









How will we look back on this time in a few years? I will not be the only one to owe you this answer for a while, because we are not yet out of the woods in this crisis. Even if the situation is easing, it has left clear traces. And that on several levels.
The economic situation of eye care practitioners was determined by several factors, including how much a business was affected by the corona crisis. It turned out that the services, range of products and the modalities decided how much turnover could be made. The possibility of online reorders also helped some practices not only to keep their heads above water, but to do good business.

This crisis has also – and this could be foreseen quite early –brought technologies forward as if on steroids. Even if the classic contact lens fitter could hardly use home offices, video conferencing or digital consultations with his customers, websites were updated, possibilities for online bookings were set up, appointments were made and virtual visits to trade fairs or even online classes for further education were taken.
Let's look a little further outside the box: imagine you put on your prescription glasses, have just read an article in GlobalCONTACT – a sudden buzz tells you that an email has just come in. A tap on your temple – and a virtual rectangular display appears crisply sharp at a distance of about 1-2 m in front of you, with the email that has just come in. If someone is sitting opposite you at this moment, they will only notice that you have changed your gaze by a few degrees. Immediately afterwards, you use this display to select a new song from your Spotify playlist while looking at your photo stream from your last holiday.
Utopia? Not at all. This technology is already beyond prototype status and has the first devices in use. This possibility was created by a joint venture between Zeiss and Telekom.
Another interesting possibility in this field is eMacula, which we present in this issue. Here, contact lenses play a big role in binocular vision and in experiencing the brave new world of mixed reality. Read our interview with Jerry Legerton starting on page 26.
For now, use our print edition – and if that's too old-fashioned for you, feel free to use our GlobalCONTACT app with further content directly on your smartphone or tablet. You’re welcome. ■

Highest surface accuracy and quality meet unprecedented productivity.

The compact and fully featured UPC 100 Vision is optimized for highly dynamic diamond turning of complex freeform surfaces like polish-free IOLs, mold inserts or complex contact lens designs.
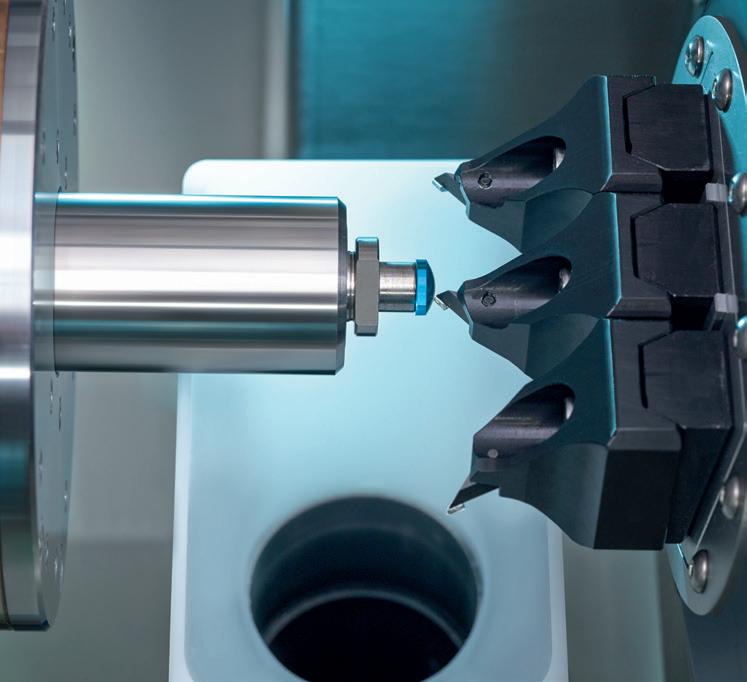
The UPC nano is the most affordable and compact machine with on-board freeform capabilities and an optional laser for manufacturing high-quality contact lenses at maximum cost-efficiency.

Both machines can be easily integrated with an optional automation system.

Title: Contamac, www.contamac.com
Inside front cover: Bausch + Lomb Inc., www.bausch.com
Page 4: Schneider GmbH & Co. KG, www.schneider-om.com
Page 7: LAMBDA-X S.A., www.lambda-x.com



Page 19: OPTOCRAFT GmbH, www.optocraft.com
Page 25: Larsen Equipment Design Inc., www.larsenequipment.com
Page 29: AMETEK Precitech, Inc., www.precitech.com
Page 37: Optimec Systems Ltd., www.optimecsystems.com
Page 39: K&Y Diamond Ltd, www.kydiamond.ca
Inside back cover: Efclin, www.efclin.com
Outside back cover: DAC International, Inc., www.dac-intl.com
Bennett, Alan 12 Jungwirth, Carola 40 Kinder, Alina 30 Kurz, Corinna 15 Lagodny, Matthias 15 Larsen, Erik 36 Lee, William 12 Legerton, Jerome 26 Roth, Hans-Walter 20 van der Worp, Eef 16, 38
LETTER
EDITOR
Opportunities and crises Silke Sage
INTERNATIONAL NEWS
All about you & Event dates


All about markets
All about products
All about research
INTERVIEW
With Alan Bennett and Dr. William Lee – Meet the new board members of EFCLIN Silke Sage
With Jerry Legerton – Extended reality for vision impaired Silke Sage


20 Kevin Tuohy Hans-Walter Roth
Imaging techniques – case study Corinna Kurz & Matthias Lagodny
Mind the gap Eef van der Worp
TECHNOLOGY
The importance of poroelasticity in soft contact lenses Alina Kinder REPORT
Menicon anniversary: 70 years Rebekka Nurkanovic
What a difference a year makes Erik Larsen
COLUMN
Glasses are for drinking Eef van der Worp
BUSINESS + MARKETING
Successful handover in family businesses Carola Jungwirth SERVICE
The board of Euromcontact met on 15th June 2021 to discuss the priorities for the organization from June 2021 onwards and elect its bureau.
Nicoletta Losi, Professional Education & Development Director in EMEA
for Johnson & Johnson Vision, was unanimously elected for a third mandate of two years.
Nicoletta Losi was first elected in May 2017 and again in June 2019 by her peers at the board. Nicoletta Losi has been a board member of Euromcontact since 2009 and was previously president of ASSOTTICA, the Italian association of contact lens manufacturers. Nicoletta has extensive experience in professional affairs education and in KOL strategy and development. The board of Euromcontact also unanimously supported the re-election of Marion Beeler, Secretary General of EFCLIN, as treasurer and of Simon Rodwell, Secretary General of ACLM, as secretary.

Discussing the priorities from June 2021 onwards, the board agreed to continue the efforts to support the business in the transition from the Medical Devices Directive to the Medical Devices Regulation and to work on distribution channels to support the contact lens consumer journey. Euromcontact also supports the European agenda towards more sustainability and will continue to engage with contact lens wearers and eye care professionals to increase education on waste collection.
A new study by Lenstore has analyzed the top countries around the world that are the most addicted to their screens. In terms of screen time, Filipinos are the most avid phone users with an average of ten hours of screen time per day since the outbreak of COVID-19, a 17-minute increase from January 2020. South Africa and Brazil are next in line with an average of 9.39 and 9.34 hours of screen time respectively. Residents in Japan, on the other hand, are the least addicted to their phones with an average of just 4.30 hours of screen time each day, followed by the Netherlands who look at their screens for 4.45 hours. Germany, Denmark and France all have an average screen time of just over five hours.
During the past year, computer and mobile screen usage drastically increased on a global scale. A staggering 76% of the population between 16 and 24 are spending more time on their phones, while 45% have increased the amount of time they spend on their laptops. And it’s not just phones and laptops that are the digital culprits: 34% of the population is spending more time watching TV, while 22% have increased their tablet usage. According to behavioural optometrist, Bhavin Shah, staring at screens can have a big impact on transient blurry vision, an increased need for wearing glasses, the discomfort of the eyes, and performance at work. It can also have a detrimental effect on our neck and shoulders.
Webinar: Contact lenses and allergy –fixing that itch (BCLA members only) www.bcla.org.uk
ICSC 2021 www.icscmeeting.com
ECLSO Symposium www.eclso.eu
IOFT 2021 International Optical Fair Tokyo www.ioft.jp/en-gb.html
American Academy of Optometry https://academymeeting.org/
ECLSO Symposium www.eclso.eu
July 14
July 23-24
online event
Fort Lauderdale, FL (USA)
Sep 4 online event
Oct 18-20
Tokyo (JPN)
Nov 3-6 Boston, MA (USA)
Nov 26-28 Sibiu (Rumania)

BostonSight has announced the election of Dr. Howard Purcell and Mr. Ron Remy to the board of directors.
Dr. Purcell is the current president and CEO of the New England College of Optometry (NECO). He began his optometric career in a group optometric practice. In 1991, he joined the faculty of Nova
Southeastern University College of Optometry, where he was a principal in the development of the department of cornea and contact lenses. Dr. Purcell has also served as the senior vice president, customer development for Essilor of America and senior director of professional affairs for Johnson & Johnson Vision Care. He is a diplomate in the Cornea and Contact Lens Section of the American Academy of Optometry and a graduate of NECO.
Mr. Remy is the chief executive officer at Mobile Heartbeat, a software company that improves clinical collaboration by connecting patients’ care teams through a single, unified platform. Mr. Remy has more than 20 years of technology management and leadership experience.
He has served as president and CEO of Auspice Corporation, and chief operating officer of Modiv Media and BioMed 20/20 Technologies. He began his career as a systems engineer for Sun Microsystems. He holds a BS in electrical engineering from Brown University and an MBA from Harvard Business School.


Furthering its commitment to address the global epidemic of childhood myopia, the World Council of Optometry (WCO) board of directors unanimously approved a resolution advising optometrists to incorporate a standard of care for myopia management within their practices.
The resolution defines the evidence-based standard of care as comprising of three main components:
• Mitigation – optometrists educating and counseling parents and children, during early and regular eye exams, on lifestyle, dietary, and other factors to prevent or delay the onset of myopia.
• Measurement – optometrists evaluating the status of a patient during regular comprehensive vision and eye health exams, such as measuring refractive error and axial length whenever possible.

• Management – optometrists addressing patients’ needs of today

by correcting myopia, while also providing evidence-based interventions (e.g., contact lenses, spectacles, pharmaceuticals) that slow the progression of myopia, for improved quality of life and better eye health today and into the future.
It also advises optometrists to incorporate within their practice the standard of care for myopia management, which shifts from simply correcting vision to managing the condition, and includes public education and early, frequent discussions with parents that explain:
• What myopia is.
• Lifestyle factors that may impact myopia.
• The increased risks to long-term ocular health that myopia brings.
• The available approaches that can be used to manage myopia and slow its progression.
The standard of care resolution can be found in its entirety on the World Council of Optometry’s website, here: https://worldcouncilofoptometry.info/advocacy/
in the first quarter of 2021, following a contraction of (minus) 0.7% in the previous quarter. Among G20 economies, China, which was affected by COVID-19 at an earlier stage than other countries, recorded the highest annual growth (18.3%), while the UK recorded the largest annual fall (minus 6.1%).

