












Happy New Year! The past two years has been an unprecedented time for all of us. We are still facing uncertainty. This includes health and mental health issues, economic struggles, political concerns and nursing care delivery issues that continue. Throughout this time, a constant has been the caring support of the Florida Nurses Association staff and members. Our staff have been front-line in support to anyone that contacted FNA. We thank all of them!
Despite the pandemic our membership continues to grow. We are continually working toward successful future ventures for the nurses in Florida.
My theme this year is: Regain, Retain and Reconnect . Resetting reminds me of a remote control device. You can hit pause, rewind and then record again. Nurses hit the pause button on many things in the past two years out of necessity. I see this year as time to regain our footing so that we can rewind and hit the record button again. We have learned so much throughout the past two years and we are charged with the goal of becoming better. Nursing has realized that we may not have been as prepared as we should have been to manage a major pandemic. For many nurses this type of health crisis has not happened in our lifetime. We learned that our public health colleagues know a lot about emergencies and managing large scale health challenges. In 2022, we will work with our colleagues to be better prepared for this ongoing pandemic and the next ones to come.
We need to retain nurses in the nursing profession. Far too many nurses are leaving the profession for several reasons. Fear, pay, stress and
burnout are just a few. Florida Hospital Association (2021) reports a twenty-five percent turnover rate (one in four registered nurses) in Florida. The workplace demands have caused burnout, anxiety and departure of nurses from the nursing workforce. The essence of the nursing role has not changed but the environments in which the nurse carries out his or her duties has changed. There has been an increase in workplace violence against nurses. As reported by Androus (2021), “Nurses leaving the profession within the first five years of their career is a significant symptom of the larger challenges in nursing. With alarming rates of up to 33% of new nurses leaving the workforce within the first two years, the (not so) great escape must be addressed overall by the profession.”
Most importantly, we need to reconnect. This can be with our home or work families, with students on campus, our stakeholder groups, our staff or whomever you need to reconnect to in life. Resign to be better, softer, gentler, kinder and to reconnect.
For the upcoming year, I ask that we take a dynamic approach to focusing on what makes nursing so exceptional. Our strategic plan has six pillars... Nurse Advocacy, Member Services, Nurse Development & Support, Public and Professional Awareness, Professional Unity, and Organizational Excellence. Our mission is to advance the profession of nursing and promote a healthy Florida. For 2022, we will continue our focus on diversity, equity, inclusivity, and accessibility to the nurses of Florida. We need to keep our finger on the pulse to support our nursing members today and those to come. Let’s do what we do best –problem solve and fix it!
Androus, A., (2021). The (not so) great escape: Why new nurses are leaving the profession. Registered Nursing. Org. Retrieved from https://www.registerednursing.org/ articles/why-new-nurses-leaving-profession/
Willa Fuller, BSN, RN
Executive Director, Florida Nurses AssociationBlack History Month (also called African-American History Month) originated in 1915, when Carter G. Woodson, the “Father of Black History” conceived the Association for the Study of Negro Life and History. This resulted in the first “Negro History Week” on February 7 in 1926. The purpose of the celebration was to raise awareness and to bring attention to the importance of Black history.
 Willa Fuller
Willa Fuller
Eventually, in 1976, Albert Broussard expanded it into a month-long celebration and it was renamed Black History Month (BHM). In the same year, which coincided with the celebration of the Bicentennial in America, President Gerald R. Ford urged Americans to “seize the opportunity to honor the too-often neglected accomplishments of Black Americans in every area of endeavor throughout our history.”
In my personal experience, growing up in Florida, in the segregated South it was not customary to see images of dark-skinned people in places of importance or positions of power. From television to movies, and the print media, blacks would have to seek out or create their own experiences, such as the creation of Black print media. Television and movie roles were often stereotypical and derogatory. As Blacks made progress in all areas of life, it was apparent that these negative images had deleterious effects in all aspects of Black culture, including both public and self-image. Several studies have been done that validate these phenomena, one being the well-publicized 1940’s doll study in which children are shown both a Black and Caucasian doll and asked which one they prefer. The (not so) surprising results revealed that the majority of Black children preferred the Caucasian dolls to the Black dolls and actually stated that the Black dolls were “bad.” In a shocking revelation, some children also stated that the white dolls “looked most like them.”
Other experiments performed more recently reveal similar results, even in adults with higher levels of education and intelligence. The psychological ramifications of years of oppression and suppression are devastating and while Black History Month cannot solve this complex issue, it provides a medium for highlighting the accomplishments of Blacks in this country and thereby creating positive images and positive energy for the

community. It can also serve to educate other cultures about our many contributions.
I was fortunate in my personal experience to have a mother who was an avid reader and especially a reader of Black history. Over the years, we learned of the accomplishments of Black Americans through our own personal reading and through Black History Month which often illuminated little known facts about Black achievers. From Garrett Morgan who invented the first traffic signal, to Daniel Hale-Williams, who performed the first successful open-heart surgery there are scores of Black Americans who made significant contributions to the world we live in today. Many of these accomplishments have only come to light in recent years. A prime example of this is demonstrated in the movie “Hidden Figures.”
This movie informed the world that not only was the trajectory of the first space flight calculated by a Black female mathematician, but that there was a whole team of these women working for the space program during those years. These accomplishments and the contribution of Black Americans, should be included as a routine matter of American History. But until it does, Black History Month ensures that there will be a recognition at least once a year.
In nursing, we also have many excellent trailblazers in the field. Dr. Elizabeth Carnegie had a retirement residence in Florida and she served as keynote at an FNA Convention and also shared many anecdotes of her struggles as a black educator as she established Florida A & M University as the first baccalaureate nursing program in Florida. She also served on the FNA Board of Directors as a member with “no voice and no vote.” She would giggle as she told the story of speaking and voting anyway. She said finally, at one meeting they asked her to leave and they voted to allow her to officially speak and vote in board meetings. She also shared that FNA was one of the first states to desegregate the association. Over the years, FNA boasts many excellent black leaders among their ranks. Kay Fullwood was serving on the Board of Directors when I became a member after graduating from nursing school. Kay was one of the early nurse practitioners in the state and served FNA in many capacities. Rose Rivers actually rose through the ranks from a certified nursing assistant, to the CNO of Shands Hospital in UF, to owning her own consulting firm. Willa Carson, my namesake and mentor, opened her own clinic to care for underserved patients in her county. Dr. Bobbie Jean Primus Cotton was an FNA member who was a faculty member at the University of Central Florida who also served on the Board of the National Black Nurses Association. She had served as my school nurse when I was in elementary schools. It is not that we do not and cannot receive support, mentorship and encouragement from our diverse colleagues, but for many, there is a security and comfort in the support and presence of someone who understands your experience. I also want to mention some contemporary trailblazers, like current board members, Dr. Marie Etienne and Dr. Linda Brown, who continue to contribute by promoting diversity and inclusion. Dr. Ora Strickland, Dean of the College of Nursing at Florida International University, an accomplished educator and leader has made a unique contribution to the FNA, by supporting and encouraging students to belong to their professional organization over several years of her tenure. With the push for diversity in the profession, role models like these are key to this goal. We are proud of our heritage and we want to share it with everyone and it is a fact that it is not always widely available to those who can be educated by it. It is important that we celebrate who we are to serve as role models for generations to come.
By the way, later in my life, the doll experiment illuminated my understanding of an experience I had as a young child. I was an avid doll collector, and in my mother’s wisdom, she only purchased Black dolls as an exercise in positive self-identification. I once entered a doll contest in my local community center, with my favorite doll. She was a beauty named “Betty the Beautiful Bride Doll.” I was about 7, which would be about 1961. All of the girls who entered their dolls were Black, but there were only two Black dolls entered into the contest and neither of them won a ribbon. I remember being very sad about that. For me, the doll experiment gave me the answer. I didn’t feel better about it, but I understood. Let’s always celebrate one another.

Owned and Published by, Florida Nurses Association
1235 E. Concord Street, Orlando, FL 32803-5403
P.O. Box 536985, Orlando, FL 32853-6985
Telephone: (407) 896-3261
FAX: (407) 896-9042
E-mail: info@floridanurse.org
Website: http://www.floridanurse.org
Office Hours: 8:30 a.m. to 4:30 p.m., Monday thru Friday
For advertising rates and information, please contact Arthur L. Davis Publishing Agency, Inc., PO Box 216, Cedar Falls, Iowa 50613, (800) 6264081, sales@aldpub.com. FNA and the Arthur L. Davis Publishing Agency, Inc. reserve the right to reject any advertisement. Responsibility for errors in advertising is limited to corrections in the next issue or refund of price of advertisement.
Acceptance of advertising does not imply endorsement or approval by the Florida Nurses Association of products advertised, the advertisers, or the claims made. Rejection of an advertisement does not imply a product offered for advertising is without merit, or that the manufacturer lacks integrity, or that this association disapproves of the product or its use. FNA and the Arthur L. Davis Publishing Agency, Inc. shall not be held liable for any consequences resulting from purchase or use of an advertiser’s product. Articles appearing in this publication express the opinions of the authors; they do not necessarily reflect views of the staff, board, or membership of FNA or those of the national or local associations.
Published quarterly, February, May, August and November by FNA, a constituent member of the American Nurses Association.
Editor – Kaitlin Scarbary, 1235 E. Concord St., Orlando, FL 32803-5403
Subscription available at $20.00 plus tax, per year. Members of FNA receive the newspaper as a benefit of membership.
COPIES of The Florida Nurse are available on 35mm microfilm, 106mm microfilm, article reprints and issue copies through Bell & Howell, 300 North Zeeb Road, Ann Arbor, Michigan 48106
Officers
Janice Adams, DNP, MPA, BSN, President
Marie Etienne, DNP, APRN, FNP, PNP, PLNC, President-Elect
Debbie Hogan, RN, BSN, MPH, Vice President
Valerie Halstead, PhD, APRN, FNP-BC, Secretary Mavra Kear, PHD, APRN, BC, Treasurer
Region Directors
Jake Bush, MSN, RN, Northwest Region
Kellyann Curnayn, DNP, APRN-BC, North Central Region
Susie Norman, MSN, Northeast Region
Constance Dey , BSN, RN, East Central Region
Meghan Moroney, BSN, RN, West Central Region
Cynthia Tagliaferri, RN, BSN, DNP Student, Southeast Region
Camille Baldwin, EdD, MSN, RN, CNE, CHSE, Southwest Region
Linda Washington-Brown, PHD, EJD, MSN, APRN-C, FAANP, FAAN, South Region
Director of Recent Graduates
Danielle Weaver, BSN, RN, CEN
LERC Liaison
Marsha Martin, RN
FNA Office
Willa Fuller, BSN, RN, Executive Director
John Berry, Jr., Director of Labor Relations & Government Affairs
Kaitlin Scarbary, Associate Director of Programs, Technology, and Membership Marketing

It’s time to spread the word about the Foundation Scholarships and Grants! The Foundation has over 30 scholarships available for nursing students residing in Florida and currently

