medications such as Fosamax (alendronate), Actonel (risedronate), Boniva (ibandronate), Prolia (denosumab), Xgeva (denosumab), and Reclast (zolendronate) to name a few.
So what does this mean for you? According to the Centers for Disease Control and Prevention (CDC), 24.5% of women 65 years of age and older

have osteoporosis. Osteoporosis is caused by an increase in bone resorption and lack of equal or appropriate bone formation, resulting in weak bones. In patients who have osteoporosis that is severe enough to make them more susceptible to fractures, they may be prescribed medications and lifestyle modification. Some of these medications, such as those listed above, accomplish this by preventing bone resorption through a few different mechanisms. In this capacity, preventing worsening of osteoporosis, they are very effective and have been shown to improve bone density in these patients. This translates to a decreased risk of fractures of multiple bones, including the most highly susceptible, the spine and hip.
Alright, so what do you do if you’re already taking these medications or considering taking these medications for the treatment of osteoporosis? I’m sure your prescribing physician has discussed this with you already, but I want to reiterate that we recommend that you begin or continue routine dental care with a general dentist. While the exact mechanism for the development of MRONJ is not fully understood, we do know that it is more likely to occur in patients on these medications who undergo an invasive dental procedure, such as dental extraction or dental implant placement. In fact, oral surgery procedures are considered a “major risk factor” for development of MRONJ in at-risk individuals. That being said, it does occur in sites of chronic inflammation such as around bad teeth even without an invasive procedure being performed. Studies have shown that in patients who received dental screenings and preventative treatments prior to starting medications used to treat osteoporosis have a significantly decreased risk for the development of MRONJ when compared to patients who did not. Therefore, we strongly recommend that you establish and/or continue routine care with your general dentist for preventive treatment

30 OCTOBER 2020 fourstatesliving.com
and early identification of any need for oral surgery procedures prior to starting these medications.
Let’s talk about what to do if you are on these medications and you require oral surgical procedures. Rest assured, you’re not the first patient to present to our office in this situation. But, a frank discussion about your risks will be had at that time. The good news is that the risk of development of MRONJ is actually quite low. For oral forms of the medications, the risk of development of MRONJ after a dental extraction is 0.5%. For intravenous (IV) forms of the medication, this risk ranges from 1.6-14.8% (depending on which intravenous medication given). The bad news is that MRONJ, if not treated early or effectively, can become quite debilitating. Untreated MRONJ can result in chronically exposed dead bone, pain, infections, and potential jaw fractures requiring further surgical procedures which could include loss of adjacent teeth and removal of diseased gums/jaw bone.
That sounds scary, but I promise it’s not meant to be. I want to remind you that taking these medications does not mean you will automatically develop MRONJ. These medications are commonly prescribed and for a majority of patients their benefits outweigh the risk of development of MRONJ. In fact, when indicated, we extract teeth and place implants on patients who have taken these medications fairly often. If you have taken these medications, we will discuss the necessary precautions to minimize the chances of this complication during your initial visit. If you do find yourself requiring an oral surgery procedure and are being treated with these medications, it is important to seek out a trained oral and maxillofacial surgeon for your treatment. In this way, your risk may be maximally mitigated and potential complications that arise can be managed properly. Thank you for taking the time to read about MRONJ, and if you ever have any Oral and Maxillofacial Surgery needs please contact our office. We are always happy to help!
Dr. Mary Laura Hastings grew up on the Gulf Coast originally from Mobile, Alabama. She attended Auburn University for undergrad and received her dental degree from the University of Alabama Birmingham School of Dentistry. She spent one year after dental school in New Orleans, Louisiana, in a General Practice Residency at the LSU School of Dentistry where she decided to pursue a career in Oral and Maxillofacial Surgery. She attended LSU Shreveport Oral and Maxillofacial Surgery Residency for her training, graduating in June 2018. Since that time, she has been extremely fortunate to practice in Texarkana at Oral and Facial Surgery of Northeast Texas with Dr. Kirby Bunel, Dr. Jacob Duke, Dr. Zachary Legan, and Dr. Matthew Burks.

31 OCTOBER 2020 fourstatesliving.com

SCENE ABOUT TOWN
LADIES IN LEATHER PARADE & RALLY
The Ladies in Leather Parade & Rally was held Septemer 11-13 at the Texarkana Convention Center. Presented by Texarkana Harley, the event’s activities included a parade, musical entertainment by the Dirty River Boys, special guest speaker Dr. Saint James, nightly shows by Gary Michaels, Wrenching with Rocky workshop, guided rides, bladesmith demos, vendors, and a dance party with DJ Fabienne Thrash.







 Howie Wright, Sharon North, Jack Daugherty, Robin Mitchell and Madison Middleton
Jennifer Sievers, Amber Cohen and Kathy Winchester
Chief Perry, Jennifer Montoya, Amber Cohen and Bess Gamble-Williams
Amber Cohen, Bess Gamble-Williams and Dee James
Iron Maiden Riding Club – Michigan Chapter Howie Wright and Madison Middleton
Howie Wright, Sharon North, Jack Daugherty, Robin Mitchell and Madison Middleton
Jennifer Sievers, Amber Cohen and Kathy Winchester
Chief Perry, Jennifer Montoya, Amber Cohen and Bess Gamble-Williams
Amber Cohen, Bess Gamble-Williams and Dee James
Iron Maiden Riding Club – Michigan Chapter Howie Wright and Madison Middleton
32 OCTOBER 2020 fourstatesliving.com
Denise Haley


BREAST CANCER SURVIVOR, BARBARA
WALKER,
BATTLES
THE DREADED “C WORD” WITH COURAGE AND STRENGTH
photo by ALAMOND PHOTOGRAPHY
FAITH
STRENGTH FEAR BIGGER THAN
by SUZY TURNER
“When fear knocks, let faith answer the door.”– Robin Roberts

At 42 years old, Barbara Walker had heard the word “cancer” mentioned often. Her mother battled breast cancer in 1995, which resulted her having a double mastectomy. Her brother and best friend, Michael “Sumo” Sams, lost his fight with testicular cancer in January of 2009 at the age of 30. Additionally, September 7, 2017, Barbara heard the words again after the results of her annual mammogram showed she had ductal carcinoma in situ (DCIS).
After consulting with oncologist Dr. Lawrence Mendelsohn at the CARTI Cancer Center in Little Rock, Arkansas, Barbara found out that her DCIS was noninvasive and found very early. Cancer cells were found in Barbara’s milk ducts but had not spread to the surrounding tissues in her breasts. Her cancer was rated a Stage 0; her treatment plan would include a lumpectomy followed by radiation which she was able to have done here in Texarkana at New Hope Cancer Institute. “I had surgery on October 18 and started my radiation treatments almost three weeks later for five days a week which turned into seven weeks due to the holiday season,” she remembers.
Right after being diagnosed with cancer, Barbara admits feeling lost. “Here I was again faced with the very thing that I have fought so hard against for years through fundraising in memory of my brother. Except now, it was attacking my body. Hearing you have the ‘C word” is not easy at all. My experience with cancer had been the worst ... losing my bother in 2009 to Stage 4 cancer. I was in complete denial then,” she says. All kinds of thoughts and emotions went through her mind once she heard her diagnosis. Would her children be okay? Would she lose her hair (which is the one thing she loves most about herself)? Would she survive? Luckily, because of her participation in the American Cancer Society’s Relay for Life, Barbara had a sense of comfort knowing about the many services available to her and her loved ones if they were needed at any time.
After treatment, Barbara’s skin became dry, and her armpit area was very sore. She developed dark areas on her breasts that looked like burns and were very tender. She treated these areas with cream and gel every day while going through radiation. After about four weeks of treatment, she became very tired and lethargic, feeling the urge to sleep a lot.
Faith was the one thing that Barbara leaned on throughout her entire journey. She kept her cancer journey pretty private at the time. “I was very blessed. I did
The reason Barbara wakes up even on the hardest of days is because of her two children, Taylor-Anne and Jaxson.
35 OCTOBER 2020 fourstatesliving.com

not have to do chemotherapy or have a mastectomy. I was just very tired. Because I was private about my diagnosis, I did feel alone at times and very emotional,” Barbara admits. “But I think anytime you are going through something like this, you feel alone, even lost sometimes. With the love of my son, Jaxson, and daughter, Taylor-Anne, along with my close family and friends, I kept smiling and pushing forward. Without prayer and my relationship with my Heavenly Father, I do not think I would have been so blessed,” Barbara admits.
Having a great support system eased Barbara’s mind and helped her mentally and physically. Friends and family pitched in to help take care of her young son and even bring food to her and her family. Her employers at Hilton Garden Inn, Jack and Brian Daugherty, allowed her to rest when needed and offered for her to take off from work whenever she needed a break. The general manager, Dennis Havranek, even set up a surprise celebration the day Barbara completed radiation. “Jack and Brian always said, ‘Take care of you first.’ It was hard ... my body was tired, but I pushed through. Being surrounded by both positive, spiritual, and uplifting people only made my journey easier,” she explains.
Barbara finished her radiation treatments on January 12, 2018, and on January 29, she was told she was cancer-free! Now, she goes to the oncologist every six months for follow-up care and will continue on hormone therapy treated with tamoxifen for five years total to help prevent reoccurrence.
Although cancer may have slowed her down for a few months, Barbara’s zest for life never wavered. Cancer-free for a little over 2-1/2 years now, she admits that she currently looks at life a little bit differently. Many things that once bothered her no longer matter, and taking care of those she loves is her life’s mission. She concludes, “I just love the Lord and focus on the little things in life like sweet tea and belly laughs with my children.”.
 Team Sumoas at Relay for Life 2018
Team Sumoas at Relay for Life 2018
36 OCTOBER 2020 fourstatesliving.com
Jaxson shows off his “I wear pink for my Mom” t-shirt.



