













Welcome to the unit ‘Design a Nutrition Plan for an Individual’. This unit is intended to provide nutrition coaches with the skills and knowledge needed to analyse a client’s nutritional aims and goals. The focus of this unit is understanding how to develop safe, functional, effective and customised nutritional plans that will allow clients to achieve their individual nutrition goals. Once the nutrition coach has completed the previous unit of ‘Apply the fundamentals of nutrition to meet a client’s needs’ and identified the needs and goals of the client, this unit then continues to the next steps in developing appropriate nutritional support programs for those goals and needs.
Firstly, nutrition coaches are reminded of their scope of practice and which client’s physical conditions they can and cannot support. Important concepts, such as basic anatomy and nutritional principles, are quickly reviewed to refresh the knowledge of nutrition coaches on the essential aspects of these concepts.
This unit then provides a detailed step-by-step process on how a nutrition coach can develop a customised nutritional plan for their client. This unit ensures the nutrition coach is aware of what goes into the process of developing a nutritional plan before diving deeper into the finer details, step by step. Nutrition coaches will develop the skills to perform the initial consultation and gather client information before learning to analyse the client’s nutritional intake, which includes everything from macro- and micronutrient intake to their discretionary food intake. This unit then provides practical guidelines for determining the client’s recommended nutritional requirements, using normal ranges and standards, and then comparing them to their current intake. Once the nutrition coach has obtained all of this information, they can either prepare a custom nutritional plan or provide general advice and guidelines, depending on what they think is more appropriate for that particular client.
This unit also extensively covers many other aspects that should be considered when a nutrition coach is designing a nutritional plan for their client and identifying particular areas that require monitoring. The nutrition coach will also be informed of the various non-diet factors that come into play when designing a nutritional plan and the importance of goal setting to successfully monitor and record the client’s progress.
One of the most beneficial aspects of this unit is the multiple meal plan examples provided at the end of the unit, which cover both male and female examples and their varying potential goals. Nutrition coaches will be able to see the end product they are working towards, allowing clarity in the process.
This unit will allow a nutrition coach to:
• Interpret a client’s pre-screen information to identify their nutritional aims and goals
• Analyse a client’s current dietary and lifestyle habits and patterns to establish factors that will prevent or influence the achievement of nutritional goals
• Develop a nutrition/meal plan based on solid nutritional fundamentals
• Support a client in implementing and monitoring the nutrition plan.
It is essential to understand that this unit will not provide the ability to develop nutrition/meal plans for:
• Individuals suffering from chronic health conditions or diseases
• People with medical conditions requiring specialised dietary advice
• Frail elderly people who are at risk of malnutrition
• Infants and toddlers
• Pregnant or breastfeeding women.
Individuals who present with a chronic health concern or appear to have symptoms indicative of a chronic health concern should be immediately referred to a medical professional or an Accredited Practising Dietitian (APD).


Like any professional field where advice is provided to a client about health and wellbeing, legal and ethical implications need to be considered. Incorrect nutritional advice provided to a client can have direct and serious implications for their physical and mental health. Accordingly, it is of utmost importance to understand the role and scope of practice as a nutrition coach.
Consequences for a client when practising outside the scope may include, but are not limited to:
• Negative impact on pre-existing health conditions
• Sub-optimal or dangerous nutrient imbalances, interactions, toxicities and deficiencies
• Negative interactions between nutrients and drugs.
As a result of this, the nutrition coach is at risk of:
• Potential legal proceedings for causing harm to a client, could incur considerable financial costs and lost time
• The potential loss of professional reputation.
A nutrition coach needs to have a sound understanding of the duty of care and responsible practice requirements inherent as a health practitioner. In Australia, the provision of health and fitness information is not governed under a single legislation, act or code but may instead be governed under codes of conduct for membership groups, peak bodies or industry authorities. However, any individual providing professional advice to clients about health and wellbeing will hold a duty of care which can be defined as “the legal obligation of professionals to safeguard others from harm while they are in their care, using their services, or exposed to their activities”.(1)
Under this concept, a nutrition coach who has provided incorrect nutritional advice, supplied or recommended products that harm a client’s health, or indirectly contributed to a client’s injury or illness through incorrect, outdated or inappropriate nutritional support services, may be in breach of their duty of care.
Health professionals are bound by additional state and federal legislation and acts relating to both health and safety, and privacy and confidentiality. There is a responsibility for health professionals to ensure that a safe, hazard-free environment is provided to clients when conducting their practical pre-screen and mentoring activities. This means that the work environment should be reviewed to identify, remove or control hazards and practical activities involving clients, should be evaluated for the risk of causing harm.
Safe Work Australia leads the development of national policy to improve work health and safety, and workers’ compensation arrangements across Australia. However, it does not regulate or enforce Workplace Health and Safety (WHS) legislation. Business owners, instead, must meet the WHS requirements set out in the acts and regulations in their state or territory.
CLICK HERE to understand more about the benefits to business owners as well as the rights and obligations as a small business owner.

Across the range of support provided to clients, nutrition coaches will also be provided with personal and confidential information such as contact information, lifestyle patterns and habits, family histories and detailed medical information. In Australia, professionals are bound by the Privacy Act 1988, which regulates the handling of personal information. The Act is underpinned by thirteen Australian Privacy Principles (APP), which govern the collection, processing, storage, protection and dissemination of personal information relating to individuals.(2)
As a result, all information is considered confidential and is not to be discussed with anyone, with the possible exception of other health professionals who are currently treating or are being referred to treat the client and with the client’s consent obtained. When discussing the general nature of the consultation and seeking advice from other health professionals, care must be taken that the client’s contact details, such as their name, address and phone number, are not disclosed.
The Office of the Australian Information Commissioner (OAIC) is an Australian Government statutory agency. It is responsible for privacy and information policies, freedom of information and provides information and advice to individuals, businesses and agencies.
CLICK HERE to view the Australian Privacy Principles (APP), which outline the obligations nutrition coaches hold in relation to client information.
Nutrition coaches are reminded to refer back to their scope of practice (SoP) (Nutrition Council Australia, 2018) for important information and requirements regarding duty of care, workplace health and safety, and client confidentiality.


Client support must be approached with a sound understanding of the nutrition coach’s scope of practice. Which means understanding what advice a nutrition coach is qualified to provide and to which clients, and in what circumstances they should make a referral to a medical or allied health professional (AHP). These parameters are developed and articulated within national guidelines in many medical fields provided by industry associations or similar organisations.
So, what is within the scope of knowledge and experience of a nutritional advisornutrition coach, having completed the 11046NAT - Certificate IV in Nutrition? This qualification provides a strong knowledge base in nutrition and the application of nutritional guidance to individuals with no underlying health conditions.
Based on the content of this course, the following is within a nutritional advisornutrition coach’s scope of practice:(3)
Provision of nutritional information and guidance to otherwise healthy individuals based on nutritional scientific evidence.
Provision of nationally endorsed public health information that will educate and support positive client health outcomes.
Engaging with other Health Professionals and utilising best practice referral/feedback processes to optimise client health outcomes.
Use of evidence-based protocols to enhance client exercise adherence through goal setting, motivation, guidance, social support, relapse prevention and feedback.
For athletes who do not have, or are not suspected to have, any underlying chronic health conditions, nutrition coaches can:
• Develop personalised meal plans
• Provide specific nutritional information and development of tailored nutritional plans
• Provide recommendations on non-prescription supplements and dietary products with supporting nutritional advice.
In addition to the above, a nutrition coach has the skills and ability to:
• Interpret a client’s pre-screen information to identify their nutritional aims and goals
• Analyse a client’s current dietary and lifestyle habits and patterns to establish factors that will prevent or influence the achievement of nutritional goals
• Develop a nutrition/meal plan based on solid nutritional fundamentals
• Support a client in implementing and monitoring the nutrition plan

The scope of practice places significant responsibility on nutrition coaches to conduct a detailed screening process to ensure that the client falls within their scope of practice.
It is essential to understand that this unit will not provide nutrition coaches with the ability to develop nutrition/meal plans for certain population groups.
The following fall outside of the nutrition coach’s scope of practice:
• Individuals suffering from chronic health conditions or diseases
• People with medical conditions requiring specialised dietary advice
• Frail elderly people who are at risk of malnutrition
• Infants and toddlers
• Pregnant or breastfeeding women
Any indication of a chronic health condition or the above-mentioned population group should automatically result in the nutrition coach referring the client to a suitably qualified AHP such as a General Practitioner (GP) or an Accredited Practising Dietitian (APD) for review and qualified assessment.
It is important to remember that the reference to chronic health conditions refers to an illness persisting for an extended period of time or constantly recurring.
Examples of chronic health conditions that impact nutrition may include, but are not limited to:
• Diabetes mellitus (type 1, type 2, gestational diabetes)
• Coeliac disease
• Renal disease
• Cancer
• Eating disorders (anorexia nervosa, bulimia nervosa, binge eating disorder)
• Bariatric surgery (including gastric sleeve, gastric bypass, lap band)
• Thyroid disease (hypothyroidism or hyperthyroidism)
• Cardiovascular diseases requiring medication, including ACE inhibitors, beta-blockers, warfarin and statins
• Mental health conditions requiring medications
• Gastrointestinal disorders, such as diverticulitis, bowel obstructions, bowel resections, irritable bowel syndrome (IBS), and inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease).

As discussed in the ‘Confirm Physical Health’ unit within the 111046NAT - Certificate IV in Nutrition, screening for ‘at risk’ clients using a Risk Stratification Screening Tool (RSST) identifies which clients are within or outside a nutrition coach’s scope of practice. The screening tool identifies several different areas in the client’s current and genetic health, which may exclude them from being able to consult with a nutrition coach until medically cleared by a GP.
The screening tool is vital as it benefits the nutrition coach and ensures the appropriate care is provided to the client, subsequently allowing for better health and wellbeing.
The RSST will work through the following steps to ensure nutrition coaches practice within their scope of practice.
SECTION 1: IDENTIFY THE CLIENT’S CURRENT HEALTH STATUS
PART A) Identify current medical conditions
PART B) Identify ‘at risk’ factors.
SECTION 2: IDENTIFY POSSIBLE FOOD INTOLERANCES AND/OR ALLERGIES
SECTION 3: IDENTIFY FAMILY HEALTH HISTORY
RISK-STRATIFICATION SCREENING TOOL
To view the Risk-Stratification Screening Tool (RSST) CLICK HERE.
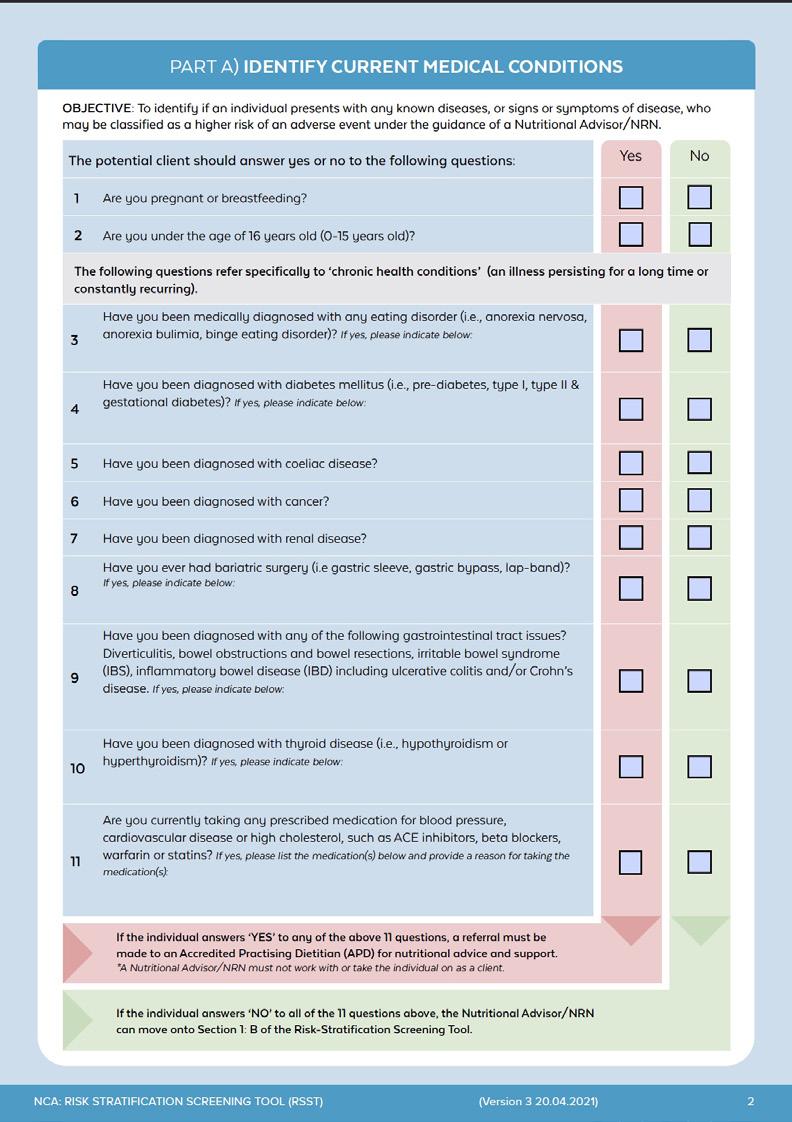



Due to the increased risk and challenges that medical conditions can have on client care, it is critical to identify clients outside the scope of practice of a nutrition coach. Section 1 of the industry-endorsed RSST focuses on identifying the client’s current health status and the need for referral.
There are two components within Section 1 of the RSST that collect vital information about the client; this includes:
PART A) Identify current medical conditions.
PART B) Identify ‘at risk’ factors.
Medical conditions refer to any condition the client has that could impact the support a nutrition coach can offer through the prescription of individualised nutritional plans. Nutrition coaches need to analyse the situation and the client’s information to make a decision based on their scope of practice and any contraindication that may be identified. This decision will also then dictate whether or not the client needs to be referred to a more suitable medical or allied health professional.
Nutrition coaches must be aware of common conditions, health factors and chronic diseases that warrant a referral to an appropriate health professional. Nutrition coaches should always refer to their scope of practice when in doubt of a client’s eligibility.
Any client presenting with the following conditions/contraindications are required to be directly referred to an Accredited Practising Dietitian (APD) for nutritional advice and support:
• Pregnant or breastfeeding
• Individuals under the age of 16 years old (0-15 years)
• Individuals with medical conditions including but not limited to:
• Eating disorders (anorexia nervosa, bulimia nervosa, binge eating disorder)
• Diabetes mellitus (pre-diabetes, type 1, type 2 and gestational diabetes)
• Coeliac disease
• Cancer – current diagnosis and/or receiving cancer treatment
• Renal disease
• Bariatric surgery (including gastric sleeve, gastric bypass, lap band)
• Chronic gastrointestinal tract issues, such as diverticulitis, bowel obstructions, bowel resections, irritable bowel syndrome (IBS), inflammatory bowel disease (IBD), including ulcerative colitis and Crohn’s disease
• Thyroid disease (hypothyroidism or hyperthyroidism)
• Prescribed medications for blood pressure, cardiovascular disease and high cholesterol, such as ACE inhibitors, beta-blockers, warfarin or statins.

If the client answers ‘yes’ to any of the questions in Section 1: B, this indicates potential risk factors. A referral must be made to a GP for a more detailed assessment, and a medical clearance must be attained. A nutrition coach can work with the client only after a clearance has been granted by the GP.
1. Is your BMI under 18.5 (<18.5)kg/m2 or over 40kg/m2 (>40)?
A BMI below 18.5kg/m2 is classed as underweight, whereas a BMI over 40 is classed as ‘Level 3 Obesity’ (very severe). Underweight and obese clients are often at risk of malnutrition and deranged pathologies such as high/ low blood sugar levels, cholesterol and blood pressure.
It is important to note that BMI is a calculation based on total body weight and total body height. BMI does not take the type of weight (muscle or fat) into consideration and, therefore, may place a client with a high muscle mass level into the obese category. Therefore, the nutrition coach must consider the distribution of total body weight and not draw conclusions based only on weight.
2. Have you been diagnosed with any conditions impacting fertility? For example, polycystic ovarian syndrome and endometriosis.
Fertility conditions can cause changes in hormones, weight and glucose regulation, which can affect a client’s macronutrient and micronutrient requirements.
3. Have you been formally diagnosed with any food allergies and/or intolerances?
Food allergies are an immune-mediated response, and food intolerances are a sensitivity to certain foods that can impact a client’s nutritional intake. Diagnosing allergies and intolerances requires specialised intervention by a GP. Care must be taken to ensure that the offending food is not included in the client’s diet to avoid adverse symptoms such as pain, gastrointestinal upset and difficulties breathing.
4. Have you been formally diagnosed with a mental health condition in which you are required to take medication?
There are many mental health conditions (including depression, ADD/ADHD, anxiety, bipolar and schizophrenia) that require medication as part of their treatment and management. Many of these medications can affect metabolism, weight and nutritional needs, which will affect the effectiveness of a nutritional plan.

The objective of Section 2 is to identify possible food intolerance or allergies that a client may have. This is a key factor in the screening process as this may require a more detailed level of assessment by a qualified Accredited Practising Dietitian (APD).
IF THE CLIENT ANSWERS YES TO TWO OR MORE OF THE FOLLOWING, A REFERRAL TO AN APD IS RECOMMENDED:
1) Do you experience bloating regularly?
2)
3)
4)
5)
Do you believe you suffer from excessive flatulence? (Note: There is no normal amount, but just asking if a client experiences more flatulence than what they consider normal and if the smell is “offensive” provides an initial indication of concern).
Do you experience irregular bowel motions (e.g. diarrhoea, constipation, difficult to pass, abnormal colours, faecal urgency)?
If yes, please provide detail on the number of eliminations per day, stool colour, stool abnormalities and stool formation where possible.
Do you believe you suffer from low energy levels? (Discuss with the client the reason for low energy levels. Unexplained low energy levels may indicate poor nutritional absorption).
Do you suspect you may have any food allergies and/or intolerances?
If yes, please identify why you think you may have an allergy/intolerance and to what specific food.
If the client answers ‘yes’ to two or more of the above questions, it is ‘recommended’, however not mandatory that a referral be made to a general practitioner (GP) for a more detailed assessment and a medical clearance.
*It is at the discretion of both the individual and the nutrition coach as to whether or not nutritional support and guidance will continue under the supervision of the nutrition coach or if the client will be referred to a GP. If the client is happy to continue with nutritional support under the guidance of the nutrition coach, then the nutrition coach can continue to work with the client.

A food allergy is an immediate immune system reaction that affects the body and may potentially be severe or even life-threatening. Allergies are the body’s immune system overreacting to allergens (such as proteins) in foods where they are treated as toxic. Food allergies affect approximately 5% of children and 2% of adults.(4)
The nine most common food allergies are:(5)
1. Eggs
2. Peanuts
3. Soy
4. Milk
5. Wheat
6. Fish
7. Shellfish
8. Tree nut
9. Sesame
Individuals who suffer from food allergies may struggle with any number of the following symptoms: (6)
• Itching, burning, and swelling around the mouth
• Swelling of face or eyes
• Runny nose
• Skin rash (eczema)
• Hives (urticaria - skin becomes red and raised)
• Diarrhoea
• Abdominal cramps/pains
• Breathing difficulties, including wheezing and asthma
• Vomiting
• Nausea.
A food intolerance, on the other hand, is a chemical reaction to a food or drink rather than an immune response.(7) An individual can experience symptoms a few minutes to a few days following ingestion of the offensive food. Typically, consuming small amounts of the food may not trigger an effect in some individuals; however, others may need to avoid the offending food altogether.
Food intolerances may stem from one of several factors, such as:
• The absence of an enzyme required to fully digest a type of food (i.e. lactose intolerance)
• A sensitivity to a type of food or a food additive (gluten intolerance), or
• An existing non-IgE (non-immunoglobulin E) mediated condition such as Coeliac disease.(7)
Individuals who suffer from food intolerances may experience any of the following symptoms:(8)
• Headaches/migraines
• Diarrhoea
• Nervousness
• Tremor
• Sweating
• Palpitations
• Rapid breathing
• Burning sensations on the skin
• Tightness across the face and chest
• Breathing problems (asthma-like symptoms)
• Allergy-like reactions.
If a client identifies as having a food allergy or intolerance, you must obtain a medical clearance from a GP before proceeding with the client.

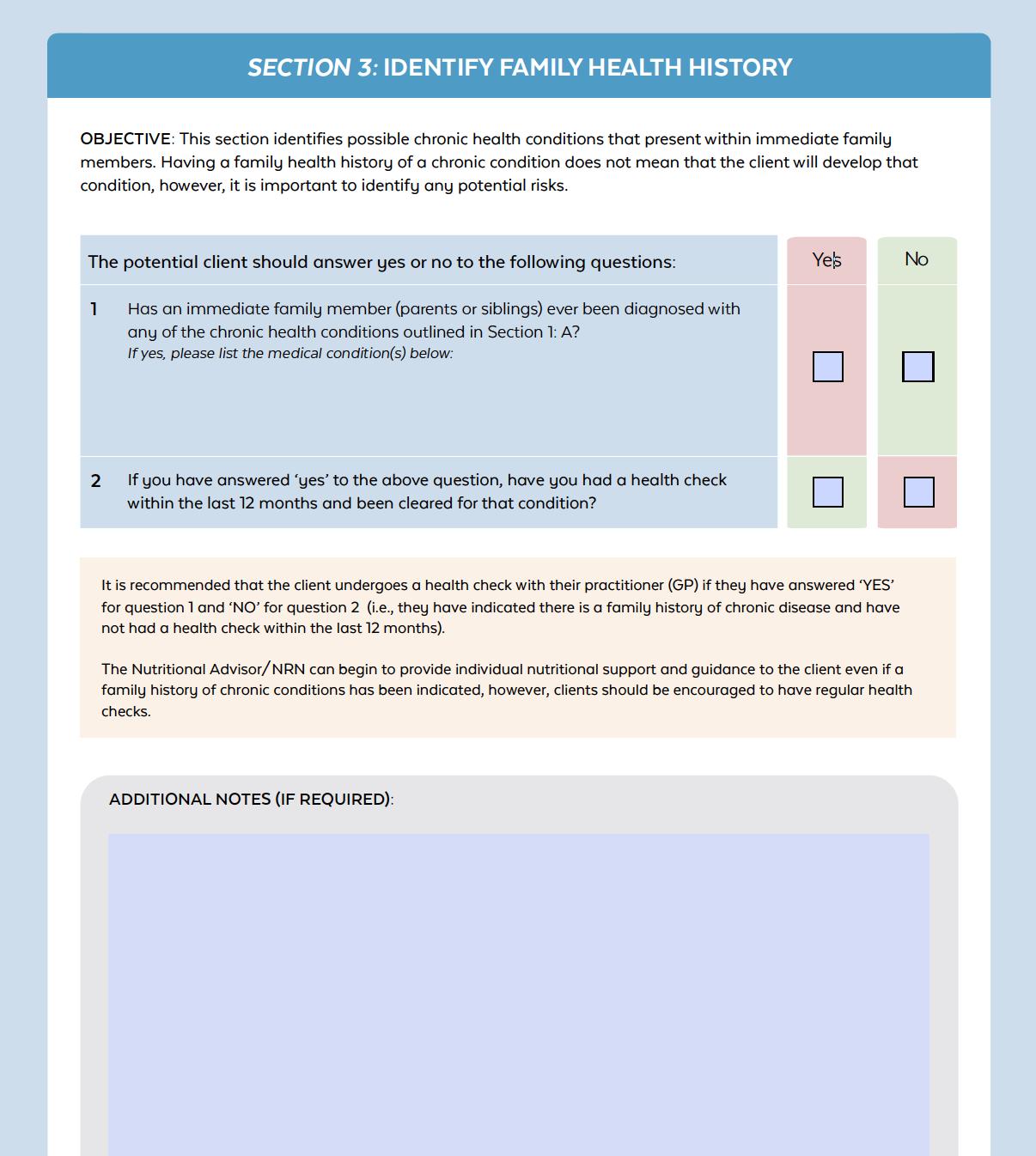
This section identifies chronic health conditions that may present among immediate family members. It enables the nutrition coach to give support and guidance around managing chronic disease risk. The nutrition coach can also use this section to emphasise the importance of regular health checks with a general practitioner (GP).
Has an immediate family member (parents or siblings) ever been diagnosed with any of the chronic health conditions outlined in Section 1: A?
1)
2)
The purpose of question one is to identify any family medical conditions. If the client ticks ‘yes’ to this question, the nutrition coach can take a record of the client’s family medical history. This health information is about a client’s immediate family members, parents and siblings. For example, their mother may have heart disease, or their sister may have gestational diabetes.
It is important to record this information because the client may be at a higher risk of developing chronic disease. For example, a client with a family history of heart disease is more likely to develop that condition compared to a client with no family history of heart disease.
If you have answered ‘yes’ to the above question, have you had a health check within the last 12 months and been cleared for the condition?
The purpose of question two is to find out if the client has had any recent health checks. Generally, it is recommended that any client undergoes a regular health check with a GP. This is particularly important because the client has indicated a family history of chronic disease, and they have not had a health check within the last 12 months.
The nutrition coach can begin to provide individual nutritional support and guidance to the client even if a family history of chronic conditions has been indicated. However, clients should be encouraged to have regular health checks, and nutrition coaches should also monitor for signs of disease.

The depth of knowledge and training/education required to effectively and safely support the previously mentioned out of scope clientele is not sufficiently covered in the training and education of the 11046NAT - Certificate IV in Nutrition. A referral to an appropriate medical or allied health professional (AHP) is required for clinical nutrition-related advice or for any clientele who falls outside of the scope of practice (who are deemed ‘at risk’) for a nutrition coach.
The appropriate health professionals to refer to are as follows:
• Accredited Practising Dietitian (APD)
• Accredited Sports Dietitian
• General practitioner (GP).
Collaborative practice with the appropriate health professional/s is an imperative approach to protect out of scope clientele from unsuitable or potentially detrimental nutritional advice. In turn, this can also prevent the possibility of legal liability linked with providing nutritional advice to such clients. Furthermore, this collaborative approach can improve the industry by growing networks for client referrals and increasing expert credibility and integrity within the health and fitness industry.
More Information can be found using the following links:
Accredited Practising Dietitian: CLICK HERE to view the link.
Accredited Sports Dietition: CLICK HERE to view the link.
It is important to remember that a nutrition coach focuses on providing advice to healthy clients. As discussed in the RSST, there are instances where a nutrition coach is required to take action if a client is at risk of falling outside of the scope of practice of a nutrition coach. Generally, there are two different requirements for a nutrition coach, which are identified in the table below:
REQUIREMENT 1
REFER DIRECTLY TO A MEDICAL OR ALLIED HEALTH PROFESSIONAL
REQUIREMENT 2
If any client is identified in Section 1: Part A of the RSST as ‘high risk’, then a nutrition coach must refer directly to a relevant medical or allied health professional, as they fall out of a nutrition coach’s scope of practice
*This would mean that the nutrition coach cannot work with the client and must refer on.
If any client is identified in Section 1: Part B of the RSST as ‘at risk’, then a nutrition coach must refer the client to a GP for a more detailed assessment and written medical clearance.
SEEK MEDICAL CLEARANCE FROM A GP

If any client is identified as answering ‘yes’ to two or more questions in Section 2 or 3, it is recommended that the nutrition coach refers the client to a GP for a more detailed assessment and medical clearance.
*It is only after a clearance has been made by the GP that a nutrition coach can continue to work with a client.
The table below outlines the roles of necessary health professionals that are relevant in the referral process for nutrition coaches:
Accredited Practising Dietitians (APDs) are university-qualified professionals that undertake ongoing training and education programs to ensure that they are the most up-to-date and credible source of nutrition information. They translate scientific health and nutrition research into practical advice and practice in line with Dietitians Australia’s (DA) Professional Standards.
An Accredited Sports Dietitian is an APD that has undergone further education and training in sports nutrition practice.
A General Practitioner (GP) is a doctor who is also qualified in general medical practice. GPs are often the first point of contact for clients of any age who feel sick or have a health concern. They treat a wide array of medical conditions and health issues.
A GP may also undergo further education in specific areas such as women’s or men’s health, sports medicine or paediatrics.
Refer the client to a GP if they have not had their cholesterol, blood glucose or blood pressure checked in the past 3-6 months.(12) The GP will write a pathology script to check blood glucose and cholesterol levels and check blood pressure in the clinic. If all results are within range, the client can return to the nutrition coach and continue under their care.


Refer the client to an APD if they have any of the listed health conditions in Section 1 or any potential diagnosed food intolerances and/or allergies identified in Section 3 of the Risk Stratification Pre-Screening Tool. The correct dietary support is detrimental in their health outcome.
The role of a psychologist is to assess, diagnose, and treat the psychological problems and the behavioural inhibitions resulting from or related to physical and mental health.(13) A nutrition coach would refer the client to a psychologist when the client is outside their scope of practice and the issues are related to mental health.
Examples of when a nutrition coach would refer a client to a psychologist include:
• Depression
• Anxiety
• Eating disorders (e.g. anorexia nervosa, bulimia nervosa, binge eating disorder)
• Negative self-talk
• Indication of self-harm
• Insomnia or severe fatigue
• Very low self-esteem
• Bipolar disorder
• Substance abuse
• Indications of verbal, physical or sexual abuse
• Addictions
• Post-traumatic stress disorder
• Strained relationships.
Refer the client to a personal trainer if they want exercise recommendations in combination with nutritional advice. Personal trainers are equipped to provide exercise recommendations to assist clients with weight loss, body composition and muscle building.
While nutrition coaches can encourage clients to exercise, it is outside their scope of practice to provide individualised exercise recommendations beyond the Australian Physical Activity and Sedentary Behaviour Guidelines (unless suitably qualified to do so).
For more information on these guidelines CLICK HERE.


There are several elements that should be documented through the client support process. Initial client records, screening surveys and documents, such as assessment results, should be retained within the client’s record. These records come together to form a ‘client profile’.
Nutrition coaches are advised to collect all relevant information and documents from their clients as this serves two primary purposes:
1. The information collected forms a record for tracking the client’s progress against their nutritional goals
2. The documents and information form a legal record of advice provided.
Whether electronic or hard copy, it is important that each client has an individual record consisting of the following documents, at a minimum:
• The client’s completed Risk Stratification Screening Tool (RSST)
• Pre-screening questionnaires and any assessment results
• Initial consultation notes
• The client’s nutrition plan and/or nutritional recommendations
• Progress records (i.e. monitoring assessment records, follow-up consultation records).
In addition to the above, nutrition coaches may also gain feedback from their clients using feedback forms, surveys or additional documentation. It is also a good idea to collect and store this information for future reference.
When considering how these documents are retained, it is important to remember the requirements of the Australian Privacy Act (1988) governing the retention and management of documentation. The information provided by the client, and that which was gathered during the support process, remains confidential. This means reasonable measures must be taken to secure the information and ensure it is not accessible by others.



Before going into detail on how to develop a nutritional plan, a nutrition coach must understand the body’s primary systems and their functions. Although this has been covered in previous units (such as the unit ‘Confirm Physical Health Status’), revisiting and understanding these systems allows for an appreciation of how nutrients are utilised and processed within the body, identifying where clients may require some modification to their diet and any potential health issues.
As a quick review of previous units within this course, the information below provides a brief summary of each of the body’s main systems:
• Digestive system
• Integumentary system
• Respiratory system
• Circulatory system
• Skeletal system
• Muscular system
• Endocrine system
• Urinary system
• Reproductive system.
DIGESTIVE SYSTEM
INTEGUMENTARY SYSTEM
RESPIRATORY SYSTEM
Breaks down food into components (such as vitamins, minerals and other nutrients) that the body can use for:
• Energy production
• Repair of tissues
• Growth
• Immune function.
• Protects the body from loss of water and abrasions from the outside.
• Movement of air and carbon dioxide through the body
• Gas exchange between air and circulating blood
• Producing sounds heard in communication
• Maintaining respiratory health.
CIRCULATORY SYSTEM
• Carries nutrients, oxygen, carbon dioxide, hormones, antibodies and blood cells to all parts of the body
• Maintains homeostasis and immunity
It can help improve the function and health of a client’s digestive system.
It can help promote healthy hair, skin and nails and efficient wound healing.
It can help maintain energy production, fat burning and help keep the respiratory system functioning correctly by supporting immune health.
It can help maintain healthy blood lipid (cholesterol) levels and blood glucose levels and reduce the likelihood of free radical damage or inflammation to blood vessels and joints.

SKELETAL SYSTEM
MUSCULAR SYSTEM
ENDOCRINE SYSTEM
NERVOUS SYSTEM
URINARY SYSTEM
• Provides support, locomotion, and protection for the body.
• Also produces red blood cells and stores important minerals for the body.
• Production of skeletal movement
• Maintenance of posture and body position
• Support and safeguard exit and entry points of the body
• Support soft tissue
• Store nutrient reserves
• Maintain body temperature, heat, and homeostasis.
• Produces hormones that regulate metabolism, growth and development, reproduction, mood, sleep and sexual function.
• How the body moves communication throughout the body
Plays a crucial role in maintaining the strength and health of the bones.
REPRODUCTIVE SYSTEM
• Responsible for the removal of waste products from the human body
It can help muscle maintenance, growth and energy for daily work and exercise.

• A system of sex organs which work together for the purpose of reproduction.
It can help support the functioning of the endocrine system by reducing stress on the body, by eliminating undesirable food choices and promoting foods that assist in immune health.
It can help provide sufficient healthy fats for brain health and all the nutrients required for nerve signallings such as sodium and potassium.
Water is an essential component of this system to aid in the excretion of waste products. A well-designed nutrition plan will account for an individual’s fluid requirements to support urinary health by preventing dehydration.
Although it is outside a nutrition coach’s scope of practice to work with pregnant or breastfeeding women, they can still encourage their clients to follow a healthy, well-formulated nutrition plan before conception. A well-designed nutrition plan that promotes appropriate nutritional intake, including adequate amounts of nutrients such as dietary fat, protein, folate, selenium, zinc and vitamin C, supports the formation of healthy sperm andthe development of eggs.

All human body functions require energy, from breathing and the heart beating to exercising and laughing. Everything the body does can only be done through using energy.
Calories and kilojoules (kJ) are both measurement for energy obtained from food, where 1 calorie equals 4.184 kilojoules. (15)
1 calorie = 1 kilocalorie
1 calorie = 4.184 kilojoules (kJ)
1 megajoule (mJ) = 1,000kJ.(15)
The energy required in the body is obtained through food, more specifically, from macronutrients. When broken down during digestion, each macronutrient produces a specific amount of energy per gram. Some macronutrients are more energy-dense than others.
The table below shows how much energy, in the form of kilojoules and calories, is found in each macronutrient and alcohol per gram.
NOTE: FOR SIMPLICITY, KILOJOULES HAVE BEEN ROUNDED TO THE CLOSEST WHOLE NUMBER)(15)
Kilojoules is the standard unit of measurement amongst health professionals and is more well-known in Australia. In Australia, kilojoule’s are commonly used on nutrition labels because it is a metric unit and therefore easier and more accurate to calculate with, given the Australian use of the metric system.(16)
The body requires a certain amount of energy each day to function optimally. It is referred to as energy intake - the daily amount of energy consumed through the diet. Simultaneously, the body uses energy for all physiological functions and all physical activity.
In healthy individuals, if their energy intake is higher than the amount of energy they expend, they will gain weight. Conversely, if a healthy individual’s energy intake is less than the amount they expend, they will lose weight. Energy balance or maintenance, therefore, occurs when an individual’s intake is equivalent to their energy expenditure.
The amount of energy required by each client depends on many factors, including height, age, weight, gender, physical activity levels and metabolic demands. Those factors will be used to calculate and develop clients’ nutritional recommendations or meal plans. Energy requirements are further discussed in the following pages.

When developing a client’s nutritional plan, it is important that the nutrition coach has a sound understanding of the key nutrients contained within foods. Understanding the nutritional value of food allows a nutrition coach to comprehend the basic requirements of each nutrient, which then forms the basis for calculating and creating a nutritional plan.
As this information has been previously covered in an earlier unit for this course, a brief summary of each major nutrient group and its relevance is provided in the section below.


Protein is needed by the body not only for muscle recovery, repair and synthesis but for the structure, function and regulation of the body’s cells and tissues.(17)
Protein is found in both animal and plant-based sources, including:
• Meat (such as chicken, beef, pork, and lamb)
• Fish
• Eggs
• Pulses (such as beans, peas and legumes)
• Nuts and seeds
• Dairy products (such as milk, yoghurt and cheese).
Proteins are made up of chains of smaller chemicals called amino acids. There are approximately 20 different amino acids that are found in food. Amino acids can be classified as those which the body can make (non-essential) and those which the body cannot make and therefore need to be obtained through the diet (essential). Different foods contain different amounts and types of amino acids.(17)
As a nutrition coach, it is important to be aware of the role of protein and further educate clients on how protein is essential for human health and wellbeing.
Humans require protein in regular, moderate quantities to ensure correct bodily function and overall health. A diet lacking in a range of proteins can lead to poor health outcomes, including weakness, fatigue, slowed recovery from exercise and muscle wastage.
Protein is not only an energy-yielding macronutrient, containing 17kJ per gram, but it also has several other significant roles in the human body.(15)
The primary role of protein relates to the structure, function and regulation of the body’s cells and tissues; this includes:
• Tissue repair and production (protein synthesis)
• Hormone production
• Enzyme production
• Immune function
• Energy production.