Some meetings such as committee meetings and recurring regional meetings are not included in the list below. View the Full FNA Calendar at www.floridanurse.org/events.
Webinar: Healing the Heart with Ho’oponopono
February 9, 2022 | 7:00pm ET Virtual Presentation on Zoom
Northwest Region Networking Event + Micro-Practices of Self-Care for Nurses
February 24, 2022 | 6:00pm – 7:30pm CT Bonefish Grill, Pensacola, FL
Nursing Workforce Townhall Discussion
March 9, 2022 | 7:00pm ET Zoom Meeting
12th Annual FNA South Region Symposium & Awards Ceremony
April 9, 2022 | 8:00am – 2:00pm ET Gulfstream Park, Hallandale Beach, FL
1st Annual Southeast Region Nurse Appreciation Event
May 12, 2022 | 10:00am – 10:00pm ET Location TBA
8th Annual FNA Nursing Research and Evidence-Based Practice Conference
July TBA | 8:00am – 4:00pm ET Location and date pending
2022 FNA Membership Assembly
September 22-24, 2022
Mission Inn Resort, Howey-in-the-Hills, FL
Health Policy Special Interest Group
Every Second Tuesday | 7:00-8:00pm EST Zoom Meeting
Ethics Special Interest Group
Every Third Tuesday | 6:00-7:00pm EST Zoom Meeting
Holistic Nursing Special Interest Group
Every Third Thursday | 5:00-6:00pm EST Zoom Meeting
Interested in presenting for FNA? Go to www.floridanurse.org/speak Members of FNA/ANA will be given priority.
We welcome all nursing students and Registered Nurses regardless of membership status to all of our events unless otherwise noted. For registration and more information about FNA events, go to www.floridanurse.org/events
enrolled in a nationally accredited nursing program. Applicants must have completed at least one semester in their nursing program to qualify. The application window is open from January 1 to June 1. There are many scholarships and grants available but each year we have awards that are not given because there are no applicants who meet the guidelines. Some of the funds have specific application requirements such as geographic location or nursing specialty. The Foundation offers scholarships for all levels of study including basic nursing programs, master’s level, and doctoral programs.
Applications are available on our website and must be completed according to specifications to be considered. Applicants submit one generic application and upon review are paired with the scholarship that best fits their profile. Descriptions of available funds are listed on our website to give applicants a sense of some of the scholarships they could be paired with. It is important to submit a complete and thorough application to provide reviewers with the best information about the applicant. Some examples of funds offered are listed below. Please review the full guidelines at www.floridanurse.org/ScholarshipsGrants
Goodman Family Nursing Scholarship Fund - Qualified candidates must be undergraduate students residing in Palm Beach County who are members of their Student Nurses Association.
District 24 Erma B. Kraft Scholarship Fund Indian River County – Qualified candidates are generic students living in Indian River county.
Ingeborg Mauksch Scholarship – Preference given to Lee County Residents.
Kay F. Fullwood Northeast Florida Geriatric Nursing Scholarship Fund – Candidates must reside in Nassau, Duval, Baker, Clay, & Bradford Counties and have a focus on geriatric nursing (both undergrad and graduate levels accepted).
Iona Pettingill Scholarship - Open to any nursing student interested in public health.
These are just a few of the funds available! Visit www.floridaunurse.org/ScholarshipsGrants for more information.
Researchers
Research Grants are Available through the Foundation!
The Florida Nurses Foundation has several opportunities for Nurse Researchers to receive grants. The purpose of the Florida Nurses Foundation (FNF) Research Grant Program is to encourage the research career development of nurses to advance the profession of nursing.
The principal investigator must be a registered nurse and be licensed to practice nursing in Florida. Applications for the research grant must be for a study (proposed or underway) that has not been completed prior to application deadline. Applications for Research Grants are due JUNE 1. Find the full guidelines and application at www.floridanurse.org/ScholarshipsGrants
The Dr. Sandra Walsh Fund is Endowed!
Thanks to the generous contributions of FNA Members, the Nurses Charitable Trust and other donors, we have met the needed threshold to establish an annual scholarship or grant award under the Dr. Sandra Walsh Fund! We are working on the guidelines for the fund and will make announcements soon about the criteria and availability date. We will continue to seek donations for this fund in order to provide additional annual awards.




We are sorry to announce that Connie Dey has found it necessary to make the difficult choice to resign the role of East Central Region Director for personal reasons. We appreciate her time with us and the contributions she made. The newly appointed East Central Region Director is Marcos Gayol, EdD, MSN, MPH, RN. Dr. Gayol has been in the healthcare industry for more than 25 years as a practicing public health nurse, mentor, entrepreneur, and progressive administrator as well as serving in senior leadership roles within areas of population and community health, informatics, and higher education. Dr. Gayol resides in Ormond Beach in Volusia County and has served as part of the Reference Committee
for the FNA. He has a deep professional alignment with the mission and vision of FNA and wishes to support the regional association’s work through volunteering his time and talents towards advancing professional nursing and serving the association’s membership. The Region held its first meeting on January 26 in which ideas were discussed for engaging members, providing educational opportunities for the EC Region, and more. The Region will hold quarterly Zoom meetings to allow members to connect with others in their area. The next meeting will be on April 27 at 6pm ET followed by July 27 and October 26. Please RSVP for the meeting at www.floridanurse.org/ events to receive the Zoom link.

Greetings everyone! We had our first virtual meeting on December 20, 2021. Thank you to those who were able to attend. We will be having a face to face meeting on February 24 at 6pm CST at the Bonefish Grill 5025 N 12th Ave, Pensacola, FL 32504. We will be inviting a guest to speak on Micro Practices of SelfCare for Nurses. The cost to attend for members is $20 and we will be providing appetizers and non-alcoholic beverages. Be on the lookout for future information via email. Also, I am seeking FNA members in our region who are interested in being part of the Northwest
Region Leadership Council. If you would like to be part of our region’s leadership council, share any professional accomplishments, or have any regional activity ideas/questions, please feel free to contact me @ stebn21@gmail.com. I look forward to hearing from you. Thank you for allowing me the opportunity to serve our region!
Dr. Jake Bush

Greetings Florida Nurses,
As South Region Director, I want to welcome all the new South Region members and committee volunteers. South Region members are working diligently to provide our members with the latest updates on issues affecting nurses and the nursing profession. We invite you to join us in our 12th Annual FNA South Region Symposium & Awards Ceremony to be held on April 9, 2022, at Gulfstream Park in Hallandale Beach, Florida. We welcome faculty, students, hospital nursing staff and administrators to join us by submitting names of prospective applicants for nursing scholarships and award recognition of nurse leaders, nurse educators, and nurse innovators for their outstanding contributions to nursing. We will also host research posters and vendor opportunities. More information will be provided in our




next newsletter.
Please join us in our planned educational webinars, beginning with the latest updates on COVID-19, pediatric COVID vaccines, and medications approved to reduce or eliminate the effects of COVID-19 and its variants. Most importantly, we will continue to present panel talks on nurses caring for nurses during these very difficult times in our nursing history. South Region meets on the 4th Tuesday of each month at 6:00 p.m. Check the FNA calendar for more information.
Dr. Linda Washington-Brown, PhD, EJD, PNP, FNP, ANP-C, FAANP, FAAN

Hello SE Region members!! Here we go…. rolling right into 2022 with much to do and lots of momentum! Thank you all for helping to make these past few months a big success! We had the pleasure of hosting Senator Bobby Powell, District 30 as well as Representative Omari Hardy’s aide and fellow RN Tricia Hallison-Mischler, District 88, for an informal meet and greet at our December zoom meeting. We discussed nursing shortages, recruitment and retention efforts, and the importance of funding the Florida Center for Nurses. This was an important advocacy opportunity prior to FNA Advocacy Days and Legislative Session in Tallahassee. Well done everyone!
I’m so happy to share how our collaborative, fourth quarter monthly meetings in 2021 helped to drive a creative and interactive start to the New Year. New Leadership Council positions are available for each of our five counties to help further develop and strengthen our region. Little effort... Big rewards!
Essentially, these liaison positions are leadership roles that will provide each county in the region with a contact person to help virtually coordinate local legislative relationship building, event planning, activities, education, fellowship, etc., with me, to support the specific needs in your area, and help to
connect the members of each of the counties in our region. Remember: strength in numbers!!
So, Help me, Help you... Submit your name and county of interest to cynthia.fna@gmail.com
FYI... Our SE Region leadership zoom meetings are scheduled monthly on Wednesday evenings, mid-month, from 6:30pm to 7:30pm throughout the year, with exact dates posted on the FNA website calendar each month. We are in the process of planning our second quarter event for May, in honor of nurse’s week, so bring your great ideas and energy to our next meeting and let’s make a statement... and honor one another – together.
Meanwhile, in the spirit of Valentine’s Day this month of February, for our first quarter event, we are getting to the Heart of the Matter! SELF CARE!!!

Join us February 9th, from 7pm to 8pm, as the SE Region sponsors a self-care focused zoom event ‘The Conscious Heart Connection’ with feature presenter Ilene Gotleib, RN, CHTP, CMI, CQP, CHP. 1 CEU provided for registered members. Theme: Heart healing self-care for nurses.
So, see you soon on zoom!
And warm heart-felt wishes to everyone for a safe, healthy, and happy year to come! 2022... the year for you!!
My Best, Cynthia
Cynthia Tagilaferri, RN, BSN, DNP Student FNA SE Region Director Cynthia.fna@gmail.com

The Southwest Region held its first meeting of the year on Friday, January 28. Despite a small attendance, the meeting boasted productive conversation about plans for the upcoming year. The goal will be to have multiple networking and educational opportunities throughout the Region so that members in the different

counties can have activities close to them. The Region encompasses Charlotte, Collier, Glades, Hendry, and Lee counties. If you are interested in serving as a county liaison and helping to coordinate activities for the Southwest Region within your area, please send an email to Kaitlin Scarbary, Director of Member Programs at kscarbary@floridanurse.org

As we usher in the New Year, may we advocate for the most trusted profession by supporting The Florida Center for Nursing located at USF. FNA is closely involved in the reestablishment of the Center as its funding occurred on behalf of FNA’s grassroot advocacy and legislative action.

Our fellow West Central Region colleague, Rayna Letourneau, PhD, RN, has been appointed as the interim Executive Director of the Center. Dr. Letourneau is the founding director of USF College of Nursing’s Office of Wellness, Innovation, Resources, Education, and Support for the Healthcare Workforce. WIRES most notable programs include both Frontline Nursing During COVID-19: A New Paradigm and Excellence in Nursing During COVID-19 and Beyond. Frontline Nursing during COVID-19 is a continuing education program with more than 900 participants from four countries and more than 775 CEUs issued since its January 2021 establishment. Excellence in Nursing during COVID-19 is a collaboration with Sarasota Memorial Health Care System to ensure an adequate supply of healthy nurses to care for our community. If you are interested and need more information, please contact healthWIRES@usf.edu
Please join us for our next West Central Region Zoom Meeting on March 3, 2022.
Wishing everyone a Happy, Healthy, and Peaceful New Year!
Dear Florida Nurses,
Caroline Porter, FNSA President
I am honored and privileged to begin my term as the 2021-2022 Florida Nursing Student Association President. Founded in 1953, the FNSA is the preprofessional nursing organization for Florida’s 100+ colleges and universities, and represents 5,000+ nursing students participating in chapters across the state. I am excited to serve in this role and work alongside my fellow student nurses in Florida.

