BUILDING UNITY





As 2025 comes to a close, we want to take a moment to celebrate what we have accomplished together and share our excitement for the year ahead This year was filled with growth for FMHCA We brought members together at seven networking events across Florida, each one creating opportunities to connect, collaborate, and strengthen our professional community.
Looking toward 2026, we are pleased to announce a new membership structure that will go into effect on January 1, 2026. These updates were designed with you in mind, adding new perks and benefits that will make membership more valuable than ever Current members who renew before December 31, 2025, will be grandfathered into the 2025 membership rate, so we encourage you to take advantage of this opportunity
We are also excited to share that our GRC Fund Run (or Walk!) begins now through the end of the month. This event is a great
way to get moving while supporting FMHCA’s Government Relations Committee Every shirt purchased and every registration directly supports our advocacy efforts, so we encourage you to join in, bring colleagues along, and proudly wear your race shirt knowing that all proceeds go toward advancing the counseling profession in Florida.
Of course, one of the highlights on the horizon is the 2026 Annual FMHCA Conference This event is always a cornerstone of our work together, offering days of education, connection, and inspiration for counselors across the state We look forward to welcoming you there as we continue to advance our profession and strengthen our community
On behalf of the FMHCA Office, thank you for your dedication and engagement throughout 2025 We are grateful for each of you and excited to see what we can accomplish together in 2026




43
46 FMHCA Committee Updates
Page 52
the Expert
InSession Magazine is created and published quarterly by The Florida Mental Health Counselors Association (FMHCA)
FMHCA is a 501(c)(3) non for profit organization and chapter of the American Mental Health Counselors Association.
FMHCA is the only organization in the state of Florida that works exclusively towards meeting the needs of Licensed Mental Health Counselors in each season of their profession through intentional and strengthbased advocacy, networking, accessible professional development, and legislative efforts
Let your voice be heard by becoming a FMHCA Member today!
Click here to view FMHCA's current Bylaws
CONTRIBUTE:
If you would like to write for InSession magazine or purchase Ad space in the next publication, please email: Naomi Rodriguez at naomi@flmhca.org
THE INSESSION TEAM:
Naomi Rodriguez- Editor
Victoria Siegel, LMHC- Expert Advisor

There shall be no discrimination against any individual on the basis of ethic group, race, religion, gender, sexual orientation, age, or disability
Information in InSession Magazine does not represent an official FMHCA policy or position and the acceptance of advertising does not constitute endorsement or approval by FMHCA of any advertised service or product. InSession is crafted based on article submissions received. Articles are categorized between Professional Experience Articles & Professional Resource Articles.
Professional Experience Articles are writer's firstperson pieces about a topic related to their experience as a mental health professional, or an opinion about a trend in the mental health counseling field
Professional Resource Articles are in-depth pieces intended to provide insight for the author's clinical colleagues on how to be more effective with a particular type of client or a client with a particular disorder, or tips for running their practice more efficiently

The Florida Mental Health Counselors Association (FMHCA) is the State Chapter of the American Mental Health Counselors Association (AMHCA) FMHCA is the only organization dedicated exclusively to meeting the professional needs of Florida’s Licensed Mental Health Counselors
The mission of the FMHCA is to advance the profession of clinical mental health counseling through intentional and strengthbased advocacy, networking, professional development, legislative efforts, public education, and the promotion of positive mental health for our communities
Its sole purpose is to promote the profession of mental health counseling and the needs of our members as well as:
Provide a system for the exchange of professional information among mental health counselors through newsletters, journals or other scientific, educational and/or professional materials
Provide professional development programs for mental health counselors to update and enhance clinical competencies
Promote legislation that recognizes and advances the profession of mental health counseling
Provide a public forum for mental health counselors to advocate for the social and emotional welfare of clients
Promote positive relations with mental health counselors and other mental health practitioners in all work settings to enhance the profession of mental health counseling
Contribute to the establishment and maintenance of minimum training standards for mental health counselors
Promote scientific research and inquiry into mental health concerns
Provide liaison on the state level with other professional organizations to promote the advancement of the mental health profession
Provide the public with information concerning the competencies and professional services of mental health counselors
Promote equitable licensure standards for mental health counselors through the state legislature













Professional Experience Article
In the ever-shifting terrain of modern life, our clients are not only navigating internal challenges but also external environments that shape their sense of identity, safety, and connection. For LGBTQIA2S+ clients in particular, therapeutic support must move beyond the “what’s wrong” model and into a broader recognition of “where are you?” and “what’s shaping your current experience?”
One powerful way to meet this need is to attune ourselves and our clients to the concept of third spaces.
Traditionally, “third spaces” are locations outside of home (first space) and work (second space) where individuals can find belonging, expression, and social identity. These include coffee shops, bookstores, community centers, hobby groups, and more recently, online communities. For LGBTQIA2S+ individuals especially those who may have experienced marginalization in their first and second spaces third spaces have often provided the critical context where their authentic self can safely emerge.
Historically, gay bars, activist collectives, and queer bookstores served as these vital third spaces. Over time, the landscape has evolved. Today, many queer individuals find community through tabletop gaming groups, fandom conventions, Twitch streams, queer Dungeons & Dragons campaigns, and other niche digital ecosystems that function as chosen family and
identity-affirming sanctuaries.
As therapists, understanding and exploring these third spaces can be transformative in helping our clients anchor themselves through periods of stress, disconnection, or transition.
Third spaces offer something incredibly therapeutic: the chance to be known in a lowstakes, non-performative way Clients often report feeling safer in these environments than in their workplaces or even in family settings. These spaces support core psychological needs such as:
Belonging: The feeling of being accepted without condition.
Agency: The freedom to explore and express identity on one ' s own terms.
Community Regulation: A soft accountability from peers who model resilience, creativity, and mutual care.
For LGBTQIA2S+ individuals, who often grow up having to “scan and adapt” for safety in heteronormative environments, these third spaces allow them to exhale That exhale can be the difference between surviving and thriving.
In clinical work, we can help our clients locate, nurture, and engage with third spaces through questions like:
“Where do you feel most like yourself?”
“Is there a group or environment real or virtual where you feel seen or understood?”
“How do you show up differently there compared to work or home?”
By incorporating these conversations, we also model that emotional regulation and healing are not just internal processes but contextually bound. A queer client who feels numb or anxious at home may come alive in a cosplay group or while streaming with affirming friends
That shift is not avoidance it’s adaptation.
Written By: Dr. Josh Littleton, LMHC, CST, NCC
Dr. Josh is a licensed psychotherapist and clinical sexologist specializing in relational wellness, LGBTQIA2S+ affirming care, and trauma-informed therapy. With over a decade of experience, he blends evidence-based practices with creativity and compassion. Dr. Josh is passionate about helping clients reclaim their voice, deepen connection, and navigate life’s transitions with authenticity, resilience, and joy.


Creative Arts Therapy as Applied to Active Imagination, an Analytical Psychology Technique
03 October 2025 | 2:00 PM-4:00 PM
Presented by: Teda Kokoneshi, LMHC Register Now
Helping Clients Heal from Narcissistic Abuse (Domestic Violence)
10 October 2025 | 2:00 PM-4:00 PM
Presented by: Stephanie Sarkis, PhD, NCC, LMHC Register Now
Leadership and Advocacy within Counselor Education: Testifying for Clients
17 October 2025 | 2:00 PM-4:00 PM
Presented by: Kendria Brown, LMHC Register Now
Sexuality and Addiction
31 October 2025 | 2:00 PM-4:00 PM
Presented by: Carol Clark, Ph.D., LMHC, CAP, CST Register Now
Which is Best? Parent Coordination, Co-Parent Therapy, Reunification Process, or Family Therapy
07 November 2025 | 2:00 PM-4:00 PM
Presented by: Christine Hammond, LMHC, NCC Register Now
Navigating Ancient Traditions: Working with Clients Within Their Meaning-Making Systems
14 November 2025 | 2:00 PM-4:00 PM
Presented by: Colette McLeod, LMHC, CCM Register Now
Join in on one of our upcoming webinars! & More!
P.S. We are seeking presenters for our 2026 Webinar Series until Nov. 1st! Learn more HERE


