OPEN THE CONVERSATION Queen’s Film Theatre, Belfast December 12th, 2022

Introduction
Thank you for attending this special event today. We hope that this offers greater insight to the complex issue of injecting drug use and the work which is being done to alleviate many of the problems associated with this.
In July 2022, Extern issued a public call for the creation of an Overdose Prevention Facility in Northern Ireland. While this was in immediate response to a rise in drug-related deaths across Belfast during the summer months, this is an issue which Extern has been supporting for many years, in keeping with our person-centred, human rights-focused approach to tackling problem drug use.
We recognise that this is a complex and controversial issue, and in this leaflet we have outlined why we believe that such a facility is vitally needed in order to save lives and make our communities safer.
Aideen D’Arcy, Chair, Extern NI
A Critical Need…
The Spring and Summer of 2022 saw the deaths of at least 16 people on the streets of Belfast due to drug-related issues. While this generated a great deal of attention from the media and political representatives, this is a situation which presents on a regular basis for those engaged in problem drug use and the professionals who provide support to them.
21212625-34
deaths due to drugs were registered in NI in 2021 –over double that of 2011
of these drug-related deaths had an opioid mentioned on the death certificate
Drug-related death rates were highest among the 25-34 age group (26.9 deaths per 100,000 people).
9.4 deaths
NI had the second highest drug death rate in the UK –9.4 deaths per 100,000 population (Scotland had 25.0)
Harm Reduction: Current approaches
Harm Reduction is the overarching approach used to mitigate the risks associated with drug use and to promote better health outcomes. Important tools/measures in achieving this include: Take-home Naloxone - providing service users and staff with this life-saving drug which temporarily reverses an opioid overdose by blocking the opioid receptors in the brain Needle exchange and supply – providing sterile injecting equipment to drug users to promote safe disposal of used needles and other drugs paraphernalia Safer injecting guidance - offering advice and information to reduce injecting-related harm Training - providing up-to-date information across the workforce and service user group Advocacy - lobbying for rights-based change including measures to reduce overdose deaths Using the evidence base - learning from research about ‘what works’
Overdose Prevention Facilities
(Also known as Safe Injection Facilities, Supervised Injection Facilities, Drug Consumption Rooms, Medically-Supervised Injection Facilities, Safe Injecting Spaces)
What are Overdose Prevention Facilities?
Overdose Prevention Facilities (OPF) are specially designated spaces where people are able to take drugs safely, using sterile equipment, under the supervision of trained staff, who can respond immediately to overdose.
Reduce the transmission of blood-borne diseases such as HIV and hepatitis
OPFs
The Benefits
Offer opportunities for drug users to engage with healthcare staff, social workers, and other supports
Reduce overdose deaths
Reduce and treat infections and infection-related wounds
Reduce drug-related litter and the visibility of drug using within communities
How do OPFs work exactly?
Overdose Prevention Facilities can be located within both medical and community spaces and operated by a range of professionals including social care staff, those with medical training and peer supporters. To date, various models exist around the world but our aim is to promote a facility that ensures the health and well-being of its service users.
Can OPFs really have an impact on drug deaths?
Evidence provided by studies suggests that, where coverage is adequate, Overdose Prevention Facilities may contribute to reducing drug-related deaths at city level. A study in Sydney, Australia, showed that there were fewer emergency service call-outs related to overdoses at the times the safe injecting site was open, while the Insite Centre in Canada has helped reverse over 6,400 overdoses since 2003. Crucially, nobody has ever died of overdose in an OPF worldwide since they were first opened over three decades ago.
For the most part, drug use is still treated almost entirely as a criminal justice issue in the UK, meaning that vast amounts of resources are channelled towards seizures of drugs and arrests. In order for meaningful action to be taken, drug use must also be treated as a health issue, particularly for those who are trapped in a spiral of problem drug use.
The Global View
Overdose Prevention Facilities currently operate in 14 countries firs Preve wa Bern
Canada, Germany, Switzerland, France, Portugal, Ukraine, Norway, the Netherlands, Australia, Belgium, Spain, Denmark, Iceland and the USA
Since opening in 2003, over 3 million people have attended the Insite OPF in Vancouver, Canada
In December 2021, New York became the first city in the USA to open two overdose prevention facilities
The U first mob injecting unit in Scotland in staffed by v and opera nine mo
Why are we so far behind other countries in setting these up?
t
d
What is the legal position regarding OPFs?
Technically, any OPF which was opened in Northern Ireland would be contrary to current legislation, namely Section 8 of the Misuse of Drugs Act 1971 and Northern Ireland’s Criminal Law Act 1967 which requires an individual to report an offence if he/she knows that an offence has been committed.
The st Overdose ention Facility as opened in e, Switzerland in 1986
Ukraine opened its first overdose prevention facility in 2018 UK’s bile safe t was set up 2020. It was volunteers ated for onths.
By July 2020, Germany had 24 OPFs operating in 16 cities which focus on a person-centred, human rights ethos
Between 2001 and 2010, a facility in Sydney, Australia, recorded no deaths on the site out of 3,426 overdoses which occurred
Drug-related harm: A Canadian Perspective
- In 2012, Vancouver introduced a Take Home Naloxone (THN) programme, but the drug was only made available without prescription in 2016, six months after a National Emergency was declared due to drug-related deaths. During this four-year period the estimated loss of life was 3,691 people. These were parents, siblings, friends and loved ones.
- Vancouver BC sits on the indigenous territory of the Coast Salish people. Indigenous people in Canada are disproportionately represented in statistics when it comes to drug related deaths. Indigenous people make up 2.6% of the total population of British Columbia, but account for 10% of overdose deaths.
- Vancouver opened its first overdose prevention facility, Insite, in 2003 as a pilot evaluation project. It faced public opposition and scrutiny but has since recorded 48,798 clinical treatment visits and 6,440 overdose interventions without any deaths.
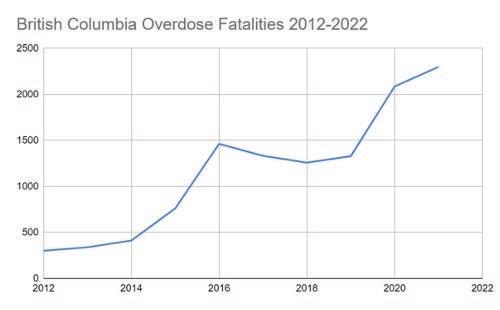
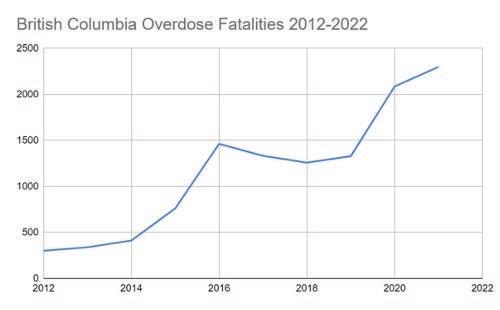
“In 2019, the population of British Columbia was 5 million compared to Northern Ireland which was 1.9 million, making it about a third of the size population-wise. Nonetheless, the exponential growth of drug-related deaths within the same decade is similarly represented in both of these graphs.

