Dr Kathie Erwin










Page 9
The Licensed Clinical Mental Health Counselor’s Role in Supporting GenderAffirming Medical Interventions
Page 15
Four Ways to Clinically Support New Parents
Page 17
A Therapist’s View: Embracing the Dating App

Page 36
Page 20
Autism & Mental Health

Page 24
Remembering Dr. Darlene Silvernail
Page 26
Clinician’s Wellbeing as a Clinical Intervention
Page 28
From Spilled Milk to Golden Moments: The Art of Kintsugi as a Mindful Parenting Lifestyle
Managing the Fallacy of Mental Health Counseling as a Cure all Solution
Page 38
Unseen Warfare: Bridging Emotional Frontlines with Holistic Care for Veterans and Their Loved Ones
Page 40
Meeting in the Middle: Connecting Clients Right Where They Are

Page 42
One Therapist’s Own Moment with Music Healing through Expressive Arts Therapy
Page 44
They Don’t Understand Me!
Page 49
Managing Self Care as a Therapist
Page 54 Legislative Update

InSession Magazine is created and published quarterly by The Florida Mental Health Counselors Association (FMHCA)
FMHCA is a 501(c)(3) non for profit organization and chapter of the American Mental Health Counselors Association
FMHCA is the only organization in the state of Florida that works exclusively towards meeting the needs of Licensed Mental Health Counselors in each season of their profession through intentional and strengthbased advocacy, networking, accessible professional development, and legislative efforts.
Let your voice be heard by becoming a FMHCA Member today!
Click here to view FMHCA's current Bylaws.
CONTRIBUTE:
If you would like to write for InSession magazine or purchase Ad space in the next publication, please email: Naomi Rodriguez at naomi@flmhca org
THE INSESSION TEAM:
Naomi Rodriguez- Editor
Victoria Siegel, LMHC- Expert Advisor
There shall be no discrimination against any individual on the basis of ethic group, race, religion, gender, sexual orientation, age, or disability
DISCLAIMER:
Information in InSession Magazine does not represent an official FMHCA policy or position and the acceptance of advertising does not constitute endorsement or approval by FMHCA of any advertised service or product InSession is crafted based on article submissions received. Articles are categorized between Professional Experience Articles & Professional Resource Articles.
Professional Experience Articles are writer's firstperson pieces about a topic related to their experience as a mental health professional, or an opinion about a trend in the mental health counseling field
Professional Resource Articles are in-depth pieces intended to provide insights for the author's clinical colleagues on how to be more effective with a particular type of client or a client with a particular disorder, or tips for running their practice more efficiently Each article is labeled with their article type
The Florida Mental Health Counselors Association (FMHCA) is the State Chapter of the American Mental Health Counselors Association (AMHCA) FMHCA is the only organization dedicated exclusively to meeting the professional needs of Florida’s Licensed Mental Health Counselors
The mission of the FMHCA is to advance the profession of clinical mental health counseling through intentional and strengthbased advocacy, networking, professional development, legislative efforts, public education, and the promotion of positive mental health for our communities
Its sole purpose is to promote the profession of mental health counseling and the needs of our members as well as:
Provide a system for the exchange of professional information among mental health counselors through newsletters, journals or other scientific, educational and/or professional materials
Provide professional development programs for mental health counselors to update and enhance clinical competencies
Promote legislation that recognizes and advances the profession of mental health counseling
Provide a public forum for mental health counselors to advocate for the social and emotional welfare of clients
Promote positive relations with mental health counselors and other mental health practitioners in all work settings to enhance the profession of mental health counseling
Contribute to the establishment and maintenance of minimum training standards for mental health counselors
Promote scientific research and inquiry into mental health concerns
Provide liaison on the state level with other professional organizations to promote the advancement of the mental health profession
Provide the public with information concerning the competencies and professional services of mental health counselors
Promote equitable licensure standards for mental health counselors through the state legislature
















Has a client ever asked you to write a letter recommending hormone replacement therapy (HRT) or gender-affirming surgery? I’ve been writing such letters since 2013, and I’ve seen practice standards shift over the past 10 years. This article highlights current practice standards, offering you a brief introduction to the role of Licensed Clinical Mental Health Counselors (LCMHCs) in supporting gender-affirming medical interventions First, though, I want to stress some legal and ethical considerations related to writing such letters
Many but not all transgender clients meet the diagnostic criteria for gender dysphoria as depicted in the most current edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5-TR) Medical interventions for treating gender dysphoria have become a politicized issue Having addressed and responded to concerns from members in my state chapter of AMHCA, where I chair our Government
Relations Committee, I’ve been exposed to a variety of perspectives on how LCMHCs should address this issue. On one end of the spectrum, some enthusiastic members think LCMHCs should “always” support clients seeking such letters, and on the other, some think LCMHCs should avoid writing such letters. My experience has been that most LCMHCs express a perspective that lies somewhere between these two extremes, believing that writing such letters is appropriate in some cases and not in others.
Depending on the state in which you practice, laws and rules may restrict your ability to write such letters For example, a law passed in May 2023 in my state of Florida (SB 254/HB 1421):
Prohibits physicians from offering hormone replacement therapy and gender-affirming surgeries to minors, Bans the use of state funds for “sex-reassignment prescriptions or procedures,”
Requires informed consent for adults receiving “sexreassignment prescriptions or procedures,” and Permits patients to recover damages for personal injury or death resulting from the provision of “sex-reassignment” prescriptions or procedures for minors as much as 20 years after such procedures.
Such restrictions undoubtedly make it much harder for clients with gender dysphoria to access gender-affirming care
The Human Rights Campaign Foundation reacted to these bills with press releases claiming that “Florida Senate Passes Extreme Gender-Affirming Care Ban” (April 4, 2023), and “Florida Legislature Sends Extreme Gender-Affirming Care Ban to Governor’s Desk” (May 4, 2023) While HRC succeeded in drawing attention to this important issue, such press releases are misleading, as Florida did not actually “ban” gender-affirming care.
For example, the bill doesn’t ban gender-affirming surgeries for adults, commercial insurance and private-pay funding for gender-affirming surgeries for adults, procedures or therapies to a minor born with a medically verifiable genetic disorder related to sexual development, gender-affirming prescriptions and procedures for minors who were already receiving such treatment before the law was passed, and social gendertransition services for minors or adults
As far as I can tell, nowhere in the country does a state law exist that bans gender-affirming care for adults, and I doubt that such a hypothetical law would be constitutional. However, some states do ban or restrict the use of public funds for genderaffirming procedures, restrict or ban certain forms of genderaffirming care for youth, and/or have no laws requiring that commercial insurance companies offer coverage for genderaffirming care
The Movement Advancement Project (MAP), a nonprofit think tank for an inclusive and equitable America, offers a frequently updated map of bans on transgender care for youth, concluding that 21 states have banned gender-affirming surgery for transgender youth. MAP also offers a map of healthcare laws and policies that permit insurance companies to deny health insurance coverage for transgender care, especially for youth.
Because of variation in state laws related to medical interventions for youths with gender dysphoria (“marked incongruence between [a person’s] experienced or expressed gender and the one they were assigned at birth,” LCMHCs should be knowledgeable about current laws and rules that may impact their roles in writing letters of support for such interventions.
In a post-pandemic world of telehealth and the upcoming Counseling Compact, LCMHCs should also know the laws and rules affecting gender-affirming interventions such as genderaffirming surgery and hormone replacement therapy in the states or countries where their clients are physically located, especially given that state laws and rules generally allow LCMHCs to be disciplined for violating laws, rules, and practice standards in other jurisdictions. According to recent articles published in U.S. News & World Report, Forbes, and the Society for Evidence Based Gender Medicine, European countries such as Denmark, Finland, Norway, Sweden, and the United Kingdom restrict gender-affirming medical interventions for transgender youth, and in other countries (e.g., France), medical academies recommend “the greatest reserve” for such interventions.
I do not intend to tell LCMHCs what to believe from a political or religious perspective, but I do think it’s important to stress that, according the AMHCA Code of Ethics, we are obligated to avoid imposing our personal beliefs on our clients (I.A.4.d), and we are called on to “ensure client autonomy and selfdetermination,” and, barring cases of imminent harm, to avoid any therapeutic approach that “impedes an individual’s right to make informed choices” (I A 1 a) These ethical directives carve out a space for LCMHCs to respect the informed choice of a client pursuing gender-affirming care even when there is friction between client choice and the LCMHC’s personal beliefs. LCMHCs are also encouraged to advocate appropriately for clients (I.F.2).
LCMHCs must, however, balance respect for client autonomy with values of nonmaleficence (i e , avoiding harmful interventions) and beneficence (doing good for clients) Sometimes, clients later regret participating in medical interventions for gender dysphoria, and some researchers report evidence of deteriorating mental health after participating in such interventions. However, regret appears rare, among both adolescents and adults. Generally, the prevalence of regret seems to be less than 1 percent. For example, a 2021 meta-analysis published in Plastic and Reconstructive Surgery found the prevalence of regret to be about 1 percent among gender-affirming surgery patients. In a review of more than 200 adolescents who obtained genderaffirming mastectomies published in 2022 in Annals of Plastic Surgery, the prevalence of regret was also about 1 percent. Nonetheless, some researchers’ reviews of others’ research have resulted in seemingly contradictory findings. For example, a
review published in 2023 in Current Sexual Health Reports reported that “systematic reviews of evidence conducted by public health authorities in Finland, Sweden, and England concluded that the risk/benefit ratio of youth gender transition ranges from unknown to unfavorable” and highlighted recent research that found previous research published on the benefits of youth gender transition services was “deeply flawed.”
A 2023 paper published in the British Medical Journal offered evidence that as the prevalence of gender dysphoria diagnoses rises, the detransitioning movement (i e , individuals discontinuing or reversing transition) has been growing, and research suggesting lower rates of regret among transitioning clients is flawed because individuals who drop out of transition treatment (over 30 percent in some studies) are more likely to experience regret and yet are not included in study results. I do not know how prevalent regret is, but I have never personally written a letter supporting a gender-affirming medical intervention and then learned that my client regretted the decision On the contrary, clients for whom I have written letters have generally reported significant relief and reduced distress when they access gender-affirming medical care I have, however, worked with several youth who at one point identified as either transgender or gender-variant (an umbrella term used to describe gender identity, expression, or behavior that falls outside of culturally defined norms associated with a specific gender) and then later re-identified as cisgender, sometimes citing the influence of social media or friends and the desire to be “special,” unique, or different as explanations for why they temporarily identified as gender-variant.
I have also worked with an adult in his late 20s who had had gender-affirming surgery at 18 years of age and deeply regretted it. He believed that he made the decision prematurely during a depressing period in his life and was not thinking clearly.
Given my experiences with such cases, it seems clear to me that in addition to bracketing our personal values and beliefs, honoring client autonomy, and advocating for our transgender and gender-diverse clients, we LCMHCs have a responsibility to ensure that the services we provide, such as writing letters of support for HRT or surgery, are unlikely to cause harm How can we balance these ethical directives?
I argue that adherence to evidence-based practice standards can facilitate the process of responding to client requests for letters of support, and this process often includes mental health professionals such as LCMHCs. AMHCA’s Standards for the
Practice of Clinical Mental Health Counseling includes a section on gender-identity counseling standards and competencies detailing the knowledge and skills that LCMHCs should possess when providing specialized work in gender-affirming counseling This document calls on LCMHCs to “demonstrate competence with documentation changes, World Professional Association for Transgender Health (WPATH) letter writing, and the counselor’s role as an advocate and ally rather than gatekeeper.”
WPATH’s Standards of Care (SOC), first developed in 1979 and most recently updated in 2022 (Version 8), are, according to WPATH, “based on the best available science and expert professional consensus ” LCMHCs can play an important role in many of the standards outlined in the SOC In this section, I will offer a description of each standard that I think highlights our expertise as LCMHCs.
For both HRT and surgical interventions, WPATH’s SOC highlight the importance of a “multidisciplinary team” (i e , SOC 12.8, 13.7, 13.8, 13.11). Such teams will often include mental health professionals, such as LCMHCs, who are working with clients seeking gender-affirming medical interventions.
Although SOC 5.5 (Assessment of Adults) asserts that although only one opinion favoring gender- affirming medical treatment is needed for the initiation of such treatment, “further written opinions/signatures may be requested where there is a specific clinical need.” In my experience, surgeons and other medical providers therefore often ask clients to obtain a letter of support from a mental health professional, especially if the client is participating in psychotherapy or has co-occurring mental disorders
Biopsychosocial Assessment of Adolescents
Standard 6 3 (Adolescents) recommends that “health care professionals working with gender-diverse adolescents undertake a comprehensive biopsychosocial assessment of adolescents who present with gender identityrelated concerns and seek medical/ surgical transition-related care, and that this be accomplished in a collaborative and supportive manner.”
WPATH asserts that biopsychosocial assessments should “aim to understand the adolescent’s strengths, vulnerabilities, diagnostic profile, and unique need to individualize their care ” Given our expertise with biopsychosocial assessment and our capacity to diagnose mental disorders, LCMHCs can be helpful in conducting such assessments. In fact, WPATH asserts that mental health professionals “have the most appropriate
training, experience, and dedicated clinical time required to obtain” such information
Standards 18.1 through 18.9 assert that although WPATH acknowledges that psychotherapy can be helpful for many clients seeking gender-affirming medical interventions, they do not think it should be “mandatory” to be eligible for such treatment. However, these standards include recommendations that mental health professionals:
Address mental health symptoms that interfere with a person’s capacity to consent to gender-affirming treatment before medical interventions are provided,
Assess the potential impact that mental health and substance-related symptoms might have on outcomes related to medical interventions,
Assess the need for psychosocial and practical support before, during, and after participation in medical procedures, and
Counsel and assist clients with abstinence from tobacco/nicotine prior to gender-affirming surgery.
To address these standards, I include the following components in my letters of support for gender-affirming medical interventions (i e , HRT and/or gender-affirming surgery):
A description of the duration of my relationship with the client and the nature of the treatment I’m providing (e g , treatment plan goals)
Whether and how the client meets diagnostic criteria for gender dysphoria, including duration of symptoms (e.g., when symptoms first emerged)
A summary of the client’s psychosocial assessment, including diagnoses and social supports with respect to the transitioning process:
For each client I assess, I ask the client to complete a biopsychosocial questionnaire that collects information about the client’s presenting concerns, treatment history, trauma history, family psychiatric history, biomedical conditions and history (including medications), substance use history, family history, social and spiritual history, developmental history, educational and vocational history, and perceived strengths and weaknesses I then meet with the client to get additional information about their responses to items on the questionnaire.
As part of the diagnostic process, I tend to administer screening instruments such as the DSM-5-TR crosscutting symptom measures, but also more sophisticated tests such as the Personality Assessment
Interview (PAI), and I tend to offer relevant data from such tests when writing my letter
If co-occurring disorders exist, I describe whether and how such conditions could potentially affect the client’s outcomes from gender-affirming medical interventions and whether/how we have addressed those conditions On occasion, I have concluded that I lacked certainty in this area. For example, I once worked with a client who was diagnosed with antisocial personality disorder, had a history of violence against animals, and in the past had sometimes struggled with impulses to harm people. I reported this information in my letter and acknowledged that I did not know how HRT might affect the client’s violent impulses and would defer to the expertise of an endocrinologist on the matter as it was beyond my expertise as an LCMHC.
A description of the client’s actions related to transition (e g , what the client has already done to transition, how long those actions have been taking place, etc )
A description of the clinical rationale supporting the client’s participation in gender-affirming surgery
Whether the client has the capacity to make a fully informed decision and to consent to medical treatments
Evidence that the client is making an informed decision to participate in a gender-affirming medical procedure (i.e., a description of how the client and I have thoroughly explored the client’s perception of perceived benefits and drawbacks associated with transitioning).
Previous versions of WPATH’s SOC have, according to a May 2022 article published in the Canadian Journal of Psychiatry, been criticized for overemphasizing the mental health professional’s role in the “gatekeeping” of gender-affirming care. I was originally trained to use the 7th version of WPATH’s guidelines, which essentially required clients to be evaluated by qualified mental health professionals to participate in HRT or surgical interventions.
The 8th and current version of WPATH’s SOC warns against the misuse of standards to practice gatekeeping (i.e., preventing some clients form accessing gender-affirming care). For example, WPATH acknowledges that, “Psychotherapy can be experienced by transgender persons as a fearful as well as a beneficial experience … and presents challenges to the therapist and to alliance formation when it is associated with gatekeeping for medical interventions.”
Therefore, LCMHCs are not only required to (a) balance our
ethical directives related to client autonomy, advocacy, beneficence, and nonmaleficence, and (b) attempt to adhere to WPATH’s SOC We must also remember the spirit of these standards, which is focused on supporting clients in accessing quality care for gender dysphoria.
This article was re-published with permission from the American Mental Health Counselors Association’s Advocate Magazine.
Written By: Aaron Norton, PhD, LMHC, LMFT, MCAP, CCMHC, CRC, CFMHE
Dr Norton is a Licensed Mental Health Counselor and Licensed Marriage and Family Therapist who serves as an assistant professor of instruction at t y of South Florida’s Department of Mental Health Law and Policy, executive director of the National Board of Forensic Evaluators, and Southern Region director for AMHCA He has 20 years of clinical experience providing psychotherapy, supervision, and clinical and forensic evaluation (www.anorton.com).


