

UNIT INTRODUCTION
Welcome to the unit Assist in Establishing Positive Digestive Health. This unit outlines the body systems related to food and digestion. This unit provides nutrition coaches with detailed knowledge regarding digestive health and its impact on general health and overall well-being. It provides the ability to advise clients on positive digestive health behaviours and recognise when a client may have digestive issues.
This unit outlines precisely why having a thorough understanding of digestive health is essential for the successful practice of nutrition coaches, as well as what it looks like when everything in the digestive system is working as it should. This unit reviews the human body systems to provide context to the information in the remainder of the unit.
The unit then begins to explain the various parts of the digestive system and their corresponding roles within the body before explaining the physiology of the digestive system. The unit then dives into the various components of the digestive system that all play a very significant role in ensuring its health. For example, nutrition coaches will thoroughly understand pH levels, bowel transit times, healthy gut flora and the impacts of diet on bacterial diversity, and many other influences. Nutrition coaches will also understand how the digestive system works in conjunction with other systems of the body and how these systems contribute to the effective functioning of the digestive system.
Digestive health influences an individual’s overall health, so acquiring a deeper understanding of this body system will give the nutrition coach an advantage in understanding the different signs and symptoms of digestive health. Further, nutrition coaches will also learn what factors negatively impact the digestive system and which health concerns or conditions can arise from ongoing mistreatment or inadequate nutrient intake. Nutrition coaches will gain the skills and knowledge required to recognise when a client may need a referral to other allied health professionals and how to do so appropriately.
This unit is intended for those nutrition coaches who are required to advise clients on positive health and nutrition behaviours, diets, and lifestyle following national guidelines as part of broader nutritional support services.
This unit does not provide nutrition coaches with the required skills or knowledge to work with:
• Individuals suffering from chronic health conditions
• People with medical conditions requiring specialised dietary advice
• Frail older adults who are at risk of malnutrition
• Infants and toddlers
• Pregnant or breastfeeding women.
Suppose a nutrition coach is faced with any of the abovementioned population groups. In that case, they must work collaboratively with allied health professionals by referring clients that fall outside their scope of practice to ensure that both the client and the nutrition coach are safe-guarded should any issues arise.
This unit will allow a nutrition coach to:
• Obtain a thorough understanding of the importance of adequate nutrition for digestive health
• Research and evaluate sources of information regarding digestive health theory and dietary trends
• Advise clients on the functions and importance of the digestive system in overall health
• Recognise factors contributing to digestive health and how to appropriately support the client or refer to other allied health professionals.
UNDERSTANDING THE IMPORTANCE OF THE DIGESTIVE SYSTEM
UNDERSTANDING DIGESTION
Earlier units in this course explored the body’s key systems and their role in overall health. However, the digestive system is responsible for breaking down and absorbing nutrients within the body; therefore, a nutrition coach must have a detailed understanding of the digestive system.
All living organisms require nutrients from their environment to sustain life. Food is the body’s fuel source and comprises various nutrients, such as vitamins and minerals. The digestive system breaks down food and drinks that are consumed into smaller molecules which the body can then utilise for many purposes, such as:(1)
• Energy production
• Repair of tissues
• Growth (especially through childhood/adolescence)
• Immune function.
Without adequate nutrition, many of these functions would be impaired, resulting in a lack of energy, slow healing, reduced growth potential, and poor immunity.
Inadequate nutrition does not simply mean not eating enough, as it can also include:
• Overeating energy requirements
• Overeating unnecessary nutrients (like sugar or trans-fat)
• Undereating required micronutrients (vitamins and minerals)
• Undereating protein.
Poor or improper nutrition can have negative impacts on the digestive system, including:(1)
• Dehydration
• Constipation
• Malabsorption
• Inflammation
• Pancreatitis
• Indigestion
• Acid reflux
• Increased hunger.
RELEVANCE AS A NUTRITION COACH

Given the importance of the digestive system through any type of nutrition intervention, it is abundantly clear that nutrition coaches need to maintain a clear and sound understanding of this system. When any type of nutrition is consumed, the way the body handles this nutrition is directly related to the digestive system.
The digestive system is also interrelated with various other systems, such as the nervous system, and the food an individual consumes directly impacts the effectiveness of these systems. Therefore, a nutrition coach requires substantial knowledge of the digestive system, not only for their understanding but also to assist with educating clients. The ability to communicate effectively with clients and educate them about the importance of the digestive system - or, more specifically, the consequences or benefits of how a client treats their digestive system - will be beneficial in practice.
RECOGNISING THE BENEFITS OF A HEALTHY DIGESTIVE SYSTEM
The health of an individual’s digestive system will directly affect overall health and well-being. The individual will encounter several health benefits when the digestive system functions effectively. These benefits can be obvious or subtle depending on prior dietary habits. A nutrition coach can assist clients in restoring and maintaining a healthy functioning digestive system by encouraging and assisting them in adopting healthier dietary habits.
A digestive system that is not functioning optimally may result in poor nutrient absorption and utilisation and irregular digestion periods (maybe too fast and thus not allow adequate time for absorption, or too slow, which may result in constipation or faecal impaction).
There are many benefits to maintaining a healthy digestive system, including:(1)
• Toxin elimination
• Energy and stamina
• Immunity
• Hormone regulation.

TOXIN ELIMINATION
A healthy digestive system optimises the body’s processes for eliminating toxins, which can considerably improve general feelings of health and well-being. The body excretes toxins via various processes such as urination, breathing, mucus, tears, sweat and bowel movements. Despite these processes occurring regularly, a poor diet can lead to challenges for the body in identifying and removing these toxins, resulting in a build-up of toxins that may lead to health complications.(1)
As a simple example, a low fibre diet can lead to an accumulation of faecal matter in various parts of the intestine, which would block the absorption of fluids and nutrients and potentially lead to health concerns such as diverticulosis (small bulging pockets that develop in the walls of the digestive tract). Further, if someone were to consume (in excess) a food to which they are intolerant, this could cause inflammation leading to:
• Poor digestion
• Bloating
• Headaches
• Fatigue
• Lethargy.
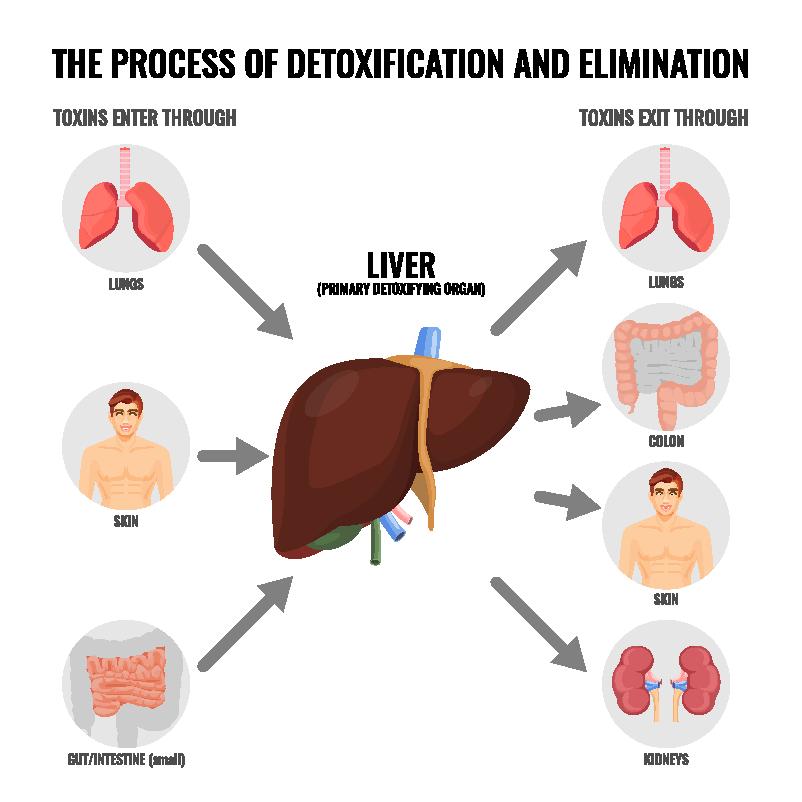
Healthy toxin elimination is often characterised or identified through regular, consistent bowel movements, which assist in removing waste products and toxins from the body regularly to optimise nutrient absorption.
ENERGY AND STAMINA
There is likely to be an increase in energy and stamina when the digestive system is functioning effectively and is fuelled by a healthy and balanced diet. There is a direct correlation between energy utilisation and the health of the digestive system; this is because the digestive system is directly responsible for the breakdown, absorption, and utilisation of nutrients, which are used to provide the body with energy.
When the digestive system is not working effectively, this will reduce energy levels as the body is not receiving the nutrients it requires through the diet. A healthy functioning digestive system, which can process and absorb nutrients, combined with toxin removal, can lead to significant gains in health and well-being and assist in improving energy levels and stamina.(2)(3)
IMMUNITY
The digestive system plays a vital role in the body’s immune system. It is understood that the greater the diversity and quantity of gut flora, the greater the immune defence. Therefore, a healthy balance of good bacteria, which assists in combating and breaking down threats to the body, is imperative in ensuring the body remains healthy and balanced.(2)
The digestive system represents up to 70 percent of the entire immune system.(4)
When the good bacteria are diminished, which can result from poor dietary intake, elevated stress levels, or consumption of alcohol, drugs or antibiotics, the immune system will suffer.
Individuals who have diminished good bacteria in their digestive system will have a decreased ability to fight off pathogens and are therefore more susceptible to illness and disease. Thus, it is essential to ensure a healthy gut microbiome and a healthy functioning digestive system to best support an individual’s immunity.
HORMONE REGULATION
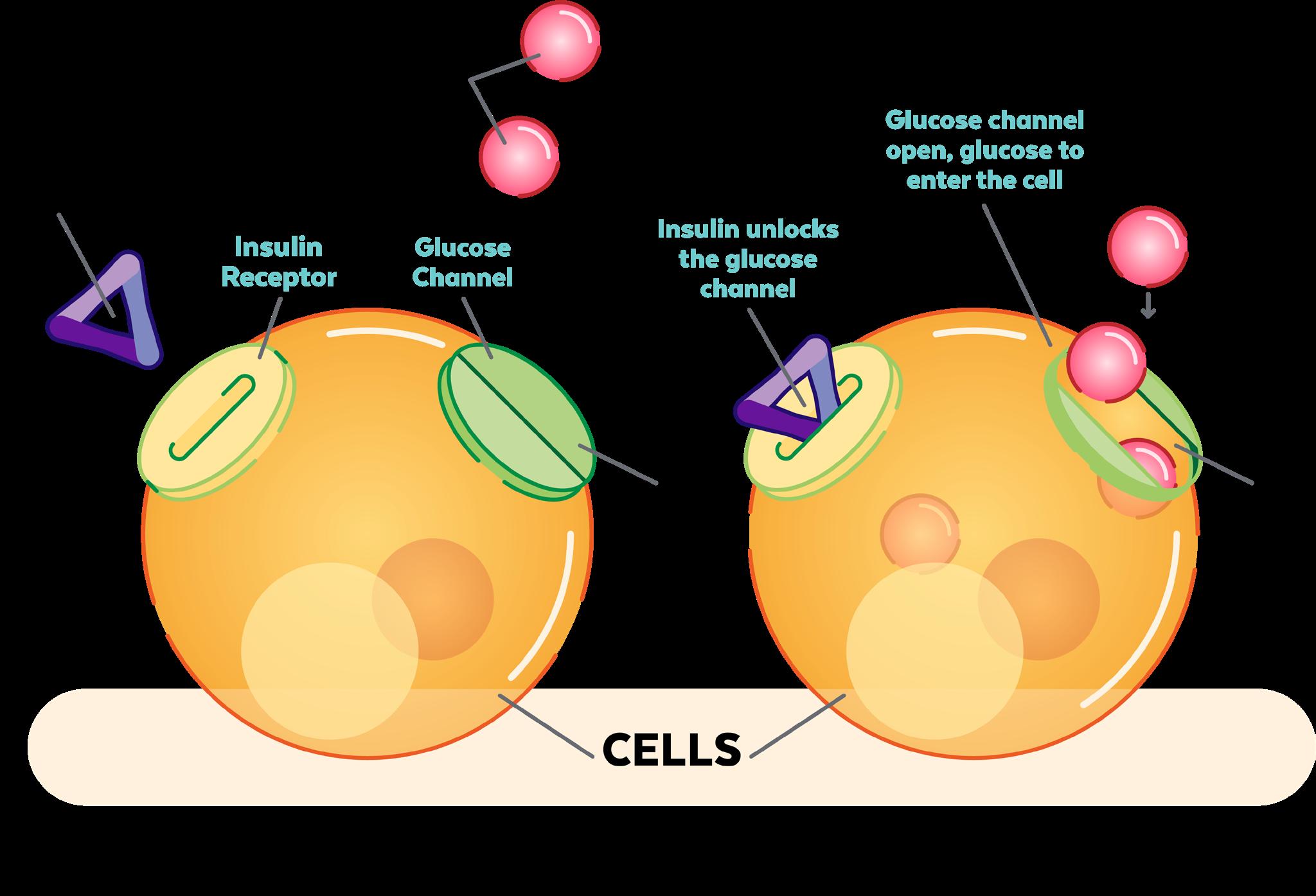
The body’s digestive system plays a significant role in controlling an individual’s mood through the production of serotonin within the gastrointestinal (GI) tract. Serotonin is a hormone that assists in controlling depression and promoting feelings of relaxation, optimism, and overall well-being. The digestive system also stimulates the release of other hormones, directly impacting the absorption or utilisation of the nutrients consumed.
For example, insulin is a hormone secreted in response to rising blood sugar levels (due to carbohydrate consumption).(2) Its role is to move the sugar from the bloodstream into cells where it is required (depicted in the image below).
UNDERSTANDING HUMAN ANATOMY AND PHYSIOLOGY (A QUICK REVIEW)
REVIEWING HUMAN BODY SYSTEMS
Before going into detail on establishing positive digestive health, it is essential as a nutrition coach to understand the body’s primary systems and their functions. Although this has been covered in previous units, revisiting, and understanding these systems provides an appreciation of the following factors: how nutrients are utilised and processed within the body, where clients may require some modification to their diet, and the ability to identify any potential health issues.
Listed in the table below is an outline of the organ systems found within the body, their primary function and the major tissues and organs within each system.(1)
ORGAN SYSTEM COMPONENTS
• Oral cavity
• Pharynx
• Oesophagus
DIGESTIVE SYSTEM
CARDIOVASCULAR SYSTEM
LYMPHATIC SYSTEM
• Stomach
• Small intestine
• Colon
• Blood vessels
• Blood
• The heart.
• Lymph nodes
• Lymph vessels
• Thyroid.
• Pituitary gland
ENDOCRINE SYSTEM
INTEGUMENTARY SYSTEM
MUSCULAR SYSTEM
• Hypothalamus
• Adrenal glands
• Hair
• Skin
• Nails.
• Cardiac muscle (the heart)
• Skeletal muscle.
• The brain
NERVOUS SYSTEM
• Spinal cord
• Nerves
Female:
• Uterus
REPRODUCTIVE SYSTEM
• Vagina
• Fallopian tubes
• Ovaries.
REPRODUCTIVE SYSTEM
• Ovaries
• Testes.
FUNCTION
Converts food into energy and nutrients to feed the body.
The cardiovascular system transports hormones, oxygen, and nutrients to cells in the body. It also moves waste and carbon dioxide away from cells.
The lymphatic system defends against infection and disease and moves lymph (fluid carried by the lymphatic system to help deliver nutrients and fight against infections) between tissues and the bloodstream.
The endocrine system produces hormones that communicate between cells.
The integumentary system helps to maintain fluid levels within the body. It also acts as a defence against infection by microorganisms and assists with temperature control.
• Smooth muscle
• Tendons.
The muscular system’s primary function is movement and heat production throughout the body.
The nervous system collects, transfers, and processes information from various external and internal stimuli.
Male:
• Penis
• Testes
• Seminal vesicles.
Produces gametes (sex cells) and sex hormones.
ORGAN SYSTEM COMPONENTS FUNCTION
• Pharynx
• Trachea
RESPIRATORY SYSTEM
SKELETAL SYSTEM
URINARY SYSTEM
• Bones
• Cartilage
• Ligaments.
• Kidneys
• Urinary bladder.
• Larynx
• Lungs.
The respiratory system delivers air to sites of the body where gas exchange can transpire between the blood and cells throughout the body, blood, and air (lungs).
The skeletal system provides structure and stability for the body and protects soft tissues. It also produces red blood cells and stores minerals.
The urinary system removes extra salts, water and waste products throughout the body. It also controls the body’s pH levels.

ORGANS IN A SYSTEM WORK IN SYNERGY
When it comes to a body system, all components of that particular body system must work together to achieve their end goal/function. Each system component is vital in achieving optimal functionality, regardless of size, energy demand or time consumption. If one part of the body system were to not function as it should, the body system would not be able to function as a whole, and problems would soon arise.(1) Mouth Salivary
glands

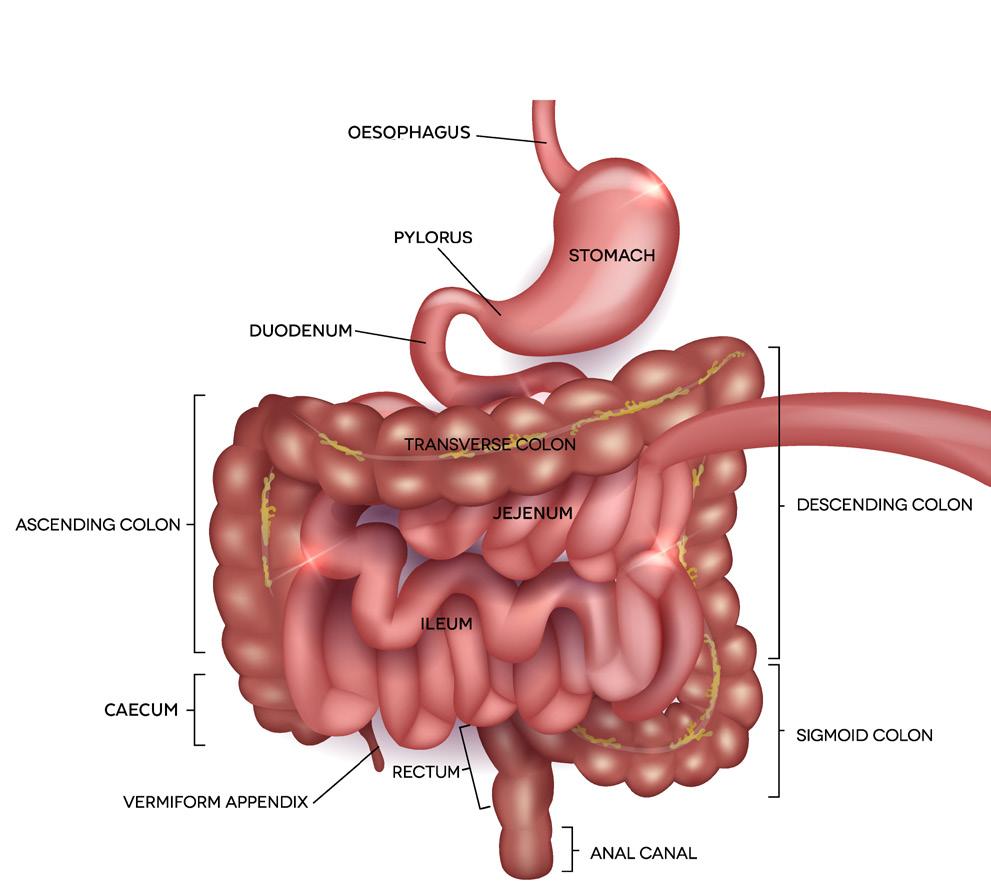
FOR EXAMPLE: THE DIGESTIVE ‘SYSTEM’
The digestive system (pictured on the previous page) is a perfect example of how important each system’s process and component is. The digestive system’s ability to break food down, absorb and utilise nutrients, and eliminate undigested waste products is wholly dependent on each component of the system working as it should.(5)
Once food has entered the oral cavity, the body will begin to digest it. There are two major types of digestion known as mechanical digestion and chemical digestion. Mechanical digestion begins in the oral cavity (mastication) and continues when the food hits the stomach, where the stomach churns the food/bolus. Chemical digestion is when larger molecules, such as proteins and starches, are broken down into smaller pieces. If chemical or mechanical digestion did not occur, the food would not be in an ideal state to allow optimal absorption.(1)
The stomach assists in the digestion of food molecules and acts as a storage tank. The stomach will release partially digested food into the small intestine at a rate the small intestine can handle.(6) If the stomach does not work as it should, it may pass too much food into the small intestine, resulting in deprived nutrient absorption secondary to being overloaded; or, as another example, if the stomach did not churn the food/ bolus adequately before passing it into the small intestine, the small intestine would have increased pressure to provide additional chemical digestion so that it can complete its job of nutrient absorption.(1)
The small intestine is responsible for a large amount of chemical digestion; this digestion is a result of the enzymes released by the pancreas and bile acid produced by the liver (bile acids are stored in the gallbladder to be released into the small intestine). The small intestine is also responsible for nutrient absorption. Absorbed nutrients are carried in the bloodstream to areas of the body which require them. If the pancreas enough enzymes, or the liver did not produce bile, there would be inadequate chemical digestion. Therefore the food would not be appropriately absorbed and utilised by the body.(1)
From here, the bolus continues to pass through the large intestine, where fluid is absorbed. The bolus continues to travel through while the digestive system absorbs and leaves what is not required. What is not required is then eliminated from the body. If the large intestine does not function optimally, it might not absorb adequate hydration, thus leaving the body dehydrated with potential diarrhoea; or it might absorb waste products into the bloodstream, consequently increasing the workload for the kidneys through filtration at a later time.(1)
Understandably, if one part of the digestive tract did not function optimally, it is easy to see how and why a problem would arise. It is therefore vital to remember that no matter how small a task may appear in the body, it is essential for the optimal functioning of the organism as a whole.(1)

ORGAN SYSTEMS ALSO WORK IN SYNERGY TOGETHER
Systems work together to ensure all tasks are completed effectively and efficiently to keep the body running. As explained above, all organs must work together in their system to accomplish their result (e.g., digestion). It is equally important for systems to work cooperatively to accomplish their various tasks.
Nutrients are absorbed via the digestive system’s small intestine and then transported into the bloodstream, which is part of the circulatory system. From here, nutrients are distributed via the circulatory system before all blood is passed through the kidneys for filtration. The kidneys form part of the urinary system, which removes waste from the blood and eliminates it from the body via the urine. Once the urinary system has filtered the blood, it is passed back into the circulatory system.(1)
Numerous other examples can show how the various organ systems work cooperatively. For example, the circulatory system is also closely linked to the respiratory system to deliver oxygen to cells and remove carbon dioxide, which the cells produce. The circulatory system receives oxygen from the respiratory system via the lungs as fresh air is breathed in, delivered to required tissues, collects carbon dioxide, and takes it back to the lungs, where it is expelled through breathing out.(1)

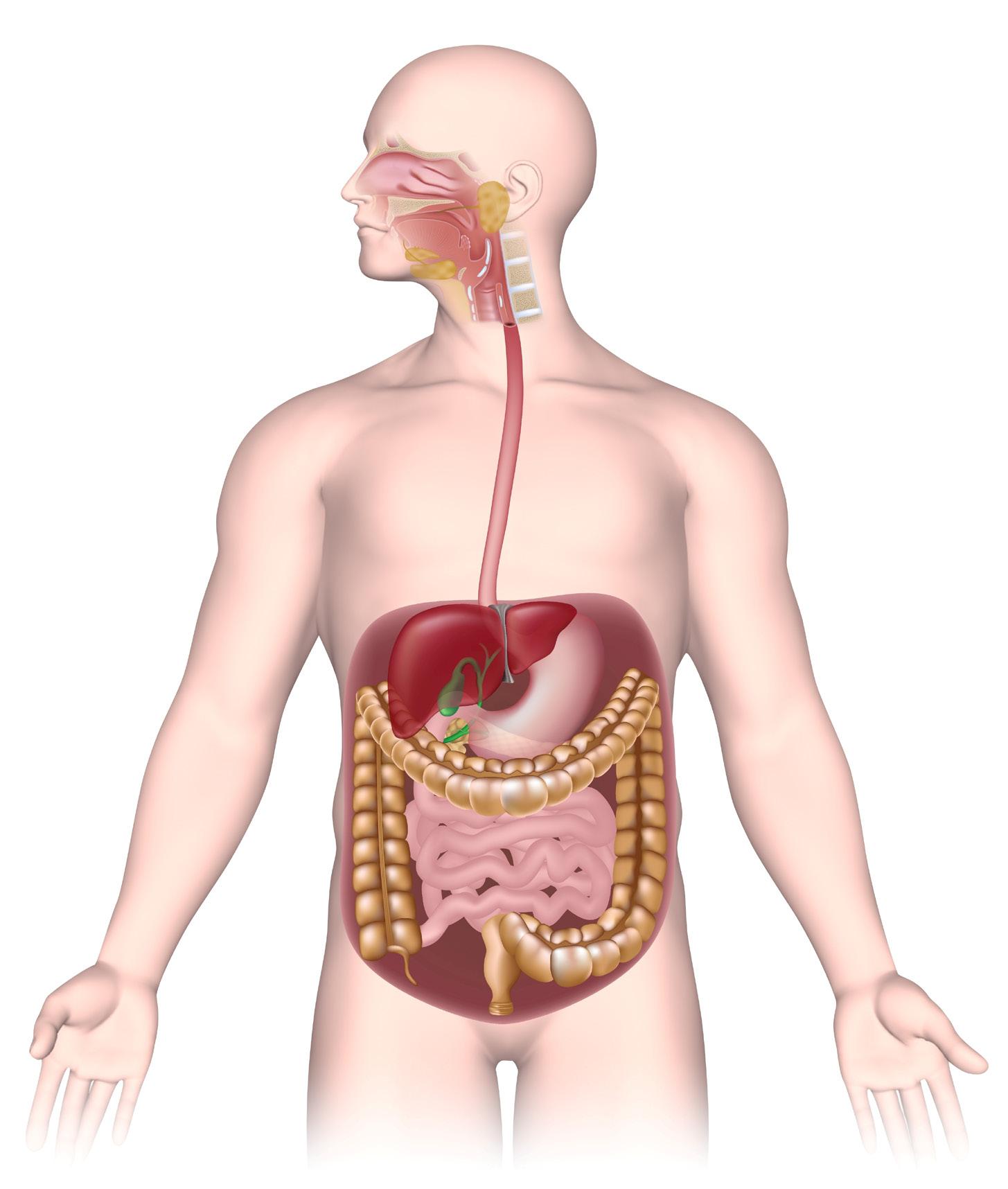
IDENTIFYING THE VARIOUS PARTS OF THE DIGESTIVE SYSTEM AND THEIR ROLE
The digestive system is comprised of several organs which are in direct contact with food. These organs combine to convert food into energy to feed the entire body. When food is consumed, it passes through a long tube inside the body known as the gastrointestinal (GI) tract, which is also commonly known as the alimentary canal.(1)
The major digestive organs that make up the GI tract include the:(1)
• Oral cavity
• Pharynx
• Oesophagus
• Stomach
• Small intestines (also known as the small bowel)
• Large intestines (also known as the large bowel).
The digestive system is also made up of accessory organs that assist the body in digesting food; however, the food itself does not pass through them. These accessory organs include the:(1)
• Teeth
• Tongue
• Salivary glands
• Epiglottis
• Liver
• Gallbladder
• Pancreas.
Oral cavity, tongue, teeth:
Mechanical processing, mixing with salivary excretion and softening.
Oesophagus:
Transports food to the stomach
Liver:
Secretes bile (Also has many non-digestive functions)
Storage of nutrients
Gallbladder:
Stores bile from the liver.
Pancreas:
Secretes pH buffers and several digestive enzymes
Salivary glands:
Secrete lubricating fluid and starchdigesting enzymes.
Epiglottis:
Pharynx: Directs food down the Oesophagus.
Stomach:
Shared digestive and respiratory passage.
Chemical breakdown of materials via acid and enzymes; mechanical processing through muscular contractions.
Large intestine:
Absorbs vitamins, minerals, and water; houses bacteria; produces faeces.
Small intestine:
Food is digested and absorbed.
Rectum:
Stores faecal matter before being passed out.

