Radiology & The Environment
New Data on Lung Cancer
Energy Saving Radiology Practice
A Journey from Ukraine to Spain

Summer 2023 ALL ABOUT DIAGNOSTIC IMAGING Image: © Javier Aramendia
Dear reader,
the climate emergency is pushing us all to rethink the way we live and work to reduce our carbon footprint and help save our world.
The healthcare sector alone generates approximately ten percent of the total carbon emissions in the United States, recent data showed. Radiology is believed to be a top contributor to this footprint due to its high energy-consuming devices and waste from interventional procedures.
So much can and should be done to minimize radiology’s impact on the environment. The industry is now creating narratives around sustainability, which features prominently on every meeting’s program.

RSNA 2022 set the tone with its Opening Lecture, in which Professor Reed A. Omary from Vanderbilt University Medical Center in Nashville, Tennessee, made a passionate plea for radiologists to step outside the confines of their specialty to promote the health of the planet.
ECR 2023 abundantly delved in the topic, and speakers explored strategies to reduce environmental pollution after, for example, contrast-enhanced examinations.
This contamination of the aquatic environment is a growing concern. In Germany, about 200 kilograms of contrast media are being released in the Rhine river every day, so 70.9 tonnes per year.
More recently, ESGAR 2023 also took the plunge, as Dr. Daniel García Párraga from the Valencia Oceanographic in Spain explained how radiologists could help preserve aquatic species.

Some radiologists actually took steps to reduce their carbon footprint years before sustainability became a burning issue.
Prof. Martin Klein from Burbach in Germany started his green practice a decade ago, and has since managed to save 85 percent off his practice’s heating costs, by using his MRI scanner as an alternative energy source.
2 DI EUROPE · SUMMER 202 3 EDITORIAL
Image: © The Little Hut · stock.adobe.com
Back to the future with new data on lung cancer
Seeing Michael J. Fox in Berlin in June was an electrifying experience and made us feel like traveling back in time, when radiology workstations looked like science-fiction starships designed in the 1960s. But radiology is essentially about looking towards the future. So we focused on cutting-edge technologies such as photon counting CT, and asked a vendor how they face the rising demand for those special detectors, whose fabrication relies on growing cadmium telluride crystals.
We spoke with Dr. Julia Camps-Herrero, who is responsible for the coordination of five breast units in Spain, about her experience with contrast-enhanced mammography, a relatively new technique.
On the topic of women’s health, initial results of an ongoing trial in France are pushing researchers to raise the alarm in lung cancer screening. Women are two to three times more at risk of developing lung cancer, emerging data from the CASCADE trial suggests. Prof. Marie-Pierre Revel from Cochin Hospital in Paris told us more in an exclusive interview. We also assessed the current state of lung cancer screening programs across Europe with Prof. Hans-Ulrich Kauczor from Heidelberg,
Germany, who is the scientific coordinator of the Strengthening the screening of Lung Cancer in Europe (SOLACE) project.
Following the holistic trend in medicine, we looked beyond radiology and attended ESTRO, the annual congress of the European Society for Therapeutic Radiology and Oncology, in Vienna; EACVI, the first unified multi-modality meeting of the European Association of Cardiovascular Imaging, in Barcelona; and EAN, the annual meeting of the European Academy of Neurology in Budapest.
And because we cannot forget about the war waging at our gates, we followed the journey of Anna Smolova, a Ukrainian radiation therapist who arrived in Spain a year and a half ago.
I hope you will enjoy our summer issue. Have a wonderful holiday and see you in September at CIRSE in Copenhagen and EUSOBI in Valencia!

3 DI EUROPE · SUMMER 202 3
Mélisande Rouger, Editor and Publisher
Image: © kittipon stock.adobe.com
IMPRINT
Excecutive Editors
Mélisande Rouger

m.rouger@dieurope.com
Guido Gebhardt
g.gebhardt@dieurope.com
Senior Editor
Alan Barclay PhD
a.barclay@dieurope.com
Article reprints
g.gebhardt@dieurope.com
6 14 22
6 Women Two to Three Times More Likely to Develop Lung Cancer
10
Disclaimer
The information and opinions expressed in articles and product entries published in DI EUROPE are solely those of the manufacturers / companies, their authors and contributors, for which the publisher holds no responsibility.
All trademarks, product names, company names and logos in this publication are the property of their respective holders. Users must obtain permission from those holders before copying or using the owner’s trademarks, product and company names or logos.
DI EUROPE is published by Mélisande Rouger
Juan Duque 7 5C
28005 Madrid · Spain & Guido Gebhardt
Adalbert-Stifter-Weg 2 b
85661 Forstinning · Germany
phone +49 1511 5674833
g.gebhardt@dieurope.com
© 2023 DI EUROPE
All rights reserved.
Reproduction in any form is prohibited without permission of the publisher.
DI EUROPE
Initial results from a French trial show that the risk of developing lung cancer is much higher than expected in female smokers.
What if We Could Fundamentally Improve Lung Cancer Care?
The European Council updated its cancer screening recommendation and member states should now explore the feasibility of lung screening with low-dose CT, expert believes.
12 AI Improves the Detection of Lung Nodules on Chest X-rays
While many pulmonary nodules may be benign, they can also represent potentially life-threatening cancers. Timely identification is vital.
14
A Journey from Ukraine to Spain
Anna Smolova left her country soon after the Russian invasion. Through her journey, we looked at the impact of the war on Ukrainian healthcare.

18
How Radiology Helps Preserve Aquatic Species
Sustainability took center stage at ESGAR 2023, as a zoologist highlighted how radiology could help in the conservation of aquatic species.
20
ESGAR 2023 in Video
Watch or re-watch our interviews conducted during the 34th annual meeting of the European Society of Gastrointestinal and Abdominal Radiology.
22 Pioneer in Energy Saving Radiology Practice Shares Tips
Rising energy costs are a problem for radiology practices. A German radiologist explains how MRI could be used as an alternative energy source.
24 Reducing Environmental Pollution after Contrast-Enhanced Scans
Radiologists called for action to reduce the release of contrast media in hospital wastewater after contrast-enhanced examinations at ECR 2023.
28
Memory Lane: PACS in the 1990s
Guido Gebhardt takes on his time machine and travels back to radiology technology last century.

DI EUROPE · SUMMER 202 3 CONTENT
Layout & Graphic Design Christoph Muschiol Germany christoph@muschiol-online.de Index of advertisers all MRI 5 Bayer 41 Cirse 47 deepc 21 ECR 33 EUSOBI 17 EuSoMII 27
30 Every Photon Counts
Siemens Healthineers is building a new factory to grow cadmium telluride crystals and match the rising demand for photon-counting CT.
34 AI Can Predict Future Brain Changes in Elderly Patients
Software can predict brain development up to six years after initial assessment of Alzheimer’s disease on FDG-PET scans, new research shows.
36 CEM: the Experience of a Large, Progressive Spanish Hospital Group
We talked about the role of contrast-enhanced mammography (CEM) in breast imaging with Dr. Julia Camps Herrero from the Ribera Salud group.
42 Expediting Workflow with Large Language Models
One of the major issues in radiology is the integration of structured reporting into the radiological workflow, a time-consuming and cumbersome task, according to many.

44
Brain Health Takes Centre Stage at EAN 2023

Neurologists expressed concern about the steeply rising prevalence of brain diseases worldwide during the meeting of the European Academy of Neurology.
48 The Changing Face of Cardiology and Imaging’s Role


Cardiology is undergoing massive changes as prevalence of cardiovascular disease continues to increase while resources decrease, a prominent cardiologist explains.
50
Companies Unveil New MSK Solutions at ESSR 2023
Manufacturers and AI software developers presented their products to image musculoskeletal (MSK) disorders, the leading contributors to disability worldwide.
52 ESTRO 2023: Newest Advances in Tumor Movement Detection
How radiotherapy strives to network the entire spectrum of cancer treatment to enable more efficient and individualized therapy in inpatient and outpatient care.
5 DI EUROPE · SUMMER 202 3 24 34 42
www.allmri.com Südstraße 23 · 74226 Nordheim Telefon: +49 71 33 / 23 70 220 · Telefax: +49 71 33 / 20 48 47 mail@allmri.com Accessories for Magnetic Resonance Imaging
“ The MRI specialist dealer that I trust”

6 DI EUROPE · SUMMER 202 3 LUNG CANCER Image: © SciePro stock.adobe.com
New data on lung cancer
Women Two to Three Times More Likely to Develop Lung Cancer
Momentum for lung cancer screening is building in Europe, as projects to boost the implementation of national programs are underway and emerging research suggests that women might be two to three times more at risk of developing the disease than men.
By Mélisande Rouger
A long awaited response to the global burden of lung cancer may soon be given, as evidence that low dose CT screening could drastically reduce mortality is piling up, especially in women with a history of smoking. Initial results from the CASCADE clinical trial in France 1 indicate that the risk of developing lung cancer is much higher than expected in female smokers, according to Prof. Marie Pierre Revel, head of the radiology department at Cochin Hospital, University of Paris.
“One year into the study we observe that, at equal tobacco consumption, cancer prevalence
in women is two to three times higher than in men, and more than double to results obtained in previous trials like NELSON,” said Revel, who is the principal investigator of the CASCADE (lung CAncer SCreening in French women using low-dose CT and Artificial intelligence for DEtection) trial.
The emerging data demands a prompt response in reaching out to potential candidates, i. e. women between 55 and 74 years old who have smoked at least one pack of 20 cigarettes per day for 20 years.
“If our study confirms that the risk to develop lung cancer is three times higher in women, then we need to do everything we can to target this population,” she said.
CASCADE, which is funded by the French Ministry of Health and the French Cancer Institute, was launched to obtain so far lacking data on women, as these were under represented in most lung cancer screening studies, she explained.
“We have a very worrying epidemiological situation in France because women now represent 35 percent of lung cancer patients, compared with 16 percent in 2000. So it’s very likely that lung cancer is the leading cause of cancer death before breast cancer in French women (…) It kills too many women and the lack of perception of the risk is distressing.”

7 DI EUROPE · SUMMER 202 3
Building awareness among healthcare professionals that lung cancer is not just a male disease is paramount to improve patient outcome.
Lung cancer screening in women could be run in parallel to breast cancer screening, Revel suggested. “We would benefit from our collaboration with screening centers and include an invitation letter to the recipients. If they are smokers, we could check their eligibility and decide if they should also be screened for lung cancer.”
Immediate action must be taken to adequately implement lung can- cer screening in France, as a large pilot study to recruit all smokers will be launched by the French National Cancer Institute (INCa) in 2024. The CT scan reading modalities will be based on the recommendations from Revel’s research group.
“I want to urge centers taking part in the program to organize a double reading validated by AI instead of another expert radiologist,” she
said. “It’s easier to screen a population using a single general radiologist trained in lung cancer screening rather than to rely on the barely 200 thoracic radiologists in France.”
The SOLACE project
Lung cancer has the highest mortality of all cancers, more than colon and breast cancer together. The key to improving outcomes is to diagnose patients early, when curative therapy is still an option.
The recommendation from the European Council to explore the feasibility and effectiveness of lowdose CT to screen individuals at high risk for lung cancer, including heavy smokers and ex-smokers, was a big step in that direction, according to Prof. Hans Ulrich Kauczor, medical director of the diagnostic and interventional radiology department at Heidelberg University Hospital, Germany.

“Now we have the opportunity to take all the accumulated evidence
on low dose CT screening and really do something,” said Kauczor, who is the scientific coordinator of the Strengthening screening Of Lung cAnCer in Europe (SOLACE) initiative, an EU4Health project launched under the Europe’s Beating Cancer Plan to facilitate the implementation of screening programs across Europe.
The initiative is in “an exciting phase”, with increased recruiting rates and a pilot project underway in ten countries. “We have a lot of activity in Hungary, Poland, Estonia, Czech Republic, France, and Germany. In Croatia, the national lung cancer screening program is living up to its reputation,” he said. “In Ireland things are moving a bit slower and Spain is taking steps. Greece and Romania are still a little behind, but there’s definitely some progress. Further away, Australia has just recently decided to launch a national screening program.”
Screening can help reduce the burden of lung cancer on health-
8 DI EUROPE · SUMMER 202 3 LUNG CANCER
Positive screening result in a 62-yearold former smoker with a 25 pack-year smoking history. This early stage lung adenocarcinoma was surgically treated and did not require any other postoperative treatment.
Image: © SciePro stock.adobe.com
care systems, especially those who cannot afford expensive treatments such as immunotherapy. “It’s easier to address these countries by showing that lung cancer screening in smokers is cost efficient,” he said.
With current CT scanners, radiation exposure is no longer an issue, he added. “Dose is going down tremendously with new equipment, below 1 mSv, so we will come to a point where radiation exposure in lung cancer screening becomes negligible.“
Successfully implementing screening programs will mean being able to reach out to the populations who are at the highest risk but have traditionally remained far from the healthcare system.
“We will release flyers and messages in the media to reach out to everyone, whether they live in city centers, remote areas or are part of isolated ethnic minorities,” Kauczor said. “We also plan to find ambassadors, i. e.
patients who have benefited from lung cancer screening and can talk about it positively to raise awareness among their communities.”
The gender issue is key and screening is expected to reduce mortality more among women than men, early research shows. “Lung cancer screening may reduce mortality by 30 percent in women and below 20 percent in men,” he said. “The holy grail is trying to reduce general mortality with these programs, and hopefully we will. But we need European guidelines that national policy makers can use to implement these programs, so we have to have a common ground of quality level.”
REFERENCE
1 https://www.lepoint.fr/sante/cancer-du-poumon-2-a-3-fois-plus-de-depistages-positifs-chez-les-femmes-31-05-2023-2522530_40.php
Marie-Pierre Revel is professor of radiology and head of the radiology department at Cochin Hospital, University of Paris, France. She is past president of the European Society of Thoracic Imaging and in charge of the Lung Cancer Screening Certification Program, which is endorsed by the European Society of Radiology (ESR), where she now serves as chair of the communication and external affairs committee.
She is the scientific director of the lung CAncer SCreening in French women using low-dose CT and Artificial intelligence for DEtection (CASCADE), a study funded by the French Ministry of Health.