2024WEBINARSERIES
Join in on one of our upcoming webinars!
Cultivating Excellence: Redefining Perfectionism in Performance Counseling
19 April 2024 | 2:00 PM-4:00 PM
Presented by: Kathy A Feinstein, PhD, LMHC, CMPC Register Now
Shadow Work
26 April 2024 | 2:00 PM-4:00 PM
Presented by: Jessmary Echevarria, LMHC Register Now
Accepting Help: Addressing Burnout and Burnout Prevention
10 May 2024 | 2:00 PM-4:00 PM
Presented by: Ashley Burchell, LMHC, LPC Register Now
The Brain Become What the Brain Does
17 May 2024 | 2:00 PM-4:00 PM
Presented by: Dr Vince Callahan Register Now
Divorce Transformation: Everything A Therapist Needs To Know About Divorce
31 May 2024 | 2:00 PM-4:00 PM
Presented by: Elinor Robin, PhD, LMFT, LMHC Register Now
How to Identify and Overcome Compassion Fatigue & Burnout in the Human Services
07 June 2024 | 2:00 PM-4:00 PM
Presented by: Elliot D Cohen, PhD & Gale S Cohen, EdD, LMHC, NCC Register Now
How to Identify and Overcome Compassion Fatigue & Burnout in the Human Services
07 June 2024 | 2:00 PM-4:00 PM
Presented by: Elliot D Cohen, PhD & Gale S Cohen, EdD, LMHC, NCC Register Now
& more here!


On February 28th, I gave birth to my 4th and final child In the days that followed, I struggled through the sleepless nights, the doubts, the worry, and the delight that comes with adding a new child to the family. I felt myself being tugged by emotions that were outside of my control and thought of clients I have worked with. Even with my training and with the 20+ years of experience as a parent, there were moments I wondered, “what have I done?” I kept coming back to the question, how can we best support those new parents going through this phase?
Clinically, there are many skills that we can exercise to assist our clients in this period Before we do, it is important to assess our own privilege Even if you have had several children and feel you know what it is like, it is essential that you look at your situation and honestly assess your positionality. Maybe you had economic resources, friends and family to help, mentors, experiences, secure housing, food resources, or lower levels of mental health and/or physical health challenges. As we assess our client, we need to be aware of our own positional bias and how it may influence our therapeutic approaches.
Normalize: The first step in addressing our postpartum parents is to normalize the experience I have heard clients say, “I feel so out of control” many times when discussing this portion of their lives. We can address this from a biopsychosocial lens and share information regarding the biological changes, effects of sleep deprivation, and social isolation that comes with the newborn stage. It is normal to feel conflicted, to feel drained and to wish for your life back. Normalizing these feelings will help move past guilt and shame and into acceptance.
Connection: Modern society doesn’t provide the village it takes to raise a child for many people As we strive for independence, we forget the power of community Compile a list of social groups that are free or low cost. Some may be online only (make sure to check the group out first as some online groups can promote misleading and even dangerous information).
Encourage your client to engage in these groups to help them process the life changes and establish mentorship with someone who has had a child recently.
Communication: If your client had their child as part of a couple, they may be noticing changes in their relationship that may be worrisome They may wonder what their relationship will look like after this newborn phase is over They may even mourn the parent they thought their partner would be. It is important for therapists to work with the couple to develop effective ways to communicate that allow each partner to express their feelings and work towards getting their needs met. Often, communication is the first casualty of sleep deprivation in a couple. Opening the lines of communication early on will help problem solve as the couple moves through the first weeks and months of their child’s life.
Realign: Most parents experience a fantasy of their child as they move through pregnancy Often, the reality of the experience does not live up to the hype. Allow your client to articulate their fantasy and then discuss the reality. Celebrate the beauty in what is real while they mourn the loss of what they had imagined. Creating new goals, hopes and dreams based on objective reality will help them refocus and move forward with purpose rather than being stuck in the sadness of a lost fantasy. Giving our clients permission to not be perfect is so empowering. Often we set the bar too high in our expectations for this period. By bringing it down, considering this period as a brief and intense season where expectations for self can and should be lowered, we create a reality that is attainable.
Giving your client time to process and heal their mind and body is the most important part of supporting a new parent. Recognition of the difficulty of this phase of life and realigning expectations will support growth and coping and can leave lasting change that promotes resilience and connection.
Written By: Nattalie Wolff-Tseng, LMHCNattalie is a mental health counselor & doctoral student pursuing a PhD in counselor education and supervision located in the Tampa Bay area. She works with individuals and couples providing and reproductive counseling support. She proudly serves the LGBTQIA+, kink, and poly communities.