Protein is found in both animal and plant-based food sources, including meat, fish, eggs, pulses, nuts, seeds and dairy products.
It is important to remember that 100g of food (e.g. 100g of chicken) does not equate to 100g of protein. For example, there is 30g of protein found in approximately 150g red meat, 100g white meat, 150g fish, 5 large eggs or 1L of milk.(17)
Some foods are understandably higher in protein and more bioavailable. Below is a table of common protein foods and the amount of protein found in a 100g serve. It is imperative to note that a food’s protein content is only a portion of the total serve size, not the entire weight of the food. For example, 100g of baked snapper has 26g of protein; therefore, only 26% of the serve is protein.
BIOAVAILABILITY
‘Bioavailability’ refers to the degree to which a substance can be absorbed and utilised by the body.(18) Protein bioavailability is therefore a measure of how well protein is absorbed and utilised in the body. There is an array of factors which will affect a protein’s bioavailability, such as the type and amount of amino acids that are present in the food, the chemical structure of the protein consumed, the amount and effectiveness of an individual’s protein-digesting enzymes and the type of dietary protein sources consumed.
POULTRY
100g chicken breast (skin off/grilled) 31
100g chicken thigh (skin off/grilled)
100g lean sirloin steak (grilled)
100g lean beef mince (raw)
100g lean tenderloin steak (raw)
100g lean tenderloin steak (raw)
100g bacon (middle rasher, lean, fried)
100g lamb leg (boneless, roasted)
100g tuna (in oil, drained)
100g snapper (baked)
100g salmon (grilled)

EGGS
1 egg (whole, large, hard-boiled)
1 egg (white only, large, poached)
100g regular cheddar cheese
100g cottage cheese (low-fat)
100g plain Greek yoghurt (low-fat)
250ml milk (low-fat)
250ml milk (full cream)
NUTS AND SEEDS
100g peanuts (dry roasted, no salt)
100g almonds
100g sunflower seeds (dry roasted, no salt)
100g pumpkin seeds (pepitas, dried)
100g cashews (dry roasted, no salt)
100g walnuts (raw)
100g macadamias (raw)
LEGUMES AND GRAINS
100g kidney beans (raw)
100g chickpeas (raw)
100g soybeans (dry roasted)
100g lentils (boiled)
100g canned baked beans in tomato sauce
100g brown rice (boiled)
100g white rice (boiled)
SUPPLEMENTS
30g scoop whey protein isolate (WPI)
30g whey protein concentrate (WPC)
30g soy protein
100g tofu (firm, hard)
coconut milk
100g coconut yoghurt

Complete proteins are sources of protein that contain all nine essential amino acids, whereas incomplete proteins refer to proteins that do not contain all nine essential amino acids.
The nine essential amino acids that make up a complete protein include:(20)
1. Histidine
2. Lysine
3. Threonine
4. Isoleucine
5. Leucine
6. Methionine
7. Phenylalanine
8. Tryptophan
9. Valine.

The table below discusses the difference between complete and incomplete proteins in more detail:
Proteins that encompass all of the nine essential amino acids are thought of as complete proteins.
Complete proteins are important because they provide the full range of essential amino acids which cannot be produced in the body. Without a regular supply of these amino acids, muscle tissue will be broken down to supply them, which is not ideal for long-term health.
These complete proteins mostly come from animal sources, such as:
• Eggs
• Chicken
• Beef
• Lamb
• Pork.
And some plant sources, such as:
• Quinoa
• Buckwheat
• Soy
• Quorn (a meat substitute made from a fungus).

Proteins that do not contain all nine essential amino acids are considered incomplete proteins.
Plant foods are predominantly incomplete protein sources; however, this does not mean that they are a lowquality protein.
Examples of incomplete proteins include:
• Grains such as rice, pasta and bread (lack/low in threonine, leucine, lysine and histidine)
• Legumes such as beans, peas and lentils (low in methionine)
• Starchy vegetables such as potato, pumpkin and sweet potato (low in lysine)
• Nuts such as walnuts, macadamia and almonds (low in threonine).
Simply because a type of protein is incomplete does not make it inferior. Incomplete proteins can be combined to form the full range of essential amino acids to create a complete protein. Someone following a vegetarian or vegan diet should consider doing this to ensure they are consuming all of the essential amino acids in their diet, especially if they are exercising regularly.
A further benefit of combining plant-based foods in the diet (to achieve a complete range of essential amino acids) is the other nutrients accompanying them, including fibre, vitamins and minerals (which will be covered later in this resource).
To do this, two plant foods with varying amino acid profiles must be combined, for instance, grains with vegetables. Proteins combined to make a complete amino acid profile (containing all the nine essential amino acids) are known as complementary proteins, after which they can then be classified as a complete protein.(21)
Examples of complementary proteins include (but are not limited to):
• Spinach salad with almonds
• Hummus and whole-grain pita bread
• Navy beans (baked beans) on wholemeal toast
• Natural peanut butter wholemeal sandwich
• Black beans with rice (white or brown)
• Tofu with rice (white or brown)
• Macaroni and cheese.
Complementary proteins do not necessarily need to be eaten together; however, since the body has limited capacity for storing amino acids, they should be eaten throughout the day.(21)





Many myths about protein circulate in the community, especially in health and fitness. Below are some evidence-based facts to disprove common myths:
The body can only absorb and use 25g of protein in one meal.
Excess protein will turn to fat if not used by the body.
The body will absorb all protein from a meal, but how much protein it uses is demand-driven; for instance, a bodybuilder will likely require and use more protein than a sedentary, untrained office worker because the body of the former has a higher requirement for muscle repair and growth.
The human body cannot store excess protein or amino acids. Unneeded amino acids get broken down by the liver and removed by the kidneys. In saying that, if a client is exceeding their EER, excess energy from any macronutrient source (including protein) will be stored as fat.(21)
Consuming a high protein diet can cause kidney damage.
It is best to consume protein within 30 minutes of finishing a resistance workout
Consumption of excess protein will result in muscle gain even if a client does not participate in any physical activity.
Protein is only needed for those who exercise regularly or want to put on muscle mass.
Protein shakes (i.e. whey protein) are the only source of protein that should be consumed after a workout
Recent scientific reviews of protein dosing and health have confirmed the safety of high protein diets in adults with healthy kidneys and no history of kidney disease.(21) However, there has been very little proven benefit in increasing protein intake above the EPR.(21) Protein needs will vary depending on activity level, gender and age. As such, it is important to remain within the recommended EPR ranges for each individual to meet their goals and avoid compromising intake of other important nutrients.
Consuming protein is recommended within 2 hours of resistance training to promote immediate muscle recovery, but protein demand can be elevated for up to 24-48 hours. So regular dosing of protein every 3-4 hours is recommended.(21)
Without sufficient physical stimulus (e.g. resistance training), the excess protein will be excreted from the body, and muscles will not grow. Amino acids help repair muscle tissue after exercise, increasing muscle growth.(21)
Adequate protein is essential for growth, repair, hormone and enzyme production, and overall health throughout the lifespan, regardless of lifestyle; it is needed for all biological processes daily and is essential for optimal health, even in individuals who do not exercise.
Protein shakes and other protein supplements are convenient and can be quickly absorbed after a workout. However, it is best to prioritise wholefood protein sources over supplements to meet the body’s protein needs, as they include various other beneficial nutrients like fibre, vitamins and minerals.

• Proteins are commonly referred to as the ‘building blocks of life’, signifying their importance in the human body.
• Proteins are nitrogen-containing substances that are digested/broken down into amino acids.
• Proteins are utilised to produce new tissues for growth and repair and to regulate and maintain body functions; they also aid in producing essential hormones and are fundamental for the digestive system and immunity enzymes.
• There are 500 known amino acids, 20 of which humans need. Of these 20, there are nine essential amino acids.
• Most health organisations recommend a protein RDI of 0.8-1.0g per kg of body weight per day; however, this recommendation can increase depending on physical activity levels, disease states, trauma and stress levels.
• Protein can be found in various foods, including animal and plant sources. The quality and bioavailability of the protein change from food to food, generally with animal-based protein containing more complete and bioavailable protein than plant-based proteins.
• A complete protein refers to a source of protein that contains all nine of the essential amino acids.


Carbohydrates (also known as saccharides or ‘carbs’) are organic compounds made up of sugars or starches. The body utilises this macronutrient as an immediate source of energy. Carbohydrates are a major food source and a key form of energy for most organisms. One gram of carbohydrate provides approximately 17kJ of energy.(15)
Regardless of origin, all carbohydrates are broken down in the body into a simple sugar, depending on their source and structure. These are most commonly glucose (honey), fructose (from fruit) and galactose (from dairy).(22)(23)
Certain parts of the carbohydrate (such as starch and fibre) slow the release of sugar into the bloodstream, resulting in increased satiety, improved gut flora (by acting as a prebiotic) and regulated bowel motions. While the body breaks down starch into simple sugars, fibre passes through relatively undigested. The fact that fibre is not broken down does not void its importance in the human diet as it dramatically benefits bowel motions, gut flora and satiety.
The Australian Government recommends carbohydrate intake to be approximately 45-65% of the diet, with the focus primarily on low GI carbs. It is important to keep in mind the type of client you’re working with, what their goals are, and their need for carbohydrates when determining where in this range they will sit.(22)(15)
As a nutrition coach, it is important to understand the role carbohydrates play in the human body to assist with individualised macronutrient recommendations.
Carbohydrates have three fundamental roles in the human body, including(24)(25)(23):
• Provide the body with an immediate fuel supply
• Provide the body with stored energy
• Assist with digestive health and disease prevention.
Carbohydrates, regardless of their origin, are broken down into their most simple form and utilised as energy for the body. Carbohydrates can be utilised as an immediate source of energy. As soon as sugar enters the bloodstream, it can be used by cells around the body that require energy to carry out any number of tasks.
Carbohydrates are especially beneficial as an immediate fuel supply for athletes completing longer distance or higher intensity events, such as marathon running or competitive rowing.
When more carbohydrates are consumed than burned, excess carbohydrates are converted to fatty acids and stored as fat. When fat is required for energy, fat is converted back to glucose through a process known as gluconeogenesis, and that glucose is then used for energy. This type of energy can be used at a later stage when there is no immediate supply of blood glucose.
The fibrous component of carbohydrates (discussed later in resource) has several important roles. These roles include:
• Feeding gut bacteria
• Regulating bowel motions
• Optimising cholesterol levels
• Regulating sugar levels
• Decreasing risk of bowel disease.

Carbohydrates can be divided into two main categories:
1. Simple carbohydrates
2. Complex carbohydrates.
MONOSACCHARIDES (one sugar molecule)
DISACCHARIDES (two sugar molecule)
OLIGOSACCHARIDES (three to nine sugar molecule)
POLYSACCHARIDES (ten or more sugar molecules) GLUCOSE SUCROSE RAFFINOSE STARCH FRUCTOSE LACTOSE STACHYOSE GYCOGEN
GALACTOSE MALTOSE CELLULOSE
The terms simple and complex refer to the complexity and length of the carbohydrate in question. Generally, the more complex a carbohydrate is, the greater the amount of fibre the food source contains.
Fibre is a dietary material resistant to the action of digestive enzymes(23). This means that the body does not break down fibre, and it passes through the gastrointestinal tract relatively intact. As mentioned above, fibre helps regulate bowel motions, slow the breakdown of carbohydrates and increase satiety(23). Examples of fibre in dietary sources include the husk of nuts and seeds and the skin on fruit and vegetables. Dietary fibre will be discussed in greater detail later in this unit.
Simple carbohydrates refer to carbohydrate-rich foods which are less complex, have minimal/less dietary fibre, and are therefore more rapidly broken down within the body. This results in a quicker release of sugar in the bloodstream and a faster supply of immediate energy. Examples of simple carbohydrates are foods that have been processed or refined, such as fruit juice, lollies and sugary cereals.
Simple carbohydrates are quicker to break down in the body than complex carbohydrates because they are shorter in length.
Simple carbohydrates include:(23)
• Monosaccharides (one sugar molecule in length)
• Disaccharides (two monosaccharides joined together).


Complex carbohydrates refer to sugar molecules that are strung together in long, complex chains. Due to the length of the chain and the fibrous and starchy components of the carbohydrate, complex carbohydrates take longer for the body to break down. As a result, complex carbohydrates have a slower release of glucose into the bloodstream. This is beneficial in assisting with satiety, cravings and energy levels.
Examples of complex carbohydrates are carbohydrate-rich foods in their most natural form, such as:(23)
• Sweet potatoes
• Quinoa
• Couscous
• 100% whole wheat pasta
• Peas
• Beans (e.g. kidney beans, cannellini beans, butter beans)
• Lentils
• Pumpkin.
These foods are a source of carbohydrates, however still contain their natural dietary fibres (such as the skin, seeds and husk) and starches.


There are a number of dietary myths encompassing carbohydrates which can confuse the general public. Below are some evidence-based facts to disprove common myths:
It is fine for clients to consume as much carbohydrate as they please, provided it comes from an unprocessed food item.
Table sugar alternatives are healthier for the human body and can therefore be consumed without limit.
Only bread and pasta contain carbohydrates.
Carbohydrates make you gain weight.
Carbohydrates are not needed in the diet, as the body creates its own glucose.
While an unprocessed carbohydrate, such as an apple, is more beneficial to human health than a processed carbohydrate, such as apple juice, the intake of excess (natural) sugar can still adversely affect health, increasing the risk of:(22)
• High blood pressure
• Type 2 diabetes
• Heart disease
While alternatives to table sugar, such as dried fruit or natural honey, are healthier due to their increased nutrient profiles (fibre, vitamins, minerals, antibacterial properties), their consumption should still be limited. While they may not spike blood glucose levels compared to refined sugars they are still high in kilojoules and sugar, which can be detrimental to health.
Carbohydrates are found in several other different dietary sources, such as:
• Fruit
• Vegetables
• Dairy products
• Oats
• Beans
Excess energy intake from any energy-yielding macronutrient (including protein and fat) will cause weight gain – not specifically carbohydrates. If consuming carbohydrates as part of a well-balanced diet that meets energy needs, weight gain will not occur. Where possible, preference should be given for more complex, lower GI and higher fibre sources of carbohydrates, such as wholegrains, legumes and starchy vegetables.(26)
These sources have an improved effect on satiety, bowel function and gut health.(26) Excess sugar or highly refined carbohydrates, such as soft drinks, white breads, lollies, chocolate should be limited, to optimise health outcomes.
In times of starvation, the body can produce its own glucose through a process known as gluconeogenesis. However, this can negatively impact on the body’s protein and fat stores. Carbohydrates are essential for a healthy functioning body and should be included in the diet on a daily basis. Little research supports the use of low carbohydrate diets in the long term, as any weight loss is often regained, any improvement in blood lipids and glucose levels are not maintained and highly energy-dense fatty foods, particularly those high in saturated fats, can cause dysbiosis in the gut and low-grade chronic inflammation.(27)
As with any macronutrient, quality and quantity can impact on their usefulness in the body. Preference should be towards high fibre, low GI carbohydrates with small amounts of added sugars.

• Carbohydrates (also known as saccharides or ‘carbs’) are organic compounds made up of sugars and utilised by the body as an instant energy source.
• One gram of carbohydrate provides approximately 17kJ of energy.
• Carbohydrates have three fundamental roles in the human body, including providing the body with an immediate fuel supply, storing energy, and assisting with digestive health.
• All carbohydrates are made of carbon, hydrogen and oxygen with the general formula of CH2O.
• Carbohydrates consist of two main types - complex carbohydrates and simple carbohydrates. Simple carbohydrates include monosaccharides and disaccharides, and complex carbohydrates include oligosaccharides and polysaccharides.
• Carbohydrates come in many forms, predominantly in fruits, vegetables and grain-based products. It can also be sourced from dairy products and foods that have been formulated with added sugar.
• Natural sugars, also known as natural carbohydrates, are sugars that are found in unprocessed foods, such as fruit, vegetables, dairy and grains.
• Refined sugars, also known as processed sugars, processed carbohydrates or refined carbohydrates, are forms of sugars that have been altered or processed in some way and are no longer in their natural state.
• Excess sugar intake can be detrimental to an individual’s health, increasing their risk of heart disease and type 2 diabetes.


Dietary fat, although once portrayed in a negative light, is an essential part of the human diet. Fat not only provides an energy source for the body but also plays an important role in the absorption of fat-soluble vitamins, production of hormones, improving satiety and improving cognitive function.(23)
Dietary fats are a class of macronutrients essential in the human diet. All living tissues contain some form of fat (or lipids as they are scientifically called).
The main types of dietary fats are:(23)
• Saturated fats
• Unsaturated fats (monounsaturated and polyunsaturated)
• Trans fats.
Dietary fats should not be confused with body fat and the fats used in the body. Once dietary fat is digested, it is broken down into fatty acids and then repackaged into other useful types of fat, such as:(23)
• Phospholipids (used for cell walls)
• Cholesterol (used for cell walls, hormone production and fat-soluble vitamin production)
• Free fatty acids (used to build other fats)
• Triglycerides (used to store fat in adipose tissue).
As a nutrition coach, it is important to be aware of the role of fatty acids and educate clients on how dietary fat is essential for human health and wellbeing. Humans require dietary fats in regular, moderate quantities to ensure correct bodily function and overall health.
Dietary fat is not only an energy-yielding macronutrient, containing 38kJ (15)per gram, but it also plays several other very important roles in the human body.
The primary role of fat relates to the structure of all cells, as well as:(28)
• Helps with the regulation of hunger
• Provides the body with energy and stored energy
• Is critical for normal nerve function
• Stores some vitamins
• Maintains healthy cholesterol levels
• Forms the outer structure of all cells
• Contributes to healthy glowing hair, healthy skin and strong nails
• Improves brain function and brain development
• Improves efficiency and effectiveness of blood clotting when/if required
• Assists in reducing inflammation and increasing immunity
• Reduces cardiovascular disease risk
• Improves blood vessel elasticity
• Production and regulation of some hormones
• Decreases the risk of depression and anxiety.
In extreme cases, vitamin deficiencies caused by a significant lack of dietary fats can lead to weak and brittle bones (vitamin D deficiency), night blindness (vitamin A deficiency) and the inability of blood to clot effectively (vitamin K deficiency).(29)

The factors in the previous list are discussed in more detail in the following table.
The mechanism by which dietary fat helps to regulate hunger is still not completely understood. Many hormones in the body regulate hunger and fullness (satiety). Research has shown that dietary fat, and the composition of a meal, are important factors in achieving satisfaction and fullness after a meal.(23)
Dietary fat is used for instant energy production as well as being stored for use later in adipose (fat) cells.
Depending on energy balance (the amount of energy available in the body) and the demands of oxygen, the body’s cells determine whether energy production will come from fat or glycogen (stored glucose). For example, because energy production from fat requires oxygen, burning fat for energy only occurs in the aerobic system. This means that fat burning mainly occurs at rest and at low to moderate levels of exertion.(23)
Energy production from glycogen (glucose) does not require oxygen and can therefore occur in the anaerobic system during intense exercise (sprinting or strength training).
Nerve cells in the brain are coated with a special coating called a ‘myelin sheath’, which allows signals to pass through them very quickly. The myelin sheath (shown in the image below) is made from phospholipids, cholesterol (types of lipid), and proteins, which protect the nerve from damage and help increase the conduction speed of signals within the brain to the extremities.(30)
If nerve cells become damaged or are not repaired properly, over time, this can lead to neurodegenerative diseases such as Alzheimer’s and Parkinson’s disease. Multiple Sclerosis is a disease of the myelin sheath that can cause blurred vision, difficulty walking, muscle weakness and tremors (uncontrolled shaking).(30)

Cholesterol is a form of fat produced by the liver and eaten in the diet which is used for three main roles in the body:(23)
• Aids in the production of sex hormones
• Used for the production of human tissues such as cell membranes
• Used for bile production in the liver.
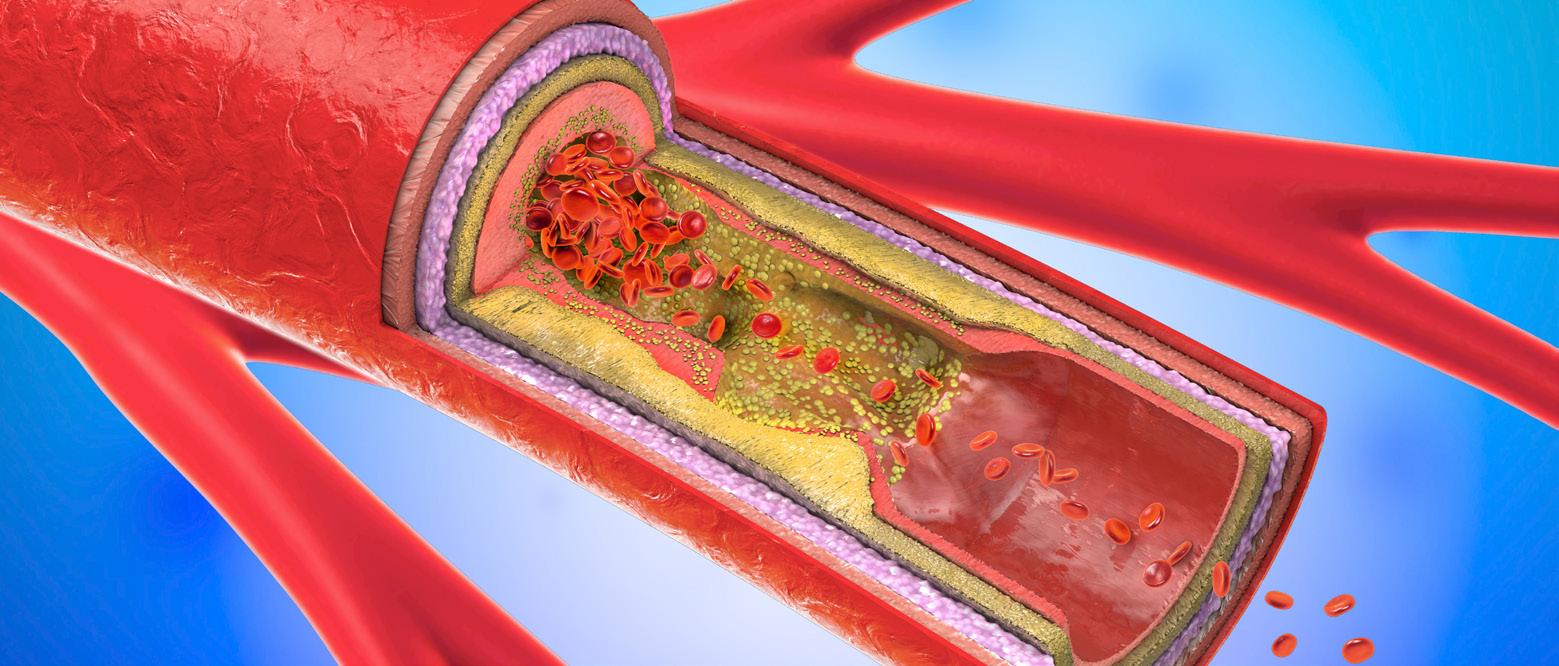
Cholesterol is transported in the body by lipoproteins. Lipoproteins are transport molecules that pick up, transport and drop off cholesterol wherever it is needed. Maintaining a healthy ratio of cholesterol is important in reducing the risk of cardiovascular disease.
There are many types of lipoprotein; however, the most important ones are:
• Low-density lipoproteins (LDL)
• High-density lipoproteins (HDL).
Lipoproteins transport many molecules and nutrients around the body, including:
• Cholesterol
• Fat-soluble vitamins (Vitamin A, D, E and K)
• Triglycerides.
This is an important role because without HDL transport, triglycerides can build up in the bloodstream, increasing the risk of atherosclerosis (hardening of the arteries). Without LDL transport, cholesterol would not get transported to tissues that need it.(31)
Lipoproteins are transport molecules made of protein and fat which carry fats (such as triglycerides) to and from the liver.(31)
The human body is composed of cells; each type of cell has an explicit structure and function and contains all the machinery needed to help the body function properly.
Cells have walls, called a ‘lipid bilayer’, which means that it has two (bi) rows (layer) of fats arranged so that they can keep certain molecules outside or inside the cell (see imagebelow).(32)
The bilayer is composed of a type of lipid called ’phospholipids’ made from saturated and unsaturated fats taken from the diet. The phospholipids are arranged into the cell membrane and form a ‘hydrophobic’ layer, meaning that the outer layer repels water.(32)
CELL STRUCTURE

This is important because it prevents unwanted molecules from penetrating the cell, giving the cell ‘selective permeability’ (control over what can enter).(31)
One type of dietary fat, called omega-3 polyunsaturated fat, is known to help with skin and hair growth. Eating too little may impact the body’s ability to produce healthy skin and hair. Especially as a deficiency in vitamin A, which relies on fat for absorption, can result in skin complaints.
Omega-3 fatty acids are also known to assist with the production of healthy nails by reducing inflammation in the nail bed, which promotes stronger nails.
While all dietary fats are encouraged as part of a varied and healthy diet, some fats are essential because the body cannot create them. These fats are identified as Essential Fatty Acids (EFAs), and will be explored in more detail further in this resource.
Dietary fat is extremely important for the development and healthy function of the brain.
Studies have shown that polyunsaturated fats help with the development of infants’ brains during pregnancy and can help improve:
• Intelligence
• Communication and social skills
• Reduce behavioural problems
• Reduce the risk of developmental delays
BRAIN FUNCTION AND BRAIN DEVELOPMENT
ASSIST IN PREVENTING BLOOD CLOTS
• Reduce the risk of autism and cerebral palsy.(31)
Dietary fats also help reduce ageing-related mental decline and Alzheimer’s disease in older adults, thanks to the anti-inflammatory properties of omega-3 fatty acids.(31)
The brain is composed of almost 60% fat and is the ‘fattiest’ organ in the body!(33) This is why nutrition coaches need to encourage clients to eat a diet that provides adequate sources of good fats and not strictly to limit them.
The polyunsaturated omega-3 fatty acids can help prevent unwanted blood clotting by preventing platelets (small particles of blood that form clots) from clumping together.(23)
Omega-6 fatty acids are known to promote blood clotting, so a nutrition coach needs to understand the best ratio of omega-6 to omega-3 fatty acids required in the diet to promote healthy blood clotting.(23)
REDUCE CARDIOVASCULAR DISEASE RISK
Some fats are known to be -healthy, meaning they can reduce the risk of cardiovascular disease (such as heart attacks, stroke and high blood pressure), when included as part of a healthy diet.
These fats are called polyunsaturated fats which include the omega-3 fat linolenic acid and the omega-6 fat linoleic acid.(23)

INFLAMMATION AND IMMUNE FUNCTION
Inflammation is considered to be a normal immune system response to something that might be harmful to the body, such as itchy and red skin because of a bee sting.
When the body detects something potentially harmful in the body, special white blood cells called ‘leukocytes’ rush to the location and attempt to neutralise the threat.(33)
The main immune responses are:(34)
• Heat
• Pain
• Redness
• Swelling
• Loss of function.
Low-level, ongoing inflammation has been proposed to be the cause of many diseases such as:(33)
• Diabetes
• Obesity
• Cardiovascular disease
• Arthritis
• Allergies (asthma, dust allergies).
Some fats, like mono and polyunsaturated fats, help produce prostaglandins (hormone-like substances) which help reduce inflammation. Conversely, some fats like omega6 fatty acids can increase inflammation when consumed in large quantities in the diet. It is important to learn about these fats, where they come from and the best ratio to consume them to prevent or reduce inflammation and promote a healthy body for clients.(33)
As explained above, inflammation is an immune response to a potential threat. In the case of an allergy, it is an overreaction by the immune system. In the case of arthritis, it is possible that a high intake of omega-6 fats may be the cause(33). By analysing a client’s dietary intake, it may be possible to identify the cause of ongoing inflammation and make recommendations to help reduce it.
Some hormones, called steroid hormones, are made from fats in the form of cholesterol.
Dietary fats are essential for the production of these hormones, and examples include:(23)
• Testosterone
THE PRODUCTION AND REGULATION OF SOME HORMONES
• Progesterone
• Cortisol
• Aldosterone
• Vitamin D.
‘Steroid hormones’ refer to sex hormones including testosterone and progesterone and corticosteroids (which work in the brain) including cortisol (stress hormone) and aldosterone (which regulates water balance).(23)

IMPROVES BLOOD VESSEL ELASTICITY
As individuals age, their blood vessels become stiffened, known as hardening of the arteries.
Long-term supplementation with polyunsaturated fats, like fish oil, has been shown to reduce the hardening of the arteries by reducing inflammation, blood clotting and blood vessel constriction (tightening).(23)
Intake of polyunsaturated fats has been linked with improvements in mental health in scientific studies. A dietary pattern like the Mediterranean Diet may help reduce unwanted symptoms of depression and anxiety.(35)
Researchers have proposed that people with depression may not have enough of the omega-3 fatty acids EPA and DHA (these are explained below). In some studies, it was shown that supplementation with omega-3 reduced depression symptoms in some participants.(35)
DECREASES THE RISK OF DEPRESSION AND ANXIETY
The mechanism by which omega-3 helps reduce depression is not currently understood. It could be due to anti-inflammatory effect in the brain or the effect Omega-3 has on serotonin (sometimes called the ‘happy chemical’) or the serotonin receptors in the brain.
It is important for nutrition coaches to remember that clients with depression and anxiety should be encouraged to speak to their GP for assessment and appropriate care.
A diet lacking a range of dietary fats can lead to poor health outcomes, including:(23)
• Vitamin deficiency
• Hormone imbalances
• Increased hunger
• Skin problems.

The classification of fat will depend on the structure of its chemical makeup. The nutrition coach needs to be able to identify fats, and their effects in the body and on overall health.
There are two ways in which fats can be classified:
1. By their degree of ‘saturation’: Saturated, Unsaturated, Trans fats.
2. By their ‘length’: Short Chain Triglycerides, Medium Chain Triglycerides, Long Chain Triglycerides.
FATTY ACIDS
Saturated fats from healthy sources, such as eggs, dairy and some meats, are natural fats and are encouraged to be consumed as part of a healthy diet. However, saturated fats from processed foods, such as pies and some meats, are not as healthy and should be limited in the diet.
Saturated fats are typically found in animal products, as well as some plant-based foods, such as:
• Animal fats (lard, tallow, ghee)
• Full cream dairy products (cream, yoghurt, cheese)
• Coconut products (coconut oil, coconut milk and cream).
Some examples of the less healthy, highly processed sources of saturated fats include:
• Processed foods (biscuits, cakes, pastries, pies, chips)
• Processed meats (sausages, salami)
• Fast food (hot dogs, burgers, pizza, fried food).
As a nutrition coach, it is important to promote healthy options for saturated fats because of the effect that they can have on cardiovascular health. Saturated fats, like those found in full cream dairy products (milk, cream, yoghurt), are composed of mainly short-chain fatty acids and appear to have a beneficial effect on gut health by feeding the gut bacteria.

Other saturated fats appear to promote HDL cholesterol which are known to be cardio (heart) protective in the correct ratio (to LDL cholesterol). However, the source of saturated fats is important; processed foods, fatty meats and fast food should be limited within the diet as they can promote an unhealthy ratio of HDL to LDL cholesterol. This is especially important because combining these saturated fats with refined and processed carbohydrates can negatively affect cholesterol levels.(31)
Saturated fat used to be classed as a ‘bad’ fat following the research findings from Dr Ancel Keys from his Seven Countries Study, released in the 1950s, which suggested that saturated fat intake increased the risk of heart disease.
Since this time, however, it has been found that this particular research had data from 22 countries (as opposed to the initially identified seven countries) and when all 22 countries are considered, it is very difficult to find an association between saturated fat intake and heart disease. There is strong evidence to support the claim that saturated fat, while not cardio (heart) protective, is not harmful to human health at intakes around 10% of total daily energy intake.(36)
Unsaturated fats are comprised of one or more double bonds in their biochemical structure and are liquid at room temperature. Unsaturated fats are well known to help reduce the buildup of cholesterol in the arteries, thus declining the risk of heart disease and stroke.(37)
Unsaturated fats can also be beneficial for:(38)
• Improving/reducing inflammation
• Improving the function of blood vessels
• Assisting in reducing triglycerides implicated in atherosclerosis (hardening of the arteries)
• Stabilising heart rhythms
• Building stronger cell membranes in the body
• Reducing blood pressure in those with hypertension
• Assisting those with type 2 diabetes
• Assisting in the maintenance of bodyweight.
For this reason, unsaturated fats have often been called the ‘good’ fats as they are beneficial in reducing the risk of disease. However, as previously mentioned, it is important to note that this does not make saturated fats ‘bad’ as they too have a role to play within the body, and often come packaged in nutrient-dense food sources such as meat and dairy.
As unsaturated fats have a double bond they are not as stable for cooking at higher temperatures when compared to saturated fats. When unsaturated fats are used for cooking at high temperatures their biochemical structure can change making it a harmful fat instead of a beneficial fat.
As unsaturated fats have a double bond they are not as stable for cooking at higher temperatures when compared to saturated fats. When unsaturated fats are used for cooking at high temperatures their biochemical structure can change making it a harmful fat instead of a beneficial fat.
There are two major types of unsaturated fat:
1. Monounsaturated
2. Polyunsaturated.

Monounsaturated fatty acids, commonly abbreviated as MUFAs, have one double bond in their biochemical structure. There are many types of MUFAs, the most common ones being oleic acid, palmitoleic acid and vaccenic acid.
Mono-unsaturated fats may have some benefits when included in the diet, such as:
• Reduction in cardiovascular disease risk (thanks to their effect on HDL/LDL cholesterol levels), and
• May help reduce inflammation (this effect was demonstrated in a study where saturated fat was replaced with monounsaturated fat).
Monounsaturated fats can be found in plant-based foods, as well as in meat and animal-based foods. The table below offers a list of food sources high in MUFAs, along with the amount found in (100 grams) of the food source:


Polyunsaturated fatty acids, commonly abbreviated to PUFAs, have two or more double bonds in their biochemical structure. Polyunsaturated fats are utilised as building blocks in the membranes that encompass all the body’s cells and contribute to the brain’s structure.(37)(40)
This fat is found mostly in plant-based foods and oils and marine foods such as oily fish. Evidence suggests that eating foods rich in polyunsaturated fatty acids can:(41)
• Improve blood cholesterol levels
• Decrease the risk of heart disease
• Decrease the risk of type 2 diabetes.
There are two different groups of polyunsaturated fats:
1. Omega-3 fatty acids (alpha-linolenic acid (ALA), EPA and DHA)
2. Omega-6 fatty acids (linoleic acid, and many others).
Both omega-3 and omega-6 fatty acids are classed as essential fatty acids as the body cannot create them naturally. (42) Therefore, these fats are required as part of a healthy, varied diet to maintain a healthy functioning body.
The two tables below outline the differences between omega-3 fatty acids and omega-6 fatty acids:
Omega-3 fatty acids are essential fatty acids that play a crucial role in:
• Brain health
• Vision
DESCRIPTION
FOOD SOURCES OF OMEGA-3 FATTY ACIDS
TYPES OF OMEGA-3 FATTY ACIDS
• Joint health
• Reducing inflammation
• Promoting heart health.
Omega-3 fatty acids can be found in:
• Oily fish (such as salmon and sardines)
• Walnuts
• Flaxseeds and sesame seeds
• Olive oil
• Garlic
• Avocados
• Whole egg
• Some dark green, leafy vegetables (spinach, kale, collards).
There are three types of omega-3 fatty acids:
1. Alpha-linolenic acid (ALA): Found mainly in plants
2. Eicosapentaenoic acid (EPA): Found mainly in animal products and algae
3. Docosahexaenoic acid (DHA): Found mainly in animal products and algae.
Alpha-linolenic acid (ALA):
While ALA may have beneficial effects in the body, it must first be converted into EPA or DHA before it can be used. Research shows that conversion only occurs in small amounts, making its use (especially as a supplement) not as effective as animal-derived EPA and DHA.
Eicosapentaenoic acid (EPA):
BENEFITS
EPA appears to provide benefits for brain health by reducing inflammation. It may also help with depression and anxiety, although the mechanism by which it works is not yet known. EPA may also help build muscle by being converted to ‘prostaglandins’ (hormone-like molecules) which play a role in:
• Maintaining testosterone levels
• Elevating growth hormone levels
• Increasing insulin sensitivity
• Increasing protein synthesis in muscle cells.
Docosahexaenoic acid:
Inadequate levels of DHA in older adults have shown to result in reduced brain size which is a sign of accelerated brain ageing. DHA is also a structural factor of the eye and may help slow macular degeneration.