37 OCTOBER 2020 fourstatesliving.com
During October 2018, Barbara and her team celebrated breast cancer awareness during Pink Out Day.

SCENE ABOUT TOWN
ONE LOVE YOGA OPEN HOUSE
One Love Yoga held its Open House on September 18 at their studio on Richmond Road. The Texarkana Chamber of Commerce held ribbon cutting ceremonies, while attendees enjoyed meeting the instructors, shopping, and refreshments.










 Jill McMahon, Natalie Haywood and Kenzie Teel
Jill McMahon and Joey Martin
Donovan Driver and Dr. Jim Booker
Janelle Williamson, Judy Sander and Carla Moon
Karen Mote and Allison Wright
Jim Bynum and Brittney Brookes
Faith Dossey and Lindsey Woodson
Dr. Jim Booker and Annemarie Sullivan
Toni and Jay Crabtree
Dr. Jim and Lauren Booker
Jill McMahon, Natalie Haywood and Kenzie Teel
Jill McMahon and Joey Martin
Donovan Driver and Dr. Jim Booker
Janelle Williamson, Judy Sander and Carla Moon
Karen Mote and Allison Wright
Jim Bynum and Brittney Brookes
Faith Dossey and Lindsey Woodson
Dr. Jim Booker and Annemarie Sullivan
Toni and Jay Crabtree
Dr. Jim and Lauren Booker
38 OCTOBER 2020 fourstatesliving.com



WARRIOR IT’S HARD TO KEEP A DOWN
PHOTOGRAPHY
photo by ALAMOND
T-Shirt by BRISTOW DESIGN CO.
DESPITE NUMEROUS BRAIN SURGERIES
CAUSED BY IDIOPATHIC INTRACRANIAL HYPERTENSION, MARYSSA REESE STAYS POSITIVE, EVEN ON HER TOUGHEST DAYS
Imagine each morning having the worst headache ever.
Imagine each morning having fears about your vision before you even open your eyes.
Imagine each day having problems with nausea, balance, memory, and ringing in your ears.
Imagine having such severe symptoms that your normal life and job are next to impossible.
Imagine having a difficult time finding knowledgeable medical professionals.
Imagine having multiple spinal taps and possible multiple shunt surgeries.
Imagine how this changes your whole world.
Imagine having hope for a cure.
Please spread HOPE and AWARENESS for Intracranial Hypertension.
- A meme created by Angie, a fellow IH patient
by JILEEN PLATT
Maryssa Reese, a 32-year-old native of Texarkana, thought for years she just suffered from migraines. After a routine visit to her eye doctor in 2014, she was informed that something else might be causing the headaches. “I was told that my optic nerves were swollen, and I possibly had a massive tumor,” says Maryssa. After being sent to Ochsner LSU Health Shreveport to see a neuro-ophthalmologist, an MRI was performed. Thankfully, this confirmed no tumor, but a spinal tap was needed for further diagnosis. “Normal pressure for cerebrospinal fluid (CSF) should be about 10-15 mmHg. Mine was at 48 mmHg!” exclaims Maryssa.
That is the day that Maryssa was told that, unlike most brains that regularly produce and absorb CSF to maintain a correct pressure, her brain creates too much fluid and has difficulty absorbing it. Her neuro-ophthalmologist confirmed that she had Idiopathic Intracranial Hypertension, IIH (or IH for short), also previously called Pseudotumor Cerebri. Regardless of the name, it is an uncommon, misunderstood disease, with little research funding, and currently no cure.
“I was first put on [medicines to help control the pressure] but started going blind because they weren’t reducing the pressure or the CSF amount,” states Maryssa. The next best option was a cerebral shunt, or piece of narrow tubing surgically placed in Maryssa’s brain and thread under the skin to specific areas of her body to drain. A small valve, surgically placed on Maryssa’s head, helps regulate CSF drainage and pressure.
Shunts that drain into the abdominal cavity are the most common. Out of 12 shunt surgeries that Maryssa has had, at least six have been abdominal shunts and revisions. The most recent abdominal shunt resulted in her body storing the excess fluid instead of soaking up the fluid and releasing it as urine. “My abdominal tissue is hostile to the CSF… I [felt like I] had gallons of fluid stored in my abdominal tissue. I looked like a woman carrying quadruplets,” exclaims Maryssa. “My neurosurgeon had never seen anything like that before.”
Shunts in her pleural cavity (lung area) have had additional complications. “One time I woke up in the middle of the night not able to breathe … my husband, John Michael, got me to the ER,” says Maryssa. “I had a pleural

41 OCTOBER 2020 fourstatesliving.com
effusion, pneumonia, MRSA (Methicillin-resistant Staphylococcus aureus) in my lung cavity, and so much fluid … that it was pushing on my heart … I almost died that time. Had we waited much longer [to get to the ER] I wouldn’t have made it because I was drowning.” Maryssa stayed 32 days in the ICU to recover. She had three different brain surgeries during that time, including an external shunt surgery to allow her excess CSF to drain into a bag hanging beside her bed.
Since both abdominal and pleural shunts did not work for Maryssa, she and her doctor decided that a shunt to her heart was the next and last option. “The tubing is thread through my jugular and sits inside my right atrium,” explains Maryssa. While there are occasional adjustments to her heart shunt, this area has worked the longest in her almost 6-year battle with IH, and coincidentally it has had the least complications.
“My support system through all of this is so great,” says Maryssa. “Between my husband, mom, grandparents, in-laws, and my dad and bonus mom … it’s amazing … even my son, Brayden, knows more about brain disease than any 10-year-old should. He is my biggest motivation!” Maryssa is also part of an IH Facebook group that shares memes and encouragements about the rare disease. Friends have continued to support and listen to her on her especially hard days “and my dad often calls just to pray with me and sends me scriptures when I’m having bad pain days,” states Maryssa. “I always know he’ll know the right scripture just to help my day.”
Maryssa continues to stay positive. “Honestly, there’s no point in NOT being positive,” she says. “No one wants to be around or listen to someone mad at the world.” Maryssa’s most inspiring religious sayings are, “God has never given anyone more than they can handle” and “All is well with my soul.” With these guiding encouragements she knows she can persevere.
A few months ago, on July 5, 2020, Maryssa began experiencing seizures, resulting in her husband calling an ambulance. At CHRISTUS St. Michael Health System’s emergency room she continued to have complications and more seizures. Maryssa stopped breathing and was intubated, then flown to Ochsner LSU Health Shreveport. “For seven days I was in a coma … my brain shut down. My doctor believed that my brain needed a rest,” says Maryssa. She was on a ventilator for 12 days and in the hospital for 16 days. When finally released, Maryssa had to use a walker because her muscles had atrophied. Every day home now she continues to heal, but it isn’t an easy road.
While Idiopathic Intracranial Hypertension affects only about 1 per 100,000 people every year, Maryssa Reese is one of the faces that bears this rare and difficult disease. She suffers on a regular basis, but chooses to hope. “Shunts are just a Band-Aid,” states Maryssa. “What I really want is a cure. It’s a rough disease and some may have it and never know until it gets really bad. I hope for more research and awareness so others won’t have to suffer like I have … all I’ve ever wanted to do is spread awareness … and help others to not feel alone in this journey.”






 While in the ICU during February 2018, Maryssa had an external shunt (a drain that pulls csf from the brain) for two weeks.
John Michael and Maryssa in 2016 when they took Brayden to WrestleMania.
Brayden was so excited for his mom to be home following her 32-day ICU stay in 2018.
Tattoo artist Jessica Dillard designed this tattoo of the IIH ribbon for Maryssa, so on her bad days she can always look down and remember that she is a warrior.
Maryssa in 2018 after having her third brain surgery in one month plus a 32-day stay in ICU after having MRSA, pleural effusion, and pneumonia.
Six weeks prior to this photo of Maryssa before her brother’s wedding this past August, Maryssa was in the hospital on a ventilator and in a coma for over a week.
While in the ICU during February 2018, Maryssa had an external shunt (a drain that pulls csf from the brain) for two weeks.
John Michael and Maryssa in 2016 when they took Brayden to WrestleMania.
Brayden was so excited for his mom to be home following her 32-day ICU stay in 2018.
Tattoo artist Jessica Dillard designed this tattoo of the IIH ribbon for Maryssa, so on her bad days she can always look down and remember that she is a warrior.
Maryssa in 2018 after having her third brain surgery in one month plus a 32-day stay in ICU after having MRSA, pleural effusion, and pneumonia.
Six weeks prior to this photo of Maryssa before her brother’s wedding this past August, Maryssa was in the hospital on a ventilator and in a coma for over a week.
42 OCTOBER 2020 fourstatesliving.com