While on line dating apps are wildly popular in the U.S. and Florida, many young women and men are becoming disillusioned with them. Can I really find a partner that will lead to a long-term relationship, even marriage, this way? After the first date, is this person really someone I want to continue to see? Is what I’m viewing on this profile really who this person is? These and many other questions are coming up in my sessions lately, especially with the late 20’s to mid-30’s age group. Most are looking for fun as well as a partnership and, in many cases, someone they can marry and have children with if that’s their goal
My young female clients report that men talk only about themselves, while men say women don’t seem interested in what they’re into or want to learn more about them. First dates are often a letdown with each party going home disappointed
and frustrated. So much of the effort that went into the initial back and forth texting, planning the date and getting ready doesn’t lead to the expected outcome. The excitement of meeting someone new seems to be gone.
How do we move past this pattern of dating and, as therapists, encourage our young clients to take chances and risks as they meet new people and look for life partners?
I have personally coached clients to use dating apps as only one of the ways they are meeting people out in the world Creating and curating a stance of openness and curiosity in all areas of their lives seems to help the burden of being “on” during a date or meet up. Humans are attracted to happy people, and want to be around someone who looks like they are enjoying life. Engagement with the world around us - be it with a coworker,
the barista or to pick up take out – makes for good practice to bring an interested energy to a first date
How does this look exactly? When meeting someone new, be it a possible new friend or potential date, I encourage my clients to follow up an initial smile with a question, and not one that has a simple yes or no answer. Practice the follow up question, the compliment, the casual comment that indicates interest in knowing more about who this person is While the benefit may not pay off in the moment, growing and stretching these social skills may pay off in a business networking event or other future meet up
I remind my clients that relaxed and engaged communication does take practice, and they should trust their instincts and comfort level when engaging new people. But I tell them it is
worth the investment and they will build self-confidence and new muscles in the process Encouraging my clients to be bold in how they engage new people – and holding space to reflect on the experience during our next session – has been a worthwhile part of my psychotherapy practice.
Written By: Noreen F. Weihe, MA,Noreen F Weihe is a psychothera Florida Licensed in Florida, Wash and California, Noreen enjoys wo looking for help with anxiety, life challenges and living lives of joy FMHCA, Noreen is currently accep www counselingmadisonpark com www psychologytoday com



Professional Resource Article
Autism Awareness Month is an excellent opportunity to shed some light on the continuing need for autism informed mental health professionals. As a societal whole, we have seen extreme
growth in the past decade in early diagnosis and therapies including occupational, physical, behavioral and speech for persons diagnosed with ASD While this progress is critical, the mental health field has fallen short with very few providers feeling trained or confident enough to treat ASD or support the families involved. There is an ever-increasing need for a specialized skill set in individual and family counseling as well as psychoeducation/parent training in ASD.
According to the CDC, 1 in 36 children born today will meet criteria for autism spectrum disorder Of that number, approximately 70 percent will meet criteria for mental health disorders including ADHD, anxiety disorders, depression and obsessive compulsive disorder (Costello et al 2003;Guerney et.al.2006; Lai et.al.2019; Simenoff et.al. 2009). Yet, there are precious few mental health professionals willing to take cases due to a lack of knowledge and skill (Brookman-Frazee et.al., 2012; Maddox et al.; 2019). There are some trainings available for those interested, but rarely are classes offered in graduate programs that are ASD specific.
I was fortunate enough to begin working with individuals with ASD about fifteen years ago It was not planned, just a life event that took place that landed me into what now has become a specialty I have felt honored to work as the mental health counselor for an internationally known charter high school for individuals with ASD in Jupiter, FL. I had very little knowledge coming into this job, but over the years have developed an understanding of what is needed from a mental health perspective. This includes the following: an understanding of the diagnosis specific to gender and age; rapport building skills based on knowledge of social communication deficits; family counseling skills with an awareness of everyone’s place on the spectrum of acceptance.

Autism is a social communication disorder. The innate ability to pick up on social cues is limiting to varying degrees. This can be a difficult concept to grasp for those of us that can tell when to stop talking or if another is uncomfortable based on facial expression or body language. Early on in my time at the school, I had an experience that truly made me understand.
I was walking with a class down a hallway with doors separating parts of it A student walked through the door without extending his arm behind him This resulted in the door hitting his classmate behind him in the face. With a first, untrained glance, it could be assumed that this boy was rude or absent minded. In reality, this simple gesture had never been programmed. I thought back to how I learned to hold a door open for the person behind me. I could not remember a parent or anyone else verbally instructing me to do so or why it is
considered good manners I observed it I observed my mother holding a door for the person behind her and that person thanking her and smiling I recognized nonverbal gestures and learned from them that this was a positive or good thing to do. Persons with ASD struggle to recognize these cues.
When we first meet most of our clients, we lean forward to show interest, we smile and maintain eye contact to produce a safe feeling These skills are reinforced in graduate school but learning them occurred throughout childhood We picked them up through the modeling of others and they were reinforced over time They became almost automatic When one has limited ability to understand social communication, these efforts on the part of the therapist may not yield results Eye contact can be difficult for many persons with ASD. It has been described to me in various ways over the years, “like nails on a chalkboard times ten”, “makes my stomach feel weird” or “it feels invasive”. These are also common responses to anxiety. Individuals with ASD may feel anxious with these typical rapport-building strategies.
I think it is important to stress my understanding of this I may state that if they are more comfortable, I can make less eye contact for now I will tell them that the counseling room is safe with words over actions I can offer a social story with these things in written words, symbols or a combination of the two as well.
Emotional dysregulation is another common trait among individuals with ASD. This manifests in several ways such as a meltdown, tantrum, impulsive behaviors or sudden outbursts. What seems like an overreaction to others is sparked many times by sensory overload (lighting, noises, sounds or smells) or delayed processing of thoughts and events throughout the day Helping clients understand precursors to these occurrences is key to managing emotions Once precursors are designated, therapist and client can explore many different calming strategies to thwart a meltdown. These may include meditation, taking a break from the setting, various breathing exercises or accessing preferred stimuli.
Of individuals diagnosed with ASD, 70 percent are male. Recent research suggests that this figure does not accurately describe the percentage of the population impacted by ASD There are theories to this statistic including the Extreme Male Brain Theory (Simon Baron-Cohen, 1994) and Female Phenotype Theory (Hannah Belcher, PhD 2019)
The Extreme Male Brain Theory compares autistic traits to the extreme of the “normal” male profile. It discusses fundamental gender differences on a continuum, with social intelligence, correlated with female thinking on one side and following rules
and recognizing patterns, correlated with male thinking on the other It goes on to offer explanation for gender diagnostic differences to include that many autistic traits are extremes of the male’s brain. This theory has been criticized because assessments utilized in its development are based on gender stereotypes.
The Female Phenotype Theory discusses differences in expression of autistic traits between male and female It supports the idea that females are innately more social than males and this contrasts with ASD being labeled a social communication disorder She asserts that this is a likely reason for under or misdiagnosis of ASD in females
Girls are often underdiagnosed or misdiagnosed in childhood or adulthood. Some common misdiagnoses are ADHD, ADD, anxiety and depressive disorders. Misdiagnosis in adult women includes borderline personality disorder and bipolar disorder. These misdiagnoses are often given because of executive functioning deficits, emotional dysregulation, impulsivity and self-injurious behavior commonly seen in autistic persons
Theories suggest that females desire to attain friendships and socialize tends to be more obvious than their male counterparts. This may invite an overlooking of other criteria met for the disorder including deficits in social-emotional reciprocity. Another example of this may be “restrictive, repetitive patterns of behavior, interests or activities”. A high school aged boy may have vast knowledge and extreme interest in dinosaurs whereas a female may have vast knowledge and extreme interest in the latest boy band. Extreme interest in a boy band is easily overlooked as a symptom of autism because it is deemed age appropriate and mirrors peers
Masking or camouflaging is a strategy sometimes used by persons on the autism spectrum to appear less autistic. They may repeat things they have seen or heard that they feel is how one model behavior seen one is expected to act given their age or setting. This is also referred to as scripting behavior. A high school student I worked with once watched a popular teenage comedy show multiple times. The scene she was interested in showed a girl flirting with a boy. The actress flipped her hair and dramatically said “that’s amazing” in response to everything that the boy was saying The student would reenact this behavior in conversation with several boys that she encountered She scripted this because the scene in this show depicted flirting behavior
Masking or camouflaging can also involve forcing eye contact or suppressing autistic traits. If an autistic person rocks back and forth to self soothe, they may choose to suppress this in social situations. If they typically avoid eye contact to decrease
sensory overload, they may concentrate on another’s eyes in conversation Essentially, these coping strategies are forcefully ignored, leaving them vulnerable to extreme emotional discomfort.
Scripting or camouflaging has been associated with increased anxiety, sensory overload, self-injurious behaviors, autistic burnout and suicidality. Autistic Burnout is a term used to describe a social-emotional withdrawal or isolation, physical and emotional exhaustion, increase in manifestation of autistic traits and a decrease in executive functioning Research indicates that the risk of suicidality is eight times more likely in females and two times more likely in males with a diagnosis of ASD (Kirby et al 2019)
The number of adults being diagnosed with autism spectrum disorder has dramatically increased in the last decade. This is likely due to improvement in assessment and recognition of autistic traits. I have had the pleasure of working with clients in their forties that had just been diagnosed with ASD. For some, it leads to a more thorough source of identity and relief A feeling of life experiences making more sense While for others there are increased struggles with self-understanding, a sense of identity and acceptance Many persons diagnosed with ASD later in life feel anger of misdiagnoses and resentment towards being prescribed mind-altering medications (with many side effects) that they were never in need of. They have described countless let downs of various cocktails of psychotropics that had made them feel hope. These experiences can lead to an exacerbation of other mental health issues including anxiety and depression. Validation of these feelings, here and now techniques and cognitive reframing have proved useful in these cases.
An autism diagnosis impacts the whole family It is important to involve parents, caregivers and siblings in mental health treatment, as each person will respond in their own way Being in touch with teachers and treating physicians will also be helpful. As therapy progresses, it is imperative to keep all involved in the know.
When a child receives an ASD diagnosis, it can affirm their identity and allow family to understand and enlist necessary supports I have found it helpful to understand what those resources are, and they include speech/language pathologists, occupational therapists, behavior analysists, pediatricians and psychiatrists
Parents of children with autism often feel inadequate and unprepared prior to the diagnosis being given. They may be dealing with a gut feeling that something is off for months or even years before then. Oftentimes they struggle with the
emotions they are experiencing including guilt, anxiety, sadness, and frustration Parents may differ in their views of ASD, appropriate treatment for it, or even if they agree with the diagnosis at all.
It is critical that all these feelings within the family are validated. Sometimes just getting one to accept (though may not agree with) the other’s stance on the subject can be helpful in progression Psychoeducational information on autism should be included in sessions Bibliotherapy suggestions and links to valid informational websites can help empower family members to understand on their own terms There are multiple virtual and in-person support groups available for family members They can provide information, support, and connection to other’s experiencing similar life changes. Siblings have their own set of challenges. They may feel left out, lost or overwhelmed by the amount of time, attention and resources being given to the brother or sister receiving the diagnosis. They may struggle with feelings of shame surrounding their sibling and may shy away from social outings where their sibling is involved, “what if he has a meltdown in front of my friends?” Concerns over their role in their autistic sibling’s life after their parent’s death is also common Validations of these feelings and encouragement of open communication between family members is paramount. Family counseling sessions are highly encouraged.
Prioritizing mental health is imperative in supporting our individuals and families with ASD. There is a pressing need for increasing autism-aware mental health professionals and clinical supervisors By giving counselors the skills necessary, we can provide effective mental health care that respects neurodiversity and improves over all well-being for autistic individuals and their families With ongoing education and trainings, we can we can foster an inclusive mental health landscape where individuals with autism feel seen, heard, and supported on their journey towards well-being.
Written By: Jennifer L Smyth, LMHCJennifer Smyth is a licensed mental health counselor in Palm Beach County, FL She is currently employed at The Learning Academy at the Els Center of Excellence in Jupiter, FL where she has practiced for thirteen years She recently opened a private practice in Palm Beach Gardens, FL, Jennifer Smyth Counseling and Consulting Jennifer specializes in autism, anxiety, depression and trauma for individuals and families