Professional Resource Article
The landscape of psychotherapy has undergone a significant transformation, with the most profound change occurring post pandemic, creating a rapid shift to teletherapy. This evolution has underscored the critical importance of understanding how to build and maintain robust therapeutic relationships and a strong therapeutic alliance in both traditional face-to-face and emerging online environments.
Decades of psychotherapy research consistently demonstrate that the therapeutic relationship and alliance are the most reliable predictors of therapeutic change. While these relational factors are critical, the concept of therapeutic presence has proven to be a foundational element, essentially serving as a precondition for effective therapeutic relationships and a strong therapeutic alliance. This article delves into the definition and comprehensive understanding of therapeutic presence, explores factors that can impede it, and discusses the unique challenges it faces in online therapy.
What illustrates Therapeutic Presence?
Therapeutic presence is defined as a way of being with a client
that optimizes both the "doing" and "technique" of therapy It involves therapists bringing their whole selves to the therapeutic encounter, being fully present on a multitude of levels: physically, emotionally, cognitively, relationally, and spiritually. This deep engagement enables therapists to attune to their own moment-to-moment experiences as well as those of their clients.
At its core, therapeutic presence involves:
Being grounded and in contact with one's integrated and healthy self. This provides a steady base for the therapist amidst challenging emotions
Being open and receptive to what is poignant in the moment, and being immersed in it This involves receptively taking in the client's verbal and nonverbal experience and being responsive in the moment.
A sense of spaciousness and an expanded awareness and perception. This allows for a broad, non-judgmental awareness.
Operating with intention, to be with and for the client, in service of their healing process. The singular purpose is the client's healing, transcending any self-centered goals or desire for a particular outcome.
By noting these elements, therapists can begin to conceptualize therapeutic presence and its importance in the therapeutic process.
The concept of therapeutic presence is trans-theoretical, meaning it is recognized as valuable and applicable across various psychotherapeutic approaches, making it a " common factor" in effective therapy. Historically, psychoanalysts such as Sigmund Freud and Theodore Reik spoke of "evenly suspended attention" and "listening with a 'third ear ' , " reflecting an open, spacious, and attentive state. Carl Rogers, a pioneer of clientcentered therapy, viewed presence as an underlying condition for empathy, unconditional regard, and congruence. In his later reflections, Rogers even suggested that his initial emphasis on the three basic conditions, congruence, unconditional positive regard, and empathic understanding, might have been an "overemphasis," with the "obvious and clear presence of the therapist as the most significant element of therapy" Modern psychodynamic, Existential, Gestalt, Emotionally Focused Therapy (EFT), Accelerated Experiential Dynamic Psychotherapy (AEDP), and even Cognitive Behavioral Therapy (CBT) approaches now highlight the importance of presence Research shows that clients who rated their therapist as present were more likely to rate the therapeutic alliance and session outcome positively across different therapy types.
From a neurophysiological perspective, specifically through the lens of Porges' Polyvagal Theory, therapeutic presence plays a crucial role in creating a sense of safety Our nervous systems are in constant bidirectional communication. When therapists are fully present and attuned, their receptive and safe presence sends a neurophysiological message to clients that they are being heard, met, felt, and understood. This process fosters a reciprocal experience of safety for both the therapist and the client, thereby strengthening the therapeutic alliance. This is mediated by what's known as neuroception an automatic and often unconscious evaluation of risk in the environment. When features of safety are detected, defensive mechanisms are down- regulated, promoting social engagement behaviors. For clients, especially those with trauma histories, this safe therapeutic environment facilitates the development of new neural pathways, helping to repair attachment injuries and fostering neural growth Therapists' presence also serves as a co-regulator for clients' emotions, with attuned limbic resonance and right-brain to right-brain communication (nonverbal cues, such as body posture, vocal expressions, and facial expressions) facilitating regulation. This "neuroception of safety" allows clients to enter their "window of tolerance," enabling them to engage in the necessary therapeutic work and express vulnerabilities.
The Therapeutic Presence Inventory (TPI), developed by Geller and colleagues, includes both a therapist (TPI-T) and client (TPI-C) version, with research suggesting that the client's perception of the therapist's presence (TPI-C) is a stronger predictor ofpositive therapeutic alliance and session outcome than the therapist's self-reported presence. This underscores that presence only impacts clients if they perceive the therapist as present with them. Therapeutic presence evolves into a relational experience, where the mutual presence of therapist and client fosters both "relational depth" and healing.
Reality tells us that therapeutic presence can be challenging to sustain, given that therapists, being human, also face their own internal and external barriers. Recognizing these potential blocks is essential for maintaining an attuned and effective therapeutic relationship:
Hyper-intellectualization: A therapist's tendency to overanalyze or focus too heavily on theoretical frameworks and analytical processing can hinder experiential processing and shift them out of present-moment contact with the client. This can lead to missing subtle client signals or failing to respond appropriately.
Fear/Anxiety/Self-doubt: Therapists may experience their own anxiety, fear, grief, or trauma around what's going on in the world, often echoing what our clients bring into session. This can be triggered by clients' distress, leading to self-doubt (e.g., "impostor syndrome") and hindering their ability to be fully present and responsive.
Fatigue: Sitting in a chair for hours on end and being on a computer for extended periods These are common in both in-person and teletherapy, and can lead to disconnection and exhaustion if not balanced with other activities and breaks General stress, social isolation, and lack of outdoor time can amplify therapist fatigue This exhaustion can make it challenging to maintain one ' s presence and even lead to burnout.
Reactivity (Countertransference): Therapists' own unresolved issues can be activated by clients' shared distress, leading to countertransference responses. This internal reactivity can interfere with the therapist's ability to stay grounded, attuned, and truly present.
Distractibility: Clients may be in their home environments with distractions, but therapists can also be distracted by internal thoughts (e.g., self-doubt, planning the subsequent intervention) or external factors (e.g., technological glitches, background noises in their own space). These distractions pull the therapist out of the moment with the client
Lack of Self-Care: Sustaining presence demands significant personal resources and active engagement from the therapist Without intentional self-care practices, there is an increased risk of burnout, which compromises the therapist's ability to maintain presence in sessions.
The sudden and widespread adoption of teletherapy in early 2020 presented unique challenges for cultivating therapeutic presence and strengthening therapeutic relationships online. Therapists, many of whom had minimal prior experience in teletherapy, had to adapt their practices quickly.
Some key challenges include:
Limited Non-Verbal Communication: Teletherapy creates physical distance between the therapist and client, significantly limiting the ability to perceive and express non-verbal cues. A core aspect of therapeutic presence involves using body-to-body non-verbal cues (e.g., prosodic vocal tone, leaning forward, gesturing, open body posture, soft facial features, mutual eye gaze, mirroring movements) to communicate presence and safety. When online,
therapists have reduced access to clients' physical cues (gestures, posture, full-body non-verbal expressions) and a reduced ability to express their own presence with their whole body, limiting the capacity to attune and convey safety and trust.
Technological Challenges and Training Gaps: Technical glitches, delays, or freezes in technology can impact therapeutic presence and the therapeutic alliance. There is legitimate concern that clients may attribute these technical issues to the therapist's skills or lack of presence rather than the technology itself. Many therapists may still benefit from training in navigating virtual platforms or conducting therapy online, as well as ways to avoid or respond to clients who face technology-related challenges
Client Environment and Safety: Clients may be in their home environments, potentially with family members or others with whom they have emotional challenges, making it difficult to feel safe or private enough to express complex emotions and vulnerabilities Emphasizing to clients the importance of having private spaces within their homes is crucial.
Increased Therapist Fatigue and Countertransference:
As noted earlier, prolonged online presence can lead to disconnection and exhaustion. Therapists' fatigue may be exacerbated by their own stress related to social isolation and a lack of balance between outdoor time and other commitments.
Therapist Bias: Some therapists historically held negative views towards telehealth, potentially impacting their approach to online therapy and inhibiting the development of a positive therapeutic alliance Shifting this bias is imperative, as online treatment has remained a mode of service delivery
Despite these challenges, research suggests that teletherapy is effective for various disorders and can foster a positive working alliance. Nursing literature and some psychotherapy studies even indicate that presence can be felt and generated online, with concepts like " co-presence " (the illusion of sharing the same distant space) highlighting the potential for therapists' minds and bodies to transcend time and space, creating a feeling of being together
To effectively embody and practice therapeutic presence with clients, therapists are advised to create a comprehensive approach that integrates self-preparation (i.e., grounding before sessions), in-session techniques (i.e., process experiential interventions), and strategies for managing challenges both in the office and online. Therapeutic presence, defined as bringing one ' s whole self to the encounter
physically, emotionally, cognitively, relationally, and spiritually is considered a precondition for effective therapeutic relationships and a positive therapeutic alliance
Recommendations for Counselors Cultivating Therapeutic Presence:
Prioritize Self-Care and Preparation: Therapists should engage in personal practices, such as mindfulness and selfcompassion, to strengthen qualities like attention, awareness, warmth, and sensitivity Before sessions, it is beneficial to take 5-10 minutes to center oneself through mindful breaths or grounding exercises to activate embodied presence Intentional self-care, including physical activity and non-screen time, is crucial for preventing burnout and sustaining presence, particularly during online work.
Optimize the Therapeutic Environment: When working online, therapists should create a consistent and predictable environment that mirrors their in- person therapy room as much as possible. This includes ensuring HIPAA/PHIPA compliance for security and confidentiality. Attention should be paid to optimal lighting that allows clear visibility of facial expressions, and therapists should position their camera and notes at eye level to maintain direct eye contact. Clients should also be encouraged to ensure their privacy and minimize distractions in their own environment
Communicate Presence During Sessions: Therapists must actively convey their presence, empathy, and resonance This involves making facial expressions visible, using a prosodic (rhythmic, warm, varied) vocal tone, and displaying open body posture and gestures. Maintaining mutual eye gaze and mirroring clients'expressions, vocal tone, and breathing rhythm can foster a sense of safety and connection. Being open and receptive to the client's moment-to-moment experience without distraction or fixation is also key. Therapists should also stay attuned to their own internal experience, recognizing emotional resonance or countertransference, and track clients' microexpressions and nonverbal cues to adjust their presence and empathy as needed.
Manage Challenges and Ruptures: Therapeutic presence can be challenging to sustain due to factors such as hyperintellectualization, fear, fatigue, reactivity, and distractibility When personal anxieties or technological glitches arise, therapists are encouraged to practice selfcompassion, acknowledge the issue, and use grounding practices like a " pause, notice, return" (PNR) technique to re-center. Authenticity in acknowledging humanness
during challenging moments can also be beneficial for both therapist and client
Integrate Training: Understanding how presence evokes psychological and emotional safety (interoception), often without conscious awareness (neuroception), is vital. Therefore, training in cultivating therapeutic presence, including its neurophysiological underpinnings and practical exercises to enhance the social engagement system, should be an essential component of psychotherapy education across all modalities.
Clinical Consultation and Supervision: Clinical consultation and supervision play a vital role in helping therapists cultivate therapeutic presence by supporting the inner work of "how to be" with clients The relationship between therapist and supervisor also works in a "parallel process, " modeling the same presence that is expected in therapy sessions Supervisors guide therapists in preparing for sessions and managing blocks and barriers, such as fear, fatigue, or distractibility Supervision fosters dual awareness attunement to both client and self and teaches therapists to convey presence through tone, posture, and expression. It also provides space to address alliance ruptures and integrate the mechanisms that enhance client safety and healing.
By embracing these recommendations, therapists can strengthen therapeutic relationships, foster a sense of emotional safety, and optimize the effectiveness of their work, whether in-person or online
Therapeutic presence is not merely a desirable quality, but a fundamental, trans-theoretical phenomenon essential for effective psychotherapy, regardless of the treatment modality It serves as a necessary precondition for cultivating psychological and emotional safety, strengthening the therapeutic relationship, and fostering the therapeutic alliance, all of which are paramount for client healing and growth. The ability of therapists to be fully present – grounded, open, spacious, and intentionally "with and for" the client – allows clients to feel truly "met" and understood, thereby downregulating their defenses and enabling deeper therapeutic work. While the core principles of therapeutic presence remain consistent, its cultivation and expression face unique challenges in the online environment, such as limitations in non- verbal communication, technological hurdles, and increased therapist fatigue and countertransference. However, intentional strategies discussed can bridge the physical distance, allowing therapists to communicate their presence effectively. The shift
towards teletherapy has highlighted an immediate and ongoing need for therapists to understand and cultivate presence in this modality
Counselor training programs are increasingly recognizing the need to integrate foundational instruction in therapeutic presence, encompassing not only the logistical and technological aspects of teletherapy but also the "inner work" of the therapist to remain grounded and attuned By doing so, mental health professionals can continue to offer profound healing experiences, ensuring clients feel emotionally and psychologically safe, even if separated by a computer screen The ongoing learning from navigating these challenges will ultimately enhance therapists' skills in developing presence and strengthening the therapeutic relationship.
References:
Feuerman, M L (2018) Therapeutic presence in Emotionally Focused Couples Therapy Journal of Experiential Psychotherapy, 21(3), 22–30.
Geller, S. (2020). Cultivating online therapeutic presence: Strengthening therapeutic relationships in teletherapy sessions. Counselling Psychology Quarterly. Advance online publication.
https://doi.org/10.1080/09515070.2020.1787348
Geller, S. M. (2013). Therapeutic presence as a foundation for relational depth. In R. Knox, D. Murphy, S. Wiggins, & M. Cooper (Eds.), Relational depth: New perspectives and developments (pp. 175–184). Palgrave.
Geller, S. M., & Porges, S. W. (2014). Therapeutic Presence: Neurophysiological Mechanisms Mediating Feeling Safe in Therapeutic Relationships Journal of Psychotherapy Integration, 24(3), 178–192 http://dx.doi.org/10.1037/a0037511
Written By: Marni Feuerman, MSW, PsyD, LCSW, LMFT

Dr. Feuerman is a licensed clinical social worker and marriage and family therapist in private practice in South Florida. She specializes in couples therapy and relationship problems and provides clinical supervision and consultation As an ICEEFT Certified Emotionally Focused Therapist and Supervisor, she uses a processexperiential approach centered on therapeutic presence Dr Feuerman is also a nationally recognized relationship expert, media contributor, accomplished author and freelance writer. Connect with her at www.DrMarniOnline.com.