To share a little about myself, I was born and raised in Destin, Florida and am in my senior year at the University of Central Florida (UCF). I serve as the Secretary for the Student Nurses’ Association— Orlando Chapter, and as a Nurse Resident at the Orlando VA Medical Center in the Veterans Affairs Learning Opportunities Residency (VALOR) Program. In May, I will be graduating with my bachelors of science in nursing with a minor in medical anthropology, becoming the first nurse in my family.
Starting nursing school in the midst of a pandemic was one the hardest challenges I have encountered in life, but I have grown into a stronger leader and future nurse. With that in mind, my personal goal for this role



Panama
is to inspire, motivate, and lead those both entering nursing school and transitioning into the nursing profession as a registered nurse. However, I cannot do this alone. I am pleased to introduce you to the rest of the 20212022 FNSA Executive Board:
• 2nd Vice President- Vanessa Iturri, UCF
• Recording Secretary- Alexandria Moran, UCF
• Region 3 Director- Christian De La Cruz Cancel, UCF
• Region 4 Director- Chris Green, Keiser University- Melbourne
• Region 5 Director- Allyson Kifer, Florida Atlantic University
• Region 7 Director- Chloe Johnson, Florida Gulf Coast University
As we continue to fill the remainder of the board and conquer the difficulties our association has faced throughout the COVID-19 pandemic, I am eager to announce that this year’s 2022 Preconvention meeting will be held on September 17, 2022, followed by the FNSA 68th Annual State Convention in Daytona, Florida, October 27-29, 2022.
This year’s FNSA Executive Board’s goal is to recharge the state in the face of COVID-19. Our plan includes encouraging more involvement of student nurses in their pre-professional chapters and FNSA, through FNSA-directed events and leadership. Understandably, the pandemic has caused a multitude of hardships for Florida colleges and their school chapters. This is why it is critically important that we as student nurses stand together to advocate for our profession and healthcare. Through involvement in FNSA-hosted events that help nursing students collaborate with fellow peers and those in government, students will be able to make their voices heard.
Being a part of FNSA gives students the opportunity to be involved in an organization that stands for advocacy, scholarship, and ingenuity. It is imperative that while students, we stay involved in our community, and build skills needed to foster healthy relationships, such as compassion, patience, professionalism, and adaptability. Developing these skills will not only shape us as the future nurses of Florida, but also the future of nursing as a whole by setting an example and leading those across the nation.
As the Executive Board prepares to travel to Salt Lake City, Utah for the National Student Nurses’ Association 70th Annual National Convention, April 6-10, 2022, I encourage our constituents to also take this opportunity to run for national office, network, and build these essential skills while representing the state of Florida. Our engagement now as students can have lasting effects on our future careers. Participation in FNSA is terrific preparation for organizational involvement after graduation. Even before graduation, we have the ability if we work together to make real change in our profession through education, advocacy, and leadership!
I look forward to working with all of you throughout my term, and I would like to express my sincere gratitude for this opportunity! Please watch for updates on our website, www.FNSA.net, for future events. Thank you.




The Florida Nurses Association held its annual Advocacy Days on January 19-20, 2022. While the conference was originally planned to take place in Tallahassee, the winter surge of COVID-19 and associated concerns led to a decision to move the conference to a virtual platform. Despite the lastminute pivot, participants did not miss out on an informative and interactive event! FNA was able to host several guests from the Florida Legislature and attendees were given the opportunity to have virtual meetings in small groups with their own elected officials. Attendees were educated on topics to discuss with their legislators prior to breaking off into their meetings. The main topics discussed were recurring funding for the Florida Center for Nursing, nursing workforce shortages, and increased benefits and wages for state-employed healthcare professionals.
Erin Ballas, Vice President of Public Affairs Consultants, the lobbying firm representing Florida Nurses Association, educated attendees on the basics of advocating for an issue. She also provided an update on the current legislative session and bills on FNA’s radar. Several bills that FNA is monitoring in the 2022 session are related to the delegation of nursing care to unlicensed assistive personnel, a topic frequently seen in the legislature. Mavra Kear, Chair of the FNA Delegation Task Force, provided an overview of the legal responsibilities and potential liability risks to RNs for the delegation of nursing care to non-nurses. Relevant bills currently moving through the legislature were discussed.
Attendees were also debriefed on the progress of the Florida Center for Nursing which is being reestablished after losing and regaining its funding in 2020 and 2021 respectively. The new center will be a partnership between the Florida Nurses Association and the University of South Florida College of Nursing. The interim Executive Director for the Center is Rayna Letourneau who is working closely with FNA’s Executive Director, Willa Fuller on meeting the requirements of the state to re-establish the Center and begin working on its statutory obligations. The Center collects, analyzes and provides reports to stakeholders regarding the nursing workforce supply and demand. The funding for the Center was re-established by the state legislature in 2021 in large part due to the advocacy efforts of FNA, the lobbying team and the nursing community at large.
On the second day of the conference, attendees received an update on nursing regulation provided by Joe Baker Jr., the Executive Director of the Florida Board of Nursing. Updates to the Nurse Licensure Compact
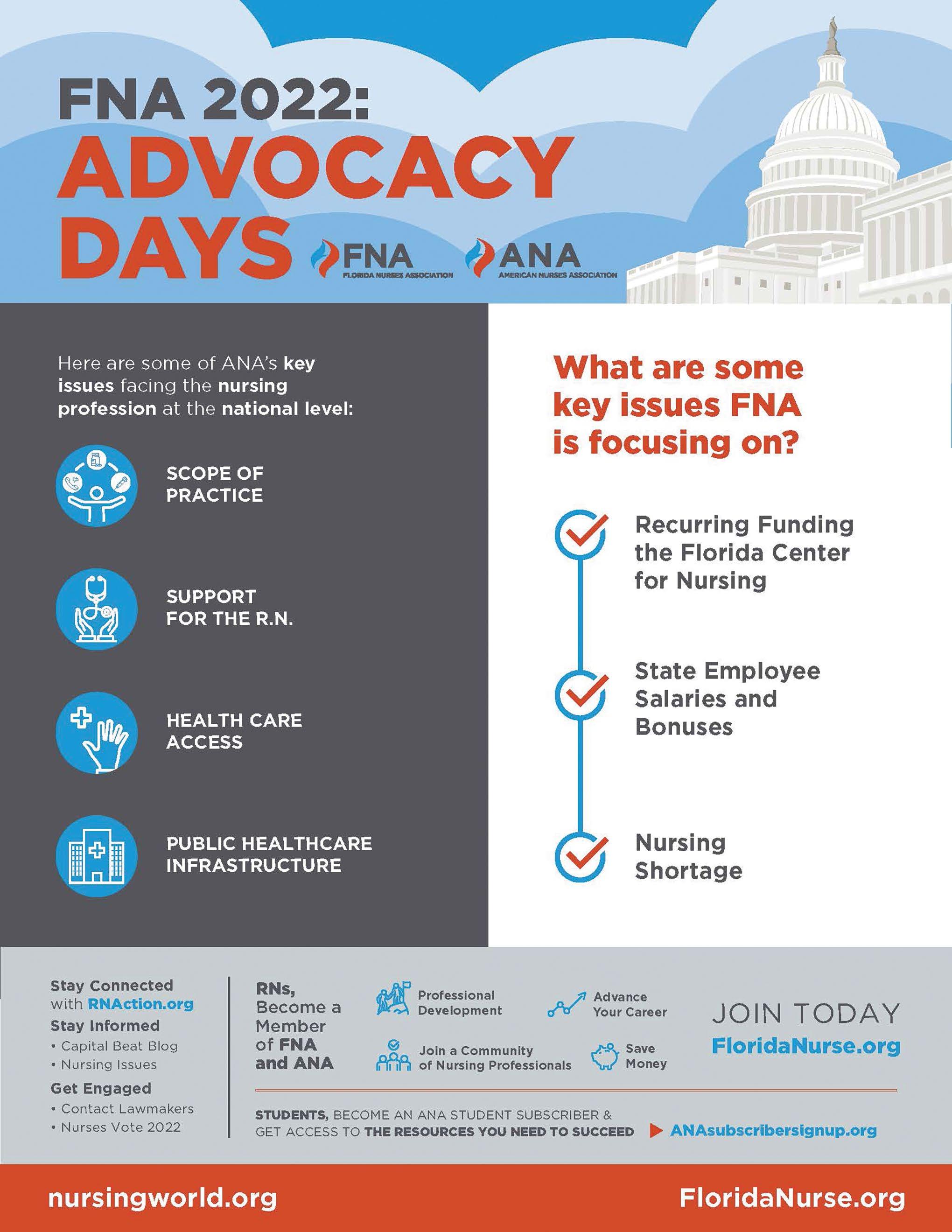
and autonomous practice for APRNs were two points of his informative presentation. Each year, participants express their appreciation for this session, which is applicable to all licensed nurses. William Pierce, the Florida representative to the Nurses on Boards Coalition (NOBC) provided an update on their national and state-wide goals and progress. The NOBC’s mission is to improve the health of communities through the service of nurses on boards and other governing bodies. Finally, Janice Adams, President of FNA and Co-Lead of the Nursing Action Coalition of Florida provided an overview of The Future of Nursing: Campaign for Action. The Campaign was launched in 2007 as an initiative of the AARP Foundation, AARP and the Robert Wood Johnson Foundation. The purpose of The Campaign from the beginning was to improve health by strengthening and leveraging the nursing workforce. State Action Coalitions were established across the country to accomplish The Campaign goals. The Florida Nurses Association is a co-lead organization for the Nursing Action Coalition of Florida.
Advocacy Days provides a hands-on opportunity for nurses to become advocates for their profession, but we always like to remind participants that advocacy doesn’t just take place during session – it is an all year affair. We encourage all nurses to familiarize themselves with the issues on FNA’s Legislative Agenda and connect with their local representatives to advocate on behalf of nursing. Go to www.floridanurse.org/advocacy to learn more.
The Florida Legislative Session convenes in March next year – stay tuned for 2023 FNA Advocacy Days dates which will take place during the March 2023 session!
Our Partner Organizations








On February 9th the Florida Legislature have arrived at the halfway point for the current Legislative Session. This is when it gets exciting! As time becomes more and more scarce, bills will take on new life as new ideas will be amended on and agreements between the House and the Senate will be reached. This year the House and Senate are constitutionally required to do two things: pass a balanced budget, and pass a new Congressional map, new Senate map, and new House of Representatives Map (also known
as Redistricting). The second requirement has already been completed, the House and the Senate have already released their respective maps and each chamber has voted on the maps. The Congressional map, however, has hit a bump in the road. The Governor has requested the Supreme Court weigh in on the Congressional map. Now the House and Senate are in a holding pattern.
Issues such as the 15-week heartbeat bill and “woke culture” bill are quickly becoming front runners for being most likely to take up bandwidth if bills were given superlatives. Why is this important to have on your radar? Because while your issue is important, the cosmos that is the State Capitol, may have outside influences that can affect the passage of your bill. These bills have resulted in hours of public testimony and highly emotional reactions for both the sides of the issues. This leaves members tired and sometimes cranky, so if you have the next bill up on the agenda, you might face some exhausted members.
Another issue garnering interest in the Capitol are a series of bills that have been drafted with the intent to end “pre-emption” bills in the future. Each year the Legislature has a set of preemption legislation aimed at correcting what the Legislature deems harmful local ordinances. Examples of these bills are Vacation Rental Legislation, Paper Straw Legislation, Plastic Bag Legislation and even Management of Local Ports Legislation. Well, President Simpson has decided he is tired of these kinds of legislation and has instead drafted Legislation whose intent is to end preemption language for future Legislatures. SB 620 Local Business Protection Act by Senator Travis Hutson of St Augustine and HB 569 by Representative Lawrence McClure, will create a cause of action for an established business to recover loss of



We are primarily looking for presenters for webinars but there may be some opportunities for face-to-face presentations.
Presentations can fall under a variety of topics such as nursing care, evidencebased practice, nursing research, legislation/health policy, public health, advancements in healthcare technology, and more. Presentations related to wellbeing, personal health, and self-care are also welcome!
If you have a topic that you’d like to share with your colleagues, please submit a proposal for our review team at www.floridanurse.org/speak
Please keep in mind that most presentations will be submitted for nursing contact hours and therefore should have learning objectives to help fill a gap in knowledge or skill.
FNA Members are given first priority for being selected to present.