THE ORAL CAVITY
The oral cavity (also referred to as the buccal cavity) is the start of the digestive tract. The oral cavity is the beginning of the digestive system and the normal food-consumption pathway; however, there will be some cases where an individual uses an alternative feeding method such as enteral feedbing. This is where the food is passed down the nasal cavity and directly into the stomach via a feeding tube, thereby passing the oral cavity and oesophagus.(1)
The oral cavity is responsible for the initial stages in the breakdown of food. This includes mechanical digestion (through chewing) to make a smaller bolus more appropriate for swallowing and easier for ongoing digestion through the GI tract. It also includes the initial stages of carbohydrate breakdown by releasing an enzyme known as amylase.(1)
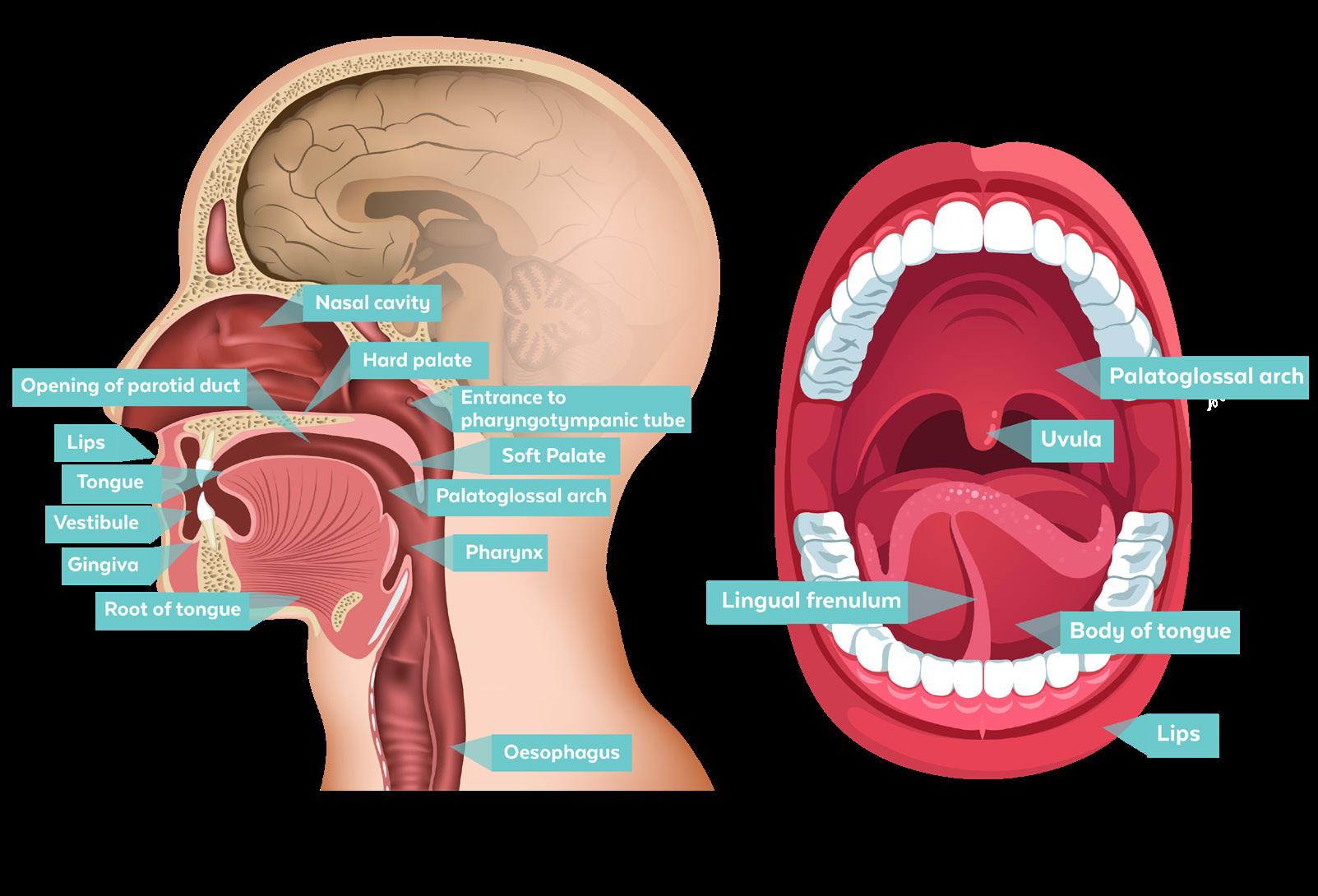
The oral cavity is home to many accessory organs, including the teeth, tongue and salivary glands, outlined in the table below:(1)
TEETH
TONGUE
SALIVARY GLANDS
There are 32 teeth in a healthy oral cavity that perform the task of chewing, otherwise known as mastication. Mastication aids in the breakdown of foods through cutting, crushing, and grinding, including harder-to-digest food such as connective tissue in meat or plant fibre in vegetable matter.
The tongue is a muscle in the mouth used for both speech and mechanical digestion. The tongue has four primary functions in the digestive tract, including:
1. Mechanical processing of food through compression, abrasion and distortion
2. Taste buds provide the sensory analysis of food through touch, taste and temperature receptors
3. Movement of food to assist in chewing and preparation for swallowing
4. Secretion of lingual lipase, an enzyme used in the digestion of lipids.
There are three pairs of salivary glands: the parotid salivary glands, the sublingual salivary glands and the submandibular salivary glands. Each pair of salivary glands produces a mixture of glandular secretions (0.6 percent) and water (99.4 percent), known as saliva. The glandular secretions encompass electrolytes, buffers, glycoproteins, antibodies, enzymes and waste products. The primary function of saliva is to lubricate the mouth, lubricate and moisten food to allow for easier passage down the oesophagus, and commence the digestion of complex carbohydrates. The salivary glands produce between 1 and 1.5L of saliva each day which helps keep the oral cavity at a pH of approximately 7.0.
These three accessory organs work symbiotically with each other to allow for the following to occur:
1. Sensory analysis of material before swallowing (e.g., allows the opportunity to determine if the food is safe to swallow through touch, temperature and taste receptors).
2. Mechanical processing uses the teeth and tongue to crush, tear and mix the food to increase its surface area for better digestion and absorption further down the GI tract.
3. Lubrication is provided by mixing the food with salivary excretions before swallowing the bolus.
4. Commences the breakdown (limited) of carbohydrates and lipids into simpler molecules.
THE PHARYNX
The pharynx is a passageway between the oral cavity and the oesophagus for solid food, liquid, and air. The pharynx works with the oral cavity and oesophagus muscles to initiate swallowing, an action that pushes the bolus down the oesophagus and into the stomach.(1)
The pharynx is comprised of three main compartments:(1)
1. The nasopharynx
2. The oropharynx
3. The laryngopharynx.
NASOPHARYNX
OROPHARYNX
LARYNGOPHARYNX
The nasopharynx is located at the back section of the nasal cavity. This section is essential for the exchange of oxygen and carbon dioxide.
The oropharynx begins at the back of the oral cavity and travels down to the epiglottis. The epiglottis is a flap of tissue that has two major functions:
1. It covers the air passage to the lungs
2. It directs food to the oesophagus to continue down the GI tract.
The oral cavity is specialised because it can take air and food into the human body.
The final section of the pharynx is the laryngopharynx. The laryngopharynx is vital in regulating air passage to the lungs and food to the oesophagus.
Nasal cavity
Nasopharynx
Larynx
Oesophagus
Lips
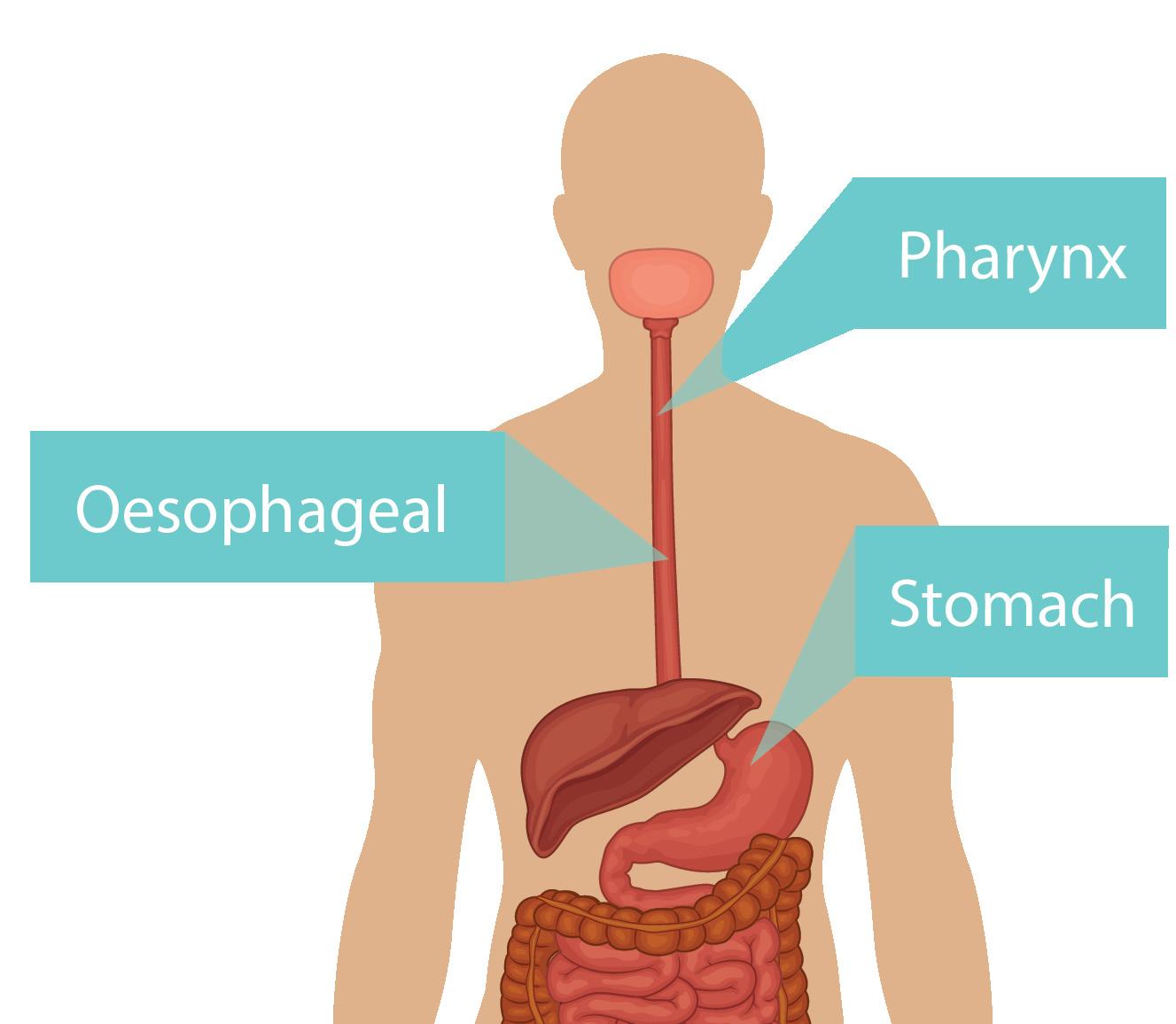
THE OESOPHAGUS
The oesophagus, also known as the ‘food pipe’, is a hollow muscular tube (approximately 25cm in length) connecting the oral cavity to the stomach. All food consumed is passed from the oral cavity to the pharynx and into the oesophagus.
The laryngopharynx is the portion of the pharynx that connects the oral cavity to the oesophagus. The gastrooesophageal junction is the area where the oesophagus joins the stomach. Food is then passed down the oesophagus and into the stomach.
The mixture of food and saliva, known as a bolus, is passed through the oesophagus using a process known as peristalsis.
Food bolus
It takes approximately 9 seconds for a typical bolus to make the trip from the oral cavity, down the oesophagus and into the stomach. The lower oesophageal sphincter is a ‘door’ between the oesophagus and the stomach, which allows food to pass from the oesophagus to the stomach and prevents the food from coming back up from the stomach into the oesophagus.(1)
Area of contraction
Area of relaxation
THE STOMACH
The stomach is a J-shaped organ that receives the bolus from the oesophagus and aids in mechanical and chemical digestion.
The stomach has three primary functions:
1. Storage of ingested food that has been received via the oral cavity
2. Mechanical breakdown through the churning and mixing of the ingested food
3. The chemical breakdown of ingested food using acid and enzymes (gastric secretions).
The mixture of ingested food and gastric secretions produces an acidic, soup-like mixture of partially digested food known as chyme. The stomach is an extremely acidic environment because of the gastric secretions of gastric juice and hydrochloric acid.(1)
This highly acidic environment is essential for the activation and role of pepsin (protein-digesting enzyme). In addition, this type of environment acts to:
• Kill most microorganisms ingested with food
• Denature proteins and inactivate most enzymes found in food
• Break down the fibrous segments of plants and connective tissue in meat.
Longitudinal layer (Outer)
Circular layer (Middle)
Oblique layer (Inner)
Body
Fundus
THE BOWELS
The bowels are made up of the small bowel (small intestine) and the large bowel (large intestine). Bowels are the parts of the human digestive system responsible for the body’s waste disposal after eating food.(1)

Small Intestine
Rectum
Large Intestine
Stomach
Anus
UNDERSTANDING HOW THE BOWELS WORK
Typically, food spends approximately 5 seconds to 2 minutes within the mouth and 8-10 seconds passing through the oesophagus before reaching the stomach. At this point, it may take between 15 minutes to 4 hours to be broken down by stomach acid before commencing transit of the small intestine, which requires approximately 1-5 hours. After this point, it will take anywhere from 12-24 hours to several days to transit through the large intestine before being expelled during a bowel movement.(7)
The total transit duration from the mouth to the anus varies between individuals and may take anywhere from 18 to 72 hours.(8)
This diagram illustrates the average time food spends in each part of the digestive system along:
Mouth Lower stomach
Esophagus
Small intestine
Large intestine
Food is transported via the digestive system through rhythmic muscular contractions (a process known as peristalsis). Peristalsis is used by both the oesophagus and the intestines. The large intestine transports waste along to the rectum through peristalsis. The enteric nervous system involuntarily controls peristalsis. Ingested food (bolus) eventually arrives at the rectum and is passed through the anus as faeces (depicted in the image below).(1)
Contraction
Bolus Moves Forward
THE SMALL INTESTINE (SMALL BOWEL)
The small intestine has an average length of three to five metres and is integral to the final stage of digestion and the absorption of nutrients.(9) It is a long, highly convoluted (tangled) tube in the digestive system that absorbs approximately 90 percent of the nutrients from the food consumed.
The small intestine’s many folds help it to pack all of its length into such a small body cavity.
The small intestine’s mucous membrane has a series of finger-like projections, known as villi. Villi are 0.5 to 1.6 millimetres long.(10)(11) The villi are then covered in microvilli, and together the villi and microvilli increase the surface area of the small intestine significantly, ultimately allowing for greater absorptive capacity.
For example, without the villi and microvilli, the small intestine would have a length of approximately 300m(2); however, with the villi and microvilli, the small intestine has a surface area of approximately 250 m2 (roughly the floor space of a spacious four-bedroom home).




Gastrointestinal tract
Villi
Epithelial cell with microvilli
A fold of intestinal lining
Small intestine
The mesentery (a thin membrane) extends from the posterior (behind) body wall of the abdominal cavity to surround the small intestine and anchor it in place. The stomach, large intestine, abdominal wall and pelvic girdle also help to restrict movement during digestion and hold the small intestine in place.(10)
Blood and lymphatic vessels and nerves transport nutrients from food in the intestines to the rest of the body. They also pass through the thin membrane (the mesentery) to support the tissues of the small intestine.(9) The primary blood vessels involved are branches of the superior mesenteric vein and the superior mesenteric artery.
The small intestine fills most of the peritoneal cavity and is positioned inferior (under) to the stomach. In addition, it is divided into three regions forming one continuous tube. Each region displays characteristic differences, but there are no distinct separations between them.(9)
Small intestine
Inferior vena cava
Ascending colon
Psoas major
Descending colon
Rectus
Mesentery
Aorta
The three regions of the small intestine include:
1. The duodenum
2. The jejunum
3. The ileum.
DUODENUM
The first part of the small intestine is called the duodenum. It is situated alongside the stomach, connects to the pyloric sphincter of the stomach and is only 20cm to 25cm in length.(9)
The duodenum receives partly digested food (or chyme) from the stomach and digestive secretions from the liver and pancreas. Chyme moves along the segments of the small intestine with weak peristalsis.
CHYME
Chyme refers to the acidic fluid which passes from the stomach to the small intestine, consisting of gastric juices and partly digested food.
The next segment of the small intestine is the jejunum (approximately 2.5 metres long), where the bulk of chemical digestion and nutrient absorption occurs.(9) It is situated centrally in the abdomen and comprises approximately two-fifths of the remaining bowel.
The jejunum is a deep red due to its extensive blood supply; its peristaltic movements are rapid and vigorous, and there is little fat in the mesentery that supports this region.
JEJUNUM
THE MESENTERY
The mesentery is a fold of membrane that attaches the intestine to the abdominal wall and holds it in place.(7)
The last region of the small intestine is called the ileum, which is approximately 3 metres in length and connected via the ileocecal valve to the large intestine and located in the lower abdomen.(9)
The walls of the ileum are narrower and thinner than in the jejunum and duodenum. Because of this, blood supply is more limited, peristaltic movements are slower, and the mesentery has more fatty areas.
PERISTALTIC MOVEMENTS:
Peristaltic movements are involuntary movements within the digestive tract and can occur in other hollow tubes in the body. Wavelike contractions occur due to the contraction of muscles in the digestive tract that run in a longitudinal and circular formation.(2)
ILEUM
THE LARGE INTESTINE (LARGE BOWEL)
The large intestine, also known as the large bowel, is an approximately 1.5m muscular tube in the shape of a horseshoe that connects the small intestine to the rectum. The large intestine is a highly specialised organ that absorbs the final 10 percent of nutrients (in particular, vitamin K, biotin, and vitamin B12) with the aid of colonic bacteria. The large intestine is also responsible for preparing and storing waste so that it can then be eliminated from the body in a process known as defecation.(12)
More than 80 percent of water is also reabsorbed in the large intestine to leave a more compact stool (mucus still plays a role in lubrication) for elimination. The average composition of faeces is 75 percent water and 25 percent solids. Bacteria may account for 30 percent of total faecal weight.(2)
The large intestine can be divided into three segments:
1. The caecum
2. The colon
3. The rectum.
These segments are described in the table below and shown in the following image:
CAECUM
COLON
The caecum is a pouch-like portion of the large intestine that collects and stores materials from the small intestine and begins the process of compaction. The caecum receives all food from the ileum of the small intestine through a valve known as the ileocecal valve.
The colon (approximately 1.5 metres long) is a muscular tube connecting the caecum to the rectum and consists of the following four sections:(11)
• The ascending colon
• The transverse colon
• The descending colon
• The sigmoid colon.
The colon plays an ongoing role in the reabsorption of water, absorption of remaining nutrients and the preparation of the stool. Usually once or twice a day it empties its contents into the rectum to begin the process of elimination.
The colon is home to over 1000 species of bacteria,(2) which play a role in nutrient metabolism, antimicrobial protection, drug metabolism and the integrity of the GI tract.(13)
The rectum is the digestive system’s last section, a 15cm chamber connecting the colon to the anus for defecation. The rectum is an expandable organ for storing faeces before voluntary elimination.
RECTUM
When faecal matter enters the rectum, it sends a message to the brain triggering the urge to defecate. The final portion of the rectum is called the anus, where the stool passes out of the body.(2)
Sigmoid
THE LARGE INTESTINE
Right colic flexure (hepatic flexure)
Ascending colon
Transverse colon
Left colic flexure (splenic flexure)
Descending colon

