




 Photo courtesy of Mason Cole
Photo courtesy of Mason Cole
Letter from the Editors
Devan Patel and Swati Kumar

2 MRICloudyPy: Python Software for Processing and Visualization of MRICloud Brain Volumetric Data
Jeremy Telezing
10 Systematic Review of Smoking over Time in Maryland
Yashas Malikarjun
16 The scope of Wildfire Impacts and the Journey to the solution
Nandita Balaji
20 Vaccine Hesitancy and Pandemic Though the lens of chronic illness
Bea Manjon
26 An Ethical Analysis Genetic A Matarial Ownership
Devan Patel
34 Eirnin Mahoney Dangers of the Splash Zone: Educational Interventions to Reduce Waterborn Bacterial Infections in Hospitals
40
Jackson Cracking the Code on the Gen Z's Mental Health Crisis.
44
A Balancing Act: To What Extent Does Conformity Influence Vaccine Refusal?

We are pleased to present our 20th volume of Epidemic Proportions: “Shifting Focus,” a compilation of academic works by students at Johns Hopkins University provoking thought and engagement surrounding pressing public health topics in Baltimore and beyond.
From our perspective, the focus in the public health world for the past couple of years has been on the COVID-19 pandemic. However, many other public health concerns still affect our communities and have been overshadowed by the momentum of the pandemic and society’s cautious transition to a state of normalcy. This year’s theme aims to shift the spotlight to these other crises to paint a more comprehensive picture of today’s global public health scene.
Since our founding in 2005, our goal has been to highlight the research and experiences of our students and disseminate their accounts in an accessible manner to the larger community. Our authors and staff have shown great perceptiveness and sincerity in composing this journal and capturing a diverse collection of issues that continue to impact the health and wellbeing of our communities and the greater population. In this issue, we invite you to reflect on topics such as food insecurity, wildfire impact, genetic material ownership, and the rising adolescent mental health crises. We hope our articles will stimulate meaningful thought and discussion on the transition in public health focus from COVID-19 to a world advancing from the pandemic.
We believe that “Shifting Focus” is a timely and essential volume. As you read through our journal, we hope you are as inspired as we are to continue learning about the diverse range of public health topics that impact our communities as we move forward into a new period of healing and recovery.
Best wishes,
Devan Patel and Swati Kumar



Swati Kumar bio: Swati Kumar is a third-year student studying Neuroscience. Following graduation, she hopes to pursue a career in medicine and explore the intersection of research and healthcare, especially with applications to neuropathology and immunology. In her free time, she enjoys dancing, reading, or traveling.

With the growing incidence of brain disorders––progressive dementias in particular––in recent decades, further neuroscientific research is essential to understanding and slowing down this alarming rise. MRICloud is a brain mapping neuroinformatics tool used to generate hierarchical cerebral volumetric data from subject-specific magnetic resonance imaging (MRI) images. MRI data, and specifically MRI cloud data, is complex and difficult to work with. Generally, no software exists to convert even processed MRI data to analytic datasets for analysis, visualization, and further manipulation. Current data processing approaches require manual, error-prone procedures. Furthermore, these approach-
es involve managing interrelated hierarchical and subject volume information. Thus, a tool was developed to streamline MRICloud data processing. MRICloudPy is a Pythonic approach to reading, manipulating, and visualizing MRICloud data for analysis in brain science research. The Python library manages data with the library Pandas and visualization with the library Plotly Express. MRICloud data files are read and organized into a Python object inheriting Pandas’ DataFrame operations. The object is structured along a series of brain volumetric data parameters, including structural hierarchy. The stored data can be manipulated and accessed via a number of library methods. Additional methods were developed to generate relevant, interactive graphics and models to facilitate data analysis. MRICloudPy gives researchers an easy tool for creating analytic datasets, providing many visualizations and analyses out of the box. All code will be open-sourced and hosted on a version control platform with a forthcoming PyPI deployment.