The mental health community in Florida, and indeed beyond, mourns the loss of a visionary leader, Dr. Darlene Silvernail, the esteemed first Executive Director of The Florida Mental Health Counselors Association (FMHCA). Dr. Silvernail’s passing leaves an irreplaceable void in the hearts of those who knew her and the profession she dedicated a huge portion of her life to advancing
Dr. Silvernail was not just a leader; she was a trailblazer, a mentor, and a friend to many. Her journey with the Florida Mental Health Counselors Association began with a profound sense of purpose and a commitment to elevating the standards of mental health care in the state.
From the outset, she demonstrated an unwavering dedication to her role, setting the bar high for professionalism, integrity, and compassion.
Under Dr Silvernail’s guidance, the Florida Mental Health Counselors Association flourished, becoming a beacon of excellence and advocacy in the field of mental health which still can be seen today via a mentee and current FMHCA Executive Director, Diana Huambachano. Her leadership was characterized by a rare blend of strategic vision and genuine empathy and inclusiveness, inspiring others to strive for greatness and empowering them to make a meaningful difference in the lives of those they served.
Her closest colleagues describe her as a "Salt of the Earth" type of person with a great sense of humor combined with excellent professionalism. They also added, “She made me feel welcome”, “ She was a lead or move over type of person”, “She moved with vigor, haste, and purpose”, and “She carried a vibrant spirit and unwavering dedication ”
As we mourn the loss of Dr. Darlene Silvernail, let us also celebrate her remarkable life and the countless lives she touched along the way. It is often said that There are special people in our lives who never leave us, even after they are gone and in that spirit, we connected with 7 of Dr. Silvernail’s colleagues, mentees, and friends to capture what Dr. Silvernail has left.
What was your favorite thing about Dr. Silvernail?
What I loved most about Darlene was her spirit of adventure in going about all of her endeavors, whether it was traveling to far-off and exotic places or planning for the next FMHCA conference
I loved her ability to envision growth and encourage her students to step out of their comfort zone and experience different leadership roles within the community. Dr. Silvernail propelled her students to tap into their full potential.
Her genuine curiosity about the world and her relentless pursuit of new experiences
She is a paragon of professionalism, dedication, and yet showed deep kindness, that we all could, and should seek to emulate.
Where was Dr. Silvernail most “in her element”?
At the FMHCA Annual Conference watching it all come together!
When she was organizing, directing and empowering everyone around her. Darlene did not suffer obstacles well They were there simply to be surmounted
When she was traveling and immersing herself in new cultures that her spirit truly soared She had a gift for connecting with people from all walks of life
What was your funniest moment with Dr. Silvernail?
Planning the FMHCA conference and going through budget cuts when needed.
One day her chair broke as she tried to adjust her position and all she could do was laugh. It was a reminder that life is unpredictable, and sometimes, the best thing we can do is laugh in the face of adversity.
All dinners we shared at the end of each FMHCA Conference!
What legacy do you feel she has left?
The legacy to move our profession forward while being inclusive.

The high bar of standards that she set for all of us in our profession, in this organization, and in the kind of people that we should all strive to be – strong, but kind – determined, but flexible – and always seeking to grow – while remembering where we came from.
Her kindness and generosity.
Her legacy lives on in the hearts and minds of all those she touched. She left behind a legacy of growth and a reminder of the importance of embracing change.
Her legacy has set the bar for excellence in growing the FMHCA organization into the force it has attained and presents today.
Dr Silvernail’s legacy will live on in the hearts of those who knew her, and her impact on the mental health profession will be felt for generations to come
In honoring Dr. Silvernail’s memory, let us recommit ourselves to the principles of compassion, empathy, and inclusivity that she held so dear. Let us carry forward her legacy with grace and determination, knowing that the work we do today is a testament to the incredible woman she was and the profound impact she had on us all. Dr. Darlene Silvernail may be gone, but her spirit will live on in the countless lives she touched and the lasting legacy she leaves behind
Special thanks to: Laura Giraldo, LMHC, NCC, CCMHC, Dr. Kathie Erwin, Diana Huambachano, LMHC, Michael G. Holler, MA, NCC, CFMHE, CCCE, CCMHC, LMHC, Joe P. Skelly, LMHC, Louise Sutherland-Hoyt, M. Ed., CAGS, LCPC, NCC, CCMHC, ACS, and Frank Hannah, LMHC for their contribution to this article.



As professionals, many of us have heard we are a healer and helper to others. That we spread awareness, assist with skill building, and provide hope where there doesn’t seem to be any. As professionals, we’ve also heard about compassion fatigue. We’ve heard about high turnover, burnout, and the mental health provider shortage You may not have only heard of it; you may have experienced it directly The widely advertised remedy has long been discussing the need for systems change and the importance of practicing self-care This article's focus is related to self-care.
We are losing students who could grow to be good providers. We are losing registered interns who could greatly support our communities with an ever-growing need. We are losing licensed professionals, looking for other options outside of being active within the field There are quite a few articles and studies that discuss the reasons for this Some of these reasons are in the first paragraph of this article: burnout, turnover, and compassion fatigue
But why?
We are trained to ask this question In fact, this comes naturally to many of us Acknowledging an entirely different discussion needs to happen around building more supportive structures
(aka systems), a simplified response to why… self-care isn’t enough. Self-care isn’t enough for a profession that supports holding the line between suffering and well-being or optimal quality of life for those who receive our services. Furthermore, while self-care practices are necessary for everyone, I believe a specific discussion must occur for those of us whose well-being, or lack thereof, greatly impacts the lives of others First responders, emergency medical providers, nurses, and of course mental health professionals would be better supported by an explicit demonstration that our well-being is a clinical intervention. We all know what an intervention is. Simply put, it is an intentional action that is meant to result in some outcome. Clinician well-being requires intentional action. It supports greater energy, capacity, and competency. These then result in better client outcomes overall. There is such a large body of work to support this.
Clinician’s well-being as a clinical intervention would require the focus to be more on clinician wellness – think eight dimensions of wellness for example – rather than self-care activities This would also mean recognizing the best way to support our communities and the integrity of our profession is through personal development as well as professional
development We are already called to have continuing education toward our professional development What if personal well-being with space for reflection and integration were interwoven within trainings? My pie-in-the-sky dream for our profession would be to have the opportunity to accrue some continuing education credit for attending training, workshops, or groups that attend to our own well-being.
I believe this trend is starting and would only benefit from gaining more traction To view clinician well-being as a clinical intervention is to fully embody how the healing and wellness of one person directly impact the healing and wellness of another Even as systems may be slow to change, we have the ability through our energy and building our capacity to do even better work within these systems through this lens.
Currently, there are numerous conversations and some programming that support this trend. Here are two simple ways we can take steps to fortify supporting people to enter the field and supporting them to be well within a long and fulfilling career
Include time and content for the clinician's well-being in as many facilitations as possible This could be trainings, workshops, meetings, supervision sessions, and general gatherings
Create and support an in-person and/or online community about clinician well-being that fosters an environment that allows for responsibility and accountability in kind and compassionate ways.
In centering clinician’s well-being in the way we center professional development, we can live more connected lives and increase our capacity for the work we do. That is a clinical intervention if there ever was one.
Written By: Colette McLeod, LMHC, Qualified Supervisor, Certified Case Manager
Colette is the founder of Colette McLeod Counseling and Consulting Services (CMCCS) which provides therapy, supervision, coaching case management, and facilitation services She is also the co-creator and Clinical Director for Gifted Ones Mental Health Initiative (GO! MHi) which supports a holistic practice of personal well-being and professional development community for all mental health professionals She is an Advisory Council member for Gifted Ones, Inc a local 501©(3)

Kintsugi is an ancient Japanese art form that involves repairing broken pottery with gold. The word 'Kintsugi' means 'golden joinery' in Japanese. This art form originated in the 15th century when a Japanese shogun broke his favorite tea bowl and sent it to China for repair. When it was returned, it was held together with unattractive metal staples, so Japanese craftsmen developed a more aesthetically pleasing solution - they used gold to repair the cracks Kintsugi not only fixes the broken pottery but also highlights the cracks, making them a beautiful part of the object's history
In our daily lives, when things go wrong, we often give up and throw things away. However, the Kintsugi philosophy can help us to mindfully embrace the ups and downs of life. Whether you are a parent, caregiver, or professional working with children, embracing the Kintsugi philosophy can increase much-needed mindfulness practices, which can repair ruptures. Mindfulness is the necessary ingredient that is often missing in many challenging scenarios
Reflective practice is a buzzword in the field of Infant and Early Childhood Mental health. It involves pausing and observing one ' s interactions, reactions, and emotions as well as what is going on around us. Embracing the philosophy of Kintsugi as a parenting lifestyle would increase self-reflection and build awareness of the parallel process between parent and child. This would promote positive mental health outcomes for both parent and child and strengthen resiliency. The philosophy of Kintsugi as a parenting lifestyle is about learning to find beauty
amidst the chaos of parenting
Here are three ways to begin applying Kintsugi within your lifestyle:
1.
Embrace Imperfections in Parenthood: Parenthood is vulnerable to cracks and imperfections, like a delicate piece of pottery. The Kintsugi philosophy invites us to view these imperfections not as shortcomings but as integral parts of the unique journey we share with our children As we embrace the idea that every challenge, stumble, and imperfect moment contributes to the richness of our family story, we cultivate a mindset of acceptance and mindfulness
Reflection as the Golden Thread: By reflecting on our interactions, reactions, and emotions, we uncover the golden moments of resiliency and areas of growth as we raise thriving little minds. Reflective journals such as “Golden Connections: Parenting the Kintsugi Way” are examples of the available tools for applying the philosophy of Kintsugi within your parenting lifestyle.
3.
2. Track and Celebrate Every Milestone: Whether it is tracking your progress with how often you are reactive to mistakes or when the little one achieves a new step in their development, take a moment to track and celebrate every moment
Parenting can feel like a delicate and complex dance. However, just as the Japanese art Kintsugi encourages us to remember that even broken objects can be repaired to be beautiful again, through practices such as reflection and embracing imperfection, parents can mend the cracks in their journey, transforming each challenge into an opportunity for growth. Parenting the Kintsugi way invites parents, caregivers, and those who work with little ones to embark on a transformative journey of mindfulness, connection, and celebration.
Written By: Alicia-Ann Samuel, NCC, IMHLMHC-QS
Alicia-Ann Samuel is a visionary psychotherapist and owner of Therapeu Beautiful LLC With almost a decade of experience as a mental health professional, she offers her clients expert guidance and personalized mental health journeys AliciaAnn is also the chair of FAIMH Broward, a boy mom to “Irish Twins,” and a doctoral candidate affiliated with the FMHCA, BMHCA, and FAIMH Alicia-Ann empowers her clients to find beauty amidst life's chaos

Find new ways to indulge your body and mind with this trio of dice that adds some spice to your wellness practice. Three six-sided dice provide more than 200 unique and inspiring ways to indulge yourself.
Dice categories include treats for the body, treats for the mind, and ways to shake things up
A 32-page activity booklet provides suggestions for a range of budgets and time frames
Order yours here
Do your clients give to others at the expense of their own emotional, physical, and mental well-being? Written by licensed therapist and NYT bestselling author Nedra Glover Tawwab, The Boundaries Flip Chart is a must-have tool for any mental health clinician seeking to help their clients identify, set, and maintain healthy boundaries.
Order yours here.


