




Welcome to the unit ‘Confirm Physical Health Status’. This unit is one of the most comprehensive units in this course and is broken into two vital sections. Part one contains in-depth information regarding the anatomy and physiology of the human body, and part two outlines how to apply this knowledge to confirm a client’s health status.
Anatomy and physiology can seem overwhelming or daunting topics to tackle, but this unit starts at the very beginning and slowly builds up to the more complex aspects. For nutrition coaches to understand how food behaves within the body, they must first understand how the body works and how it utilises nutrients and energy.
Part one begins by explaining the basics of anatomy and physiology and common terminology that a nutrition coach will encounter throughout this unit. This section involves learning about the anatomy of organs, their structure and function, the processes these systems undertake, and their overall role in maintaining life. Nutrition coaches will thoroughly understand the human body’s synergistic nature and how vital these systems are for a healthy life.
Part two of this unit focuses on identifying the many factors that come into play to confirm a client’s health status and the necessary underpinning knowledge needed to do so. Further, this unit also covers processes responsible for supporting the healthy functioning of the human body, such as homeostasis, maintaining electrolyte balance and blood pressure, and the importance of regular physical activity.
Part two of this unit then takes the nutrition coach through a step-by-step process of the very important skill of confirming a client’s health status.
Nutrition coaches will learn:
• How to conduct screening processes with their clients
• When to refer clients to allied health professionals
• How to adequately gather necessary information from the client
• How to review the client’s current diet and exercise
• How to determine a client’s body composition
• How to make recommendations on how clients can achieve their ideal body weight.
Not only is this unit essential for understanding and implementing the rest of the information that will be held within this course, but it is also beneficial for the future practice of all nutrition coaches.
This unit will allow a nutrition coach to:
• Obtain a thorough and necessary understanding of the human body and how it works
• Obtain a better understanding of how food affects human physiology and how it is used within the body
• Obtain accurate information about physical health status through observation, questioning or review of documentation
• Recognise and promote ways to support the healthy functioning of the body
• Use the information to identify any actual or potential problems regarding health status.

The human body is an extremely complex organisation of various systems working simultaneously to ensure its health and survival. Understanding the anatomy (structure) of the human body and physiology (function) is crucial for any health professional, including nutrition coaches.
Anatomy and physiology are the most crucial part of the human body, upon which everything else is based. Gaining thorough knowledge of the basic anatomy and physiology of the human body will allow a greater understanding of the entire course and, in turn, enable better service to clients through confident explanations of relevant topics relating to health and nutrition. This will also allow nutrition coaches to fully comprehend information and apply problem-solving skills instead of simply rote learning.
ANATOMY
Anatomy relates to structure.
PHYSIOLOGY
Physiology relates to function.
EXAMPLE 1 (scientific explanation)
A human heart is a muscular organ located in the thoracic cavity (anatomy), with the function (physiology) of pumping blood around the body to distribute oxygen and nutrients.
EXAMPLE 2 (non-scientific explanation)
Consider an anatomist and a physiologist examining an apple. The anatomist would look at the size of the apple, the apple’s location and what the apple is made of, whereas the physiologist would look at the purpose of an apple (e.g., to provide nutrition).
INTERACTIVE ANATOMY AND PHYSIOLOGY
The Get Body Smart website is an excellent online tool that students can utilise as an additional (optional) resource. This website allows students to learn, navigate and examine human anatomy and physiology.
CLICK HERE to view the link.

ANATOMY
Anatomy means ‘cutting open’, with Greek roots originating more than 1500 years ago.(1) The study of anatomy traditionally depended on cutting up or dissecting, but now, with imaging technology, it is increasingly possible to see how a body is made up without dissection.
Anatomy combines medical and biological study, with its main emphasis on studying the structure of all living things. This can include animals, humans and plants; however, as a nutrition coach, the main concern is the human body.
Anatomy is considered one of the oldest medical sciences, with anatomical drawings from Egyptians dating back to approximately 1600 BC! Their drawings illustrated the basic layout of blood vessels in the human body.
In recent years, there have been tremendous scientific advances whereby a much deeper understanding of the human body has been established.
There are two different ways of looking at anatomy, which include:
• Gross (or macroscopic) anatomy
• Microscopic anatomy.

Gross anatomy refers to the study of relatively large structures and features visible to the eye, which can be clearly seen without assistance from a microscope.
Within gross anatomy, there are many different forms, and these include:
SURFACE ANATOMY
REGIONAL ANATOMY
SYSTEMIC ANATOMY
DEVELOPMENT ANATOMY
CLINICAL ANATOMY
The study of general form and superficial markings.
The study of the anatomical organisation of specific areas of the body. For example, the neck, head, trunk or limbs.
The study of the structure of human organ systems (also known as body systems), which are groups of organs that coordinate to perform the main function.
This area of study focuses on the changes in form between conception (fertilisation) and physical maturity.
This area includes a number of sub-specialisations that are considered imperative in clinical practice.
This includes:
• Pathological anatomy (anatomical features that adapt or change during illness)
• Radiological anatomy (using specialised imagery, i.e. X-rays, to see and observe anatomical structures)
• Surgical anatomy (anatomical landmarks relevant to surgery).
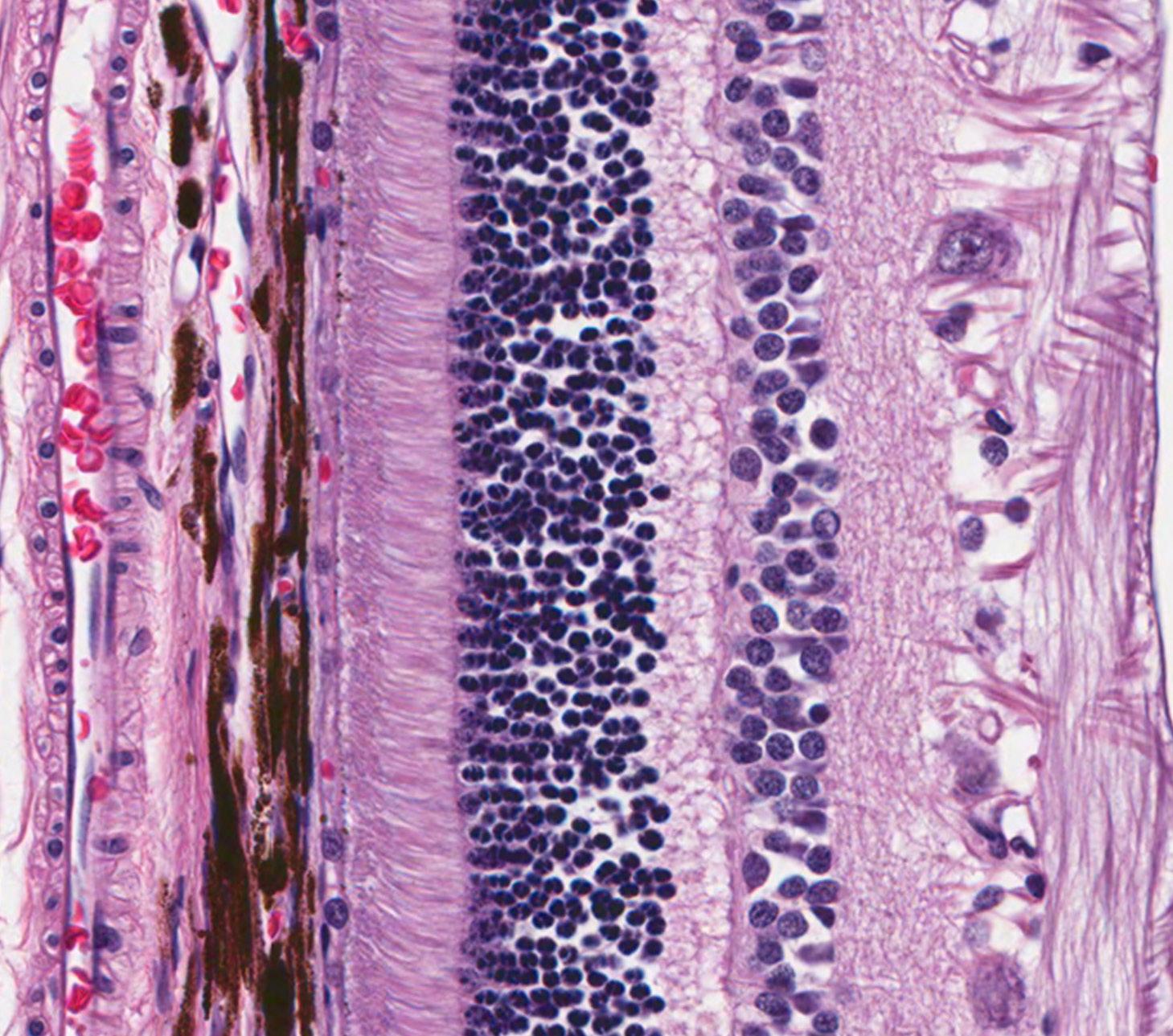
Microscopic anatomy is the opposite of gross anatomy in that a person would need to utilise a microscope to view the tissue or cell of interest. Microscopic anatomy can often be limited due to the specialised equipment required. There are two main subdivisions relating to microscopic anatomy; cytology and histology.
The suffix -logy, or -ology, means the ‘study of’. To find out what is being studied, look to the prefix cyto, which means ‘cell’.
CYTOLOGY
HISTOLOGY
Cytology is an area of science that studies how cells function and grow and what they are made of.
The suffix -logy, or -ology, means the ‘study of’. To find out what is being studied, look to the prefix histo, which means ‘tissue’.
Histology is an area of science that studies microscopic structures, chemical composition and how humans, animals and plants tissue (or tissue systems) function.
Physiology is another Greek term, and, as previously mentioned, it refers to the function of anatomical structures for living organisms. In other words, it refers to how a living organism (i.e. the human body) works, as opposed to its structure. As a nutrition coach, the main concern is human physiology.
Human physiology is very complex and much more difficult to study than the majority of anatomical structures. Due to its complexity, there are many specialisation areas related to human physiology; these areas are briefly discussed in the table below:
CELL PHYSIOLOGY
ORGAN PHYSIOLOGY
SYSTEMIC PHYSIOLOGY
PATHOLOGICAL PHYSIOLOGY
The study of cells: considering events at the chemical and molecular level, chemical processes and interaction within cells.
Organ physiology is the area of study that focuses on specific organs. For example, the study of how the heart functions are referred to as ‘cardiac physiology’.
Includes studying all aspects of how specific body systems (organ systems) function. For example, the cardiovascular system.
Refers to the study of the effects that disease can have on the correct functioning of organs or body systems.
SYSTEMIC PHYSIOLOGY
The study of human anatomy and physiology are closely interconnected medical sciences that are usually taught simultaneously. This is because information regarding human anatomy is significant to the examination of physiology. Likewise, physiology is important for those who want to learn about the performance of the diverse anatomical structures in the human body.
PATHOLOGICAL PHYSIOLOGY
‘Anatomy and physiology are closely integrated, both theoretically and practically. Anatomical information provides clues about functions, and physiological mechanisms can be explained only in terms of the underlying anatomy.’(1)
Anatomy and physiology are an extremely important part of any health professional’s basic knowledge, particularly nutrition-based health professionals, such as nutrition coaches.
The reasons for this are discussed below:
• Ability to confidently offer explanations about the body to clients: Nutrition coaches need to know how the body and its various systems work to know how food works within the body (how it is digested and absorbed etc.). Knowing this will allow the nutrition coach to explain to clients why it is important to implement certain changes or to explain certain symptoms.
• Understanding food at a chemical level:
All food is made up of and broken down into simple molecules such as amino acids (protein), fatty acids (fat) and glucose (carbohydrates). Understanding the chemical science behind food enables nutrition coaches to effectively explain to their clients how the body uses these molecules and cater to their individual needs/nutritional requirements.
• Understanding that the body only functions with optimal vitamin and mineral intake:
Along with the macronutrients mentioned above, vitamins and minerals are used widely within the body for multiple processes. To understand the importance of these micronutrients and their role in optimal functioning, a nutrition coach must know the various physiological processes that utilise vitamins and minerals.
• Understanding the effects of nutrient deficiency:
Understanding anatomy and physiology is not confined to how the body operates when everything is working perfectly; it also includes what happens when it is not working at its peak. For example, inadequate macronutrient and micronutrient intake will negatively impact various human body parts. When the body becomes deficient in certain nutrients, it is vital for a nutrition coach to understand how this affects the body and to help rectify the deficiency.
• Ability to explain the importance of the digestive system:
A thorough understanding of the digestive system and associated systems is fundamental knowledge in how food is digested, absorbed, utilised and excreted. Without the body system’s foundational anatomical and physiological knowledge, nutrition coaches would struggle to cater effectively to their client’s needs and nutritional requirements.
• Understanding foundational knowledge at the cellular level:
Cells rely on adequate nutrition to function optimally; without optimal function at the cellular level, the rest of the body suffers. As a result, nutrition coaches need to know and understand the anatomy and physiology of the body’s numerous cells. Understanding how cells are made, their functions and what happens if they are not looked after will allow for a deeper appreciation of the human body and why it requires certain nutrients in certain amounts.
• Ability to recognise healthy body systems and when a client may fall outside of a nutrition coach’s scope: A crucial aspect of a nutrition coach’s role is recognising when a client may fall outside their scope of practice. To do so, a nutrition coach must have a thorough understanding of the anatomy and physiology of the various body systems to detect the warning signs that may suggest a client is outside their scope. For example, if a client presents with severe bloating, constipation and other digestive issues, recognising these as signs of an unhealthy body system, which requires an allied health professional’s diagnosis, is extremely important for the safety and health of the client.
In the early days of anatomy and physiology, scientists struggled with communicating specific information and identifying exact locations on the body. As a result, anatomical terminology was developed to solve these communication errors. This terminology is based on:
• Word roots:
Basic, meaningful parts of a word which cannot be used as another term with another definition. For example, ‘anatome’ is the word root for ‘anatomy’.
• Prefixes:
A word segment that attaches to the beginning of the word to alter or modify its meaning but cannot stand alone. For example, the prefix ‘ana-’ means up, and the prefix ‘path-’ means disease.
• Suffixes:
A word segment that attaches to the end of a word to form another word. For example, the suffix ‘-tomy’ means to cut, and the suffix ‘-ology’ means to study.
• Combining Form:
Independent words that work with those mentioned above to build a new term.
Therefore, when joining these examples of prefixes and suffixes, the word anatomy means ‘to cut up, and the word pathology means the ‘study of disease’. Below is a list of commonly used anatomical/medical prefixes, roots and suffixes:
ANATOME Root word for ‘anatomy’
DENT Tooth
HAEM(ATO) Blood
NUTRI Nourish
SOMAT(O) Body
-OLOGY To study (science of)
-ITIS Inflammation
CYTO- Cell
NEURO- Nerves
HYPER- OR SUPRA- Excessive/above
INTER- Between
SYN- Together with PRE- Before
POD-, -POD- OR PED- ‘of’ or pertaining to the foot
MUSCUL(O)- Muscle
-RRHEA Flowing discharge
-LYSIS Separation/destruction
PSEUD- Denotes something is fake or false
MON- Single
-ERIOR Indication of position
ANTERIOR Front/ventral
ANA- Up CARDI Heart
GASTR(O) Stomach
THORAC(O) Chest
-TOMY Incision
PATHY Disease
-AEMIA Condition of blood
HISTO-, HISTIO- Tissue DERMA- Skin
HYPO - OR SUB- Below/beneath
INTRA- Within /Inside
POST- After
SUPER- In excess, superior or above
-METER
Instrument used to count or measure
DYS- Painful/difficult
HYDR(O)- Water
LIP(O)- Fat
NAS(O)- ‘Of’ or pertaining to the nose
THERAP- Treatment
INFERIOR Low or low in position
POSTERIOR Back/dorsal
In anatomy and physiology, the body’s features are identified in reference to other body parts. As a result, there is a standardised point of reference known as the anatomical position. The anatomical position is sometimes referred to as the ‘anatomical starting position’, ‘neutral position’ or ‘fundamental starting position’.
Just like maps, which are oriented with north at the top, the standardised map for the body, or anatomical position, is when the body is in a standing/upright position, with feet parallel at shoulder width apart and toes pointing forward.
The arms are resting on each side of the body, and the palms of the hands face forward, as shown in the image below:
ANATOMICAL POSITION ANATOMICAL POSITION
The purpose of this terminology and the anatomical position is to increase precision when referring to parts of the body and to reduce medical errors. Thus, nutrition coaches must become familiar with this terminology, particularly when working collectively with general practitioners (GPs), dietitians, naturopaths, psychologists, and fitness professionals.
Understanding relevant anatomy and physiology terminology is imperative as a nutrition coach working in the health and wellness industry. By learning and utilising relevant health terminology, nutrition coaches can effectively communicate with other professionals that also fall within the health, fitness or wellness industry, such as but not limited to general practitioners (GPs), dietitians, naturopaths, psychologists and fitness professionals.
As a nutrition coach, there are also many benefits to utilising appropriate anatomical and physiological terminology within the health and wellness industry.
These include:
• Standardised communication between professionals
• Improved client safety
• Improved client experiences and confidence.
STANDARDISED COMMUNICATION BETWEEN PROFESSIONALS
IMPROVED CLIENT SAFETY
Using standard terminology within the health industry helps nutrition coaches communicate with other health professionals by understanding a client’s specific condition or issue.
Understanding a client’s particular goal, condition or issue can assist a nutrition coach in interpreting complex information and, in turn, help determine if the client is within their scope of practice.
By effectively communicating among all professionals within the industry, a nutrition coach can improve a client’s safety simply by reducing the number of mistakes. For example, suppose a nutrition coach knows the client’s full health history, including any prior conditions or health/nutritional concerns. In that case, it assists that nutrition coach in developing a safe, effective solution for that client.
If, on the other hand, the terminology is misinterpreted or incorrect language is used, this can make a significant difference in the care the client receives, and, in some cases, it may put the client at risk.
When nutrition coaches understand and utilise relevant anatomical and physiological terminology, this can also benefit the client as they too can learn what specific terminology means.
IMPROVED CLIENT EXPERIENCES AND CONFIDENCE
Educating clients can then assist them in taking a more active role in the process of achieving their goals, and the nutrition coach is more likely to experience improved client satisfaction.
Knowing and using appropriate terminology as a nutrition coach can also help instil confidence in clients and assure them that they have chosen the right health professional to assist them with their goals.
The human body is extremely complex; it has excellent organisational properties. Learning this organisational structure as a nutrition coach can be beneficial and assist in visualising and understanding how the human body is constructed and functions.
There are six levels of structural organisation; these include:
1. The chemical level
2. The cellular level
3. The tissue level
4. The organ level
5. The system level
6. The organismal level.
It is important to be aware that before a nutrition coach can appreciate the human body’s various systems, an understanding of the six levels of organisation must be gained. This understanding gives a nutrition coach an advantage in understanding the human body and the ability to adequately confirm the physical health status of a client, before beginning any health or nutrition-related interventions.
The smallest level of organisation is the chemical level. Atoms are the smallest stable chemical units in chemistry and are the most basic chemical building blocks. When atoms are combined in unique combinations called molecules, they form large and complex organisms such as humans, plants and animals.
Atoms are essentially microscopic units of matter. There are billions upon billions of atoms that form larger organisms. An average 70kg human body is made up of approximately 7x1027 atoms, which is essentially a seven followed by twenty-seven zeros!(2)
Number of atoms in the human body = 7, 000, 000, 000, 000, 000, 000, 000, 000, 000.
There are two major types of chemical reactions which are important for nutrition coaches to understand.
These chemical reactions are called:
1. Catabolism (or degradation)
2. Synthesis (or anabolism).
CATABOLISM
SYNTHESIS
A chemical reaction that breaks a molecule into smaller fragments. For example, a client who consumes inadequate protein and nourishment may experience catabolism of muscles (the breakdown and wastage of muscle).
A chemical reaction which two (or more) simpler substances combine to form a more complex substance. For example, two hydrogen atoms and one oxygen atom come together to form water (H20).
Hydrogen is a colourless, odourless, highly flammable gas with an atomic number of 1.
Comprehending and interpreting the simplest units of the body allows a much greater understanding whilst moving forwards through the higher levels of organisation. If a client were to present with visible catabolism, it is important that a nutrition coach is able to not only understand the process themselves but also have the ability to relay this information to the client and explain the scientific background. The ability to explain this level of organisation well will improve the understanding from the client’s perspective, therefore improving their likelihood of implementing strategies to mend the issue at hand.
Another important part of chemistry, which requires study from nutrition-based health professionals, is the chemical makeup of macronutrients, including protein, carbohydrates, fats and alcohol.
*PLEASE NOTE: *This topic will be discussed further in the next unit within this course.
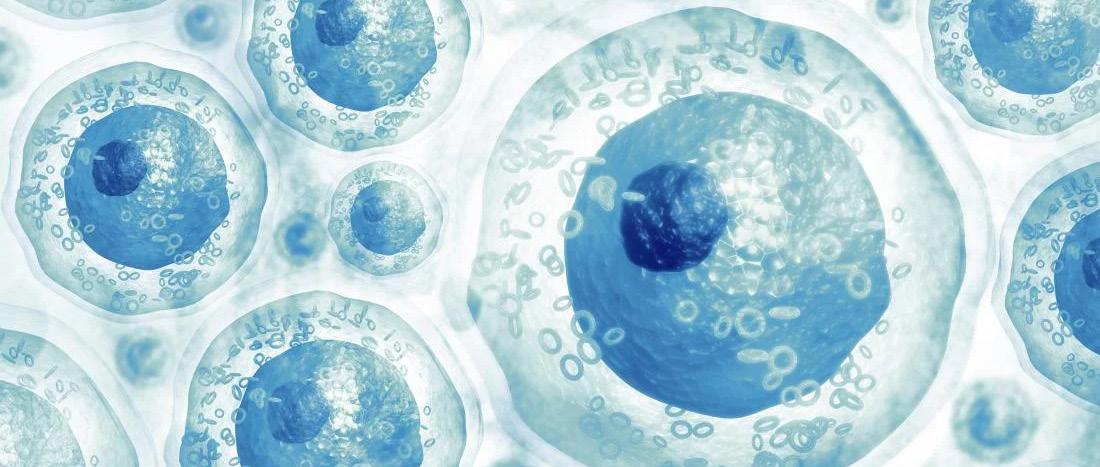
Combinations of molecules form cells which contribute to the trillions and trillions of cells in the human body. These tiny structures come in all shapes and sizes and are the basic unit of living organisms. Cells are microscopic, averaging a minute 0.1mm in size. Cells are the building blocks of all plants and animals and perform all vital physiological functions such as homeostasis (discussed later in this unit) and energy production.
The basic concept of cells can be summarised as:(1)
• Cells are the building blocks of all plants and animals
• All cells come from the division of pre-existing cells
• Cells are the smallest units that conduct all vital physiological functions
• Each cell maintains homeostasis at the cellular level.
CYTOPLASM
CELL MEMBRANE
NUCLEOLUS NUCLEUS
INTRODUCTION TO CELLS
CLICK HERE to watch the video.
CELLS IN THE HUMAN BODY
CLICK HERE to watch the video.
Cells attained their name from Robert Hooke in 1665, who, when looking at thin slices of cork under a magnifying glass, described the millions of irregular, small units as ‘cells’ because the small, bare spaces reminded him of the cell rooms in monasteries and prisons.(1)
There are approximately 200 different types of cells in the human body, and within these cells, there are about 20 different kinds of structures or organelles. The role of each different type of cell can vary, depending on the part of the body in which it resides. For example, different types of cells make up the nervous system, the respiratory system, and every other part of the body.
Types of cells in the human body can be categorised into two general classes, which include:
1. Sex cells (also known as gametes, germ cells or reproductive cells)
2. Somatic cells (where ‘soma’ refers to ‘body’).
Sex cells (gametes) are the reproductive cells of humans and exist in two varieties within the body: sperm and eggs (sperm cells from males and oocytes from females). These cells are haploid cells containing only one pair of chromosomes.
The combining of these two types of cells commences the reproduction process and the development of a new individual. Both male (sperm) and female (egg) sex cells consist of genetic material (known as DNA), and the grouping of the genetic material results in an individual genetically different from the parents.

Somatic cells are those that makeup all the internal and external structures of the body, except for the germ cells (sex cells). These types of cells are diploid cells, which means they contain two sets of chromosomes (one is derived from the mother and one from the father). For example, in the human body, there are 46 chromosomes in each somatic cell (23 pairs). In other words, each pair of chromosomes contains one chromosome from the mother and one from the father.
The table below summarises the differences between somatic cells and gametes:
All cells in the body other than sex cells.
They are the same in males and females.
Diploid cells (contain two complete sets of chromosomes).
Only includes cells that take part in reproduction.
Different in males and females (sperm in males and eggs in females).
Haploid cells (consist of only one complete set of chromosomes).
Produced by mitosis (involves one cell division). Produced by meiosis (involves two successive cell divisions).
Required for the formation of internal and external organs of the body.
Found everywhere in the human body.
Do not fuse during reproduction.
Not required for the formation of any structures in the body.
Restricted to certain parts only (i.e. reproductive parts of the body).
Egg fuses with sperm during reproduction.
An average somatic cell has several important structures which allow it to do its job effectively and efficiently. While studying cells (known as cytology) is extremely complex, the table below provides basic information on some of the most important cell features.
Poro nuclear
Membrane nuclear
Mitochondria
Smooth endoplasmic reticulum
Centrioles
Peroxisome
Secretory vesicle
PLASMA MEMBRANE
CYTOSKELETON
MICROVILLI
NUCLEUS
ENDOPLASMIC RETICULUM
Nucleolus
Ribosomes
Acts as a protective membrane for the cell, which controls the entry and exit of various materials.
Provides structural strength and support for the cell.
Finger-like projections located particularly on cells in the digestive system, which increase surface area, thus aiding in increased absorptive capacity.
Controls metabolism and protein synthesis and holds the cell’s deoxyribonucleic acid (DNA).
The rough and smooth endoplasmic reticulum work together to control lipid and carbohydrate synthesis.
MITOCHONDRIA The powerhouse of a cell for producing energy.
GOLGI APPARATUS
Responsible for transporting, modifying, and packaging proteins and lipids into vesicles for delivery to targeted destinations.
As discussed earlier, there are many diverse types of cells in the body, and although their functions are all very different, every cell works cooperatively with every other cell to enable the body to function. For example, some cells produce substances the body needs for survival, such as insulin and other substances that are bound together to form bones, muscles, and organs. Nerve cells permit communication between all the different parts of the body and assist in regulating its various functions.
If the role of one type of cell is interrupted, the entire body can be affected. No one type of cell is more vital than the other. Without all the different types of cells, the body would be unable to function.
As a nutrition coach, it is important to have a sound understanding of the cellular level of human systems, as this knowledge will often be used in explanations during consultations. For example, during a discussion about gut health, digestion or absorption, the presence and function of microvilli are expected to be discussed to assist the client in understanding why their digestive system or gut may or may not be working as optimally as it should be.
When a variety of cells are organised into layers, they form tissues. Tissues are the collection of specialised cells and cell products that perform specific functions.(1)
The study of tissues, known as histology, has identified four major types of tissue in the human body:
1. Epithelial tissue
2. Connective tissue
3. Muscle tissue
4. Neural tissue.

Epithelial tissues refer to:
• Epithelia: Layers of cells covering all surfaces of the human body, including both internal and external surfaces
• Glands: Produce fluid secretions and are attached to or derived from epithelia.
Epithelial tissues are involved in several functions; these include:
• Providing physical protection from harm (such as abrasion)
• Providing feedback to various stimuli and sensations (such as sight, sound, scent, taste and balance/equilibrium)
• Producing regulated and required secretions from various glands (such as saliva from the salivary glands).
Cells attained their name from Robert Hooke in 1665, who, when looking at thin slices of cork under a magnifying glass, described the millions of irregular, small units as ‘cells’ because the small, bare spaces reminded him of the cell rooms in monasteries and prisons.(1)
Simple squamous
• Lines blood vessels and air sacs of lungs
• Permits exchange of nutrients, wastes and gases
Simple cuboidal
• Lines kidney tubles and glands
• Secretes and reabsorbs water and small molecules
Stratified squamous
• Outer layer of skin, mouth, vagina
• Protects against abrasion, drying out, infection
Stratified Cuboidal
• Lines ducts of sweat glands
• Secretes water and ions
Simple columnar
• Lines most digestive organs
• Absorbs nutrients, produces mucus
Stratified columnar
• Lines epididymus, mammary glands, larynx
• Secretes mucus
Most epithelia tissues line or cover surfaces or body cavities
Most epithelial tissues line or cover surfaces or body cavities
The major function of connective tissue is to provide structural support for the body; however, it is also involved in transporting fluids and materials within the body, protecting organs, defending the body from invasions and storing energy reserves.(1)
Connective tissue includes bone, tendons, ligaments, cartilage and adipose tissue (fat) and is found throughout the entire body. However, unlike epithelial tissue, the connective tissue is never exposed to the outside environment.
This type of tissue contains sensory receptors which can detect:
• Pain
• Pressure
• Temperature
• Other stimuli.
It is the connective tissue that connects the epithelium to the rest of the body.

DENSE CONNECTIVE TISSUE
ADIPOSE TISSUE (CONNECTIVE TISSUE)
AREOLAR TISSUE (CONNECTIVE TISSUE)
COMPACT BONE (CONNECTIVE TISSUE)
BLOOD (CONNECTIVE TISSUE)
Muscle tissue is responsible for the body’s movement through synchronised contraction of various muscles and muscle groups.
In the human body, there are three different types of muscle tissue:
1. Skeletal muscle tissue (responsible for the movement of bones and other structures)
2. Smooth muscle tissue (responsible for changing shape to facilitate bodily functions and internal organs)
3. Cardiac muscle tissue (responsible for contracting the heart to pump blood around the body).
Muscle tissue, in particular, skeletal muscle, will be discussed in more detail at a later stage in this resource. This section is purely directed at introducing the different types of muscle tissue.
Skeletal muscle tissue tends to be long (at least 0.3m in length) and slender and thus forms the large muscles responsible for major body movement and locomotion. Skeletal muscle responds to stimuli from the nervous system and is under voluntary control. For example, an individual makes a conscious decision to walk across the road, wave their hands or brush their teeth.
Skeletal muscles are the muscles that connect to bones and have the main function of contracting to facilitate the movement of the skeleton. These muscles can also be labelled as ‘striated muscles’ due to their striped appearance.
Skeletal muscles are sometimes known as ‘voluntary muscles’ because the body has conscious control over these muscles. This control is made through a nerve impulse sent from the brain and carries messages to the muscle. Voluntary contractions produce powerful, fast movements or small precision actions. Skeletal muscles also have the capability to stretch or contract and still return to their original shape.
Smooth muscle tissue is located in the walls of blood vessels, around specific organs (providing support and elasticity), and around the respiratory, circulatory and digestive systems. Smooth muscle tissue, while it has input from the nervous system, is not under voluntary control. Contractions of smooth muscles occur involuntarily. For example, an individual has no control over the contraction of their digestive tract or blood vessels.
Another name for smooth muscle is ‘unstriated muscle’, as it does not have the striped appearance of skeletal muscle. This type of muscle tissue is stimulated by involuntary impulses and has slow, rhythmical contractions to control internal organs. An example is the moving of food through the oesophagus or the contracting of blood vessels during vasoconstriction.

Smooth muscle tissue can regenerate after injury, whereas skeletal muscles can partially repair themselves after injury.
Cardiac muscle tissue is found solely in the heart and is responsible for blood circulation. Although this type of muscle is only found in the heart, it has similar characteristics to skeletal muscles in that it is also striated. Cardiac muscle tissue is highly specialised; it is under the control of the autonomic nervous system, which means that even without a nerve input, contractions can occur due to cells that are known as pacemaker cells.

The table below shows a comparison between each type of muscle:
MUSCLE TYPE DESCRIPTION
SKELETAL MUSCLE
CARDIAC MUSCLE
Skeletal muscle is the only one of the three muscle types that function with the movement of the body.
This includes providing balance, warmth, and conscious motions such as walking, moving limbs, and speaking.
Cardiac muscles are only found in the heart. This muscle contracts the heart and pumps blood throughout the body. The autonomic nervous system controls this muscle.
SMOOTH MUSCLE
Smooth muscle (also known as visceral muscle) is found inside organs such as the stomach, intestines, and blood vessels. It is called smooth muscle because, unlike skeletal muscle, it does not have the banded appearance of skeletal or cardiac muscle.
STRUCTURAL CHARACTERISTICS
• Comprised of sarcomeres
• Striated appearance
• Voluntary (conscious) movement
• Fibres are long in shape
• Multinucleated (multiple nuclei per cell).
• Comprised of sarcomeres
• Striated muscles
• Involuntary (unconscious) movement
• Fibres are shaped like branches that are crosslinked to one another
• Typically one nucleus per cell.
• Does not consist of sarcomeres
• Non-striated
• Involuntary (unconscious) movement
• Fibres shaped like almonds (tapered ends)
• One nucleus per cell.
DIAGRAM





























Neural tissue, also known as nervous tissue, is responsible for the electrical communication of stimuli from one part of the body to another. It is understood that approximately 98% of nervous tissue is located in the brain and spinal cord, which are the control centres for the nervous system.
The nervous system includes the brain, spinal cord, sensory organs and the nerves that work together to connect the rest of the body to these specific organs. The nervous system is how the body moves communication throughout the body.
The tissue level of organisation is important for nutrition coaches to understand, as it is fundamental in comprehending the more complex levels and body systems. The tissue level of organisation is responsible for ensuring all organs and systems are held in place, including the digestive tract, which plays a pivotal role in the digestion, absorption, and utilisation of nutrients.
The tissue level also provides the structure for the body, enabling a nutrition coach to understand muscular anabolism versus catabolism and allowing the systems to communicate effectively.
The organ level refers to individual and accessory organs in an organism and how they interact with other systems to ensure vital life processes are maintained. As many as 78 organs form groups and work in conjunction with one another to accomplish a particular task. For example, the skin is one of the body’s largest organs.
While there is a large number of organs within the body, the major organs that will be focused on throughout this unit are:
• The brain
• The heart
• The lungs
• The liver
• The kidneys
• The stomach.
Each of these major organs is a vital part of the body’s organ systems, which will be discussed later in this unit. It is a collaborative effort from all 11 of these organ systems, ensuring optimal function in an individuals!
A comprehensive understanding of the anatomy and physiology of these important organs is imperative. Each organ is affected by, and dependent on, adequate nutrient intake in one way or another. Thus, it is very important to identify the body’s signs and symptoms when something is not working as it should. This ability will assist nutrition coaches in suggesting the correct nutrients to assist their clients or referring clients to an allied health professional if any issues are deemed out of their scope of practice.
Further, understanding the role and function of these organs will give additional perspective to the importance of various nutrients. Nutrition coaches will then be able to explain and educate their clients on why certain nutrients are important for certain organs and what could result if the client were to omit essential nutrients from their diet or consume them in excess.
To instil a sense of trust within a client, a nutrition coach must understand how nutrition can affect the body and the efficiency of the body’s organs.

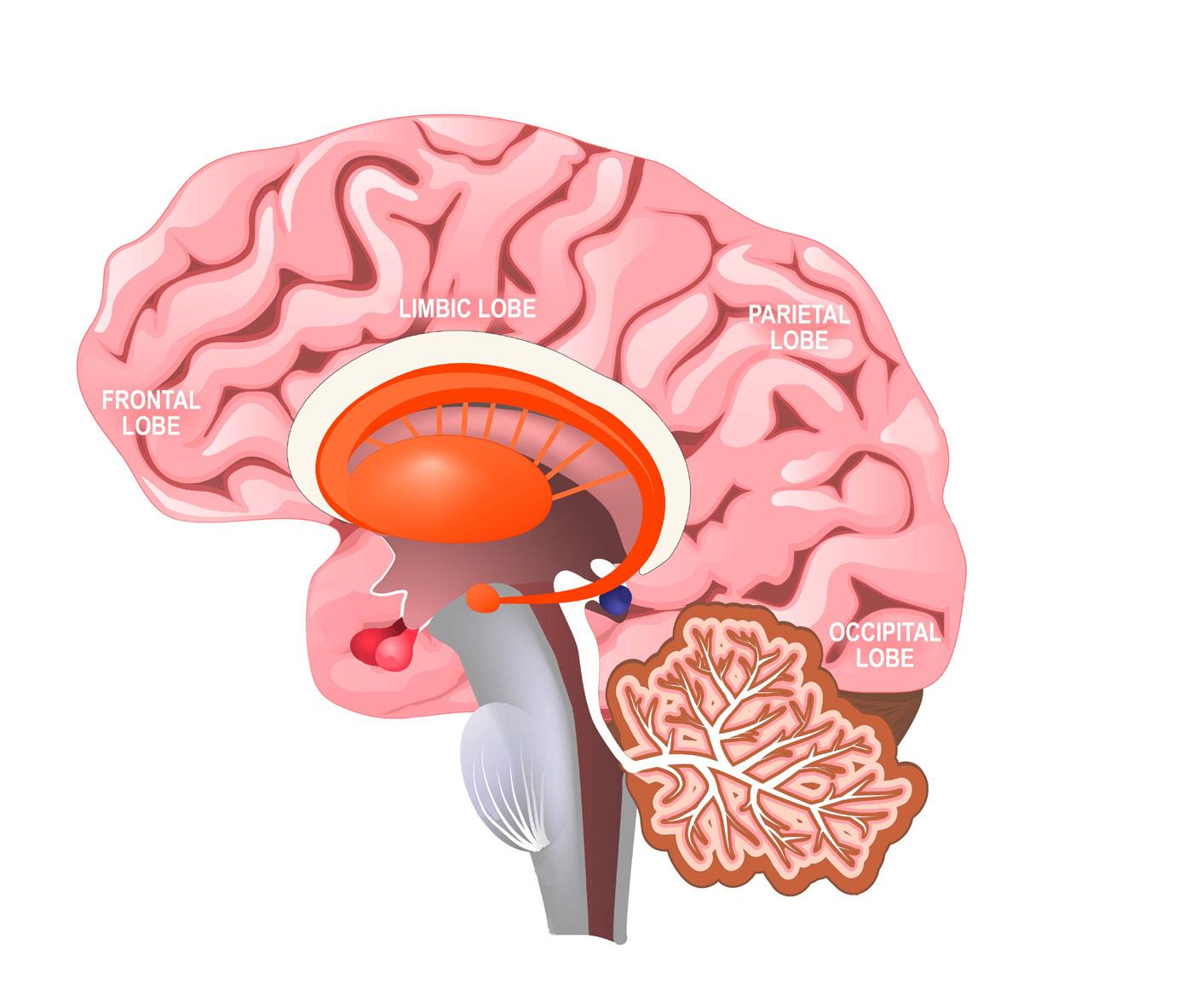
The brain is the major control centre for everything that takes place within the body; because of this, it is one of the most (if not the most) complex and vital organs and one of the largest.(1) Understanding the brain will bring a great deal of perspective on the rest of the human body.
Over the years, scientists have discovered and named various areas of the brain based on their unique function and purpose; this categorisation of the brain’s specialised areas includes the structures and lobes of the brain and assists greatly in understanding this complex organ.
CEREBRUM
CORTEX
CEREBELLUM
DIENCEPHALON
The cerebrum is divided into two hemispheres - the right and left hemispheres. The largest area of the brain comprises several elevated ridges and shallow depressions to increase the brain's surface area. Conscious thought, sensations, intellect, memory and complex movements originate in the cerebrum.
Also known as the neural cortex, it is the brain's outermost layer and covers both the left and right hemispheres.
The second largest part of the brain and responsible for maintaining coordination, balance, speech and other voluntary actions by receiving sensory information from the brainstem and spinal cord.
A structural and functional link between the two hemispheres and the brainstem. It is comprised of the thalamus and hypothalamus.
The thalamus contains relay and processing centres for sensory information, whereas the hypothalamus contains centres involved with emotional control and hormone production. The hypothalamus is also physically connected to the pituitary gland; together, they are responsible for integrating the nervous and endocrine systems.
Three different structures make up the brainstem:
1. The mesencephalon
2. Pons
3. Medulla oblongata.
The collective functions of these structures within the brainstem include:
BRAINSTEM
• Visual and auditory processing
• Maintenance of consciousness
• Reflex motor responses
• Relaying of sensory information between other structures of the brain
• The regulation of visceral (internal organs in the main cavity of the body) functions such as cardiovascular, respiratory and digestive system activities.
FRONTAL LOBE
PARIETAL LOBE
OCCIPITAL LOBE
TEMPORAL LOBE
Responsible for the voluntary control of skeletal muscles and motor control, as well as language, personality, social and self-awareness, attention, mood and moral reasoning.(3)
Responsible for the perception of touch, pressure, pain, taste and temperature.
Responsible for conscious perception of visual stimuli and visual processing.
Responsible for processing and perception of auditory and olfactory stimuli and memory.
For each structure and area of the brain to function effectively, the brain needs to be protected as much as possible from movement, injury and nutrient deficiency. The first line of defence for the brain (after the skull) consists of three layers of fibrous tissues (known as cranial meninges) covering the brain’s surface for protection.
The second line of defence for the brain is the cerebrospinal fluid which surrounds the brain and the spinal cord entirely. This fluid is responsible for cushioning the brain and spine by literally making them float within the fluid to avoid excessive movement within the skeleton whilst also transporting nutrients, chemical messages and waste products.
FUN FACTS ABOUT THE BRAIN(1)
• The brain of a human is the largest brain of all vertebrates respective to body size
• The brain weighs about 1.5kg
• Approximately 2% of a human’s body weight is the brain
• The grey matter is about 86 billion nerve cells (neurons)
• The white matter is billions of nerve fibres (axons and dendrites).

The heart is a small organ, roughly the size of a clenched fist, and is the only muscle in the entire body that never stops working. It is located in the thoracic cavity, directly posterior to the sternum.
The heart’s main function is pumping blood (in blood vessels) around the body, which is estimated to pump approximately 100,000 times daily(1) The blood is pumped throughout the body via two different circuits: the pulmonary and systemic circuits, which both begin and end at the heart and contain arteries, veins and capillaries.(1)
• Arteries: Blood exits the heart through arteries - also known as efferent blood vessels.
• Veins: Blood arrives at the heart by veins (also known as afferent blood vessels).
• Capillaries: These are microscopic blood vessels connecting the smallest arteries and the smallest veins. Gas exchange also occurs within the capillaries.
THE RIGHT ATRIUM Receives blood from the systemic circuit and passes it to the right ventricle.
THE RIGHT VENTRICLE Pumps blood into the pulmonary circuit.
THE LEFT ATRIUM Collects blood from the pulmonary circuit and unloads it into the left ventricle.
THE LEFT VENTRICLE Pumps blood to the systemic circuit.
• The heart pumps about 7,500L of blood every day
• The heart can continue beating even if it is disconnected from the body
• An electrical system is what controls the beating of a heart
• A woman’s heart beats slightly faster than a man’s heart.
The lungs are a pair of air-filled, sponge-like organs located in the thoracic cavity of the chest, on either side of the heart. Each lung is described as a ‘blunt cone’ in which the apex, or tip, points towards the face and extends superior to the first rib.(1) The concave base of each lung rests against the superior surface of the diaphragm.
The lungs are made up of distinct lobes, which are noticeable through the presence of deep fissures or narrow openings.(1) The right lung is made up of the superior, middle and inferior lobes, whereas the left lung is made up of the superior and inferior lobes. The left lung only has two lobes because it needs to allow room for the heart; as a result, the left lung is smaller and, therefore, only has two lobes.
The lungs are enclosed within a thin tissue layer, or membrane, known as the pleura. This helps to lubricate the lungs for smoother movement during inhalation and exhalation.
FUN FACTS ABOUT THE LUNGS
• The lungs are the only organs in the human body that can float on water
• The left lung is smaller than the right lung to make room for the heart
• The largest amount of waste elimination takes place simply by breathing
• Up to 17.5 mL of water is exhaled per hour.
As the lungs are a major organ of the respiratory system, they will be further explained later in this resource.
The liver is the largest visceral organ and one of the body’s most versatile organs. It is separated into two major lobes: the left and right lobes; and two minor lobes: the caudate and quadrate lobes.(1)
The anterior surface of the liver shows only the two major lobes, which are separated by the falciform ligament.(1) On the posterior surface, all four lobes can be identified. The inferior vena cava (a large vein that carries deoxygenated blood from the lower body back to the heart) separates the left and right lobes and distinguishes the caudate lobe. The quadrate lobe is inferior (below) to the caudate lobe and is between the left lobe and the gallbladder.(1)
There are three main physiological functions carried out by the liver daily, including:
HAEMATOLOGICAL REGULATION
SYNTHESIS AND SECRETION OF BILE
As blood passes through the liver, it executes the following functions: removes circulating hormones, removes antibodies, removal and safe storage of toxins, and synthesises bile.(1)
The role of bile in the liver is to aid in the digestion and absorption of lipids by secretion of bile salts which coat the droplets of lipids and allows the lipiddigesting enzymes to attach to the lipids and begin breaking them down.(1)
METABOLIC REGULATION
The liver is the major organ for regulating the composition of the body’s circulating blood. Extraction of nutrients and toxins from the blood, storage of excessive nutrients, and correction of nutrient deficiencies all happen within the liver.(1)
Following on from the table on the previous page, understanding the importance of healthy liver function is imperative as a nutrition coach; this is because the liver’s regulatory activities will affect the following:(1)
• Carbohydrate metabolism: by stabilising blood glucose levels and initiating gluconeogenesis if glucose levels are low.
• Lipid metabolism: by regulating the levels of fatty acids, triglycerides and cholesterol, which circulate in the bloodstream.
• Amino acid metabolism: by removing excess amino acids from the bloodstream, which are then used to either synthesise proteins or used as energy storage.
• Vitamin storage: fat-soluble vitamins (A, D, E, K, and B12) are all stored in the liver and used if the diet provides inadequate levels of these nutrients.
• Mineral storage: the liver converts excess iron found in the bloodstream to ferritin - a protein that stores and releases iron when it is low.
• Waste product removal: when the body needs additional energy, the liver uses amino acids or lipids and converts them to carbohydrates. Doing so creates a waste product called ammonia which is then neutralised by the liver and removed. Other waste products, toxins, or drugs are also inactivated and removed by the liver.
• Drug inactivation: circulating drugs are inactivated and broken down by the liver, which limits the duration of their effects. Nutrition coaches need to be aware of the rate at which the liver breaks down certain nutrients before making a prescription.
CLICK HERE to watch the video.
• The liver weighs about 1.5kg
• It contains the largest reservoir of blood in the body
• It receives about 25% of cardiac output
• Liver cells (hepatocytes) are arranged into clusters of cells called ‘liver lobules’ which take on a hexagonal shape. The hepatocytes within the liver lobule are arranged into a series of lines which look like spokes on a wheel.