“Overdose deaths are not an issue with a single fix. Drug-related harm is tied to prohibition, multi-generational trauma and generational poverty. This is true of both British Columbia and Northern Ireland. Opening an overdose prevention facility will not provide a cure-all tomorrow. It will take a multi-disciplinary approach to fix the damage, and it will take multiple generations to do so. But if we don’t start now, then when?
“I plead with everyone reading this to understand and support the opening of this facility. I left Vancouver in May 2016 to move to Dublin, at the brink of this crisis, and have since watched from the other side of the world as my community suffers neglect and death. And it has broken my heart. My friends who are left fighting - working in supported living, in hostels, as street nurses, doing outreach, providing care to one another - are traumatised and burnt out. Several have died from overdose, some have taken their own lives.
“This is not something that affects one demographic of society. It affects us all.”
Lynn Jefferys, Operations Manager, European Network of People Who Use Drugs (EuroNPUD)
An ongoing journey
Establishing an Overdose Prevention Facility cannot happen without considerable input from a range of stakeholders, agencies and interested parties. And while there is no straightforward path to achieving this, there are a number of key areas for us all to consider moving forward:
Legal position – how a solution can be found to allow an OPF to operate without breaking the law
Stakeholder engagement – giving all relevant stakeholder communities an opportunity to discuss their views
Political lobbying – promoting the messaging to those who can effect change
Suitability - using the existing evidence to determine which of the medical, community or peer-led models would work best in NI
Impact - examining possible outcomes for an OPF and what this would mean for service users, stakeholders and commissioners
Evaluation – reviewing our learning to date to create a proposal for an OPF, and how this would be evaluated
Communication – explaining the benefits of OPFs to communities affected by drug use
Crucially, all of these ideas need to be explored against a backdrop of continued conversation with relevant agencies, groups and communities. So too do they need to co-exist with ongoing monitoring of trends and emerging themes amongst people who inject drugs, in order to gather data to enhance future service provision
Extern believes that Overdose Prevention Facilities are just one of a number of interlinked solutions to tackling problem drug use. We must also ensure that we continue to develop and promote the many other approaches to overdose prevention which exist, including the vital importance of early intervention/prevention.
Sources
Northern Ireland Statistics & Research Agency
European Monitoring Centre for Drugs and Drug Addiction Health Department, New York City
NSW Health, Australia
Transform Drug Policy Foundation Public Health England Drug Science
British Columbia Coroners Service
Vancouver Coastal Health
We would like to thank Lost Time Media for kindly releasing their film to the Queen’s Film Theatre for today’s special screening.
If you wish to discuss today’s event further with a member of Extern staff, please contact: comms@extern.org

For further information and resources on Overdose Prevention Facilities and the themes discussed here today, please scan the below QR code.