This year the Florida Nurses Political Action Committee (FNPAC) will be holding Candidate Interviews prior to the Elections. The purpose of the interviews is to determine how candidates align with FNA’s Legislative Agenda. FNPAC exists to raise funds to support candidates that will work with us on issues related to nursing, patients and healthcare.
We are asking members to do three things:
1. Make an appointment and visit with your legislators to discuss FNA’s Legislative Agenda and to build a working relationship. Download our Legislative Toolkit at www.floridanurse.org/Advocacy
2. As candidates emerge, please begin to meet with them and ask them questions about our agenda and THEIR priorities.

3. Watch your emails for announcements about our Candidate Interviews. We want representatives from all aspects of nursing present.
DONATE: We must make our presence known through both our voice and our donations. We want to make this an EPIC year for the PAC.
Five Reasons to give to the Florida Nurses Political Action Committee:
• FNPAC endorses candidates that have stated that they will support FNA issues.
• FNPAC vets candidates to determine their positions on nursing and healthcare issues.

• Legislators and candidates actively seek the FNA endorsement through FNPAC.
• FNPAC has a record of success with endorsements over many years.
• Donations to FNPAC provide a way to contribute to the political advocacy for FNA and for nurses and patients throughout the state.
BECOME A TRUSTEE: We have openings for new trustees on our PAC this year. Trustees help with fundraising activities, participate in candidate interviews, and vote on which candidates to support. If you are interested in being involved, please complete the application on our website at www.floridanurse.org/FNPAC
For questions about FNPAC, donations or becoming a PAC trustee, email Iris Lopez at info@floridanurse.org

 John Berry
John Berry
As the 2022 Legislative Session continues, each of us should be thinking, how can I help to advance my profession, my practice? We can all start by taking a look at the Florida Nurses Association website, www. floridanurse.org. You’ll see “Advocacy” on top of the right side of the page. Under the heading you’ll find the Association’s “Legislative Agenda” which will list the issues the Association will be advocating for in the upcoming session, as well as how our members can contribute to the Florida Nurses Political Action Committee or “FNPAC.” Money that is contributed by our members to the FNPAC helps to elect candidates that are supportive of our legislative agenda.
We become advocates because we are passionate about a certain issue or cause that can personally affect us or others that we know. There are no finer advocates than nurses when they are fighting for the treatment of their patients. But the fight doesn’t just end there. Nurses need to take that fight to the halls of the state legislature in Tallahassee. Legislators need to hear the personal stories from nurses on their daily fight in their health care institutions to ensure that proper funding is provided to their facilities for patient care, for programs, and for their safety and their practice.
I know that as nurses you are the consummate professionals and display the utmost confidence in everything you do when advocating for your patients. But in unfamiliar surroundings such as a legislator’s office, it can make you feel a little uneasy. Start out by introducing yourself, and if you are a constituent, make sure that you say so. We may not feel it at times, but as constituents, our word carries a lot of weight. It’s because we represent a vote, a family’s vote, a friend’s vote, a colleague’s vote and even an acquaintance’s vote. That is how you are viewed by a legislator. He or she knows that you have the power to put them in
office or to vote them out. Tell them where you work, what your job title is and how long you’ve worked there. You are there to tell your story, to educate, to make an impact on that legislator so that he or she has the proper information and knows how they should be voting on a particular piece of legislation. Sometimes you might not get to speak with the elected official because they could be in session or in a committee meeting. Although it’s great to speak with your representative, you shouldn’t be disappointed if the meeting is with their staff. There are plenty of legislative staff that are more versed on the subject matter than your representative is. When you’re through with your meeting, thank them for their time and always leave them with information to review. Be sure to leave your contact information and let them know that if they need anything further, you are available to answer questions.
January 19th and 20th of 2022 were the Florida Nurses Association’s Advocacy Days. Whether you lobbied in person, or virtually with your elected representative, I hope you took every opportunity to make your voice heard. Don’t leave it up to someone else. Get involved and make a difference.
Legislative Update continued from page 9
Debbie Hogan, MPH, BSN, RN President, FNA State of Florida, Professional Healthcare UnitThe past two years have been an unprecedented time in the field of public health, as you and other public health care professionals here in the state of Florida have battled the COVID-19 virus in order to protect our residents, the wards of the state and our visitors. As “first responders” on the front lines, we are forever grateful for your hard work, expertise and dedication.

The Florida Nurses Association, OPEIU, Local 713, AFL-CIO Health Care Professionals Bargaining Unit wants you to know that we will continue to fight for you and your workplace protections spelled out in your state contract. It is an ongoing challenge in our state. We need your help if we are to strengthen our position in negotiating with the state of Florida on your behalf. Will you join us?
Increasing our membership is essential. The state needs to see that our professional health care employees believe in their contract, and its protections and belong to their bargaining unit. Do this by maintaining your membership and encouraging your co-workers to join too!


As current members who want to become even more involved, join us by running for office in the HCP Bargaining Unit. With enough participation, we will be holding an election for our state offices this year. According to our Bylaws, the Executive Board is made up of:
President – Presides at all meetings and Negotiation sessions, and serves as an ex-officio member of all committees, except Nominating committee.
Vice-President – In the absence of the President, the Vice-President shall perform the duties of the President, and become President in case of vacancy.
Secretary/Treasurer – Work with the FNA Bargaining unit staff to maintain records and reports.
These officers shall be elected for three years, or until their successors are elected. Retirees who have been active while employed, can also run for office.
We also need Local Representatives at each workplace to communicate with the Bargaining Unit regarding workplace concerns and share updates at your workplace. Please join us!
Watch for the ballot that is coming soon. Please vote for your Bargaining Unit leadership and return your ballot as soon as possible. Also, please volunteer to serve as a local representative, so that we can better communicate with all our workplace sites! We want and need to hear from you!!!
In Solidarity, Deborah Hogan, RN, MPH FNA HCP Bargaining Unit
business damages from a count of municipality whose regulatory action causes a significant impact on the business. While this legislation will keep businesses whole, it will cost local governments and therefore taxpayers millions of dollars in lawsuits.
As session moves into the final portion of the 2022 Legislative Session, things will move quickly. Budget negotiations will take place and final negotiations on priority bills will commence. Much like sand in an hourglass, time will slip away. We encourage you to stay connected with FNA for updates on priority bills and possible call to actions. Our top priority is the continued funding of the Center for Nursing. Be on the lookout for possible emails or calls to be made to encourage lawmakers to include this essential funding in the budget.
FNA is asking members to stay in touch with their legislators by encouraging support for RECURRING funding for the Florida Center for Nursing. With the current staffing crisis, it is essential that we have data on the workforce to be able to understand future needs for our state and to make recommendations for action.
We are also concerned about a proliferation of bills that create new unlicensed roles and positions for nurses to delegate nursing tasks to. We are monitoring those bills and have asked FNA members to voice their concerns regarding this issue.
As always, should you have any questions, please feel free to reach out to me, Erin Ballas at 850-7286387 or Jack Cory at 850-566-9175. It is our pleasure to represent you the Nurses of the great State of Florida.


We are looking forward to hearing from you!


The Florida Nurses Association is a member-driven organization. As your Vice President, it is my privilege to work with you, our members, to sustain and increase our membership. Through our Membership Committee, we will develop strategies to support our current members, and to welcome new members. We appreciate your ideas! Some of my goals include:
1) Based on your input, meet current members’ needs in order to sustain membership.
2) Working with you, the FNA Board, and Staff, continue to advocate for nurses’ professional and practice needs, especially during these challenging times.
3) Educate members regarding approaches to welcome and encourage other nurses to join.
4) Develop creative communication approaches to reach out to nonmembers to encourage them to join their professional organization.
Can we count on you to help? You, our members, are our most important resource in encouraging other nurses to join! I look forward to working with you!
-Debbie Hogan, Vice President, FNA

In 2021, the Florida Nurses Association (FNA) facilitated formation of a task force to promote social justice in nursing and health care. This initiative was a response to the increasing lack of diversity, equity, and inclusion in nursing.
What is social justice? There are many definitions which the task force explored in an effort to offer a definition pertinent to our FNA membership and Floridians. With support members attending a town hall meeting, the task force articulated social justice in healthcare to mean:
A non-judgmental space where all persons give and receive care in a supportive environment that promotes open communication about beliefs and health goals. Health care providers must be selfaware, take responsibility for developing interpersonal skills to engage with diverse individuals and groups, and continually advocate for equitable and inclusive delivery of services within their care agencies.
As health care professionals, nurses have a moral imperative to advocate for equitable health care for all. This position is evidenced in our code of ethics which clearly states that “the nurse collaborates with other health professionals and the public to protect human rights, promote health diplomacy, and reduce disparities” (ANA, 2015). This directive and definition of social justice in health care propelled the task force’s effort forward in addressing the FNA general assembly in September.
FNA’s statement on this position is that: The Florida Nurses Association advocates for equitable and inclusive care delivery in our state. How are we going to do this? The actions, approved by the assembly, include the following:
1. Offer education to nurses and nursing students on social determinants of health and inequities in healthcare outcomes.
2. Collaborate with QUIN Council to increase awareness of implicit injustices that may exist within each members’ realm.
3. Develop partnerships with state and local organizations, within and outside of nursing, to create initiatives that promote equitable health care for all persons in all settings.
4. Explore health care policies related to social determinants of health and inequities in healthcare outcomes.
The next steps will start with a focus on education. The task force will collaborate with the Diversity, Equity, and Inclusion (DEI) Task Force in these efforts. An educational program focusing on this topic is being discussed for 2022. What can you do, as a FNA member? Address your own barriers to social justice – your thinking and/or actions. Tap your compassion to be culturally competent. Engage in discussions with your diversity officer where you work. Identify vulnerable populations in your workplace and community and make an attempt to understand their situation. Increase your awareness about social justice in health care, just as FNA will take steps to advance our understanding and efforts to promote equitable health care for all persons in all settings. And finally, encourage diversity of thought and equity excellence every day.
References
American Nurses Association. (2015). Code of ethics for nursing. American Nurses Publishing.
Members of the task force include: Susan Fowler, Charles Buscemi, Mavra Kear, George Smith, Karen Kuperberg, Willa Fuller


During Membership Assembly 2019, the Board of Directors were directed to form three task forces through Reference Proposal and one main motion. Those task forces were a Pandemic and Disaster Task Force, A Diversity, Equity and Inclusion Task Force and a Social Justice Task Force. The following is a brief update of their progress.
Pandemic and Disaster Task Force
This task force, chaired by Dr. Deirdre Krause have fashioned their work around the goal of promoting a coordinated effort by the state in the management of pandemics and disasters with nurses as essential workers being included in the process. They have taken on several projects including managing an updated Coronavirus Dashboard on the FNA Website, collecting data regarding vaccines and vaccine hesitation to promote vaccination and the ameliorating of the spread of the virus, activities related to improving the mental health and well-being of nurses and a special project to tell the Florida nursing story of the role nurses have played during the pandemic and the impact on their practice and their personal lives. This group continues to meet to complete their objectives during this year.
Social Justice Task Force
This group, chaired by Dr. Sue Fowler and Dr. Charles Buscemi took time to examine the issue of social justice and determine nursing’s role in moving forward in an impactful way. They produced a Reference Proposal for the 2021 Membership Assembly that concluded with four recommendations for action to be carried out in the coming year and beyond. These are:
1. Offer education to nurses and nursing students on social determinants of health and inequities in healthcare outcomes.
2. Work with Quality and Unity in Nursing (QUIN) Council to increase awareness of implicit injustices that may exist within each member’s realm.