The kidneys are two organs that play a vital role in the urinary system. They produce urine, a waste fluid consisting of water, ions and small soluble compounds.(1) Urine leaves the kidneys through the urinary tract, which involves the ureters (a pair of tubes that lead to the bladder). The urinary bladder is a temporary storage area for urine before it leaves the body via the urethra.(1)
The kidneys are positioned on either side of the vertebral column, between vertebrae T12 and L3. On the surface of each kidney rests an adrenal gland, and each kidney is protected and held in place by three layers of protective connective tissue:(1)
1. The fibrous capsule: a layer of collagen that covers the whole kidney on the outer surface.
2. The perinephric fat capsule: a thick layer of adipose (fat) tissue surrounding the fibrous capsule.
3. The renal fascia: this layer anchors the kidney to its surrounding structures.
This arrangement of protective layers ensures that the daily movement does not disrupt the function of the kidneys.
FUN FACTS ABOUT THE KIDNEYS(1)
• A typical adult kidney is a reddish-brown colour
• A single kidney is approximately 10cm in length, 5.5cm in width, and 3cm thick
• Each kidney weighs about 150g
• The left kidney lies slightly superior to the right kidney.
The stomach is a J-shaped organ located in the body’s thoracic cavity, directly underneath the diaphragm and adjacent to the liver. The stomach connects the oesophagus to the small intestine and forms part of the digestive tract.
The stomach consists of four regions, all of which are responsible for a different aspect of the digestive process, outlined in the table below:
THE CARDIA
THE FUNDUS
THE BODY
THE PYLORUS
This is the smallest section of the stomach and is located on the superior, medial section, closest to the opening of the oesophagus. This portion of the stomach is responsible for protecting the opening of the oesophagus from stomach acid and enzymes through mucous, which is secreted by an abundance of mucous glands.
This is located superior to the opening of the oesophagus on the lateral side and is in contact with the diaphragm. The fundus contains secretory gastric glands, which secrete acid and enzymes for digestion.
This is the largest region of the stomach and is located in between the fundus and the sharp curve of the ‘J’. This portion of the stomach acts as a ‘mixing pot’ for the food ingested and the secretions of the stomach. This portion of the stomach also contains gastric glands, which secrete the most acid and enzymes to break down food.
This is the sharp curve of the ‘J’ and is split into three different features: the pyloric antrum, which connects to the body; the pyloric canal, which connects to the small intestine; and the pyloric sphincter, which is a muscular ring which regulates the emptying of food into the small intestine.
Longitudinal layer (Outer)
Circular layer (Middle)
Oblique layer (Inner)
The stomach plays an imperative role in the chemical and mechanical digestion of food. Once it receives food from the oesophagus, it has a number of main functions which aid in the digestion of food before passing it onto the small intestine.
The main functions of the stomach are:
• Storage of ingested food
• Continuation of mechanical breakdown of food (after mastication)
• Breakdown of chemical bonds in food through the utilisation of acids and enzymes
• The creation of intrinsic factor which is necessary for the absorption of vitamin B12.
This particular organ is of great importance to a nutrition coach as it forms one of the main components of the digestive system.
• The shape and size of the stomach are variable from person to person, and even meal to meal!
• It is possible to live without the stomach
• The lining of the stomach regenerates every 4-5 days
• The shorter curve of the stomach is about 10cm; whereas the longer curve can be as long as 40cm
• Regular exercise keeps the muscles of the digestive tract in good shape so they can work more effectively.







RESPIRATORY SYSTEMREPRODUCTIVE SYSTEMREPRODUCTIVE SYSTEMDIGESTIVE SYSTEM
This particular unit focuses on the anatomy and basic physiology of the human body systems (also referred to as organ systems or the system level of organisation).
There are 11 organ systems in the human body that each have different functions; these include:
1. The cardiovascular system (also referred to as the circulatory system)
2. The respiratory system
3. The muscular system
4. The skeletal system
5. The endocrine system
6. The digestive system
7. The urinary system
8. The integumentary system
9. The reproductive system
10.The lymphatic system
11. The nervous system.
Organ systems or body systems are comprised of numerous individual organs, which work in synergy to carry out a particular function for the organism (i.e. the human body). In other words, different organs can work together to perform a common purpose. For example, there are many different organs within the digestive system, but they all work together to break down, digest and absorb nutrients.
The interaction or cooperation of two or more organisations, substances, or other agents to produce a combined effect greater than the sum of their separate effects.(4) An example is the physiological regulation of hormones which requires the synergy of the nervous system and the nervous system to coordinate and work together.(5)
Just as individual organs within a system work together, entire organ systems work together. The digestive system works to break down food to absorb its nutrients. It then works with the circulatory system to deliver those nutrients to the rest of the body. After use within the body, excess nutrients and other waste are transported to the kidneys for filtration, which is part of the urinary system. There are countless examples of how organ systems work in synergy, but their primary goal is to keep the body nourished, energised and functioning optimally.
Each body/organ system will be individually discussed in more detail on the following pages.

The term organism refers to an individual animal, plant or single-celled life form.(1) Therefore, the organismal level refers to the organism as a whole, made up of individually and synergistically functioning systems.
The organismal level is the highest level of organisation, as it is the result of all body systems working as one to form a functioning and complete life form (i.e. the human body). The cooperative functioning of all body systems constitutes the life and health of the organism as a whole. Although the organism is made up of individual systems, organs and cells, their objective is ultimately the organism’s survival.

This section will elaborate on each body system so that nutrition coaches can thoroughly understand how each system works individually and synergistically within the body.
As previously mentioned, organ systems do not work alone in the body. They must all be able to work together. For example, one of the most important functions of organ systems is to provide cells with oxygen and nutrients and to eliminate toxic waste products such as carbon dioxide. Several organ systems, including the cardiovascular and respiratory systems, all work together to do this.
Provided below, however, is a summary of each organ system, the primary organs found within it and what its main function is:
CARDIOVASCULAR (CIRCULATORY)
• Heart
• Blood vessels
• Blood.
• Lymph nodes
• Lymph vessels.
LYMPHATIC SYSTEM
DIGESTIVE SYSTEM
ENDOCRINE SYSTEM
INTEGUMENTARY SYSTEM
• Oesophagus
• Stomach
• Small intestine
• Large intestine
• Liver
• Gallbladder.
• Pituitary gland
• Hypothalamus
• Adrenal glands
• Ovaries/testes.
• Skin
• Hair
• Nails.
• Cardiac (heart) muscle
• Skeletal muscle
MUSCULAR SYSTEM
NERVOUS SYSTEM
Transports oxygen, hormones, and nutrients to the body cells. Moves waste and carbon dioxide away from cells.
Defends against infection and disease and moves lymph (fluid carried by the lymphatic system to help deliver nutrients and fight against infections) between tissues and the bloodstream.
Breaks down and digests food and absorbs macronutrients, minerals, vitamins, and water. Eliminates toxins and waste from the body.
Produces hormones that communicate between cells.
Provides protection from injury and water loss, physical defence against infection by microorganisms, and temperature control.
Involved in movement and heat production.
• Smooth muscle
• Tendons.
• Brain
• Spinal cord
• Nerves.
Collects, transfers, and processes information from various external and internal stimuli.
REPRODUCTIVE SYSTEM
RESPIRATORY SYSTEM
SKELETAL SYSTEM
URINARY SYSTEM
FEMALE :
• Uterus
• Vagina
• Fallopian tubes
• Ovaries.
MALE:
• Penis
• Testes
• Seminal vesicles.
• Trachea
• Larynx
• Pharynx
• Lungs.
• Bones
• Cartilage
• Ligaments.
• Kidneys
• Urinary bladder.
Produces gametes (sex cells) and sex hormones.
Brings air to sites where gas exchange can occur between the blood and cells (around the body) or blood and air (lungs).
Supports, protects and defends soft tissues of the body; produces blood cells; stores minerals; provides structure and stability.
Removes extra water, salts, and waste products from the blood and body; controls pH; controls water and salt balance.
While each system can be classified individually, it is important to remember that systems work synergistically with each other and that a certain part of one system may also form part of another system. For example, the oral cavity plays a role in the digestive system, as well as the respiratory system.
In addition, each body system not only shares certain parts with other systems, but their functionality may overlap. For example, the circulatory system is responsible for delivering oxygen and nutrients to various cells across the body as its primary function; however, by doing this, it achieves other bodily functions. Other functions of blood circulation include temperature control (through vasodilation and vasoconstriction) and transport of hormones produced by the glands of the endocrine system; the white blood cells also play a pivotal role in the immune system.
Therefore, body systems need to be studied and understood in how they work synergistically with each other and how they individually function.












When it comes to a body system, all components of that particular body system must work together to achieve their end goal or function. Each system component is vital in achieving optimal functionality, regardless of size, energy demand or time consumption. If one part of the body system were to not function as it should, the body system would not be able to function as a whole, and problems would soon arise.(1)
The digestive system is a perfect example to indicate how important each process and component of a system is. The digestive system’s ability to break down food, absorb and utilise nutrients, and eliminate undigested waste products is wholly dependent on each component of the system working as it should.(1)(6)(7)
Once food has entered the oral cavity, the body will begin to digest it. There are two major types of digestion known as mechanical digestion and chemical digestion. Mechanical digestion begins in the oral cavity (mastication) and continues when the food hits the stomach, where the stomach churns the bolus. Chemical digestion is when larger molecules, such as proteins and starches, are broken down into smaller pieces. If chemical or mechanical digestion did not occur, the food would not be in an ideal state to allow for optimal absorption.
The stomach assists in the digestion of food molecules and acts as a storage tank. The stomach will release partially digested food into the small intestine at a rate the small intestine can handle. If the stomach does not work as it should, it may pass large amounts of food into the small intestine, resulting in poor nutrient absorption. As another example, if the stomach did not churn the food/bolus adequately before passing it into the small intestine, the small intestine would have increased pressure to provide additional chemical digestion to complete its nutrient absorption job.
The small intestine is responsible for a large amount of chemical digestion; this digestion results from the enzymes and bile released by the pancreas and the gallbladder.(1) The small intestine is also responsible for nutrient absorption. Absorbed nutrients are carried in the bloodstream to areas of the body which require them most. If either the pancreas or the gallbladder did not produce enzymes and bile as required, there would be inadequate chemical digestion, and therefore the food would not be able to be appropriately absorbed and utilised by the body.
From here, the bolus continues to pass through the large intestine, where fluid is absorbed. The bolus continues to travel through while the digestive system absorbs what it requires and leaves what is not required.11 What is not required is then eliminated from the body. If the large intestine does not function optimally, it might not absorb adequate hydration, thus leaving the body dehydrated with potential diarrhoea; or it might absorb waste products into the bloodstream, consequently increasing the workload for the kidney’s filtration system at a later time.
Understandably, if one part of the digestive tract did not function optimally, it is easy to see how and why a problem would arise. It is, therefore, important to remember that no matter how small a task or organ may appear in the body, it is essential for the optimal functioning of the organism as a whole.
As explained above, it is crucial that all organs work together in their system to accomplish the end result (e.g. digestion). As such, it is equally important for systems to work cooperatively with each other to accomplish their various tasks. Systems work together to ensure all tasks are completed effectively and efficiently to keep the body operating.
Following on from the above example, nutrients are absorbed via the small intestine and into the bloodstream, which is part of the circulatory system. From here, nutrients are distributed via the circulatory system before all blood is passed through the kidneys for filtration. The kidneys form part of the urinary system, which removes waste from the blood and eliminates it from the body via urine. Once the urinary system has filtered the blood, it is passed back into the circulatory system.
There are many examples to show how the various organ systems work cooperatively with each other. For example, the circulatory system is also closely linked to the respiratory system to deliver oxygen to cells and remove carbon dioxide that the cells produce. The circulatory system (blood) receives oxygen from the respiratory system via the lungs as fresh air is inhaled, delivers it to required tissues, collects carbon dioxide, and takes it back to the lungs, where it is expelled through exhalation.
It’s worth asking a few trusted people in your life what they think of when they first see the business name or if it clearly depicts your business. As they are not personally invested in the name, they may point out something that you hadn’t yet considered.
There is an expectation from clients and the general public that nutrition coaches will have a foundational understanding of all body systems, in particular, the digestive system. As nutrition is so interrelated, where one system speaks with and affects the others, it is difficult to say that a nutrition coach only needs to be educated on a particular type of system. Rather, they require a solid knowledge base on all the human body systems.
For example, if a nutrition coach consulted with a client who had diabetes, food intolerances, and raised cholesterol levels, they would be expected to refer them for specific individualised chronic disease advice. However, the nutrition coach would still need to understand that this client’s endocrine, cardiovascular, and digestive systems were immediately impacted.
Another example may be if a client presents with polycystic ovarian syndrome or general difficulty in falling pregnant. While it is commonly thought that nutrition may not play a role in reproductive health, it absolutely does. The correct nutrition will allow the female body to successfully carry and nurture the foetus, with all nutrition feeding not only the mother but the foetus as well. When the baby is born, the mother’s nutrition is passed straight onto the infant through breast milk. If the mother has a nutritionally inadequate diet, breast milk is unlikely to hold all the nutritional qualities the infant requires.
Therefore, nutrition coaches are expected to have a basic understanding of all systems and the knowledge to know when to refer clients for specific disease-related advice
While it is outside a nutrition coach’s scope of practice to consult with women who are pregnant, it is within their scope to consult with women during preconception to ensure a nutritionally adequate and well-balanced diet. This will ensure optimal nutritional health and assist in conceiving. Nutrition coaches must ensure compliance by staying within their scope of practice.
The circulatory system (also known as the cardiovascular system), is responsible for all blood flow in the body. Blood flow, which occurs through arteries (oxygenated) and veins (deoxygenated), is responsible for carrying nutrients, oxygen, carbon dioxide, hormones, antibodies and blood cells to all body parts.
The cardiovascular system is inclusive of three main components:
• The heart (the organ that pumps the blood)
• An extremely complex network of blood vessels (arteries, veins, capillaries)
• Blood.
The circulatory system is a critical body system providing the entire body’s cells with nutrients and oxygen while also removing waste. If the circulatory system were to stop working, even if only for a minute, the heart would stop pumping, and the individual would die.
In addition to pumping the blood, the circulatory system is also responsible for maintaining homeostasis and immunity, delivering white blood cells where they need to be to fight against infection.
The circulatory system’s major organ is the heart. The heart is a hollow, muscular pump with four chambers (right atrium, left atrium, right ventricle, and left ventricle) and is responsible for pumping blood around the body. The heart is located in the chest cavity behind the rib cage. The heart pumps blood around the body in response to the individual’s immediate oxygen needs; for example, less blood is pumped when an individual is asleep, and more blood is pumped when the individual has higher oxygen requirements, such as completing exercises or when frightened.

TED TALK - HOW THE HEART ACTUALLY PUMPS BLOOD CLICK HERE to watch the video.
RIGHT ATRIUM
The right atrium obtains blood from the systemic circuit through two major veins: the superior (the Latin word meaning ‘above’) vena cava and the inferior (Latin word meaning ‘below’) vena cava. The superior vena cava receives blood from the upper body, while the inferior vena cava receives blood from the torso down.
RIGHT VENTRICLE
LEFT ATRIUM
LEFT VENTRICLE
Blood is received from the right atrium into the right ventricle. There is a valve in place, known as the right atrioventricular valve (AV), which prevents the backflow of blood from the ventricle back into the atrium. Blood flows from the right ventricle via the pulmonary artery to enter the pulmonary circuit.
The left atrium receives blood via the pulmonary veins. The left AV, like the right, permits the ongoing flow of blood to the left ventricle but does not permit the blood to pass back through.
The left ventricle has much thicker walls than the right ventricle and hence appears larger in size. These thicker walls allow adequate pressure for the ventricle to push the blood through the entire systemic circuit, whereas the right ventricle only needs to push blood through the pulmonary circuit. Blood leaves the left ventricle through the aortic valve to enter the systemic circuit.
Blood, nutrients, oxygen, and gases are carried around the body through a complex network of blood vessels, including veins, arteries and capillaries.
VEINS
ARTERIES
CAPILLARIES
Veins are blood vessels that transport blood toward the heart.
Arteries are blood vessels that transport blood away from the heart.
Capillaries are microscopic blood vessels that connect arteries and veins together.
Blood vessels transport blood throughout the body, in which blood itself plays a number of important roles in a healthy functioning body, including:
• Transportation of important substances (i.e. oxygen)
• Regulation of pH
• Decreased fluid loss at the time of injury
• Toxin and pathogen defence
• Regulation of body temperature.
TRANSPORTATION OF IMPORTANT SUBSTANCES
BLOOD AND FLUID LOSS
DEFENCE AGAINST PATHOGENS AND TOXINS
REGULATION OF BODY TEMPERATURE

Blood vessels have an extremely important role in continuously transporting blood to all the organs, tissues, and cells across the entire body. Blood delivers oxygen from the lungs to peripheral tissues and then removes the carbon dioxide from those peripheral tissues back to the lungs for another exchange of oxygen. This process occurs without any voluntary stimulation from the person.
Blood also transports and distributes nutrients to all parts of the body. These nutrients are taken from the digestive tract, or nutrients may also be released from storage. In addition, blood carries waste products found within the body to the kidneys, which can then be filtered and passed out through the urinary system.
Vitamin K in blood assists with blood clotting. Blood contains enzymes that respond to an injury internally and externally and initiate blood clotting (known as coagulation). The blood clot prevents further blood loss, as it acts as a temporary patch.
While this is beneficial in most situations, it can also be harmful if the blood clot is internal and unknown. Doctors may, therefore, prescribe those who are at risk of internal blood clots anticoagulant medication to minimise this risk.
While the immune system largely regulates the body’s defence against pathogens and toxins, the blood vessels play an important role in the transportation of the white blood cells (WBCs), which help to fight infection. In addition to WBCs, the blood vessels also carry antibodies which are proteins that attack foreign compounds (e.g. gravel in an open wound).
Blood absorbs the heat generated by working skeletal muscles and redistributes it to other tissues. If the individual’s temperature is already too high, the blood vessels widen/dilate (known as vasodilation), allowing more heat to be carried to the skin, where it can then be lost to the air and thus provide a cooling effect. If the individual is cold, the blood vessels will constrict (known as vasoconstriction) which constricts the flow of blood in certain areas such as the peripheries (e.g. outer limbs such as arms and legs).
As a result, vasoconstriction retains core body heat as the heat isn’t lost to the air, and is instead protecting the body’s vital organs from the cold.
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for cardiovascular problems or conditions, it is still important to have an understanding of common problems that might arise within this system.
Understanding common issues relating to the cardiovascular system can help a nutrition coach identify the need to refer their clients to the appropriate medical or allied health professional.
Common cardiovascular problems include:
• Cardiac arrest
• Angina and angina pectoris
• Cardiomyopathy
• Congestive cardiac failure (CCF).
Cardiac arrest occurs when the heart ceases its rhythm and stops beating. This causes a severe lack of oxygen to the rest of the body due to the interruption of blood flow, as well as brain drainage if not treated immediately.
CARDIAC ARREST
ANGINA AND ANGINA PECTORIS
Cardiac arrest can be prevented through the implementation of healthy lifestyle habits and diet.(9)
Angina is severe chest pain due to insufficient oxygen reaching the heart. It can stem from one or both shoulders or arms and hands. Stable angina can occur from intense physical exertion or extreme emotion, while unstable angina is more serious as it can indicate a high risk of a heart attack.
Angina is likely to indicate coronary heart disease, with plaque build-up restricting oxygen flow.(10)
Cardiomyopathy refers to a weakening of the heart muscles and walls of the chambers.
The severity of symptoms will depend on the individual and can include:
• Shortened breath
CARDIOMYOPATHY
• Fatigue
• Light-headedness.
The main concern with cardiomyopathy is that if the muscles grow too weak, the condition can develop into congestive cardiac failure.(11)
Congestive cardiac failure (CCF) refers to the inability of the heart to pump blood efficiently enough to meet the demands of the body.
CONGESTIVE
CARDIAC FAILURE (CCF)
CCF can either be systolic or diastolic:
• Systolic: refers to when the walls of the chambers are weakened and thin, resulting in the inability to pump blood
• Diastolic: refers to when the walls of the chambers are thickened and stiff, resulting in the inability to fill with enough blood.
CCF can be treated and prevented with healthy lifestyle habits and diet.(12)
The respiratory system is responsible for taking in oxygen and expelling carbon dioxide.
While the major organ of the respiratory system is the lungs, there are many other parts of the body involved as well:
• The nose or mouth as air is inhaled
• The sinuses to regulate the temperature of the air
• The trachea (or windpipe) to filter the air
• The bronchi to carry the air into the lungs
• The cilia to carry mucus up and out of the lungs (through sneezing, coughing and swallowing)
• The alveoli to exchange oxygen for carbon dioxide
• The diaphragm which controls breathing.
While the respiratory system’s main function is the movement of air and carbon dioxide through the body, it is also responsible for several other functions, including:
• Gas exchange between air and circulating blood
• Producing sounds heard in communication
• Maintaining respiratory health.
GAS EXCHANGE BETWEEN AIR AND CIRCULATING BLOOD
The respiratory system’s main function is exchanging two gases: oxygen and carbon dioxide. Oxygen enters the body through the nasal and oral cavities. When oxygen enters the lungs, it is passed over the air-blood barrier from the alveoli into the blood of the capillaries through a process known as diffusion.
Oxygen is then carried in the blood and distributed around the body. Carbon dioxide is returned from various parts of the human body back to the lungs, where again it is diffused across the air-blood barrier from the deoxygenated veins back to the alveoli and is then exhaled as carbon dioxide.
PRODUCING SOUNDS HEARD IN COMMUNICATION
MAINTAINING RESPIRATORY
HEALTH
The respiratory system works in conjunction with the voice box (scientifically known as the larynx) to produce sounds involved in speaking, singing, and other forms of communication.
The tone and pitch of the voice can be controlled so that an individual can speak softly or loudly and emphasise different emotions such as empathy, anger, or excitement.
The respiratory system is also involved in maintaining respiratory health and, as such, is responsible for:
• Protecting the respiratory surfaces from dehydration
• Controlling temperature changes
• Defending the respiratory system and other tissues from potential invaders (such as pathogens)
• Facilitating the detection of olfactory stimuli (e.g. smelling if something is ‘off’ or unsafe to eat).
A properly and efficiently operating respiratory system is essential for maintaining energy production, fat burning and ease of eating (respiratory conditions like colds or chronic diseases affecting the airways, like chronic obstructive pulmonary disease (COPD), make eating more difficult).
TED TALK - OXYGEN’S SURPRISINGLY COMPLEX JOURNEY THROUGH YOUR BODY CLICK HERE to watch the video.
The respiratory system includes the following:
• Nose
• Nasal cavity
• Paranasal sinuses
• Pharynx
• Larynx
• Trachea
• Lungs
• Bronchi
• Bronchioles
• Alveoli.







NASAL CAVITY
PARANASAL SINUS
PHARYNX







The nose is the most common passageway of air into the respiratory system. Air is inhaled from the outside environment and enters the nasal cavity through the nostrils, also known as external nares. The hair located around the entry of the nostrils prevents unwanted particles from entering the nasal cavity, such as insects and dust.
Air is inhaled through the nose and enters the nasal cavity. The nasal cavity is an airfilled space above and behind the nose. The cavity is split into two by the nasal septum, for the right and left nostrils.
Paranasal sinuses produce mucus secretions which aid in keeping the nasal cavity moist and clean, lighten the weight of the head, and humidify and heat inhaled air. There are four sets of paranasal sinuses, including maxillary, frontal, sphenoid, and ethmoid.
The pharynx is the region of the throat that is located behind the nasal and oral cavity. The pharynx is connected to the inferior portion of the nasal cavity and extends to the entrances of the larynx (voice box) and oesophagus.
The pharynx is made up collectively of the:
• Nasopharynx
• Oropharynx
• Laryngopharynx.
The trachea also referred to as the windpipe, is a tough, flexible tube just over 10cm in length. The trachea’s major function is to pass air to and from the lungs.
The trachea contains 15-20 tracheal cartilages, which protect the airway and provide both stiffness and flexibility to the trachea. For example, an unusually large bolus of food would distort the trachea, thus allowing the food to continue down the oesophagus.
As air leaves the pharynx, it passes through a narrow opening (called the glottis) and enters the larynx. The larynx, known as the voice box, is responsible for sound production. As air passes through the glottis, it vibrates the vocal cords and produces sound waves. The pitch and volume of the sound depend on the vocal cords’ diameter, length, and tension.
As the main organ in the respiratory system, the lungs are essential for the survival of humans. They are responsible for bringing oxygen into the body and transporting carbon dioxide out of the body.
As shown in the image below, air enters the lungs through the trachea, which then splits into the two primary bronchi - one of which goes to the left lung and one to the right lung. The primary bronchi then split into a series of secondary bronchi before eventually reaching bronchioles, which house the alveoli.
Each lung contains about 150 million alveoli - it is their presence that gives lungs their sponge-like nature. Each alveolus has a network of capillaries associated with it, and it is here that gas exchange occurs within the lungs - the deoxygenated blood becomes oxygenated and is taken back to the heart to be pumped around the body.
Right inferior lobe
TED TALK - HOW DO THE LUNGS WORK? CLICK HERE to watch the video.
Left superior lobe
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for respiratory problems or conditions, it is still important to understand common problems that might arise within this system. Understanding common issues relating to the respiratory system can help a nutrition coach identify the need to refer their clients to the appropriate medical or allied health professional.
Common respiratory problems include:
• Bronchitis
• Asthma.
ASTHMA
Bronchitis can be explained by the inflammation of the bronchial tubes, which carry air to the lungs, caused by excessive mucus lining these tubes. Bronchitis can either be acute (a result of severe flu or chest infection) or chronic, which means it is a longlasting ongoing condition.(13)(14)
If a client presents with bronchitis, it is essential that they adhere to any prescriptions from their general practitioner or medical professional.
Asthma is a long-term or chronic disease of the airways, which causes sufferers to have difficulty breathing at times. There is currently no cure; however, there are many options for managing asthma.
Asthma is characterised by the swelling of the walls of the airway, as well as the presence of mucus, thereby creating a restriction to an individual’s breathing.(15)
NORMAL BRONCHIAL TUBE
INFLAMED BRONCHIAL TUBE OF AN ASTHMATIC
The human body comprises over 600 muscles working together to facilitate movement. The major purpose of the muscular system is to:
• Allow for movements of the body
• Uphold the position of the body against the force of gravity
• To allow movements of structures within the body
About half of the body’s weight is made up of muscle. Each type of muscle tissue (skeletal, smooth, and cardiac) in the human body has a unique structure and a specific role.
The muscular system is responsible for the movement of the human body and includes all muscles, from those connected to the skeletal system (such as the biceps and quadriceps) to those inside the body, such as the heart.
While muscles commonly require adequate (not excessive) protein for growth, they also require many vitamins and minerals for optimal health, such as vitamin B1, calcium, magnesium, potassium and sodium.
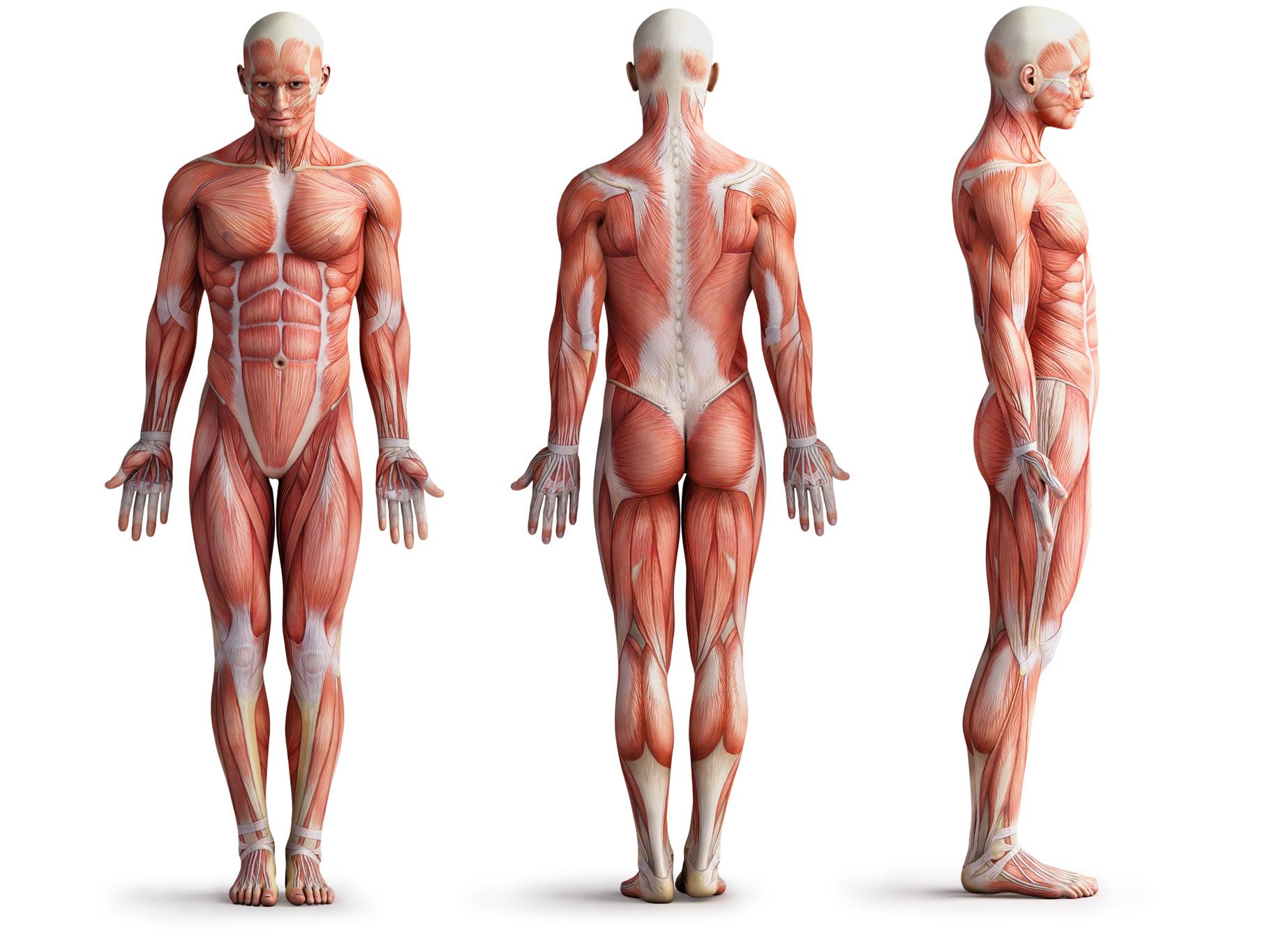
Because the different types of muscle tissue have already been discussed in earlier pages of this resource, this section will focus mainly on the function and importance of healthy skeletal muscle tissues.
TED TALK - HOW YOUR MUSCULAR SYSTEM WORKS? CLICK HERE to watch the video.
Skeletal muscles are under voluntary control and are responsible for the movement of the body. They are attached to bones with the help of tendons or are directly connected to the rough bone surfaces. The function and location of skeletal muscle tissue make it one of the most vital tissues of the human body.
Skeletal muscles are responsible for the following six functions:
1. Production of skeletal movement
2. Maintenance of posture and body position
3. Support and safeguard exit and entry points of the body
4. Support soft tissue
5. Store nutrient reserves
6. Maintain body temperature, heat, and homeostasis.
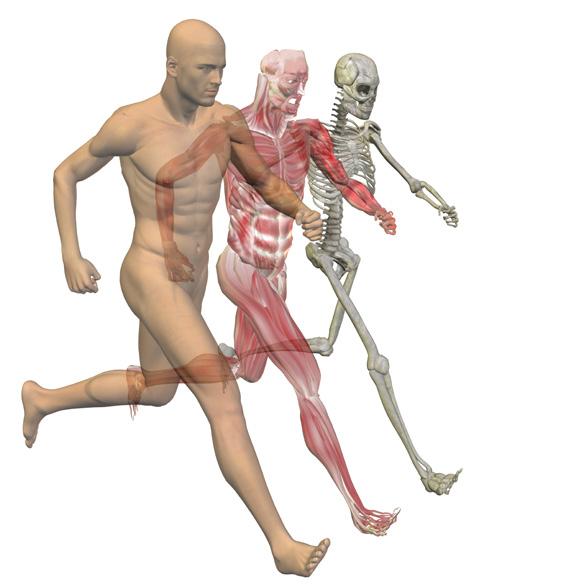
Skeletal muscles do more than just move various parts of the body. They also help with nutrition and body temperature regulation.
One of the main functions of skeletal muscles is that they allow a person to move their body in many ways - muscles pull on tendons, which are attached to bones. Contraction of the muscle causes the muscle to shorten; this moves the specific bone, and thus, that specific body part will move. These movements include the extension and flexion rotation of a person’s limbs, breathing, cycling, typing, writing, etc.
Examples of skeletal muscle movements include:
• The diaphragm, an important muscle for breathing, helps a person to not only inhale and exhale but also laugh, sneeze, and cough
• The gluteal muscles help stabilise the hips for walking and running
• The deltoids in the shoulders help the arms to be raised above the head
• The contraction of the biceps and triceps assists in bending and unbending the arm at the elbow.
The tension in skeletal muscles assists in maintaining posture within the body - without constant muscular activity from the skeletal muscles, it would be impossible to sit upright or stand. The muscles enable a person to hold their head still when reading, writing or exercising and to balance their body weight above their feet when they walk or run.
The numerous openings of the body, such as the mouth, urinary tract and anus, are all covered by sphincter muscles, most of which are skeletal muscles due to voluntary control. When these muscles contract, the opening gets smaller; when the muscles relax, the opening enlarges. As such, they assist in swallowing food, urination, and defecation.
The abdominal wall and the pelvic floor cavity are made up of layers of skeletal muscle. These muscles help to support the weight of visceral organs and act as a defence against injury to the internal tissue.
Excess glucose is converted into glycogen and stored in muscle fibres throughout the body. When energy is needed (as glucose is the body’s preferred fuel source), glycogen is taken from the muscle and converted back into glucose for the body to utilise. Additionally, in times of extreme fasting or carbohydrate restriction, the body can start to break down muscle to produce glucose.
In addition to providing movement and support, skeletal muscles are necessary for some homeostatic functions. When skeletal muscles contract, they generate heat, which warms the body and helps to maintain a relatively constant body temperature. Due to the majority of the body being skeletal muscle, they provide an effective means of temperature regulation.
Evaporation (perspiration)
Radiation
Conduction
Heat produced by muscles
FUN FACTS ABOUT MUSCLES
• Muscle contractions produce heat
• Around 70% of body heat is produced by energy from muscle tissue
• Blood is a vital element in temperature regulation during exercise; this is because blood takes heat from the body’s core and working muscles and redirects it to the skin for cooling when the body is overheating
• When the body shivers in the cold, skeletal muscles assist in the process of temperature regulation.
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for diseases or disorders of the muscular system, it is still important to understand common problems that might arise. Understanding common issues relating to muscular health can help a nutrition coach identify when to refer their clients to the appropriate medical or allied health professional.
Examples of common diseases/disorders relating to the muscular system include:
• Muscular dystrophy
• Tendinosis
• Mitochondrial myopathy
• Myasthenia gravis.
MUSCULAR DYSTROPHY
TENDINOSIS
MITOCHONDRIAL MYOPATHY
Muscular dystrophy refers to more than 30 inherited diseases that all affect the muscle’s strength and result in muscle loss. Some forms of the disease appear at birth; others can appear as late as middle age.
Symptoms can range from mild and worsen slowly, while others can be severe, debilitating and quick-moving. Usually, sufferers lose their ability to walk and sometimes even talk. There is no cure, only a range of treatments.(16)
Not to be confused with Tendinitis (the inflammation of the tendon), Tendinosis refers to the breakdown of the collagen within a specific tendon. This usually occurs from excessive overuse and repetition without letting the tendon heal.(17)
Mitochondrial myopathies (‘myo’ refers to muscle and ‘pathies’ refers to disease) are genetic diseases affecting the cells’ mitochondria. Mitochondria are the energy producers of the cell.
When these components are defective, sufferers can expect to feel extreme fatigue upon physical exertion as well as increased exercise intolerance.(18)
MYASTHENIA GRAVIS
Myasthenia gravis is an autoimmune neuromuscular disease affecting the body’s skeletal muscles. Its name (derived from Greek and Latin) means ‘serious muscle weakness’. This disorder results from a loss of communication between the nerve and the muscle cell.(19)
Understanding the role of the muscular system and how a person’s dietary choices greatly impact it is of significant importance to a nutrition coach. As a nutrition coach, it is essential to understand the anatomy and physiology of the muscular system and have a sound understanding of nutrients required for optimal functioning, such as protein.
Of the three macronutrients, protein is the key macronutrient of relevance for the muscular system. Adequate protein daily is essential for the optimal functioning and overall health of the body’s muscles. Inadequate dietary protein may result in muscle catabolism, whereby the body will begin to break down its muscle mass to supply energy for the body.
The skeletal system involves 206 bones which make up the skeleton of the human body. The skeletal system includes bones and joints, which provide the basic supporting structure of the body.
The main purpose of the human skeletal system is to provide support, locomotion, and protection for the body. Vital organs, such as the brain, heart and lungs, are protected by the skeletal system. In addition to locomotion, support, and protection, the skeletal system produces red blood cells and stores important minerals for the body.
These functions are outlined in more detail in the table below:
The skeleton provides shape, protection and support to the body and keeps the internal organs in their appropriate place. The bones of the pelvis, spine and legs are extremely strong, as they enable the body to stand upright and support its entire weight.
SHAPE AND SUPPORT
Body cavities are hollow spaces framed by the skeleton which hold the internal organs and provide support for the body. For example, the cranium (skull) houses the brain, the chest cavity encompasses the lungs and the heart, and the abdominal cavity encases the organs of the digestive, urinary, and internal reproductive systems.
The muscular and skeletal systems work synergistically as the ‘musculoskeletal system’, which allows body movement and stability. When muscles become active (contract), they pull on ligaments and tendons, which are attached to the bones of the skeleton. This produces movement or holds the bones in a stable position.
Diverse types of movements come from different shapes of bones and their joints. For example, the bones in the leg come together at the knee, forming a type of hinge joint that permits the knee to bend back and forth (flexion/extension). The connecting portions of the hip and shoulder bones have a much different shape, and form of ball-and-socket joints - these allow movement in a number of different directions (flexion/extension, adduction/abduction/ rotation etc).
The skeleton provides mechanical protection by surrounding many of the body’s internal organs, reducing the risk of or preventing injury to these parts of the body.
BLOOD CELL PRODUCTION
The axial skeleton (consisting of the skull, sternum, ribs, and vertebral column) is a key part of the skeleton responsible for protecting vital organs. For example, the skull protects the brain, and the vertebral column protects the spinal cord: both are considered vital organs within the nervous system. The sternum and rib cage work synergistically to protect the heart and lungs.
The larger bones of the skeleton contain bone marrow (a spongy tissue located inside bones). There are two main types of marrow: red and yellow.
Red marrow is responsible for producing all of the body’s red blood cells and many of its white blood cells. These cells transport life-sustaining oxygen to the body tissues. Yellow bone marrow contains primary fat cells but can transform into red marrow if the body needs to increase red blood cell production.
Bones store vital minerals such as calcium and phosphorus for the body. When required, bone releases minerals into the blood to maintain the balance of minerals in the body.
When the amount of one of these minerals in the blood has increased to levels that are too high, it will be stored in the bones. On the contrary, when blood levels of the minerals get too low, they are transferred out of the bones back into the blood.
• The adult human body contains 206 bones
• Bones are living organs that are comprised of protein fibres, minerals, and cells
• Bones provide support and protection for the softer organs and tissues that are vital for the health of the body
• Bones allow muscles to move around joints by giving points where muscles can attach
• Bones also store calcium, iron, and energy as a source for the rest of the body
• During childhood, bones provide the frame in which the body will continue to grow until adulthood
• The typical adult human skeleton has fewer bones than when humans are first born. Bones from the earlier stage of life gradually fuse together as the body matures
• Bone is living tissue that is hard and strong but slightly flexible to resist breaking. The flexibility is due to a substance known as ‘collagen’. The combination of strength and flexibility allows the skeleton to absorb the impact of blows to the body without breaking.
As the skeletal system is responsible for storing certain minerals, is involved in producing blood cells, and provides structural support, nutrition coaches must acknowledge its importance and maintain a basic understanding and appreciation of its roles.
Understanding not only the anatomy and physiology of the skeletal system but also comprehending the key nutrients involved in its functioning (such as calcium) is essential. For example, an individual with low calcium stores may have weaker bones and may be more prone to breaks and fractures.
A nutrition coach can help an individual increase dietary calcium to strengthen bones, thus decreasing their risk of ongoing breaks and fractures.
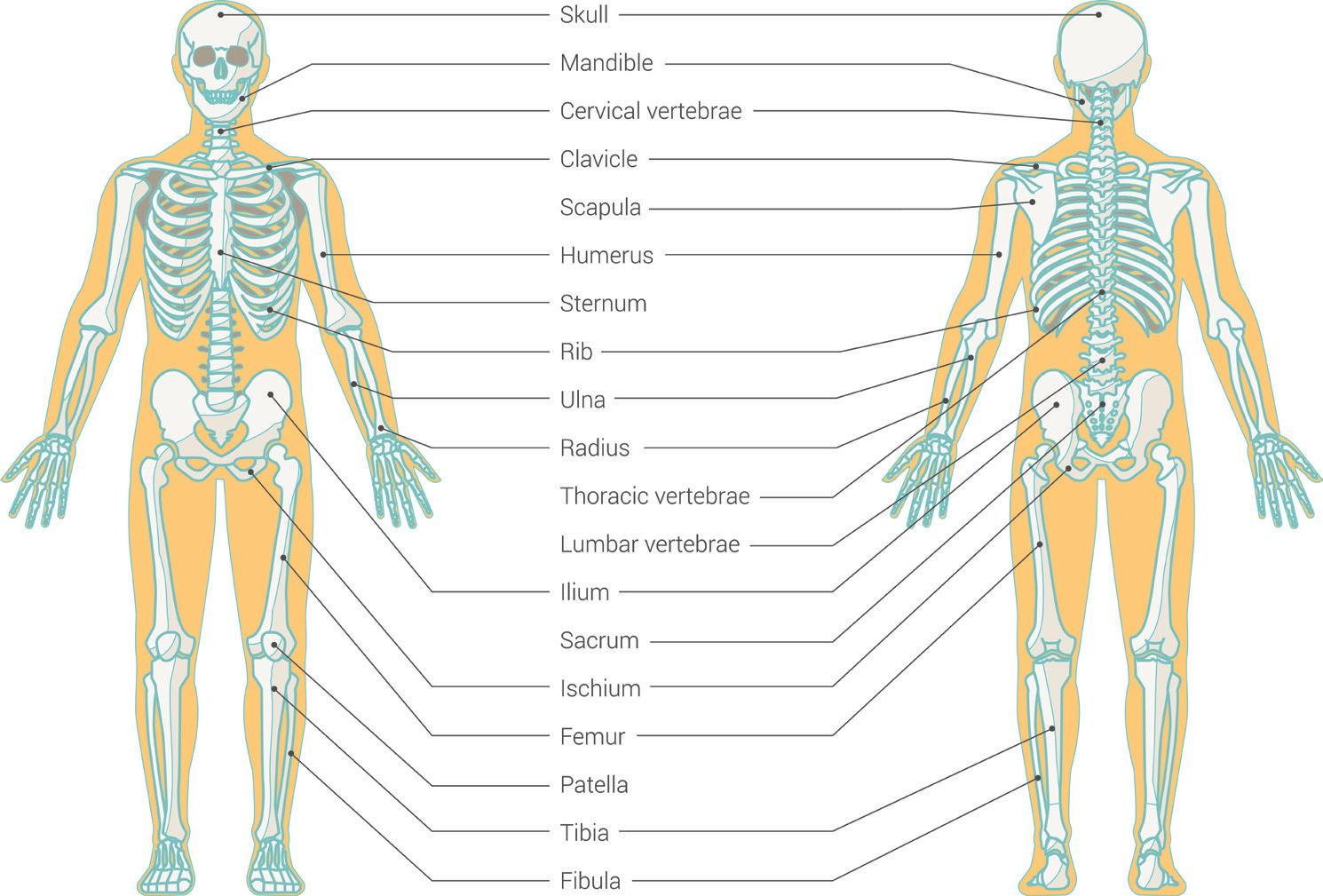
Teeth and dental health are considered part of the skeletal system. However, they are not counted as bones. Instead, teeth are made of the following:
• Dentin
• Enamel
• Cementum
• Pulp.
ENAMEL
Tooth enamel is the hard, outer surface layer of the teeth that protect against tooth decay. Tooth enamel is considered the hardest mineral substance in the body, even stronger than bone.(20)
Although enamel is considered the strongest substance in the body, unlike bones, it can’t regenerate or repair itself after significant damage. This is why treating tooth decay and cavities sooner rather than later is essential.
Dentin is a light yellow, hard, porous layer of tissue directly underneath enamel and cementum. Dentin constitutes the largest portion of the tooth and consists of approximately 70% inorganic matter and 30% organic matter and water.(21)
Dentin differs from enamel because it is living tissue with the ability for constant growth and repair.
Cementum, or root cementum, is a mineralised tissue covering the entire root surface under the gum line, which helps the tooth stay in place.(22) As teeth are not living tissue, it’s important to maintain healthy oral hygiene since early damage to teeth cannot be naturally repaired. PULP
The pulp refers to the innermost region of a tooth. It is composed of nerves, blood vessels and connective tissues. The pulp is surrounded by dentin, which is then covered by enamel.(21)
Although teeth are considered part of the skeletal system, they play a key role in digestion. In carnivores, teeth are designed for killing and breaking down meat, while herbivores’ teeth are made for grinding plants and other food to ease digestion.(23) The term ‘edentulous’ refers to an individual lacking or having no natural teeth, while ‘denate’ is a term that refers to an individual who has natural teeth.
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for dental health concerns or conditions, it is still important to understand common problems that might arise. Understanding common terminology and issues relating to dental health can help a nutrition coach identify when to refer their clients to the appropriate medical professional (such as a GP or a dentist).
Common dental health concerns/problems are outlined in the below table:
HALITOSIS
DENTAL CAVITIES
Gingivitis is a common and mild form of gum disease, which presents as inflammation of the gums at the base of the teeth (called the gingiva). Gingivitis is caused by the build-up of plaque deposits on the base of the teeth, which, as they harden, attract bacteria and lead to infection and irritation.
Poor oral health is the main cause of gingivitis; however, uncontrolled diabetes and some illnesses can also cause this gum disease.(24)
Halitosis is the medical term for bad breath. When food particles are trapped in teeth and mouth, they are naturally broken down by the enzymes in the mouth, causing a release of gases and odours, leading to halitosis.
It is recommended for nutrition coaches to encourage their clients toward good dental hygiene to prevent the onset of halitosis. However, if a nutrition coach suspects a client may have this concern, they should refer to a suitable medical professional.(25)
Dental cavities, otherwise known as tooth decay or caries, occur when acids found in some foods (particularly sugars) react with the enamel of the teeth and drain them of calcium and phosphate. This demineralisation weakens the teeth in vulnerable areas and results in slow decay.
Without medical intervention, the condition can worsen significantly, so it is encouraged to schedule regular dentist appointments to ensure adequate oral health.(26)
The nervous system comprises various networks of cells that signal different impulses throughout the body. It comprises neurons, nerve cells, and neuroglia, or helper cells. Neurons will work to communicate through electrochemical signals throughout the body while neuroglia or glial cells assist the neurons.
The nervous system includes the:
• Brain
• Spinal cord
• Sensory organs
• The nerves.
The above all work together to connect the rest of the body to specific organs. The nervous system is also how the body moves communication throughout the body. For example, if an individual were to place their hand on a hot plate, the nerve cells would send signals to the brain identifying pain, and in response, the brain would send the signal to remove the hand from the hotplate.
The nervous system interacts with the digestive system in the following ways to maintain proper function:
• Digestive processes supply the building blocks for some neurotransmitters
• The autonomic nervous system controls the muscle tone of the digestive tract
• The brain controls drinking and feeding behaviour
• The brain controls the muscles required for eating and elimination
• The digestive system sends sensory information to the brain.
As a nutrition coach, understanding that the nervous system is fundamental to the body’s capacity to function and live in every way is imperative. Previously, this unit discussed how muscles create movement by contracting and pulling on bones; however, it is the nervous system that is responsible for stimulating the muscles and causing them to contract in the first place.
As a nutrition coach, it is essential to ensure adequate nutrient, vitamin, and mineral intake to ensure the nervous system has what is required for its functioning. For example, as the nervous system is inclusive of the brain, a diet with inadequate dietary fat or suboptimal fatty acid ratios would negatively impact the functioning of the human brain and, thus, the overall functioning of the nervous system.
As a nutrition coach, it is therefore important to have a solid understanding of the anatomy and physiology of the nervous system and individual nutrient requirements.
There are three main functions of the nervous system; these functions include:
• Sensory functions
• Integration functions
• Motor functions.
The sensory function collects information from different sensory receptors throughout the body, which are constantly evaluating both the internal and external conditions of the body. From there, afferent neurons will then pass the information to the central nervous system for further evaluation.
Integration is the process in which sensory signals are passed through to the central nervous system via the afferent neurons. The sensory signals that are received are thoroughly inspected and evaluated for decisions to be made. Integration also determines what will be left for memory and what should be discarded. This process takes place in the grey matter of the brain and spinal cord.
When the sensory and integration functions of the central nervous system have done their job, it is time for action. The motor function of the central nervous system is in place when a decision of action has been made. Efferent neurons will then take information from the grey matter of the central nervous system and pass this information throughout the peripheral nervous system to the appropriate effector cells. From there, the effector cell can release a hormone or will move the part of the body accordingly.
If a person experiences severe trauma to their spinal cord, it can often lead to paralysis of their body below the specific point of trauma. For example, if the spinal cord is injured above the nerves that activate their lower body, then they will not be capable of walking again.
This is because the neural messages intended for the legs can no longer reach them. This would be similar to the power cable to a house being cut and the lights going out.
Structurally, the nervous system has two divisions:
1. Central nervous system (CNS)
2. Peripheral nervous system (PNS).
CENTRAL NERVOUS SYSTEM
The body’s master control system.
SPINAL CORD:
A column of nerves between the brain and peripheral nervous system
BRAIN STEM: Connects the brain to the spinal cord.
BRAIN: Divided into three major parts: The hindbrain (lower), midbrain and forebrain.
AUTONOMIC NERVOUS SYSTEM ANS:
The ANS is a division of the PNS that provides autonomic regulation of smooth muscle, cardiac muscle and glandular secretions. Involuntary contractions are controlled at the subconscious level. Also known as the visceral motor system.
SYMPATHETIC DIVISION: Prepares the body for action and stress. This is called the “fight or flight”.
PERIPHERAL NERVOUS SYSTEM
The body’s link to the outside world.
SOMATIC NERVOUS SYSTEM SNS:
The SNS is a division of the PNS that controls skeletal muscle contractions. Voluntary contractions are under conscious control.
PARASYMPATHETIC DIVISION: Calms the body and helps the body to conserve energy.