DIABETES SCREENING is Key To Early Detection
by LEE ALISON MCCRARY, AGNP-C
As a Nurse Practitioner in a rural primary care clinic, I see women of all ages, races, and cultural backgrounds. Health screenings, disease process management, and education is an important part of maintaining and promoting health. In the clinic, I encounter patients with undiagnosed diabetes almost daily. Diabetes is a major concern in this area, particularly Type II diabetes. About 1 in every 9 adult women have diabetes. Although diabetes affects men and women equally, in Bowie County women have a higher incidence than men. Worldwide, women are more severely impacted by complications of diabetes. Women are at higher risk for heart disease, blindness, kidney disease, and depression from the complications of diabetes. Heart disease is the most common complication of diabetes experienced by women, and it is increased
by about four times that of men.
Both men and women may experience the following symptoms of undiagnosed diabetes: increased thirst and hunger, frequent urination, sudden weight gain or loss, fatigue, blurred vision, frequent infections, and breath that has a sweet or fruity odor. Women experience many of the same symptoms as men; however, some symptoms are unique to women. These include frequent vaginal and/or oral yeast infections, urinary infections, and sexual dysfunction. Risk factors exclusive to women include a history of gestational diabetes and polycystic ovary syndrome (also known as PCOS). If you are experiencing any of these symptoms, please speak with your physician and ask them about being screened for diabetes.
Although knowing the symptoms of diabetes is important, screening is key to early detection. Many women do not experience symptoms and often go years before they are officially diagnosed. The earlier diabetes is diagnosed, the better your chances are of reducing irreversible complications. Screening should begin at age 40. If you are obese or have other risk factors, screening should begin earlier than 40. Typically, diabetes is screened for and diagnosed with a HgbA1C test. This is a simple fingerstick blood sample, and results of this test can be received at your appointment.
There is no cure for diabetes. Once you have been diagnosed, you can only manage your symptoms. This includes diet, exercise, and behavioral/lifestyle changes. If these interventions fail, medications are prescribed, along with lifestyle modifications, to manage symptoms and prevent complications. I have found that people are very hesitant and often unwilling to make changes in their diet or lifestyle, but it is my responsibility to make them aware of the importance in making these changes and consequences if they do not follow through.
It is vital for women to maintain a healthy weight and stay active to lower their risk of diabetes. If you are over 40, at your next appointment with your physician ask to be screened for diabetes. If you have already been diagnosed with diabetes, you should take your medications as prescribed, make regular follow-up appointments, and stay active.
Lee Alison McCrary has worked at De Kalb Physicians Clinic since 2016. She has two children, Adison (14) and Titan (9), who attend De Kalb ISD and are very involved in sports. They love to travel as a family, and Lee Alison admits that her kiddos keep her grounded.
44 OCTOBER 2020 fourstatesliving.com

NELDA TIMMONS MAKES SURE THAT EACH DAY FORWARD COUNTS FOR SOMETHING IN LIFE AFTER HER BATTLE WITH LEUKEMIA

by
photo
ALAMOND PHOTOGRAPHY
healing The Gift Of
by LISA PORTERFIELD THOMPSON
Seeing your child’s college graduation, getting a promotion at work, watching your daughter walk into a room in her gorgeous Homecoming dress … all these are milestones that we sometimes take for granted. We know we want to be present for them, but we do not often realize how quickly they could disappear, or worse yet, never materialize at all.
For Nelda Timmons, these moments could have easily been missed had her journey with leukemia ended differently. Her brave battle against the disease started in the fall of 2008, the night of Pleasant Grove’s Homecoming game. She was diagnosed a few short days later with a rare aggressive form of the disease called Acute Promyelocytic Leukemia (APL).
“Some people with APL die before they ever know what they have,” Nelda said. “Fortunately for me, I was in the care of fast-acting providers that knew where I needed to be. MD Anderson told me, had I waited until Sunday without the immediate treatment, I would not have survived to see Monday. It was that close of a call.”
On Thursday, Nelda was in Little Rock leading a meeting with her sales team, and by Saturday night of the same week, she was fighting for her life in Houston at MD Anderson. To this day, according to Nelda, the first 72 hours of her journey is still a blur.
“I had been to the doctor earlier in the week regarding some minor symptoms and bruising,” she said. “I knew something was wrong but had no idea what was in store for me. I was thinking I may be anemic or something. While in Little Rock [for work], my doctor called me to tell me he spoke to a specialist in town. He said they did not want to scare me, but this was presenting like leukemia. He thought it best for me to go to the hospital for some tests to rule it out. My response was, ‘I can’t go to the hospital now, I am out of town and in the middle of a meeting.’ I wanted to wait until Monday because we had big plans for the weekend – it was my daughter’s senior year Homecoming weekend. We had a football
47 OCTOBER 2020 fourstatesliving.com
game, Homecoming dance, pictures, and more. I simply did not have time for this. Nonetheless, Dr. Blane Graves talked me into going to the hospital first thing Friday morning. I was still thinking it would be a quick in and out kind of day, but that’s not quite how it worked out.”
In a single day, Nelda’s blood work was showing aggressive changes each hour. Some friends and church members happened to be in the hospital and circled around her to pray. “It was then I realized my life as I knew it was about to change,” she said.
By Saturday evening, local oncologist, Dr. Gary Engstrom confirmed the diagnosis and explained to Nelda the seriousness of what was happening. For him to confirm what type of leukemia she had, he would need to send out for lab work which would take a couple of days to return. As rapidly as her platelet counts were falling, he said she needed to get to a facility that had a lab onsite so the provider could have the results within hours, not days.
Options were discussed and Nelda chose to seek treatment at MD Anderson Cancer Center in Houston, Texas. “My daughter was at dinner before her Homecoming dance when her dad called to tell her she needed to come to the hospital immediately,” Nelda said. “She came into my hospital room still wearing her Homecoming dress. I remember thinking how beautiful she looked, and then we dropped a bomb on her that changed her world as she knew it. My mom was there to console her, and we then spoke with my niece who is like a daughter to me. We cried together, then I was on my way to MD Anderson. We left, leaving Taylor and her dad to figure out the details of how we were going to manage all this.”
By the time Nelda, her mom, and a family friend loaded up in the car, she was starting to experience the results of the low platelet count,

and severe pain set in, as head bleeds were starting to occur. “I cannot describe the headache,” she said. “Bruises would just appear out of nowhere. My mom sat in the back of my reclined seat and literally held my head in her hands to comfort me for the hours it took to get to Houston. Upon arrival, the leukemia team met me outside and immediately started giving me high doses of medications before I even crossed the threshold.”
Nelda began her journey that weekend, but the battle against leukemia would rage on for more than 10 months of treatments, while she endured six days in the ICU, a month-long hospital stay, and daily appointments for treatments. The treatment for APL is a cycle of daily infusions of a medication derived from Arsenic, along with a potent oral drug called ATRA.
“Yes, the treatments are from Arsenic, the same ingredients used in rat poison,” Nelda said. “The treatments in the months to follow were grueling, but effective. Although, I felt terrible, the platelet count and other numbers were on the rise. The chemo nurses and doctors that cared for me in Texarkana were positive and motivating. I was known as the “arsenic patient.” Being there every day, I really got to know the staff and learned the schedule of other patients. One patient in particular helped me deal with survivor’s guilt, which was a real struggle for me. As our treatments went on, I continued to improve as he declined. He said although he knew he was losing his battle, me getting better made him happy in knowing that there are people that win the battle. He advised me to keep moving forward and live on for people like him and send a message that cancer can be beaten. He was such an encourager and cheered me on as long as he had the strength to do so. Ironically, I received my last treatment on the day of his funeral – I knew he would find that satisfying and it made his spirit smile. His advice to keep moving forward was some of the best I have ever received, and I still practice that philosophy when faced with other challenges in my life.”
Nelda said that after completing treatments it took her years to feel normal again, and that she still feels side effects from time-to-time. She said life since leukemia has had its ups and downs, but mostly has been good. “I learned many things through my battle with leukemia,” Nelda said. “First and foremost is the power of faith in God. I had a warm peace from the beginning, during the first prayer circle, and knew I was going to be okay. I did not know whether I would live or die,

48 OCTOBER 2020 fourstatesliving.com
Nelda (right, holding baby Garren Russell) and her niece, Chalissa Russell; mother, Owetta Walton-Bost; and daughter, Taylor Timmons, celebrating her mother’s retirement in September 2015.
but either way, I knew I would be okay because of my faith.
“I also learned the people of Texarkana really know how to rally with support and encouragement during dark times,” she said. “I was so humbled by the generosity and love offered to me and my family. We had needs met before I even knew we had them. Special friends and church members planned for housing in Houston, transportation, flights for Taylor. My Bunko girls put together a big bright box full of miscellaneous items that I called my ‘happy box.’ When my feet were cold, there were socks in the happy box. If my lips were dry, there was ChapStick in the happy box. They thought of everything. They set up a CareBridge page to help with communications and updates. Cards arrived by the dozens at the hospital. People wore orange



Since Sweden has always been on Nelda’s bucket list, she and Taylor took a motherdaughter trip there during August 2019. Here, they are in Stockholm with Julia Stridsberg, a PG exchange student they hosted shortly after Nelda’s remission.
 Nelda, her father, Johnny Walton, and daughter, Taylor, during a 2016 gathering in Ft. Worth to participate in an 80th birthday surprise party for a family member.
Taylor graduated from Savannah College of Art and Design (SCAD) in May 2015. Nelda admits that this is one of the proudest moments she has had as a mother.
Nelda, her father, Johnny Walton, and daughter, Taylor, during a 2016 gathering in Ft. Worth to participate in an 80th birthday surprise party for a family member.
Taylor graduated from Savannah College of Art and Design (SCAD) in May 2015. Nelda admits that this is one of the proudest moments she has had as a mother.
49 OCTOBER 2020 fourstatesliving.com
bracelets, ran awareness marathons and had blood drives in my honor. I received handmade angel quilts, which were a godsend during the infusions. Teachers showed up at the house to check on Taylor. Our lawn was automatically cared for, and the list goes on and on. There is no way I can ever repay such acts of kindness. I am forever grateful for my caring network of friends and family. All I know to do is try to pay it forward.”
Not every battle with such a nasty disease ends as well as Nelda’s did, but one thing is for sure – she has not taken for granted the gift of healing and life she has been given. She is making sure that each day forward counts for something in life after leukemia. <<<



 Taylor and Nelda making silly faces in 2011 ... this photo is Taylor’s all-time favorite picture of them because she was finally getting her mom back after that Homecoming night when their lives were forever changed.
The Timmons’ family Halloween Party has been a lifelong tradition. Nelda’s daughter, Taylor, has now been named as the hostess.
Taylor and Nelda making silly faces in 2011 ... this photo is Taylor’s all-time favorite picture of them because she was finally getting her mom back after that Homecoming night when their lives were forever changed.
The Timmons’ family Halloween Party has been a lifelong tradition. Nelda’s daughter, Taylor, has now been named as the hostess.
50 OCTOBER 2020 fourstatesliving.com
Nelda’s awesome friends held a surprise 50th birthday. She felt blessed and thankful that she was able to reach this milestone.