DESCRIPTION
EXAMPLES
TYPES OF OMEGA-6 FATTY ACIDS
Omega-6 fatty acids are a type of polyunsaturated fat that has been found to be cardioprotective (heart healthy), thus decreasing the risk of heart disease. These fats, while essential in the diet, are often over-consumed in the Western diet. Overconsumption of omega-6 fatty acids can have an inflammatory effect on the human body.
Omega-6 fatty acids can be found in:
• Dairy (milk, cream, cheese, butter)
• Nuts and seeds (i.e. sunflower seeds, pistachio nuts)
• Olives and olive oil
• Evening primrose oil
• Eggs
• Vegetable oils (soybean, canola, sunflower)
• Commercially baked products
• Deep fried foods.
There are four types of omega-6 fatty acids:
1. Linoleic acid (LA)
2. Gamma-linoleic acid (GLA)
3. Dihomo-Gamma-linolenic acid (DGLA)
4. Arachidonic acid (AA).
Linoleic Acid (LA):
Linoleic Acid is an essential fatty acid that can not be produced in the body. Like EPA, LA is found in most human tissues and is used in the production of cell membranes and as a cell signaller, ‘prostaglandins’, which help with vessel dilation (opening) and prevent unwanted blood clotting.
Gamma Linolenic acid (GLA):
GLA is a non-essential fatty acid, as the body can produce it by breaking down linoleic acid. It appears to serve an anti-inflammatory role and is popular as a homeopathic supplement for use in treating arthritis, eczema, high blood pressure and others; however, there is little evidence to support its use.
BENEFITS

Dihomo-Gamma-linoleic Acid (DGLA):
DGLA may again show anti-inflammatory qualities.(46)
Arachidonic acid (AA):
AA is a conditionally-essential fatty acid (where an LA deficiency occurs) that forms part of cell membranes and acts as a cell signaller. AA is sourced from animal foods (such as meat, poultry and eggs) and may contribute to unwanted inflammation in high quantities.
While omega-6 fatty acids are necessary in the diet, overconsumption can cause inflammation, which may drive long term poor health conditions like Alzheimer’s disease and arthritis.(46)(47)(48) Supplementation with omega-6 is unnecessary.
Nutrition coaches must understand what trans fats are, where they come from, and the effect they have on health.
Trans fats are found in two sources:
• Naturally occurring in some animals (cows, sheep, goats and deer)
• Artificial through industrial processing
Although trans fats may be found in small quantities in the products derived from some animals, the largest source of trans fats (by far) in the Western diet is from processed oils and foods.
Trans fats are an unsaturated fat produced as a byproduct of the processing of unsaturated fats into another product, such as:
• Hydrogenated margarines
• Processed baked goods (cakes, biscuits)
• Processed cooked meat foods (pies, hot dogs, pizza)
• Foods deep fried in vegetable oils (hot chips, fish).
The term ‘byproduct’ refers to an incidental or secondary product made in the manufacture or synthesis of something else.(49)
Trans fat, although an unsaturated fat, can act more like a saturated fat. They became popular in the processed food industry during the twentieth century because of their favourable characteristics in food processing.
These characteristics include:
• Increase a product’s shelf-life
• Decrease product refrigeration requirements
• Less expensive than animal fats like butter and lard
• Less expensive than semi-solid vegetable oil like palm oil
• Provide a higher melting point than unsaturated fats (which is ideal for crisper biscuits and crunchier chips).
Trans fats are known to increase the amount of LDL cholesterol in the blood, which is a risk factor for heart disease. There is also evidence that trans fats may reduce levels of HDL cholesterol in the blood which is undesirable. Trans fats are not a natural source of dietary fat and are therefore not essential in the human diet, as such, the World Health Organization (WHO) recommends limiting energy intake from trans fats to less than 1% of total daily energy intake.(50)


Micronutrients refer to elements (vitamins and minerals) required in trace amounts (very small amounts) which enable the body to produce enzymes, hormones and other substances required for normal growth and development.(51) Even though micronutrients are only required in small amounts, a depletion of any micronutrient can have devastating effects on the functioning of the human body.
Nutrition coaches need to understand what micronutrients are, the many roles they play in the human body, how they affect an individual’s health when an inadequate amount is consumed (deficiency) or if they are consumed to excess, and how to adapt an individual’s diet to ensure adequate micronutrition on a day-to-day basis.
Vitamins and minerals are required in small amounts to assist with the thousands of chemical reactions occurring in the body continuously.
These chemical reactions are responsible for hundreds of roles within the body, including (but not limited to):(37)
• Improved immunity
• Bone strength and bone metabolism
• Blood clotting
• Nerve function
• Wound healing
• Metabolism of macronutrients
• Night vision
• Assists with constriction and relaxation of blood vessels
• pH regulation
• Regulates body fluid volume
• Normal function of all cells
• Glucose metabolism.
Vitamins and minerals can be obtained from a healthy, varied diet and consumption is required on a regular, daily basis to avoid deficiencies. Consuming a healthy and well-varied diet will allow a person to reach all vitamin and mineral requirements without supplementation.
Understanding the importance of micronutrients gives a nutrition coach the ability to assist individuals in ensuring an adequate intake of micronutrients on a day-to-day basis.

Vitamins are organic substances (meaning they contain carbon) made by plants or animals and are essential to sustain life. Vitamins are considered ‘essential’ because the body cannot make them, and they are therefore required to be consumed through dietary measures. While the body only needs small amounts of vitamins, a deficiency in any vitamin can have negative health impacts on the client.
There are a total of 13 different vitamins, which can be categorised into two different groups:
1. Fat-soluble vitamins (vitamin A, D, E and K)
2. Water-soluble vitamins (B vitamins and vitamin C).
When it comes to nutrition, a mineral is an inorganic substance (chemical element) required as an essential nutrient by the body to perform functions necessary for life. Minerals are found in the earth (soil) and cannot be synthesised by living organisms. In other words, the human body cannot make minerals; for a client to meet their daily requirements, minerals must be consumed through food.
Essential minerals are micronutrients that are required by the human body in small amounts regularly. There are two major categories of essential minerals: trace and major. Trace minerals are required by the human body in smaller amounts than major minerals, although both play fundamental roles in maintaining health.
Essential minerals are divided into two categories: 1. Major minerals (also known as macrominerals) 2. Trace minerals (also known as microminerals).


Water is an integral part of the human body, making up over two-thirds of body weight. Even a reduction of as little as 1-4% in body water can trigger signs of dehydration such as:(52)(53)
• Headaches
• Increased body temperature
• Decreased blood pressure
• Nausea
• Dizziness
• Excessive thirst
• Lethargy
• Deterioration in concentration/cognitive function.
Dehydration can often be confused with hunger, causing individuals to overeat.
Water plays many roles in the human body, including regulating temperature, eliminating waste, aiding in swallowing, lubricating cells and providing a medium in which most chemical reactions occur within the body.(52)
The amount of fluid required is personalised and depends on various factors such as age, weight, climate (e.g. hot and humid or cold and dry), work environment (e.g. labourer or desk worker) and additional physical activity levels. On average, individuals require approximately 2.1L for women and 2.6L for men per day.(54)
Estimated Fluid Requirements (EFR) = 2.1L for women and 2.6L for men.
This figure would increase for those living in hot and humid environments, those who are physically active throughout their day-to-day lives, and those who participate in regular exercise, where excess fluid may be lost through sweat. In comparison, fluid requirements may be lower for those individuals such as the sedentary or the elderly, who are less active and may consume more water-based foods like soups and stews.
Fluid can be sourced from the direct consumption of water and other caffeinated and non-caffeinated drinks (e.g. tea/coffee, natural juice, milk and soda water), and through the consumption of certain foods (e.g. fruits, vegetables, yoghurt and soups).

The term macronutrients refer to the grouping of protein, carbohydrates and fats. As the primary energy sources for the body, the breakdown and ratio of these three macronutrients can significantly impact weight management, general health and nutrition status.
Below is a table of macronutrient recommendations from the Australian Government:(55)
of total EER
of total EER
of total EER
EER = Estimated Energy Requirements
The table below provides ranges for macronutrient recommendations that are based on varying research and individual requirements.
EER = Estimated Energy Requirements
EMERGING RESEARCH FOR CARBOHYDRATE AND FAT RECOMMENDATIONS
It is the responsibility of the nutrition coach to stay up to date with the latest, high-quality research in order to make best practice decisions in regards to carbohydrate and general nutritional recommendations.
For further research on the recommended daily intake of carbohydrates CLICK HERE. For further research on the recommended daily intake of dietary fats CLICK HERE.


To analyse a client’s food intake, nutrition coaches must be able to identify the macronutrient composition of common foods. While prior knowledge and ongoing learning will be useful, some basic assessment tools can assist with the learning process and help make analysing foods quicker and easier.
A number of tools can be utilised to help with identifying the breakdown of common foods; these include:
• Ready Reckoners
• Mobile phone apps
• Websites and databases.
Over time, reliance on tools like these will reduce as the knowledge becomes embedded from ongoing day-to-day use.
The table below shows the six main food groups and the dominant macronutrient found in each. For instance, vegetables like broccoli, cauliflower and potatoes will be mainly composed of carbohydrates, as will grains such as rice, oats and wheat. On the other hand, dairy will be mainly composed of protein and fats, while meats like chicken, beef and fish will be mainly protein.
DAIRY
GRAINS
VEGETABLES
FRUIT
NUTS AND SEEDS Fat
Fat, carbohydrates, minerals, vitamins
fibre, minerals, vitamins
Fibre, protein, minerals, vitamins
Fibre, minerals, vitamins
Carbohydrates, fibre, vitamins, minerals, protein


A ready reckoner is a document that provides the approximate breakdown of protein, carbohydrate, fat and energy found in standard serves of common foods. These can be created by the nutrition coach or sourced from various organisations.
Once a client has provided their diet history, nutrition coaches can look at the serving sizes of various items provided by the client and match them to the ready reckoner to find the approximate amount of protein, carbohydrate, fats and energy found in their diet. This can save time compared to using an app or website to find the information; however, data will not be as accurate. Sometimes, clients may forget to include serving sizes for each item, and the nutrition coach will need to use estimated quantities in the ready reckoner.
EXAMPLE OF A READY RECKONER
CLICK HERE to view an example of a Ready Reckoner. (Adapted from Rowan Stewart et al. 2015. Toolkit for NCP/Handbook of clinical nutrition & dietetics).
As a nutrition coach, it can be very beneficial and time effective to incorporate apps in day-to-day practices. Many different databases can be used to enter specific foods and serving sizes to find highly accurate nutritional composition information.
The advantage of using an app is the range of data available, which would be impossible to fit into a simple Ready Reckoner. However, apps can be time-consuming and may not contain specific branded foods. The accuracy of the information in an app’s database may not be reliable since many rely on user reporting or are location specific (e.g. USA based).
Nutrition coaches are recommended to test various apps to see which they like the best (if any). It is also a good idea to check the accuracy of an entry against a food nutrition panel or manufacturer’s website.
Nutrition coaches are also encouraged to source reliable websites and databases to find relevant information. Many websites exist to provide nutritional information for thousands of food items. Much like apps, websites can be useful; however, they can also be time-consuming and location-specific.
Examples of reliable websites include:
• Food Nutrition Facts and Free Calorie Counter | CalorieKing (Australia)
• The Australian Food Composition Database (previously called NUTTAB)
• SELF Nutrition (USA).
• Nutritionix (USA).
Nutrition coaches can also pay to access databases like FoodWorks©, which can produce highly accurate nutritional information and is widely used by Australian health services.
In addition to the above, nutrition coaches can also use the following credible sources of information to find more health/nutrition-related information:
• National Health and Medical Research Council (NHMRC)
• World Health Organisation (WHO)
• Nutrient Reference Values (NRV)
• Food Standards Australia and New Zealand (FSANZ)


Once the pre-screening process has been conducted, the client has been cleared of potential risks, and all appropriate information has been gathered (through a food diary and initial consultation/questionnaires), it is time to begin analysing the client’s current nutritional information. Analysing and comparing a client’s current nutritional intake will give a nutrition coach the ability to make recommendations and/or design a tailored nutritional plan for the client safely and effectively.
There is a process to follow for a nutrition coach to plan a safe and effective nutritional plan for a client. Having a set process and a well laid out structure is the best practice to ensure that all bases and nutritional requirements are covered. This structure includes key elements that must be identified to design a nutritional plan. This can prove to be beneficial, as it ensures that the standards of nutrition coaches are met and upheld.
As a bare minimum, a nutrition coach will need to ensure that the below key elements are covered and included in the process of designing a nutritional plan for a client:
• Energy
• Macronutrients
• Micronutrients
• Fibre
• Fluid
• Discretionary items.
The main focus of this particular unit is to educate nutrition coaches on the best approach to take when designing tailored nutritional plans. However, it is beneficial to know that the approach itself can be changed or adapted to best suit the nutrition coach.
All elements listed above must be covered as a minimum requirement, regardless of the approach taken.


Below is an overview of the step-by-step guide as a brief reminder of the best way to approach the development of a nutritional plan. This resource will also explain this process in more detail further.
Conduct RSST and client questionnaire.
Identify the clients goals and possible barriers to reaching their goals.
This is where the client’s food intake and information gathered from step 1 is analysed.
Factors completed in this step include:
A. Analysing the client’s current intake for energy (EEI)
B. Analysing the client’s current intake of macronutrients
C. Analysing the client’s current intake of micronutrients
D. Analysing the client’s current intake of fibre
E. Analysing the client’s current intake of fluid
F. Analysing the client’s current intake of caffeine
G. Analysing the client’s current intake of alcohol
H. Analysing the client’s current intake of discretionary items.
This is where the client’s individual recommended nutritional requirements are calculated/ determined using the correct equations and industry norms/standards.
Factors completed in this step include:
A. Identifying a client’s estimated energy requirements (EER)
B. Identifying a client’s recommended macronutrients requirements
C. Identifying a client’s recommended micronutrients requirements
D. Identifying a client’s recommended requirements for fibre
E. Identifying a client’s recommended intake for fluid
F. Identifying a client’s recommended caffeine intake
G. Identifying a client’s recommended alcohol intake
H. Identifying a client’s recommended intake for discretionary items.
STEP 5
This is where a comparison is made between what the client is currently eating (step 2) and their individual recommended nutritional requirements (step 3) to identify gaps in their diet.
OPTION A: Create a custom meal plan for the client.
OPTION B: Make dietary adjustments/recommendations for the client if a nutrition plan is not suitable or required.

This step includes monitoring the client’s progress and recognising any area that may need to be modified based on the client’s feedback.

When developing a nutritional plan, it is beneficial to follow a process to ensure all aspects of the nutritional plan are addressed appropriately and effectively. Below is outlined in detail, what is addressed in each of the steps, explaining the full process for a nutrition coach when developing a nutritional plan.
Step 1 of designing an individual nutritional plan for a client requires the nutrition coach to identify a client’s health status, goals/preferences and current food intake.
This step was completed in the ‘HLTAAP002 - Confirm Physical Health Status’ unit. As a nutrition coach, this is an important stage that needs to be completed before developing a nutritional plan for an individual client.
This step is one of the most crucial aspects of the nutritional plan for the following reasons:
• It allows the nutrition coach to determine the client’s risk factor to deem them either within or outside of their scope of practice.
• It allows the nutrition coach to gather all information in the client questionnaire regarding their personal preferences, likes and dislikes.
• It assists the nutrition coach in determining the current activity levels of the client, which in turn allows for more accurate nutritional recommendations.
• It allows the nutrition coach to conduct a ‘food diary’ with the client to identify their current eating patterns and intake.
The resources are provided below to assist students in the consultation and information-gathering process:
• Risk-Stratification Screening Tool (RSST)
• Client Questionnaire (template)
• Client Questionnaire (example)



To support your clients best, clarifying and discussing health goals with them in more detail will allow for a smooth and confident planning process. Ensuring you are both on the same page in what they want to achieve at the end is crucial before moving on to the next step. Clients often give quite a simple response to start with. However, helping turn them into SMART, short, medium, and long-term goals will allow you to understand what they mean and the expected time frame in which they expect to achieve them. It is common for a client to have more than one goal, and it is also common for clients to state unrealistic goals; this is when a nutrition coach may need to come in and explain to the client why it is unrealistic and figure out a more realistic goal.
Common health goals clients have are:
• Lose weight
• Gain weight
• Gain muscle/ improve strength
• Maintain/improve the overall health
• Stay fit
• Prolong life
• Prevent developing chronic illnesses
• Role model for children/siblings/parents/friends
• Improve confidence
Identifying clients’ challenges are equally as important as their goals. These are factors contributing to their current eating habits. Nutritional plan/recommendations are entirely based on their current lifestyle and how to incorporate changes without disrupting their life. They are important to know, as you want to avoid misjudgements when making recommendations. For example, you wouldn’t recommend a full hot home-cooked breakfast every morning to a busy mum trying to get children ready and out the door for school. You want to identify the barriers they may be experiencing, find ways to combat them and work around them. You can’t change their job, lifestyle or family, but you can consider them when making changes.
Common challenges/barriers clients have are:
• Children
• Long/ obscure working hours (night shifts, FIFO)
• Lack of support around the house
• False/insufficient education on nutrition
• Bad habits
• Lack of energy
• Lack of confidence/willpower
• Their dislike of healthy food items, e.g. vegetables, fruit
• Lack of time
• Stress and anxiety
• Influence from support persons
• Cooking skills

When conducting an initial consultation and gaining information from a client, their current diet will always be the foundational block of any considered lifestyle change. Integrating a food diary into an initial consultation benefits the nutrition coach and the client. Completing a food diary allows a nutrition coach to identify, confirm and investigate their clients’ current nutrition status.
While a food diary is beneficial for the nutrition coach to assess and comprehend the client’s dietary intake, it can also prove to be motivational for the client as they record everything. The client may not recognise how much they are eating or what type of diet they are following until they begin recording this.
It may be common that clients will omit certain information from the food diary; however, they must be encouraged to complete an honest food diary. An honest food diary will provide the nutrition coach with an accurate understanding of what the client is consuming of which recommendations and education can be tailored to suit.
A food diary is a simple day-by-day document completed by the client over generally three to seven days prior to the initial consultation. The purpose of the food diary is to allow a more comprehensive understanding, review current dietary habits and identify patterns.
While Queensland Health provides a basic Food Diary template, most health professionals like to update the table to allow for a more detailed assessment. CLICK HERE to view the template.
A Food Diary should include the following information:
1. Type of food/drink (e.g. chicken breast, baby spinach, soda water)
2. Preparation methods (e.g. oven-baked, pan-fried, grilled)
3. The quantity of food/drink consumed (e.g. 100g, 1 cup, 200ml)
4. Time of consumption (e.g. 6am, 11.30am, 7.45pm)
Some optional extras which allow for an even more detailed data collection include:
• Environmental setting (e.g. home, work, friend’s house).

- The environment may impact what the client eats. For example, a client may eat a chicken salad while at home yet be tempted by a fast food outlet while out. Knowing what the environment encourages regarding intake can be beneficial as recommendations are tailored to suit individual situations.
• The client’s mood at the time of consumption (e.g. angry, sad, happy).
- This can be beneficial to help identify emotional eaters or particular mood triggers. For example, a sad person may be tempted to binge on chocolate or wine.
• Any exercise conducted including activity, time, intensity and duration (e.g. basketball game, 7.30 pm, mod-high intensity, 45 minutes).
- Knowing exercise information can help decipher if more nutrition is required prior, during or post-exercise times. If the client is completing the earlier Exercise Review Table, they do not need to complete it on the food diary as well.

Below is an example of a more detailed food diary that can be provided to clients to better understand the foods consumed daily.
CLICK HERE to download a copy of the food diary template.
When conducting this activity with clients, it is vital that a nutrition coach encourages the client to write as many details about their food intake as possible and remind them that too much information is better than too little. If the client is having a difficult time completing their food diary, advise them to get in contact for advice and assistance. Often clients may forget to include quantities in their food diary. This can make it difficult to assess how much of that food item they consume, however it is best to make a judgement call and estimate an average amount for that item. You can always reach out to the client if need be. It may be helpful to organise a face-to-face, phone or Skype meeting to discuss the details of the food diary for them to fully understand the expectations and instructions.
Provided below are additional tips that can help a nutrition coach in assisting clients in completing a food diary:
• Remind the client that you can help them best achieve their nutritional and health goals when they are as honest as possible with their food diary.
• Encourage the client to keep their food diary with them at all times so they can complete it throughout the day when they are eating. Having the diary easily accessible removes the stress of remembering what they have eaten and allows a more accurate description of the food consumed.
• Discuss the different ways the client can complete their food diary. While some prefer pen and paper, others may prefer entering it in their phone, putting it onto a spreadsheet or inputting their intake straight onto a food analysis app such as MyFitnessPal.
• If the client does not have their food diary with them when they are eating (as they may be at an event or have simply forgotten it), encourage them to take a photo of what they eat so they can accurately enter the information later in the day.
• Encourage the client to estimate amounts when they are unsure. Otherwise, look up measurements or read the food label. They could also take a photo to show you, however too many photos can become time-consuming to analyse in the consultation.
• Ensuring the client has a clear understanding of food measurements when completing their food diary will help to improve their accuracy and therefore, the result of their dietary analysis.

Once a client’s information and current eating patterns have been compiled from step 1, a nutrition coach can then begin to analyse the provided information. Doing so allows a nutrition coach to identify and analyse, as an overview, where the client is currently sitting regarding their daily nutritional intake.
As previously discussed, having a set process and a well-laid-out structure to follow is the best practice for a nutrition coach to design nutritional plans for a client effectively. This can prove to be beneficial, as it ensures that the standards of nutrition coaches are met and upheld. This structure includes key elements that must be identified to design a nutritional plan.
Factors completed in this step include:
A. Analysing the client’s current intake of energy (EEI)
B. Analysing the client’s current intake of macronutrients
C. Analysing the client’s current intake of micronutrients
D. Analysing the client’s current intake of fibre
E. Analysing the client’s current intake of fluid
F. Analysing the client’s current intake of caffeine
G. Analysing the client’s current intake of discretionary items
It is important to remember that calculations are an estimate and will not be 100% accurate. Attempting to achieve 100% accuracy would be impossible and can create an unhealthy relationship with food. A range either side of an energy or macronutrient estimate is acceptable (e.g. 500 kJ over or under their EER).


For a nutrition coach to identify (or analyse) the client’s current energy intake, the total amount of energy the client consumes over the day will need to be calculated. This is achieved by examining the client’s food diary and adding up the energy of all food and fluids sources to understand their current energy intake. An example of calculating a client’s energy intake for one meal is provided below and calculated using Calorie King Australia; this will then be repeated across all meals from the food diary in order to identify the client’s current energy intake.
It is common for clients to consume more energy than they require, and they may be unintentionally gaining weight or struggling with weight loss. On the other hand, clients can also consume less energy than they require, and they may struggle to put on muscle or unintentionally lose weight.
EXAMPLE
Breakfast
2 hard-boiled, whole eggs = 513kJ
2 middle rashers of bacon = 572kJ
1 cup spinach = 35kJ
7 cherry tomatoes = 88kJ
1 cup tea with 15ml full cream milk and no sugar = 52kJ
Total kJ = 1,260kJ
To analyse the client’s current protein intake, a nutrition coach will need to identify which foods contain protein in their current diet, achieved by examining the client’s food diary. Once these foods have been identified, a nutrition coach can calculate the amount of protein every food item yields. Following this, the sum of the quantity of protein in each meal is calculated to provide an approximate daily protein intake.
It is important to remember that 100g of food (e.g. 100g of chicken) does not equate to 100g of protein. There is 30g of protein in approximately 100g of cooked red meat, 100g of cooked chicken breast, 130g of fish, 5 large eggs or 1L of milk. Don’t forget about the small amounts of protein in other food items, too; for example, there is 5g of protein in 2 slices of multigrain bread and 2g of protein in one banana.
When calculating a client’s current protein intake, ensure the figure is written in grams. An example is provided below on how to calculate the sum of protein within one meal (the estimations have been rounded to the nearest whole number).
This will then be repeated across all meals from the food diary in order to identify the client’s current protein intake.
EXAMPLE
Snack
150g Greek yoghurt = 13g protein (average across different brands).
½ cup fresh blueberries= 1g protein.
8 almonds = 2g protein.
5 macadamias = 1.g protein.
15g chia seeds = 3g protein.
30g pumpkin seeds (pepitas) = 9g protein.
Estimated protein intake for this particular meal = 29g protein.

The same process outlined above for protein can be implemented to identify a client’s current carbohydrate intake. It is important that nutrition coaches are aware of the wide variety of carbohydrate-containing foods that could be present in a client’s food diary and whether they would be considered complex or simple sources. Further, educating clients on the difference between the two and how swapping to more complex, wholefood sources is beneficial for overall health.
The example below demonstrates how to calculate the total carbohydrate content of mixed meals over the course of one day (the estimations have been rounded to the nearest whole number).
EXAMPLE
Breakfast:
½ cup rolled oats (35g CHO), 1 cup full cream milk (16g CHO), 10 fresh raspberries (2g CHO), 1 tbsp pure Australian honey (21g CHO)
Morning tea: apple (10g CHO)
Lunch:
sandwich - slices of wholemeal bread (24g CHO), 1 tbsp mayonnaise (1g CHO), butter, ham, and cheese (all have negligible amounts of CHO)
Dinner:
curry - 1 cup Jasmine rice (42g CHO), 1 chicken breast (0g CHO), ¼ jar pre-made butter chicken sauce (10g CHO)
Dessert: Magnum Classic ice cream (21g CHO)
Total CHO = 182g carbohydrates
Lastly, identifying a client’s dietary fat intake. It can also be calculated in the same way as the two previous macronutrients.
Nutrition coaches must be aware of the wide variety of fat-containing food that could be present within a client’s food diary and the quality of those sources (for example, are they comprised of saturated and trans-fats or poly- and monounsaturated fats). Further educating clients on the difference between sources of fat and which are more beneficial for long-term health is encouraged.
The example below uses the same meals from the above example to demonstrate how different foods contain varying combinations of the three macronutrients. All quantities have been taken from Calorie King Australia (the estimations have been rounded to the nearest whole number).
EXAMPLE
Breakfast:
½ cup rolled oats (5g fat), 1 cup full cream milk (9g fat), 10 fresh raspberries, 1 tbsp pure Australian honey (both have negligible amounts of fat).
Morning tea: 1 x apple (0g fat)
Lunch:
Sandwich using 2 slices of wholemeal bread (2g fat), 1 tsp butter (4g fat ), 100g shaved deli leg ham (3g fat), 2 thin slices of cheddar cheese (14g fat), 1 tblsp mayonnaise (19g fat).
Dinner:
Curry with 1 cup of jasmine rice (3g fat), 1 lean chicken breast (6g fat), ¼ jar pre-made butter chicken sauce (approx. 8g fat).
Dessert: Magnum Classic ice-cream (17g fat).
TOTAL FAT INTAKE = 90g fat

To calculate an individual’s fruit intake, the nutrition coach will need to analyse the client’s diet in detail and identify the type and quantity of fruit consumed. The nutrition coach will need to identify how many serves of fruit the client is consuming.
1 serving of fruit is approximately 150g (350kJ) which is:(33)
• 1 medium piece of fruit such as an apple, banana, orange, mandarin, peach, grapefruit or pear
• 2 small fruits such as apricots, kiwi fruits, nectarines or plums
• 1 cup berries or diced fruit such as mango or pawpaw
• 1 ½ cups pineapple or watermelon
• 15-20 grapes
• 1 cup canned fruit (no added sugar)
• 30g dried fruit such as 4 dried apricot halves or 1 ½ tablespoon sultanas
• 3 ½ whole passionfruit.
1 MEDIUM PIECE 2 SMALL PIECES 1 CUP CHOPPEP OR CANNED FOOD
EXAMPLE
Fiona has 1 medium banana (1 serve) on her breakfast, eats 1 medium pink lady apple (1 serve) at morning tea and has a cup of strawberries (1 serve) with her yoghurt after dinner.
TOTAL FRUIT INTAKE = 3 serves for the day.
To calculate an individual’s vegetable intake, analyse the client’s current dietary information and calculate how many serves of vegetables are being consumed. Starchy vegetables, such as potato, sweet potato, corn and pumpkin, are higher in carbs and energy and lower in fibre. Because of this, it is best to keep starchy vegetable serves at a lower amount than other vegetables.
1 serve of vegetables is approximately 75g (100-350kJ) which is:(33)
• ½ cup cooked green or orange vegetables (for example, broccoli, carrots, green beans, capsicum, cauliflower, celery, snow peas, onion or zucchini )
• ½ cup cooked dried or canned beans, peas or lentils preferably with no added salt (for example, lima beans, kidney beans or chickpeas
• 1 cup green leafy or raw salad vegetables (for example, beetroot, bok-choy, choy sum, cabbage, lettuce or spinach)
• 1 medium tomato
• ½ medium avocado
• ½ cup tinned vegetables
• ½ cup corn
• ½ medium potato/ 1 small or other starchy vegetables (for example, sweet potato or pumpkin).

½ CUP COOKED VEGETABLES OR COOKED LEGUMES
½ CUP COOKED VEGETABLES OR COOKED LEGUMES 1 SMALL POTATO
An example is provided below:
EXAMPLE
John eats 2 cups of salad (2 serves) for lunch and has 1 cup of broccoli (2 serves), 1 small baked potato (1 serve) and 1 cup of green beans (2 serves) with his dinner.
TOTAL VEGETABLE INTAKE = 7 serves for the day.


To calculate the calcium (milk, yoghurt, cheese and/or their alternatives) intake, analyse the client’s current dietary information and calculate how many serves of calcium (milk, yoghurt, cheese and/or their alternatives) are being consumed. The nutrition coach will need to identify how many serves of calcium (milk, yoghurt, cheese and/or their alternatives) the client is consuming.(56)
One (1) serve of calcium (Milk, yoghurt, cheese and/or their alternatives) is 500-600kJ which is: (56)
• 1 cup (250ml) fresh, UHT long life, reconstituted powdered milk or buttermilk
• ½ cup (120ml) evaporated milk
• 2 slices (40g) or 4 x 3 x 2cm cube (40g) of hard cheese, such as cheddar
• ½ cup (120g) ricotta cheese
• ¾ cup (200g) yoghurt
• 1 cup (250ml) soy, rice or other cereal drink with at least 100mg of added calcium per 100ml.
*Choose mostly reduced fat
The following alternatives contain about the same amount of calcium as a serve of milk, yoghurt or cheese:
• 100g almonds with skin
• 60g sardines, canned in water
• ½ cup (100g) canned pink salmon with bones.
An example is provided below:
Isaiah drinks 1 cup of milk in the morning and has 1 tub of strawberry yoghurt mid-afternoon.
TOTAL = 2 serves for the day.


To analyse a client’s current fibre intake, a nutrition coach will analyse the client’s food diary and identify how many grams of fibre all the foods in their diet have. Food high in fibre are wholegrains, nuts, seeds, fruit, vegetables, beans, lentils and legumes. To calculate an individual’s current fibre intake, use Calorie King Australia and record how many fibre grams are in every food item. Once done, add each amount of fibre together to form a total amount.
The example below demonstrates how to calculate the total fibre content of mixed meals over one day (the estimations have been rounded to the nearest whole number).
EXAMPLE
Breakfast:
½ cup rolled oats (6g), 1 cup full cream milk (0g), 10 raspberries (1g), 1 tbsp honey (0g
Morning tea:
1 medium apple (3g).
Lunch: sandwich - 2 slices of wholemeal bread (4g), butter, ham, cheese, and mayonnaise (all have 0g).
Dinner: curry - 1 cup rice (2g), 1 chicken breast (0g), ¼ jar butter chicken sauce (2g).
Dessert: magnum ice-cream (0g).
TOTAL FIBRE= 18g fibre
If the client’s diet is largely unprocessed, they will often meet fibre recommendations. Fruit and vegetable intake and fibre intake usually go hand-in-hand. If the client is not meeting their vegetable and fruit intake, they most likely won’t be meeting their fibre intake. If the client is not meeting recommendations, it may be found that they struggle with health issues such as:(57)
• Energy crashes
• Uncontrolled sugar levels
• Irregular bowel motions
• Insatiable hunger.
To calculate the grain (cereal) foods, mostly wholegrain and/or high cereal fibre varieties intake, analyse the client’s current dietary information and calculate how many serves of grains are being consumed. The nutrition coach will need to identify how many serves of grain (cereal) foods, mostly wholegrain and/or high cereal fibre varieties the client is consuming.(58)
One (1) serve of grain (cereal) foods, mostly wholegrain and / or high cereal fibre varieties is 500kJ which is:(58)
• 1 slice (40g) bread
• ½ medium (40g) roll or flat bread
• ½ cup (75-120g) cooked rice, pasta, noodles, barley, buckwheat, semolina, polenta, bulgur or quinoa
• ½ cup (120g) cooked porridge
• ²/³ cup (30g) wheat cereal flakes
• ¼ cup (30g) muesli
• 3 (35g) crispbreads
• 1 (60g) crumpet
• 1 small (35g) English muffin or scone
*Grain (cereal) foods, mostly wholegrain and/or high cereal fibre varieties

EXAMPLE
Isaiah eats 1 cup of pasta with lunch and has 1 crumpet mid-afternoon.
TOTAL = 3 serves for the day.
To analyse a client’s current fluid intake, a nutrition coach can analyse the client’s dietary intake and calculate how much fluid has been consumed within the day. Be careful not to include highly caffeinated beverages (energy drinks) or alcohol in the fluid count. This means any water which is consumed directly or through indirect sources such as tea, coffee, juice, milk, soups, and smoothies can be counted. Milk is approximately 87% water, which must be considered when calculating fluid intake.(59) It is important to consider their fluid intake as a whole, as most of their intake should be coming straight from water.
EXAMPLE
Breakfast:
Coffee (200ml milk), cereal w/milk (approx. 150ml)
Morning Tea:
Orange juice (200ml).
Lunch:
A glass of water (approx. 250ml).
Afternoon tea:
Coffee (200ml milk)
Dinner:
A glass of water (approx. 250ml) and a glass of red wine (150ml).
TOTAL FLUID INTAKE =1,250mL (remember alcohol isn’t included in the fluid count)
To analyse a client’s current intake of caffeine, a nutrition coach can analyse the client’s dietary intake and identify the amount of caffeine they are currently consuming using the below guide:
espresso shot
tsp instant coffee
energy drink can
tsp matcha
cup black tea
cola drink
cup green tea
EXAMPLE
Breakfast: 1 medium latte (2 espresso shots) = 290mg
Morning tea: 1 cup of instant coffee (2 tsp instant coffee) = 160mg
Afternoon tea: 1 cup of green tea = 28mg
TOTAL = 3 serves for the day.

A nutrition coach must identify how many standard drinks the client consumes over the week. It is important to understand how many standard drinks, as opposed to the volume, as there may be more than one standard drink per glass consumed.
Below is a table adapted from an Australian Government website(60) showing how many standard drinks are in one typical serving of alcohol. It is encouraged that nutrition coaches take some time to form an understanding of what one standard drink looks like and use this as a reference when analysing the client’s intake.

To analyse a client’s current intake of discretionary items, a nutrition coach can analyse the client’s dietary intake and identify the frequency and type of junk food consumed. Discretionary items should only be consumed sometimes and in a small amount.
The table below provides examples of discretionary food and drink items:(61)
Energy drinks
Fruit juice
Sweeteners - maple syrup, honey, agave syrup, coconut sugar
Jams, marmalades
Most condiments (tomato sauce, BBQ sauce)
Soft drinks
Confectionary
Processed meats
Chips
Corn chips and corn products - tacos, nachos, enchiladas
Commercial pies
Commercial pizzas
Some sauces/ dressings
Deep-fried items
Biscuit
Cake
Chocolate
Doughnuts
Ice cream
Muesli Bars
Muffins
Beer
Liqueur
Wine
Port
Sherry
Spirits
Mixed alcohol drinks
The World Health Organisation (WHO) has recommended for all adults and children to keep their added sugars down to less than 10% of their total energy intake, and remind clients that reducing it down further to 5% per day would provide additional health benefits. The American Heart Association (AHA) provide a quantitative figure instead, recommending that females do not consume more than six teaspoons of added sugar per day, and men no more than nine teaspoons of added sugar per day.
AUSTRALIAN DIETARY GUIDELINES
WORLD HEALTH ORGANISATION
AMERICAN HEART ASSOCIATION
Consume less of these foods in much smaller quantities.
<10% of daily energy to come from added sugars.
<5% of daily energy coming from added sugars has additional health benefits.
Consume less of these foods in much smaller quantities.
<10% of daily energy to come from added sugars.
<5% of daily energy coming from added sugars has additional health benefits.
<9 tsp (36g) of added sugar per day. <6 tsp (24g) of added sugar per day.