Hans Ulrich Kauczor is professor of radiology and chairman of radiology at the University of Heidelberg, Germany. He is also medical director of its department of diagnostic and interventional radiology. He is the scientific coordinator of the Strengthening the screening of Lung Cancer in Europe (SOLACE) project and first author of both joint statement papers from the ESR and the European Respiratory Society (ERS) on lung cancer screening.

9 DI EUROPE · SUMMER 202 3
What if We Could Fundamentally Improve Lung Cancer Care?
Lung cancer is the deadliest type of cancer worldwide. It has the highest mortality rate and one of the worst five-year survival rates of all cancers at 17 percent for men and 22 percent for women.1 Because the lungs have no pain receptors, lung cancer usually remains symptom-free for a long time. Patients often only come to the clinic when cancer cells have attacked the lymph nodes or have metastasized. By the time they complain of symptoms like difficulty breathing, the disease is usually far advanced. In stages III or IV, curative therapy is nearly impossible, and the five-year survival rate drops to just five percent.2
One way to reduce lung cancer mortality is to diagnose the disease when it’s clinically silent. There’s strong evidence that with low-dose computed tomography (LDCT) scans, lung cancer can be detected at stage I, where curative surgical treatment is feasible.
Survival improves when lung cancer is detected early
To put it concisely: The earlier the disease can be diagnosed, the better the prognosis for the patient. But screening programs are far from standard in the EU. Sebastian Schmidt knows the reasons: “One of the big concerns is healthcare costs. But there have been many analyses showing that screening costs are significantly lower than what we pay today for late-stage treatments. Another reason is that there have been issues in the past with false positives, which is a commonly mentioned reason for not implementing national screening programs. But there are now guidelines and strategies for solving the problem of false positives. For example, in the UK pilots there are only two percent false positives. You’ll achieve a very, very low rate of false positives if you do it properly.”
DID YOU KNOW? IN THE COUNTRIES OF THE EU, LUNG CANCER RESULTS IN 240,000 DEATHS ANNUALLY. 3
Have you seen the discussion “What can the radiology community do to drive lung screening in Europe?” at ECR 2023 in Vienna?
Photon-counting: Drastic improvements in lung screening
Computed tomography is the imaging method of choice to assist physicians in diagnosing lung cancer.4 However, the diagnostic benefits of lung cancer screening need to be balanced with the inherent risks of ionizing radiation. Screening basically consists of performing a LDCT, which takes five seconds and is painless. But NAEOTOM Alpha, the world’s first photon-counting CT (PCCT) provides up to a 45 percent lower radiation dose compared with conventional CT detectors.5 With higher spatial and contrast resolution of soft tissue and reduced artifacts, PCCT improved the ability to depict pulmonary emphysema and lung nodule borders.6
“A question of political decision-making”
Multiple studies conducted worldwide have consistently demonstrated the benefits of LDCT lung screening.7 To give just one example: England has had screening on a regional level since 2018 and is seeing success with almost three-quarters of the patients in the screening programs diagnosed in stage I or II. Croatia and Poland are also beginning implementation, and pilot projects are underway in countries like Slovakia, Hungary, and Germany. But there are still no
10 DI EUROPE · SUMMER 202 3 LUNG CANCER
?
By the time symptoms appear, only 20 percent of patients will be in an early stage. With screening it’s the opposite: 80 percent of patients will be in an early stage.
nationwide lung cancer screening programs in EU countries.
It was a very important signal for many countries that the European Council updated its cancer screening recommendation. Whereas the previous cancer screening recommendation from 2003 was limited to breast, cervical and colorectal cancer, member states agreed to broaden the focus. Countries should now explore
Learn more about how AI can be used to enhance medical imaging and improve patient outcomes in lung cancer screening.

the feasibility and effectiveness of lung screening with use of low-dose CT.8 “Everything is ready to start,” says Sebastian Schmidt. “The infrastructure is there, the technology is there, and there are training programs for doctors. Now it’s all a question of political decision-making.”
How artificial intelligence supports radiology professionals
But what if the number of examinations increases, but there continues to be a shortage of radiology professionals? AI could then play a critical role by providing a second opinion in diagnostic assessment, because it can help produce faster and more precise results. The AI-Rad Companion Chest CT9 highlights abnormalities and helps radiologists interpret CT images of the thorax. And AI in
REFERENCES
1 https://www.krebsdaten.de/Krebs/EN/Content/Cancer_ sites/Lung_cancer/lung_cancer_node.html (June 2023)
2 https://www.lung.org/lung-health-diseases/lung-disease-lookup/lung-cancer/resource-library/lung-cancerfact-sheet
3 https://ecis.jrc.ec.europa.eu/factsheets.php
4 https://www.cdc.gov/cancer/lung/basic_info/screening. htm
5 https://www.siemens-healthineers.com/press/releases/ naeotomalpha
NAEOTOM Alpha is not commercially available in all countries. Due to regulatory reasons, its future availability cannot be guaranteed. Please contact your local Siemens Healthineers organization for further details.
6 https://journals.lww.com/jcat/Abstract/2023/03000/ Lung_Cancer_Screening_Using_Clinical.8.aspx
7 https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6037972/
8 https://data.consilium.europa.eu/doc/document/ ST-14770-2022-INIT/en/pdf
9 AI-Rad Companion Chest CT consists of several products that are medical devices in their own right. AI-Rad Companion Chest CT is not commercially available in all countries. Its future availability cannot be ensured.
10 The statements by Siemens Healthineers’ customers described herein are based on results that were achieved in the customer's unique setting. Because there is no “typical” hospital and many variables exist (e.g., hospital size, case mix, level of IT and/or automation adoption) there can be no guarantee that other customers will achieve the same results.
conjunction with medical imaging can do much more: A special sequence from Siemens Healthineers calculates patient movements and triggers the acquisition of CT images at the exact moment when conditions are right for the optimal image quality. That helps reduce image artifacts that occur when the patient breathes during an examination.
France is preparing to start a pilot study funded by the Ministry of Health and the National Cancer Institute to evaluate the role of AI in screening. The study will assess the potential of using AI as a second reader of the results. If it shows that the negative predictive value of AI is very high, it would be a good way to simplify screening.10
https://www.siemens-healthineers.com/
11 DI EUROPE · SUMMER 202 3 Advertorial !
All images: sSiemens Healthineers
AI Improves the Detection of Lung Nodules on Chest X-Rays
Typically arising from previous lung infections, pulmonary nodules are very common abnormal growths that form on the lung. While many nodules may be benign, nodules can also represent potentially life-threatening cancers, so timely identification is vital.
By Alan Barclay
Chest X-ray is the imaging modality that is the most widely used in the world, and is one of the common screening methods used for identifying lung nodules – and indeed it is one of the crucial tasks in chest X-rays.
However, detection by radiologists of pulmonary nodules on chest radiographs can be quite challenging, especially when radiologists are experiencing a high volume of cases. 1
Since the adoption of artificial intelligence (AI), several AI-based Computer-Aided Detection (CAD) systems have been developed and have been reported to substantially improve radiologists’ performance in the detection of lung nodules. However, so far these evaluation studies

have all been retrospective, and have several major limitations. For example the retrospective data sets used in the evaluations are often arbitrarily selected to have a disease-enriched distribution. Additionally, the performance tests were typically conducted under conditions where readers could be more focussed and sensitive than is usually possible in real time clinical routine. Finally, proper integration with a PACS system, which is necessary for use in real work place situations, was lacking in the previous evaluation studies.
To address all these issues, a pioneering randomized control trial has been carried out to identify the actual effect that AI based soft-
ware has in real clinical practice on the detection of lung nodules. The results have just been published. 2
The study used a commercially available AI-based CAD software (the Lunit INSIGHT CXR package version 2.0.2.0 from the Korean company Lunit). This was embedded into a commercial PACS system (M6; Infinitt Healthcare). The Lunit INSIGHT CXR software uses a deep learning-based algorithm developed for ten common radiological abnormalities in chest X-rays (pneumothorax, mediastinal widening, pneumoperitoneum, nodule/mass, consolidation, pleural effusion, linear atelectasis, fibrosis, calcification and cardiomegaly). This software has been extensively validated. 3
Workflow of chest radiography interpretation in the clinical trial. In contrast to previous retrospective trials, the AI software was integrated into the PACS workflow, so representing a real-life clincal routine situation. Image reproduced from Ref [2] Radiology, Copyright RSNA

12 DI EUROPE · SUMMER 202 3 LUNG CANCER
Study corresponding author Jin Mo Goo, M.D., Ph.D. Department of Radiology at Seoul National University Hospital and the Cancer Research Institute, Seoul National University, Republic of Korea
(A) Frontal chest radiograph shows a subtle nodular opacity (arrow) in the right middle lung zone.

(B) The lesion was detected by the AIbased computer-aided detection software, with an abnormality probability of 81.1 percent. The designated radiologist reported this chest radiograph as positive.
(C) Axial, noncontrast, low-dose chest CT scan shows a 1.1-cm solid nodule (arrow) in the right lower lobe.
In the recent study to identify the actual effect that AI has in clinical practice, researchers from the department of radiology at Seoul National University Hospital in Korea, included 10,476 patients, who underwent chest X-rays at a health screening center between June 2020 and December 2021.
“As our trial was conducted with a pragmatic approach, almost all enrolled participants were included, which is a real clinical setting,” said corresponding author Dr. JM Goo. Patients completed a self-reported health questionnaire to identify baseline characteristics such as age, sex, smoking status and past history of lung cancer. Eleven percent of the patients were current or former smokers.
The patients were randomly divided evenly into two groups – AI or non-AI. The first group’s X-rays were analyzed by radiologists aided by AI while the second group’s X-rays were interpreted without the AI results.
Solid nodules with diameters either larger than eight millimeters or subsolid nodules with a solid portion larger than six millimeters were identified as actionable, meaning that the nodule required follow-up, according to lung cancer screening criteria.
Results
Lung nodules were identified in two percent of the patients. Analysis showed that the detection rate for actionable lung nodules on chest X-rays was higher when aided by AI (0.59 percent) than without AI assistance (0.25 percent). There were no differences in the false-referral rates between the AI and non-AI interpreted groups. While older age and a history of lung cancer or tuberculosis were associated with positive reports, these and the other health characteristics did not have an impact on the efficacy of the AI system. This suggests that AI may work consistently across different populations, even for those with diseased or postoperative lungs.
Conclusions
The authors concluded that in their randomized controlled trial of 10,486 health checkup participants, comparing performance of radiologists aided by AI versus non-aided radiologists, the AI-assisted group improved the detection of actionable lung nodules on chest radiographs with a similar false-referral rate between the two groups.
“Our study provided strong evidence that AI could really help in interpreting chest radiography. This will contribute to identifying chest diseases, especially lung cancer, more effectively at an earlier stage,” Dr. Goo said.
The researchers plan to conduct a similar study using chest CT, which will also identify clinical outcomes and efficiency of workflow.
REFERENCES
(A) Frontal chest radiograph shows a small nodular opacity (arrow) in the left upper lung zone, which was missed by the designated reporting radiologist.

(B) Axial, noncontrast, low-dose chest CT scan shows a 9-mm solid nodule (arrow) in the left upper lobe. The nodule showed low metabolism at PET and decreased in size at follow-up CT. It was confirmed to be an inflammatory nodule
1 Auffermann WF. AI Nodule Detection on Chest Radiographs Using Randomized Controlled Data: The Effect on Clinical Practice. Editorial in Radiology. 2023; 223186. https://doi.org/10.1148/radiol.223186
2 Nam JG et al. AI Improves Nodule Detection on Chest Radiographs in a Health Screening Population: A Randomized Controlled Trial Radiolog. 2023 Feb 7; 221894. https://doi.org/10.1148/radiol.221894
3 Nam JG et al. Development and validation of a deep learning algorithm detecting 10 common abnormalities on chest radiographs. Eur Respir J. 202; 57(5): 2003061. https://doi.org/10.1183/13993003.03061-2020
13 DI EUROPE · SUMMER 202 3
from Ref [2] Radiology,
Image reproduced
Copyright RSNA
Image
from Ref [2] Radiology, Copyright RSNA
reproduced
Nothing is unattainable
A Journey from Ukraine to Spain
By Mélisande Rouger
She takes a sip from her Martini Rosso, flips her hair and looks me straight in the eye. “I want Ukrainians to have a voice,” says Anna Smolova, a 33 year-old radiation therapist from Sumy, Ukraine.
Smolova is one of the eight million Ukrainian refugees who have been registered across Europe since the Russian invasion of Ukraine last year. She arrived in Spain in Febru-
ary 2022 and started working at the Bizkotxalde Clinic near Bilbao in March 2023, after a long administrative process. “It was complicated,” she remembers. “They kept asking: why can’t you bring your documentation? And I answered: because it’s in a bunker!’’
Smolova had already managed to get her diploma homologated before the war, prompted by a desire
to work abroad. “To be honest, I never thought that this diploma would be useful,” she sighs. “But here you go.” As she waited to have her paper work approved, she volunteered to help other migrants and give them visibility in the public space. “It’s actually my second interview here,” she says in her
14 DI EUROPE · SUMMER 202 3 RADIATION THERAPY
Image: © Tatyana stock.adobe.com
Image:© sldesign1· stock.adobe.com
mellifluous Spanish. “I want to raise awareness of migrants and explain why they had to leave their home.”
Getting out
Her own escape in the early days of the war was not free of danger. Sumy, a city in northeastern Ukraine, is located only 30 kilometers away from Russia.
“The Russian troops were crossing our region and destroying houses, and at the beginning, they were waiting for people to come and collaborate,” she recalls with emotion. “We had been planning our escape for at least ten days, but we were not sure if we were really going to leave or when. It was very risky.”
One morning, she received confirmation that the soldiers had left the streets. “Groups of neighbors
were always watching outside, and communicated with each other using WhatsApp,” she says. “We heard that the Russians were having breakfast, so we took the opportunity and left.”
Smolova left with her then fiveyear-old son and her parents. “I wasn’t working when the war broke out. I wanted to go back to the hospital but there was a lot of chaos after the invasion, so I decided to leave. My dad came back the same day to Ukraine. My husband chose to stay. Both also work at a hospital.”
Compared with other areas of Ukraine, Sumy, although geographically close to Russia, has barely been touched by bombs.
“The Russians tried to bomb our critical infrastructure but missed the marks. They have destroyed a lot of the south and east of the country though. We’ve been lucky we had so many people who wanted to fight back,” she says proudly.
Smolova comes from a family of physicians. Her father is an oncology surgeon and her mother worked as a radiologist for many years. Smolova’s husband is a pediatrician, rescuer and sonographer. “Even my parents-in-law are physicians,” she says laughing.
Smolova trained in Kharkiv and Kyiv, and received her medical degree from Sumy State University, and her degree in radiation therapy from Kharkiv Medical Academy of Postgraduate Education. She worked at the Sumy Regional Oncology Center between 2012 and 2017, with a five-year interruption as part of her maternity leave.