Mental health and wellness have certainly become more widely accepted terms over the last few years. With the expanding acceptance that mental health is a necessary focus in our lives has come an increased need for care and care professionals. We’ve seen a dramatic increase in telehealth practices, residential facilities, individual private practices etc. But then that begs the question: Which level of care is right for our clients? Which avenue would best suit them? It seems to be a prerequisite for work in the mental health field that a provider has a strong desire to help others (and rightfully so) We all want to help our clients; but what if the level of care we offer isn’t the one with the most potential for improvement
I’ve been working in a hospital setting over the last three years in intensive outpatient programs (both PHP and IOP). We are often required to describe what Partial Hospitalization Program(s) and Intensive Outpatient Program(s) entail and what this level of care can address. If you aren’t familiar with these terms, which I wasn’t until I began work in this level of care, I can provide a brief description here Each individual program my vary slightly, but will follow the same general guidelines
Partial Hospitalization Programs are either a step down from inpatient mental health treatment/psychiatric hospitalization,
a step up from intensive outpatient level of care or a step up from standard outpatient level of care Although the term ‘hospitalization’ is in there and can cause some confusion, this is a voluntary outpatient level of care Clients come and go from their homes each day (unless your program offers PHP/IOP housing) and they are not forced to stay or engage Don’t worry, I can help describe those levels mentioned as step downs or step ups, too.
For our program, PHP is a five-day per week program that is group-focused and consists of five fifty-minute groups per day. Group modality is meant to help clients find empathy and relate to others, reintegrate healthy structure into their lives and to gain information about healthy coping strategies While group modality is amazing and I’ve studied the intricacies of how short and long-term groups can work throughout my professional career, I’d be doing everyone a disservice if I didn’t mention some of the limitations Mixed-gender groups for mixed mental health concerns (like depression, anxiety and psychotic symptoms which are more common than one might think!) should not be recommended for complex, specialized concerns. Specialized concerns like those related to trauma should be addressed through either individual care from a specialized professional or through a specialized group format.
Although PHP/IOP may seem long from the outside (we estimate about 3-4 weeks of PHP and 3-4 weeks of IOP for each client), it’s not long enough to open, organize, and resolve complex issues that may involve slight regressions or disruptive episodes before progression. Additionally, while the combination of groups, medication management and individual check ins can work wonders, it is not by any means a magic quick fix. Expectations should be set for clients and family members that, while we hope for the quickest turnaround possible, we can’t guarantee significant progress in any particular set amount of time. Mental health treatment is individualized and client progress/responsiveness may vary.
Through PHP, clients also receive medication management consultations frequently (we offer weekly) and are assigned to an individual program therapist for check-ins. This is a huge perk, as standard outpatient medication management typically occurs once per month or every other month. Weekly visits allows for close monitoring of medication efficacy and potential side-effects. Psychiatric medication management is offered from professionals who specialize in just that; psychiatric medication. Many clients, family-members or professionals may misconstrue the offer of medication management for overall physical health monitoring. This is not the case. While psychiatric medical professionals have knowledge in other health areas that allow them to make educated choices when prescribing medication, like if someone has a heart condition and a specific medication has a potential side effect related to heart-rate for example, all professionals are required to operate only within their scope of practice Psychiatric medical professions do not prescribe medication outside of psychiatric needs or side-effects from current psychiatric medication(s); just like therapists not prescribing medication or a podiatrist not assessing chest x-rays. While psychiatric medical professionals may request bloodwork, checks or scans to ensure safety in taking psychiatric medication, clients need to have primary health physicians or specialized doctors to provide care outside of psychiatry-specific concerns when involved in PHP/IOP.
For many of our clients at the PHP level of care, functioning has been impaired in the major areas used for diagnosis of a mental health disorder (work, school, relationships, self-care) and suicidal ideation may be present. In this case, safety plans should be in place and there should not be any genuine intent present in clients to act on suicidal ideation. We see clients in the PHP level of care who need help stabilizing their symptoms (anxiety, depression, panic, psychosis and substance abuse).
Intensive Outpatient level of care (IOP) is the lesser intense of
the two programs (I know the names try to fool you) This is also a voluntary outpatient level of care Intensive outpatient is a three-day per week program that is group-focused Number of groups per day may be dictated by insurance but generally three groups per day. Clients requiring this level of care need help with stabilization that hasn’t been addressed in standard outpatient level of care, or who are slowly weaning themselves off the level of support they received in PHP. Clients are assigned to an individual program therapist and medication management provider for less frequent check-ins than in PHP. Safety and overall functioning concerns are not as intense as PHP level of care would warrant, and medication changes are not being made as frequently (which may require increased supervision offered at higher levels of care)
Okay. So now we’ve gone over PHP/IOP levels of care…but these lay sandwiched between other options. It’s important we understand those other options because, even though we may wish we could help everyone, we want to make decisions for clients that are ethical and appropriate. As my boss likes to question, “if not us then who”? If we’re not it, what direction would yield highest therapeutic benefit?
We’ll start at the bottom, as I like to think about levels of care on a spectrum Standard outpatient level of care is what most people might think of when the term ‘therapy’ is used. Sessions are typically weekly or even bi-weekly and are intended to help the client(s) work through emotional struggles or history that bothers them past the point of working through it on their own, but not to the point where safety or functioning is a concern. Standard outpatient can be individual, family, couples, etc. Standard outpatient level of care is maintained as the client works through a particular issue(s) and should be terminated once the stated issue(s) have been resolved. Clients may utilize standard outpatient medication management providers (such as psychiatrists or psychiatric nurse practitioners) to receive prescription for medication that they can take on their own; following instructions for their regimen appropriately If functioning or ability to care for oneself becomes a concern, consider referring this client to a higher level of care That’s where intensive outpatient or partial hospitalization come in
Moving up the spectrum from PHP/IOP we find ourselves at residential treatment. Residential treatment, as the name states, provides housing and mental health treatment for their clients. This often includes a combination of group, individual and medication consult. You will find that residential treatment suits clients who struggle with independence or autonomy This may present itself as medication non-compliance or confusion, nonadherence to program rules/structure at the PHP/IOP level
of care or disruptive behavior that interrupts the success of others in group(s), etc Keep in mind this is not often a permanent option, as many residential treatment facilities offer time-limited support at this level before a client should attempt stepping down to a level of care that will help them transition back into a more autonomous life.
At the top of the spectrum is psychiatric hospitalization or inpatient level of care This isn’t as scary as old movies may depict Many modern inpatient facilities attempt to promote a therapeutic atmosphere The goal here is stabilization so that a client is more capable of engaging in lower levels of care on the spectrum Inpatient assessment will gauge whether the client is a danger to themselves or others, whether they have the current capacity to care for themselves and/or whether their symptoms are causing significant distress and disruption in their lives. To achieve stabilization, psychiatric medications are provided or adjusted to yield better results. Clients are removed from outside stressors and monitored consistently to ensure safety and progress. Inpatient level of care may be voluntary or involuntary depending on the client’s ability to recognize their deficits at the time. In Florida, our procedures outline that if a client engages in voluntary admission, they may state to their care team when they feel ready for discharge and their progress will be reviewed for final decision. If a client is admitted to inpatient involuntarily (a baker act here in Florida) it is completely up to the care team (ultimately the psychiatrist) to determine readiness for discharge A detailed discharge plan should be in place to ensure client success and follow-up
If your client isn’t benefitting from their current level of care, take the time to consider if a different level of care may suit them better. This consideration may happen during initial assessment, or after attempt to engage in treatment. Continuous assessment and case review is best practice to ensure we aren’t continuing to attempt a level of care that the client isn’t suited for at this time Think about working from the outside ends of the level-of-care spectrum inward; in other words if you start at standard outpatient level of care, try working up until you find the right fit If you’re starting at the top with inpatient level of care, work downward to slowly reintegrate important balance into your life
While most of this article has consisted of information to be considered from the professional’s standpoint, it would leave a big gap in our practice not to discuss client input. At the PHP/IOP level of care particularly, I’ve been met with the challenge of explaining the rationale for why a specific level of care is being recommended Clients may come in for assessment with an expectation or understanding of one level of care vs
another Resistance to interrupting certain aspects of their lives can feel scary, as well as being faced with revealing their struggles to family members or employment personnel to clear schedules and allow for three or five day per week treatment is a big ask. Remember, it is your job and responsibility as a mental health professional to steer your client in the direction of the best fit. It’s tempting to accept client pleas to engage in a lower level of care than is recommended; and in some cases something really is better than nothing. Just because a program is voluntary, doesn’t mean a client can engage as they please in whichever level of care they are willing.
I try to explain it to clients like this when I encounter resistance: Let’s say you’re experiencing pain in your arm after a fall You go to the doctor and they perform an x-ray revealing a broken bone. The doctor will recommend the appropriate level of care with the goal to mend the bone; likely a cast. You don’t want a cast, as it will get in the way of your work and you don’t want to have to explain it to peers so you tell the doctor that you’d rather just go with a bandaid. The doctor may refuse to move forward with that plan of care with the knowledge that it’s not safe and won’t mend the bone properly. It’s the same for mental health. It’s not wrong, it’s not illegal, it’s most ethical to refuse a level of care that is inappropriate for your client’s symptoms and may pose a safety risk.
It's a lot to take in. It’s a lot to consider. It’s continued process of learning and understanding as we work with clients and come to understand appropriate recommendations. Ultimately, we want our clients to live the happies, most independent lives they can. We want to help and, even when it feels counterintuitive, turning away a client for a more appropriate level of care can be the best way to offer help.
Written By: Jocelyn Patterson
Jocelyn currently works within intensive outpatient mental health programs in a hospital setting, offers individual telehealth sessions currently through Betterhelp, and has experience within forensic settings. Jocelyn has been working to offer continuing education courses online (keep an eye out for Paint Your Progress courses in the near future!) More of Jocelyn’s featured content and perspectives on professional development within the counseling field can be found on LinkedIn and/or professional social media accounts @paintyourprogress. Jocelyn has been working to promote art therapy and to introduce clients to communication using an alternative language of visuals