Brain science research often uses brain imaging techniques such as MRI. MRI data is especially useful when observing and assessing neurodegenerative disorders such as Alzheimer’s disease.1
“More specifically, structural MRI data helps researchers examine the brain in terms of its geometry and size to extract relevant features.”
These measurements include but are not limited to, regional changes to the brain and relative volume changes. Given the observational nature of brain imaging data, models are a useful tool.
MRICloud is a cloud-based, neuroinformatics software developed to model these measurements. The software provides a supercomputational analysis of MRI imaging data to organize and output brain mapping data.2 The brain mapping data contains a hierarchical, segmented quantification of brain volume and geometry, which can be interpreted as a brain fingerprint.
This research project involved the development of Python software called MRICloudPy to process and visualize cerebral volumetric MRICloud data for further analysis. The software streamlines the widespread, error-prone process of organizing and modeling MRICloud data into readable modes. Without this tool, researchers are required to manually organize large MRICloud output datasets, a complex and tedious procedure. The tool aims to enable brain science research by eliminating a major obstacle in consolidating brain mapping data.
“The burden of brain disorders has grown drastically in recent decades across the United States, posing a pressing public health and biomedical threat.3”
Further brain science research is required to better understand this alarming rise and develop effective solutions and treatments. The increased efficiency offered by MRICloudPy helps facilitate such critical research.