Impact of the war on healthcare in Ukraine
One of the key characteristics of Russia’s strategy has been to try to destroy the Ukrainian healthcare system. A recent article in The Lancet stated that there had been more than 1,000 attacks on Ukraine’s health centers and staff by the end
15 DI EUROPE · SUMMER 202 3
Back then in Ukraine: Anna Smolova with husband Oleksandr Smolovyi and their son Dima, now seven years old.
Image: Anna Smolova
of 2022, resulting in a decline in the quality of healthcare and service delivery. 1
“During the first three months of the invasion, Russian forces also used other techniques to reduce patient access to medical care,” Smolova explains. “Some people were kidnapped and couldn’t recieve their treatments. I remember the case of a patient with cancer who was trying to explain to her captors that she had to go to the hospital to receive her chemotherapy. They detained her and her husband for weeks.”
Over a year after the war started, things are not back to normal. Many facilities are running without water or electricity, and some hospitals and clinics are beyond the point of repair. Medical teams tend to patients the best they can in dreadful conditions, without schedule.
“Waiting lists, for a while, didn’t exist anymore,” she says. “Now everything gets done as soon as possible, like before the war.” The Russian invasion has also caused important migratory movements inside the country and at least six million Ukrainians have been internally displaced.
The number of patients who need medical care has therefore doubled, or even tripled in some areas, Smolova reports. “My father is overwhelmed,” she says. “He tends to 60 patients a day, instead of 20 before the war. There is no limit to the number of patients to tend to per day.”
The contrast with the Spanish healthcare system is stunning, but not in a way that one would expect, she explains. “I went back to Ukraine last January for my son to receive tonsillectomy because every

patient there is treated right away. In Spain, there are huge waiting lists and he would have had to wait for months. Delays here are unbelievable and I’m surprised people are not more indignated.”
Another big difference she notices between the two countries is that physicians in Spain can only chose one specialization. “In Ukraine, you can specialize in whatever you want – pediatrics, ultrasound, oncology, etc. In Spain the training is stricter, but they lack doctors across the country.”
She is however glad to live in Spain, a country she had visited many times and whose language she had learned long before the war. “Living here is a challenge, but I feel like I’m progressing every day. My son is happy at school, I’m happy. Security gives you a lot of things. We can’t plan anything as long as the war is raging. So for now, we will continue here in Bilbao, but we hope to be reunited as a family as soon as possible. It doesn’t really matter where.”
In the future, Smolova, who also has a degree in international management and teaching, plans to complete a PhD in microbiology. “There is nothing unattainable,” she says gracefully.
Her grit resonates with what other Ukrainians have achieved so far, back home.
16 DI EUROPE · SUMMER 202 3 RADIATION THERAPY
REFERENCES 1 DOI: https://doi.org/10.1016/S0140-6736(23)00387-2
New life in Spain: Anna Smolova working at the Bizkotxalde Clinic in Basauri, near Bilbao.
Image: Anna Smolova

How Radiology Helps Preserve Aquatic Species
 By Mélisande Rouger
By Mélisande Rouger
Sustainability took center stage at ESGAR 2023, the annual meeting of the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), as a zoologist highlighted how radiology can help in the conservation of aquatic species last June in Valencia, Spain.

The world is going through a sixth mass extinction, which is ocurring at a much faster pace than any other similar event in the past, according to Dr. Daniel García Párraga, Director of Zoological
Operations at the Valencia Oceanographic, who spoke on the first day of the conference.
“We are experiencing a very high rate of extinction,” he told a packed audience. “The current rate is between 100 and 1,000 times the background rate of exctinction that should be expected.’’ While domestic mammals and human populations are growing exponentially, the number of wild species is constantly declining, mainly due to human activities.
“Some researchers (have linked) large amounts of emitted CO2 with former extinctions of species,” he said. “Today, human activities generate the largest
SUSTAINABILITY 18 DI EUROPE · SUMMER 202 3
Image: © AGSTRONAUT stock.adobe.com
Image: © pham stock.adobe.com
amounts of CO2 in the atmosphere.” Healthcare and particularly radiology have a big impact on the environment.
“The healthcare sector generates approximately ten percent of the total carbon emissions in the Unites States, a recent study has showed,” he said. “Radiology is thought to be a top contributor to the healthcare carbon footprint due to its high energy-consuming devices and waste from interventional procedures, using on average eight kilograms of material per case.”
But just as radiology improves and saves human lives, it can also contribute to the conservation of species, he added.
Helping manage a wide range of animal diseases
For example, the Imaging Department at La Fe Hospital in Valencia, which is led by former ESGAR President Professor Luis Martí-Bonmatí, cooperates with the Oceanographic to improve the health of aquatic species. “This partnership is a chance to include radiology as an additional tool for saving different species,” García Párraga said.

One of the most important findings his team has discovered thanks to radiology is the decompression sickness disease (DCS), a debilitating and potentially fatal condition in sea turtles after alterations of their physiological dive when forcibly retained at depth and then brought to the surface.
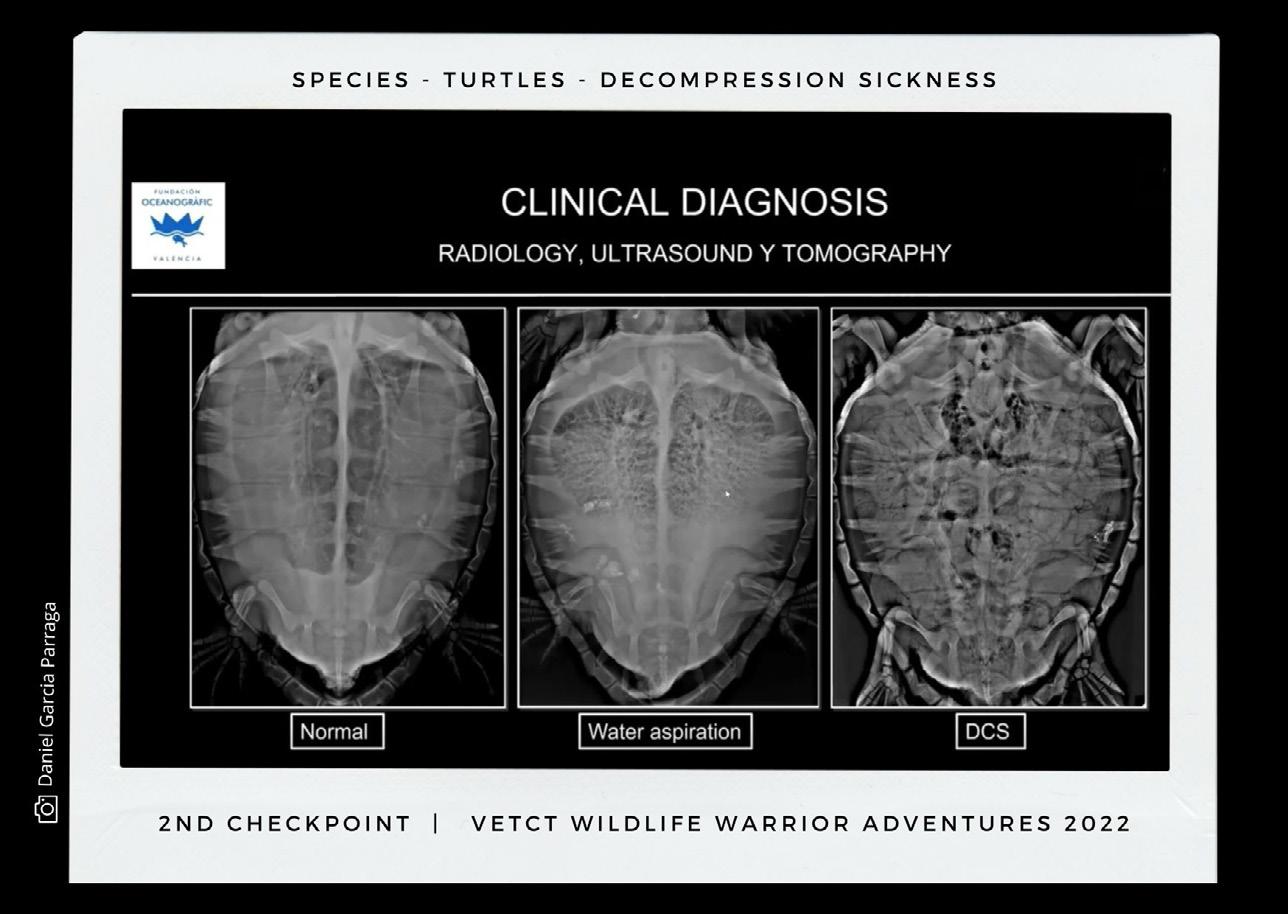
The researchers have studied DCS in seven marine turtles with both ultrasound and CT. “Ultrasound offers maximum sensitivity to detect gas embolism,” he said. “With the ultrasound device,
we discovered that the right atrium is one of the regions where gas bubbles are most easily detected and where they can appear earlier.”
Establishing severity of the disease is difficult with ultrasound and so the team examined the individuals with CT. “CT is the ideal technique to quantify and characterize in detail the distribution patterns of pathological gas.”
The main threat for sea turtles remains fishery activities – for example, when turtles get stuck in fishnets. “These activities are the number one accidental cause of death in marine turtles,” he said.
“Hundreds of thousands turtles die every year.”
The Oceanographic carries out research on how to mitigate the impact of fishery on aquatic species. “We work with fishermen to convince them to include exit strategies for turtles in the nets, for example by including a guiding tunnel, grid, and escape opening,” he said.
García Párraga also tackled the effects of MRI in magneto sensitive species such as turtles, frogs, bats and birds, and detailed how he has worked on active sensing in marine mammals in his talk.
https://www.esgar.org/annual-meeting/esgar-2023
Image: © vet-ct.com 19 DI EUROPE · SUMMER 202 3
X-rays of a healthy turtle, drowned turtle, and turtle with extreme gas embolism
ESGAR 2023 in Video
By Mélisande Rouger and Guido Gebhardt

ESGAR 2023, the 34th annual meeting of the European Society of Gastrointestinal and Abdominal Radiology (ESGAR), brought together 1,500 delegates at the Palau de Congressos in Valencia, Spain, last June.

We interviewed Spanish KOLs about AI in abdominal radiology, predicting treatment response with contrast-enhanced CT and MRI, and fire in the abdomen. (Re)watch and enjoy!


Martí-Bonmatí on AI in abdominal radiology
Projects to advance AI use in abdominal radiology are booming, according to Prof. Luis Martí-Bonmatí, head of the medical imaging department and chairman of radiology at La Fe Hospital in Valencia, Spain, who tackled the topic in a dedicated session.
President Torregrosa on inflammation, ultrasound and trilateral cooperation
“We wanted to deal with all the inflammatory diseases and conditions that affect the abdomen and prepared dedicated sessions under this theme,” Asunción Torregrosa, head of the abdominal section in the medical imaging department at La Fe University Hospital in Valencia, told Mélisande Rouger, publisher and executive editor of Diagnostic Imaging Europe.
Martí-Bonmatí on how to predict and assess response
Prof. Luis Martí-Bonmatí, head of the medical imaging department at La Fe Hospital in Valencia, Spain, explained how contrast-enhanced CT and MRI can help evaluate and predict response in abdominal oncology during a Bracco-sponsored symposium on the second day of the conference.
20 DI EUROPE · SUMMER 202 3 ESGAR 2023

Pioneer in Energy Saving Radiology Practice Shares Tips
Rising energy costs are a problem for radiology practices and clinics, especially since the beginning of the war in Ukraine. Prof. Hans-Martin Klein from Burbach in Germany started looking into alternative energy sources more than ten years ago. He told us more about his green practice, and how low-field MRI is experiencing a “renaissance”.
By Guido Gebhardt
◾ Prof. Klein, you have recently become the man to watch when it comes to reducing energy costs in radiology. How did this come about?