One serve of discretionary food or drink is the equivalent of approximately 600kJ.(61) The below table identifies what 1 serve of a discretionary item looks like and how many grams of sugar it contains:
1 can (375ml) soft drink
1 tbsp Jam/honey
2-3 sweet Biscuits
2 scoops of regular Ice cream
1 Doughnut
1 Muffin/ small slice of cake
¼ cup condensed milk
50-60g (about 2 slices) processed meats, salami, mettwurst
2 thin higher fat/salt sausages
30g salty crackers
5-6 small lollies
½ small chocolate bar
2 tbsp cream
1 tbsp butter/margarine
60g fried hot chips


Identifying an individual’s recommended nutritional requirements is pivotal in providing appropriate energy support and dietary recommendations. This means that the nutrition coach will identify what the client should include in their diet according to industry standards and based on the client’s needs/preferences.
To identify a client’s recommended nutritional intake, a nutrition coach must be able to identify the following factors:
A. Identifying a client’s estimated energy requirements (EER)
B. Identifying a client’s recommended macronutrient requirements
C. Identifying a client’s recommended micronutrient requirements
D. Identifying a client’s recommended fibre requirements
E. Identifying a client’s recommended fluid intake
F. Identifying a client’s recommended caffeine intake
G. Identifying a client’s recommended intake for discretionary items.
All individuals have different nutritional requirements, and it is therefore important that all non-diet-related factors such as age, weight, gender, health status and activity levels are considered for calculations.
While many equations are used to estimate energy requirements, the Harris-Benedict equation is the most commonly used in clinical practice despite the limitations of accuracy in individuals who are above or below a normal or healthy weight.(62)
The Harris-Benedict equation estimates an individual’s Basal Metabolic Rate (BMR) and Estimated Energy Requirements (EER) in a two-step process. The equation will estimate how many kilojoules should be included in the client’s diet.
However, it is extremely unrealistic to meet the exact number everyday; therefore, consuming as close to the EER as possible is ideal, within 500kJ on either side of the EER is usually appropriate.
The first step is an equation used to calculate the BMR. There are different equations to determine the BMR for men and women, based on the assumption that men have a higher percentage of lean bodyweight than women (which increases BMR in men).(15)
Men: 278 + (57.5 x W) + (20.93 x H) - (28.35 x A) kJ/day
Women: 2741 + (40 x W) + (7.74 x H) - (19.56 x A) kJ/day
W = Weight in kilograms (kg), H = Height in centimetres (cm), A = Age in years
The second step is simply multiplying the BMR by the physical activity level (PAL), to establish the final EER.
Simply multiply the individual’s BMR with their corresponding PAL using the table below. A working example is provided on the following page.
TOTAL FLUID INTAKE =1,250mL (remember alcohol isn’t included in the fluid count)

At rest, exclusively sedentary or lying (chair-bound or bed-bound).
Exclusively sedentary activity/seated work with little or no strenuous leisure activity.
Sedentary activity/seated work with some requirement for occasional walking and standing but little or no strenuous leisure activity.
- 1.9
Predominantly standing or walking work.
Heavy occupational work or highly active leisure
Office employees, precision mechanics.
Laboratory assistants, drivers, students, assembly line workers, homemaker/ stay-at-home parent.
Domestic duties, salespersons, waiters, mechanics, traders. HEAVY TO VIGOROUS ACTIVITY 2.0 - 2.4
Your occupation with additional strenuous exercise.
Construction workers, farmers, forest workers, miners, high performance athletes
If your activity level for work/occupation fits into level 1.4-1.9 and you exercise strenuously (30-60mins, 4-5 times a week), change your selection to the next highest level of activity. For example, James is a waiter and has a PAL of 1.8, but he goes to the gym 4 times a week for 30mins, this means he would fall into the next highest category of heavy activity, with a PAL of 2.0. If a client does not participate in regular exercise, they will stay at the level according to their occupation.
A 62-year-old male who is 170cm tall and weighs 82kg, works behind a desk all week and enjoys working at a ‘moderate-intensity’ at the gym 4-5 times per week would have an EER of:
STEP 1:
W = 82kg
H = 170cm
A = 62
BMR = 278 + (57.5 x weight) + (20.93 x height) - (28.35 x age) kJ/day
BMR = 278 + (57.5 x 82) + (20.93 x 170) – (28.35 x 62) kJ/day
BMR = 278 + (4,715) + (3,558.1) – (1,757.7) kJ/day
BMR = 8,551.1 – 1,757.7 kJ/day
BMR = 6,793.4 kJ/day
STEP 2:
PAL = 1.6
EER = BMR x PAL
EER = 6,793.4 x 1.6
EER = 10,869.44 kJ/day

In order to lose or gain weight, a client has the option to increase physical activity, decrease energy intake or use a combination of the two. When calculating EER, because activity factors have already been considered, EER will be for weight maintenance given the projected activity factors. Therefore, if weight loss or gain is desired, increasing or decreasing the individual’s energy intake is wise.
It is important to know how to calculate EER for people who may want to lose or gain weight. It is advisable to encourage slow weight loss or weight gain, with approximately 0.5-1kg change per week(23). Weight loss of more than this may be unsustainable longer term as it involves a larger energy deficit, which in itself may be unsustainable (e.g. client may become hungry, light-headed, dizzy, faint, experience reduced cognitive function or reduced ability to concentrate on the task at hand). Ultimately, the size of a deficit and the client’s success with that deficit will depend on their motivation and ability to adhere.
For example, If a client initially consumes over their calculated EER, it is recommended to have them drop back to their EER before implementing a deficit. Their EER is already a decrease in kilojoules from what they were initially consuming. Clients will struggle to adhere to such a large deficit early on. Jumping to large deficits can cause extreme hunger and binge eating, resulting in straying from the plan. It is recommended to start small and increase from there.
It is also important to note that clients may lose more weight initially, then plateau a little. Therefore, it is crucial to remember that the EER will need to be re-calculated continuously as the individual’s weight changes, affecting their continued weight loss.
As muscle weighs more than fat, it is important to remember that weight on the scales can increase if a person is exercising and incorporating resistance training as they are putting on muscle. Therefore, relying on the scales as a means of measuring progress might demotivate the client.
To lose or gain approximately 500g of weight per week, approximately 2,000kJ needs to be subtracted (weight loss) or added (weight gain) to the client’s calculated daily EER to provide an adjusted daily EER(23). This adjusted daily EER will then be used to create meal plans for the client.
Using an example of a 62-year-old male who has a calculated daily EER of 10,232kJ per day: if he wanted to decrease weight by approximately 500g per week, the nutrition coach would simply subtract 2,000kJ from his calculated daily EER to provide an adjusted daily EER, which would be used for meal planning. Alternatively, if he wanted to increase weight by 500g per week, the nutrition coach would add 2,000kJ to his calculated daily EER to provide an adjusted daily EER, which would be used for meal planning.
10,232kJ - 2,000kJ = 8,232kJ
Therefore, this male would need to drop his EER to 8,232kJ per day for weight loss of approx. 500g per week.
10,232KJ + 2,000KJ = 12, 232KJ
Therefore, this male would need to increase his EER to 12, 232kJ per day for weight gain of approx. 500g per week.
To lose or gain approximately 1kg of weight per week, approximately 4,000kJ needs to be subtracted (weight loss) or added (weight gain) to the client’s calculated daily EER to provide an adjusted daily EER(23). This adjusted daily EER will then be used to create meal plans for the client.

The symbol ‘~’ means: approximately.
Using an example of a 62-year-old male, who has an EER of 10,232kJ per day: if he wanted to decrease weight by approximately 1kg per week, the nutrition coach would simply subtract approximately 4,000kJ from his calculated daily EER to provide an adjusted daily EER which would be used for meal planning, and if he wanted to increase weight by approximately 1kg per week the nutrition coach would add approximately 4,000kJto his calculated daily EER to provide an adjusted daily EER which would be used for meal planning.
10,232kJ - 4,000kJ = 6,232kJ
Therefore, this male would need to drop his EER to 6,232kJper day for weight loss of ~1kg per week.
10,232KJ + 4,000KJ = 14,232KJ
Therefore, this male would need to increase his EER to 14,232per day for weight gain of ~1kg per week.
As a nutrition coach, it is essential to identify how much of each macronutrient the client requires to assist them in reaching their nutritional requirements and health goals. Once macronutrient requirements are calculated, they can be compared to the client’s current intake to identify where dietary changes are required.
Most health organisations recommend a protein intake of ~0.8-1.0g per kg of body weight per day; however, this recommendation can increase depending on physical activity levels, disease states, goals, trauma and stress levels.
It is important to remember that even sedentary individuals require moderate amounts of protein (at the lower end of the range) to maintain their muscle stores and health. Older adults also require protein in the higher range to reduce the effect of ageing-related muscle decline, known as Sarcopenia.
As a nutrition coach, the most influential factor to consider when calculating an EPR for a client is how much exercise they are doing per week. The table below helps identify protein requirements for various amounts of exercise a client undertakes.
EPR is always presented in a range, not one singular number, as it is unrealistic to recommend an exact amount to hit daily. Consuming within a range of grams is more realistic and achievable. 20g under or over the calculated range is also acceptable, considering there are small amounts of protein in many food items.
Protein requirements increase as activity levels increase. This is to aid in muscle maintenance, recovery and synthesis. It can sometimes be difficult to decide what exercise level they fall in. Therefore, recommending to consume towards the lower or higher end of their calculated EPR is an easier way to ensure they are consuming appropriate amounts of protein for the amount of exercise they are engaging in.

SEDENTARY
(Sedentary job, nil physical activity)
MODERATE-INTENSITY
0.8-1.0g per kg body weight per day.
(One to three days moderate-intensity activity per week) 1.0-1.5g per kg body weight per day.
HIGH-INTENSITY
(Four days or more high-intensity activity per week) 1.5-2.0g per kg body weight per day.
A 90kg male who exercises at a high-intensity >4 times per week would require 1.5-2.0g of protein per kg per day.
1.5 x 90 = 135g
2.0 x 90 = 180g
Therefore, this male would require 135-180g of protein per day.
A sedentary 52kg female would require 0.8-1.0g of protein per kg per day.
0.8 x 52 = 42g
1.0 x 52 = 52g
Therefore, this female would require 42-52g of protein per day.
The Australian Government guidelines recommend carbohydrate intake to be ~45-65% of total daily energy intake(66) with the focus primarily on low GI carbs. It is important to keep in mind the type of client you’re working with, what their goals are, and their need for carbohydrates when determining where in this range they will sit.
Based on current research and guidelines, Nutritional Advisors can advise their clients’ daily carbohydrate intake to be anywhere between approximately 20-60% of total daily energy intake, depending on their goals or preferences. Where a client’s carbohydrate intake is at the lower end of the range, the Nutritional Advisor must ensure that clients are consuming sufficient fats for adequate energy intake.
It is the responsibility of the nutrition coach to stay up to date with the latest, high-quality research to make best practice decisions regarding carbohydrate and general nutritional recommendations.
Carbohydrate recommendations depend on a variety of factors including:
• Age
• Metabolic demands
• Disease state (e.g. diabetes)
• Medications (e.g. insulin)
• Physical activity levels (including intensity, duration and frequency).
For example, a client completing high-intensity physical activity daily is likely to require a higher ratio of carbohydrates than an elderly, sedentary client.

It is also important to space the consumption of carbohydrates out over the day. As carbohydrates are broken down into their most simple form of sugar (glucose), having a large intake all at once will cause an influx of glucose to enter the bloodstream. This can result in an energy high; however, as sugar is absorbed from the bloodstream into the cells, this can cause an energy crash where the client may struggle with fatigue, lethargy, mood changes and slowed cognition.
EXAMPLE
A 60kg female who is consuming 10,845kJ a day would require between 45-65% of carbohydrates. 10,845 x 0.45-0.65 = 4,990kJ- 7,049kJ ÷ 17kJ (1g carbs = 17kJ) = 294g- 414g carbs per day
Carbohydrate spacing (also known as ‘timing’) also needs to be considered for athletes; this will be covered in more detail in the sport nutrition coachspecialisation stream (NAT11046008 Design a diet to assist clients in achieving exercise related goals).
For further research on the recommended daily intake of carbohydrates CLICK HERE
The National Health and Medical Research Council (NHMRC) recommends that total fat intake is 20-35% of total daily energy intake, depending on age and physical activity. It further recommends that fats come predominantly from mono and polyunsaturated food sources.(67)
A broad dietary fat recommendation of between 20-60% may be advisable to allow for variation between client preferences and goals. This will enable the Nutritional Advisor to provide a wider range of intakes for clients who choose to restrict their carbohydrate intake, for example, while still meeting their energy requirements.
It is the responsibility of the nutrition coach to stay up to date with the latest, high-quality research to make best practice decisions regarding dietary fats and general nutritional recommendations.
Dietary fat intake is essential for a healthy body. The amount of dietary fat a person consumes in their diet should be based on their energy requirements.
EXAMPLE
A 85kg male who is consuming 12,045kJ would require between 20-35% of fats per day. 12,045 x 0.20-0.35 = 2,409kJ-4,216kJ / 38kJ (1g fats = 38kJ) = 63g-111g fats per day

The table below provides the recommendations for fat intake for each type of fat.(66)
UNSATURATED FAT
- Polyunsaturated omega-3
- Polyunsaturated omega-6
- Monounsaturated
SATURATED FAT
TRANS FATS
250-1g per day
4-10% total energy
15-20% of total energy
<10% of total energy intake
<1% of total energy intake
The table below indicates a breakdown of the recommended daily intake for polyunsaturated, monounsaturated and saturated fats:
The Australian Heart Foundation recommended intake of omega-3 and omega-6 fatty acids is based on population studies by the NHMRC and WHO. Population research demonstrates that dietary intake of omega-6 is very high in Western nations and that this was not the case before the introduction of vegetable oils in the twentieth century.
POLYUNSATURATED FATS
MONOUNSATURATED FATS
Many sources recommend consuming a ratio between 4:1 to 1:1 of omega-6 to omega-3. In practice, this means aiming to increase omega-3 sources of food by consuming 2-3 servings of oily fish (like salmon) each week, or supplementing with fish oil if necessary.(41) Further, reducing omega-6 intake can be achieved by reducing intake of confectionary and convenience foods, processed meats and fast food/ takeaway food.
No specific recommendation for the amount of daily energy from monounsaturated fats exists in Australia. The American Dietary Guidelines (2015-2020) recommend that 50-65% of daily energy from fat comes from monounsaturated fat sources. (69) This does not mean that 50-65% of a person’s daily energy should come from monounsaturated fat, but that if someone were to eat 30% of their daily energy needs from fat, then 15-20% of their total energy should come from monounsaturated fats.
The current recommended intake of saturated fats stands at around 10% of total daily energy requirements.(66) Although this is still an area of ongoing research, population studies continue to demonstrate that this intake level reduces the risk of cardiovascular disease.(36)
Increasingly it is recommended that a person’s total energy from fats should come from MUFA and PUFA sources as part of a plant-based diet, such as the Mediterranean diet.(70)
It is the responsibility of the nutrition coach to stay up to date with the latest, high-quality research to make best practice decisions regarding dietary fats and general nutritional recommendations.
(Four days or more highintensity activity per week)
For further research on the recommended daily intake of dietary fats, CLICK HERE.

As a nutrition coach, it is essential to ensure adequate micronutrition for all clients. Micronutrient deficiencies can significantly impact the client’s overall health and wellbeing and their ability to reach their health-related goals.
While several different vitamins and minerals make up the micronutrients, micronutrient adequacy can be estimated relatively easily. This is done by identifying the amount and variety of fruit and vegetables in the client’s diet. Fruit and vegetables are rich sources of various vitamins and minerals. Therefore, a diet rich in variety and meets/exceeds minimum recommendations (especially for vegetables) is likely to reach minimum micronutrient recommendations.
A diet that may reach minimum requirements of fruit and vegetables but also lacks variety can decrease the likelihood of the client reaching their minimum micronutrient requirements. Each fruit and vegetable have a different micronutrient profile, so it is essential to encourage a wide variety to ensure nutritional adequacy. A good way to do this is ensuring there are a variety of different coloured fruits and vegetables in the diet.
The Australian Dietary Guidelines recommend consuming 2 serves of fruit a day. It is recommended to include various coloured fruits in your diet, especially orange, red and yellow, as these fruits are high in vitamin A and assist with immune function.(71)
As a nutrition coach, it is important to encourage clients to increase fruit intake. However, some clients will consume very little to no fruit in their diet. Initially, it is unlikely these clients will instantly be able to commit to consuming 2 serves of fruit a day. To increase client adherence, recommend approximately 1 serve of fruit in their diet. Once this becomes a regular process, their fruit intake can increase further until they meet their 2 serves a day.
Trying to consume as close to the recommendations as possible is ideal, as they are there for a reason. If clients are consuming slightly over the recommended amount of 2 serves per day, this is okay. However, consuming fruit in a large excess of the recommendations is not advised.
Fruit comprises predominantly carbohydrates, with one serving of fruit provides the body with roughly 5-22g of carbohydrates. Fruit also contains a high amount of vitamins, minerals, and phytochemicals essential to the diet. Most fruits are a particularly good source of vitamin C, vitamin E, folate, potassium and magnesium, which can help reduce the risk of some chronic diseases.(71)
Dried fruit should not be consumed regularly due to their high amount of kilojoules and sugar. This can increase the likeliness of tooth decay. It is encouraged to consume fruit in its most natural and whole form, including the fibrous components which increase satiety.
Fruit juices can be high in kilojoules, low in fibre, and sometimes contain excessive amounts of sugar as well. As learned earlier in this unit, fibre will also help slow the release of sugar in the body. For example, consuming an apple with the skin is a better option than consuming apple juice.

The Australian Dietary Guidelines recommend adults to consume a minimum of 5 serves of a variety of vegetables and legumes per day.(67) In Australia in 2014-2015, 93% of Australians DID NOT meet this minimum requirement, meaning only 7% of individuals consumed adequate vegetable intake. Vegetables and legumes are high in fibre, phytochemicals, vitamins and minerals, making them indispensable in any diet.
As a nutrition coach, it is important to encourage clients to increase their vegetables intake. However, some clients will consume very little to no vegetables in their diet and initially is unlikely they will instantly be able to commit to consuming 5 serves of vegetables a day. In order to increase client adherence, suggesting that clients just increase their vegetable intake above what they are currently consuming will still be an improvement in their diet. Once this becomes a regular process, their vegetables recommendation can be increased further until they meet their 5 serves a day.
If clients are consuming slightly over the recommended amount of 5 serves per day, this is okay. However, trying to consume as close to the recommendations as possible is ideal.
1 serve of vegetables is approximately 75g (100-350kJ) which is:(72)
• ½ cup cooked green or orange vegetables (for example, broccoli, , carrots, green beans, capsicum, cauliflower, celery, snow peas, onion or zucchini )
• ½ cup cooked dried or canned beans, peas or lentils preferably with no added salt (for example, lima beans, kidney beans or chickpeas
• 1 cup green leafy or raw salad vegetables (for example, beetroot, bok-choy, choy sum, cabbage, lettuce or spinach)
• 1 medium tomato
• ½ medium avocado
• ½ cup tinned vegetables
• ½ cup corn
• ½ medium potato/ 1 small or other starchy vegetables (for example, sweet potato or pumpkin).
CUP COOKED
Including various vegetables with various colours in your diet will provide you with a vast range of health-promoting benefits, as different vegetables help protect our bodies in different ways.
For example:
• Green vegetables, capsicum and tomatoes are particularly high in vitamin C and support your body’s immunity.
• Beetroot, cauliflower and beans are a great source of folate to promote healthy cell growth and function.
• Vegetables are also high in fibre, which is believed to have compounds that protect against some cancer (73)
Vegetables are broken down into starchy and non-starchy vegetables. Starchy is a complex carbohydrate high in vegetables like potatoes, sweet potato, corn and pumpkin. Starchy vegetables should only make up a part of your vegetable intake as they are much higher in kilojoules when compared to other vegetables(73). Due to this, it is essential to include a variety of vegetables in your diet and keep starchy vegetables at a smaller amount to non-starchy vegetables.
Keep in mind if potatoes are in the form of hot chips or crisps, they are considered discretionary items due to their added fat and salt and are not included in vegetable intake.

The Australian Dietary Guidelines recommend adults a reach a minimum of 2-3 calcium (milk, yoghurt, cheese and/or their alternatives) serves daily, however, the minimum recommended will vary.(56)
Age, sex and life stage can vary the minimum requirements for an individual. For example, women 51+ years need 3-4 calcium (milk, yoghurt, cheese and/or their alternatives) serves a daily for calcium balance and bone maintenance.(56)
Dairy products such as milk, cheese and yoghurt provide easily absorbed types of calcium. “They also have various health benefits and are a good source of many nutrients, including calcium, protein, iodine, vitamin A, vitamin D, riboflavin, vitamin B12 and zinc.” Individuals may require or prefer a dairy-free meal plan due to diagnosed food sensitivities (such as lactose). However, the avoidance of calcium rich foods can be detrimental to an individual’s health long term.(56)
Dietary fibre relates to the edible parts of plants such as vegetables, fruits, beans and legumes, which are resistant to digestion and absorption in the small intestine, usually with partial or complete fermentation in the large intestine.
Dietary fibre includes the non-digestible part of polysaccharides (4-9 monosaccharides in length), oligosaccharides (>9 monosaccharides in length) and lignans (structural material in plant matter).(37) It is beneficial for satiety, laxation, decreasing blood cholesterol levels and modulation of blood glucose levels (dietary fibre slows the release of glucose into the bloodstream.(74)
The Adequate Intake (AI) of fibre for adult men is 30g per day and 25g per day for adult women, as set by the Australian Government.(75)
When advising clients to increase their fibre intake, there are two important considerations to also include:
1. With increased fibre intake comes the necessity for increased water intake. As discussed, soluble fibre in particular, absorbs water into the stool. If water intake is not increased in conjunction with fibre intake, this can lead to, or exacerbate, the occurrence of constipation.
2. With increased fibre intake comes the likelihood of increased flatulence - temporarily. Gas production in the large intestine and colon is necessary for gut bacteria to do their job and comes about as a result of the fermentation process. If flatulence persists long-term, becomes excessive, or causes any abdominal pain, that is when a nutrition coach will need to refer the client to a GP for a medical clearance.
Inadequate fibre intake can be identified in various ways, as outlined below:
• Feeling hungry soon: After eating fibre works to fill a client up and to keep them feeling fuller for longer (satiety). If a client is constantly hungry after meals, they need to increase their fibre intake to improve their satiety.
• Irregular bowel motions: If the client has irregular bowel motions, whether it be constipation or more towards diarrhoea, both can indicate inadequate fibre intake. When it comes to bowel motions, it is important to identify what type of fibre the client may be lacking, insoluble or soluble fibre.
• Lots of energy post-meal followed by a crash: This identifies the client is initially on a sugar high following the meal as there is inadequate fibre to slow the rate of sugar rushing into the bloodstream, which is then followed by a crash in energy. This sort of effect can be stabilised through adequate fibre intake and ensuring fibre is consumed with every meal.

The AI is set at the median for dietary fibre intake in Australia and New Zealand, based on the 1995 National Nutrition Survey of Australia and the 1997 National Nutrition Survey of New Zealand.
The value within each gender was set for all ages at the highest median of any of the age groups plus an allowance of slightly more than 4 g/day for men and slightly less than 3 g/day for women for the component of resistance starch (RS) not included in the food database for dietary fibre used for these surveys and rounding.
(Four days or more high-intensity activity per week)
The Australian Dietary Guidelines recommend adults a reach a minimum 4-6 grain (cereal) foods, mostly wholegrain and/or high cereal fibre varieties serves daily, however, the minimum recommended will vary.(58)
Age, sex and individual energy needs can vary the minimum requirements for an individual. For example, physically activity adults may require more grains when compared to sendentary adults due to their differing energy demands.(58)
Grain foods can minimise the risk of developing conditions such as heart diseasde, type II diambetes melitis and gastrointestinal diseases (such as colon cancer and diverticulosis). The fibre content present in grain foods can assist with regularity and maintence of the gastrointestinal tract. Grain foods are an integral component of weight management plans, as the are slowly digested and deter overeating.(58)
“The nutrients provided by grains include carbohydrates/starch (energy), protein, fibre and a wide range of vitamins and minerals including the B vitamins folate, thiamin, riboflavin, niacin, iron, vitamin E, zinc, magnesium and phosphorus.”(58)


EFR can differ depending on a client’s activity level, the climate in which they live and disease states which may affect urine output, such as renal disease. Nutrient Reference Values state a simple recommendation for each gender.
MALE
FEMALE
EXAMPLE ONE
(INCLUDING PLAIN WATER, MILK AND OTHER DRINKS, NOT INCLUDING ENERGY DRINKS, SOFT DRINKS OR ALCOHOL)
2.6L/day (about 10 cups)
2.1L/day (about 8 cups)
<1% of total energy intake
A female living in a hot, humid climate and exercising every day would have an EFR of 2.1L a day.
Let the client know that her EFR is 2.1L; however, she will likely require more due to the hot environment in which she lives, combined with sweating from her exercise. Encourage her to check the colour of her urine to help determine if she requires more water.
EXAMPLE TWO
(Four days or more high-intensity activity per week)
A male living in very cold conditions and exercising once a week would have an EFR of 2.6L a day.
Let the client know that his EFR is 2.6LIt is unlikely that he would require additional hydration considering his climate and activity levels; nevertheless, encourage him to check the colour of his urine as an indication.
An additional method or approach for checking the hydration levels of a client is by the colour of their urine, where:
• Pale straw colour: suggests that the body is well hydrated
• Dark yellow colour: suggests that the body is dehydrated
• Clear colour: suggests that the body is possibly over hydrated


According to FSANZ (Food Standards Australia and New Zealand) the recommended amount of caffeine for adults is no more than a total of 400mg per day.(76) This means adults should consume no more than 1 double espresso shot coffee a day OR no more than 2 single espresso shot coffees a day. If caffeine is consumed in excess, it can cause dizziness, restlessness and anxiety.
When recommending caffeine choices to clients, suggest opting for coffee or tea options instead of energy or cola drinks, as these items have a discretionary nature due to their high sugar content. Limiting caffeine intake to the recommendations and substituting it with coffee or tea options will ensure client adherence when following dietary guidance.
When it comes to alcohol, there are two main guidelines to follow. These guidelines ensure alcohol is not consumed in excess and that there are minimal risks of any immediate or lifelong injuries or diseases caused by alcohol.
These guidelines are listed below:
1. To reduce the risk of harm from alcohol-related disease or injury, healthy men and women should drink no more than 10 standard drinks a week and no more than 4 standard drinks on any one day. The less you drink, the lower your risk of harm from alcohol.(77)(78)
2. The Nutrient References Values for Australia and New Zealand states that alcohol should not exceed more than ~5% of daily energy intake on any given day.(79)


Discretionary items refer to food and drinks which are not essential in a healthy diet. These items are usually high in kilojoules, sugar and vegetable oils. These contain low levels of essential nutrients and are consequently referred to as energy-dense and nutrient-poor.
The Australian Dietary Guidelines25 encourage clients to consume less of these foods in much smaller quantities.
Eat For Health recommends no more than 2.5 serves per day, and emphasises there is only room for them in the diet when individuals have high energy expenditure (taller or highly active) and have met all serves for other food groups.(80)
Aim for very minimal discretionary items. If you notice a client consumes excessive amounts, minimise or substitute these items until they are almost completely removed.


Once the client’s dietary intake has been established/analysed (step 2), it is important to compare this against recommended nutritional standards (identified in step 3) to identify if the client lacks any vital food groups and/or nutrients. It also makes it clear whether they are exceeding in any areas too.
Making a comparison (between step 2 and step 3) provides the nutrition coach with evidence to support suggested nutritional recommendations. Based on the comparison, it can be determined what changes need to be made to their meal plan.
It allows nutrition coaches to determine whether the client is under requirements and requires additions in an area, whether they are meeting requirements and require no changes, or exceeding requirements and requiring a reduction in an area.
Melanie is a stay-at-home Mum of two kids who lacks energy and finds herself losing weight but doesn’t know why. She is reasonably active with her young children and regularly goes for walks. Her goals are to increase her energy and overall health so she can keep up with her children.
ANALYSE
ANALYSE THE CLIENT’S CURRENT NUTRITIONAL INTAKE
IDENTIFY THE CLIENT’S RECOMMENDED NUTRITIONAL REQUIREMENTS
JUSTIFICATION
THE CLIENT’S RECOMMENDED NUTRITIONAL REQUIREMENTS
6,706 kJ 9,432 kJ
Increase energy intake by 2,726 kJ. Increase energy-dense and nutrient-dense food items. Increase the number of meals or density of meals. Ensure Melanie doesn’t skip any meals.
61g 52-65g Currently within recommendations, no change is needed. Possibly look at the quality of her protein sources.
(YOUR JUSTIFICATION WILL BE BASED ON YOUR
(YOUR JUSTIFICATION WILL BE BASED ON YOUR CLIENT’S GOAL)
6,706 kJ 9,432 kJ kJ. Increase energy-dense and or density of meals. up with her children. Will be consuming maintain her weight. is losing weight.
Increased energy to keep up with her children. Will be consuming enough energy to maintain her weight. This would be a main contributor as to why she is losing weight.
Maintaining current protein intake to ensure her meals have a healthy balance of macronutrients. CARBOHYDRATES
recommendations, no change is needed. Possibly look at the protein intake to macronutrients.

126g 250-361g Increase carbohydrate content by at least 124g. Evenly spaced out throughout the day. Increase high carbohydratedense foods, with a focus on wholegrain products.
by at least 124g. Evenly spaced out throughout the day.
Increased overall energy and sustain energy for a longer period of time.
dense foods, with a focus on wholegrain products. and sustain energy for a longer period of time.
Currently within recommendations, no change is needed.
Currently within recommendations, no change
Maintaining current fat intake to ensure her meals have a healthy balance of macronutrients.
Maintaining current fat macronutrients.
1.1L 2.1L
12g
FIBRE
25g
Increase fluid intake by 1L, with a particular focus on plain water.
Increase fibre intake by at least 13g.
Focus on increasing vegetable, fruit and wholegrains in meals.
0 serves 2 serves Increase fruit intake by 2 serves. Include a variety of different fruits and colours.
ALCOHOL
DISCRETIONARY ITEMS
2 serves 5 serves Increase vegetable intake by at least 3 serves. Include a variety of different vegetables and colours.
Average of 3.5 standard drinks a day 18.5 standard drinks in 5 days
No more than 4 standard drinks a day. No more than 10 standard drinks in a week.
1.5 serves Minimal amounts with an absolute max of 2.5 serves
Reduce number of days per week Melanie consumes alcohol so she consumes under 10 standards a week. And/ or reduce size/ number of standard drinks a day too. Substitute for non-alcoholic beverages if possible.
Decrease discretionary items slowly until there is no need for them. Melanie needs to focus on meeting her other requirements. Start by decreasing to just 1 serve a day, then make further reductions in the future.
Reduced risk of feeling lethargic.
Increased energy and sustain energy for a longer period of time.
Increased carbohydrate content and fibre resulting in an increase in energy.
Increased carbohydrate content and fibre resulting in an increase in energy.
More available room for nutrient-dense food items and/or water intake.
CAFFEINE
580mg Max of 400mg
Decrease caffeine intake by at least 180mg.
Aim for just 1 double shot espresso coffee a day, instead of 2.
More available room for nutrient-dense food items.
Less reliance on caffeine for energy.
More available room for energy from wholefoods. CALCIUM 1 serve 2-3 serves Increase calcium intake by at least 1 serve. Focussing on low-fat dairy items.
GRAINS 3 serves 4-6 serves Increase grains by at least 1 serve. Focussing on wholegrain options.
Improve bone health to support her active lifestyle.
Increased carbohydrate and fibre resulting in an increase in energy.
Once it has been established how well the client is meeting their requirements, the nutrition coach can assist the client to better reach them through dietary recommendations or the provision of an individually tailored meal plan. It is important to remember that it will ultimately be up to the client to decide which method they prefer: an individualised meal plan or simply a recommendation of dietary changes.
As a nutrition coach, it is one thing to ‘compare’ a client’s nutritional intake to a recommended range; however, it is also important to articulate this information to the client. In other words, a nutrition coach needs to take this step further by explaining their findings to the client for their understanding, so they too can understand any gaps that might be found in their current eating regime.

*The approach that will be taken to support the client will then determine the next step
Step 5 is where a nutrition coach determines what approach they will take with their client to effectively and safely support their nutritional needs and individual goals. As discussed throughout this resource, the goals and nutritional needs will differ from client to client. This is why a nutrition coach needs to remember that the approach they take is on a case-by-case basis, as all clients have differing goals/motives, personalities, likes/dislikes and lifestyles.
Nutrition coaches can take two different approaches/options with their clients. These include:
1. Designing/developing a custom/individualised meal plan for the client
2. Providing the client with individual recommendations and guidelines to follow.
The client’s goals and lifestyle factors will determine whether they would be more suited to a custom/ individualised meal plan or would be better off being provided with individual recommendations.
For a nutrition coach to determine the best approach to take with a client, they must consider the factors discussed above, and get to know the client by building a rapport and identifying what motivates the client toward success. This information is obtained when completing the client questionnaire; however, at later stages, it may be found that what the client has requested may not always be the most appropriate option for them.
For example, the client may initially request a structured meal plan, but after ongoing contact, it may be discovered that the client is better suited to a more flexible approach. It is important always to consider the client’s goals and individual needs when determining which approach to take.
As a nutrition coach, it is important to remember that the process for establishing the client’s nutritional requirements can vary, and the process taught within this unit is not the only way to design an appropriate nutritional plan. This approach is taught simply to provide a benchmark and a starting point.
As a nutrition coach gains more experience and becomes more confident with their services and skills, they can begin to personalise or change this approach to better suit their business structure, themself or their clients.


A custom/individual meal plan refers to an eating guide that has been specifically tailored to the client’s nutritional requirements, food likes/dislikes, lifestyle, eating patterns and health goals. A custom meal plan will specify exactly which foods are to be consumed, the quantity and any required recipes.
It is within the nutrition coach’s scope of practice to create custom meal plans for their healthy adult clients, following the nutrition standards set out in the qualification and industry-endorsed scope of practice. There are many potential benefits for clients who wish to follow a custom meal plan, including:
• Less stress thinking about meal planning
• Little food knowledge required
• Ensures clients meet their nutritional requirements
• Meets budgetary requirements.
The list below provides some examples of the types of people who would be better suited to a structured or individualised meal plan:
• Clients who prefer structure
• Clients who prefer to work methodically
• Clients who are particular about meeting dietary requirements
• Clients who have very strict dietary requirements or allergies
• Clients that require a strict diet for training/exercise or sporting-related requirements
• Clients that lack the creative ability in the kitchen or when designing their own meals.
Nutrition coaches are reminded to refer back to their scope of practice (SoP) developed by the Nutrition Council Australia (NCA, 2018) as a continuous reference guide to operate within their scope of practice, particularly when designing individual nutrition plans for clients.
When designing an individualised meal plan, the following factors should always be considered:
• Likes and dislikes
• Social and work commitments
• Allergies
• Physical activity
• Goals
• Variety/food choices
• Portion sizes
• Meal timing
• Meal frequency
• Measurements and quantities.
Don’t forget to include quantities next to every food item in the meal plan. For example - 100g, 2 cups, 1 tbs, or a handful.
It will help your client knows exactly how much of each item to consume. Also, you will need to use that information when determining how many kilojoules and grams of macronutrients each food item has. Ensuring your client meets their requirements.

To ensure that the client has a well-balanced meal plan and meets all nutritional requirements, it is important that all the steps previously discussed are considered. However, regarding the sequence of designing the nutritional plan, the nutrition coach can customise this to suit the specific situation at hand.
Below is a suggested order of sequence to ensure all nutritional requirements are considered and included to make the planning process easy to follow:
1. Determine daily energy requirements
2. Determine daily protein requirements and then divide by the number of meals (i.e. 100g protein/4 meals = 25g protein per meal each day)
3. Determine energy requirements from carbs
4. Determine energy requirements from fats
5. Confirm requirements of vegetable/fruit intake
6. Confirm fibre requirements
7. Confirm fluid requirements
8. Confirm caffeine recommendations
9. Confirm discretionary item recommendations.
Some clients will opt to have a customised nutrition plan developed for them, whereas others will prefer just to have recommendations provided. Providing dietary adjustments and recommendations is very different from individualised meal planning, as it requires a greater level of client involvement and control over their dietary management.
Counselling clients toward healthier choices to achieve nutritional adequacy via recommendations can empower the client to change poor nutrition habits, which may have a lasting impact. Whilst a custom meal plan provides structure, it may reduce choice, and while some clients do not want to think about food choices, others do. Providing adjustments or recommendations gives clients control over how they approach change and their relationship with food; this is considered more of a ‘client-centred approach’.
Providing recommendations means the same changes are being made. However, instead of a nutrition plan, write the steps as recommendations.
• Consume 5 serves of vegetables a day
• Consume 2 serves of fruit a day
• Ensure you meet the EER of _________ kJ a day
• Ensure you meet the EPR of _________ g a day
• Ensure you meet the EFR of _________ ml a day
• Switch to extra virgin olive oil when cooking
• Include a high-protein mid-morning snack
• Include a high-fibre snack after dinner
• Reduce fast food intake to once a week
• Reduce soft drink intake to once a week

A nutritional adviser must use the orientation methodologies listed below to ensure the client will remember each recommendation and easily understand it.
• Write each recommendation down and provide a copy for the client
• Record yourself explaining them to the client
• Bring a support person to the consultation, so they are both aware of the recommendations
• Get the client to write down the recommendations themselves to ensure they are remembered and understood
• A visual presentation (slideshow, handout etc.)
Provided below are some examples of the types of clients who would be better suited to receiving nutritional/dietary recommendations:
• Clients who prefer flexibility with their nutrition
• Clients who would be better suited to a slower approach with steady changes rather than a complete nutritional overhaul
• A client who simply wants to ensure dietary requirements are met to maintain a healthy lifestyle.
• A client who loves to experiment with food while adding variety to their meals
• Clients confident with making changes within the nutritional advisor’s recommendations.
It is within the nutrition coach’s scope of practice to use this approach with clients deemed to have no risk. Nutrition coaches, however, must practise under industry standards. Nutrition coaches are reminded to refer back to their scope of practice (SoP) developed by the Nutrition Council Australia (NCA, 2018) as a continuous reference guide to stay within their scope of practice, particularly when providing nutritional recommendations to clients.
When developing individual recommendations, it is important that this process is a collaborative effort between the nutrition coach and the client to ensure that the client feels comfortable and capable of achieving the recommendations.