Sigmoid colon
Caecum
Rectum
Anal canal
IIeocecal valve
Jejunum
THE LIVER AND GALLBLADDER
The liver is a large brownish-red organ that weighs approximately 1.5kg and plays a crucial role in metabolic and synthetic functions. The liver is the largest visceral organ and one of the body’s most diverse and versatile organs.(2) The anterior view is separated into two major lobes: the left and right lobes (which are separated by the falciform ligament); and two minor lobes: the caudate and quadrate lobes, can be seen from the posterior view (shown in the images below).
ANTERIOR VIEW
POSTERIOR VIEW
Falciform ligament
The liver is responsible for haematological regulation, where blood passes through the liver and executes the following functions:(1)
• Removes circulating hormones
• Removes antibodies
• Removes and safely stores toxins
• Synthesises and secretes bile.
In addition to the above, the liver has two main functions specific to digestion, and these functions are shown in the table below:
METABOLIC REGULATION
BILE PRODUCTION
All blood leaving the digestive tract enters the hepatic portal system and flows into the liver. The liver cells remove and store nutrients and mobilise stored nutrients to correct deficiencies. The liver also assists in all macronutrient metabolism.(1)
Bile is synthesised (approximately 1L produced daily) in the liver, secreted into the gallbladder, and then into the duodenum upon digestion of fat-containing meals. Bile is made of water, ions, bilirubin, cholesterol, and lipids, collectively known as bile salts. Bile salts assist in emulsifying lipids, thus increasing their surface area for better digestive and absorptive opportunities.(1)
TED TALK - WHAT DOES THE LIVER DO?
CLICK HERE to watch the video.
Hepatic vein
Inferior vena cava
Inferior vena cava
Teres ligament
Gallbladder
Right lobe
Left lobe
Portal vein
Fissure for teres ligament
Proper hepatic artery Quadrate lobe
THE GALLBLADDER
The gallbladder is a small organ that is situated under the liver. It is a small pear-shaped, hollow structure that stores and concentrates a yellow-brown digestive enzyme produced by the liver (known as bile) before being excreted into the duodenum.
The gallbladder can hold approximately 40 to 50ml of bile at capacity.(2) Bile is continuously secreted into the small intestine and can be reabsorbed so that it can be reused to aid in the digestion of subsequent lipid (fat)-containing meals.
Bile is essential for the digestion of fats. The gallbladder, on the other hand, is not necessarily classed as essential as individuals who have their gallbladders removed are still able to survive. Because the gallbladder stores bile, individuals who have their gallbladders removed (known as cholecystectomy) generally need to consume smaller amounts of fat in their meals as there is no stored bile for digesting excessive amounts of dietary fat. If fat is consumed in excess by an individual without a gallbladder, that individual may notice fat malabsorption.(2)
Liver
Gallbladder Pancreas
Common Bile Duct
Gallstones are small, hard, pebble-like stones that form in the gallbladder and can become extremely painful when caught in the bile duct or if the stones become quite large. Gallstones are made of cholesterol and bilirubin, both of which are components of bile and occur due to bile crystallising. One of the current remedies for gallstones is the removal of the gallbladder. A healthy diet rich in fibrous vegetables, regular physical activity, and maintaining a healthy weight is suggested to help reduce an individual’s risk of developing gallstones.(14)
Interesting fact: Gallstones are twice as common in women as they are in men.(15)
THE PANCREAS
The pancreas is an elongated pinkish-grey organ located slightly inferior (below) and posterior (behind) to the stomach. The pancreas is surrounded by other organs, including the liver, the small intestine, and the spleen.(1)
The pancreas has three distinct sections:(1)
1. The head
2. The neck
3. The tail.
THE HEAD
THE NECK
THE TAIL
The head of the pancreas is located where the stomach meets the first part of the small intestine. As the stomach empties partially digested food into the small intestine, the pancreas will release pancreatic enzymes into these contents to help with their digestion.
The neck of the pancreas refers to the central part of the organ.
The thin end of the pancreas is often referred to as the tail.
The pancreas has two major functions:
1. Digestion of food:
The pancreas produces enzymes that are essential for digestion. These enzymes include trypsin and chymotrypsin to digest proteins, amylase to digest carbohydrates, and lipase to digest dietary fats. Along with the bile, these enzymes assist with macronutrient digestion.(1)
2. Regulation of blood glucose levels:
The islet cells in the pancreas (commonly known as the Islets of Langerhans) produce two different hormones which assist with the regulation of blood glucose levels. These two hormones include insulin, which helps to lower blood glucose levels, and glucagon, which helps to raise blood glucose levels.(1)
Gallbladder
UNDERSTANDING THE PHYSIOLOGY OF THE DIGESTIVE SYSTEM
The primary roles of the digestive system are digestion and absorption. Digestion is the breakdown of food into smaller molecules, which are then absorbed into the body and utilised as energy. Through a series of steps, the digestive system digests and absorbs nutrients from ingested food for energy, repair and growth of the human body; this is called the digestive process.(1)
The digestive process can be looked at as a series of steps, and the six major steps of the digestive system include:(1)
1. Ingestion
2. Mechanical processing
3. Digestion
4. Secretion
5. Absorption
6. Excretion.
The digestive process is outlined in more detail on the following page.
Your teeth perform “mechanical” digestion.
The oesophagus pushes food down.
The liver secretes bile to help fat digestion.
The large intestines absorbs remaining water/electrolytes and compacts faecal matter.
Salivery glands secrete saliva to start “chemical” digestion.
Food travels down the pharynx into the oesophagus.
The Stomach secretes gastic juices, and “chemically” digests food.
The small intestine completes digestion.
The rectum stores faeces until it leaves the body through the anus.
STEP 1: INGESTION
Ingestion refers to the intake of food via the oral cavity. Ingestion is a conscious decision to place food or drink into the mouth. The oral cavity is the first section of the GI tract.
STEP 2: MECHANICAL PROCESSING
Mechanical processing is the mixing, crushing, and tearing of food to increase its surface area, ensuring that food is easier for the body to digest and absorb further down the GI tract. The teeth and tongue complete this process in the oral cavity. The stomach also completes mechanical processing through the muscular churning of ingested food as it turns it into chyme. Not all food needs to be mechanically processed; for example, liquids generally require no mechanical processing at all. All solids require mechanical processing, with some foods requiring more processing than others.
STEP 3: DIGESTION
The breakdown (chemical breakdown) of food into smaller molecules to allow proper absorption is known as digestion. In other words, digestion is the process of breaking down larger macronutrients and longer chains of polysaccharides, protein and triglycerides into their most simple form.
For example, complex proteins are of no use to the body until they are broken down into simple amino acids, which the body can use for energy, muscle maintenance and repair. Digestion begins in the oral cavity, where salivary amylase begins the breakdown of carbohydrates and is otherwise completed in the stomach and small intestine with the assistance of gastric and pancreatic juices.
STEP 4: SECRETION
Secretion refers to the release of digestive enzymes, buffers and salts from glandular organs and the epithelium of the GI tract. These secretions play a large role in the chemical breakdown of food in which they help to moisten the bolus of food in the oral cavity, the stomach, and the small intestine.
These secretions include:
• Saliva: Moistens food in the oral cavity and contains salivary amylase, a digestive enzyme that begins the process of carbohydrate digestion.
• Mucus: Acts as a lubricant inside the large intestine to soften stools and prevent the intestine from drying out.
• Gastric juices: Assist with chemical digestion and kill harmful bacteria found in the bolus. An example of gastric juice is hydrochloric acid.
• Digestive enzymes: Break down larger macronutrients into their smaller, simpler form. Examples of digestive enzymes include lipase, pepsin, and amylase.
• Bile: Secreted by the liverand stored in the gallbladder. It is used to emulsify large lipid molecules into smaller globules for easier digestion.
• Hormones: Released in response to digestion cues. Examples of hormones released include cholecystokinin, secretin and gastrin
STEP 5: ABSORPTION
Absorption refers to the transfer of nutrients, vitamins, minerals, salts, and electrolytes from the digestive epithelium across to the interstitial fluid of the digestive tract. The small intestine is where 90 percent of absorption occurs due to its great surface area. The remaining 10 percent of absorption is completed in the large intestine.
STEP 6: EXCRETION
Excretion is the last stage (or role) of the digestive system. Excretion refers to the removal of waste products via a process known as defecation. Undigested matter and organic waste products continue to pass through the large intestine, where water and any remaining nutrients are absorbed, thus leaving a compacted stool as waste to be excreted through the rectum.
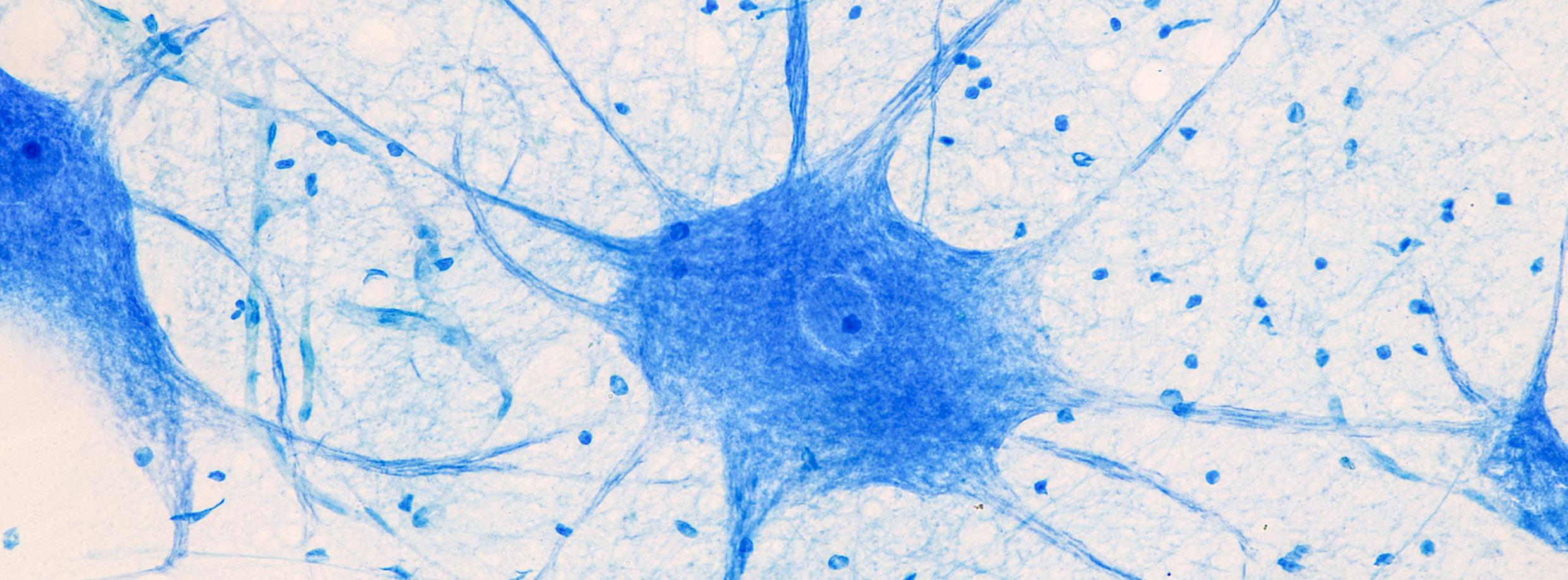
THE INTERACTION BETWEEN THE NERVOUS SYSTEM AND THE DIGESTIVE SYSTEM
The nervous system comprises various networks of cells that signal different impulses throughout the body. It is made up of neurons (nerve cells) and neuroglia (helper cells). Neurons will work to communicate through electrochemical signals throughout the body while neuroglia or glial cells assist the neurons.
In other words, the nervous system includes the brain, spinal cord, sensory organs, and nerves that work together to connect the rest of the body to these specific organs. The nervous system is how the body moves communication throughout the body.(10)
As a nutrition coach, understanding that the nervous system is fundamental to the body’s capacity to function and live in every way is imperative. As discussed in previous units of this course, the nervous system is responsible for exciting (stimulating) muscles and causing them to contract to move the body. Therefore, without neural impulses of the nervous system, muscles would simply be unable to contract/move.
The nervous system, however, is not only responsible for stimulating muscle; it stimulates every tissue and organ within the body and works synergistically with the digestive system. Thus, a healthy nervous system is important. Without a properly functioning nervous system, the body would not have the ability to effectively utilise the digestive system, resulting in the body not being able to absorb any of the food that is consumed.
The nervous system interacts with the digestive system in the following ways to maintain proper function:(10)
• Digestive processes deliver the building blocks for some neurotransmitters.
• The autonomic nervous system controls the muscle tone of the digestive tract.
• The brain controls drinking and feeding behaviour.
• The brain controls the body’s muscles required for eating (ingestion) and elimination.
• The digestive system relays sensory information to the brain.
Brain
Heart
Stomach
Bladder
Spinal cord
The nervous system is initially divided into the following two divisions:
1. Central Nervous System (CNS)
2. Peripheral Nervous System (PNS).
From here, the peripheral nervous system is divided into the somatic nervous system (SNS) and the autonomic nervous system (ANS). The ANS is then divided into the sympathetic division and the parasympathetic division.(10) This organisation of the nervous system is shown in the image below:
NERVOUS SYSTEM
CENTRAL NERVOUS SYSTEM (CNS)
(the body’s master control system containing the brain, brainstem and spinal cord)
AUTONOMIC NERVOUS SYSTEM (ANS)
(a division of the pns that communicates with internal organs and glands. Involuntary contractions are controlled at the subconscious level)
PERIPHERAL NERVOUS SYSTEM (PNS)
(the body’s link to the outside world)
SYMPATHETIC DIVISION
SOMATIC NERVOUS SYSTEM (SNS)
(the body’s link to the outside world)
PARASYMPATHETIC DIVISION SENSORY OUTPUT (AFFERENT)
MOTOR OUTPUT (EFFERENT) (prepares the body for action and stress. This is called ‘ ght or ight’) (calms the body and helps the body conserve energy)
THE CENTRAL NERVOUS SYSTEM (CNS)
In conjunction, the brain and spinal cord form the central nervous system (CNS), where information is processed, and responses originate. These are complex organs that include neural tissue, blood vessels, and the various connective tissues that provide physical protection and support.
The CNS is responsible for integrating, processing, and coordinating sensory data and motor commands. The CNS controls higher functions of the nervous system such as language, creativity, expression, emotions, and personality.
Sensory data conveys information about conditions inside or outside the body. Motor commands control or adjust the activities of peripheral organs such as skeletal muscles. For example, if an individual stumbles or falls, the CNS integrates information regarding their balance and the position of their limbs. It then coordinates their recovery by sending motor commands to appropriate skeletal muscles.(16) This happens in a split second and without conscious thought/effort.
Dura and arachnoid mater
Medullary cone
Dural sac
Brain
Spinal cord
Spinal nerves
Cauda equina
THE PERIPHERAL NERVOUS SYSTEM (PNS)
Nerves located outside the spinal cord and the brain form the peripheral nervous system (PNS). The PNS includes all neural tissue outside the CNS. It consists of sensory neurons, ganglia (clusters of neurons), and nerves that connect to one another and to the central nervous system.
The PNS delivers sensory information to the CNS and carries motor commands to peripheral tissues and systems. Bundles of axons, or nerve fibres, carry sensory information and motor commands in the PNS. These bundles, with associated blood vessels and connective tissues, are called peripheral nerves, or simply nerves.(10)
The PNS is made up of two main parts:
1. The autonomic nervous system (ANS)
2. The somatic nervous system (SNS).
SOMATIC NERVOUS SYSTEM (SNS) AUTONOMIC NERVOUS SYSTEM (ANS)
SOMATIC VS AUTONOMIC NERVOUS SYSTEM
CLICK HERE to watch the video.
THE SOMATIC NERVOUS SYSTEM (SNS)
The somatic nervous system (SNS) is a division of the PNS that includes all the voluntary efferent neurons. The SNS is the only consciously controlled part of the PNS and is responsible for stimulating skeletal muscles in the body.(10) Voluntary contractions occur under conscious control. For example, a person exerts conscious control over their arm as they raise a full glass of water to their lips.
Viseral Effectors
Smooth muscle
Glands
Cardiac muscle
Adipocytes
Upper motor neurons in primary motor cortex
Visceral motor nuclei in hypothiamus
Spinal cord
Somatic motor nuclei of spinal cord
Preganglionic neuron
Somatic motor nuclei of brain stem
Lower motor neurons
Autonomic ganglia
Ganglionic neurons
Autonomic nuclei in spinal cord
Autonomic nuclei in brain stem
THE AUTONOMIC NERVOUS SYSTEM (ANS)
The autonomic nervous system (also referred to as the visceral motor system) is a division of the PNS that provides automatic regulation of smooth muscle, cardiac muscle, and glandular secretions. The ANS controls involuntary (subconscious) body processes which are not under conscious control, for example, digestion.(17)
Besides the voluntary act of ingesting food, the remainder of digestion and absorption occurs subconsciously. Regarding digestion, the ANS is responsible for:(17)
• Salivary excretions
• Peristaltic contractions
• Gastric juice production
• Hormone release
• Storing energy
• Opening and closing digestive sphincters such as the ileocecal sphincter.
Within the ANS, there are another two divisions:
1. The sympathetic division
2. The parasympathetic division.
The diagram below outlines how each division regulates functioning organs:
PARASYMPATHETIC
Eyes
Constrict pupil
Salivary glands
Stimulates salivation
Lungs
Constrict bronchi
Heart Slows heartbeat
Stomach Stimulates digestion
Liver
Stimulates bile release
Intestines
Stimulates peristalsis and secretion
Bladder
Contracts bladder
Chain of sympathetic ganglia
SYMPATHETIC
Eyes
Dialate pupil
Salivary glands
Inhibit salivation
Lungs
Dilate bronchi
Heart
Accelerates heartbeat
Stomach Inibits digestion
Liver
Stimulates glucose release
Intestines
Inhibit peristalsis and secretion
Stimulate epinephrine and norepinephrine release
Bladder
Contracts bladder Kidneys
The parasympathetic division of the ANS forms the body’s ‘rest and digest’ response when the body is relaxed, resting, or feeding.(18) The parasympathetic division works to undo the work of the sympathetic division after a stressful situation.
Spinal cord
Brain
Among other functions, the parasympathetic division works to:(10)
• Decrease respiration
• Decrease heart rate
• Increase digestion
• Permits the elimination of waste.
The parasympathetic division is active throughout the entire digestive tract ensuring adequate digestion, absorption, and excretion of nutrients from the foods ingested. This division also works towards relaxation, stimulating digestion at appropriate times, and absorption of nutrients.(18)
In particular, the parasympathetic division conducts the following functions in the digestive system, outlined in the table below:
FUNCTION
SALIVARY PRODUCTION
SPHINCTER RELAXATION
SECRETORY GLAND STIMULATION
BLOOD FLOW
PERISTALSIS
FAT UTILISATION
HORMONE SECRETION
DEFECATION
EXPLANATION(10)(18)
The parasympathetic division stimulates the production of saliva to assist in the initial chemical digestion of carbohydrates in the oral cavity.
The parasympathetic division allows the various sphincters of the GI tract to subconsciously dilate, thus allowing matter to pass through to the next phase of the GI tract.
For example, the ileocaecal sphincter allows the bolus to pass from the ileum of the small intestine through to the caecum of the large intestine.
The parasympathetic division stimulates secretory glands, thereby increasing the production of gastric juices and enzymes used to break down the food.
The parasympathetic division increases blood flow to the digestive tract, stimulating digestion.
The parasympathetic division increases peristaltic contractions, aiding in the movement of food down the oesophagus and through the bowels. These contractions increase and improve the digestion of food and absorption of nutrients.
The parasympathetic division utilises fat as an energy source.
The parasympathetic division stimulates the secretion of hormones which promote the absorption and utilisation of nutrients by peripheral cells.
The parasympathetic division provides the stimulation and coordination of defecation.
PARASYMPATHETIC NERVOUS SYSTEM ANATOMY
CLICK HERE to watch the video.
The sympathetic division of the ANS forms the body’s ‘fight or flight’ response to stress, danger, excitement, exercise, emotions, and embarrassment. This division is best described in this way: If an individual is in a sudden dangerous situation, their heart rate increases, their mouth can dry out, and their muscles involuntarily contract. This heightened level of alertness, speed, and tension is the body’s response to preparing for either a ‘fight’ (to stay with the danger and fight it) or ‘flight’ (the speed required to flee from the danger).(19)
In a stressful or aroused setting, the sympathetic division:
• Increases respiration and heart rate
• Releases adrenaline and other stress hormones
• Decreases digestion to cope with these situations.
In addition to the above, the table below outlines how the sympathetic division influences the digestive system during a stimulating event:
FUNCTION
BLOOD
SPHINCTERS
EXPLANATION(10)(19)
Blood is directed to travel away from the digestive tract and therefore decelerates (reduces) digestion. Energy is reserved for larger, more critical organs, given the situation, such as the heart, large muscle groups, and lungs.
The body may retort to this negatively with constipation, diarrhoea, or bloating.
The sympathetic division constricts sphincters throughout the GI tract, slowing the digestion process to reserve energy.
TED TALK - SYMPATHETIC NERVOUS SYSTEM ANATOMY CLICK HERE to watch the video.
After the sympathetic division has dealt with a stressful, dangerous, or stimulating situation/event, it is then up to the parasympathetic division to restore the calming effects in the body and recommence digestive processes.(10)
THE DIGESTIVE SYSTEM WORKING WITH OTHER BODY SYSTEMS
Like all organ systems within the human body, the digestive system works in concert with many other body systems.
For example, another system less involved, albeit equally important, is the support and protection the skeletal system provides the digestive system. A number of the skeletal bones, including the skull, vertebrae, ribs, and pelvis, support and protect most parts of the digestive tract, and teeth provide the initial mechanical breakdown of food. In addition, the skeletal system absorbs calcium and phosphate for incorporation into the bone matrix.(10)
The table below provides a summary of how other systems in the body contribute to the functioning of the digestive system.
CONTRIBUTION OF OTHER BODY SYSTEMS TO THE DIGESTIVE SYSTEM(10)
BODY SYSTEM
INTEGUMENTARY
SKELETAL
MUSCULAR
NERVOUS SYSTEM
CARDIOVASCULAR
ENDOCRINE
RESPIRATORY
URINARY
BENEFITS RECEIVED BY THE DIGESTIVE SYSTEM
• Provides vitamin D3, which is needed for the absorption of calcium and phosphorous
• Adipocytes in the subcutaneous layer provide storage for lipids.
• Ribs, skull, and vertebrae help protect and support digestive organs
• Teeth aid in the mechanical breakdown of food.
• Protects and supports digestive organs in the abdominal cavity.
• Reflexes coordinate and regulate muscle contraction to allow the passage of materials along the GI tract
• Control over skeletal muscles regulates ingestion and excretion.
• Carries nutrients, water, hormones, and other materials to and from the
• digestive tract
• Absorbs vitamin K
• Delivers nutrients and toxins to the liver.
• Endocrine cells of the pancreas secrete insulin to control blood sugar levels
• Endocrine hormones regulate secretion in digestive glands and accessory organs
• Stimulates contraction of sphincters.
• Provides oxygen and removes carbon dioxide.
• Expels toxins absorbed by the digestive tract
• Absorbs water needed to excrete waste products from the kidneys.
THE DIGESTIVE PROCESS: CONTROLLED BY HORMONES
The digestive process is fundamentally controlled by a combination of hormones. In response to food entering the digestive system and its associated pH levels, many hormones are released to stimulate or decrease various secretions to aid optimal digestion. These hormones are released in response to several different cues, such as hunger and satiation signals, when different nutrients progress through the GI tract or in response to the release of chyme.(1)
Hormones play a number of vital roles in the digestion process including:(1)
• The secretion of bile
• The stimulation of certain glands
• The inhibition of acid production
• Increasing stomach motility.
Some of the essential hormones involved in controlling the digestive process can be found in the table below:
HORMONE
SECRETIN
CHOLECYSTOKININ
MAJOR ACTIVITIES
Secretin stimulates production of pancreatic fluid and bicarbonate, and neutralises gastric acid, resulting in a raised pH in the duodenum and inhibition of gastric motility.(20)
Cholecystokinin quickens the production and secretion of all digestive enzymes and increases the flow of bile and pancreatic juice into the duodenum.
STIMULI FOR RELEASE (SECRETION)
Secretin is released when chyme arrives in the duodenum.
GASTRIN
Gastrin increases stomach motility and stimulates the production of acids and enzymes.(1)
GHRELIN
GASTRIC INHIBITORY PEPTIDE (GIP)
VASOACTIVE INTESTINAL PEPTIDE (VIP)
LEPTIN
Cholecystokinin is secreted when chyme reaches the duodenum, especially when the chyme contains lipids and partially digested proteins.
Gastrin is secreted when exposed to large amounts of incompletely digested proteins.(1)
Ghrelin increases appetite and hunger.(1) Ghrelin is secreted primarily from the stomach in response to hunger or fasting.(1)
GIP stimulates duodenal glands, stimulates lipid synthesis in adipose tissue and increases glucose use by skeletal muscles.
VIP stimulates buffer secretion, inhibits acid production, and dilates intestinal capillaries.
Leptin sends signals to the brain (more specifically, the hypothalamus). Leptin assists in maintaining weight and is often referred to as the ‘satiety hormone’ or the ‘starvation hormone’.(21)
Leptin assists in inhibiting hunger and regulating energy balance, so the body does not trigger hunger responses when it does not need energy.(22)
GIP is secreted when fats and carbohydrates enter the small intestine.
VIP is secreted when chyme arrives in the duodenum.
Leptin is released from adipose tissue found in fat cells.(1)
The thyroid gland is responsible for the release of three hormones. These hormones include:
1. Thyroxine (T4)
2. Triiodothyronine (T3)
3. Calcitonin.
These hormones play a vital role in metabolism and energy regulation in the body and can affect how cells work throughout the body.
When the thyroid is not performing correctly, the release of hormones can become either ‘excessive’ (hyperthyroidism may arise) or ‘deficient’ (hypothyroidism may arise). As these hormones are involved in metabolism, a problem with the thyroid can result in gastrointestinal (GI) symptoms.(23)
THE ROLE OF LEPTIN AND GHRELIN IN THE REGULATION OF FOOD INTAKE
Leptin and ghrelin are two hormones that have been recognised to have a significant influence on energy balance. Leptin is a mediator of long-term regulation of energy balance, suppressing food intake and thereby inducing weight loss. On the other hand, Ghrelin is a fast-acting hormone, seemingly playing a role in meal initiation.(24)
Leptin is commonly known as the ‘satiety hormone’, while ghrelin is known as the ‘hunger hormone’. When ghrelin levels are high, it stimulates a hunger response, resulting in an individual feeling hungry. After eating, ghrelin levels fall, and leptin increases, resulting in a person feeling satisfied.(24) The image below describes the different roles of leptin and ghrelin before and after eating.
LEPTIN & GHRELIN
GHRELIN
Tissue
LEPTIN GHRELIN
LEPTIN
BEFORE EATING AFTER EATING
UNDERSTANDING FACTORS THAT CONTRIBUTE
TO DIGESTIVE HEALTH
UNDERSTANDING THE IMPORTANCE OF STOMACH ACID FOR DIGESTIVE HEALTH
The structure of the digestive system and the role played by enzymes and hormones have been explored; however, it is also important to understand both the functions and the importance of maintaining a suitable balance of stomach acid.
While the most notable function of stomach acid is to assist in the breakdown of foods, or more specifically, the protein within foods, stomach acid also performs several other key actions, including:
1. Killing most of the unwanted microorganisms ingested with food
2. Denaturing proteins and deactivating most of the enzymes in food
3. Aiding in the breakdown of plant cell walls and the connective tissues in meat
4. Being essential for the activation and role of pepsin, a protein-digesting enzyme.
The primary gastric acid present in the stomach is hydrochloric acid (HCL). The parietal cells secrete approximately 1.21.5L of HCL each day.(7) HCL would be strong enough to break down the walls of the stomach if the stomach were not protected by a mucous lining.
ACID-BASE (PH) BALANCE
An individual is considered to be in an acid-base balance when the amount of hydrogens produced is directly offset by their loss. When body fluids are compromised in any way (e.g. overhydration or dehydration), it is likely to affect the pH balance of the body.
The acidity or alkalinity of any solution is measured on a pH scale (described below). To be in acid-base balance refers to an individual maintaining an internal pH ideal for optimal body functioning. The human body maintains a slightly alkaline pH between 7.35 and 7.45, with an average pH of 7.4.(25) A person’s acid-base balance is measured through carbon dioxide (acidic) levels and bicarbonate (alkaline) levels in the blood.(26)
UNDERSTANDING PH LEVELS
pH is the alkalinity or acidity of a solution measured on a scale from 0-14. The lower the number on the scale, the higher the level of acidity, and the higher the number on the scale, the higher the level of alkalinity. The neutral balance is 7.4, which is roughly the level the body aims to maintain according to the needs of different body systems.(2)(25)
pH of 7.4 is neutral
pH less than 7.35 is acidic
pH greater than 7.45 is alkaline
The stomach acid needs to maintain an appropriate pH balance (1.5-3.5) to ensure the digestive system functions effectively. If pH levels are not balanced, this may result in decreased nutrient digestion and absorption, which in turn could result in symptoms such as:(27)
• Acid reflux
• Halitosis (bad breath)
• Tiredness
• Lethargy.
BLOOD AND PH LEVELS
As the body needs to maintain a set pH balance depending on the location, the blood vessels will assist in ensuring an optimal pH range at all times. For example, the blood vessels absorb and neutralise acids produced by active tissues (muscles that have undergone intense exercise/activity), such as lactic acid (a by product of intense exercise when insufficient oxygen is available to convert pyruvate to usable energy). Blood pH is slightly alkaline, with venous blood at 7.35 and arterial blood at 7.45 being normal values.(28)
BLOOD ACIDITY
BLOOD ALKALINITY
Blood acidity increases when the levels of acidic compounds increase (e.g. ingestion of acidic compounds, poor elimination) or when levels of alkaline compounds decrease (through decreased ingestion or increased elimination).
Blood alkalinity rises when the level of acid within the body decreases or when the level of alkalinity increases, both of which may occur due to increased consumption of alkalising foods or increased elimination of acidic compounds.
BODY SYSTEMS AND PH LEVELS
A pH level that is too acidic (a state known as ‘acidosis’) or too alkaline (a state known as ‘alkalosis’) can have numerous effects on the individual. The pH levels are maintained primarily by the respiratory system (lungs) and the urinary system (kidneys). When either of these systems is compromised, an individual’s acid-base balance can also become compromised.(29)
Complications of respiratory (lungs) acidosis include:
• Shock
• Respiratory failure
• Organ failure.
Respiratory acidosis occurs due to the lungs not removing excess carbon dioxide from the body. Because carbon dioxide is acidic, this results in respiratory acidosis.
Respiratory acidosis may occur as a result of:(29)
• Obesity
• Chest deformities
• Chronic respiratory disorders, for example, COPD (Chronic obstructive pulmonary disease)
• The overuse of sedatives.
Complications of metabolic (kidneys) acidosis include:(29)
• Rapid breathing
ACIDOSIS
• Fatigue
• Confusion
• Diarrhoea
• Shock.
Metabolic acidosis generally occurs for one of three reasons, this includes:
• Diabetic acidosis
• Hyperchloremic acidosis
• Lactic acidosis.
Diabetic acidosis: Also known as diabetic ketoacidosis, is the buildup of ketone bodies due to poorly controlled blood sugar levels.
Hyperchloremic acidosis: Results from the body losing excessive quantities of sodium bicarbonate (often following diarrhoea).
Complications of alkalosis include:(29)
• Muscle twitching
• hand tremors
• Muscular spasms
• Numbness and tingling
• Nausea and light-headedness
• Vomiting
• Confusion.
ALKALOSIS
Alkalosis may transpire as a result of:(29)
• Fever
• Lack of oxygen
• High altitudes
• Lung disease
• Liver disease
• Salicylate poisoning.
Lactic acidosis: Results from excess lactic acid build up. This can be caused by prolonged exercise, excessive alcohol intake, liver failure, low blood sugar levels, lack of oxygen, or severe dehydration.(17)
BODY FLUIDS
IDENTIFYING AVERAGE pH LEVELS WITHIN THE DIGESTIVE SYSTEM
The stomach is typically acidic, with a pH of approximately 2 (ranging from around 1 to 3). This high level of acidity is essential because:
• It breaks down the food
• Kills any pathogens that may be in the food.
When various food reaches the stomach, it is then mixed with gastric juices to assist in breaking it down. The pH of hydrochloric acid is acidic (approximately a pH of 1-1.5), which aids in maintaining the sterile environment of the stomach.
Below is a table outlining the average pH of various parts of the digestive system, which can be expected in an average, healthy individual.(30)
SITE OF DIGESTIVE TRACT
GASTRIC SECRETION
SUBSTANCES
1.6-2.4
BILE 7.8-9.6
PANCREATIC SECRETION
INTESTINAL SECRETION
7.8-9.6
7.8-9.6 SALIVA
6.6-7.7
The image below shows the acidity levels across the digestive system. As the diagram demonstrates, the stomach is the most acidic, with a pH of 1-2.5, and as food moves through the small intestine and into the large intestine, it becomes more alkaline with a slight peak in acidity in the ascending colon.
Oesophagus
pH approximately 7.0
pH 2 pH 5 pH 7
Ascending colon
pH 5.26-6.72
Stomach
pH 1-2.5 (up to 5 when fed)
Proximal small intestine
pH 6.15-7.35
Descending colon
pH 5.20-7.02
Distal small intestine
pH 680-7.88
RECOGNISING WHEN STOMACH ACID pH IS TOO ALKALINE
If the parietal cells do not secrete enough stomach acid, stomach pH increases and becomes more alkaline (in other words, less acidic). When the stomach pH becomes less acidic, the breakdown of food becomes weaker/harder.
The body‘s goal is to keep chyme within the stomach until it reaches the right pH level. If acid production is too low, the stomach will be too alkaline, and food will sit in the stomach for longer than it should without breaking down.
Low stomach acid will also allow pathogenic bacteria to grow, which are fed by fermenting waste. The result is the body’s inability to absorb the nutrients contained within the food, leading to bacterial overgrowth and symptoms such as:
• Bloating
• Heartburn
• Gas from undigested food.
RECOGNISING WHESTOMACH ACID pH IS TOO ACIDIC:
An over acidic stomach acid pH will mean that the parietal cells are overproducing acid within the stomach. This makes the environment more acidic than is required, which may aggravate sensitive tissues of the GIT.
As a result, this can cause inflammation and damage, which can further result in issues such as:
• Kidney stones
• Muscle deterioration
• Cancer
• Liver disease
• Heart disease
• IBD.
Larger meals, or meals that are not adequately broken down through adequate mechanical digestion require larger volumes of gastric juices to process, affecting the stomach’s pH levels.
IDENTIFYING THE pH LEVEL OF COMMON FOODS
Consumption of a wide variety of foods will assist in ensuring dietary intakes are not excessively acidic or too alkalising. Different types of foods will have different acidity levels. Foods such as sugar, grains, dairy, and meat tend to have a higher acidity level, whereas green leafy vegetables, gluten-free grain, fats, mushrooms, and cabbage are much more alkaline. The table below provides a list of foods and their pH level:(15)
FOOD TYPE pH LEVEL
LEMON JUICE
2.00-2.35
2.00-2.80
2.80-3.40
2.90-3.82
3.00-3.75
3.20-4.00
3.69-4.34
3.30-3.60
5.20-6.80
5.30-6.60
5.90-7.50
6.00-6.70
UNDERSTANDING THE RELEVANCE OF BOWEL TRANSIT TIME
Bowel transit time (BTT) refers to the length of time taken from when food is ingested to it being evacuated out of the body. In other words, transit time refers to the time it takes for food to travel from the mouth through the digestive tract to the anus.(31)
Transit time is considered a critical factor in good health; when food makes its way through the GI tract, various harmful degradation products are produced, which are then evacuated safely as faeces. On the other hand, if transit time is impaired or slow, harmful degradation products remain in the body much longer than they should, which can result in toxins being absorbed into the bloodstream.(32)
Bowel transit times can also indicate general digestive health or the presence of conditions that may need to be addressed. As a nutrition coach, it is important to remember that a client’s diet will always be different from individual to individual, just as everyone’s digestive system is different, and both factors will directly affect BTT. What may be normal for one client may be entirely different for the next.(32)
Food transit time of a person on a Standard American Diet (low fibre). Average transit is 65-100 hours.
Food transit time of a person on a high fibre diet. Average transit is 20-45 hours.
RECOGNISING NORMAL TRANSIT TIME
A normal BTT is generally considered to be between 12 and 48 hours, or more practically, passing 1-2 bowel motions every 1-2 days. The human body is very diverse, and because a person’s lifestyle and body are all different, it is difficult to classify what is considered a ‘normal’ stool. However, there is an ‘ideal’ stool. Ideal stools are those which require no effort or straining to pass. This is usually referred to as Type 3 or 4 on the Bristol Stool Chart.(33) This chart is discussed on the following pages.
Abnormal or irregular stools are those which cause a feeling of pressure through the anal canal or involve straining. Abnormal also includes watery stools that contain too much fluid (such as diarrhoea).(34)
RECOGNISING SLOW TRANSIT TIME
Food that takes longer than 48 hours to pass is considered a slow transit time. A slow transit time can result in constipation or small, hard ‘pebble-like’ stools which are difficult to pass. This is a sign that food is sitting in the colon for too long and that waste products spend too long sitting in the intestines ‘rotting’. Waste products contain toxins: the more time this waste sits in the intestines, the more time toxins have to be reabsorbed into the bloodstream.(34)
A sluggish digestive system, particularly a sluggish colon, has been called Slow Transit Constipation (STC). STC comes about because as the waste moves slowly through the bowels, the body has more time to reabsorb water, leaving little water in the stool and causing many complications.(35)
There are numerous signs and symptoms of a slow transit time; these can include:(36)
• Abdominal pain
• Constipation
• Bloating
• Gas
• Indigestion.
• Straining to pass a motion
• A sensation of incomplete evacuation
• Irregular bowel motions
• Incontinence
• Nausea
• A poor appetite.
Research has found that those who suffer from chronic constipation are almost two times as likely to be diagnosed with colorectal cancer.(37)
RECOGNISING FAST TRANSIT TIME
Food that takes fewer than 12 hours to pass is typically unformed, loose, or soft. Food passing through the bowel too quickly may result in inadequate nutrient absorption in the small and large intestines, leading to ongoing lethargy, fatigue, nutrient deficiencies, and malnutrition.(38)
FACTORS THAT AFFECT BOWEL TRANSIT TIMING
As a nutrition coach, it is important to know the many factors that can affect bowel transit time. Some of these factors include:
• Diet
• Hydration
• Age
• Climate
• Lifestyle
• Stress
• Medications
• The liver
• Medical conditions
• Behavioural traits.
DIET
HYDRATION
AGE(39)
CLIMATE
LIFESTYLE
HYDRATION
An individual’s diet has a vast role in BTT as food that is consumed is the substance being processed. Certain types of food and nutrients take an extended time to break down compared to others, just as some are broken down more rapidly.
The speed at which food is broken down depends on the amount of fibre in the food and the complexity of its molecular structure. For example, the connective tissue of red meat and the fibrous parts of plant matter take longer to break down, given their more complex structure than something refined and processed, such as fruit juice. As a result, meat and fibrous matter will have a longer transit time than something more refined. Slower digestion due to complex food molecules allows the body additional time for nutrient absorption.
Hydration plays a crucial role in the digestive system as it helps to soften the stool for easier evacuation. Without enough water, stools can become hard, making them difficult to pass and potentially resulting in acute or chronic constipation.
The occurrence of chronic constipation can increase with age as a result of:
• The division rate of epithelial stem cells declines, making the digestive system more susceptible to damage.
• Smooth muscle tone decreases the strength of peristaltic contractions resulting in a slower movement of matter through the GI tract.
• Changes in other systems can affect digestive health, for example, damage or loss of teeth in the skeletal system, which may impact food choices and mechanical breakdown of food.
• Cumulative damage over many years to accessory organs can begin to affect their efficiency and productivity. For example, a sluggish liver as a result of excessive alcohol consumption over previous decades.
Seasonal variation may affect bowel transit time. Hot weather causes individuals to lose more fluid, increasing the risk of constipation secondary to decreased fluid in the digestive system.
Changing seasons will ultimately affect the foods chosen for consumption; for example, cold juices and smoothies may be consumed in warmer months, while in colder months, fibrous soups and casseroles may be preferred.
Moderate to high-intensity physical activity is suggested to speed up bowel transit time by stimulating the digestive system. In the same way, immobility can result in a sluggish digestive system, increasing the risk of chronic constipation.
Hydration plays a crucial role in the digestive system as it helps to soften the stool for easier evacuation. Without enough water, stools can become hard, making them difficult to pass and potentially resulting in acute or chronic constipation.
STRESS
MEDICATIONS
THE LIVER
Studies have shown that prolonged mental stress that increases anxiety levels can increase bowel transit time.(40) Chronic diarrhoea may also be linked to anxious personality traits.
It has been shown that different parts of the GI tract are affected differently by different types of stress.(40)
The digestive system may respond to stress in a variety of ways including:(41)
• Inhibiting defecation
• Increasing intestinal transit time
• Stimulating large bowel contractions
• Increasing oesophageal motor activity and contractions.
Different types of medications can potentially slow bowel transit time or in contrast, speed it up. For example, laxatives and enemas help to evacuate bowel motions, however if taken in excess can cause unwanted diarrhoea. Other medications or supplements, such as fibre supplements, work to add bulk to the stool to prevent diarrhoea; however, may cause constipation if taken in excess.
The liver is an important accessory organ in digestion, and if it is not working efficiently or effectively, it will have direct repercussions on transit time. BTT, metabolic regulation, haematological regulation, and bile production are all intrinsically linked to liver function. Longer bowel transit times also increases the burden of toxins on the liver.(42)
MEDICAL CONDITIONS
BEHAVIOURAL TRAITS
Medical conditions such as thyroid disorders, liver disease, pancreatic cancer, and bowel resections are likely to result in a slower and more sluggish transit time. Which part of the digestive system is affected and how dietary intake should be adapted will depend on the disease.
Behavioural traits, such as delaying passing a bowel motion or forcing a bowel motion to move is not encouraged as it may result in issues such as a haemorrhage (ruptured blood vessel which can lead to blood in the stools) or faecal impaction.