In 2010 I built a medical center on the high Westerwald, where the wind is known to be very cold. The Energy Saving Ordinance (EnEV), which came into force in 2009, favored the use of alternative heat sources. At the time, I thought that somehow the MRI scanner could be used as an alternative energy source, because the system produces about 20 kW of waste heat 24 hours a day, seven days a week. In addition, the energy needed to cool the helium could be saved. This concept also reduced the number of requirements for the building structure, which saved additional costs.
These measures enabled us to save about 85 percent of our heating costs. We were surprised ourselves at the time.
◾ Can such heat exchangers be installed anywhere or was this something specific to your practice?
The waste heat from the superconducting MRI scanners is not something practice-specific. The problem with this interface, however, is that not all practice owners actually own the practice space, because the conversions have to be coordinated with the building heating system.
◾ Surely there are additional potential savings in radiology?
After the medical center was built, I started planning an energy-optimized practice with an open MRI. Knowing how little energy low-field
“ As a radiologist, you deal intensively with technology. Radiology is both a craft and applied physics. And that is a good thing!”
Hans-Martin Klein from Burbach, Germany
MRI scanners require, we bought an 0.35 Tesla system in 2019.
Another aspect of conservation or sustainability in radiology is, of course, helium. It is quite expensive in technical synthesis. In addition, natural helium is slowly becoming scarce. Superconducting MRI systems require up to 2,000 liters of the gas, which is in liquid form at around – 270 °C, to cool the system.
Particularly in older systems, some evaporates regularly and must be refilled. New MRI scanners get
22 DI EUROPE · SUMMER 202 3 SUSTAINABILITY
Prof.
by with significantly less than 10 liters of helium. The system with the lowest helium filling is even only 0.7 L at a field strength of 0.55 Tesla.
◾ Are there noticeable differences in image quality between an 0.55 Tesla low-field and a superconducting 1.5 Tesla MRI scanner?
The image quality of MRI scanners is something like this: if you double the measurement time, you get roughly identical image quality at half the field strength.
In addition to field strength, the homogeneity of the system and the gradients also play an important role in image quality. Furthermore, it is a question of how the K-space is sampled. Compressed sensing is one of the buzzwords here – along with matrix coils or concepts such as Simultaneous MultiSlice Imaging. Modern low-field MRI systems with permanent magnets already use some of these techniques. Doubling the coil elements has the same effect as doubling the field strength.

Images from low-field systems are surprisingly good. In addition, there are specific advantages of lower field strengths such as less metal artifacts, better T1 contrast, better phase separation in Dixon sequences, less dielectric effects, and less impact on implants such as VP shunts or cochlear implants.
In the past, low-field systems were always a bit frowned upon, but currently they are somehow experiencing a renaissance.
◾ To what extent does artificial intelligence play a role in MR image quality?
Image quality is essentially about the signal-to-noise ratio. So you can either increase the signal by putting more power into the field strength and the gradients, the coils and so on, or you can try to reduce noise.
If you reduce noise with classical felting, the images always lose information. Deep learning reconstruction, on the other hand, is able to reduce noise without losing information by preserving contour information.
Of course, this can only be used within certain limits, because otherwise one runs the risk of pretending an accuracy that is not there at all. But compared to the filters that were available in the past, we now have very powerful AI algorithms at our disposal. This will bring significant advantages for low-field systems.
https://www.greenscan-imaging.de/

A new approach to the Improvement of Energy Efficiency in Radiology Practices, Prof. Hans-Martin Klein,
Verlag, https://www.thieme-connect. com/products/ejournals/abstract/10.1055/a-1123-7944
23 DI EUROPE · SUMMER 202 3
All images: GreenScan GmbH
With the energy-optimized low-field MRI practice, Prof. Hans-Martin Klein pursues the idea that economy, ecology and gentle medicine are congruent principles. Since November 2022 a new open MRI is in operation. More image quality, more comfort, even less energy consumption!
Thieme
Reducing Environmental Pollution after Contrast-Enhanced Scans
 By Mélisande Rouger
By Mélisande Rouger
Radiologists called for action to reduce the release of contrast media in hospital wastewater after contrastenhanced examinations in a dedicated session at ECR 2023 last March.
An estimated 300 million CT examinations are being performed
each year in the world. This number is expected to grow, and with it, the amount of iodinated contrast media (ICM) used in radiology, according to Professor Olivier Clément, Head of Imaging at Georges Pompidou European Hospital in Paris, and Chair of the contrast media committee of the Europe-
an Society of Urogenital Radiology (ESUR). “If you assume that 40 percent of CT scans are being carried out with an average of of 100 milliliters of contrast media you end up with 12 million liters of ICM that are being injected in patients and then evacuated in the sewage,” he told the audience in Vienna.
24 DI EUROPE · SUMMER 202 3 SUSTAINABILITY
This article was first published in European Hospital · www.healthcare-in-europe.com Image: © Viktoriia stock.adobe.com
This contamination of the aquatic environment is being increasingly studied. In Germany, for example, about 200 kilograms of contrast media are released in the Rhine river every day. “That’s 70.9 tons per year. It’s a lot and it means that we can really recover ICM from the aquatic environment,” he said.
A global issue
There are also review studies about contrast media’s effects on the environment. In a paper published in the Science of the Total Environment in 2021, a team of researchers found that, whatever the contrast media used, a large amount was found not just in hospitals’ sewage wastewater but also in surface, ground and drinking water in North America, Asia and Europe.
“It’s a global problem, a world issue of contamination of surface and drinking water due to contrast media release,” he said.
The contribution of ICM to water pollution can be as high as 80 percent in the mass loading of pharmaceuticals in a hospital’s effluent, because of the amount of ICM that is being injected, he went on. “When we inject antibiotics, we inject up to three grams per patient. But when we inject ICM, we inject up to 45 grams per patient so the mass of contrast media is much higher.”

In themselves ICMs are not dangerous. The threat comes from the disinfection process in the treatment plants, that use chemicals such as chlorine and chloramine. These
products create toxic iodinated disinfection byproducts (IDBPS) that can be found in the aquatic environment and drinking water. “This is really the environmental problem of using contrast media,” he said.
Radiologists should be aware of the issue and work to decrease pollution linked with ICM use. “First we should inject less contrast media and respect the indication, i.e. always inject dose which is related to weight, especially for oncologic imaging,” he suggested. “We should reduce waste and use the adequate vial for the patient, i.e. open a vial of 100 milliliters when we use 90 and not a vial of 150. We should also recycle the residue in the vial.”
Taking steps is also important because of the high demand for ICM all over the world. “Vendors can produce a certain amount of ICM per year that isn’t even sufficient for all the examinations,” he said. “So we must think of how we use these products and find new ways to inject less contrast, with low kV and AI for example.”
Although different software are being trained to reduce ICM dose, a small amount of contrast media remains necessary to create contrast in the image, he believes. “We will still need contrast media in radiology for a long time.”
Strategies to reduce pollution include releasing ICM in hospital
25 DI EUROPE · SUMMER 202 3
Image: ©
The Greenwater project aims to evaluate the extent of retrievable ICM and GBCA from the urine collected after CT and MRI scans, and to assess patient acceptance to participate in the study – the “green sensitivity”.
flywish stock.adobe.com
circuits linked with specific plants, installing dry toilets for patients who have undergone a contrast-enhanced examination, and collecting urine in bags to be incinerated, since incineration is less polluting than using ICBPs to purify the water.
“The radiology community should be aware of the huge amount of iodine contrast media released in the environment,” he concluded. “We should inject wisely, know about toxic IDBPs in plants and take specific measures to decrease the effluence.”
The Greenwater project
Iodine contrast media are not the only source of concern when it comes to residuals in hospital wastewater. About 50 million of gadolinium-based contrast agents (GBCA) doses are being injected per year and then evacuated in the sewage, according to Professor Franceso Sardanelli, Director of the Department of Radiology at the Research Hospital (IRCCS) Policlinico San Donato in Milan, where the Greenwater study was recently launched.
The project aims to evaluate the extent of retrievable ICM and GBCA from the urine collected after CT and MRI
scans, and to assess patient acceptance to participate in the study – the ‘green sensitivity’.
The study was carried out with urine collection within 60 minutes of administering the contrast agent, so about 30 minutes after the examination. Results have been both surprising and encouraging, Sardanelli explained.
“The first unexpected finding to me was the high acceptance from patients,” he said. “94 percent of them agreed to take part in the study and stay half an hour more in the department. That means that we can go in this direction quite effortlessly.”
The fact that patients wanted to cooperate in the project is very good news for manufacturers and hospitals, he added. “It shows patients are highly sensitive to sustainability. Even in a hectic city like Milan, people took the time. We have to use this availability.”
The future will be to recycle both iodine and gadolinium agents, by creating virtuous cycles in which the product comes back to the producer after it has been injected in the patient. “That would make sense,” he concluded. “Recycling is the solution.”
Olivier Clément is Professor of Radiology at Descartes Paris University and Head of Imaging at Georges Pompidou European Hospital in Paris, France. He is also Chair of the contrast media committee of the European Society of Urogenital Radiology (ESUR).


26 DI EUROPE · SUMMER 202 3 SUSTAINABILITY
Franceso Sardanelli is Professor of Radiology at Milan University and Director of the Department of Radiology at the Research Hospital (IRCCS) Policlinico San Donato in Milan, Italy.

Memory Lane PACS in the 1990s
Guido Gebhardt takes on his time machine and travels back to radiology technology last century.
By now, nearly every clinic and radiology practice in Europe is equipped with a digital image and findings management system, so looking back at the equipment 30 years ago really feels like time travel.

In the 1990s, diagnostic consoles looked like a command bridge in a spaceship and 21-inch tube
monitors could not be lifted by one person alone. Long-term archives were mostly MOD (magnetooptical discs) or CD (compact disc) jukeboxes. Compared to film archive shelves they were small, but big ponderous dinosaurs with a fraction of storage capacity compared to today's SSD flash storage. And the cloud didn't even exist back then.
A copy of the DeLorean car used

Back To The Future at Bits & Pretzels’ Health Tech Conference in June 2023 in Munich, Germany.
Storage media that hardly anyone knows today: MOD (Magneto-Optical Disk) and a 3/4-inch D-2 magnetic tape from 1988. In 1991 a 130 mm MOD had a whole 650 MB storage capacity as WORM (Write Once Read Many).

28 DI EUROPE · SUMMER 202 3
IN TIME
FLASHBACK
Image: © Tryfonov · stock.adobe.coma
to travel through time in the movie
First-generation 4-monitor workstations back then are more reminiscent of the bridge of the StarTrek’s show’s Enterprise than diagnostic radiology.

At ECR 1991, radiologists talked about digital image storage in Kodak jukeboxes, equipped with 52 media disks of 5 ¼ inch, each with a storage capacity of 650 MB, so in total 34 GB.


Just 25 years ago, high-end monitors looked like the Barco MWD321: 21" tube with 1,600 × 1,200 pixels.
The beginnings of teleradiology: a camera took the X-ray image and transmitted it via ISDN. About 28 years ago, an Indy from Silicon Graphics was needed to generate the enormous computing power.


29 DI EUROPE · SUMMER 202 3
StraTrek image: © Willrow Hood stock.adobe.com Image circles: © natrot stock.adobe.com
Every Photon Counts
In Japan, the current production facility for growing cadmium telluride crystals, an essential compound for the fabrication of photon counting detectors, is nearing its capacity limits. Siemens Healthineers is thus building a new factory in Germany to match the expected rising demand for photon-counting CT.
By Guido Gebhardt
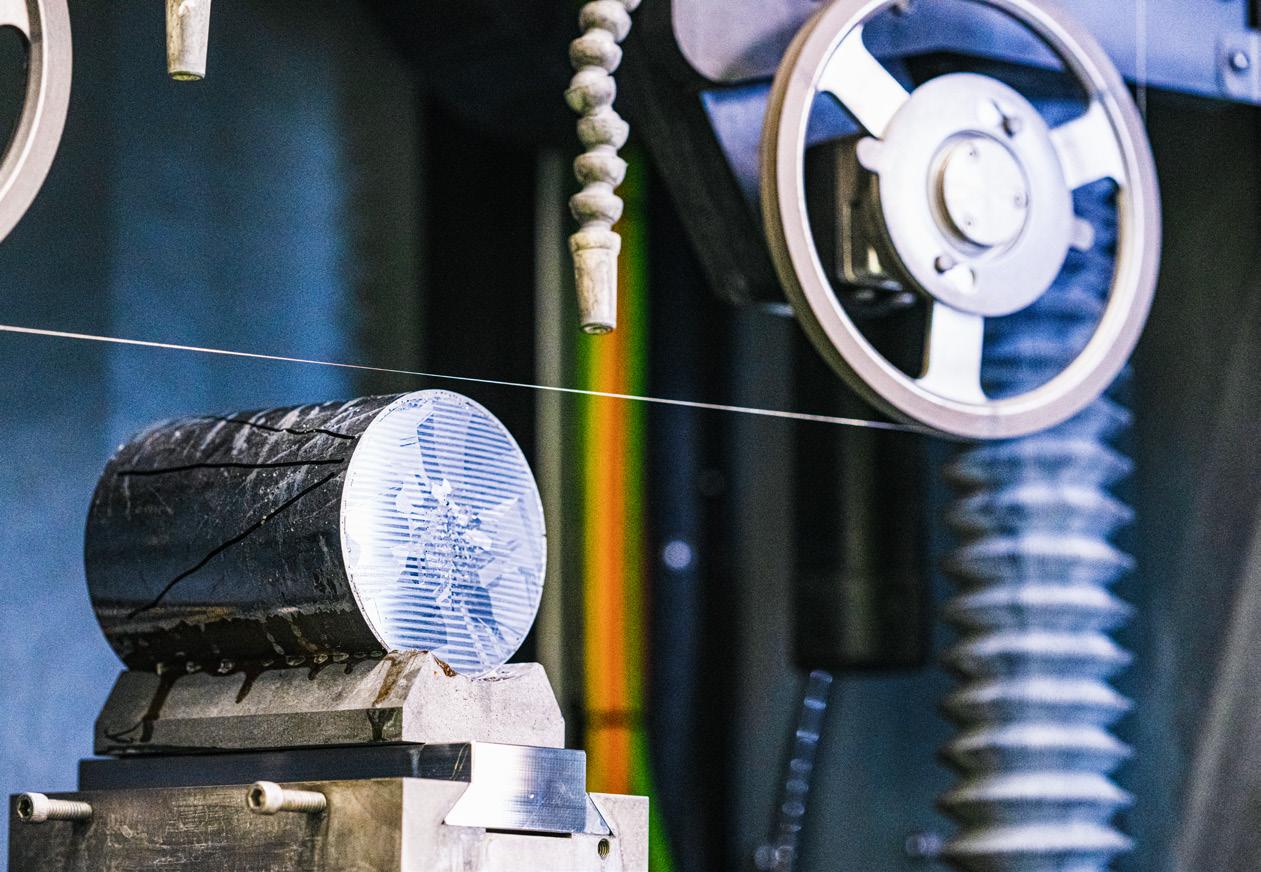
In 2019 Siemens Healthineers’ materials scientists began looking at growing cadmium telluride (CdTe) crystals to build another factory in addition to working with Acrorad’s crystal factory in Japan, to meet the growing demand for CTs with photon-counting detectors.
Conventional CT detectors have several disadvantages. They first convert incoming X-ray photons into visible light, which is then converted into an electrical signal by photodiodes. And the light pulses generated in the scintillator are emitted not only in the direction of the photodiode, but also in all spatial directions. Therefore,

30 DI EUROPE · SUMMER 202 3 COMPUTED TOMOGRAPHY
At the heart of a photon-counting CT is the new quantum-counting detector, whose detection layer consists of a cadmium telluride single crystal (CdTe) and offers clear advantages over conventional CT detectors.
on the one hand, a grid is required to prevent pulses from neighboring pixels from being measured. On the other hand, only a small part of the light arrives at the photodiode.
More sensitivity
“Photon-counting detectors are much more sensitive to X-rays because they convert the energy of each photon directly into an electrical signal,” said Paul Heimann, development engineer in crystal growth, describing the advantage of the new technology.

