COULD THIS BE
Motor Neurone Disease? Alison Mudie of MND Australia tells the Bulletin how to spot the early stages of this debilitating disease
M
otor neurone disease (MND), a progressive and ultimately fatal neurodegenerative disease, is often clinically difficult to diagnose with insidious onset and different combinations of upper and lower motor neurone findings including changes in speech and swallowing. Dental professionals who are at the frontline of identifying early dysphagia and dysarthria now have access to a diagnostic tool developed for GPs and other health professionals by MND Australia. Painless, progressive weakness – Could this be motor neurone disease? highlights MND ‘red flags’ and aims to prompt early recognition of potential MND symptoms during health examinations and treatments. There is no single investigation specific to MND (also referred to as Amyotrophic Lateral Sclerosis or ALS) and no sensitive diseasespecific biomarker, so diagnosis is based on symptoms, clinical findings and the results of electrodiagnostic, neuroimaging and laboratory studies.1 In reaching a confirmation of MND, the diagnostic period is often lengthy. On average, the time from first symptoms to diagnosis is 14 months while, for people diagnosed with MND, the time from diagnosis to death is just 2.5 years. Rapid and accurate diagnosis is crucial in ensuring the needs of people living with MND are met from the earliest possible stage.
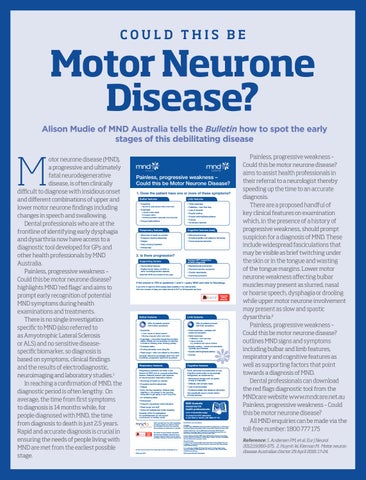
Painless, progressive weakness – Could this be Motor Neurone Disease? 1. Does the patient have one or more of these symptoms? Bulbar features
Limb features
• Dysarthria • Slurred or quiet speech often when tired
• Focal weakness
• Dysphagia • Liquids and/or solids • Excessive saliva • Choking sensation especially when lying flat
• Loss of dexterity
• Tongue fasciculations
• Falls/trips – from foot drop • Muscle wasting • Muscle twitching/fasciculations • Cramps • No sensory features
Respiratory features
Cognitive features (rare)
• Shortness of breath on exertion
• Behavioural change
• Excessive daytime sleepiness
• Emotional lability (not related to dementia)
• Fatigue
• Fronto-temporal dementia
• Early morning headache • Orthopnoea
2. Is there progression? Supporting factors
Factors NOT supportive of MND diagnosis
• Asymmetrical features
• Bladder/bowel involvement
• Positive family history of MND or other neurodegenerative disease
• Prominent sensory symptoms
Note that MND can present at any age.
• Double vision/ptosis • Improving symptoms
If the answer is YES to questions 1 and 2 – query MND and refer to Neurology. If you think it might be MND please state explicitly in the referral letter. Common causes of delay are initial referral to ENT or Orthopaedic services. Accepted clinical resource
Bulbar features
Limb features 70% of patients present with limb symptoms
25% of patients present with bulbar symptoms • Dysarthria • Quiet, hoarse or altered speech • Slurring of speech often when tired
• Dysphagia – more often liquids first and later solids. Initially can be sensation of catching in throat or choking when drinking quickly. • Excessive saliva • Choking sensation when lying flat • Weak cough – often not noticed by the patient Consider referral to neurologist rather than ENT if painless, progressive dysarthria is present.
• Focal weakness – painless with preserved sensation • Distal weakness • Falls/trips – from foot drop • Loss of dexterity e.g. problems with zips or buttons
• Muscle wasting – hands and shoulders. Typically asymmetrical. • Muscle twitching/fasciculations • Cramps
Respiratory features
Cognitive features
Respiratory problems are often a late feature of MND and an unusual presenting feature. Patients present with features of neuromuscular respiratory failure:
Frank dementia at presentation is rare. Cognitive dysfunction is increasingly recognised, as evidenced by:
• Shortness of breath on exertion
• Behavioural change such as apathy or lack of motivation
• Excessive daytime sleepiness
• Difficulty with complex tasks
• Fatigue
• Lack of concentration
• Early morning headache. Patients often describe a ‘muzziness’ in the morning, being slow to get going or as if hung over.
• Emotional lability (not related to dementia) Ask specifically about a family history of these features.
• Un-refreshing sleep • Orthopnoea • Frequent unexplained chest infections • Weak cough and sniff • Nocturnal restlessness and/or sweating Consider MND if investigations for breathlessness do not support a pulmonary or cardiac cause. MND Australia thank the MND Association of England, Wales and Northern Ireland for permission to amend and reproduce this publication for distribution in Australia.
Accepted clinical resource
The Motor Neurone Disease diagnostic tool has been officially recognised as an Accepted Clinical Resource by the Royal Australian College of General Practitioners.
MND Australia resources for health professionals: www.mndaustralia.org/gp To contact the MND association in your State or Territory call: 1800 777 175 Reviewed for use in Australia by: Neurology Dr William Huynh MBBS BSc (Hons), PhD, FRACP; Neurologist, Brain and Mind Centre, University of Sydney, Camperdown, NSW. Prince of Wales Hospital, Randwick, NSW. Professor Matthew C. Kiernan MBBS (Hons), PhD, DSc, FRACP; Bushell Professor of Neurology, Royal Prince Alfred Hospital. Co-director, Brain and Mind Centre, University of Sydney, Camperdown, NSW. Dr Susan Mathers MB ChB, MRCP (UK), FRACP; Clinical Director of Neurology, Calvary Health Care Bethlehem, Caulfield South, Victoria. Consultant Neurologist, Monash Medical Centre, Clayton, Victoria. General Practice Dr Catherine (Kate) George BMed, DCH (Dip Child Health), FRACGP; General Practitioner, The Leichhardt General Practice, Leichhardt, NSW. Clinical Editor, HealthPathways Sydney.
Creative proudly sponsored by DesignLogic Australia. designlogic.com.au
Dr Lara Mihaljevic MBBS, DCH (Dip Child Health), GradDip Public Health; General Practitioner DMC Medical Centre, Drummoyne, NSW. Clinical Editor, HealthPathways Sydney.
© Copyright 2016
MND Australia, State MND Associations.
Painless, progressive weakness – Could this be motor neurone disease? aims to assist health professionals in their referral to a neurologist thereby speeding up the time to an accurate diagnosis. There are a proposed handful of key clinical features on examination which, in the presence of a history of progressive weakness, should prompt suspicion for a diagnosis of MND. These include widespread fasciculations that may be visible as brief twitching under the skin or in the tongue and wasting of the tongue margins. Lower motor neurone weakness affecting bulbar muscles may present as slurred, nasal or hoarse speech, dysphagia or drooling while upper motor neurone involvement may present as slow and spastic dysarthria.2 Painless, progressive weakness – Could this be motor neurone disease? outlines MND signs and symptoms including bulbar and limb features, respiratory and cognitive features as well as supporting factors that point towards a diagnosis of MND. Dental professionals can download the red flags diagnostic tool from the MNDcare website www.mndcare.net.au Painless, progressive weakness – Could this be motor neurone disease? All MND enquiries can be made via the toll-free number: 1800 777 175 Reference: 1. Andersen PM, et al. Eur J Neurol 2012;19:360-375. 2. Huynh W, Kiernan M. Motor neuron disease Australian Doctor 29 April 2016: 17-24.