Factors to consider when devising nutritional recommendations for clients:
PROVIDE QUANTITATIVE INFORMATION
GIVE THE CLIENT OPTIONS AND PROVIDE FLEXIBILITY
ALWAYS CONSIDER THE GOALS OF THE CLIENT
MAKE RECOMMENDATIONS BASED ON THE CLIENT'S CAPABILITY TO ACCEPT CHANGES
Make recommendations based on the motivation and drive for positive changes

Be specific in the nutritional recommendations by providing a quantitative amount so the client knows exactly what is expected.
For example, if the client needs to increase their daily amount of fluid, make a recommendation for how much fluid is needed, rather than simply telling them to ‘increase their fluid’.
One of the reasons the client may opt for nutritional recommendations over a structured meal plan could simply be for more variety and flexibility. Teaching clients different ways to achieve the same goal is important.
For example, instead of recommending the client to eat only chicken in a particular meal to reach their protein requirement, other meat sources/quantities that also meet the protein requirements could be provided.
When making recommendations, the client’s goals must be considered, first and foremost. If they are working to achieve their health goals and seeing results, they are more likely to be satisfied with their progress and motivated to continue with guidance.
While a nutrition coach may think other goals are equally important, it is ultimately up to the client to decide which goals they would like to focus on first. It is then the responsibility of the nutrition coach to support them in reaching their goals.
Keep in mind that some people can be hesitant to make changes and may benefit from smaller, steady changes. In other words, the client might not be able to adapt to all recommendations, but they might have the confidence to make one or two changes at a time. For example, suggesting the client add a source of protein to their current meal instead of changing the whole meal to something completely different.
Sometimes knowing whether or not the client is capable of change can be challenging. Compassion and patience must be shown so that the client feels supported in this process because, for some individuals, even the smallest change can be a daunting experience.
Basing recommendations on what the client is motivated and driven to do, as opposed to what they are hesitant to change, will produce greater success and increase confidence, drive and motivation to continue with their health improvements.
For example, suppose the client is confident they can make positive changes to their breakfast intake but is hesitant to change their dinner, given family pressures and time restraints. In that case, it is beneficial to encourage the client to make changes to their breakfast initially, and after some time, encourage changes to dinner.
While it is great to push clients to achieve what they did not think initially possible, it can also damage their confidence if they cannot achieve it and can throw them off making further changes or cause them to revert back to their old ways. It is therefore a delicate balance between what they know they can do and what they are encouraged to do, while ensuring the client’s motivation is there to
MAKE RECOMMENDATIONS BASED ON THE MOTIVATION AND DRIVE FOR POSITIVE CHANGES
Basing recommendations on what the client is motivated and driven to do, as opposed to what they are hesitant to change, will produce greater success and increase confidence, drive and motivation to continue with their health improvements.
For example, suppose the client is confident they can make positive changes to their breakfast intake but is hesitant to change their dinner, given family pressures and time restraints. In that case, it is beneficial to encourage the client to make changes to their breakfast initially, and after some time, encourage changes to dinner.
While it is great to push clients to achieve what they did not think initially possible, it can also damage their confidence if they cannot achieve it and can throw them off making further changes or cause them to revert back to their old ways. It is therefore a delicate balance between what they know they can do and what they are encouraged to do, while ensuring the client’s motivation is there to drive them to complete the recommendation.
The client may have all the drive and motivation they need to accomplish the set recommendations, but their likelihood of success diminishes if their limitations are not accounted for. A limitation refers to any obstacle which may affect the client’s ability to achieve their goal.
Some examples of limitations may include:
• Having a fussy family to feed
• Having little time in the evenings to prepare a meal
• Tight budget restraints
TAKE A CLIENT’S LIMITATIONS INTO ACCOUNT WHEN CREATING RECOMMENDATIONS
Take a client's limitations into account when creating recommendations

• Not having certain kitchen equipment
• simply not having the support from family or friends to make healthy lifestyle changes.
For example, a client may be enthusiastic about increasing their vegetable intake by juicing some of their vegetables, however, if they do not own a juicer, they are unlikely to be able to complete the recommendation. Another example may be time restraints, where a nutrition coach may need to discuss the importance of food preparation with the client instead of simply giving them a nourishing meal plan.
Accounting for the client’s limitations, commonly referred to as barriers to change, will allow the nutrition coach to make suitable and achievable recommendations for clients.
The client may have all the drive and motivation they need to accomplish the set recommendations, but their likelihood of success diminishes if their limitations are not accounted for. A limitation refers to any obstacle which may affect the client’s ability to achieve their goal.
Some examples of limitations may include:
• Having a fussy family to feed
• Having little time in the evenings to prepare a meal
• Tight budget restraints
• Not having certain kitchen equipment
• simply not having the support from family or friends to make healthy lifestyle changes.
For example, a client may be enthusiastic about increasing their vegetable intake by juicing some of their vegetables, however, if they do not own a juicer, they are unlikely to be able to complete the recommendation. Another example may be time restraints, where a nutritional advisor may need to discuss the importance of food preparation with the client instead of simply giving them a nourishing meal plan.


Following the initial consultation with the client, it is important to confirm their understanding of the nutritional plan or recommendations and gather feedback on whether the client believes it is something that can be achieved.
It is vital that a nutrition coach discusses the plan or approach with the client and provides them with the opportunity to ask questions. The aim is to ensure clients are confident in maintaining the changes daily.
Another important factor to consider is discussing potential barriers the client believes may limit their success. Discussing these barriers with the client can help a nutrition coach develop potential strategies for overcoming them. For example, simple strategies such as changing grocery shopping habits can significantly impact a client’s access to and consumption of nutritionally rich food.
To ensure that the client is following the nutritional plan or dietary suggestions, nutrition coaches must be actively engaged in the client’s journey as much as possible. The most effective way to achieve this is to recognise the importance of follow-up consultations and regular check-ins with the client to monitor their progress.
Benefits of conducting follow-up consultations (or ongoing reviews) with clients:
• Monitor the client’s progress and gain regular feedback from the client
• Make any modifications to the nutritional plan or dietary approach (if necessary)
• Effectively support the client and encourage them to achieve their goals
• Get to know the client over some time, rather than just having a one-off consultation where the client is never seen again
• Build a rapport with the client, which ensures client adherence and general satisfaction with the services provided by the nutrition coach
• Ensure repeat service is made, which in turn, means repeat revenue for the nutrition coach
• Provide quality service to current clients, which can lead to the current client referring the nutrition coach to friends/family.
While ensuring that follow-up consultations are incorporated into a client’s nutritional strategy, it is also important to ensure that the client understands the monitoring process and timeline, so that they can ensure their commitment to their goals.

While there is no hard and fast rule for monitoring progress as a nutrition coach, the following timeline provides a start point to discuss with the client:
A 2-3 day post initial up, similar to a ‘check-up’, is simply a follow-up made to see how the client finds the nutritional plan (or dietary strategy) and to confirm whether they have any additional questions now that they have commenced their journey.
Setting a post-initial follow-up or even a brief check-in with the client also shows that the nutrition coach is engaged and supportive of the client’s goals and sets a good standard for professional practice.
This initial follow-up with the client does not have to be made face-to-face: it can be done just as effectively via email, phone, skype or even in today’s society, by text message (depending on the client).
A 7-10 day follow-up consultation provides the opportunity for nutrition coaches to answer any further questions and fine-tune the plan based on the client’s feedback.
7-10 DAYS POST INITIAL (1ST REVIEW CONSULTATION)
2-4 WEEKS POST INITIAL (2ND REVIEW CONSULTATION)
As major changes are unlikely to have occurred within a -week period, physical evaluations such as weight, circumference, energy etc. are typically not required.
Ideally, this consultation will be conducted in person; however, it may be conducted via phone or skype if this is unachievable.
In a 2-4 week follow-up consultation, it is recommended that an assessment be conducted to compare against baseline measurements from the initial screening process.
This can include:
• Weight changes and/or body fat measurements
• Circumference measurements
• Energy levels
• Cravings.
This consultation provides an opportunity to modify the program if required and to give additional information to further assist their progress, such as meal preparation techniques. It is also appropriate to discuss the client’s goals, identify how they are managing their previous barriers to change and discuss how to overcome any new barriers to change. Additional goals may be added at this time if the client believes they can achieve them.
6-8 WEEKS POST INITIAL (3RD REVIEW CONSULTATION)
The 6-8 week follow-up consultation should mirror the 2-4 week evaluation, discuss ongoing barriers, and introduce new health/nutrition goals as the client continues their progress (if the client feels ready).

While regular follow-ups are an effective tool to support clients and ensure client adherence, nutrition coaches can also decide to conduct ongoing reviews with their clients as they see fit or when it suits both parties. This could be once a month, once a fortnight or some clients even enjoy a quick catch-up once a week to help keep them on track.
During these review sessions (or meetings), the nutrition coach would focus on the following:
• Continue to monitor weight, circumference, energy etc. every 2-4 weeks
• Continue to discuss barriers and how to overcome them
• As the client reaches current goals, help them to set new goals to keep them motivated.
As a nutrition coach, it is important to recognise that not all clients are the same or require the same number of review sessions. Some clients may feel confident and not want to catch up regularly, while others may come to rely on regular review sessions, where the nutrition coach provides advice and support to the client. In other words, some clients may like regular monitoring, feedback and assistance; others prefer to be left to their own devices for several months at a time.
If the client declines further support and ongoing review sessions, then general periodic communication (made by the nutrition coach) is recommended and extremely beneficial. For example, an email 1-3 months afterwards to see how the client is tracking and to check if they have any questions.
It is advised that ongoing follow-ups with clients be discussed to gain an understanding of how frequently they want to follow up. Financial and time constraints also impact bear in mind that follow ups. Even if clients would like to follow up once a fortnight, they may only be able to afford a consult once every six weeks. In this scenario, a nutrition coach must be adaptable and able to work within client limitations.


As discussed in this resource, there are a wide range of factors which may prevent a client from adhering to their nutritional plan. Sometimes clients do not achieve their desired results, or progress slower than they had hoped. Similarly, the nutritional plan may not have the exact impacts planned for during the initial consultation and may not directly assist the client in achieving their goals. There is also a possibility that adjustments to the client’s dietary habits and lifestyle may lead to some other changes in their overall health and variations in their results.
Accordingly, as a nutrition coach, it is critical that ongoing reviews are provided for the client, and a flexible approach is maintained to assist them in achieving their goals and overcome variations in their results.
Some potential variations include:
• Weight gain when trying to lose
• Weight loss when trying to gain
• Increased bloating or loosely formed stools
• Decreased energy.
There is no single, simple answer for what to do when variations in results are encountered. Therefore, nutrition coaches must discuss with the client and identify what the issue may be.
The following questions may help clients to identify what is preventing progress:
• What do they think is happening?
• Is the meal plan being followed?
• If not, why not?
At each point, a nutrition coach can identify potential barriers, rethink the nutritional plan and make some changes or recommendations that better suit the client.


Monitoring certain factors in the individual’s life can help keep the client on track with their progress. Various factors can be monitored to track both the progress and adherence of a client, including:
• Weight
• BMI
• Body fat percentage
• Circumference measurements (waist, hips and WHR)
• Energy levels
• Cravings
• Bowel motions
• Physical abilities
• Motivation
• Barriers to change (i.e. meal fatigue, finance, time, support).
The above factors are further outlined in the table below:
FAT
FAT-FREE
CIRCUMFERENCE (WAIST, HIPS, BELLY BUTTON, WAIST-TO-HIP RATIO)
ENERGY LEVELS (RATE OUT OF 10)

CRAVINGS (HOW MANY IN
Most weight loss clients like to keep a close eye on the scales to ensure their weight is decreasing. While this can motivate the client, it can also be detrimental if they weigh themselves too frequently. It is therefore important to highlight other factors to monitor and measure, such as waist circumference and energy levels, to avoid disappointment in weight. Encourage the client to weigh themselves at home, at the same time of day, preferably in the nude and at a maximum of once a week. Remind them that the scales are reflective of minor weight fluctuations, such as going to the toilet or drinking additional fluids.
As a client loses weight, their BMI will change. Over time they will be able to see themselves changing BMI categories, with the obvious end goal of being in the healthy weight category. BMI changes take longer than weight or circumference changes and are therefore encouraged to be used in conjunction with other measurements.
Using a Bio-electric Impedance Analysis (BIA) scale is a highly motivational tool for clients as they can identify fat loss instead of total body weight loss. For example, a weight loss client may feel disappointed as they have not lost any weight according to regular scales; however, when on the BIA scales they can see that their fat mass has decreased.
Fluid status is a great way to check how hydrated a client is and can be eyeopening for the client too. Fluid status changes immediately, depending on how much water is in the body.
There are a great variety of BIA scales on the market, and it is important to obtain good quality scales for consistency and accuracy. It is also important to remember that no matter which scales are purchased, there can be fluctuations in the scales and they are to be used as a guide only.
Taking circumference measurements is one of the most motivational measurements to track, as this is where a lot of change can occur. Most health professionals stick to waist, hips and chest circumference measurements; however, there is potential to include all other circumferences such as thigh, neck and upper arm, depending on client goals.
(I.E. MEAL FATIGUE, FINANCE, TIME, SUPPORT)
Clients often do not realise how much better they feel until they rate their energy levels. While other measurements may take several weeks to show progress, energy levels can begin to improve within a few days of dietary changes.
While cravings are not beneficial for all clients, helping those who are decreasing sugar intake identify how frequently they crave food can be extremely motivational. Cravings reduce rapidly, depending on food intake, and clients often do not realise how much they have improved until they rate their cravings.
Nutrition coaches may consider the following questions:
• Are they becoming more formed, more regular, less offensive? Even clients who believe they have regular bowel motions may notice a change in motions as they begin to change their diet. While bowel motions may not be as motivating as other measurements, they can provide a nutritional advisornutrition coach with a guide to the client’s gut health, fibre intake and hydration status.
• Flatulence (more or less with the nutritional plan? What may be the cause?)
• Bloating (more or less with the nutritional plan? What may be the cause?)
Physical abilities relate to fitness levels and ability to complete certain tasks, such as bending over, squatting or running for a set period. It is outside the scope of practice for a nutritional advisornutrition coach to comment and provide feedback outside the Australian Guidelines of Physical Activity; however, conversing with the client about observed improvements can be motivational.
Checking on the client’s motivation levels is extremely important, as low motivation affects their results. If a client is struggling with motivation, it may be an idea to go back and revisit the reasons why they are making healthy changes in the first place and what their health goals are.
Have an open discussion with the client regarding barriers to change and develop strategies to overcome these barriers. For example, prep time required for final exams may be a barrier to change for the next two weeks and, therefore may be decreasing the client’s motivation levels.
Barriers to change are significant to discuss regularly with clients. Barriers will change weekly and the client may require support to find strategies to overcome or minimise these barriers.
As a nutrition coach, it is also important to remember that some of the most significant factors to monitor are generally based on the client’s goals and what they want to achieve. Anything that has been measured at baseline during the initial consultation may be reviewed throughout the consultations, and new measurements can be added as their goals change.


Providing the client with a copy of written records is often beneficial to track their progress. Providing written confirmation can be highly motivational if the client is progressing well and may assist in refocusing the client if they have been unsuccessful following their plan.
Written records can be simple or comprehensive, however should provide enough information to be useful to the client without being confusing or overwhelming. Some examples are provided below.
Client Name: James Smith
Goal: Weight loss of 10kg by this November to bring total body weight down to 86kg.
2/week, constipated, sore to pass, offensive smelling 4/week, softer motions, offensive smelling More regular, easier to pass


As nutrition coaches begin to see clients regularly, it will be essential to tailor interventions and strategies to ensure progress towards goals. It must be remembered that each client and their situation is unique and, as such, what works to achieve one client’s goal may not work for another. Therefore, getting regular feedback about how the client is progressing with a strategy, whether it is working, being enjoyed, or what could be done to tweak or modify it.
Feedback methods refer to the way feedback is presented. Feedback can be positive, negative or constructive, and when delivered well, it can positively impact the client. Feedback is provided from the client to the nutrition coach and the nutrition coach to the client. There is a constant feedback process, which provides information to either party about how the other individual is taking and processing the information.
Positive feedback can be reinforced to a client through statements, such as:
• You have followed everything in your meal plan this week - well done!
• You have really stuck to your goals this past month - you must be so proud!
• You have made great progress this week!
• You have amazing willpower!
• You have done an excellent job!
Negative or constructive feedback, on the other hand, may need to be delivered more subtly so that the feedback does not upset or demotivate the client. Often, positive feedback is provided before the negative/ constructive feedback, and more positive feedback is provided at the end. This technique can often be referred to as the ‘sandwich technique’ whereby the negative/constructive feedback is softened with positive feedback before and after.
THE FEEDBACK SANDWICH THE FEEDBACK SANDWICH
POSITIVE FEEDBACK
POSITIVE FEEDBACK CONSTRUCTIVE FEEDBACK

The table below outlines how the sandwich technique works: the positive feedback is delivered as the two slices of bread, and the negative/constructive feedback is delivered as the ‘filling’.
THE FIRST LAYER OF THE BREAD
Point out something positive that the client is doing around their performance.
‘You have been putting in a massive effort this past month to achieve the goals we have set together for you’.
THE ‘FILLING’ OF THE SANDWICH
THE OTHER LAYER OF THE BREAD
Let the client know about their performance and what they can or should work on. This feedback needs to be delivered carefully to avoid upset or demotivate the client.
Reinforce the client’s positive behaviour and encourage them to stay motivated. It is important to provide the a ‘cushion’ to the negative feedback. Even though the ‘filling’ of the sandwich was the real message, the receiver will get that message loud and clear, but the negative impact will be diluted with the ‘bread’ or the positives of the sandwich.
‘I need you to stick to your healthy eating plan and exercise regime over the holidays as I know it can be a tough time of year to stay motivated. Remember we also went through this at the same time last year?’.
‘I am sure you will achieve your goals as you are almost there and have already lost 3kg. You have been able to adapt to these changes extremely fast. Well done, you should be proud of yourself.
Nutrition coaches can also ask for feedback from their clients. This can be achieved informally, by casually asking the client questions about how they feel about the nutritional support program and/or nutritional plan they are undertaking. This can happen regularly and the responses of the client can be recorded and kept on file for future monitoring.
Another informal method of receiving a client’s feedback is when they offer their feedback voluntarily. In other words, they were not asked for their feedback at the time. This type of feedback is important for a nutrition coach and should also be noted in the client’s profile.
• Surveys
• Interviews
• Emails
• Phone calls
• Face to face.
Reinforce the client’s positive behaviour and encourage them to stay motivated. It is important to provide the a ‘cushion’ to the negative feedback. Even though the ‘filling’ of the sandwich was the real message, the receiver will get that message loud and clear, but the negative impact will be diluted with the ‘bread’ or the positives of the sandwich.
‘I am sure you will achieve your goals as you are almost there and have already lost 3kg. You have been able to adapt to these changes extremely fast. Well done, you should be proud of yourself.
When deliberately seeking feedback from clients, there are also several more formal approaches that a nutrition coach can take, such as:
In addition to the above, an effective way to formally gain feedback from a client is to provide them with a feedback form to fill out. Feedback forms generally have pre-designed questions for the client to answer and/or provide, in writing, their thoughts on the nutritional plan, dietary recommendations and even the support provided. This written feedback can then be added to the client’s profile for future reference.
The information from the client’s formal and informal feedback is important to monitor and evaluate the effectiveness of a nutrition coach’s nutritional plan. It also shows the client that the nutrition coach is serious about their progression and is supportive throughout the process.

CLIENT NAME:
DATE:
Instructions for client:
Please answer the following questions carefully and make appropriate comments where necessary. Use the following scale to answer the questions, place a circle around the number that best reflects your response.


Communication is key to the success of any relationship. For a nutrition coach to give and receive feedback successfully, it is important to develop the ability to communicate effectively with clients. Effective communication relies on the ability of the sender to explain their meaning and the interpretation of the message by the receiver.
Communication can be verbal, non-verbal or written. Examples of each have been provided in the table below:
Talking is the major form of communication through consultations with clients. It is generally the preferred method of conveying information from one individual to another and allows immediate clarification and response.
Throughout the consultation, the professional and the client may make various sounds to show active listening and agreement.
Handshaking is seen as a sign of respect and courtesy in Australia. While males mostly conduct the handshake, many females use this method of communication when greeting or bidding farewell to a client.
While not used frequently during a consultation, clapping may indicate excitement or pleasure. For example, clients may reach their goal weight and clap with excitement.
Throughout the consultation, each party may show their understanding or agreement by simply verbalising ‘yes’.
Maintaining eye contact through verbal communication shows respect and the client that the professional is actively listening and not being distracted. When eye contact is not given, the individual may be disinterested, bored or uncomfortable with the topic at hand.
Text messages are frequently used to remind clients about their appointment times. Some clinics allow clients to text back, while others request a phone call if the appointment time needs amending.
Media sources, such as journals, brochures and websites, are frequently used to help advertise a nutritional advisornutrition coach's clinic, expertise and products. A wide variety of audiences can access these.
Emails can be used throughout clinical practice to communicate with clients, health professionals and the wider community through email updates.
Throughout the consultation, each party may show their lack of understanding or disagreement by simply verbalising ‘no’.
While not frequently used throughout consultations, hugs are a method of intimate communication that may be a greeting, a good wish or farewell.
A memo (short for memorandum) is a note or document to record information. Where letters are generally used to communicate with external recipients, a memo could be used for internal purposes in a business.

used for internal purposes in a business.
When communicating, emphasis can be placed on certain words to highlight various parts of the message.
Facial expressions can often communicate more than words themselves. Facial expressions will show immediate emotions throughout the consultation, such as frustration, confusion, happiness or agreement. A written letter is often used to communicate information about a client from one health professional to another. This is a common courtesy to assist the fellow health professional in providing optimal care and advice for the client.
The tone of voice used can provide a lot of information regarding the emotions (e.g. happy, sad, frustrated, angry), and feelings about the topic (e.g. disapproval, apprehensive).
It is important to control speech’s tempo (speed) for effective communication. Speaking too quickly can be challenging to understand, while talking too slowly can be distracting for the client.
Patting on the back can be used for both a congratulatory message and a sympathy message, depending on the situation.
An individual’s posture while communicating can say a lot about their interest levels. For example, an individual slouched back in their chair would not look as professional or engaged as an individual sitting upright listening intently.
Gestures can be used to assist with non-verbal communication, usually using the head or the hand. For example, an individual may cock their head to one side to show they do not fully understand something or may put their hand up, palm facing forward, to interject or pause the conversation.
A very popular form of nonverbal communication is sign language. This mode of communication is predominantly used by deaf individuals and allows individuals to communicate using their hands to sign words fully.

There are several strategies that can be utilised when communicating with a client. Outlined below are some common tips for effective communication between a nutrition coach and a client:
• Keep the message simple and meaningful
• Describe the client’s behaviour or the situation based on the way they may see it
• Prioritise the feedback. Is this needed right now, or would this information be too overwhelming for the client?
• Inspire, encourage and positively reinforce the intended message
• Treat the client the same as the nutritional advisor would want to be treated themself. Consider how the information may be coming across and adjust the tone, the intensity of information and reiteration as required
• Use examples to reiterate information
• Avoid distractions when consulting, as this can appear rude and give the client the impression they are not being listened to properly.


In addition to the composition of foods and the nutritional breakdowns developed within a nutritional plan, nutrition coaches need to be aware of other dietary factors that can impact the success of a nutritional plan. This allows for a nutrition coach to be more accommodating to a client’s individual preferences and, in turn, improve client progress and adherence.
As discussed throughout this resource, a multitude of factors can impact the client’s success when following a suggested dietary approach or nutritional plan. Some of these factors are listed and outlined (but not limited to) below:
• Nutrient timing
• Meal frequency
• Functional foods
• Meal fatigue
• Client likes and dislikes
• Organic vs non-organic foods
• Detox theory.
The above considerations are discussed in greater detail on the following pages.

The timing of meals each day depends on personal preference and time constraints. Therefore, the reasons for nutrient timing can be varied and not always based on science, with personal preference playing a role. For non-athletes, nutrient timing is driven by meal frequency, size and snacking. Some individuals prefer small, regular meals throughout the day, while others prefer maybe 2-3 main meals and no snacking.
CARBOHYDRATES
Probably the most well-known use of nutrient timing about protein is the ‘anabolic window’, which is elevated for up to 48 hours after a resistance training session. During the early stages of this window (up to 2 hours post training), it is beneficial to consume enough protein to maximally trigger muscle protein synthesis to ensure that muscles get the amino acids required to repair tissue damage caused by training.
The suggested minimum is approximately 20g of protein, including 3-5g of the amino acid leucine, which induces a strong protein response. Research also recommends that protein requirements be evenly distributed across the day.(81)(53)
Carbohydrate timing can be most beneficial for pre and post-exercise nutrition, to maximise muscle glycogen stores and circulating blood glucose for energy production. Timing intake for exercise can result in improved performance, reduced fatigue and faster recovery from exercise, which is important for many competitive athletes.(82)
Carbohydrates are also best utilised around exercise due to their fast breakdown/ absorption and use in both the aerobic and anaerobic system.(53)
The timing of fats is less important to athletic performance than carbohydrates and protein; however, fat is important for exercise recovery as it is used for many important bodily processes such as the production of hormones and cell structures. There is little evidence for recommending specific nutrient timing for fats. Meal frequency does not affect overall metabolic rate.(53)

One of the most common factors affecting the breakdown and absorption of nutrients is the frequency of meals and the timing of nutrient intake. While there are several theories for the most appropriate times to consume meals and nutrients, most research indicates that for general health and nutrition, there is no benefit to specific meal frequency.
Where a benefit may exist, this is only for athletes with body composition or performance goals requiring specific nutritional manipulation. For non-athletes, dietary quality, energy balance and sustained energy for activities of daily living should be the focus of their eating pattern.
Meal frequency refers to how many meals and snacks a client consumes daily, independent of specific timing. For example, an athlete may time two of their meals around their training sessions; however, they may eat 4-5 meals spread out across the day.
Whilst the recommended daily intake levels of food indicate the overall quantities required by an individual, eating all of these in a single meal is unlikely to allow the body sufficient time to break down and utilise all elements. This is why it is important to spread meals throughout the day for the client to reach their recommended intake of nutrients effectively.
For a client with no health concerns, the amount of meals consumed over the day is a matter of personal preference. Some clients may choose to consume 3 main meals with snacks between meals (totalling 6 meals per day), whereas others are more comfortable with simply eating 4-5 medium-large meals throughout the day with no snacks in between. It has been argued that eating 3 meals and 2-3 snacks a day (or every 3 hours) helps to ‘stoke the metabolism’ and increase metabolic rate, but this is not true. Eating food requires energy to break it down, known as the ‘Thermic Effect of Food’ (TEF), and it is this requirement leads to increased metabolism - it is a temporary effect of eating rather than an ongoing one.(83) A benefit to not snacking between meals may be in allowing the body to enter the post-fed state (around 4 hours after eating) whereby energy production will largely come from fat stores. This will reduce blood glucose and insulin spikes associated with small regular meals, which could result in better blood glucose control and stable mood.
This choice is generally up to the client as it will be what works best for them, given their preference and other lifestyle commitments. With this being said, the nutrition coach’s role is to ensure that a client’s chosen eating pattern (or frequency) fits with their lifestyle, activity levels and energy requirements. Encouraging clients to spread their meals out to provide sustained energy for their daily activities and nutrition goals is sensible advice; however it still must fit with the client’s preferences. Therefore, the nutrition coach must work collaboratively with the client to ensure a sensible and achievable strategy is put in place when deciding how frequently the client should eat their meals. Listing meals in the order you want them to be consumed, and labelling meals (breakfast, lunch, dinner, snacks) can help clients follow the plan easily.
Further guidance should be provided to the client regarding physical activity and the frequency of meals. If physical activity is strenuous, such as resistance training or endurance-related, discussing nutrition around pre- and posttraining to ensure adequate energy for training and recovery is important.
The reason health professionals used to advocate for six smaller meals throughout the day was simply to avoid hunger and cravings. The thinking was that by providing individuals with small amounts of food every few hours, they would always be satiated and therefore, it would decrease the likelihood of them reaching for foods that they are craving. However, this is not how all clients operate, and while this approach may work for some clients, it most certainly does not work for all. It is now better understood that it is not so much the timing and frequency of meals but instead the nutritional value within those meals that greatly impacts satiety.

Once a general nutrition plan has been established for a client, the indication for functional foods can then be examined. Functional foods can be defined as foods that have a potentially positive effect on health beyond basic nutrition,(49) and includes the nutrients found within foods that perform specific functions that may improve health, including, but not limited to:
• Vitamins
• Minerals
• Essential fatty acids
• Essential amino acids
• Prebiotics
• Superfoods and botanicals.
Proponents of functional foods claim they promote optimal health and help reduce the risk of disease. Foods that contain these functional elements that may improve health are often referred to as ‘superfoods’.
The International Food Information Council Foundation have provided a detailed, but not exhaustive list of functional foods in their background information sheet.
CLICK HERE To view the list.
Before recommending any functional foods, it is important to consider a client’s current dietary intake, as they may not require additional nutritional support. Ask the questions: Is the client already getting sufficient nutritional value from other elements within their diet? Is there another food, nutrient or supplement that would allow the client to gain the same benefit without exceeding the daily requirements? Asking these questions will allow the nutrition coach to decide what is best for their client and whether functional foods are incorporated.
There are two important considerations when incorporating functional foods into a client’s nutrition plan:
1. Firstly, are the listed benefits officially recognised? When conducting research, nutrition coaches should look at whether official bodies (such as the US Food and Drug Administration [FDA]) have conducted evidence-based testing on the product’s claimed benefits.
2. Secondly, it is important to identify whether there are potential side effects of using a product beyond the desired benefit. For example, while the item may address the client’s fatigue, it may also lead to issues with sleep or digestion, which is therefore counterproductive.


Superfoods are known as ‘super’ because of their high levels of phytonutrients. Phytonutrients are the natural compounds in fruits, vegetables and plants that help protect the plant from UV radiation, germs, fungi and other harmful effects. These phytonutrients are also extremely beneficial to humans, helping to sustain healthy life and vitality.(84)
Botanicals (often called ‘herbal products’ come solely from a plant (or plant parts) valued for their medicinal or therapeutic properties, flavour, or scent. Like superfoods, food/products made from botanicals are often used to maintain or improve health.(85)

Phytonutrients, also known as phytochemicals, are chemical compounds found in all plant foods that are essential for optimal human health, enable the body to function normally and are protective against various diseases.(84) They are also responsible for many of the colours, tastes and aromas of foods.
There are about 10,000 known phytochemicals that have been identified so far, with these chemical compounds working as antioxidants in the body, some also having anti-inflammatory and immune system strengthening properties.(84)
The major classes of phytonutrients are shown in the table below:
FLAVONOIDS
ORGANIC ACIDS

Terpenoids (also known as terpenes) are the largest and most diverse class of plant phytonutrients.(86) Some terpenoids in herbs and spices have medicinal and antimicrobial properties, are used in food preservation, as well as being responsible for the flavour of some foods, for example, saffron, lemongrass and ginger.(86)
Terpenoids like limonene are found in citrus foods and menthol, carotenoids (vitamin A precursors), coenzyme Q10, phytosterols, and the tocopherols and tocotrienols.
Flavonoids include anthocyanins, flavonols, flavanones, flavones and isolflavones and are the plant pigments that give plants their colours, like the deep blue of blueberries, the purple of grapes, the orange of pumpkins, or the red of tomatoes.(87) There are an estimated 10,000 different members of flavonoids. Flavonoids include the anthocyanidins in blueberries and quercetin found in onions.
Isoflavonoids are a member of flavonoids, and lignans are a large group of polyphenols found in plants. For example, genistein and daidzein are found in soy foods and the lignans in flaxseed and rye.
Organic acids are best described as organic compounds with acidic properties; they are produced from the catabolism of amino acids. For example, ferulic acid, which is found in whole grains, and coumarins, which are found in parsley, liquorice and citrus fruits.
ACAI
(88)(89)
(90)(91)
(92)(93)(94)(95)(96)
Acai berries come from a palm tree that grows in South America. Research has shown that acai is even higher in antioxidants than cranberries, raspberries, blackberries, strawberries, or blueberries. Antioxidants are needed to protect the body’s cells from free radicals generated through stress, toxins, alcohol and processed food.
A green grass rich in vitamins and minerals with all its naturally occurring cofactors intact, Barley grass contains significant quantities of calcium, copper, iron, magnesium, potassium, zinc, β-carotene, folate, pantothenic acid, vitamins B1, B2, B6, C, and E, superoxide dismutase, catalase, and chlorophyll.
Young barley shoots absorb nutrients from the soil and are an entirely natural source of valuable nutrients for detoxification and healthy cell regulation. Barley grass may contain 11 times more calcium than cow’s milk, five times the iron of spinach and seven times the vitamin C of oranges - plus a range of other potent vitamins. It is high in organic sodium, which benefits joints and digestion.
Barley can be consumed as raw barley grass (added to salads or juiced), juiced or as a powder, which can be added to smoothies, drinks or cold foods. It is noted that powdered barley grass may not contain all the nutrients of fresh or juiced barley grass.
It’s worth asking a few trusted people in your life what they think of when they first see the business name or if it clearly depicts your business. As they are not personally invested in the name, they may point out something that you hadn’t yet considered.
Pollen is the male seed of flowers and is necessary for fertilising plants. It is also what young bees feed upon. Research proves that bee pollen contains an average of 25% protein, with some research suggesting protein content to be as high as 40% (half of which is in the form of free amino acids that can be used immediately by the body). This makes a powerful source of protein for humans as well as bees. Bee pollen contains nearly all the nutrients humans require - the necessary components of life. Bee pollen has very similar overlapping health properties and benefits as honey. Therefore, bee pollen could be used as an alternative to honey if desired.
A fruit native to North America and grown all over the world, blueberries are rich in phytonutrients. Research shows they provide as much antioxidant protection as 1700mg of vitamin E and more than 1200mg of vitamin C.
(97)(98)
(99)(100)(101)(102)
New research shows blueberries are also beneficial for improving memory and slowing down or postponing the onset of other cognitive problems associated with ageing. It is also possible to freeze blueberries without damaging their antioxidant content. Their low GI means they provide sustained energy.
Cacao is the unrefined form of the cacao bean. Research shows that 60-90% of the antioxidant content of cacao is lost when it is treated and processed (i.e. turned into cocoa powder). Cacao has approximately 40 times the antioxidants of blueberries and contains more calcium than cow’s milk. Best of all, it contains mood-boosting neurotransmitters known as serotonin and dopamine, which are important for regulating mood and optimising mental health.

(103) (104)(105)
(106)(107)(108)
Chia seed is a species of flowering plant from the mint family, native to Mexico and Guatemala. When soaked, the seeds absorb up to 12 times their weight in liquid. Soaking gives them a mucilaginous gel-like coating.
Chia seeds are an quality source of carbohydrates and fibre, and their mucilaginous form aids digestion and elimination. Chia seeds are a concentrated source of the essential omega-3 fatty acid, Alpha Alpha-Linolenic Acid. They are also high in B vitamins thiamine and, niacin, and a range of dietary minerals, including calcium and zinc.
Chlorella is green algae that grows in fresh water under direct sunlight. It reproduces rapidly through photosynthesis using only carbon dioxide, water, sunlight and a small amount of minerals. Chlorella’s photosynthetic efficiency makes it a source of food and energy. It comprises 45-60% protein and more than 20 vitamins and minerals when dried. It also contains the highest amount of chlorophyll of any known plant, 18 amino acids and many essential fatty acids. It has been an energising food source for centuries, especially throughout Asia.
Research on chlorella and spirulina is limited, with more studies required to support the health benefits and determine their safety. Despite this, the evidence is still very promising, and small amounts of chlorella and spirulina are regarded as generally safe for consumption.(109)(110)(111)
An edible oil extracted from the kernel or meat of mature coconuts, coconut oil has long been used in cosmetics and food. Virgin organic coconut oil is the best source. While some may be concerned about this oil’s high saturated fat content, it is important to note that it is made mostly of medium-chain fatty acids as opposed to long-chain fatty acids.
These include healthy fats such as lauric acid, caprylic acid and capric acid;
• Lauric acid: Helps to raise total blood cholesterol levels by increasing both high-density and low-density lipoprotein
• Caprylic acid: Is a potent anti-fungal and can be useful in treating Candidiasis
• Capric acid: May allow for greater energy expenditure to assist in weight loss.
Coconut oil’s saturated fatty acid profile means it has a higher smoke point than many polyunsaturated or monounsaturated oils, making it more heat stable for higher temperature cooking.
As the clear liquid inside young green coconuts, coconut water holds the endosperm of the coconut until the endosperm matures and deposits into the coconut meat.
Coconut water is a natural source of electrolytes and carbohydrates, making it great as a sports drink. Although the electrolyte minerals are in small amounts, coconut water is still a fast means of rehydration. It is a healthy and delicious alternative to commercial sports drinks/processed drinks.
When fermented by lactobacillus bacteria, vegetables become a source of beneficial bacteria and enzymes. The culturing process produces beneficial microbes that help balance intestinal flora and overall immunity. Lactobacilli provide antitoxic, antitumour and antioxidant actions. They help fight infections and prevent gastrointestinal tract diseases, including peptic ulcer disease and gastric cancer.(113)(114)
This also helps with the production of serotonin in the gut, essential for mood regulation. Fermented foods are also excellent chelators and detox agents, helping rid the body of toxins and heavy metals.

(115)(116)(117)
Goji berries are considered one of the only fruits containing all essential amino acids. They also contain the highest concentration of protein of any fruit. Goji berries are high in fibre, and vitamin C and contain more carotenoids than any other food. They also harbour natural anti-inflammatory, antibacterial and antifungal compounds, and their powerful antioxidant properties and polysaccharides help boost the immune system.
Kale is a green, leafy vegetable that comes from the Brassica family, grown in most countries and can be easily sourced. Kale is known for its antioxidants, anti-inflammatory nutrients and potential anti-cancer nutrients in glucosinolates.
(118)(119) (120)(121)
(123) (124)(125)
KELP, ARAME, WAKAME)
(126)(127)
(106)(107)(108)

418kJof kale provide over 350mg of the most basic omega-3 fatty acid, ALA. Raw and steamed kale helps to lower cholesterol by binding its bile acids. It is also rich in vitamins, especially vitamins A and K.
It is important to note that prolonged and very high consumption of raw kale (mostly by people with hypothyroidism) can affect the thyroid due to the increased amount of goitrogens consumed, which block iodine from entering the thyroid gland.(122)
A cultured, creamy product similar to yoghurt contains beneficial yeast and friendly probiotic bacteria. Loaded with vitamins, minerals and easily digestible complete proteins, kefir is great for nourishing the gut.
Kefir is made from gelatinous white or yellow particles called ‘grains’, using any type of milk such as cow, goat, sheep, coconut, rice or soy.50 These grains contain the bacteria/yeast mixture clumped together with casein (milk proteins) and complex sugars. The grains ferment the milk, incorporating their friendly organisms to create the cultured product. The grains are then removed with a strainer before consumption of the kefir and added to a new batch of milk. Kefir helps to create healthy conditions in the digestive tract for the colonisation of friendly bacteria.
Maca, also known as ‘Peruvian ginseng’, is a root that belongs to the radish family and grows in the mountains of Peru.
Maca is most known for its energy-boosting properties and ability to increase libido and fertility. Maca contains 55 phytochemicals, including vitamins B1, B2, B12 and C, and zinc. It also has amino acids, calcium and phosphorus, plus 22 fatty acids, which function as a fungicide and a local antiseptic.
Seaweed is a marine algae that lives near the seabed. It can include red, brown and green algae. Seaweed is considered one of the greatest nutritionally-dense plants on earth and is also the most plentiful source of minerals in the plant kingdom, as it has access to all the nutrients in the ocean. Its high chlorophyll component makes seaweed a powerful detoxifier, alkaliser and chelator of toxins in the body. Iodine in seaweed is also beneficial in supporting healthy thyroid function.
Spirulina is a blue-green algae that can be cultivated worldwide. Spirulina contains high concentrations of phycocyanin, a phytochemical that may help prevent cancer and gives spirulina its unique blue tint.
Dried spirulina contains about 60% (51-71%) protein and all essential amino acids. It is rich in gamma-linolenic acid (GLA) and many other fatty acids. It also contains vitamins B1, B2, B3, B6, B9, A, C and E, as well as a host of minerals. Spirulina has a high chlorophyll content, making it an excellent detoxifier and alkaliser.
Wheatgrass is made from the common wheat plant seed leaf and can be grown indoors or outdoors. Wheatgrass is an excellent source of potassium, dietary fibre, vitamins A, C, K and B1, B2, B3, B6 and B5. It also contains iron, zinc and other minerals.
Wheatgrass is a complete protein source, delivering all nine essential amino acids. This protein is in the form of polypeptides (simpler and shorter chains of amino acids) that the body utilises more proficiently in the bloodstream and tissues.