Photon-counting detectors can not only count each individual photon, but also measure its energy, thereby eliminating scattered radiation. In addition, there is no need for a grid.
The greatest advantage of PCD, however, is that not only can scattered radiation be eliminated, but also different materials can be displayed, based on energy thresholds that can be set in different ways. It is assumed that future detectors will already be able to discriminate four or even six energy levels.
Cadmium telluride has proved to be an ideal detector material for photon-counting detectors. The crystal is particularly heavy and has a high density – both basic requirements for good x-ray absorption.
The big challenge, however, is that CdTe crystals of high purity are needed for CT detectors. This is why Siemens Healthineers decided to work with Acrorad, as the Japanese company has had the necessary know-how for growing the purest CdTe crystals for several years.
Complex manufacturing process
Siemens Healthineers expects the demand for photon-counting CT scanners to increase significantly in the future, and has therefore set up a laboratory as early as 2019 at its site in Forchheim to learn, start and optimize growing CdTe crystals. Following this successful test phase, ground was broken for a dedicated CdTe crystal factory in May 2023.
However, it is important to the Siemens scientists not to simply copy the production systems already available in Japan oneto-one, but to establish their own infrastructure and use production lines from European manufacturers. One reason for this decision is the different regulations that apply in Europe for the operation of electrical systems.
Now that the transfer of knowhow and the establishment of the crystal laboratory have been achieved, the processes are being scaled up in order to go into “series
“Photon-counting CTs not only use the very sensitive detector material, but also require very powerful computer systems due to the large amount of data to be processed.”
production” with the new plant, to grow crystals on an industrial scale over several weeks.
First, the cadmium, whose melting point is 320°C, must be homogeneously fused with tellurium, which liquefies at around 450°C, to form a polycrystalline ingot. The temperature required for proper “mixing” is about 1,100°C. Only then can crystal growth be initiated with the aid of an ideal seed in an evacuated glass cylinder coated with carbon, so that
31 DI EUROPE · SUMMER 202 3
Paul Heimann, development engineer in crystal growth at Siemens Healthineers
All images: Siemens Healthineers
the finished CdTe crystal consists of perfect alternating layers of cadmium and tellurium.
More flexibility
"While the individual elements cadmium and tellurium are classified as hazardous materials, the final CdTe crystal is much less hazardous," Paul Heimann explained.
"As far as materials’ purity is concerned, we are a little paranoid. The clean room atmosphere is important to prevent even the smallest impurities during the crystal growth phase."
Only when cadmium telluride has solidified into a inhomogeneous gray block, the crystal growth can be started. To do this, the polycrystalline semiconductor is pulled through an oven for ten to twelve weeks so that the atoms, which go into solution again in the process, have enough time to rearrange themselves on the nucleation surface and the crystal can grow perfectly ordered layer by layer.
Siemens Healthineers has put a great deal of effort into setting up its own manufacturing process by growing CdTe crystals for photon-counting detectors. The company expects the two factories on different continents to provide maximum supply security and flexibility, to respond in the best possible way to the increasing demand for photon-counting CT equipment.
https://www.siemens-healthineers.com/

32 DI EUROPE · SUMMER 202 3 COMPUTED TOMOGRAPHY
Ideally, the cadmium telluride crystal solidifies into a completely homogeneous gray block. In a further production step, thin slices are cut off.
The new building will significantly increase production capacity for crystals, prevent supply bottlenecks and shorten construction times. Research and development for the highly complex production of crystals is also to be expanded here.
All images: Siemens Healthineers



MYESR.ORG
AI Can Predict Future Brain Changes in Elderly Patients
◾ Preliminary study shows that a deep learning-based algorithm is able to forecast brain development from images obtained in fluorodeoxyglucose (FDG)-positron emission tomography (PET) examinations.
◾ The newly developed tool can accurately predict the third scan taken after two years of consecutive imaging using data modeling in patients aged 55 or older.
◾ The ongoing trial could help improve early diagnosis of Alzheimer’s disease (AD), by looking at predicted longitudinal changes of the whole brain for the first time in brain imaging research.
By Mélisande Rouger
Deep learning can predict brain development up to six years after initial assessment of Alzheimer’s disease on FDG-PET scans, according to a preliminary study presented at EAN 2023, the 9th annual meeting of the European Academy of Neurology (EAN) that took place on July 1 – 4 in Budapest, Hungary.
Researchers from Germany and Iceland have successfully trained
an algorithm using a convolutional neural network (CNN) on the first two FDG-PET scans to predict the third scan acquired in elderly (> + 55 years) participants from the Alzheimer’s Disease Neuroimaging Initiative, who received FDG-PET imaging in three consecutive years.
“The algorithm accurately predicted the overall future FDG-PET signal of the entire brain, i.e. metabolic reduction, which reflects neuronal activity,” Elena Doering, a PhD
Elena Doering is a PhD student at the German Center for Neurodegenerative Diseases (DZNE) in Bonn, Germany.

student at the German Center for Neurodegenerative Diseases (DZNE) in Bonn, said. “The algorithm was able to anticipate future signal decline – i. e. metabolic reduction, reflecting loss of neuronal activity.”
By iteratively feeding the trained algorithm with the predicted scans, the team was even able to show that FDG-PET could be predicted for up to six years.
34 DI EUROPE · SUMMER 202 3 ARTIFICIAL INTELLIGENCE
“With our algorithm, we are currently able to predict brain development up to six years after initial assessment,” she said. “Predictions for a particular year were achieved by using scans from the two previous predicted years.”
Furthermore, the tool appeared to detect ongoing neurodegenerative processes already at baseline, as it predicted a significant signal decline in year two in Alzheimer’s disease (AD) patients in AD-prone regions, such as the bilateral inferior temporal and parietal regions, and the posterior cingulate cortex.
A one-of-a-kind study
The trial is exploring unknown territory, as prediction of longitudinal metabolic changes in the brain as measured by FDG-PET has barely been tested yet.
“Previous studies demonstrated that AI could be used to predict clinical symptomatic changes of neuropsychiatric disorders on the basis of baseline neuroimaging information,” the authors wrote. “However, studies that successfully predict actual longitudinal changes of the whole brain are very sparse, compared with the amount of studies that observe specific longitudinal changes, such as hippocampal volume.”

Having a tool that predicts longitudinal FDG-PET scans from scans collected at baseline and one year later, could help improve patient care.
“Such an algorithm would allow physicians to read an anticipated “future” FDG-PET brain scan as they would in their normal routine, but years in advance,” Doering said.
Previous studies such as IDEAS 1 have shown that imaging-informed diagnoses can lead to changes in clinical management compared to diagnoses provided solely based on clinical characteristics.
As databases continue to increase and to capture longer time frames, the prediction may become available for even more extended time frames than six years, Doering believes.
“We hope that our work can provide clinical benefit in two ways: improving early diagnosis or providing reliable prognosis; and allowing individual prediction of brain pathological changes over time,” she said
The study may also help improve understanding on the natural course of AD, whose etiology remains elusive to date.
“One of the main risk factors is age, but genetic variations and lifestyle factors, such as diet, physical exercise and years of education,
also play a part in the development of the disease,” she said. “Our results could aid in the identification of factors leading to more or less rapid progression and obtain a more individualized prognosis, even without the need of repeated brain imaging examinations.”
For therapy trials, the new tool may become relevant to judge the effect of a specific drug in an individual patient, as assessed by comparison of the actual versus the predicted brain status following therapy.
“Another potential application of our algorithm could be to predict drug efficacy within clinical trials, even without the need for longer follow-up or repeated imaging examinations,” she concluded.
1 https://jamanetwork.com/journals/jama/
35 DI EUROPE · SUMMER 202 3
FDG-PET scans of an Alzheimer’s disease patient at baseline (top) and two years later (bottom) show reductions in brain metabolism. The project is aimed at predicting brain metabolism changes in individuals with and without cognitive impairment.
REFERENCES
fullarticle/2729371
CEM: the Experience of a Large, Progressive Spanish Hospital Group
The recent approval by the EU and the US of the iodine-based contrast enhanced mammography (CEM) highlights the steady progression of this relatively new breast imaging modality. We thought that this would be a good occasion to take stock of the current status, future potential and likely role of CEM in breast imaging, so we talked to Dr. Julia Camps Herrero, breast radiologist, Corporate Head of Breast Health and responsible for the co-ordination of five breast units in the Ribera Salud group of hospitals in Spain.
By Alan Barclay
◾ Before we get into the details of your experience with CEM, could you please give us a brief overview of the breast imaging services provided by your hospital?
First of all let me explain the structure of the Ribera Salud group in Spain as a whole. Our group, which is devoted to the development of public-private partnership initia -
tives in the healthcare field, has hospitals in the Valencian community (Hospital del Vinalopó, Hospital de Denia), in the Madrid area (Hospital de Torrejón), and in the Galician community (Hospital Povisa and Hospital Polusa). All these hospitals carry out breast imaging, with three of them (Hospital del Vinalpo, Hospital Torrejon and Hospital Povisa) also equipped with CEM systems.
Against that background, let’s now go more into breast imaging, starting with screening. In Spain, the recommended regimens for population-based breast screening vary by geographical area. In some areas, the recommendation is for screening mammography every two years in women aged 45 to 69, whereas in other areas it is every two years

36 DI EUROPE · SUMMER 202 3 BREAST IMAGING
Dr. Julia Camps-Hererro is a breast radiologist and Corporate Head of Breast Health in the Ribera Salud group of hospitals in Spain
in women aged 50 to 69 years of age. The overall average percentage take-up in the Spanish breast screening programs is approximately 75 percent of all eligible women, but this varies from region to region.
We are the referral clinics for the population-based screening programs in the areas where we have hospitals, so the cases we see are all diagnostic.
To give you an idea of the number of breast imaging procedures we carry out annually, the three medium-sized hospitals which also have CEM carry out a total of almost 9,000 breast exams per year. The majority of these are mammography or tomosynthesis. In addition to this, two of the hospitals also routinely carry out 2,000 CEM examinations per annum, with the third hospital now implementing CEM since February 2023.
Of course it’s not just mammography / tomosynthesis and CEM. We also have a complete armory of other breast imaging modalities from a variety of vendors.
For example:
• Hospital del Vinalopó in Elche, in the Valencian community: Philips Ultrasound machines, Hologic tomosynthesis and CEM, and Philips 1.5T Elition MRI equipped with coil for MR-guided biopsies.
• Hospital de Denia also in the Valencian community: Siemens Ultrasound machines, GE Pristina tomosynthesis, and Siemens 1.5T MRI.
• Hospital de Torrejón in Madrid: Philips and Samsung Ultrasound machines, Hologic tomosynthesis and CEM, and Philips 1.5T Achieva Intera equipped with coil for MR-guided biopsies.
• Hospital de Povisa in Vigo, Galicia: Philips Ultrasound machines, GE Pristina tomosynthesis with contrast-enhanced biopsy, and Philips 1.5T Achieva Intera equipped with coil for MR-guided biopsies.
• Hospital de Polusa in Lugo, Galicia: Canon Ultrasound machines, GE Pristina tomosynthesis, and Siemens 1.5T MRI.
You can see that throughout the group we have a wide selection of equipment from most of the major vendors, so we are well placed to evaluate the relative pros and cons of each manufacturer’s products.
The majority of breast imaging is carried out by mammography / tomoynthesis. CEM has been shown to be more sensitive than mammography or ultrasound for the detection of malignancy, with its sensitivity reported to be approximately the same as that of MRI, which is generally considered as the most sensitive modality for breast imaging.
◾ OK, given that, let’s dwell a bit on breast MRI. Later in our conversation, we will no doubt get on to the subject of comparing the performance characteristics of breast MRI with those of CEM. But for the moment can you describe the principal indications for breast MRI ? There are many such indications:
• In all our centers, we use breast MRI for pre-operative staging. In cases of any contraindications for MRI, we perform CEM in all those centers which are equipped with CEM systems.
• In the evaluation of response to neoadjuvant treatment
• For high-risk patients (those with an estimated breast cancer risk of 20 to 25 percent)
• For patients with high-risk B3 lesions before and after vacuum-assisted biopsy, as well as for the follow-up of those with a higher cancer risk (lobular neoplasia and atypical ductal hyperplasia)
• For patients with equivocal findings in conventional imaging such as mammography
• For patients with a breast cancer of unknown primary origin (CUP)
• Selected patients with a history of breast cancer at higher risk of relapse (triple negative or HER2+ breast cancer patients).
One other occasional use we make of MRI is in the estimation of breast density, although we usually determine breast density by visual examinations of mammography images.
◾ To start with, since when have you been using CEM? In what clinical situations do you use the modality and what is your opinion of its value in these situations?
Our experience with CEM is already quite extensive and increasing steadily. Precise details of experience vary from hospital to hospital:
• In the Hospital del Vinalopó (Valencia) we have been using Hologic tomosynthesis and CEM system since February 2020. Since then we have carried out more than 3,100 CEM examinations, the majority for monitoring cancer patients.
• In the Hospital de Torrejón (Madrid) our experience dates a little further back: we have been using Hologic tomosynthesis and CEM since September 2019.
37 DI EUROPE · SUMMER 202 3
From then till January 2023 we have performed 2,600 CEM procedures, again mostly for the monitoring of breast cancer patients
• In the Povisa hospital in Galicia we have a Pristina tomosynthesis system from GE which also has the possibility of taking contrast-enhanced biopsies.