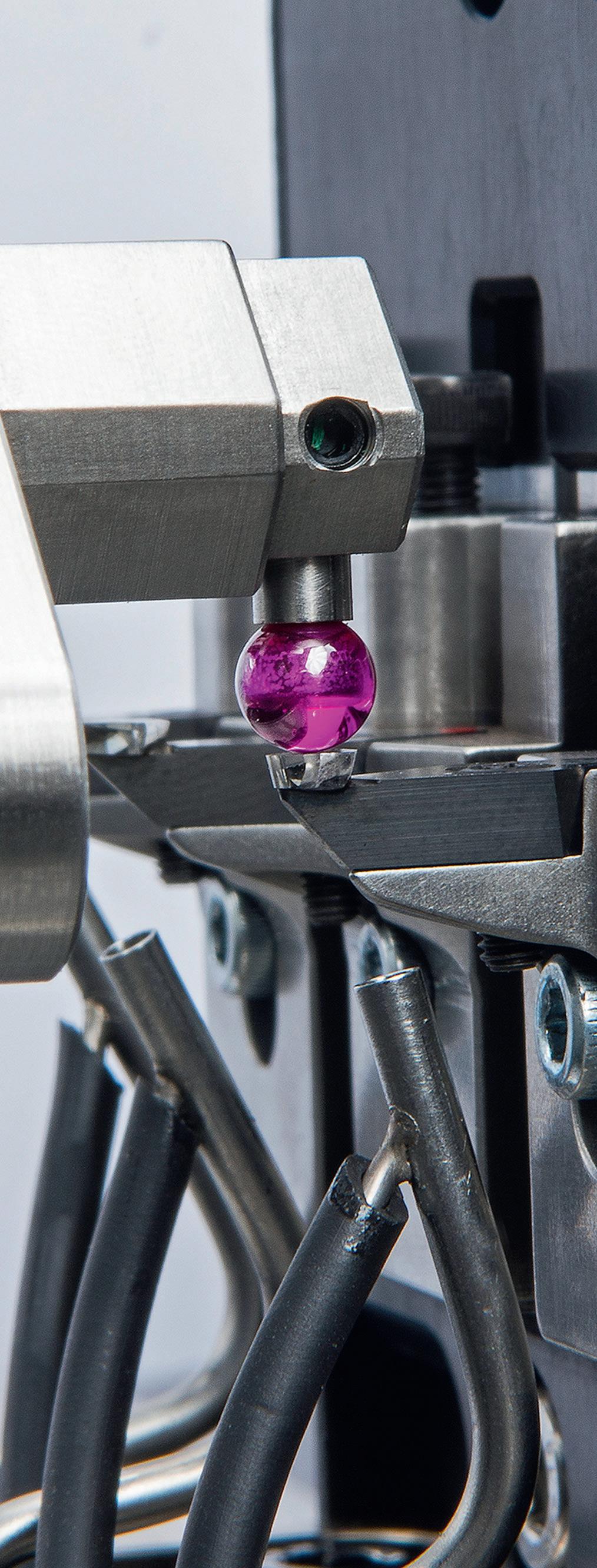
At K&Y Diamond Ltd, it’s all about finding the best solutions for our valued customers. Whether it’s manufacturing a special diamond tool used to make scleral lenses (as shown) or helping to solve surface finish issues, out team of dedicated technicians and engineers are always willing to go the extra mile. It’s one reason why we’ve grown into one of the world’s largest manufacturers of single-crystal diamond tools used to make RGP lenses, IOL’S and optical molds. Our diamonds are in both large and small labs in over 60 countries. It’s earned us a reputation for delivering a superior product at a fair price. Our consistent growth allows us to invest in both state-of-the art manufacturing systems and the latest metrology; some of which is found nowhere else. If you’re not using us for your tooling needs, why not? Let us put our +40 years of experience to work for you! kydiamond@kydiamond.ca, www.kydiamond.ca

Comprehensive IOL testing in R&D WaveMaster® IOL 2 is TRIOPTICS universal measuring system for the quality control of all common refractive intraocular lenses such as monofocal, toric, spherical and aspherical lenses. Based on a Shack-Hartmann sensor the system runs fully automatically and user independently. It determines refractive power, lens aberrations with comprehensive Zernike analysis, toric axis deviation and marker orientation, MTF, EFL and PSF. Measurements are possible in air as well as in the heated in-situ model eye that was designed in accordance with ISO 11979. With a measurement accuracy that is three times more exact than required in ISO, the WaveMaster IOL 2 is the perfect choice for each R&D lab. info@trioptics.com, www.trioptics.com

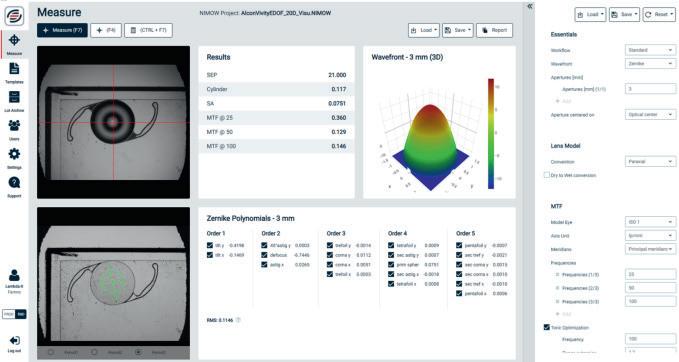
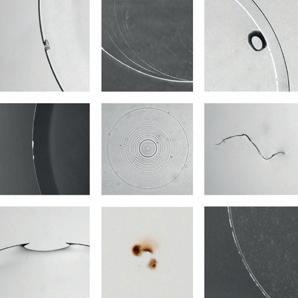
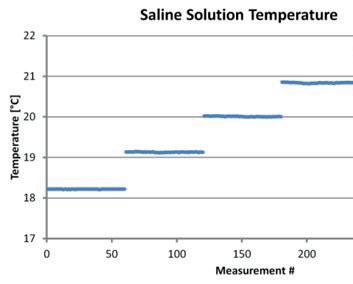
Contact lens metrology – NIMOEVO & CLE-MENTOR’s API: a success story illustrated by the NIMO/FocalPoints integration. Medical Device Regulation (MDR) has become a major point of concern for all contact lenses manufacturers. Today, a metrology tool cannot only be reliable and performant, it also requires a high level of data safety and traceability. Thanks to its database and its powerful API (Application Programming Interface), NIMO has been efficiently interfaced with the ERP system of several Labs. Among the new functionalities of CLE-MENTOR, discover the NIMO/ FocalPoints integration now in operation in various Specialty Labs. See our customer testimonials here: https://www.lambda-x.com/en/nimo-focalpoints sales-ophthalmics@lambda-x.com , www.lambda-x.com

Information technology increasingly finds its way into health research. Two studies show how smart contact lenses are intended to help diagnose and treat diabetes. The pre-lens drying time of two types of daily disposable contact lenses was the focus of research by Sebastian Marx, Julia Eckstein and Wolfgang Sickenberger.
concentration in the conjunctival blood vessels by analyzing the near infrared light. They put their LED contact lenses on rabbit eyes with diabetic retinopathy disease and irradiated light repeatedly for a month. As a result, they confirmed that there was significant reduction of angiogenesis (production of new blood vessels) in the retina and verified the clinical feasibility of the smart LED contact lens for the diabetic retinopathy therapy. This device is supposed to let diabetic patients monitor their blood-sugar level in real-time and also enable medical treatment for retinopathy which is caused by diabetic complications.
Geon-Hui Lee, Hanul Moon, Hyemin Kim, and a team of researchers developed a technology that allows diagnosis of diabetes and treatment of diabetic retinopathy by wearing a 'smart light-emitting diode (LED) contact lens.'
The team invented a photonic contact lens and a wearable medical device which can diagnose diabetes and treat diabetic retinopathy. The research team developed a contact lens with integrated micro LED and photodetector which can measure glucose
Based on these results, the team also developed a wearable medical device to analyze glucose concentration in sweat, and verified that it could be clinically feasible for diabetes diagnosis. With the company PHI Biomed, they developed a blue-tooth system that can send data wirelessly, with the goal of allowing patients to check their diabetic diagnostic results on their mobile phones.
Sources: Abstract of the study [1], EurekAlert 2020-02-10 [2]

artificial tears in the channels were measured at different levels of hydration, with zero flow measured at complete dehydration and full spontaneous flow observed at full hydration.
A collaborative team, which includes a group from the Terasaki Institute for Biomedical Innovation, has developed a fabrication method to meet the challenges in making a hydrogel contact lens for biomarker sensing. The work was supported by a grant from CooperVision. The team began by optimizing the components of the hydrogel to obtain elastic characteristics which would allow it to be engineered into various shapes with a smooth surface profile. They next fashioned microchannels in the hydrogel with the use of a 3D printed mold. The final step in the fabrication process was to enclose the hydrogel channels by bonding an additional layer of hydrogel onto the microchannel surface.
Once the prototype was completed, it was tested for its performance in channeling and collecting fluids. Flow rates of
The wettability of a contact lens plays an important role in the experience of comfort for its wearer. Sebastian Marx, Julia Eckstein and Wolfgang Sickenberger have evaluated the non-invasive pre-lens drying time of two types of daily disposable contact lenses (DDCLs) after twelve hours of wear in vivo.

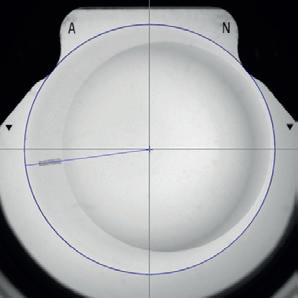
As stated in the abstract of the paper the prospective, randomized, single-center, cross-over pilot study evaluated 31 subjects aged 18–44 years with normal eyes and good tear film stability who were adapted soft contact lens wearers at the time. The researchers had the subjects wear Nelfilcon A and Stenfilcon A DDCLs for twelve hours each on two different days. They recorded non-invasive video keratography drying-up time (NIK-DUT) videos of each eye twelve hours after lens insertion for about 25 seconds. A five minute tear film recovery time was allowed between video recordings of the right and left eyes to avoid bias. The team measured the post-blink time required to reach 15% distortion of the projected rings and the speed of break-up at 15 seconds post-blink at each time point. They determined the on-eye wettability by ring mire projection under white light illumination.
Referenzen:
A noteworthy observation during these tests was that when the hydrogel was mildly dehydrated, liquid flow in the channels would stop, but when additional rhythmic pressure was applied, the flow would resume. This was a demonstration of support for the hypothesis that eye blinking would also provide the necessary pressure and additional hydration needed to allow for tear flow in the contact lens, and therefore, in the eye.
Next, the team prototyped sensors to collect, test for and measure pH levels of artificial tears flowing through the microchannels. Sodium levels were also tested, and the results showed an acceptable and predicted range of sodium detection for diagnostic purposes.
Additional goals would be to fine-tune factors such as humidity, hydrogel hydration and applied pressure in order to enhance all the flow rates and dynamics of the biosensing contact lens. There are also plans to experiment with smaller channels in thinner hydrogel films before a final contact lens is devised.

Sources: Abstract of the study [3], EurekAlert 2020-11-23 [4]
The researchers found that the mean time to reach 15% ring distortion was similar for Nelfilcon A and Stenfilcon A DDCLs but varied highly among subjects. The mean speed of break-up at 15 sec post-blink is reported as 0.3±0.38% distortion/sec for Nelfilcon A and 0.2±0.23% distortion/sec for Stenfilcon A DDCLs.
Marx, Eckstein and Sickenberger came to the conclusion that multifunctional topography allowed the objective evaluation of in vivo pre-lens tear film stability using ring mire projection. The researchers describe the dynamic method as being simple, fast and non-invasive, enabling measurements of NIK-DUT and evaluating wettability over an area that is larger than the optical zone of the contact lens surface, for the entire inter-blink interval.
Source: Abstract of the study [5]
[1] Lee, GH., Moon, H., Kim, H. et al. Multifunctional materials for implantable and wearable photonic healthcare devices. Nat Rev Mater 5, 149–165 (2020). https://doi.org/10.1038/s41578-019-0167-3 [2] https://www.eurekalert.org/pub_releases/2020-01/puos-nnt011020.php [3] Chen, Yihang et al. Microengineered poly(HEMA) hydrogels for wearable contact lens biosensing. Lab Chip, 2020,20, 4205-4214. DOI: 10.1039/ D0LC00446D [4] https://www.eurekalert.org/pub_releases/2020-11/tifb-clf112020.php [5] Marx S, Eckstein J, Sickenberger W. Objective Analysis of Pre-Lens Tear Film Stability of Daily Disposable Contact Lenses Using Ring Mire Projection. Clin Optom (Auckl). 2020;12:203-211 https://doi.org/10.2147/OPTO.S262353
The European Federation of the Contact Lens and IOL Industries, EFCLIN, has elected two new members to its board of directors in 2021. Alan Bennett, a senior quality leader for the specialty vision products team of Bausch & Lomb, now serves as secretary to EFCLIN. Dr. William Lee, VP of R&D and regulatory affairs at AST Products, Inc. (U.S.A.) and president of ICARES Medicus, Inc. (Taiwan), has taken on the role of treasurer.
GlobalCONTACT has asked both the same seven questions. By Silke Sage
For the second year in a row, EFCLIN members were unable to meet in person due to the pandemic. On April 16, 2021 – for the first time in its history – they met online for the annual general meeting. This date also marked the end of the second period of service for two board members: Tanja Malkus , B+L Boston Materials, who served as secretary on the board, and Peter Vermeulen Ophtecs-Europe B.V., hitherto treasurer. Both were honored for their commitment to EFCLIN and their work was acknowledged.
It was also announced when the next live meeting will take place: The 2022 EFCLIN Annual Congress and Exhibition will be held from 28th to 30th April 2022 at the Melia Hotel in Sitges/Barcelona, Spain. The organizers will stay with the concept of lectures in the morning, exhibition in the afternoon.
But first things first: Let's take time to get to know the new players. 7 questions, 7 answers to Alan Bennett and Dr. William Lee.
GlobalCONTACT: Briefly describe yourself: what is your professional background and which of your skills are of particular value to EFCLIN? Bennett: My professional background was originally in the field of industrial engineering (process improvements, process measurement and operational planning) for the Royal Mail in the UK. After 20 years I needed a change and moved to Bausch & Lomb. I have been in the field of medical device quality for eleven years and have found myself increasingly involved at an industry level through collaboration with Euromcontact, the ACLM (UK) and now with EFCLIN as a newly appointed board member.