Meal fatigue refers to becoming tired/bored of consuming one food/type of meal over and over again. A good example is a female wanting to lose weight and gain lean muscle and therefore only consuming baked chicken breast and steamed broccoli. Soon enough, she becomes tired of that one meal repeatedly, and craves a larger variety of flavours, textures and smells.
As a nutrition coach, it is essential to keep the impacts of meal fatigue in mind. To achieve this, a nutrition coach can ensure that the meals are well-varied, with an abundant choice of flavours, meats, vegetables and cooking methods. It is important to work with the client to identify which meals they find ‘boring’ and which sort of meals excite them. Adopting a collective approach, one that is client-focused, can ultimately improve the client’s adherence to following the nutritional plan or dietary strategies.
When writing a meal plan, the following factors are worth considering as a nutrition coach:
TEMPERATURE

Ensure there are at least two to three different textures on the plate. Various textures may include smooth mashed potato, crunchy lettuce, crispy bacon or chunky guacamole.
Use a wide variety of cuisines to draw flavour inspiration from. High flavour ingredients generally include herbs, spices, broths, creams and tomatoes. Vary the flavour combination from one meal to the next to avoid meal fatigue.
Even if a client says they enjoy Mexican, if they were to have Mexican three times a day until their next consultation, they might get sick of it.
Consider the time of year and the temperature of the food being suggested. If it is hot outside, a client may prefer colder food items such as salads and wraps; and vice versa, if it is cold outside, a client may prefer warmer food items such as stews and soups.
A combination of temperatures is also a good idea; for example, a burrito bowl generally has warm beans, cold salad and cold dressings such as sour cream. On the other hand, a soup may be hot liquid with a dollop of cold cream or a warm bread roll.
As smell is one of the five senses, it is important to consider this when creating a meal plan. The smell of the food can excite a client or completely turn them off the food. If the food smells delicious, they are much more likely to try it and enjoy it, whereas if the smell is off-putting, they may try the food with decreased expectations and a negative mindset.
When creating a nutritional plan for a client, it is fundamental that a nutrition coach takes into account the client’s food likes and dislikes. Likes and dislikes should be discussed in an initial consultation with the client and can be further discussed and updated in follow-ups.
When creating a nutritional plan, if the client does not enjoy certain foods which have been recommended, it is unlikely that they will follow the plan. If clients do not enjoy the foods in their nutritional plan, they are more likely to make their own adjustments and changes, resulting in nutritional inadequacies and impacting their overall health or goals.
When creating a nutritional plan for a client, it is fundamental that a nutrition coach takes into account the client’s food likes and dislikes. Likes and dislikes should be discussed in an initial consultation with the client and can be further discussed and updated in follow-ups.
When creating a nutritional plan, if the client does not enjoy certain foods which have been recommended, it is unlikely that they will follow the plan. If clients do not enjoy the foods in their nutritional plan, they are more likely to make their own adjustments and changes, resulting in nutritional inadequacies and impacting their overall health or goals.
A client may dislike certain foods based on their:
• Texture
• Colour
• Flavour
• After taste
• Mouthfeel
• Appearance.


In addition to the above, they may also dislike foods due to intolerances, allergies, ethical viewpoints (such as animal cruelty) or religious beliefs. Knowing why a client may dislike a certain food will help guide alternative recommendations.
For example, there is little point in suggesting bacon if the client avoids pork for religious reasons. A more appropriate alternative may be beef, chicken or fish. Another example could be a client dislikes sweet potato simply because of the taste. In this case, nutrition coaches could recommend various sweet potato recipes which hide the taste or select an alternative vegetable such as pumpkin or white potatoes.

On the other hand, particular foods the client enjoys should be used as much as possible in creating a nutritional plan. If the food they particularly enjoy is not necessarily great for their health or specific goals, a strategy that a nutrition coach could utilise with their client is to try alternative options of preparing the food at home or save the food for days when the client may have a scheduled break (i.e. one or twice a week, or on weekends).
For example, a client may particularly enjoy pork belly, therefore, one meal each week could contain pork belly, with a variety of recipes provided for cooking. Another example may be that the client particularly enjoys sweet and sour noodles from their local Chinese takeaway; as this is high in sodium, trans fats and sugars, it may be beneficial to provide some recipes for cooking the same recipe at home. This will ensure that the client can control the type of fat used and the amount of sugar and salt added.
While the ideal world would prefer clients who enjoy all foods, the reality is that food likes and dislikes need to be considered to improve the likelihood of them adhering to nutritional recommendations. Nutrition coaches should work with their clients to gain an in-depth understanding of food likes and dislikes and why they have particular likes and dislikes. By doing so, they can work collaboratively with the client to formulate a nutritional plan that is not only sustainable but will be enjoyed by the client.

The term ‘organic’ refers to produce and other ingredients grown without pesticides, synthetic fertilisers, genetically modified organisms, radiation treatment or sewage sludge. Animal products (such as meat, eggs and dairy) that are certified organic have been raised without antibiotics or growth hormones.
There are strict regulations around labelling a product as organic:
• A product can only be labelled as ‘100% organic’ if 100% of its ingredients are certified organic (except water and salt)
• Foods can be labelled as ‘Certified Organic’ if 95% or more of their ingredients are certified organic
• Where less than 95% but more than 70% of ingredients are certified organic, the food label may say ‘made with x% organic ingredients’.
Products labelled as organic generally attract a premium price compared to those produced using artificial fertiliser, chemicals or pesticides and non-essential food additives or processing aids. Businesses that make organic claims must be able to substantiate those claims.
Organic product standards:(129)
There is a voluntary Australian standard for growers and manufacturers wishing to label their products ‘organic’ and ‘biodynamic’ (AS 6000–2009). This standard is a useful reference point when determining whether a product is organic.
‘Certified’ products:(129)
Many products carry a symbol, logo or other trademarks to show that they are certified organic. Various private bodies provide this certification, and the minimum standards required to obtain certification may vary. A business that labels its product as certified organic must ensure that the product is certified. If a business claims to meet a particular standard, it must ensure that this claim is true. All organic claims, whether they reference a standard or not, should be able to be

The presence of chemicals and preservatives in food can impact the body and mind. It is generally accepted that organic foods taste better and contain a higher proportion of natural nutrients than non-organic foods.
In addition to this, additional benefits of organic foods include:
• Organic food contains no pesticides
• Organic food is fresher and free from preservatives
• Organic animal produce is free from antibiotics and hormones
• Organic meat and milk contain higher amounts of nutrients
• Organic food is GMO-free.
Australian Certified Organic (ACO) is Australia’s largest certifier for organic and biodynamic produce and has over 1,500 operators within its certification system. This logo helps consumers identify which products are Australian Certified Organic products. There is a review process that companies and food products must adhere to to use this logo on their products.

Detoxification is the ‘process of removing toxic substances from both endogenous and exogenous origin’ which may accumulate as a result of:(130)
• Industrial chemicals
• Pesticides
• Heavy metals
• Xenobiotics
• Radioactive elements.
These substances have carcinogenic, epigenetic, endocrine-disrupting, digestive, and immune-altering actions.(131)
The liver, an important organ weighing approximately 1.4kg, is responsible for eliminating toxic materials from the body through the mobilisation, biotransformation and conversion into more water-soluble metabolites, which are then excreted via the urine.(132)
Benefits of detoxification include:
• Improved energy
• Improved pH balance
• Skin health
• Weight loss
• Decreased inflammation.
Phase I: Involves the oxidation, reduction and hydrolysis
Phase II: The conjugation of functional groups for elimination.(37)
One way to detox is to make acute and significant changes to the diet. Generally, this would involve dietary changes, whereby only unprocessed foods are consumed. Often, these unprocessed foods are juiced to make them easier to consume and more micronutrient-dense. For example, someone could consume five celery stalks, one avocado, three cups of spinach, two beetroots and one grapefruit in one juice but would likely struggle to consume these items in their whole forms as the fibre would be too filling.
There are various detoxification methods, from complete fasting and clean eating to chelation therapy. The type of detoxification which may work for one person may not work for another, as it is dependent on the toxin from which a particular client is detoxing. Many commercial ‘detoxifications’ are simply a clean eating approach, which a person should be aiming for anyway.


In short, no. The human body has an extremely complex detoxification system to complete the detoxification on its own. Detoxification, as described above, is completed by the liver and toxins are excreted through the kidneys and passed out as urine. However, with all the additional toxins polluting food (herbicides, pesticides, heavy metals), the air (pollution) and the chemicals in a standard home (detergents, shampoos, soaps and lotions),(132) there is a potential argument that detoxification once or twice a year can be beneficial.
Detox can be as simple as eating only whole foods for a couple of weeks or as complex as fasting, juicing, supplementation, colonics, chelation and gut support. Deciding what sort of detox, if any, would be beneficial depends on the lifestyle a client leads. For example, someone who consumes only organic fruit and vegetables, grass-fed, organic meat and does not consume processed food may not need to detox, as the liver would be unlikely to be stressed. However, a miner constantly exposed to chemicals in the workplace and is only given processed foods and lots of tuna (containing mercury) may suffer heavy metal toxicity and therefore benefit from chelation detoxification.(130)(133)
Detoxifications are personal, just like nutrition. There is no one-size-fits-all approach. When determining whether someone needs to detoxify, it is important to consider their lifestyle, food intake and household chemical and pollutant exposure.

As a nutritional advisor, it is important to help clients understand the role and indications of a detoxification diet. For most individuals, unless clinically indicated (e.g. a client with chronic heavy metal toxicity), detoxification is not indicated, and simple strategies to help guide clients towards healthy eating patterns are all that are required. Individuals who may require a detoxification protocol generally have chronic medical conditions and therefore fall outside the scope of a nutritional advisor.
While detox diets promote the intake of nutrient-dense foods, like fruit and vegetables, and removal of energy-dense foods, like fast food and takeaways, this can also be achieved through the adoption of simple habits and practices, without the need for extreme measures. Helping clients improve their relationship with energy-dense foods is as important as improving their relationship with nutrient-dense foods. As a nutritional advisor, it is important to educate clients on the benefits of these health strategies and work with them to adopt healthier eating patterns.

Nutrition coaches will encounter many clients seeking weight loss who have attempted to lose body fat unsuccessfully. While intentional dieting to lose body fat is successful for some people, many do not reach their desired weight or regain the weight they lost. This is because dieting is physiologically and psychologically hard to maintain for some people, while others find the process easy. For those who struggle with weight loss or fear weight regain, it is important to program in diet breaks and reverse dieting patterns, as this can make the process easier.
A diet break is simply a break of 1-2 weeks (can be longer) where the client increases their energy intake up to their predicted maintenance energy requirements. This gives the body a break from being in an energy deficit and gives the client a psychological break from dieting by providing more energy, more variety and more volume in their diet. This can help increase adherence to deficit periods and reduce the likelihood of binge eating, under-reporting or low mood/energy.
A diet break could be incorporated every 8-12 weeks in a diet cycle, provided weight loss has occurred. It is necessary to recalculate the client’s EEI based on their current weight, not their starting weight (as this would estimate a higher EEI than their new, lower bodyweight).
Diet breaks can help keep clients motivated on their long-term goal weight, especially if they have a lot to lose.
Reverse dieting is most closely associated with bodybuilding clients, where energy deficits have been profound and sustained for a long time in the build-up to a competition. Reverse dieting is used because of the deep dietary restrictions that bodybuilders often place on themselves and the physiological and psychological effect that returning to normal eating can have (as there is often a fear of gaining body fat too quickly).
Reverse dieting can also be applied with non-athletic clients, especially those who worry about rapid weight gain after a fat loss phase.
Reverse dieting can be completed in two ways:
• Immediate return to maintenance energy requirement, or
• Slow return to maintenance energy requirements.
An immediate return to maintenance energy intake is desirable because it can stop the negative impacts of dieting – hunger, low energy, and poor mood. It is also desirable because it increases the variety and volume of food an individual can consume. Depending on the size of the energy deficit the individual was in, this could be a substantial increase in energy and food intake. Therefore, the decision to return immediately to maintenance energy intake needs to be discussed with the client and the pros and cons considered.
A slow return to maintenance energy intake may be desirable for an individual with a deep and sustained energy deficit. It may also be desirable for individuals with very low body fat percentages who are concerned about losing their physique. It will enable them to return to normal eating while giving them confidence that they will not gain fat mass quickly. A slow return to maintenance energy intake is completely individual and would need to be designed with client input. A simple method may be to add 800-1,200kJ) per week until maintenance is achieved over a few weeks.
There are no hard and fast rules with diet breaks and reverse dieting; however, they may be beneficial for clients who struggle with long-term dieting, those who wish to achieve very low body fat levels, those who have yo-yo dieted in the past or those who express reluctance to stop dieting for fear of regaining body fat. Nutrition coaches should educate their clients about these techniques early on, as they are a useful tool to ensure success and client adherence.


Nutrition coaches need to be aware of the impacts of non-dietary factors on a client’s progress. Recognising nondietary factors when designing nutritional plans or dietary strategies for clients allows a nutrition coach to be more accommodating to a client’s individual preferences and, in turn, improve client progress and adherence.
As discussed throughout this resource, a multitude of factors can impact on the client’s success when following a suggested dietary approach or nutritional plan.
Examples of non-dietary factors are provided in the list below (this is not an exhaustive list):
• The NEAT principle
• Food measurements
• Decreasing kilojoules vs increasing physical activity for weight loss
• Social, cultural and behavioural influences
• Appetite and exercise
• Understanding diet therapy
• Online calculators
• Food safety practices.
The above considerations are discussed in greater detail on the following pages.


‘Non-exercise activity thermogenesis (NEAT) is the energy expended for everything that is not sleeping, eating or sportslike exercise. It ranges from the energy expended walking to work, typing, performing yard work, undertaking agricultural tasks and fidgeting. Even trivial physical activities increase metabolic rate substantially and it is the cumulative impact of a multitude of exothermic (energy releasing) actions that culminate in an individual’s daily NEAT. It is therefore not surprising that NEAT explains a vast majority of an individual’s non-resting energy needs.’(134)
While NEAT might not seem like a great amount, it can considerably impact metabolic rate and energy expenditure. The amount of kilojoules NEAT burns can vary from client to client.
A study in 2014 found that the amount of kilojoules burned from NEAT varies by up to 8,370kJ a day between two individuals of a similar size. Several factors can account for this difference, including environment and genetics. An individual’s career and lifestyle can also impact NEAT, as two people with the same BMI but different jobs (one sedentary vs the other active) will likely burn different amounts.
BMR + TEF + NEAT + EAT = Daily Energy Requirement
BMR or RMR (approximately 60-70%) NEAT (approximately 10-15%) EAT (approximately 20-30%) TEF (approximately 10-15%)
An individual’s Basal Metabolic Rate (BMR), the Thermic Effect of the Foods (TEF) a client eats, NEAT and Exerciserelated Activity Thermogenesis (EAT) make up an individual’s energy requirements for each day.

The components of energy expenditure are further explained in the table below:
BMR, OR RESTING METABOLIC RATE (RMR)
THERMIC EFFECT OF FOOD (TEF)
BMR/RMR is the energy requirement of the body without any activity. BMR/ RMR accounts for approximately 60-70% of an individual's daily energy requirements.
TEF is the amount of energy needed to digest food. It accounts for about 10-15% of an individual’s energy requirements. The rest of their energy requirements are dependent on how active they are in both intentional exercise, known as activity thermogenesis, and NEAT activities. NEAT
NEAT is any activity that is not a ‘planned exercise’ (such as fidgeting, walking, standing up, carrying something etc.). This can account for as little as 10% of energy expenditure in the very sedentary and up to 50% in very active individuals.
EXERCISE-RELATED ACTIVITY THERMOGENESIS (EAT)
EAT is the energy required for planned exercise. Exercise-related Activity Thermogenesis (EAT) is highly variable among individuals, and the type of training, as well as its intensity and duration, will result in different amounts of energy being used in different sessions or between different individuals.
If a male has a BMR of around 8,455 kilojoules, he could burn about 627 kilojoules digesting the food he eats daily. He may also burn anywhere from 627-2092 kilojoules more per day, depending on whether he has a full day of walking around, cleaning, or spending the entire day sitting and working on the computer.
NEAT is considered a contributing factor in how bodies can manage or maintain weight. If a client gains weight, NEAT tends to rise; whereas when a client loses weight, NEAT often plummets, and individuals end up sitting more without moving. As NEAT researcher James Levine stated, ‘we may come to appreciate that spontaneous physical activity is not spontaneous at all, but carefully programmed’.


There are several ways NEAT can be incorporated into life. This can be done at work, at home, and at school. Some examples include:
• Standing at a desk instead of sitting at work
• Using a stability ball instead of, or in addition to, a chair
• Using the stairs instead of the elevator at work
• Making it a habit to regularly stretch, even for just 5 minutes a couple of times per day.
According to the National Academy of Sports Medicine, a 65kg client can expect to burn approximately 426 kilojoules an hour while sitting at work. If that client stood while working, they would burn 728 kilojoules.(65) An extra 426 kilojoules might not seem like a lot, but it can add up over a week/months/years. Another example could include finding small ways to move while waiting in line or sitting while stuck in traffic. It may not burn as many kilojoules as jogging, but even tapping feet or bobbing the head helps increase NEAT.
Being mindful of making choices to be more active and get moving can increase NEAT. For example, when grocery shopping, carrying a basket instead of using a trolley or taking the stairs instead of the elevator/escalator.
If a client’s job requires them to sit at a desk all day, advise them to take breaks and stand when they work. If they can, this includes when they are on the phone or during a staff meeting. When clients are standing, they are working more muscles than they would if they were sitting, which creates more exercise on the body.


Clarifying measurements when writing the nutritional plan is important to avoid confusion or miscommunication.
TIP: Ensuring the client has a clear understanding of food measurements when completing their food diary will help improve their accuracy and therefore, the result of their dietary analysis.
When it comes to measurements, there are various methods to utilise. Some clients find one way easier than another, or they may like to use a combination of the different approaches. These approaches include cup and spoon measures, weight and physical measures (e.g. fists, thumb, palm, etc.).
Show the client a physical example of a cup, a spoon and a teaspoon. Ask them to purchase these for home if they do not already have any. As there are many different ways of abbreviating measurements, make sure to be upfront and clear with the client to avoid confusion.
Measurements are commonly written as:
• Cup - C (1C = 250ml)
• Tablespoon - tbsp (1 tbsp = 15ml)
• Teaspoon - tsp (1 tsp = 5ml)
• Grams - g
• Kilograms - kg.
CUP MEASURES
SPOON MEASURES

A cup measure is suitable for liquid items such as milk, water and juice, and smaller items such as quinoa, couscous, rice, oats and soup. The client can either measure the item out or use an estimate of how much is consumed with the knowledge of what 1 cup looks like.
Example:
The client may have consumed not quite 1 cup of water; however, they are certain it was more than half. They may then estimate this to be ¾ cup of water.
Spoon measures are ideal for measuring small items which are consumed in relatively small quantities such as sugars, honey, syrup, sauerkraut, seeds, butter and oils. Spoon measures include both tablespoons and teaspoons. If the client is struggling to take too much information on board, only show the tablespoon, and explain that 1 teaspoon is simplystruggles to take too much information on board, only show the tablespoon, and explain that 1 teaspoon is ¼ of a tablespoon.
Example:
The client may use 1 tbsp of pumpkin and sunflower seeds on their salad.

Weight measurements are the most accurate way to measure food. Food is to be measured in its raw state as opposed to cooked. Explain to the client the different types of weight measurements and which type is preferred (imperial or metric). Clients can be shown life-size photographs of what different weights of common foods may look like, or food models may be used instead.
It can be helpful to encourage the client to weigh their food in the first few days to get a feel for what different measurements look like. After this, they may like to either continue weighing their food or may simply make educated estimates of the food’s weight.

Physical measurements refer to measurements mainly using the hands as a guide. While this method is the most inaccurate, it is less time-consuming and quicker to complete.
As each client’s hand is a different size, it is encouraged that the nutrition coach look at their hand and suggest how many ‘cups’ would fit into their fist and how many grams of food their palm, thumb and cupped hand would be. This way, the client can simply place their hand next to their food and make a quick analysis in regards to the quantity they are consuming.
Usually:
• The palm is used to determine protein serve sizes. It is generally recommended that red meat should fit in the palm, poultry fit in the palm and up to the first knuckle, and fish fit in the entire hand.
• The clenched fist determines vegetable portions, with 1 fist being approximately 1 portion.
• The cupped hand determines carbohydrates such as potato, quinoa and oats. It is important to show the client how to cup their hands, as some may make small cups while others may make huge cups, which can provide inaccuracy in the analysis.
• The thumb length is generally a good indicator of fat intake such as butter, lard and ghee. Some also measure cheese using their thumb as the baseline measure.
Use this “handy” chart to visualize approximately sized portions for meals, snacks and recipes (examples are provided for each corresponding measurement).

This question is a bit like what came first, the chicken or the egg? Regarding weight loss, it is generally up to the client to decide which they would prefer to work on first; however, it is important as a nutrition coach always to encourage safe and effective nutritional strategies.
First and foremost, it is important to note that when a client seeks weight loss, they are seeking fat loss.
Weight loss includes loss of muscle and body fat, which is undesirable because muscle is significant to maintain for the following reasons:
• Metabolism
• Physical ability (functional capacity and strength)
• Long-term health.
Therefore, when a client seeks help for weight loss nutrition coaches are looking to support the loss of body fat while retaining muscle mass (or lean muscle).
Since the energy in vs. energy out equation is two-sided, clients can be encouraged to use three approaches to fat loss:
• Reduce energy intake
• Increase energy expenditure
• Complete both at the same time.
Helping clients decide which approach is best for them will be determined by their motivation to change their lifestyle, eating habits and overall goals.
For example:
• If a client is extremely overweight or presents with health complications that make exercise hard, contraindicated or not yet within their capability, then reducing energy intake will be the main strategy.
• If a client is time-poor, then the nutrition coach can work with them to focus on nutrition, increasing their NEAT and work toward introducing exercise through methods like scheduling.
• Another client who may struggle with emotional eating and is not yet ready to make dietary changes could be encouraged to focus on exercise and their ‘happy hormones’ first, thus increasing energy out and producing fat loss.

Nutrition coaches should help the client identify which area would provide better results more efficiently. However, the goal is to ensure exercise and diet align with health recommendations.
Encouraging clients to participate in a resistance training program while dieting to lose body fat will help them maintain and potentially increase their muscle mass, which will provide several benefits:
• Maintenance or improvement in metabolism
• The faster appearance of ‘toning’ (muscle gain/fat loss)
• Increased confidence
• Maintenance of or improved posture and functional capacity.
While physical exercise benefits clients who are dieting, diet plays the most important role in reducing body fat. Clients may exceed the Australian Guidelines for Physical Activity yet still struggle with abdominal adiposity (fat distributed around the stomach) secondary to a poor diet. And while it is recognised that diet (energy deficit) is the key to fat loss and resistance training is the key to muscle maintenance, health is not about one part being more important than the other but instead achieving a sustainable balance of exercise and nutrition.
A nutrition coach’s role is to educate, inspire and motivate change, but ultimately, only the client can make the alterations necessary to change their body/mind, etc.
It is also important to remember that clients should be exercising for health and fitness first and for energy expenditure second. A wealth of scientific research demonstrates that exercising for fat loss in the absence of dietary change or support is not as effective as changing dietary habits or combining dietary change with exercise.(135) With this being the case, and with exercise energy expenditure being difficult to calculate accurately, it can be beneficial to ensure that clients do not include estimated energy usage from exercise in their overall daily total energy expenditure. This will help ensure that they create an adequate energy deficit required for fat loss.


Diet therapy simply refers to eating a specific way for a specific outcome. For example, limiting refined carbohydrates while losing weight or increasing vegetable consumption to provide additional fibre for more regular bowel motions.
As a general rule, healthy eating practices apply to all clients, and the use of a well-balanced diet will provide significant benefits across a spectrum of health and wellbeing. However, when considering specific diet therapies for a client, it is important to think about whether there are any contraindications that may be relevant.
A contraindication is a condition that makes a particular treatment or procedure inadvisable.(136) In effect, contraindication is when a particular type of diet would negatively impact a client’s condition. As an example, consider the fasting approach to weight management. Conditions where fasting may have a negative impact and accordingly be inadvisable include pregnancy, with low blood pressure and with diabetes.
It is essential that a nutrition coach conducts pre-screening processes to capture any pre-existing medical conditions and that these are factored into any decision determining a dietary recommendation.
‘Contraindication’ refers to a sign that someone should not continue with a particular medicine or treatment because it is or might be harmful.(136) In other words, contraindications are known as particular conditions that a client presents with, which may be aggravated if a nutrition coach provides nutritional support or individualised nutritional plans. If a client presents with an absolute contraindication, then a referral must be made to a more suitable medical or health professional.
Contraindication is the opposite to ‘indicated’, when something is either advisable or necessary. For example, a client with no medical conditions or contraindications (and is deemed ‘healthy’ during screening processes) may seek to employ a nutrition coach to create an individualised nutritional plan to help them maintain a healthy weight. This is considered an ‘indication’ of nutritional support, as it is a valid reason for a nutrition coach to begin supporting the client and their nutritional goals.


All humans, regardless of age, religion, financial status or gender, require appropriate nutrition. There are no individuals who would not benefit from improved nutrition. In saying this, each case requires its consideration. For example, the diet therapy recommended to a pregnant woman would differ from that given to a triathlete.
While diet therapy benefits every single client, there are a few limitations that need to be considered:
• Client compliance or adherence to recommended nutritional plan.
• If the client is not prepared to commit to the plan, there will most likely be minimal to no changes
• Client finances/budget for ongoing nutritional consultations to monitor/evaluate/support.
• This may prevent the client from beginning in the first place, as they may not see the need to if they cannot continue
• Food security in impoverished areas.
• If the client cannot access the food items you are recommending (fresh fruit and vegetables), they may not be able to follow the plan you are recommending entirely
• Religious dietary restrictions.
• This may reduce the types of food the nutritional advisor can recommend, and the client may feel their restrictions are too much for the nutritional advisor to work with, therefore reducing appointments
• Variations in circumstances and lifestyle factors.
• The client could have long work hours, be a busy mum or have limited spare time, making it difficult to find the availability to book a consultation.
Identifying a client’s previous failed attempts will allow a greater understanding for the nutrition coach in terms of what barriers to change the client may have, their limitations to the treatment and where they may need additional support to ensure that the client has the best chance at success.


‘Health Knowledge’ is an organisation developed to support public and multidisciplinary health specialists in providing nutritional advice and support to clients. Within their public health textbook, they have identified six health and social behaviour determinants that may impact diet therapy’s success with a client.
The determinants identified are:(137)
1. Biological determinants such as hunger, appetite, and taste
2. Economic determinants such as cost and income
3. Physical determinants such as access, education, skills and time
4. Social determinants such as class, culture, and social context
5. Psychological determinants such as mood, stress and guilt
6. Attitudes, beliefs and knowledge about food.
As a simple example of how these determinants may impact a nutritional plan, time constraints are included as a physical determinant. Clients who are time-poor are less likely to maintain a nutrition/diet plan due to the potential increased time requirements to prepare nutritious meals and the ready availability of fast food alternatives.
Similarly, psychological determinants such as stress can significantly impact a client’s meal selections and portion sizes, with individuals over or under eating based on their individual responses to stress. Furthermore, individuals are less likely to select nutritious meal choices during periods of high stress, leading to challenges in adhering to meal plans.
For a more detailed overview of how social and behavioural influences impact a client’s diet choices and nutrition plan, nutrition coaches can visit the ‘Health Knowledge’ website by CLICK HERE


There can be some confusion regarding exercise, weight loss and hunger. While exercise is known to aid in weight loss, it is also associated with increased hunger; this combination can appear counterproductive. So while exercise can increase energy out, it can also stimulate the need for energy in.
Through moderate-high intensity exercise, body temperature is increased due to burning energy. When body temperature is raised, immediate hunger signals decrease. When the body cools back down, the hunger hormone ghrelin is released as the body seeks to replace the energy lost by stimulating appetite. This is suggested to be why a client may not feel hungry immediately after exercise (when body temperature is increased) but ravenous 30-60 minutes later.
In addition, exercise, especially resistance weight training and high-intensity interval training results in an increased metabolic rate for 24-48 hours after a training session. This increased metabolic rate means that energy consumed in the post-exercise period will be used more efficiently as the body seeks to recover glycogen stores and repair muscle and tissues damaged during exercise.
Additionally, by building muscle, individuals increase their metabolism due to muscle’s higher metabolic requirements. Therefore, individuals who exercise often have a higher metabolic rate than sedentary individuals, meaning they have a higher energy requirement and may be less prone to unintentional weight gain. To illustrate this, an 80kg sedentary male with 30% body fat will have a lower RMR than an 80kg active male with 15% body fat. This is because muscle requires more energy for maintenance, and the man with the lower body fat percentage exercises regularly.
Whether exercise results in compensatory physiological or behavioural mechanisms to replace lost energy has been studied extensively; however conclusions are mixed. It appears that women are more likely to replace energy after exercise than men.(138)(139)


Nutrition coaches may offer services to their clients that involve the direct handling and production of food products, and as such, it is good practice to be aware of food safety practices. Australian businesses and food handlers are subject to food safety standards, which obligate them to produce safe and suitable food for consumption.
Food Standards Australia and New Zealand (FSANZ) contain health and hygiene obligations that aim to reduce the incidence of foodborne illnesses and include five standards:(140)
1. Interpretation and Application
2. Food Safety Programs
3. Food Safety Practices and General Requirements
4. Food Premises and Equipment
5. Food Safety Programs for Food Service to Vulnerable Persons.

Food safety standards place obligations on Australian food businesses to produce food that is safe and suitable to eat. A food business is any business or activity that involves handling any type of food for sale or the sale of food in Australia. The standards, which also contain health and hygiene obligations for food handlers, aim to lower the incidence of food-borne illness.
To view the full standards, CLICK HERE to view the link.
It is important that nutrition coaches acquire the skills and understanding of safe food handling and storing so they can pass these skills on to their clients where needed. Food handling is not innate, and knowledge of these skills is dependent on family and cultural practices. It is common for people from different countries and cultures to adopt very different food safety practices in comparison to those used in Australia. While those practices may be suitable for some foods or some climates, they may not be suitable in the hot climate of many places in Australia.
The four main areas of knowledge required for safe food handling and storage are listed below:
1. Cleanliness
2. Separation
3. Cooking
4. Chilling/refrigeration.


The previously mentioned factors are discussed in more detail in the following table:
• Clients must be encouraged to wash their hands before they start handling and preparing food. This reduces the risk of contaminating food with bacteria that could cause food poisoning.
• Washing hands thoroughly with warm, soapy water and drying them before and between handling food is good practice.
• Nutrition coaches can also encourage clients to ensure they clean cooking utensils before cooking, including wiping down kitchen surfaces such as benches and hot plates.
• These practices should also be adopted between handling different foods such as raw meat, chicken and fresh vegetables to reduce the risk of contaminating food that may be cooked differently (or not cooked), such as salads.
• Different types of food must be separated for storage and preparation.
• Raw meat, poultry, seafood and eggs should be kept separate from other foods like fruits and vegetables, especially salads that will not be cooked.
• Nutrition coaches can encourage clients to ensure that ready-to-eat foods are not placed on surfaces that raw meat, poultry, seafood or eggs have been on.
• Different foods need to be cooked to different internal temperatures to ensure that they are fully cooked through and to reduce the risk of bacteria remaining active in them.
• While some meats like steak, pork and lamb can be eaten without needing to be fully cooked, most meats (i.e. chicken, ground meats) should be cooked thoroughly before eating. Similarly, tuna and salmon can generally be served rare but it is safest to ensure that all fish is cooked thoroughly before eating.
• Additionally, bacteria grow best and fastest between 5°C and 60°C. Thus, food should be warmed to around 70°c for 2 minutes to ensure bacteria are killed before eating, especially when reheating leftovers.(141)
• The table below shows different types of food and the internal temperature they need to reach to ensure their safety for consumption.
Beef, pork, veal, lamb 63°C
Ground meat 71°C
Ham (uncooked, fresh or smoked) 63°C
Ham (cooked, to reheat) 60°C
Poultry 74°C
Egg dishes 71°C
With a 3 minute rest.
With a 3 minute rest.
CHILLING/ REFRIGERATION
Fish 63°C Or, flesh is opaque and separates easily with a fork.
Leftovers / casseroles 74°C
• Refrigerators should be set to 4°C and freezers set to -18°C.
• Fresh foods like meat, poultry, eggs, seafood and perishables like fruit, and vegetables should be refrigerated within 2 hours of purchasing.
• Frozen food should be thawed in the fridge, in cold water or in the microwave, never at room temperature.
• Foods that are thawed in the microwave should be cooked immediately.
• Foods that are being marinated should be left in the fridge, not at room temperature. Once the food is cooked, it should be cooled within 2 hours to ensure it chills below 5°c to reduce the growth of bacteria.


During an initial consultation, it is important to establish a client’s desired outcomes and goals. The client’s goals are an extremely powerful motivator to ensure the client remains focused. This information is critical to developing a nutritional plan, and care must be taken to structure recommendations effectively to achieve success.
When discussing these outcomes with the client, it is important to approach via open-ended questions, as multiple, unintended desires may emerge during the discussion. These could be more defined/realistic outcomes that are achievable in the time frame given; they may also extend onto the original goals/outcomes if the original ones are not powerful or detailed enough.
Individuals have a wide range of potential reasons for wanting to receive nutritional advice, nutritional plans and support.
Some potential reasons include:
• To increase or decrease weight
• To modify body shape or appearance
• To increase strength, endurance or performance
• To address health concerns (such as fatigue, stress or immunity)
• To improve lifestyle and enhance general health and wellbeing.
Once the desired outcomes are articulated, they should be captured as SMART goals (Specific, Measurable, Attainable, Realistic and Timebound) to provide a genuine end state that clients can pursue. Although goal setting and the importance of SMART goals have been discussed in previous units throughout this course, it is important to recap these factors as a nutrition coach, for continued progress and development of knowledge.


When assisting clients in setting goals, it is beneficial to help them set what are commonly referred to as SMART goals. SMART goals are Specific, Measurable, Attainable/Achievable, Relevant/Realistic and Timebound.
G O A L S
WHAT DO YOU WANT TO DO?
HOW WILL YOU KNOW WHEN YOU’VE REACHED IT?
IS IT IN YOUR POWER TO ACCOMPLISH IT?
CAN YOU REALISTICALLY ACHIEVE IT?
WHEN EXACTLY DO YOU WANT TO ACCOMPLISH IT?
Setting goals using the SMART principle enables clients to be completely sure of what needs to be done to reach their long-term goals. Furthermore, clients can create shorter, medium and longer-term goals using the SMART method.
SMART GOAL/S MAY BE:
‘To lose 5kg of weight within the next 4 months’.
For the client to lose weight, they may have multiple strategies in place, such as decreasing processed foods and increasing vegetable intake, exercising more and practising mindful eating. The client may therefore have set goals around each of these areas. In regards to vegetable consumption, the client’s SMART goal may look something like this:
‘Within the next 4 weeks, to be consuming 5 serves of vegetables (1 serve = 1 cup raw vegetables or ½ cup cooked vegetables) at least 5 days of every week, with at least 3 different types of vegetables each day’.

The following table examines SMART goals further, using the example of increasing vegetable intake to assist in weight loss.
Nutrition coaches should ensure they understand exactly what their client wants to achieve. The more specific the goal, the better the nutrition coach can structure the nutritional program to meet client expectations. They should ask their clients these questions so they can think more specifically about determining objectives and goals:
• What exactly do you want to accomplish?
• How do you want to accomplish this?
• Who do you want to accomplish this with?
• What limitations do you have?
• Why specifically do you want to reach this goal?
FOR EXAMPLE:
If the aim is to increase vegetable intake to assist in weight loss, the goal must specify how many serves of vegetables need to be consumed each day to reach the desired result. So, instead of simply saying ‘increase vegetable intake’, a specific goal would be to increase vegetable intake to 5 serves per day every day of the week.
Measurable goals mean determining what the vision for meeting the goal may look like and the ability to provide evidence that clients are meeting their goals or breaking the goal down into measurable elements. Measurable goals can be beneficial in refining exactly what it is that a client wants to achieve. Defining the physical proof (or evidence) of a client’s goal or objective makes it clearer, and easier for them to reach.
MEASURABLE
FOR EXAMPLE:
The number of serves of vegetables consumed can be counted; therefore, it is measurable. A weight loss goal could be measured using the measurements from scales or circumference measurements.
Can the client’s goal be reached? A nutrition coach will need to assist the client in determining if the goal is a realistic expectation. The client will need to consider the time and effort that will be required to meet their goal.
Another factor that needs to be considered for ‘attainable goals’ is if the goal is going to conflict with other priorities in life. If there are not enough resources or the goal conflicts with other priorities, the client can fail. It does not mean that the goal cannot be reached; however, the timeframe and the planning may need to be adjusted to make it realistic.
FOR EXAMPLE:
Is it achievable to consume 5 serves of vegetables per day? For some, this may be very easy, while for others, this may not be achievable, secondary to food security, allergies, major dislikes or time restraints. When creating a goal, it is important that the goal can be achieved, to ensure the client does not become disheartened part way through.
Is this goal relevant to the client? Is it realistic?
This can be determined by asking the client the following questions:
• Why do you want to accomplish this goal?
• What is the primary objective of reaching this goal?
• Will meeting this goal provide you with what you are looking for?
FOR EXAMPLE:
Consuming the 5 serves of vegetables per day is realistic for an average client. However, setting a goal to lose 10kg in 2 weeks is not as realistic. The goal must be achievable without causing harm. A personal goal should be relevant and realistic to avoid disappointment and unnecessary setbacks.
Put a time limit on the goal.
It is natural for people to procrastinate when there is no deadline set. If the client’s goal is to lose 10kg, is that in 12 weeks or 6 months? Clients must be set up for success by being encouraged to create achievable time-bound goals. If deadlines are not set, some goals may never be achieved, which can be disheartening for the client. By providing a timeframe of when to accomplish goals, the client will be more likely to increase their motivation to meet these goals.
Can the client’s goal be reached? A nutrition coach will need to assist the client in determining if the goal is a realistic expectation. The client will need to consider the time and effort that will be required to meet their goal.