APPROPRIATE TESTING PROTOCOLS FOR NUTRITIONAL ADVISORS
TO TEST
BOWEL TRANSIT
TIME
A simple, non-invasive, and cost-effective way for a nutrition coach to identify the transit time of their client’s bowels is to utilise indigestible or colourful foods, such as corn, beetroot, or sesame seeds. A nutrition coach can use this method to identify a client’s BTT whilst still ensuring that they stay within their professional scope of practice.
TESTING INSTRUCTIONS USING INDIGESTIBLE OR COLOURED FOODS:
METHOD
Ask the client to consume 1 cup of corn kernels or beetroot or 5-10 charcoal tablets (read the safety guidelines on the specific box of charcoal tablets) with a meal. Ensure the client records the exact time and date at which the meal was consumed.
Note: It can be useful to encourage the client to do this first step with a meal directly following a bowel motion.
MONITOR:
Over the next 120 hours (5 days), ask the client to observe their stool and write down the time they first see the corn, beetroot, or a black motion.
RECORD:
The nutrition coach or the client can calculate the hours between the first meal and the time the first change was observed in their bowel motion to identify their BTT.
ANALYSE:
After identifying the BTT of the individual client, this information can then be used to identify whether or not the client presents with a slow or fast BTT.
RECOGNISING CHARACTERISTICS OF A CLIENT’S STOOL
SIZE AND CONSISTENCY (BRISTOL STOOL CHART)
Medical practitioners formulated the Bristol Stool Chart (shown below) as a clinical assessment tool to classify stools based on seven categories. The Bristol Stool Chart allows clients to easily provide information about their bowel motions, which assists the nutrition coach in their recommendations.(34)
The Bristol Stool Chart categorises bowel motions into seven different types, ranging from hard, pebble-like motions through to liquid motions. Showing clients the below infographic will allow them to easily identify which type of bowel motion most closely resembles their own motions. This will make it easier for the nutrition coach to get a thorough understanding of what sort of bowel motions a client is experiencing and as such, what their bowel motions may be indicating.(34)
BRISTOL STOOL CHART
1 Separate hard lumps/pellets, often shaped like nuts (hard to pass/abrasive).
Overall shape is like a sausage/log, however, the appearance is chunky/lumpy texture (hard/painful to pass).
2
5
3
4
In the shape of a sausage/ log with cracks on its surface (often soft).
Overall shape like a sausage or snake, with a smooth and soft texture.
Similar to ‘type 1’, however, the shape/texture of this stool is soft blobs with clear-cut edges (easily passed).
These lumps/pellets are typically painful to pass and can indicate that the stool has moved too slowly through the bowels and the client is constipated. It is best if this type of stool does not occur frequently.
This type of stool may be caused by a lack of fibre and/or bacteria, which means there is nothing to retain water in the stool. This could also be an indication of inadequate fluid intake.
As with type 1, this could also be an indication of inadequate fluid and/or fibre intake.
This type of stool can also be a possible sign of mild/slight constipation and a slow bowel transit time that ideally shouldn’t occur on a regular basis. It can often cause pain during elimination due to its size exceeding the maximum opening of the anal canal.
Clients can often have feelings of incomplete bowel motions, abdominal pain and/or bloating. Constipation can lead to straining and the development of haemorrhoids, in which nutritional advisors should refer their clients if they present with regular or constant constipation (chronic constipation).
This is considered as a ‘normal’ type of stool, especially if it’s somewhat soft and easy to pass. Often a sign of a healthy bowel motion.
This type of stool is easy to pass, also an ‘ideal’ or ‘normal’ stool, likely passed 1-3 times a day. Often a sign of a healthy bowel motion and/or adequate fibre intake.
The consistency of this stool is soft, which could suggest mild diarrhoea. This type of stool typically contains excess liquid and can potentially indicate a lack of fibre/vegetable intake.
5
Similar to ‘type 1’, however, the shape/texture of this stool is soft blobs with clear-cut edges (easily passed).
Fluffy pieces with ragged edges (a mushy stool/too soft).
6
7
Watery, no solid pieces (the stool is entirely liquid).
The consistency of this stool is soft, which could suggest mild diarrhoea. This type of stool typically contains excess liquid and can potentially indicate a lack of fibre/vegetable intake.
The consistency of this stool is too soft, which could be a potential sign of mild diarrhoea. This can indicate inflammation or be a possible sign of a hyperactive colon due to stress or an inadequate diet.
Clients can often have feelings of faecal urgency or incontinence issues with their stool at this point on the scale.
This type of stool typically indicates that a client may have diarrhoea (often referred to as ‘the runs’). This can mean that the stool has moved through the bowels too quickly and wasn’t given enough time to form into a healthy stool.
This may indicate too much water in the small intestine, causing stools to be spread throughout the length of the intestine. Diarrhoea can also be the result of anxiety, inflammation, a food allergy, medication, or a long-term condition, such as irritable bowel syndrome (IBS). A nutritional advisor should refer their clients if they present with regular or constant diarrhoea as prolonged diarrhoea may lead to malnourishment and/or dehydration.
EDUCATING CLIENTS ON THE VARIOUS TYPES OF STOOLS
It will be useful for nutrition coaches to educate their clients on what constitutes a healthy stool and the possible reasons why some stool types are considered abnormal or less healthy than others.
The most common and ideal stool types are types three and four from the Bristol Stool Chart, as they are easier to pass, indicating that the diet typically contains sufficient fibre and fluid for good stool formation.(34)
Depending on a person’s health status, diet, and fluid intake, type one, two, and five stools become more common where fibre and fluid are insufficient to form ideal stools or where gastrointestinal issues such as IBS, constipation, haemorrhoids or abnormal bowel flora exist.(34) Addressing these issues can help rectify the problem to enable proper stool formation over time; however, nutrition coaches should always ensure that they refer their clients to the appropriate medical professional if they fall outside their scope of practice.
Type six and seven stools are the least common and usually indicate diarrhoea, gastrointestinal illness (such as food poisoning), malabsorption, or a hyperactive colon due to stress or diet. Again, identifying and addressing the underlying potential cause of impaired digestive function can help to rectify stool formation to the ideal type, as long as it falls within the scope of a nutrition coach.(43)

IDENTIFYING THE VARIOUS COLOURS OF STOOL
While the Bristol Stool Chart focuses on the size and consistency of stool, the colour of a client’s stool can also indicate issues within the gastrointestinal tract. A stool can come in a range of different colours, in which various shades of brown are considered the ‘normal’ colour of a stool and a slight green colour is also considered to be ‘normal’.
The colour of a client’s stool is largely influenced by what they eat and the amount of bile pigment (a greenish-yellow fluid that digests the fat in the stool). As this bile pigment passes through the gastrointestinal tract, it is chemically adjusted by enzymes, which change the pigments from green to brown.
Bilirubin pigment is the reason for the various shades of brown in the stool:(10)
• It is a yellow pigment compound found in the blood and stool.
• It is created from the breakdown of red blood cells in the body.
• When the body has too much bilirubin, an individual’s skin and the whites of their eyes will start to yellow (a condition known as jaundice).
• After circulating in the blood, bilirubin travels to the liver, where it is processed and mixed into bile. After this, it is excreted into the bile ducts and stored in the gallbladder. Eventually, the bile is delivered into the small intestine to aid in the digestion of fats and ultimately excreted within the stool.
If the stool begins to veer towards other various colours, this can indicate a potential concern. Should a client report any discolouration or abnormality in the colour of their stool, nutrition coaches are recommended to refer their client to the most appropriate medical health professional (i.e., a general practitioner).
The image below provides a basic overview of the various colours of stool and their possible meaning:
An indication that the client has eaten a lot of greens, which are potentially passing too fast.
• An indication that the client has eaten licorice
• Potential indication of iron supplements or other medication
• Potential bleeding in the upper intestinal tract.
Considered to be ‘normal’ Ideal colour.
Any shade of brown
• Potential bleeding n the lower intestine. Potential sign of a blocked bile duct.
• An indication that the client has eaten red food
• Hemorrhoids
• Too much fat in the stool
• Malabsorption
• Possible concern for coeliac disease.
A little green
Super green
Black Pale, white, clay-coloured
Red
Yellow
UNDERSTANDING THE ROLE OF BACTERIA IN DIGESTIVE HEALTH
Our gut microbiota plays a pivotal role in digestion and immunity. Bacteria live in the nose, skin, and ears and reside in the human gut. It is estimated that the digestive system contains up to 35,000 different species of bacteria, all of which work symbiotically to perform several important roles.(44)
GUT MICROBIOTA
Gut microbiota is the preferred term used by scientists when referring to the bacterial microorganisms that inhabit the digestive tract, with microbiota, human gut bacterial ecosystem, and gut bacteria also considered correct terminology.(45) The term gut microbiome is an overlapping term and refers to the gut bacteria or ‘bugs’ and their genes. The terms ‘flora’ and ‘gut flora’ (which you may have heard of) are sometimes used; however, this is older, inaccurate terminology. The terms gut ‘bugs’ and ‘friendly’, ‘good’ or ‘bad’ bacteria may be used for ease of understanding; though not technically correct, these are acceptable.
Gut bacteria assist in nutrient metabolism, drug metabolism, structural maintenance of the gut mucosal barrier, and protection against unwanted bacteria, viruses, and pathogens.
Overall poor gut health has been associated with a number of conditions, these include:(44)
• Inflammatory bowel disease
• Irritable bowel syndrome
• Obesity
• Diabetes
• Allergies.
FUNCTION OF GUT MICROBIOTA
As briefly described above, gut microbiota plays several key roles in the human body, including:(46)
• The metabolism of nutrients
• Drug metabolism
• Protection against pathogens
• Structural support.
The table below briefly summarises how gut microbiota works in various roles.(44)
• Assists with lipid metabolism by enhancing lipase activity and upregulating colipase, an enzyme required by pancreatic lipase for lipid digestion
NUTRIENT METABOLISM
DRUG METABOLISM
IMMUNITY
PROTECTION
STRUCTURAL SUPPORT
OTHER BENEFITS
• Assists in protein metabolism
• Synthesises vitamin K and several components of vitamin B
• Assists in the breakdown of polyphenols.
• Metabolises xenobiotics (chemical substances not naturally produced by humans) and drugs
• Inactivates poisonous substances such as digoxin.
• Assists in normal homeostasis
• The shaping of immune lymphoid tissues
• Essential for development and function of certain cells in the intestines.
• Maintains the structure and function of the GI tract
• Contributes to the structural development of gut mucosa.
• Improves energy levels
• Improves cholesterol levels
• Regulates hormones
• Supports a healthy weight
• Reduces yeast infections.
BACTERIAL DIVERSITY
It is becoming more widely understood that a healthy and diverse range of gut microbiota is linked with the health of its host. The greater the number of healthy bacteria and the diversity of bacterial species, the better the host’s health. Gut microbiota in children as young as three years old closely resembles the gut microbiota of an adult.(44)
Healthy gut microbiota is predominantly made up of two major bacterial phylum (Firmicutes and Bacteroidetes), followed by the bacterial phylum Actinobacteria and Verrucomicrobia. It is interesting to note that more than 70 percent of all bacteria found in the human body are located in the colon.(44)
With over 35,000 different species of bacteria inhabiting the human body, the image below focuses on the dominant bacteria found throughout the digestive system, from the oesophagus to the colon.(44)
Oesophagus pH < 4.0
Bacteroides, Gemella, Megasphaera, Pseudomonas, Prevotella, Rothia sps., Streptococcus
Colon pH 5-5.7
Bacteroides, Clostridium, Prevotella, Porphyromonas, Eubacterium, Ruminococcus, Streptococcus, Enterobacterium Enteroccus, Lactobacillus, Peptostreptococcus, Fusobacteria
Caecum pH 5.7
Lachnospira, Roseburia, Butyrivibrio, Ruminococcus, Fecalibacterium, Fusobacteria
Stomach pH 2
Streptococcus, Lactobacillus, Prevotella, Enterococcus, Helicobacter pylori
Small intesine pH 5-7
Bacteroides, Clostridium, Streptococcus, Lactobacillus, Proteobacteria, Enterococcus
RECOGNISING FACTORS THAT IMPACT GUT MICROBIOTA
Given the influence of the diet and environment on the digestive system, it is important that a nutrition coach also develops a sound understanding of the potential impacts of negative digestive behaviours on overall health.
Several major factors can affect bacterial diversity. These factors are outlined in the below table:
The mode of birth (vaginal or caesarean) will affect an infant’s baseline microbiota profile. When an infant is born, a vaginal birth will cover the infant in a protective layering which has been found extremely protective for gut health later in life.
CHILDBIRTH AND INFANCY
DIETARY AND NUTRITIONAL IMPACTS
In addition to this, the initial food chosen for the infant, either breast milk or formula, will greatly impact bacterial diversity too. Breast milk is the most natural source of nutrition for an infant and is full of healthful bacteria. Abnormal colonisation of microbiota established during childbirth and infancy may result in a number of paediatric diseases, secondary to poor immunity.
The diet is the most influential factor shaping the diversity and composition of gut microbiota. Because the bacteria feed off fibre, a diet rich in a variety of fruit and vegetables results in a healthy microbiota. Cultural dietary differences will affect bacterial diversity within each individual.
For example, as seasons come and go, it has also been found that gut microbiota changes as a result of seasonal dietary changes. For example, an individual may consume more salad and fibrous vegetables in summer and more starch and red meat in winter, thus affecting the food available for the bacteria to feed off.
THE IMPACT OF ANTIBIOTICS
Antibiotics, while necessary in certain situations, if used frequently can result in both short- and long-term consequences for an individual’s gut microbiota. Antibiotics work to kill unwanted bacteria; however, result in killing both the bad and good bacteria. As a result, an individual taking antibiotics may have a decreased amount of good bacteria in their digestive system. This can have negative long-term effect on the overall bacterial diversity, colonisation, and composition. This may result in poor nutrient absorption and utilisation, as well as decreased immunity.
It is often encouraged that a course of probiotics is taken alongside the course of antibiotics, or immediately afterwards. It is important to be mindful that probiotics should be taken at least two hours away from antibiotics, as otherwise, the antibiotics will kill the beneficial bacteria provided by the probiotics. In addition, a nutritional advisor can also encourage the consumption of a prebiotic and probiotic-rich diet including fibrous vegetables, fermented foods, nuts, and seeds to help recolonise and restore the gut microbiome.
Probiotics refer to the bacteria which live in the gut. Probiotics are used as a collective term for all the different species of bacteria, not just a single species. Ingesting probiotics assists in enhancing the diversity and composition of the gut microbiota. Probiotics are also available as dietary sources from fermented foods such as sauerkraut, kombucha and kimchi, and naturally fermented yoghurts, or they can be purchased in a capsule or powder form.
PROBIOTICS
PREBIOTICS
When looking at capsulated or powdered forms of probiotics, it is important to consider the range of bacteria and look for the one with more living bacteria, as this will be the most effective. The two major strains of bacteria in supplements are Lactobacillus and Bifidobacterium. It is encouraged that probiotic rich foods are consumed in conjunction with a healthy, balanced diet.
Prebiotics, on the other hand, are essentially the ‘food’ for the probiotics. Prebiotics are consumed as part of a healthy, well-balanced diet, which in turn feeds the bacteria living in the gut. Prebiotics are the indigestible parts of carbohydrates, known as fibre. Prebiotic-rich food is primarily fibrous foods such as fibrous vegetables (e.g., celery, dark green leafy vegetables, and asparagus), the skin and seeds of fruits, and the husk of nuts and seeds.
IDENTIFYING BEHAVIOURS AND LIFESTYLE FACTORS THAT CAN NEGATIVELY IMPACT THE DIGESTIVE SYSTEM

The composition of an individual’s diet and environment can significantly impact overall health, whether positive or negative. As the digestive system is in a state of balance between good and bad bacteria, lifestyle factors such as smoking, lack of exercise, stress, and obesity can significantly reduce the ability of the digestive system to achieve key functions.
By understanding the factors that can negatively impact the digestive system, nutrition coaches can help guide their clients toward choices that can improve their digestive health.
There are several factors that can significantly impact the digestive system, and these include:
• Poor dietary choices (meal timing, meal composition, and eating style)
• Inadequate water intake/hydration
• Inadequate dietary fibre intake
• Excessive intake of alcohol and smoking
• Sedentary lifestyles
• Acute or chronic stress
• Bacterial imbalances
• Genetic factors (such as age, gender, and ethnicity).
These factors are discussed in more detail on the following pages.
UNDERSTANDING THE IMPACTS OF POOR DIETARY CHOICES ON THE DIGESTIVE SYSTEM
Poor eating habits can affect digestion; therefore, it is important to consider the food’s composition and the client’s physical eating habits. The speed at which food is consumed and how it is chewed before swallowing are some of the factors to consider, among others, outlined in the table below:
MEAL TIMING
• The timing and structure of meals can impact digestion. For example, eating too close to bedtime or exercising can cause indigestion and gastric reflux.
• Irregular eating patterns can result in eating larger meals which can make it difficult for the body to completely digest food products. This is a factor which is often compounded by the behavioural trait of poor meal selection during periods of hunger.
MEAL COMPOSITION
EATING STYLE
• Meals high in fat, spice, or caffeine can impact circadian rhythms, resulting in poor sleep and a failure to fully digest meals.
• Additionally, consuming too much fluid during a meal can dilute the stomach acids, making it more difficult or time-consuming to break down food within the gut.
• Poor physical eating habits, such as eating too quickly, eating too much food in one sitting, or even something as simple as not chewing food properly, can result in bloating and abdominal pain or discomfort.
• Some people tend to swallow air whilst eating (perhaps due to talking or chewing with their mouth open) which can result in excess gas being trapped in the gastrointestinal system, resulting in belching or flatulence.