DOCTOR, DO I NEED A HYSTERECTOMY?
by DEBORAH SHUMAN, M.D.
Okay, ladies, let’s be frank. No one enjoys “that time of the month.” For some women, their periods can be torture. This can range from debilitating pain to heavy cycles that prevent even leaving the house. If you are one of those women who can’t leave your home without a travel bag filled with supplies, you know what I mean. While I always advocate for medical management for these type of female problems, sometimes surgery can be necessary.
Several conditions can cause a woman’s menstrual cycle to become agony each month. Most of these issues are benign and include uterine fibroids, polyps, and hormonal imbalances. However, precancerous and cancerous cells in the uterus can cause similar symptoms. That’s why it is so important to get in touch with your healthcare provider to establish a diagnosis (that is, what’s causing the problem) and

devise a treatment plan. You don’t have to suffer.
Are there other reasons a woman might need a hysterectomy? In addition to uterine fibroids, endometriosis and prolapse can be indications for surgery. Fibroids are benign growths on the uterus. They can cause heavy bleeding, pain, and pressure among other symptoms. Endometriosis can cause pelvic pain and infertility. Prolapse occurs when the tissue supporting the uterus becomes lax, causing it to drop. This can create a bulge or pressure sensation. Prolapse can also cause issues with your bladder or bowels. In addition, abnormal pap smears, precancerous and cancerous conditions of the uterus, cervix, or fallopian tube, or ovary can warrant a hysterectomy. Sometimes, minimal or no symptoms are present. This is why yearly checkups are so important!
Oftentimes prescription medications and other treatments can improve symptoms and a woman’s quality of life substantially. Medical treatment is often indicated in women who have not had children yet or still want to have more babies. However, some female issues may be best treated with surgical interventions. Fortunately, there are options! For some women, a traditional “abdominal” or “open” hysterectomy may be necessary. This is where an incision is made on the abdomen to remove the uterus. This can include a “partial” hysterectomy where only the uterus and cervix (the opening to the uterus) are removed. It can also include a “full” hysterectomy, where the uterus, cervix, fallopian tubes, and ovaries are all removed. Usually a woman is admitted in the hospital for 2 to 3 days after surgery. After going home, generally the recovery lasts about six weeks. For many women, a less invasive hysterectomy can be an option. This includes vaginal and laparoscopic hysterectomies. Full and partial hysterectomies can be performed with these methods. For my patients, I use the da Vinci robotic system. This allows for smaller incisions and a quicker recovery, getting you back to your family/job/life sooner! Most women can return home in one day or less, and some can be back to work (think desk jobs) within two to three weeks! A hysterectomy can change a woman’s life when she has been suffering with heavy, painful periods for months (or even years!). There are several factors to consider when deciding which type of hysterectomy is best for you, and your gynecologist can discuss all the options with you.
Frequently, women are so busy with their families and careers that they put off going to the gynecologist. However, taking care of yourself is just as important as taking care of others in your life. If it has been more than a year since your last exam, or if you are suffering from female problems, it is time to schedule a checkup!
For 11 years, Dr. Deborah Shuman has been board certified in Obstetrics and Gynecology. She moved from Louisiana to Texarkana over a year ago to be closer to family. Dr. Shuman is currently on staff at Texarkana OB/GYN and affiliated with Wadley Regional Medical Center. She is married and has two daughters, ages 13 and 11. In her spare time, she enjoys running, cooking, baking, and reading.
52 OCTOBER 2020 fourstatesliving.com

 by ELLEN ORR
by ELLEN ORR
Kicking to the curb! Cancer
AFTER KIM HORNBUCKLE’S BREAST CANCER DIAGNOSIS, SHE BECAME PROACTIVE AND TOOK CHARGE OF HER HEALTH
Annual mammograms for women over 40 reduce overall breast cancer mortality by about 40 percent (according to breastcancer. org)—and yet, despite this fact, it is estimated that only 72 percent of all American women ages 40–85 have had a mammogram within the last two years; the numbers in Texas and Arkansas are even lower than the national average (Kaiser Family Foundation).
Redwater teacher and counsellor Kim Hornbuckle prided herself on being a part of that 72 percent. Whether at Wadley or Collom & Carney Clinic, she always scheduled her annual mammogram every summer, “as many educators do because we don’t usually have time during the school year,” she said. “I had always been diligent about getting regular mammograms in the past.”
In June of 2017, for the first time, her routine mammogram results came back irregular. Kim assumed the recommendation for a second mammogram was a formality based on an abundance of caution. “I wasn’t even going to get the second one until a friend convinced me that I should, just for peace of mind,” Kim said. The second mammogram confirmed the presence of a tumor; she needed a biopsy.
After the biopsy, Kim refused to wait for the results. “Instead of waiting for my appointment [with the surgeon] the following week, I called and asked for my results,” she said. “I was told that this is not something they customarily do, but I wasn’t concerned about customs. I persisted, and on July 28, 2017, I was told over the phone that I had breast cancer.
“My daughter [Sydney, then-14] was sitting beside me and listening to the phone call. She asked me, ‘Mom, are you going to die?’”
Kim was in disbelief; she judged herself to be typically healthy, had no family history of breast cancer, had no lumps, showed no signs. “I even asked if they had possibly gotten [my results] confused with someone else’s,” she recalled.
The standard path forward was for her doctor’s office to refer her to a breast cancer specialist, “but I was not about waiting [for a referral],” Kim said. “I gathered all of my scans and results and started making phone calls.”
When Kim connected with a specialist, she was presented with two options, one being a bilateral mastectomy. “Although I discussed my options extensively with my husband, there was never really a doubt in my mind what the best option was for me,” Kim said. “I opted to have the mastectomy and reconstruction and rid myself of this.”
On August 9, Kim underwent a five-hour surgery to remove the breast tissue and implant “expanders” for eventual reconstruction. “My mom, dad, sister, and brother-in-law waited on me in the hospital,” Kim remembered. “Theirs were the first faces I saw, and that made me happy. I had so many people praying for me and checking on me daily. My husband has been my rock, in more ways than he can imagine. When I saw my scars in the mirror the first time, he caught me, literally, because it was such a shock. My daughter stepped up when she was needed and went above and beyond what most kids her age would do to help.”
Motivated by a desire not to miss any part of her daughter’s life, Kim began an active post-op recovery. “A week after my surgery, I was at a volleyball game


Not quite a year after she found out she had breast cancer and five months after all surgeries were completed, Kim enjoyed a vacation trip to Virginia Beach.
 Kim, Sydney and Bruce in 2017, three weeks before Kim found out she had breast cancer.
Kim, Sydney and Bruce in 2017, three weeks before Kim found out she had breast cancer.
55 OCTOBER 2020 fourstatesliving.com


to watch Sydney. Two weeks later, I was at a cross-country meet and then at a football game to watch Sydney cheer. I was back at work three weeks after the surgery,” Kim said. “We went on with life.”
Despite Kim’s quick return to her day-to-day, the reconstruction process took six long months. Every three-to-four weeks, she underwent tissue expansion, preparing her for a final reconstructive surgery. “The expansion was the worst and most painful part of the ordeal,” Kim said. “Most days, I felt like an
elephant was sitting on my chest.” In January, a final surgery completed the reconstruction.
In February, Kim was told that she needed no further treatment. “I came out okay thanks to early detection,” Kim said. “I’m an intensely private person, and I wasn’t going to do this [story because of that], but, as I discussed it with my husband and daughter, my daughter said, ‘If you could help just one person understand the importance of regular mammograms, then it would be worth it.’ Hopefully someone will see this and understand that, if I had not had mine detected so early, it could have been so much worse.”
Scheduling and enduring annual mammograms was the first of many proactive decisions that led to Kim’s survival and recovery. “I learned the importance of taking charge of your own health and advocating for your own medical care,” she said, referring to her assertive approach of retrieving results and seeking out specialists—and then making the brave, swift choice of a double mastectomy.
“I feel healthy and well now, and if I had to make the decision again, I would do exactly the same thing,” she said.
 Bruce, Sydney and Kim at the Redwater football field during September 2017, six weeks after Kim’s bilateral mastectomy.
Completely recovered and back to her active lifestyle, Kim and her family enjoyed hiking Mt. Quandary in Breckenridge, Colorado, during the summer of 2019.
Kim completed her reconstruction during early 2018. This photo of her and Sydney was taken a few weeks after the surgery.
Bruce, Sydney and Kim at the Redwater football field during September 2017, six weeks after Kim’s bilateral mastectomy.
Completely recovered and back to her active lifestyle, Kim and her family enjoyed hiking Mt. Quandary in Breckenridge, Colorado, during the summer of 2019.
Kim completed her reconstruction during early 2018. This photo of her and Sydney was taken a few weeks after the surgery.
56 OCTOBER 2020 fourstatesliving.com