The brain and spinal cord form the central nervous system (CNS), where information is processed, and responses originate. These are complex organs that include not only neural tissue but also blood vessels and the various connective tissues that provide physical protection and support.
THE CNS IS COMPRISED OF
Dura and arachnoid mater
Medullary cone
Dural sac
THE CNS IS RESPONSIBLE FOR
The CNS is responsible for integrating, processing, and coordinating sensory data and motor commands. The CNS controls higher functions of the nervous system, such as language, creativity, expression, emotions, and personality.
Sensory data conveys information about conditions inside or outside the body. Motor commands control or adjust the activities of peripheral organs such as skeletal muscles. For example, if you stumble or fall, the CNS integrates information regarding balance and the position of the body’s limbs. It then coordinates the body’s recovery by sending motor commands to appropriate skeletal muscles.(1) This all happens in a split second and without conscious effort.
THE PNS IS COMPRISED OF
THE PNS IS RESPONSIBLE FOR
Nerves that are outside the brain and spinal cord form the peripheral nervous system (PNS). The peripheral nervous system includes all neural tissue outside the CNS. It consists of sensory neurons, ganglia (clusters of neurons), and nerves that connect to one another and to the central nervous system.
The PNS delivers sensory information to the CNS and carries motor commands to peripheral tissues and systems. Bundles of axons, or nerve fibres, carry sensory information and motor commands in the PNS. These bundles, with associated blood vessels and connective tissues, are called peripheral nerves, or simply nerves.(1)
The PNS is made up of two main parts:
THE PNS IS RESPONSIBLE FOR
1. The autonomic nervous system (ANS) 2. The somatic nervous system (SNS).
Viseral Effectors
SOMATIC NERVOUS SYSTEM (SNS)
AUTONOMIC NERVOUS SYSTEM (ANS)
The somatic nervous system is a division of the PNS that includes all of the voluntary efferent neurons. The SNS is the only consciously controlled part of the PNS and is responsible for stimulating skeletal muscles in the body. Voluntary contractions occur under conscious control. For example, a person exerts conscious control over their arm as they raise a full glass of water to their lips.
The autonomic nervous system (also referred to as the visceral motor system) is a division of the PNS that provides automatic regulation of smooth muscle, cardiac muscle, and glandular secretions. The ANS controls involuntary (subconscious) effectors such as visceral muscle tissue, cardiac muscle tissue, and glandular tissue.
Within the ANS, there are another two divisions: 1. The sympathetic 2. The parasympathetic divisions.
The sympathetic division forms the body’s ‘fight or flight’ response to stress, danger, excitement, exercise, emotions, and embarrassment (discussed in more detail below). The sympathetic division increases respiration and heart rate, releases adrenaline and other stress hormones and decreases digestion to cope with these situations.
The parasympathetic division forms the body’s ‘rest and digest’ response when the body is relaxed, resting, or feeding. The parasympathetic division works to undo the work of the sympathetic division after a stressful situation. Among other functions, the parasympathetic division works to decrease respiration and heart rate, increase the digestion, and permit the elimination of waste.
TED TALK - SYMPATHETIC NERVOUS SYSTEM ANATOMY
CLICK HERE to watch the video.
TED TALK - PARASYMPATHETIC NERVOUS SYSTEM ANATOMY
CLICK HERE to watch the video.
The diagram below describes how each division regulates functioning organs:
Eyes
Constrict pupil
Salivary glands
Stimulates salivation
Lungs
Constrict bronchi
Heart Slows heartbeat
Stomach Stimulates digestion
Liver Stimulates bile release
Intestines
Stimulates peristalsis and secretion
Bladder Contracts bladder
Spinal cord
Brain
Eyes
Dialate pupil
Salivary Glands Inhibit salivation
Lungs
Dilate bronchi
Heart
Accelerates heartbeat
Stomach Inibits digestion
Liver Stimulates glucose release
Intestines
Inhibit peristalsis and secretion
Kidneys
Stimulate epinephrine and norepinephrine release
Bladder
Relaxes bladder
Chain of sympathetic ganglia

As mentioned previously, the survival technique of fight or flight occurs within the sympathetic division of the autonomic nervous system. The body has innate responses to various forms of stress. Any type of stress, be it physical or emotional, causes a homeostatic imbalance (an internal physiological imbalance in the human body) to which the body needs to respond. While some stressors (such as being stressed about the first day at work) may not require immediate attention, other stressors (such as having a gun pulled on a family member) require immediate action to eliminate the primary stressor.
When faced with stress, it is suggested that the body goes through the following three phases:
1. The alarm phase
2. The resistant phase
3. The exhaustion phase.
This is the initial response to the stressor, which is detected by the sympathetic division of the autonomic nervous system.
During the alarm phase, individuals experience a number of involuntary responses, such as:
• Improved mental alertness
• The mobilisation of energy reserves
• Increased blood flow to muscles,
• Decreased blood flow to the skin, digestive organs, and kidneys,
• Reduction in digestion and urine production
• Increased sweat secretion
• Increased blood pressure, heart rate, and respiratory rate.
It is during this phase that the body has to decide whether it will deal with the stress using the fight or flight response.
The fight response is remaining with the stressor and fighting it (e.g. fighting bullies, performing a show, or confronting an individual with opposing views), whereas the flight response refers to fleeing the stressful environment.
THE RESISTANCE PHASE
THE EXHAUSTION PHASE
The resistance phase refers to stressors lasting more than a few hours. These stressors may include acute illness, starvation, severe depression, severe anxiety, and relationship breakdown. These stressors may last from a few days to a few weeks, thus increasing energy demands by the body.
During the resistance phase, the endocrine system mobilises stored lipid and protein reserves, conserves glucose for neural tissues, conserves sodium and water, and eliminates potassium and hydrogen.
The exhaustion phase, if met, can be fatal. The exhaustion phase refers to the inability to maintain homeostasis and can result in multiple organ failure.
*Homeostasis is discussed in more detail at a later stage in this unit.
Homeostasis refers to the existence of a stable internal environment. It is absolutely crucial for the body to maintain homeostasis to survive in a changing external environment. Homeostatic regulation is the adjustment of physiological systems to preserve homeostasis. All body systems work together in harmony to ensure homeostasis.
•
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for problems or conditions of the nervous system, it is still important to understand common problems that might arise within this system. Understanding common issues relating to the nervous system can help a nutrition coach identify when to refer their clients to the appropriate medical or allied health professional.
Examples of common diseases or concerns relating to the nervous system include:
• Alzheimer’s disease
• Shingles
• Epilepsy
• Parkinson’s disease
• Stoke.
ALZHEIMER'S DISEASE
EPILEPSY
Alzheimer’s is the most common form of dementia, where degeneration occurs within and between neurons. This loss in cells and neurotransmitters significantly affects the brain’s function and, therefore, the rest of the body.
Symptoms can include:
• Mild to severe forgetfulness
• Changes in personality and mood
• Difficulty speaking and understanding
• General difficulty in performing daily activities.
Alzheimer’s usually affects those over the age of 85; however, it can have early-onset in younger individuals.(27)
Shingles is a painful rash that is caused by the same virus as chickenpox. It usually locates itself on one side of the body’s face, neck, back, or abdomen and can occur at any age.
Shingles can be brought on by:
• Extreme physical or emotional stress
• Recent organ transplant
• Medical procedures (such as chemotherapy and bone marrow transplant).
Shingles are treatable, and an individual usually only experiences it once in their lifetime.(28)
Epilepsy presents as recurrent seizures of varying intensity and length. They occur when the regular pattern of the brain’s electrical impulses is disrupted, causing them to fire all at once. The cause of this disruption can sometimes be identified (i.e. brain tumour), but some individuals never actually find out why they have epilepsy.(29)
Parkinson’s disease usually occurs in the older generation but can have early onset.(30) This occurs due to the degeneration of the neurons that produce the neurotransmitter dopamine. This neurotransmitter is responsible for smooth muscle movement and control.
Without adequate levels of dopamine, individuals begin to see symptoms such as:
• Trembling
• Shaking
• Difficulties with balance.
Strokes occur when the blood supply to the brain is disrupted. There are two types of strokes: ischaemic stroke and haemorrhagic stroke. The former is a result of a blockage in the arteries that carry the blood and oxygen to the brain, whereas the latter results from a burst artery.
A stroke usually causes drooping on one side of the face, weakened movement on the same side of the body and slurred speech. Immediate treatment is crucial.(31)
The endocrine system is responsible for the hormonal balance in the human body and includes several hormone-secreting glands and associated organs.
As a whole, the hormones of the endocrine system are responsible for a large number of activities, with the most common being:
• Normal maturation
• Tissue function
• Growth and development
• Sexual function
• Reproduction
• Mood
• Energy production
• Hunger regulation
• Behaviour
• Sleep.
The endocrine system is a collection of glands, including the thyroid, pituitary, hypothalamus, adrenals, pancreas, ovaries and testes. These glands are responsible for a number of roles, including the production of hormones that regulate metabolism, growth and development, reproduction, mood, sleep and sexual function.
The major glands, organs, and tissues involved with the endocrine system include:
• Pineal gland
• Pituitary gland
• Thyroid gland
• Parathyroid glands
• Adrenal glands
• Suprarenal glands
• Pancreas
• Gonads (males: testes, females: ovaries)
• Hypothalamus.

The table below outlines a summary of the function of the major glands, tissues, and organs in the endocrine system.
PINEAL GLAND
• Melatonin.
PITUITARY GLAND
• Luteinizing hormone
• Growth hormone
• Prolactin
• Oxytocin
• Endorphins.
THYROID GLAND
PARATHYROID GLANDS
• Thyroxine (T4)
• Triiodothyronine (T3)
• Calcitonin.
• Parathyroid Hormone (PTH)
• Mineralocorticoids
• Glucocorticoids
• Androgens
• Epinephrine
• Norepinephrine.
ADRENAL GLANDS
• Insulin
• Glucagon.
PANCREAS
• Timing of sexual maturation
• Protection against free radicals
• Circadian rhythms (day-night pattern).
• Controls other glands in the endocrine system
• Stimulates milk production in the mammary glands
• Antidiuretic
• Inhibits pain sensation
• Regulates immunity
• Controls mood
• Stimulates muscle and bone growth
• Growth and development.
• Energy utilisation/expenditure
• Regulates metabolism
• Increases oxygen consumption
• Growth and development
• Decreases calcium ion concentration in body fluids.
• Increases calcium ion concentration in body fluids
• Increases cardiac activity, blood pressure, and blood glucose levels
• Releases lipids by adipose tissue
• Blood formation
• Muscle and bone growth
• Anti-inflammatory effects
• Urinary losses of potassium
• Increases the breakdown of glucose to provide adenosine triphosphate (ATP); thus increasing muscular strength and endurance
• Increases the rate and force of contraction of the heart.
• Acceleration of glucose uptake and utilisation
• Stimulates glycogen formation and breakdown
• Stimulates amino acid absorption and protein synthesis
• Stimulates triglyceride formation and breakdown in/ from adipose tissue
• Stimulates the production of glucose in the liver.
• Androgens
• Inhibins
• Oestrogens
GONADS
• Progestins.
• Follicular and sperm maturation
• Prepares uterus for implantation of sperm
• Prepares mammary glands for secretion
• Secondary sex characteristics
• Inhibits secretion of follicle-stimulating hormone (FSH).
HYPOTHALAMUS
• Sends hormones to be released from the pituitary gland.
• Maintains homeostasis (a state of internal physiological equilibrium) in all areas such as body temperature, pH, or hormonal balance
• Responds to internal and external cues such as hunger, temperature, stress, and blood pressure.
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for problems or conditions of the endocrine system, it is still important to understand common problems that might arise within this system. Understanding common issues relating to the endocrine system can help a nutrition coach identify when to refer their clients to the appropriate medical or allied health professional.
If the endocrine system is not operating optimally or the internal human hormones are not in balance, individuals may suffer from a number of issues such as:
• Diabetes mellitus
• Delayed puberty/growth
• Difficulties falling pregnant
• Hypothyroidism and hyperthyroidism
• Difficulty managing stress levels.
Diabetes mellitus is characterised mainly by hyperglycemia (high blood glucose levels) and exists in two forms (discussed below).
TYPE 1 DIABETES:
DIABETES MELLITUS
DELAYED PUBERTY
An autoimmune disease that is often genetic and results when the pancreas ceases to produce insulin.
TYPE 2 DIABETES:
Can occur through poor diet and lifestyle choices and results from insulin resistance, where the body’s cells are partial towards insulin. This form of diabetes can be reversed, but type 1 cannot be cured.
Delayed puberty refers to the late onset of sexual maturation, where physical and hormonal changes within a teenager do not appear until 13 to 15 years of age. Often, this is simply a genetic predisposition and runs within a family; however, sometimes, it can result from chronic illness or, in rare situations, tumours on either the pituitary gland or hypothalamus.(28
DIFFICULTIES FALLING
PREGNANT
HYPOTHYROIDISM
Reasons for difficulties in falling pregnant can be numerous and vary from woman to woman. Issues with timing and missing the ovulation window is the most common issue. However, various conditions such as polycystic ovarian syndrome, endometriosis, and pelvic inflammatory disease (causing blocked fallopian tubes) can significantly impact the chances of falling pregnant. In men, the issue may result from impaired sperm quality, mobility, or sperm count.(28)
Couples should be aware of their physical health and weight, as well as sperm health, and seek the help of a medical professional if they are concerned.
Hypothyroidism refers to the decreased activity of the thyroid gland, which is responsible for producing certain hormones and chemicals. An underactive thyroid, especially when left untreated, can lead to weight gain, fatigue, joint pain, heart disease and infertility.(32)
HYPERTHYROIDISM
DIFFICULTY
MANAGING STRESS LEVELS
Hyperthyroidism is the opposite condition of hypothyroidism, where the thyroid is overactive in its function. As a result of the increase in metabolic processes, this can cause rapid weight loss, excessive sweating and arrhythmia. Hyperthyroidism is incurable; however, it can be treated with great caution to avoid the development of hypothyroidism.(33)
Stress can be difficult to manage and can present in varying levels of severity depending on the person and situation. Stress can negatively affect the body, so clients are encouraged to address the matter as soon as possible to prevent the onset of stress-related illness.
The digestive system is the most crucial system for a nutrition coach to understand. Because it is such an important system, another unit is based solely on the digestive system later in the course. As such, the information below acts as a brief introduction.
The digestive system consists of the digestive tract and accessory organs. The digestive system is responsible for breaking food down into components that the body can use, such as vitamins, minerals, and macronutrients.
The digestive system breaks down the food and fluid that is consumed into smaller molecules, which the body can then utilise for many purposes, such as:
• Energy production
• Repair of tissues
• Growth (especially through childhood and adolescence)
• Immune function.
Mouth Salivary glands
Oesophagus

Liver
Gallbladder
Small intesine
Appendix
Stomach
Pancreas
Large intesine
Rectum Anus
The digestive system is made up of a number of organs that are in direct contact with food. These organs work together to convert food into energy to feed the entire body. When food is consumed, it passes through a long tube inside the body known as the gastrointestinal (GI) tract, which is also commonly known as the alimentary canal.
The major digestive organs that make up the GI tract (alimentary canal) include the:
• Oral cavity
• Pharynx
• Oesophagus
• Stomach
• Small intestines (also known as the small bowel)
• Large intestines (also known as the large bowel).
The digestive system also comprises accessory organs, which are organs that assist the body in digesting food; however, the food itself does not pass through them. These accessory organs include the:
• Teeth
• Tongue
• Salivary glands
• Epiglottis
• Liver
• Gallbladder
• Pancreas.
The oral cavity refers to the mouth, teeth, and tongue. Food enters the oral cavity voluntarily and is mechanically broken, torn, ripped, and shredded by the teeth. The tongue is used to push food around the oral cavity to assist in its mechanical breakdown.
Three pairs of salivary glands secrete saliva into the oral cavity; these include:
1. The parotid salivary glands,
2. The sublingual salivary glands
OESOPHAGUS
3. The submandibular salivary glands.
These glands produce an average of 1-1.5L of saliva each day. Saliva plays several roles in ingestion and digestion, including lubricating both the oral cavity and the food ingested, moistening the food ingested, making it easier to break down; breaking down chemical bonds, and initiating complex carbohydrate digestion through an enzyme known as salivary amylase.
Food is passed from the oral cavity through to the start of the oesophagus via a voluntary action known as a swallow. The bolus of food enters the oesophagus along with saliva for lubrication. The food is quickly passed down the length of the oesophagus using peristaltic contractions and enters the stomach.
Peristalsis is wave-like muscle contractions that push the bolus of food through various parts of the gastrointestinal tract, such as the oesophagus and intestines.
The stomach is a muscular sac that is highly acidic. The main functions of the stomach include:
• The storage of ingested food
• The mechanical breakdown of ingested food
• The chemical breakdown of food (through the use of specialised enzymes and an acidic environment)
• The production of intrinsic factor required for the absorption of vitamin B12.
From the stomach, the bolus of food is passed through to the small intestine. There are three major parts of the small intestine, these include:
1. The duodenum
2. The jejunum
3. The ileum.
SMALL INTESTINE
LARGE INTESTINE
The internal lining of the small intestine is covered with small finger-like projections known as villi and microvilli, which increase its surface area. The bigger the surface area, the greater the nutrient absorptive capacity.
Individuals with damaged villi (due to undiagnosed coeliac disease, food intolerances, or cancer, for example) tend to have less absorptive capacity and are therefore at heightened risk of nutritional deficiencies, even when consuming a nutritionally adequate diet.
The small intestine begins absorption of nutrients, which are absorbed into the bloodstream and distributed to the rest of the body.
Much like the small intestine, the large intestine is divided into three major parts: the cecum, the colon, and the rectum.
The major role of the large intestine is to:
• Reabsorb water into the body to allow for a compact stool
The small intestine begins absorption of nutrients, which are absorbed into the bloodstream and distributed to the rest of the body.
Much like the small intestine, the large intestine is divided into three major parts: the cecum, the colon, and the rectum.
The major role of the large intestine is to:
• Reabsorb water into the body to allow for a compact stool
• Absorb important vitamins
• Store faecal matter before defecation.
The pancreas is an elongated organ located slightly below and behind the stomach. It is surrounded by other organs, including the small intestine, liver and spleen.
The pancreas has two major functions:
1. Assists with the digestion of food
The pancreas produces enzymes that are important for digestion. These enzymes include trypsin and chymotrypsin to digest proteins, amylase to digest carbohydrates, and lipase to digest dietary fats. Along with the bile (released from the gallbladder), these enzymes assist with macronutrient digestion.
2. Assists with the regulation of blood glucose levels
The cells on the pancreas produce two different hormones which assist in the regulation of blood glucose levels. These two hormones include insulin, which helps to lower blood glucose levels, and glucagon, which helps to raise blood glucose levels.
The liver is a large organ that weighs approximately 1.5kg and plays a key role in metabolic and synthetic functions. The liver is the largest visceral (internal) organ and one of the body’s most versatile organs.
The liver is a large organ that weighs approximately 1.5kg and plays a key role in metabolic and synthetic functions. The liver is the largest visceral (internal) organ and one of the body’s most versatile organs.
The liver is responsible for haematological regulation, where blood passes through the liver and executes the following functions:
• Removes circulating hormones
The liver is responsible for haematological regulation, where blood passes through the liver and executes the following functions:
• Removes antibodies
• Removes circulating hormones
• Removes and safely stores toxins
• Removes antibodies
• Synthesises and secretes bile.
• Removes and safely stores toxins
• Synthesises and secretes bile.
In addition to the above, the liver has two main functions specific to digestion; these include: 1. Metabolic regulation
All blood leaving the digestive tract flows into the spleen and liver. The liver cells remove and store nutrients before the blood returns to the heart. The liver can also mobilise stored nutrients to correct deficiencies and assist in macronutrient metabolism.
In addition to the above, the liver has two main functions specific to digestion; these include: 1. Metabolic regulation
All blood leaving the digestive tract flows into the spleen and liver. The liver cells remove and store nutrients before the blood returns to the heart. The liver can also mobilise stored nutrients to correct deficiencies and assist in macronutrient metabolism.
2. Bile production
2. Bile production
Bile is a digestive enzyme synthesised (approximately 1L produced each day) in the liver, stored in the gallbladder and secreted into the duodenum. Bile is made of water, ions, bilirubin, cholesterol and lipids, collectively known as bile salts. Bile salts aid in the emulsification of lipids, thus increasing their surface area for better digestive and absorptive opportunities.
Bile is a digestive enzyme synthesised (approximately 1L produced each day) in the liver, stored in the gallbladder and secreted into the duodenum. Bile is made of water, ions, bilirubin, cholesterol and lipids, collectively known as bile salts. Bile salts aid in the emulsification of lipids, thus increasing their surface area for better digestive and absorptive opportunities.
The gallbladder is a small organ that is situated under the liver. It is a small pear-shaped, hollow structure that stores and concentrates bile before its excretion into the duodenum.
The gallbladder is a small organ that is situated under the liver. It is a small pear-shaped, hollow structure that stores and concentrates bile before its excretion into the duodenum.
The gallbladder can hold between 40-70ml of bile at capacity. Bile is continuously excreted into the small intestine and can be reabsorbed to be reused to aid in the digestion of subsequent lipid-containing meals.
into the small intestine and can be reabsorbed to be reused to aid in the digestion of classed as an essential organ, as individuals who have their gallbladders removed are still (known as cholecystectomy) generally have to consume smaller amounts of fat in their meals
Bile is essential for the digestion of fats. The gallbladder, on the other hand, is not necessarily classed as an essential organ, as individuals who have their gallbladders removed are still able to survive. As the gallbladder stores bile, individuals who have their gallbladders removed (known as cholecystectomy) generally have to consume smaller amounts of fat in their meals as there is no stored bile for digesting excessive amounts of dietary fat. If fat is consumed in excess for individuals without a gallbladder, that individual may notice fat malabsorption as a result.
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for digestive problems or conditions, it is still important to understand common problems that might arise within this system.
Understanding common issues relating to the digestive system can help a nutrition coach identify when to refer their clients to the appropriate medical or allied health professional.
Common digestive problems can include:
• Gallstones
• Gastroenteritis
• Gastrointestinal bleeding.
Diverticulitis, irritable bowel syndrome and inflammatory bowel diseases such as Crohn’s and ulcerative colitis are discussed in part two of this guide.
Gallstones are hard deposits of either cholesterol or the remnants of blood cells that accumulate in the gallbladder.
Gender, ageing, family history, unhealthy dietary patterns, and rapid weight loss can all lead to the presence of gallstones; however, a healthy diet and lifestyle patterns play a vital role in their prevention.(34)(35)
Gallstones can further impact the digestive system as gallstones can block the bile ducts. This means that bile cannot be passed into the small intestine, which can result in the malabsorption of fat.
Gastroenteritis (commonly shortened to ‘gastro’) is caused by the ingestion or presence of viruses, bacteria or parasites. It is usually characterised by vomiting, nausea and diarrhoea when the stomach becomes inflamed.
GASTROENTERITIS
GASTROINTESTINAL BLEEDING
The body’s immune system is capable of treating gastroenteritis, although it is essential that fluid intake is increased.(34)
Gastrointestinal bleeding can occur either in the higher or lower sections of the gastrointestinal tract.
It is essential that clients presenting with gastrointestinal bleeding (or even the suspicion of) are referred to a general practitioner immediately, as this problem can be due to polyps, cancer, haemorrhoids, or other infections.(36)
This section is merely an overview of the digestive system. The digestive system and the processes of digestion are discussed in more detail in a later unit.
The urinary system is responsible for removing waste products from the human body. The major organs that are involved are the kidneys and bladder.
The kidneys essentially act as a filter system for the blood, removing all waste substances and passing this waste, via the ureters, to the bladder, which is then passed out as urine.
The urinary system is made up of the following organs:
• Kidneys
• Ureter
• Bladder
• Urethra.
KIDNEYS
URETER
BLADDER
URETHRA