UNDERSTANDING THE IMPACTS OF INADEQUATE HYDRATION
A nutrition coach needs to be aware that water intake is critical in the digestion process. The GI tract absorbs and secretes about 8-10L of fluid daily, with about 1.5L absorbed by the colon and 100mL lost within the stool daily. Beyond the immediate requirement for the body to maintain hydration for proper function, water is also responsible for softening stools to allow smoother and easier transition through the GI tract and out of the body.(47)
Through periods of dehydration, the body may prioritise water retention and therefore not provide sufficient fluid for healthy stool composition, leading to conditions such as constipation. For this reason, people are advised to drink 3035mL of water per kg of body weight.(48) For example, a 70kg woman would require 2.1-2.4L of water for proper hydration.
WATER AIDS THE DIGESTION SYSTEM
UNDERSTANDING THE IMPACTS OF INADEQUATE DIETARY FIBRE INTAKE
Dietary fibre, the indigestible component of plant foods such as fruit, vegetables, and grains, is another key element for healthy digestion. Fibre assists in softening stools and moving waste through the digestive tract efficiently, with the added benefit of binding to dietary cholesterol to help remove it from the body.(1)
As a nutrition coach, it is important to be aware that low fibre diets may result in constipation and subsequent haemorrhoids (a result of straining). Low fibre diets also cause diverticulosis, an asymptomatic condition where small pouches (diverticula) develop in the colon. This condition may develop into diverticular disease. Diverticular disease is where the diverticula become inflamed or infected (diverticulitis) causing symptoms (outlined in the diagram below).(1)
DIVERTICULITIS
Traverse colon
Ascending colon Appendix
Small intestine
Sigmoid colon
Descending colon
Diverticulosis
DIVERTICULOSIS
Diverticulosis occurs when small defects in the muscle of the wall of the large intestine or colon allow small pockets or pouches (diverticula) to form.(49)
While low fibre diets may be recommended for the recovery of the GI tract in some health conditions, chronic low fibre intake can result in:(1)
• An increased risk of reduced bowel microbiota diversity
• Gut inflammation
• Obesity
• Impaired immune function.
Diverticula
Diverticula infected or inflamed
UNDERSTANDING THE IMPACTS OF SMOKING AND EXCESSIVE ALCOHOL CONSUMPTION ON
THE DIGESTIVE
SYSTEM
THE EFFECTS OF SMOKING
Smoking increases the risk of many GI tract cancers, including mouth, oesophagus, stomach, pancreas, colon, and rectal cancers.(50)
Smoking may also contribute to common disorders of the GI tract, including:(51)
• Heartburn
• Gastro-oesophageal reflux disease (GORD)
• Peptic ulcers (shown in the image below)
• Crohn’s disease
• Pancreatitis
• Gallstones.
Smoking and airborne toxins are believed to reach the bowel via mucociliary clearance from the lungs, which may contribute to conditions such as inflammatory bowel disease.(51)
THE EFFECTS OF EXCESSIVE ALCOHOL CONSUMPTION
Excessive alcohol consumption can interfere with nutrient digestion and absorption since the liver prioritises the metabolism of alcohol over other nutrients. Over time, chronic alcohol consumption may result in various alcohol-related diseases, including cirrhosis (liver disease) and fatty liver disease.(52)
MUCOCILIARY CLEARANCE
Mucociliary clearance in the lung is a critical and physiologically regulated protective function of the airways and lungs that is essential for the clearance of respiratory pathogens.(53)
Mucociliary clearance is the primary innate defence mechanism of the lung. The functional components are the protective mucous layer, the airway surface liquid layer, and the cilia on the surface of ciliated cells.(54)
Oesophagus
UNDERSTANDING THE IMPACTS OF A SEDENTARY LIFESTYLE ON THE DIGESTIVE SYSTEM
While most people know of the link between diet and exercise concerning weight, the link between a sedentary lifestyle and poor digestive health is often overlooked. When an individual does not get sufficient exercise, and cardiovascular health begins to suffer, the body is often unable to divert sufficient blood flow to the digestive system efficiently. This can lead to fatty build-up around major organs and may also result in an inefficient process for transporting critical vitamins, minerals, and nutrients around the body to where they are required.(55)
Additionally, spending too much time being immobile in a seated position can lead to challenges in the body’s ability to smoothly move waste through the digestive system. As a result, an individual may encounter symptoms such as constipation, bloating, or potentially more severe conditions stemming from a build-up of waste or fatty products throughout the digestive tract.(56)
Sedentary behaviour has been linked to increased risk of developing:
• Type 2 diabetes mellitus
• Gastrointestinal and colorectal cancer
• Gallstones (shown in the image below).
GALLSTONES (Cholelithiasis)
Gallstones
Gallbladder
Common bile duct
Duodenum
Pancreatic duct
A stone in the common bile duct
UNDERSTANDING THE IMPACTS OF STRESS ON THE DIGESTIVE SYSTEM
The negative impacts of stress on the body have also been well documented and are often identified as a contributing factor in a number of chronic health conditions.(57) It is important for nutrition coaches to be aware that individual reactions to stress may vary significantly and may be compounded by other elements within the lifestyle.
Prolonged mental stress that increases anxiety levels can increase bowel transit time with chronic diarrhoea linked to anxious personality traits.(58) Alterations to gut microbiota can also occur due to stress, with disturbances to various species and their number (increase or decrease in bacterial count) residing in the gut.(58)
The digestive system is filled with nerves of the sympathetic nervous system (and controlled by the ANS), which regulates digestion. Stress responses can affect the homeostasis of the ANS, disrupting digestive function and can result in the following:(59)
• Altered stool motility
• Decreased blood flow to the GI tract
• Increased intestinal permeability
• Altered (increased or decreased) stomach acid
• Decrease in serotonin production
• Impairs absorption of nutrients
• Increases inflammation
• Can cause stomach pain, diarrhoea, and nausea.

Pituitary gland
Adrenal gland Cortisol Adrenaline
UNDERSTANDING THE IMPACTS THAT BACTERIAL IMBALANCES CAN HAVE ON THE DIGESTIVE SYSTEM
Whilst a constant balance of good and bad bacteria is working within the digestive system, some bacteria are damaging to health.
The table below outlines some examples of bacteria that are particularly damaging to the digestive system, and includes:
Salmonella infection is usually caused by eating raw or undercooked meat, poultry, eggs, or egg products.
Shigella infection (shigellosis) is an intestinal disease and causes bloody diarrhoea.
Yersinia is an infection as a result of eating raw or undercooked pork.
Vibrio cholera is a disease common in countries with poor water and food sanitation. Cholera results in diarrhoea which can be fatal if untreated.
Campylobacter is a common form of food poisoning from eating raw or undercooked poultry or drinking contaminated water, resulting in diarrhoea, cramps, fever, and vomiting.
E.Coli is a type of bacteria that usually lives in the intestine of animals and humans; however, it can be found in food products through cross-contamination.
There are good E. coli and bad E. coli. Some live in the gut and help the body to stay healthy; others can cause serious disease, even death!
SALMONELLA
SHIGELLA
YERSINIA
VIBRIO CHOLERAE
CAMPYLOBACTER
ESCHERICHIA COLI (E.COLI)
The bacteria outlined in the above table are particularly dangerous and may lead to symptoms such as:(60)(61)
• Vomiting
• Cramps
• Dehydration
• Permanent intestinal damage.
These bacteria may even lead to death in severe cases or within high-risk groups, such as children or the elderly.(60)(61)
Other harmful bacteria may be found in lower numbers within the digestive system as part of general bacterial populations without causing concern; however, when harmful bacteria are larger in numbers than good bacteria, it does become a cause for concern. Examples may include:
• Citrobacter
• Enterobacter
• Klebsiella
• Proteus
• Serratia
• Pseudomonas.
The bacteria in the list above may contribute to various forms of irritable bowel syndrome (IBS) or other similar conditions; however, at a minimum, they may lead to:
• Gas
• Bloating
• Abdominal pain
• Issues with irregular bowel motions.
In some instances, this may be due to their inability to adequately break down matter within the digestive system, while in other instances, it may stem from their production of gases during the breakdown process.

UNDERSTANDING PERSONAL CHARACTERISTICS AND GENETIC FACTORS ON DIGESTIVE HEALTH
The function and long-term health of the digestive system can be influenced by several personal characteristics and genetic factors, outlined in the table below:
As humans age, digestive function changes and begins to decline, resulting in the increased risk of nutrient deficiencies and physical complications with parts of the gastrointestinal tract.(62)
One example of this is the condition diverticulosis which becomes more common over the age of 40. Diverticulosis is where small pouches develop in the intestine wall, possibly due to weakening gastrointestinal muscles. Food particles can become lodged inside the pouches (called ‘diverticula’) and can become inflamed, creating the acute condition called diverticulitis. Diverticulitis can be extremely painful, often requiring medical attention to resolve. A low fibre diet is recommended to manage the flare-up causing diverticulitis, whereas a high fibre diet is recommended once recovered as a prevention strategy.(63)
AGE
GENDER
ETHNICITY
Some older adults over the age of 65 are susceptible to deficiencies in vitamin B12. This is due to a reduction in the stomach’s ability to produce intrinsic factor, an enzyme that assists with the absorption of the vitamin B12. This can result in reduced energy levels and can lead to anaemia if left untreated.(64)
Gastric motility and absorptive ability also slow with age, resulting in slower transit of food through the gastrointestinal tract and increasing the likelihood of constipation and other bowel problems (impacted bowel, infections, and reduced nutrient and drug absorption).(65)
Reflux becomes more prevalent with age due to the weakening of the sphincter muscles that separate the stomach and oesophagus.(66)
Very few gender differences exist that affect digestive function and health. It appears that there are male-female differences in gastric emptying, with women experiencing slower gastric emptying than men.(67) Women are also at higher risk of developing conditions like Irritable Bowel Syndrome.(68)
Ethnicity can play a role in digestive differences between people and countries, with differences in the risk of experiencing digestive illnesses, allergies, and intolerances being higher in some groups.(69)
Lactose intolerance is a common issue for as much as 65 percent of the human population; however, its prevalence is higher for people of East Asian, West African, Jewish, Arab, Greek, and Italian descent.(70)
Cultural differences between ethnic groups can also play a role in a person’s microbiome, environmental hygiene, and nervous system, resulting in a different response to similar exposures in the same environment. For instance, some Caucasian travellers develop ‘traveller’s diarrhoea’ (or gastroenteritis) in response to pathogen-containing food or water in a foreign country, where a local inhabitant eating the same food would not experience gastrointestinal upset from the same exposure.(71)
Illnesses like coeliac disease, peptic ulcer disease, and diverticular disease also appear to affect some ethnicities more than others; however, the development of illness is multifaceted, and many factors play a role in the development of disease over a lifetime.(72)(73)
IDENTIFYING APPROPRIATE NUTRITION, LIFESTYLE, AND DIETARY CHOICES TO SUPPORT A HEALTHY DIGESTIVE SYSTEM
This unit has highlighted the importance of GIT and gut health for healthy digestion. Therefore, it is essential that an individual maintains appropriate nutrition for healthy digestion. A nutrition coach can educate a client and help enable dietary changes to best support digestion.
A nutrition coach can support their clients to improve or maintain their digestive health by educating and guiding them towards healthy choices. Some techniques/strategies include:
1. Encouraging clients to consume whole foods
2. Ensuring adequate consumption of fibre
3. Ensuring adequate intake of fluid
4. Supporting clients to exercise regularly
5. Educating clients about eating before sleep/bedtime
6. Educating and encouraging clients to maintain a healthy weight
7. Supporting clients to manage stress and incorporating relaxation techniques
8. Educating clients on the implications of smoking and alcohol intake
9. Encouraging appropriate mastication while eating meals (chewing food properly)
10.Educating clients about the use and benefits of gut-supporting nutrients/supplements where needed (probiotics, prebiotics, glutamine, and zinc)
11. Encourage and support clients to consume all macronutrients (protein, fats, and carbohydrates).
ENCOURAGING CLIENTS TO CONSUME WHOLE FOODS
ENCOURAGING ADEQUATE CONSUMPTION OF FIBRE
Encourage clients to consume a healthy and well-balanced diet consisting of various whole foods from each food group. Whole foods should be emphasised for their health benefits as they contain essential nutrients in their whole form that are often reduced when processed, especially highly processed; educate the client on the importance of fibre-rich whole foods.
Regarding what is consumed to support digestion, it is important to start eating sufficient fibre. The fibre in vegetables not only acts as a prebiotic for gut bacteria but also adds bulk to the stool, slowing the digestion of sugars and improving satiety. Encourage clients to fill half their plate with fibrous vegetables to ensure adequate fibre intake.
Some examples of highly fibrous fruit and vegetables include:
• Berries (strawberries, raspberries, blackberries, blueberries)
• Dark leafy greens (broccoli, cabbage, green beans).
Nutrition Australia and Dietitians Australia both recommend an acceptable fibre intake for adults (over 18 years) of 25-30 g per day.(74)(75)
A 2018 review article(76) investigated dietary fibre intake in Australia and found the following:
• The most recent Australian survey found that most Australians are not meeting recommended fibre intake
• Specific groups were least likely to meet fibre targets (14-18-year-old children/ adolescents, young adults 19-30 years, and men of all ages)
• Low socioeconomic groups of all ages
• The issue is global, with most countries across 76 studies (children and adults) not meeting recommendations
• Adolescents are the highest risk group, with low dietary fibre habits likely to follow them into adulthood.
ENCOURAGING ADEQUATE INTAKE OF FLUIDS
SUPPORTING CLIENTS TO EXERCISE REGULARLY
EDUCATING CLIENTS ABOUT EATING BEFORE SLEEP/ BEDTIME
EDUCATING AND ENCOURAGING CLIENTS TO MAINTAIN A HEALTHY WEIGHT
SUPPORTING CLIENTS TO MANAGE STRESS AND INCORPORATE RELAXATION TECHNIQUES
EDUCATING CLIENTS ON THE IMPLICATIONS OF SMOKING AND ALCOHOL INTAKE
Encourage clients to consume adequate fluids based on their weight, activity level, and season and to reduce their intake of fluids that may negatively impact hydration, such as highly caffeinated beverages (energy drinks) and alcohol.
To increase water intake, drinking soda water or adding a squeeze of lemon or lime to non-carbonated water can help increase palatability. Setting regular reminders to drink may help some people get into better habits.
Encourage clients to reach physical activity recommendations (approximately 30-60 minutes of moderate to high-intensity cardiovascular exercise daily and 1-2 resistance training sessions per week), reminding them that physical activity can improve BTT and decrease the likelihood of acute or chronic constipation.
Encourage clients to leave a gap of at least 60 minutes (or greater) between their last meal of the day and sleeping (or lying down) to allow time for food to leave the stomach and be fully digested, reducing the risk of indigestion, heartburn, and reflux.
Clients may also benefit from eating a smaller meal in the evening, which will take less time to digest.
Encourage clients to achieve a healthy body weight through dietary changes focusing on fibre-rich, unprocessed foods. This can help improve digestion by improving overall diet quality and reducing stress on the digestive system created by excess body fat
Encourage clients to take time for themselves and relieve stress. This may be talking to a trusted person, a referral to a health professional, taking time out to do an enjoyable hobby, or even taking a nap. Remind clients of the distress caused to the digestive system by high-stress levels.
Encourage clients to reduce and eventually give up smoking by contacting their GP for cessation support and encourage alcohol reduction or changes in purchasing habits.
ENCOURAGING APPROPRIATE MASTICATION WHILE EATING MEALS
Mastication (chewing) is a physiological process controlled by the central nervous system and modulated by inputs from the mouth. During meals, it is important to ensure that an individual eats at an appropriate speed and chews their food properly to provide a solid foundation for initial mechanical digestion. Because the food is exposed for a longer time to the saliva when chewed properly, the digestive enzymes in the saliva allow a greater breakdown of the food. Therefore, making digestion easier on the stomach and small intestine allows for better absorption of energy and nutrients.
In addition, science has found that eating slowly, and chewing food properly, has beneficial effects for reducing caloric intake and assisting in weight maintenance/loss. Research has shown that when food is eaten slowly, total caloric intake is lower, and satiation is higher compared to those consuming food quickly.(77)
It is often encouraged to put the knife and fork down between mouthfuls to ensure food is chewed at least 32 times or to have the food in the oral cavity for at least 30 seconds before swallowing. While there is no hard and fast rule, it is important to ensure that food is chewed properly to allow longer exposure to salivary digestive enzymes and better mechanical digestion.
EDUCATING CLIENTS ABOUT THE USE AND BENEFITS OF GUT SUPPORTING NUTRIENTS/ SUPPLEMENTS WHERE NEEDED (PROBIOTICS, PREBIOTICS, GLUTAMINE, AND ZINC)
For most people, the remaining digestive system requirements can be met through the consumption of a healthy and balanced diet and limiting consumption of unhealthy options such as foods that are deep-fried or high in sugar or trans fat. In some instances, probiotic-rich foods and supplements can assist in providing a balance of the gut microbiota.
Probiotics, as defined by the Food and Agriculture Organisation of the United Nations World Health Organisation, are: “live microorganisms which when administered in adequate amounts confer a health benefit on the host.” When referring to food sources of probiotics, the definition can be adjusted to emphasise that the beneficial effect is exerted by the microorganisms “when consumed in adequate amounts as part of food”(78)
PROBIOTICS:
As probiotics are better understood, they are becoming more widely used in the prevention and treatment of gastrointestinal infections and antibiotic-associated diarrhoea diseases. Probiotics work to inhibit the growth of pathogens, secrete antimicrobial substances, and are involved in toxin inactivation too. While these can be consumed in capsule form, they are also found in fermented food such as sauerkraut, kombucha, kimchi, kefir, and certain yoghurts.
As probiotics are live bacterial cultures, their benefits vary significantly based on the type of bacteria being consumed. Some probiotics provide a positive benefit for the digestion of foods, while others are natural immunity boosters.
PREBIOTICS:
In addition to the beneficial effects of probiotics, it is also important to look at and ensure adequate consumption of prebiotics: A type of non-digestible dietary fibre known as prebiotic fibre that is especially beneficial for gut health.(79) This fibre feeds the good bacteria in the GIT, allowing them to proliferate (increase in number).(80)
Good bacteria are highly beneficial for improving digestive health; therefore, including prebiotic foods within the diet can be helpful.
Prebiotics are found in fibrous foods, including:(81)
• Apples
• Onions, spring onions and shallots
• Leek
• Asparagus
• Garlic
• Cooked then cooled rice (resistant starch)
• Oatmeal
• Banana (unripe or as green banana flour)
• Jerusalem artichoke
• Chicory
• Fennel bulb
• Green peas.
A balanced diet containing prebiotics and probiotics will maintain a healthy balance of bacteria within the digestive system and assist in the breakdown of food and ensure a healthy and functional immune system.
GLUTAMINE:
Glutamine is an amino acid that assists with the maintenance and support of the intestinal lining. It is mainly found in animal products (such as chicken, beef, milk, and yoghurt), and sufficient intake will help maintain healthy digestive function.(82)
ZINC:
Zinc is essential for healthy digestion as it helps maintain the lining of the intestine (improves barrier function), is required for the action of enzymes, and regulates insulin production, storage and release, among many other uses.(83)
ENCOURAGE AND SUPPORT CLIENTS TO CONSUME ALL MACRONUTRIENTS (PROTEIN, FATS, AND CARBOHYDRATES)
Each macronutrient can have a different effect on digestive health, depending on the type of food or composition of the meal they are found in. For instance, a protein-only meal with no carbohydrate or fat accompanying it may result in excess gas production and small, hard stool formation. A fat only meal may result in fast gastrointestinal transit and loose stools.
Learning about how each macronutrient affects the gastrointestinal tract can help nutrition coaches understand why some foods affect the gut in specific ways.
PROTEIN:
Proteins take longer to be digested than carbohydrates because of their complex structures. Consuming protein alone and in large quantities can result in excess gas production due to the amount of time it spends in transit through the GIT being fermented by gut bacteria.
CARBOHYDRATES:
Carbohydrates are the fastest digesting macronutrient because of their simple structure. They are completely digested and absorbed in the small intestine, leaving only indigestible fibre to be fermented in the large intestine. However, consuming large quantities of simple carbohydrates can cause GI upset in some people due to overwhelming the GIT or where digestive issues (like coeliac disease) exist.
FATS
Fats are the slowest digesting macronutrient because of their often complex structure. Saturated and trans-fats are digested the fastest, followed by mono and polyunsaturated fats. Fats are usually fully digested and absorbed by the time they reach the end of the small intestine unless malabsorption occurs due to illness or disease.

RECOGNISING
DIGESTIVE HEALTH CONCERNS AND CONDITIONS AND REFERRING
CLIENTS
AS REQUIRED
IDENTIFY DIGESTIVE CONCERNS WITHIN THE NUTRITIONAL ADVISOR’S SCOPE OF PRACTICE
A nutrition coach can work with a range of mild digestive issues that clients may be experiencing. Identifying a condition based on the reported signs and symptoms and working through an effective treatment strategy will enable clients to manage and resolve their digestive issues.
If a client’s symptoms persist, the nutrition coach must refer the client to a GP or dietitian for further assessment.
The conditions that are suitable for nutrition coaches to work with include:
• Constipation
• Diarrhoea.
UNDERSTANDING CONSTIPATION
Constipation is a common digestive issue that can be a consequence of issues such as:(84)
• Poor hydration
• Lack of dietary fibre (or excessive intake)
• Medication usage
• Poor gut motility
• Food intolerances
• Lack of physical activity
• Lack of certain digestive enzymes
• Ignoring the urge to pass a motion.
Constipation produces bowel movements that are infrequent or consist of dry, hard stools. Stools become dry because food moves slowly through the digestive tract, resulting in more water being absorbed from the stool by the colon, making stools small, hard, pebbly, and often hard to pass.(85)
There are two types of constipation: acute (sudden) or chronic (ongoing). A nutrition coach can work with clients experiencing the acute form.(86)
Acute constipation refers to a sudden and noticeable hardening, difficulty in passing, and reduced frequency of stools, whereas chronic constipation persists for several weeks to months. Chronic constipation usually produces a bowel motion less than once per week. If a client presents with chronic constipation or progresses from acute to chronic, the nutrition coach must refer the client to a GP or APD for further assessment.(87)
FOOD ALLERGIES AND INTOLERANCES
LACK OF DIGESTIVE ENZYMES
LACK OF DIETARY FIBRE
CAUSES OF CONSTIPATION
Certain food types may be more difficult for some people to digest, which can slow BTT. Typical problem foods include dairy, yeast, nuts, gluten/wheat, and artificial sweeteners.(88)
Many adults lack the digestive enzyme lactase required to digest milk. Therefore consuming dairy products can result in symptoms such as constipation or bloating.(1)
Fibre is required to bulk out the stool so that it is easy for the digestive system to move the bolus along the intestines. All clients are encouraged to consume the recommended 25-30g of fibre per day.(87)
Being physically active has the potential to aid in gut motility. In contrast, being sedentary slows the digestive system down. Nutrition coaches can encourage clients who live sedentary lives and suffer from constipation to take up aerobic exercises such as a gentle walk or a swim.(89)
LACK OF PHYSICAL ACTIVITY
NICHE
Denoting products, services, or interests that appeal to a small, specialised section of the population.(2)
Certain types of medications are known to cause constipation, for example:(87)
• Pain relievers
• Antidepressants
• Anticonvulsants
• Calcium channel blockers
MEDICATIONS
• Antacids
• Diuretics.
If suffering from constipation, nutrition coaches should encourage the client to speak with their doctor as they may need to decrease certain medications or take medications spaced apart to avoid any interactions.
DEHYDRATION
CHANGES TO ROUTINE
IGNORING THE URGE
Stools containing less water are more likely to become harder and, therefore, more difficult to pass. Therefore, nutritional advisorsnutrition coaches should always encourage their clients, especially clients suffering from constipation, to consume adequate fluid throughout the day.(91)
When the body’s normal routine is interrupted, this too can cause constipation. For example, changes to a sleep routine, eating meals at different times, travel or traumatic life events may all impact the digestive system and BTT.
Delaying or postponing the necessity to pass a bowel movement can ultimately, over time, cause the body to stop creating the urge altogether. This can be consequential down the GIT as faeces can build up in the rectum and colon and may result in haemorrhoids from straining to pass the motion.
• Soluble fibre such as psyllium can help relieve both constipation and diarrhoea.(92)
• Overusing laxatives can cause further constipation.
• Laxatives are an effective way to treat occasional constipation but can lead to dependence if used regularly.
However, it is important to remember that a nutrition coach cannot prescribe laxatives to a client; only a medical professional can recommend a client to use laxatives.
SUPPORTING CLIENTS WITH ACUTE CONSTIPATION
Several strategies can be recommended to support clients struggling with acute constipation. The following recommendations are safe, non-invasive, and likely to provide relief quickly.
RECOMMENDATION
HYDRATION
INCREASE FIBRE
EXERCISE
SUPPLEMENT RECOMMENDATIONS
EXPLANATION
The amount of water the body needs daily varies from person to person depending on their current health condition, diet, physical activity, the environment, and many other contributing factors. Generally, drinking a minimum of 6-8 glasses of water per day is recommended.(91)
Nutrition coaches can support their clients by increasing their intake of soluble and insoluble fibre from fruits and vegetables.
Increasing soluble fibre can assist with acute constipation as it absorbs water, making faecal matter softer and easier to pass. However, it is important to ensure that the client drinks plenty of water with soluble fibre intake. Otherwise, it can lead to further constipation.(91)
Moderate aerobic exercise such as swimming or brisk walking can assist with acute constipation by stimulating the bowels, aiding in constipation as it causes the intestines to move waste along more quickly.(91)
MAGNESIUM:
Magnesium is vital for healthy muscle function and muscular contractions, and relaxation. These movements allow the digestive tract to function properly. Magnesium also helps to relieve muscle stress and tension.
PROBIOTICS:
For healthy digestion in the large intestine.
ESSENTIAL FATTY ACIDS:
Essential fatty acids (EFA) are precursors to the prostaglandin hormones, which help to keep the bowels functioning regularly. Purified fish oil is the most concentrated source of EFAs, along with oils from chia seeds and flaxseeds.
Foods containing healthy fats include:
• Avocado
• Nuts
• Salmon
• Flaxseeds.
DIGESTIVE ENZYMES:
Digestive enzymes may aid in the digestion of food before it reaches the colon, allowing for faster transit and more efficient waste elimination.
UNDERSTANDING DIARRHOEA
DIARRHOEA
Diarrhoea is frequent (>3 times per day) passing of watery or liquid stools.
Most instances of diarrhoea are categorised as acute diarrhoea (short-term). Acute diarrhoea can be described as three or more loose or watery stools, occurring for 14 days or less, with a sudden onset. This is often due to an infection or parasites in the gut. In these instances, the body attempts to expel (eject) the harmful bacteria as quickly as possible.(93)
Chronic (or persistent) diarrhoea is described as episodes of diarrhoea lasting 14 days or more. Chronic diarrhoea is typically a sign of illness such as bowel inflammation, IBS, motility disorders, and malabsorption, and as a result, these conditions can ultimately lead to serious health problems such as nutritional deficiencies and electrolyte imbalance.(94)
WHAT CAUSES DIARRHOEA?
Diarrhoea can be caused by several different factors, including(94):
• Bowel infections (i.e. viruses, bacteria, or parasites).
• Stress and anxiety
• Food intolerance or allergy
• Certain medications
• Bowel irritability
• Inflammatory bowel disease (IBD)
• Hyperthyroidism
• Pancreatic disorders.
The image below depicts the difference between a ‘normal’ or typical stool travelling through the digestive tract in contrast to how diarrhoea would travel through (at a faster pace).