KELSI ALLEN HAS LEARNED TO CONTROL HER DIABETES INSTEAD OF LETTING IT CONTROL HER
photos by ALAMOND PHOTOGRAPHY
GOD Wants Her to Be Right Where
by SARA ROTHWELL
Kelsi Allen was introduced to the medical field at a young age because she was diagnosed with Type 1 diabetes when she was just 5 years old. She was born and raised in Texarkana, and many of her role models were medical professionals. She has learned from them throughout her life and continues to grow in her knowledge and abilities as she now works with them in the medical field. Kelsi’s childhood dream was to help people like her who have diabetes. She says, “I think it makes a world of difference when you can empathize with people because you have walked in their shoes.”
Kelsi has been blessed with amazing parents that have been great role models throughout her life. Her father works as a Nurse Practitioner at Family Medical Group and has been a nurse for as long as she can remember. Her mother is a teacher and currently a professor at Texarkana College. Kelsi has a little brother, two sets of grandparents, “two adorable dogs and one crazy cat,” that she couldn’t imagine life without!
After graduating from Texas High School in 2015, Kelsi moved to Conway, Arkansas, with a plan to study nursing at the University of Central Arkansas. She completed all prerequisites after her first year but unfortunately was put on the waitlist for UCA’s nursing program. Kelsi was heartbroken about this news, and after multiple talks with her family, she had been convinced that she should at least apply to Texarkana College’s nursing program. “I waited until the last day to put in my application, and not even a week later was accepted. After a lot of tears and many prayers, my gut, which is never wrong, told me I needed to move back home,” Kelsi admitted.
Soon enough, Kelsi started the Associate’s Degree in Nursing (ADN) program at TC, and she says it was the best decision she made that year! In the process, she met her best friend who currently works as a nurse in the ICU with her. Kelsi was also able to learn from what she says are some of the best professors out there.
During May of 2019, Kelsi graduated from TC with an amazing support system behind her. Soon after graduation, she started her dream job as an ICU nurse. Kelsi says, “I am currently working in the Cardiovascular Intensive Care Unit and CHRISTUS St. Michael Health System as an RN, and I love it!”
As a Type 1 diabetic, Kelsi feels as though some people are uninformed about the subject which can lead to misunderstanding. A Type 1 diabetic is a person whose pancreas does not produce insulin. Controlling their blood sugar with a low carb diet or taking a pill is not an option. Their bodies convert everything they eat into sugar, that is glucose. When the glucose rises, the pancreas is supposed to release insulin which is what the human body uses to
convert glucose into energy. Type 1 diabetics have to do the job of their pancreas since it can’t on its own. Kelsi explains, “If we do not control our blood sugar by taking the correct dose of insulin, the glucose stays in the bloodstream and can cause further complications that are very dangerous.” Stress, sleep, hormones, exercise, mood, and many other things affect blood sugar levels. Depending on what your life looks like, your body needs different amounts of insulin every day. This makes it difficult for people like Kelsi to control their blood sugar levels in a convenient way.
Despite her diabetes, Kelsi has always been active. She played travel soccer when she was 8 years old until she turned 14 and made the varsity soccer team as a freshman in high school. She is currently a member of CrossFit Texarkana

 T1D has shaped Kelsi into the person she is today. She shares that this photo reflects her the most. Taken on the Texarkana College campus in her TC scrubs, this photo shows her insulin pump in her right hand and the continuous glucose monitor (aka Dexcom) in her left arm.
CrossFit Texarkana is the place Kelsi goes to relieve stress. She loves working out and enjoys being around people who push her to be better every day.
T1D has shaped Kelsi into the person she is today. She shares that this photo reflects her the most. Taken on the Texarkana College campus in her TC scrubs, this photo shows her insulin pump in her right hand and the continuous glucose monitor (aka Dexcom) in her left arm.
CrossFit Texarkana is the place Kelsi goes to relieve stress. She loves working out and enjoys being around people who push her to be better every day.
59 OCTOBER 2020 fourstatesliving.com


Attending K.I.D.S. Day Camp has served as one of Kelsi’s biggest support systems. She attended for the first time at age 5 (pictured here with friend, Kaylee on the right) in 2002 and has gone back every summer since then. She nows serves as a counselor/group leader for the kids.

where she continues to try and stay healthy and fit. She is very conscious of what she puts in her body, even though she can eat whatever she wants just as long as she takes the correct amount of insulin. “I choose to eat healthy in order to make things easier for me and my body,” says Kelsi.
Since technology continues to advance, Kelsi is very thankful for the devices that help her manage her diabetes through her everyday life. She wears an insulin pump and a glucose monitor which allows her to continuously check her blood sugar levels. Kelsi says she prays daily that there will be a cure someday, “but until then I will continue to show people how I control this disease instead of letting it control me.”
COVID-19 has not made being a brand new nurse easy for Kelsi. Through this pandemic she continues to grow in her abilities as a nurse and become a stronger woman every day. Having an autoimmune disease makes her more susceptible but, “I work with the best team of nurses who make challenges like these seem easy,” acknowledges Kelsi.
Kelsi has learned so much more about herself through the challenges she has faced this year. She’s been encouraged to push herself more than she ever thought possible. Empathy, compassion, respect, and integrity are only a few things that Kelsi’s patients and their families have taught her. She has thoroughly learned how to manage stressful situations with a good attitude and think critically when need be. At first, it was overwhelming for her to know that people’s lives were depending on her. After the first few weeks of work, Kelsi was questioning if she could really be a nurse. She soon realized that God had her right where he needed her to be. “When I spend four, 12hour shifts with a very critical patient, and I get to see them leave the ICU, it’s the most rewarding feeling and makes me realize how lucky I am to be able to do what I do,” remarks Kelsi.
Her future plans include going back to school and getting another degree. Kelsi is unsure what degree that will be but the thought of the unknown excites her. “I am looking forward to seeing where life takes me!” she exclaims.
 Kelsi (right) with her brother, Conner, and parents Melanie and Steve, during their 2018 summer vacation to Fort Walton Beach, Florida.
July 5, 2020, marked Kelsi’s one year anniversary of nursing.
Kelsi (right) with her brother, Conner, and parents Melanie and Steve, during their 2018 summer vacation to Fort Walton Beach, Florida.
July 5, 2020, marked Kelsi’s one year anniversary of nursing.
>>>
This group photo was taken at K.I.D.S. Day Camp held at the Texarkana Fun Park in 2016.
60 OCTOBER 2020 fourstatesliving.com

EXQUISITE INTERIORS
TIMELESS. CONVERSATIONAL. REFINED.
BY SUZY TURNER. PHOTOS BY SARA ROTHWELL.

Melissa Keil’s 4 bedroom, 4 bath Pleasant Grove home features a mix of timeless beauty and grace. Even though the home was originally built around 1986, this refined space never goes out of style. Located on three beautiful wooded acres, the comfortable home easily blends contemporary and modern styles while celebrating natural materials, earth tones, and minimal detailing.
A circular drive leads up to the immaculate home while a beautiful freeform fountain area adds soothing sounds heard while walking up the sidewalk. Melissa handpicked these large rocks from a limestone quarry in Idabel, Oklahoma, on land her father owns. Many of the rocks resemble formations you don’t see every day, including the state of Texas, a monster, and a ghost.
Mementoes from Melissa’s travels with her daughters, Jayce and Erin, are found throughout the home. Accessories from Colorado to Italy to Bali to Peru bring in colorful design elements while adding to the home’s character and personality. Melissa’s love and appreciation for art is evident while meandering throughout the tranquil space.
In the master bedroom, a beautiful four poster bed holds regal bedding in jewel tones. Area rugs
from Turkey serve as the foundation to the elegant space. A dual rotational ceiling fan provides air circulation and is a great conversation piece. The attached bath features granite flooring, marble countertops, and a porcelain tub original to the home. Decorator Jeff Brown’s knack for design is apparent as elegant fixtures and massive framed mirrors add the perfect touch, and Kathi Couch art complements the color scheme of the room.
Although the living area is eclectic, the perfect combination of design elements, including furs, artwork, and animal wall mounts, mix seamlessly. A tabletop sculpture from Bali adds dimension on the coffee table, while a Murano glass floor sculpture creates a sense of intrigue.
The sunroom features a Jump, Jive and Jam theme, while posters from TRAHC’s former signature event line the walls. Artwork from Melissa’s former boutique, Two Friends, is displayed, along with her preferred bottles of bubbly.
Each of the girls’ bedrooms reflect their individual styles and tastes. Jayce’s upstairs bedroom, accented in pink and green, is a fashionista’s dream. Beautiful furs from Colorado, an Andy Warhol original found at a museum, a

vintage Barbie collection, and Moulin Rouge prints from Paris finish out her space. Erin’s room, located downstairs, carries a purple and blue theme while a large Kathi Couch fun paisley painting is the focal point in the room. Her themed tree displays whimsical Batman, Star Trek, and Superman ornaments.
In the beautiful outdoor oasis, a colorfully painted custom table from Italy is displayed featuring Melissa’s favorite decorative item – bees – and two beautiful butterflies, symbolizing Jayce and Erin. Aromatic Angel’s trumpets bloom at night, adding color to the evening landscape.
Most homes are a reflection of the family who owns it, and this one is no exception. Melissa, Jayce, and Erin’s individual personalities are displayed in their respective spaces while artwork from numerous local artists, including Dean Lynn, Judy Jones, Harold Stevenson, and Polly Cook transforms the entire home. Whether traveling across the world or gathering sentimental items that she just can’t live without, Melissa Keil lets her home showcase the story of her life ... and it is a vibrant life that is very well-lived..