Connect More is a brand new spin on a popular 4 in a row connect game. Connect More is a communication and social skills game that utilizes gameplay and over 300 questions for players to gain a deeper understanding of their friends, family, coworkers, classmates, and beyond!
Order yours here.
Don’t neglect those dried-out hands, chipped nails, and cracked knuckles give them three times the TLC they love. This trio of spa-quality treatments in different scents.
Every collection includes one set of 3 treatments in each scent: Green Tea Detox, Vitamin Recharge, and Lavender Relieve. Each treatment includes a sugar scrub, cream mask, massage butter, and nail file.
Order yours here


Sometimes school, kids, work, pets, and life in general can make us forget the little things, like that brown plant languishing on your windowsill (Oops!) Rest a little easier knowing your botanical babies won’t go thirsty with a joyful ceramic planter that keeps them hydrated for up to eight weeks Each two-piece ceramic planter set has a duo of cotton “feet” that draw in water from the “foot spa” to keep greenery happy (just look at that face), hydrated, and healthy.
Order yours here.
On average, adults typically take about 5,000 steps per day; with each step, your toes bear half your body weight. That translates to about 75% of Americans experiencing foot problems at some point. Let the hundreds of protruding nodes on this mat provide an at-home massage for sore and aching feet.
The mat focuses on acupressure points believed to alleviate foot pain
Features contoured, rounded nodes raised at the center said to stimulate your arch
The comfortable and versatile mat is useful while sitting or standing at a workstation.
Order yours here
This tote has room for snacks, suntan lotion, books, makeup, and more. What makes the Bogg Bag unique is its patented design, durability, and it's washable! Unlike other totes, the Bogg Bag won't tip over The bottom won't leak And at the end of the day you have BOTH style AND functionality!

Order yours here.

Lemme Chill DeStress Gummies use clinically-studied KSM-66 Ashwagandha and a botanical blend to help keep you calm, cool and connected to your highest self.
Order yours here.
Ingredients:
2 watermelon radishes trimmed and thinly sliced
Zest and juice of 1 lemon
¼ tsp. Morton kosher salt
2 Tbsp. extra-virgin olive oil
1 bunch asparagus, trimmed
1 tsp. freshly ground black pepper
¼ tsp. crushed red pepper flakes
8 Medjool dates, pitted, halved lengthwise
3 oz. fresh goat cheese
2 Tbsp. coarsely chopped mint
Preparation:

Toss radishes, lemon zest and juice, and ¼ tsp. Morton kosher salt in a small bowl; set aside. Heat 1 Tbsp. oil in a large nonstick skillet over medium-high. Working in batches if needed, cook asparagus in a single layer, undisturbed, until slightly charred underneath, about 2 minutes. Shake pan to turn asparagus and cook, shaking pan occasionally, until asparagus is crisp-tender and charred in spots, about 4 minutes Sprinkle with black pepper and red pepper flakes; season with salt Transfer asparagus to a platter
Wipe out skillet Heat remaining 1 Tbsp oil over medium Cook dates, stirring occasionally, until charred in spots and beginning to stick to pan
Scatter dates over asparagus, then crumble goat cheese over Top with mint and reserved radishes, then drizzle with oil and any liquid from radish bowl.
The purposeful act of making art can be more than a creative outlet. It can also help individuals gain self-awareness, process difficult thoughts, and even ease the effects of past traumas. Essential Art Therapy Exercises, a cognitive behavioral therapy workbook, offers a range of creative activities to help you better understand yourself, develop control over your emotions, and aid the healing process.
Order yours here.
Whether working or browsing online, you're most likely moments away from needing your smartphone Maintain full battery strength at an optimal distance (just an inch or two) from your computer with a mouse pad that doubles as a Qi-certified wireless charging station.
Order yours here.
These shower steamers are themed around positive intentions as reminders that a little self-care (and a steamy shower filled with soothing scents) can make your day. Choose from two different aromas: De-stress: Zesty, citrusy grapefruit blends with cooling, crisp mint.
Relax: Warm, musky patchouli mingles with bright, citrusy lime.
Order yours here.


Committee Chair: Laura Peddie-Bravo, LMHC, NCC
Greetings! While it may seem our committee has been quiet thus far in 2024, please know your Committee Co-Chairs and I have been hard at work on what to offer you in 2024 and at the 2025 FMHCA conference Firstly, we are going to try a different approach to our quarterly meetings This year, we are going to pre-set the meeting dates and times in hopes you will be able to mark all of 2024’s meetings on your calendar (as opposed to taking a survey of meeting times each quarter ) Our first meeting of 2024 will take place on Monday, March 25th at noon. We will continue to record the meetings and post them into our Committee Forum on the FMHCA website: (on the Home page, move your cursor over the “home” button and a drop-down menu will appear. The Committee page is four down from the top.) If you do this and find you do not have access to the page, please contact the FMHCA office at Office@FLMHCA.org to gain access. Our committee page has been very active this year with multiple important posts, so please make sure you have access to keep up to date on the very latest information Secondly, we welcome the return of FMHCA’s Student and Intern Summer Bash! What is the Summer Bash? It is a two-week span of time during July which is focused specifically for Graduate Students and Registered Mental Health Counselor Interns This year’s Summer Bash will take place during the last two weeks of July Everything you need for licensure will be offered during the Summer Bash! If you have questions about the Summer Bash, please feel free to contact the FMHCA office. Thirdly, and last but not least, we will have an in-person mixer at the annual FMHCA conference! Please mark your calendars now, we will be meeting at 6:30 pm on the first evening of the conference which will be Thursday, January 29th at 6:30 pm.
Government Relations Committee
Committee Chair: Aaron Norton, PhD, LMHC, LMFT
Renaming Registered Interns and Interns Needing a Licensed Professional " on the Premises" for Clinical Services (SB 210/HB 297)
HB 287 passed through all committees and was added to the House calendar for a second reading. SB 210, however, did not pass its first committee (the Senate Policy Committee). The GRC met with various legislators and legislative aides and talked to the Staff Director of the Committee. We could not identify any
particular concerns about the bill that could be blocking it, and it is has been suggested that its inaction on the Senate side is due to the large volume of bills the committee must consider and only having so much time to address them. Unfortunately, this bill was not passed this legislative session, but we remain optimistic that we will be able to do so in a future legislative session.
Currently, F.S. 916.115 reads, "To the extent possible, the appointed experts shall have completed forensic evaluator training approved by the department, and each shall be a psychiatrist, licensed psychologist, or physician." This requirement applies when the court is appointing experts "to determine the mental condition of a defendant in a criminal case, including competency to proceed, insanity, involuntary placement, and treatment " We believe this outdated statute (which we believe to have originally been written in 1980, 7 years before Florida started licensing counselors) needs to be updated to include the 491 Board professions, as (1) our scope of practice permits us to diagnose and treat mental disorders, (2) the majority of licensed mental health professionals in Florida are 491 board licensees, (3) there are shortages of forensic mental health experts in some judicial circuits in Florida, and (4) our unique training and expertise can be helpful in the court system.
We were unable to secure a bill sponsor for this issue this legislative session and will continue to prioritize this issue in future legislative sessions
Given that this legislative session has now come to a close, the GRC intends to work on other important issues that involve liaison work with government agencies, including:
Encouraging the Division of Vocational Rehabilitation (DVR), an agency under the Florida Dept of Education, to revise its policy manual, which only permits diagnoses offered by 491 board licensees to be used for eligibility for DVR services if the 491 Board licensee is under the supervision of a psychiatrist or psychologist.
Encouraging the Florida Dept. of Education to revise standards so that evaluations for disability-related accommodations can be accepted when conducted by 491
Advocating for the 491 Board to add a rule mirroring a rule published by the Board of Psychology clarifying that 491 board licensees should refrain from offering raw test materials to entities requesting medical records.
Addressing a request from the Florida Psychological Association for a unified approach to working with school districts on the prevention and mitigation of school shootings.
Committee Chair: Maria G. Giuliana, LMHC, Qualified Supervisor LMHC/LMFT, US Navy Veteran, FMHCA President-Elect
Attention all mental health professionals passionate about supporting our military personnel and their families! Whether you are already involved in this noble endeavor or are keen on dedicating your expertise to it, we warmly invite you to join our thriving community at the Florida Mental Health Counselors Association’s Military Committee
Our upcoming monthly gathering is designed to nurture a supportive environment for counselors committed to the welfare of our military community. These meetings are an excellent opportunity for professional development, knowledge exchange, and staying abreast of the latest advancements in military counseling.
Case Staffing and Peer Support: Engage in meaningful discussions on challenging cases, drawing on the collective wisdom and experiences of your peers.
Latest Developments: Keep updated with the most up-todate news, events, and training opportunities specific to military counseling.
Our Collective Goal: We strive to ensure every member is equipped with the highest level of competency, enabling the provision of unparalleled care to our heroes and their families
Professionals currently counseling military members (active, retired, or former) and their families. Those interested in specializing in military counseling.
Share your unique experiences, resources, and strategies. Connect with peers navigating similar challenges and achievements.
Enrich our collective knowledge base to better support our military heroes and their loved ones.
Mark Your Calendar! Join us on Apr 25, 2024, at 12:00 PM for our next meeting and become a vital part of our mission towards excellence in military mental health counseling Together, let's foster a culture of collaboration, learning, and growth, ensuring the military community receives the support and understanding they richly deserve.
Save the Dates & Spread the Word! Let’s amplify our impact through collective effort
May 30, 2024 12:00 PM
Jun 27, 2024 12:00 PM
Jul 25, 2024 12:00 PM
Aug 29, 2024 12:00 PM
Sep 26, 2024 12:00 PM
Oct 31, 2024 12:00 PM
We are looking for members interested in joining the Military Committee Contact the Chair at mariagiuliana13@gmail com
Joining a committee is a great way to participate in FMHCA and increase your presence in our community. We have several committees that we would love you to participate in! Below is a list of all our committees and their chairperson
Ethics Committee
Chair: Michael Holler
Bylaws Committee
Chair: Michael Holler
Chapter Relations Committee
Chair: Grace Marin
Registered Intern & Graduate Student Committee
Chair: Laura Peddie-Bravo
Government Relations Committee
Chair: Aaron Norton
Education, Training Standards & Continuing Education Committee
Chair: Aaron Norton
Military Committee
Chair: Maria Giuliana
Indigenous Mental Health Subcommittee
Chair: William Gouveia
We invite you to contribute your efforts as there are numerous opportunities for you to get involved and make a difference For more information on how to participate right away, please contact the chair committee or fill out this form


Recently I saw and ad from one of the large telehealth counseling companies promising a “cure” and that you will “get better in 12 weeks” This is an alarming, misleading, and dangerous claim from a call-center that employs unlicensed therapists.
When individuals are struggling with mental health issues, seeking counseling can feel overwhelming. Seeing marketing ads with the promise of feeling better, being “cured”, and finding peace in a few weeks can be incredibly alluring These ads are dangerously perpetuating the idea that there is a quick fix
As a therapist, you understand that mental health is a complex and multifaceted issue that cannot be magically cured overnight.
Mental health counseling is a valuable tool that can provide clients with coping strategies, help with self-awareness, and provide crucial emotional support through these processes Promising that mental health counseling will cure an individual sets unrealistic expectations that can ultimately lead to disappointment and frustration. It’s crucial for counselors to manage these expectations and help their clients understand that counseling is a process that takes time and effort- it is a journey, not a destination.
As a therapist, you know that mental health issues are often rooted in a combination of biological, psychological, and environmental factors Viewing counseling as a quick fix overlooks the intricate nature of mental health and undermines the importance of personalized, long-term treatment plans
Instead of focusing on a cure, mental health counseling should be seen as a tool for personal growth and self-improvement
Setting realistic goals and milestones with your clients can help individuals track their progress and stay motivated throughout the counseling journey.
It is irresponsible for any counselor or organization to make promises that there is a “cure” or time frame around when the “feeling better” should happen Therapists are taught through years of coursework and internships, that you are there to support, guide, and empower clients to make positive changes in their lives Although every day as therapists, we wish we could wave a magic wand and make all our client's problems vanish
If you want to provide the best, most balanced experience for your clients, they must have a health mindset. You can foster this by:
Educating your clients that they first have to embrace the process of growth, self-discovery, and healing. Setting expectation that it takes time, effort, and commitment to see progress
Assuring clients that setbacks are a natural part of the journey- a bad day does not equal a bad life
Talking about the fact that healing is not linear, and setting realistic milestones and goals.
By managing your client’s expectations, helping them to embrace the process, and understand the complexities of their mental health, you will set realistic expectations with your clients there they can truly benefit from the transformative power of mental health counseling
Written By: William Carmody, M.Ed., Ed.S., MBA, LMHC, NCC
William is the founder of Counseling Hope, a private practice with locations in Windermere, and Maitland Bill earned his Master’s Degree an Specialist Degree in Mental Health Counseling fr University of Florida He completed post-graduate training at Harvard Medical School and is a nationally certified counselor Bill enjoys helping new grads learn how to navigate the business side of working in a private practice