Food insecurity remains a troubling reality for many individuals, with an annual estimate of more than 47.4 million Americans, including 9 million children, according to the Food Research Action Center. (1) Food insecurity is a social determinant and is a household-level economic and social condition of limited or uncertain access to adequate food. The United States Department of Agriculture (USDA) distinctly categorizes food insecurity as:
Low food security: “Reports of reduced quality, variety, or desirability of diet. Little or no indication of reduced food intake.”
Very low food security: “Reports of multiple indications of disrupted eating patterns and reduced food intake.” (2)
A Feeding America survey showed that 90% of responding food banks reported seeing either an increase or steady demand for food assistance in one month, August 2024, compared to July 2024 ( 3) There’s also an increase in food insecurity according to a USDA data report indicating 13.5% of households were experiencing it in 2023, up from 12.8% in 2022. This amounts to roughly 47 million people, including 14 million children.(4) SNAP, Supplemental Nutrition Assistance Program, applications
are expected to increase due to recently proposed Federal legislative budget cuts to the Program. These proposed cuts include reductions in benefit levels and stricter work requirements, potentially impacting millions of people, likely widening food insecurity and financial hardship among lowincome individuals who rely on SNAP. (5) A household’s condition of being food insecure may be long term or temporary, is influenced by several factors. There does exist a correlation between food insecurity increasing when money to buy food is limited or unavailable. Food insecurity does not necessarily cause hunger, but hunger is a probable outcome of food insecurity (6 ) These findings lay the foundation of this article, to assist colleagues with recognizing childhood disordered eating correlates with exposure to traumatic life events, (7) presented as Food Maintenance Syndrome
A 2006 publication, by Tarren-Sweeney and Hazell investigated aberrant eating patterns in pre-adolescent children in foster care and kinship placements. The term Food Maintenance Syndrome was indicated as a specific “pattern of excessive eating, food acquisition, and hoarding without concurrent obesity”. ( 8 ) For this demographic, Food Maintenance
Syndrome seems to be a relatively recent area of specific focus to understand the broader problematic childhood eating behaviors, with its prevalence connecting to reports of abuse or neglect. However, this condition is considered atypical in children who are not in the foster care system, but its symptoms are being discussed among clinicians regarding children, absent of placement in the child welfare system, requiring behavioral health treatment for other primary conditions. These discoveries afford therapists insight to a child’s survivalist response to the absence of food.
The survivalist response creates an anxious attachment to food and an emotional preoccupation with food. The brain is set in survival mode, triggered by the fear that food may not be available in the future Research suggests that individuals with Food Maintenance Syndrome may have experienced years of food deprived cycles Therefore, early identification and intervention is needed to recognize disordered eating patterns Common signs of Food Maintenance Syndrome include, but may not be limited to:
Overeating to the point of feeling uncomfortably full and nauseous
Apparent lack of satiety (feeling satisfied)
Eating quickly
Becoming upset if someone eats from their plate
Stuffing food in the mouth
Hoarding and hiding food to eat later
Stealing food from stores or homes they visit
Refusal to throw away any leftover food
Only eating a specific amount of food
Purposely not eating enough ( 9)
Food Maintenance Syndrome is not currently recognized as a mental health disorder in the Diagnostic and Statistical Manual of Mental Disorders-5 (DSM-5). However, children presenting with Food Maintenance Syndrome often have co-occurring disorders, because of abuse and trauma, such as:
Obsessive-compulsive disorder
Anxiety disorder
Depression
Rumination disorder
Post-traumatic stress disorder
If the trauma-driven onset of the eating behavior isn’t identified, Food Maintenance Syndrome can sometimes be misdiagnosed as an Other Specified Feeding and Eating Disorder (OSFED) or as obsessive-compulsive disorder. (10) Generally, disordered eating versus being diagnosed with a more severe eating disorder will focus on the duration of
symptoms, their frequency and severity of the disordered behaviors, and the effects on their physical health, including weight
Trauma is defined as “Any disturbing experience that results in significant fear, helplessness, dissociation, confusion, or other disruptive feelings intense enough to have a long-lasting negative effect on a person’s attitudes, behavior, and other aspects of functioning Traumatic events include those caused by human behavior (e g , rape, war, industrial accidents) as well as by nature (e g , earthquakes) and often challenge an individual’s view of the world as a just, safe, and predictable place any serious physical injury, such as a widespread burn or a blow to the head ”(11)
Each traumatic event, requires defining, according to findings in Epidemiology of Traumatic Experiences in Childhood. Estimates suggest that 46% of youth aged seventeen and under report experiencing at least one trauma including:
8-12% - sexual assault
9-19% - physical abuse by a caregiver or physical assault
9% - internet-assisted victimization
20-25% - a natural or man-made disaster
20%-48% - multiple types of victimization to multiple types of traumas
38-70% - witnessed serious community violence
Also, within this population, 1 in 10 have witnessed serious violence between caregivers and 1 in 5 has lost a family member or friend to homicide (12)
Children in foster care experience Post-Traumatic Stress Disorder, PTSD, at a significantly higher rate than children not in foster care. Approximately, 15% of youth in foster care have PTSD, roughly twice the rate of 7% found in the general population. Some research suggests that up to 30% of children in foster care may meet the criteria for PTSD, while estimates between 6% and 15% of all children and adolescents exposed to trauma may develop PTSD PTSD presents with a higher prevalence in youth in foster care with a comorbid diagnosis of ADHD The Centers for Disease Control, CDC, reports an estimated 55% of children enter foster care for neglect, but they experience greater mental health diagnoses, such as AttentionDeficit/Hyperactivity Disorder (ADHD) with rates ranging from 10% to 21%. ADHD prevalence rates is estimated at 3.4% for children in the general population. (13) Comparatively, PTSD is specifically linked to experiencing a traumatic event and involves symptoms like re-experiencing the trauma, avoidance, negative alterations in mood and cognition, and hyperarousal, while ADHD is characterized by inattention, hyperactivity, and impulsivity not necessarily related to trauma. (14) For example, a child with PTSD may appear inattentive due to being
preoccupied with intrusive memories and avoidance, while a child with ADHD may struggle to follow instructions due to distractibility
For those of us living along coastal communities the life-long, annual preparatory rituals for hurricane season, June 1 to November 30 , and its post-recovery, may provoke an awareness of how Food Maintenance Syndrome behavioral patterns develop over time Natural disasters can significantly contribute to trauma and anxiety, often leading to food insecurity, in altered communities The experience of a disaster can disrupt access to food, causing both immediate and longterm food insecurity Food Maintenance Syndrome assimilates both PTSD and ADHD and can present with overlapping symptoms like inattention, impulsivity, and difficulty regulating emotions, making differential diagnosis and treatment difficult. The symptomatology of comorbid diagnoses may be compounded, for all children, when they are exposed to environmental traumatic events. st th
Has a routine of anticipatory, “storm-watching”, hurricane preparation, exacerbated anxiety or stress, causing the mental re-visiting of previous hurricanes, and any of its associated negative aspects, such as food availability? Can the existing link between natural disasters and trauma manifest into Food Maintenance Syndrome, with each successive event, and subjection to food unavailability or rationing? Has repeated food insecurity and trauma exposure created a cycle of unsupported and/or untreated mental health issues? For intervention success, possessing an understanding of the etiology of the trauma-derived, Food Maintenance Syndrome, in an atypical population, is critical. In children six years and older, PTSD diagnostic criteria align with adults, requiring exposure to a traumatic event and experiencing specific symptoms, which must begin after the traumatic event, though they can emerge immediately or be delayed by up to six months. There are four categorized symptom clusters: intrusion, avoidance, negative alterations in cognition and mood, and hyperarousal The DSM-5 has separate criteria, for children under six, with modifications addressing developmental differences (15) Traumatic experiences can leave historical reminders, persisting for years, setting in motion unexpected changes. For children not in foster care, identifying and assessing the anxiety responses to cumulative trauma: multiple traumatic experiences over time, or complex trauma: exposure to prolonged and repeated traumatic events, creates a more intricate clinical picture.
Being cognizant of how a child’s “normal” developmental stages are overwhelmed when impacted by community-wide
disruptions, such as accompanying caregivers in “hot meal” lines or receiving food in alternative settings, such as food banks, can be positive or negative behavioral reinforcers
Children progress with reactions to traumatic events slightly different for children of different ages. They may regress after a disaster, losing skills they previously acquired or return to behaviors they had outgrown. Physiological, emotional, and behavioral reactions in response to their environment and caregiver may change. Research consistently shows children experience severe reactions to stress following a natural disaster. Food and environmental attachment are intertwined across developmental stages to form secure and healthy social relationships. Positive experiences contribute to a child's sense of security and attachment Food insecurity and traumatic experiences can negatively impact a child's attachment and overall well-being ( 16)
Clinical Director, Dr. Shantrell Charles, noted her findings yield to the interrelatedness of trauma within specific aspects of a “child’s response to external stimuli and that stimuli will likely condition that child’s learned responses.” These conditioned responses can become hard-wired in the child’s brain and function automatically. After all, “the thought of not having access to a basic physiological need, food, would likely cause anyone to feel threatened, especially, if food vulnerability has been a regular occurrence ” Reprogramming the child’s emotional response about food access is essential Dr Charles emphasizes that the goal of foster care is temporary Children are to be reunified with their families, whenever possible Understanding family dynamics surrounding food security is a valuable tool when entering culturally sensitive discussions. A comprehensive interdisciplinary case plan is recommended as a goal prior to reunification, if food insecurity was factored in the child’s removal and if Food Maintenance Syndrome characteristics were observed, while in care, individually or in combination with other diagnoses. Finally, youth formerly in foster care will reintegrate into their communities, requiring the same level of support, or more, as non-foster care placed youth.
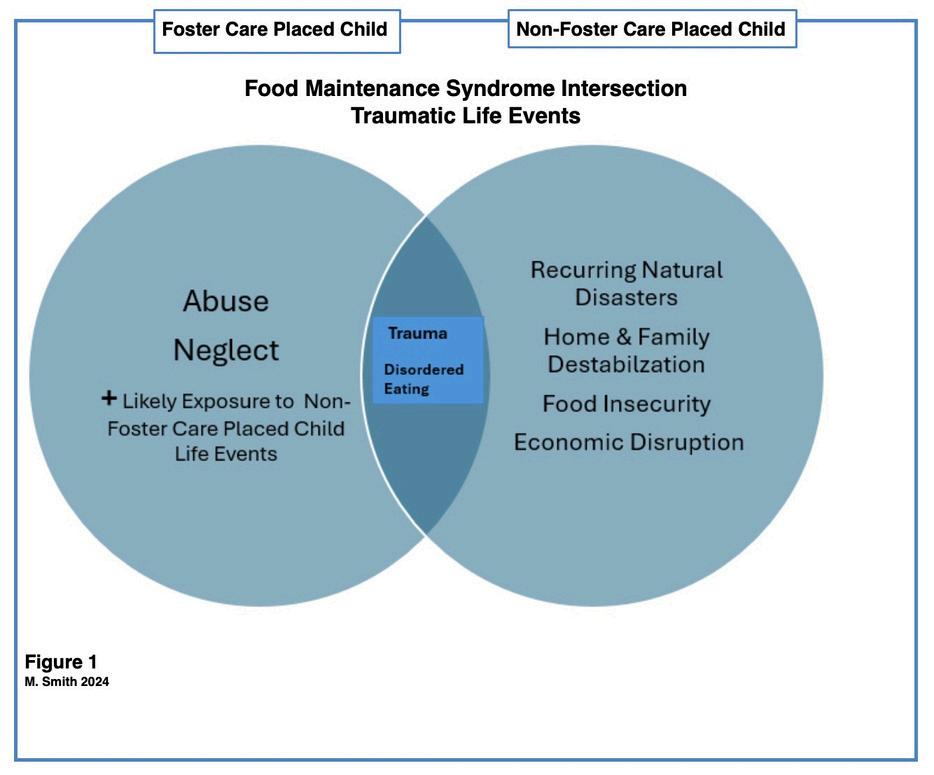
Figure 1 - Intersects possible environmental traumatic events between foster care placed children and children not in care, both having the clinical presentation of Food Maintenance Syndrome. Enhanced screening, early intervention, and targeted support services specifically designed to address the unique needs of children and adolescents appropriate to the child’s developmental stage are needed. (17) Awareness of the relationship between adverse childhood events and their correlation to trauma, benefits clinicians’ insight relative possible root causes of disordered eating.
Trauma-driven Food Maintenance Syndrome sets a child’s brain in survival mode. The clinical observation of children eating excessively, sometimes to the point of being painfully full, and hoarding food, as if their access to food will be unpredictable, can manifest physically and behaviorally, not only in care settings, but in school, impacting academic performance.
School administrator, Toshei Woods, recognized incidents surrounding ongoing student cafeteria behaviors, such as food stashing, reducing food intake, and/or asking peers for food. A voluntary, visually and emotionally-comforting “snack exchange”, non-discard, judgment-free, area for unopened food items was established. The one-to-one ratio, give-one and take one, exchange for non-preferred food items, minimized
reported behaviors of peers feeling “bullied” into giving away their food, reduced the daily banter with cafeteria staff, expressing what they “didn’t like” or “want” on their tray, and gave access to extra food during scheduled breaktimes By using data informed decision-making to further stabilize the emotional and physical feelings of student satiety, throughout the day, broader support strategies were implemented, including the following instructional enhancements:
The school enrolled in the weekend Feeding America Backpack Program (18) and incorporated items from the snack exchange.
Modifications were made to student questionnaires to identify traumatic experiences and symptomology (19) Home room meetings included reading of the daily lunch menu
A food-embracing cultural shift was cultivated centering
around students’ needs Other embedded shifts were in horticulture and cooking classes, using student-created menus and health education about farm-to-table food resources Art classes included more food/still-life images with daily journal reflection. Overall, strategies prevented disruptive, escalating, unwelcome behaviors promoting healing and a positive school environment.
Childhood trauma encompasses a range of adverse experiences, including natural disasters which can have a profound and lasting effect restructuring life-long behaviors and create disordered thinking and eating patterns Pinpointing signs and effects of trauma such as behavioral changes, nervous system dysregulation, and difficulty trusting others, is essential in providing therapeutic techniques such as Cognitive Behavior Therapies: Exposure and Response Prevention, Narrative Exposure, in mitigating the impact of trauma and promote recovery. Applying Measurement-Informed Care (20) to transdiagnostic functionality across cognitive, affective, and interpersonal mechanisms connects trauma exposure to specific disordered eating symptoms to structure prevention techniques. In many communities, reliable access to adequate, nutritious food, leaning into food insecurity requires fortifying protective factors. Even in homes where adequate food is available, the fear of future deprivation remains, proportional or exceeding, in disaster-exposed children, forever shaping their psychology about food Food Maintenance Syndrome isn’t just a condition of disordered eating or hunger, it’s a multifaceted issue with far-reaching consequences for social determinants of health
General Considerations:
Challenge the origin of and resolve one’s own personal beliefs about food
Be receptive to professional guidance once disordered eating is identified
Refrain from dismissing disordered eating cues
Seek to dispel negative, judgmental conversations about food, i.e., the amount to eat, cleaning the plate, using food
as punishment, or other food bargaining acts
Intervene early in settings where the behavior occurs and identify professionals to cross train with care givers/providers
Make food available at regular intervals
Observe and record patterns of food related behaviors, such as time of day and across settings
Utilize brief diverse trauma screeners, at specific intervals When visiting alternative food sources, at any time, openly communicate about the reason(s)
Consider further research on Food Maintenance Syndrome to build additional qualifiable and quantifiable interventions advancing Measurement-informed Care practices
Written By: Marie Smith, Ph.D., NCC, LPC-S, LMHC, CFMHE; Shantrell Charles, DSW, LMSW and Toshei Woods, M.Ed.
Dr Marie Smith has administrative and supervisory experience in clinical, detention: juvenile and adult, K-12 and higher education settings. Her work encompasses advocacy and effective mental health treatment through research and practice.


Dr Shantrell Charles supervises, as the Principal Clinical Director, the administration of a state-wide foster care program. She has extensive practitioner, clinical and administrative/ supervisory experience across child welfare programs and policy development in state government and in the private sector.