As we are all starkly aware the regulatory landscape within Europe has dramatically changed since the publication of the EU MDR, and continues to present additional challenges – such as the PFAS chemicals issue. With my strong background in quality and experience of working closely with the incredible industry associations I intend to leverage this knowledge to the industry’s benefit by working in a much more influential way with the EFCLIN community.
B e nnettLee: I am the VP of R&D and regulatory affairs at AST Products, Inc. (U.S.A.) and the president of Icares Medicus, Inc. (Taiwan). As an engineer, executive and entrepreneur, I have over 30 years of experience in surface treatment technology, and product design and development for IOLs and IOL injectors. I am the sole inventor of the LubriMATRIX surface treatment technology that has been applied onto more than five million IOL injectors annually, and was awarded the 2020 Heroes of Chemistry Award by the American Chemical Society (ACS). I obtained my Ph.D. in chemistry and biotechnology, B.Eng. and M.Eng. in chemical engineering from the University of Tokyo, Japan. I am fluent in seven languages including English, Japanese, Mandarin and Malay, and a serial Japanese calligraphy awardee in Japan.
 Dr
Dr
GlobalCONTACT: What are your goals and plans for your upcoming time as a board member?
Bennett: My primary focus is split two ways: The first is to support the industry in every way I know how in terms of the regulatory challenges that have been so prominent in our industry. There is the EU MDR – a monumental hurdle to cross for companies large or small; there are the new UK regulations (post-Brexit), and then there are the new challenges from the PFAS chemicals issue (as a result of the EU Chemicals Strategy).
The second is to help promote EFCLIN and build sustainable growth in active membership, which is why I volunteered to serve as secretary within the board structure. I have learned over the past few years that our industry has grown stronger and more effective in how it tackles regulatory and quality challenges if we all work together – one unified, stronger voice!
Lee: Firstly, to assist in expanding the network of EFCLIN to the IOL and contact lens communities around the world. Particularly, I think the IOL section of EFCLIN still has a lot of room to expand and improve in order to create more value for our members. Secondly, to match academic research with industries for more innovative commercialization of technologies that will bring value and benefits to the end users.
WITH ALL OF THE REGULATORY CHALLENGES THE INDUSTRY HAS HAD TO FOCUS ON THESE IN ORDER TO PROTECT ITSELF LONG TERM.
(ALAN BENNETT)Alan
W il liam Lee(DR. WILLIAM LEE)
GlobalCONTACT: What excites you about serving as a board member?
Bennett: Working with such a talented and energized group of industry professionals – both on the board, and being able to work more closely with the various member companies. When you get such a diverse range of talents together in one place you are always going to get a result that is something special. Our industry has the benefit of presenting endless learning opportunities, so by working with so many different people those opportunities remain fresh and exciting.
Lee: As mentioned above, to assist on expanding the IOL section of EFCLIN.
GlobalCONTACT: What have you achieved so far?
Bennett: So far, having attended my first board meeting, I have started contributing to the initial plans for the 2022 EFCLIN Congress. In the last few weeks I have also acted as moderator for the IOL edge profiles webinar delivered by Dr. Mayank Nanavaty (Consultant Ophthalmologist).
Lee: To get Santen Pharmaceutical to become a corporate member of the EFCLIN this month.
GlobalCONTACT: What does the industry need most right now?
Bennett: In short – stability! With all of the regulatory challenges that have happened over the past few years, as well as the ongoing ones, the industry has had to focus on these in order to protect itself long term. These challenges create a lot of worry that ultimately detracts from the creative process of bringing new and innovative products to market. We now need a stable period wherein we can all implement the required changes, get our organizations onto a good track and then do what we all do best – support our professional customers as they support their patients.
Lee: Integration of various technologies in order to create and commercialize the so-called smart contact lenses and smart IOLs, and eventually bring values and benefits to the end users.
GlobalCONTACT: How can EFCLIN continue to increase its number of members?

Bennett: Continue to reach out to companies that are not members and help them to understand how working with one voice will help the industry, both to endure and to grow. In addition we can extend our reach through creative use of remote working tools – something that the COVID pandemic has taught us all.
Lee: While the number is important, I think more importantly, the quality of members has to be achieved. In order to do so, EFCLIN needs to step up its standard and quality so that all members can have a win-win relationship. We need to create a common place for members to exchange ideas that would eventually lead to innovative creations. Before achieving such, we need to provide valuable lectures, seminars and an annual conference in order to attract more members and attendees.
GlobalCONTACT: What do you like to say to the members of EFCLIN?
Bennett: These difficult times will pass us by. As an industry we have amazing products that help our professional clinical colleagues to protect the precious gift of sight. EFCLIN is committed to bringing together our industry and to support its growth through innovation. Thank you to all of our members for supporting our goals, and I – along with my board colleagues – look forward to continuing to work with you all long into the future.
Lee: I am very honored to have been elected as a board member and I will try my best to bring more values to all of us in the EFCLIN family.
GlobalCONTACT: Thank you for the interview.
WE NEED TO CREATE A COMMON PLACE FOR MEMBERS TO EXCHANGE IDEAS THAT WOULD EVENTUALLY LEAD TO INNOVATIVE CREATIONS.

When looking at the back surface of the lens with the specular illumination, two sharply defined circles can be seen in the lower nasal area of the right eye in figure 1. No abnormalities are visible on the posterior surface of the left lens.
Slitlamp: 40 x magnification, specular illumination (Haag-Streit BQ 900, Koeniz, Schweiz)
The hyaloid artery, which was present during embryonic development to supply nutrients to the developing lens, started at this point. It regresses again until birth. Presumably, the posterior circle was the point of attachment of the canalis hyaloideus – also called the Cloquet's canal, which once encased the arteria hyaloidea within the vitreous body. This finding could also be mistaken for a cyst on the posterior surface of the eye lens (see image 2, 25x magnification). However, as two circles are clearly visible on picture 1 at 40x magnification (on the lens posterior surface and posterior lens capsule), the above-mentioned finding – also called Mittendorf Dot – is very likely.
This is a physiological anomaly. In rare cases, partial anopsia may occur if the hyaloid artery has not regressed (arteria hyaloidea persistens).
Treatment is not necessary in this case and a change in abnormality is not expected as the hyaloid artery has completely regressed.

The knowledge gap between understanding ocular surface shape and contact lens shape is narrowing quickly as of late, which is contributing to a better understanding of on-eye soft lens fitting characteristics and the future of the modality. It seems that one little gap needs to be closed: the gap in between the ocular surface and the back surface of the contact lens. By Eef van der Worp
A popular Netflix documentary ‘The Social Dilemma’ sheds a completely new light on social media and how this can be used in the future – an eye-opening film that perhaps everyone should see. In our soft lens arena, we are facing an equally interesting ‘dilemma’ as discussed here previously in GlobalCONTACT. In short: eye care practitioners do not ‘fit’ soft lenses; at best, they select one. But based on what? That is the big question. In line with the mentioned documentary, new technology could be a game changer for this dilemma.
Let’s start at the beginning. What do we know about the ocular surface and its shape? Parts of this have been covered in GlobalCONTACT before, as most of this research stems from
studies done on scleral shape with the sole purpose of fitting scleral lenses. Based on different methods including optical coherence tomography (OCT), profilometry and Scheimpflug technology, the overall sagittal height (OC-SAG) over a 15 mm chord in the horizontal meridian is thought to be in the 3750-micron range. Some Placido disc topographers are also capable of fairly accurately estimating the OC-SAG based on extrapolation from measured corneal data. The chord or diameter of 15 mm is chosen and generally accepted as the ‘workbench’ for soft lens fitting, because a typical soft lens is in the 14.2 mm range and allows for about 0.2 or 0.3 mm of movement on each side.
But what about individual variation within each eye? A number of recent studies looked at the amount of difference within
different (semi-)meridians of the normal eye. Consejo et al looked at anterior scleral regional variation between Asian and Caucasian populations using the Eye Surface Profiler (Eaglet Eye). They used 6 mm , 7 mm , 8 mm and 9 mm distances from the centre in 121 eyes. Looking at the 7 mm data (approximately our desired 7.5 mm half-chord, for our purposes), it showed that the maximum difference between the eight meridians (in the 0°, 45°, 90°, 135°, 180°, 225°, 270° and 315° directions) was 240 microns based on the averages of all eyes. So, this suggests that 240 microns is the amount of ‘relative flexure’ that a soft lens must go through to fully conform to the anterior ocular surface shape in different meridians/segments.
‘To flex’ is a slang term meaning ‘to show off’. Wouldn’t it be nice if we could measure the amount of OC-SAG variation within one eye? Then we could really ‘show off’ and better predict soft lens flexure on-eye. A practical question in conjunction with this is: can we measure just the horizontal OC-SAG (as this is by far the easiest to measure) to predict the overall OC-SAG value?
In considering horizontal versus vertical differences in eye dimensions, we are typically ‘stuck’ in thinking about corneal diameter and visible iris diameter (VID). Our current understanding is that the vertical VID is substantially smaller compared to the horizontal one (HVID). Hence, the common advice is to measure the oblique VID (to be in between, as an artificial average). Does this translate to OC-SAG? The difference in the Consejo paper between the average horizontal OC-SAG (H/OC-SAG) and the vertical (V/OC-SAG) of all eyes was 60 microns over a 7 mm half-chord. The difference between the average H/OC-SAG meridian and the average OC-SAG of all eyes was only 20 microns. This looks promising, but remember that these are all average values. If the OC-SAG is sometimes smaller and sometimes bigger, then the average would artificially generate a low number.
Markus Ritzmann published a paper in Contact Lens & Anterior Eye a number of years ago looking into the same matter using OCT imaging (Zeiss Visante). On 39 normal healthy subjects, he too looked at eight meridians at a distance of 7.5 mm from the centre. The difference among eyes was 118 microns. His average values show comfortably low numbers for average values similar to the Consejo paper; the difference between H/ OC-SAG and V/OC-SAG was only 13 microns, and it was only 5 microns between H/OC-SAG and the overall average OC-SAG.
Going back to the original Ritzmann source data, though, and analysing individual eyes rather than mean values as was suggested by Consejo, a slightly different picture is painted: the average eye shows 227 microns of difference (with a standard
deviation (SD) of ± 74 microns). E.g., this is the amount of relative ‘flex’ in microns of a soft lens on the eye. The minimum difference on an individual eye was 90 microns, but the maximum difference was up to 390 microns for another eye. It appears that some eyes have substantially higher OC-SAG values horizontally than vertically, but equally often it is the other way around. This explains the low ‘mean difference’ reported earlier. Comparing H/OC-SAG and V/OC-SAG in absolute terms, the difference is 109 microns (SD ± 79), with a range of 0-255 microns. For the H/OC-SAG compared to the average overall OC-SAG, this is a 79-micron difference (SD ± 49 micron), with a range of 8-190 microns. What this seems to imply is that you can measure H/OC-SAG with a given instrument, but you have to take into account that this number is ‘somewhat’ off: roughly 100 microns on average, but more for some individual eyes, of course. Hence, ideally you would measure the average OC-SAG in 360 degrees to calculate the actual average ocular surface shape. Having said that, soft lenses are very forgiving and flexible, and the clinical significance of a 100-micron variation is up for debate. To emphasise that differences between eyes and individuals exist, Consejo et al did find differences between Asian eyes and Caucasian eyes in that the Asian anterior sclera was found to be flatter than in Caucasians.
What do we know about our ‘tools’ – the lenses that we have in our arsenal – to fit that ocular surface? First and foremost, the new CLEAR publications on evidence-based contact lens practice by the BCLA group state that: ‘Ideally the lenses’ sagittal height (CL-SAG) should be matched to corneal sagittal height’. Please note that sagittal ‘height’ is used for both the ocular surface and for the lens (not ‘depth’). The paper also states that these SAG values for lenses are not widely available. A new study recently published in Contact Lens & Anterior Eye by a team at Pacific University explores the CL-SAG of 44 commercially available daily disposable and reusable lenses in spherical and toric variations. As we speak, new lenses are
THERE IS A LOWERING OF THE SAGITTAL HEIGHT VALUE WHEN THE LENS IS APPLIED TO THE EYE, POSSIBLY IN THE 180-MICRON RANGE BASED ON THEORETICAL CALCULATIONS.