Figure 1 depicts a compositional model of two martini beverages. The beverages vary in total liquid volume while sharing the same total glass volume. Although the taste of the martini is derived from the proportion of each ingredient relevant to the total liquid volume (i.e., the composition), the structural composition of the right beverage is derived relative to the total glass volume. This demonstrates the distinction of considering compositional hierarchies with different normalizing denominators.
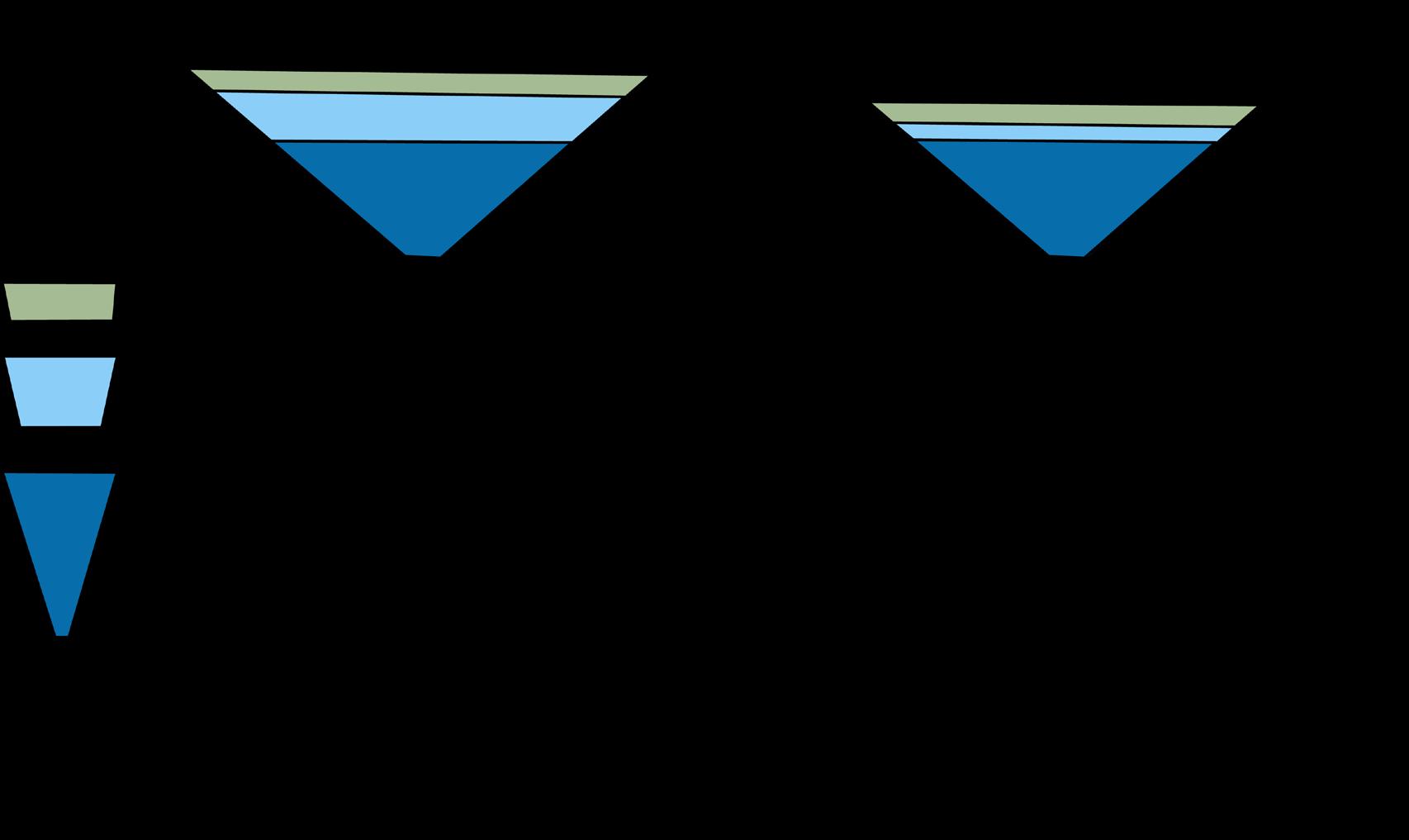
Like the martini example, volumetric analysis of the brain benefits from a similar strategy. The intracranial volume (ICV) of the brain serves as the “total glass volume” available to store brain matter. In contrast, the total brain volume (TBV) is the volume of brain tissue equivalent to the total liquid in the glass. Thus, similar to volumetric variations in martini ingredients, differences in the volume of brain regions are of interest when studied relative to ICV, TBV, and further compositional levels. The study of compositions, especially when they exist in a hierarchy, allows us to interrogate finely tuned questions about neuronal decline. Figure 2 highlights this principle. The parietal lobe volume highlighted in the far left and far right diagrams are equal relative to ICV, suggesting compositional equivalence in both brains. With the far left brain as a reference, the middle two brains are showing signs of structural atrophy, while the far right brain, despite having lower ICV and brain matter, does not. This concept informs researchers studying diseases that present with brain atrophy, like progressive dementias, and is equivalently useful for studying brain development.