There is a legitimate shortfall in the mental health world There is a significant gap between civilian mental health providers and military veterans and their families seeking care This isn't just about a lack of understanding; it's about a failure to connect on the essential levels of military experience and the resulting traumas My mission is straightforward: to close this gap and ensure veterans and their families get the specialized, informed care they need. For mental health providers interested in supporting veterans, the first step is education. Learn about military culture, understand the common traumas, and recognize the significance of moral injury as a result of military service. This shouldn’t be optional, and it's vital in providing the kind of care that can truly make a difference. Instead of veterans being doubted or interviewed on the details of their experiences, they need to be understood and supported through them. This can be difficult without a lack of understanding of military culture
Serving in the military impacts individuals in unique and monumental ways, leading to unique psychological challenges such as moral injury, military sexual trauma, combat stress, and survivor's guilt. These aren't just abstract concepts; they're real, painful experiences that shape our lives as a veteran. When it
comes to getting help, too many veterans are met with providers who lack basic knowledge of military culture and the specific nature of military traumas From my personal experience, seeking therapy often felt like an exercise in frustration. Instead of focusing on healing, sessions got overhauled with me explaining military terminology and structures. It was clear that some therapists viewed me more as an educational project than a person in need of help. This isn't just disappointing; it's a failure of the care system.
Despite the new efforts by the military to reduce the stigma around mental health issues, changing deeply ingrained attitudes and long-lived institutional concepts is not a small or expedient task The truth is, we ' re fighting against decades of a culture that often views seeking help as a weakness. Changing this culture is essential, but it's going to take time and a lot of work. Closing the gap between civilian mental health care and veterans is about more than just improving therapy outcomes; it's about respect, understanding, and acknowledging the sacrifices made by those who have served and how traumas and struggles are different in a military environment. By truly understanding the veteran experience, you can begin to provide the level of care that's not just deserved but urgently needed.
That is why we built a training workshop:
“Unseen Warfare: Bridging Emotional Frontlines with Holistic Care for Veterans and Their Loved Ones” is an upcoming 2-day workshop dedicated to equipping mental health professionals with the knowledge and tools needed to provide effective, empathetic care to veterans and their families.
Location: Online (Via Zoom)
Credits: 16 General CEUs - CE Broker Tracking # 20-1155178
Date & Time: May 2nd and 3rd 2024 (8 AM - 5 PM Each Day)
Presented By: Maria Giuliana, LMHC, and Theresa Gathers, ICF-ACC, CDTLF
We hope to see you there!
Written By: Theresa J Gathers, ICF-ACC,
CDTLFTheresa, a retired military veteran, is the founder of Athena UNCHAINED Coaching & Consulting LLC. She is certified by Brené Brown as a Dare to Lead™ facilitator and is an ICF-ACC Coach. Her involvement with mental health extends from Psychodrama training and co-leading FMHCA events, to major military policy change, furthering counseling skills and emotional support for service members. Her dedication to mental health care is showcased as a leading advocate and transformative leader.


Imagine going to school and getting your 4-year degree with the “American dream” of a white picket fence, a dog, and your adoring family living comfortably in an affordable single family home high in your mind. However, once you leave school and start working, you realize that it costs your entire paycheck to make 1 month’s rent and the cost of groceries has risen so high that you frequently have to decide between paying your light bill on time and buying enough groceries for the week. Now imagine that continuing to happen for years on end, despite several slight pay increases, getting married and becoming a dual income household, and working constantly to keep up with the day-to-day living expenses. This is the story for many middle-income families residing in the sunshine state of Florida and across the county
As a practitioner working within the communities of middleincome families, I have found that many of the clients, despite working diligently, are struggling to keep up with the rising cost of standard living expenditures like gas, rent, and electricity. "Economic hardship reigns in the United States, with many households living paycheck-to-paycheck at best," according to Grand Challenge 12 (Barth, Gehlert, Joe, et al., 2019). "Living paycheck to paycheck" is a term used to imply having little to no extra or uncalculated expenditures or emergency funds (Thamm,2020) Because of the inability to accumulate emergency savings while living "paycheck to paycheck," an unexpected loss of income inside the home has the potential to result in drastically bad life-altering conditions
Some of these concerns include (but are not limited to) the inability to keep enough healthy food in the house, an increased risk of mental and physical health instability, and housing
insecurity Furthermore, due to a lack of support resources available to assist with specific financial requirements, many families struggle to recover from such losses, even if the loss is only temporary.
Therapy can be one of the most intimate professional relationships within the healthcare industry. Meeting clients where they are with resources is going to play a key role in supporting families where their needs are.
Collaboration
As we all know in the mental health world (and other fields alike) there is power in working together. Sometimes, it’s not always what you know, it’s who you know. Making intentional connections with your community resources provides opportunities to learn about what all a community has to offer to those who have fallen on hard times Empowerment can be one of the greatest tools in our toolboxes Be intentional in reaching out to social service agencies in your community to stay up to date on what is going on so that as your clients are expressing concerns, we can empower them with resources that make sense for their lives. These types of collaborations also benefit your practice, by promoting visibility of your services and your opening work working with other agencies to support clients well.
Connection
Forming partnerships with other practitioners in your area fosters conversations about client care and how to best serve a client who is struggling with these difficulties. It also opens
opportunities to be able to work together to create resources that make sense for the reported needs of your clients Additionally, this opens conversations about learning about which practices may offer sliding scales to patients in need or case management resources that fill gaps where your clients may need assistance.
As previously said, one of the most significant challenges I have faced in this line of business is the lack of support options for middle-income clientele. Working together to develop the tools needed to change our community in this way has the potential to impact not just the lives of the clients but also our own practices. Although we may not have all of the resources within our own toolbelts, someone will have something that can help. Working with community partners and other providers is a key move towards empowering the families we serve. Our work as practitioners is valuable, and our clients are better when we work together to meet their needs well, one conversation at a time
Barth, R.P., Gehlert, S., Joe, S., Lewis, Jr. C. E., McClain, A., Shanks, T.R., Sherraden, M., Uehara, E., Walters, K.L. (2019). Grand Challenges for social work: Vision, mission, domain, guiding principles, & guideposts to action. Grand Challenges for Social Work.
https://grandchallengesforsocialwork.org/wpcontent/uploads/2019/09/GCSWPrinciples-2-5-19.pdf
Thamm , S. z. (2020, December 28). Some Florida statistics on wealth, middle class and census responses. Fernandina Observer. Retrieved July 7, 2022, from https://fernandinaobserver.com/2020/12/28/some-florida-statistics-onwealthmiddle- class-and-census-responses/
Written By: Kiana Gadson, LCSKiana has been practicing in t Work for the past 12 years and completing her Doctorate of S concentration in leadership, a is the founder of Healing Care Christian mental health pract throughout the state of Florid



As an expressive arts therapist there are many times when clients look up at me trying to find words to explain their processing and end with, “you know what I mean?” My answer is almost always, “I do.” Even after all these years, I’m always amazed at how expressive arts seems to find its way into the cracks within, creating a space for processing and change. One morning recently it was through music that I was reminded of the power of expressive arts in my own experience. I was sinking into a little more “me time” before getting ready for work, enjoying the last few sips of my coffee, when I opened Instagram to find a recent post by Mel Robbins. Her adult daughter had just released her first single and the Instagram video showed Mel listening to it and celebrating with her staff I watched it about 3 times feeling the excitement with her, listening to the song and now crying I had no idea why, maybe it was because I also have adult children and felt her celebration? Maybe it was about watching her with her staff and feeling the sometimes isolating feelings of running a one person private practice? I wasn’t sure. All I was sure about was that once feelings show up, I allow them to find their way through. Taking the last sips of my coffee, and downloading the song on Spotify, I went upstairs to get ready for work. I cried through my shower, cried through getting dressed and then
cried my way to Starbucks with the song on repeat It wasn’t until I was in the space between ordering my drink and picking up that I realized where the crying was coming from The song was written by a 20 something artist singing about a relationship, or really about being a “past time” in a relationship and it was like my own 20 something self yelled, “Me too!” The tears came flowing from my own 20 something year old self. The part of me who fell in love in high school went to college and not even a week after college graduation got married. The marriage ended ten years ago, almost to the day, and in these 10 years there’s been so much growth, healing, remembering my true self and creating a life that was all mine. Divorce was the best thing that happened, but in the years of survival after my divorce, financial rebuild, needing my private practice to work, showing everyone on the outside that I was “fine,” walking around in some sort of emotional armor, this song allowed space for my 20 something me to let me know how she felt All this time when I was “looking at the bright side” I hadn’t given myself, or at least this part of myself, enough space to feel heartbroken. I was so busy being strong and brave that there was no room to feel defeated, used, stupid and like the rug was pulled out from under me. When I first heard the song, I was really just watching the Instagram post not even really paying attention to the lyrics, but my subconscious was. My 20 year old me was listening to Kendall’s lyrics and I finally felt what she had been feeling this whole time “I was a past time wasn’t I, and it’s about damn time that I knew.” So many times I forget about my precious younger selves and at almost 55, I realize they are my greatest teachers about myself. Healing is not just about the me now, It’s about hearing the stories of what I have experienced through the parts of me who lived them This time I allowed myself to cry and feel and within the hour I was sipping my Starbucks drink in my office I was surrounded by sand trays, clay, paints, client’s art, collage materials, music and drums with a little more love for myself, for the young woman I was, for the child I was, and feeling so much awe at how expressive arts can invite those unprocessed experiences to a space of healing in the exact way I needed.
Written By: Marie Celeste, MS, LMFTIn using expressive art modalities such as s tray, psychodrama and art, combined with Internal family systems methods, Marie sup her clients in reawakening the deeper true with feelings of truth or purpose, releasing aligns with their somatic experiences, and redefining relationships with both self and others