Toshei Woods is a social sciences educational administrator and licensed nutritionist. Her work integrates community education with health condition management through whole food choices and life-style behavioral changes.


Through FMHCA’s Local Chapters A CONVERSATION WITH GRACE CANTOR
FMHCA’s mission is clear: to get closer to members’ hometowns through local chapters, creating meaningful connections that strengthen the counseling profession at every level At the heart of this effort is Grace Cantor, FMHCA’s Northeast Regional Director and Co-Chair of the Chapter Relations Committee.
Grace is a licensed mental health counselor in Florida and Washington, a licensed professional counselor in Oregon, and a qualified supervisor in Florida She is a Certified EMDR therapist and an EMDRIA-approved Consultant-in-Training with over 15 years of experience in the mental health field Grace specializes in trauma therapy, anxiety-related disorders, and couples counseling, and has maintained a private practice for the past decade She has also worked in community mental health, inpatient psychiatric care, and provided international supervision to counselors and trainees in Egypt and Ukraine. Currently a third-year doctoral student in the Counselor Education and Supervision PhD program at Regent University, Grace brings both clinical depth and leadership experience to her work with FMHCA, where she advocates for counselors and fosters professional community across the state.
From Regional Director to Chapter Relations Chair
For Grace, stepping into the role of Chapter Relations Committee Chair feels like a natural extension of her service as Northeast Regional Director. “Serving in that position, collaboration was always my goal,” she shares. “There is so much knowledge and wisdom in our chapters, and I want to use that to support new chapters or help smaller ones grow.”
Her experience has also highlighted the importance of teamwork. “Recruiting is essential, no one can do this alone,” she says. “And building relationships is just as important. Our profession can be isolating, and chapters give us a way to connect meaningfully with one another.”
Grace knows firsthand the value of local support. After moving from Portland, Oregon, to Jacksonville, Florida, she struggled to find her footing professionally. “The chapter in Jacksonville had dissolved around COVID, and that was hard. But now there is momentum to re-establish it, and I want to make sure counselors have the support they need to do this heavy work.”
Local chapters, she explains, bring connection to life “It is about facetime, being able to see each other regularly at CEs or networking events That builds relationships, referral networks, and support systems. It also makes it easier to step into statelevel involvement. When you already know someone locally, it is less intimidating to get involved.”
She recalls a recent event in Jacksonville that reenergized the
local counseling community “We had interns seeking licensure who did not even know about FMHCA After one networking event, they felt excited to have support, and that energy helped drive momentum to reform the chapter. But events like that do not happen alone. It took our staff, generous sponsorship from Sophros, and a lot of collaboration. The gratitude we received showed just how much people needed it.”
Grace emphasizes that engagement at the local, state, and national levels is what truly builds a united profession. “At the local level, we can better understand community needs,” she explains “The more connected we are locally, the more momentum we have at the state level And at the state level, FMHCA has a stronger voice for advocacy ”
That local-to-state alignment strengthens FMHCA’s statewide goals. “There is strength in numbers. The stronger our chapters are, the stronger our footprint is at the state level.”
On the national scale, membership with AMHCA creates an even broader impact “FMHCA does amazing work at the state level Honestly, I have lived in other states where there was not anything like it By being strong here, we can serve as a role model for others, while also contributing to the national effort. It extends our reach and ensures our profession has a united front.”
She sees the relationship between these three levels as reciprocal. “The more connected I am locally, the more motivated others are to engage at higher levels And in turn, what we learn nationally and statewide helps us better serve locally It is a cycle of growth and support ”
FMHCA’s current theme of unity resonates deeply with Grace “Burnout is common in our profession, and community is a protective factor If you are interested, there is a place for you There are so many spaces to get involved, and the more connected you are, the more supported you will feel ”
Looking ahead, she sees the Chapter Relations Committee as a hub for collaboration. “There is incredible passion and wisdom in our chapters. By sharing resources and structures, we can help establish new chapters and strengthen existing ones. The generosity of our chapters is what will make this work possible.” What excites her most is the momentum. “There is such a need for counselors in our communities, and our members are passionate about serving By working together, we can build resilience and a robust support system that serves counselors, chapters, and the communities we dedicate ourselves to ”



Professional Experience Article
Social exclusion is a normative yet painful developmental experience that arises as children navigate shifting peer groups, academic transitions, and differing levels of maturity. Events such as birthdays, holidays, athletic competitions, or school performances and achievements, often highlight exclusion most acutely. For many children, these moments activate feelings of rejection and diminished self-worth, placing parents in the position of primary support providers outside the clinical setting.
Parental responses that emphasize validation, containment, and perspective-taking are most effective in mitigating distress and fostering resilience. Within my practice, Social Sense Palm Beach, parents appreciated having these tools outlined for reference when challenging social scenarios arise for their children.
Six core strategies are outlined:
Validation of Affect: Acknowledge the child’s emotional experience directly (e g , “I can see this feels disappointing”) Normalizing distress fosters affect regulation and actively prevents internalization of shame
Reflective Listening: Allow space for narrative processing before offering solutions. Reflective statements provide containment and respect the child’s developmental need for agency. Premature problem-solving can undermine selfefficacy.
Cognitive Reframing: Reframe exclusion as situational rather than identity-defining. Clarifying that social events are often constrained by size, circumstance, or shifting dynamics helps reduce globalized negative self-appraisals. Coping and Confidence Building: Encourage adaptive
self-talk, participation in meaningful activities, and engagement with affirming peers Such strategies broaden social identity and build resilience.
Modeling Adaptive Responses: Age-appropriate disclosure by parents of their own experiences with exclusion communicates universality and demonstrates coping pathways. Modeling enhances observational learning and reduces isolation
Perspective Maintenance: Differentiate between situational exclusion (e g , small gatherings, family-only events) and recurrent patterns warranting further assessment. Persistent exclusion may indicate broader social skill challenges or systemic peer dynamics requiring school collaboration.
Elementary School (6–10 years): Characterized by concrete, dichotomous thinking Exclusion may be perceived as global rejection (“I have no friends”). Supportive reassurance and redirection to prosocial outlets are indicated
Middle School (11–13 years): Heightened self-consciousness and peer orientation amplify the impact of exclusion. Open dialogue and collaborative coping strategies help mitigate internalized rejection.
High School (14–18 years): Exclusion is often equated with diminished worth Joint problem-solving, reframing, and encouragement to broaden social networks are protective. Social exclusion is an expected developmental challenge but can be buffered by parental strategies that prioritize validation, reflection, and resilience-building. When exclusion becomes patterned or pervasive, collaboration with educators or mental health professionals may be warranted
Crick, N. R., & Grotpeter, J. K. (1995). Relational aggression, gender, and socialpsychological adjustment. Child Development, 66(3), 710–722.
Masten, A. S., & Coatsworth, J. D. (1998). The development of competence in favorable and unfavorable environments. American Psychologist, 53(2), 205–220. Beck, J. S. (2011). Cognitive Behavior Therapy: Basics and Beyond (2nd ed.). Guilford Press.
Written
By: Hayley Schapiro, LCSW
Hayley has over a decade of experience in nonprofits, hospitals, & schools, specializing in CBT. She founded the South Florida Mental Health Network to expand access & connect clients with trusted professionals She also consults with schools on student mental health, crisis response, parent education, & policy



Professional Experience Article
It starts before I even get into the car. My mind runs through possibilities. What if a tire blows out? What if the engine fails in the middle of an intersection? What if my brakes go out? What if someone swerves into my lane, and I can’t get out of the way? These aren’t just anxious thoughts They’re parts of me They show up with urgency and intensity because they believe they’re keeping me alive and safe.
IFS (Internal Family Systems) taught me to recognize that we all have many parts inside us, like a little inner family. Let me tell you, my “inner driving crew” has some strong personalities There’s the hypervigilant part, constantly scanning for danger, gripping the wheel like it’s holding me to Earth. There’s the control freak part, unwilling to let someone else drive, because that feels like asking for an accident to happen. There’s the inner critic who is telling me to pull myself together and stop worrying so much. Underneath all my protective parts, there’s a softer, quieter part, an exiled young girl, curled in on herself. She feels there’s too much happening at once, too many chances for everything to fall apart in a split second. She feels so helpless and so small she could disappear between the cracks in the seat.
She doesn’t trust the other drivers on the road, but she also doesn’t trust me. The little girl holds on to every memory in which no one came, no one comforted her. In her world, help never arrives, and when she needs someone the most, she was and will be alone.
And here’s the thing: these parts of mine don’t just bring thoughts, they also bring physical sensations. When my protective parts take over, I feel it in my body: the sweaty palms, the racing heart, the tight jaw, the jittery legs. That’s not just anxiety; it’s all my parts reacting to danger to keep the vulnerable little girl alive and alert. They remember every moment of danger, real or perceived. They remember the shaking, the bracing, the frozen moments of “what if?” from the past. Therefore, when something feels remotely similar, they send the same signals. They don’t believe they are overreacting, and they are desperately trying to protect me with the only tools they’ve ever known
Before I understood IFS, I used to fight these parts. I’d get annoyed at myself: “Why are you being so dramatic?” “Just drive. Nothing’s going to happen.” But it never worked. It only
made the fear louder because these parts weren’t being heard They were being pushed aside like screaming toddlers ignored in the backseat
Now, when those fears come up, I do something different. I pause. I breathe. I check in. I might say (silently, but sincerely): “Hey, I know you’re scared. You’ve seen some things. You’ve been through a lot. You’re doing your best to protect me. I’ve got us now ”
That moment of kindness, of not shaming or rushing, changes everything. When I stop trying to shut them up and start trying to understand them, my parts soften. They don’t vanish, but they settle. They stop screaming and start listening. Just like real kids, they calm down when they know they’re safe and someone is paying attention and tending to them.
I’m a therapist, but I’m also a person with fears, trauma, and protective parts that can go into overdrive I know what it’s like to feel that surge when the world suddenly seems uncertain or unsafe.
That’s why I love IFS. It doesn’t pathologize our fear. It doesn’t rush us to “get over it.” It invites us to get curious, to relate instead of resist. It reminds us that healing doesn’t come from
silencing our parts but from welcoming them from within
We all have fears, maybe not about driving, but about love, parenting, success, failure, or simply being seen. IFS gives us a gentle roadmap to explore those fears, not by fighting them, but by understanding why they’re there in the first place.
You don’t have to kick your fear out of the car You just don’t have to let it drive
Written By: Jessica Sahoury, LMFTA
Jessica Sahoury is a Marriage and Family Therapist Associate licensed in Indiana and a registered MFT Intern in Florida. She provides clinical services to couples, adolescents, and individuals, with a focus on relatio health and emotional well-being. Her therapeutic approach is integrative, drawing from Emotionally Focused Therapy (EFT), Internal Family Systems (IFS), Eye Movement Desensitization and Reprocessing (EMDR), and attachment theory to facilitate insight, strengthen relationships, and promote lasting change. She currently works at Mosaic Counseling Services.





Instructions:
1 Tbsp. neutral oil
1 medium yellow onion, chopped
1 jalapeño, seeded, finely chopped
2 cloves garlic, finely chopped
1 tsp. dried oregano
1 tsp. ground cumin
3 boneless, skinless chicken breasts, cut into thirds
5 cups low-sodium chicken broth
2 (4 5-oz ) cans green chiles
Kosher salt
Freshly ground black pepper
2 (15-oz.) cans white beans, drained, rinsed
1 1/2 cups frozen corn
1/2 cup sour cream
1 avocado, thinly sliced, for serving 1/4 cup chopped fresh cilantro, for serving 1/4 cup crushed tortilla chips, for serving 1/4 cup shredded Monterey Jack, for serving
Step 1: In a large pot over medium heat, heat oil Add onion and jalapeño and cook, stirring, until softened, about 8 minutes Add garlic, oregano, and cumin and cook, stirring, until fragrant, about 1 minute. Add chicken, broth, and chiles; season with salt and pepper. Bring to a boil, then reduce heat and simmer, uncovered, until chicken is cooked through, 10 to 12 minutes. Transfer chicken to a plate and shred with 2 forks.
Step 2: Add beans to pot and bring to a simmer Cook, smashing about one-quarter of beans with a wooden spoon, until slightly thickened, about 10 minutes Add corn and shredded chicken and cook, stirring, until heated through, about 1 minute more. Remove from heat and stir in sour cream.
Step 3: Ladle chili into bowls. Top with avocado, cilantro, chips, and cheese.