Stool



NORMAL









DIARRHOEA
Body reabsorbing water
Excess water in stool. Body cannot reabsorb water
SUPPORTING CLIENTS WITH ACUTE DIARRHOEA
While chronic diarrhoea will generally require a referral to a more suitable medical or health professional, there are still strategies a nutrition coach can implement to help clients manage acute diarrhoea.
The table below provides a list of recommendations that a nutrition coach may suggest to support their clients who are suffering from acute diarrhoea:
RECOMMENDATION
HYDRATION
INCREASE FIBRE
SUPPLEMENT RECOMMENDATIONS
EXPLANATION
Nutrition coaches can support their clients by ensuring they maintain fluid intake to reduce the risk of dehydration. Encourage clients to keep their fluid intake at a minimum of 2L per day and increase further with the severity of diarrhoea.
If diarrhoea persists, it may be necessary to encourage clients to replenish electrolytes to replace lost minerals.
Just like with acute constipation, nutrition coaches can support their clients by increasing their intake of soluble fibre such as chia seeds, flaxseeds, and psyllium husk powder.(92)
Soluble fibre is helpful for diarrhoea as it absorbs excess water and helps to bulk out the watery stool, slowing down bowel transit time. Soluble fibre can help by slowing down the transit time of the gut, soaking up more fluid and producing better-formed stools.
PROBIOTICS:
Certain strains of probiotics, such as Saccharomyces boulardii (commonly referred to as S. boulardii), have been shown to treat acute diarrhoea by balancing the natural microbiota of the digestive system. S. boulardii may be present in dairy products, fermented foods and beverages such as kefir or as a supplement.(95)
UNDERSTANDING THE DIFFERENCE BETWEEN FOOD ALLERGIES AND FOOD INTOLERANCES
Nutrition coaches are likely to encounter clients with various food allergies and intolerances. Knowing the difference between allergies and intolerances and how to approach them is extremely important as nutrition coaches need to know how to help clients seeking assistance or identify those who need referring to other specialists.
Research demonstrates that food allergies and intolerances are increasing, particularly among children. Below are some theories on why allergies and intolerances are becoming more common.(96)
GENETICS
Parents with the genes for food allergies will pass them on to their children. If both parents possess the genes for a food allergy, the risk of expression of the allergy increases for the child. As generations continue, the genes spread amongst the population and expression becomes more prevalent.
DIET
It has been suggested that the increase in processed food in the diet has contributed to a lower intake of nutrients, which reduces the immune system’s ability to function properly. The foods commonly eaten also contain a higher amount of allergens, such as gluten and peanuts. How foods (such as wheat) are processed differs from how they were processed 50 years ago.
Many people are unaware of the difference between food intolerances and food allergies, particularly as the signs and symptoms of each are often common to both.
ARE TWO DIFFERENT THINGS
A food allergy is an immediate immune system reaction that affects the body and may potentially be severe or even life-threatening. Allergies are the body’s immune system overreacting to allergens such as proteins in foods where they are treated as if they were toxic. On the other hand, a food intolerance is a chemical reaction to a food or drink rather than an immune response. An individual can experience symptoms a few minutes to a few days following ingestion of the offensive food.
UNDERSTANDING FOOD ALLERGIES
A food allergy occurs due to an immune system reaction to allergens that are harmless to other individuals. Most food allergies are caused by one of the ten most common allergens, including eggs, peanuts, soy, milk, wheat, fish, shellfish, tree nuts, sesame, and lupin; however, any food can trigger an allergic reaction in an individual.(96)
Individuals who suffer from food allergies may struggle with any number of the following symptoms:(96)
• Itching, burning, and swelling around the mouth
• Swelling of face or eyes
• Runny nose
• Skin rash (eczema)
• Hives (urticaria - skin becomes red and raised)
• Diarrhoea
• Abdominal cramps/pains
• Breathing difficulties, including wheezing and asthma
• Vomiting
• Nausea.
UNDERSTANDING FOOD INTOLERANCES
Food intolerance is a chemical reaction to a food or drink. An individual can experience symptoms from a few minutes to a few days following ingestion. Typically, consuming small amounts of the food may not trigger an effect in some individuals; however, others may need to avoid the offending food altogether.(97)
Food intolerances may stem from one of a number of factors, such as:(98)
• The absence of an enzyme required to fully digest a type of food (i.e. lactose intolerance)
• A sensitivity to a type of food or a food additive (gluten intolerance)
Reactions to a food intolerance can include rashes, hives, stomach pain, bloating, flatulence, diarrhoea irritable bowel symptoms, asthma, a runny nose, lethargy, headaches, and migraines.(99)
DIAGNOSING A FOOD INTOLERANCE OR ALLERGY
As previously discussed, it is paramount to identify offending foods as their consumption can result in profound detrimental effects to the health of the client and their digestive tract. To correctly diagnose an allergy or intolerance, it is important to undergo testing by a qualified professional to isolate the element causing the reaction. It is outside the scope of practice for a nutrition coach to diagnose food intolerances or allergies.
DIAGNOSING FOOD ALLERGIES
Food allergies are complicated to diagnose, and if the nutrition coach or client suspects a food allergy, a referral must be made immediately for professional support. Unlike food intolerances, food allergies are generally lifelong and can sometimes be life-threatening.(99)
While some clients identify food allergies simply by consuming an unknown offending food, others may go through Immunoglobulin E (IgE) mediated testing using skin pricks on either the forearm or the back. This testing exposes the client to a very small amount of different proteins and identifies an immune response through red and itching skin.(100)(99)
This type of testing can only be done by a qualified health professional, such as a general practitioner.
Allergen
solution is placed on skin
Positive test: Skin is red and itchy
DIAGNOSING FOOD INTOLERANCES
Food intolerances can occur at any age, and a person can even develop an intolerance to a food they have previously been able to consume without problems. For example, an individual who has consumed dairy their entire life may begin reacting to it later in life and as a result, may need to decrease or eliminate their consumption of dairy.
In addition, individuals may also find that certain foods which cause a reaction now may no longer affect them later in life, leaving them to enjoy that food as part of a healthy diet again. In the event of food intolerance, improving the digestive system may minimise the impacts or address the underlying condition of food intolerances.
Typically, symptoms from food intolerances may appear immediately or take a few days to appear and can be dosedependent. For example, an individual with a wheat intolerance may consume a small amount of wheat each day with no ill effect; however, they may experience symptoms if they consume wheat more than once a day.
There are several ways to diagnose food intolerances, all of which need to be carried out by a qualified health professional such as a general practitioner.
STAYING WITHIN THE SCOPE OF PRACTICE AS A NUTRITION COACH (ALLERGIES AND INTOLERANCES)
It is outside the scope of practice for a nutrition coach to diagnose an allergy or intolerance. This is because diagnosing conditions requires clinical knowledge, equipment, or procedures not taught at the Certificate IV level. The use of diagnostic tools, measures, and interpretation of the results can only be carried out by medically qualified persons such as dietitians, pathologists, and doctors.
IDENTIFYING CHRONIC DIGESTIVE HEALTH
CONDITIONS WHERE A REFERRAL IS REQUIRED
A nutrition coach is limited practically and legally in their ability to provide nutritional advice to individuals with chronic health conditions. Upon identifying that an individual has or is at risk of having a chronic digestive health issue, it is important to refer the individual to a qualified medical professional who will be able to assist the client in diagnosing and treating the condition.
In the previous section of this resource, food allergies and intolerances were discussed, both of which are chronic conditions requiring support. As outlined, the diagnosis of these conditions requires specialist testing and individuals suspected of having one of them should be referred to a GP or an APD to undergo further examination.
Some other chronic conditions include:
• Coeliac disease
• Crohn’s disease
• Gastrointestinal permeability (leaky gut)
• Gastritis
• Ulcerative colitis (UC)
• Gastro-oesophageal reflux disease (GORD)
• Irritable bowel syndrome.
[These conditions are further explained on the following pages]

UNDERSTANDING COELIAC DISEASE
WHAT IS COELIAC DISEASE?
Coeliac disease is an autoimmune condition in which gluten triggers a severe reaction from the immune system in susceptible people.(101) When gluten is ingested, it unnaturally passes through the tight junctions in the intestinal wall. As a result, the immune system recognises these proteins as a threat and produces antibodies to attack them. Unfortunately, these antibodies attack the delicate lining of the bowel and other tissues, causing inflammation and deterioration of the intestinal cells. Coeliac disease is usually diagnosed by serological tests (to detect antibodies associated with coeliac disease) by endoscopy or colonoscopy of the small intestine, along with a biopsy.(101)
To ensure a diagnosis can be made early and not left untreated, nutrition advisors must refer clients presenting with the following symptoms of coeliac disease:(101)(102)
• Abdominal pain
• Nausea
• Diarrhoea
• Constipation
• Anaemia
• Vomiting and diarrhoea following consumption of gluten-based foods.
DAMAGE CAUSED BY COELIAC DISEASE
The small intestine is lined with millions of tiny finger-like hairs called villi. On top of the villi are micro-villi, which make up the brush border lining of the gut. Microvilli increase the gut’s surface area and allow the absorption of nutrients from food. Inflammation caused by gliadin in gluten can damage microvilli to the point where they reduce in size and become flat, known as villous atrophy. Once damaged in this way, the microvilli are less able to absorb nutrients properly. The gut lining also becomes more permeable, which means potentially harmful substances can pass into the bloodstream. Therefore, there is an increased risk for both nutrient deficiencies or further intolerances as a result of micro-villi and villi damage. This is why, for those who have been diagnosed with coeliac disease, adhering to a gluten-free diet is critical, as regrowth of intestinal villi can occur 12-24 months after strictly following a gluten-free diet.(103)
WHAT IS GLUTEN?
Gluten is the generic name for proteins found in wheat, including durum, semolina, spelt, rye and barley. Gluten is a mixture of two proteins, gliadin and glutenin. When combined with water, gluten becomes sticky and acts as a glue to hold foods together. Gluten is present in many of the foods we eat, even those we wouldn’t expect. Modern food production uses gluten because it produces a lighter, softer texture in cakes, biscuits and pastries. The current treatment for individuals with coeliac disease is to strictly avoid all foods containing gluten, including foods that may be crosscontaminated.(101)
COMMON GLUTEN-CONTAINING FOODS
• Bread
• Baked goods: biscuits, cakes, pastries
• Soups
• Pasta
• Cereals
• Sauces and dressings
• Beer
• Confectionary
• Processed foods.
INTESTINAL LUMEN
LAMINA PROPRIA
CELIAC DISEASE
Gliadin
Glutenin
Microvilli
Flattened microvilli
UNDERSTANDING CROHN’S DISEASE
Crohn’s disease is characterised by uncontrolled inflammation anywhere along the GI tract from the mouth to the anus. Crohn’s disease is a condition that falls within the group of conditions known as inflammatory bowel disease (IBD). The cause of Crohn’s disease is not yet understood; however, it is known that it can occur at any age and affects both men and women equally. Research suggests that genetically susceptible individuals may develop Crohn’s disease due to environmental factors that trigger inflammation, which include smoking, poor diet and medications.(104) Further, stress and dietary factors may aggravate the disease; however, they are not the cause.
Symptoms of Crohn’s disease will vary for individuals, however common symptoms include:
• Abdominal pain
• Urgency to move bowels
• Persistent diarrhoea
• Constipation, which may lead to bowel obstruction
• Sensation of an incomplete bowel evacuation
• Rectal bleeding
CROHN’S DISEASE
As this is a chronic condition, it may develop further over time and lead to complications in other areas of the body due to the decreased ability to absorb essential nutrients and vitamins.
Cobblestone appearance of mucosal surface Most commonly involves the end of small intestine and the beginning of the colon
creeping fat
CROHN’S DISEASE
UNDERSTANDING INCREASED INTESTINAL PERMEABILITY (AKA, LEAKY GUT SYNDROME)
PERMEABLE
Permeable refers to a property of a membrane or channel pore in allowing substances to pass through.
The lining of the gut is naturally permeable, and this is how nutrients pass into the bloodstream. The term intestinal permeability refers to how easily various substances can pass through the intestinal wall. In a normal gut, the cells lining the GIT are in control of substances that enter the bloodstream. Substances that pass through the cells then enter the bloodstream, where they are transported throughout the rest of the body.
The cells in the GIT lining work as gatekeepers by:
1. Acting as a barrier to prevent harmful substances such as antigens, toxins, and other invaders entering the bloodstream.
2. Acting as a selective filter to aid the uptake of nutrients, electrolytes, water, and other beneficial substances from the intestines.
The lining of the gut is naturally permeable. The term ‘increased permeability’ or ‘hyperpermeability’ is used when too many substances (including harmful substances) are able to pass through the barrier.
PHYSIOLOGY OF THE EPITHELIAL BARRIER (GUT LINING)
The lining of the intestinal wall comprises cells joined together in a series of tight junctions. Tight junctions are tiny gaps that allow water and nutrients to pass into the bloodstream but block harmful substances. However, when these tight junctions are damaged or weakened, they cannot do their job correctly. The junctions may become loose and thus more permeable, allowing bacteria and toxins to pass into the bloodstream.(105)(106) This is commonly referred to as leaky gut. Although widely publicised on the Internet, leaky gut syndrome is a hypothetical condition unrecognised and not entirely proven in medical studies.
LEAKY GUT: REAL OR NOT?
Although commonly blamed as the cause for many allergies and autoimmune diseases, leaky gut syndrome is not a medically recognised condition. The lack of scientific evidence for leaky gut syndrome means there are no specific diagnostic methods or treatments. However, medical professionals agree that increased intestinal permeability or hyperpermeability may be a factor in certain chronic diseases.(107)
Current research links gastrointestinal permeability to a wide range of chronic health conditions such as:
• Allergies
• Autoimmune disease
• Skin disorders (such as eczema)
• Food sensitivities
• Fatigue
• IBS.
In essence, increased intestinal permeability involves the tight junctions within the intestines (i.e. the points that allow the passage of elements into the bloodstream) failing to function effectively and therefore allowing the passage of toxins, microbes, and undigested food to pass into the blood. This is effectively called a ‘leaky gut’ and is shown in the image on the page below.
Paracellular Transcellular Pathogens
Food allergen
Increased gastrointestinal permeability may result from a number of factors, such as:
• An imbalance of gut bacteria
• Excessive sugar consumption
• Excessive intake of alcohol or other drugs
• Nutritional deficiencies
• Inflammation.
GUT BACTERIA IMBALANCE
EXCESSIVE SUGAR CONSUMPTION
EXCESSIVE INTAKE OF ALCOHOL OR OTHER DRUGS
An imbalance of gut bacteria may result in a condition known as dysbiosis. This is when there are potentially more bad bacteria than good bacteria or an overgrowth of a particular form of bacteria in the digestive system.
Regular sugar consumption has been shown to damage the tight junctions of the gut lining. Fructose is the worst offender, potentially causing intestinal bacterial overgrowth and increased intestinal permeability.(108)
Chronic or excessive use of non-steroidal anti-inflammatory drugs (NSAIDs) and alcohol are linked to increased intestinal permeability and cause significant GI damage, such as:(109)
• Ulcers
• Perforation
• Haemorrhage
• IBD.
NUTRITIONAL DEFICIENCIES
INFLAMMATION
Deficiencies in vitamins and minerals such as vitamins A and D and zinc appear to increase susceptibility to poor barrier function.(110)
When inflammation is chronic (continues over a long time), tissues will be damaged, resulting in increased permeability.
Any one or a combination of multiple of the above factors may result in the weakening of the tight junctions and therefore allow unwanted material to pass into the blood.
UNDERSTANDING ULCERATIVE COLITIS
Ulcerative colitis is often confused with Crohn’s disease as it typically presents with similar symptoms and refers to an inflammation of the GI tract. It is typically limited to the large bowel (colon and rectum) and only in the surface layers.
Common symptoms of ulcerative colitis may include:
• Diarrhoea
• Fever
• Fatigue
• Abdominal pain
• Blood in the stool
• Reduced appetite
• Weight loss
• Mouth sores
• Sores or ulcers in the lining of the bowel.
Ulceration within the mucosa
Surviving mucosa
Loss of haustra
Haustra (the small pouches)
Healthy mucosa
NORMAL COLON
ULCERATIVE COLITIS
UNDERSTANDING GASTRITIS
Gastritis is a condition that involves inflammation of the stomach lining on varying scales. In some individuals, the symptoms may be mild and heal on their own accord, while others may last for several years (acute vs chronic).
Typically, Gastritis stems from bacterial infection and can potentially weaken the lining of the stomach leading to further damage from the body’s natural stomach acids.
Symptoms of gastritis often include:
• Burning pain in the upper stomach area
• Nausea
• Vomiting
• A feeling of unnatural fullness after eating.
Healthy mucosa Inflammation of the lining
NORMAL GASTRITIS
UNDERSTANDING GASTRO-OESOPHAGEAL REFLUX DISEASE
Gastro-oesophageal reflux disease (GORD) is commonly referred to as reflux or acid reflux. It is typically caused by a complication or difficulty with the lower oesophageal sphincter (LOS), the muscle at the bottom of the oesophagus. The LOS opens to allow fluid and food to travel into the stomach and acts like a valve by closing to prevent acid from leaking out of the stomach (shown in the image below).
While it is common for individuals to experience reflux from time to time, it is considered GORD when it occurs more than twice a week for a consistent period.
Oesophagus
Diaphragm
Stomach
HEALTHY STOMACH
Lower oesophageal sphincter
GORD STOMACH
Lower oesophageal sphincter open allowing acid reflux
There are a variety of factors that can cause or increase the risk of developing GORD. These factors can include:
• An individual’s family history of GORD
• Smoking and alcohol
• Excessive amounts of caffeine
• Consuming large meals
• Consuming particular food and fluids that cause aggravation
• Some medications
• An individual who is overweight or obese
• Consuming large amounts of fatty foods (due to the stomach taking longer to dispose of stomach acids)
• Pregnancy
• Stress.
ACID REFLUX
Typical signs and symptoms of GORD can include:
• Heartburn (when an individual experiences discomfort after eating or a burning feeling rising from the lower chest or stomach)
• Regurgitation (when an individual experiences stomach acid travelling back up to the mouth, causing a sour/ unpleasant taste to occur)
• Pain and difficulty when swallowing.
To assist in reducing the symptoms of GORD, a nutrition coach can encourage their clients to adopt the following selfcare measure:
• Eat food in an upright position
• Remain in an upright position for at least 60 minutes following eating
• Lose weight (if indicated)
• Avoid trigger foods and fluids (such as coffee, carbonated drinks, citrus foods, spicy foods, fatty foods, tomatobased)
• Avoid or limit alcohol and smoking
• Consume smaller, more regular meals throughout the day.
• Consume food and fluids separately, rather than drinking and eating at the same time
• Avoid eating or drinking right before exercise
• Time meals appropriately and avoid eating directly before going to bed (waiting anywhere from 60 mintues to two hours).
Nutrition coaches can support and encourage self-care measures with their clients. However, if symptoms persist or worsen, the client must be referred to an appropriate health professional (i.e., a doctor or Accredited Practising Dietitian).

UNDERSTANDING IRRITABLE BOWEL SYNDROME (IBS)
Irritable bowel syndrome (IBS) is a condition that affects the healthy functioning of the bowel. The underlying cause of IBS is unknown; however, many factors can contribute to triggering IBS in susceptible individuals.
Contributing factors can include:
• The bowel becoming more overactive than usual (which can lead to an individual feeling sensation that they would not normally feel)
• Gastrointestinal infections
• Stress and anxiety
• Certain types of foods
• Hormonal changes
• Chronic inflammation of the bowel
• Problems with digestion (a transit time that is too slow or too fast)
• Abnormal contractions in the bowel (shown in the image below).
The symptoms of IBS can come and go over time and differ depending on the individual. Typically, IBS is used as a broad diagnosis capturing the ongoing presence of the following symptoms:
• Constipation
• Diarrhoea
• Abdominal pain, cramping or discomfort (often relieved after passing a stool or ‘wind’)
• Excessive flatulence
• Stomach bloating.
Diarrhoea does not always present as urgent and explosive (known as faecal urgency) and may be in the form of regular stools but not in the proper size, shape, or consistency. Less than half of IBS patients are estimated to present with diarrhoea; in some instances, clients may alternate between diarrhoea and constipation.
With constipation, most people should have at least one normal bowel movement each day; however, if less frequent than this, then it may characterise constipation. Stools during constipation are typically dry and hard and may not pass in one sitting, resulting in multiple attempts to pass a single full bowel movement. Passing a bowel motion may also be painful and may cause bleeding.
Abnormal contractions
Bowel
Abdominal pain often varies significantly for clients with IBS and may not be present in many cases. Abdominal pain often overlaps with those individuals encountering bloating. Bloating is not necessarily accompanied by gas; however, it can lead to visible signs such as a swollen stomach.
IBS is diagnosed by a medical professional (i.e., doctor) using a process of ‘exclusion, meaning that diagnosing IBS is usually provided after a patient has been cleared of a number of serious gut health conditions, including:
• Ulcerative colitis
• Crohn’s disease
• Coeliac disease
• Lactose intolerance.
Medical professionals need to exclude the above conditions as they can do permanent damage to the lining of the intestine and colon and present serious health complications if not identified.
Due to the variation in symptoms experienced by individuals suffering from IBS, it is divided into four categories based on the individual’s predominant symptoms:
1. IBS-D (diarrhoea predominant IBS)
2. IBS-C (constipation-predominant IBS)
3. IBS-Mixed (a mixture of diarrhoea and constipation IBS)
4. IBS-U (undetermined type of IBS).
The most common problem foods for those with IBS include:(111)
• Milk and lactose-containing products
• Artificial sweeteners
• Alcohol
• Vegetables from the brassica family (cabbage, broccoli)
• Legumes
• Onions and garlic
Individuals with IBS may benefit greatly from completing the FODMAP protocol to identify which foods they may be reacting to.

KNOWLEDGE AND APPROPRIATE USE OF DIETARY PROTOCOLS AIDING IN DIGESTIVE HEALTH
UNDERSTANDING FODMAPS
The Low FODMAP protocol was devised by a team of researchers from Monash University in Melbourne to reduce the symptoms associated with IBS. Dietitians and doctors now use it as one of the most popular management plans for IBS.
WHAT ARE FODMAPS?
Constipation is a common digestive issue that can be a consequence of issues such as:(84)
• Poor hydration
• Lack of dietary fibre (or excessive intake)
• Medication usage
• Poor gut motility
• Food intolerances
• Lack of physical activity
• Lack of certain digestive enzymes
• Ignoring the urge to pass a motion.
FODMAPs are short-chain carbohydrates with chains of up to 10 sugars, some of which are poorly absorbed in the small intestine.(112) Instead of being absorbed, these sugars pass through the digestive tract to the large intestine where they start to ferment and cause some of the problems associated with IBS: gas, bloating and pain.
FODMAPs is an acronym used to describe these sugars. The low-FODMAP diet is often used in clinical management plans for IBS in suitable candidates. It is vital to note that the low-FODMAP diet should only be followed under the guidance and supervision of an accredited practising dietitian as it is outside the scope of practice for a nutrition coach. (113)(114) The information provided in this section is to provide nutrition coaches with an awareness of the contributing factors that may present in consultations to help to identify the need to refer a client to an APD.
FODMAPs
Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols.
FERMENTABLE:
Fermentation is the process through which bacteria break down the undigested short-chain carbohydrates, resulting in gases.
OLIGOSACCHARIDES:
Oligosaccharides include fructans (fructooligosaccharides or FOS) and galactooligosaccharides (GOS). Humans don’t have the digestive enzymes to break these sugars down, so they are not absorbed in the small intestine, which is particularly problematic for individuals with IBS.
Foods containing fructans (fructooligosaccharides or FOS):
• Artichokes (globe, Jerusalem)
• Garlic (in large amounts)
• Leek
• Onion (brown, white, Spanish, onion powder)
• Spring onion (the white part) and shallots
• Wheat, rye, and barley (in large amounts)
• Inulin.
Foods containing galactooligosaccharides (GOS):
• Beans (e.g. baked beans, kidney beans)
• Lentils
• Chickpeas
DISACCHARIDES:
These include lactose (present in milk), which comprises two sugar units that need to be broken down by lactase, a digestive enzyme. Many people lose or have reduced lactase enzymes as they grow older and become lactose intolerant.
Foods containing lactose:
• Milk
• Yoghurt
• Soft cheeses
• Ice cream
• Foods produced using milk products (for example, salad dressings and soups).
MONOSACCHARIDES:
Monosaccharide foods with more fructose than glucose are included in this category. As glucose acts as a carrier for fructose, it can assist fructose across the intestinal membrane to be absorbed. If more fructose than glucose is consumed, the glucose cannot carry the fructose, so it is less likely to be absorbed.
Foods containing high levels of fructose:
• Apples
• Melons (cantaloupe, rock melon, honeydew)
• Corn Syrup, Fruit
• Juice Concentrate
• Guava
• Honey and agave syrup
• Lychee
• Mangoes
• Pears (regular and nashi)
• Persimmon
• Quince
• Dried figs and dates.
POLYOLS:
Sugar alcohols such as sorbitol and mannitol, often used as artificial sweeteners in lollies or chewing gum. The absorption of polyols is slow or often incomplete.(115)
Food products containing polyols:
• Apples
• Apricots
• Nectarines
• Pears
• Plums
• Prunes
• Mushrooms
• Hard confectionary
• Chewing gum
• Dried fruits
• Frozen desserts
• Baked goods
• Sugar alcohols: erythritol, sorbitol, mannitol, xylitol, maltitol, lactitol and isomalt
FRUCTOSE MALABSORPTION
Fructose malabsorption occurs when there is a deficiency of the transporters GLUT-5 and GLUT-2 that enable fructose to be absorbed. If not absorbed, the fructose continues through the intestines to the colon, where harmful bacteria break it down and create gases and bloating, flatulence and diarrhoea.(116)
HOW THE LOW FODMAP DIET WORKS
The FODMAP diet plan excludes all foods high in FODMAPs for a short period to allow the gut to heal. FODMAPs can then be gradually reintroduced according to individual tolerance.
A typical program involves:
• Reducing or excluding all high-FODMAP foods for 6-8 weeks or until symptoms improve.
• Substituting high-FODMAP foods with low-FODMAP foods.
• After the elimination period, small amounts of high FODMAP foods are reintroduced. The aim is to build up a tolerance level that allows as much variety in the diet as possible.
WHO SHOULD FOLLOW A LOW FODMAP DIET?
A FODMAP diet is intended for people with medically diagnosed IBS. If a medical doctor has not diagnosed gastrointestinal symptoms, a client should not follow this diet as there are many conditions with symptoms similar to IBS, such as coeliac disease, inflammatory bowel disease, bowel cancer and endometriosis.(117) The low FODMAP protocol is gaining popularity in the general community; therefore, nutrition coaches may come across clients who have selfdiagnosed themselves and decided to implement this diet.
In these situations, it is important for nutrition coaches to educate their clients about the diet, especially because the elimination phase of the diet is not designed for longevity. This is largely due to the elimination of FODMAPs leading to a low fibre intake, which can negatively impact the variety of the gut microbiome.
Suppose a client has commenced a FODMAP diet. In that case, a nutrition coach should encourage them to seek the support of a dietitian or GP to ensure they have been screened for coeliac disease, IBD and lactose intolerance before completing the protocol. If a nutrition coach suspects that clients of this nature require medical clearance before they continue treatment, then this is strongly encouraged. Taking extra precautions is also recommended when treating individuals’ health, as it safeguards both the client and the nutrition coach should any complications arise.
UNDERSTANDING THE ‘ELIMINATION DIET’
An elimination diet is considered the gold standard for food sensitivity testing as it is one of the most common and accurate means of identifying and confirming a food reaction.(118) The diet involves eliminating a particular type of food for a period of time to see if symptoms subside. The food is then reintroduced, and the resulting symptoms - if anyare observed. The following summary is intended to inform nutrition coaches of what is involved in elimination diets; however, it must not be utilised in practice due to being outside the scope of practice.
SCOPE OF PRACTICE FOR NUTRITION COACHES:
Like the FODMAP diet, this protocol can only be undertaken by a doctor or a dietitian as it is intended to diagnose the potential allergies of the client.
Implementing an elimination diet falls outside the scope of practice of nutrition coaches, who are not qualified to diagnose digestive concerns or conditions. Suppose a client has already been diagnosed by a doctor and knows what they are allergic to. In that case, the nutrition coach can support the client in adhering to the diagnosis under the guidance of the GP or APD, but only once a medical clearance has been obtained. Therefore, having an understanding of this diet and how it is conducted is necessary for the success of supporting these types of clients.
REASONS FOR CONDUCTING AN ELIMINATION DIET
Research shows that symptoms such as digestive disorders or skin conditions may be due to certain food allergies or sensitivities. Long-term, allergies and sensitivities can also affect other body systems. However, most people with food sensitivities react to more than one food. It is not always clear which foods may be causing the reaction. An elimination diet may help to pinpoint the cause of certain sensitivity reactions. It can also help to identify the severity of the sensitivity to the food or foods.
COMMON PROBLEMATIC FOODS
A number of foods commonly show up as problematic for those doing the elimination diet. These common problematic foods include:(118)
• Gluten
• Dairy
• Soy
• Eggs
• Peanuts
• Shellfish
• Corn
• Chocolate
• Beans/lentils
• Coffee
• Citrus fruits
• Nuts
• Nightshade vegetables such as potatoes, tomatoes, eggplant, and capsicum/peppers.
DIGESTION AND ITS RELATION TO HOLISTIC HEALTH AND
MENTAL
HEALTH
GUT-BRAIN CONNECTION
Gut health is paramount to an individual’s total health and well-being. For this reason, gut health and digestion is a popular topic in terms of holistic health. Not only is the gut responsible for digestive processes, but the type and quantity of certain gut microbiota plays a pivotal role in hormone synthesis, toxin elimination and nutrient absorption.
The composition of an individual’s gut microbiota has been linked to the following:(119)
• Metabolic disorders (such as diabetes and obesity)
• Mental health disorders (such as anxiety and depression).
Interestingly, an individual’s total health and well-being may be heavily reliant on the integrity of the gut and the composition (quantities and types of microbiota residing in the GI Tract) of the gut microbiome.
HOLISTIC
‘Holistic’ or ‘holistically’ refers to relating to or concerned with wholes or with complete systems rather than with the analysis of, treatment of, or dissection into parts.
As research emerges, it is becoming more and more evident that there is a direct correlation between gut health and mental health, with a bidirectional communication link found between the gut and the brain (known as the gut-brain axis).(119)
It was once thought that brain neurotransmitters relevant to depression AKA ‘happy hormones’ (such as serotonin), were only synthesised in the brain, it is now becoming better understood that gut microorganisms can produce and deliver neuroactive substances such as serotonin as well.(119) It has now been estimated that approximately 95 percent of serotonin is found in the GI tract.(120)
With the continuous emerging information, it is becoming more obvious to scientists, researchers, and health professionals that there is a direct link between the integrity of an individual’s gut health and their mental health status. An individual with a poor gut microbiome is more likely to suffer with their mental health, just as an individual with a great gut microbiome is less likely to suffer from mental health disorders.
While chronic and severe mental health disorders require an ongoing referral to an appropriate health professional, a nutrition coach can support a client’s gut health by ensuring adequate probiotic and prebiotic-rich foods to improve mental health and well-being.
THE GUT ACTS AS THE SECOND BRAIN:
There is a direct line of communication (the vagus nerve) between the brain and the intrinsic nervous system (a division of the autonomic nervous system [ANS]). The intrinsic nervous system is a vast network of gut microbiota that lines the intestinal tract and transports messages from the gut to the brain. This communication works both ways, linking the cognitive and emotional centres of the brain with peripheral intestinal function.(121)
Evidence shows that the microbiota in the gut can interact with the nervous system, which directly affects the messages and actions sent around the body. Gut microbiota can influence the messages and chemicals associated with the body’s response to stress, anxiety, memory function and mood.(122)(123)(124)
SECOND BRAIN
FIRST BRAIN