microns over its labelled diameter, then this would mean a roughly 75-micron difference to take into account for the change from room to on-eye temperature.
being analysed by Ben Coldrick at Optimec in the UK with the is830 instrument. What all lenses analysed, recently and in the past, have in common is that the lenses (per ISO standards) are measured at room temperature or 20°C. However, if the lens goes on the eye, the temperature actually rises to a mean of 34°C. One would expect that number to be dependent on environmental circumstances (e.g., cold or warm weather), but it appears that outside conditions are only responsible for just a few degrees of difference in on-eye temperature – hardly clinically relevant, it seems.
But making the transition from room temperature to eye temperature does make a huge difference in lens shape. It may be surprising for eye care practitioners to learn that the average lens ‘shrinks’ on-eye. By how much is the question. A landmark paper by Graeme Young et al in 2016 looked at the effect of temperature on soft lens diameter. To determine the difference, they calculated the ‘shrink factor’ by taking the on-eye temperature diameter and dividing that by the room temperature diameter. He looked at 24 different lenses: the shrink factor on average was 0.982 (a 2% difference), varying between 0.997 and 0.950 (depending on material). This is for diameter – what does this mean for CL-SAG? Could the shrink factor used for diameter be applied to CL-SAG too? A small study by Coldrick and Richards presented as a poster at the Global Specialty Lens Symposium (GSLS) in 2016 looked at both diameter and CL-SAG versus temperature change. Although this was a small pilot study, with a large variation of lens materials, thicknesses and powers, the shrink factor for diameter was 0.968, and this was in line with the shrink factor for CL-SAGs (0.966). The range in shrink factor was 0.991 and 0.941 for that potpourri of different lenses.
This shows that temperature indeed is a factor to take into account. The exact magnitude is to be determined, though. The new lenses currently being analysed are going to be measured at 20°C and at 34°C to get a better understanding of this. If we would use – hypothetically – the shrink factor found by Young of 2% (although variance up to 5% seems possible) and use the average of all spherical lenses in the Pacific study of 3666
So, on the contact lens side, the gap in knowledge is closing too. But what happens if a soft lens goes on the eye? There is not enough room in this article to cover that in detail – more on that in future editions of GlobalCONTACT – but the essence is that the lens has to be substantially ‘steeper’ than the ocular surface to create an acceptable lens fit. If the CL-SAG matches the OC-SAG, the lens moves too much, influenced by tear film and eyelid/blinking and even gravity forces. How much steeper?
In Graeme Young’s landmark publications on mathematical modelling of soft lens fitting and the inter-relationship between diameter, base curve and lens fit – the term ‘edge strain’ was coined. The optimal or ideal ‘edge strain’ supposedly is 2.7%, according to Young. Simplified, this means that a lens has to be steeper than the ocular surface to create the ‘right’ amount of flexure, and thus the right amount of grip, for a good lens fit to be achieved. In that case, the on-eye lens diameter increases by 2.7% after flexure.
In essence, according to Young, there is a lowering of the sagittal height value when the lens is applied to the eye. With a typical optimally fitting lens (i.e., an edge strain 2.7%), the sagittal height of the lens decreases by approximately 5% on-eye. Going back to the mentioned Pacific database of all spherical lenses (average CL-SAG of 3666 microns) and after applying a temperature shrinkage factor of 2% to that, a further 5% on-eye decrease would be in the 180-micron range.
One other factor that is mentioned regarding soft lens fitting is that there could be something ‘lost,’ as the lens does not per se fully align with the ocular surface. In other words, there could be a ‘post-lens gap’ between CL-SAG and OC-SAG, after flexure. Recent OCT studies have shown the post-lens gap to be extremely low, though; up to a few microns – less than the thickness of a red blood cell, typically – and this factor therefore appears to be a neglectable one.
Bringing it back to our terminology in contact lens practice, this edge strain and relative steepness of the lens could therefore be transformed into a ‘flex-factor’ describing the amount of flexure of a given lens on the ocular surface. One would want ‘a number’ to add to the OC-SAG to come up with the optimal lens of first choice. However, this depends on a number of variables including the exact material of the lens, the thickness of the lens and external factors such as tear film and eyelid forces. The term fitting factor therefore could prove to be more practical than flex-factor. But in essence, this factor might not be that easy to uncover and may prove to be a pain in the butt to nail down, as it is dependent on material and many other
factors. Hence, the F-factor, in a way, almost seems like it would be the best term. But no matter how you look at it, ‘F-factor’ seems to be the appropriate term for this final piece of the puzzle. Mind the gap. It’s the missing piece of the puzzle.
See the Pacific website via the URL and QR code for full access (and future updates and additions).
CME, Nagra M, Pult H, Sulley AL, Vianya-Estopa M, Walsh K, Wong S, Stapleton F. CLEAR - Evidence-based contact lens practice. Cont Lens Anterior Eye. 2021 Apr;44(2):368-397. doi: 10.1016/j. clae.2021.02.008. Epub 2021 Mar 25. PMID: 33775383.

• Young G. Mathematical model for evaluating soft contact lens fit. Optom Vis Sci. 2014; 91:e167–76.

• Young G. The inter-relationship of soft contact lens base curve radius, diameter and fit. ECLSO meeting, Izmir (Turkey). Oct 2015.
• Young G, Potts M, Sulley A.The Effect of Temperature on Soft Contact Lens Diameter. Eye Contact Lens. 2016; 42(5):298-302
Sources:
• Consejo A, Wu R, Abass A. Anterior Scleral Regional Variation between Asian and Caucasian Populations. J Clin Med. 2020 Oct 25;9(11):3419.
• Ritzmann M, Caroline PJ, Börret R, Korszen E. An analysis of anterior scleral shape and its role in the design and fitting of scleral contact lenses. Cont Lens Anterior Eye. 2018 Apr;41(2):205-213

• Van der Worp Eef, Matthew Lampa, Beth Kinoshita, Mari J. Fujimoto, Benjamin J. Coldrick, Patrick Caroline. Variation in sag values in daily disposable, reusable and toric soft contact lenses. Cont Lens Anterior Eye. Jan 2021. DOI: https://doi.org/10.1016/j.clae.2020.11.006

• Wolffsohn JS, Dumbleton K, Huntjens B, Kandel H, Koh S, Kunnen

Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as a head of the contact lens department at the school for over eight years. He received his PhD from the University of Maastricht (NL) in 2008. He is a fellow of the AAO, IACLE, BCLA and the SLS. He is currently adjunct Professor at the University of Montreal University College of Optometry (CA) and adjunct assistant Professor at Pacific University College of Optometry (Oregon, USA). He lectures extensively worldwide and is a guest lecturer at a number of Universities in the US and Europe.


The history of contact lenses begins in the late Middle Ages when the first attempts were made to compensate for malformations of the eye using water-filled glass bowls. The breakthrough came towards the end of the 19th century when the German ophthalmologist Adolf Eugen Fick, the French ophthalmologist Eugène Kalt and the German doctoral student August Müller developed the first scleral shells made of mineral glass that could be worn on the eye. Around 1888 they experimented independently with small shells that rested on the cornea and parts of the sclera. A decisive contribution to today’s contact lenses was made in the first half of the 20th century by the American optician Kevin Tuohy. By Hans-Walter Roth

The first scleral shells made of glass at the end of the 19th century served exclusively to compensate for malformations of the cornea, evening out irregularities of the anterior surface of the eye by applying gentle pressure to the cornea. These anomalies were the consequences of a variety of symptoms such as corneal staphyloma, the historical term for keratoconus or cicatricial astigmatism as a result of malformation, inflammation or injury. In such cases, it was not possible to achieve satisfactory compensation with spectacle lenses. Early attempts at contact optics often failed because the glass available was difficult to mold and the original two-curve design still required a lens diameter of over 20 mm which, due to its poor gas permeability, significantly impaired corneal metabolism (Fig. 1). Frequent lens breakage also made the lenses difficult to wear for a long time.



The breakthrough in contact optics only came with the successful synthesis of a transparent plastic: polymethyl methacrylate. Its easy formability when heated, the ease with which it could be reworked and lastly its high breaking strength made it the plastic of choice in contact optics for many years. However, the disadvantage remained that large scleral lenses could still only be worn for a limited amount of time each day. Impairment of the corneal metabolism due to lack of oxygen permeability of the material and restricted tear convection under the scleral lens made it impossible to wear such lenses for longer periods. In the long run, smaller lens diameters had to be achieved. This would become possible thanks to the American optician Kevin Tuohy (1919-1968) (Fig. 2) who was the first to patent a much smaller corneal lens in 1948. He called it corneal lens (Fig. 3), a term that was confusing at the time. The reason for this was that some inventors before him also referred to their lenses as corneal lenses. Although these lenses also covered the cornea, with their wide rim they were seated on the sclera; thus they were better termed scleral shells or scleral lenses.
Like many great inventions, the discovery of the corneal lens was ultimately due to an accident. While measuring the diameter of a scleral lens on the lathe, its haptic part – i.e. the part located on the sclera – accidentally split off; all that remained was its central part, i.e. its optical zone. The lens was

Fig. 6: List of fitting parameters for the first corneal lenses.

going to be discarded but somehow Tuohy came up with the idea of trying out this fragment which only covered the cornea on himself, or as other reports say on his wife. Contrary to expectations, this middle part of the scleral lens positioned itself spontaneously directly in front of the cornea. The foreign body feeling also seemed to be acceptable. The development of a corneal lens which could be worn for longer periods of time had begun. In 1948 Kevin Tuohy was granted the first patent in the USA for a contact lens made of PMMA, now known as a corneal or mini-lens (Fig. 5). As noted in the patent specification, his lens still had a diameter of 11.0 mm and a central thickness of 0.3 mm (Fig. 4). At the time, Tuohy was working for Solex, who immediately skillfully brought this new kind of "corneal mini-lens" to the attention of the public. However, before they could go to market, it was still necessary to introduce standardization of the lens parameters, in contrast to the scleral lenses previously produced from thermoplastic impressions of the eye or on a lathe. The purpose of this

standardization was to make it easy for as many opticians as possible to fit them, as well as to be able to manufacture them in large quantities. In order to achieve an optimal fit, the inner radii had to be curved in such a way that ultimately the lens could only move up and down in front of the cornea through a capillary gap filled with tear fluid when the eye blinked or was closed. Initially, the inner curvature of the lens was calculated based on the central radii of curvature of the front surface of the cornea, from which pre-defined parameters for the fitting sets could then be derived (Fig. 6).
It was soon realized that the lens fit was only optimal when multispherical inner curves were used. Now the use of Gullstrand's ophthalmometer for determining the central radii of curvature of the cornea and their use for selecting the base curve of the corneal lens took on a particular importance. Indeed, this measurement data is still the basis of all contact lens fitting today.
Like many great inventions, the corneal lens was ultimately discovered by chance.
Fig. 8:
Fig. 9: Distance vision test charts from the Solex contact lens studio.



Fig. 10: Test chart for children.
Once it had been proven that contact lenses with the diameter of the cornea could be worn comfortably on the eye, Tuohy continued with his experiments. He recognized that the design of the edge of the lens was largely responsible for the fit on the eye, the loss rate and ultimately for the wearing comfort. While the back surface of the corneal lens – also known as the inner or base curve – was primarily responsible for the seat of the lens on the eye, an optical zone had to be incorporated into its front surface. Its values were based on the respective refraction values of the eye. The first corneal lenses were still over 10 mm in diameter with rounded edges. After measuring the central radius of curvature as a basic value, the optimal lens design had to be determined by trial and error. The Solex product range (Fig. 7) contains the lens parameters available for the first fitting set of Tuohy’s corneal lenses.
Some of the equipment from Tuohy's workplace is still on display. It can be seen in the Contact Lens Museum at Forest Grove, Oregon, USA on the Atlantic coast. Not only is there
Fig. 11: Test chart for near vision, card game.

equipment from his workshop on display but also some of his drawings (Fig. 8), graphs and the first fitting sets of his corneal lenses. Even the test charts from his studio at Solex are still to be seen (Figs. 9, 10 & 11).
Tuohy knew better than anyone else how to advertise his "Tiny Lenses" as he called his contact lenses in the media. (Fig. 12). With catchy advertising slogans, he knew how to get people’s attention. "The new window for your eyes" was the headline of the New York Times in 1949, going on to explain that his lenses were "held on the eye by tears alone". “The new mini-lenses do not irritate the eye,” wrote the London Observer in 1951. To demonstrate the quality of PMMA as a lens material, the article mentions that it was the same plastic material as used for the cockpits of US Air Force bombers.
Fig. 12: "Tiny Lenses" made of plastic material from aircraft panes.
Fig. 14: Eye casts for molding contact lenses .

Fig. 13: Advertisement for Tuohy's invisible vision aid, 1952.
Almost all the media at the time reported on his invention and its wearers, and he constantly encouraged prominent artists, actors and athletes to wear the lenses. At the time, however, not all lens wearers were as enthusiastic about the "invisible lens for everyone" (Fig. 13). Corneal lenses were still often accompanied by a strong foreign body feeling in the eye, and it often took several weeks to get used to them. There was no advice on lens cleaning or care, and artificial tear drops for rewetting the lenses had not yet been introduced.