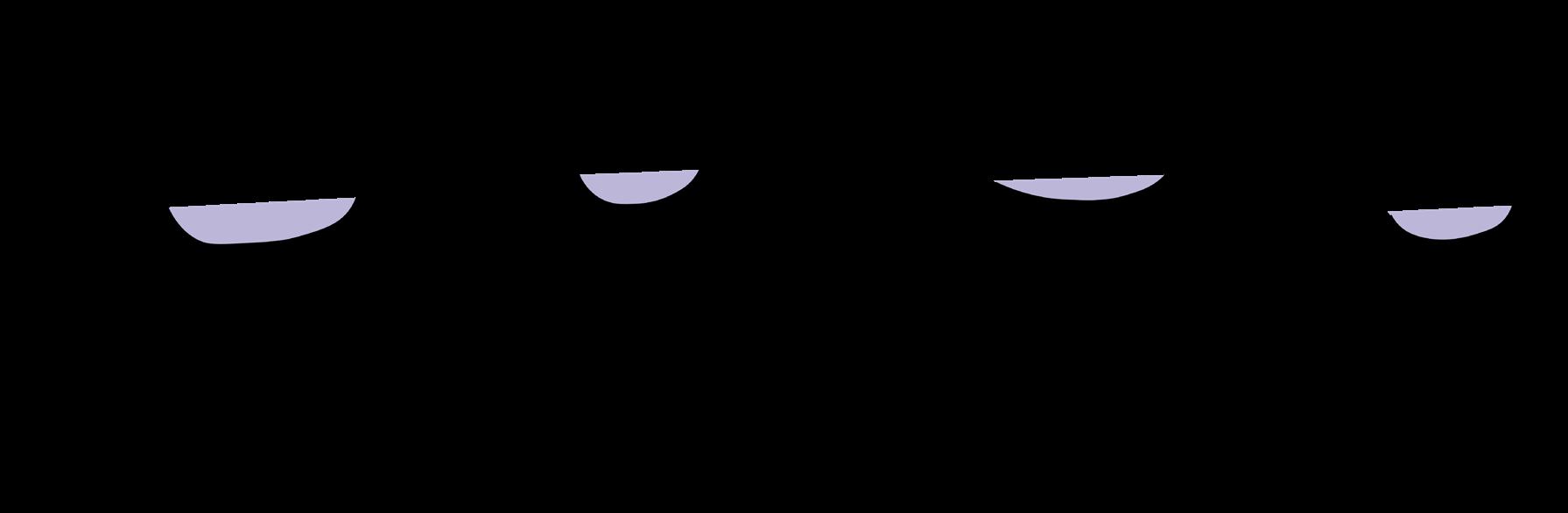 Figure 1. Composition of two martini beverages
Figure 1. Composition of two martini beverages
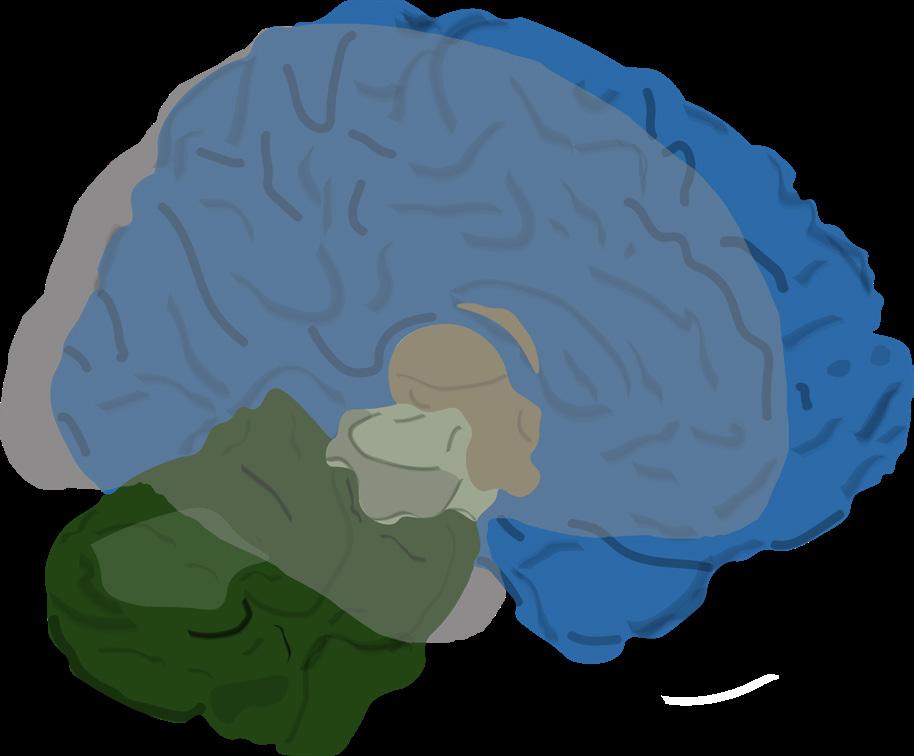
Figure 3 is a high-level compositional 3D rendering of a subject brain from MRICloud. The rendering visualizes one of the five increasingly granular hierarchical levels of the brain. The brain regions found at this specific level are highlighted in color. This level corresponds to a “Type 1” structural organization of the brain. The type of structural organization can be thought of as how one parcellates the brain. Just as a watermelon can be sliced in different ways for one’s serving needs, the brain can be “sliced” in different ways for one’s analytical needs. Different strategies for parcellating the brain include organizing by geometric landmarks, such as sulcal and gyral geometry, or by functional specialization (i.e., by areas that tend to serve the same
 Figure 3. Compositional 3D render of MRICloud subject
Figure 3. Compositional 3D render of MRICloud subject
functional purpose). Of course, these two kinds of parcelations overlap, but not perfectly. For example, bilateral function of symmetrically opposite regions in the two hemispheres is quite common, even if the areas are geometrically separated. MRICloud offers two types of structural organizations, referred to as “Type 1” and “Type 2,” which are primarily defined via neuroanatomy organization. It is worth noting that our software would require little change if a new hierarchical organization, such as one entirely predicated on function, was used instead.