MAINTAINING KNOWLEDGE OF DIGESTIVE HEALTH
Various information sources are available concerning digestive health, from scholarly articles and textbooks to government websites. It is important to understand what information sources are available and be able to adequately evaluate them to confirm their relevance, reputability, and the currency of their information.
For most chronic health conditions relating to digestive health, various websites gather the most up-to-date information from the medical community. It is essential, however, to ensure, when reviewing these sites, that the credibility of the information is assessed, rather than simply relying on a sufferer’s anecdotal accounts of things that did or did not assist in their own treatment.
A significant number of journal articles also provide up-to-date, evidence-based information on chronic conditions related to the digestive system.
For general health information about digestive health, many government bodies such as health departments or hospitals have specific information about positive digestive health and dietary and lifestyle habits. These sites are regularly updated and typically present best practice advice without looking in detail at more experimental or nonconventional treatment methodologies.
Below is a list of some useful and reliable sites with credible research and information:
• Nutrition Education Materials Online
• Dietitians Australia
• National Health and Medical Research Council
• Nutrition Australia
• Gastroenterological Society of Australia.
It is important to note that the medical community is still exploring the digestive system and that the causes of many conditions remain unknown. This means that, as nutrition coaches, it is critical to continuously review the latest available information to ensure a sound understanding of positive digestive health practices.
SCOPE OF PRACTICE AS A NUTRITIONAL ADVISOR WITH REGARDS TO DIGESTIVE HEALTH
Through a careful pre-screening process, nutrition coaches should be able to identify clients that are out of scope. Further, this will allow identifying ‘at risk’ indicators of common conditions that may require specialist medical support. A nutrition coach should then be able to identify simple health issues that may be alleviated through dietary shifts or changes.
Client support regarding digestive health must be approached with a sound understanding of the nutritional coach’s scope of practice. This means understanding what advice a nutrition coach is qualified to provide and to which clients, and what circumstances require a referral to a medical or allied health professional (AHP).
This qualification provides a strong knowledge base in nutrition and the application of nutritional guidance to individuals with no underlying health conditions.
Based on the content of this course, the following would be regarded as within a nutritional coach’s scope of practice:
The provision of nutritional information and guidance to otherwise healthy individuals based on nutritional scientific evidence.
For clients who do not have, or are not suspected of having, any underlying chronic health conditions, nutrition coaches can:
• Provide specific nutritional information and develop tailored nutritional plans
• Provide non-prescription supplements and dietary products with supporting nutritional advice
• Support clients in promoting positive digestive health.
The provision of nationally endorsed public health information that will educate and support positive client health outcomes.
Engaging with other health professionals and utilising best practice referral/feedback processes to optimise client health outcomes.
Use of evidence-based protocols to enhance client exercise adherence through goal setting, motivation, guidance, social support, relapse prevention, and feedback.
These guidelines place significant responsibility on the nutrition coach to conduct a detailed screening process to ensure that the client falls within their scope of practice.
Any indication of a chronic health condition should automatically result in the nutrition coach referring the client to a suitably qualified AHP such as a general practitioner (GP) or APD.
It is important to remember that chronic health conditions refer to an illness persisting for a long time or constantly recurring. Examples of chronic health conditions that impact nutrition may include, but are not limited to:
• Diabetes mellitus (pre-diabetes, type 1, type 2, gestational diabetes)
• Coeliac disease
• Renal disease
• Cancer – current diagnosis or receiving treatment for cancer
• Eating disorders (anorexia nervosa, bulimia nervosa, binge eating disorder)
• Bariatric surgery (including gastric sleeve, gastric bypass, lap band)
• Thyroid disease (hypothyroidism or hyperthyroidism)
• Cardiovascular diseases requiring medication, including ACE inhibitors, beta-blockers, warfarin, and statins
• Mental health conditions requiring medications
• Gastrointestinal disorders, such as diverticulitis, bowel obstructions, bowel resections, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease).
Nutrition coaches are reminded to refer to their scope of practice developed by the Nutrition Council Australia (NCA, 2018) as a contiguous reference guide to stay within their scope of practice.