3. Develop partnerships with state and local organizations, within and outside of nursing, to create initiatives that promote equitable health care for all persons in all settings.
4. Explore health care policies related to social determinants of health and inequities in healthcare outcomes.
They also felt that it might be prudent to consider merging the Social Justice and DEI task forces. They are planning a joint meeting in February to discuss the possibilities for this option.
This task force is chaired by Dr. Marie Etienne and was formed to examine DEI as it applies to nursing in Florida. As a first step, this group decided to launch a survey to assess the
diversity of the members of FNA. The survey was developed and launched and had nearly 300 responses. Analysis and the development of a report is in process.
The FNA Board of Directors is concerned about the number of bills in recent years that focused on registered nurses delegating tasks to nonlicensed personnel. The task force, chaired by Dr. Mavra Kear, met several times to review bills in the current session and we also requested an analysis of the Nurse Practice Act by legal counsel to make an assessment of risk to nurses. This information was shared in a presentation by Dr. Kear at the 2022 Advocacy Days and we continue to monitor bills and will continue meeting to make recommendations regarding this important issue.

FNA and the New Grad special interest group will be planning a series of events for recent graduates in 2022 starting with virtual meetings to network and discuss some of the topics that are at the forefront of nurses’ minds. The past two years have been one of the most challenging times to begin a nursing career and there are many areas of concern to discuss. We will also soon be releasing a newsletter geared towards


our members that are recently graduated nurses. Stay tuned for more information coming out soon. If you are currently member of FNA, please be sure to join the New Grad Special Interest Group through the community forum on our website. Joining will ensure that you receive the latest news and updates for this group, including the forthcoming newsletter. If you are a recent graduate and are not yet a member of FNA, we strongly encourage you to join. Being a member of your professional association provides a network that you can turn to while navigating the first few years of your career and beyond. We recently reduced our membership rates to only $15 per month, making membership more accessible than ever. Members of the Florida Nursing Students Association receive their first year of membership in FNA for free. Go to joinfna. org for more information.



“Navigating
Changes in Healthcare Monitoring Through Education and Support”
This year’s IPN/FNA Conference theme, “Navigating Changes in Healthcare Monitoring Through Education and Support,” will address topics of: the impact of COVID-19 on nurses under monitoring; the resurgence of substance abuse among nurses; the relationship of trauma and PTSD to substance abuse; and changes in Employee Assistance Programs post COVID-19.
Our speakers include:
• Scott Teitelbaum, MD, FAAP, FASAM
• Patricia O’Gorman, PhD
• Carol Burrell-Jackson, PhD, MSW, LCSW, Basic ART
• Myrtle Greene, PhD, LMHC, CAP, ICADC
Target Audience:
• Registered Nurses of all specialties, Licensed Practical Nurses, Certified Nursing Assistants
• Other healthcare professionals interested in the monitoring for compliance by an alternative to discipline program (ATD)
• Treatment Programs staff members (therapists, psychologists, case managers, toxicology coordinators)

8:30‐9:00 am Log in for Attendees Sponsorship Slideshow
9:00‐9:15 am Opening Remarks
9:15‐10:15 am Speaker: Scott Teitelbaum, MD, FAAP, FASAM
10:15‐10:25 am Break/Slideshow
10:25‐11:25 am Speaker: Carol Burrell–Jackson, MSW, PhD., LCSW, Basic ART
11:25‐11:35 am Break/Slideshow
11:35‐12:35 pm Speaker: Myrtle Greene, PhD., LMHC, CAP, ICADC
12:35‐12:45 pm Breaks/Slideshow 12:45‐1:45 pm Speaker: Patrica O Gorman, PhD 1:45 pm Closing Remarks
Registration
Registration available at www.ipnfl.org Click on Education drop down for Annual Conference registration 1‐day registration: $50.00
Current IPN participant rate: Free




Dec 29th 2021
SILVER SPRING, MD –The American Nurses Association (ANA) is deeply concerned about the latest guidance from the Centers for Disease Control and Prevention (CDC) for health care settings, citing insufficient evidence, concern for health care workers’ safety, and the potential for it to lead to an increase in COVID-19 cases. The emergency guidance shortens the time for isolation and quarantine for health care workers infected with or exposed to COVID-19. This guidance is premature given what is known about the Omicron variant and tips toward economic needs as opposed to the health needs of nurses and other health care workers.
Released on December 23, changes to the guidance are specific to contingency and crisis strategies that reduce the isolation period for nurses and other health care workers who have tested positive for COVID-19. ANA is concerned that the return-to-work guidance for all health care personnel under the updated mitigation strategies will endanger the health and safety of health care workers and those they encounter.
This guidance is especially problematic when reliable testing is not widely available, and particularly difficult to access in places experiencing surge conditions. In order for the revised guidance to work, health care employers must continue to provide ready access to personal protective equipment (PPE) and


Each year, FNA Advocacy Days empowers its members to have a voice in legislative issues related to nurses and the patients we serve. In our 20th year of representing Florida’s nurse practitioners, the Florida Nurse Practitioner Network (FNPN) was honored to be a contributing partner to
the 2022 FNA Advocacy Days. FNPN members joined FNA members virtually to learn how to become involved in critical legislative issues through grassroots advocacy and encourage nurses in all roles to become involved. In groups organized according to legislative districts, attendees met virtually with some of Florida’s state senators and representatives. Advocacy Days attendees also received updates from the Board of Nursing, The Nursing Action Coalition of Florida, and the Nurses on Boards Coalition. The event was a success, and FNPN looks forward to partnering with FNA in 2023.
Deborah Tedesco, DNP, APRN, ANP-BC, AP-PMN, CBCN, CWS, CWCN-AP, CPHQ President, Florida Nurse Practitioner Network
ongoing testing at the worksite to inform return-towork status.
“Nurses have endured intense stress for almost two years as the pandemic has persisted and evolved with the emergence of new variants. Despite exhaustion, nurses continue to provide care to patients under extremely difficult conditions,” said ANA President Ernest J. Grant, PhD, RN, FAAN. “While staffing shortages are challenging for facilities experiencing a surge in cases, we must prioritize health care workers’ and patients’ health and safety, including allowing for sufficient time off for health care employees. I urge the CDC to reconsider these guidelines and for policymakers to aggressively pursue other strategies to bolster the health care system. We support the Administration’s steps to call up more surge teams and use the Defense Production Act to increase access to testing while continuing to use every strategy to increase the number of Americans who are fully vaccinated and boosted.”
ANA met with and provided comments to the CDC expressing significant concerns about the proposed changes to this guidance. In September, ANA also urged the U.S. Department of Health and Human Services (HHS) to declare the current and unsustainable nurse staffing shortage facing our country a national crisis. The pandemic has exacerbated underlying, chronic nursing workforce challenges that have persisted for decades.



The FNA Research Special Interest Group invites you to submit your nursing research or evidence-based practice project to be considered for poster or podium presentation at the FNA Annual Research & EBP Conference to be held in Orlando in July 2022. Lit reviews and concept analyses will be considered for poster presentation. Abstracts will be peer-reviewed for selection.
Submissions are due by Monday, May 9
Guidelines for submission can be found at www.floridanurse.org/ResearchConference

Distress for Healthcare Professionals (MMD-HP). The instrument was provided to registered nurses, oncology technicians, providers, respiratory therapists, and ancillary team members.


Moral distress is a concept that has experienced a significant metamorphosis over the last ten years and continues to broaden in its inclusion of emotional, physical, and psychological consequences. As a strong focus topic for the American Association of Critical Nurses, it has been examined with the hope of helping the profession of nursing better understand the result of working in an environment where prolonged or unnatural death is sometimes a daily occurrence. Nurses’ core values consist of attempts to help patients feel better, but as technology advances patients become dehumanized by mechanical and chemical sustainment and nurses struggle with the artificial and sometimes barbaric attempts to sustain life while trying to maintain or improve a patient’s comfort. From a moral standpoint, nurses feel that a natural, symptom managed death is ethically ideal versus the choices they see that are made by families and sometimes providers. It then becomes more and more difficult to carry out orders and tasks when the situation is in direct conflict with this belief. Descriptions of these end-of-life interventions now include dramatic terms such as heroic efforts, extraordinary measures, and exhaustive resources.
As a result of this type of care environment, significant outcomes of experiencing MD include burnout and job dissatisfaction leading to poor retention.
We set out to describe perceptions of MD among our critical care interdisciplinary team members. This descriptive cross-sectional design collected a single set of measurements using the Measure of Moral
Sixty-seven team members completed the survey. Three of the 27 items had a mean response above eight (halfway point of scale indicating higher MD):
• “Follow family’s insistence to continue aggressive treatment even though I believe it is not in the best interest of patient”
• “Continue to provide aggressive treatment for a patient most likely to die regardless of this treatment when no one will make a decision to withdraw it”
• “Witness providers giving ‘false hope’ to patient/ family”
Furthermore, higher total scores were related to having left or considered leaving a job. “Continuing to provide aggressive treatment” was associated with having ‘considered leaving due to MD’ and ‘considering leaving now due to MD.’
Our findings suggest that MD associated with aggressive treatment and false hope are areas to further explore in our setting with focused efforts at reducing MD. During the Covid-19 pandemic, the critical care environment experienced its worst assault in history due to critical staffing shortages, the high acuity of these patients, inadequate supplies of sufficient personal protective equipment, and harsh working conditions. Nurses seemed to be caught in this dynamic and evolving situation and were often unable to either take the time or have the courage to use their voice and advocate for their own care. The realities of this type environment were compared to the emotional state of battle fatigue with soldiers. It quickly accelerated some organizations’ acknowledgement of moral distress and execution of strategies to attempt to address it. Organizations would be wise to continue to monitor this phenomenon as a way to develop programs that could retain staff, alleviate or prevent burnout, and improve job satisfaction.
Sandberg, A., Beuer, G., Reich, R. R., & Mason, T. M. (2021). Moral distress among interdisciplinary critical care team members at a comprehensive cancer center. Dimensions of Critical Care Nursing, 40 (5), 301-307. doi: 10.1097/DCC.0000000000000490


The newly released report, The Future of Nursing 20202030, Charting a Path to Achieve Health Equity is focused on the nursing profession creating a culture of health, reducing health disparities, and improving the health and well-being of Americans in the 21st century. The emphasis is on multisector teams and partnerships with a focus on the question: “what can nurses do to address the culture change needed to improve nursing?” (NASEM, 2021). The state of Florida has been, and continues to be, grappling with these same issues.
In 2019, members of the Florida Nurses Association (FNA) West Central (WCEN) region identified a gap in knowledge regarding available data about the culture of the nursing work environment that might influence nurse staffing, retention, and turnover. This finding indicated a need to conduct research aimed to explicate characteristics of the culture of the nursing work environment. Toward that end, WCEN partnered with the Florida Action Coalition (FLAC) to begin work on this critical need.
The study used a multimethod design with IRB approval. The first stage included structured interviews, which were recorded and then transcribed. The open-ended questions centered on the culture of nursing within the work environment. A thematic analysis of the transcripts was conducted by each researcher individually. They then compared their results, discussed the findings, and came to consensus on the resulting six themes: nurses’ role misunderstood; nurses not valued; lack of teamwork; power struggles; job security concerns related to speaking up; and ways to make it better. The interviews concluded just as the Covid-19 pandemic began, which caused the researchers to consider how the pandemic would impact the culture of nursing. To further explore this aspect, stage two of the research design was added. A survey based on the original six themes was developed and administered. Under each theme question the respondent could select any of the comments identified in the original transcripts that applied to their work environment. Also included in the survey was the opportunity