Even one US president is reputed to have worn the lenses, and Marilyn Monroe is also said to have been one of his customers. While the eye casts in a museum in Ulm, Germany, made for the production of contact lenses (Fig. 14) could possibly be ascribed to her, this cannot be proven beyond doubt because the relevant prescription data is missing. All that is known for certain is that the casts came from Tuohy's workshop.
Kevin Tuohy was not the only person who worked on the development of hard contact lenses in the post World War II years, countless others contributed to improving the wearing
comfort of contact lenses through their own developments. Both before and after him, opticians, optometrists and ophthalmologists were constantly searching for new, better-tolerated plastics and lens designs, in order to extend daily wearing times and reduce foreign body irritation. For example, Heinrich Wöhlk, a scientist from Kiel in Germany who developed a contact lens made of Plexiglas in 1946, should undoubtedly be considered one of the pioneers of the corneal lens. He certainly made a mistake in not applying to patent his lens in 1947, ahead of Kevin Tuohy. As a result, Tuohy took precedence and the credit for having developed the scleral lens into the corneal lens, thus making it suitable for almost everyone with ametropia to wear.
Dr. Hans-Walter Roth

Institut für Wissenschaftliche Kontaktoptik
Ulm, Germany.
E-mail: institut.roth.ulm@t-online.de
In 2004, Keith Parker and I opened Advanced Vision Technologies (AVT). At that time, the economy was going through a very bad recession and as a result, it was impossible for a new business starting up to get a loan. We immediately reached out to Erik and Pam at Larsen Equipment to get refurbished equipment to use in our Laboratory. As AVT’s business grew, we invested in many different pieces of new equipment from Larsen Equipment and this helped us grow into one of the Premiere Labs in the United States. Our success is due in part to Erik and his Team with their state-of-the-art equipment and maintenance of their products. AVT is forever grateful for Larsen Equipment’s support of AVT. It is great to know AVT is working with Industry leaders with the Larsen Equipment and their Team!
Janine Bungo, VicePresidentI have known Erik Larsen since 1992. Since then I have used just about every piece of equipment his company has built. My experience with Erik and the Larsen team has been one of great appreciation as they have always helped me in my needs of fully understanding equipment used to manufacture quality contact lenses. Erik has also been able to engineer any part needed for me even it was a custom part. Erik (Larsen equipment) has been and still is a pioneer in the contact lens and optical industry, and I am thankful to him for his support over the years.
Randy Mingoy Quality ManagerI have had the pleasure of working Erik since the beginning of Larsen Equipment. The first piece of equipment, a 6 spindle horizontal arm polisher revolutionized our production of GP contact lenses. Through the years, I watched his business grow as he and his team listened to our Industry needs and developed now numerous products not only simplifying many tasks of manufacturing but improving the consistency of quality in our finished products. Innovation has been an ongoing experience of our Company only made possible through the innovation of necessary equipment developed and made available by the Larsen team.
Advanced
Vision Technologies
There can be a lot of moving parts when it comes to managing operations, so it is key to have reliable precision equipment that assists in overall efficiency. Larsen Equipment delivers just that! I have been utilizing Larsen manufacturing equipment for over 15+ years and have yet to run in to an issue they could not resolve. I am a satisfied owner of bladder polishers, edge roller’s and auto-blockers etc. Each one of these units greatly assist in the reduction of rejects and manufacturing waste. Their ability to customize and retrofit specific tools certainly sets them apart from the competition. Larsen stands behind their equipment with a knowledgeable staff that provides exceptional service. Simply put, we are a better laboratory because of our relationship with the folks at Larsen.
Jordan Gobel Director of Operations/Consultant Advanced Vision TechnologiesLarsen Equipment is a family owned business hosting a team of willing Staff all having the attitude of serving their Customer’s needs. As a Customer, we are made to feel like we have a friend in the business helping us develop a more efficient process allowing our Company to deliver better products for our Customers.
Our success of AVT simply could not have been possible without the help, assistance and dedication of Larsen Equipment. I will be forever grateful for my opportunity to work with Erik and his very capable Staff.
 Keith Parker President
Keith Parker President
 Interview with Dr. Jerome Legerton, Innovega
Interview with Dr. Jerome Legerton, Innovega
What would happen if you lost most of your sight, if things you are used to recognising were suddenly no longer visible? Finding your way around in everyday life would become increasingly difficult. This is not only a problem obvious in the pandemic, where visually impaired people are dependent on help anyway. It affects many people in various stages of visual impairment. A new device, glasses in combination with contact lenses, can improve recognition and vision to a certain extent. But beyond that, it pushes open a new door: Welcome to the world of virtual, augmented or mixed reality.
By Silke Sage Photo: Silke SageGlobalCONTACT: Who are emacula's target groups?
Legerton: The eMacula system is categorized as extended reality eyewear. Extended reality (XR) includes virtual reality (VR), augmented reality (AR), and mixed reality (MR). Each system provides visual content to the user in different ways. The eMacula system enabled by the iOptik contact lens may be used for all three forms of XR. VR employs an occluded display in glasses or a headset. The real world is blocked by the display. Even so, the content or media on the display can be very high resolution, bright, and in a full color gamut. The first target group for the eMacula VR system will be the visually impaired. The advantage and benefit of the eMacula system over other VR systems for the visually impaired is the wide field of view in combination with lightweight and stylish eyeglass form factor. The software that takes the image from an onboard camera or from a mobile phone or PC enhances the image for the visually impaired. The first enhancement is to enlarge the image in proportion to the best corrected visual acuity. The user can control the image enlargement, brightness, contrast and color rendering. The wider the field of view of the system, the greater the ability to enlarge the image and still see enough of the image. Small field of view systems cause a loss of context when the image is enlarged. In other words, the user sees less of what they want to view even though the image is large enough to resolve.
GlobalCONTACT: How does the use of the devices work?
Legerton: Innovega designed two systems for the visually impaired that we call ambulatory and non-ambulatory. The ambulatory system or mobile system can be worn in all settings and is expected to be used by the visually impaired for driving in the same manner as bioptic telescopes. The ambulatory eMacula system delivers variable magnification, brightness, contrast and scene manipulation while the bioptic telescope is fixed for each of these.
The non-ambulatory system is designed for stationary activities like reading, desk work, and vocational tasks. The field of view can be larger than the ambulatory system and thereby allow for greater magnification while maintaining more image context. These same systems may be used by fully sighted individuals. There is value in the ambulatory system for anytime-anywhere information. The system may be used for spectator activities to eliminate the need to use binoculars while also allowing simultaneous media feed to enhance the enjoyment of the spectator event. Sports training or performance enhancement is anticipated with the ambulatory system as well. Sensors and information content systems are already in use for cycling. These data may be presented in the eyewear instead of on a display on the handle-bars. The cyclist can see the information without looking away from the path.
Occupational enhancement, also called enterprise, is already a significant target for XR headsets and eyewear. The eMacula systems may be employed in many industries to allow for
anytime-anywhere information, direction and instruction. The contact lens enabled system brings the advantages and benefits of wide field of view, high resolution, full color gamut, low latency, greater brightness, and potential to be less power hungry.
GlobalCONTACT: How can I imagine the view through the glasses?
Legerton: AR and MR employ a transparent display technology in glasses that allows the user to see the display content and the real world at the same time. AR presents the image in the transparent display without being registered to the real world. The image simply is viewed simultaneously like an insect on a windshield is seen simultaneously with the real world when driving. MR employs greater technology to register the image with the real world to allow it to be manipulated in size, position and action with the real world. MR presents far greater challenges with the need for additional sensors, electronics, processing and power consumption. MR is regarded as one of the most difficult technology challenges of this decade. We see the added challenge of making the MR display eyewear useful while making it usable with regard to weight, comfort and appearance. This understanding supports the prediction that VR and AR systems will be adopted well before full MR systems.
GlobalCONTACT: On what technology is augmented reality achieved?
Legerton: AR is achieved by way of image processing to micro-displays that are placed in a near eye location. There are three primary technologies: Waveguide, off axis projection which is sometimes called holographic, or beam combining by use of occluded micro-displays and some form of optical combiner. The goal in each case is to put an image in front of the line of sight of each eye in a pair of glasses or a headset.
GlobalCONTACT: The lens power is generated via the contact lens. Up to what prescription does the glasses/CL-system work? Are there limits, if so what are they?
Legerton: The Innovega iOptik contact lens is similar to any disposable soft lens and the power limit is governed in the same manner as any molded soft lens.
GlobalCONTACT: How many smart glasses do you currently produce and who are your customers?
Legerton: This question actually addresses our business model. Innovega is executing a licensing model wherein we are licensing our technology to contact lens partners and to display eyewear and application partners. We do not plan to produce or sell finished products.
GlobalCONTACT: When will the product be available, and where?
Legerton: The first application is for the visually impaired. We are seeking FDA market clearance for the iOptik contact lens and then will follow with CE marking. The first markets will be North America, the United Kingdom and Europe.
GlobalCONTACT: Where is production taking place?
Legerton: We see value in the contact lenses being produced close to or in the market where they are distributed. Ideal licensees will be located close to the eye care practitioners who will be fitting the iOptik lenses in the same region.

GlobalCONTACT: What are the biggest challenges in production?
Legerton: Our lens is in the category that we call component containing. The lens has an encapsulated two-state gas permeable light polarizing filter. We developed methods of transferring the filter to the lens substrate during molding. This method of manufacturing is more complex than single stage molding used for disposable soft lenses. We have ongoing process engineering to drive the cost out of the manufacturing.
GlobalCONTACT: Currently there is a product from Germany that uses a Fresnel lens integrated monocular into the spectacle lens. The lens power can be integrated directly (no matter what power) into the spectacle lenses. Why do you think the solution with a contact lens is better?

Legerton: We clearly believe in what we call eye-borne optics. The lens power required to directly view a near eye display ranges from +60.00 to +85.00 diopters depending on the vertex distance of the display from the eye. The majority of users also need vision correction and the majority of those needing vision correction have some astigmatism and need for a cylindrical lens component. It just makes sense to us to put the refractive correction along with the micro-lens for viewing the display in a contact lens or intra-ocular lens. We also believe in providing users with binocular vision and fulfilling the global mission of eye care professionals to provide clear comfortable two-eyed vision at all distances. All of our reference designs and methods of fitting are directed to binocular vision and usual and customary correction of refractive error.
We are pleased to see that other XR developers are thinking about refractive correction. We anticipate that XR will be another reason for wearing contact lenses since the placement of spectacle lenses behind an already heavy or bulky headset or display eyewear seems to exacerbate the comfort and appearance challenges that already exist. The Fresnel solution helps to keep the weight down. Visual noise must be avoided in all systems and we believe fully sighted consumers will demand excellent clarity.
GlobalCONTACT: How much does the unit weigh?
Legerton: Our eyewear weight goal is to be less than 60 grams. There will be a constant push to achieve 45 grams and then 30 grams. The reality that today’s conventional eyewear is very light must be respected.
GlobalCONTACT: Who will distribute the glasses and contact lenses?
Legerton: We are in discussions with a global distributor of products for the visually impaired. They will distribute the eyewear and the regional contact lens manufacturer will distribute the contact lenses to the eye care providers who fit them. North America and Europe have different channel economics and systems. The low vision specialist in the US is most often an independent practitioner or an employed practitioner in an institutional setting. The same individual will fit the iOptik contact lens and dispense the eMacula eyewear. It is ideal to have the two parts of the system delivered under the same roof.
GlobalCONTACT: Will the glasses be roadworthy?
Legerton: The eyewear must be robust. The industrial design of the eyewear is a major development component in the same manner as the design of a mobile phone. Impact tolerance and heat dissipation are design requirements along with weight and power use reduction.
GlobalCONTACT: How can the product be arranged with data protection? Are there any hurdles here?


Legerton: The software developers for each application follow the state of the art that is applied to other electronic devices. Efforts are made to employ connectivity that is contemporary with all electronic devices.




GlobalCONTACT: Does the device have to be equipped with its own (electronic) simcard or does it only use the connection to the smartphone. Which implies: It must be carried at all times? Also during sports?
Legerton: We have reference designs for tethered eyewear and eyewear that has wireless connectivity. Keep in mind that a fundamental goal for the eyewear is to be lightweight and stylish. This usually means that it is best to put everything possible somewhere other than in the eyewear or work to significantly reduce what is called SWaP, size, weight and power. There is a rapidly growing group of folks who believe in the post mobile phone era. The 5G providers are all eager to move the telecommunications console to eyewear and away from mobile phones. The achievement of this vision will require

significant minification of components. We believe consumers will see fully functional telecommunication eyewear at some point. Before that time, we see value in tethered eyewear in an effort to keep power and data sources off the eyewear to achieve the weight reduction and improved styling.