Within five minutes of our session, she burst into tears, overwhelmed by emotion. This time, it wasn't just disappointment in herself for self-harming; instead, she seemed to have lost all hope. She expressed feeling profoundly lonely and misunderstood, confessing, “I feel terrible because I should be grateful to my mother for her support. But instead, I'm angry with her I know she means well, but she just doesn’t get me ”
As our session progressed, I discovered that my 15-year-old patient’s mother had been actively "affirming" her daughter, who was struggling with mood dysregulation and self-harm
To my client, her mother’s words of encouragement felt invalidating and painful. More than that, they triggered a deep sense of guilt over the resentment she harbored towards her mom. “How can I be so angry and disappointed when she keeps telling me I’m strong, resilient, and capable? I feel like a mess, beyond ‘repair.’”
In my office, I hear adolescents repeatedly express feeling unheard and unseen. Simultaneously, parents admit to feeling helpless despite their relentless efforts to support their children. They offer help and reassurance, yet their messages often fail to penetrate the emotional turmoil their children are experiencing.
While I typically focus on teaching clients effective communication skills in cases like this, today I want to emphasize something different: validation All my 15-year-old patient needed that morning was for her mother to acknowledge her feelings without judgment In fact, hearing how strong and capable she was only served to invalidate her experience further.
Over time, I’ve observed that when clients feel invalidated, they

affirmation. It's simply about genuinely acknowledging and accepting a person’s thoughts, feelings, and experiences as valid, even when you don’t agree with them. Recent studies suggest that chronic invalidation may contribute to emotional dysregulation in teenagers
In cases like this, I've found Dialectical Behavior Therapy (DBT) to be particularly effective. I equip my clients with practical skills to navigate emotional challenges. Moreover, involving parents in this process is crucial for them to learn and apply these skills at home. To parents, I empathize with the complexity of supporting your child. I know it requires every ounce of your being to find the right words and offer reassurance. But sometimes, all they need to hear is that you understand how they feel
Written By: Monik Mossini, M.S. Registered Mental Health Counseling InternMonik is a psychotherapist specializing in mood disorders, working with teenagers and adults
DBT trained and pursuing certification, Monik ha DBT skills training program for parents of teenag with emotional dysregulation Also a Certified Yo Health Specialist, Monik brings expertise from va including PHP, IOP, and outpatient care With a passion for empowering individuals and families, Monik is dedicated to fostering emotional well-being and resilience


FMHCA Member Questions Answered by President and Managing Partner of The Health Law Firm, George F. Indest, J.D., M.P.A., LL.M.
Mr. Indest is board certified by The Florida Bar in the legal specialty of health law. He is the President and Managing Partner of The Health Law Firm, based in Orlando, Florida. The information provided in this article is for educational and informational purposes only and does not constitute the provision of legal advice.
AQI am a mental health counselor with my own private practice How extensive must my records be on my own clients?
Generally, your health records on a client should be as comprehensive as might be necessary for another psychotherapist later treating the same client to understand exactly what treatment you provided and why
you were providing it If an insurer or third party is paying the bill, then it should be comprehensive enough to document that the services billed for were actually necessary and were provided
However, that being said, you also need to consider the minimum that your state's laws and administrative rules may require, as well as those which may be required by any health insurer you bill (especially if it is Medicare, Medicaid or Tricare) or any other contract that you have may require If you are employed by or contracted with a larger group, then that group's policies and procedures need to be followed as well
For example, the administrative rule enacted by the Florida board which governs mental health counselors and social workers, Rule 64B4-9 002(2), Florida Administrative Code, requires the following:
1. Dates of therapy sessions (but also include notes, as well),
Basic information about the client including name, address and telephone number (in other words, basic patient demographics),
2. Treatment plan and results achieved,
3. Diagnosis if applicable,
4. Financial transactions between therapist and client including fees assessed and collected,
5 Notes or documentation of the client’s consent to all aspects of treatment (a written informed consent form is the best practice here),
6. Copies of all client authorizations for release of information,
7. Legal forms pertaining to the client (specifically any applicable court orders), and
9.
8. Documentation of any contact the therapist has with other professionals regarding the client
The words in parentheses are my words, not the rule's.
The American Counseling Association's Code of Ethics, in Section A, provides some additional details that you will find useful, especially in relation to client consent You should review these
It is highly advisable to have preprinted forms, many of which can be obtained from your professional association, and a checklist similar to the above that you can use whenever you are opening a record on a new client




Self-care has become a buzzword in recent years, highlighting the importance of looking after our physical, emotional, and mental health. It's more than just spa days - it is a vital practice for therapists and mental health professionals to sustain a fulfilling career.
Self-care is defined as "the ability to care for oneself through awareness, self-control, and self-reliance in order to achieve, maintain, or promote optimal health and well-being" (Martinez et al., 2021). This can include a wide range of activities such as getting enough sleep, eating a balanced diet, staying physically active, setting boundaries, and managing stress levels.
Therapists and mental health professionals experience high levels of burnout and compassion fatigue, leading to an increased risk of physical and emotional exhaustion These factors can negatively impact the quality of care provided to clients and ultimately hinder a therapist's ability to do their job effectively (Shapiro et al., 2007).
However, those who practice self-care are better able to manage stress, maintain a healthy work-life balance, and prevent burnout In fact, research has shown that self care can lead to higher levels of job satisfaction and improved overall well-being (Monroe et al , 2021)
Moreover, self care for therapists can also benefit clients. When you prioritize your own self-care, you are better able to provide high-quality care to your clients. This can include being fully
present during therapy sessions, having more energy and enthusiasm, and avoiding burnout that may lead to excessive absences or early retirement.
By incorporating self-care practice into your daily routine, you can better care for yourself and, in turn, provide the best possible care for your clients. However, self-care is not a onesize-fits-all solution and may look different for each individual. Experimenting with various self-care practices to find what works best for you and your unique needs is important.
Self care is often associated with indulgent activities like taking a bubble bath or getting a massage. While these can be beneficial, self care encompasses much more than just pampering oneself. It is an intentional act of caring for one ' s physical, emotional, and mental well-being
Research emphasizes the critical significance of implementing self-care practices among therapists to effectively manage stress, prevent burnout, improve client outcomes, and establish and maintain healthy professional boundaries (Posluns & Gall, 2019; Baker & Gabriel, 2021).
The demanding nature of therapy sessions can cause you to overlook your own well-being, leading to heightened stress, fatigue, and compassion fatigue. Prioritizing self-care enables you to better navigate these challenges and deliver top-notch
care to clients
Moreover, you can act as a role model by showcasing the value of self-care to clients, setting positive examples for maintaining healthy boundaries, and managing stress. Self care activities can also help you recharge and rejuvenate, leading to increased job satisfaction and improved overall mental health.
Additionally, self-care can improve your ability to empathize with clients and better understand their experiences, as you have a deeper understanding of the importance of maintaining good mental health.
Furthermore, self-care can help you identify and address any personal triggers or vulnerabilities that may arise during therapy sessions, leading to improved self-awareness and personal growth
Implementing self-care practices can also serve as a form of preventive care, reducing the risk of experiencing burnout or compassion fatigue in the long run. By prioritizing your own well-being, you are setting yourself up for a sustainable and fulfilling career as a therapist.
As mentioned, therapists and mental health professionals often face elevated levels of burnout and compassion fatigue, heightening the likelihood of both physical and emotional exhaustion.
Your lack of self-care can lead to feelings of resentment, negativity, and cynicism towards work and life in general It can cause you to feel overwhelmed, unmotivated, and disconnected from your work. These negative emotions can then lead to a downward spiral of decreased productivity, increased absenteeism, and, ultimately burnout.
Furthermore, burnout and compassion fatigue can also have a negative impact on the therapeutic relationship with clients, potentially hindering their progress and overall satisfaction with therapy
In contrast, engaging in self-care practices can help you manage stress levels, increase resilience, and maintain a healthy worklife balance. Self-care also allows you to take breaks when needed, set boundaries for yourself, and prioritize your wellbeing. By doing so, you can prevent burnout and emotional exhaustion, leading to a happier and more fulfilling life, both personally and professionally.
Burnout can manifest in various ways and may differ from person to person. While it is important to note that experiencing occasional feelings of stress or exhaustion is
normal, consistently feeling overwhelmed, exhausted, and emotionally drained could be a sign of burnout
Here are some common signs of burnout to watch out for:
Physical symptoms: Burnout can cause physical symptoms such as headaches, stomach aches, and loss of appetite These can be a result of chronic stress and exhaustion
Emotional detachment: Burnout can lead to individuals feeling emotionally disconnected from their work and those around them. They may become detached, cynical, or apathetic towards their responsibilities.
Decreased performance: Burnout can decrease productivity and motivation, leading to poor work performance.
Increased irritability: Burnout can cause individuals to become more irritable and easily frustrated, leading to strained relationships with colleagues and loved ones.
Isolation: Those experiencing burnout may withdraw from social interactions and isolate themselves from others, further worsening feelings of disconnection.
Lack of self-care: Burnout can lead to a neglect of one ' s physical and emotional needs, as individuals prioritize work over their well-being
Mental health issues: If left unaddressed, burnout can lead to more serious mental health issues such as depression and anxiety
Studies also found that burnout can have a negative impact on physical health, increasing the risk of chronic conditions such as heart disease and depression (Salvagioni et al , 2017; Precker, 2022) It is important to recognize these signs and take steps to address burnout before it becomes a more serious issue
You can practice self-care to prevent burnout and prioritize your well-being in many ways. Here are 10 self-care activities you can incorporate into your daily routine:
Set boundaries: Learning to say no and setting clear boundaries with clients, colleagues, and in your personal life is crucial for maintaining a healthy work-life balance. By clearly defining your limits, you can prevent burnout and prioritize your well-being effectively.
Take breaks: Prioritize breaks throughout your day to allow yourself time to rest, rejuvenate, and refocus. Whether it's a short walk outside, a moment of deep breathing, or simply stepping away from your desk, these breaks can enhance your productivity and overall wellbeing.
Practice mindfulness: Integrating mindfulness practices like deep breathing exercises or meditation into your daily routine can significantly impact your stress management and overall mental well-being. By cultivating mindfulness, you can enhance your ability to stay present, reduce anxiety, and improve your overall resilience.
Get enough sleep: Sleeping 7-9 hours of quality sleep is vital for optimal performance and cognitive function. Quality rest ensures that you wake up refreshed, energized, and ready to tackle the day ahead, enhancing your productivity and overall health.
Physical activity: Regular exercise boosts physical health, significantly reduces stress, enhances mood, and boosts energy levels Physical activity is a key component of a balanced and healthy lifestyle, whether it's a brisk walk, yoga session, or strength training
Engage in hobbies: Setting aside time for activities that bring you joy and relaxation, such as reading, painting, or cooking, can help you unwind and recharge Engaging in hobbies provides a creative outlet, reduces stress, and allows you to focus on activities that bring you fulfillment outside of work.
Connect with loved ones: Cultivating meaningful connections with friends and family is essential for emotional well-being. Taking time to nurture these relationships provides a sense of support, belonging, and happiness, contributing to your overall mental health and resilience.
Take care of your physical health: Maintaining a balanced diet, staying hydrated, and attending regular check-ups are fundamental aspects of caring for your physical well-being You can support your body's vitality and longevity by prioritizing your health through nutritious choices and regular medical assessments
Seek support: If you ' re feeling overwhelmed, don't hesitate to seek support from colleagues, mentors, or a therapist Sharing your concerns and seeking guidance can help you navigate challenges, gain perspective, and develop effective coping strategies to manage stress and maintain wellbeing.
Unplug and disconnect: Establishing boundaries with technology and carving out time away from screens are essential for mental rejuvenation and digital detox. By disconnecting, you can create space for relaxation, reflection, and genuine connection with yourself and those around you.
Self-care is not selfish or indulgent - it is essential for maintaining your mental, emotional, and physical well-being.
By prioritizing self-care, you can cultivate a healthier, happier, and more fulfilled life Listen to your needs, set boundaries, and make time for yourself Your well-being is important and deserves attention and care.
With so many self care for therapists activities available, it can be overwhelming to figure out which ones will work best for you. Here are a few steps to help identify the best self care options for you:
Identify your needs: Take a moment to pause and deeply reflect on your present state of well-being. Consider exploring areas that might benefit from enhancement, whether it's related to your physical health, mental wellbeing, emotional balance, or spiritual fulfillment
Consider your interests: Think about activities that you already enjoy or have been meaning to try out Self care should be enjoyable and fulfilling, so choosing activities that align with your interests can make it more effective. Try different activities: Don't be afraid to try out different self care activities to see what works best for you. This could include exercise, meditation, journaling, or spending time in nature. Keep track of how each activity makes you feel and which ones bring the most benefits.
Listen to your body: Pay close attention to how your body responds to various activities. If you notice that a particular activity is causing you excessive stress or discomfort, it might not be the most suitable option for you. Instead, opt for activities that help you relax and leave you feeling rejuvenated and refreshed
Evaluate your availability: As a therapist, you may have a busy schedule and limited free time Consider the amount of time and energy you can realistically dedicate to self care activities Prioritizing your own well-being is not just beneficial for you but also enhances the quality of care you provide to your clients.
Seek professional guidance: If you ' re still struggling to identify the best self care activities for you, consider seeking guidance from a therapist or counselor. They can provide personalized recommendations based on your individual needs and preferences.
It's easy to overlook your own needs when you are busy caring for others, but self care is crucial for maintaining your own wellbeing. It's important to acknowledge that self care looks different for everyone and there is no one-size-fits-all approach. What works for someone else may not work for you, so take the time to determine what activities benefit you most. Self care
shouldalsobearegularpracticeratherthanatemporaryfix Justlikeeatingwellorexercising,itrequiresconsistencyin ordertoseelong-termbenefits.
Takingcareofyourselfallowsyoutobethebestversionof yourselfforothersandcanimproveyouroverallwell-being.
Prioritizingselfcarecanalsosetagoodexampleforthose aroundyou,whetherit'sfamily,friends,orcolleagues.
Don'tbeafraidtotrynewactivities,seekguidance,andmake selfcareapriorityinyourdailyroutine.Maketimeforyourself andyourwell-being–youdeserveit!Incorporateregularselfcareactivitiesandbeopentochangeifsomethingisn'tworking foryou Takingcareofyourselfleadstoahappieryou
Baker,C.,&Gabriel,L.(2021).Exploringhowtherapistsengageinself-careintimesofpersonal distress.BritishJournalofGuidance&Counselling,49(3),435–444. https://doi.org/10.1080/03069885.2021.1885010
Martinez,N.,Connelly,C.,Perez,A.,&Calero,P.(2021).Self-care:Aconceptanalysis.International JournalofNursingSciences,8(4),418–425.https://doi.org/10.1016/j.ijnss.2021.08.007
Monroe,C.,Loresto,F.,Horton-Deutsch,S.,Kleiner,C.,Eron,K.,Varney,R.,&Grimm,S.(2021).The valueofintentionalself-carepractices:Theeffectsofmindfulnessonimprovingjobsatisfaction, teamwork,andworkplaceenvironments.ArchivesofPsychiatricNursing,35(2),189–194. https://doi.org/10.1016/j.apnu.2020.10.003
Posluns,K.,&Gall,T.L.(2019).Dearmentalhealthpractitioners,takecareofyourselves:Aliterature reviewonself-care.InternationalJournalfortheAdvancementofCounselling,42(1),1–20. https://doi.org/10.1007/s10447-019-09382-w
Precker,M.(2022,October12).Howjobburnoutcanhurtyourhealth–andwhattodoaboutit. Www.heart.org.https://www.heart.org/en/news/2022/10/12/how-job-burnout-can-hurt-yourhealth-and-what-to-do-about-it
Salvagioni,D.A.J.,Melanda,F.N.,Mesas,A.E.,González,A.D.,Gabani,F.L.,&Andrade,S.M.de. (2017).Physical,psychologicalandoccupationalconsequencesofjobburnout:Asystematicreview ofprospectivestudies.PLOSONE,12(10),e0185781.https://doi.org/10.1371/journal.pone.0185781
Shapiro,S.L.,Brown,K.W.,&Biegel,G.M.(2007).Teachingself-caretocaregivers:Effectsof mindfulness-basedstressreductiononthementalhealthoftherapistsintraining.Trainingand EducationinProfessionalPsychology,1(2),105–115.https://doi.org/10.1037/1931-3918.1.2.105
Written By: Jamie Frew
Jamie Frew, co-founder and CEO of Carepatron, is transforming healthcare by combining technology with patient care Focused on breaking down obstacles that prevent healthcare professionals from delivering exceptional care, Carepatron enables providers to prioritize patient care by investing in advanced technology Jamie enables healthcare professionals to dedicate their attention to providing excellent patient care and strongly advocates for ensuring healthcare is available worldwide