62 OCTOBER 2020 fourstatesliving.com









63 OCTOBER 2020 fourstatesliving.com








64 OCTOBER 2020 fourstatesliving.com


65 OCTOBER 2020 fourstatesliving.com
Experts Ask the

JOEY MARTIN
Owner, Express Employment Professionals
Is Attracting The Right Talent Important To Your Culture?
For successful businesses to maintain a competitive advantage in their market, it is imperative to cultivate a strong and vibrant culture. A company’s culture is composed of the shared values and behaviors that comprise the unique social environment of a business.
From a more laid-back, remote workforce to a classic suit-and-tie, 8-5 setting, a culture not only changes the way in which an organization conducts business, but it can also impact the type of individuals recruiters seek.
One of the best recruiting talent pools is among your existing workforce. Your core team members are the heartbeat of your culture so simply asking your employees for referrals is the easiest option.
870.773.1313 | 3206 Jefferson Ave. | Texarkana, AR
EVENTS | CALENDAR
OCTOBER 2020
OCTOBER 8
The 12th annual HandsOn Texarkana Wine and TAPAS event will be held on the grounds of the Collins Building. New California wines will be offered, along with food by Chef Jeff Loving. For tickets, call 903-798-3211 or email: handsontexarkana@aol.com.
OCTOBER 10
The Caddo Area Council, Boy Scouts of America, will host its annual Scouting for Food program. Call 903- 793-2179 for more information.
Our Content
To be included in the “Ask the Experts” column, contact our sales team for pricing and availability.

GET NOTICED TODAY
Contact our sales team to find out how your business can be featured in Ask the Experts.
How can advertising in Four States Living help me?
We at FSLM are involved in what matters to you. We are part of the very fiber that makes up our community. FSLM presents stories and coverage of local people doing important things. We keep a finger on the pulse of the people, businesses, and philanthropies in Texarkana.
Our Mission
The staff of Four States Living Magazine is determined to offer to you the very best coverage of the positive energy that makes up this community so that by flipping through our pages, as a reader, your mind will be stirred, your soul entertained, and your optimism elevated to new heights to be a part of the four states area we call our “home.”
903.792.2262 | 4106 Summerhill Sq. | Texarkana, TX
OCTOBER 11
The Angels of Opportunities Guild will host its second annual Brewery Benefit from 3-7 p.m. at Pecan Point Gastropub & Brewery. An afternoon of football, craft beer, food, and fun will be enjoyed. For more information, visit: www.oppinc.org/ brewery-benefit.



OCTOBER 24
Temple Memorial Pediatric Center will host its inaugural Cornhole Tournament at 102 Highway 134 in Garland City, Arkansas. Held in memory of Kevin Cowling and Trey Varner, the cost for a two-person team will be $50. Prizes will be awarded for first, second, and third place. Call 903-794-2705 for more information.

66 OCTOBER 2020 fourstatesliving.com


RAISING MY TRIBE
by A li D e A l

Back when my husband used to coach, I used to be a substitute teacher. It was so fun, and I loved it. Before COVID hit us all like a Mack truck, I was busy updating all of my information to be able to sub again. It’s not like I have anything going on. Just a working mom of three, who has a million other side jobs, two dogs, tries to cook all of her meals, and exercise. Why not sub?
When COVID hit, there was not much we could do to help. We were forced to stay home. I remember feeling helpless at times. But then, the heavens opened up, and people were talking about schools starting back. Thank you, Lord. God bless the homeschool kids. Y’all rock. And you moms (friends of mine) who do it, y’all are amazing. We aren’t those people here in this household. We love school. We love cafeteria food. We love everything about school here in this household. Teachers are like celebrities over here. I love bulletin boards, and when people make announcements over the intercom. So, when I heard school was opening back up, I knew it was time to expedite my sub papers through the system so I could officially sub again.
Now, I’ve been blessed enough to sub about five times so far as I write this. Let me give you a glimpse into the school world.
Teachers and staff are working their tails off. Whatever you are thinking in your head, double it. Triple it. They are inventive. They are thinking on their feet. They are creative. If you are worried about your child at school, don’t be. Remember, a lot of these teachers were miserable during the quarantine because they actually MISSED your kids. Imagine that! They are so happy to be on campus and in the classroom that they are happily wearing masks and making up games to make it fun for kids to socially distance. I have never been more proud of teachers. Teachers are the game changers in this situation. Teachers aren’t skipping a beat. Everyone go get your teachers gift cards now. Not gifts, they need something they FOR SURE can use. And they might not like the scent of candle you swear that they are going to love. Amazon, Target, Walmart, Starbucks, Chick-fil-A, The Party Factory … this is what I’m talking about here. Don’t get creative in this area.
And the students. Well, there is not much to say, except, there are lots of smiling eyes coming from underneath those masks. I hear laughing. I see dancing down the hallways. These kids are sanitizing like it is their job. They are happily
68 OCTOBER 2020 fourstatesliving.com
wiping down tables, seats, basically anything with a surface. Moms, do not worry. Your kids are having FUN, trust me.
And now to the moms. Parents, they are feeding off of us. The teachers are doing way more than their fair share of holding up their end of the bargain. It’s up to us to continue it at home. You know, like the times, say, when your kid falls out of a tree and splits their lip open so wide you are starting to see facial bones … and you call your husband and so casually say, “Oh hey, no big deal, we are heading to the ER. Nothing to see here! Not bleeding hardly at all!” all while trying to keep the kids calm while there is so much blood you are on your second beach towel applying pressure while driving down the road casually. Peaceful adrenaline comes during those times. Our kids need to see that peaceful adrenaline now.
We are heading into colder weather. Don’t be the parent that freaks out when the first person gets the flu or coughs. It is going to happen. The kids are feeding off of us. For the love, play it cool in front of the kids. And if you don’t know what to do, ask a teacher! The teachers are doing right during the school hours. Let’s not screw them up from 3:30 on!



Always witty and fun, Ali Deal is a part-time hairdresser/counselor and full-time mom to three children. She enjoys writing and sharing stories about her crazy everyday life in the “House of Deal.” Among her many talents, she serves as a partner-in-crime to her husband Cody, pancreas to John Morris, nurse to Rosemary, and baby whisperer to James.

69 OCTOBER 2020 fourstatesliving.com

THE ROAD Tra veled less
BY NICHOLE HOLZE


Hidden Gems and Field Trips: Shreveport, Louisiana
One of our favorite day trips is Shreveport. Sometimes I take my kids down for a weekday mini adventure, or sometimes we wander down on a Sunday afternoon to check out SciPort and some shopping. Most of us think of the shops and restaurants on Youree Drive and the Boardwalk, but there is so much more to Shreveport to discover. Here are my TOP FIVE for Shreveport/Bossier City:
1. Shreveport Aquarium – For this school year, the aquarium is offering private tours! These two-hour tours dive deep behind-the-scenes and answer all of your questions about the sea life at the aquarium, what animal “husbandry” is, what your favorite sea animals eat, how it’s prepared, and so much more. You get to feed the stingrays, touch the jellyfish, and even see the tops of the tanks from above! We were blown away with how great the tour was. Plus, we are fairly well convinced that Santa works at the aquarium in the off-season. Due to COVID-19 restrictions, the tours are only available to family groups for now. During the month of October, the aquarium is serving up a “frightfully” good time by working with a local haunted house production company. They will be open extended hours, with a slightly more scary tour available in the later hours. Learn more on their website or Facebook page. These tours would be a wonderful opportunity for a field trip and break from virtual learning, or a “non-toy” gift idea for the upcoming holidays.
2. R.W. Norton Art Gallery – This art museum is an absolute must-see. Their collection is astounding for a smaller gallery, with works ranging from Auguste Rodin (Yes, THAT Rodin), Mary Cassatt, Winslow Homer, to an extremely rare copy of John James Audubon’s “Birds of America.” The mid-century modern architecture and design is worth a visit in and of itself. My personal favorite: Albert Bierstadt’s “Yellowstone Fall.” The museum is free to visit and is an excellent opportunity to visit a fine art museum so close to home.
Santa works at the Aquarium 72 OCTOBER 2020 fourstatesliving.com
Touch Tank

3. Rhino Coffee – There are two locations, one downtown, and one very close to the Norton museum. My favorite is the Norton location. The coffee shop offers a large menu with vegetarian-friendly options. Get the eastside latte made with almond milk.
4. The Thrifty Peanut/Book Warehouse – A book lover’s dream. I could spend hours there. It’s a large store with books of all types. Plus, you can sell your old books. No appointment necessary.
5. Well + Fed – Our favorite place to eat in Shreveport, the ENTIRE menu is vegan and gluten-free. They have fresh juice, smoothies of all kinds, and a great menu. A tip: go on a Friday and get the vegan nachos. They will change your life.
Other items of note: Sci-Port has reopened with their new gallery, “Adventures in Intrigue.” Also check out the Boom or Bust Byway website for more road trip ideas in Northwest Louisiana.





Never afraid of a long drive, Nichole is a homeschooling mom to two and wife to Ryan. Coffee, always, and black please. You can probably find her scheming up their next road trip while hiking in the woods. Experience-based learning and good books abound in their homeschool, as they chase the spark of curiosity where it wanders on the road less traveled.
Shreveport Aquarium Dome
Behind-the-Scenes – Food Prep
R.W. Norton Art Museum
73 OCTOBER 2020 fourstatesliving.com
Overhead View
the FRIENDS list
Each month, Four States Living will choose two people who have “liked” our Facebook page to be featured in The Friend List. Chosen randomly, these two “friends” will answer questions we provide so our readers can get to know them better. The bonus question (the last question) will be related to the theme of each month’s issue.