Dr. Jerome A. Legerton: OD, MS, MBA, FAAO, Director of Innovega Practiced for 26 years prior to launching a successful career in contact lens development and commercialization; 57 issued U.S. patents, co-inventor of Paragon CRT contact lenses, the market leader for overnight corneal reshaping. Co-founder and former CTO and EVP of SynergEyes, Inc., the world leader in hybrid contact lenses, before joining Innovega to lead contact lens design and clinical and regulatory activities.

Evidence of the pore space of a silicone hydrogel contact lens as transport path for pore diffusion and molecular diffusion – Part 1.
Scleral lenses, hybrid lenses or Ortho-K: To ensure safe use of these types of contact lenses, the main focus is on the oxygen permeability of the plastic material of the lens. The metabolism of the cornea and the limbus should suffer as little irritation as possible. The aim of this article is to explain how this transport mechanism occurs and why it is so important. By Alina Kinder
In an age of retro looks and vintage design, even conventional systems are being updated offering newer approaches to solutions. Scleral lenses have made a comeback in contact lens optics. Using these lenses where only the edge is seated on the sclera, and which thus can be adapted to more complex corneal geometries [1], the discomfort to the physiology of the already stressed cornea through contact lens wear is kept as low as possible thanks to new materials and higher oxygen permeability. [2]
In addition, lens systems such as hybrid lenses and also piggyback lenses catering for more complex corneal geometries have made a comeback in contact lens optics. Here, too, the benefit of lenses made of newer materials is to ensure a better oxygen supply to the cornea. [3] Current studies show that treating keratoconiosis, keratoplasty and some forms of corneal
degeneration/dystrophy using contact lenses made of modern materials not only stabilizes the vision but the lenses are also physiologically safer for wearing all day long.
Other contact lenses, such as the orthokeratology contact lenses (Ortho-K), have also gained in significance since the introduction of modern materials and have been able to reposition themselves in contact lens optics since the advent of higher oxygen permeable materials. Furthermore, the importance of corneal swelling is not insignificant, especially with Ortho-K lenses.
To ensure safe use of the above-mentioned systems, the main focus is on the oxygen permeability of the plastic material of the contact lenses. The lens material must perfectly satisfy the optical requirements in addition to the requirements
regarding the comfort of the contact lens wearer, without irritating the metabolism of the cornea and the limbus; or with only minimal irritation. For this reason, oxygen permeability is already taken into account during the production of the plastic material.
An inadequate supply of oxygen to the cornea can lead to
• too high acidity of the cornea resulting in lactate build up in the stroma.
• osmotic water influx into the cornea resulting in edema formation.
• structural changes of the cornea, such as loosening of the cell bond in the epithelium with an associated increase in the rate of loss of epithelial cells.
Thus one of the main aims when fitting contact lenses is to preserve the anatomical and functional integrity together with the rigidity of the cornea, in order to minimize the physiological changes mentioned above. [4,5]
Contact lens optics use the permeability or transmissibility of the contact lens material as a suitable parameter for describing or predicting whether the plastic material has a high or low impact on the physiology of the cornea.
In science, soft matter is used to describe a state where a distinction cannot easily be made between liquid and solid. Soft matter can also be described as amorphous. Polymer melts and solutions as well as elastomers (rubber), for example, are classified as soft matter, and the same is also true for soft contact lens materials. [6]
In the literature, the transmissibility of solutes in soft matter is described by permeability. In chemistry, with regard to soft matter, permeability also refers to the aggregate state of the material.
Permeability alone cannot adequately define the solute transmissibility of a soft matter material. [7] Such amorphous polymers are produced by polymerization processes based on polyaddition or polycondensation. The particular polymerization process used in turn determines the properties of the plastic.
Permeability describes the transmissibility of dissolved particles in the material. The oxygen permeability of a contact lens material is referred to by manufacturers as the Dk value (permeability), where D is the diffusion constant of the material and k the solubility constant of the material.
For a better analogy, in contact lens optics the property of oxygen transmission in soft contact lenses is given by the Dk/t value. For this purpose, the geometric thickness of the center of the contact lens to be compared with a power of -3.00 dpt is set as the reference distance.
Nowadays, modern equipment can track the potential oxygen transmissibility over the entire surface of a soft contact lens in relation to the dioptric effect of the lens. This theoretical approach, aimed at visualizing the oxygen permeability of the contact lens, is realized purely theoretically via the ratio of the permeability to the corresponding thickness of the lens with a dioptric effect. For this, the transmissibility, i.e. the Dk/t value of the individual points of the lens, is allocated a color code designed to indicate the permeability (Fig. 1). The color codes correspond to the internationally valid minimum Dk/t values. As early as 1984, Holden and Mertz identified a critical limit value of 84 Dk/t for extended wear, in order to keep corneal swelling overnight as low as possible. In 2009, Harvitt and Bonnano's study recommended higher limits, such as a minimum value of 35 Dk/t for daytime wear and a minimum of 125 Dk/t for extended wear (EW), with a minimum of 140 Dk/t for EW. [9,10]

With hard contact lenses, which are clearly in a solid state, the analogy with the Dk/t value clearly cannot be maintained. In such cases, comparison of the oxygen permeability of the respective materials is given purely by the Dk value. Here contact lens optics attributes the reason for good oxygen transmission through hard contact lenses to the high amounts of silicone and fluorine as oxygen carriers. Accordingly, a comparison of soft and hard contact lenses with regard to material permeability is only possible based on the Dk value.
A study by Hideji Ichijima and H. Dwight Cavanagh compared the permeability of a hard contact lens with a value of 90 Dk/t *10-9 ml(O2) * cm/ml * hPa*s with a soft silicone hydrogel contact lens with a value of 125 Dk/t *10-9 ml(O2) * cm/ml * hPa*s and found that the hard contact lens delivered more oxygen in total to the cornea than the highly oxygen-permeable silicone hydrogel contact lens. [11] This result was not due to the respective permeability of the contact lens materials, but rather to the different diameter sizes of the lenses, and thus to the different areas of the cornea covered.
The size of the lens diameter of a hard contact lens may be 20% to 30% smaller than the diameter of the cornea. The exposed area of the cornea thus enables oxygen to reach the cornea via the physiological way, through the tear film by diffusion, driven by the partial pressure difference of the oxygen.
The product descriptions of contact lens optics emphasize the benefits of the individual elements such as silicone and fluorine as oxygen carriers. The selling point of the good oxygen permeability of modern contact lens materials lies in the high silicone content and the lattice structure of the plastic polymer.
On the one hand, silicone acts as an oxygen carrier and, on the other hand, the regular lattice structure of the silicone hydrogel material acts as a water reservoir and thus as an oxygen carrier, as in conventional soft lenses.
In conventional contact lenses made of hydrogel material, the clear polymer lattice structure serves as a good water reservoir. Thus the water stored in the so-called cavities (lattice interspaces) can serve as an oxygen carrier. [12] However, based on experience with hydrogel contact lenses, it is well known that the oxygen permeability performance of such hydrogel lenses does not satisfy the demands of the cornea; thus this stored water alone is not sufficient as an oxygen carrier.

Due to the internal structure of the silicone hydrogel material, the cross-linking, the interpenetrating network (IPN) of the two constituents silicone and hydrogel, the ion exchange (according to the manufacturer's information) takes place in the water channels (Fig. 2). At the macroscopic level, the crystalline lattice structure of the silicone hydrogel polymer is said to be responsible for the diffusion of the oxygen.
The cross-linking of the two components is said to be responsible for the improved oxygen permeability of the material. This, at least, is consistent with the current view of oxygen transmission through polymeric contact lens materials. Current studies of contact lens materials do not

suggest any other means for transporting solutes. It is interesting to note that the product description does not make any distinction between the different aggregate states "solid" and "soft". The Dk/t value is rarely mentioned for hard contact lenses, because it is difficult to imagine that oxygen can diffuse through the solid contact lens material within a reasonable wearing time. In this regard, the industry does not seem to make use of the transmissibility method, whereby the Dk value is only divided by the center thickness of the contact lens, for hard contact lenses.
The transport path of solutes through the material can also be illustrated using another model.
The first possible model is that of capillaries – cavities running through the contact lens. Oxygen dissolves in the tear film, enters the material through the surface openings (pores) and flows through the lens pore system to the rear surface of the lens, thus reaching the epithelium of the cornea. This is another way of describing the physiological path and is similar to the process of pore diffusion. Pore diffusion or diffusion of gas into liquid lends itself to, and can realistically describe, the process of oxygen diffusion through the contact lens material.
Oxygen flow through the silicone is not the simplest of diffusion processes. The hypothesis of pore diffusion cannot be applied to all materials, only to materials that exhibit porous characteristics.
In an interpenetrating polymer network (IPN) consisting of a combination of two polymers in the form of a network, the relevant polymerization process creates a suitable cavity that can be used as a pore space for pore diffusion. [13]
IPN technology is a combination of silicone with a hydrogel material and results in a plastic mixture which is cloudy due to dispersion and thus opaque. The solution to the transparency problem lies in the network structure that connects the two phases separately. There is a broad range

of applications of IPN technology, including biomedical applications, coatings and adhesives. Some of these IPNcrosslinked plastics exhibit a two-phase structure in the range of several 100 angstroms. This corresponds to a magnitude of several 10 nm, meaning that the void space available is also in the range of soft matter pore spaces. In contact lens optics, pores – and thus openings of 1 - 10 nm (10 - 100 Å) – are known. [15,16]
According to the International Union of Pure and Applied Chemistry (IUPAC), the pores of polymer hydrogel materials, which are openings on the outer surfaces of soft matter, are in the range of mesopores.
Pore diameter Nomenclature (IUPAC) Examples
would be significantly reduced. Diffusion through the pores serves as a transport path for the dissolved particles.
To avoid scarring after keratoplasty or other penetrating eye surgery, a bandage lens is subsequently placed on the cornea to protect it. [18] Here, too, the healing process is protected and encouraged by pore diffusion.
This is part 1 of this article. Read part 2 in the upcoming issue of GlobalCONTACT and in our app.
< 2 nm Micropores
Activated carbon 2 - 50 nm Mesopores Polymer hydrogels > 50 nm Macropores Plants
Tab. 1: Pore size according to IUPAC. [17]
Film dressings used in the treatment of severe skin burns are an example of the use of IPN technology for biomedical materials. Made of polymeric material, the transparent dressings transport fluid away from the damaged tissue while facilitating the ingression of oxygen to preserve the tissue cells which are still alive and enabling new tissue to form. Diffusion in the dressings is of great importance in this process, allowing a healing environment (i.e. maintaining the moisture balance) to develop at the damaged tissue site. In addition, transparent dressings allow the treating physicians to optimally follow the healing process. [13, 14]
The process of pore diffusion is the process that contributes to better healing due to these transparent film dressings. It is only thanks to this film covering that the moist wound environment can be created appropriately and help the tissue to form new cells. If the processes of oxygen transport and fluid removal were to take longer, then the healing process would be considerably slowed down and thus the benefit of such dressings
References are available on request from the editorial office or are listed in the GlobalCONTACT app.
More information on using the GlobalCONTACT app on page 46.

Alina Kinder (EurOptom, Master of Science (Klin. Optometry)) is a lecturer at the Professional School for Optometry in Cologne (HFAK). She also works as an examiner on the examiner board of ECOO diploma and optometrist (ZVA/ HWK).

DO NOT SUGGEST ANY OTHER POSSIBLE WAYS OF SOLUTE TRANSPORT.
Kyoichi Tanaka was only 19 years old when he set out to develop the first Japanese contact lens in 1951. Equipped with determination, modest tools and using his own eyes for the first prototype test, he managed to produce a functioning contact lens after six years of work. This laid the foundation for the company that would later be called Menicon. In the years since then, Menicon has grown into an international group that is celebrating its 70th anniversary in 2021. By Rebekka Nurkanovic

Menicon today offers a broad product portfolio that enables contact lens specialists to successfully correct almost any refractive error with contact lenses: Flat pack daily disposable lenses, silicone hydrogel monthly disposable lenses, custom soft lenses, high-quality form-fitting contact lenses with innovative designs and materials, keratoconus lenses, Ortho-K lenses, plus care products and accessories. The range is rounded off by Menicon's Easyfit fitting program. Decades of experience in research and development and high quality standards have gone into this innovative and high-quality
product range. By constantly improving its technologies and quality assurance systems, Menicon has been able to achieve many goals.
Today, all Menicon products are manufactured in the company's own production facilities in Japan, Singapore, The Netherlands, Great Britain and France.
Founder Kyoichi Tanaka was working in an optician's store when he first heard about contact lenses from the wife of a US Army officer. He had never seen a contact lens but his interest was piqued and he decided to develop a contact lens himself. He set to work in 1951, researching and testing, and in 1957 he succeeded for the first time in producing a working contact lens. He then founded Nippon Contact Lens Co. Ltd, the predecessor of Menicon.