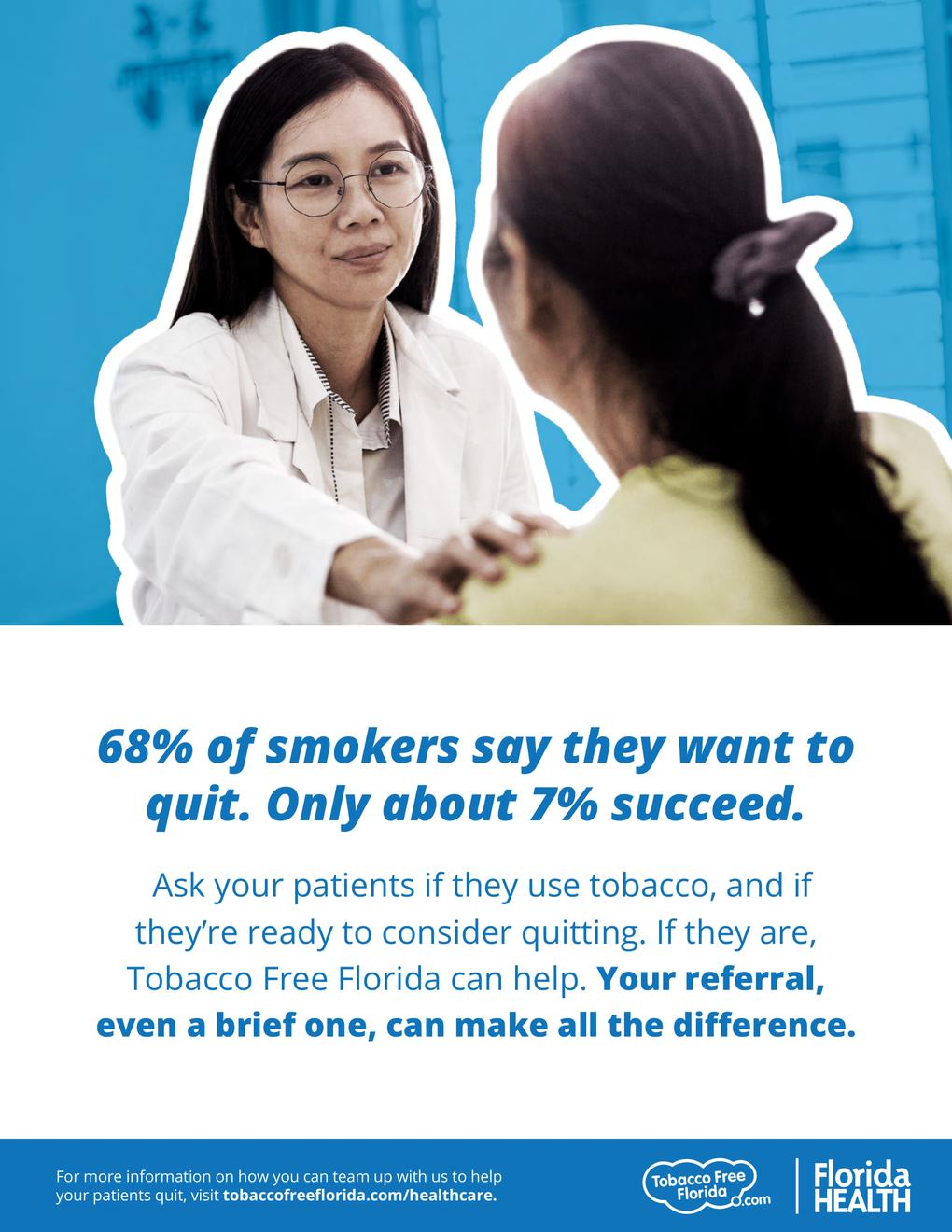

The Florida Legislative Session concluded at 2:35 PM on March 8, 2024 after 60 days of vetting and debate. The legislature filed 1,925 bills, but only 325 passed and will be considered by Governor Ron DeSantis for veto or approval
Several bills passed that will have an impact on FMHCA’s members and one FMHCA priority will have to be considered again next year.
Lines 759-889 Includes loan reimbursement under the Florida Reimbursement Assistance for Medical Education (FRAME) program, formerly the “Reimbursement and Loan Repayment Program,” of up to $75,000 for mental health counselors working in underserved areas for four consecutive years.
Line 2155 – 2305 -- Creates the Training, Education, and Clinicals in Health (TEACH) Funding Program The program enables qualified facilities, such as federally qualified health centers and community mental health centers, to apply for state dollars to offset the administrative costs and loss of revenue associated with establishing, maintaining, or expanding clinical training programs for mental health counselors. For behavioral health providers, the funds available to the qualifying facility total $15 per student, per hour.
The bill which reclassifies intern registrations as associate licenses for clinical social work, marriage and family therapy, and mental health counseling and eliminates the requirement for a licensed mental health professional's presence during clinical services by associate licensees in private practices will require more time for passage. Although the House of Representatives moved quickly to pass the bill through the necessary committees, the bill became bottlenecked and garnered opposition in the Senate
FMHCA, and the respective MFT and CSW organizations remain committed to lobbying these topics over the coming months and course-correcting any opposition. It is common for a bill to fail in its first year or two of filing, so we are hopeful these efforts will pay off.
HB 7021, Relating to Mental Health and Substance Abuse (Baker Act) This bill is long, so we recommending reviewing the staff analysis
Now that the 2024 Florida Legislative Session has concluded, FMHCA is focused on next year’s legislative efforts. The Government Relations Committee is already meeting regarding next steps. We will have a targeted and direct ask for FMHCA’s members to establish relationships with their respective state senator and state representative Those directives are forthcoming
Written By: Corinne Mixon, DPLCorinne is a registered professional lobbyist with sixteen years of experience representing clients’ state governmental interests
At Rutledge Ecenia, Corinne represents a broad client base with a particular emphasis on health care practitioners, education and regulated industries and professions She has been instrumental in passing myriad legislation and killing bills which would have negatively impacted her clients

FMHCA'sgoalistoprovideeducation, legislativeoversight,andnetworking opportunities.OurAnnualConference& VirtualSummitprovidesanopportunityfor advancedprofessionaltraining.
Takeadvantageofthisopportunityand presentattheFMHCA2025AnnualConference and/or2025VirtualSummit!
PresenterProposalsDueBy: August1st2023
Submitaproposaltobeapresenterat: www.FMHCA.org
BenefitsofPresenting:
Presenterswillreceiveadiscountonconference registration.
Promotionofyournameandcredentialsonour websiteandinallelectronicandprintmarketing materials,whereappropriate.
RecognitionofyourexpertisebyFMHCAandby otherindustryprofessionals.
Networkingopportunities
PresenterEligibility: Tobeconsidered,presentersmusthave professionalqualificationsingoodstandingwith theirprofessionalregulatoryboard,ifapplicable, possessthetechnicalexpertisenecessaryto presentonasubjecteffectively,andmeetoneor moreofthefollowing:
Havereceivedspecializedgraduateorpostgraduateleveltraininginthesubjectof presentation;and/or Haveextensiveexperienceincludingatleast fiveyearsofpracticalapplicationofresearch involvingsubjectofpresentation.