BONNIE BERNARDI
age: 40
occupation: Personal Trainer at Fitness Pros
If you won the lottery, what is the first thing you would do?
If I won the lottery, the first thing I would do is pay off my entire family’s debt. And then I would give each family member some extra cash to do with what they please. I would also donate to Make-A-Wish Foundation to help fulfill the wishes of children with lifethreatening illnesses.
When you have 30 minutes of free time, how do you pass the time?
With just 30 minutes of free time, how I would spend it would depend on where I am at the time. If at the gym waiting on a client, I would get 30 minutes of cardio in; at home, I’d be cleaning.
If you were allowed to have one wish granted, what would it be?
My one wish would definitely have to be: to have plenty of energy to live each day to the fullest.
LINDA HOOKS
age: 56
occupation: Library Aide
If you won the lottery, what is the first thing you would do? I would take my family on a vacation.

When you have 30 minutes of free time, how do you pass the time? I would sleep.
If you were allowed to have one wish granted, what would it be?
Build a house that would be accessible for my son, CJ.
At what business could you max out a credit card?
I could easily max out a credit card at Victoria’s Secret or Lululemon.
Choose a movie title for the story of your life. “National Lampoon’s Christmas Vacation.”
What are you currently watching on Netflix?
I am currently watching “The Office” on Netflix.
If you could visit anywhere in the world, where would you go?
If I could go anywhere in the world it would definitely have to be Italy, since I’m Italian.
If you could only have three apps on your smartphone, which would you pick?
My 3 apps would have to be: MyWorkout+, Spotify, and Facebook.
What’s your favorite sport to watch, and which team do you root for?
My favorite sport is definitely football. I root for the Texas Longhorns and America’s team, the Dallas Cowboys.
WOMEN’S
At what business could you max out a credit card? Dillard’s.
Choose a movie title for the story of your life. “I Will Survive!”
What are you currently watching on Netflix? “Black Lightning.”
If you could visit anywhere in the world, where would you go? Paris.
If you could only have three apps on your smartphone, which would you pick? Facebook, Messenger, and Pinterest.
What’s your favorite thing about FSLM?
I like to watch Dallas Cowboys football.
HEALTH & WELLNESS”
WHAT STEPS DO YOU TAKE TO BE PROACTIVE WITH YOUR HEALTH?
I am proactive with my health by always being in the gym, which isn’t hard since I work there. Putting in two-a-days is very normal for me. I do cardio in-between clients and stay busy with my clientele helping them reach their fitness goals,. I always get my weight training session in, too.
I am a 14-year breast cancer survivor. I’m proactive about getting my mammograms and other wellness checks yearly. I walk daily for exercise and take vitamins.
“
74 OCTOBER 2020 fourstatesliving.com
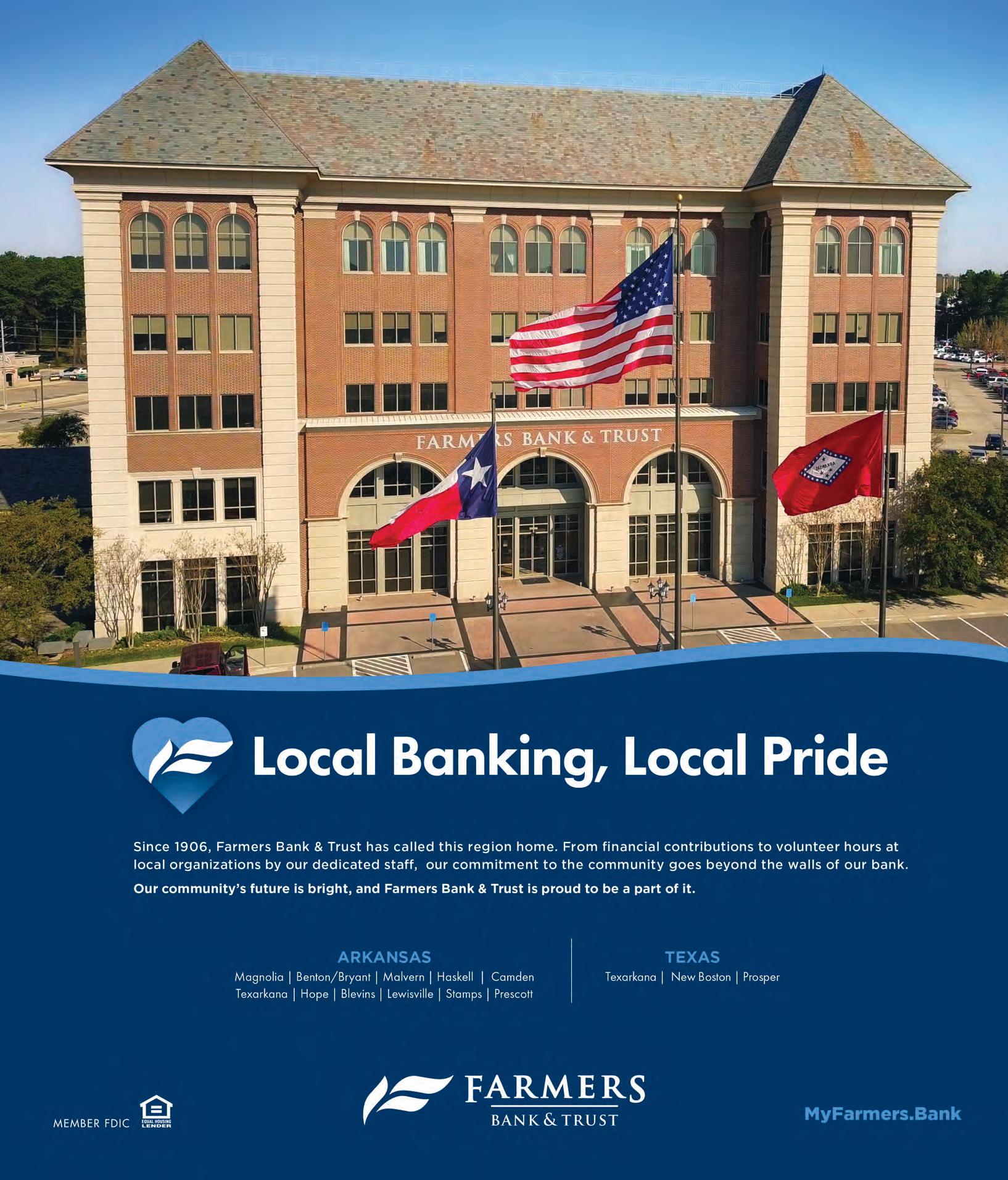











 Ben Tice (Robyn’s brother), Katy Nix (Robyn’s sister) and Rick Tice (Robyn’s father) celebrated Katy’s birthday while Robyn was in the hospital with Macaroni Grill and a bota box. (No wine for Robyn, of course.)
Ben Tice (Robyn’s brother), Katy Nix (Robyn’s sister) and Rick Tice (Robyn’s father) celebrated Katy’s birthday while Robyn was in the hospital with Macaroni Grill and a bota box. (No wine for Robyn, of course.)


 Robyn (right) with her sisters Katy Nix and Stacy Proctor, and mother, Brenda Jones, during a girls’ weekend in Houston, Texas, last November.
Robyn (right) with her sisters Katy Nix and Stacy Proctor, and mother, Brenda Jones, during a girls’ weekend in Houston, Texas, last November.












 Kim Fowler and Kaye Baxter
John and Susie Stanley
Laney Bassham and Dr. Charles Fortenberry
Steve Brown and Jeff Brown
Debbie Gilliam, Tiffani Whitehead and Kelly Burkhalter
Judge Josh and Diana Morriss
Phyllis Carter, June Owen and Charles Carter
Dr. Beverly Rowe, Dr. Alyce Bunting and Brandy Aaron
Brian Goesl, Noah Crissman and Randal Conry
Kim Fowler and Kaye Baxter
John and Susie Stanley
Laney Bassham and Dr. Charles Fortenberry
Steve Brown and Jeff Brown
Debbie Gilliam, Tiffani Whitehead and Kelly Burkhalter
Judge Josh and Diana Morriss
Phyllis Carter, June Owen and Charles Carter
Dr. Beverly Rowe, Dr. Alyce Bunting and Brandy Aaron
Brian Goesl, Noah Crissman and Randal Conry




 photo by ALAMOND PHOTOGRAPHY
photo by ALAMOND PHOTOGRAPHY





 Tylan, Amy and Braylee in downtown Texarkana before getting Braylee’s senior photos taken during March 2019.
Braylee took this photo of her mom’s surgical incision after Amy’s skull had been put back in and the drains were removed. She was still in ICU at this point but was discharged to go to rehab shortly thereafter.
Tylan, Amy and Braylee in downtown Texarkana before getting Braylee’s senior photos taken during March 2019.
Braylee took this photo of her mom’s surgical incision after Amy’s skull had been put back in and the drains were removed. She was still in ICU at this point but was discharged to go to rehab shortly thereafter.