◾ So how does the performance of CEM compare to that of MRI?
As mentioned above, it should be remembered that CEM has been shown to be more sensitive than mammography or ultrasound for the detection of malignancy, so the most meaningful comparison of CEM with other modalities is indeed with MRI.
In most of the published metaanalyses of comparative performance parameters, CEM has been shown to have sensitivities and specificities that are broadly similar to those of MRI.
However, I find that in general MRI performs better than CEM in terms of detection and characterization of lesions because through ultrafast and dynamic sequences it yields superior kinetic information, as well as providing diffusion data, which is helpful for lesion characterization and thus for differentiation between malignant and benign lesions. In addition, MRI can yield multiplanar and 3D reconstructions and also provides more extensive anatomical coverage such as of the axillary tail, posterior regions of the breast, and internal mammary lymph nodes, all of which can be difficult, if not impossible, to image in CEM. Signal-to-noise ratio is also better in MRI and the pooled diagnostic odds ratio indicates a higher overall diagnostic performance of MRI compared to CEM.
However, in non-mass lesions adjacent to breast cancers, CEM seems to perform better (higher specificity) than MRI although we have
not analyzed this finding in-depth. In the future this might enable us to reduce biopsies. In patients with up-front BI-RADS four lesions, CEM also gives us the possibility of avoiding unnecessary biopsies, especially in architectural distortions and asymmetric densities, as well as pseudonodules. CEM is especially helpful in patients referred from the populational screening setting, avoiding follow-up exams and unnecesary biopsies.
The above comments are made on the basis of the comparison of performance characteristics, but clearly there are other factors such as length of time of the exam, accessibility to the imaging system and its cost, which also must be considered. Those mentioned all favor CEM. For us, it is always easier to schedule a CEM examination than an MRI (on average, we perform 16 CEM procedures per week in each of the two hospitals where the technique has been established for some
38 DI EUROPE · SUMMER 202 3 BREAST IMAGING
Image: Hospital Univeritario de Torrejón
The Hospital de Torrejon in Madrid is just one of the three hospitals in the large group of hospitals in the Ribera Salud group, that are equipped to carry out Contrast Enhanced Mammography (CEM). So far more than 2,600 CEM examinations have been carried out in the hospital.
time now). In our clinics, the waiting times for CEM examinations are virtually non-existent.
The time needed for the whole CEM procedure, including the intravenous access, to be carried out is around 15 minutes, so shorter than that needed for MRI. Currently we don’t have a programmable contrast medium injector. Such an accessory could render the whole procedure more efficient and could be helpful in calculating the exact contrast dose for each patient
However, despite the advantages of CEM, the cornerstone technique for breast cancer staging remains MRI. It’s not a question of either CEM or MRI — the techniques complement each other and are synergistic.
◾ What are the clinical applications where CEM is most useful?
• Clearly it is of use in breast cancer patients for whom MRI would normally be used but is, for one reason or another, contraindicated. In addition, CEM also has the advantage that it can depict additional lesions and helps us to stage the patient. This use of CEM also applies to patients who are undergoing neoadjuvant treament but cannot have MRI.
• We also find CEM to be helpful in ruling out malignancies in patients with equivocal lesions, for example in distortions or asymmetries. It should be noted however that CEM is less helpful in microcalcifications
• In addition, the comparatively easy access to and availability of CEM systems compared to MRI as mentioned above opens up the promise
of a “blanket” use of the modality in all patients with a history of breast cancer. To examine the feasibility of such an approach, we are currently analyzing our data using a cohort of 2,000 patients, 70 percent of whom have had more than two CEM exams.
The first version of the BI-RADS lexicon has recently been published 1 and allows for consistency in reporting and also the validation of standardized terms through studies looking at the performance of CEM in a variety of clinical settings 1
◾ What about biopsies?
In case of an extensive non-mass lesion identified only by CEM, we perform an additional ultrasound examination. Most of the time, there is a good correlation between the ultrasound and CEM findings. In the rare case of a nodule or a small lesion not seen in ultrasound, we will perform an MR-guided vacuum-assisted biopsy (VAB). We ensure radio-pathologic correlation with a 2D mammography post-biopsy. In our Povisa hospital, we now have a CEM-guided biopsy system which we are currently setting up and evaluating. Of course a CEM-guided biopsy system seems logical for lesions identified by CEM.
We usually try to carry out a CEM examination upfront for all BI-RADS 4C or BI-RADS 5 lesions so that we can biopsy on the same day not only the suspicious lesion but any additional suspicious lesions. Thereafter, we always try to perform MRI in order to confirm that all the significant lesions have been biopsied and tagged with clips.
◾ How do the patients react to CEM? And what about the technologists and radiologists?
In general, patients react very well to CEM, mainly because the exam only takes a little bit longer than standard 2D mammography and tomosynthesis, techniques with which they are usually already familiar. Occasionally patients complain of the metallic taste left after the contrast injection, but this is transient. The procedure is well tolerated — the percentage of allergic reactions we have observed is well under one percent and we have had no severe allergic reaction or death in a total of more than 6,000 exams.
Inevitably, there was a learning curve when CEM was first implemented, but for the technicians this didn’t last any more than two or three months. The learning curve for the breast radiologists was perhaps slightly longer, mainly because of the diversity and varied nature of CEM findings — it can take some time to get used to background parenchymal enhancement, the various artifacts, as well as the heterogeneous grades of enhancement in mass and non-mass lesions, etc. Previous experience with breast MRI makes the learning curve easier for the breast radiologists.
◾ And now, looking ahead, how do you see the future role of CEM in general and in your hospitals in particular? As I hope you have seen from our conversation so far, the role of CEM in our hospitals is very well established and already plays an important role in the indications we have talked about.
39 DI EUROPE · SUMMER 202 3
As for the future, in addition to its current roles, I can imagine CEM being increasingly used in the following clinical scenarios:
• In patients at a high risk of breast cancer. The risk is usually identified using risk-assessment protocols. By the way, the role of artificial intelligence (AI) in such risk-assessment protocols is likely to become more important in the future — AI has already been shown to improve the accuracy of risk assessment compared to classical risk-assessment methods.
Women with a family history of breast cancer should have a risk assessment carried out — currently this is not done routinely.
• Women with dense breasts. Although studies have shown that breast MRI can be of undoubted benefit in patients with very dense breasts, the reality is that there are simply not enough MRI systems
available to follow-up all such patients. However we might be able – perhaps using advanced AI analysis – to stratify which dense breast patients should undergo MRI and who can benefit from CEM. Such assessment need not necessarily be carried out every 12 months as the DENSE trial showed (every two to four years is cost-effective in patients with very dense breasts) 2 .
In the context of relatively difficult accessibility to MRI, the increased use of abbreviated MRI might help –it would be very interesting to analyze the performance of abbreviated MRI in women with dense breasts and compare it to that of CEM.
• Speaking of AI-derived algorithms, these are currently not generally available for image interpretation in CEM. In the future, however, AI could enable us to avoid unnecessary biopsies
and follow-up exams, as well as perhaps build prediction models of the likely response to therapeutic regimens used to treat specific breast cancers. Likewise AI-derived protocols could also be used to evaluate early response to neoadjuvant treatments (hormone therapy as well as chemotherapy) in order to de-escalate any unnecessary further chemotherapy.
In addition to helping us widen the spectrum of patients in whom we can perform high-quality functional imaging, CEM may also be able to avoid unnecessary radiation therapy in patients with unifocal and early breast cancers, as has been shown with MRI in the PROSPECT trial3. Other MR-guided de-escalation trials such as the MiniVAB (NCT04107636) have shown that we may be able to de-escalate unnecesary surgery in patients with unifocal breast cancer. CEM could conceivably play a role here. In summary, all breast cancer treatment procedures could/should be guided by CEM.
https://www.riberasalud.com
REFERENCES
1 Contrast Enhanced Mammography. 2022. A supplement to ACR BI-RADS® Mammography 2013 2022. https://www.mdpi.com/2075-4418/13/6/1011
2 Veenhuizen SGA et al. Supplemental Breast MRI for Women with Extremely Dense Breasts: Results of the Second Screening Round of the DENSE Trial. Radiology. 2021; 299(2): 278. http://dx.doi.org/10.1148/radiol.2021203633
3 Mann et al. Results of ANZ 1002 : Post-operative Radiotherapy Omission in Selected Patients with Early breast Cancer Trial (PROSPECT) following pre-operative breast MRI http://dx.doi.org/10.1016/S0959-8049(22)01476-9

40 DI EUROPE · SUMMER 202 3 BREAST IMAGING
Low and high-energy cranio-caudal (CC) and medio-lateral oblique (MLO) views of a patient with a 17 millimeter breast cancer in the union of lower right breast quadrants in whom CEM also showed an additional five millimeter lesion in the union of upper quadrants that was found with ultrasound and biopsied at the same time as the index cancer. Both lesions were histologically found to be invasive ductal cancer, Luminal A molecular subtype.
Ultravist® – Your Contrast Agent in Contrast-Enhanced Mammography


Ultravist® 300/370 is approved for use in contrast-enhanced mammography (CEM): an emerging, easy to use, and effective diagnostic modality in breast imaging.1,2

41 DI EUROPE · SUMMER 202 3
1. Zanardo M et al. Technique, protocols and adverse reactions for contrast-enhanced spectral mammography (CESM): a systematic review. Insights Imaging. 2019;10(1):76.; 2. Sogani J et al. Contrast-enhanced mammography: past, present, and future. Clin Imaging. 2021; 69:269-279 For more information on Ultravist visit: https://www.radiology.bayer.com/products/ultravist The German prescribing information can be accessed here: PP-ULT-DE-0140-1 June 2023
References:
Expediting Workflow with Large Language Models
One of the major issues in radiology is the integration of structured reporting into the radiological workflow, a task which is seen as time-consuming and cumbersome by many radiologists. We interviewed Markus Vogel, MD, Chief Medical Officer at Nuance Communications, about new developments in speech recognition.
 By Guido Gebhardt
By Guido Gebhardt
◾ Dr. Vogel, many radiologists associate structured reporting with many clicks in another IT system. In addition to RIS and PACS, they now also have to click through the user interface of the reporting solution. To what extent do modern speech recognition technologies help to make the workflow smoother?
When we talk about automated speech recognition, we should start with the microphones. While many radiologists still envision a doctor with a microphone in his hand with digital dictation, modern microphones today are not only much more sensitive, but have also become wireless and integrated. This means that the doctor has both hands free to switch between different applications with the mouse.
As far as speech recognition is concerned, Natural Language Processing (NLP) is still state of the art, although with Dragon Medical One we have also perfected the voice control of the computer hardware. Switching between RIS or PACS and a structured findings solution or jumping to specific input fields is now standard. This eliminates the need to reach for the mouse.
◾ And what about speech recognition and AI? Does Chat GPT have an influence on the reporting of the future and can it further improve the workflow?
Yes of course, but in a different way as many think. ChatGPT is often confused
with a search engine in the media as well but ChatGPT is not there to search for hits like Google. First of all, I would delete Chat in the context of speech recognition and that brings us to the actual topic, since GPT stands for Generative Pretrained Transformer. This means that the system is able to access pretrained
42 DI EUROPE · SUMMER 202 3 ARTIFICIAL INTELLIGENCE
Markus Vogel, MD, Chief Medical Officer at Nuance Communications
content and transform it to generate new texts. And in our opinion, this technology will also be the basis for reporting in the future.