to provide additional comments along with a question that asked, “What impact has the Covid Pandemic had on the work culture?” The survey was distributed to the original participants in stage one about one year after the interviews were complete.
Consistent with the interviews, all respondents reported that teamwork was required to get through, but 67% still felt that nurses continue to work in silos and need to collaborate more. All reported that the nurse’s role is still not understood, they still believe that power dynamics impact the work culture, but they all felt valued with 67% reporting that their work was appreciated. One respondent commented that “once nursing speaks in one collective cohesive voice, we can make real lasting change.” Contrary to the interviews the respondents were not as concerned about the impact of speaking up about issues, but they were concerned that physical separation has impacted communication.
These nurse concerns should be addressed with comprehensive, significant, and lasting approaches to improve the work culture for nurses individually and collectively. Strategies and interventions co-created and implemented by a collaboration of directcare, academic, executive, and middle management nurses will be more likely to be accepted integrated into the workplace than changes made by leadership alone (Bowles et al, 2019).
Interdisciplinary education for nursing and other healthcare professions could provide opportunities for future healthcare providers to learn early in their careers about each other’s professional roles, how to collaborate in teams, how to communicate across disciplines, and the importance of advocating for each other. Engaging early in professional associations as students could help eliminate silos and promote team approaches to the provision of healthcare. Nursing leadership skills acquisition is essential to supporting nurses and reducing the effect of power dynamics in the work environment. Continued availability of opportunities for leadership development is essential to management of the workplace.
A comprehensive approach to changing the culture of the nursing workplace and keeping nurses in the profession is essential. This includes nursing advocacy, interdisciplinary education, and advancing nursing leadership development with multiple approaches and strategies. Highly knowledgeable and skilled nurses in the profession are essential to achieving optimal health outcomes of the diverse populations they serve.
References
Bowles, J. R., Batcheller, J., Adams, J. M., Zimmermann, D., & Pappas, S. (2019). Nursing’s leadership role in advancing professional practice/work environments as part of the Quadruple Aim. Nursing Administration Quarterly, 43(2), 157–163. https://doi.org/10.1097/ NAQ.0000000000000342
National Academies of Sciences, Engineering, and Medicine (2021). The Future of Nursing 20202030: Charting a Path to Achieve Health Equity. Washington, DC: The National Academies Press. https://doi.org/10.17226/25982



Numerous studies show the prevalence and devastating impact disruptive behaviors have on nurse retention and satisfaction, patient safety and the financial health of an organization. Today, more than ever, the unpredictable, life-and-death nature of the pandemic has created an environment that is ripe for an increase in workplace bullying and incivility. Research at the Healthy Workforce Institute shows an uptick in bad behavior and nurses are experiencing greater workplace incivility now more than ever before. Additional studies show:
• 45.7% of nurses said they witnessed more incivility than before the pandemic (El Ghaziri et al., 2021).
• 14.3% of surgery patients had higher complications with surgeons who had one to three reports of unprofessional behaviors compared to those surgeons who had no reports of disruptive behaviors (Cooper et al., 2019).
• 94% of individuals have worked with a toxic person in the last five years; 51% of the targets stated they are likely to quit as a result (Kusy, 2017).
Developing successful, targeted interventions to reduce bullying and incivility among nurses will require that leaders develop awareness and understanding of nurses’ unique experiences with disruptive behavior. One of the biggest areas of confusion that makes it difficult to address and eliminate bad behavior is a misunderstanding about the differences between bullying and incivility. An important first step to educating yourself and your employees is to get clear on those differences. This will help you raise awareness, set expectations, and develop
appropriate strategies to eliminate each type of disruptive behavior. Bullying should be a NEVER event, but not everything is bullying and when we call everything bullying, we lessen our chances of identifying and addressing true bullying behavior.
For a behavior to be considered bullying, it must include three things:
A Target-This target can be a single person or group of people. Group targets can include the opposite shift, new nurses, or nurses who have a particular ethnic background.
Harmful-The behavior must be harmful in some way. This harm can be to the target or harmful to a patient. Repeated-The most important element of bullying. The behavior can’t be just a one-time event, it must be repeated over time.
Incivility is different from bullying but tends to be much more pervasive. While the behaviors can be similar, they tend to be lower level. Incivility shows up as your typical rude, unprofessional, inconsiderate behaviors: eyerolling, condescension, favoritism, alienation, gossiping, mocking, cursing. Make no mistake about it, incivility is a healthy and professional workplace killer, and needs to be addressed.
The Bottom Line
Bullying and incivility can destroy work environments and impact patients in a negative way. The key is to get very clear on the behavior – is it bullying (target, harmful, repeated) or incivility (low level, rude, and unprofessional). We are hemorrhaging nurses due to bad behavior and it’s time we get educated on how to recognize and address bullying and incivility so that we can cultivate a more respectful and professional work culture.
References Cooper, W., Spain, D., Guillamondegui, O., et al. (2019, June). Association of Coworker Reports About Unprofessional Behavior by Surgeons with Surgical Complications in Their Patients. JAMA Surgery, 154(9), 828–834. doi:10.1001/jamasurg.2019.1738
El Ghaziri, M., Johnson, S., Purpora, C., Simons, S. and Taylor, R. (2021, July). Registered Nurses’ Experiences with Incivility During the Early Phase of COVID-19 Pandemic: Results of a Multi-State Survey. Workplace Health & Safety. doi:10.1177/21650799211024867
Kusy, M. (2017). Why I don’t work here anymore: A leader’s guide to offset the financial and emotional cost of toxic employees. Boca Raton, FL: CRC Press
Bio:
As an international speaker and consultant, Dr. Renee Thompson tackles the challenges facing healthcare leaders today. With 30 years as a nurse, Renee is an expert on creating healthy workforces by eradicating bullying & incivility. She is in demand as a keynote speaker and has authored several books on bullying.

Beautiful lakefront setting with heated pool. Salary, room, board and travel — families welcome. Partial summer available.
Season dates: June 15th-Aug. 21st. Must enjoy working with children in a camp setting. Day Camp & Sleepover Camp, coed, ages 3 to 16. 917-703-2128 | email: leron@campkimama.org www.kimamahalfmoon.com


Reprinted with permission from Tennessee Nurse May 2021 issue
Dependency and Abuse of Opioids
Prescribing opioids is not the problem. Opioids provide highly effective pain management for acute pain originating from injury, surgery, cancer, and palliative or end-of-life-care. Appropriate prescribing achieves adequate pain control; reduces patient addiction risks, abuse, or toxicity; and minimizes drug diversion.
Nevertheless, abuse and overdose deaths are still problematic, although data indicate US healthcare providers are making headway; since 2012, prescription overdose deaths have been declining. There were 67,367 US drug overdose deaths in 2018, which represented a 4.1% decline from 2017. Seventy percent of US drug overdose cases involved opioids. But deaths from natural and semi-synthetic opioids such as those typically prescribed by primary care practitioners (hydrocodone, oxycodone, or codeine) actually declined 14% from 2017 to 2018. Tennessee deaths from prescribed opioids also declined in 2018.
Nursing Roles
All RNs contribute to safe care delivery, patient assessment, pain management and education, whether working as an office RN, Advanced Practice Registered Nurse (APRN), or Nurse Practitioner (NP) with advanced practice credentials that include specialized pharmacology education with prescriptive authority.
The diversified roles of RNs extend beyond primary care to assorted direct patient care and leadership positions. As skilled educators and patient advocates, nurses help patients and families understand other pain management modalities such as physical therapy, psychological management options, complementary medicine and non-opioid management strategies to ease the burden of pain. The American Nurses Association (ANA) noted that in part, the current US crisis has been created by ineffective medical efforts to manage chronic pain. The ANA applauds nurses as key players for pain management by providing early recognition and pain interventions in primary care settings, including patient-centered, interdisciplinary and self-management strategies.
How Can Nurses Provide Safe Pain Management?
Remove Barriers to Effective Pain Management
Several barriers exist that can impact effective pain management. Nurses can overcome these barriers by transforming their practice to eliminate key problems that interfere with adequate pain control.
1) At the clinical institution level, interdisciplinary teams can develop best practices for pain management, treatment plans and drug prescriptions.

2) Individually, nurses should expand their education by attending conferences, searching for current evidence-based practices via professional literature, and taking additional coursework (CEUs) on opioid prescription best practices. Best practice should include an interdisciplinary focus that includes mental health, behavioral health, and complementary or alternative pain management approaches.
3) Nurses must remain diligent to avoid cultural or societal stigma for those who report pain. It is our duty and responsibility to treat pain to promote an optimal quality of life and reduce suffering. Likewise, we must be cognizant that patient cultural barriers might exist that could impede the patient’s willingness to discuss pain.
4) Costs of pain management can be a barrier, particularly if we recommend or order treatment plans other than drug management. Some insurances will not pay for alternative or complementary medicine options, mental health services, or other care modalities outside drug regimens. Anti-inflammatory herbals may be useful, but not if the patient cannot afford these expensive nutritional supplements. Even rehabilitation services such as PT may be limited under many insurances and Medicare plans.
All 50 states have developed PDMPs. Access to PDMPs may determine if the patient has a history of using multiple doctors, frequent ER visits, or demonstrates other evidence of prior drug abuse such as frequent opioid prescriptions. The PDMP also records primary care prescription activity. It is the provider’s responsibility to know all state regulations and required reporting. Unfortunately, inconsistent data collection and non-standardized regulations have created confusion for providers and thus have not been as effective as hoped. Worse, in some cases, these regulations have thwarted some primary care providers’ desire to order opioids, which have caused fears that some patients’ pain management needs are not effectively met which could lead to patients seeking illicit pain relief strategies.
Other state or federal guidelines. To curb abuses, states mandate physical assessments prior to prescribing an opioid drug. To protect the public, prosecution immunity is enacted for citizens who attempt to assist a person who may have overdosed. Drug disposal, community education, and expanded naloxone distribution are other safety mechanisms set forth by legislation.
Nurses obtain thorough patient histories and should verify injury by usual diagnostic assessments. Assessments should include level and intensity

of pain; pain relief measures; how pain interferes with quality of life, such as its impacts on physical and psychological function; household support systems; and if pain is interfering with work, home relationships, mood, sleep, exercise, leisure activities, or food consumption.
Information from family members, the patient interview, and a thorough assessment include screening tools to define the patient’s addiction risks. Low-risk patients would receive the usual amount of monitoring and follow-up. As the risk increases, the level of monitoring and frequency of follow-up visits increase. Monitoring could include pill counts and urine drug screens. Higher risk patients should be referred to pain management clinics and always receive short acting opioid formulas.
Based on the patient’s history and family member accounts, the nurse determines if the patient demonstrates or verbalizes behaviors that might suggest high risk for drug addiction or abuse. Behaviors that might suggest a problematic return to normal daily activities include daytime sleeping instead of night; lack of usual family involvement and interactions; decreased appetite; poor hygiene and appearance, mood swings or volatility; and impaired functioning due to potential effects of drug use.
The decision to continue, alter, or stop opioid drug regimens is based on the patient’s progress in meeting treatment plan objectives while avoiding adverse behaviors suggestive of overdose or diversion. Satisfactory plan of care outcomes are improving pain levels, function, and quality of life.
Opioid Prescription Patient Education by Nurses
1) Take opioid as prescribed, noting the importance of sticking with the dose regimen. Patients should know what to do if they miss a dose or if pain is not managed by the recommended doses.
2) Remind patients that the medication should not be crushed or chewed.
3) Warn patients of the dangers of using CNS depressants, including sedatives, alcohol, or illicit drugs.
4) Reinforce the fact that due to the addictive nature of the drugs, discontinuation should be accomplished by tapering the drug’s dosing with primary care provider assistance.
5) Drugs should never be shared. To avoid diversion, opioids should be locked up in a secure location.
6) Potential side effects include death due to respiratory depression.
7) The drug could impact one’s ability to drive, operate machines, or affect balance that could cause falls.
8) Instruct the patient on safe disposal of unused opioids. Many senior centers or primary care offices are depositories for unused drugs.
Community awareness. Nurses are often instrumental in providing community education. These educational sessions might be in schools, at hospitals, senior centers, or at other community locations. All aspects of opioid safety should be taught to interested key community members to heighten awareness. Naloxone. Release of Naloxone (Narcan) toolkits to the general public, families of those who use opioids, and patients themselves has increased in the US over the last few years. These life-saving kits do not treat overdoses of benzodiazepines, stimulants, or barbiturates but do reverse the effects of opioids, including heroin and fentanyl, when the first symptoms of respiratory arrest or coma occur. Since 2019, Narcan can be dispensed for Tennessee individuals at risk of opiate-related overdose.
Conclusion