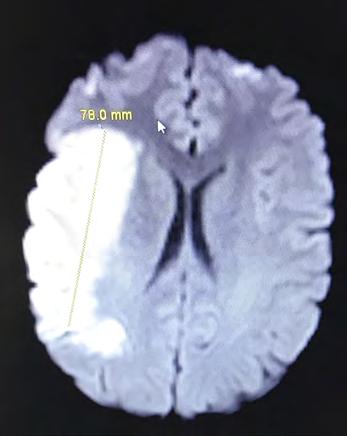















 Mayor Allen Brown and FaEllen Yates
Dajha Smith and Miss Texarkana Twin Rivers Outstanding Teen Gracie Britton
Katrena Goodwin and Mieashia Lindsey Sherry Young, Rebekah Drennon and Clay Roberts Dan Edmonds and Hershel Flanagan
Billy Power and Bruce Hornbuckle
Mayor Allen Brown and FaEllen Yates
Dajha Smith and Miss Texarkana Twin Rivers Outstanding Teen Gracie Britton
Katrena Goodwin and Mieashia Lindsey Sherry Young, Rebekah Drennon and Clay Roberts Dan Edmonds and Hershel Flanagan
Billy Power and Bruce Hornbuckle










 David Rolf and Bob Hubbard John Flippo, Chris Richards, Ryan Morgan and Jon Sheppard
Dan Edmonds, Ron Copeland, Corey Jerry and Jeff Butler
Dr. Hesham Hazin, Brandon Rampy, Dr. Chad Patterson and Tim Asimos
Katie Andrus and Lyndsey Craig
Rebekah Dannar, Mieashia Lindsey, Treston Osby and Jeremiah Stacks
Mike Rogers, Jason Ross, Matt Keil and Brock McCorkle
Mayor Allen Brown, David Hickerson, Sonny Brainerd and Calvin Williams David Rolf, Dr. Tom Hunley, FaEllen Yates and Bob Hubbard
David Rolf and Bob Hubbard John Flippo, Chris Richards, Ryan Morgan and Jon Sheppard
Dan Edmonds, Ron Copeland, Corey Jerry and Jeff Butler
Dr. Hesham Hazin, Brandon Rampy, Dr. Chad Patterson and Tim Asimos
Katie Andrus and Lyndsey Craig
Rebekah Dannar, Mieashia Lindsey, Treston Osby and Jeremiah Stacks
Mike Rogers, Jason Ross, Matt Keil and Brock McCorkle
Mayor Allen Brown, David Hickerson, Sonny Brainerd and Calvin Williams David Rolf, Dr. Tom Hunley, FaEllen Yates and Bob Hubbard







 Emily (center) with her aunt, Lori Rochelle; cousin, Olivia Rochelle; grandmother, Paula Hawkins; and mother, Stephanie Hawkins, during the Pleasant Grove Academic Award ceremony when Emily was right in the middle of battling her eating disorder.
Emily (center) with her aunt, Lori Rochelle; cousin, Olivia Rochelle; grandmother, Paula Hawkins; and mother, Stephanie Hawkins, during the Pleasant Grove Academic Award ceremony when Emily was right in the middle of battling her eating disorder.











 Howie Wright, Sharon North, Jack Daugherty, Robin Mitchell and Madison Middleton
Jennifer Sievers, Amber Cohen and Kathy Winchester
Chief Perry, Jennifer Montoya, Amber Cohen and Bess Gamble-Williams
Amber Cohen, Bess Gamble-Williams and Dee James
Iron Maiden Riding Club – Michigan Chapter Howie Wright and Madison Middleton
Howie Wright, Sharon North, Jack Daugherty, Robin Mitchell and Madison Middleton
Jennifer Sievers, Amber Cohen and Kathy Winchester
Chief Perry, Jennifer Montoya, Amber Cohen and Bess Gamble-Williams
Amber Cohen, Bess Gamble-Williams and Dee James
Iron Maiden Riding Club – Michigan Chapter Howie Wright and Madison Middleton




 Team Sumoas at Relay for Life 2018
Team Sumoas at Relay for Life 2018













 Jill McMahon, Natalie Haywood and Kenzie Teel
Jill McMahon and Joey Martin
Donovan Driver and Dr. Jim Booker
Janelle Williamson, Judy Sander and Carla Moon
Karen Mote and Allison Wright
Jim Bynum and Brittney Brookes
Faith Dossey and Lindsey Woodson
Dr. Jim Booker and Annemarie Sullivan
Toni and Jay Crabtree
Dr. Jim and Lauren Booker
Jill McMahon, Natalie Haywood and Kenzie Teel
Jill McMahon and Joey Martin
Donovan Driver and Dr. Jim Booker
Janelle Williamson, Judy Sander and Carla Moon
Karen Mote and Allison Wright
Jim Bynum and Brittney Brookes
Faith Dossey and Lindsey Woodson
Dr. Jim Booker and Annemarie Sullivan
Toni and Jay Crabtree
Dr. Jim and Lauren Booker










 While in the ICU during February 2018, Maryssa had an external shunt (a drain that pulls csf from the brain) for two weeks.
John Michael and Maryssa in 2016 when they took Brayden to WrestleMania.
Brayden was so excited for his mom to be home following her 32-day ICU stay in 2018.
Tattoo artist Jessica Dillard designed this tattoo of the IIH ribbon for Maryssa, so on her bad days she can always look down and remember that she is a warrior.
Maryssa in 2018 after having her third brain surgery in one month plus a 32-day stay in ICU after having MRSA, pleural effusion, and pneumonia.
Six weeks prior to this photo of Maryssa before her brother’s wedding this past August, Maryssa was in the hospital on a ventilator and in a coma for over a week.
While in the ICU during February 2018, Maryssa had an external shunt (a drain that pulls csf from the brain) for two weeks.
John Michael and Maryssa in 2016 when they took Brayden to WrestleMania.
Brayden was so excited for his mom to be home following her 32-day ICU stay in 2018.
Tattoo artist Jessica Dillard designed this tattoo of the IIH ribbon for Maryssa, so on her bad days she can always look down and remember that she is a warrior.
Maryssa in 2018 after having her third brain surgery in one month plus a 32-day stay in ICU after having MRSA, pleural effusion, and pneumonia.
Six weeks prior to this photo of Maryssa before her brother’s wedding this past August, Maryssa was in the hospital on a ventilator and in a coma for over a week.








 Nelda, her father, Johnny Walton, and daughter, Taylor, during a 2016 gathering in Ft. Worth to participate in an 80th birthday surprise party for a family member.
Taylor graduated from Savannah College of Art and Design (SCAD) in May 2015. Nelda admits that this is one of the proudest moments she has had as a mother.
Nelda, her father, Johnny Walton, and daughter, Taylor, during a 2016 gathering in Ft. Worth to participate in an 80th birthday surprise party for a family member.
Taylor graduated from Savannah College of Art and Design (SCAD) in May 2015. Nelda admits that this is one of the proudest moments she has had as a mother.



 Taylor and Nelda making silly faces in 2011 ... this photo is Taylor’s all-time favorite picture of them because she was finally getting her mom back after that Homecoming night when their lives were forever changed.
The Timmons’ family Halloween Party has been a lifelong tradition. Nelda’s daughter, Taylor, has now been named as the hostess.
Taylor and Nelda making silly faces in 2011 ... this photo is Taylor’s all-time favorite picture of them because she was finally getting her mom back after that Homecoming night when their lives were forever changed.
The Timmons’ family Halloween Party has been a lifelong tradition. Nelda’s daughter, Taylor, has now been named as the hostess.



 by ELLEN ORR
by ELLEN ORR


 Kim, Sydney and Bruce in 2017, three weeks before Kim found out she had breast cancer.
Kim, Sydney and Bruce in 2017, three weeks before Kim found out she had breast cancer.


 Bruce, Sydney and Kim at the Redwater football field during September 2017, six weeks after Kim’s bilateral mastectomy.
Completely recovered and back to her active lifestyle, Kim and her family enjoyed hiking Mt. Quandary in Breckenridge, Colorado, during the summer of 2019.
Kim completed her reconstruction during early 2018. This photo of her and Sydney was taken a few weeks after the surgery.
Bruce, Sydney and Kim at the Redwater football field during September 2017, six weeks after Kim’s bilateral mastectomy.
Completely recovered and back to her active lifestyle, Kim and her family enjoyed hiking Mt. Quandary in Breckenridge, Colorado, during the summer of 2019.
Kim completed her reconstruction during early 2018. This photo of her and Sydney was taken a few weeks after the surgery.


 T1D has shaped Kelsi into the person she is today. She shares that this photo reflects her the most. Taken on the Texarkana College campus in her TC scrubs, this photo shows her insulin pump in her right hand and the continuous glucose monitor (aka Dexcom) in her left arm.
CrossFit Texarkana is the place Kelsi goes to relieve stress. She loves working out and enjoys being around people who push her to be better every day.
T1D has shaped Kelsi into the person she is today. She shares that this photo reflects her the most. Taken on the Texarkana College campus in her TC scrubs, this photo shows her insulin pump in her right hand and the continuous glucose monitor (aka Dexcom) in her left arm.
CrossFit Texarkana is the place Kelsi goes to relieve stress. She loves working out and enjoys being around people who push her to be better every day.


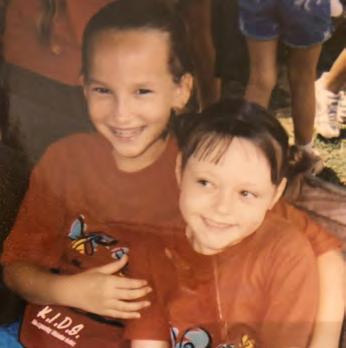

 Kelsi (right) with her brother, Conner, and parents Melanie and Steve, during their 2018 summer vacation to Fort Walton Beach, Florida.
July 5, 2020, marked Kelsi’s one year anniversary of nursing.
Kelsi (right) with her brother, Conner, and parents Melanie and Steve, during their 2018 summer vacation to Fort Walton Beach, Florida.
July 5, 2020, marked Kelsi’s one year anniversary of nursing.