MAINTAINING KNOWLEDGE OF DIGESTIVE HEALTH
KEY TERMS AND DEFINITIONS
TERM
ABDOMINAL DISTENSION:
DEFINITION
When the abdomen expands or bloats unnaturally due to the accumulation of substances such as gas or fluid.
ACUTE: A condition that is temporary or short-term.
ALKALISE: To neutralise an acidic environment.
ANTACIDS:
A class of medicines used to neutralise acid in the stomach and relieve symptoms of acid reflux, heartburn, or indigestion (dyspepsia). Antacids are available in tablets or liquid and contain ingredients such as aluminium, calcium, or magnesium, which act as bases (alkalis) to counteract the stomach acid and lower pH.
ANTIBIOTICS: (anti = destroy, biotics = bacteria): Antibiotics are medications (prescription only) used to treat infections caused by pathogens. Kills both good and bad bacteria.
ANTIBODY (ALSO KNOWN AS AN IMMUNOGLOBULIN OR IG):
ANTIGEN:
AUTOIMMUNE REACTION /DISEASE:
BILE:
A large protein used by the immune system to destroy or neutralise pathogens such as bacteria and viruses. The antibody recognises an invader (an antigen) and binds to it so the immune system will attack it.
A substance capable of causing a reaction in which the immune system produces antibodies to ‘fight’ the antigen. Sometimes antigens are actually a part of the body but are recognised as an ‘invader’. This is called an autoimmune reaction.
A condition in which the body’s tissues are attacked by its own immune system. The immune system seeks and destroys what it believes to be ‘invaders’ of the body. People with autoimmune conditions often have unusual antibodies circulating in their bloodstream that target their own body tissues.
The greenish-brown alkaline fluid needed to aid digestion. It is secreted by the liver and stored in the gallbladder.
BIOCHEMICAL: Chemical processes that occur within the body.
BIOPSY: A medical test in which a sample of cells or tissues is extracted and examined for the presence/extent of a disease.
BOLUS: A small mass of food that has been chewed and swallowed.
BOWEL MOTILITY: The movement of waste through the bowels.
BOWEL TRANSIT TIME: The time it takes for food and nutrients to travel through the bowels of the digestive tract.
CARBOHYDRATE: One of the three macronutrients that the body needs for regular energy. Carbohydrates supply the body with energy and are present in the form of starch, sugar, and fibre.
CANDIDA ALBICANS:
CHOLESTEROL:
CHRONIC:
CHYME:
COELIAC DISEASE:
COLONIC BACTERIA:
COMPROMISED IMMUNITY:
COMPREHENSIVE DIGESTIVE STOOL ANALYSIS (CDSA):
CONSTIPATION:
CORTICOSTEROIDS (SYNTHETIC):
DIARRHOEA:
DIGESTIVE ENZYMES:
A fungal species that live naturally in the GIT and only becomes pathogenic when there is an imbalance of microbiota or the immune system is compromised.
A fat-like substance that occurs naturally in the body and is needed in small amounts for the healthy functioning of the body.
A condition or illness that continues over a long period of time that can have adverse effects on the body.
The pulpy acidic fluid made up of gastric juices and partly digested food. This is passed from the stomach to the small intestine.
An autoimmune disease in which the immune system reacts abnormally to gluten (a protein found in wheat, rye and barley), causing small bowel damage.
Also referred to as gut microbiota, gut microbiota, gut bacteria, or gastrointestinal microbiota) It describes the complex and diverse community of microorganisms that live in the colon and break down fibre through fermentation.
When the immune system does not have the ability to defend against illness or invading pathogens, it is said to be compromised. This may occur in those with heart disease, diabetes, cancer, or any chronic illness.
A laboratory examination of a stool sample to analyse the quantity/quality of digestive enzymes, microbiota, or presence of diseases.
Infrequent stools or bowel movements that are hard to pass. This condition may persist over several days or weeks. Some doctors describe constipation as having fewer than three bowel movements a week.
A class of synthetic steroid hormones used to moderate immune response and regulate inflammation.
Passing three or more watery or loose stools per day, or more than is normal for a particular individual.
Digestive enzymes break down food into nutrients so that the body can absorb them. They are largely produced in the pancreas and small intestine.
DIGESTIVE JUICES: The ‘gastric juices’ in the stomach which are made up of hydrogen and chlorine. HCL helps to digest proteins and kill any germs present in food. Healthy pH is about 1.5.
DYSBIOSIS:
An imbalance in gut microbiota produced by too few beneficial bacteria and an overgrowth of bad bacteria, yeast, and/or parasites.
ELIMINATION DIET: A two-phase diet involving the avoidance of a number of foods for 2-3 weeks, followed by careful re-introduction of each food one at time to monitor the body’s reaction.
ENDOSCOPY:
An invasive procedure in which a medical professional inserts a microscopic camera into the body in order to view internal organs and vessels.
ENZYME DEFICIENCY: A lack of the digestive enzymes required to break down a certain food.
EPITHELIAL BARRIER:
The epithelium lining the gastrointestinal mucosa works as a barrier that prevents the entry of commensal organisms. Poor barrier function is thought to play a role in diseases entering the bloodstream.
EXCRETION/ DEFECATION:
FAT-SOLUBLE VITAMINS:
The passing of waste through the anus (as a stool).
Includes vitamins A, D, E and K. These vitamins are absorbed alongside dietary fats and stored in fatty tissue. Found in both plant and animal foods or dietary supplements.
FATTY ACID:
FREE RADICALS:
FERMENTATION:
FIBRE:
FODMAPS:
FOOD ALLERGY:
FOOD DIARY:
FOOD INTOLERANCE/ SENSITIVITY:
FOOD MARKER:
FRUCTOSE (FRUIT SUGAR):
FUNCTIONAL BOWEL DISORDER:
FUNGI:
FUNGAL PARASITE/ PARASITE FUNGI:
GASTROINTESTINAL TRACT (GI TRACT):
GASTROINTESTINAL MUCOSA/GASTRIC MUCOSA:
A type of organic acid mainly composed of long chains of hydrocarbons ending in a carboxyl group. A fatty acid is saturated when the bonds between carbon atoms are all single, and unsaturated when any of these bonds is a double bond. Found in animal and vegetable fats.
Waste products from numerous chemical reactions in the cell. When free radicals build up, they can harm cells in the body and lead to chronic diseases.
The chemical breakdown of a substance or matter by yeasts, bacteria or other microorganisms, usually through effervescence and heat.
The material in certain foods that is mostly indigestible but is used to slow glucose uptake, maintain a healthy gut microbiota, enhance satiety, and improve bowel motions. Also called bulk or roughage.
Acronym for fermentable oligosaccharides, disaccharides, monosaccharides and polyols: A set of sugars in certain foods that, when ingested, have been shown to cause IBS symptoms in sensitive individuals.
An immune system reaction caused by eating a certain food. Typical reactions are usually immediate and can include skin rashes and digestive issues. Severe reactions such as airway constriction or anaphylaxis can also occur.
A daily record of foods eaten and symptoms experienced in order to gauge reactions to particular foods.
A reaction to a certain food such as headache, fatigue, bloating, diarrhoea, or constipation. The symptoms can be immediate or delayed.
An indigestible food that, when observed in the stools, can help to gauge bowel transit time.
A simple sugar found in many species of plants, often associated with glucose to form the disaccharide sucrose.
The term used to describe a type of bowel disorder characterised by chronic abdominal distension that appears to have no structural or biochemical cause.
A species of microbiota that are present in the gut and usually kept in balance by good gut microbiota.
Fungi that can cause harm by feeding off live tissues and potentially robbing them of nutrients. They are usually kept in balance by healthy gut microbiota.
The GI tract is the pathway that food travels down from the mouth, down the oesophagus, into the stomach, and through the small and large intestines to the rectum where it is evacuated. Along the way, nutrients are digested and absorbed.
The mucous membrane layer of the stomach. It is about 1mm thick and consists of various cells that function as ‘gatekeepers’ for nutrients from food being digested.
GLIADIN: A protein found in wheat and many other gluten-containing grains. Gliadin has the ability to provoke an autoimmune response in those with coeliac disease.
GLUTAMINE: A natural amino acid, one of the building blocks for proteins.
GLUTEN: Gluten is the generic name for proteins found in wheat, rye, and barley. Gluten acts as a ‘glue’ to help foods keep their shape.
GLUTENIN: One of the major types of protein found in gluten.
GUT-BRAIN AXIS: The biochemical signalling between the gastrointestinal tract and the central nervous system.
GUT MICROBIOTA: Gut microbiota (or gastrointestinal microbiota) is the complex community of microorganisms that live in the digestive tracts of humans.
GUT PERMEABILITY: When the tight junctions that line the gut become separated, substances can leak into the bloodstream. This can lead to major health problems.
GLYCEROL MOLECULE: The glycerol backbone is found in all lipids known as triglycerides (fats).
HORMONES:
HYDROCHLORIC ACID (HCL):
Compounds that are produced in endocrine glands and secreted within the body that affect the functions of specific organs or tissues.
The ‘gastric juices’ in the stomach which are made up of hydrogen and chlorine. HCL helps to digest proteins and kill any germs present in food. Healthy pH is about 1.5.
HYPER-PERMEABILITY: See Intestinal Permeability.
HYPERTHYROIDISM:
A condition/illness caused by the thyroid gland producing an excessive amount of hormones.
HYPHAE: The long, branch-like structures of a fungal parasite.
INDIGESTIBLE: Food matter that cannot be broken down by the body’s digestive enzymes.
IMMUNE SYSTEM:
IMPERMEABLE BARRIER:
INCOMPLETE EVACUATION:
INFECTION:
INTESTINAL PERMEABILITY:
Our body’s defence system, which is comprised of many biological structures and processes to protect us against disease. The immune system detects pathogens (from viruses to parasites) and distinguishes them from the body’s own healthy tissues before attacking them.
The ‘defence barrier’ formed by the cells lining the GI tract to prevent harmful substances or pathogens entering the bloodstream.
The feeling that the bowels have not been emptied, even after a bowel movement.
Infection can result when bacteria, viruses, and parasites invade the body and multiply, causing illness and/or inflammation. Bacteria that live naturally in the body are not considered infectious.
The lining of the gut is naturally permeable to allow nutrients into the bloodstream. However, when the tight junctions that line the gut become loose or separated, harmful substances can leak into the bloodstream. This is referred to as ‘increased’ intestinal permeability or ‘leaky gut’ and may lead to certain health problems.
INFLAMMATION: The body’s response to tissue damage or injury. Symptoms include pain, heat, redness, and swelling.
INSOLUBLE FIBRE: Adds bulk to the stool and helps food pass more quickly through the stomach and intestines. Found in foods such as bran, vegetables, and whole grains.
INSULIN:
LACTULOSE AND MANNITOL:
LIPIDS:
Insulin is a hormone made by the pancreas that allows the body to use sugar (glucose) from carbohydrates in the food that an individual eats for energy or to store glucose for future use. Insulin helps keep the blood sugar level from getting too high (hyperglycaemia) or too low (hypoglycaemia).
Two non-absorbable sugars that can be used to detect the degree of permeability in the intestines.
Naturally occurring organic compounds commonly known as oils and fats. Lipids are needed for building cell structure, providing energy, and many biological processes.
LIPOPROTEINS: A class of proteins that contain a lipid combined with a simple protein.
MICROBES: A microorganism (usually a type of bacteria) that causes disease or fermentation.
MEMBRANE:
METABOLISM:
MICROBIOTA:
The thin, pliable sheet or layer of animal or vegetable tissue which lines an organ or connects parts of the cell.
The process by which the body gets energy from food by breaking it down and absorbing its nutrients.
Bacteria present in the large intestine that work to break down food and absorb nutrients.
MONOUNSATURATED: A fat containing only one double or triple bond per molecule.
NEUROTRANSMITTER: A substance in the body that transmits a signal from one nerve cell to another.
NUTRIENTS:
NUTRIENT ABSORPTION:
A nutrient is a component in food that the body uses to survive and grow. This includes proteins, carbohydrates, fats, vitamins, and minerals.
The process of assimilating (or absorbing) substances into cells or across the tissues and organs through diffusion or osmosis, as in the absorption of nutrients by the digestive system, or absorption of drugs into the bloodstream.
OESOPHAGUS/ ESOPHAGUS: The muscular tube that attaches the pharynx to the stomach.
OLIGOSACCHARIDES:
A chain of sugars present in certain vegetables. Oligosaccharides cannot be digested in the small intestine, so it is the job of beneficial bacteria in the large intestine to break them down (ferment them) into absorbable nutrients.
ONSET: The beginning of something.
OXIDATIVE DAMAGE: This occurs when the body cannot detoxify or repair the body from the harmful effects of free radicals.
PARASYMPATHETIC NERVOUS SYSTEM (PNS):
PREBIOTICS:
The ‘rest and digest’ response which controls digestion and relaxation. The PNS conserves energy, slows heart rate, increases digestion, and relaxes sphincter muscles in the digestive tract.
A type of food that ‘feeds’ gastrointestinal microbiota. Found in insoluble fibres and raw foods such as garlic, onions, and asparagus.
PROBIOTICS: Healthy bacteria that live in the gut and help to digest food and fight any pathogens.
PATHOGENS:
A type of bacteria, virus, or other microorganism that can cause illness and disease.
PEPSIN: The main digestive enzyme in the stomach which breaks down protein.
PERISTALSIS:
PHASE I AND PHASE II LIVER DETOXIFICATION:
The wave-like muscular action of the digestive system which pushes swallowed food through the stomach and intestines.
The two fundamental stages of the body’s detoxification process are known as Phase I and Phase II. These are two different biochemical processes that enable the body to get rid of all foreign chemical substances and toxins.
POLYUNSATURATED: An oil or fatty acid that has many double or triple bonds in a molecule.
PROTON PUMP INHIBITORS (PPIS):
A group of drugs that reduce the secretion of gastric (stomach) acid. PPIs work by binding with the enzymes which are referred to as the ‘proton pump’.
PSORIASIS: An autoimmune disease characterised by patches of red, itchy, and scaly skin.
RANCIDITY:
REFINED SUGARS:
SATURATED FAT:
SOLUBLE FIBRE:
STEROID:
STARCH:
STOMACH ACID:
STOMACH PH:
SYMPATHETIC NERVOUS SYSTEM (SNS):
SYNDROME:
Rancidity occurs when oxygen molecules damage the natural structure of the oil in a way that causes free radicals and other harmful compounds to form. It also changes the odour, taste, and safety of the oil.
Sugar that has been stripped of its natural fibres. Raw sugar is softened and dissolved, then the components are separated to yield the white, pure sugar known as table sugar, or pure sucrose.
Found in relatively high amounts in many meat and dairy products (full-fat milk, cheese, butter, and cream). This type of fat has no double bonds between carbon molecules because they are saturated with hydrogen molecules. Saturated fats are typically solid at room temperature.
Fibre that attracts and absorbs water, forming a gel during digestion. This gel helps to slow digestion. Found in psyllium husk, oat bran, barley, nuts, seeds, legumes, and some fruits and vegetables.
Steroids can be either the hormones produced by the body or artificially produced medications that duplicate the actions of natural steroids. Steroid hormones help to control metabolism, inflammation, immune functions, salt and water balance, development of sexual characteristics, and healing from illness and injury.
Usually tasteless, odourless white substance typically found in plants such as cereals and potatoes.
Stomach acid plays a major role in the immune system by killing harmful bacteria and parasites that are ingested with food. Stomach acid activates the enzyme pepsin needed for protein digestion, and signals to the pancreas produce digestive juices and enzymes to further break down food. HCL is the majority of gastric acid in the stomach.
The stomach has a pH which can range from approximately 1 to 3 but is usually closer to 2. Food in the stomach can raise the pH to 4-5. After the food leaves the stomach, bicarbonate ions are secreted to alkaline the mixture.
The ‘fight or flight’ response which prepares the body to run away from a threat by stimulating blood-flow to major muscles and decreasing gut motility.
A group of symptoms that usually occur together, or a condition characterised by a particular set of symptoms.
TIGHT JUNCTIONS: Cells of the GI tract mucosa whose membranes join together forming a virtually impermeable barrier to fluid and pathogens.
TOXINS: A harmful or even poisonous substance produced within living cells or organisms.
TRANSIT TIME:
The time it takes for food to travel from the mouth through the digestive tract to the anus.
TRIGGER FOODS: Food which typically causes a reaction in the body.
TRIGLYCERIDE: The main constituent of body fat in humans and animals, and foods. Comprised of a chemical compound with three fatty acids.
UNDIGESTED: Food that is not digested and therefore passed out of the body as waste.
WASTE: Undigested food (such as insoluble fibre) that is passed to the anus to be excreted.
REFERENCES
1. Whitney E, Rolfes SR, Crowe T, Cameron-Smith D, Walsh A. Understanding Nutrition. Third. Pope J, editor. South Melbourne, Australia: Cengage Learning; 2017.
2. Gropper SS, Smith JL, Carr TP. Advanced Nutrition and Human Metabolism. Seventh. Boston. USA: Cengage Learning; 2018.
3. MacLaren D, Morton J. Biochemistry for Sport and Exercise Metabolism. First edit. West Sussex, UK: WileyBlackwell; 2012.
4. Vighi G, Marcucci F, Sensi L, Di Cara G, Frati F. Allergy and the gastrointestinal system. Clin Exp Immunol [Internet]. 2008 Sep [cited 2022 Jul 1];153 Suppl(Suppl 1):3–6. Available from: https://pubmed.ncbi.nlm.nih. gov/18721321/
5. National Digestive Diseases Information Clearinghouse. The Digestive System. J Pract Nurs [Internet]. 2022 Jun [cited 2022 Jul 1];60(2):525–601. Available from: https://onlinelibrary.wiley.com/doi/full/10.1002/9781119118633. ch8
6. National Digestive Diseases Information Clearinghouse. The Digestive System. J Pract Nurs. 2022 Jun;60(2):525–601.
7. Sensoy I. A review on the food digestion in the digestive tract and the used in vitro models. Curr Res Food Sci. 2021 Jan 1;4:308–19.
8. Mahan LK, Raymond JL. Krause’s Food & The Nutrition Care Process. 14th ed. Elsevier; 2017.
9. Collins JT, Nguyen A, Badireddy M. Anatomy, Abdomen and Pelvis, Small Intestine. StatPearls [Internet]. 2021 Aug 11 [cited 2022 Jul 20]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK459366/
10. Tortora GJ, Derrickson B. Principles of Anatomy & Physiology. Thirteenth. John Wiley & Sons, Inc.; 2012.
11. Kiela PR, Ghishan FK. Physiology of Intestinal Absorption and Secretion. Best Pract Res Clin Gastroenterol [Internet]. 2016 Apr 1 [cited 2022 Jul 27];30(2):145. Available from: /pmc/articles/PMC4956471/
12. Azzouz LL, Sharma S. Physiology, Large Intestine. StatPearls [Internet]. 2021 Aug 9 [cited 2022 Jul 20]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK507857/
13. Schwalfenberg GK. The Alkaline Diet: Is There Evidence That an Alkaline pH Diet Benefits Health? J Environ Public Health [Internet]. 2012 [cited 2022 Jul 1];2012. Available from: /pmc/articles/PMC3195546/
14. Institute for Quality and Efficiency in Health Care. Gallstones: Overview [Internet]. InformedHealth.org. 2017 [cited 2022 Jul 1]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK424895/
15. Institute for Quality and Efficiency in Health Care. Gallstones: Overview. InformedHealth.org. 2017.
16. Thau L, Reddy V, Singh P. Anatomy, Central Nervous System. BMJ [Internet]. 2021 Oct 14 [cited 2022 Jul 21];1(4293):478–478. Available from: https://www.ncbi.nlm.nih.gov/books/NBK542179/
17. LeBouef T, Yaker Z, Whited L. Physiology, Autonomic Nervous System. StatPearls [Internet]. 2022 May 8 [cited 2022 Jul 21]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK538516/
18. Tindle J, Tadi P. Neuroanatomy, Parasympathetic Nervous System. StatPearls [Internet]. 2021 Nov 5 [cited 2022 Jul 21]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK553141/
19. Alshak MN, Das JM. Neuroanatomy, Sympathetic Nervous System. StatPearls [Internet]. 2022 May 14 [cited 2022 Jul 21]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK542195/
20. Bohórquez D V., Liddle RA. Secretin - an overview | ScienceDirect Topics. In: Gastrointestinal and Liver Disease [Internet]. Eleventh. Elsevier; 2021 [cited 2022 Jul 21]. p. 34–51. Available from: https://www.sciencedirect.com/ topics/neuroscience/secretin
21. Margetic S, Gazzola C, Pegg GG, Hill RA. Leptin: a review of its peripheral actions and interactions. Int J Obes Relat Metab Disord [Internet]. 2002 Nov 1 [cited 2022 Jul 7];26(11):1407–33. Available from: https://pubmed.ncbi. nlm.nih.gov/12439643/
22. Margetic S, Gazzola C, Pegg GG, Hill RA. Leptin: a review of its peripheral actions and interactions. Int J Obes Relat Metab Disord. 2002 Nov;26(11):1407–33.
23. Beynon ME, Pinneri K. An Overview of the Thyroid Gland and Thyroid-Related Deaths for theForensic Pathologist. Acad Forensic Pathol [Internet]. 2016 Jun 1 [cited 2022 Jul 7];6(2):217. Available from: /pmc/articles/ PMC6507001/
24. Klok MD, Jakobsdottir S, Drent ML. The role of leptin and ghrelin in the regulation of food intake and body weight in humans: A review. Obes Rev. 2007;8(1):21–34.
25. Hopkins E, Sanvictores T, Sharma S. Physiology, Acid Base Balance. Urolithiasis [Internet]. 2021 Sep 14 [cited 2022 Jul 27];19–22. Available from: https://www.ncbi.nlm.nih.gov/books/NBK507807/
26. Quade BN, Parker MD, Occhipinti R. The therapeutic importance of acid-base balance. Biochem Pharmacol [Internet]. 2021 Jan 1 [cited 2022 Jul 1];183:114278. Available from: /pmc/articles/PMC7544731/
27. Eleanor Whitney, Sharon Rady Rolfes, Tim Crowe, David Cameron-Smith AW. Understanding Nutrition. 3rd ed. 2017.
28. Tamgadge S. INTERNAL PH IN HEALTH AND DISEASE. Iran J Pathol [Internet]. 2016 [cited 2022 Jul 27];11(2):176–80. Available from: https://www.researchgate.net/publication/304538339_INTERNAL_PH_IN_HEALTH_AND_ DISEASE
29. Seifter JL, Chang H-Y. Disorders of Acid-Base Balance: New Perspectives. Kidney Dis [Internet]. 2016 [cited 2022 Jul 25];2(4):170–86. Available from: https://www.karger.com/Article/FullText/453028
30. Schwalfenberg GK. The Alkaline Diet: Is There Evidence That an Alkaline pH Diet Benefits Health? J Environ Public Health. 2012;2012.
31. Heitmann PT, Vollebregt PF, Knowles CH, Lunniss PJ, Dinning PG, Scott SM. Understanding the physiology of human defaecation and disorders of continence and evacuation. Nat Rev Gastroenterol Hepatol 2021 1811 [Internet]. 2021 Aug 9 [cited 2022 Jul 6];18(11):751–69. Available from: https://www.nature.com/articles/s41575021-00487-5
32. Heitmann PT, Vollebregt PF, Knowles CH, Lunniss PJ, Dinning PG, Scott SM. Understanding the physiology of human defaecation and disorders of continence and evacuation. Nat Rev Gastroenterol Hepatol 2021 1811. 2021 Aug;18(11):751–69.
33. Continence Foundation of Australia. Faecal - Bristol Stool Chart [Internet]. 2022 [cited 2022 Jul 5]. Available from: https://www.continence.org.au/bristol-stool-chart
34. Continence Foundation of Australia. Faecal - Bristol Stool Chart. 2022.
35. Bharucha AE, Philips SF. Slow-transit Constipation. Curr Treat Options Gastroenterol [Internet]. 2001 Aug [cited 2022 Jul 1];4(4):309–15. Available from: https://pubmed.ncbi.nlm.nih.gov/11469989/
36. Tillou J, Poylin V. Approaches and Treatment of Intussusception, Volvulus, Rectal Prolapse, and Functional Disorders of the Colon, Rectum, and Anus: Functional Disorders: Slow-Transit Constipation. Clin Colon Rectal Surg [Internet]. 2017 Feb 1 [cited 2022 Jul 28];30(1):76. Available from: /pmc/articles/PMC5179270/
37. Guérin A, Mody R, Fok B, Lasch KL, Zhou Z, Wu EQ, et al. Risk of developing colorectal cancer and benign colorectal neoplasm in patients with chronic constipation. Aliment Pharmacol Ther [Internet]. 2014 Jul 1 [cited 2022 Jul 1];40(1):83–92. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/apt.12789
38. Institute of Medicine. Krause’ s Food & the Nutrition Care Process. Food and Nutrition Board, Institute of Medicine, National Academies. 2017.
39. Madison AA, Kiecolt-Glaser JK. The Gut Microbiota and Nervous System: Age-Defined and Age-Defying. Semin Cell Dev Biol [Internet]. 2021 Aug 1 [cited 2022 Sep 12];116:98. Available from: /pmc/articles/PMC8257779/
40. Cann PA, Read NW, Cammack J, Childs H, Holden S, Kashman R, et al. Psychological stress and the passage of a standard meal through the stomach and small intestine in man. Gut [Internet]. 1983 [cited 2022 Sep 12];24(3):236. Available from: /pmc/articles/PMC1419932/?report=abstract
41. Konturek PC, Konturek, Brzozowski SJ. Stress and the gut: pathophysiology, clinical consequences, diagnostic approach and treatment options - PubMed. J Physiol Pharmacol [Internet]. 2011 [cited 2022 Sep 12];62(6):591–9. Available from: https://pubmed.ncbi.nlm.nih.gov/22314561/
42. Hechtman L. Clinical Naturopathic Medicine. 1st ed. Churchill Livingstone; 2011.
43. Department for Education South Australia. Bristol stool chart [Internet]. Department for Education South Australia. 2019 [cited 2022 Sep 12]. Available from: https://www.education.sa.gov.au/doc/bristol-stool-chart
44. Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Reddy DN. Role of the normal gut microbiota. World J Gastroenterol [Internet]. 2015 Aug 7 [cited 2021 May 21];21(29):8836–47. Available from: / pmc/articles/PMC4528021/
45. ESNM. Glossary - Gut Microbiota for Health [Internet]. Gut Microbiota for Health by the European Society of Neurogastroenterology and Motility. 2021 [cited 2021 May 12]. Available from: https://www. gutmicrobiotaforhealth.com/glossary-index/
46. Jandhyala SM, Talukdar R, Subramanyam C, Vuyyuru H, Sasikala M, Reddy DN. Role of the normal gut microbiota. World J Gastroenterol [Internet]. 2015 Aug 8 [cited 2022 Jul 1];21(29):8787. Available from: /pmc/ articles/PMC4528021/
47. Kiela PR, Ghishan FK. Physiology of Intestinal Absorption and Secretion. Best Pract Res Clin Gastroenterol [Internet]. 2016 Apr 1 [cited 2022 Jul 6];30(2):145. Available from: /pmc/articles/PMC4956471/
48. Kiela PR, Ghishan FK. Physiology of Intestinal Absorption and Secretion. Best Pract Res Clin Gastroenterol. 2016 Apr;30(2):145.
49. Onur MR, Akpinar E, Karaosmanoglu AD, Isayev C, Karcaaltincaba M. Diverticulitis: a comprehensive review with
usual and unusual complications. Insights Imaging [Internet]. 2017 Feb 1 [cited 2022 Jul 5];8(1):19. Available from: /pmc/articles/PMC5265196/
50. Berkowitz L, Schultz BM, Salazar GA, Pardo-Roa C, Sebastián VP, Álvarez-Lobos MM, et al. Impact of Cigarette Smoking on the Gastrointestinal Tract Inflammation: Opposing Effects in Crohn’s Disease and Ulcerative Colitis. Front Immunol [Internet]. 2018 Jan 30 [cited 2022 Jul 6];9(74):1. Available from: /pmc/articles/PMC5797634/
51. Berkowitz L, Schultz BM, Salazar GA, Pardo-Roa C, Sebastián VP, Álvarez-Lobos MM, et al. Impact of Cigarette Smoking on the Gastrointestinal Tract Inflammation: Opposing Effects in Crohn’s Disease and Ulcerative Colitis. Front Immunol. 2018 Jan;9(74):1.
52. Bode C, Bode JC. Alcohol’s Role in Gastrointestinal Tract Disorders. Alcohol Health Res World [Internet]. 1997 [cited 2022 Jul 6];21(1):76. Available from: /pmc/articles/PMC6826790/
53. Munkholm M, Mortensen J. Mucociliary clearance: pathophysiological aspects. Clin Physiol Funct Imaging [Internet]. 2014 [cited 2022 Jul 6];34(3):171–7. Available from: https://pubmed.ncbi.nlm.nih.gov/24119105/
54. Munkholm M, Mortensen J. Mucociliary clearance: pathophysiological aspects. Clin Physiol Funct Imaging. 2014;34(3):171–7.
55. Park JH, Moon JH, Kim HJ, Kong MH, Oh YH. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J Fam Med [Internet]. 2020 Nov 1 [cited 2022 Jul 6];41(6):365. Available from: /pmc/ articles/PMC7700832/
56. Park JH, Moon JH, Kim HJ, Kong MH, Oh YH. Sedentary Lifestyle: Overview of Updated Evidence of Potential Health Risks. Korean J Fam Med. 2020 Nov;41(6):365.
57. Bhatia V, Tandon RK. Stress and the gastrointestinal tract. J Gastroenterol Hepatol. 2005;20(3):332–9.
58. Chang YM, El-Zaatari M, Kao JY. Does stress induce bowel dysfunction? Expert Rev Gastroenterol Hepatol [Internet]. 2014 [cited 2021 Feb 9];8(6):583–5. Available from: /pmc/articles/PMC4249634/
59. Cherpak CE. Mindful Eating: A Review Of How The Stress-Digestion-Mindfulness Triad May Modulate And Improve Gastrointestinal And Digestive Function. Integr Med A Clin J [Internet]. 2019 Aug 1 [cited 2022 Aug 1];18(4):48. Available from: /pmc/articles/PMC7219460/
60. Dekker JP, Frank KM. Salmonella, Shigella, and Yersinia. Clin Lab Med [Internet]. 2015 Jun 1 [cited 2022 Aug 1];35(2):225. Available from: /pmc/articles/PMC4443274/
61. Lekshmi N, Joseph I, Ramamurthy T, Thomas S. Changing facades of Vibrio cholerae: An enigma in the epidemiology of cholera. Indian J Med Res [Internet]. 2018 Feb 1 [cited 2022 Aug 1];147(2):133. Available from: / pmc/articles/PMC5991131/
62. Soenen S, Rayner CK, Jones KL, Horowitz M. The ageing gastrointestinal tract. Curr Opin Clin Nutr Metab Care [Internet]. 2016 Jan 1 [cited 2022 Jul 5];19(1):12–8. Available from: https://pubmed.ncbi.nlm.nih.gov/26560524/
63. Onur MR, Akpinar E, Karaosmanoglu AD, Isayev C, Karcaaltincaba M. Diverticulitis: a comprehensive review with usual and unusual complications. Insights Imaging. 2017 Feb;8(1):19.
64. Stover PJ. Vitamin B12 and older adults. Curr Opin Clin Nutr Metab Care [Internet]. 2010 Jan [cited 2022 Jul 5];13(1):24–7. Available from: https://pubmed.ncbi.nlm.nih.gov/19904199/
65. Soenen S, Rayner CK, Jones KL, Horowitz M. The ageing gastrointestinal tract. Curr Opin Clin Nutr Metab Care. 2016 Jan;19(1):12–8.
66. Lee J, Anggiansah A, Anggiansah R, Young A, Wong T, Fox M. Effects of age on the gastroesophageal junction, esophageal motility, and reflux disease. Clin Gastroenterol Hepatol [Internet]. 2007 Dec [cited 2022 Jul 5];5(12):1392–8. Available from: https://pubmed.ncbi.nlm.nih.gov/17936081/
67. Mori H, Suzuki H, Matsuzaki J, Taniguchi K, Shimizu T, Yamane T, et al. Gender Difference of Gastric Emptying in Healthy Volunteers and Patients with Functional Dyspepsia. Digestion [Internet]. 2017 Jan 1 [cited 2022 Jul 5];95(1):72–8. Available from: https://pubmed.ncbi.nlm.nih.gov/28052285/
68. Kim YS, Kim N. Sex-Gender Differences in Irritable Bowel Syndrome. J Neurogastroenterol Motil [Internet]. 2018 Oct 1 [cited 2022 Jul 5];24(4):544–58. Available from: /pmc/articles/PMC6175559/
69. Anguita-Ruiz A, Aguilera CM, Gil Á. Genetics of Lactose Intolerance: An Updated Review and Online Interactive World Maps of Phenotype and Genotype Frequencies. Nutrients [Internet]. 2020 Sep 1 [cited 2022 Jul 5];12(9):1–20. Available from: /pmc/articles/PMC7551416/
70. Anguita-Ruiz A, Aguilera CM, Gil Á. Genetics of Lactose Intolerance: An Updated Review and Online Interactive World Maps of Phenotype and Genotype Frequencies. Nutrients. 2020 Sep;12(9):1–20.
71. Steffen R, Hill DR, DuPont HL. Traveler’s diarrhea: a clinical review. JAMA [Internet]. 2015 Jan 6 [cited 2022 Jul 5];313(1):71–80. Available from: https://pubmed.ncbi.nlm.nih.gov/25562268/
72. Krigel A, Turner KO, Makharia GK, Green PHR, Genta RM, Lebwohl B. Ethnic Variations in Duodenal Villous Atrophy Consistent With Celiac Disease in the United States. Clin Gastroenterol Hepatol [Internet]. 2016 Aug 1 [cited 2022 Jul 5];14(8):1105–11. Available from: https://pubmed.ncbi.nlm.nih.gov/27155557/
73. Bhopal RS, Cezard G, Bansal N, Ward HJT, Bhala N. Ethnic variations in five lower gastrointestinal diseases: Scottish health and ethnicity linkage study. BMJ Open [Internet]. 2014 [cited 2022 Jul 5];4(10). Available from: https://pubmed.ncbi.nlm.nih.gov/25335961/
74. Nutrition Australia. Fibre | Nutrition Australia [Internet]. Nutrition Australia. 2021 [cited 2022 Aug 2]. Available from: https://nutritionaustralia.org/fact-sheets/fibre-2/
75. Dietitians Australia. Fibres for your gut: sorting through the roughage | Dietitians Australia [Internet]. Dietitians Australia. 2022 [cited 2022 Aug 2]. Available from: https://dietitiansaustralia.org.au/health-advice/fibres-yourgut-sorting-through-roughage
76. Fayet-Moore F, Cassettari T, Tuck K, McConnell A, Petocz P. Dietary fibre intake in australia. Paper i: Associations with demographic, socio-economic, and anthropometric factors. Nutrients. 2018 May 11;10(5).
77. Kolay E, Bykowska-Derda A, Abdulsamad S, Kaluzna M, Samarzewska K, Ruchala M, et al. Self-Reported Eating Speed Is Associated with Indicators of Obesity in Adults: A Systematic Review and Meta-Analysis. Healthc (Basel, Switzerland) [Internet]. 2021 Nov 1 [cited 2022 Jul 5];9(11). Available from: https://pubmed.ncbi.nlm.nih. gov/34828605/
78. Kechagia M, Basoulis D, Konstantopoulou S, Dimitriadi D, Gyftopoulou K, Skarmoutsou N, et al. Health Benefits of Probiotics: A Review. ISRN Nutr [Internet]. 2013 Jan 2 [cited 2022 Aug 2];2013:1–7. Available from: /pmc/ articles/PMC4045285/
79. Carlson JL, Erickson JM, Lloyd BB, Slavin JL. Health effects and sources of prebiotic dietary fiber. Curr Dev Nutr [Internet]. 2018 Mar 1 [cited 2021 Mar 18];2(3). Available from: /pmc/articles/PMC6041804/
80. Davani-Davari D, Negahdaripour M, Karimzadeh I, Seifan M, Mohkam M, Masoumi SJ, et al. Prebiotics: Definition, types, sources, mechanisms, and clinical applications. Foods [Internet]. 2019 Mar 1 [cited 2021 Feb 9];8(3). Available from: /pmc/articles/PMC6463098/
81. Davani-Davari D, Negahdaripour M, Karimzadeh I, Seifan M, Mohkam M, Masoumi SJ, et al. Prebiotics: Definition, types, sources, mechanisms, and clinical applications. Foods [Internet]. 2019 Mar 1 [cited 2021 Mar 18];8(3). Available from: /pmc/articles/PMC6463098/
82. Kim MH, Kim H. The Roles of Glutamine in the Intestine and Its Implication in Intestinal Diseases. Int J Mol Sci [Internet]. 2017 May 12 [cited 2022 Aug 2];18(5). Available from: /pmc/articles/PMC5454963/
83. Skrovanek S, DiGuilio K, Bailey R, Huntington W, Urbas R, Mayilvaganan B, et al. Zinc and gastrointestinal disease. World J Gastrointest Pathophysiol [Internet]. 2014 Nov 11 [cited 2022 Aug 2];5(4):496. Available from: / pmc/articles/PMC4231515/
84. Jani B, Marsicano E. Constipation: Evaluation and Management. Mo Med [Internet]. 2018 May 1 [cited 2022 Jul 7];115(3):236. Available from: /pmc/articles/PMC6140151/
85. Jani B, Marsicano E. Constipation: Evaluation and Management. Mo Med. 2018 May;115(3):236.
86. Forootan M, Bagheri N, Darvishi M. Chronic constipation: A review of literature. Medicine (Baltimore) [Internet]. 2018 May 1 [cited 2022 Jul 7];97(20). Available from: /pmc/articles/PMC5976340/
87. Forootan M, Bagheri N, Darvishi M. Chronic constipation: A review of literature. Medicine (Baltimore). 2018 May;97(20).
88. E Manea; E Ailenei; D Deleanu. Food allergies and food intolerances. Food Stand Aust New Zeal [Internet]. 2021 [cited 2022 Jul 7];89(1):5–10. Available from: https://www.foodstandards.gov.au/consumer/foodallergies/ allergies/Pages/default.aspx
89. Krogh K, Chiarioni G, Whitehead W. Management of chronic constipation in adults. United Eur Gastroenterol J [Internet]. 2017 Jun 1 [cited 2022 Jul 7];5(4):465. Available from: /pmc/articles/PMC5446139/
90. Norcliffe-Kaufmann L, Kaufmann H. Autonomic Dysfunction. Encycl Mov Disord. 2010 Jan 1;103–12.
91. Krogh K, Chiarioni G, Whitehead W. Management of chronic constipation in adults. United Eur Gastroenterol J. 2017 Jun;5(4):465.
92. McRorie JW. Evidence-Based Approach to Fiber Supplements and Clinically Meaningful Health Benefits, Part 2: What to Look for and How to Recommend an Effective Fiber Therapy. Nutr Today [Internet]. 2015 Mar 10 [cited 2022 Aug 3];50(2):90. Available from: /pmc/articles/PMC4415970/
93. Rudolph JA, Rufo PA. Diarrhea. Encycl Infant Early Child Dev [Internet]. 2021 Nov 29 [cited 2022 Jul 7];1–3:394–401. Available from: https://www.ncbi.nlm.nih.gov/books/NBK448082/
94. Rudolph JA, Rufo PA. Diarrhea. Encycl Infant Early Child Dev. 2021 Nov;1–3:394–401.
95. Lazo-Vélez MA, Serna-Saldívar SO, Rosales-Medina MF, Tinoco-Alvear M, Briones-García M. Application of Saccharomyces cerevisiae var. boulardii in food processing: a review. J Appl Microbiol [Internet]. 2018 Oct 1 [cited 2022 Aug 3];125(4):943–51. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/jam.14037
96. E Manea; E Ailenei; D Deleanu. Food allergies and food intolerances. Food Stand Aust New Zeal. 2021;89(1):5–10.
97. Bégin P, Nadeau KC. Diagnosis of food allergy. Pediatr Ann [Internet]. 2013 [cited 2022 Jul 7];42(6):102–9. Available from: https://pubmed.ncbi.nlm.nih.gov/23718238/
98. Food intolerance [Internet]. Australasian Society of Clinical Immunology and Allergy. 2019 [cited 2022 Jul 7]. Available from: https://allergy.org.au/patients/food-other-adverse-reactions/food-intolerance
99. Food intolerance. Australasian Society of Clinical Immunology and Allergy. 2019.
100. Bégin P, Nadeau KC. Diagnosis of food allergy. Pediatr Ann. 2013;42(6):102–9.
101. Parzanese I, Qehajaj D, Patrinicola F, Aralica M, Chiriva-Internati M, Stifter S, et al. Celiac disease: From pathophysiology to treatment. World J Gastrointest Pathophysiol [Internet]. 2017 May 5 [cited 2022 Aug 3];8(2):27. Available from: /pmc/articles/PMC5437500/
102. Tarar ZI, Zafar MU, Farooq U, Basar O, Tahan V, Daglilar E. The Progression of Celiac Disease, Diagnostic Modalities, and Treatment Options. J Investig Med High Impact Case Reports [Internet]. 2021 Oct 25 [cited 2022 Aug 3];9. Available from: https://journals.sagepub.com/doi/full/10.1177/23247096211053702
103. Caio G, Volta U, Sapone A, Leffler DA, De Giorgio R, Catassi C, et al. Celiac disease: a comprehensive current review. BMC Med 2019 171 [Internet]. 2019 Jul 23 [cited 2022 Aug 3];17(1):1–20. Available from: https:// bmcmedicine.biomedcentral.com/articles/10.1186/s12916-019-1380-z
104. Oshima S, Watanabe M. Genetic and environmental factors drive personalized medicine for Crohn’s disease. J Clin Invest [Internet]. 2018 Nov 1 [cited 2022 Aug 3];128(11):4758–60. Available from: https://doi.org/10.1172/ JCI124303.
105. Odenwald MA, Turner JR. Intestinal Permeability Defects: Is It Time to Treat? Clin Gastroenterol Hepatol [Internet]. 2013 Sep [cited 2021 May 18];11(9):1075–83. Available from: /pmc/articles/PMC3758766/
106. Fukui H. Increased Intestinal Permeability and Decreased Barrier Function: Does It Really Influence the Risk of Inflammation? Inflamm Intest Dis [Internet]. 2016 [cited 2021 May 18];1(3):135–45. Available from: www.karger. com/iid
107. Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke J-D, Serino M, et al. Intestinal permeability – a new target for disease prevention and therapy. BMC Gastroenterol [Internet]. 2014 Dec 18 [cited 2021 May 18];14(1):189. Available from: https://bmcgastroenterol.biomedcentral.com/articles/10.1186/s12876-014-0189-7
108. Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, Serino M, et al. Intestinal permeability – a new target for disease prevention and therapy. BMC Gastroenterol [Internet]. 2014 Nov 18 [cited 2022 Aug 8];14(1). Available from: /pmc/articles/PMC4253991/
109. Maseda D, Ricciotti E. NSAID–Gut Microbiota Interactions. Front Pharmacol. 2020 Aug 7;11:1153.
110. Suzuki T. Regulation of the intestinal barrier by nutrients: The role of tight junctions. Anim Sci J [Internet]. 2020 Jan 1 [cited 2022 Aug 8];91(1):e13357. Available from: https://onlinelibrary.wiley.com/doi/full/10.1111/asj.13357
111. Dietitians Australia. Diet and nutrition health advice | Dietitians Australia [Internet]. 2022 [cited 2022 Aug 5]. Available from: https://dietitiansaustralia.org.au/diet-and-nutrition-health-advice
112. Portincasa P, Bonfrate L, De Bari O, Lembo A, Ballou S. Irritable bowel syndrome and diet. Gastroenterol Rep [Internet]. 2017 Feb 1 [cited 2021 May 20];5(1):11–9. Available from: https://academic.oup.com/gastro/ article/5/1/11/2931986
113. Basnayake C. Treatment of irritable bowel syndrome. Aust Prescr [Internet]. 2018 Oct 1 [cited 2021 May 19];41(5):145–9. Available from: https://www.nps.org.au/australian-prescriber/articles/treatment-of-irritablebowel-syndrome
114. Halmos EP, Gibson PR. Controversies and reality of the FODMAP diet for patients with irritable bowel syndrome. J Gastroenterol Hepatol [Internet]. 2019 Jul 1 [cited 2021 May 20];34(7):1134–42. Available from: https:// onlinelibrary.wiley.com/doi/full/10.1111/jgh.14650
115. Lenhart A, Chey WD. A systematic review of the effects of polyols on gastrointestinal health and irritable bowel syndrome. Adv Nutr [Internet]. 2017 Jul 1 [cited 2021 May 20];8(4):587–96. Available from: /pmc/articles/ PMC5508768/
116. Latulippe ME, Skoog SM. Fructose malabsorption and intolerance: Effects of fructose with and without simultaneous glucose ingestion. Crit Rev Food Sci Nutr [Internet]. 2011 Aug [cited 2021 May 20];51(7):583–92. Available from: /pmc/articles/PMC3471321/
117. Monash University. Low FODMAP Diet | IBS Research at Monash University - Monash Fodmap [Internet]. The Low FODMAP Diet. 2019 [cited 2022 Aug 5]. Available from: https://www.monashfodmap.com/
118. Manea I, Ailenei E, Deleanu D. Overview of food allergy diagnosis. Clujul Med [Internet]. 2016 [cited 2022 Aug 5];89(1):5. Available from: /pmc/articles/PMC4777468/
119. Evrensel A, Ceylan ME. The Gut-Brain Axis: The Missing Link in Depression. Clin Psychopharmacol Neurosci [Internet]. 2015 Dec 1 [cited 2022 Aug 5];13(3):239. Available from: /pmc/articles/PMC4662178/
120. Terry N, Margolis KG. Serotonergic Mechanisms Regulating the GI Tract: Experimental Evidence and Therapeutic Relevance. Handb Exp Pharmacol [Internet]. 2017 Jan 1 [cited 2022 Aug 5];239:319. Available from: /pmc/ articles/PMC5526216/
121. Breit S, Kupferberg A, Rogler G, Hasler G. Vagus Nerve as Modulator of the Brain–Gut Axis in Psychiatric and Inflammatory Disorders. Front Psychiatry [Internet]. 2018 Mar 13 [cited 2022 Aug 5];9(MAR):1. Available from: / pmc/articles/PMC5859128/
122. Mitrea L, Nemeş SA, Szabo K, Teleky BE, Vodnar DC. Guts Imbalance Imbalances the Brain: A Review of Gut Microbiota Association With Neurological and Psychiatric Disorders. Front Med. 2022 Mar 31;9:706.
123. Rea K, Dinan TG, Cryan JF. The microbiome: A key regulator of stress and neuroinflammation. Neurobiol Stress. 2016 Oct 1;4:23–33.
124. Carabotti M, Scirocco A, Maselli MA, Severi C. The gut-brain axis: interactions between enteric microbiota, central and enteric nervous systems. Ann Gastroenterol Q Publ Hell Soc Gastroenterol [Internet]. 2015 [cited 2022 Aug 8];28(2):203. Available from: /pmc/articles/PMC4367209/
125. Holtmann GJ, Ford AC, Talley NJ. Pathophysiology of irritable bowel syndrome. Lancet Gastroenterol Hepatol. 2016 Oct 1;1(2):133–46.