The following example meal plans have been provided to show how an individual meal plan might be created to suit a client’s individual goals. The example meal plans on the following pages display a visual representation of how to design a healthy meal plan for a client.
In addition to this, the following meal plans also provide examples of how a nutrition coach can:
• Calculate macronutrient and energy requirements for specific scenarios
• Calculate the estimated energy from each macronutrient against total energy to help a client achieve a specific goal.
These examples combine elements of the current and previous units of the 11046NAT - Certificate IV in Nutrition, to produce realistic examples of how to help arrange a client’s dietary intake using the evidence provided throughout the course. While ranges for elements like protein and energy have been used from the resources provided, it must be remembered that tailoring individual nutritional plans for clients is open to interpretation and change based on client feedback, progress, evidence-based research and ongoing learning.


Sophie is a 55-year-old female seeking advice on weight loss. She has light activity in her work as a laboratory assistant and exercises at a light-moderate intensity for 30 minutes, 2 days each week. She currently weighs 90kg, is 170cm tall, and would like to focus on slow and steady weight loss. She has trialled many programs in the past but never anything personalised. She enjoys a hot breakfast, dislikes mushrooms and has no allergies or other dietary restrictions. As her downfall is mindless eating (while watching TV or working at her computer), she has suggested regular meals throughout the day may work best for her.
STEP 1: Calculate BMR
Women: BMR = 2741 + (40.0 x W) + (7.74 x H) - (19.56 x A) kJ/day
BMR = 2,741 + (40 x 90) + (7.74 x 170) – (19.56 x 55)
BMR = 2,741 + (3,600) + (1,315.8) – (1,075.8)
BMR =7,656.8 – 1,075.8
BMR =6,581 kJ/day
STEP 2: Multiply BMR by PAL
EER = BMR x PAL
EER = 6,581 kJ x 1.6
EER = 10,530 kJ/day
Explanation: The physical activity level (PAL) of 1.6 has been selected because Sophie completes light activity throughout her workday, and only completes an additional 60 minutes of light-moderate intensity exercise per week. Even though she is participating in additional exercise, she is not exercising strenuously and will therefore stay in the level based on her occupation. Should she increase her exercise, her PAL will need to be adjusted.
STEP 3: Adjust EER for desired weight loss
Adjusted EER = EER - 2,000
Adjusted EER = 10,530 - 2,000
Adjusted EER = 8,530 kJ
Explanation: As slow and steady weight loss is desired, 2,000kJ is removed from the daily calculated EER to provide the daily adjusted EER, which will be used for all meal plan creations. This will allow Sophie a weight loss of ~500g per week.
EPR = 0.8-1.0 x W
EPR = 0.8-1.0 x 90
EPR = 72- 90g/ day
Explanation: Sophie exercises twice a week at a light-moderate intensity, so she requires 0.8-1.0g of protein for every kilogram of body weight. If she increases her intensity and frequency, she will require her EPR to be recalculated.

CARBOHYDRATES = 45-65% of EER
CARBOHYDRATES = EER x 0.45-0.65
CARBOHYDRATES = 8,530kJ x 0.45-0.65
CARBOHYDRATES = 3,838.5 - 5,544.5 ÷ 17kJ (1g carbohydrate = 17kJ)
CARBOHYDRATES = 226-326g/ day
Explanation: Sophie needs to stay within these recommended amounts to ensure she has enough energy throughout her day.
FATS = 20-35% of EER
FATS = EER x 0.20-0.35
FATS = 8,530kJ x 0.20-0.35
FATS = 1,706 – 2,985.5 ÷ 38kJ (1g fats = 38kJ)
FATS = 45-79g/ day
Explanation: Sophie needs to stay within these recommended amounts to ensure her body can function adequately and to keep her feeling full throughout the day.
For weight loss Sophie will be consuming fewer kilojoules than her usual intake; therefore, it is important to ensure protein, fat and/or fibre are contained in every meal to increase her satiety and satisfaction levels. Reminding Sophie the importance of hydration is also important, as thirst can often be mistaken for hunger.
MEAL 1:
As Sophie mentioned that she enjoys a hot breakfast, eggs were selected to be the base of her first meal of the day. Eggs are high in protein and contain good quality fats, which both help increase satiety. An omelette with cheese and tomato (excluding mushrooms, as Sophie says she does not like mushrooms) was then selected to bulk the eggs up. To increase her fibre content the omelette can be placed in a wrap.


MEAL 2:
Porridge has been selected, along with some fruit, yoghurt and granola, this well-rounded meal will provide a good amount of energy for the morning. Greek yoghurt was selected simply because it has high protein and fibre and is a good source of healthy fats. Full fat dairy products are selected due to their higher fat content (increased satiety and less sugar than low fat/reduced-fat products).
MEAL 3:
While a chicken pita wrap has been selected for Sophie’s third meal of the day, there is no reason that she could not replace the chicken with another source of protein such as beef, lamb or eggs. Before the afternoon hits, it is important to provide a source of fibre and protein to keep her full and decrease the likelihood of the ‘3 pm slump’. The chicken provides the protein, the veggies provide the fibre, and the avocado is an easy way to include fat.
MEAL 4:
As Sophie has mentioned, she enjoys snacking throughout the day. Something small like a banana is a great way to replace other foods usually associated with mindless eating (e.g. chips, lollies).

MEAL 5:
Sophie can use lamb roast or can easily replace it with another cut of meat or source of protein. Sweet potato is selected over white potato as it has a higher vitamin content and a slower release of sugar (lower GI). However, it is important to remind Sophie not to be afraid of white potato, as it is still a great source of carbohydrates.
MEAL 6:
Grapes are a quick and easy snack before the day ends, and because of the fibre in them, they will increase satiety and reduce the likelihood of late-night cravings.


ENERGY
PROTEIN
CARBOHYDRATES
FAT
FRUIT
VEGETABLES
FIBRE
FLUID

Sophie’s EER is 8,530kJ, including the energy deficit. This plan has approximately 8,848kJ; this isn’t too far from her EER. 500kJ on either side of the EER is sufficient.
Sophie’s EPR is 72-90g/ day. This meal plan has approximately 90g of protein. This falls within Sophie’s protein requirements, at the higher end of the range.
Sophie’s carbohydrate recommendations are 225-326g/day. This meal plan has approximately 253g of carbohydrates, this falls within her requirements.
Sophie’s fat recommendations are 45-79/day. This meal plan has approximately 70g of fats, this falls within her requirements.
3.5 serves of fruit are included in the meal plan. As fruit recommendations are at least 2 serves per day, Sophie is meeting her minimum fruit recommendations.
Approximately 6.5 serves of vegetables is in this meal plan. As it is recommended to consume a minimum of 5 serves of vegetables per day, Sophie has reached her minimum vegetable requirements.
There is 42g of fibre in this meal plan. It is recommended for women to have at least 25g of fibre a day. Sophie is meeting her minimum requirements.
It will be important to remind Sophie to drink a minimum of 2.1L fluid each day in addition to the above meal plan. And to increase her water intake during exercise/ on a hot day.
Jennifer is a 35-year-old female who is seeking advice on muscle gain. She currently weighs 55kg and is 170cm tall. She has light activity in her work as an assembly line worker and exercises at a moderate intensity for 45 minutes, 4 days each week. She has trialled many programs in the past but never had anything personalised. She enjoys a hot breakfast, dislikes capsicum and has no allergies or other dietary restrictions. As her downfall is skipping meals, she has suggested regular, scheduled meals throughout the day may work best for her.
STEP 1: Calculate BMR
Women: BMR = 2741 + (40.0 x W) + (7.74 x H) - (19.56 x A) kJ/day
BMR = 2,741 + (40 x 55) + (7.74 x 170) – (19.56 x 35)
BMR = 2,741 + (2,200) + (1,315.8) – (684.6)
BMR =7,656.8 – 1,075.8
BMR =5,572 kJ/day
STEP 2: Multiply BMR by PAL
EER = BMR x PAL
EER = 5,572 kJ x 1.8
EER = 10,030 kJ/day
Explanation: The physical activity level (PAL) of 1.8 has been selected. Jennifer completes light activity throughout her workday, making her fall into the PAL of 1.6; however, she also completes an additional 45 minutes of moderate intensity exercise 4 days a week, making her jump to the PAL of 1.8.
EPR = 1.0-1.5 x W
EPR = 1.0-1.5 x 55
EPR = 55- 82.5g/ day
Explanation: Jennifer exercises four times a week at a moderate intensity, so she requires 1.0-1.5g of protein for every kilogram of body weight. If she increases her intensity and frequency, she will require her EPR to be recalculated. Incorporating enough protein in her diet will help Jennifer reach her goal of gaining muscle mass.
CARBOHYDRATES = 45-65% of EER
CARBOHYDRATES = EER x 0.45-0.65
CARBOHYDRATES = 10,030kJ x 0.45-0.65
CARBOHYDRATES = 4,513.5 – 6,519.5 ÷ 17kJ (1g carbohydrate = 17kJ)
CARBOHYDRATES = 266-384g/ day
Explanation: Jennifer needs to stay within these recommended amounts to ensure she has enough energy throughout her day. Sufficient amounts of carbohydrates will help fuel her exercise too.

FATS = 20-35% of EER
FATS = EER x 0.20-0.35
FATS = 10,030kJ x 0.20-0.35
FATS = 2,006 – 3,510.5 ÷ 38kJ (1g fats = 38kJ)
FATS = 53-92g/ day
Explanation: Jennifer needs to stay within these recommended amounts to ensure her body can function adequately and to keep her feeling full throughout the day.
As Jennifer is looking to gain muscle, the focus of the meal plan is a combination of assisting muscle synthesis (through small, regular intakes of protein throughout the day) and ensuring nutritional adequacy. As Jennifer is participating in regular and moderate intense exercise, this exertion will lead to an increased appetite; therefore, satiety needs to be factored in at all times. A meal plan full of protein, fat, and fibre is paramount to ensure Jennifer is satisfied and satiated throughout the day; otherwise, she may be tempted to stray from the meal plan and get quick hits of energy from nonbeneficial foods such as refined carbohydrates.
MEAL 1:
As Jennifer mentioned that she enjoys a hot breakfast, eggs were selected to be the base of her first meal of the day. Eggs are high in protein and contain good quality fats, increasing satiety. A mixture of vegetables (excluding capsicum as Jennifer says she doesn’t like capsicum) was then selected to bulk the eggs up, increase her fibre content (as fibre improves satiety), and provide Jennifer with some of her vegetable requirements for the day. This meal alone would provide Jennifer with majority of her vegetable requirements (keep in mind it is fine to exceed vegetable requirements). A bagel is included to provide a good source of carbohydrates and fibre to start the day of with an adequate good amount of energy.


MEAL 2:
Dried fruit and fresh fruit have been selected as the mid-morning snack. Strawberries were selected to provide extra flavour and contain fibre and many vitamins and minerals. However, if Jennifer would prefer another type of fruit, this could easily be accommodated. Dried fruits contain a fair amount of carbohydrates which will help push Jennifer through the mid-morning slump until lunch time. Keep in mind dried fruit should be kept to a minimum because of their high sugar content.
MEAL 3:
MEAL 4:
Jennifer can use lamb roast or replace it with another meat cut or protein source. Her protein intake has increased slightly to help her reach her higher protein intake. Sweet potato and green beans are selected for their fibre, vitamin and mineral content and a slower release of sugar (lower GI). Wholemeal pasta provides Jennifer with a great amount of fibre and low GI carbs to fill her up before bedtime.
While chicken and vegetable fried rice has been written for Jennifer’s third meal of the day, there is no reason that she cannot replace the chicken with another source of protein such as beef, lamb or eggs. Before the afternoon hits, it is important to provide fibre, protein and fat to keep her full and decrease the likelihood of fatigue. The chicken provides the protein, vegetables provides the fibre, and the olive oil is an easy way to include fat. Rice will provide carbohydrates for energy during Jennifer’s workout. Jennifer can mix up her infused olive oils to increase flavour variety. QTY

MEAL 5:
Jennifer can use lamb roast or replace it with another meat cut or protein source. Her protein intake has increased slightly to help her reach her higher protein intake. Sweet potato and green beans are selected for their fibre, vitamin and mineral content and a slower release of sugar (lower GI). Wholemeal pasta provides Jennifer with a great amount of fibre and low GI carbs to fill her up before bedtime.
MEAL 6:
Popcorn is a quick and easy snack before the day ends, and, because of the fat in the olive oil, it will increase satiety and reduce the likelihood of late-night cravings. As these items are physically smaller, it may take her a bit longer to consume them, which can be extremely beneficial for someone who often eats mindlessly.


ENERGY
CARBOHYDRATES
FAT
FRUIT
VEGETABLES
FIBRE
FLUID

Jennifer’s EER is 10,030kJ. This plan has approximately 9,676kJ, this isn’t too far from her EER. 500kJ either side of the EER is sufficient.
Jennifer’s EPR is 55-82g/ day. This meal plan has approximately 82g of protein. This falls within her protein requirements, at the higher end of the range which will help with her muscle gain.
Jennifer’s carbohydrate recommendations are 266-384g/day. This meal plan has approximately 270g of carbohydrates, this falls within her requirements.
Jennifer’s fat recommendations are 53-92/day. This meal plan has approximately 89g of fats, this falls within her requirements.
4 serves of fruit is included in the meal plan. As fruit recommendations are at least 2 serves per day, Jennifer is meeting her minimum fruit recommendations.
Approximately 8.5 serves of vegetables is in this meal plan. As it is recommended to consume a minimum of 5 serves of vegetables per day, Jennifer has reached her minimum vegetable requirements.
There is 43g of fibre in this meal plan. It is recommended for women to have at least 25g of fibre a day. Jennifer is meeting her minimum requirements.
It will be important to remind Jennifer to drink a minimum of 2.1L fluid each day in addition to the above meal plan. And to increase her water intake during exercise/ on a hot day.
Gail is a 55-year-old female seeking advice on weight maintenance and ensuring she is getting adequate nutrition. She currently weighs 60kg and is 170cm tall. She has very minimal activity at work in the office and exercises at a light-moderate intensity for 30 minutes 2 days weekly. She has trialled many programs in the past but never anything personalised. She enjoys porridge for breakfast most days and has no allergies, food dislikes or other dietary restrictions. As her downfall is mindless eating (while watching TV or working at her computer), she has suggested regular meals throughout the day may work best for her.
STEP 1: Calculate BMR
Women: BMR = 2741 + (40.0 x W) + (7.74 x H) - (19.56 x A) kJ/day
BMR = 2,741 + (40 x 60) + (7.74 x 170) – (19.56 x 55)
BMR = 2,741 + (2,400) + (1,315.8) – (1,075.8)
BMR =6,456.8 – 1,075.8
BMR =5,381 kJ/day
STEP 2: Multiply BMR by AF
EER = BMR x PAL
EER = 5,381 kJ x 1.4
EER = 7,533 kJ/day
Explanation: The activity factor of 1.4 has been selected because Gail completes minimal activity throughout her work day and only an additional 60 minutes of light-moderate-intensity exercise per week. Even though she is completing her planned exercise at a light-moderate intensity, she is not completing it regularly, so she will stay at the PAL of 1.4. Through the consultation, Gail is encouraged to focus her two exercise sessions around resistance training, rather than cardiovascular training, for muscular benefit, and a referral to a local PT is made. Should Gail increase her exercise frequency, intensity or duration under the care of the PT, her EER can be re-calculated.


EPR = 0.8-1.0 x W
EPR = 0.8-1.0 x 60
EPR = 48- 60g/ day
Explanation: Gail exercises twice a week at a light-moderate intensity so she requires 0.8-1.0g of protein for every kilogram of body weight. If she increases her intensity and frequency, she will require her EPR to be recalculated.
CARBOHYDRATES = 45-65% of EER
CARBOHYDRATES = EER x 0.45-0.65
CARBOHYDRATES = 7,533kJ x 0.45-0.65
CARBOHYDRATES = 3,389.8 – 4,896.4 ÷ 17kJ (1g carbohydrate = 17kJ)
CARBOHYDRATES = 199-288g/ day
Explanation: Gail needs to stay within these recommended amounts to ensure she has enough energy throughout her day.
FATS = 20-35% of EER
FATS = EER x 0.20-0.35
FATS = 7,533kJ x 0.20-0.35
FATS = 1,506.6 – 2,636.5 ÷ 38kJ (1g fats = 38kJ)
FATS = 40-69g/ day
Explanation: Gail needs to stay within these recommended amounts to ensure her body can function adequately and to keep her feeling full throughout the day.
When designing any meal plan, it is always important to ensure the client will be satisfied throughout the plan, otherwise they may be more likely to look for a quick hit of energy from sugary foods. Taking their likes, dislikes and dietary restrictions into account is also important as the plan is a lot more achievable for the client to follow.


MEAL 1:
Gail mentioned that she enjoys porridge for breakfast, but because porridge is traditionally low in protein, bulking it up with nuts will increase the protein content. Adding raspberries will add fibre increasing satiety.
MEAL 2:
A nut bar, along with an apple has been selected. A nut bar was selected simply because it has high amounts of fibre and is a good source of healthy fats. Gail can switch up flavours and types of bars if she wishes, this is easy to accommodate. The apple provides high amounts of carbohydrates and are great for a slight boost in immediate energy levels.
MEAL 3:
Egg salad has been written for Gail’s third meal of the day, however, there is no reason that she cannot replace the egg with another source of protein such as beef, lamb or chicken. Before the afternoon hits, it is important to provide fibre, protein and fat to keep her full and decrease the likelihood of the ‘3 pm slump’. The eggs and beans provide the protein, greens provide the fibre and the avocado and olive oil is a great way to introduce extra fats.

MEAL 4:
As Gail has indicated that she struggles with mindless eating, providing small items in larger numbers can be a beneficial way to provide Gail with the sense she is ‘mindless eating’ all the while the food is fully accounted for and increasing satiety levels. Foods such as hummus and veggie sticks are a great option as they are relatively low in kilojoules and can therefore be eaten in larger amounts.
MEAL 5:
Gail can use roast turkey or can easily replace it with another meat cut or protein source. Zucchini was selected to provide some variety to her vegetable intake. Sweet potato is selected over white potato as it contains higher vitamin content and a slower release of sugar, improving satiation.
MEAL 6:
Fruit is a quick and easy snack before the day ends, and because of their fibre, it will reduce the likelihood of late-night cravings. Gail can easily switch up the different fruits to suit her liking.


Gail’s EER is 7,533kJ. This plan has approximately 7,205kJ; this isn’t too far from her EER. 500kJ on either side of the EER is sufficient.
FAT
FRUIT
FIBRE

Determining an exact energy intake for weight maintenance is very difficult (due to variations in activity level, exercise and dietary intake). Should Gail’s weight increase beyond 1-2kg over the coming weeks, it would be best to reduce her food intake to reduce her energy intake.
Gail’s EPR is 48-60g/ day. This meal plan has approximately 60g of protein. This falls within Gail’s protein requirements, at the higher end of the range.
Gail’s carbohydrate recommendations are 199-288g/day. This meal plan has approximately 200g of carbohydrates; this falls within her requirements at the lower end of the range.
Gail’s fat recommendations are 40-69/day. This meal plan has approximately 63g of fats, this falls within her requirements.
5 serves of fruit is included in the meal plan. As fruit recommendations are at least 2 serves per day, Gail is meeting her minimum fruit recommendations.
Approximately 7.5 serves of vegetables are in this meal plan. As it is recommended to consume a minimum of 5 serves of vegetables per day, Gail has reached her minimum vegetable requirements.
There is 56g of fibre in this meal plan. It is recommended for women to have at least 25g of fibre a day. Gail is meeting her minimum requirements.
It will be important to remind Gail to drink a minimum of 2.1L fluid each day in addition to the above meal plan. And to increase her water intake during exercise/ on a hot day.
CASE STUDY: BEC
Bec is a 21-year-old female seeking advice for weight gain after struggling with illness. She currently weighs 50kg and is 170cm tall. She has received medical clearance from her GP, whose BMI is 17 (underweight) and her goal weight is 60kg. She is mainly sedentary as an office worker and exercises at a light-moderate intensity for 30 minutes, 2 days each week. She has trialled many programs in the past but never anything personalised. She is not usually hungry for breakfast (but is willing to try something), and has no allergies, food dislikes or other dietary restrictions. Bec has suggested regular meals throughout the day may work best for her as she tries to increase her food intake for weight gain.
STEP 1: Calculate BMR
Women: BMR = 2741 + (40.0 x W) + (7.74 x H) - (19.56 x A) kJ/day
BMR = 2,741 + (40 x 50) + (7.74 x 170) – (19.56 x 21)
BMR = 2,741 + (2,000) + (1,315.8) – (410.76)
BMR =6,056.8 – 410.76
BMR =5,646 kJ/day
STEP 2: Multiply BMR by PAL
EER = EER = BMR x PAL
EER = 5,646 kJ x 1.4
EER = 7,904 kJ/day
Explanation: The activity factor of 1.4 has been selected because Bec only exercises twice a week at a low to moderate intensity and isn’t active as a student. If she increases her exercise intensity and frequency, she would require her EER to be recalculated.
STEP 3: Adjust EER for desired weight gain
As weight gain is desired, 2,000kJ is added to the EER to allow the client a weight gain of ~500g per week.
Adjusted EER = EER + 2,000
Adjusted EER = 7,904kJ + 2,000
Adjusted EER = 9,904kJ/day
Explanation: As weight gain is desired, 2,000kJ is added to the daily calculated EER to provide the adjusted daily EER, which will be used ongoing. This will allow Bec a weight gain of ~500g per week. It is important to remember that as her weight increases her EER will need to be adjusted.


EPR = 0.8-1.0 x 50
EPR = 0.8-1.0 x 50
EPR = 40- 50g/ day
Explanation: Bec exercises twice a week at a low-moderate intensity, so she requires 0.8-1.0g of protein for every kilogram of body weight. If she increases her intensity and frequency, she would require her EPR to be recalculated.
CARBOHYDRATES = 45-65% of EER
CARBOHYDRATES = EER x 0.45-0.65
CARBOHYDRATES = 9,904kJ x 0.45-0.65
CARBOHYDRATES = 4,456.8 – 6,437.6 ÷17kJ (1g carbohydrate = 17kJ)
CARBOHYDRATES = 262-379g/ day
Explanation: Bec needs to stay within these recommended amounts to ensure she has enough energy throughout her day.
FATS = 20-35% of EER
FATS = EER x 0.20-0.35
FATS = 9,904kJ x 0.20-0.35
FATS = 1,980.8 – 3,466.4 ÷ 38kJ (1g fats = 38kJ)
FATS = 52-91g/ day
Explanation: Bec needs to stay within these recommended amounts to ensure her body can function adequately and to keep her feeling full throughout the day.
As Bec wants to gain weight, not particularly muscle, a meal plan has been created, which is 2,000kJ above her daily EER. While it is known that excess carbohydrate and sugar-rich foods can lead to weight gain, this weight gain is also associated with uncontrolled blood glucose levels, increased risk for diabetes and decreased energy and concentration levels. Therefore, a meal plan created for a client wanting to increase weight can be slightly more lenient on carbohydrates; however, it still needs to ensure all other nutrient recommendations are met too.
If the client is struggling with being too full, evaluate the meal plan and consider reducing fat intake and increasing carbohydrate intake (however, always be sure to stick within guideline recommendations).

MEAL 1:
As Bec has mentioned that she is not usually hungry at breakfast, a liquid breakfast like a smoothie might be a good option as liquid kilojoules can be easier to consume if appetite is poor. A green smoothie is a fantastic way of adding healthy fats, vegetables and nutrients at breakfast.
MEAL 2:
Rice thins with peanut butter, sultanas and banana has been selected for a snack. Rice cakes and fruit were selected as they are a good source of carbohydrates that will provide Bec with energy at the start of the day. Peanut butter is high in healthy fats and will help Bec stay full until lunch time.
MEAL 3:
A salad wrap has been selected for Bec’s third meal of the day. Before the afternoon hits, it is important to provide fibre and fat to keep her full and decrease the likelihood of the ‘3 pm slump’.

MEAL 4:
Fresh fruit and veg is a great snack to include, as it is high fibre. An orange and snow peas have been selected here, however, Bec may swap it out for any others that she likes.
MEAL 5:
Bec can use minced beef or can easily replace it with another cut of meat or source of protein. The rice is a great source of carbohydrates. While it is usually more beneficial to opt for wholegrain options over white options, white rice has been chosen for Bec as it is higher in kilojoules and this will help her to meet her high energy intake. The fibre has instead been replaced in the many vegetables in this meal. Olive oil is a great way to introduce fats into a meal too.
MEAL 6:
Mixed nuts and dark chocolate is a quick and easy snack before the day ends, and because of the fat in them, it will reduce the likelihood of late-night cravings.

ENERGY
PROTEIN
CARBOHYDRATES
FAT
FRUIT
VEGETABLES
FIBRE
FLUID

Bec’s EER is 9,904kJ including the energy surplus. This plan has approximately 9,510kJ, this isn’t too far from her EER. 500kJ either side of the EER is sufficient.
Bec’s EPR is 40-50g/ day. This meal plan has approximately 50g of protein. This falls within Sophie’s protein requirements, at the higher end of the range.
Bec’s carbohydrate recommendations are 262-379g/day. This meal plan has approximately 316g of carbohydrates, this falls within her requirements.
Bec’s fat recommendations are 52-91/day. This meal plan has approximately 85g of fats, this falls within her requirements.
4 serves of fruit is included in the meal plan. As fruit recommendations are at least 2 serves per day, Bec is meeting her minimum fruit recommendations.
Approximately 9.5 serves of vegetables is in this meal plan. As it is recommended to consume a minimum of 5 serves of vegetables per day, Sophie has reached her minimum vegetable requirements.
There is 42g of fibre in this plan. It is recommended for women to have at least 25g of fibre a day. Bec is within her recommendations.
It will be important to remind Bec to drink a minimum of 2.1L fluid each day in addition to the above meal plan. And to increase her water intake during exercise/ on a hot day.
CASE STUDY: JOSEPH
Joseph is a 42-year-old male seeking advice on weight loss. He works as a carpenter (active 7hrs+ 4 days per week) and completes 45-60 minutes surfing or swimming at a high intensity, 2-3 days per week. Joseph currently weighs 82kg and is 174cm tall. He is recently divorced and is now learning to cook for himself. While he is eager to learn, his skills are basic, and he does not want to spend long periods in the kitchen. He claims to enjoy all foods, especially fish. He dislikes brussel sprouts, capsicum and ginger. Due to personal preference, he has also requested a meal plan with no dairy. He tends to opt for just 2 main meals per day with a couple of snacks if he has time.
STEP 1: Calculate BMR
Men: BMR = 278 + (57.5 x W) + (20.93 x H) - (28.35 x A) kJ/day
BMR = 278 + (57.5 x 82) + (20.93 x 174) - (28.35 x 42) kJ/day
BMR = 278 + 4,715 + 3,641.82 – 1,190.7
BMR = 8,634.82 – 1,190.7
BMR = 7,444 kJ/day
STEP 2: Multiply BMR by PAL
EER = BMR x PAL
EER = 7,444 kJ x 2.2
EER = 16,377 kJ/day
Explanation: The activity factor of 2.2 has been selected because Joseph is active 7 hours per day 4 days of the week and completes an additional 45-60 mins of high-intensity physical activity on 2-3 days of the week.
STEP 3: Adjust EER for desired weight loss
Adjusted EER = EER - 2,000kJ
Adjusted EER = 16,377 - 2,000
Adjusted EER = 14,377 kJ/day
Explanation: As a general rule, weight loss of 500g per week is recommended. Weight loss of ~500g per week is achieved by decreasing the client’s EER by ~2,000kJ per day.


EPR = 1.5-2.0g/kg body weight per day
EPR = 123-164g/day
Explanation: Joseph is active in his work 4 days per week and requires higher amounts of protein because he is trying to lose body fat. His work activity would be at a high-intensity and is working actively 4 days per week. He is also completing additional exercise at a high- intensity 2-3 days per week; therefore he would require the higher protein requirements to assist with muscle repair and retention while being in an energy deficit.
CARBOHYDRATES = 45-65% of EER
CARBOHYDRATES = EER x 0.45-0.65
CARBOHYDRATES = 14,377kJ x 0.45-0.65
CARBOHYDRATES = 6,469.65 – 9,345.05 ÷ 17kJ (1g carbohydrate = 17kJ)
CARBOHYDRATES = 381-550g/ day
Explanation: Joseph needs to stay within these recommended amounts to ensure he has enough energy to fuel his active lifestyle.
FATS = 20-35% of EER
FATS = EER x 0.20-0.35
FATS = 14,377kJ x 0.20-0.35
FATS = 2,875.4 – 5,031.95 ÷ 38kJ (1g fats = 38kJ)
FATS = 76-132g/ day
Explanation: Joseph needs to stay within these recommended amounts to ensure his body can function adequately and to keep him feeling full throughout the day.
Throughout the meal plan, Joseph likes (meat) and dislikes (Brussel sprouts, capsicum, ginger) have been taken into account, and dairy has been avoided completely as per his request. The meal plan has been split into two main meals with a few snacks. The main meals are easy for Joseph to make, considering his limited kitchen skills.


MEAL 1:
As Joseph says he typically only has time for 2 meals a day, this meal isn’t necessarily ‘breakfast’ but can be consumed on the way to work in the morning as his first meal of the day. This meal is high in carbs and fibre to give Joseph energy to start his active day.
MEAL 2:
This will be Joseph’s mid-morning snack that he can prepare ahead of time to eat at work. The egg and salad sandwich will provide him with a good amount of fats to keep him full until lunch time. Fruit and nuts have been chosen so he can snack on them through the morning, to keep him going until lunch time. Joseph stated he likes meat, so beef jerky was selected to provide a good amount of protein and cure cravings.
MEAL 3:
Steak is something that not only Joseph will enjoy but requires minimal skills in the kitchen. Sweet potato and white potato has been selected to include a variety and increase his carbohydrate intake. It has been mixed with cauliflower and broccoli to increase volume and fibre. Brown rice has been chosen to increase the carbohydrate content in this meal, to give Joseph energy to fuel his day. Olive oil is always an easy way to add healthy fats to your diet.

As Joseph has specified that he enjoys fish, smoked salmon, crackers and alfalfa has been selected for one of his meals throughout the day. Along with some more fruit and pretzels as a source of carbohydrates to increase energy levels.
Oven-baked items are really easy for Joseph to cook and have been added to his meal plan. Chicken has been included as it is high in protein, essential for muscle repair after his very active day. The vegetables are a great source of carbohydrates and fibre. Joseph can mix the pasta, frozen vegetables and tinned tomatoes together to make a colourful side dish.


ENERGY
FAT
FLUID

Joseph’s EER is 14,377kJ including the energy deficit. This plan has approximately 14,494kJ, this is within his energy requirements.
Joseph’s EPR is 123-164g/ day. This meal plan has approximately 162g of protein. This falls within Joseph’s protein requirements, at the higher end of the range to help with muscle recovery considering he is very physical active.
Joseph’s carbohydrate recommendations are 381-550g/day. This meal plan has approximately 388g of carbohydrates, this falls within his requirements.
Joseph’s fat recommendations are 76-132/day. This meal plan has approximately 121g of fats, this falls within his requirements.
5 serves of fruit is included in the meal plan. As fruit recommendations are at least 2 serves per day, Joseph is meeting his minimum fruit recommendations.
Approximately 13 serves of vegetables is in this meal plan. As it is recommended to consume a minimum of 5 serves of vegetables per day, Joseph has reached his minimum vegetable requirements. It is important to consider his current vegetable intake, as this may be a big jump from his usual intake. It would be important to remind Joseph of the effects that can come with increased vegetable and fibre intake.
There is 76g of fibre in this meal plan. It is recommended for men to have at least 30g of fibre a day. Joseph is meeting his minimum requirements. Again, it is important to remind Joseph of the effects that can come with fibre intake.
It will be important to remind Joseph to drink a minimum of 2.6L fluid each day in addition to the above meal plan. And to increase his water intake during exercise/ on a hot day.
Thomas is a 35-year-old male who is seeking advice on muscle gain. He works as a carpenter (active 7hrs+ 4 days per week) and completes 30 minutes rowing or mountain biking at a moderate-intensity, 2-3 days per week. Thomas currently weighs 95kg and is 180cm tall. He lives with his wife and daughter and enjoys all foods, especially meat and fruit. He has no food dislikes, allergies, intolerances or dietary requirements. He has been skipping breakfast some days due to lack of time and usually has two main meals per day, with a couple of snacks if he has time.
STEP 1: Calculate BMR
Men: BMR = 278 + (57.5 x W) + (20.93 x H) - (28.35 x A) kJ/day
BMR = 278 + (57.5 x 95) + (20.93 x 180) - (28.35 x 35) kJ/day
BMR = 278 + 5,462.5 + 3,767.4 – 992.25
BMR = 9,507.9 – 992.25
BMR = 8,516 kJ/day
STEP 2: Multiply BMR by PAL
EER = BMR x PAL
EER = 8,516 kJ x 2.0
EER = 17,032 kJ/day
Explanation: The activity factor of 2.0 has been selected because Thomas is active 7 hours per day 4 days of the week and completes an additional 30 minutes of moderate-intensity physical activity on 2-3 days of the week.
EPR = 1.5-2.0g/kg body weight per day
EPR = 1.5-2.0 x 95
EPR = 142.5-190g
Explanation: Thomas has an EPR of 1.5-2.0g/kg per day as he will be swapping his bike riding, rowing and hill running for resistance training to increase muscle mass, with the assistance of a personal trainer. Thomas will still get his cardiovascular fitness from work 4 days per week. Thomas would already be doing exercise to retain muscle mass through his work; however, increasing resistance training will aid muscle synthesis.


CARBOHYDRATES = 45-65% of EER
CARBOHYDRATES = EER x 0.45-0.65
CARBOHYDRATES = 17,032 kJ x 0.45-0.65
CARBOHYDRATES = 7,664.4 – 11,070.8 ÷ 17kJ (1g carbohydrate = 17kJ)
CARBOHYDRATES = 451-651g/ day
Explanation: Thomas needs to stay within these recommended amounts to ensure he has enough energy to fuel his active lifestyle.
FATS = 20-35% of EER
FATS = EER x 0.20-0.35
FATS = 17,032 kJ x 0.20-0.35
FATS = 3,406.4 – 5,961.2 ÷ 38kJ (1g fats = 38kJ)
FATS = 90-157g/ day
Explanation: Thomas needs to stay within these recommended amounts to ensure his body can function adequately and to keep him feeling full throughout the day.
Throughout the meal plan, Thomas’s likes (meat & fruit) have been considered. The meal plan itself has been split into three main meals with two snacks, accompanied by protein source from wholefoods and supplements. The main meals are easy for Thomas to prepare, especially breakfast, due to his lack of time in the mornings.
MEAL 1:
Thomas does not have time to prepare a full breakfast in the morning, so a protein shake with added fruit and chia seeds will provide protein, fibre and energy to keep him going and begin meeting his protein recovery needs for the day.

A simple snack of homemade protein balls, fruit and rice cakes will allow the body to utilise a fresh protein intake to aid in muscle recovery and synthesis. As well as carbohydrates to keep energised for the day.
Wraps with chicken breast, salad, beans and hummus, with homemade popcorn and fruit on the side will provide fibre, protein and healthy fats to keep Thomas full and properly fuelled for work.

MEAL 4:
Dinner will centre around a good serve of protein like pulled pork, but he can swap it for chicken or fish too, and plenty of vegetables to boost fibre and satiety. The sweet potato can be baked and topped with cheese and sour cream to increase healthy fats and help Thomas feeling full.
MEAL 5:
This final snack can be eaten after dinner or between meals to add some variety and extra fibre, which is important where a high protein diet is followed.


FAT
VEGETABLES
FLUID

Thomas’ EER is 17,032 kJ. This plan has approximately 16,565 kJ, this is within his energy requirements. 500kJ either side of the EER is sufficient.
Thomas’ EPR is 142.5-190g/ day. This meal plan has approximately 190g of protein. This falls within Thomas’ protein requirements, at the higher end of the range to help with muscle recovery considering he is very physical active.
Thomas’ carbohydrate recommendations are 451-651g/day. This meal plan has approximately 457g of carbohydrates, this falls within his requirements.
Thomas’ fat recommendations are 90-157g/day. This meal plan has approximately 133g of fats, this falls within his requirements.
7.5 serves of fruit is included in the meal plan. As fruit recommendations are at least 2 serves per day, Thomas is meeting his minimum fruit recommendations.
Approximately 10.5 serves of vegetables is in this meal plan. As it is recommended to consume a minimum of 5 serves of vegetables per day, Thomas has reached his minimum vegetable requirements.
There is 103g of fibre in this meal plan. It is recommended for men to have at least 30g of fibre a day. Thomas is meeting his minimum requirements. It is important to consider his current fibre intake, as this may be a big jump from his usual intake. While it is fine to consume over the fibre minimum, it is important to remind Thomas of the effects that can come with increased fibre intake.
It will be important to remind Thomas to drink a minimum of 2.6L fluid each day in addition to the above meal plan. And to increase his water intake during exercise/ on a hot day.