Over time, Menicon succeeded in inventing methods to bond and polymerize materials, design innovative products, develop new manufacturing methods and build its own production facilities with fully automated production processes. Thus, the company developed Japan's first oxygen-permeable form-stable contact lens. In 1995, Menicon established a new research and development center. From the very beginning, all processes at Menicon have been carried out internally: From material development to product designs, manufacturing, distribution and sales. After many decades of experience, the company began to apply the findings to other fields: veterinary ophthalmology,

environmental biotechnology and life science. One example for veterinary ophthalmology is the Meni-One X, an intraocular lens for dogs, which was released in 2020. With the increasing prevalence of myopia worldwide, Menicon has also designed the Bloom Myopia Control Management System, a full-service myopia control concept.
Dr. Hidenari Tanaka was appointed president in 2000, succeeding his father. At the time, the Japanese economy was deteriorating and the market was flooded with daily disposable contact lenses from global companies. Menicon decided to offer a monthly flat rate lens replacement service called MELS Plan that has now become one of the company’s pillars with 1,3 million plan members in Japan. From a small company with only two products in the beginning, Menicon has developed into a globally active company with a high profile within the industry. For example, Menicon has been listed on the Tokyo Stock Exchange and the Nagoya Stock Exchange since June 2015. The capital available from the IPO was invested in the construction of a new manufacturing facility for daily disposable lenses. Menicon now operates in more than 80 countries and has 16 business offices in Japan and 13 overseas. The high-quality Menicon products are manufactured in a total of eleven production facilities. The company generates approximately $770 million (2019/FY 63) and employs around 3,500 people worldwide.


On the occasion of its 70th anniversary, Menicon announced that it has renewed its vision of Miru. "Miru" means to see, but it is also about having fun and enjoyment through the five senses, as well as being empathetic. With this new vision of Miru, Menicon aims to make everyday life richer and filled with laughter through all the senses, not just the sense of sight, the company says.
Menicon also stated that it plans to continue their commitment to sustainable development by providing safe vision products, developing environmentally friendly products and implementing sustainable measures in its factories.
“We are so proud to be celebrating this milestone 70 th anniversary. Menicon manufactures specially controlled medical devices, so our top priority has always been the safety of our customers' eyes,” said Hidenari Tanaka. “Challenge, safety, end-user first philosophy and high-quality products remain the cornerstone of Menicon’s continued growth and success. These principles are why we are able to celebrate such a significant anniversary.”
The company’s achievements will be celebrated through special promotions from April 2021 to March 2022. Further information and a video of Menicon’s 70-year history can be found on the company’s website: www.menicon.com n

BY CONSTANTLY IMPROVING ITS TECHNOLOGIES AND QUALITY ASSURANCE SYSTEMS, MENICON HAS BEEN ABLE TO ACHIEVE MANY GOALS.
This article is different from my usual topics of tips, tooling, and technique. I will look at what was going on in Larsen Equipment Design (LED) and in our industry in May of 2020 as compared with May of 2021. I will look at three areas of the industry: Our partner labs, LED business, and LED suppliers. By Erik Larsen
Starting in early 2020, we were beginning to hear from our partner labs about their business situations. Orders were starting to slow, and the future was not clear. We at LED saw a similar trend. We saw no indication that our suppliers were having problems with filling orders to us. By May of 2020, business was very different along with every other aspect of daily life. Most of the labs saw an extreme down-turn in business as did our suppliers and us. Many of the labs and our suppliers put their workforce on furlough. This situation would prove to be a concern later in the year as orders started increasing requiring the workforce to return.

Custom labs try to deliver lenses in a few days. So, they do not have an extended backlog of work on hand. Our suppliers operate
in a similar fashion. We as machine tool manufactures however, operate on a weeks-long delivery schedule. In May of 2020, we had a backlog of work of about four weeks. While this situation was uncomfortable, we all had work to do. As we entered June, our backlog was two weeks, but we had orders to fill. As it turned out, June was the lowest month of work in-house for us. We did have an unexpected increase in business from a few labs that had lost local suppliers due to the general downturn. These labs needed custom items (tooling, replacement parts, etc.). Another source of orders were the medium size and multinational companies who were progressing with their plans as were set prior to the pandemic. Mergers and acquisitions continued. Typically, we see orders soon after these transactions are completed. Plus, we get to develop relationships with the
new engineers and staff. The over-all benefit of this additional business may have just enabled us to keep everyone at LED actively employed.
Another source of work was research and development, both internal and for customers. Some customers decided to go ahead with projects as they saw the pandemic providing a window of opportunity. According to our government’s criteria, LED is an essential business, so we were able to stay open.
It occurred to me that our partner labs, we at LED, and most of our suppliers share a working arrangement where each person had a cubical or workstation that is at least 6’ (2 m) apart. This arrangement, along with no retail customers, allowed us to fit in with the distancing requirements. May of 2021 has shown an almost complete reversal (both plus and minus) as compared to May of 2020. Most labs have seen a return of orders, but for various reasons, many needed to hire new people who require training. This situation puts an additional burden on lab managers. We saw a gradual upswing in orders after a level summer of 2020 and business has steadily grown to a current backlog of orders of 10-12 weeks. We have been able to weather the pandemic with our team intact but with administration staff working from home, which they still are.


What effect has the pandemic had on materials and components? I have not heard from any labs about a shortage in lens material or consumables. Similarly, local utilities seem to have been able to maintain their services. However, costs may have fluctuated. At LED, we source material and components from a few dozen

suppliers. These range from raw materials to purchased components. For raw materials, we use plastics, metals and wood. We have seen single digit percent price increases for plastic and metals, but up to 500% for wood used in shipping crates. Of course, these costs are a very small part of our over-all costs. Purchased components – electronics, motors, bearings – have seen price increases in the single digit percent and availability has remained at a few weeks. We do have a few suppliers who do post-processing of our in-house manufactured components. With our region being an aero-space manufacturing centre, it was hit hard by the pandemic and other problems. Our post processing suppliers are heavily tied to the aero-space industry. They furloughed a large part of their workforce. In the last few months, we have seen the usual turn-around time of a week grow to 3-4 weeks due to a lack of trained workers. We have been able to absorb the delay in our 10-12-week lead time, but we are managing the situation more closely to maintain the delivery schedule.
To say that we at LED have been fortunate is an understatement. We are also happy to see the optical industry and our suppliers returning to pre-pandemic business volumes. I am optimistic that our industry and associated businesses will come away stronger. n

Let’s face it – we can be a bit myopic in our contact lens industry, especially when we relate contact lenses to other vision correction methods. But myopia management is not a contact lens device-driven field. It is about myopia development at a young age and how it relates to myopic retinopathy later in life. There may be ways to slow that down – the progression of myopia that is, as we cannot stop or prevent myopia from happening. By Eef van der Worp

A favourite phrase used previously at the Dutch contact lens association meeting (NCC) is: “glasses are for drinking” (e.g., not for vision correction). A tongue-in-cheek phrase, of course, deliberatly emphasising the ‘myopic viewpoint’ which you can expect from a meeting solely devoted to contact lenses. On the other hand, it sometimes rubs a bit the wrong way for some (including for me), for instance with presbyopia, that it is so easy (and profitable) to sell a pair of multifocal glasses when contact lenses may be the preferred option by the client or patients or even the option that would provide the best optical solution for their needs.
Back to myopia then: a new spectacle lens has entered the market that has been developed especially for myopia management. It consists of a lens with a clear centre and multiple droplet-like peripheral +3.5D segments. The lenses use DIMS (Defocus Incorporated Multiple Segments) technology developed by the Hong Kong Polytechnic University and HOYA.
The good thing about these glasses compared to other interventions is that they are completely pupil independent. Do they work? The 2-year data looked very promising, quoting reduction rates of 60%. We have to realise that this is in Asian eyes. We simply don’t know how that relates to other ethnicities. Now, we also know from the contact lens field in myopia management that this is no fair way of putting things. Even íf the lens is capable of providing that 60% reduction under all
circumstances (not just in a trial setting), then we have to be very careful, as this relates only to a very short period of time during which the eye grows. The bulk of the treatment typically has to happen before the age of twelve. Hence, a -6D myope will not become a -3D myope, unfortunately, with treatment. In fact, we can probably get about 1D of reduction in reality on average, as work by Brennan and Bullimore shows. Not that this is negligible: at the same time, the same investigators claim that ‘every dioptre counts’ in myopia management later in life. The 3-year data on the DIMS lenses is just out, and it shows surprising similarities to contact lenses: there seems to be a tapering of the effect after the early results. They report over three years the spherical equivalent refraction and the axial length changes in the test group of 65 subjects to be −0.52±0.69D and 0.31±0.26mm compared to a control group. So, the DIMS glasses were effective in reducing myopia progression to a degree – in line with what we see with orthokeratology and soft multifocal lenses. Other glasses from other manufacturers will follow shortly. At ARVO 2021 results of a test by Essilor will be presented.
What is the best intervention method? The answer most probably is that there is not one, at least not a generic one. All things considered, orthokeratology, soft multifocal lenses and DIMS glasses perform in the same range if you apply them to a single patient. Only very high-dose atropine may have a better track record, although this has substantial side effects. Atropine
remains a perfectly good option, though, for some, as do glasses. The only thing that may be clear is that other intervention methods, apart from the ones mentioned here, are substantially less effective. This includes 0.01% atropine, regular hard lenses and standard bifocal glasses. The lesson here? Let’s not be myopic about the intervention methods for myopia. The best intervention method out of the ones mentioned here is the one that best suits the particular patient in the chair at that moment. Let’s raise our glasses to that. Cheers!


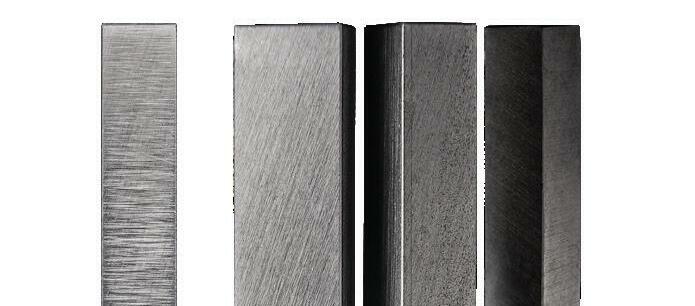
• Brennan NA, Toubouti YM, Cheng X, Bullimore MA. Efficacy in myopia control. Prog Retin Eye Res. 2020 Nov 27:100923. doi: 10.1016/j.preteyeres.2020.100923. Epub ahead of print.

• Lam CS, Tang WC, Lee PH, Zhang HY, Qi H, Hasegawa K, To CH. Myopia control effect of defocus incorporated multiple segments (DIMS) spectacle lens in Chinese children: results of a 3-year follow-up study. Br J Ophthalmol. 2021 Mar 17:bjophthalmol-2020-317664. doi: 10.1136/bjophthalmol-2020-317664. Epub ahead of print.
Eef van der Worp, BOptom, PhD, FAAO, FIACLE, FBCLA, FSLS is an educator and researcher. He received his optometry degree from the Hogeschool van Utrecht in the Netherlands (NL) and has served as a head of the contact lens department at the school for over eight years. He received his PhD from the University of Maastricht (NL) in 2008. He is a fellow of the AAO, IACLE, BCLA and the SLS. He is currently adjunct Professor at the University of Montreal University College of Optometry (CA) and adjunct assistant Professor at Pacific University College of Optometry (Oregon, USA). He lectures extensively worldwide and is a guest lecturer at a number of Universities in the US and Europe.


Family businesses have once again proven their worth in the corona crisis. With their entrepreneurship and sustainable business practices, they were able to respond more flexibly to the crisis than many large corporations. However, the pandemic also shows that structural changes are needed in family businesses. But regardless of how they position themselves in the future, the regulation of business succession remains a bottleneck for the secure continuation of every family business. The reasons for this are complex
By Carola JungwirthFamily businesses traditionally form the backbone of the economy, e.g. 89% of companies in Germany are family-run. In the USA, family businesses contribute around 54% of private sector GDP and are responsible for employing 59% of private sector workforce. The Institut für Mittelstand (a German institute for small and medium-sized businesses) assumes that half of all family businesses aim for internal succession. However, statistics show that only seven out of ten family businesses succeed in transferring to the second generation. Only two of the ten family businesses still exist in the third generation. And finally, only one family business in the fourth generation is still managed by the founding family at the operational or ownership level.
What exactly makes the cross-generational continuation of family businesses more difficult? Even though every family business is unique and every succession is individual, typical pitfalls that complicate the succession process emerge especially during the generational transition. The five most common are presented in this article.