The kidneys filter waste products and produce urine. The renal artery carries blood into the kidneys. Once the blood is in the kidneys, the kidneys then filter the blood in what is known as the renal corpuscle and remove waste products. The waste products are then mixed with water which creates urine. The filtered blood moves out of the kidneys via the renal vein.
The ureter is a 25-30cm long tube responsible for transporting urine from the kidneys to the bladder.
The bladder is a muscular sac used by the body to temporarily store urine before elimination. Once the bladder is approximately 50% full, the body signals to the brain that it needs to eliminate the urine.
The urethra is a tube (approximately 4cm long in females and approximately 18-20cm long in males) that transports urine out of the human body through voluntary bladder contraction.
The contents of urine can indicate a lot about an individual’s health. Doctors may require an individual to complete a urinalysis to assist with their diagnosis or treatment. Some waste products may be found in excess if the body is not absorbing nutrients adequately or if certain nutrients are being taken in excess. While at other times, the kidneys may not be working effectively due to disease, and this may result in inadequate waste clearance.
If a client has any abnormalities in regards to their kidneys, it is essential that a referral is made to a nephrologist or local general practitioner (GP) before continuing their care, as special precautions may be required.
The table below outlines some substances which can be found in the urine, some of which are normally found and others that may indicate an inflammatory or diseased state. While some of the following substances have been listed as normal, it is important to remember that while a substance may be normally present, it can also reach higher levels which would then class the substance as abnormal. Therefore, it is important to always read and utilise reference ranges on the results and never diagnose or treat abnormal results, as this is outside the scope of practice for a nutrition coach.
UREA A byproduct of protein metabolism
CREATININE A compound produced by the metabolism of creatine
AMMONIA A colourless gas made of nitrogen and hydrogen
URIC ACID The breakdown product of nitrogenous metabolism
NORMAL OR ABNORMAL
Normal
Normal
Abnormal
Normal
BILIRUBIN A product of haemoglobin breakdown formed in the liver Abnormal
CARBOHYDRATES Unutilised and unabsorbed glucose passed out in the urine Abnormal
KETONE BODIES
Products produced naturally when the body has nil serum (blood) glucose
LIPIDS Unabsorbed fat passed out in the urine
AMINO ACIDS Unutilised and waste protein passed out in the urine
SODIUM Electrolyte
CHLORIDE Electrolyte
POTASSIUM Electrolyte
CALCIUM Mineral
MAGNESIUM Mineral
Normal (in small amounts only)
Normal (in small amounts)
Normal (in small amounts)
Normal
Normal
Normal
Normal
Normal
• Another word for urination is micturition.
• Urine has a pH of 4.5-8
While it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for urinary system problems or conditions, it is still important to understand common problems that might arise within this system. Understanding common issues relating to the urinary system can help a nutrition coach identify when to refer their clients to the appropriate medical or allied health professional.
Common diseases or concerns relating to the urinary system include:
• Bladder infection (cystitis)
• Incontinence
• Kidney infection
• Kidney stones.
BLADDER INFECTION (CYSTITIS)
INCONTINENCE
Cystitis, also known as a urinary tract infection (UTI), causes inflammation in the bladder due to a bacterial infection. Usually, the bacteria responsible for the inflammation is E.Coli, which is located within the bowel.
Sexual intercourse or extremely unhygienic bathroom situations can lead to cystitis; however, some medications and even radiation can also increase the risk of this infection.(37)
Incontinence refers to the inability to control the bladder. Incontinence is first experienced in children (who are still learning this type of control) but can resurface as one enters older age.
Incontinence is quite common amongst the older generation, particularly those suffering from varying forms of dementia or other illnesses.
A kidney infection usually begins as the above-mentioned UTI; however, it becomes more serious as the infection ‘backs up’ the urethras and travels to either one or both kidneys.
KIDNEY INFECTION
KIDNEY STONES
This concern requires immediate medical attention because, if not treated, the infection can cause serious kidney damage and result in the bacteria entering the bloodstream.
Symptoms include:
• Frequent urge to urinate
• Pain in the back, side or abdomen
• Burning during urination.(38)(34)
Kidney stones are the build-up of solid materials (minerals and salts) which make their way into the urine. Some can be as small as a grain of sand and pass through the urinary tract without any symptoms or medical intervention, while others can accumulate to be quite large. In these instances, the stones are likely to get stuck in the urinary tract, causing great pain and discomfort and requiring medical intervention or treatment.(39)
The role of this system is to protect the body from loss of water and abrasions from the outside world. The skin is what makes up the majority of this system
Although the skin is only a few millimetres thick, the integumentary system is the largest of all body systems and is made up of two primary components:
1. The cutaneous membrane (skin)
2. Accessory structures (i.e. hair, nails, and exocrine glands such as sweat glands).
Hair
Sebaceous gland
Epidermis
Subcutaneous
Cutaneous membrane is the scientific word for skin.
The skin can be further broken down into two components:
1. The epidermis
Pacinian corpuscle
The epidermis is the superficial layer of epithelium that is exposed to the outside world.
2. The dermis
The dermis is the connective tissue located beneath the epidermis
Many skin conditions can develop or worsen due to dietary choices, and the skin can often indicate what is going on within the body. In the same way, there are specific nutrients that play a role in skin health. These include but are not limited to vitamins A, D and E as well as mono- and polyunsaturated sources of fats. It can be useful in consultations to acknowledge any skin conditions as it is possible that these can be improved as a result of dietary changes that are implemented for a client to achieve their nutrition-related goals.
It is important to remember that while a nutrition coach can acknowledge a particular skin condition, it is outside their scope of practice to diagnose or treat it, and they are required to refer on to an appropriate professional.
• The human body has approximately 2.5 million hairs, of which 75% are on the general body and not on the head!
• The integumentary system accounts for approximately 16% of an individual’s total body weight.
Accessory structures include hair, nails and specific glands (such as sweat glands). These structures mostly originate in the dermis and protrude through the epidermis, becoming visible on the skin surface.
The table below describes each accessory structure in more detail:
Hair covers the majority of the human body with the exception of a few areas, including:
• The sides of the fingers and toes
• The soles and sides of feet
• The palms of hands
• The lips
• Part of external genitalia.
Hair, depending on where it is located, plays various roles:
1. Head
Hair on the head protects a person from UV radiation and provides warmth for the scalp.
2. Nostrils and ears
Hairs around the nose and ear entrances help prevent the entrance of foreign objects such as dust, sand, and insects.
3. Eyes
Eyebrows prevent excessive sweat from entering the eyes, while eyelashes are helpful to prevent foreign particles, such as sand, from entering the eyes.
EXOCRINE GLANDS
Nails provide protection for the tips of toes and fingers as well as providing structural support. Nails are made of dead, keratinised epidermal cells. The appearance of a nail can provide valuable information regarding an individual’s health. For example, nails may get white marks on them with nutrient deficiencies or may turn yellowish in individuals with chronic respiratory or thyroid disorders.
The integumentary system has several different types of glands, with the two most important ones being sebaceous glands and sweat glands. Sebaceous glands are glands that secrete an oily discharge into hair follicles.
There are two types of sweat glands:
1. Apocrine sweat glands
2. Merocrine sweat glands.
Apocrine sweat glands are located in the armpits, around the nipples, and in the pubic region, whereas merocrine sweat glands are far more numerous (2-5 million merocrine sweat glands per person) and are located all over the body. Apocrine sweat glands shed their cytoplasms and secretory products, whereas, with merocrine glands, only the product is released via a process known as exocytosis.
Sweat performs several functions in the integumentary system; these include:
• Assisting with body temperature control (by cooling the body)
• Excreting excess water and electrolytes.
The integumentary system has many important functions; these include:
DEFENCE
SENSORY
EXCRETION
TEMPERATURE
VITAMIN D
The integumentary system is the body’s first line of defence for the underlying tissues and organs against any outside intrusion, abrasion, impact, or offence. Examples include cuts, scrapes, sunburn, and bites.
Information is gained from sensory neurons about pain, pressure, temperature, and touch, which is communicated back to the central nervous system (CNS).
Examples include:
• Touching a hot plate
• Feeling a mosquito land on the skin
• Sitting too close to a fire.
Sensory neurons are nerve cells that obtain information relating to sensation or physical senses from the external environment and transmit the messages via electrical impulses to the appropriate cells in the internal environment.
Exocrine glands are responsible for the excretion of salts, water and organic waste. Examples include the sweat glands and the salivary glands.
The integumentary system is responsible for maintaining normal body temperature. Examples include sweating to cool the body and goosebumps to insulate the body.
Ultraviolet (UV) radiation from sunlight causes the epidermal cells to convert a steroid into vitamin D3, also known as cholecalciferol.(40)
The liver then converts cholecalciferol into a hormone known as calcitriol, which is essential for the normal absorption of calcium and phosphorus. Vitamin D is, therefore, crucial for calcium regulation to ensure the production and maintenance of strong and healthy bones.
The integumentary system also regulates the production of melanin, a pigment occurring in the eye’s skin, hair, and iris, which protects underlying tissues from UV radiation.
Lipids are stored in adipocytes (fat cells) in the dermis as well as adipose tissue in the subcutaneous layer. An example of this is an increased amount of fat on the thighs as weight is gained. This can be measured through circumference measures or skin folds.
The integumentary system works with the cardiovascular and nervous systems, ensuring important sensory information is communicated. Beneath the integumentary system is a complex network of blood vessels with sensory receptors.
Through this, the body communicates information about various sensations, including touch, pressure, pain, and temperature back to the CNS.
It is important to remember that while a nutrition coach can acknowledge a particular skin condition, it is outside their scope of practice to diagnose or treat it, and they are required to refer on to an appropriate professional. Dermatologists are the appropriate physicians specialising in treating diseases, disorders and skin injuries, hair and nails.
Examples of other common skin conditions are outlined below:
• Acne
• Eczema
• Skin cancer.
Acne refers to a condition that affects the skin’s oil glands. Small holes in the skin (pores) connect to oil glands under the skin, and these glands make a substance called sebum. The pores connect to the glands by a canal called a follicle.
When the follicle of a gland clogs up (with dirt, oil and bacteria), acne can develop. Acne is the most common skin condition and mainly affects those between the ages of 15 to 24 years.(41)
Eczema is an allergic reaction that is exhibited as dry, itchy skin patches resembling rashes. It may be partnered with swelling of the skin, flaking, and in severe cases, bleeding.(42)
Eczema is best treated with topical anti-inflammatory creams and ointments, which can reduce itching and redness or for mild symptoms; over-the-counter medications are also effective.(43)
Skin cancer occurs when skin cells are damaged by overexposure to ultraviolet (UV) radiation from the sun. Approximately two in three Australians will be diagnosed with skin cancer by the time they are 70 years old. Non-melanoma skin cancer is more common in men, with almost double the incidence compared to women.(44)
Skin cancer symptoms can include:(34)
• Any crusty, non-healing sores
• Small lumps that are red, pale or pearly in colour
• New spots, freckles or any moles changing in colour, thickness or shape over a period of weeks to months.
The reproductive system is the only system in the human body that is not required for the survival of an individual. However, as the reproductive system is imperative to the survival of the human race, many scientists believe it to be the most important body system. The reproductive system in both males and females comprises internal and external organs that work in conjunction with each other for reproduction (or procreation).
REPRODUCTIVE SYSTEM
FEMALE REPRODUCTIVE SYSTEM
The male and female reproductive systems are slightly different given their different functions - while a female’s sex organs are located internally within the pelvis, the male reproductive organs are located both inside and outside the pelvis.
The male reproductive system is inclusive of the following:
• Gonads (testes)
• The duct system (made up of the epididymis and the vas deferens)
• Accessory glands and organs
• External genitalia (such as the penis).
GONADS
PENIS
In the male reproductive system, the male gonads are responsible for producing the sex hormones called androgens. The testes also produce the male gametes, also known as sperm. Sperm is ejaculated from the penis in a mixture known as semen.
The penis is the male organ used in sexual intercourse. It consists of three parts:
1. The root (the region that attaches to the wall of the abdomen)
2. The body (also known as the shaft)
3. The glans (identified as the cone-shaped region at the end of the penis and also known as the ‘head’ of the penis).
Sperm are the reproductive cells released through the end of the penis. This occurs when a man reaches sexual climax. When the penis is in an erect state, urine is blocked from the urethra; this allows only sperm to be ejaculated when a man orgasms.
The male reproductive tract starts at the epididymis, continues through the 4045cm long vas deferens and ends at the 18-20cm long urethra. The urethra spans from the bladder to the tip of the penis.
The male reproductive accessory glands include the seminal vesicles, the prostate gland, and the bulbourethral glands.
These glands are responsible for:
• Activating sperm
• Providing adequate nutrients to enable sperm motility
• Propelling sperm along the reproductive tract through peristaltic contractions
• Producing buffers that counteract the acidity of the urethra and vagina.
An average male produces half a billion sperm each day, while a female produces only one immature gamete per month.
The female reproductive system consists of several internal organs around the pelvic region.
The female reproductive system contains the:
• Ovaries
• Fallopian tubes
• Uterus
• Vulva
• Mammary glands
• Vagina
• Breasts.
Fallopian tube
Uterine
These organs are involved in the making of sex hormones and also the creation and transportation of gametes.
This reproductive system also facilitates the conception of ova (the female reproductive cell or egg) by sperm and assists in the growth of offspring while a woman is pregnant.
The vagina is an internal muscular canal (approximately 10cm in length). This canal acts as the entry point for the reproductive tract. It also serves as the exit from the uterus during menses (menstruation) and childbirth.
The ovaries are considered the ‘female gonads’; they are a pair of small internal organs that are responsible for:
• The production of mature female gametes (oocytes, also known as eggs’)
OVARIES
• Secretion of female sex hormones (e.g. oestrogen and progesterone)
• The secretion of inhibin (which is involved in the feedback cycle for the production of follicle-stimulating hormone).
The fallopian tubes are narrow tubes connected to the upper region of the uterus and act as a pathway for the ova to transit from the ovaries through to the uterus.
UTERUS (WOMB)
Fertilisation of an egg by a sperm normally occurs in the fallopian tubes. The fertilised egg is then carried through to the uterus, where it embeds itself into the uterus lining.
The uterus is located in the middle of the pelvis, in front of the rectum and behind the bladder.
The uterus is divided into two parts:
1. The cervix (the lower region that opens into the vagina)
2. Corpus (the main body of the uterus).
The corpus is designed to expand to carry/hold a growing baby, and the cervix dilates to enable the baby to travel through the birth canal.
Although these two cycles can be confused as the same thing, they have very different aspects and functions. The menstrual cycle (which is most commonly referred to) only includes the changes that occur within a woman’s uterus, whereas the ovarian cycle specifically refers to what takes place within the ovaries with the preparation of the egg cell.
A woman experiences these cycles simultaneously, during which the menstrual cycle is dictated by the ovarian cycle. These cycles are also known as a period and occur between puberty and menopause, during which time they serve to regulate sexual reproduction.
For easier understanding, the table below provides different explanations for each of these cycles:
The monthly ovarian cycle controls the development of the egg within the ovary.
This cycle includes:
• The development of the follicle
• Ovulation
• The secretion of hormones by the follicle
• The formation and degeneration of the corpus luteum.
This process takes place in the ovary over approximately 28 days (this differs for each individual) in which it is managed by the hormones: gonadotropin-releasing hormone (GnRH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), progesterone and oestrogen.
The ovarian cycle includes the formation and maturation of the follicle and oocyte in preparation for ovulation (follicular phase) and the return of the empty follicle and ovary to its original state for the beginning of the next cycle (luteal phase). These phases will be discussed in more detail below.
The monthly menstrual cycle is also known as the uterine cycle because it specifically refers to the changes to the uterine wall in preparation for embedding an embryo. This cycle occurs in response to the levels of the hormones called progesterone and oestrogen, associated with the ovarian cycle.
The menstrual cycle has three phases that occur at the same time as the ovarian cycle:
THE MENSTRUAL (UTERINE) CYCLE
The shedding of the uterine wall, known as the endometrium
2. The proliferative phase
Epithelial cells restore the integrity of the endometrium, and it begins to thicken and develop mucous glands important for implantation.
3. The secretion phase
Glands enlarge, increasing the secretion rate, and blood supply to walls increases. Begins at ovulation and ends at the disappearance of the corpus luteum.
Menses and the proliferation phase occur during the follicular phase, and the secretory phase occurs during the luteal phase of the ovarian cycle.
The ovarian cycle can be divided into two phases:
1. Follicular Phase (two weeks before ovulation)
2. Luteal Phase (ovulation and one week post ovulation).
The follicular phase is also known as the preovulatory phase. This phase is the lead up to ovulating where the body is forming follicles (fluid-filled structures where the oocytes grow to maturity). This phase begins with the formation of primary follicles, which house a primary oocyte. They then mature into secondary follicle(s) and mature further into tertiary follicle(s), which now hold a secondary, or mature, oocyte. This phase generally takes 10 to 13 days after the start of the ovarian cycle. Ovulation occurs between days 1 and 16, and identifies the end of the follicular phase of the ovarian cycle and the development of the luteal phase.
The luteal phase is also known as the postovulatory phase because it occurs after ovulation. Once the oocyte is released from the ovary, the follicle in which it was housed then collapses, before specific cells invade the area to begin its degeneration. This creates an endocrine structure known as the corpus luteum. The primary hormone in the luteal phase is progesterone, which is produced by the corpus luteum, and is responsible for preparing the uterus for pregnancy. The degeneration of the corpus luteum then marks the end of the ovarian cycle.
Although reproductive health falls outside of a nutrition coach’s scope of practice, it is still essential to have an understanding of this body system to identify and confirm the health status of a client and to know when to refer the client to an appropriate medical or allied health or medical professional.
Examples of common diseases or concerns relating to the reproductive system include:
• Endometriosis (female only)
• Sexually transmitted diseases (i.e. genital herpes, syphilis, gonorrhea)
• Polycystic ovarian syndrome (female only)
• Prostate cancer (male only).
Endometriosis refers to the abnormal growth or presence of the endometrial or uterine tissue in any location outside the endometrial cavity. This tissue can grow on the outside of the uterus, ovaries and even on parts of the bowel and pelvis and is a problem occurring in approximately 10-15% of women.(34)
ENDOMETRIOSIS
SEXUALLY TRANSMITTED DISEASES (I.E., GENITAL HERPES, SYPHILIS, GONORRHOEA)
Although displaced, this endometrial tissue continues to thicken, break down and bleed with each menstrual cycle. As a result, the individual can experience severe pain and even infertility.(34)(45)
There are more than 20 different types of sexually transmitted diseases (STDs) that present as a result of bacteria, parasites or viruses. They can arise in both men and women; however, the consequences for women can often be a lot more severe (such as causing infertility or harming the baby if a woman is pregnant).
STDs that are bacterial or parasitic can be treated with antibiotics, but those that are viral are often incurable.(28)
Polycystic ovarian syndrome (PCOS) occurs when a woman’s ovaries or adrenal glands produce too much of the male sex hormones, which leads to the growth of cysts on the ovaries.
POLYCYSTIC OVARIAN SYNDROME (PCOS)
PROSTATE CANCER
This overproduction of male hormones also results in increased growth of body hair in male patterns (such as on the chest, face and stomach etc.), as well as thinning hair and acne.
Common signs of PCOS can include:
• Irregular or infrequent periods
• Abnormally heavy periods
• Insulin resistance.(34)(46)
Cancer of the prostate affects 1 in 7 men over the age of 75 and 1 in 5 men over the age of 85 years. It is an age-related disease, meaning that as males age, their chances of prostate cancer increases.
Prostate cancer forms when abnormal cells grow in the prostate and develop over time. It can cause difficulty and pain when urinating, as well as pain in the back or hips and the presence of blood in the urine.(34)(47)
The lymphatic system is responsible for safeguarding and preserving the human body from environmental hazards such as infectious diseases and internal threats such as tumours. The lymphatic system is responsible for an individual’s immunity, providing immune responses to fight an array of internal and external threats and pathogens.
The lymphatic system is made up of:
• Lymphocytes
• Lymph fluid
• Lymphatic vessels
• A number of lymphoid tissues (tonsils)
• Lymphoid organs (lymph nodes, spleen and thymus).
LYMPHOCYTES
LYMPH FLUID
LYMPHATIC VESSELS
LYMPHOID TISSUES
Lymphocytes are the primary cells of this system and are pivotal in defending against and fighting infection and disease. Lymphocytes use a variety of chemical and physical attacks on various pathogens to ensure they are unable to do any harm to the human body.
A fluid similar to plasma (the colourless fluid part of the blood), however, contains a lesser amount of proteins.
Lymph is also a colourless fluid and contains white blood cells, which are responsible for immunity and fighting infections.
A complex network of lymphatic vessels carries lymph from peripheral tissues (extremities) to the veins. These vessels collect fluid from the tissues and take it to the lymph nodes, where bacteria and other harmful substances are filtered out and destroyed. The fluid is then returned to the circulatory system via the veins.
The smallest type of lymphatic vessels are called lymphatic capillaries and are present in almost every tissue and organ in the human body.
Lymphoid tissues are connective tissues that are dominated by lymphocytes. Examples of lymphoid tissues are the tonsils and the mucosa-associated lymphoid tissue.
LYMPHOID ORGANS
Examples of lymphoid organs include the lymph nodes, spleen, and thymus. Lymph nodes filter lymph before it reaches the venous system. The thymus produces a number of hormones that play an important role in the maintenance of immunological defence. Finally, the spleen is responsible for removing abnormal blood cells, storage of iron, and initiating immune responses as required.
Lymphocytes account for approximately 1kg of total body weight.
As the lymphatic system is responsible for protecting the human body against various threats, it has two major defence mechanisms: non-specific defence and specific defence.
When the body encounters a pathogen, virus or harmful bacteria, it will activate one of its two defences:
1. Non-specific defence
2. Specific defence
Non-specific defences do not identify what type of threat the body has and provide the same response no matter what the threat may be. Non-specific defences are present from birth.
Examples of non-specific defences may include:
• Fever
• Inflammation
• Physical barriers (such as the skin or mucous membranes)
Specific defences, on the other hand, fight certain threats and pathogens in a specific way.
One type of defence may be able to kill one type of virus, but not another, and therefore specific defences ensure the correct defence is used depending on what the body is being threatened by.
The body’s specific defence is also known as immunity. Those with poor immunity tend to get sick more often due to poor specific defence.
Immunity is one of the responsibilities of the lymphatic system. Immunity refers to the specific defence the human body has against pathogens. An individual with poor immunity generally has poor specific defences against particular threats, pathogens and invaders.
Immunity can be categorised into either:
• Innate immunity
• Acquired immunity.
Innate immunity is the immunity one is genetically given, not influenced by previous exposure to a specific invader.
The only exception to this rule is AIDS or other diseases which decrease the ability for specific defence.
Acquired immunity, on the other hand, refers to immunity gained only through exposure to specific pathogens. Acquired immunity is not present at birth but rather built up through life experiences such as vaccinations and exposure to various diseases, bacteria, and viruses. Examples of acquired immunity are exposure to chickenpox or getting the hepatitis B vaccination.
The intention of vaccination is to expose the body to a small sample of a natural pathogen in a somewhat controlled environment. When the individual is exposed to the pathogen in a small quantity, the body creates a defence against that particular pathogen, and when exposed again in a natural setting, it is more likely to be able to fight off the invader.
Immunity is also a responsibility of the digestive system. The immune system isn’t contained to just one body system. In fact, aspects of several body systems work together to ensure an adequate immune response for an individual.
Like many other body systems, it is outside the scope of practice of a nutrition coach to diagnose or provide treatment for problems or conditions relating to the lymphatic system. However, it is still important to understand common problems that might arise within this system.
Understanding common issues relating to the lymphatic system can help a nutrition coach identify when to refer their clients to the appropriate medical or allied health professional.
Examples of common diseases or problems relating to the lymphatic system include:
• Glandular fever
• Tonsillitis
• Crohn’s disease
• Lymphoedema (primary and secondary).
Glandular fever is caused by the Epstein-barr virus infection, which is spread through saliva.
It can take anywhere between 30 and 50 days for the infection to develop and cause noticeable symptoms such as:
• Extreme fatigue
• Sore throat
• Swollen glands.
Individuals are contagious for months after the fever and can experience symptoms for up to months at a time.(48)
CROHN’S DISEASE
Tonsillitis is simply the swelling of tonsils due to the presence of bacteria. They will often become red and swollen, causing pain when swallowing. Those with tonsillitis will also experience fevers, headaches and swollen lymph nodes in the neck. Tonsillitis is treatable with antibiotics and other medications; however, those with recurrent tonsillitis tend to have them removed surgically.(49)
Crohn’s disease is a type of inflammatory bowel disease (IBD) that can affect different parts of the digestive system in different people. Crohn’s disease affects all layers of the intestinal wall, not just the mucosal layers on the surface, and can severely affect nutrient absorption.(34)
Individuals with Crohn’s disease experience abdominal pain, frequent diarrhoea, rapid weight loss and many other symptoms.(50)
LYMPHOEDEMA
(PRIMARY AND SECONDARY)
Lymphoedema is characterised by swelling that occurs in one arm or leg, or sometimes both arms and legs. The swelling results from the build-up of lymphatic fluid that hasn’t been properly drained from the body.
Primary lymphoedema is a rare genetic condition that indicates an issue with the lymphatic system as a whole; whereas secondary lymphoedema can occur after surgery or during cancer treatment, such as radiation.(51)(52)
Through education and experience, a nutrition coach can recognise and identify a healthy body system compared to an unhealthy one. This is important so that a nutrition coach can recognise and report signs or symptoms that suggest there may be an issue or problem relating to their client’s individual health.
All living organisms have particular characteristics that distinguish them from living or nonliving. In other words, when it comes to the human body (the most complex form of life), specific processes are crucial for an organism to sustain healthy functioning body systems.
These processes, which are all necessary for survival, are commonly known as life processes and include:
1. Nutrition/feeding
2. Order and organisation
3. Movement
4. Metabolism and energy utilisation
5. Adaptation/responsiveness
6. Sensitivity (taste, smell, sight, hearing, and touch)
7. Growth and development
8. Reproduction
9. Excretion
10.Homeostasis.
Different sources organise lists of life processes in different ways; some lists show four processes while others show as many as ten. The same life processes appear on all the lists; however, they are sometimes grouped and labelled differently.

Nutrition refers to the process by which the body utilises food as an energy source. This imperative process helps living organisms obtain and maintain their energy from various food sources to survive.
Nutrients found in food and liquids contain chemical substances that are then used by the body for energy, cell building, and repair. Carbohydrates, vitamins, minerals, proteins, and fats are all vital in maintaining a healthy body. For example, calcium helps make bones strong, and vitamin D is needed to absorb sufficient amounts of calcium.(53)
When an organism (i.e. plants or humans) is deprived of essential nutrients, symptoms of deficiencies can begin to develop. For example, plants can become yellow through a lack of the mineral magnesium needed to produce chlorophyll, and humans can develop scurvy when they lack vitamin C in their diet.(54)(55)

The human body is an incredibly organised organism. It is composed of trillions of cells that are organised internally to maintain distinct internal compartments. In more complex organisms such as humans, cells also have specialised functions. Specialised cells are organised into tissues, in which tissues then form organs, organs then form organ systems and the outcome of the combined organ systems then make up the organism.
In addition to the structural organisation, the human body maintains stringent physiological and biochemical processes to ensure survival. There are also numerous ‘backup’ processes that can be activated at any moment, should the need arise.
*The organisation of the human body is discussed in more detail on the previous pages of this resource (structural levels of organisation).
Living organisms have the ability to move, especially when responding or reacting to stimuli from the environment. Movement of the human body ranges from the smallest movements (such as a smile, a twitch of an eyebrow or breathing) to larger movements (such as walking and running).
It is the nervous system, muscular system and skeletal system together that are responsible for the facilitation of movement. Without this ability, the human body wouldn’t be able to perform the life functions necessary to survive.
Living organisms have the ability to move, especially when responding or reacting to stimuli from the environment. Movement of the human body ranges from the smallest movements (such as a smile or a twitch of an eyebrow) to breathing and the flow of blood cells to much larger movements (such as walking and running).
Metabolism falls under the science of biochemistry, and it is important for nutrition coaches to understand what metabolism means and how it relates to the study of nutrition.
BIOCHEMISTRY
Biochemistry (‘bio’ meaning biological) is the study of chemicals and chemical reactions in the body.
Metabolism is the set of chemical reactions that release energy for cellular processes. All living organisms require energy to complete tasks such as walking, eating, reading, sleeping and reproducing. In other words, metabolism refers to all the chemical processes the body uses to produce energy.
There are hundreds of known metabolic pathways in the human body, and many remain to be mapped. However, put simply, when food is consumed, it gets broken down and absorbed by the body, and the resulting nutrients get shuttled into cells of the liver, muscles, and other tissues to be used for energy.
METABOLIC PATHWAY
A metabolic pathway refers to a series of processes found in biochemical reactions that help change molecules into different, more readily usable materials.
Energy production occurs in the mitochondria of the cell. The mitochondrion is an organelle (or specialised structure) known as the ‘powerhouse’ of cells and is where adenosine triphosphate or ATP is produced. ATP, known as the body’s energy currency, makes all human processes possible. The image below shows a mitochondrion and the pathways that each metabolite (simple sugar, fatty acid or amino acid) must go through for energy to be produced.
Metabolism consists of the following two processes that are carefully regulated to remain in balance:
1. Catabolism
The process of breaking down food or nutrients into simpler/smaller forms to release energy. For example, in a catabolic state, more proteins are being broken down than made.
2. Anabolism
The process of using energy for the growth and repair of cells in the body. For example, in an anabolic state, more proteins are being made than broken down.
Certain health concerns can affect an individual’s metabolism; these include:
• Hyperthyroidism
This condition can increase an individual’s metabolism/metabolic rate and cause sudden weight loss, excessive sweating, or an altered heartbeat.
• Hypothyroidism
This condition can disrupt an individual’s metabolism/metabolic rate and cause it to slow down. This can lead to excessive weight gain or obesity, joint pain, and in extreme circumstances, infertility.
The term ‘metabolic syndrome’ is a collection of conditions including:
• High blood pressure
• Obesity
• Elevated blood glucose (sugar)
• Elevated blood triglyceride (a type of fat) and adjusted blood cholesterol levels that may increase an individual’s risk of heart disease
• Stroke
• Diabetes.
While an individual’s health can impact their metabolism, it is essential to understand that an individual’s metabolism can also affect their health. This can be related to the influence of metabolic rates on a person’s weight; being overweight or underweight can negatively affect health.(34)
Responsiveness is a crucial life function as it gives an organism the ability to detect, respond or adapt to changes in the external and internal environments. For example, if an individual cuts their hand open on a sharp knife, the body’s response is to produce a reflex: an involuntary response will pull the hand away from the knife. This response requires no thinking, as the body naturally pulls the hand away. Many other systems within the human body act in the same way through involuntary movements.
Another response in the body is a process known as cellular adaptation, which refers to changes that are made by a cell in response to harmful environmental changes. Cellular adaptation can produce a normal (physiologic) or abnormal (pathologic) response.
There are four major types of cellular adaptation; these include:
1. Atrophy
2. Hypertrophy
3. Hyperplasia
4. Dysplasia.
ATROPHY
This term refers to the decrease in the size of an organ or tissue of a living organism, accompanied by a disorder or cessation of function.(1)(34) Physiological atrophy is a normal response to the growth changes of an organism. For example, atrophy of the thymus takes place during early puberty.
Pathological atrophy arises from insufficient nutrition, intoxication, and chronic infection. For example, the atrophy of skeletal muscle is a common pathologic adaptation to skeletal muscle disuse.
HYPERPLASIA
DYSPLASIA
This term refers to an increase in the size of a cell, tissue or organ. Physiologic hypertrophy can occur as a normal response to a stressor. For example, the size of skeletal muscle increases with resistance exercise.
Pathologic hypertrophy can arise as an abnormal response to a stressor. For example, an increase in the size of the heart due to aortic stenosis. Aortic stenosis is due to a change in the aortic valve, which obstructs the orifice, resulting in the left ventricle working harder to pump blood into the aorta.(34)
Unlike hypertrophy, where the size of a cell increases, hyperplasia is an increase in the number of cells. Examples of physiologic (normal) hyperplasia include the increase in the size of the breasts during pregnancy, an increase in the thickness of the endometrium during the menstrual cycle, and liver growth after partial resection.(34)
Abnormal or pathologic hyperplasia can also arise in response to a stimulus. Congenital adrenal hyperplasia is an example of this, which is an inherited disorder of the adrenal glands.
Dysplasia is an abnormal and potentially reversible process where there is disordered growth and maturation of cells and the tissues and organs they make up. In other words, dysplasia refers to a cell that looks abnormal under a microscope but is not cancerous.(56)
A common example of this is cervical dysplasia, which indicates that abnormal cells are found on the surface of the cervix.(34)
All living organisms (including humans) grow and develop in the patterns determined by their DNA. Growth occurs because cells grow larger or increase in number.
Development refers to the changes that the body undergoes throughout life. The development includes the process of differentiation, in which unspecialised cells become specialised in structure and function to perform certain tasks in the body.(34) Development also involves the processes of repair and growth, both of which involve cell differentiation. For example, some cells become skin cells while others become bone, muscle or other specialised cells.(34)
The term ‘biological maturation’ refers to a process that marks progression towards an organism’s adult (mature) state. In other words, maturation is a process, whereas maturity is a state. All body tissues, organs, and organ systems mature, but they do so at different times and rates.
Two commonly used systems for the assessment of maturation are the skeletal and reproductive systems(34):
• Skeletal maturity
• Sexual maturity.
SKELETAL MATURITY
SEXUAL MATURITY
The maturation of the skeleton can be identified by various stages of growth, size and shape across the lifespan.(57) When a child is born, they start with a skeleton of cartilage and progress toward the completely ossified, axial skeleton of an adult.(1)
Sexual maturation is a process that extends from the early embryonic differentiation of the sexual organs to the full maturity of these organs and fertility.(1) The transitional period between childhood and adulthood is referred to as puberty, during which the maturity of the reproductive organs takes place.
Reproduction in humans occurs in two distinct ways, both of which are vital to the survival of the human race:
1. The formation and birth of a new person, where life is transferred from one generation to the next through the organism’s reproduction.
2. Cells reproduce through mitosis so that the organism can grow or so the cells can replace themselves. The DNA information contained in each cell provides the instructions for this reproduction.(58)(34)
Excretion refers to the removal of waste. All organisms produce waste substances; if the human body is to operate correctly, it must be able to eliminate waste and non-essential items. The build-up of waste in the human body can be hazardous to the cell and the entire organism.
Various organ systems participate in the excretion of waste products; examples include:
• The respiratory system: produces carbon dioxide
• The urinary system: disposes of nitrogenous waste
• The digestive system: cleanses the body of indigestible food by producing faeces.
Sensitivity is an important function for living organisms that assists with survival in their environment. The human body relies on an abundance of information gained from its external environment. It gains this information through what is called its ‘special senses’ or ‘human senses’. The five human senses fall under this category, which has helped to ensure human survival over thousands of generations.
The five types of special senses include:
1. Smell (olfaction)
2. Taste (gustation)
3. Sight (vision)
4. Touch
5. Hearing.
Babies use their five senses from birth to communicate their needs and wants to their parents. Over the years, these senses are further developed and utilised throughout their entire lifespan. Should a certain sense become impaired (e.g. loss of sight or smell), the body compensates by increasing the sensitivity of the remaining senses.
SMELL (OLFACTION)
TASTE (GUSTATION)
The sense of smell is achieved through paired olfactory organs located in the nasal cavity. These organs use olfactory receptors, which are highly modified neurons. The olfactory system is very sensitive.
While the olfactory system can identify approximately 50 primary smells, it can distinguish 2,000-4,000 different chemical stimuli.
Taste (gustation) results from the taste receptors found predominantly on the tongue’s surface. Taste receptors are the combination of taste buds with specialised epithelial cells. Taste buds allow individuals to identify different properties and information about the food and liquid being ingested.
Humans experience five primary taste sensations. These include: 1. Sweet 2. Salty 3. Sour 4. Bitter 5. Umami.
VISION (SIGHT)
Vision is one of the most relied upon senses; however, surviving and leading a fulfilling life is still possible without vision. Visual receptors are contained in the eyes, allowing humans to detect light and create detailed visual images.
The accessory structures of the eye, such as the eyelids, provide protection, lubrication, and support, while the complex make-up of the eye itself is responsible for vision.
Touch is one of the most dominant sources of sensory information sent to the brain.
Many different types of nerves and receptors just below the skin surface respond to numerous stimuli, such as:
• Temperature
• Pain
• Pressure
• Vibration
• Acute sensations (that occur when a part of the body comes into contact with anything else).
This information is then sorted to travel down specific sensory pathways to the brain, where it is understood and categorised for future reference.
This sense is quite complex and involves a fair amount of detail; as such, it is discussed in depth within the integumentary system.
Hearing involves the detection and interpretation of sound waves. The outer part of the ear collects and directs sound waves to the middle ear; the middle ear then transmits these sound waves to an appropriate portion of the inner ear which contains the hair cells for hearing. More specifically, the receptors within the cochlea, a spiral-shaped bony chamber, provide the sense referred to as ‘hearing’.
Information regarding the intensity and region of stimulation received by the receptors in the cochlea is then relayed to the central nervous system. This information is relayed via the cranial nerve and is then distributed to various centres in the brain.
A state of equilibrium becomes prominent when opposing forces are in balance. Equilibrium is controlled by receptors located in the inner ear. These receptors are called hair cells, which are also involved with hearing. These receptors convey information to the cerebellum, cerebral cortex, and the motor nuclei in the brain stem about gravity, rotation, and linear acceleration.
An average adult has approximately 3,000 taste buds.
Throughout this unit, the term ‘homeostasis’ has been mentioned numerous times. The following information will define the term for better understanding and discuss how homeostasis is relevant to the practice of a nutrition coach.
(‘homeo’ meaning unchanging and ‘stasis’ meaning standing)
Homeostasis refers to the existence of a stable internal environment. The body must maintain homeostasis to survive in a changing external environment. Homeostatic regulation is the adjustment of physiological systems to preserve optimal balance. All body systems work together in harmony to ensure homeostasis.
A sound understanding of homeostatic regulation is imperative for a nutrition coach to make accurate predictions about the body’s responses in both normal and abnormal situations. This understanding also allows the nutrition coach to identify certain signs and symptoms that may indicate whether or not that client is within their scope of practice.
The body maintains very tight regulation via homeostasis to prevent harmful changes to the fluids and the environment within the body’s cells, tissues, or organs. Regardless of which physiological system is involved, the main role of homeostasis is to ensure that the characteristics of the body’s internal environment remain within certain limits.
Another way to explain homeostasis is by maintaining equilibrium. Equilibrium occurs when opposing processes are in balance; for example, in the case of body temperature, when the amount of heat lost is equal to the amount of heat produced by the body, it is in a state of equilibrium.
The body has two main ways (or mechanisms) through which it preserves equilibrium or homeostasis. These mechanisms include:
1. Intrinsic regulation
2. Extrinsic regulation.
INTRINSIC REGULATION
EXTRINSIC REGULATION
Intrinsic regulation is when a cell, tissue, organ, or organ system implements an automatic adjustment in response to an environmental change. For example, when oxygen levels become too low within a particular tissue, the blood vessels dilate to allow greater blood flow - thus, more oxygen to that tissue.
Extrinsic regulation occurs through the adjustments made by the nervous and endocrine systems, which receive information from many places, including the external environment. These two systems are then responsible for simultaneously adjusting the necessary systems. Generally speaking, the above two mechanisms have a three-part process:
1. The receptor the sensor that responds to a particular environmental change (otherwise known as a stimulus)
2. The control centre receives the information from the stimulus, processes it, and then sends specific commands out to rectify the environmental change
3. The effector the cell, tissue, or organ that responds to the control centre’s command by making some adjustments.
*This process is shown in the diagram on the following page.
Stimulus:
Maintaining equilibrium occurs on a gross and acute scale and involves every physiological process within the body. As such, several internal homeostatic controls allow identification of imbalance and when to commence specialised techniques to get it back into balance.
Some of these processes include:
• Thermoregulation
• Acid-base balance, fluid balance, electrolyte balance
• Blood pressure control/maintenance
• Protection from infection.
*These processes will be discussed in detail on the following pages.
Failure to regulate or maintain homeostasis can result in an inability of the human body to adapt to external or internal environments, and ultimately, this can lead to disease or even death in extreme cases (i.e. drastic change in body temperature). Homeostatic regulation can also be compromised as a person ages due to the body’s control mechanisms becoming less efficient. As a result, this can increase the risk of illness and disease in the ageing population.
An internal imbalance can be detected through any of the following signs or symptoms:
• Fever
• Chills
• Body temperature above or below 37 degrees
• Dehydration
• Dry mouth
• Headaches
• Lethargy
• Fatigue
• Poor blood clotting
• Cramps
• Malabsorption
• Nutritional deficiencies
• Hypertension
• Vertigo
An aspect of homeostasis, thermoregulation refers to the internal regulation of the body’s temperature.
VASODILATION
The dilation or swelling of blood vessels to increase blood flow. There are many reasons for vasodilation, such as increased oxygen requirements during exercise; however, in the context of body temperature, vasodilation of blood vessels in the skin allows more heat to be lost, decreasing body temperature.
VASOCONSTRICTION
The opposite of vasodilation, vasoconstriction in the blood vessels in the skin reduces blood flow enough to hold onto heat and protect body temperature from cooling too much. Vasoconstriction works in conjunction with shivering, which is an involuntary activation of muscles for the purpose of producing heat.
The body has the ability to maintain its internal temperature, and this is known as thermoregulation. Thermoregulation occurs due to a negative feedback system that responds to heat loss via the body’s surface and heat production resulting from movement or other active tissues. The hypothalamus, situated in the brain, is the primary control centre for thermoregulation and works to keep the body’s internal temperature at 37 degrees Celsius.
If body temperature rises above 37 degrees, the hypothalamus will activate muscle tissue in the walls of the blood vessels in the skin and sweat glands. As a result, vasodilation and sweating occur, thus providing a cooling mechanism for the body.
The integumentary system (heat loss), muscular system (heat production), cardiovascular system (heat distribution), and nervous system (coordination of all activities) all play a fundamental role in thermoregulation.
There are various reasons a client may suffer from imbalanced body temperatures, including medications causing vasodilation or vasoconstriction, overweight and obesity, physical activity, dehydration, and illness such as a cold.
A common nutrition example is an allergic reaction to a certain food. For example, a client who consumes food that they may be intolerant of or allergic to may experience fevers or chills, among other side effects such as lethargy, diarrhoea, and a rash. Another common example that nutrition coaches may come across is the simple act of exercising. Physical activity will heat the core body temperature from active tissue. The body will then attempt to cool itself down by sweating and vasodilation.
Acid-base (pH), fluid, and electrolyte balance can all affect one another; therefore, an imbalance in one of these is likely to cause an imbalance in the other two. For example:
• Acid-base imbalances can result in tissue damage
• Electrolyte imbalances can result in heart arrhythmias
• Fluid imbalances can result in severe dehydration or fluid overloads such as oedema or ascites.
Fluid balance and electrolyte balance directly affect each other. For example, as fluid volume decreases (e.g. sweat, urination), electrolyte concentration increases as a result. Similarly, when electrolytes are lost or gained (e.g. nutrition intake, sweat, respiratory losses, defecation), there is an associated water gain or loss due to osmosis.
Nutrition coaches must have a solid understanding of the homeostatic mechanisms within the human body to maintain pH, fluid and electrolyte balance. Understanding what the body requires to control pH, fluid and electrolyte balances will allow a nutrition coach to provide suitable dietary advice to maintain these balances. For example, encouraging electrolyte and fluid replacement through dietary measures during an endurance event, in which the client would have excessive losses, will help prevent acute imbalances in electrolytes and fluids.
Maintaining balance is not only important in exercise but also everyday life. For example, an individual who consistently drinks inadequate fluid (especially during the summer months) may become at risk of chronic dehydration, just as someone who consumes food high in particular electrolytes (e.g. bananas - potassium) may be at risk of complications if suffering from certain diseases such as kidney disease.
As a nutrition coach, it is important to have a sound understanding of homeostatic mechanisms and how to realistically assist with dietary measures (and refer on when outside the scope of practice).
To survive, a person must maintain a normal volume and composition of fluid within their body. The term ‘fluid’ encompasses all liquids inside the body, such as water, plasma, interstitial fluid, and other bodily fluids, such as urine. (1) Fluid balance, then, refers to the balance between the volume of fluid excreted by the body (urine, sweat, the GIT and excretion of water vapour from the lungs) and the volume of fluid gained (or ingested).(34)
An individual is considered to be in fluid balance when they expel (through micturition, sweat, and defecation) the same amount ingested (oral intake). For example, if a healthy individual consumed a total of 3L of fluid during the day through the intake of food and beverages, it is expected that they would excrete 3L of fluid in the form of urination, defecation and sweat.(59)
EXPEL
To force out, especially from the body.(1)
EXCRETION
A removal of body fluids.(1)
Everyone needs to consume eight glasses of water each day.
By the time you get thirsty, you are already dehydrated.
Just like nutrition, fluid requirements are very individualised. For example, a relatively sedentary individual will require less fluid than an athlete. Several factors need to be considered regarding fluid requirements, such as activity levels, gastrointestinal health, chronic diseases, and health goals.
The body’s automatic thirst signals set off before an individual becomes dehydrated. When an individual feels thirsty, it is their body letting them know they have decreased fluids in their body and need to increase them.
It is important to note that with age, the thirst signal may become delayed. It is, therefore, especially important for the elderly to listen to their signals and maintain adequate hydration, even if they are not feeling thirsty.
Bottled water is better than tap water.
Bottled water is definitely better when tap water is unsafe to drink (due to contamination). However, in Australia, safe drinking water is abundant from taps which has the same benefits as bottled water. When water is bottled in plastic water bottles, it is important to consider BPA levels. The best type of water is filtered water.
Given that fluid makes up approximately 60% of adult males and approximately 50% of adult females, it is no surprise that the inability to consume adequate water can be detrimental to a person’s immediate and long-term health.(1)(34) Women tend to have less fluid in their bodies in comparison to men simply because they usually have higher levels of adipose tissue.(34) Body water contains many electrolytes, such as sodium, magnesium, calcium, and potassium. Therefore, it is essential to ensure electrolyte and fluid replacement throughout the day, especially in individuals with higher levels of physical activity and increased sweating.
Adequate water consumption is essential for human survival. Water is not only involved in maintaining a healthy fluid balance but also has several other essential roles in the human body.
Some of these benefits include, but are not limited to:(60)(61)
• Improved mood and cognitive function
• Assists with weight management
• Assists in the removal of toxins from the body
• Helps to regulate bowel motions, especially for those who struggle with constipation
• Improved skin complexion
• Reduces and treats headaches
• Helps to maintain a comfortable body temperature
• Maximises physical performance
• Improves overall energy levels
• Bladder health
• Decreased frequency of Urinary Tract Infections (UTIs)
• Decreases postural hypotension
• The skin is less prone to tearing.
Inadequate fluid intake can result in:(62)(63)
• Constipation
• Dehydration
• Dizziness
• Fatigue
• Confusion
• Muscle cramping
• Headaches
• Decreased cognitive function
• Decreased physical performance
• Decreased energy levels
• Increased electrolyte concentration
• Decreased renal and cardiac function.
Brain (80-85%)
Lungs (75-80%)
Liver (70-75%)
Blood (50%) Skin (70-75%)
Inadequate fluid intake (if severe enough) can even result in death.(64) Therefore, maintaining daily fluid requirements is essential for ongoing health and quality of life.

Electrolytes are ‘soluble inorganic compounds whose ions will conduct an electrical current in solution’.(1) Examples of electrolytes include sodium, chloride, potassium, magnesium, calcium, and phosphorous. Electrolytes enter the body through the food and fluids consumed and leave the body via sweat, micturition, and defecation. The amount lost on a daily basis must be equivalent to the amount ingested. This occurs naturally for the general population as a byproduct of a healthy and well-balanced diet. Specific attention is needed for the athletic population, however.
Maintaining electrolyte balance is essential for two reasons:
1. The total amount of electrolytes will directly affect water balance
2. Cell function is affected by the concentrations of different electrolytes.
SODIUM
CHLORIDE
POTASSIUM
MAGNESIUM
CALCIUM
PHOSPHORUS
• Assists with the regulation of body fluid osmolarity, pH and body fluid volume.
• Works closely with sodium
• Component of gastric hydrochloric acid.
• Regulates pH and osmolarity
• Required for carbohydrate and protein metabolism.
• Activates many enzymes
• Influences almost all body processes.
• Constriction and relaxation of blood vessels
• Nerve impulse transmission
• Muscle contraction
• Structural strength of bones and teeth
• Blood clotting.
• Component of every cell and metabolite
• Assists with pH regulation.
FUN FACTS ABOUT ELECTROLYTES
Below are some interesting facts about electrolytes:(1)
• Approximately 98% of the potassium content in the human body is in the intracellular fluid
• Calcium is the most abundant mineral in the human body, with the average human maintaining 1-2kg of it
• Approximately 99% of calcium is stored in the skeleton
• Chloride ions are the most abundant anions in the extracellular fluid
• The average adult human contains approximately 29g of magnesium, of which approximately 60% is found in the skeleton.
Maintaining an appropriate electrolyte balance in the body is essential for optimal health and functioning of the body cells. When electrolytes become deranged, a number of complications can occur.
Some of these complications are explored in the table below:(1)
Hypernatremia (>145) Thirst, dryness, and wrinkling of the skin, reduced blood volume and pressure
SODIUM
(136-145 mmol/L)
POTASSIUM
(3.5-5.5 mmol/L)
Hyponatremia (<136). Disturbed central nervous system function, confusion, hallucinations, convulsions, coma, and death in severe cases
Hyperkalemia (>5.5). Severe cardiac arrhythmias, muscle spasms
Hypokalemia (<3.5). Muscular weakness, paralysis
CALCIUM
(4.5-5.5 mmol/L)
MAGNESIUM
(1.2-2.1 mmol/L)
PHOSPHATE
(1.8-2.9 mmol/L)
CHLORIDE
(97-107 mmol/L)
Hypercalcemia (>5.5) Confusion, muscle pain, cardiac arrhythmias, kidney stones, calcification of soft tissues
Hypocalcemia (<4.5) Muscle spasms, convulsions, intestinal cramps, weak heartbeats, cardiac arrhythmias, osteoporosis
Hypermagnesemia (>2.1)
Hypomagnesemia (<1.2)
Hyperphosphatemia (>2.9)
Hypophosphatemia (<1.8)
Hyperchloremia (>107)
Confusion, lethargy, respiratory depression, hypotension
Hypocalcemia, muscle weakness, cramps, cardiac arrhythmias, hypertension
Nil immediate symptoms. Chronic elevation leads to calcification of soft tissue
Anorexia, dizziness, muscle weakness, osteoporosis
Acidosis, hyperkalemia
Hypochloremia (<97) Alkalosis, anorexia, muscle cramps, apathy
Dehydration, loss of hypotonic fluid
Overhydration, infusion or ingestion of large volumes of hypotonic solution
Renal failure, use of diuretics, chronic acidosis
Low potassium diet, diuretics, chronic alkalosis
Cancer, vitamin D toxicity, calcium supplement overdose
Poor diet, lack of vitamin D, renal failure, hypomagnesemia
Overdose of magnesium supplements or certain medications (e.g. antacids)
Poor diet, alcoholism, severe diarrhoea, kidney disease, malabsorption syndrome, ketoacidosis
High dietary phosphate intake
Poor diet, kidney disease, malabsorption syndrome, vitamin D deficiency
Dietary excess, increased chloride retention
Vomiting, hypokalemia
A sound understanding of the human body’s electrolytes is essential for nutrition coaches. If a client is presenting with particular acute symptoms, such as diarrhoea, leg cramps, or muscular weakness, it is important that a nutrition coach can make the connection between the electrolyte imbalance and dietary requirements. This is particularly important for nutrition coaches working with sports nutrition, as these clients are at heightened risk of electrolyte imbalance in addition to more acute fluid losses and the need for adequate replenishment in a timely fashion.
An individual is considered to be in acid-base balance when the amount of hydrogen produced is directly offset by its loss. When body fluids are compromised in any way (e.g. overhydration or dehydration), it is likely to affect the body’s pH balance.
The acidity or alkalinity of any solution is measured on a pH scale (described below). To be in acid-base balance refers to an individual maintaining an internal pH ideal for optimal body functioning. The human body maintains a slightly alkaline pH, averaging 7.35-7.45. A person’s acid-base balance is measured through carbon dioxide (acidic) levels and bicarbonate (alkaline) levels in the blood.(34)
pH is the measure of acidity or alkalinity of a solution. The pH scale is measured from 0-14. The lower the number, the higher the level of acidity, and the higher the number, the higher the level of alkalinity. The neutral balance is 7, which is roughly the level the body aims to maintain, according to the needs of different body systems.
pH of 7 is NEUTRAL
pH less than 7 is ACIDIC
pH greater than 7 is ALKALINE
As the body needs to maintain set pH balances, depending on the location, the blood vessels will assist in ensuring an optimal pH range at all times. For example, the blood vessels absorb and neutralise acids produced by active tissues (muscles that have undergone intense exercise/activity), such as lactic acid (a byproduct of intense exercise when insufficient oxygen is available to convert pyruvate to usable energy).
A pH of 7 is classified as neutral, with anything higher classed as alkaline and anything below classed as acidic.
BLOOD ACIDITY
BLOOD ALKALINITY
Blood acidity increases when the level of acidic compounds increases (e.g. ingestion of acidic compounds, poor elimination) or when levels of alkaline compounds decrease (through decreased ingestion or increased elimination).(34)
Blood alkalinity increases when the level of acid in the body decreases or when the level of alkalinity increases, both of which may occur as a result of increased consumption of alkalising foods or increased elimination of acidic compounds.(34)
The pH levels are maintained primarily by the respiratory system (lungs) and the urinary system (kidneys). When either of these systems is compromised, an individual’s acid-base balance can become compromised. A pH level that is too acidic (acidosis) or too alkaline (alkalosis) can have numerous effects on the individual.
Complications of respiratory (lungs) acidosis include:
• Shock
• Respiratory failure
• Organ failure.
Respiratory acidosis occurs due to the lungs not removing excess carbon dioxide from the body. As carbon dioxide is acidic, this results in respiratory acidosis.
Respiratory acidosis may occur as a result of:(34)(65)
• Obesity
• Chest deformities
• Chronic respiratory disorders
• The overuse of sedatives.
Complications of metabolic (kidneys) acidosis include:(66)
• Rapid breathing
• Fatigue
• Confusion
• Shock.
Metabolic acidosis generally occurs as a result of one of three reasons:
1. Diabetic acidosis - Also known as diabetic ketoacidosis, is the build-up of ketone bodies as a result of poorly controlled blood sugar levels
2. Hyperchloremic acidosis - This results from the body losing excessive quantities of sodium bicarbonate (often following diarrhoea)
3. Lactic acidosis - This results from excess lactic acid build-up.
This can be caused by:(34)(67)
• Prolonged exercise
• Excessive alcohol intake
• Liver failure
• Low blood sugar levels
• Lack of oxygen
• Severe dehydration
Alkalosis is high blood alkalinity caused by an excessive increase of bicarbonate in the blood.
Alkalosis is high blood alkalinity caused by an excessive increase of bicarbonate in the blood. Complications of alkalosis include:
• Muscle twitching
Complications of alkalosis include:
• Hand tremor
• Muscle twitching
• Spasms
• Hand tremor
ACIDOSIS
ALKALOSIS
• Numbness and tingling
• Spasms
• Nausea
• Numbness and tingling
• Vomiting
• Nausea
• Vomiting
• Lightheadedness
• Confusion.
• Lightheadedness
Alkalosis may occur as a result of:(68)
• Fever
• Confusion. Alkalosis may occur as a result of:(68)
• Lack of oxygen
• Fever
• High altitudes
• Lack of oxygen
• Lung disease
• High altitudes
• Liver disease
• Lung disease
• Salicylate poisoning.
• Liver disease
• Salicylate poisoning.
The table below outlines normal pH levels for various bodily substances:(1)(28)(69)
The table below outlines normal pH levels for various bodily substances:(1)(28)(69)
PH AND THE STOMACH
The stomach is normally acidic, with a pH of around 2 (ranging from 1-3). This high level of acidity is necessary to a) break down the food and b) kill any pathogens that may be in the food.
When food reaches the stomach, it is combined with gastric juice to help break it down. The pH of hydrochloric acid is acidic, about 1–1.5, which helps to maintain the sterile environment of the stomach.
If the parietal cells do not secrete enough acid, stomach pH rises and becomes less acidic. The less acidic, the weaker the breakdown of food.
The body wants to keep chyme in the stomach until it reaches the right pH level. If acid production is too low, the stomach will be too alkaline, and food will sit in the stomach for longer than it should without being broken down. Low stomach acid will also allow pathogenic bacteria to grow, fed by fermenting waste. The result is bacterial overgrowth and symptoms such as bloating, heartburn and gas from undigested food. The body also cannot absorb the nutrients contained within the food.
A low stomach pH means the parietal cells are over-producing stomach acid, making the environment more acidic than it needs to be. The acid may irritate the sensitive tissues of the GIT, causing inflammation and damage.
As a nutrition coach, it is important to understand what constitutes a healthy functioning body. In addition to this, nutrition coaches need to be able to identify when an imbalance or malfunctioning system might present. While keeping this in mind, it is also vital that nutrition coaches educate their clients on how the health of the body is not just about one system at a time but how all the systems work together holistically.
Understanding the effect that one system has on another and how changes in one system could be consequential in another, is integral for the complete understanding of a healthy functioning body.
Educating clients on what constitutes healthy body systems will, in turn, improve the individual health of the client in the long run and enhance their ability to apply healthy attitudes and habits in their daily practices.
For a client to understand the importance of the body systems, or more so, what is malfunctioning inside their own body, they need to have an understanding of:
• Which systems are involved
• How will it affect them immediately, medium-term, and longer-term
• What will happen if they do nothing to correct it
• What signs and symptoms can they expect to experience without making changes
• What changes are required to make positive outcomes
• How long will the changes take to make
• How long will they need to sustain the changes
• Can they expect to feel or look any different if they make the changes.
By having knowledge of the body systems, nutrition, motivational techniques, and what constitutes overall health, nutrition coaches can play a pivotal role in motivating clients to make positive changes.
Encouraging and helping clients make nutritionally beneficial changes in their lives will bring a multitude of positive changes, including:
• Improved quality of life
• Improved self-esteem
• Improved confidence
• Improved mental and emotional states
• Potentially improved social state
• Positive example for family members
• Improved energy levels
• Better workplace conduct and commitment
• Heightened sense of self-worth
• Sense of accomplishment
• Improved functioning of body systems.
Having a sound understanding of the interrelationship of all the body systems will not only benefit the nutrition coach but will also improve the quality of each consultation provided to clients.