The ANA advocates for all RNs, APRNs and NPs to practice in the fullest extent of their education and practice authority for the implementation of patient treatment plans and access to care to combat pain and the opioid crisis. The ANA promotes care delivery instead of litigation or legal actions against those who have fallen victim to this national epidemic.
Reprinted with permission from Illinois The Nursing Voice, June 2021 issue
The idea that gender is binary (male or female) and determined at birth predominates Western cultures. However, research evidence and lived experiences suggest that gender exists on a spectrum with many options. Some people identify as a gender different from their gender determined at birth (Deutsch, 2016). Our traditional understanding of gender, based on chromosomes and primary (genitalia) and secondary sex characteristics, is often called biological sex or gender (or sex) assigned at birth. Gender identity, on the other hand, is the innermost concept of self as male, female, a blend of both, or neither (Lambda Legal, 2016.).
The majority of people are cisgender, which occurs when gender assigned at birth and gender identity are the same. However, the best available data suggest that approximately 1.4 million adults do not self-identify with their gender assignments (e.g., someone assigned female at birth but identifies as male) (Flores et al., 2016). Transgender is an umbrella term for this population. A visibly growing segment of the U.S. population does not identify with the binary notion of gender. Nonbinary is a collective term for this population, but individuals may use terms such as genderqueer, gender fluid, or gender non-conforming.
There is no standard or correct way to be (or be seen as) transgender. Some people who are transgender choose gender-affirming hormone therapy to achieve masculinizing or feminizing effects; others do not. Surgery that revises genitals to conform to gender identity is a critical part of the transition for many people who are transgender (Deutsch et al., 2019). Others do not feel that genital surgery is a necessary part of transition but may opt for non-genital surgeries to produce desired characteristics, including breast augmentation or removal and body contouring procedures. In other words, the importance of therapy related to the quality of life varies by individual. Also, some people who are transgender may want these services but do not have access to them because they are (a) unavailable in the community; (b) not covered by insurance (even if the individual has insurance, and many do not), and (c) too expensive.
Remember: there is no one way to “be” transgender or cisgender. People choose to express their gender identities in personally satisfying ways, which may or may not match social expectations of what it means to look and behave as a male or female. Some transgender women choose not to wear makeup or dresses, and some cisgender men choose to wear their hair long and earrings.
Negative attitudes and discrimination toward the transgender community create inequalities that prevent the delivery of competent healthcare and elevate the risk for various health problems (Grant et al., 2011). In comparison to their cisgender counterparts, people who are transgender experience higher incidences of cancer, mental health challenges, and other health problems (Department of Health & Human Services, n.d.). For instance, transgender women, compared to all other populations, are at the highest risk of injury from violence and death by homicide. People who are transgender are also more likely to smoke, drink alcohol, use drugs, and engage in risk behaviors (Institute of Medicine, 2011).
Furthermore, discrimination and social stigma increase poverty and homelessness in people who are transgender (Safer et al., 2017). The inability to afford basic living needs may lead to employment in underground economies, such as survival sex work or the illegal drug trade, which place the person who is transgender at an even higher risk for violence, drug use, and sexually transmitted infections (Deutsch, 2016).
People who are transgender are more likely to rely on public health insurance or be uninsured than the general population. Even those insured report coverage gaps caused by low-cost coverage that does not include standard services for preventative, behavioral health, or
gender-affirming therapies, including hormones (Deutsch et al., 2019). Lack of access to comprehensive health care leads some people who are transgender to seek hormones from the community and social networks without clinical support and monitoring, putting them at additional risk for adverse reactions and complications.
Researchers suggest that healthcare providers’ inability to deliver supportive and competent care serves as a powerful mechanism underlying health disparities (Fenway Institute, 2016). The experiences of people who are transgender are often not included in healthcare provider diversity and inclusiveness training. While transgender-related content in health professions basic education programs would effectively improve provider knowledge, skills, and attitudes, transgender health has not been prioritized in nursing education. The result is a nursing workforce inadequately prepared to care for people who are transgender (McDowell & Bower, 2016).
Nursing Care of People Who Are Transgender Competent, supportive transgender care requires nurses to recognize potential biases and understand gender that may differ from their current beliefs and social norms. Honest reflection on these feelings is an essential step in providing competent transgender care. Using a lens of cultural humility, where cisgender nurses acknowledge that they do not adequately know about being transgender while also being open to learning, is helpful. In this spirit, open, transparent inquiry on the part of nurses when they do not know something (When I speak to your children, what name should I use to refer to you?) or how to proceed with care (I need to place a catheter into your bladder, and I know you have had gender-affirming surgery. Do you want to give me any special instructions?) can build trust.
While gender-affirming care such as hormones, androgen-blocking agents, and surgeries require specialist care management, nurses will encounter transgender patients in all healthcare areas. Assessing the history and current status of gender-affirming therapies is critical to inform safe care. For example, hormone-induced changes in muscle and bone mass, along with menstruation or amenorrhea, can alter gender-defined reference ranges for laboratory tests such as hemoglobin/hematocrit, alkaline phosphatase, and creatinine (Deutsch, 2016). Nurses should consider the gender assigned at birth (especially if it is the only gender information to which the lab has access) and gender-affirming therapy-induced physiological changes to make valid inferences about lab values. Nurses should also ensure that a complete history of the use of hormones and androgen blockers (including those obtained from non-licensed providers) is taken. Nurses should work with other providers to ensure that hormone therapy does not stop with hospitalization unless contraindicated by current pathology or prescribed medications. Abrupt cessation of hormone therapy can have a significant and negative impact on emotional and physiological health.
Professional nurses can play a crucial role by advocating for policies and processes that promote safe, effective, and supportive care for people who are transgender. Misgendering a patient (making an incorrect assumption about gender identity) can cause emotional distress and erode patient-provider trust. Unfortunately, electronic health records (EHR) often do not support competent care for people who are transgender. For instance, healthcare providers should use a 2-step gender identification process (Deutsch, 2016). However, many do not, and EHR systems rarely provide prompts for the processor space for easy documentation and access to information derived from the process. Asking about a patient’s current gender identity can result in several responses. The EHR should make checkboxes for a reasonable number of those responses, including male, female, transgender male, transgender female, and nonbinary. A fill-in-the-blank is needed for other identifies. The gender assigned at birth also requires options beyond male or female; people born with external genitalia, gonads, or both that do not conform to what is typically male or female (intersex) may have been identified incorrectly at birth. The EHR should provide an intersex option to this question. Some people
who are transgender are uncomfortable revealing gender assigned at birth, so decline-to-state should be another option. Note that this process should be the standard for all patients, not just those assumed to be transgender. People who are transgender may use names other than their legal names (Lambda Legal, 2016). Navigating a legal name change is complicated and costly. Some people who are transgender do not have the resources for a legal name change; for others, it may not be safe, given current social or legal circumstances. Using a patient’s chosen name and pronouns is critical to patient-centered care. The EHR should prominently document the patient’s chosen name and pronouns, which should also be used outside the EHR, including for appointments and prescriptions. Patients should only have to provide the information once, decreasing the need to correct providers and improving patientprovider relationships. EHRs should also contain an organ inventory, perhaps as part of surgical history, as providers will need to know about the presence or absence of reproductive and gonadal organs to inform clinical decision-making. This information must be clear, unambiguous, and easily accessible in the EHR to inform care and prevent medical and surgical errors.
Nurses should work within governance processes to ensure that all institutional policies support transgender patients, staff, and visitors. Nondiscrimination statements should include gender identity. Policies about restrooms and staff changing rooms (usually labeled in genderbinary terms) should state that a person’s gender identity rightly determines the room to be used and that that right should not require any proof (e.g., health provider confirmation) related to gender or gender identity. Finally, clear guidelines concerning non-private room assignments should include assigning roommates based on gender identity rather than gender assigned at birth.