◾ Can you explain this in a little more detail?
The new buzzword is LLM, short for Large Language Model, which is nothing more than an association space that has been trained with radiological findings. And it is the same with Chat GPT: this is not a knowledge database, but a system that has been trained to deal with language on the basis of selected data material.
Let me illustrate this with an example: A Large Language Model is basically a file in which mappings between linguistic units are made. If you ask the system: What is the most common rare disease? You will get the answer: Acute lymphoplastic leukemia. But not because the system knows that, but because the association space is so large and has been trained so well and extensively.
◾ Got it. But how do we now get the sheet to the structured findings solution, for which there are certain specifications – for example from different international professional societies, as to what the sheets should look like and what information they should feature?
The great thing about a large language model is that I can train the association space not only with linguistic content, but also with findings templates. In the future, it will be completely sufficient to freely dictate the findings and the system will independently create a structured findings sheet that is not only formulated in a standardized way, but whose structure is also based on the templates of the various professional societies.
And this is where it gets interesting, of course, to return to your topic: a radiologist would like to have a structured report, but he or she does not feel like putting in the effort that has gone into a structured report so far. Now this is
where the Large Language Model comes in.
This means that I simply tell the Large Language Model: Look, I have input A here, this is what a structured report should look like in the end. Input B, a freely spoken text, is added to this. The task for the LLM is to convert the radiologist’s text into the specified form. The structured report is ready.
◾ And if we now want to integrate the measured values of the AI solution?
Then we simply tell the language model: Now you also have input C. These are the measured values of the AI solution, which you add to the findings at the appropriate points.
This is exactly what Large Language Models can do perfectly. That is what they are for, and that is what is going to happen in medicine in the next few months.
43 DI EUROPE · SUMMER 202 3
From the point of view of a clinical organization, the hospital does not only consist of radiologists. In clinical practice, you need a platform that is broader, addresses all clinical departments, and can be used by both the radiologists and clinical physicians.
All
https://www.nuance.com/
images: Nuance Communications GmbH





 6,000 delegates attended EAN 2023 at Hungexpo in Budapest, Hungary
6,000 delegates attended EAN 2023 at Hungexpo in Budapest, Hungary
Brain Health Takes Center Stage at EAN 2023
by Mélisande Rouger
Nearly 8,000 delegates gathered both onsite and online for EAN 2023, the 9th annual meeting of the European Academy of Neurology (EAN) that unfolded on July 1 – 4 in Budapest, Hungary.
EAN is a young society ready to embark the future, according to EAN president Prof. Paul Boon, who delivered his Welcome Address in the Opening session on the first day of the conference.
“We are a growing community, with more than 45,000 members from more than 47 countries,” he told a packed audience in the Main Auditorium of Hungexpo, which hosted the meeting this year.
With an all time high of submitted (2,318) and accepted abstracts (1,912), EAN 2023 delivered the latest research in neurological disorders including stroke, dementia, movement and sleep disorders, and rare neurological diseases.
Brain health demands more cooperation
Brain health was a special focus of the meeting this year and neurologists expressed concern about the steeply rising prevalence of brain diseases worldwide.
“At least one in three people will have a neurological disorder, but new data not yet published indicate that this number may be higher, actually 40 percent,” Boon
said. “And to make things worst, it’s increasing.”
Neurological disorders are the single most important contributor to disability-adjusted life year (DALYs) and early mortality. “The cost of all cancers added to the cost of all cardiovascular diseases together is inferior to the cost of neurological disorders,” he said. “It’s a tremendous burden to society.”
This burden demands a holistic approach that goes far beyond diagnosis and treatment. “Most of the people with brain conditions may not have access to diagnosis, he explained.
The situation demands urgent action from all stakeholders, echoed Prof. Claudio Bassetti, EAN Past
45 DI EUROPE · SUMMER 202 3
Image: © kras99 stock.adobe.com
President and Vice President of the European Brain Council. “It’s time we work together across different disciplines of neuroscience to try to maximize the ways to diagnose, rehabilitate and also prevent diseases,” he said.

The EAN has produced the “One Brain, One Life, One Approach” white paper, detailing its approach for brain health in Europe, including strategic pillars such as awareness, education, intersectoral approach, and research. The EAN also launched a major initiative in its headquarters in Vienna to bring all stakeholders beyond medical associations and companies, and also organizes the Brain Health Summit. “We are in a network where different health providers need to work together across the countries, and also across the continent,” Bassetti said.
Huge amount of data and AI
Another overarching theme of the congress was big data, and experts
discussed challenges and opportunities of the rising tide of data neurologists now have to deal with. “The amount of data available in neurology, neuroscience, neurobiology and related disciplines is rising exponentially and challenging clinicians’ ability to analyze and use those data,” said Prof. Maria J. Molnar from Budapest, Hungary, who co-chaired a dedicated session with Prof. Charlotte Cordonnier from Lille, France.
“Data available range from routinely collected clinical data and population health data, through genomics and other omics and to clinical diagnostics – i.e. MRI and neurophysiology,” she added.
Cordonnier, a professor of neurology and head of the department of neurology and stroke center at the Lille University Hospital, focused on multi-modal data approaches to predict clinical outcomes after stroke. “We have to combine different types of data – from medical
imaging, demographics, biology medical imaging data and clinical assessment – and observe how they interact with each other to predict clinical outcomes after stroke,” she said.
Clinicians already combine different data every day when they assess outcome after stroke, for example with the ICH score. But there are limitations to human decision making capacities, Cordonnier insisted. “It is challenging to be able to integrate and generate predicting modeling, due to data heterogeneity and the different semantics of all these variables,” she said.
Machine learning-fed algorithms could enhance the ability to capture a broader range of stroke-related factors and their interactions, leading to more robust predictive models, she concluded.
46 DI EUROPE · SUMMER 202 3 EAN 2023
https://www.ean.org/congress2023
EAN President Paul Boon talking in a panel moderated by Conny Lee (left), with EAN Past President Claudio Bassetti, Prof. Carlayne Jackson, President of the American Academy of Neurology, and Vladimir Hachinski, professor of Neurology and Epidemiology at Western University Ontario in Canada and former President of the World Federation of Neurology.
47 DI EUROPE · SUMMER 202 3 Cardiovascular and Interventional Radiological Society of Europe CIRSE 2023 9-13 Copenhagen SEPT www.cirse.org BUILDING BETTER CARE produced by LOOP.ENTERPRISES media www.loop-enterprises.com
The Changing Face of Cardiology and Imaging’s Role
Three diseases particularly contribute to CVD burden: intracerebral hemorrhage, ischemic heart disease and ischemic stroke. These last two diseases are actually the major cause of death worldwide. “CVD causes almost 18 million deaths per year,” he said. “That’s almost the double of cancer, which is another terrible disease.”
However, the progress that cardiovascular medicine has made recently is second to none, he was quick to add. “Looking at life expectancy in the United States over a time period of 30 years, the average life expectancy increased by nearly six years,” he said. “That’s mainly due to improvements in treatment and management, and, to some extent, prevention of CVD, especially coronary artery disease.”
By Mélisande Rouger
Cardiology is undergoing massive changes as prevalence of cardiovascular disease continues to increase while resources decrease. Imaging can help in more than one way, a leading German cardiologist explained at EACVI 2023 on May 10 – 12 in Barcelona, Spain.

The burden of cardiovascular disease (CVD) is tremendous and varies from country to country, accord-
ing to Stephan Achenbach, Chairman of the Department of Cardiology at Friedrich-Alexander-University of Erlangen-Nürnberg, Germany. “The burden is very high in central Asia, eastern Europe and Africa,” Achenbach told delegates in the keynote lecture that kickstarted the first unified multi-modality meeting of the European Association of Cardiovascular Imaging (EACVI). “There’s a lower burden in western Europe, Australia and high income North America.”
In spite of the strides made in CVD management, the burden is not decreasing – quite the opposite. While 12.3 million patients died of cardiovascular disease in the world in 1990, 17.3 million did in 2013 – a 41 percent increase. So what is causing this paradox? Although treatment has improved, the increasing population and especially the number of elderly patients are causing more CVD deaths every year. The increasing population is responsible for more than 25 percent of cardiovascular deaths and more than 55 percent are due to aging,” Achen-
48 DI EUROPE · SUMMER 202 3 EACVI 2023
bach said. “These deaths overcompensate by far the improvements we’ve made in CVD management.”
More patients, older patients: a ticking time bomb
It is important to remember that CVD are diseases of the older age, he argued. “In Germany, for example, there is an exponential increase in the prevalence and number of deaths when age goes beyond 70 in women and 60 in men. CVD in the aging population is exponentially more frequent than in younger cohorts.” The prevalence of valvular heart disease in particular increases exponentially as the population grows older, a trend which is expected to continue over the next decades, with a massive growth in the number of people aged 70 or more. “If there’s an exponential increase of valvular heart disease with age, even a slight increase in the average patient population will lead to a massive increase in the number of patients who will need CVD care. That is something we cannot neglect,” Achenbach said.
The phenomenon is already tangible in hospitals, he added. “You can feel how the number of patients is increasing from year to year. And this is only the beginning.” In a study looking at heart failure (HF) in four million patients between
2004 and 2014 in the UK, researchers observed a two percent increase in HF incidence, a 12 percent increase in annual new diagnoses and a 23 percent increase in HF prevalence, due to the increasing volume of elderly patients. With aging, the number of comorbidities is also increasing. The average number of significant comorbidities in patients with HF was 3.4 in 2004 and 5.4 in 2014. “Comorbidities become more and more frequent because patients are getting older,” he said. “There’s so much we can and should do. But there’s also a problem of resources.”
In Germany, 1.2 million 65 yearold people leave the workforce every year, compared with 750,000 20 year-olds who start working. “The newcomers want a better work life balance than in the past and the boomers who leave the workforce will live longer than ever before,” he said. “We don’t have a solution, but this will be a problem for cardiology and medicine in general.”
Cardiac imaging has a tremendous opportunity to make cardiovascular care more effective and efficient – by helping make more accurate diagnoses and better therapeutic decisions based on imaging findings, and by guiding interventional procedures to ensure
Prof. Dr. med. Stephan Achenbach is Chairman of the Department of Cardiology and Professor of Medicine at the University of Erlangen, Germany. His main clinical interests and areas of research are cardiac interventions and cardiac imaging with a special focus on computed tomography of the heart and the use of imaging to support coronary and structural interventional procedures.
their optimal effect and avoid complications, especially in the elderly.
“Along with the changes that AI will bring about in imaging, by relieving imagers from repetitive tasks, and by providing tremendous potential to enhance diagnostic and prognostic accuracy, I expect a massive change from the traditional “diagnostic“ role of cardiac imaging, which will become an essential component of therapeutic management,” he said.
This will be a challenge and come at a cost, he conceded. “Imagers will need to have highly specialized knowledge not only in imaging, but also in disease etiology and therapeutic options. If we want to be valuable as imagers, we have to acquire this knowledge otherwise it’s going to be the interventionist reading the imaging scans and making their own decisions. We really have to keep that in mind,” he concluded.
https://www.escardio.org/ Congresses-Events/EACVI-Congress
Stephan Achenbach was the President of the Society of Cardiovascular Computed Tomography from 2005 to 2007, as well as the President of the European Society of Cardiology (ESC) for the mandate 2020 to 2022.

49 DI EUROPE · SUMMER 202 3
Companies Unveil New MSK Solutions at ESSR 2023
By Mélisande Rouger
Musculoskeletal (MSK) disorders are the leading contributors to disability worldwide and are expected to increase, partly due to an aging population and rising incidence of obesity.
To meet the upcoming challenges in MSK imaging, 900 specialists gathered at the annual meeting of the European Society of Skeletal Radiology (ESSR) on June 22 – 24 in the Euskalduna Conference Center, overlooking the River Nervión in Bilbao, Spain.


The main topic of the congress was ankle and foot imaging, and speakers reviewed the most significant advances in the field from a multidisciplinary perspective.
Besides the traditional ultrasound course offered each year at the meeting, the program featured three workshops on spondyloarthritis, a group of arthritis conditions that affect bones in the spine and nearby joints, causing pain and inflammation.
Sessions on Thursday June 22nd, the first day of the congress, also focused on artificial intelligence (AI),
while subcommittees organized dedicated workshops.
AI-boosted ultrasound systems in the limelight
With barely 20 companies displaying their products in the main hall of the building, the technical exhibition was buzzing with activity, networking and new equipment. Some of the main manufacturers were present, and a quarter of the exhibitors were AI software developers, reflecting the growing interest of MSK radiologists in such solutions to ease workflow.
50 DI EUROPE · SUMMER 202 3 ESSR 2023
Technical exhibition in the main hall of Euskalduna
French company Gleamer presented its BoneView measurements and BoneView Bone Age solutions. Three other French companies –AZMed, Milvue and Incepto, a platform provider – were also present at the show, while Bulgariabased SmartSoft Healthcare featured CoLumbo, its AI assistant software for the interpretation of lumbar spine MR scans.

Austrian provider IB Lab showcased its animal-inspired ZOO portfolio that covers the leg, knee, hand, hip, spine and foot, and launched SQUIRREL, its newest tool to expedite and improve assessment and monitoring of scoliosis.
The industry was also very much present in the scientific program, with two main manufacturers holding dedicated symposia featuring key opinion leaders in the field.
On Friday, ESSR President Professor Carlo Martinolli, head of the imaging department at University Hospital Genoa, Italy, gave an impressive lecture on challenges in small nerves imaging.
“Most of those nerves running in the arm and forearm are forgotten,” he said. “They are so tiny and so superficial that they’re very hard to see using conventional transducers.”
Probe in hand, he showed a mesmerized audience how to image small nerves of the upper limb with a Philips EPIQ Elite advanced ultrasound system installed directly on stage.

ESSR immediate past president Doctor Eva Llopis, a radiologist at the European Musculoskeletal Institute (IMSKE) in Valencia, Spain, shared her tips on how to efficiently use MRI and manage requests in MSK studies.
“There’s an increased demand for MRI scans in any specialty and especially in MSK, but resources are limited both in equipment and technology,” she said. “Many factors such as increased average age and sports practice, particularly in older patients, are causing this growing demand. (We have to consider) the importance of activity combined with sarcopenia, a type of muscle loss that occurs with aging and / or immobility.”
On Saturday, Prof. Martinolli also spoke about exploring elbow ligaments with the next generation high-frequency probes during a symposium organized by Italian manufacturer Esaote, who showcased its recently launched MyLab X-90 advanced ultrasound system.
https://www.essr2023.org/
51 DI EUROPE · SUMMER 202 3
Prof. Martinolli showing small nerves of the upper arm
ESSR 2023 delegates enjoying a break in sunny Bilbao


52 DI EUROPE · SUMMER 202 3
More than 6,000 visitors came to Vienna to learn about the latest trends and technology in radiotherapy.
ESTRO 2023’s industry exhibition featured technologies and services covering the entire patient pathway from screening to aftercare.
BrainLab’s newest solution ExacTrac Dynamic Surface, was designed specifically for surface-guided radiotherapy (SGRT).