Health can mean different things to different people, and each client has their own health goals. The World Health Organisation defines health as: “a state of complete physical, mental and social wellbeing and not merely the absence of disease or infirmity.”(70)
Health can have many different meanings depending on the client or professional specialisation. For example, a medical professional such as a general practitioner (GP), may define health as the absence of a physical illness. For a psychologist, it may be the absence of any mental health condition, such as anxiety or depression. For a dietitian, it may be the absence of gut health problems and the inclusion of various vegetables in the diet. For a religious person, it may include spiritual health. For this reason, a client’s health status is subjective, and perhaps the most important person in deciding health status is the person being assessed.
The health status of an individual can be influenced by many variables, including the determinants of health:
• Income and socioeconomic status
• Education
• Physical environment (food environment)
• Social support networks
• Genetics and gender
• Government services (health system).
Due to the difficulties or complexities in defining health status, developing an objective measure of health is important, especially for screening clients as a nutrition coach. An objective measure is a set of measurable criteria that any professional or person can use to determine what is considered ‘healthy’ or ‘unhealthy’. This is based on a set of predetermined questions or physical assessments that have previously and reliably resulted in an accurate determination of the presence or lack of disease or condition (which could be physical or mental).
Nutrition coaches can confirm a client’s ‘health status’ through an industry-endorsed Risk Stratification Screening Tool (NCA, 2018). This will be introduced in subsequent pages within this resource.

As a nutritional advisor, it is important to understand that the qualification 11046NAT - Certificate IV in Nutrition does not allow its graduates to work with clients in a clinical setting (similar to the role of an Accredited Practising Dietitian [APD]) or with clients who are deemed ‘high risk’ by industry endorsed screening tools. This is why it is essential for all nutritional advisors to first check the health status of their clients to ensure that they can begin to support and implement nutritional protocols and interventions.
It is imperative to be aware of the risks involved when it comes to supporting clients and developing nutritional recommendations as a nutritional advisor. By identifying a client’s current ‘health status’, nutritional advisors can ensure that they are working within their scope of practice, which provides legal protection for them, and their clients should something occur during the course of treatment that results in a dispute.
Provided in the scenario below is a brief example of what may occur if a nutritional advisor doesn’t confirm the health status of a client before designing and implementing nutritional strategies or interventions.
If a nutrition coach were to screen a client and suspect an eating disorder, they should refer the client to a more suitable health professional for an official diagnosis and a higher level of care. However, had the client not been screened, the nutrition coach would be liable for the client’s declining health and any legal proceedings that may arise from their negligence.

The industry-standardised ‘Risk Stratification Screening Tool’ (RSST) has been developed and endorsed by Nutrition Council Australia (NCA). The RSST is a mandatory requirement for all nutrition coaches (those who have completed the 11046NAT - Certificate IV in Nutrition), as it provides nutrition coaches with a set of objective measures that will enable them to determine whether a potential client is suitable for their level of qualification.
The RSST can also make clients aware of their health issues or the limitations on care that a nutrition coach can provide. Without the RSST, nutrition coaches can not successfully screen their clients or begin to support them with their nutrition or health-related goals.
The RSST is a MANDATORY requirement for nutrition coaches. Nutrition coaches cannot support a client’s nutrition or health-related goals without first conducting the RSST (NCA, 2018).
As previously discussed, nutrition coaches must screen all clients who wish to engage in their services. This screening tool must be conducted by the nutrition coach and not the client alone.
It is during the process of completing the RSST that nutrition coaches can also get a feel for their clients by identifying the following:
• Current health status and potential needs of the clients
• Any variations from normal physical health status
• The clients’ motives for change
• The clients’ barriers to achieving their goals.
While completing an RSST may appear time-consuming, it is the ideal opportunity for a nutrition coach to build rapport with potential clients and promote the benefits of their services. It enables trust to be developed and clearly outlines the expected relationship between client and coach- one of respect, openness and responsibility.
Completing the screening tool will also be the most appropriate time to outline the nutrition coach’s expectations around their service provision and the potential need to refer to another health professional if the client is unsuitable for care.
The RSST is to only be conducted by the nutrition coach in the presence and with the consent of a potential client. It should not be completed by a client’s family or friend unless explicit permission and reason have been provided.
As a nutrition coach, to confirm the physical health status of a client, it is important to consider and acknowledge other factors that contribute to the health of a client, such as lifestyle or physiological conditions.
Having this underpinning knowledge can assist a nutrition coach in determining whether or not the client falls within their scope of practice or requires a referral to a more suitable health professional.
Additional underpinning knowledge required by nutrition coaches to identify a client’s health status includes:
• Using and interpreting anatomical terminology in the health industry
• The various ‘life processes’ required for the survival of an organism
• Homeostasis and the relationship between homeostatic imbalances and disease
• The levels of structural organisation of the human body, including cells, tissues and organs
• The function of various body systems, their relevance to health and common concerns/problems associated with each body system.
The above topics have been discussed in greater detail throughout the previous section of this resource. It is still important for nutrition coaches to continuously review and maintain this knowledge as they progress through their studies and eventually begin working as health professionals.
In addition to the above topics, knowledge of the following topics are also important for a nutrition coach to effectively conduct screening procedures and confirm a client’s health status. These topics are discussed in more detail on the following pages and include:
• Factors that may be the cause of the disease (such as genetics, environmental hazards, and the loss of normal control mechanisms)
• Understanding and maintaining blood pressure
• The various forms of ‘physical activity’ (active and passive)
• Body composition (types of body fat, body fat distribution and somatotypes).

Disease can often occur through an individual’s genetic predisposition, despite lifestyle or dietary considerations. A genetic disorder is caused by an altered or faulty gene or set of genes.(71) Many diseases often have a prominent genetic component, meaning that when a child inherits a gene from their parents that is altered toward a specific disease, their chances of developing that disease increases significantly.(72) These conditions are known as hereditary, as they are passed from one generation to the next.
There are four broad groups of genetic disorders. These include:(73)
• Single gene disorders
• Chromosome abnormalities
• Mitochondrial disorders
• Multifactorial disorders.
A single gene disorder can also be referred to as monogenic or Mendelian inheritance. This type of genetic disorder is caused by mutations (changes) occurring in the DNA sequence of a single gene. More than 6,000 known single-gene disorders occur in approximately 1 out of every 200 births.(74)(34)
SINGLE GENE DISORDERS
CHROMOSOME ABNORMALITIES
Some examples of single gene disorders include:(75)
• Hemochromatosis
• Cystic fibrosis
• Sickle cell anaemia
• Huntington’s disease.
A chromosome abnormality means there is a change in either the structure or the number of chromosomes.
This can occur in three main ways:(73)
• The altered chromosome is passed from the parent to the child
• The abnormality occurs when either the sperm or egg (germ cells) is created
• The abnormality occurs during fertilisation/conception.
There are many chromosome abnormalities, some of which include:(75)
• Down syndrome
• Turner syndrome
• Klinefelter syndrome.
Mitochondrial disease is an inherited chronic illness that can be present at birth or developed at later stages in life. It is estimated that 1 in 5,000 adults has this disease.(76) It’s a progressive disorder with no current cure.
Mitochondrial disease causes debilitating physical, developmental and cognitive disabilities, with symptoms including:(77)(34)
MITOCHONDRIAL DISEASE
• Poor growth
• Loss of muscle coordination
• Muscle weakness and pain
• Seizures
• Vision or hearing loss
• Gastrointestinal issues
• Learning disabilities
• Organ failure.
Multifactorial disorders sometimes referred to as polygenic inheritance, are disorders caused by a combination of the environment interacting with the action of multiple genes.
Examples of multifactorial inheritance include: (73)
• Congenital disabilities (are caused by the action of several genes and also depend on the amount of folate in the mother’s diet during pregnancy)
• High blood pressure (influenced by a large number of genes or influenced by a person’s diet and salt intake)
• Arthritis
• Obesity
• Cancer
• Diabetes
• Heart disease.
A nutrition coach needs to inquire about the health of a client’s family and extended family to obtain an accurate representation of the client’s current or potential health concerns. However, it is also important to remember that it is outside a nutrition coach’s scope of practice to diagnose or treat chronic health conditions.
Nutrition coaches are reminded to refer back to their scope of practice (SoP) developed by Nutrition Council Australia (NCA, 2018) as a continuous reference guide.

The environment, in this case, refers to all that is external to the human host. This usually includes physicochemical, biological, social and cultural factors, which individually (and in combination) influence human health and wellbeing. The environment is having a greater impact on a client’s health, more than it has ever done in the past.(78)
The environment plays a significant role in the health of humans in a variety of ways, either directly or indirectly. A direct effect would be the exposure to harmful chemicals or agents, and an indirect effect would be the substantial loss of ecosystems disrupting life-sustaining processes.
Although the exact ramifications of environmental factors on human health haven’t been firmly established, the World Health Organisation attributes 13 million deaths per year worldwide to preventable environmental factors, thus, illustrating the environment’s significant role in disease causation.(78)(79)
The list below outlines common diseases and conditions that may be strongly linked to environmental exposures:(80)
• Asthma
• Autism
• Cancer
• Autoimmune diseases (such as lupus)
• Obesity
• Reproductive health
• Lung disease.
Environmental health forms the basis of public health initiatives, which have improved people’s quality of life and longevity across the last 100 years. Such public health initiatives include:(81)
• Sanitation
• The quality of drinking water
• Food safety
• Disease control
• Housing conditions.







Loss of normal control mechanisms usually refers to the unpredictable and uncontrollable growth of cancer cells. Rather than responding to the mechanisms and processes set within the physiology of the human body, cancer cells are known to proliferate (increase rapidly in number) in a continuous and unregulated manner, bypassing the boundaries of their origin to invade tissues of other parts of the body.
In some instances, the cause of disease is unknown and is simply attributed to the uncontrolled growth of cells, causing danger to the health of the individual.(28)(34)
Although a nutrition coach does not need to concern themselves with diagnosing or treating cancerous cells, being aware of the causes of disease can better equip a nutrition coach when providing adequate nutritional support in the hopes of preventing certain cancers that are dietary related or referring their clients to an appropriate medical or health professional (i.e a doctor) when necessary.
Trauma, in this instance, refers to physical injury, bodily injuries or wounds. Physical injury refers to the impairment of an individual’s physical condition.
Some examples include:
• Bone fractures
• Cuts or scratches
• Hematomas
• Burns
• Bruises
• Damage to any organ or body system
• Injuries caused by medical treatment.
In terms of medicine and physiology, physical trauma is a serious injury to the body or a part of the body (internal or external). This can commonly occur due to accidents and falls; however, factors such as surgery can also cause wounds.
Minor wounds generally aren’t considered as serious implications to the body; however, to ensure the prevention of illness, infection or diseases, they must be kept clean.
The two major types of physical trauma include:
1. Blunt force trauma: when an object or force strikes the body, often causing concussions, deep cuts, or broken bones.(82)
2. Penetrating trauma: when an object pierces the skin or body, usually creating an open wound.(83)
Physical trauma, wounds or injury can often lead to more severe concerns, such as injury-related infections, chronic conditions or diseases. For example, a back injury caused by continuous heavy lifting or bending at work may lead to degenerative changes in a person’s spine, such as arthritis.
Another example of serious physical trauma or injury is when an individual has an open wound with significant bleeding. In this circumstance, the main concern would be the risk of infection of the surrounding tissue, such as lockjaw (caused by tetanus - a bacterial infection), necrotizing fasciitis (severe soft tissue infection caused by bacteria) or cellulitis (a bacterial infection that appears as rapid swelling, redness and pain to the skin).(84)(34)
Tissue damage caused by heat is known as a burn, which can be caused by incidents involving chemicals, electricity, sunlight and even radiation. Burns are commonly caused by factors in and around the home, such as flammable liquids and gases (aerosol cans and gas stoves), hot liquid or steam (i.e. boiling water, irons, etc.), campfires or backyard fires.
While the above information is common knowledge, many individuals don’t realise that severe burns can also cause serious problems throughout the body, leading to infection or disease. As the skin’s protective barrier is damaged, this then means that foreign invaders, pathogens and bacteria can enter the body.
Many individuals are unaware that it is the body’s excessive inflammatory response that responds to severe burns/infections.
“A ‘normal’ inflammatory response protects the body from invaders, such as bacteria, viruses, fungi, cancerous cells, toxins, and foreign materials. It activates in response to infection, injury, or other threats, but when faced with large or deep burns, it can overreact, often making the injury more severe and harmful to the heart, lungs, blood vessels, kidneys, and other organ systems”.(85)
Fluid is lost while this inflammatory response occurs, leading to a quick and deadly drop in the body’s blood pressure (commonly referred to as shock). Shock can potentially cause an organ or tissue to suffer from damage and eventually fail if it does not secure adequate oxygen levels. In this instance, organs such as the heart, lungs, kidneys and the brain, are also vulnerable to damage.
Severe burns also decrease proper functioning of the body’s immune system, which means that the body’s ability to fight off threats becomes compromised i.e. an infection can overtake not only the site of a burn, but also spread to organs such as the lungs and bloodstream.
Iatrogenic disease refers to a type of disease that is the direct result of another form of medical intervention or treatment (or advice that has been provided to a client).
There are many reasons as to why iatrogenic diseases can occur; some examples include:
• Complications after surgery or medical treatment
• Indirect interaction from medications or drug therapy.
Iatrogenic diseases aren’t always harmful to clients; however, in many cases, can lead to serious health concerns and risks. Iatrogenic diseases can also simply be an effect or symptom rather than a serious disease. For example, a keloid scar is sometimes a common result of medical procedure or surgery, and it is considered to be an iatrogenic disease, even though the scar doesn’t necessarily cause the individual any harm.

Blood pressure (BP) is a measure of the force exerted onto the walls of the arteries when blood is pumped out of the heart and is a vital part of how the heart and blood circulation works. BP measurements are usually taken on the upper arm with a sphygmomanometer.
The body’s blood pressure naturally goes up and down as it adjusts to the heart’s needs depending on what type of activity a person is doing. High blood pressure occurs when blood pressure is consistently higher than normal, as is the same with low blood pressure. Both of which can have numerous causes.
As a general guide:(86)
• A blood pressure reading under 120/80mmHg is considered optimal.
• A blood pressure reading between 120/80 and 129/84 is considered normal
• A blood pressure reading of 130/85mmHg and up to 139/89mmHg are in the normal to high-normal range (which is considered acceptable)
• A person is defined as having high blood pressure if they have a blood pressure reading that is greater than or equal to 140/90mmHg.
Blood pressure that is consistently high over a long period is considered to be one of the main risk factors for heart disease. As a person ages, the chances of having persistently high blood pressure increase.
SYSTOLIC
DIASTOLIC
Less than 120mmHg.
Less than 80mmHg.
Between 120 and 129mmHg.
Between 80 and 84mmHg.
Between 130 and 139mmHg.
Between 85 and 89mmHg.
Greater than or equal to 140mmHg.
Greater than or equal to 90mmHg.
Blood pressure is maintained by a combined effort of the endocrine system and the cardiovascular system, in which it is regulated by several different hormones, including:
• Epinephrine and Norepinephrine
These hormones stimulate the amount of blood the heart can pump (cardiac output) and vasoconstriction/dilation in the peripheries.
• Antidiuretic Hormone (ADH)
ADH is released in response to a decrease in blood volume or an increase in osmotic plasma concentration (electrolytewater balance in plasma). This can result in peripheral vasoconstriction, which increases total blood pressure.
• Angiotensin
Angiotensin is released in response to a fall in renal (kidneys) blood pressure. Angiotensin stimulates the release of aldosterone (hormone essential for sodium concentration), the release of ADH, increased thirst, and cardiac output, thus elevating systemic blood pressure (the pressure exerted on arteries during circulation).
• Erythropoietin (EPO)
EPO is released in response to a decrease in blood pressure or if serum oxygen levels (the amount of oxygen in the blood) fall too low. EPO stimulates the production of red blood cells to increase the volume and viscosity (thickness/ stickiness) of the blood and improve its oxygen-carrying capacity.
Blood pressure is commonly recorded as two numbers and is typically written with systolic pressure over diastolic pressure, for example, 123/94mm Hg.
Systolic pressure refers to the top number (or first number), which is also the higher of the two numbers. It measures the pressure in the arteries when the heart beats (when the heart muscle contracts).
Diastolic pressure refers to the bottom number (or second number), which is also the lower of the two numbers. It measures the amount of pressure in the arteries between heartbeats (when the heart muscle refills with blood and is resting between beats).
Hypertension (increased blood pressure) is an extremely common disorder in Western society. Therefore, it is important for nutrition coaches to understand what causes hypertension and which foods exacerbate or contribute to it. While it is expected that clients with any disease are referred on to an appropriate health professional, it is still important that nutrition coaches have sound background knowledge.
CLICK HERE For more information on blood pressure and understanding how to measure blood pressure.

Physical activity refers to any movement undertaken by the body that requires burning calories/energy. Regular everyday activities such as walking the dog, cleaning, gardening, walking upstairs and dancing are all considered physical activities.
Exercise is also a form of physical activity; however, the term exercise is typically used to describe an activity that requires physical effort, which is carried out to:
• Maintain or improve health
• Improve performance
• Develop a particular part of the body
• Enhance fitness levels (i.e. strength, endurance).
Another term commonly used to describe exercise is ‘active physical activity’.
Passive physical activity (also known as passive range of motion exercises) refers to the motion applied to a segment or region of the body by another individual, machine, or other external force. In other words, passive physical activity is movement that is applied to the body (or a body part) by another person (such as a physiotherapist) or through the use of a motion machine.
When a passive physical activity is exerted, the body (or segment) of the individual receiving the passive exercise is entirely relaxed, while at the same time, the external force applied pushes the body part throughout the available range of motion (ROM).
While there is no replacement for simply being active and moving the body, at times, there are situations where a vast array of clients do not have the capability to engage in this type of movement every day.
Barriers limiting the ability to move or exercise on a daily basis can include:
• Physical challenges
• Age restrictions/limitations
• Injury
• Illness.
In addition, daily routines and time constraints such as commuting, sleeping, working, or even raising a family can also hinder a person’s ability to participate in adequate exercise or any form of movement.

Active physical activity is where an individual’s physical effort is required to exert muscular activity. In other words, active exercise is where the body moves under conscious control and muscular activation of the individual. Active exercise can include active ROM (such as self-stretching) or general exercises that require movement of the body’s muscles without assistance.
There are two main types of active physical activity, aerobic and anaerobic, which are discussed later in this unit.
As a nutrition coach will encounter and work with a wide variety of clients from different backgrounds and all with different goals and experiences, it is important to understand the difference between active and passive exercise, as well as the benefits that exercise can have on their clients’ health.
Encouraging clients (who have the ability) to take part in regular active exercise (in any variety or form) can have the following benefits:
• Improved strength and endurance
• Improved body composition
• Improvement and maintenance of healthier muscles, joints, and bones
• Increased cardiovascular fitness
• Assistance in preventing many diseases
• Increased metabolism (when the percentage of lean muscle mass increases)
• Increased energy and overall wellbeing
• Increased ability to cope with high stress
• Improved quality of life and sleeping patterns
• Lowered blood pressure and cholesterol, and reduced risk of heart attack
• Improved ability to maintain a healthy weight
• Improved mood and potential assistance in the management of mental health conditions.
Low/insufficient levels of physical activity can put clients at greater risk of the following health factors:
• Cardiovascular disease
• Colon and breast cancers
• Type 2 diabetes
• Osteoporosis.

AEROBIC EXERCISE
ANAEROBIC EXERCISE
Aerobic exercise is commonly known as cardio exercise (aerobic means ‘with air’). This type of exercise requires oxygenated blood to be pumped by the heart around the body to deliver oxygen to working muscles.
Types of aerobic exercise can include (but are not limited to):
• Cycling
• Brisk walking
• Dancing
• Swimming
• Rowing
• Running.
As a nutrition coach, there are many benefits to encouraging clients to participate in aerobic exercise. Regular aerobic exercise conditions the heart and strengthens the cardiovascular system. It is also beneficial in releasing hormones that trigger a positive feeling in the bodyknown as endorphins.

Aerobic means ‘with oxygen’, and anaerobic means ‘without oxygen’. Anaerobic exercise is any type of activity that purely relies on energy sources stored in the muscles. This energy source is stored glucose in the form of glycogen.
In contrast with aerobic exercise, anaerobic exercise can only be sustained for short periods, so it is most often seen in short, explosive sessions of exertion before the body requires the intake of oxygen once again.
The most comment examples of anaerobic exercise include:
• Heavy weight-lifting (or resistance exercises)
• All types of sprints (running, biking etc.)
• Interval training (or any rapid burst of intense exercise).
Anaerobic exercise is often conducted in combination with aerobic exercise to some degree. Both anaerobic and aerobic exercise provide the numerous health benefits outlined on the previous page. As such, the nutrition coach must encourage their clients to partake in regular physical activity when able. However, it is likely nutrition coaches will work with clients who are already implementing physical activity, so having the ability to explain how diet can affect these two types of physical activity is imperative. For example, consuming adequate carbohydrates will provide stored glucose that can be utilised during active physical activity.
In today’s society, an increasing number of clients are becoming concerned with matters surrounding weight, obesity and body image. A nutrition coach will encounter many clients concerned about their weight who have set goals or even made New Year’s resolutions to lose weight, get in shape or become healthier.
It is important to be aware of clients who become obsessed with the number on the scales, as it is often a misguided way of thinking about general health. A scale measurement, while it can be useful and motivating for the client, only takes into account total body weight as a whole. It does not discern between fat mass, muscle mass, hydration levels or bone density. As such, whilst a client is making changes, if their weight increases, they may become disheartened. This is why, as a nutrition coach, it is important to understand what contributes to body composition and what the client’s weight is actually made up of to explain this to clients. For example, if clients understand that their fat mass has decreased and lean muscle mass has increased, they are more likely to maintain motivation levels.
Understanding the concept of body composition is often misconstrued, especially by the general public. Body composition is precisely what the name states – it is everything a body is composed of. In a broad overview or a general sense, it is easy to assume that all individuals are made up of the same bodily parts, meaning that every individual body contains muscles, bones, organs, tissues, and fat. However, proportionately, fat and muscle tissues fluctuate considerably from individual to individual. This is why the primary area of body composition that a nutrition coach is concerned with is the percentage of stored fat mass in the body versus lean muscle mass.
The image below indicates what body composition comprises, including bone density, fat tissue, muscle mass and internal organs. Body composition can also be influenced by hydration status.
Body composition - when outworked in practice - is an analysis of the percentage of stored fat mass in the body compared to lean muscle mass.
There are many methods to measure body composition, the majority of which are more accurate than simply using a person’s body mass index (BMI).
As a nutrition coach, it is important to understand the different types of fat in the body. Everyone needs a certain degree for the body to function effectively; this type of fat is known as essential fat.(59)
Essential body fat constitutes approximately 2-5% of the total fat in men and 10-13% in women(59) and is present in the nerve tissues, bone marrow, and organs. Loss of essential fat would result in compromised physiological function.
‘Stored fat’ is also a source of stored energy for the body, with levels up to 16% body weight in males and 22% in females being considered above average. Excessive accumulation of stored fat is thought to impair the body’s ability to function at optimal health and increases the risk of otherwise preventable diseases such as cardiovascular disease.(88)
Stored fat is found in adipose tissue, mostly beneath the skin and around major organs, and when in excess, it can be detrimental to an individual’s overall health and wellbeing.(59)(34)
Body fat has three basic functions:
1. Insulator to retain body heat
2. Stored energy for metabolism
3. Padding against physical trauma to the body.
In general terms, a healthy body usually has less stored fat and lean mass and can therefore indicate a person’s health status rather than weight alone. This is why it is essential that a nutrition coach gains a better understanding of why a client’s weight is not always an accurate measure of good health.
For example, when comparing two individuals who present the same weight on the scales, in most cases, it would be found that their body composition differs. The first individual may have a higher percentage of fat mass and less lean muscle mass, whereas the other individual may have less fat mass and more lean muscle mass. Therefore, the first individual may be at greater risk of health complications.
There are a number of different types of fat within the body, which can be categorised into the following types:
• Brown fat
• White fat
• Beige fat
• Subcutaneous fat
• Visceral fat.

Brown fat, also known as brown adipose tissue (BAT), is one of two types of fat that humans and other mammals have. Brown fat is composed of several small lipid (fat) droplets and a large number of iron-containing mitochondria (the cell’s energy-burning machine). The iron, as well as many tiny blood vessels, give this fat its brownish appearance. Brown fat is generally located in the front and back of the neck and upper back.
The role of brown fat is to burn calories to generate heat. This is why brown fat is often referred to as “healthy” fat since it helps to burn, not store, calories. Brown fat is acquired from muscle tissue and is found commonly in hibernating animals and newborns. As an infant grows, the quantity of brown fat significantly decreases. Adults who have additional brown fat are generally younger and slender and have normal blood sugar levels.
White fat, also known as white adipose tissue (WAT), is composed of a single lipid (fat) droplet and has fewer blood vessels and mitochondria, therefore resulting in its lighter white or yellow appearance. White fat generally amounts to 20% of body weight in men and 25% in women.
It is much more plentiful than brown fat and has many purposes, these include:
• Providing the largest energy reserve in the body
• Acting as a thermal insulator and cushion for internal organs, and providing cushioning during external
• Interactions with the environment
• Being a major endocrine organ, it produces one form of oestrogen as well as leptin, a hormone that helps regulate appetite and hunger
• Containing receptors for insulin, growth hormone, adrenaline, and cortisol (stress hormone).
White fat is typically the type of fat that many individuals try to avoid accumulating. Although it does help to regulate temperature by insulating organs, it does little to burn calories in comparison to brown fat. This type of fat is located subcutaneously (below the skin) and around the organs (visceral fat, which can be particularly dangerous) and increases from a surplus of calories in the diet.
Scientists have discovered that lean individuals tend to have more brown fat than overweight or obese clients and that when stimulated, it can burn calories. Scientists are researching it as a potential obesity treatment if they can design a way to stimulate existing brown fat or increase a person’s brown fat levels.
Whilst it has been common to only refer to fat cells as brown or white, there has been a recent discovery of beige fat cells. Beige fat (or beige adipocytes) has characteristics that sit somewhere in the middle of white fat and brown fat. Beige fat cells can accumulate energy in the same way that white fat cells can; however, they also have the ability to produce heat and increase energy expenditure.(89)(90)
Beige fat cells were recently discovered, and scientists are now researching their use as a potential obesity treatment. Beige cells have the ability to burn calories; therefore, stimulating these could induce weight loss.(89)
Beige fat, like brown fat, contains mitochondria and can burn energy. The protein required for mitochondria to generate heat and burn energy is lower in beige fat cells than in brown; however, beige cells can increase this protein in response to cold temperatures, which enables beige fat cells to burn calories almost as effectively as brown fat.(91)
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat stores energy in the form of a single large fat reservoir
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Brown fat is located in the neck and shoulder region and can stretch down the chest and spine.
• Brown fat is located in the neck and shoulder region and can stretch down the chest and spine.
• Brown fat is located in the neck and shoulder region and can stretch down the chest and spine.
• The generation of body heat requires a lot of energy, and this calls upon using the body’s excess fat stores for fuel
• The generation of body heat requires a lot of energy, and this calls upon using the body’s excess fat stores for fuel
• The generation of body heat requires a lot of energy, and this calls upon using the body’s excess fat stores for fuel
• Regulates temperature without shivering (also known as nonshivering thermogenesis).
• Regulates temperature without shivering (also known as non-shivering thermogenesis).
• Regulates temperature without shivering (also known as non-shivering thermogenesis).
• White fat stores energy in the form of a single large fat reservoir
• White fat affects an individual’s hormone production and hunger levels
• White fat stores energy in the form of a single large fat reservoir
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• White fat affects an individual’s hormone production and hunger levels
• White fat affects an individual’s hormone production and hunger levels
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• White fat is located below the skin (subcutaneous) and around the organs (visceral fat, which can be especially dangerous to health).
• White fat is located below the skin (subcutaneous) and around the organs (visceral fat, which can be especially dangerous to health).
• White fat is located below the skin (subcutaneous) and around the organs (visceral fat, which can be especially dangerous to health).
• Beige cells are comprised of a high number of mitochondria and medium-sized fat reservoirs
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Beige cells can generate heat and can burn energy
• Have both thermogenic and storage capabilities.
• Beige cells can generate heat and can burn energy
• Have both thermogenic and storage capabilities.
• Have both thermogenic and storage capabilities.
• Beige fat cells can be found deposited beneath the skin near the collarbone and along the spine (similar to brown fat) in adult humans.
• Beige fat cells can be found deposited beneath the skin near the collarbone and along the spine (similar to brown fat) in adult humans.
• Beige fat cells can be found deposited beneath the skin near the collarbone and along the spine (similar to brown fat) in adult humans.

• White fat helps to regulate body temperature by insulating organs but does little to burn calories like brown fat
• White fat helps to regulate body temperature by insulating organs but does little to burn calories like brown fat
• Source of stored energy for use during times of low energy intake.
• White fat helps to regulate body temperature by insulating organs but does little to burn calories like brown fat
• Source of stored energy for use during times of low energy intake.
• Source of stored energy for use during times of low energy intake.
• Beige fat cells can act like brown fat cells and assist heat generation in the body (thermogenesis) depending on the environmental conditions of the individual.
• Beige fat cells can act like brown fat cells and assist heat generation in the body (thermogenesis) depending on the environmental conditions of the individual.
• Beige fat cells can act like brown fat cells and assist heat generation in the body (thermogenesis) depending on the environmental conditions of the individual.
Subcutaneous fat is found directly under the skin. This fat is measured using skin-fold callipers to estimate total body fat.
Subcutaneous fat contains not only fatty tissue but also nerves and blood vessels, which supply the skin with oxygen. This type of fat is a shock absorber that aids to cushion skin against trauma and also stores energy, which the body uses during aerobic respiration.
Too much subcutaneous fat can cause the skin to become stretched or tight, and result in cellulite (a dimpled look of the skin). When this type of fat is present in relatively small amounts, it tends to lie loosely under the skin layers and is, therefore, less visible.
Hypodermis (subcutaneous fat)
Muscle Layer
Visceral fat is fat stored within the abdominal cavity around a number of important internal organs such as the liver, pancreas and intestines.
Visceral fat is associated with an increased risk of diabetes and heart disease and is a more accurate indicator of health risk than BMI. Researchers believe this type of fat may be a side effect of an unhealthy lifestyle, and many individuals with excessive amounts of subcutaneous belly fat also have a lot of visceral fat.
Body structure refers to the distribution or arrangement of body parts, such as the skeleton and muscle-fat distribution (shown in the diagram below).
COMPOSITION OF THE HUMAN BODY
COMPOSITION OF THE HUMAN BODY
FAT MUSCLE BODY MASS BONE ORGANS
COMPOSITION OF THE HUMAN BODY
FAT MUSCLE WATER BONE ORGANS
COMPOSITION OF THE HUMAN BODY
ESSENTIAL FAT STORAGE FAT WATER BONE ORGANS
An individual’s pattern of stored fat distribution is an important indicator of health and prognosis (refer to the diagram above for the roles of fat tissue) and two main terms to describe stored fat distribution include:
• Android fat distribution, and
• Gynoid fat distribution.
ANDROID FAT
DISTRIBUTION
Excessive android fat distribution (obesity) is characterised by excessive fat storage on the trunk (or torso), including the abdomen, chest, back, shoulders and neck often called abdominal obesity.
Excessive gynoid fat distribution (obesity) is characterised by excessive fat storage around the hips and thighs.
Abdominal fat is more closely linked to metabolic syndrome and cardiovascular disease than fat within subcutaneous compartments. Circumference (girth) measurements can provide a general indication of body composition and health risk.
Health risks are considered very high when the waist-to-hip ratio (WHR) is greater than 0.95 for young men and 0.86 for young women. Individuals 60–69 years of age have a higher cut-off point, with men considered at high risk with a WHR of greater than 1.03 and women 0.90.
*A worked example of the WHR is provided on page 191.
Over time it has been found that men and women will store fat in different areas of their bodies.
WOMEN: Generally around the buttocks and thighs (gluteofemoral) – ‘pear-shaped’.
MEN: Generally around the abdomen -“apple-shaped”.
These are the predominant patterns - but both ‘apple’ and ‘pear’ shaped distribution can be found in either gender. This fat distribution relates to the term ‘somatotypes’, which will be discussed in more detail later within this resource.
KNEE
UPPER ARM
ABDOMEN
INNER THIGH
OUTER THIGH
BUTTOCKS
LOWER BACK
CHEST
Fat can build up on the inside region of the knees in overweight women.
Fat build-up over the middle to the upper region of the upper arm (tricep area) is more common in women; however, it can also be seen in overweight males.
Fat build-up around the abdominal area is common in both men and women. It is also one of the areas for fat deposition in slim women, which is thought to be secondary to poor dietary choices.
Fat storage on the inner thighs is common in women but can also occur in men. It is more noticeable in females due to the pelvis’s width, which influences the thigh’s position (femur).
Sometimes called “Riding Breeches” - this area is the most likely place for the pitted or ‘quilted’ appearance of cellulite. This fat concentration also blends with fat tissue on the inner thigh and the buttocks. Cellulite is more commonly seen among women than in men.
Fat on the buttocks provides padding for sitting and is held in place by the gluteal fold. If significant fat is lost from the buttock, then only appropriate training can prevent the buttock from sagging down against the thigh.
This fat concentration often merges with the buttock area and is common in both overweight males and females.
Breast tissue consists of the mammary glands surrounded by fat. Men also have atrophied glands and fat in this area. Both sexes gain fat in this area.
The body loses fat through a series of complex physiological processes and metabolic pathways. Fat loss occurs when fats are required by the body to produce energy. When the body loses fat, fat cells do not disappear, but stay in the same location. It is the fat that is stored inside the fat cells (triaglycerol aka triglycerides) that is released. It is not burnt inside the cell, but released into the bloodstream as free fatty acids (FFAs) and delivered to the muscles and into the mitochondria where they are burned (used for energy). Fat is then predominantly exhaled as carbon dioxide (CO2), however some is also lost in sweat, faeces and urine.(93) The result is a smaller or shrunken fat cell which gives a leaner appearance.(94)
Scientists have stated in simple terms that “we don’t actually lose fat cells, we “empty out” fat cells”.(94)

Somatotypes are a set of generalised body types. In the 1940s, American Psychologist, William Sheldon, developed the concept of somatotypes, which was one of the greatest biological theories created in this time period. This theory attempted to explain and predict personality and delinquency based on a person’s physique.
The three somatotypes are:
1. Endomorph
2. Mesomorph
3. Ectomorph.
Sheldon created these somatotypes based on existing knowledge of how embryos develop in layers (the inner layer, or the endoderm; the middle layer or the mesoderm; and the outer layer, or the ectoderm).
From a visual perspective, ectomorphs are more slender and may appear fragile, mesomorphs tend to have more developed muscles and appear strong and powerful, and endomorphs are round and solid and often appear to be overweight.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
An ectomorph is tall and thin, with a narrow body, thin arms and legs, little body fat and smaller muscles.
Ectomorphs generally show signs of:
• A high forehead
• Receding chin
• Narrow shoulders and hips
• A narrow chest and abdomen
• Thin arms and legs
• Little muscle and fat.
• White fat stores energy in the form of a single large fat reservoir
• White fat affects an individual’s hormone production and hunger levels
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• The generation of body heat requires a lot of energy, and this calls upon using the body’s excess fat stores for fuel
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Have both thermogenic and storage capabilities.
A mesomorph is strongly built, with a broad muscular chest and shoulders, very muscular arms and legs, and little body fat.
Mesomorphs generally show signs of:
• A wedge-shaped body
• A cubical head
• Wide broad shoulders
• Muscled arms and legs
• Narrow hips
• Narrow from front to back rather than side-to-side
• A minimum amount of fat.
An endomorph is generally stocky, with a large round body, a short thick neck, short legs and arms, and with an aptness to store body fat.
Endomorphs are best suited to sports such as powerlifting, rugby and sumo wrestling.
Endomorphs generally show signs of:
• A pear-shaped body
• A rounded head
• Wide hips and shoulders
• Are generally wider from front to back, rather than side to side
• A lot of fat on the body, upper arms and thighs.
• White fat helps to regulate body temperature by insulating organs but does little to burn calories like brown fat
• Beige fat cells can act like brown fat cells and assist heat generation in the body (thermogenesis) depending on the environmental
Before a nutrition coach begins working with a client, it is important that there is a set process to follow to conduct business with the client in a professional manner. As a nutrition coach, following a step-by-step process can assist in determining whether or not to accept a particular client.
In addition to this, collecting the required information during a consultation is important for nutrition coaches to effectively support and provide accurate nutritional advice, and develop an individualised meal plan or recommendations.
Following a set process will also help to identify:
• Any clients that fall outside of a nutrition coach’s scope of practice, in which a referral to a more suitable medical or health professional is required (i.e. an Accredited Practising Dietitian)
• Any client that may be ‘at risk’, who will then require a medical clearance prior to working with a nutrition coach.

• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
An overview of the six-step process to confirm the health status of a client is outlined below. Please refer to the additional content throughout this resource for further information and in-depth details for each of the following steps: temperature in response to the changing external environment
HOW ARE THEY DIFFERENT?(91)(92)
• Have both thermogenic and storage capabilities.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat stores energy in the form of a single large fat reservoir
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
Identifying the health status of a client by screening for out-of-scope clients or clients who may be ‘at risk’ is a mandatory requirement for a nutritional advisor. This is achieved by first conducting an RSST with the client.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• White fat stores energy in the form of a single large fat reservoir
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
The Industry Endorsed Risk Stratification Screening Tool (RSST) required for nutritional advisors is developed and endorsed by Nutrition Council Australia (NCA).
HOW ARE THEY DIFFERENT?(91)(92)
• Have both thermogenic and storage capabilities.
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
This step focuses on referring out-of-scope clients, or gaining a medical clearance for clients who may be ‘at risk’.
HOW ARE THEY DIFFERENT?(91)(92)
• White fat stores energy in the form of a single large fat reservoir
BROWN FAT WHITE FAT BEIGE FAT
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
A client questionnaire is not a mandatory requirement for nutritional advisors; however, it is an essential tool for building rapport with the client, understanding their likes/dislikes, food preferences, goals and motives. Conducting the Client Questionnaire can also assist the nutritional advisor in determining which approach to take with a client to best support their goals.
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
• White fat stores energy in the form of a single large fat reservoir
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
This step focuses on reviewing the client’s current food intake (using a ‘food diary’) and exercise regime (using an ‘exercise review table’).
• White fat stores energy in the form of a single large fat reservoir
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Have both thermogenic and storage capabilities.
This step focuses on utilising appropriate anthropometric methods to determine the client’s body composition, such as body mass index (BMI), waist circumference, waist to height ratio (WHR) or skinfold measurements.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
This step focuses on calculating the client’s Ideal Body Weight (IBW) and Adjusted Ideal Body Weight (AIBW) to determine an appropriate weight for height of an individual and/or to determine a long-term weight goal.
As previously discussed, the Risk Stratification Screening Tool (RSST) was developed by Nutrition Council Australia (NCA, 2018). This unit has been designed to provide nutrition coaches with an overview of the tool and how it can be best conducted and evaluated to make informed judgments about client suitability, their health status and when to refer clients for medical clearance.
Prior to conducting an initial consultation and before completing a client questionnaire, it is mandatory to screen potential clients to determine whether or not they fall within the scope of practice of a nutrition coachThis is achieved by completing an industry endorsed Risk Stratification Screening Tool (NCA, 2018) with the potential client.
The Risk Stratification Screening Tool (commonly abbreviated to RSST) has been designed, implemented and endorsed by the Nutrition Council Australia (NCA) and is used by nutrition coaches (those who have graduated from a 11046NAT - Certificate IV in Nutrition) to identify whether or not a client falls within their scope of practice. The RSST is imperative in daily practice so that nutrition coaches can ethically and legally provide nutritional information to clients within their scope of practice.
Without the use of the industry-endorsed RSST, there is the potential for significant consequences in the event that a nutrition coach fails to accurately identify those who do not fall within their scope of practice.
NUTRITION COUNCIL AUSTRALIARISK STRATIFICATION SCREENING TOOL (RSST) CLICK HERE to download the RSST.

fromCouncilAustralia(NCA),foranyinjury,loss,harmordamagethatmayemergeorbecomeapparent screeninganypersonactingontheinstructionof(oranystatementorinformation)thisrisk-stratification tool.
IDENTIFYTHECLIENT’SCURRENTHEALTHSTATUS
Duetotheincreasedriskandchallengesthatmedicalconditionscanhaveonclientcare, iscriticalSectionthatclientswhofalloutsidethescopeofpracticeforaNutritionalAdvisor/NRNareidentified. oneoftheindustryendorsedRSSTfocusesonidentifyingtheclient’scurrenthealthstatusTheretheneedforreferral.
The 11046NAT - Certificate IV in Nutrition uses the RSST screening tool to identify clients who are ‘high risk’ and are outside the scope of practice for a nutrition coach. Before conducting a Client Questionnaire or developing nutritional protocols for a client, an RSST must be completed.
The RSST works through the following steps to ensure nutrition coaches are practising within their scope.
SECTION 1: IDENTIFY THE CLIENT’S CURRENT HEALTH STATUS
PART A) Identify current medical conditions.
PART B) Identify ‘at risk’ factors.
SECTION 2: IDENTIFY POSSIBLE FOOD INTOLERANCES/ALLERGIES
SECTION 3: IDENTIFY FAMILY HEALTH HISTORY

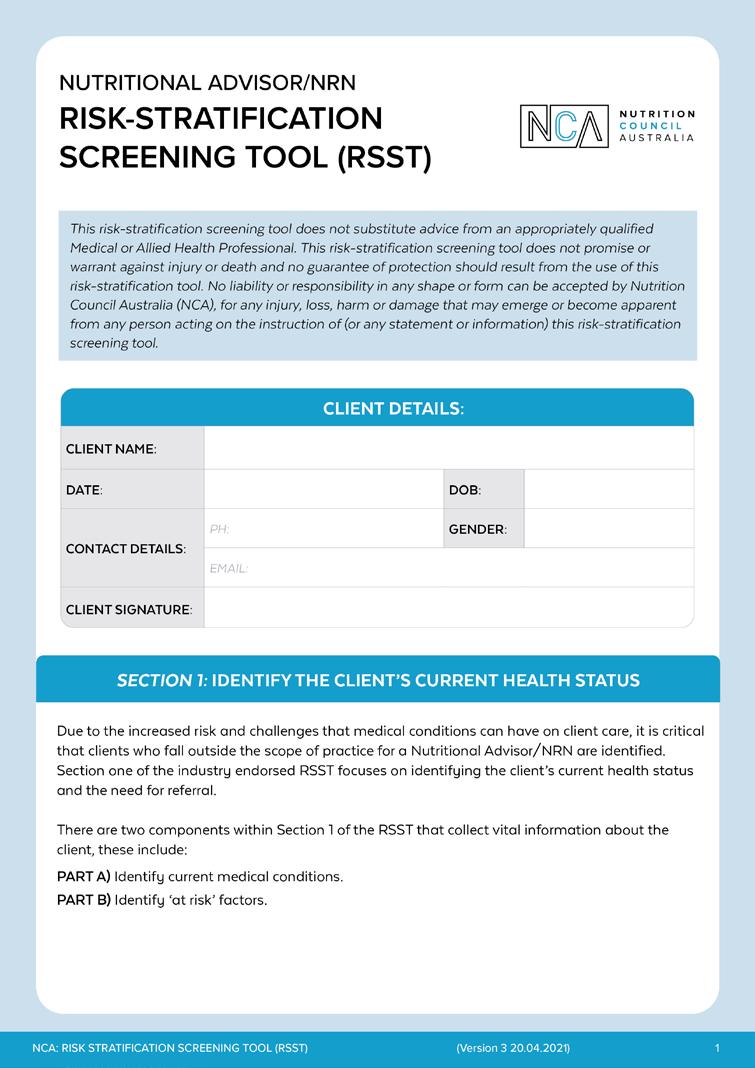





Due to the increased risk and challenges that medical conditions can have on client care, it is crucial to identify clients who are outside the scope of practice of a nutritional advisor. Section 1 of the industry endorsed RSST focuses on identifying the client’s current health status and the need for referral.
PART A) Identify current medical conditions.
PART B) Identify ‘at risk’ factors.
Medical conditions refer to any medical condition that the client has which may have an impact on the support a nutrition coach can offer to their client and the prescription of individualised nutritional plans. With their scope of practice in mind, nutrition coaches need to analyse the situation and the client’s information to identify any contraindications. This will dictate whether or not the client will need to be referred on to a more suitable medical or allied health professional.
Contraindication refers to a sign or indication that someone should not continue with a particular medicine or treatment because it might be harmful.(28) In other words, contraindications are particular conditions that a client presents with that may be aggravated if a nutrition coach were to provide nutritional support or individualised nutritional plans. If a client presents with an absolute contraindication, then a referral must be made to a more suitable medical or allied health professional.
Contraindication is the opposite of ‘indicated’ which is when something is either advisable or necessary. For example, a client with no medical conditions or contraindications (and is deemed ‘healthy’ during screening processes) may seek to employ a nutrition coach to create an individualised nutritional plan to help them maintain a healthy weight. This is considered to be an ‘indication’ of nutritional support as it is a valid reason for a nutrition coach to begin supporting the client and their nutritional goals.
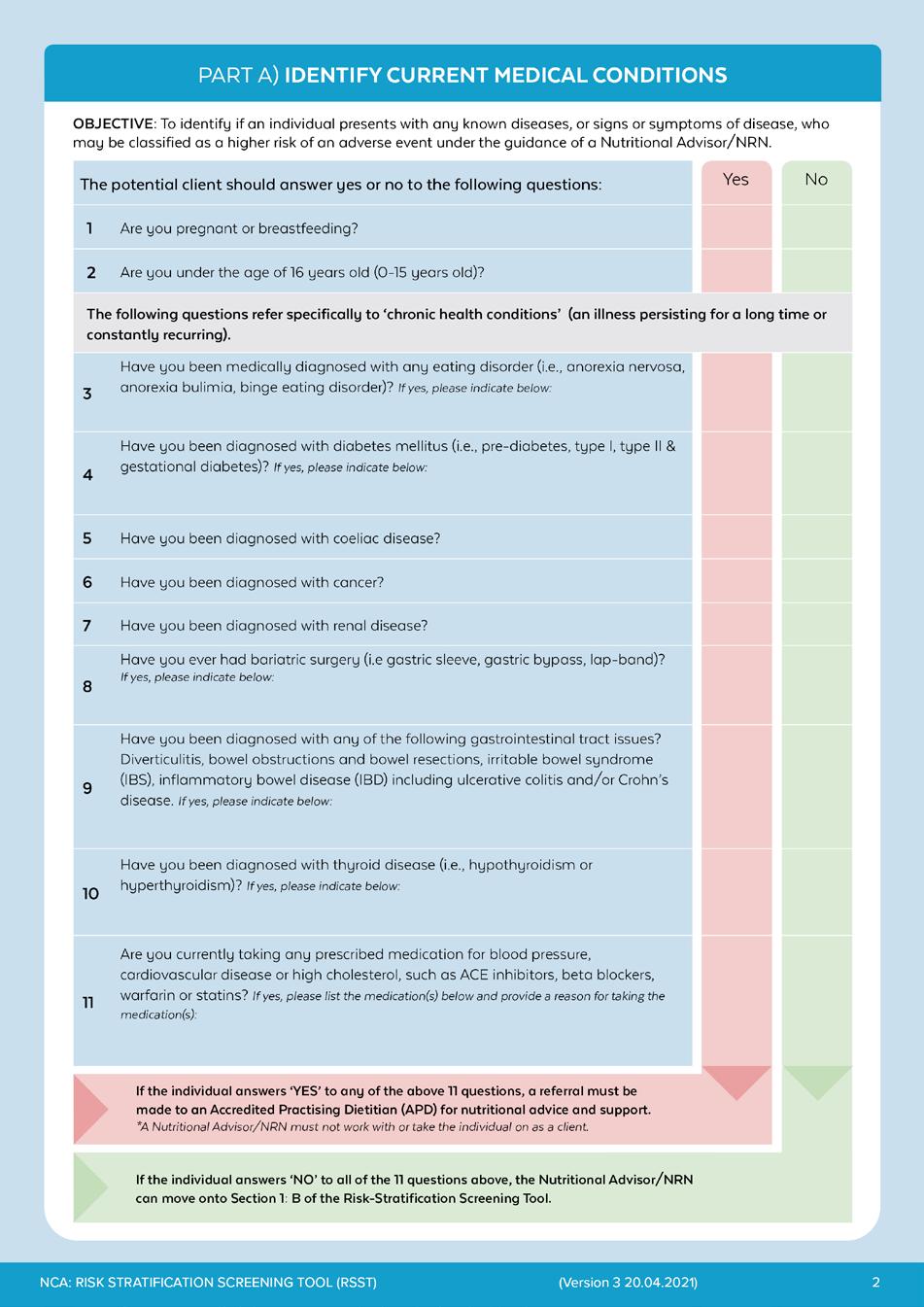

Nutrition coaches must be aware of common conditions, health factors and chronic diseases in which a referral to a more appropriate/qualified health professional is required. When in doubt, nutrition coaches should always refer back to their scope of practice to identify clients who may fall outside of their scope.
Any client presenting with the following conditions or contraindications is required to be directly referred to an Accredited Practising Dietitian (APD) for nutritional advice and support:
• Pregnant or breastfeeding
• Individuals under the age of 16 years old (0-15 years)
• Eating disorders (anorexia nervosa, bulimia nervosa, binge eating disorder)
• Diabetes mellitus (pre-diabetes, type 1, type 2 and gestational diabetes)
• Coeliac disease
• Cancer (current diagnosis or receiving cancer treatment)
• Renal disease
• Bariatric surgery (including gastric sleeve, gastric bypass, lap band)
• Chronic gastrointestinal tract issues, such as diverticulitis, bowel obstructions, bowel resections, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease
• Thyroid disease (hypothyroidism or hyperthyroidism)
• Prescribed medications for blood pressure, cardiovascular disease and high cholesterol, such as ACE inhibitors, beta blockers, warfarin or statins.
As you will learn throughout this resource, the 11046NAT - Certificate IV in Nutrition does not qualify a nutrition coach to take a detailed medical history or to interpret medical test results in the way that a general practitioner (GP) or dietitian would during a consultation. It is important, however, that a brief health history is discussed and captured to allow nutrition coaches the ability to identify potential chronic health conditions or factors which may be impacting current or future health.

PREGNANCY AND BREASTFEEDING
DIABETES
BUTTOCKS
During pregnancy additional energy is required to support the mother and the foetus. Therefore, the nutritional requirements for macro- and micronutrients are different for pregnant women compared to other female populations. It is important that the mother is not underweight in pregnancy as this can affect foetal growth and put the mother at risk of anaemia and preterm birth.
In addition, obesity during pregnancy is associated with adverse outcomes for the mother including gestational diabetes, thromboembolism, pre-eclampsia, miscarriage and still birth. Dietary management must ensure sufficient micronutrients, and protein. The diet should also avoid foods that may be dangerous for the foetus.Post-partum, the mother’s body requires extra nutrition for the production of breast milk.
Diabetes mellitus is a disease that affects the body’s ability to produce or respond to the hormone insulin, resulting in unusual or irregular metabolism of carbohydrates and elevated levels of glucose in the blood.
Long-term consequences of uncontrolled diabetes include nephropathy (kidney damage/disease), neuropathy (tingling, pain, numbness or weakness in hands and feet) and diabetic retinopathy (vision loss or blindness).
There are several forms of diabetes mellitus - type 1, in which the body does not produce insulin; type 2, in which the body is unable to respond to insulin; and gestational diabetes, in which the placenta affects the body’s regulation of blood sugar levels. Pre-diabetes is a condition in which blood glucose levels are higher than normal recommended ranges, but not high enough to be considered diabetes
Coeliac disease is a lifelong autoimmune disorder causing inflammation of the small intestines. This is an immune response to ingested gluten (found in wheat, rye, spelt and oats). The lining of the small intestine is damaged, and this gives rise to malabsorption of micro- and macronutrients, as well as a reduction in enzyme production.
Trace amounts of gluten can trigger symptoms, including diarrhea, flatulence, bloating, steatorrhea, weight loss, anaemias. Some adults with coeliac disease can be asymptomatic. The disease can be detected by a blood test followed by a biopsy.
Long exposure to gluten for someone with coeliac disease can increase the risk of cancer, type 1 diabetes, thyroid disease, infertility, osteoporosis and arthritis. Nutritional management must ensure strict exclusion of gluten in diets, including any trace amounts caused by cross-contamination.
Eating disorders are severe mental health disorders that cause abnormalities in eating behaviours. This can range from restrictive eating patterns, excessive eating patterns or food avoidance. Frequently, there are associated purging and compensatory behaviours around food and eating.
The eating disorder often develops from a fear of fatness and weight gain, together with body image distortion. Management of people with eating disorders is undertaken by a GP, psychologist and dietitian, all with specialised training in this field.
Bariatric surgery is a treatment option for morbid obesity. Generally, candidates for the surgery have a BMI greater than 40 or a BMI greater than 35 with serious medical comorbidities. There are many types of bariatric surgery, for example, a Roux-en-Y gastric bypass or a gastric sleeve.
Some of the expected long-term outcomes for the surgery are:
• An improvement or resolution of type 2 diabetes
• Metabolic syndrome
• Coronary artery disease
• Hypertension
• Sleep apnoea.
However, the surgical intervention has pre- and postoperative nutritional complications and also leads to lifelong deficiencies in protein, iron, vitamin B12, folate, calcium, fatsoluble vitamins A, D,E and K and other micronutrients. Dietary management must ensure sufficient micronutrients and protein.
Thyroid disease is a broad condition covering both hyperthyroidism and hypothyroidism. Hyperthyroidism is the excessive functioning of the thyroid gland and the release of thyroid hormones, whereas hypothyroidism is the under-functioning and release of thyroid hormones.
(Hypo- and hyperthyroidism)
Both conditions can greatly affect individuals:
• Metabolism
• Weight
• Menstrual cycle (women)
• Digestion and sexual function.
The above may require ongoing medical nutrition intervention and supplementation. Hashimoto’s and Graves’s disease are also two common yet severe thyroid conditions.
Cancer includes a wide range of malignant tumours and growths that can affect all body parts. Depending on the location of the cancer and whether cancer treatment is provided (chemotherapy, radiation, surgery etc.), this can cause:
• Severe muscle wasting (catabolism)
• Poor appetite
• Nausea or vomiting
• Nutrient malabsorption
All of the above require specialised nutritional support by a dietitian to ensure adequate nutrition. This is especially important as the mortality risk for cancer is higher if nutritional intervention is not adequate.
Renal disease includes any disorder of the kidney/s causing a decline in kidney function. Those with renal disease or abnormal renal function cannot adequately balance fluid and electrolytes, as well as waste removal.
Common side effects of renal disease include:
• Muscle wasting (catabolism)
• High cholesterol
• Mineral deficiencies
• Electrolyte imbalances.
This condition requires strict management of fluids, electrolytes and protein by a specialised dietitian and medical professionals.
(Diverticulitis, bowel obstructions/resections, IBS/IBD)
Diverticular disease occurs when small pockets in the lining of the large intestine develop. These pockets can become inflamed and infected, known as diverticulitis. There are specific dietary requirements in preventing and managing diverticulitis flare ups, which must be supervised by an APD.
Bowel obstruction is when the normal movement of the bowels is obstructed, causing food, fluids, acids and gas to build up behind the blockage site. This is a very serious condition that requires immediate medical attention and a highly modified diet. Bowel resection is the removal of a specific section of the bowel, usually as a result of cancer, diverticulitis or IBD. Recovery requires ongoing alteration to the diet, in order to promote healing.
Irritable bowel syndrome (IBS) is a functional gastrointestinal tract disorder, resulting in disturbed bowel habits (either diarrhoea, constipation or both). Treatment of IBS includes the low FODMAP diet (implemented by trained dietitians), stress management and medication.
Inflammatory bowel disease (IBD) is a chronic disorder of the gastrointestinal tract whereby the body produces an uncontrolled inflammatory response at the bowel lining, that can cause:
• Bleeding
• Diarrhoea
• Nutrient malabsorption
• Weight loss.
Crohn’s disease and ulcerative colitis are sub-types of IBD, both affecting different parts of the bowel and degree of ulceration/damage, often requiring surgery. IBD requires manipulation of energy and micronutrient requirements.
The objective of this section is to identify if a client presents with any risk factors in which a nutritional advisor would need to refer the client to a GP for a more detailed assessment and medical clearance prior to working with the client.
If the client answers ‘yes’ to any of the below four questions, a referral must be made to a GP for a more detailed assessment and a medical clearance must be attained. A nutritional advisor can work with the client only after the GP has given medical clearance
1. Is your BMI under 18.5 (<18.5)kg/m2 or over 40kg/m2 (>40)?
A BMI below 18.5kg/m2 is classed as underweight, whereas a BMI over 40 is classed as ‘Level 3 Obesity’ (very severe). Underweight and obese clients are often at risk of malnutrition and deranged pathologies such as high/low blood sugar levels, cholesterol and blood pressure.
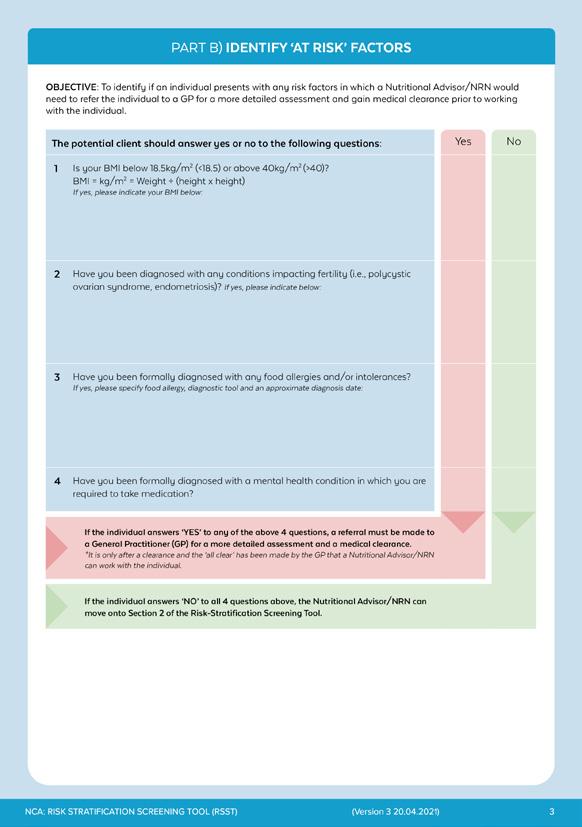

It is important to note that BMI is a calculation based on total body weight and total body height. BMI does not take the type of weight (muscle or fat) into consideration and, therefore, may place a client who displays a high level of muscle mass into the obese category. Therefore, the nutrition coach must consider the distribution of total body weight and not draw conclusions based only on weight.
2. Have you been diagnosed with any conditions impacting fertility? For example, polycystic ovarian syndrome or endometriosis.
Conditions relating to fertility can cause various changes in hormones, weight and glucose regulation, which can affect a client’s macronutrient and micronutrient requirements.
3. Have you been formally diagnosed with any food allergies and/or intolerances?
Food allergies are an immune-mediated response, and food intolerances are a sensitivity to certain foods that can impact a client’s nutritional intake. Diagnosing allergies and intolerances requires specialised intervention by a GP. Care must be taken to ensure that the offending food is not included in the client’s diet to avoid adverse symptoms such as pain, gastrointestinal upset and difficulties breathing.
4. Have you been formally diagnosed with a mental health condition in which you are required to take medication?
Many mental health conditions (including depression, ADD/ADHD, anxiety, bipolar and schizophrenia) require medication as part of their treatment and management. Many of these medications can affect metabolism, weight and nutritional needs, which will affect the effectiveness of a nutritional plan.
Knowing the type of medication/s the client is taking is important when determining an effective nutritional plan. Some medications may interact with specific nutrients, resulting in decreased effectiveness or adverse reactions. Common examples include ACE Inhibitors, Beta Blockers, Warfarin or Statins. These are medications for common medical/health conditions that can affect nutrient requirements and must be monitored by a GP or a dietitian.
ACE Inhibitors are used for treating high blood pressure. The nutritional implication is an increase in blood potassium levels. Beta Blockers reduce the force of heart contractions and reduce blood pressure. The nutritional implications are lower blood lipid levels which can cause nausea or a change in bowel function. Warfarin is a blood thinning medication for treating cardiovascular disorders. The nutritional implications are a change in vitamin K levels. Certain foods and supplements can interact with warfarin and reduce the ability of blood to clot. Statins lower blood lipid levels and the nutritional implications are micronutrient deficiencies, and the medication interacts with grapefruit juice.
Nutrition coaches are encouraged to identify any medications that the client is currently being prescribed by a GP. While it is not the role of the nutrition coach to understand in extensive detail all medications readily accessible on the market, they must be aware that some medications may interact with specific nutrients/foods, resulting in decreased effectiveness or adverse reactions from the client.
Nutrition coaches must identify if a client is currently taking any of the following prescribed medications for common chronic conditions:
• ACE Inhibitors
• Beta Blockers
• Warfarin
• Statins.
Nutrition coaches cannot work with clients who are currently taking any of the above medications and must refer the client to an Accredited Practising Dietitian for ongoing dietary intervention and support.

The objective of this section is to identify possible food intolerance or allergies that a client may have. This is an important factor in the screening process, as allergies/intolerances require a more detailed level of assessment by a qualified Accredited Practising Dietitian.

1 Do you experience bloating regularly?
Do you believe you suffer from excessive flatulence?
2
3
4
Note: there is no normal amount, but asking if a client experiences more flatulence than what they consider normal and if the smell is “offensive” provides an initial indication of concern.
Do you experience irregular bowel motions (e.g. diarrhoea, constipation, sore to pass, abnormal colours, faecal urgency)?
If yes, please provide details on the number of eliminations per day, stool colour, stool abnormalities and stool formation where possible.
Do you believe you suffer from low energy levels?
Discuss with the client the reason for low energy levels. Unexplained low energy levels may indicate poor nutritional absorption.
5 Do you suspect you may have any food allergies and/or intolerances?
If yes, please identify why you think you may have an allergy/intolerance and to what specific food.
If the client answers ‘yes’ to two or more of the above questions, it is ‘recommended’; however, not mandatory that a referral be made to a general practitioner for a more detailed assessment and a medical clearance.
*It is to the discretion of both the individual and the nutrition coach as to whether or not nutritional support and guidance will continue under the supervision of the nutrition coach or if the client will be referred to a GP. If the client is happy to continue with nutritional support under the guidance of the nutrition coach, then the nutrition coach can continue to work with the client.
The additional information provided in the table below discusses the above questions in more detail, which a nutrition coach can use to assist client understanding whilst completing the RSST:
Bloating refers to the abdominal area becoming swollen with fluid or gas and can be uncomfortable, painful or cause feelings of excessive fullness. This usually occurs after eating a trigger food which can increase gas production or due to digestive muscle disturbances.
As clients change their dietary habits, they may notice that they become less bloated, and therefore having a baseline knowledge of their current bloating can be useful when measuring progress.
Flatulence is considered a normal part of the body’s digestive process; however, the RSST is querying whether the client believes they have more flatulence than normal. Excessive flatulence may be a sign of digestive issues such as lactose intolerance or irritable bowel syndrome; however, it can also occur when a client increases their fibre intake. Clients may note that their flatulence odour is particularly offensive (more so than usual, especially after eating certain foods).
As clients change their dietary habits, they may notice that they become less flatulent or that their flatulence has a less offensive smell, and therefore having a baseline knowledge of their current flatulence can be useful for measuring progress.
Bowel motions can vary between diarrhoea and constipation. The type of bowel motion a client experiences can be directly related to hydration status, food reactions, fibre intake/type and physical activity.
Bowels motions can also be influenced by many other factors including, but not limited to:
• Hydration
• Fibre intake (and type of fibre)
• Protein intake
• Caffeine intake
• Stress
• Illness
• Medication usage
• Genetic factors.
The frequency of defecation is also important information to know, as well as any abnormalities within client bowel motions, such as blood or mucus in their stool, difficulty or pain when passing the motion or if there is any abnormal colouring.
The frequency of bowel motions differs between clients. For example, going to the toilet three times daily to once every three days is considered normal; however, one movement a day is average.
TThe Bristol Stool Chart (shown on the following page) can help the client identify and communicate what their bowel motions are like, or alternatively, the nutrition coach can simply ask if the client’s bowel motions are “constipated”, “normal/well-formed”, “soft”, “runny”, or “watery”.
For various reasons, many clients suffer from poor energy levels, which impact their quality of life. Most clients will find that they will experience an increase in energy levels through positive lifestyle changes.
Ongoing monitoring of energy levels can be a useful non-weight-related measure of health improvement, especially where primary goals (i.e. weight loss) may not be met at the pace desired by the client.
Diagnosing allergies and intolerances requires specialised intervention by a GP. Care must be taken to ensure that the offending food is not included in the client’s diet, to avoid adverse symptoms such as pain, gastrointestinal upset and difficulty breathing.
TYPE DESCRIPTION
Separate hard lumps/ pellets, often shaped like nuts (hard to pass/ abrasive).
TYPE 1
Overall shape is like a sausage/log, however, the appearance is chunky/lumpy texture (hard/painful to pass).
TYPE 2
3
4
In the shape of a sausage/log with cracks on its surface (often soft).
Overall shape like a sausage or snake, with a smooth and soft texture.
Similar to ‘type 1’, however, the shape/texture of this stool is soft blobs with clear-cut edges (easily passed).
Fluffy pieces with ragged edges (a mushy stool/too soft).
Watery, no solid pieces (the stool is entirely liquid).
EXPLANATION / POSSIBLE INDICATIONS
These lumps/pellets are typically painful to pass and can indicate that the stool has moved too slowly through the bowels and the client is constipated. It is best if this type of stool does not occur frequently.
This type of stool may be caused by a lack of fibre and/or bacteria, which means there is nothing to retain water in the stool. This could also be an indication of inadequate fluid intake.
As with type 1, this could also be an indication of inadequate fluid and/or fibre intake.
This type of stool can also be a possible sign of mild/slight constipation and a slow bowel transit time that ideally shouldn’t occur on a regular basis. It can often cause pain during elimination due to its size exceeding the maximum opening of the anal canal.
Client’s can often have feelings of incomplete bowel motions, abdominal pain and/or bloating. Constipation can lead to straining and the development of hemorrhoids, in which Nutritional Advisors should refer their clients if they present with regular or constant constipation (chronic constipation).
This is considered as a normal type of stool, especially if it’s somewhat soft and easy to pass. Often a sign of a healthy bowel motion.
This type of stool is easy to pass, also an ‘ideal’ or ‘normal’ stool, likely passed 1-3 times a day. Often a sign of a healthy bowel motion and/or adequate fibre intake.
The consistency of this stool is soft, which could suggest mild diarrhoea. This type of stool typically contains excess liquid and can potentially indicate a lack of fibre/vegetable intake.
The consistency of this stool is too soft, which could be a potential sign of mild diarrhoea. This can indicate inadequate fluid intake, inflammation or be a possible sign of a hyperactive colon due to stress or inadequate diet.
Client’s can often have feelings of faecal urgency or incontinence issues with their stool at this point on the scale.
This type of stool typically indicates that a client may have diarrhoea. This can mean that the stool has moved through the bowels too quickly and wasn’t given enough time to form into a healthy stool.
This may indicate too much water in the small intestine, causing stools to be spread throughout the length of the intestine. Diarrhoea can also be the result of anxiety, inflammation, a food allergy, medication, or a long-term condition, such as Irritable Bowel Syndrome (IBS).
Nutrition coaches should refer their clients if they present with regular or constant diarrhoea, as prolonged diarrhoea may lead to malnourishment and dehydration.
This section identifies chronic health conditions that may present among immediate family members. It enables the nutrition coachal advisor to give support and guidance around managing chronic disease risk. The nutrition coachal advisor can also use this section to emphasise the importance of regular health checks with a general practitioner.
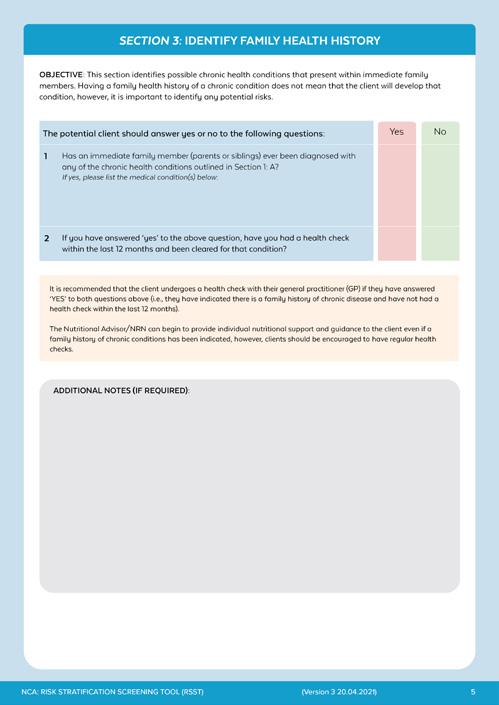
Has an immediate family member (parents or siblings) ever been diagnosed with any of the chronic health conditions outlined in Section 1: A?
1
2
The purpose of question one is to identify any family medical conditions. If the client ticks ‘yes’ to this question, the nutrition coach can take a record of the client’s family medical history. This health information is about a client’s immediate family members, parents and siblings. For example, their mother may have heart disease, or their sister may have gestational diabetes.
It is important to record this information because the client may be at a higher risk of developing chronic disease. For example, a client with a family history of heart disease is more likely to develop that condition compared to a client with no family history of heart disease.
If you have answered ‘yes’ to the above question, have you had a health check within the last 12 months and been cleared for that condition?
The purpose of question two is to find out if the client has had any recent health checks. Generally, it is recommended that any client undergoes a regular health check with a GP. This is of particular importance if the client has indicated there is a family history of chronic disease and they have not had a health check within the last 12 months.
The nutrition coachNRN can begin to provide individual nutritional support and guidance to the client even if a family history of chronic conditions has been indicated; however, clients should be encouraged to have regular health checks.
The depth of knowledge and training required to effectively and safely support the previously-mentioned ‘out of scope’ clientele is not sufficiently covered in the 11046NAT - Certificate IV in Nutrition. A referral to an appropriate medical or allied health professional (AHP) is required for clinical nutrition-related advice or for any clientele who falls outside of the scope of practice (who are deemed ‘at risk’) for a nutrition coach.
The appropriate health professionals to refer to are as follows:
• Accredited Practising Dietitian (APD)
• Accredited Sports Dietitian
• General practitioner (GP).
Collaboration and communication with the appropriate health professional/s is an imperative approach to protect out-of-scope clientele from unsuitable or potentially detrimental nutritional advice, and in turn, this can also prevent the possibility of legal liability. Furthermore, this collaborative approach can improve the industry by growing networks for client referrals and increasing expert credibility and integrity within the health and fitness industries.
More information can be found using the following links:
ACCREDITED PRACTISING DIETITIAN
CLICK HERE to view the link.
ACCREDITED SPORTS DIETITIAN
CLICK HERE to view the link
It is important to remember that the aim of a nutrition coach is to provide advice to healthy clients. As discussed in the RSST, there are instances where a nutrition coach is required to take action if a client potentially falls outside of their scope of practice.
Generally, there are two different requirements for a nutrition coach, which are identified in the table below:
REQUIREMENT 1
REFER DIRECTLY TO A MEDICAL OR ALLIED HEALTH PROFESSIONAL
REQUIREMENT 2
SEEK MEDICAL CLEARANCE FROM A GP
If any client is identified in Section 1: Part A of the RSST as ‘high risk’, then a nutrition coach must refer directly to a relevant medical or allied health professional.
*This would mean that the nutrition coach can not work with the client and must refer on.
If any client is identified in Section 1: Part B of the RSST as ‘at risk’, then a nutrition coach must refer the client to a GP for a more detailed assessment and written medical clearance.
If any client is identified as answering ‘yes’ to two or more questions in Section 2 or 3, it is recommended that the nutrition coach refers the client to a GP for a more detailed assessment and medical clearance.
*It is only after a clearance has been made by the GP that a nutrition coach can continue to work with a client.
The table below outlines the roles of health professionals who are important within the referral process for nutrition coaches:
HEALTH PROFESSIONAL
ACCREDITED
PRACTISING DIETITIAN (APD)
ACCREDITED SPORTS DIETITIAN (ACCSD)
GENERAL PRACTITIONER (GP)
PSYCHOLOGIST
PERSONAL TRAINER OR EXERCISE PROFESSIONAL
Accredited Practising Dietitians (APDs) are university-qualified professionals that undertake ongoing training and education programs to ensure that they are the most up-to-date and credible source of nutrition information. They translate scientific health and nutrition research into practical advice and practice in line with Dietitians Australia (DA) Professional Standards.(95)
An Accredited Sports Dietitian is an APD who has undergone further education and training in sports nutrition practice.(96)
A general practitioner (GP) is a doctor who is also qualified in general medical practice. GPs are often the first point of contact for clients of any age who feel sick or have a health concern. They treat a wide array of medical conditions and health issues.
A GP may also undergo further education in specific areas such as women’s or men’s health, sports medicine or paediatrics.(97)
The role of a psychologist is to assess, diagnose, and treat the psychological problems and the behavioural inhibitions resulting from or related to physical and mental health. A nutrition coach would refer the client on to a psychologist when the client is outside their scope of practice, and the identified issues are related to mental health.
Some common examples of these issues include:
• Depression
• Anxiety
• Eating disorders (e.g. anorexia nervosa, bulimia nervosa)
• Indication of self-harm
• Insomnia or severe fatigue
• Very low self-esteem
• Bipolar disorder
• Substance abuse
• Indications of verbal, physical or sexual abuse
• Addictions
• Post-traumatic stress disorder
• Strained relationships.
Personal trainers are equipped to provide individualised exercise recommendations to assist clients with weight loss, improved performance and muscle building.
While nutrition coaches can encourage clients to exercise, providing individualised exercise recommendations beyond the physical activity and exercise guidelines for all Australians is outside their scope of practice.
For more information on the physical activity and exercise guidelines for all Australians CLICK HERE.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
HOW ARE THEY DIFFERENT?(91)(92)
• White fat stores energy in the form of a single large fat reservoir
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
As discussed throughout this resource, the 11046NAT - Certificate IV in Nutrition qualification does not qualify a nutrition coach to analyse a detailed medical history or to interpret medical test results in the way that a general practitioner (GP) or Accredited Practising Dietitian would during a consultation. It is important, however, that a nutrition coach conducts their standardised screening tools (RSST) and non-clinical health history to allow them to identify potential chronic health conditions or aspects of these conditions which may be impacting their client’s current or forthcoming health status.
HOW ARE THEY DIFFERENT?(91)(92)
• Have both thermogenic and storage capabilities.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• White fat stores energy in the form of a single large fat reservoir
The following steps are guidelines on the most appropriate process for initiating and conducting a referral.
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
HOW ARE THEY DIFFERENT?(91)(92)
• White fat affects an individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
SECTION 1: IDENTIFY THE CLIENT’S CURRENT HEALTH STATUS
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
PART A) Identify current medical conditions
PART B) Identify ‘at risk’ factors
• White fat stores energy in the form of a single large fat reservoir
BROWN FAT WHITE FAT BEIGE FAT
• Have both thermogenic and storage capabilities.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
SECTION 2: IDENTIFY POSSIBLE FOOD INTOLERANCES AND/OR ALLERGIES.
HOW ARE THEY DIFFERENT?(91)(92)
SECTION 3: IDENTIFY FAMILY HEALTH HISTORY
• White fat affects an individual’s hormone production and hunger levels
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat stores energy in the form of a single large fat reservoir
• Beige cells can generate heat and can burn energy
BROWN FAT WHITE FAT BEIGE FAT
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
HOW ARE THEY DIFFERENT?(91)(92)
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
Ensure understanding of a nutrition coach’s scope of practice and evaluate the results from the ‘Risk Stratification Pre-Screening Tool’ to determine if a medical clearance or referral is required.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat stores energy in the form of a single large fat reservoir
BROWN FAT WHITE FAT BEIGE FAT
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
Identify which type of Medical or Allied Health Professional is best for the client’s needs.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat affects an individual’s hormone production and hunger levels
HOW ARE THEY DIFFERENT?(91)(92)
• Beige cells can generate heat and can burn energy
• White fat stores energy in the form of a single large fat reservoir
BROWN FAT WHITE FAT BEIGE FAT
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat affects an individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
Develop a referral form that includes appropriate, factual and succinct information about the client for the purpose of a referral.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat stores energy in the form of a single large fat reservoir
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
HOW ARE THEY DIFFERENT?(91)(92)
• Have both thermogenic and storage capabilities.
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
BROWN FAT WHITE FAT BEIGE FAT
• White fat affects an individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
Prior to completing and sending off the referral form, it is important to gain the client’s trust and informed consent to share their health information with the appropriate medical professional.
• Have both thermogenic and storage capabilities.
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• White fat stores energy in the form of a single large fat reservoir
Connect and communicate with the appropriate medical professional and develop a professional relationship. Send the referral off and wait for professional advice to be relayed back.
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
Receive advice from medical professional and action the professionals requests.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
*In some situations a medical clearance is solely needed, in which case continue to work with the client to assist their nutritional needs.
Using the feedback received from the medical professional, this will determine the nutritional approach to be conducted with the client. The nutrition coach should commit to providing a professional and ethical relationship with the client in order to cater to their individual needs/requirements
It is important to remember that the aim of a nutrition coach is to provide advice to healthy clients. As previously mentioned, if any client is identified in the screening process as ‘high risk’, then a nutrition coach is required to refer directly to a relevant medical or allied health professional. As such, it is important to become familiar with health professionals in the local area and know where to find experienced and recommended health care providers (i.e. doctor, psychologist or dietitian).
As a nutrition coach, it is important to take the time to meet and develop a relationship with these professionals so that when the need to refer a client arises, a referral can be made confidently.
When completing an initial referral, it is important to include all necessary information and who this is sourced from (nutrition coach), who the information is regarding (client), to who the referral is written (health professional) and why the referral has been written. Providing all adequate information in the initial referral will provide the referred health professional with a clear understanding of what is being requested of them and why they have been referred.
Some important information to include when completing a referral includes:
• Referrer’s name and occupation
• Referrer’s ABN and business name
• Referrer’s contact details (e.g. phone number, email address, fax number, address)
• Referrer’s business logo
• Name of health practitioner being referred to
• Contact details of health practitioner being referred to
• Name of client and their date of birth
• Reason for referral
• Client’s relevant health conditions
• Client consent for referral.
Provided below is an appropriate referral letter template that a nutrition coach can use when referring clients. A completed referral template has also been provided as an example.
CLICK HERE to view the link.
REFERRAL LETTER (TEMPLATE).
CLICK HERE to view the link.
There are instances where a nutrition may not need to refer a client on to work directly with an AHP and, instead, may only require a medical clearance from a qualified medical or health professional. Once a medical clearance request has been made by the nutrition coach and the relevant medical professional has returned the medical clearance with approval, a nutrition coach can then begin to work with the client.
In addition to this, some medical clearances that are returned may also provide a nutrition coach with recommendations and suggestions to assist the client, in which a nutrition coach must follow. Gaining a medical clearance is also beneficial for nutrition coaches as it is used to determine whether a proposed nutritional plan or activity could affect the client’s condition or, conversely, if the client’s condition could affect the proposed nutritional plan or activity.
Provided below is an appropriate medical clearance template that a nutrition coach can use in their day-today practice. A completed medical clearance template has also been provided as an example.
CLICK HERE to view the Medical Clearance Request Form (template).
CLICK HERE to view the Medical Clearance Request Form (template).
There are many ways in which a nutrition coach can send referral letters or medical clearance requests
Referrals can be sent via:
• Fax
• Posted letter
• In-person (provided by the client or the nutrition coach)
• Electronic transfer/E-Referral/email.
However, it is important that all referrals or medical clearance forms be signed by the referring practitioner or health professional.
A client questionnaire is completed by the client after they have been cleared as a ‘non-risk’ client through the Risk Stratification Screening Tool or after medical clearance has been granted by a medical or allied health professional. Clients who are ‘non-risk’ are within a nutrition coach’s scope of practice and should progress to completing the client questionnaire.
The client questionnaire is a series of questions provided by the nutrition coach to the client. It is a platform for gathering valuable information before or during their initial consultation.
6)
While it is best practice to utilise an industry-endorsed client questionnaire template, all health professionals, including nutrition coaches, can create their own set of questions and customise them to suit their target market/clientele. With this in mind, it is still important to cover a wide range of questions to build rapport and understand the client.
An effective client questionnaire (at a minimum) should cover the following details:
• Specific goals the client wishes to achieve, both short and long-term
• Identifying why the client wants to make changes and how they feel the changes will impact their current life
• What their motivating factors are, and why
• What they believe needs to change in their current lifestyle and why
• Barriers to change
• What has and hasn’t worked in the past for implementing lifestyle changes
• Confidence levels
• Food likes and dislikes
• Dietary restrictions
• Establishing exactly what the client is expecting from the consultation
• Identifying any additional supplements or vitamins the client is using.
The following information discusses how and when to provide the client questionnaire and illustrates examples and discussion of why certain information is gathered.
The client questionnaire can be completed before or during the initial consultation to provide the nutrition coach with lifestyle information, health goals and dietary history.
When a client books their appointment, the nutrition coach may like to send the client questionnaire via email or may request the client to arrive 15-30 minutes before the consultation to complete the client questionnaire. Alternatively, a nutrition coach may like to take the client into an office or a comfortable space to read the questionnaire together, as they may then ask questions and clarify answers.
Reviewing the client questionnaire before the initial consultation provides nutrition coaches with more opportunity to plan the consult, given the specified goals, history and objectives of the client. However, the method chosen is up to the discretion of each nutrition coach and depends solely on what they are most comfortable doing and what works best for them and the client.
The client questionnaire can be as detailed as the nutrition coach wishes. Any information not gathered via the questionnaire will need to be gathered in the initial consultation; therefore, time restraints need to be taken into account. The client questionnaire allows the client an opportunity to think about their answers before writing them down. For example, they can have the time to check exactly what supplements they are taking, reflect on why past lifestyle changes have or haven’t worked, or identify their overall goals.
The questions outlined on the following pages are included in the client questionnaire template and form a starting point for nutrition coaches to gain a more thorough understanding of the clients:
• General dietary habits
• Health-related goals and motives
• Lifestyle factors/social support networks.
CLIENT DETAILS:
The questions outlined in the client questionnaire are a guide for nutrition coaches; however, these questions can be adapted to better suit a nutrition coach’s individual consulting style or the goals of different clients.
CLIENT NAME:: DOB: MALE/FEMALE:
DATE:
CLIENT DETAILS:
WEIGHT (KG):
CLIENT DETAILS:
HEIGHT (CM):
The questions outlined on the following pages are included in the client questionnaire template and form a starting point for nutrition coaches to gain a more thorough understanding of the clients:
CLIENT NAME::
CONTACT DETAILS: PH:
DOB:
EMAIL:
MALE/FEMALE:
CLIENT NAME:: DOB: MALE/FEMALE:
OCCUPATION:
DATE: WEIGHT (KG): HEIGHT (CM):
DATE:
This section of the client questionnaire (questions 1 to 12) focuses on the general dietary habits of the client. These questions are not designed to identify any risks, as these have previously been identified in the RSST before completing this questionnaire. Instead, these questions are designed to understand the client’s daily eating habits so that a nutrition coach can implement or suggest appropriate dietary interventions.
WEIGHT (KG): HEIGHT (CM):
CONTACT DETAILS: PH: EMAIL:
GENERAL DIETARY HABITS:
CONTACT DETAILS: PH: EMAIL:
OCCUPATION:
1) How many glasses of water do you drink per day?
OCCUPATION:
Gathering information about a client’s hydration status allows a nutrition coach to identify how much water the client is drinking and then make recommendations to either increase/decrease their fluid intake.
GENERAL DIETARY
Obtaining this information is important as this can have an effect on the client’s:
1) How many glasses of water do you drink per day?
2) Do you drink alcohol? (yes/no) (If yes, how many standard drinks would you consume in an average week?)
• Bowel movements
• Energy levels
1) How many glasses of water do you drink per day?
• Overall health.
2) Do you drink alcohol? (yes/no)
3) Do you ever skip breakfast, lunch or dinner? (If so, please provide details below)
(If yes, how many standard drinks would you consume in an average week?)
2) Do you drink alcohol? (yes/no)
(If yes, how many standard drinks would you consume in an average week?)
It is important to identify whether a client consumes alcohol, as alcohol contains energy that contributes toward their estimated energy intake (EEI). Alcohol intake, especially in excessive amounts, is also linked to many long-term health issues, and advice to limit or stop intake is recommended within health literature.
3) Do you ever skip breakfast, lunch or dinner?
4) Do you drink tea or coffee regularly? (yes/no)
(If yes, how many standard cups of tea or coffee would you have per day?)
(If so, please provide details below)
3) Do you ever skip breakfast, lunch or dinner?
(If so, please provide details below)
Obtaining this information will enable nutrition coaches to build an understanding of a client’s schedule and eating patterns and will highlight areas for improvement in their current nutritional intake.
4) Do you drink tea or coffee regularly? (yes/no)
5) Do you feel as though you have a ‘bad’ relationship with food?
(If yes, please provide more details below)
(If yes, how many standard cups of tea or coffee would you have per day?)
4) Do you drink tea or coffee regularly? (yes/no)
(If yes, how many standard cups of tea or coffee would you have per day?)
Understanding the reasons why the client may skip meals is beneficial for making recommendations and can also aid in clarifying any food myths/misconceptions the client may have (i.e. skipping dinner because eating before bed increases body fat).
6) Do you smoke or have you previously smoked in the past? (yes/no)
5) Do you feel as though you have a ‘bad’ relationship with food? (If yes, please provide more details below)
(If yes, provide details for how often you smoke per day. If you no longer smoke, please provide details on when you stopped)
5) Do you feel as though you have a ‘bad’ relationship with food?
(If yes, please provide more details below)
6) Do you smoke or have you previously smoked in the past? (yes/no)
(If yes, provide details for how often you smoke per day. If you no longer smoke, please provide details on when you stopped)
3) Do you ever skip breakfast, lunch or dinner?
(If so, please provide details below)
3) Do you ever skip breakfast, lunch or dinner?
4) Do you drink tea or coffee regularly? (yes/no)
4
(If so, please provide details below)
(If yes, how many standard cups of tea or coffee would you have per day?)
Identifying how many caffeinated beverages a client consumes can be beneficial as it can help a nutrition coach calculate total fluid intake and identify if the client may be dependent on caffeinated beverages.
4) Do you drink tea or coffee regularly? (yes/no)
(If yes, how many standard cups of tea or coffee would you have per day?)
4) Do you drink tea or coffee regularly? (yes/no)
(If yes, how many standard cups of tea or coffee would you have per day?)
5) Do you feel as though you have a ‘bad’ relationship with food? (If yes, please provide more details below)
This information is also important as these types of beverages count toward the client’s EEI, and excessive intake can be an area for nutritional recommendations.
5) Do you feel as though you have a ‘bad’ relationship with food?
(If yes, please provide more details below)
5) Do you feel as though you have a ‘bad’ relationship with food? (If yes, please provide more details below)
6) Do you smoke or have you previously smoked in the past? (yes/no) (If yes, provide details for how often you smoke per day. If you no longer smoke, please provide details on when you stopped)
Obtaining this information can be beneficial for a nutrition coach as it can assist in identifying negative issues associated with eating/body image (such as binge eating, emotional eating, or regularly skipping meals), which may require referral to an appropriate health professional.
6) Do you smoke or have you previously smoked in the past? (yes/no)
(If yes, provide details for how often you smoke per day. If you no longer smoke, please provide details on when you stopped)
6) Do you smoke or have you previously smoked in the past? (yes/no)
(If yes, provide details for how often you smoke per day. If you no longer smoke, please provide details on when you stopped)
Smoking is linked to many illnesses of the gastrointestinal tract and also impacts appetite and dietary intake. Nutrition coaches, like all health professionals, should encourage clients to reduce and eventually quit smoking for their long-term health.
1 CLIENT QUESTIONNAIRE (EXAMPLE) - VAST FITNESS (V:1. 2018)
Obtaining this information can also help identify the reason why the client might be smoking (i.e. a client might commence smoking as it distracts them and prevents them from overeating).
1 CLIENT QUESTIONNAIRE (EXAMPLE) - VAST FITNESS (V:1. 2018)
1 CLIENT QUESTIONNAIRE (EXAMPLE) - VAST FITNESS (V:1. 2018)
77) Please list any foods below that you particularly like or dislike.
7) Please list any foods below that you particularly like or dislike.
Gathering this information will enable nutrition coaches to produce personalised dietary recommendations that respect the diverse needs of their clients. It may also highlight areas where nutritional adequacy is not currently being met, e.g. avoiding dairy and impacting calcium intake.
8) Beside allergies or intolerances, do you have any other dietary restrictions?
8) Beside allergies or intolerances, do you have any other dietary restrictions?
Knowing exactly what a client can and can’t eat is invaluable information for a nutrition coach to obtain before developing a nutrition plan and personalised recommendations.
9) Do you regularly suffer from any cravings?
Please discuss in detail including craving frequency, food type and if you are aware of any triggers.
9) Do you regularly suffer from any cravings?
Please discuss in detail including craving frequency, food type and if you are aware of any triggers.
If there are particular foods that the client dislikes or doesn’t eat due to taste preferences, cultural or religious practices or personal beliefs, nutrition coaches may want to discuss these foods and offer alternative options to achieve adequate nutrition.
For example, if a client avoids green vegetables simply because they grew up with them being overcooked and mushy, a nutrition coach may be able to discuss various ways to cook and eat the vegetables to make them more enjoyable/ palatable.
10) Are you currently using any supplements and/or vitamins? Please list these below and provide dosage details. (This question is not referring to medications)
10) Are you currently using any supplements and/or vitamins? Please list these below and provide dosage details. (This question is not referring to medications)
Another client may follow the Muslim religion and therefore may not eat pork, or they may live with someone who has coeliac disease and therefore choose to minimise gluten themselves, even though they are not allergic, intolerant or dislike it.
11) How often do you have a bowel movement?
Please tick the most appropriate box below:
11) How often do you have a bowel movement?
Please tick the most appropriate box below: More
Gathering all this information is important as it will directly influence the development of the client’s nutritional plan and may also highlight the need to refer a client to an appropriate health professional for further investigation and treatment.
Once every 2-3 days A few times per week Once per week
Once every 2-3 days
A few times per week
Once per week
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no)
If you answered yes for the above question, please describe below:
The methods/types of diet have you tried in the past to change your dietary habits.
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no)
Why you stopped/discontinued the approach(s)?
If you answered yes for the above question, please describe below:
The methods/types of diet have you tried in the past to change your dietary habits. – Why you stopped/discontinued the approach(s)?
9) Do you regularly suffer from any cravings?
Please discuss in detail including craving frequency, food type and if you are aware of any triggers.
7) Please list any foods below that you particularly like or dislike.
A discussion with the client on their craving levels remains a subjective assessment; however, nutrition coaches can ask their clients to recall the frequency of their cravings (e.g. 2-3 times per week or 2-3 times per day), with their response forming a benchmark for ongoing review and assessment.
10) Are you currently using any supplements and/or vitamins? Please list these below and provide dosage details. (This question is not referring to medications)
8) Beside allergies or intolerances, do you have any other dietary restrictions?
Once a nutrition coach knows the foods their client is prone to craving, they can work with the client to offer alternative food sources or strategies to satisfy the craving. For example, if a client craves a whole bag of salted chips multiple times a week, a nutrition coach may suggest alternative crunchy and salty options, such as crispy roasted broccoli with salt and vinegar or home-made oven roasted and salted sweet potato chips.
11) How often do you have a bowel movement?
Please tick the most appropriate box below:
Nutrition coaches may also investigate the client’s triggers for cravings and develop strategies to take their mind off the craving, such as:
• Breathing techniques
9) Do you regularly suffer from any cravings?
• Craving control techniques
Please discuss in detail including craving frequency, food type and if you are aware of any triggers.
• Going for a walk
• Calling a friend.
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no) If you answered yes for the above question, please describe below:
10) Are you currently using any supplements and/or vitamins? Please list these below and provide dosage details. (This question is not referring to medications)
– The methods/types of diet have you tried in the past to change your dietary habits.
Why you stopped/discontinued the approach(s)?
Like medication, it is important to understand the indications, contraindications, role, limitations, adverse reactions, and medication interaction of supplementation, as many supplements contain active ingredients that can have strong effects on the body.
12)
11) How often do you have a bowel movement?
On a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above approach(s)? (please circle)
Please tick the most appropriate box below:
More than 3 times per day 1-2 times per day 2-3 times per day
Caution should always be promoted to clients of the possibility of unexpected side effects, especially with the introduction of a nutritionally adequate diet and increased intake of certain vitamins/minerals. Side effects can also occur when taking new or slightly different nutritional products or medications, either by themselves or in conjunction with other products.
Once every 2-3 days A few times per week Once per week
For example:
• Vitamin K can reduce the ability of the blood thinner Coumadin® to prevent blood from clotting
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no) If you answered yes for the above question, please describe below:
• St. John’s Wort can accelerate the breakdown of many drugs (including antidepressants and birth control pills) and thereby reduce their effectiveness
– The methods/types of diet have you tried in the past to change your dietary habits.
– Why you stopped/discontinued the approach(s)?
13) List your top three priorities in life.
• Antioxidant supplements (such as vitamins C and E) might reduce the effectiveness of some types of cancer chemotherapy
12)
• Vitamin C enhances the absorption of iron, which is recommended for a client with anaemia but can be dangerous for a client with hemochromatosis (a hereditary disorder where excess iron is stored in tissues).
On a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above approach(s)? (please circle) 1 2 3 4 5 6 7 8 9 10
It is also important to remember that many foods nowadays are fortified and may, therefore, contain an increased nutrient profile. As a result, certain nutrients may be ingested in higher than recommended amounts, which can result in nutrient toxicity and damage to the body.
For example:
• Vitamin A toxicity can cause headaches and liver damage, reduce bone strength, and cause birth defects
• Iron toxicity can cause nausea and vomiting and may damage the liver and other organs.
13) List your top three priorities in life.
Clients that are pregnant or breastfeeding MUST be referred to an appropriate health professional, as supplements required at this level should always be recommended by a medical professional. This would also apply to anyone under the age of 16 years.
11)
9) Do you regularly suffer from any cravings?
11) How often do you have a bowel movement?
Please discuss in detail including craving frequency, food type and if you are aware of any triggers.
often do you have a bowel movement?
Are you currently using any supplements and/or vitamins? Please list these below and provide dosage details. (This question is not referring to medications)
Please
Please tick the most appropriate box below: More than 3 times per day 1-2 times per day
10) Are you currently using any supplements and/or vitamins? Please list these below and provide dosage details. (This question is not referring to medications)
How often do you have a bowel movement?
Please tick the most appropriate box below:
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no) If you answered yes for the above question, please describe below:
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no)
If you answered yes for the above question, please describe below:
The methods/types of diet have you tried in the past to change your dietary habits.
The methods/types of diet have you tried in the past to change your dietary habits.
Identifying the bowel habits of a client indicates to the nutrition coach the adequacy of the client’s fibre intake, hydration status and overall gut health, which is useful in forming specific recommendations to help improve bowel health.
Why you stopped/discontinued the approach(s)?
Why you stopped/discontinued the approach(s)?
11) How often do you have a bowel movement?
Please tick the most appropriate box below:
12)
More than 3 times per day 1-2 times per day 2-3 times per day
Once every 2-3 days A few times per week Once per week 12)
As a nutrition coach, it is important to remember that this is sensitive information, and the client may not feel comfortable sharing this type of personal information. Therefore, it is imperative that nutrition coaches make the client feel comfortable and reassure the client that their information is kept confidential. If a client does not feel comfortable sharing this information, they should not feel obligated or pressured into doing so.
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no)
Once every 2-3 days A few times
If you answered yes for the above question, please describe below:
a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above
On a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above approach(s)? (please circle)
– The methods/types of diet have you tried in the past to change your dietary habits. – Why you stopped/discontinued the approach(s)?
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no)
If you answered yes for the above question, please describe below: – The methods/types of diet have you tried in the past to change your dietary habits.
Why you stopped/discontinued the approach(s)?
On a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above approach(s)? (please circle)
13) List your top three priorities in life.
On a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above approach(s)? (please circle)
By understanding a client’s previous efforts or approaches to changing their dietary habits, a nutrition coach can form an impression of how likely the client is to maintain a nutritional plan and which areas they may require further assistance with.
13) List your top three priorities in life.
Understanding the difficulties encountered by the client during past dieting attempts is important for a nutrition coach, as it allows them to provide simpler or more realistic recommendations based on this information.
13)
Clients who have a history of unsuccessful dieting attempts may also require ongoing support and are unlikely to respond well to major changes imposed immediately. Taking the time to understand the client’s barriers to change will allow the nutrition coach and client to work together to formulate strategies to avoid/manage the same barrier/s and increase the likelihood of the client reaching their goals.
List your top three priorities in life.
Have you tried any diets or approach(s) in the past in an attempt to change any dietary habits? (yes/no)
If you answered yes for the above question, please describe below:
The methods/types of diet have you tried in the past to change your dietary habits.
Why you stopped/discontinued the approach(s)?
This section of the client questionnaire (questions 13 to 21) focuses on the client’s goals and their motives for reaching those goals.
12)
Identifying the health-related goals and motives of the client allows a nutrition coach to:
• Build rapport with the client and successfully support them to reach their goals
On a scale of 1 – 10 (10 being the hardest) how difficult did you find the process of the above approach(s)? (please circle)
• Effectively design nutritional plans or make dietary suggestions that cater specifically to the client’s unique goals and objectives
• Ensure a ‘one size fits all’ approach is avoided.
Below are the questions within this section of the client questionnaire, explaining why each particular question can be useful for a nutrition coach.
13) List your top three priorities in life.
The client should be prompted to discuss their top priorities in life to identify which may influence their adherence to a nutritional plan (such as time with family, work, health etc.). These priorities should then form the basis of the client’s goals and motivations for change.
Reminding a client of their priorities and who/what else will benefit from their changes can be very powerful to help keep them motivated.
14 14)
What are your current health-related goals?
Please also provide details on how long you think it will take to achieve these goals?
It is important to have the client clearly articulate their goals, but for many clients, these goals will be delivered in generic, broad terms. As a nutrition coach, it is important to assist clients in rewording their goals into SMART goals, to provide the client with clear, defined goals where they can monitor their progress as they work towards achieving them.
14) What are your current health-related goals?
Please also provide details on how long you think it will take to achieve these goals?
It is fundamental that both the nutrition coach and the client are aware of the goals, as this will help to guide the consultation and ongoing dietary changes. All dietary changes made should be working towards achieving the client’s goals, and therefore having a thorough understanding is crucial. 15
15) In what ways do you think your weight is negatively impacting on your health or lifestyle (if any)?
15) In what ways do you think your weight is negatively impacting on your health or lifestyle (if any)?
This question may require some additional information from the client during a consultation.
A nutrition coachal advisor should look to confirm if the client’s weight impacts their health in any way, including (but not limited to):
16) What is your greatest motivation to become healthy?
• Joint strain
• Sleep issues
16) What is your greatest motivation to become healthy?
• Respiratory
• Immunity issues.
17) What do you think you would have to change in your diet or lifestyle to enable you to achieve your goals?
This information is also beneficial to help motivate the client. For example, if the client comments that their weight is impacting their joints and therefore affecting exercise ability; it can be motivating for them to be reminded that as they lose more weight, they will potentially suffer less with joint pain and therefore be able to complete more physical activity, which in turn, will assist with further weight loss.
17) What do you think you would have to change in your diet or lifestyle to enable you to achieve your goals?
18) What do you think are the biggest challenges to achieving your goals? (Please tick the boxes and explain where possible).
This reiterates to the client that improvements in their weight can benefit their quality of life in many ways.
18) What do you think are the biggest challenges to achieving your goals? (Please tick the boxes and explain where possible).
15) In what ways do you think your weight is negatively
16) What is your greatest motivation to become healthy?
14)
14)
What are your current health-related goals?
What are your current health-related goals?
Please also provide details on how long you think it will take to achieve these goals?
on your health or lifestyle (if any)?
Identifying a client’s motivation for becoming healthy is beneficial to a nutrition coach, as it assists in developing strategies to engage and motivate the client throughout their journey and assists in developing goals and ongoing support strategies.
Please also provide details on how long you think it will take to achieve these goals?
17) What do you think you would have to change in your diet or lifestyle to enable you to achieve your goals?
Gaining this information also allows a nutrition coach to review a client’s motivation to identify potentially dangerous factors such as mental health or eating disorders.
16) What is your greatest motivation to become healthy?
15) In what ways do you think your weight is negatively impacting on your health or lifestyle (if any)?
If the client cannot comment on their greatest motivation for change, consider rephrasing the question to: ‘why do you want to make the changes?’, which may be more direct and easier to understand.
15) In what ways do you think your weight is negatively impacting on your health or lifestyle (if any)?
18) What do you think are the biggest challenges to achieving your goals? (Please tick the boxes and explain where possible).
17) What do you think you would have to change in your diet or lifestyle to enable you to achieve your goals?
Asking this question allows the client to begin thinking about and taking responsibility for their own goals and what changes they will have to make themselves, as opposed to someone else telling them what to do. This provides the client with a greater understanding of what is involved with reaching their goals.
16) What is your greatest motivation to become healthy?
16) What is your greatest motivation to become healthy?
18) What do you think are the biggest challenges to achieving your goals? (Please tick the boxes and explain where possible).
Knowledge Willpower Time
Support Finances
Boredom
17) What do you think you would have to change in your diet or lifestyle to enable you to achieve your goals?
This information then allows a nutrition coach to provide further education on any additional aspects which may be involved that the client has not considered. For example, the client may suggest that for them to build lean muscle mass, they need to eat more protein. The nutrition coach can then educate the client on other factors involved with gaining lean muscle mass (such as decreasing processed foods, the timing of protein-rich meals and types of protein consumed).
17) What do you think you would have to change in your diet or lifestyle to enable you to achieve your goals?
19) How confident are you that you can reach your health goals?
Energy Stress Health Issues
Communicating this information with the client can also help them to develop an appreciation for what is required of them to see changes.
18) What do you think are the biggest challenges to achieving your goals? (Please tick the boxes and explain where possible).
20)
18) What do you think are the biggest challenges to achieving your goals? (Please tick the boxes and explain where possible).
How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
19) How confident are you that you can reach your health goals?
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
20) How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
This question identifies barriers to change that may prevent the clients from achieving their goals. These barriers must be addressed with suitable behaviour management strategies to support the client’s nutritional journey.
Understanding the client’s barriers to change will provide nutrition coaches with the opportunity to pre-plan to avoid or overcome their identified barriers to change, which are pivotal for the client to reach their goals.
19) How confident are you that you can reach your health goals?
19) How confident are you that you can reach your health goals?
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
If a client’s barriers to change are not discussed and strategies are not implemented, the client may not be able to stick to dietary recommendations. This may decrease motivation, increase negative self-talk, and as a result, the client may struggle to reach their goals.
20) How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
20) How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
Behaviour management strategies are discussed in the unit ‘NAT11046005 - Analyse and Apply Principles of Psychology and Behaviour Management’.
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
19) How confident are you that
19) How confident are you that you can reach your
20) How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
19) How confident are you that you can reach your health goals?
20) How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
It is important to identify the client’s current confidence levels and ways in which their confidence levels can be increased. Tracking confidence levels as a benchmark throughout their health journey can help indicate when the client may be at risk of straying from their nutritional goals and when they may require additional support or modification of their plan.
20)
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
How could I help you increase your confidence? (e.g. recipe ideas, handy tips, regular appointments etc).
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
When the nutrition coach knows exactly how the client will feel more confident (e.g. meal plan, regular follow-up contact), they can provide the client’s preferred form of support and strategies. If a nutrition coach is unaware that certain aspects will improve a client’s confidence levels, the nutrition coach may not think to offer that particular strategy; this may slow or stop their progress. 21
21) Are you looking for a full meal plan or would you prefer to adjust your current lifestyle with some additions? (If neither, please advise what are you hoping to achieve in today’s session?)
Understanding what the client wants to achieve and gain from the consultation is extremely important. If the client’s goal/s is not clearly defined or worked towards, they may be unsatisfied with the service provided.
The client may request a full meal plan or prefer to modify their current dietary habits to better reach their nutritional requirements. Alternatively, they may want to discuss nutrition strategies based solely on their exercise regime and are requesting tips, tricks and recipes.
CLIENT QUESTIONNAIRE (EXAMPLE) - VAST FITNESS (V:1. 2018)
3