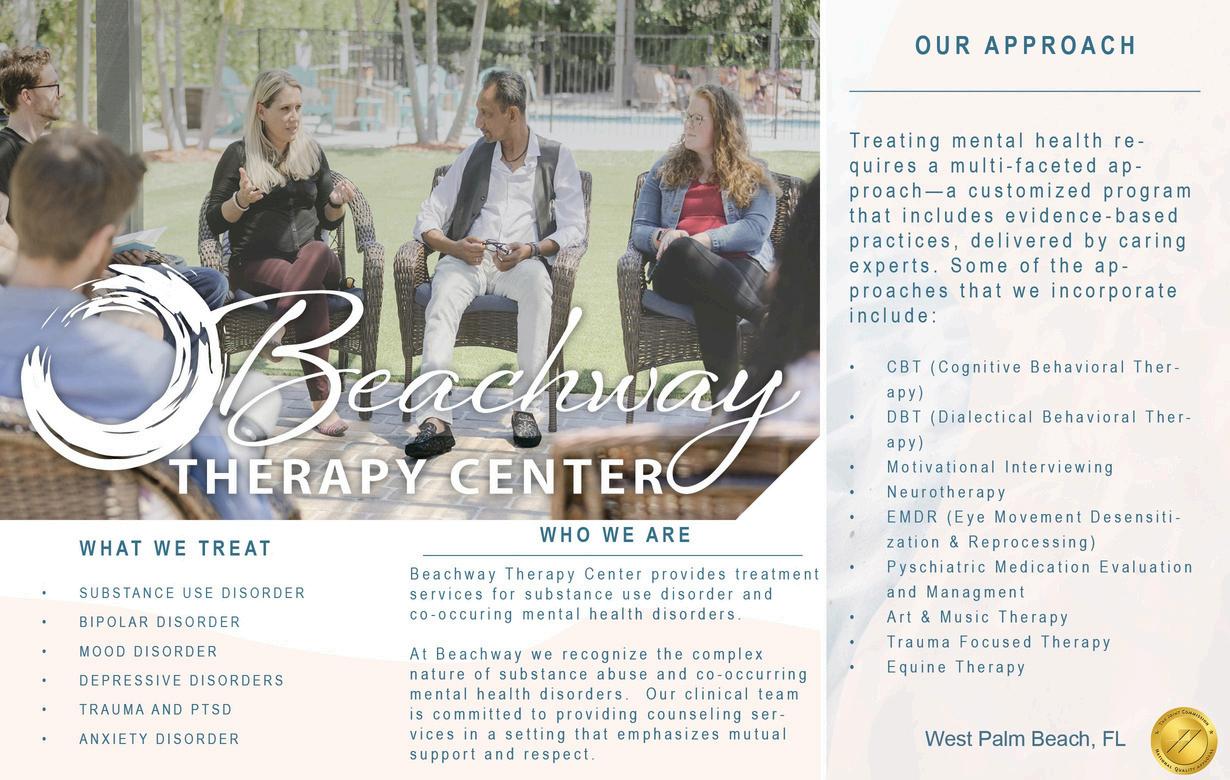
This holiday season, discover flavors of the world like never before through candy! As you count down to Christmas, savor 4 sweet treats from a different country each day (totaling nearly 100 snacks talk about a gift that keeps on giving). Each calendar also includes an informational booklet about the goodies and a sheet to rank your favorites as you eat your way across the globe.

Golden light filters through your window, a mug of something pumpkin-spicy sits within arm’s reach, and the air smells just a little like woodsmoke. It’s the kind of afternoon that calls for quiet creativity like the kind you'll find with this all-in-one watercolor set. It brings the comforting charm of autumn straight to your table, with everything you need to unwind and paint the season in your own colors, whether you're a practiced painter or just looking for a cozy moment of calm. Perfect for all ages and skill levels no prior drawing or watercolor experience needed.
Some nights call for just one more chapter This bibliophile’s sidekick is ready to keep the story going with glowing eyes that illuminate your page Best of all, it marks your spot when you're ready to call it quits or when you fall asleep midsentence. We’ve been there too.
What's even better than a supersoft, oversized hoodie? One that has a slumber-friendly eye mask built right into it. This clever pullover lets you go from airport hustle to in-flight nap with total ease, while enjoying a relaxed fit and cozy cotton blend It's just the thing for savvy travelers, weekend wanderers, and anyone who likes their comfort carry-on ready


What's even better than a supersoft, oversized hoodie? One that has a slumber-friendly eye mask built right into it. This clever pullover lets you go from airport hustle to in-flight nap with total ease, while enjoying a relaxed fit and cozy cotton blend. It's just the thing for savvy travelers, weekend wanderers, and anyone who likes their comfort carry-on ready.
Sure, it's colorful enough to catch the eye, but it's absolutely captivating once you get it in your hands Experience tactile fidgeting delight with this mesmerizing ellipsoid, crafted for quiet, engaging play. Its dynamic ability to stretch, collapse, and flex offers an immersive sensory experience that won't disrupt your surroundings. Whether you need a break from stress or a focus-enhancing fidget, this compact marvel promises endless fascination.
Posting your latest group selfie is great for likes, but nothing beats physical photos for hanging and decorating. This pocket-sized, inkless printer connects to your smartphone via Bluetooth®, then shoots out IRL pics to share.


In Poland, the traditional czerpak, or loop mug, was once used to scoop water from wells or ladle stew from simmering pots. Today, artisans Jacek Kalich and Weronika Kalich carry on that legacy reimagining this classic shape as a cozy, multipurpose mug for modern life. Handmade from stoneware, this charming piece is perfect for a hearty cup of soup or stew.



Blanket, book, and brew the trifecta is ready for maximum coziness and self-care time. But you forgot to take out the tea bag and the sofa is too comfy to leave.
Sarah Welch’s ceramic mug and tea bag tray have you covered. Her unique lid design allows you to keep your beverage steamy while it’s steeping, and also gives you a place to store the bag when you’re ready to sip. Personalize it by adding initials, a brief name, or special date to the bottom of the tray for a thoughtful gift for your favorite tea lover.
You can only toil away on your computer screens for so long before you need to give your brain and eyes a break. Instead of doomscrolling, adopt a few paper pets to watch over your desk and keep you company You don’t need to be an origami master to fold your own clowder of kitties of pack of puppies each envelope contains 50 pre-printed paper squares with instructions, just choose between cats (for beginners) or dogs (for a range of skill levels).

Professional Experience Article
Today’s political climate marked by polarization, intolerance, and uncertainty requires intentional strategies to foster emotional regulation, empowerment, and community connection. As counselors, we must support clients facing fears of deportation, loss of benefits, and deteriorating mental health due to threatened access to services, while also navigating and sustaining our own well-being. Here are some steps to keep in mind while navigating these difficult times:
Acknowledge and Validate Emotions - Whether you ' re the counselor or the client Emotional responses to injustice or intolerance are not signs of weakness; they are deeply human reactions When working with clients, avoid minimizing their concerns. Instead, recognize that fears such as losing healthcare coverage are valid and often rooted in real policy debates and lived systemic inequities.
Limit Media Exposure - Rather than continually scrolling to no end, set designated times to check the news. Disable alerts to reduce stress Choose reputable, fact-based sources and avoid sensationalist media Help clients focus on what is known, not speculative, and emphasize practical steps for preparation and planning
Focus on What Can Be Controlled - Small actions volunteering, voting, organizing documents make all the difference for empowerment and resilience. Support clients in managing online accounts for Medicaid or Medicare, identifying community clinics, and accessing medication discount programs. Advocacy, public education, and writing to representatives can help channel distress into meaningful action.
Build Connection and Boundaries - Connection is equally important Encourage supportive networks that affirm identity and reduce isolation Establish boundaries around harmful conversations Prioritize relationships rooted in dignity and mutual respect. Remind clients and yourself that the only behaviors, emotions, and beliefs you can truly control are your own.
Make Self-Care a Priority - Self-care should be a consistent, non-negotiable practice. Physical wellness supports emotional resilience, so remember to prioritize sleep, nutrition, and movement Teach grounding techniques like focused breathing or guided imagery Schedule joy, rest, and reflection even from advocacy or political engagement to recharge Small acts of kindness can be deeply healing
Balance Hope with Realism - Social change is slow, but progress is possible Connect clients with legal aid, ombudsmen, and advocacy groups Seek professional support when needed; counselors are not immune to emotional fatigue. Healing spaces like therapy or community circles are essential.
Lead with Courage and Care - Ethical self-disclosure can normalize fear and foster connection. Healing and resilience are collective as well as personal By staying grounded, informed, and connected, we cultivate strength and compassion Let us walk alongside those we serve, modeling both courage and care In closing, remember that healing and resilience are collective as well as personal. We are navigating challenging times, but we do not have to do it alone. By staying grounded, informed, and connected to us, our clients, and our communities we cultivate strength, compassion, and the capacity for meaningful change. Let us lead by example, modeling both courage and care, as we walk alongside those we serve.
Written By: Dr. Julie Vogel EdD, LMHC, LPC, ACS, NCC
JDr. Vogel has been a faculty member at South University since July 2018 and operates a private practice, Julie Vogel Counseling, specializing in trauma, women’s issues, and supporting the LGBTQ community. She earned her EdD from Argosy University in Nashville, TN. Over the course of her career, she has held various roles, including Case Manager, Community Organizer, and Regional Director at an adoption agency in New York Dr Vogel completed her master’s degree at Long Island University/CW Post in New York Originally from Wisconsin, she has lived and worked in Long Island, NY, Tennessee, Virginia, and currently resides in West Palm Beach, FL.


For many, hearing the words “You’re in remission” or “Treatment is over” marks the end of a difficult chapter But for the individuals sitting across from us in therapy, survivorship often brings a new set of emotional, physical, and relational challenges that don’t fit neatly into the idea of a “happy ending.”
As mental health providers, it’s important to remember that cancer doesn’t end when treatment does Survivorship is its own chapter one that deserves careful attention, compassionate presence, and validation Clients may arrive in our office unsure of why they are struggling, even as everyone around them says, “You should be so grateful ” Our role is to help them name and navigate what often goes unseen.
While family and friends may celebrate survival, clients often carry invisible burdens that remain unspoken Fear of recurrence can shadow moments of relief Physical changes, long-term side effects, and fatigue can disrupt daily rhythms. There is often a disorienting gap between what others expect of them “back to normal” and how their body and mind actually feel.
This disconnect can leave survivors feeling isolated, even in supportive environments As providers, it helps to frame this not as pathology but as a natural response to a life-altering experience. Survivorship is not about returning to who they were before. It is about slowly learning how to inhabit life as it is now.
Survivors frequently grieve not just what was threatened by cancer, but also what was lost along the way. They may grieve the body they once trusted, the predictability of ordinary life, or roles and dreams that shifted during treatment. Grief in survivorship often shows up quietly through sadness, irritability, longing, or a sense of disconnection from one’s own identity.
When we make space for this grief in the therapy room, we affirm that it belongs. Naming it does not diminish strength; it allows clients to move toward wholeness. Creating space for grief alongside what has carried them through invites integration rather than fragmentation.
Redefining Strength and Self-Care
In survivorship, strength does not always look like determination or productivity Often, strength looks like rest It may show up in setting boundaries, asking for help, or honoring the need for slowness in a culture that values speed.
Self-care, in this context, is not indulgence but sustainability. Survivors may need support in redefining what care looks like for them now. For some, it is reconnecting with movement in gentle ways; for others, it is learning to say no without guilt As therapists, we can normalize these shifts and help clients see them not as weakness, but as the natural wisdom of a body and mind finding their way forward
The uncertainty of the future is a frequent companion in survivorship Scans, follow-up appointments, and anniversaries can reignite anxiety For providers, it can be tempting to reassure or minimize these fears, but often what clients need most is a safe place to acknowledge them
Hope in this space is not about promising certainty or demanding positivity. It is about cultivating the possibility that meaning, joy, and connection can still emerge even with
uncertainty present By modeling how to hold both fear and hope, we help survivors practice living in the tension between what was lost and what is still possible
For mental health professionals, the work is not about ushering clients back into their pre-diagnosis lives, but about walking with them as they step into what comes next Survivorship is not a return it is a threshold. It is moving beyond what was.
Written By: Jessica M. Kilgore, M.Ed CCMHC, NCC
Jessica is the owner and founder o Beyond What Was Counseling. Wit nearly two decades of experience, supports individuals and families by cancer and life transitions. Offe across Florida, Jessica creates a co clients to be seen, heard, and supp toward healing beyond what was