MRICloudPy takes an object-oriented approach to creating analyzable and manipulatable MRICloud datasets. Steps 1–5 of the example workflow demonstrate a sample use case of the tool. Step one highlights the package importing process, giving users access to the MRICloudPy tools within their project. Step two introduces the creation of a dataset object from a given file path containing a collection of MRICloud data files for multiple patients. These data files are read and stored into the ‘dataset’ object to run a series of object methods. Step 3 illustrates one of these methods being called upon the dataset object named ‘long_to_ wide.’ This method converts a long, or vertically oriented dataset, to a wide, or horizontally formatted dataset, where each row or entry corresponds to a patient file and each column corresponds to a relevant field.
Step 4 shows various visualization methods being called. This would produce interactive data visualization models, which output to an interactable environment, such as a web browser. An interactive high-level “Type 1“ volumetric sunburst model visualizes the proportional volumetric structure of the brain through increasingly narrowing subdivisions. This allows users, for example, to compare patient brains to healthy controls and recognize notable atrophies and their corresponding regions. An Interactive Bland-Altman/mean difference plot describes the comparative volumetric differences between the left and right hemispheres of a patient’s brain. Users can visualize and investigate potential regional differences in a patient’s

brain between the left and right hemispheres, which may be present due to underlying brain atrophy. An interactive volumetric correlation matrix heatmap details the volumetric correlations between a number of brain regions. This is useful in assessing how the size of different regions depends on or relates to one another, which can help in understanding structural composition.
Alzheimer’s disease is a neurodegenerative brain disorder that currently lacks a cure or many effective treatments. Importantly, the prevalence of Alzheimer’s disease has risen dramatically over the last few decades with no sign of slowing down. Alzheimer’s disease mainly affects those aged 65 or older with 6.2 million individuals, or more than 1 in 9 members of that population group, living with the disease as of 2021.4 Without preventative measures to slow down or cure Alzheimer’s disease, a projected 7.2 million people could be affected by 2025 and 13.8 million people by 2060. Furthermore, deaths from Alzheimer’s disease have increased 145.2% between 2000 and 2019.5 Without adequate intervention, Alzheimer’s will place additional strain on our nation’s public health infrastructure, owing to increases in its prevalence, mortality, and depletion of health care resources, in addition to a worsening of its negative impacts on caregivers. These consequences pose major implications for the overall well-being of the United States’ increasingly aging population.
“Sociocultural elements beyond interpersonal discrimination exist in the form of racist systems and guidelines that outline countless societal institutions.”
Importantly, Alzheimer’s disease notably affects certain groups of people disproportionately, even in the dementia caregiving population. Older Black and Hispanic populations are disproportionately affected by Alzheimer’s disease compared to their white counterparts.5 Evidence suggests the stark difference in incidence rates is largely explained by disparities in medical, socioeconomic, and health-behavior conditions.6 These medical disparities include an elevated risk of chronic conditions, such as heart disease, that are associated with an elevated risk of developing Alzheimer’s disease.5 Socioeconomic disparities include poor levels and quality of education, higher poverty rates, and high exposure to adverse discrimination.5 Both historic and systemic racism play a part in creating and exacerbating these disparities. Sociocultural elements beyond interpersonal discrimination exist in the form of racist systems and guidelines that outline countless societal institutions. These institutions include the medical, law, banking, criminal justice, and occupational systems to name a few.5 Consequent disparities in areas such as health care access, environmental hazard exposure, and occupational safety, especially in early life, influence the risk of developing Alzheimer’s disease.5
In addition to incidence disparities, certain groups face increased likelihood of a missed or delayed dementia diagnosis event. Relative to non-Hispanic white populations, non-Hispanic Black and Hispanic populations averaged a 3-month and 1-year delay in diagnosis of dementia symptoms, respectively.7 Furthermore, at the time of diagnosis, these disparities persisted in dementia severity, with both groups presenting statistically significant declines in cognitive function compared to the reference.7
With diseases like Alzheimer’s, it is only a recent occurrence that disproportionately affected groups are being extensively examined and included in treatment research. This phenomenon is present across a variety of public health research areas and contributed to widespread, longstanding misconceptions about how certain groups were affected by various public health threats, alongside a severe lack of knowledge of how to address them. Moving forward, it is essential for public health researchers to not only include and con-
sider different groups in their studies but also separate analyses that consider how historical and systemic threats contribute to the respective public health findings. Additionally, researchers can create socio-economic- and race-conscious methodologies and study specific underrepresented groups, centering future studies on such groups.