The ANA Code of Ethics obligates nurses to practice “compassion and respect for the inherent dignity, worth, and unique attributes of every person” (ANA, 2015, para 1). While some nurses may intentionally discriminate against people who are transgender, it is more likely that a lack of knowledge and experience leads to nursing actions that result in suboptimal care. Nurses play critical roles in transgender care by (a) providing supportive, affirming care, (b) creating an inclusive environment, and (c) leading interprofessional teams toward genderaffirming care. Education and a commitment to understanding the lived experiences of people who are transgender is, therefore, essential for all nurses.
References
American Nurses Association. (2015). What is the nursing code of ethics? https://nurse.org/education/nursing-code-ofethics/
Department of Health and Human Services, Office of Disease Prevention and Health Promotion. (n.d.). Healthy people. Lesbian, gay, bisexual, and transgender health. https:// www.healthypeople.gov/2020/topics-objectives/topic/ lesbian-gay-bisexual-and-transgender-health
Deutsch, M.B. (2016). Guidelines for the primary and genderaffirming care of transgender and gender nonbinary people (2nd ed.). Center of Excellence for Transgender Health, University of California at San Francisco. https:// transcare.ucsf.edu/sites/transcare.ucsf.edu/files/ Transgender-PGACG-6-17-16.pdf
Deutsch, M.B, Bowers, M.L., Radix, A., & Carmel, T.C. (2019). Transgender medical care in the United States: A historical perspective. In J.S. Schneider, V.M.B. Silenzio, & Erikson-Schroth, L. (Eds.). The GLMA Handbook on LGBT Health (1, 83-131). Santa Barbara, CA: Praeger. Fenway Institute, National LGBT Health Education Center. (2016). Providing inclusive services and care for LGBT people. https://www.lgbtqiahealtheducation.org/ publication/learning-guide/
Flores, A.R., Herman, J.L., Gates, G.J., & Brown, T.N.T. (2016). How many adults identify as transgender in the United States? UCLA School of Law, William Institute. https:// williamsinstitute.law.ucla.edu/publications/trans-adultsunited-states/
Grant, J. M., Mottet, L. A., Tanis, J., Harrison, J., Herman, J. L., & Keisling, M. (2011). Injustice at every turn: A report of the National Transgender Discrimination Survey. https://www. transequality.org/sites/default/files/docs/resources/ NTDS_Report.pdf
Institute of Medicine. (2011). The health of lesbian, gay, bisexual, and transgender people: Building a foundation for better understanding. http://www. nationalacademies.org/hmd/Reports/2011/TheHealth-of-Lesbian-Gay-Bisexual-andLambda Legal. (2016). Transgender rights toolkit. https:// www.lambdalegal.org/issues/transgender-rights
McDowell, A. & Bower, K. (2016). Transgender health care for nurses: An innovative approach to diversifying nursing curricula to address health inequalities. Journal of Nursing Education, 55(8), 476-479. DOI 10.3928/01484834-20160715-11
Safer, J. D., Coleman, E., Feldman, J., Garofal, R., Hembree, W., Radix, A., & Sevelius, S. (2017). Barriers to health care for transgender individuals. Current Opinion in Endocrinology, Diabetes, and Obesity, 23 (2), 168-171. DOI: 10.1097/ MED.0000000000000227
Singh, S., & Durso, L. E. (2017). Widespread discrimination continues to shape LGBT people’s lives in both subtle and significant ways. Center for American Progress. https://www.americanprogress. org/issues/lgbt/news/2017/05/02/429529/ widespread-discrimination-continues-shape-lgbtpeoples-lives-subtle-significant-ways/
Northwest Sherry Adams
Michele Barclay
Monica Barfield
Lisa Barton
Irina Born
Lesleigh Clinton
Jenny Defee
Andrew Finkelstein
Alexandria Folsom
Donna Fowler
Sharon Hamilton
Love Hawkins
Julie Holmer
Dolores Holtmann
Katie Kennedy
Kimberly McIntosh
Stacy Oliaro
Michelle Peterson
June Phillips
Soraya Quintana
Enita Schmucker
David Smith
Audrey Smith
North Central
Chloe Abolverdi
Jennifer Archuleta
Ashley Badal
Megan Borden
Melissa Brown
Melissa Buchkovich
Heather Burke
Jamie Burrow
Chelsey Campbell
Sarah Cates
Kelly Chewning
Jennifer Croft
Faith Cruz
Chante’ Fletcher
Denise Forbes
Jessica Gage
Aileen Grant
Tara Haines
Brittany Haynes
Tricia Hendrickson
Erika Hernandez
Amanda Hill
Brenda Hogan
Amy Hopping
Lashana Jones
Tiffany Klein
Elaine Lagasse
Stacie Lilly
Brad McLaughlin
Tatiana Petithomme
Lori Phelps
Sapheria Pollard
Lindsey Poole
Joseph Pozdol
Cassandra Rivera
Angela Santiago
Chloe Siple
Lara Thompson
Northeast Alaina Allen
Josmine Bernadin
Tonya Brown
Paula Chamberlain
Tina Dalessandro
Zachary Dismer
Sona Dolsenhe
Bienvenida Doyle
Erica Elek
Sarah Firmin
Rebecca Fischer
Patricia Flanagan
Morghan Gaskill
Jillian Gutierrez
Tara Herndon
Tina Hollie
Pamela Hosch
Deborah Huffman
Antoinette Jackson
Amanda Kreuter
Regina Lancaster
Mary Leen
Heather Leonardy
Margaret McDonald
Mayuko Mondestin
Kathy Neely
Vasudeva Olsen
Taylor Oppermann
Emily Poloji
Nicole Potter
Rebecca Ricchi
Marco Rodriguez
Samantha Schneider
Kelly Segars
Shannon Stone
Renae Vaughn
Christy Wagner
Tina Williams
Christy Wright
East Central
Jennifer Abreu
Amanda Acevedo
Myrna Aloma
Mary Amusu
Chantal Archer
Josephine Avecilla
Valerie Babino
Rachel Baird
Sarah Beck
Courtney Bernard
Kathryn Boufford
Karen Bova
Marcia Bygrave
Kathryn Carpenter
Michaela Chua
Luis Collazo
Dawn Collier-Hezel
Jennifer Conaway
Michelle Cornell
Elsa Dandridge
Magdala Desrosiers
LaToya DeSuze
Sharon Dudley-Wilken
Julius Erezih
James Ferencsik
Ivelisse Fontanez Rivera
Sophia Fouche
Cindy Freeman
Courtney Garrison
Kathy Jo Gearhart
Leslie Gomillion-Cushing
Amanda Hartz
Magali Aiko Hashimoto Khan
Lincoln Haynes
Keshia Henry
Nicholas Husain
Lys Ice
Kimberly Irby
Jennifer Jean-Louis
Raymonda Johnson
Sharon Jones
Verkeitta Jones
Natassia Jones
Tanisha Khan
Joseph Knapp
Patricia Knight
Amanda Kurtz
Pamela Lazarus
Kusuma Lott
Serena Lucas
Manoucheka Luzincourt
Ahkira McPherson
Diane Meadows
Judy Meyer
Melanie Miller
Angela Delfina Mitra Perez
Maxine Moul
Rosana Narvaez Colon
Louis Ngerem
Natacha Nicholas
Aiza Nimeh
Theresa Noel-Belasco
Candice Omega
Marcela Paba Lerma
Kathleen Patanaude
Kimberly Peck
Kathleen Perillo
Susan Perry
Suzanne Pettko
Eric Pineiro
Jean Arlie Nina Quinones
Brinda Raju
Johanna Rodriguez
Dianne Ross
Shazia Sadler
Nancy Sanchez
Amy Schumacher
Katharine Sinnett
Debra Stevens
Rose Thompson
Jeanne Tracy
Kathleen Washburn
Yvonka Williams
Corinne Wilson
Elizabeth Wind
Patricia Yorgan Lai Zaporteza
West Central
Tiffany Aceituno
Marie Akers
Barbara Anderson
Quarshiwaa Asante
Danielle Baldwin
Beverly Bokovitz
Winsome Brown-Ellington
Melissa Bryant
Patricia Burland
Paulette Burton
Amy Card
Ma Luz Chavez
Jennifer Chouinard
Coleen Clark
Abigail Cobarras
Edgar Dadural
Mary Beth Darling
Cynthia Deveaux-Moona
Laura Devore
Merline Duclos-Ukwute
Linda Fagan
Christine Fechter
Joyce Gagliardi
Jennifer Garcia Flores
Brenda Gerst
Nicholas Gilman
Tasha Goff
Pedro Luis Gomez
Evgeny Gorobtsov
Jennifer Grinder
Kristen Hamilton
Brittany Hartup
Rachel Hermann
Joyce Hudson
Mindy Huynh
Franjesca Jackson
Cresha Jaurequi
Nicole Johnson
Melissa Joiner
Jazmin Jones
Nia Joseph
Vivian Kaiser
Cherie King
Kristine Konstantakos
Nicole Krier
Jolyn Lambert
Catherine Landrigan
Meagan Leddy
Leigh Linsenman
Cynthia Little
Joy Magnan
Monica Malone
Nimmi Maxmillian
Gina McCabe
Angela McDowell
Christen McNew
Shannon McQueeney
Omayra Merced
Melissa Miller
Oonagh Nechodom
Grant Neeley
Kenya Nelson
Gina Norris
Leah Olson
Oluwaseyi Omaivboje
Chelci Owen
Iris Pagay
Jessica Perez
Deborah Proscia
Rayna Rios
Henry R Rivera
Callie Rivera
Joyce Saba
Icel Janell Sabino
Alyssa Schafer
Anastasha Schon
Heather Shipp
Lia Sierra
Sarah Steinmetz
John Sullivan
Norma Thermidor
Chelsie Thibault
Kimberly Timmons
Katherine Vance
Teresa Walling
Amber Williams
Walter Wills
Southeast
Nicole Aguila
Patrick Amorelli
Marie Antoine
Maureen Avella
Oscar Azmitia
Constance Baskin
Vennessa Beaumont
Deborah Bennett
Clarissa Blackshear
Nancy Bourg
Michelle Broadbent
Tsobi Brown
Roxana C Reyes
Lystra Chang
Tammy Chaundy Bajhia Chong
Sara Corwin
Lisa Cox
Nicole Crocker
Caitlin Dade
Valentine Dantes
Gisella Dejesus
Heidi Delcourt Calhoun
Ashley Demorcy Hutchins
Marie Desire
Sanya Diaz
Keithnora Edmond
Fedora Elipe
Rahonie Evans
Michelle Fergus
Virginia Garner
Charla Giles
Sheri Grisso
Brooke Harper
Chris Held
Crystal Jackson
Patricia Jones
John Kramer
Olivia Labrador
Maureen Laimann
Ashley Lannon
Heather Loguidice
Jessica Lopez
Judith Louis
Christina McDeavitt
Grisel Medina
Luciene Mendonca-Cali
Angela Mennie
Thomas Moran
Dyana Moro
Beatrice Murillo
Priscilla Nagbuya-Potestades
Nicola Notice
Susan Peak
Marie Pestana-Garcia
Stanley Polich
Hannah Rabinowitz
Andres Ramirez
Jean-Joseph Rendel
Yolanda Rivera
Jonnell Robinson
Cookie Romeo
Anna Mora Rosen
Farah Sajous
Jean Santaguida
Betty Taylor
Leandro Tejeda
Elizabeth Timmer
Laura Turscak
Brooke Van Nice
Onelis Vega
Emma Viets
Kaydeion Watson
Bonnette Webb
Devon Weiss
Erica Zuniga
Southwest
Ronya Ahmad
Marcela Alvarez-Lazo
Jose Arroyo Ferrer
Cari Barbuto
Jennifer Barr
Julie Best
Jessica Bundy
Stacee Burton
Jacqueline Carlson
Erin Carr
Magdala Chavarria
Donna Ciggia
Danielle Collado
Daniel Creel
Laura Jacobson
Troy Kilpatrick
Devon Lilly
Kathleen McGowan-Anthony
Ana Montane
Marguerite Natoli
Felicia Noland
Sandra R
Judith Rinella
Kelly Rios
Rachel Ross
Ashley Ruffing
Lori Schloegel
Hunter Spencer
Debra Stewart-Delancy
Erika Stone
Carol Swaby
Jennifer Weightman
Lisa Wilson
Beverly Wiltshire
Monica Woodward-Luberto
Brandon Young
South
Michael Akinsoji
Krystle Allegue
Andy Aramburo
Carlos Arteta Higgins
MahalahLouse Batto
Jacqueline Beckford
Jonnell Beckles
James Begert
Melissa Benitez
Beverly Best-Lewis
Dianez Canto
Loisses Casanova
Cassandre Castor
Nastacia Chambers
Marie Charleston
Jessica Colangelo
Jessie Constant
Brenda Cooper
Lilia Corral
Daniela Coto
Jennifer Davis
Kayla Delahunty
Myriam Denose
Karina Diaz
Meilin Diaz-Paez
Johanne Domond
Nicole Duncan
Jean Emile
Saily Estopinan
Teresa Fernandez
Jennifer Fernandez
Samantha Fonte
Brenda Francis
Odalys Gamarra
Genesis Garcia
Nancy Gaspard
Alexander Gil
Missilia Gilbert
Diana Gomez
Gilma Gonzalez
Kimberly Graham
Ingrid Hernandez
Alyssa Hidalgo
Rochelle Hockaday
Katelyn Horan
Jami Horvat
Maniela Jean
Yvette Jeffrey
Tammy Jenkins Raleigh
Rani John
Trudian Jones
Janessa Lau
Andrea Liguori
Jennifer Lucy
Maday Marin Mees
Sophie Martinez Lopez
Eshia McLymont
Michael Montes
Jessica Moreda-Cardenas
Elizabeth Noriega
Henry Olivera
Jola Onime
Esther Oyetunji
Briana Padron
Monique Prosper
Colleen Quinn
Sapna Rao
Debbie Raymond Lucienne Reese
Fania Reyes
Jamie Rhatigan
Gudelia Rhoades
Lerae Richardson
Arelis Rivera
Gabriel Rojas
Ally Rosenberg
Christopher Rosselot
Natalie Rufin
Lydie Saintfenix
Joanna Santa Ana
Monica Sedano
Santana St. Remy
Clenette Surpris
Charline Tebeu
Jienne Torres
Lissete Vega
Lony Vega
Jessica Vera
Brenda Villalobos
Robert Weiss
Keithlyn Wharwood
Angela Wilson
Leydi Wohlfeld Ivet Yong
Other
Jean Dazulma
Katerina Gradeva
Sabrina Walden
Tammy Williams
Corinne Laberdee