The greatest challenge for family businesses is the interplay between family and business concerns. Unlike a business, a family is not designed for success, but for love and harmony. Both systems – if family and business are considered as two systems here – pursue different interests. Family businesses are particularly affected by these conflicting interests. The reason for this can already be seen in the name: in a family business there is always family and business. These two systems are blended when they interact. Ideally, both sets of interests should be taken into account when making business decisions in a family business. However, this is not always possible. Operationally, it becomes difficult when greater importance is attached to family peace than to professional aspects in important business decisions. Here is a case study: An entrepreneurial couple has two children and would like to start the family-internal generation change in the company. Both children have signaled their general willingness to take
IF THE SENIOR GENERATION RELINQUISHES INFLUENCE IN THE COMPANY AGAINST ITS WILL BUT CONTINUES TO RETAIN POWER IN THE COMPANY, IT UNDERMINES THE AUTHORITY OF THE SUCCESSOR GENERATION.
on the succession. One of the children is objectively more suitable for succession because of their education. If the two children were external applicants, the couple would have an easy time choosing – they would let the objective criteria speak for themselves. As parents, however, they want to treat their offspring equally, and so they decide to appoint a joint leadership team of both siblings as the new management. From a family perspective, it is understandable that parents want to treat their children equally. Equal treatment contributes to peace within the family. From a corporate perspective, this approach can cause problems. In the example case, the dual leadership, which was chosen for family reasons, could jeopardize the company's ability to act. If the two managing directors cannot agree, a stalemate situation may arise. This can also happen in the case of a non-sibling dual leadership. In the latter case, however, it is less likely that emotional arguments will lead to the stalemate.

A real-life example is also useful for this stumbling block: Advisory board meeting in the medium-sized family business. In addition to the three external advisory board members, the company founder and his successor daughter are present. Both are active in the company as managing directors. Future investments are to be discussed. In the middle of the discussion, the company founder takes off his spectacles, looks at the lenses and pushes the spectacles over to his daughter sitting next to him with the remark: “Could you clean them?”
The founder of the company did not communicate with his co-manager as the senior boss. Instead, it was the father who spoke to his daughter. It's hard to imagine that two unrelated
managing directors would speak to each other in this tone, even more so in front of third parties. Keeping roles separate is a daily challenge that only arises in family businesses. At Sunday coffee, the two protagonists still sit together as father and daughter. But as soon as they enter the company, their roles change. They have to put on a different „hat” in order to be able to meet as joint managing directors at eye level. This constant change of roles is difficult in many family businesses. It quickly comes across as artificial and wooden when trying to maintain a certain form and professionalism in the company with the person you meet on Sundays in the family circle.
Why does this role dilemma pose a threat to the success of corporate succession? When two generations of a company converse in a “parent-child” relationship, the authority of the successor generation is limited in its outward appearance. This applies above all to the perception of employees, who have a sixth sense for “true authority” in the company.
In some cases, senior entrepreneurs are still active in the company at the ripe old age of 75, whether operationally or at shareholder level.
For them, succession is primarily a process of letting go personally. That takes time. They probably spent most of their working lives in the company, so that it became their main purpose in life. Many long-time entrepreneurs remain in the company because they don't have a “plan B” for what their lives might look like without the family business.
This constellation can have a negative impact on the success of the company successor. If the previous management leaves the company only at an advanced age, the family successor may also already have passed the age of 50. For the next generation of executives, the long wait to take over the company
means a loss of energy and authority, and it blocks new entrepreneurial impulses. There is no objectively right time for company succession. According to the so-called rating criteria of the banks, the succession should be clarified by the 55th year of life of the company owners, i.e. there should be an appropriate plan. The handover process can easily take up to five years. This should be taken into account when planning the timeframe. If the succession cannot be arranged within the family, an external solution is an alternative. This is also a personal matter for the senior generation, which takes time and needs to be well planned. Succession planning under time pressure increases the risk of not achieving the best solution for those involved and the company.
Regardless of whether the company succession is to be handled internally or externally – the financial aspects of a succession can be a stumbling block for all variants. If the company is to be sold to an external successor, the purchase price expectations of the buyer and seller often diverge. It tends to be the owner/ seller who makes succession planning more difficult with unrealistic price expectations. Emotional aspects also play a role in this. As a rule, the owner is not just selling a company, but his life's work, in which he has invested energy, time and money for decades. Many entrepreneurs find it difficult to reduce their life's work to sober numbers. Unfortunately, life's work is not an assessment criterion when determining the value of a company.
In the case of internal succession, the main factor to consider is the tax burden involved in the transfer. If the company shares are to be transferred to the next generation free of charge, gift or inheritance tax will be incurred. If no reserves have been set aside for this purpose, the company may get into difficulties due to a lack of liquidity. After all, the tax office does not wait long to be paid for the transaction and, in case of doubt, the next generation is not in a position to pay the tax amounts from its private capital.
The success of an internal succession can also be jeopardized if the company shares are transferred to the next generation solely for tax-saving reasons. Tax advisors often suggest transferring the company shares to the children at an early stage in order to take advantage of gift tax allowances. However, if tax reasons are the sole reason for a generational change, the central question remains unanswered as to whether the current management is at all ready to take a step back in the company and relinquish power. If this is not the case, the senior management may keep (legal) loopholes open in order to
continue to exert influence within the company. This can be done, for example, by reserving retransfer rights.
If the senior generation relinquishes influence against its will but continues to retain some power in the company, it undermines the authority of the successor generation. This weakens the new management because there are no clear decision-making structures.
A company succession is only successful if the family business is led safely into the future while preserving family peace. The complexity of succession issues and the interplay between family and business aspects can best be resolved with professional support. After all, corporate succession is an individual and personal process that must be tailored to the needs of those involved if it is to succeed.
Two concrete measures are a good start to maneuver the flagship “family business” through the choppy sea of business succession:
A succession process is lengthy and extensive. In addition to numerous legal, tax and financial issues, there are personal issues to be addressed. To manage the complexity of this process, three to five years should be scheduled for the implementation of the succession and an individual succession strategy should be created with professional help.
During the succession process, conflicts may arise between family members. The more conflicts arise, the more important it is for the success of the succession to get disputes out of the way in good time, if necessary with outside support. Even legal or tax issues can pose a risk to a successful generational change. In addition, there may be conflicts within the family, the resolution of which is indispensable for securing family peace AND the future of the company.
In any case, the realization remains: those who are aware of the typical pitfalls in succession at an early stage take their force away and are also able to counter them proactively.
Succession consultant Carola Jungwirth advises family businesses and accompanies entrepreneurial families during their internal succession. As a lawyer and coach, she has extensive expertise in her work. Carola Jungwirth herself comes from an entrepreneurial family, worked for almost ten years as a legal advisor in a large construction group, and then managed her own family business as a managing partner in the 3rd generation. Since 2015, she has been working exclusively as a succession consultant. www.jungwirth-nachfolgeberatung.de

DAC International, Inc. Headquarters: 6390 Rose Lane Carpinteria, CA 93013 USA Phone: +1 805 684 8307 Fax: +1 805 566 2196 www.dac-intl.com info@dac-intl.com Europe: Phone: +44 (0) 7578 636 656 dgolden@dac-intl.com www.dac-intl.com

“Diamonds for all purposes”
APEX DIAMOND PRODUCTS LIMITED Unit 10, Bartleet Road, Washford Industrial Estate, Redditch,Worcestershire B98 0DQ
Unit 10, Bartleet Road, Washford Industrial Estate, Redditch, Worcestershire B98 0DQ
Tel: +44(0)1527 529011 Email: sales@apexdiamond.co.uk “Diamonds for all purposes”
United Kingdom
APEX DIAMOND PRODUCTS LIMITED www.apexdiamond.co.uk
Phone: +44(0)1527 529011 sales@apexdiamond.co.uk www.apexdiamond.co.uk
Diamond Tools
BRIO Ultrasonics
Calle Ciudad de Barcelona, 1J, Polígono Industrial Fuente del Jarro, 46988, Paterna, Valencia Spain
Phone: +34 96 134 11 09 info@brioultrasonics.com www.brioultrasonics.com
Phone: +41 41 372 10 10 Fax: +41 41 372 06 83 www.efclin.com info@efclin.com
Boston Materials Group Bausch + Lomb Wintergasse 32 69469 Weinheim Germany
Boston Materials Group Bausch + Lomb Wintergasse 32 69469 Weinheim Germany
Phone: +49 6201 17869 tanja.malkus@bausch.com susanne.krostitz@bausch.com www.fit-boston.eu
Contact Lens Material
T +49 6201 17869 F +49 6201 62184 tanja.malkus@bausch.com www.fit-boston.com
Contamac LTD Carlton House, Shire Hill Saffron Walden Essex CB11 3AU United Kingdom
Phone: +44 1799 514800 sales@contamac.co.uk www.contamac.com Contact
K & Y Diamond Ltd. 1801 Boul Saint Regis Dollard-des-Ormeaux (Quebec) Canada H9B 2M9
Phone: +1 514 676 0640 Fax: +1 514 676 0645 sales@kydiamond.ca www.kydiamond.ca

LAMBDA-X S.A. Avenue Robert Schuman 102 B-1400 Nivelles Belgium
Phone: +32 67 79 40 80 Fax: +32 67 55 27 91 info@lambda-x.com www.lambda-x.com
Instruments
Larsen Equipment Design 1117 N.W. 52nd Street Seattle, WA 98107 USA
Phone: +1 206 789 5121 Fax: +1 206 789 7756
erik@larsenequipment.com www.larsenequipment.com


OPTOCRAFT GmbH Am Weichselgarten 7 D-91058 Erlangen Germany

Phone: +49 9131 691500 Fax: +49 9131 691511 sales@optocraft.de www.optocraft.de
MisupcoTM Inc. 1378 Osceola Avenue Saint Paul, MN 55105 USA
MisupcoTM Inc. 1378 Osceola Avenue Saint Paul, MN 55105 USA
Phone: +1 651 353 8632 Fax: +1 651 698 0719 www.misupco.com mikef@misupco.com
Phone: +1 651 353 8632 Fax: +1 651 698 0719
mikef@misupco.com www.misupco.com
SCHNEIDER GmbH & Co. KG
Biegenstrasse 8 –12 35112 Fronhausen Germany
SCHNEIDER GmbH & Co. KG
Biegenstrasse 8 –12 35112 Fronhausen Germany
Phone: +49 (64 26) 96 96-0 Fax: +49 (64 26) 96 96-100 info@schneider-om.com www.schneider-om.com
Phone: +49 (64 26) 96 96-0 Fax: +49 (64 26) 96 96-100 info@schneider-om.com www.schneider-om.com

The App on your tablet, smartphone or computer.

CONTACT
The Website and the Magazine: The complete communication system for the contact lens industry. The magazine, 2,500 copies, is distributed to contact lens laboratories, wholesalers and other organizations active in the contact lens and IOL industry. The website www.g lobal-cl.com is free for all industry related professionals
PUBLISHERS ADDRESS
Eyepress Fachmedien GmbH Saarner Str. 151, D-45479 Mülheim a. d. Ruhr Tel.: +49-208-306683-00 Fax: +49-208-306683-99 Website: www.g lobal-cl.com E-mail: info@ g lobal-cl.com
p.sioutis@eyepress.de
Silke Sage, Efstathios Efthimiadis, Petros Sioutis
EDITOR-IN-CHIEF Dipl.-Ing (FH) Silke Sage silke@global-cl.com britta@mafo-optics.com

John Saniter, Bopfingen, Germany
EDITORIAL BOARD
Wim Aalbers, Erik Larsen, Eef van der Worp
PRODUCTION & LAYOUT Efstathios Efthimiadis
PressUp GmbH, Postbox 70 13 11, D-22013 Hamburg Tel.: +49-40-386666-308, Fax: +49-40-386666-299
MEDIA CONSULTANT
Tel.: +49-208-306683-20 Fax: +49-208-306683-99 constanze@global-cl.com
ADVERTISING AGENT GREAT CHINA
Beijing FOCUS Optics Culture Commnication Co. Ltd. Room 319, Building 2, Nr. 1, Northbank 1292,
ocus@126.com Skype: jennywang611
You do not have a subscription yet?
Just go to our website and make sure you get all the benefits.


Spanish culture combined with ancient and modern science has found Sitges/Barcelona to be the perfect location for business and leisure time as well. The 48th EFCLIN Congress & Exhibition takes place there from 28th – 30th April 2022. For an engaging lecture program, manufacturer’s forum and the best trade exhibition in the business, it can’t be beaten. It’s where the Contact Lens & IOL Industry from Europe, the Far East, North America and beyond come together… will you be there?