Professional Experience Article
With my area of clinical focus I ask probing questions about sexual thoughts, behaviors, and identities to all the clients I work with. One of those questions is: What’s the content of the porn you watch? The answer I receive a high majority of the time is “normal stuff”, “the regular stuff”, “nothing too crazy”. When rapport has been established, and the client feels a greater ease with me in session, knowing that I am coming from a place of curiosity and care rather than a lens of judgment, they start to open up Porn, like all drugs, has a beginning point The majority of my clients do not start watching the fentanyl of pornography They start with nicotine and caffeine types of porn content. Over time this no longer satisfies the drug saturated brain and alcohol and weed types of porn content come into play. You see where this is going.. By the time a client enters into therapy with me they have been watching porn consistently for years, even decades. The type of content they watch can often bring feelings of shame. They may be into porn that does not align with their value system as well as porn that doesn’t align with their partner’s value system or interests. It’s not uncommon for a partner to experience shock, confusion and betrayal when they discover the content their partner watches. “You’re into that?” they might ask Or, “Are you even attracted to me anymore?”
“What am I actually into?”. Many of my clients utter these words in the beginning phases of our work together. We all have preferences; likes, dislikes and in-differences. We have them to food, media, style, to sex, to everything! Many of my
clients are unsure of what they would be aroused by if they never were exposed to porn I use the word exposed intentionally as most of my clients were shown porn by another person. Not a single client of mine has every shared that they saw porn for the first time over the age of 18. For most it was elementary school and middle school, the minority in their high school years. The days of discovering a magazine under the mattress is long gone. In our hands for hours a day, we now have instant access to the most hardcore and stimulating porn that the human brain has ever experienced in all of our evolutionary history. Read that sentence again, please. And it’s impacting our brains, our preferences, our cravings, our sexuality, our relationships, our lives. But are we talking about this in our society? I want to be clear that I am not anti-porn I am pro intimacy and sex I prescribe porn to clients and couples on occasion I prescribe porn the way a doctor ought to prescribe opiates- when medically necessary For the majority of clients, taking a break from porn is advised This is often very challenging as porn has been a coping mechanism for stress, boredom, loneliness and pleasure for as long as they can remember. When the brain doesn’t get the drug it’s been getting it starts to ask for it through a variety of unpleasant withdrawal symptoms. Porn will always be there a few clicks away, but will your relationship be? When my clients renounce porn and stay away for a period of time, they typically experience a reduction in sexual dysfunctions and an increase in frequency and satisfaction in their sex lives. This motivates them to stay away from porn and not return. Though relapses are common. Porn recovery can be quite challenging and working with a therapist that is trained and experienced in the treatment of porn and sex addiction is key Time and time again, The adults and couples that I work with experience greater intimacy in their relationships, a reduction in mental health symptoms, and once again can be aroused by, you know, like ‘normal stuff’
This article was written with my human therapist brain. Ai was not used in any element and I think it is important for this to be noted.
Written By: Evan Kotler, LCSW

Evan is a licensed psychotherapist providing virtual sessions to clients in Florida, Maryland, New Jersey and Pennsylvania, as as well as in-person therapy in his Boca Raton office. He works with adults and couples facing a wide range of challenges, including anxiety, depression, stress, life transitions, and relationship issues. Evan also specializes in the treatment of sex and pornography addiction.

How it affects other relationships: Other relationships in your life, like those with friends, your children, or romantic partners, can also suffer when you do not take care of your mental health.
Preventing these issues by addressing stress is ideal. There’s no award for not asking for help There’s also no award or reward for waiting until problems emerge or worsen
Here are some steps you can take to care for your mental health as a professional.
It likely comes as no surprise that behavioral healthcare professionals, such as therapists, counselors, and social workers, have high rates of burnout. In fact, it's an epidemic: research shows that over half of behavioral health providers experience symptoms of burnout.[1]
Unfortunately, burnout in the workplace can lead to an array of challenges, like depression, anxiety, insomnia, and substance abuse Many people working in the mental health space also have pre-existing conditions, whether mental or physical, which may be compounded by workplace stress
If you’re like most of us, you likely have stressors that aren’t in your control, such as a large caseload or issues with insurance companies. Structural change is the ideal solution to many of these problems. However, structural change takes time, and many of us can’t wait.
Before we get into how to take care of your mental health as a mental health professional, let’s discuss why it matters in the first place.
How it affects you: In addition to mental health challenges, an increased risk of physical health issues (e g , cardiovascular disease), decreased job satisfaction, and isolation can emerge as a result of unaddressed burnout.[2]
How it affects clients: Frequently rescheduling or missing sessions, being behind on case notes, poor boundaries, or being unattentive during sessions are all possibilities for providers struggling with their mental health.
Be mindful of your needs and meet them using what is within your control This might look like not scheduling clients backto-back when possible, setting aside time for breaks during the day, or creating a comfortable work environment (e.g., temperature, decor).
Many behavioral health providers face traumatic experiences in the workplace. If a traumatic event or stressor arises, don’t ignore it. Whether it relates to your job or another aspect of your life, seek trauma-informed care of your own. Acknowledge these stressors as real, significant challenges that require support.
Maintaining self-care routines is one of the most valuable things we can do for ourselves. For example, healthy sleep hygiene habits, eating regular meals, and physical activity. During times of stress, continuing the healthy routines you establish can help keep you going and ensure that your wellbeing doesn't fall to the wayside.
Workplace boundaries can take different forms. For example:
Don’t check your emails (or otherwise engage in workrelated tasks) for a set amount of time each day and week. Take time away from all work-related functions on weekends and after a specific time (e.g., 6 PM) on weekdays.
Don’t take too much on. Know when to refer prospective clients out.
Don't “take work home” with you. When needed, redirect your thoughts
Remember, workplace boundaries are equally important for your clients. You don’t want to be overwhelmed.
What if you ' re in a situation where your current work is not sustainable in the long run? For example, you might have a negative work environment (e.g., unfair demands, workplace bullying), inconsistent income, or fear of losing income. It might be time to make changes Not all of these need to be immediate Looking for a new job may be necessary in some cases. In others, changing when you work or how you work (e.g., more virtual sessions) could be a solution.
Behavioral health professionals often encounter unique challenges. With so many providers enduring burnout and related issues, it's crucial to remember the value of taking care of yourself. If you’re ever in a situation where you aren’t sure what to do, seek guidance from supervisors or peers.
[1] SAMHSA (n.d.). Evidence-Based Resource Guide Series. Addressing Burnout in the Workforce through Organizational Strategies.
[2] De Hert, S (2020, October 28) Burnout in healthcare workers: Prevalence, impact and preventative strategies Local and regional anesthesia
Written By: Dane Ramdin, Registered Me Counselor Intern

Dane has experience in private practice, schools, and as an Assistant Clinical Director at a foster care agency He supports individuals and couples with anxiety, depression, and relationship challenges, and is passionate about fostering growth and resilience