As a nutrition coach, additional questions can be asked to gain a better understanding of the client’s lifestyle and support networks, which may hinder or assist them in reaching their goals. Examples of the types of questions a nutrition coach could ask their clients are outlined below (questions 22-28).
Below are the questions within this section of the client questionnaire, explaining why each particular question can be useful for a nutrition coach.
22) Who do you live with (i.e. family or friends)?
This doesn’t necessarily require the names of people a client lives with; instead, it refers to the ‘type’ of person the client lives with (i.e. parents, partner, housemates etc.). Asking the client who they live with gives the nutrition coach an idea of how many people are in the household and what their life may look like.
23) Who does most of the cooking at home?
For example, a middle-aged lady who lives alone may be expected to have fewer distractions, more opportunities to cook what she likes and fewer people to influence her cooking decisions. On the other hand, a middle-aged lady who lives with her fly-in-fly-out husband and four children may be expected to have far less time (requires quick and easy meal options), have children influencing her cooking decisions (family-friendly recipes), and may have abnormal eating patterns, varying from day to day.
22) Who do you live with (i.e. family or friends)?
24) Are your friends and family supportive of your lifestyle goals?
23) Who does most of the cooking at home?
25) How frequently do you consume takeaway or eat out at restaurants? Please provide details.
22) Who do you live with (i.e. family or friends)?
Knowing who cooks in the household will provide insight into potential barriers to change. If the client does the cooking themselves, this indicates that they are able to control what is cooked and at what time. However, if the spouse or a family member makes the meals, they may not be as willing to change their way of cooking.
24) Are your friends and family supportive of your lifestyle goals?
26) Approximately, how much do you budget for groceries each week?
If it is identified that another member of the household does the majority of the cooking, it can be beneficial to encourage the client to invite that family member along to a couple of the consults so that they can gain an appreciation and understanding of the dietary changes. Including family members in the process may empower them to make the changes, especially if the changes will benefit them as well.
23) Who does most of the cooking at home?
22) Who do you live with (i.e. family or friends)?
25) How frequently do you consume takeaway or eat out at restaurants? Please provide details.
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
24) Are your friends and family supportive of your lifestyle goals?
23) Who does most of the cooking at home?
28) How much sleep are you getting?
26) Approximately, how much do you budget for groceries each week?
(Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
For some clients, the nutrition coach may be the only source of support they have to make positive health changes, while for others, they may come from an extremely supportive environment. If the client comes from an unsupportive environment, this can provide a large barrier to change, as they will constantly be negatively influenced.
25) How frequently do you consume takeaway or eat out at restaurants? Please provide details.
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
24) Are your friends and family supportive of your lifestyle goals?
It can be beneficial to explore this area with the client and ascertain their confidence level to achieve their goals, despite unsupportive friends and family. From here, the nutrition coach and client can address unsupportive environments and develop solutions to this barrier.
26) Approximately, how much do you budget for groceries each week?
28) How much sleep are you getting? (Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
25) How frequently do you consume takeaway or eat out at restaurants? Please provide details.
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
It is important to understand how frequently the client chooses to consume food outside of the home, which type of restaurant/takeaway outlet is selected and what food and drinks are ordered. By obtaining this information, it may be discovered that a client eats out five times a week; therefore, this may have to be worked into a meal plan.
26) Approximately, how much do you budget for groceries each week?
28) How much sleep are you getting?
Clients may also require education on which takeaways/restaurants are healthier options and which food options are the better choice. Nutrition coaches may also like to educate on how to make similar meals at home to improve the food’s nutritional content and enhance confidence in cooking.
(Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
28) How much sleep are you getting?
(Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
24) Are your friends and family supportive of your lifestyle goals?
26) Approximately, how much do you budget for groceries each week?
23) Who does most of the cooking at home?
While this question may seem somewhat intrusive, nutrition coaches need to know what budgetary constraints their clients may have. When the client answers, nutrition coaches should not pass judgement or comment; this information should be considered when developing the nutritional plan.
25) How frequently do you consume takeaway or eat out at restaurants? Please provide details.
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
24) Are your friends and family supportive of your lifestyle goals?
For example, if a nutritional plan is given to the client which contains large amounts of exotic ingredients and more expensive fruits and nuts, the client may not be able to afford it. Therefore, they would likely not stick to the plan and potentially not return for a follow-up consultation. However, if the same person was given a meal plan, taking their budget into account, they can easily go to shops, purchase the required ingredients and eat as per their plan.
28) How much sleep are you getting?
26) Approximately, how much do you budget for groceries each week?
(Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
25) How frequently do you consume takeaway or eat out at restaurants? Please provide details.
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
Identifying the cooking equipment/utensils the client has access to is also important for nutrition coaches to consider. It is important that assumptions aren’t made and that the nutrition coach knows that not all clients have access to basic cooking equipment.
26) Approximately, how much do you budget for groceries each week?
28) How much sleep are you getting?
(Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
27) Do you have access to all basic cooking equipment such as an oven, stove, microwave and blender?
Clients may not have had access due to their blender breaking or are in the process of building a home and therefore staying at a caravan park, or simply because they do not believe microwaves are safe to use. Whatever their reasoning, this information should be considered when developing their nutritional plan.
28) How much sleep are you getting?
(Please provide details on hours of sleep each night as well as details if its broken/unbroken sleep)
Sleep/lack of sleep can impact hormone levels (especially cortisol - a stress hormone) and hunger/satiety signalling. Establishing a client’s sleep patterns is beneficial as this can inform specific dietary recommendations to help manage any sleep-related issues.
CLIENT QUESTIONNAIRE (EXAMPLE) - VAST FITNESS (V:1. 2018)
To optimise results and client adherence, a sound understanding of the client’s past and current exercise habits/regime must be obtained. Even if the client does not have any prior exercise experience, it is good to understand their baseline fitness levels (if any) so that encouragement and support can be provided to help them reach exercise goals.
While a nutrition coach can encourage and motivate clients to achieve the physical activity and exercise guidelines for all Australians,(98) individualised exercise recommendations must be provided by a qualified exercise scientist or personal trainer (PT), as this is outside a nutrition coach’s scope of practice.
When discovering the client’s exercise habits, ask questions relating to their past and current training and their preferred physical activities, paying special attention to the following areas:
• Type of exercise routine, intensity and duration
• Past exercise
• Motivation
• Limitations.

Understanding a client’s current exercise routine will allow a nutrition coach to utilise this information to encourage the client to reach minimum physical activity guidelines and calculate caloric and macronutrient requirements. For example, a sedentary client will have lower caloric requirements when compared to a client who exercises for 200 minutes most weeks.
The following questions can help obtain information regarding the client’s current exercise regime:
• What does their weekly exercise routine look like?
• What time of day do they exercise, and which days of the week work well for them? Why?
Below is an example of an exercise review table that can be completed to help identify the client’s current exercise habits.
• Type of Activity: refers to what activity was completed. For example, bike riding, walking, HIIT or Yoga
• Time of Day: refers to what time of day the client usually chooses to complete their physical activity
• Duration: refers to the length of time the activity takes to complete. This could be 15 minutes, 45 minutes or 90 minutes
• Intensity: refers to how hard the client believes they pushed themselves. Intensity is generally rated as low, medium or high intensity.
MONDAY
TUESDAY
WEDNESDAY
THURSDAY
FRIDAY
SATURDAY
SUNDAY
Understanding a client’s past exercise history is valuable to identify if their energy expenditure or caloric requirements have changed, which may have influenced their current health status, weight, nutritional intake and fitness levels. For example, a client may have a history of playing soccer all their life; however, in the past two years, has had to stop, which they feel may be caused by their current weight gain and joint pain.
This information can, therefore, be utilised to motivate the client to make healthy changes (i.e. if the client recommences light exercise, they might optimise weight loss), which will reduce pressure and pain on joints and therefore, they may be able to play soccer again.
Questions that can help to determine a client’s past exercise regime include:
• What exercise have you done in the past?
• Do you have a history of exercise? Or are you commencing exercise for the first time?
• Which physical activities have you enjoyed doing in the past (e.g. sports or activities like hiking)?
It is important to discover what motivates the client to undertake exercise, as this information will be useful in maintaining motivation levels if/when they begin to drop.
There are many reasons why a client may take part in exercise/physical activity; these include (but are not limited to):
• Exercising because it makes them feel better
• Exercising to lose weight
• Exercising because they want to maintain mobility in the later stages of their life
• Exercising is an opportunity to meet new people.
Questions that a nutrition coach can ask to determine a client’s motivation for exercise include:
• What motivates you to be healthy?
• What are your fitness goals? (consider creating a SMART goal with the client).
Reminding the client in a positive way of their goals and the many benefits of exercise can help them surge through the negative self-talk and periods of low motivation.
Understanding the clients’ limitations to completing exercise or improving their physical capabilities is important.
For example, some limitations may include:
• Financial constraints
• Time constraints
• Injury
• Lack of support
• Lack of motivation.
When limitations are fully understood, a nutrition coach can discuss potential strategies to overcome these limitations or can complete a referral to an appropriate health professional for further support.
Questions that can be asked to determine a client’s exercise limitations include:
• What limits do you have when it comes to exercise?
• Do you have any pre-existing injuries?
• What medical history could impact the client’s exercise activity?
• Are there any barriers to change, such as being time-poor, financially restricted or inadequate support from friends or family?

It is important to remember that it is not within a nutritional advisor’s scope of practice to advise clients on specific exercise programs or requirements, as the depth of knowledge required to effectively and safely support exercise requirements for clients is not sufficiently covered in the performance criteria of the 11046NAT - Certificate IV in Nutrition.
A nutrition coach can, however, provide general physical activity advice and guidelines for physical activity that align with their scope of practice and the physical activity and exercise guidelines for all Australians.
CLICK HERE to view the link.
*To reiterate, it is outside the scope of practice for a nutrition coach to recommend, prescribe and/or conduct individualised or tailored exercise plans with explicit types of exercises, timeframes, intensities, or frequency. If a nutrition coach was to develop a tailored exercise plan for a client, it could possibly injure the client or be unsuccessful, which could result in legal liability and long-term health issues.
The appropriate qualifications required for prescribing personalised exercise plans include Vocational Education and Training (VET) qualifications and higher education programs, such as:
• Certificate III in Fitness
- Gym Instructor
- Group Exercise Instructor
- Aqua Exercise Instructor
• Certificate IV in Fitness (personal trainer)
• Diploma of Fitness
• Higher Education/university degrees such as
- Bachelor of Sport and Exercise Science
- Bachelor of Human Movement
- Bachelor of Clinical Exercise Science.

When conducting an initial consultation, the client’s current diet will be the foundation for any lifestyle changes. Integrating a food diary into an initial consultation is beneficial for the nutrition coach and the client, as it allows a nutrition coach to identify, confirm and investigate their clients’ current nutritional intake.
A food diary is a simple daily record of food and drinks consumption, which is completed by the client over a period of three to seven days prior to the initial consultation. The purpose of the food diary is to allow a more comprehensive understanding, review current dietary habits and identify patterns.
While a food diary is beneficial for the nutrition coach to fully assess and comprehend the client’s dietary intake, it can also prove to be motivational for the client as they write everything down. For example, the client may not previously recognise how much they are eating or exactly what type of diet they are following until they write it down for themselves.
It may be common that clients will omit certain information from the food diary; however, they must be encouraged to complete an accurate food diary. An accurate food diary will provide the nutrition coach with a deeper understanding of what the client is consuming, of which recommendations and education can be tailored to suit.
While Queensland Health provides a basic food diary template, the majority of health professionals like to update the table to allow for a more detailed assessment. CLICK HERE to view the link.
A food diary should include the following information:
• Type of food/drink (e.g. chicken breast, baby spinach, soda water)
• Preparation methods (e.g. oven baked, pan fried, grilled)
• The quantity of food/drink consumed (e.g. 100g, 1 cup, 200ml)
• Time of consumption (e.g. 6am, 11.30am, 7.45pm).


Some additional information to collect, which allows for an even more detailed data collection, include:

• Environmental setting (e.g. home, work, friend’s house) - the environment may impact what the client eats. For example, a client may eat a chicken salad while at home yet be tempted by a fast food outlet while out. Knowing what the environment encourages in terms of dietary intake can be beneficial as recommendations can be tailored to suit each environment.
• The mood of the client at the time of consumption (e.g. angry, sad, happy) - this can be beneficial to help identify emotional eaters or particular mood triggers. For example, a sad person may be tempted to binge on chocolate or wine.
• Any exercise conducted including activity, time, intensity and duration (e.g. Basketball game, 7.30 pm, modhigh intensity, 45min) - understanding a client’s exercise regime can help to decipher if more nutrition is required prior, during or post-exercise. However, if the client has completed the earlier Exercise Review Table, they do not need to record this information on the food diary.
Monday 22/10/18
Bacon x3 rasher
Boiled Egg x2
Tomatoes
Capsicum
Porterhouse
Monday 22/10/18
Diane
Doritos Cheesy Sour cream
Avocado dip
FOOD DIARY
CLICK
When completing a food diary, it is vital that a nutrition coach encourages the client to write as many details about their food intake as possible and remind them that too much information is better than too little.
If the client is having difficulties in completing their food diary, advise them to get in contact for advice and assistance. It may be helpful to organise a face-to-face, phone or Skype meeting for the client to fully understand the expectations and instructions
Provided below are additional tips to assist clients in completing a food diary:
• Remind the client that a nutrition coach can help them best achieve their nutritional and health goals when their food diary is as honest and accurate as possible
• Encourage the client to keep their food diary with them at all times so that they can complete it throughout the day at the time of eating, which increases accuracy and avoids forgetting certain foods/drinks. If they forget their diary, encourage the client to take a photo of their food and enter it into their diary later
• Discuss the different methods for keeping a food diary, i.e. pen and paper, phone notes, computer spreadsheet or food analysis app, such as MyFitnessPal
• Ensure that the client has a clear understanding of food measurements and if unsure, encourage the client to estimate quantities of food or to look up quantities on the internet or read the food label.
It is important to be aware that a nutrition coach may encounter clients who do not have the literacy or writing skills to effectively record a food diary. In this case, there are many technological methods that a nutrition coach can recommend as an alternative, such as mobile apps, which allow clients to take pictures before and after their meals and snacks or even scan specific products to record their food consumption. Encouraging this alternative with clients can make recording a food diary faster and easier.
Some of the most popular mobile apps include:
• MyPlate
• MyFitnessPal
• LifeSum
• MyNetDairy
• Calorie Mama.
MOBILE APP
MYPLATE
LIFESUM
MYFITNESSPAL
MY NET DIARY
DESCRIPTION
Weight and exercise tracker, allowing the client to track macronutrients and total calories. MyPlate can also provide community support and encouragement by others using the app.
Food tracking application allowing the client to set nutritional goals (e.g. protein goals, carbohydrate intake) and track their macronutrients, total calories and micronutrients. LifeSum also offers barcode scanning, recipes and eating plans.
Food and fitness tracking allowing the client to track macronutrients, total calories, micronutrients and daily activity. MyFitnessPal also allows photographs of progress to be added, creates nutrition charts, scans barcodes and can link to social media.
Food and fitness tracking application allowing the client to track macronutrients, total calories and micronutrients. MyNetDiary can be personalised with dietary goals and provides a breakdown of the nutritional value of each food item, meal and entire day.
Food tracking application allowing the client to track macronutrients and total calories. Calorie Mama automatically counts calories by taking photos of food and offers recipes and meal plans.
Apps are usually free to download but can have in-app purchases for premium features. Each app will have positive and negative aspects, and it is best to try a few apps to begin with to see which works best for a client, especially if they are considering paying for premium features.
If the client shows a preference for an electronic method of completing their food diary, below is an example of an excel spreadsheet template that can be utilised for each day of the week:

Step 5, in the process of confirming a client’s health status, refers to collecting body composition data using specific anthropometric methods. There are numerous methods to measure body composition, all of which are beneficial for a nutrition coach to understand to enable active and effective monitoring of their client’s progress.
Anthropometric methods refer to the comparative study of sizes and proportions of the human body. It is a branch of anthropology dealing with measuring the human body to determine differences in individuals and groups. It is used in medicine, space programs and archaeology.(99)
Obtaining initial anthropometric measurements from the client is important for a number of reasons, including:
• Gaining a greater understanding of the client’s nutritional health
• Many of the initial measurements are used to conduct baseline equations to calculate the client’s Estimated Energy Requirements (EER), Estimated Protein Requirements (EPR), Estimated Fluid Requirements (EFR), Ideal Body Weight (IBW) and Adjusted IBW (AIBW)
• Assisting the client in setting SMART goals and understanding what is achievable
• Providing motivation for the client as they observe their baseline measurements increase or decrease according to their goals.
There are various methods that a nutrition coach can utilise with their clients to collect body composition measurements, including:
• Height, weight, BMI
• Waist measurements
• Waist-to-hip ratio
• Skinfold measurements. Further details and instructions for obtaining these measurements are outlined on the following pages.
Body Mass Index (BMI) uses weight and height measurements to determine if an adult is within the healthy weight range, underweight, overweight or obese. It establishes an estimate of total body fat and the potential risk of developing weight-related diseases.
BMI scores can be written simply as the number (e.g. BMI = 25) or with the equation attached (e.g. BMI = 25kg/m2), which is the more formal approach recommended when writing to other health professionals.(100)
If a client is overweight (with a BMI over 25kg/m2) and physically inactive, they are at increased risk of:
• Cardiovascular disease (CVD)
• Gallbladder disease
• High blood pressure (hypertension)
• Diabetes
• Osteoarthritis
• Fatty liver disease
• Sleep apnoea
• Kidney disease
• Gout
• Certain types of cancer, such as breast cancer or colon cancer
• Depression and other mental health disorders.
If a client is underweight (BMI less than 18.5kg/m2), they may be malnourished and at increased risk of:
• Compromised immune function
• Respiratory disease
• Digestive diseases
• Cancer
• Fertility issues
• Osteoporosis.
BMI is an approximate measure of the ideal weight for health. To calculate BMI, the following information is required:
• Weight in kilograms (kg)
• Height in metres (m).
To calculate BMI, divide the client’s body weight in kilograms by their height (in metres) squared (BMI = kg/m2).
For a person that is 175cm tall with a weight of 70kg: = 70kg / (1.75m)2
= 70 ÷ (1.75 x 1.75) = 70 ÷ 3.063
BMI = 22.86kg/m2
HOW TO CALCULATE BMI:
BMI = Kg / (Height [m])2
There are also many online calculators that can be used to determine BMI, including:
‘Health direct’ BMI CALCULATOR.
The Heart Foundation BMI CALCULATOR.
NSW Government Health BMI CALCULATOR
The National Institute of Health BMI CALCULATOR.
Once BMI has been calculated, it can then be identified if the client is classed as underweight, healthy weight, overweight or obese using the BMI ranges below. The ranges are based on associations between chronic diseases (comorbidities) and mortality risk and have been adopted for use internationally by the World Health Organisation (WHO).(100)
BMI ranges for weight classification in adults are as follows:
It is important to note that BMI is not considered the best measurement of weight and potential health risk since it does not distinguish between fat and fat-free mass (bones, muscles, fluid etc.).
A person’s waist circumference is considered a better predictor of health risk than BMI.
Obese (>30)
Overweight (25-30)
(18.5-25)
HEIGHT IN FEET/INCHES AND CENTIMETERS
Note: BMI Values rounded to the nearest whole number. BMI categories based on CDC (Centers for disease control and prevention) criteria. BMI= Weight(kg) / (Height[(m]) = 703 x Weight [lb] / (Height [in])
Underweight (<18.5)
BMI does not differentiate between body fat and fat-free mass (muscle), meaning that there are some exceptions to the BMI rule, including:
• High muscle mass
• Low muscle mass/muscle wastage
• Height
• Ethnicity.
Clients with a higher than average percentage of muscle mass are not appropriate for BMI calculation as the BMI does not differentiate between fat mass and muscle mass. In this case, BMI would simply identify the person as overweight or obese.
For example, Olympic weightlifters are often classified as overweight or obese according to their BMI.
In contrast to the above, BMI underestimates the amount of total fat mass for those with low muscle mass or muscle wastage. Groups particularly susceptible to low muscle mass or muscle wastage include the elderly, those with eating disorders and those with physical disabilities.
BMI provides a calculation for the average height of a human, and unfortunately, this means that those who are unusually tall or unusually short will have their BMI underestimated or overestimated.
As a general guide, BMI should not be calculated on clients shorter than 150cm or taller than 190cm.
As each ethnic group has varying ratios of muscle to fat mass, it is inappropriate to use the same BMI reference ranges for all ethnic groups.
For example, Asian and Indian clients tend to have a higher fat mass than clients of European descent and, therefore, may require lower BMI reference ranges. On the other hand, clients of Torres Strait Islander and Maori descent are known to maintain a heavier build without increased health risk and can, therefore, have higher BMI reference ranges.
The link between being overweight or obese and the risk of illness/disease is not well defined. Research is ongoing, although statistically, there is a greater chance of developing some diseases when overweight or obese. For example, the risk of death increases by approximately 20 to 30% as BMI increases from 25kg/m2 to 27kg/m2. Additionally, as BMI increases above 27kg/m2, the risk of death increases more steeply by approximately 60%.
Although working with children falls outside the scope of practice of a nutrition coach, it is still important to understand BMI ranges and how they can differ among children.
Children are continuously growing and developing, which makes it difficult to establish set values for BMI cut-offs. For many adults, where the growing process has stopped, an increase in BMI is usually caused by increased body fat. However, as children grow, their fat, muscle and bone mass changes, as does their BMI. For example, BMI generally decreases during preschool years and then increases during adolescence into adulthood.
For this reason, BMI calculations for children or adolescents are interpreted differently and take into account the age and sex of the child or adolescent.
The current BMI charts for children have been created by the US Centres for Disease Control and Prevention. These charts are useful for the assessment of overweight and obesity in children aged over two years; however, they should only be used as a guide to indicate when lifestyle changes may be necessary and when to seek further guidance from a GP or an APD.
As with any source of information or guideline, there will always be ongoing research and debate as to the pros, cons and longevity of the topic at hand. While the pros and cons of the BMI have been explored above, it is encouraged that nutrition coaches complete additional learning on this topic to extend their knowledge of the BMI calculation and enhance confidence in using the BMI calculation by itself or with the addition of other anthropometric measurements.
PODCAST - BODY MASS INDEX (BMI) ON THE RISE (THE HEALTH REPORT)
CLICK HERE to view the link.
PODCAST - RETHINKING BMI & MORTALITY (THE HEALTH REPORT)
CLICK HERE to view the link.
ASSOCIATION OF MORTALITY WITH OVERWEIGHT & OBESITY USING BMI CATEGORIESA SYSTEMATIC REVIEW AND META-ANALYSIS (JOURNAL ARTICLE)
CLICK HERE to view the link.
HEALTHY BODY FAT RANGES - AN APPROACH FOR DEVELOPING GUIDELINES BASED ON BMI (JOURNAL ARTICLE)
CLICK HERE to view the link.
Waist circumference (WC) reflects subcutaneous abdominal fat storage and, according to the World Health Organisation (WHO), has been shown to indicate a health risk.
A client’s waist circumference is a better predictor of health risk than BMI. Stored fat around the abdomen (known as ‘abdominal adiposity’ or ‘central obesity’), regardless of body size, indicates a greater risk of developing obesity-related health conditions such as:(101)
• Cardiovascular disease (CVD)
• High blood pressure
• High cholesterol
• Diabetes.
This increased risk is due to increased fat around vital organs within the abdominal area. Men, for example, often store weight in the waist/stomach region and therefore have an increased risk of obesity-related disease. Comparatively, fat predominantly deposited (or stored) around the hips and buttocks (seen typically in females) doesn’t appear to have the same health risk.
Generally, the link between health risks and body fat distribution are as follows:
• Lowest risk (slim/evenly distributed body fat)
• Moderate risk (overweight with no abdominal adiposity)
• Moderate to high risk (slim with abdominal adiposity)
• High risk (overweight with excess abdominal adiposity).
Waist circumference can also be used as an indication of a client’s health risk for chronic diseases (outlined in the following table):
MALE
FEMALE
Less than 94cm 94cm or more 120cm or more
Less than 80cm 80cm or more 88cm or more
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
• White fat stores energy in the form of a single large fat reservoir
HOW ARE THEY DIFFERENT?(91)(92)
• Have both thermogenic and storage capabilities.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
To identify a client’s health risk, it is important to measure their waist circumference accurately by following the steps below:
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
HOW ARE THEY DIFFERENT?(91)(92)
• Have both thermogenic and storage capabilities.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• White fat stores energy in the form of a single large fat reservoir
Place the tape measure directly around the client, preferably over no more than one layer of light clothing.
• White fat affects an individual’s hormone production and hunger levels
• White fat stores energy in the form of a single large fat reservoir
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
Ensure correct placement of the tape measure, halfway between the lowest rib and the top of the hip bone (generally in line with the belly button).
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat affects an individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
• Have both thermogenic and storage capabilities.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
Ask the client to breathe out normally and take the measurement.
Make sure the tape is pulled tight, without squeezing the skin.
Before a nutrition coach takes any sort of circumference measurement, it is essential that the client is aware of the process and provides consent, as taking a circumference measurement requires close contact between the client and the nutrition coach, which may make the client feel uneasy if they are not prepared. Simply explaining to the client what the process involves and asking for their consent to take the measurement is essential.