1. What is duty of care? | Slater and Gordon [Internet]. 2022 [cited 2022 Jun 2]. Available from: https://www. slatergordon.com.au/personal-injury/public-liability/what-is-duty-of-care
2. Australian Privacy Principles - Home [Internet]. 2021 [cited 2022 Jun 2]. Available from: https://www.oaic.gov. au/privacy/australian-privacy-principles
3. 0763NAT CERTIFICATE IV IN NUTRITION SCOPE OF PRACTICE Developed and endorsed by Nutrition Council Australia (NCA) [Internet]. 2020 [cited 2022 Jun 2]. Available from: https://www.nutritioncouncilaustralia.com. au/wp-content/uploads/2020/10/NCA-10763NAT-Certificat-IV-Nutrition-Scope-of-Practice-V2.pdf
4. Mannion C, Page S, Bell LH, Verhoef M. Components of an Anticancer Diet: Dietary Recommendations, Restrictions and Supplements of the Bill Henderson Protocol. Nutrients [Internet]. 2011 [cited 2022 Jun 2];3(1):1. Available from: /pmc/articles/PMC3257729/
5. Common Allergens - Peanut, Egg, and Sesame Allergies | FARE [Internet]. 2022 [cited 2022 Jun 2]. Available from: https://www.foodallergy.org/living-food-allergies/food-allergy-essentials/common-allergens
6. Zukiewicz-Sobczak WA, Wróblewska P, Adamczuk P, Kopczynski P. Causes, symptoms and prevention of food allergy. Adv Dermatology Allergol Dermatologii I Alergol [Internet]. 2013 [cited 2022 Jun 2];30(2):113. Available from: /pmc/articles/PMC3834685/
7. Food intolerance - Australasian Society of Clinical Immunology and Allergy (ASCIA) [Internet]. 2019 [cited 2022 Jun 2]. Available from: https://www.allergy.org.au/patients/food-other-adverse-reactions/food-intolerance
8. Nutrition Australia. Food intolerances 4 minute read |. 2021 [cited 2022 Jun 2]; Available from: https://www. foodauthority.nsw.gov.au/consumer/life-events-and-food/allergy-and-intolerance.
9. Dietitians Australia. The role of an Accredited Practising Dietitian | Dietitians Australia [Internet]. [cited 2022 Jun 29]. Available from: https://dietitiansaustralia.org.au/working-dietetics/standards-and-scope/role-accreditedpractising-dietitian
10. Healthy Eating and How to Get the Right Advice - Sports Dietitians Australia (SDA) [Internet]. [cited 2022 Jun 29]. Available from: https://www.sportsdietitians.com.au/sda-blog/healthy-eating-right-advice/
11. Dan Brennan M. What Is a General Practitioner? What They Do, When to See One, and What to Expect [Internet]. [cited 2022 Jun 29]. Available from: https://www.webmd.com/a-to-z-guides/what-is-a-general-practitioner
12. How to lower blood pressure - hypertension, lifestyle, medication | healthdirect [Internet]. 2021 [cited 2022 Jun 29]. Available from: https://www.healthdirect.gov.au/how-to-lower-blood-pressure
13. Allied Health Professions Australia. Psychology - Allied Health Professions Australia [Internet]. 2022 [cited 2022 Jun 29]. Available from: https://ahpa.com.au/allied-health-professions/psychology/
14. Daniel D. Chiras. Human Body Systems: Structure, Function, and Environment - Daniel D. Chiras - Google Books [Internet]. 2013 [cited 2022 Jun 29]. Available from: https://books.google.com.
15. Rowan Stewart. Handbook of Clinical Nutrition and Dietetics. Fifth Edit. Australian Dietitian; 2015.
16. Eat For health. Frequently Asked Questions | Eat For Health [Internet]. Australian Government NHMRC. 2020 [cited 2022 Sep 13]. Available from: https://www.eatforhealth.gov.au/food-essentials/frequently-askedquestions
17. Protein | Dietitians Australia [Internet]. 2022 [cited 2022 Jun 29]. Available from: https://dietitiansaustralia.org. au/health-advice/protein
18. Srini Srinivasan V. Bioavailability of Nutrients: A Practical Approach to In Vitro Demonstration of the Availability of Nutrients in Multivitamin-Mineral Combination Products. J Nutr [Internet]. 2001 Apr 1 [cited 2022 Jun 29];131(4):1349S-1350S. Available from: https://academic.oup.com/jn/article/131/4/1349S/4686865
19. Food Nutrition Facts and Free Calorie Counter | CalorieKing (Australia) [Internet]. [cited 2022 Jun 29]. Available from: https://www.calorieking.com/au/en/
20. Lopez MJ, Mohiuddin SS. Biochemistry, Essential Amino Acids. StatPearls [Internet]. 2022 Mar 18 [cited 2022 Jul 4]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK557845/
21. Kadey M. Protein, You Complete Me.: EBSCOhost. Newsl Food, Nutr Heal [Internet]. 2019 [cited 2022 Jul 4];42(9). Available from: https://web-p-ebscohost-com.ezproxy.usc.edu.au/ehost/pdfviewer/ pdfviewer?vid=0&sid=96a8eb04-8980-41da-9bea-616cc50f0e12%40redis
22. Sugar [Internet]. [cited 2022 Jul 4]. Available from: https://www.foodstandards.gov.au/consumer/nutrition/ Pages/Sugar.aspx
23. Eleanor Whitney, Sharon Rady Rolfes, Tim Crowe, David Cameron-Smith AW. Understanding Nutrition. 3rd ed. 2017.

24. Carbohydrate | Nutrient Reference Values [Internet]. [cited 2022 Jul 4]. Available from: https://www.nrv.gov.au/ nutrients/carbohydrate
25. Holesh JE, Aslam S, Martin A. Physiology, Carbohydrates. StatPearls [Internet]. 2021 Jul 26 [cited 2022 Jul 4]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK459280/
26. Slavin J, Carlson J. Carbohydrates. Adv Nutr [Internet]. 2014 [cited 2022 Sep 21];5(6):760. Available from: /pmc/ articles/PMC4224210/
27. Kim JY. Optimal Diet Strategies for Weight Loss and Weight Loss Maintenance. J Obes Metab Syndr [Internet]. 2021 Mar 3 [cited 2022 Sep 21];30(1):20. Available from: /pmc/articles/PMC8017325/
28. Fats: Total fat & fatty acids | Nutrient Reference Values [Internet]. [cited 2022 Jul 4]. Available from: https://www. nrv.gov.au/nutrients/fats-total-fat-fatty-acids
29. Gale. The Gale Encyclopedia of Children’s Health: Infancy Through Adolescence. 4th ed. Gale; 2021.
30. Yoon H, Kleven A, Paulsen A, Kleppe L, Wu J, Ying Z, et al. Interplay between exercise and dietary fat modulates myelinogenesis in the central nervous system. Biochim Biophys Acta [Internet]. 2016 Apr 1 [cited 2022 Jul 4];1862(4):545. Available from: /pmc/articles/PMC4788558/
31. Feingold KR, Grunfeld C. Introduction to Lipids and Lipoproteins. Endotext [Internet]. 2021 Jan 19 [cited 2022 Jul 4]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK305896/
32. Tortora GJ, Derrickson B. Principles of Anatomy & Physiology. Thirteenth. John Wiley & Sons, Inc.; 2012.
33. Chia-Yu Chang, Der-Shin Ke J-YC. Essential fatty acids and human brain. Acta Neurol Taiwan [Internet]. 2009;18(4):231–41. Available from: https://pubmed.ncbi.nlm.nih.gov/20329590/#:~:text=The human brain is nearly,integrity and ability to perform.
34. Crowley L V. An Introduction to Human Disease: Pathology and Pathophysiology. 9th ed. Learning, Jones & Bartlett; 2013.
35. Bozzatello P, Rocca P, Mantelli E, Bellino S. Polyunsaturated Fatty Acids: What is Their Role in Treatment of Psychiatric Disorders? Int J Mol Sci [Internet]. 2019 Nov 1 [cited 2022 Jul 4];20(21). Available from: /pmc/articles/ PMC6862261/
36. Dehghan M, Mente A, Zhang X, Swaminathan S, Li W, Mohan V, et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017 Nov 1;390(10107):2050–62.
37. Gropper SS, Smith JL, Carr TP. Advanced Nutrition and Human Metabolism. Seventh. Boston. USA: Cengage Learning; 2018.
38. Mahan LK, Raymond JL. Krause’s Food & The Nutrition Care Process. 14th ed. Elsevier; 2017.
39. Food Standards Australia New Zealand. Food Details - Monounsaturated oils [Internet]. Food Standards Australia New Zealand. 2022 [cited 2022 Sep 21]. Available from: https://www.foodstandards.gov.au/science/ monitoringnutrients/afcd/Pages/fooddetails.aspx?PFKID=F006177
40. Aly J, Engmann O. The Way to a Human’s Brain Goes Through Their Stomach: Dietary Factors in Major Depressive Disorder. Front Neurosci. 2020 Dec 7;14:1244.
41. Nestel P, Clifton P, Colquhoun D, Noakes M, Mori TA, Sullivan D, et al. Indications for Omega-3 Long Chain Polyunsaturated Fatty Acid in the Prevention and Treatment of Cardiovascular Disease. Hear Lung Circ [Internet]. 2015 [cited 2021 Mar 16];24:769–79. Available from: http://dx.doi.org/10.1016/j.hlc.2015.03.020
42. Wells ML, Potin P, Craigie JS, Raven JA, Merchant SS, Helliwell KE, et al. Algae as nutritional and functional food sources: revisiting our understanding. J Appl Phycol [Internet]. 2017 Apr 1 [cited 2021 Apr 8];29(2):949–82. Available from: /pmc/articles/PMC5387034/
43. O’Donovan F, Carney S, Kennedy J, Hayes H, Pender N, Boland F, et al. Associations and effects of omega-3 polyunsaturated fatty acids on cognitive function and mood in healthy adults: a protocol for a systematic review of observational and interventional studies. BMJ Open [Internet]. 2019 Jun 1 [cited 2022 Aug 23];9(6). Available from: /pmc/articles/PMC6596976/
44. Burns-Whitmore, Froyen, Heskey, Parker, San Pablo. Alpha-Linolenic and Linoleic Fatty Acids in the Vegan Diet: Do They Require Dietary Reference Intake/Adequate Intake Special Consideration? Nutrients [Internet]. 2019 Oct 4 [cited 2021 Feb 2];11(10):2365. Available from: https://www.mdpi.com/2072-6643/11/10/2365
45. Ramsden CE, Zamora D, Leelarthaepin B, Majchrzak-Hong SF, Faurot KR, Suchindran CM, et al. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: Evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ [Internet]. 2013 Feb 9 [cited 2021 Feb 1];346(7894). Available from: /pmc/articles/PMC4688426/?report=abstract
46. Sergeant S, Rahbar E, Chilton FH. Gamma-linolenic acid, Dihommo-gamma linolenic, Eicosanoids and Inflammatory Processes. Eur J Pharmacol [Internet]. 2016 [cited 2021 Apr 22];785:77–86. Available from: /pmc/ articles/PMC4975646/

47. Patterson E, Wall R, Fitzgerald GF, Ross RP, Stanton C. Health implications of high dietary omega-6 polyunsaturated fatty acids [Internet]. Vol. 2012, Journal of Nutrition and Metabolism. Hindawi Limited; 2012 [cited 2021 Jan 28]. p. 16. Available from: /pmc/articles/PMC3335257/?report=abstract
48. Tallima H, El Ridi R. Arachidonic acid: Physiological roles and potential health benefits – A review. J Adv Res [Internet]. 2018 May 1 [cited 2021 Feb 23];11:33–41. Available from: /pmc/articles/PMC6052655/
49. Longdom. By-Product | Peer Reviewed Journals [Internet]. Longdom Open Access Journals. 2021 [cited 2022 Sep 13]. Available from: https://www.longdom.org/peer-reviewed-journals/byproduct-1961.html
50. World Health Organisation. Nutrition: Trans fat [Internet]. World Health Organisation. 2022 [cited 2022 Sep 13]. Available from: https://www.who.int/news-room/questions-and-answers/item/nutrition-trans-fat
51. Organisation WH. Micronutrients [Internet]. World Health Organisation. 2022 [cited 2022 Sep 13]. Available from: https://www.who.int/health-topics/micronutrients#tab=tab_1
52. Shaheen NA, Alqahtani AA, Assiri H, Alkhodair R, Hussein MA. Public knowledge of dehydration and fluid intake practices: variation by participants’ characteristics. BMC Public Health [Internet]. 2018 Dec 5 [cited 2021 Mar 30];18(1):1346. Available from: https://bmcpublichealth.biomedcentral.com/articles/10.1186/s12889-018-6252-5
53. Jeukendrup A, Gleeson M. Sport Nutrition. Third edit. Human Kinetics Publishers Inc.; 2019.
54. National Health and Medical Research Council. Water | Nutrient Reference Values [Internet]. Nutrient Reference Values for Australia and New Zealand. 2014 [cited 2022 Sep 13]. Available from: https://www.nrv.gov.au/ nutrients/water
55. National Health and Medical Research Council. Macronutrient Balance | Nutrient Reference Values [Internet]. Nutrient Reference Values. 2014 [cited 2022 Sep 13]. Available from: https://www.nrv.gov.au/chronic-disease/ macronutrient-balance
56. Milk, yoghurt, cheese and/or their alternatives ( mostly reduced fat ) | Eat For Health [Internet]. [cited 2022 Sep 29]. Available from: https://www.eatforhealth.gov.au/food-essentials/five-food-groups/milk-yoghurt-cheeseandor-their-alternatives-mostly-reduced-fat
57. Murray MT, Nowicki J. Textbook of Natural Medicine [Internet]. 5th ed. Pizzorno JE, Murray MT, editors. Elsevier; 2020. Available from: https://www.sciencedirect.com/topics/medicine-and-dentistry/low-fiber-diet#:~:text=A low-fiber diet that is high in refined,obstructing the flow of blood up the legs.
58. Grain ( cereal ) foods, mostly wholegrain and / or high cereal fibre varieties | Eat For Health [Internet]. [cited 2022 Sep 29]. Available from: https://www.eatforhealth.gov.au/food-essentials/five-food-groups/grain-cereal-foodsmostly-wholegrain-and-or-high-cereal-fibre
59. International Dairy Foods Association. Definitions - IDFA [Internet]. International Dairy Foods Association. 2022 [cited 2022 Sep 14]. Available from: https://www.idfa.org/definition
60. Australian Government Department of Health. Standard drinks guide | Australian Government Department of Health. Australian Government Department of Health. 2020.
61. Eat For Health. Discretionary food and drink choices | Eat For Health [Internet]. Eat For Health. 2017 [cited 2021 Jun 22]. Available from: https://www.eatforhealth.gov.au/food-essentials/discretionary-food-and-drink-choices
62. Bendavid I, Lobo DN, Barazzoni R, Cederholm T, Coëffier M, de van der Schueren M, et al. The centenary of the Harris–Benedict equations: How to assess energy requirements best? Recommendations from the ESPEN expert group. Clin Nutr. 2021 Mar 1;40(3):690–701.
63. AUSactive. ADULT PRE-EXERCISE SCREENING SYSTEM (APSS) USER GUIDE STAGE 1 (COMPULSORY) AIM [Internet]. AUSactive. 2022 [cited 2022 Apr 12]. Available from: www.exercisesciencetoolkit.com
64. Eat For Health. Daily energy requirements calculator | Eat For Health [Internet]. Eat For Health. 2019 [cited 2022 Sep 14]. Available from: https://www.eatforhealth.gov.au/webform/daily-energy-requirements-calculator
65. Potgeiter S. Sport nutrition: A review of the latest guidelines for exercise and sport nutrition from the American College of Sport Nutrition, the International Olympic Committee and the International Society for Sports Nutrition. South African J Clin Nutr. 2013;26(1):6–16.
66. NHMRC. Macronutrient Balance | Nutrient Reference Values [Internet]. National Health and Medical Research Council. 2014 [cited 2021 Mar 16]. Available from: https://www.nrv.gov.au/chronic-disease/macronutrientbalance
67. NHMRC. Educator guide - Eat for health [Internet]. 2013 [cited 2021 Jan 21]. Available from: www.daahttps:// www.eatforhealth.gov.au/sites/default/files/files/the_guidelines/n55b_educator_guide_130709.pdf.asn.au.
68. Dietary fat & Heart Healthy Eating Dietary Position Statement.
69. Recommended Amount of Unsaturated Fat per Day [Internet]. [cited 2022 Jul 12]. Available from: https:// healthyeating.sfgate.com/recommended-amount-unsaturated-fat-per-day-6385.html
70. Liu AG, Ford NA, Hu FB, Zelman KM, Mozaffarian D, Kris-Etherton PM. A healthy approach to dietary fats: Understanding the science and taking action to reduce consumer confusion. Nutr J [Internet]. 2017 Aug 30 [cited 2021 Mar 16];16(1). Available from: /pmc/articles/PMC5577766/
71. Fruit | Eat For Health [Internet]. [cited 2022 Jul 12]. Available from: https://www.eatforhealth.gov.au/food-

essentials/five-food-groups/fruit
72. Healthy Living NT. What is a serve of fruit? [Internet]. [cited 2022 Jul 12]. Available from: https://www. healthylivingnt.org.au/system/files/f/HLNT_What_is_a_serve_Fruit_Veg_info_sheet.pdf
73. Vegetables and Legumes / Beans | Eat For Health [Internet]. [cited 2022 Jul 12]. Available from: https://www. eatforhealth.gov.au/food-essentials/five-food-groups/vegetables-and-legumes-beans
74. Croxford S, Itsiopoulos C, Forsyth A, Belski R, Thodis A, Shepherd S, et al. Food & Nutrition Throughout Life. 1st ed. Allen & Unwin; 2015.
75. NHMRC. Dietary Fibre | Nutrient Reference Values [Internet]. Australian National Health and Medical Research Council. 2019 [cited 2021 May 10]. Available from: https://www.nrv.gov.au/nutrients/dietary-fibre
76. Caffeine [Internet]. [cited 2022 Jul 13]. Available from: https://www.foodstandards.gov.au/consumer/ generalissues/Pages/Caffeine.aspx
77. Australian Government. Australian Alcohol Guidelines revised | Australian Government Department of Health and Aged Care [Internet]. Department of Health and Aged Care. 2020 [cited 2022 Sep 26]. Available from: https:// www.health.gov.au/news/australian-alcohol-guidelines-revised
78. Australian Government Department of Health. Standard drinks guide | Australian Government Department of Health [Internet]. Australian Government Department of Health. 2020 [cited 2021 Jun 15]. Available from: https://www.health.gov.au/health-topics/alcohol/about-alcohol/standard-drinksguide?utm_source=alcohol.gov.au&utm_medium=redirect&utm_campaign=digital_transformation&utm_ content=%2Finternet%2Falcohol%2Fpublishing.nsf%2FContent%2Fdrinksguide-cnt
79. NHMRC. Nutrients | Nutrient Reference Values [Internet]. Australian Government National Health and Medical Research Council. 2014 [cited 2021 Mar 17]. Available from: https://www.nrv.gov.au/nutrients
80. Recommended number of serves for adults | Eat For Health [Internet]. [cited 2022 Jul 13]. Available from: https:// www.eatforhealth.gov.au/food-essentials/how-much-do-we-need-each-day/recommended-number-servesadults
81. Jäger R, Kerksick CM, Campbell BI, Cribb PJ, Wells SD, Skwiat TM, et al. International Society of Sports Nutrition Position Stand: protein and exercise. J Int Soc Sport Nutr 2017 141 [Internet]. 2017 Jun 20 [cited 2022 Jul 4];14(1):1–25. Available from: https://jissn.biomedcentral.com/articles/10.1186/s12970-017-0177-8
82. Burke LM, Hawley JA, Wong SHS, Jeukendrup AE. Carbohydrates for training and competition. J Sports Sci [Internet]. 2011 Jan 9 [cited 2021 Feb 5];29(sup1):S17–27. Available from: https://www.tandfonline.com/doi/full/10 .1080/02640414.2011.585473
83. Sutton EF, Bray GA, Burton JH, Smith SR, Redman LM. No evidence for metabolic adaptation in thermic effect of food by dietary protein. Obesity (Silver Spring) [Internet]. 2016 Aug 1 [cited 2022 Sep 26];24(8):1639. Available from: /pmc/articles/PMC4963285/
84. Zhang YJ, Gan RY, Li S, Zhou Y, Li AN, Xu DP, et al. Antioxidant phytochemicals for the prevention and treatment of chronic diseases. Molecules [Internet]. 2015 Nov 27 [cited 2021 Apr 6];20(12):21138–56. Available from: /pmc/ articles/PMC6331972/
85. NIH National Institute of Health. Botanical Dietary Supplements - Background Information - Consumer [Internet]. NIH National Institute of Health. 2020 [cited 2022 Sep 26]. Available from: https://ods.od.nih.gov/ factsheets/BotanicalBackground-Consumer/
86. Pichersky E, Raguso RA. Why do plants produce so many terpenoid compounds? New Phytol [Internet]. 2018 Nov 1 [cited 2021 Apr 6];220(3):692–702. Available from: http://doi.wiley.com/10.1111/nph.14178
87. Hui C, Qi X, Qianyong Z, Xiaoli P, Jundong Z, Mantian M. Flavonoids, Flavonoid Subclasses and Breast Cancer Risk: A Meta-Analysis of Epidemiologic Studies. Polyak SJ, editor. PLoS One [Internet]. 2013 Jan 18 [cited 2021 Apr 6];8(1):e54318. Available from: https://dx.plos.org/10.1371/journal.pone.0054318
88. Khoo HE, Azlan A, Tang ST, Lim SM. Anthocyanidins and anthocyanins: Colored pigments as food, pharmaceutical ingredients, and the potential health benefits. Food Nutr Res [Internet]. 2017 [cited 2021 Feb 11];61(1). Available from: /pmc/articles/PMC5613902/
89. Proestos C. Superfoods: Recent data on their role in the prevention of diseases. Curr Res Nutr Food Sci. 2018 Dec 1;6(3):576–93.
90. Zeng Y, Pu X, Du J, Yang X, Li X, Mandal MSN, et al. Molecular Mechanism of Functional Ingredients in Barley to Combat Human Chronic Diseases. Oxid Med Cell Longev. 2020;2020.
91. Zeng Y, Pu X, Yang J, Du J, Yang X, Li X, et al. Preventive and therapeutic role of functional ingredients of barley grass for chronic diseases in human beings. Oxid Med Cell Longev. 2018;2018.
92. Eteraf-Oskouei T, Najafi M. Traditional and modern uses of natural honey in human diseases: A review. Iran J Basic Med Sci [Internet]. 2013 Jun [cited 2021 Apr 7];16(6):731–42. Available from: www.mums.ac.ir/basic_ medical/en/index
93. Nguyen HTL, Panyoyai N, Kasapis S, Pang E, Mantri N. Honey and its role in relieving multiple facets of atherosclerosis. Nutrients [Internet]. 2019 Jan 1 [cited 2021 Apr 7];11(1):167. Available from: www.mdpi.com/

94. Cianciosi D, Forbes-Hernández TY, Afrin S, Gasparrini M, Reboredo-Rodriguez P, Manna PP, et al. Phenolic compounds in honey and their associated health benefits: A review. Molecules [Internet]. 2018 Sep 11 [cited 2021 Apr 7];23(9). Available from: /pmc/articles/PMC6225430/
95. Albaridi NA. Antibacterial Potency of Honey. Int J Microbiol [Internet]. 2019 [cited 2021 Apr 7];2019. Available from: /pmc/articles/PMC6589292/
96. Cheung Y, Meenu M, Yu X, Xu B. Phenolic acids and flavonoids profiles of commercial honey from different floral sources and geographic sources. Int J Food Prop [Internet]. 2019 Jan 1 [cited 2021 Apr 7];22(1):290–308. Available from: https://www.tandfonline.com/doi/full/10.1080/10942912.2019.1579835
97. Routray W, Orsat V. Blueberries and Their Anthocyanins: Factors Affecting Biosynthesis and Properties. Compr Rev Food Sci Food Saf [Internet]. 2011 Nov 1 [cited 2021 Apr 9];10(6):303–20. Available from: http://doi.wiley. com/10.1111/j.1541-4337.2011.00164.x
98. Kalt W, Cassidy A, Howard LR, Krikorian R, Stull AJ, Tremblay F, et al. Recent Research on the Health Benefits of Blueberries and Their Anthocyanins. Adv Nutr [Internet]. 2020 Mar 1 [cited 2021 Feb 11];11(2):224–36. Available from: https://doi.org/10.1093/advances/nmz065.
99. Katz DL, Doughty K, Ali A. Cocoa and chocolate in human health and disease. Antioxidants Redox Signal [Internet]. 2011 Nov 15 [cited 2021 Feb 11];15(10):2779–811. Available from: /pmc/articles/PMC4696435/
100. Oracz J, Nebesny E. Antioxidant Properties of Cocoa Beans ( Theobroma cacao L.): Influence of Cultivar and Roasting Conditions. Int J Food Prop [Internet]. 2016 Jun 2 [cited 2021 Feb 11];19(6):1242–58. Available from: https://www.tandfonline.com/doi/full/10.1080/10942912.2015.1071840
101. Nehlig A. The neuroprotective effects of cocoa flavanol and its influence on cognitive performance. Br J Clin Pharmacol [Internet]. 2013 Mar [cited 2021 Apr 1];75(3):716–27. Available from: /pmc/articles/PMC3575938/
102. Nehlig A. The neuroprotective effects of cocoa flavanol and its influence on cognitive performance. Br J Clin Pharmacol [Internet]. 2013 Mar [cited 2021 Apr 8];75(3):716–27. Available from: /pmc/articles/PMC3575938/
103. Hrncic MK, Ivanovski M, Cör D, Knez Ž. Chia Seeds (Salvia Hispanica L.): An overview-phytochemical profile, isolation methods, and application. Molecules [Internet]. 2020 [cited 2021 Apr 7];25(1). Available from: /pmc/ articles/PMC6994964/
104. Ullah R, Nadeem M, Khalique A, Imran M, Mehmood S, Javid A, et al. Nutritional and therapeutic perspectives of Chia (Salvia hispanica L.): a review. J Food Sci Technol [Internet]. 2016 Apr 1 [cited 2021 Feb 11];53(4):1750–8. Available from: /pmc/articles/PMC4926888/
105. Khushboo R, Dilipkumar P. CHIA SEED IN HEALTH AND DISEASE PREVENTION: PRESENT USAGE AND FUTURE PERSPECTIVES | INTERNATIONAL JOURNAL OF PHARMACEUTICAL SCIENCES AND RESEARCH. Int J Pharm Sci Res [Internet]. 2020 [cited 2021 Feb 11]; Available from: https://ijpsr.com/bft-article/chia-seed-inhealth-and-disease-prevention-present-usage-and-future-perspectives/?view=fulltext
106. Karkos PD, Leong SC, Karkos CD, Sivaji N, Assimakopoulos DA. Spirulina in clinical practice: Evidence-based human applications. Evidence-based Complement Altern Med [Internet]. 2011 [cited 2021 Feb 11];2011. Available from: /pmc/articles/PMC3136577/
107. Vanková K, Marková I, Jašprová J, Dvorák A, Subhanová I, Zelenka J, et al. Chlorophyll-mediated changes in the redox status of pancreatic cancer cells are associated with its anticancer effects. Oxid Med Cell Longev [Internet]. 2018 [cited 2021 Apr 8];2018. Available from: /pmc/articles/PMC6051000/
108. Dinicolantonio JJ, Bhat AG, Okeefe J. Effects of spirulina on weight loss and blood lipids: A review. Open Hear [Internet]. 2020 Mar 8 [cited 2021 Feb 11];7(1):1003. Available from: /pmc/articles/PMC7061888/
109. Bito T, Okumura E, Fujishima M, Watanabe F. Potential of chlorella as a dietary supplement to promote human health. Nutrients [Internet]. 2020 Sep 1 [cited 2021 Feb 11];12(9):1–21. Available from: /pmc/articles/PMC7551956/
110. Halperin SA, Smith B, Nolan C, Shay J, Kralovec J. Safety and immunoenhancing effect of a Chlorella-derived dietary supplement in healthy adults undergoing influenza vaccination: Randomized, double-blind, placebocontrolled trial. CMAJ [Internet]. 2003 Jul 22 [cited 2021 Feb 11];169(2):111–7. Available from: /pmc/articles/ PMC164975/
111. Rzymski P, Budzulak J, Niedzielski P, Klimaszyk P, Proch J, Kozak L, et al. Essential and toxic elements in commercial microalgal food supplements. J Appl Phycol [Internet]. 2019 Dec 1 [cited 2021 Feb 11];31(6):3567–79. Available from: https://doi.org/10.1007/s10811-018-1681-1
112. Dimidi E, Cox SR, Rossi M, Whelan K. Fermented foods: Definitions and characteristics, impact on the gut microbiota and effects on gastrointestinal health and disease. Nutrients [Internet]. 2019 Aug 1 [cited 2021 Feb 11];11(8). Available from: /pmc/articles/PMC6723656/
113. Huang CH, Li SW, Huang L, Watanabe K. Identification and classification for the Lactobacillus casei group. Front Microbiol [Internet]. 2018 Aug 22 [cited 2021 Apr 9];9(AUG):22. Available from: /pmc/articles/PMC6113361/

114. Di Cerbo A, Palmieri B, Aponte M, Morales-Medina JC, Iannitti T. Mechanisms and therapeutic effectiveness of lactobacilli. J Clin Pathol [Internet]. 2016 Mar 1 [cited 2021 Apr 9];69(3):187–203. Available from: /pmc/articles/ PMC4789713/
115. Ma ZF, Zhang H, Teh SS, Wang CW, Zhang Y, Hayford F, et al. Goji berries as a potential natural antioxidant medicine: An insight into their molecular mechanisms of action. Oxid Med Cell Longev. 2019;2019.
116. Ma ZF, Zhang H, Teh SS, Wang CW, Zhang Y, Hayford F, et al. Goji berries as a potential natural antioxidant medicine: An insight into their molecular mechanisms of action. Oxid Med Cell Longev [Internet]. 2019 [cited 2021 Feb 11];2019. Available from: /pmc/articles/PMC6343173/
117. Kulczyski B, Gramza-Michałowska A. Goji Berry (Lycium barbarum): Composition and Health Effects - A Review. Polish J Food Nutr Sci. 2016 Jun 1;66(2):67–75.
118. Fujioka N, Ransom BW, Carmella SG, Upadhyaya P, Lindgren BR, Roper-Batker A, et al. Harnessing the power of cruciferous vegetables: Developing a biomarker for brassica vegetable consumption using urinary 3,3’-diindolylmethane. Cancer Prev Res [Internet]. 2016 Oct 1 [cited 2021 Feb 11];9(10):788–93. Available from: / pmc/articles/PMC5220883/
119. Šamec D, Urli B, Salopek-Sondi B, Samec D, Urli B. Critical Reviews in Food Science and Nutrition Kale (Brassica oleracea var. acephala) as a superfood: Review of the scientific evidence behind the statement Kale (Brassica oleracea var. acephala) as a superfood: Review of the scientific evidence behind th. 2018 [cited 2021 Apr 1]; Available from: http://www.tandfonline.com/action/journalInformation?journalCode=bfsn20
120. Carlsen MH, Halvorsen BL, Holte K, Bøhn SK, Dragland S, Sampson L, et al. The total antioxidant content of more than 3100 foods, beverages, spices, herbs and supplements used worldwide. Nutr J [Internet]. 2010 [cited 2021 Apr 1];9(1):3. Available from: /pmc/articles/PMC2841576/
121. Royston KJ, Tollefsbol TO. The Epigenetic Impact of Cruciferous Vegetables on Cancer Prevention. Curr Pharmacol Reports [Internet]. 2015 Feb 1 [cited 2021 Apr 1];1(1):46–51. Available from: /pmc/articles/PMC4354933/
122. Bajaj JK, Salwan P, Salwan S. Various possible toxicants involved in thyroid dysfunction: A review. J Clin Diagnostic Res [Internet]. 2016 Jan 1 [cited 2021 Feb 11];10(1):FE01–3. Available from: /pmc/articles/ PMC4740614/
123. Bourrie BCT, Willing BP, Cotter PD. The microbiota and health promoting characteristics of the fermented beverage kefir. Front Microbiol [Internet]. 2016 [cited 2021 Feb 11];7(MAY). Available from: /pmc/articles/ PMC4854945/
124. Bourrie BCT, Willing BP, Cotter PD. The microbiota and health promoting characteristics of the fermented beverage kefir. Front Microbiol [Internet]. 2016 [cited 2021 Apr 9];7(MAY). Available from: /pmc/articles/ PMC4854945/
125. Prado MR, Blandón LM, Vandenberghe LPS, Rodrigues C, Castro GR, Thomaz-Soccol V, et al. Milk kefir: Composition, microbial cultures, biological activities, and related products. Front Microbiol [Internet]. 2015 [cited 2021 Apr 9];6(OCT). Available from: /pmc/articles/PMC4626640/
126. Cherry P, O’hara C, Magee PJ, Mcsorley EM, Allsopp PJ. Risks and benefits of consuming edible seaweeds. Nutr Rev [Internet]. 2019 May 1 [cited 2021 Apr 1];77(5):307–29. Available from: /pmc/articles/PMC6551690/
127. Cherry P, O’hara C, Magee PJ, Mcsorley EM, Allsopp PJ. Risks and benefits of consuming edible seaweeds. Nutr Rev [Internet]. 2019 May 1 [cited 2021 Feb 11];77(5):307–29. Available from: /pmc/articles/PMC6551690/
128. Gore RD, Palaskar SJ, Bartake AR. Wheatgrass: Green blood can help to fight cancer. J Clin Diagnostic Res [Internet]. 2017 Jun 1 [cited 2021 Feb 11];11(6):ZC40–2. Available from: /pmc/articles/PMC5534514/
129. ACCC. Organic claims | ACCC [Internet]. ACCC Australian Competition &Consumer Commision. 2022 [cited 2022 Sep 26]. Available from: https://www.accc.gov.au/consumers/groceries/organic-claims
130. Genuis SJ, Sears ME, Schwalfenberg G, Hope J, Bernhoft R. Clinical detoxification: Elimination of persistent toxicants from the human body. Sci World J. 2013;2013.
131. Cline JC. Cline-Nutrition, Detox, and Clinical Practice 54 ALTERNATIVE THERAPIES. Altern Ther Heal Med. 21(3):54–63.
132. Chiang J. Liver Physiology: MetaboLism and Detoxification. In: Pathobiology of Human Disease: A Dynamic Encyclopedia of Disease Mechanisms. Elsevier Inc.; 2014. p. 1770–82.
133. Ferrero ME. Rationale for the Successful Management of EDTA Chelation Therapy in Human Burden by Toxic Metals. Biomed Res Int [Internet]. 2016 [cited 2021 Feb 10];2016. Available from: /pmc/articles/PMC5118545/
134. Loeffelholz C von, Birkenfeld A. The Role of Non-exercise Activity Thermogenesis in Human Obesity. Endotext [Internet]. 2018 Apr 9 [cited 2022 Sep 27]; Available from: https://www.ncbi.nlm.nih.gov/books/NBK279077/
135. Schwingshackl L, Dias S, Hoffmann G. Impact of long-term lifestyle programmes on weight loss and cardiovascular risk factors in overweight/obese participants: a systematic review and network meta-analysis. Syst Rev [Internet]. 2014 May 1 [cited 2022 Sep 27];3(1):130. Available from: /pmc/articles/PMC4227972/
136. Farlex Medical Dictionary. Contraindication | definition of contraindication by Medical dictionary [Internet]. Farlex

Medical Dictionary. 2022 [cited 2022 Sep 27]. Available from: https://medical-dictionary.thefreedictionary.com/ contraindication
137. Health Knowledge. Social, behavioural and other determinants of the choice of diet | Health Knowledge [Internet]. Health Knowledge Education. 2008 [cited 2022 Sep 27]. Available from: https://www.healthknowledge.org. uk/public-health-textbook/disease-causation-diagnostic/2e-health-social-behaviour/social-behaviouraldeterminants#5
138. Ebrahimi M, Nia FR, Damirchi A, Mirzaie B, Pur SA. Effect of Short-term Exercise on Appetite, Energy Intake and Energy-regulating Hormones. Iran J Basic Med Sci [Internet]. 2013 [cited 2022 Sep 27];16:829–34. Available from: www.mums.ac.ir/basic_medical/en/index
139. Alkahtani SA, Byrne NM, Hills AP, King NA. Acute interval exercise intensity does not affect appetite and nutrient preferences in overweight and obese males. Asia Pac J Clin Nutr. 2014;23(2):232–8.
140. FSANZ. Food safety standards (Australia only) [Internet]. Food Standards Australia New Zealand. 2015 [cited 2022 Sep 27]. Available from: https://www.foodstandards.gov.au/industry/safetystandards/pages/default. aspx
141. Food Standards Australia New Zealand. Temperature control [Internet]. Food Standards Australia New Zealand. [cited 2022 Sep 27]. Available from: https://www.foodstandards.gov.au/consumer/safety/faqsafety/ pages/foodsafetyfactsheets/charitiesandcommunityorganisationsfactsheets/temperaturecontrolma1477.