Provided by Committee Chairs
Get Involved! View all of FMHCA’s Committees here.
Registered Intern & Graduate Student Committee Committee Chair: Laura Peddie-Bravo, LMHC, NCC
It has been a busy few months since our last committee update! Since our last update, our committee participated in FMHCA’s annual Summer Bash, and had guest speakers: Dr Aaron Norton, who spoke with us about FMHCA’s Government Relations Committee (GRC), and Dr Linton Hutchinson who spoke with us about the NMHCE Exam: how to prepare and what to watch out for
Meetings for the rest of 2025
We have two meetings left for this year and we hope you will join us! Our guest speakers will be September, 25 , Bridget Glass, Ph D , LMHC, ACS, Program Director of The Clinical Mental Health Counseling Program at South University and the current FMHCA Secretary, and October 30 , our last meeting of 2025, Jessi Roeder, LMHC, Qualified Supervisor will speak with us about common pitfalls new therapists face. th th
Graduate Student Co-Chair OPEN
We are searching for a new Graduate Student Co-Chair. Please submit your resume to LauraPeddieBravoLMHC@gmail.com.
The 2025 Fund Run!
We have our own Committee Team for FMHCA’s annual “Fund Run”! It will take place between 10/1/25 – 10/30/25. We are all getting our steps in so why not donate those steps to FMHCA! The funds raised go to benefit FMHCA’s Government Relations Committee, (GRC). Specifically, it will go to cover FMHCA’s annual Legislative Days, our PAC fund, and any other advocacy needs determined by the GRC. To sign up, it only costs $15! Join our team! Here’s the link to our team’s sign up: https://runsignup.com/Race/FL/WestPalmBeach/PACFundRun ?raceRefCode=afZ0xYUn and our password is GrcFunRun2025! Questions? Contact Naomi@FLMHCA.org.
The 2026 FMHCA Conference:
The annual conference will be held again in Lake Mary, Florida, beginning with Pre-Conference workshops on 2/4/26, and the main conference taking place 2/5/26-2/7/26.
Volunteer Opportunities: We will look forward to seeing you all at FMHCA’s Annual conference! Graduate Students will be
given priority to volunteer at the conference. If you are interested in volunteering, the applications will open in November. Please visit www.FMHCA.WildApricot.org
Graduate Student Poster Session: Please visit this link in order to register for the 2026 Student Poster Session at the conference: https://www surveymonkey com/r/HD9TQH6 The deadline is 11/30/25, and those selected will be notified by 12/20/25 This is a terrific opportunity to show off your hard work!
Did you know we have our very own Committee Forum on the FMHCA website? Links to previous meetings, important topics, opportunities, and valuable information are posted there All committee members may have access to the forum, and may post questions, issues, desired topics for the committee to cover and of course anything that could be helpful to the group such as learning opportunities, scholarships, and so on. One needs to be granted access to our committee’s forum on the FMHCA website. For assistance, please contact Office@FLMHC.org or call FMHCA’s NEW office phone number 561-916-5556.
Did you know there is a special section on the FMHCA website just for Graduate Students and Registered Interns? It is called “Student Corner,” and it is located in the far upper right-hand side of the top of the FMHCA home page. Here is a link: https://fmhca.wildapricot.org/page-1075394
There are terrific resources there, including information about scholarships, licensure, and much more!
We would also like to announce a change in leadership of this committee After Chairing for five years, Laura Peddie-Bravo, LMHC, NCC, QS, will be stepping down, and Lauren Malone, Registered Mental health Counselor Intern, will be taking over as the new Chair. Jessi Broom will be the Registered Mental Health Counselor Intern Co-Chair, and the Graduate Student Co-Chair is currently vacant (we are accepting applications!)
If you have any questions, please do not hesitate to contact any of us!
Military Committee
Committee Chair:
Maria Giuliana, LMHC, QS
This quarter the Military Committee continued its mission of providing a collegial, practice-focused forum for clinicians who serve veterans, active-duty service members, and military families. Conversations emphasized clinician self-care, TRICARE billing and reimbursement, evolving clinical presentations (including moral injury and military sexual trauma), and strategies to strengthen cultural competency when working with military and law-enforcement populations Below is an updated magazine-style summary of the quarter’s themes, clinical implications, resources, and meeting logistics
Clinician well-being & coping strategies
Clinicians described the personal toll of holding space for clients affected by policy shifts, deployment stress, and highprofile media events Practical coping strategies discussed included limiting news exposure, delegating informationgathering to trusted supports (for example, relying on a partner for headlines), and setting intentional boundaries around media use to reduce secondary trauma.
Why this matters for practice: Modeling and normalizing media boundaries with clients can reduce family anxiety and improve decision-making during high-stress events
Committee purpose: a supportive, practice-focused forum
The Military Committee is a space to bring policy updates, billing questions, case consultation, and peer support. Staying current on legislative, policy, and political developments that affect military populations is a core function because these external forces directly influence access to care and clinical decision-making
Why this matters for practice: Regular engagement with a military-competent peer network helps clinicians respond quickly and ethically to shifting system requirements.
TRICARE billing & reimbursement: practical guidance
Key takeaways shared this quarter:
Use the DoD Benefits Number (DBN) typically on the back of the TRICARE card to verify eligibility and populate claims.
Superbills (itemized statements): TRICARE requires beneficiaries to submit claims (DD Form 2642) within one year of service. While TRICARE does not mandate a fixed issuance frequency, clinicians are encouraged to issue superbills promptly ideally at each session or immediately upon request to protect clients’ ability to file timely claims.
Keep a copy of both sides of the TRICARE card (or record
DBN, name, DOB, expiration) in the chart to avoid claim delays
Providers may pursue TRICARE authorization (nonnetwork) or full in-network contracting (which requires additional credentialing and contracting steps). Nonnetwork providers require patients to submit claims; innetwork providers bill TRICARE directly.
Why this matters for practice: Timely documentation and correct use of DBNs reduce administrative friction and support veterans’ access to reimbursement
Media impact on military families
Media coverage can amplify uncertainty and stress for families Clinical responses discussed include helping families identify reliable information sources, set limits on news consumption, and use grounding techniques during high-anxiety periods
Why this matters for practice: Coupling information-hygiene strategies with safety planning reduces family distress when public events dominate coverage.
Trends in Tricare & VA systems: access & clinical needs
Members reported expanded community-care access and removal of one extra VA-physician review step for referrals, intended to streamline access. However, provider shortages and long wait times persist, alongside increased disclosures of moral injury and military sexual trauma (MST).
Why this matters for practice: Routine screening for MST and moral injury and maintaining updated referral pathways are critical for timely, effective care.
Moral injury: clinical approach
Moral injury harm from actions or inactions that violate one’s moral code was highlighted as a growing clinical presentation. Military-specific complexities (e.g., intra-unit harm, remote/technological operations) require traumainformed, values-centered interventions and meaning-making approaches.
Why this matters for practice: Add moral-injury screening into intake and outcome tracking; use interventions that emphasize restoration of meaning, accountability where appropriate, and trauma-informed repair strategies
Cultural competency: military & law-enforcement populations
The group discussed similarities and differences between military and law-enforcement cultures, noting educational gaps in standard curricula Recommendations included pursuing supervised consultation, targeted continuing education, and
Why this matters for practice: Clinicians should seek focused training or supervision before independently treating specialized populations beyond a generalist scope.
Workforce development: motivations, licensure, & peer learning
Several members shared pathways from peer-support roles into clinical practice after observing gaps during critical incidents. The Committee emphasized mentorship, study groups, and pooled resources to aid clinicians preparing for licensure and specialty practice
Why this matters for practice: Local study cohorts and mentorship pairings bolster workforce capacity and clinician retention.
Future directions & action items
Committee priorities moving forward include:
Deep-dive case presentations on moral injury and MST
Exploration of coordinated advocacy to broaden TRICARE access and streamline veteran care
Continued peer support, resource-sharing, and policy monitoring to protect access and quality of care.
Resources shared with the Committee (Full resource links and downloadable forms are posted on the FMHCA member portal):
Moral injury presentation & podcast (links in member portal)
PTSD measures & resources National Center for PTSD
TRICARE guidance on superbills, DBN usage, and the oneyear filing deadline (official guidance referenced)
TRICARE provider certification portals Humana Military Provider Certification & Network applications (East Region)
Veteran support organizations and referral partners: VA, DAV, Wounded Warrior Project, Boulder Crest Foundation, Songwriting with Soldiers, Save a Warrior, Veterati, SVRN.
Meetings & logistics please join us
All FMHCA members are welcome to join the Military
Committee Regular meeting details:
When: Monthly on the last Friday of each month at 12:00 PM ET
Holiday pause: No meetings in November and December; the Committee will reconvene in January 2026.
Registration reminders: Members typically receive an email reminder to register about one week prior to each meeting. Please watch your inbox and register early to receive Zoom access.
The Military Committee exists to support clinicians working at the intersection of policy, culture, and clinical care for militaryconnected clients. Whether you bring questions about TRICARE billing, a challenging moral-injury case, or simply want to expand your referral network, this committee is a practical place to connect with peers, deepen competency, and advocate for better care Visit the FMHCA member portal for meeting updates, resource sharing and downloads Members are encouraged to contribute tools and referral contacts
Over the summer the EIC Collaborative met virtually to share clinical experiences, surface practice-level challenges, and pool resources for supporting neurodivergent, transgender, and other marginalized clients The July and August sessions focused, candid, and practice-oriented highlighted three interlocking priorities for clinicians: peer collaboration, ongoing competency-building, and clinician self-care. Below is an updated synthesis of the quarter’s key themes, practical takeaways, and upcoming opportunities for engagement.
Peer-to-peer consultation as core practice
The Collaborative continues to be a practical forum for clinicians to present real-world questions billing and reimbursement, ethical boundaries, complex family dynamics and receive peer feedback, referral ideas, and resources. Members repeatedly noted the value of a regular, low-stakes space to test clinical approaches and expand referral networks.
Neurodivergence: late diagnosis, grief, and re-storying life narratives
Late autism and ADHD diagnoses especially among adult women and gender-diverse people evoke both relief and grief. Clinicians named key interventions: psychoeducation, narrative re-storying (e.g., relationship-tree or life-map work), and permission to grieve lost opportunities for earlier support. Research gaps remain, particularly for transgender and nonconforming populations, underscoring the need for ongoing clinician humility and learning
Gender-affirming care: misgendering, ambiguous loss, and family dynamics
Early transition periods were described as emotionally volatile: misgendering at work, family members struggling with name/pronoun changes, and ambiguous loss even in supportive homes Practical approaches discussed included rehearsal spaces for families, values-based work to normalize transitional developmental stages, and targeted tools to help coworkers and
friends acknowledge milestones in safe, affirming ways
Moral injury & system-level stressors
Policy changes and sociopolitical climates that affect access to care surfaced repeatedly in clinical casework Members emphasized combining individual-level skills (traumainformed approaches, screening for moral injury and military sexual trauma) with macro-level engagement (advocacy, resource linkage, and community education).
A strong theme: clinicians should operate within demonstrated competence When needs exceed a clinician’s expertise whether advanced gender-affirming care, intensive neurodivergence work, or moral-injury treatment referral and specialist supervision are ethical necessities. Qualifiedsupervisor training and focused continuing education provide clear pathways for safe expansion of practice skills.
Practical takeaways & shared resources
Qualified Supervisor Training: Typical expectation is five years of clinical experience (commonly counted as two years during internship plus three post-licensure); however, coursework can be started earlier and conferences often provide applicable CE components.
Recommended client resources: Unmasking Autism and Unlearning Shame (Devon Price) were recommended for client psychoeducation on masking and shame.
Therapeutic tools: Relationship-tree work, ambiguousloss worksheets, and structured psychoeducation modules for late-diagnosis clients will be made available in the member portal
Referral maintenance: Keep updated lists for genderaffirming medical providers, voice coaches, and psychologists who write supporting letters; include local and out-of-state options.
Clinician supports: Peer consultation groups and moderated professional spaces are essential for processing secondary stress and politically charged cases.
Insufficient military and first-responder cultural training in many academic programs.
Ongoing provider shortages and long waitlists for specialized services (autism assessments, gender-affirming care).
Complex family histories that interfere with acceptance, requiring grief-focused and attachment-informed interventions.
Ethical navigation of political content in therapy and maintaining scope when facing novel clinical presentations
Meetings, conference notes & how members are notified
Meeting cadence: The EIC Collaborative meets monthly on the last Friday at 12:00 PM ET The group pauses in November and December for the holidays and resumes in January. (Exceptions and schedule changes will be announced on the member portal.)
Conference & CE: The FMHCA annual conference remains a prime opportunity to earn targeted CEs and advance qualified-supervisor training requirements watch preconference offerings for relevancy to EIC topics.
Member portal & resources: Resource packets (ambiguous-loss worksheets, relationship-tree templates, curated readings) will be uploaded to the forum. Members are encouraged to contribute tools and referral contacts.
Registration reminders: Members typically receive email registration reminders approximately one week prior to each meeting please watch your inbox and register early to receive Zoom access details
The EIC Collaborative exists to strengthen clinicians’ capacity to serve marginalized clients with skill, compassion, and ethical clarity Whether you work with neurodivergent, transgender, immigrant, veteran, or other underserved populations or you want to deepen your cultural competency please join us Bring a case, share a resource, or listen and reconnect with peers who carry similar concerns.
Visit the FMHCA member portal for meeting updates, resource downloads, and announcements. Together, through regular peer collaboration and shared learning, we can build more effective, equitable, and resilient clinical practices
Government Relations Committee
Committee Chair: Aaron Norton, PhD, LMHC, LMFT
We are in between legislative sessions, so the GRC has been focused on preparing for the upcoming legislative session but also addressing rules and policies that are important to our members, including the following: Drafting and sending a Board-approved letter to the Governor’s Office urging the Governor to appoint board members to fill the six vacant positions on the Board of Clinical Social Work, Marriage and Family Therapy, and Mental Health Counseling (a.k.a. the “491” Board) so that critical board functions are not further delayed. Drafting documents explaining concerns related to the
passage of HB 1091/ SB 1240, which resulted in several FMHCA members being removed as court-appointed experts for certain questions related to criminal cases, contributing to a critical shortage of experts in some areas of Florida, sending those documents to the bill’s sponsor and to the Florida Association of Criminal Defense Lawyers, and requesting meetings with legislators to discuss those issues.
Investigating two Board of Education rules that do not include counselors on lists of professionals whose diagnoses can be considered for eligibility for Vocational Rehabilitation services and evaluations related to ESE program eligibility, submitting a report to the Boad about the issue, securing survey responses from FMHCA’s members about the issues, and drafting a sample letter that was submitted to the FMHCA Board of Directors for review and approval
Seeking and obtaining clarification from the 491 Board about whether graduates of 60-credit hour CACREPaccredited school counseling programs are eligible for licensure as a mental health counselor.
Forming a subcommittee that will work on creating a detailed annual report of 491 Board disciplinary cases that can be used as an educational tool for counselor educators and a cautionary report for practicing counselors.
Investigating possible conflicts between recently passed Florida statutes and CACREP standards for counselor education programs
Preparing for 2025-2026 efforts to pass legislation renaming registered mental health counselor interns as registered associate counselors and removing a line in statute that requires registered interns in private practice settings to have a licensed mental health professional on the premises when providing clinical services (even when those services are provided via telehealth from a home office).
Joining a committee is a great way to participate in FMHCA and increase your presence in our community. We have several committees that we would love you to participate in! Below is a list of all our committees and their chairperson.
We invite you to contribute your efforts as there are numerous opportunities for you to get involved and make a difference. For more information on how to participate right away, please contact the chair committee or fill out this form.


FMHCA Member Questions Answered by President and Managing Partner of The Health Law Firm, George F. Indest, J.D., M.P.A., LL.M.
AQAs a Qualified Supervisor, can you bill insurance using your credentials for your supervisees / Registered Mental Health Counselor Interns?
Yes, as long as your contract with the paying insurance company does not state that it is prohibited In the case of a Medicaid managed care insurance company, this is allowed by Medicaid laws and guidelines
It is probably better to have a group provider number, and make sure the intern is signed up as a provider within the health insurance company and with the Medicaid Program, with their provider number re-assigned to the group The group should then bill for the services
AQWhen treating a minor child of divorced, separated or never married parents, what type of consent is necessary and from whom? and services.
Unless there is an order from a court providing otherwise that you are aware of, each parent of a minor child is considered the natural guardian of a minor child Either parent can sign a consent form and authorize any and all care
Mr. Indest is board certified by The Florida Bar in the legal specialty of health law. He is the President and Managing Partner of The Health Law Firm, based in Orlando, Florida. The information provided in this article is for educational and informational purposes only and does not constitute the provision of legal advice.
Want your question featured in the next InSession issue? Submit Here
Must be a FMHCA member to submit Become a FMHCA member by clicking here