Waist-to-Hip Ratio (WHR) is used frequently by health professionals (on adult clients only) to identify a client’s weight status (healthy or overweight) and health risk. The WHR is a simple calculation that determines the ratio between the waist circumference (previously discussed) and the hip circumference (HC) (explained below).
HOW ARE THEY DIFFERENT?(91)(92)
This calculation provides a greater indication of how much excess fat is stored in the abdominal region and health risks, such as high blood pressure and high cholesterol.
HOW ARE THEY DIFFERENT?(91)(92)
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
BROWN FAT WHITE FAT BEIGE FAT
• White fat stores energy in the form of a single large fat reservoir
With the client standing tall, legs slightly apart and breathing normally, place the tape measure around the widest part of their body (this will be over the greatest protrusion of the client’s gluteal (buttocks) muscles).
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
Ensure that the tape measure is straight, has no twists and is firmly against the body.
HOW ARE THEY DIFFERENT?(91)(92)
• White fat affects an individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
• White fat stores energy in the form of a single large fat reservoir
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
BROWN FAT WHITE FAT BEIGE FAT
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
The steps for calculating a client’s WHR are as follows:
• White fat affects an individual’s hormone production and hunger levels
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
• Beige cells can generate heat and can burn energy
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• Brown fat cells are comprised of mitochondria and multiple small fat reservoirs.
• White fat stores energy in the form of a single large fat reservoir
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
• Have both thermogenic and storage capabilities.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• Beige cells are comprised of a high number of mitochondria and mediumsized fat reservoirs
Ask the client to stand straight and breathe normally. Use a tape measure to identify the circumference around their waist (the smallest part of their body, generally just above their belly button).
• Generates heat and helps regulate the body’s internal temperature in response to the changing external environment
• White fat affects an individual’s hormone production and hunger levels
• Beige cells can generate heat and can burn energy
• Have both thermogenic and storage capabilities.
• Brown fat acts similarly to muscle tissue and can use white fat for fuel (at times).
• In humans of healthy weight, it can comprise up to 20% of body weight in men and 25% in women.
Ask the client to remain standing tall. Use a tape measure to identify the circumference around their hips (the widest part of their body, generally around their buttocks).
Divide their waist circumference (in cm) by their hip circumference (in cm) to get their WHR (WHR = WC ÷ HC).
EXAMPLE:
Female with a WC of 75cm and an HC of 80cm
WHR = WC ÷ HC = 75cm ÷ 80cm
Therefore, WHR = 0.93 (which is more than 0.85, therefore high risk for poor health outcomes).
The table below can be used to identify if the client’s health is at an increased risk based on their WHR:
The fundamental principle of skinfold measurements is to measure the thickness of fat that sits directly below the skin (subcutaneous fat). Taking skinfold measurements at various locations around the body provides a very good indication of an individual’s body fat percentage; however, the accuracy of this method is heavily reliant on the tester’s experience and ability.
In regards to weight loss, monitoring body composition can be just as helpful, if not more, in assessing the client’s progress and is more reliable than just tracking numbers on the scales. Skinfold tests are widely used by fitness professionals/exercise scientists to estimate both body density and body fat percentage (BF% or BFP) of their clients.
Testing for body fat using skinfold analysis requires the use of a tool known as a ‘calliper’ and pinching the skin and subcutaneous fat, pulling the skinfold away from the muscle, and measuring the thickness of the skinfold with the calliper. Measurements are taken at numerous sites around the body (usually 3-9 separate locations). The individual pinch results for each skinfold site are then added together and entered into an equation along with age, weight, and height.
The equation/result of all sites then gives an indication of the client’s body fat percentage or body composition, which is the relationship between body volume (how much space the body takes up) to body weight.
There are many advantages to conducting skinfold measurements. These include:
• This method can be used by nutrition coaches on many types of clients, not just for athletes, and can be used for improving and monitoring a client’s general health or weight-loss goals
• Skinfold testing allows for a subcutaneous fat measurement, which can help identify different health risks related to an excess of body fat
• As a nutrition coach, having the ability to calculate body fat percentage before, during and after is a very effective tool that effectively monitors a client’s progress and adherence. If a nutrition coachnotices that the client is losing a considerable amount of lean mass and fat, they can take the proper steps to adjust the client’s nutritional plan to improve outcomes for the client.
In addition to the above, research indicates that many clients who attempt ‘fad diets,’ and partake in little or no exercise can lose as much muscle tissue as fat, increasing the likelihood that the client will return to their pre-diet weight or gain back more fat and less lean muscle. Essentially, this means they are the same weight, but their body fat percentage is higher, with less lean muscle mass.
The benefit of having the skill set to perform a skinfold analysis gives nutrition coaches the advantage of determining whether the client’s body composition has changed for the better or worse. In other words, only using a set of scales will not show any of these changes but measuring the client’s body fat percentage will.

Just like many other methods for measuring body fat, skinfold measurements also have their limitations, including:
• There is a larger risk of error in skinfold measurements due to large variability from one measure to another or from one nutrition coach to the next
• Some obese clients cannot be measured via skinfold testing because their fat mass exceeds that of the equipment’s limit
• Conducting a skinfold test only evaluates subcutaneous fat, and studies show that visceral fat is a greater indicator of cardiovascular health than subcutaneous fat
• Accurate skinfold testing is highly reliant on the skill of pinching the subcutaneous fat and pulling it away from the muscle tissue underneath. Therefore, improper techniques can introduce errors into the results
• The equation used to calculate body fat can only predict body composition. The Jackson/Pollock formula is one of the most common equations used; however, this equation is only reliable and valid when measuring clients similar to those used when Jackson/Pollock first developed the equation
• This equation was also based on hydrostatic weight measurements (which also contained errors)
• The accuracy of the callipers can vary depending on the brand and quality of the callipers. Plastic callipers will often produce results with larger error margins.

Ideal Body Weight (IBW) is calculated to determine an appropriate weight for the height of a client to establish a long-term weight loss goal. IBW calculations are used for any client who falls outside the healthy BMI range, be it underweight, overweight or obese. Identifying an IBW can be very motivational for clients, and will assist them in setting their health goals.
The IBW is a calculation that identifies the appropriate weight for a client based on their height and current BMI ranges. Current BMI guidelines, as discussed earlier, suggest that a healthy BMI should be within the range of 18.5-25kg/m2. The IBW essentially identifies a healthy weight range for the client’s height. However, the same limitations regarding body composition within BMI calculations also apply to IBW calculations.
An IBW range is calculated using both of the following two equations. Please note that the first equation is calculating the client’s IBW at a BMI of 18.5kg/m2, and the second equation is calculating the client’s IBW at a BMI of 25kg/m2 both of which are calculated in order to get the IBW range.
IBW = Ht2 x 18.5
IBW = Ht2 x 25
Where:
IBW = Ideal body weight.
Ht = Height in metres.
EXAMPLE:
A client who is 1.9m tall would have an IBW range of:
IBW = Ht2 x 18.5
(1.92) x 18.5
(1.9 x 1.9) x 18.5
3.61 x 18.5
67kg
IBW = Ht2 x 25 (1.92) x 25
(1.9 x 1.9) x 25
3.61 x 25
90kg
Therefore, a client who is 1.9m tall would have an IBW range of between 64kg and 90kg.
It is important to remember that IBW may not be realistic, and for overweight and obese clients, this calculation needs to be adjusted to what is known as Adjusted Ideal Body Weight (AIBW) which is discussed below.
The Adjusted Ideal Body Weight (AIBW) is a calculation used for overweight and obese clients as it provides a more realistic IBW for the client. The AIBW is calculated using both the clients’ height and their current weight.
The AIBW takes into account a client’s IBW and then buffers this weight goal with an additional 25%. The AIBW can be a more realistic and achievable goal for the client, and once their AIBW has been met, they can revisit their goals for further weight loss (if required).
The AIBW is also used to calculate appropriate energy and macronutrient requirements for overweight and obese clients. Using the AIBW to calculate macronutrient and energy requirements will assist with overall calorie restriction, and thus assist with overall weight loss.
EQUATION:
AIBW = IBW + [(actual weight – IBW) x 0.25]
Note: IBW = weight at BMI 18.5 kg/m2 and at BMI 25 kg/m2
Please see the previous calculation for how to identify a client’s IBW range.
A client who weighs 132kg and is 170cm tall, their AIBW would be calculated as shown below: STEP 1 STEP 2
Calculate the client’s IBW range using their height Calculate the client’s AIBW by using their IBW and factoring in their current weight.
IBW = Ht2 x 18.5 (1.72) x 18.5 (1.7 x 1.7) x 18.5 2.89 x 18
53kg
IBW = Ht2 x 25 (1.72) x 25 (1.7 x 1.7) x 25 2.89 x 25
72kg
This client’s IBW range is between 52kg and 72kg. From here, the AIBW can be calculated by factoring in their current weight of 132kg.
Calculate AIBW for lower IBW:
AIBW = IBW + [(actual weight – IBW) x 0.25]
52 + [(132 - 52) x 0.25]
52 + [80 x 0.25] 52 + 20 72kg
Calculate AIBW for high IBW:
AIBW = IBW + [(actual weight – IBW) x 0.25]
72 + [(132 - 72) x 0.25]
72 + [60 x 0.25]
72 + 15
87kg
Therefore the AIBW range would be 72 - 87kg.
The one-on-one initial consultation between the nutrition coach and client is generally guided by a proforma or a type of health questionnaire. This consultation allows the nutrition coach the opportunity to build rapport with the client and gather all relevant information to effectively analyse and provide appropriate recommendations.
There are many factors that can contribute to an effective consultation, these can include:
• The location of the consultation
• Rapport building
• Effective goal setting techniques.

The initial consultation is generally conducted in a consult room in a set business location; however, there is an opportunity to conduct an initial consultation at the client’s home, in a preferred cafe or park or at a nutrition coach’s home office.
The location is dependent on what the nutrition coach and client is most comfortable with and certain factors need to be taken into consideration, such as:
• Noise
• Travel
• Professionalism
• Safety.
Noise can be disruptive and distracting for both the nutrition coachal advisor and the client. It is therefore advised that the location is in a quiet place, so that outside interference/noise can be shut out if required. Some may find intentional background music soothing and helps to avoid ‘awkward silences’ softer music without words is generally preferred.
When conducting the initial consultation from a location other than a home office or business setting, it is important to factor in and consider travel time.
Before agreeing to a consultation at the client’s home or preferred cafe, analyse the travel distance and decide whether this is convenient or not. If the distance is too far, it may be beneficial to discuss some alternatives with the client such as a quiet cafe closer by or meeting in a set business location.
Whether a meeting takes place at a cafe, an office or a home, it is important to maintain professional standards at all times. Dress accordingly for the role of a nutrition coach and in a professional manner.
Ensure the location is maintained to professional standards (e.g. appropriate hygiene and cleanliness, bathroom facilities, space to sit and talk, quiet area) and ensure that there is access to all tools required such as scales, measuring tapes and the internet.
It is important to consider personal safety, especially when consulting with clients in home environments. Consider providing someone (friend, colleague, family member) with a schedule and locations, including start and finish times for appointments.
Make contact before and after the consultation to confirm safety. If the environment feels unsafe, do not go ahead with the consultation. Safety should always be the first priority for nutrition coaches.
It is important that nutrition coaches establish rapport with the client. If the client is not comfortable or at ease, the information gathered may be forced or inaccurate and trust may not be built with the client.
Some clients can find attending consultations and discussing their lifestyle very confronting, awkward or unsettling and it is therefore important that the client is made to feel comfortable and at ease with the nutrition coach.
Prior to commencing the consultation, a nutrition coach may like to ask a number of non diet-related questions to ‘break the ice’. Questions may be as simple as:
• “Did you find the place okay?
• How was your weekend?
• Isn’t this weather beautiful?”
Something simple to get the client talking before delving into the client questionnaire may help the client to relax and open up a little more.
While the location of a consultation and rapport building are important and effective strategies for ensuring a consultation runs effectively, goal setting can also influence the effectiveness of an initial consultation. Not only does goal setting allow a nutrition coach to identify the motives behind the client’s goals, but it also ensures that the initial consultation is purposeful and effective.
There are many benefits to setting goals, these include (but are not limited to):
• Ensuring a clear focus for the client and the nutrition coach
• Optimal preparation and use of relevant resources for the nutrition coach to support and educate the client
• Ability to identify how to effectively utilise consultation time
• Peace of mind for the client in writing down their goals and ideas, while applying perspective and priority
• Ensuring clarity in the decision-making process between the nutrition coach and the client.
When assisting clients to set goals, it is beneficial to help them set what is commonly referred to as S.M.A.R.T goals.
S.M.A.R.T goals are Specific, Measurable, Attainable/Achievable, Relevant/Realistic and Timebound.
S M A R T SPECIFIC MEASURABLE ACHIEVABLE REALISTIC TIMELY
G O A L S WHAT DO YOU WANT TO DO? HOW WILL YOU KNOW WHEN YOU’VE REACHED IT? IS IT IN YOUR POWER TO ACCOMPLISH IT? CAN YOU REALISTICALLY ACHIEVE IT? WHEN EXACTLY DO YOU WANT TO ACCOMPLISH IT?
Setting goals using the S.M.A.R.T principle enables clients to be completely aware of what needs to be done to reach their longer-term goals. Furthermore, clients can create shorter, medium and long-term goals using the S.M.A.R.T method.
“To lose 5kg of weight within the next 4 months”.
For the client to lose weight (long-term goal), they may have multiple strategies (short-term goals) in place, such as decreasing processed foods and increasing vegetable intake, exercising more and practising mindful eating.
In regards to vegetable consumption, the client’s SMART goal may be:
“Within the next 4 weeks, to be consuming 5 serves of vegetables (1 serve = 1 cup raw vegetables or ½ cup cooked vegetables) at least 5 days of every week, with at least 3 different types of vegetables each day”.
The table on the following pages examines S.M.A.R.T goals further, using the example of increasing vegetable intake to assist in weight loss.
Ensure understanding of exactly what the client wants to achieve. The more specific the goal, the better the nutrition coach can structure the program to meet the client’s expectations.
These questions can be asked to the client so they can think more specifically about determining objectives and goals:
• What exactly do you want to accomplish?
• How do you want to accomplish this?
• Who do you want to accomplish this with?
• What limitations do you have?
• Why do you want to reach this goal?
If the aim is to increase vegetable intake to assist in weight loss, the goal must specify how many serves of vegetables need to be consumed each day to reach the desired result. So, instead of simply saying “increase vegetable intake”, a more specific goal would be to increase vegetable intake to 5 serves per day every day of the week.
Measurable goals mean determining what the vision for meeting the goal may look like and the ability to provide evidence that clients are meeting their goals or breaking the goal down into measurable elements.
Measurable goals can be beneficial in refining what exactly it is that a client wants to achieve. Defining the physical proof (or evidence) of a client’s goal or objective makes it clearer and easier for them to reach.
The number of serves of vegetables consumed can be counted; therefore, it is measurable. A weight loss goal could be measured using the measurements from scales or circumference measurements.
Can the client’s goal be reached? A nutrition coach will need to assist the client in determining if the goal is a realistic expectation. The client will need to consider the time and effort that will be required to meet their goal.
RELEVANT/ REALISTIC
TIMEBOUND
Another factor that needs to be considered for ‘achievable goals’ is if the goal is going to conflict with other priorities in life. If there are not enough resources or the goal conflicts with other priorities, this can set the client up for failure. It does not mean that the goal cannot be reached; however, the timeframe and the planning may need to be adjusted to make it realistic.
FOR EXAMPLE:
Is it achievable to actually consume 5 serves of vegetables per day? For some, this may be very easy, while for others, this may not be achievable secondary to food security, allergies, major dislikes or time restraints. When creating a goal, it is important that the goal can actually be achieved to ensure the client does not become disheartened part way through.
This can be determined by asking the client the following questions:
• Why do you want to accomplish this goal?
• What is the primary objective of reaching this goal?
• Will meeting this goal provide you with what you’re looking for?
FOR EXAMPLE:
Consuming 5 serves of vegetables per day is realistic for an average individual. However, setting a goal to lose 10kg in 2 weeks is not as realistic. The goal must be achievable without causing harm. A personal goal should be relevant and realistic to avoid disappointment and unnecessary setbacks.
It is natural for clients to procrastinate when there is no deadline set. If the client’s goal is to lose 10kg, they need to decide on a suitable time frame - whether that will be achieved in 12 weeks or 6 months. Clients need to be set up for success by being encouraged to create achievable time-bound goals.
If deadlines are not set, some goals may never be achieved, which can be disheartening for the client. By providing a timeframe of when to accomplish goals, the client will be more likely to increase their motivation to meet them.
As a nutrition coach, keeping the timeline realistic and flexible is important to keep the clients’ morale high. Being too strict on the timely aspect of goal setting can sometimes have adverse effects on clients and cause unwanted stress.
ANATOMICAL POSITION
ANTERIOR
POSTERIOR
SUPERIOR
INFERIOR
PROXIMAL
DISTAL
LATERAL
MEDIAL
SUPERFICIAL
DEEP
CRANIAL
CAUDAL
VENTRAL
DORSAL
The position with the body standing erect, feet together, with the arms at the side, the palms forwards, and thumbs facing outwards.
Towards the ‘front’ of the body.
Towards the ‘back’ of the body.
The part is above another or closer to the head (cranial).
The part is below another or towards the feet (caudal).
Used to describe a part that is closer to the trunk of the body or closer to another specified point of reference than another part (the elbow is proximal to the wrist).
Used to describe a part that is farther from the trunk or farther from another specified point of reference than another part (fingers are distal to the wrist).
Towards the side with respect to the imaginary midline dividing the body into equal right and left sides (the ears are lateral to the eyes).
Relates to the imaginary midline dividing the body into equal right and left halves (the nose is medial to the eyes).
Situated near the surface.
Used to describe parts that are more internal.
Synonym of ‘superior’ - meaning at, or near, the head or superior of the body.
Synonym of ‘posterior’ - meaning at, or near, the tail or posterior of the body.
Used to describe the underside or abdominals of the body.
Used to describe the upper side or back of the body.
ATOM
ABDUCTION
ADDUCTION
AFFERENT
ANTIDIURETIC
BOLUS
Atoms are the smallest stable unit of any matter - from air, to food, to humans.
Refers to the movement of a limb away from the midline (or other specified location) of the body.
The opposite of abduction, adduction is the movement of a limb towards the midline (or other specified location) of the body.
Can refer to blood vessels or neurons ‘arriving’ at the heart, spinal cord, or other organ.
A substance that suppresses urination to help control the body’s fluid balance.
The name given to ingested food which has been mechanically broken down by the teeth.
CATABOLISM Refers to the breakdown of large particles into smaller particles.
CEREBROSPINAL FLUID (CSF)
CHOLESTEROL
CHROMOSOMES
The fluid which surrounds the brain and spinal cord for protection and transportation of nutrients.
A type of fat that is found in, and essential for, all animal cells. It is made by the body, so does not need to be consumed in the diet.
Are tightly packed bundles of DNA located within the nucleus of every cell. Humans have 23 pairs of chromosomes.
CIRCADIAN RHYTHM The body’s internal pattern which cycles sleepiness and awakeness within a 24hr period, and signals when it is night and day.
COAGULATION
Usually refers to the clotting of blood; however can also mean the changing of a liquid to a solid or semi-solid state.
CORPUSCLE Can refer to a single cell, or to a small multicellular body with a distinct purpose.
CRANIAL MENINGES The three membranous layers which encase the brain and spinal cord.
CYTOLOGY The study of cells.
DEOXYGENATED
DIPLOID
EFFERENT
ELECTROLYTE
ENZYMES
Free of oxygen. This term is usually used to describe blood once it has delivered oxygen to various sites - it is now deoxygenated and needs to return to the heart, to be pumped to the lungs to receive more oxygen.
These cells contain two sets of chromosomes - one from the mother and one from the father. Refers to all body cells other than gametes.
Can refer to blood vessels or neurons ‘exiting’ the heart, spinal cord, or other organ.
Are minerals which enter the plasma of the blood and are essential for regulation of the body’s fluids.
ENZYMES
EQUILIBRIUM
EXOCRINE GLANDS
Are biological molecules which either speed up the rate of chemical reactions, or are used to bring about certain chemical reactions.
A state of equilibrium exists when two opposing forces are in balance with one another.
Are all glands which secrete substances onto the surface of epithelial tissue.
EXTENSION To stretch or lengthen or extend a limb, away from the body.
FISSURES
A narrow and long opening, caused by cracking or splitting.
FLEXION To bend a limb towards the body.
GAMETES
GLUCONEOGENESIS
HAPLOID
HAEMATOLOGICAL
HOMEOSTASIS
INSULIN
IONS
The term given to mature haploid sex-cells which are used to reproduce.
The term given to the process in which the kidneys and liver use stored glycogen to create ready-to-use glucose.
These cells are only gametes, and they contain only one pair of chromosomes, either from the mother or the father. When they join another gamete during reproduction to form a zygote, they create a diploid cell.
Haematology refers to the study of blood - its processes, regulations, diseases, etc.
Is the internal regulation of the physiological characteristics and properties of the body to maintain the optimal internal environment.
A hormone produced by the pancreas which regulates the amount of glucose in the bloodstream.
Atoms with an electric charge, due to the loss or gain of electrons (which hold a negative charge).
LOCOMOTION Is simply the movement of an organism from one location to another.
MACRONUTRIENTS
MEIOSIS
MICTURITION
MITOSIS
NEURON
ORGANELLES
Refers to carbohydrates, fats, and proteins, which need to be consumed in larger amounts than micronutrients (vitamins and minerals).
The process of cell division specifically for gametes, which involves two successive divisions.
The controlled reflex otherwise known as urination.
The process of cell division specifically for somatic cells, which only involves one division.
The name given to cells in the nervous system which are used to transmit nerve impulses, allowing the sending of various messages.
The name given to the components inside a cell which hold specialised roles and functions (i.e. the nucleus).
ORGANISM An individual plant or animal; a living thing; a life form.
OSMOLARITY
Takes into consideration the solutes/particles within a fluid to determine its concentration.
OXYGENATED Contains, or is holding, oxygen.
PATHOGENS
Refers to a micro-organism which can cause disease or illness, such as bacteria or another form of virus.
OSMOLARITY
Takes into consideration the solutes/particles within a fluid to determine its concentration.
OXYGENATED Contains, or is holding, oxygen.
PATHOGENS
PERIPHERAL
PERISTALSIS
RECEPTORS
SENSORY
SOLUBLE
SOMATIC
STIMULI
SYNERGY/ SYNERGISTIC
Refers to a micro-organism which can cause disease or illness, such as bacteria or another form of virus.
Refers to anything that is situated on the edge of something else.
The name given to the type of contracting movement found in the oesophagus and the intestine.
A specialised area on a cell which receives neurotransmitters, hormones, or other substances as a binding site to facilitate communication.
Refers to information received from the sensors.
Able to be dissolved in any or a specific solution.
Refers to all cells within the human body other than gametes.
Refers to a change in either the internal or external environment which is detectable and elicits a response from physiological components.
The ability for various systems, organs, processes, etc. to work together to achieve a common goal.
SYNTHESIS To produce, create, make.
THERMOREGULATION
THORACIC CAVITY
TRIGLYCERIDES
VASOCONSTRICTION
VASODILATION
VISCERAL
ZYGOTE
An aspect of homeostasis, thermoregulation refers to the internal regulation of the body’s temperature.
Another term for chest cavity - the division of the body which houses the heart, lungs, and diaphragm.
A type of fat found in foods - particularly natural fats and oils.
The narrowing of blood vessels in response to a change in environment, and a method through which the body maintains homeostasis.
The widening of blood vessels in response to a change in environment, and a method through which the body maintains homeostasis.
Refers to internal organs usually located either in the chest or abdomen; although the brain is also referred to as a visceral organ.
A fertilised ovum, or diploid cell, occurring through the joining of two haploid gametes.
1. Tortora GJ, Derrickson B. Principles of Anatomy & Physiology. Thirteenth. John Wiley & Sons, Inc.; 2012.
2. Kross B. Questions and Answers - How many atoms are in the human body? [Internet]. JLab Science Education. 2022 [cited 2022 Sep 7]. Available from: https://education.jlab.org/qa/mathatom_04.html
3. Queensland Health. Brain Map Frontal Lobes | Queensland Health [Internet]. Queensland Government. 2022 [cited 2022 Sep 7]. Available from: https://www.health.qld.gov.au/abios/asp/bfrontal
4. Berthoud HR. Synergy: A Concept in Search of a Definition. Endocrinology [Internet]. 2013 Nov 1 [cited 2022 Sep 14];154(11):3974–7. Available from: https://academic.oup.com/endo/ article/154/11/3974/2422558
5. Geary N. Understanding synergy. Am J Physiol - Endocrinol Metab [Internet]. 2013 Feb 1 [cited 2022 Sep 14];304(3):237–53. Available from: https://journals.physiology.org/doi/10.1152/ajpendo.00308.2012
6. Sensoy I. A review on the food digestion in the digestive tract and the used in vitro models. Curr Res Food Sci. 2021 Jan 1;4:308–19.
7. Gropper SS, Smith JL, Carr TP. Advanced Nutrition and Human Metabolism. Seventh. Boston. USA: Cengage Learning; 2018.
8. Geary N. Understanding synergy. Am J Physiol - Endocrinol Metab. 2013 Feb;304(3):237–53.
9. The Heart Foundation. What is cardiac arrest | The Heart Foundation [Internet]. The Heart Foundation. 2022 [cited 2022 Sep 7]. Available from: https://www.heartfoundation.org.au/bundles/your-heart/ cardiac-arrest
10. The Heart Foundation. What is angina | Heart Foundation [Internet]. The Heart Foundation. 2020 [cited 2022 Sep 8]. Available from: https://www.heartfoundation.org.au/bundles/your-heart/angina
11. Healthdirect Australia. Cardiomyopathy [Internet]. Healthdirect Australia. Healthdirect Australia; 2021 [cited 2022 Sep 8]. Available from: https://www.healthdirect.gov.au/cardiomyopathy
12. Aggarwal M, Bozkurt B, Panjrath G, Aggarwal B, Ostfeld RJ, Barnard ND, et al. Lifestyle Modifications for Preventing and Treating Heart Failure. J Am Coll Cardiol. 2018 Nov 6;72(19):2391–405.
13. Widysanto A, Mathew G. Chronic Bronchitis. Adjuv Med Care [Internet]. 2022 Jul 12 [cited 2022 Sep 8];39–41. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482437/
14. Singh A, Avula A, Zahn E. Acute Bronchitis. StatPearls [Internet]. 2022 May 8 [cited 2022 Sep 8]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK448067/
15. National Asthma Council Australia. What is asthma? - National Asthma Council Australia [Internet]. National Asthma Council Australia. 2022 [cited 2022 Sep 8]. Available from: https://www. nationalasthma.org.au/understanding-asthma/what-is-asthma
16. NIH National Library of Medicine. Muscular Dystrophy | MD | MedlinePlus [Internet]. NIH National Library of Medicine. 2016 [cited 2022 Sep 8]. Available from: https://medlineplus.gov/musculardystrophy. html#summary
17. Bass E. Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork [Internet]. 2012 Mar [cited 2022 Sep 8];5(1):14. Available from: /pmc/articles/ PMC3312643/
18. Bass E. Tendinopathy: Why the Difference Between Tendinitis and Tendinosis Matters. Int J Ther Massage Bodywork. 2012 Mar;5(1):14.
19. Healthdirect Australia. Myasthenia gravis [Internet]. Healthdirect Australia. Healthdirect Australia; 2022 [cited 2022 Sep 8]. Available from: https://www.healthdirect.gov.au/myasthenia-gravis
20. Dentalcare. Divisions and Components of the Teeth - An Overview of Dental Anatomy - Dentalcare [Internet]. Dentalcare.com. 2022 [cited 2022 Sep 12]. Available from: https://www.dentalcare.com/enus/ce-courses/ce500/divisions-and-components-of-the-teeth
21. Dentalcare. Divisions and Components of the Teeth - An Overview of Dental Anatomy - Dentalcare. Dentalcare.com. 2022.
22. Yamamoto T, Hasegawa T, Yamamoto T, Hongo H, Amizuka N. Histology of human cementum: Its structure, function, and development. Jpn Dent Sci Rev [Internet]. 2016 Aug 1 [cited 2022 Sep 5];52(3):63. Available from: /pmc/articles/PMC5390338/
23. The Teeth of Herbivores, Carnivores and Omnivores [Internet]. [cited 2022 Sep 15]. Available from: https://www.miamicosmeticdentalcare.com/teeth-herbivores-carnivores-omnivores/
24. Mayo Clinic. Gingivitis - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 13]. Available from: https://www.mayoclinic.org/diseases-conditions/gingivitis/symptoms-causes/ syc-20354453
25. Australia H. Halitosis. Heal Aust [Internet]. 2022 [cited 2022 Sep 13]; Available from: https://www. healthdirect.gov.au/halitosis
26. Yadav K, Prakash S. (PDF) Dental Caries: A Review. Asian J Biomed Pharm Sci [Internet]. 2016 [cited 2022 Sep 14]; Available from: https://www.researchgate.net/publication/306394930_Dental_ Caries_A_Review
27. Mendez MF. Early-Onset Alzheimer’s Disease. Neurol Clin [Internet]. 2017 May 1 [cited 2022 Sep 14];35(2):263. Available from: /pmc/articles/PMC5407192/
28. Walker BR, Colledge NR, Ralston SH, Penman ID. Davidson’s Principlers & Practice of Medicine. 22nd ed. Churchill Livingstone, Elsevier; 2014.
29. Epilepsy Action Australia. Understanding Epilepsy | Epilepsy Action Australia [Internet]. Epilepsy Action Australia. 2022 [cited 2022 Sep 8]. Available from: https://www.epilepsy.org.au/about-epilepsy/ understanding-epilepsy/
30. Healthdirect Australia. Parkinson’s disease [Internet]. Healthdirect Australia. Healthdirect Australia; 2022 [cited 2022 Sep 8]. Available from: https://www.healthdirect.gov.au/parkinsons-disease
31. Stroke Foundation Australia. What is a stroke? | Stroke Foundation - Australia [Internet]. Stroke Foundation Australia. 2022 [cited 2022 Sep 8]. Available from: https://strokefoundation.org.au/aboutstroke/learn/what-is-a-stroke
32. Mayo Clinic. Hypothyroidism - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 12]. Available from: https://www.mayoclinic.org/diseases-conditions/hypothyroidism/ symptoms-causes/syc-20350284
33. Better Health Channel. Thyroid - hyperthyroidism - Better Health Channel [Internet]. Better Health Channel. 2021 [cited 2022 Sep 12]. Available from: https://www.betterhealth.vic.gov.au/health/ conditionsandtreatments/thyroid-hyperthyroidism
34. Crowley L V. An Introduction to Human Disease: Pathology and Pathophysiology. 9th ed. Learning, Jones & Bartlett; 2013.
35. Healthdirect Australia. Gallstones. Heal Aust [Internet]. 2021 [cited 2022 Sep 12]; Available from: https:// www.healthdirect.gov.au/gallstones
36. Mayo Clinic. Gastrointestinal bleeding - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 12]. Available from: https://www.mayoclinic.org/diseases-conditions/ gastrointestinal-bleeding/symptoms-causes/syc-20372729
37. Healthdirect Australia. Cystitis [Internet]. Healthdirect Australia. Healthdirect Australia; 2020 [cited 2022 Sep 12]. Available from: https://www.healthdirect.gov.au/cystitis
38. Mayo Clinic. Kidney infection - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 12]. Available from: https://www.mayoclinic.org/diseases-conditions/kidney-infection/ symptoms-causes/syc-20353387
39. Plus M. Kidney Stones | Kidney Stone Symptoms | Nephrolithiasis | MedlinePlus [Internet]. Medline Plus. 2022 [cited 2022 Sep 12]. Available from: https://medlineplus.gov/kidneystones.html
40. Cancer Council. Vitamin D | Cancer Council [Internet]. Cancer Council. 2022 [cited 2022 Sep 12]. Available from: https://www.cancer.org.au/cancer-information/causes-and-prevention/sun-safety/vitamin-d
41. Healthdirect Australia. Acne [Internet]. Healthdirect Australia Australia. Healthdirect Australia; 2021 [cited 2022 Sep 12]. Available from: https://www.healthdirect.gov.au/acne
42. Better health Channel. Eczema (atopic dermatitis) - Better Health Channel [Internet]. Better Health Channel. 2021 [cited 2022 Sep 12]. Available from: https://www.betterhealth.vic.gov.au/health/ conditionsandtreatments/eczema-atopic-dermatitis
43. Better health Channel. Eczema (atopic dermatitis) - Better Health Channel. Better Health Channel. 2021.
44. Cancer Council. Skin cancer | Causes, Symptoms & Treatments | Cancer Council [Internet]. Cancer Council. 2021 [cited 2022 Sep 12]. Available from: https://www.cancer.org.au/cancer-information/typesof-cancer/skin-cancer
45. Mayo Clinic. Endometriosis - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 12]. Available from: https://www.mayoclinic.org/diseases-conditions/endometriosis/ symptoms-causes/syc-20354656
46. Centers for Disease Control and Prevention. Common Reproductive Health Concerns for Women | Reproductive Health | CDC [Internet]. Centers for Disease Control and Prevention. 2018 [cited 2022 Sep 12]. Available from: https://www.cdc.gov/reproductivehealth/womensrh/healthconcerns.html
47. Prostate Cancer Foundation Australia. Understanding prostate cancer | PCFA | PCFA [Internet]. Prostate Cancer Foundation Australia. 2017 [cited 2022 Sep 12]. Available from: https://www.pcfa.org.au/ awareness/what-you-need-to-know-about-prostate-cancer/
48. Australia H. Glandular fever [Internet]. Healthdirect Australia. Healthdirect Australia; 2022 [cited 2022 Sep 12]. Available from: https://www.healthdirect.gov.au/glandular-fever
49. Australia H. Tonsillitis [Internet]. Healthdirect Australia. Healthdirect Australia; 2021 [cited 2022 Sep 12]. Available from: https://www.healthdirect.gov.au/tonsillitis
50. Mayo Clinic. Crohn’s disease - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 12]. Available from: https://www.mayoclinic.org/diseases-conditions/crohns-disease/ symptoms-causes/syc-20353304
51. Manrique OJ, Bustos SS, Ciudad P, Adabi K, Chen WF, Forte AJ, et al. Overview of Lymphedema for Physicians and Other Clinicians: A Review of Fundamental Concepts. Mayo Clin Proc [Internet]. 2020 [cited 2022 Sep 12]; Available from: https://www.mayoclinic.org/diseases-conditions/lymphedema/ symptoms-causes/syc-20374682
52. Mayo Clicic. Lymphedema - Symptoms and causes - Mayo Clinic [Internet]. Mayo Clinic. 2022 [cited 2022 Sep 12]. Available from: https://www.mayoclinic.org/diseases-conditions/lymphedema/ symptoms-causes/syc-20374682
53. NIH. Calcium and Vitamin D: Important at Every Age | NIH Osteoporosis and Related Bone Diseases National Resource Center [Internet]. NIH Osteoporosis and Related Bone Diseases National Resource Center. 2018 [cited 2022 Sep 12]. Available from: https://www.bones.nih.gov/health-info/bone/bonehealth/nutrition/calcium-and-vitamin-d-important-every-age
54. Guo W, Nazim H, Liang Z, Yang D. Magnesium deficiency in plants: An urgent problem. Crop J. 2016 Apr 1;4(2):83–91.
55. Better Health Channel. Vitamins and minerals - Better Health Channel [Internet]. Better Health Channel. 2020 [cited 2022 Sep 12]. Available from: https://www.betterhealth.vic.gov.au/health/healthyliving/ Vitamins-and-minerals#vitamin-c-deficiency-and-scurvy
56. NIH National Cancer Institute. Definition of dysplasia - NCI Dictionary of Cancer Terms - NCI [Internet]. NIH national Cancer Institute. 2022 [cited 2022 Sep 12]. Available from: https://www.cancer.gov/ publications/dictionaries/cancer-terms/def/dysplasia
57. Shin SM, Kim YI, Choi YS, Yamaguchi T, Maki K, Cho BH, et al. The skeletal maturation status estimated by statistical shape analysis: axial images of Japanese cervical vertebra. Dentomaxillofacial Radiol [Internet]. 2015 Mar 1 [cited 2022 Sep 12];44(3). Available from: /pmc/articles/PMC4614167/
58. Scitable by Nature Education. Replication and Distribution of DNA during Mitosis | Learn Science at Scitable [Internet]. Nature Education. 2014 [cited 2022 Sep 12]. Available from: https://www.nature. com/scitable/topicpage/replication-and-distribution-of-dna-during-mitosis-6524841/
59. Jeukendrup A, Gleeson M. Sport Nutrition. Third edit. Human Kinetics Publishers Inc.; 2019.
60. Beck KL, Thomson JS, Swift RJ, Hurst PR von. Role of nutrition in performance enhancement and postexercise recovery. Open Access J Sport Med [Internet]. 2015 Aug [cited 2022 Jun 15];6:259. Available from: /pmc/articles/PMC4540168/
61. Riebl SK, Davy BM. The Hydration Equation: Update on Water Balance and Cognitive Performance. ACSMs Health Fit J [Internet]. 2013 Nov [cited 2022 Jun 21];17(6):21. Available from: /pmc/articles/ PMC4207053/
62. Young HA, Cousins A, Johnston S, Fletcher JM, Benton D. Autonomic adaptations mediate the effect of hydration on brain functioning and mood: Evidence from two randomized controlled trials. Sci Reports 2019 91 [Internet]. 2019 Nov 11 [cited 2022 Jun 21];9(1):1–13. Available from: https://www.nature.com/ articles/s41598-019-52775-5
63. Institute of Medicine. Krause’ s Food & the Nutrition Care Process. Food and Nutrition Board, Institute of Medicine, National Academies. 2017.
64. Popkin BM, D’Anci KE, Rosenberg IH. Water, hydration, and health. Nutr Rev [Internet]. 2010 [cited 2021 Mar 30];68(8):439–58. Available from: /pmc/articles/PMC2908954/
65. Medline Plus. Respiratory acidosis: MedlinePlus Medical Encyclopedia [Internet]. NIH National Library of Medicine. 2022 [cited 2022 Sep 12]. Available from: https://medlineplus.gov/ency/article/000092.htm
66. Medline Plus. Metabolic acidosis: MedlinePlus Medical Encyclopedia [Internet]. NIH National Library of Medicine. 2022 [cited 2022 Sep 12]. Available from: https://medlineplus.gov/ency/article/000335.htm
67. MacLaren D, Morton J. Biochemistry for Sport and Exercise Metabolism. First edit. West Sussex, UK: Wiley-Blackwell; 2012.
68. Manual M. Alkalosis - Hormonal and Metabolic Disorders - MSD Manual Consumer Version [Internet]. MDS Manual. 2021 [cited 2022 Sep 12]. Available from: https://www.msdmanuals.com/en-au/home/ hormonal-and-metabolic-disorders/acid-base-balance/alkalosis
69. Hopkins E, Sanvictores T, Sharma S. Physiology, Acid Base Balance. Urolithiasis [Internet]. 2021 Sep 14 [cited 2022 Jul 27];19–22. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507807/
70. World Health Organisation. Frequently asked questions [Internet]. World Health Organisation. 2022 [cited 2022 Sep 12]. Available from: https://www.who.int/about/frequently-asked-questions
71. Better Health Channel. Genetic conditions - Better Health Channel [Internet]. Better Health Channel. 2021 [cited 2022 Sep 12]. Available from: https://www.betterhealth.vic.gov.au/health/ conditionsandtreatments/genetic-conditions
72. National Human Genome Research Institute. Genetic Disorders [Internet]. NIH. 2018 [cited 2022 Sep 6]. Available from: https://www.genome.gov/For-Patients-and-Families/Genetic-Disorders
73. Better Health Channel. Genetic conditions - Better Health Channel. Better Health Channel. 2021.
74. Stoppler MC. 18 Common Genetic Disorders: 4 Types, Symptoms, Causes & Human Genome [Internet]. MedicineNet. 2022 [cited 2022 Sep 12]. Available from: https://www.medicinenet.com/genetic_disease/ article.htm#what_is_a_genetic_disease_how_is_it_defined
75. Stoppler MC. 18 Common Genetic Disorders: 4 Types, Symptoms, Causes & Human Genome. MedicineNet. 2022.
76. Ng YS, Turnbull DM. Mitochondrial disease: genetics and management. J Neurol [Internet]. 2016 Jan 1 [cited 2022 Sep 12];263(1):179. Available from: /pmc/articles/PMC4723631/
77. Ng YS, Turnbull DM. Mitochondrial disease: genetics and management. J Neurol. 2016 Jan;263(1):179.
78. Webb P, Bain C, Page A. Essential Epidemiology. 3rd ed. Press CU, editor. 2017.
79. Remoundou K, Koundouri P. Environmental Effects on Public Health: An Economic Perspective. Int J Environ Res Public Health [Internet]. 2009 [cited 2022 Sep 12];6(8):2160. Available from: /pmc/articles/ PMC2738880/
80. NIH National Institute of Environmental Health Sciences. Conditions & Diseases [Internet]. NIH National Institute of Environmental Health Sciences. 2022 [cited 2022 Sep 12]. Available from: https://www.niehs. nih.gov/health/topics/conditions/index.cfm
81. Australian Government Department of Health and Aged Care. Overview of Environmental Health. Australian Government Department of Health and Aged Care. Australian Government Department of Health; 2022.
82. NIH National Institute of General Medical Science. Physical Trauma [Internet]. NIH National Institute of General Medical Science. 2022 [cited 2022 Sep 12]. Available from: https://www.nigms.nih.gov/ education/fact-sheets/Pages/physical-trauma.aspx
83. NIH National Institute of General Medical Science. Physical Trauma. NIH National Institute of General Medical Science. 2022.
84. Healthdirect Australia. Cellulitis [Internet]. Healthdirect Australia. Healthdirect Australia; 2020 [cited 2022 Sep 12]. Available from: https://www.healthdirect.gov.au/cellulitis
85. NIH National Institute of General Medical Science. Burns [Internet]. NIH National Institute of General Medical Science. 2022 [cited 2022 Sep 12]. Available from: https://www.nigms.nih.gov/education/factsheets/Pages/burns.aspx
86. Better Health Channel. Blood pressure - Better Health Channel [Internet]. Better Health Channel. 2021 [cited 2022 Sep 12]. Available from: https://www.betterhealth.vic.gov.au/health/ conditionsandtreatments/blood-pressure
87. Better Health Channel. Blood pressure - Better Health Channel. Better Health Channel. 2021.
88. Censin JC, Peters SAE, Bovijn J, Ferreira T, Pulit SL, Mägi R, et al. Causal relationships between obesity and the leading causes of death in women and men. PLOS Genet [Internet]. 2019 [cited 2022 Aug 25];15(10):e1008405. Available from: https://journals.plos.org/plosgenetics/article?id=10.1371/journal. pgen.1008405
89. Lizcano F. The beige adipocyte as a therapy for metabolic diseases. Int J Mol Sci [Internet]. 2019 Oct 2 [cited 2021 Jun 3];20(20). Available from: /pmc/articles/PMC6834159/
90. Chait A, den Hartigh LJ. Adipose Tissue Distribution, Inflammation and Its Metabolic Consequences, Including Diabetes and Cardiovascular Disease. Front Cardiovasc Med [Internet]. 2020 Feb 25 [cited 2021 Jun 14];7:22. Available from: /pmc/articles/PMC7052117/
91. Zoico E, Rubele S, De Caro A, Nori N, Mazzali G, Fantin F, et al. Brown and beige adipose tissue and aging. Front Endocrinol (Lausanne) [Internet]. 2019 Jun 20 [cited 2021 Jun 3];10(JUN):368. Available from: www.frontiersin.org
92. Kiefer FW. The significance of beige and brown fat in humans. Endocr Connect [Internet]. 2017 Jul 1 [cited 2021 Jun 15];6(5):R70–9. Available from: /pmc/articles/PMC5510441/
93. Meerman R, Brown AJ. When somebody loses weight, where does the fat go? BMJ [Internet]. 2014 Dec 16 [cited 2022 Apr 13];349. Available from: https://www.bmj.com/content/349/bmj.g7257
94. El-Zayat SR, Sibaii H, El-Shamy KA. Physiological process of fat loss. Bull Natl Res Cent 2019 431 [Internet]. 2019 Dec 30 [cited 2022 Apr 13];43(1):1–15. Available from: https://bnrc.springeropen.com/ articles/10.1186/s42269-019-0238-z
95. Dietitians Australia. What to expect | Dietitians Australia [Internet]. Dietitians Australia. 2022 [cited 2022 Sep 7]. Available from: https://dietitiansaustralia.org.au/seeing-dietitian/what-expect
96. Australia SD. Our Members - Sports Dietitians Australia (SDA) [Internet]. Dietitians Australia. 2022 [cited 2022 Sep 7]. Available from: https://www.sportsdietitians.com.au/our-members/
97. Victoria BH. General practitioner services [Internet]. 2018 [cited 2022 Jul 15]. Available from: https:// www.betterhealth.vic.gov.au/health/serviceprofiles/General-practitioner-services
98. Australian Government Department of Health and Aged Care. Physical activity and exercise guidelines for all Australians | Australian Government Department of Health and Aged Care [Internet]. Department of Health and Aged Care. 2021 [cited 2022 Sep 7]. Available from: https://www.health.gov.au/ health-topics/physical-activity-and-exercise/physical-activity-and-exercise-guidelines-for-allaustralians?utm_source=health.gov.au&utm_medium=callout-auto-custom&utm_campaign=digital_ transformation
99. Utkualp N, Ercan I. Anthropometric measurements usage in medical sciences. Biomed Res Int [Internet]. 2015 [cited 2021 Jun 14];2015. Available from: /pmc/articles/PMC4564618/
100. World Health Organisation. A healthy lifestyle - WHO recommendations [Internet]. World Health Organisation Fact Sheet. 2010 [cited 2022 Sep 7]. Available from: https://www.who.int/europe/newsroom/fact-sheets/item/a-healthy-lifestyle---who-recommendations
101. Better Health Channel. Obesity - Better Health Channel [Internet]. Better Health Channel. 2022 [cited 2022 Sep 12]. Available from: https://www.betterhealth.vic.gov.au/health/healthyliving/obesity