ESTRO 2023: Newest Advances in Tumor Movement Detection
The current challenge in radiotherapy is to network the entire spectrum of cancer treatment to enable more efficient and individualized therapies in inpatient and outpatient care.
By Guido Gebhardt
The ESTRO 2023 industry exhibition featured technologies and services that covered the entire patient pathway from screening to follow-up. Vendors placed particular emphasis on integrated and automated workflows to improve treatment decisions and outcomes.
One such workflow is to go from planning a CT or MRI examination to a finished radiation plan with as few clicks as possible. AI algorithms help to segment the tumors faster and more precisely in order to protect the healthy tissue surrounding the lesions as much as possible.
The individual companies also presented different methods that detect tumor movement during irradiation and interrupt therapy if necessary. Here, too, the primary goal is to protect healthy tissue in order to continue therapy after correcting patient movement. Thus even the smallest move-
ments are detected and can be taken into account during radiation therapy to ensure that the treatment is as precise and safe as possible.
While Siemens Healthineers and Varian are taking a one-stopshop approach, several other vendors have joined forces under “unite RT” to allow users to assemble their own heterogeneous “best of breed” solution from their favorite vendors.
Siemens Healthineers and Varian unveiled a CBCT imaging solution called Connected Imaging, which is available for the Halcyon and Ethos systems. The 86-by-43-centimeter detector provides more accurate images in less time, indicating tumor change and

enabling rapid therapy adjustment. “If we want to help create a world without fear of cancer, we need to look beyond the treatment room and consider how we can work with our customers to use our technology to optimize the treatment pathway,” said Kevin O’Reilly, president of Radiation Oncology Solutions at Varian
BrainLab is also focusing on active motion management with ExacTrac Dynamic Surface, a new product in the ExacTrac Dynamic line designed specifically for surface-guided radiation therapy (SGRT). The system projects a structured blue light pattern onto the patient’s body surface, which is captured by two 3D cameras located in the same unit. Each surface point is assigned a heat signature, which is registered by a third camera in the unit to increase the precision of the irradiation based on thermal information.
53 DI EUROPE · SUMMER 202 3
Siemens Healthineers and Varian showcased a CBCT imaging solution under the Connected-Imaging banner, available on the Halcyon and Ethos systems.
Image: Brainlab AG
Image: Siemens Healthineers
“ExacTrac Dynamic Surface is about more than just surface monitoring,” said Stefan Vilsmeier, founder and CEO of Brainlab. “This further development is based on the extensive know-how we have gained in thirty years of innovations in the field of radiation therapy.”
GE HealthCare showcased three innovations in radiation oncology with intelligent Radiation Therapy (iRT), Auto Segmentation and an updated Magnetic Resonance (MR) Radiation Therapy Suite (AIR Open Coil Suite).
Key features of the iRT platform include an integrated workflow that connects multiple applications in one intuitive interface, multi-vendor interoperability that connects existing RT systems through an automated back-end service, seamless data transfer and task automation, and a catalog of RT applications from GE HealthCare and third-party vendors.
With the introduction of Automated Segmentation, GE HealthCare is also streamlining the process of delineating organs at risk (OARs). Delineation of OARs helps ensure that a patient’s tumor receives the maximum dose of radiation therapy while minimizing exposure to surrounding tissue.

In addition, the company showed the AIR Open Coil Suite, three separate AIR coils designed for a clinically beneficial signal-tonoise ratio, and a new table design that accommodates all necessary patient immobilization equipment as well as eliminates the need to purchase a separate couch.
“These new technologies can help transform the future of radiation therapy by optimizing and accelerating the oncology treatment pathway, as we know this is critical to the outcomes of patients fighting cancer around the world,” said Ben Newton, PhD, general manager for oncology solutions at GE HealthCare.
The latest version of RaySearch’s RayStation includes new and updated segmentation models for automatic contouring using machine learning techniques and support for brachy planning with Elekta Flexitron afterloaders. Other highlights include robust evaluation on multiple images, new and much faster electron Monte Carlo dose engine, and improvements for CyberKnife planning.
Users of RaySearch’s oncology infiormation system RayCare saw several improvements to the patient chart, including usability and efficiency enhancements such as user configured templates for selected workspaces and a new patient chart feature providing support for financial accounts for charge capture. The latest version of RayCare also offers improved connectivity and opportunity for seamless integration to other hospital information systems by the addition of new external interfaces.
The latest version of Research’s RayStation includes new and updated segmentation models for automatic contouring using machine learning techniques.
54 DI EUROPE · SUMMER 202 3 ESTRO 2023
Image: RaySearch Laboratories
Johan Löf, founder and CEO of RaySearch, said: “Being at ESTRO and having the ability to interact with many customers in a short time frame are always one of the highlights during the year. At RaySearch, we believe that open interfaces and joint collaborations are an important step towards further advancements in the field of radiation therapy.”
In addition to GE HealthCare and RaySearch, Infinitt has joined the unite RT initiative with RT PACS to streamline the radiotherapy workflow. RT PACS is a dedicated Radiotherapy Treatment (RT) image and data management solution optimized to streamline the oncology workflow.
In total, more than 6,000 visitors came to Vienna to learn about the latest trends and technology in
radiotherapy. ESTRO 2024 will be held in Glasgow from May 3 to 7.
https://www.estro.org
Diagnostic Imaging Europe (DI Europe) is the leading pan-European online resource for news and interaction for medical imaging professionals.

Continuing the tradition set by aDiagnostic Imaging, a respected newspaper founded in 1985, DI EUROPE provides extensive coverage of the latest trends and developments in diagnostic and interventional radiology.

The publication tackles issues related to radiology business and education of imaging professionals to help them improve patient care. www.linkedin.com/company/diagnostic-imaging-europe
info@dieurope.com
GE HealthCare’s AIR Open Coil Suite consists of three separate AIR coils designed to provide a clinically beneficial signal-to-noise ratio.
Image: GE Healthcare Image:
© Kzenon stock.adobe.com
www.dieurope.com

























 By Mélisande Rouger
By Mélisande Rouger


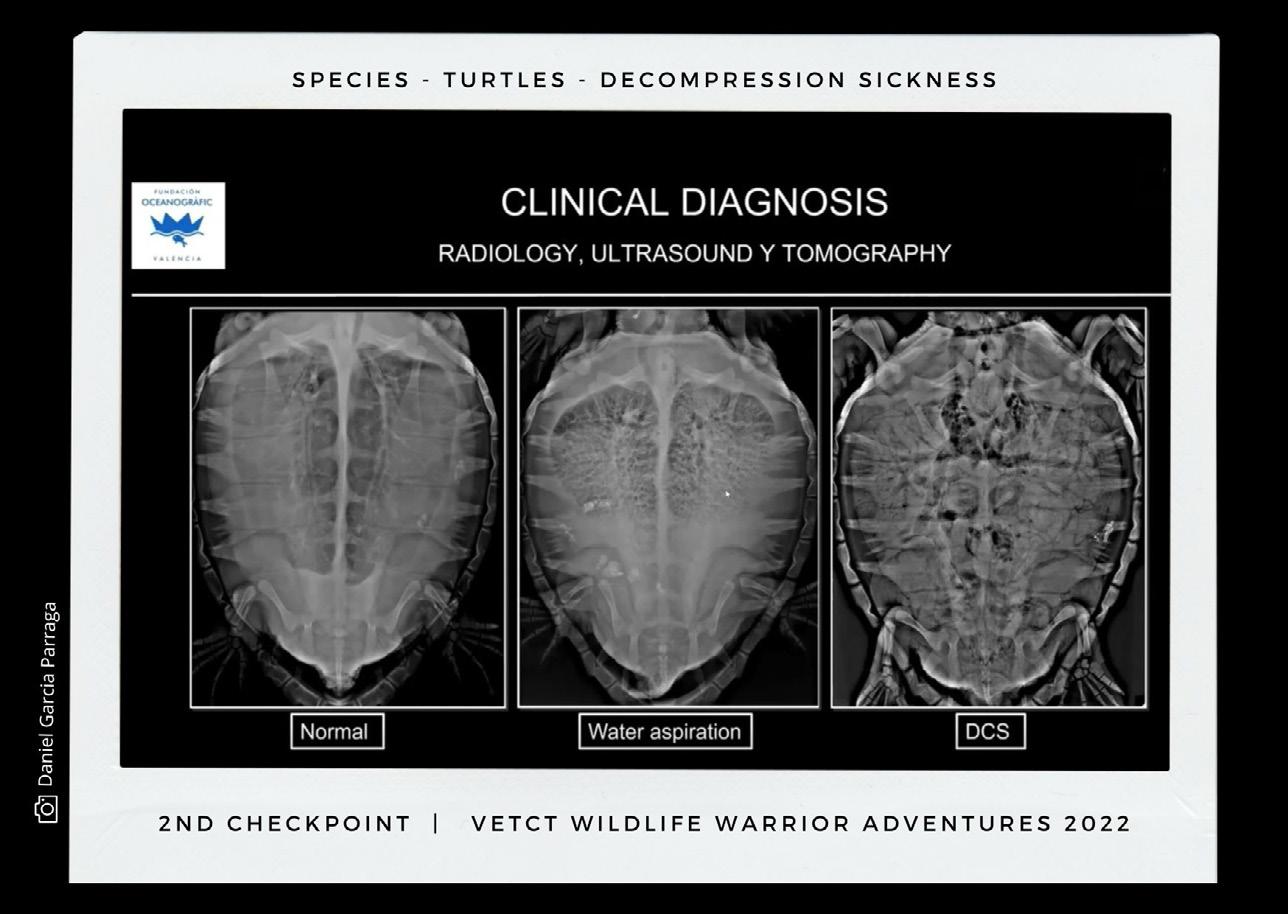








 By Mélisande Rouger
By Mélisande Rouger














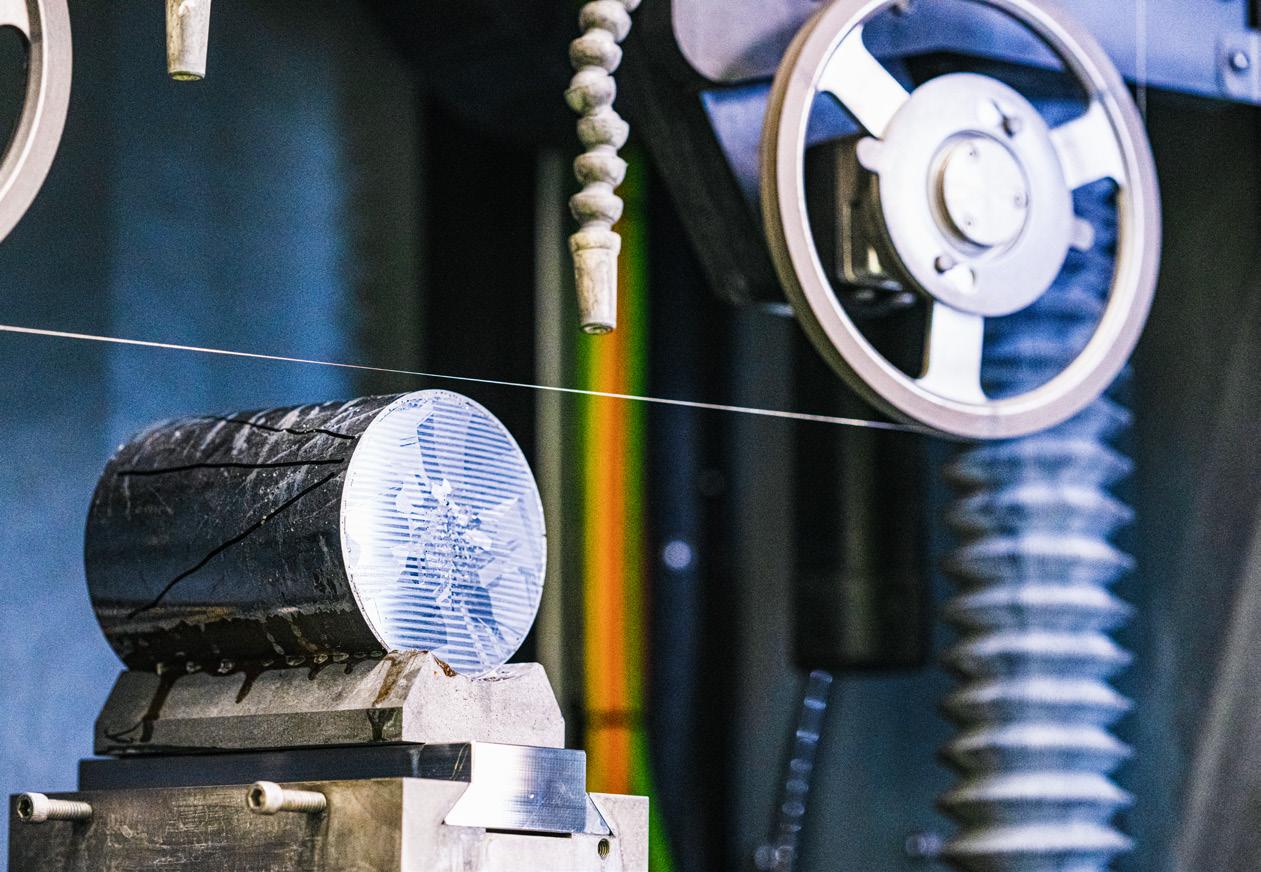












 By Guido Gebhardt
By Guido Gebhardt






 6,000 delegates attended EAN 2023 at Hungexpo in Budapest, Hungary
6,000 delegates attended EAN 2023 at Hungexpo in Budapest, Hungary