Impacted groups are represented indirectly via the accessible nature of the software. By releasing the software with an open-source license on a free and accessible version control platform, researchers from any institution, background, or country can use this tool to examine underserved and disproportionately affected populations anywhere in the world. Furthermore, researchers can append different software features and functionalities to the existing software to streamline sorting and filtering data based on valuable and applicable characteristics present in disproportionately affected populations. These features may include adding new subject data parameters relating to demographic characteristics such as race, ethnicity, income, age, educational attainment, geographic residence, etc. These elements can be tailored by specific labs to search for answers to specific questions about specific groups. It should be noted that more can be done to address potential disparities in awareness of the tool as well as convenient access to it. Moving forward, it is important that extensive documentation exists for the tool in conjunction with widespread and simple access to the software. Ultimately, this combination will help facilitate critical research on how Alzheimer’s disease affects underserved populations, with as much ease for all institutions and groups as is possible.
1.Chandra, A., Dervenoulas, G., Politis, M., & Alzheimer’s Disease Neuroimaging Initiative (2019). Magnetic resonance imaging in Alzheimer’s disease and mild cognitive impairment. Journal of neurology, 266(6), 1293–1302. https://doi.org/10.1007/s00415-0189016-3
2.Mori, S., Wu, D., Ceritoglu, C., Li, Y., Kolasny, A., Vaillant, M. A., Faria, A. V., Oishi, K., & Miller, M. I. (2016). MRICloud: Delivering high-throughput MRI neuroinformatics as cloud-based software as a Service. Computing in Science & Engineering, 18(5), 21–35. https://doi.org/10.1109/mcse.2016.93
3.GBD 2016 Neurology Collaborators (2019). Global, regional, and national burden of neurological disorders, 1990-2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet. Neurology, 18(5), 459–480. https://doi.org/10.1016/S14744422(18)30499-X
4.Rajan KB, Weuve J, Barnes LL, McAninch EA, Wilson RS, Evans DA. Population estimate of people with clinical Alzheimer’s disease and mild cognitive impairment in the United States (2020-2060). Alzheimers Dement. 2021;17(12):1966-1975. doi:10.1002/ alz.12362
5.2022 Alzheimer’s disease facts and figures. Alzheimers Dement. 2022;18(4):700-789. doi:10.1002/alz.12638
6.Glymour MM, Manly JJ. Lifecourse social conditions and racial and ethnic patterns of cognitive aging. Neuropsychol Rev. 2008;18(3):223-254. doi:10.1007/s11065-008-9064-z
7.Lin PJ, Daly AT, Olchanski N, et al. Dementia Diagnosis Disparities by Race and Ethnicity. Med Care. 2021;59(8):679-686. doi:10.1097/MLR.0000000000001577

Jeremy is a senior majoring in Public Health Studies with a focus in biostatistics. He is interested in the application of data science to both public health and clinical care. Some of his work involves building machine learning models and software tools to streamline the development of health solutions.


America was arguably built on tobacco and its products. The rich tobacco exports from Virginia helped build the current capital of the United States.1 Now, we face a public health crisis hinging on the continued use of tobacco: smoking.
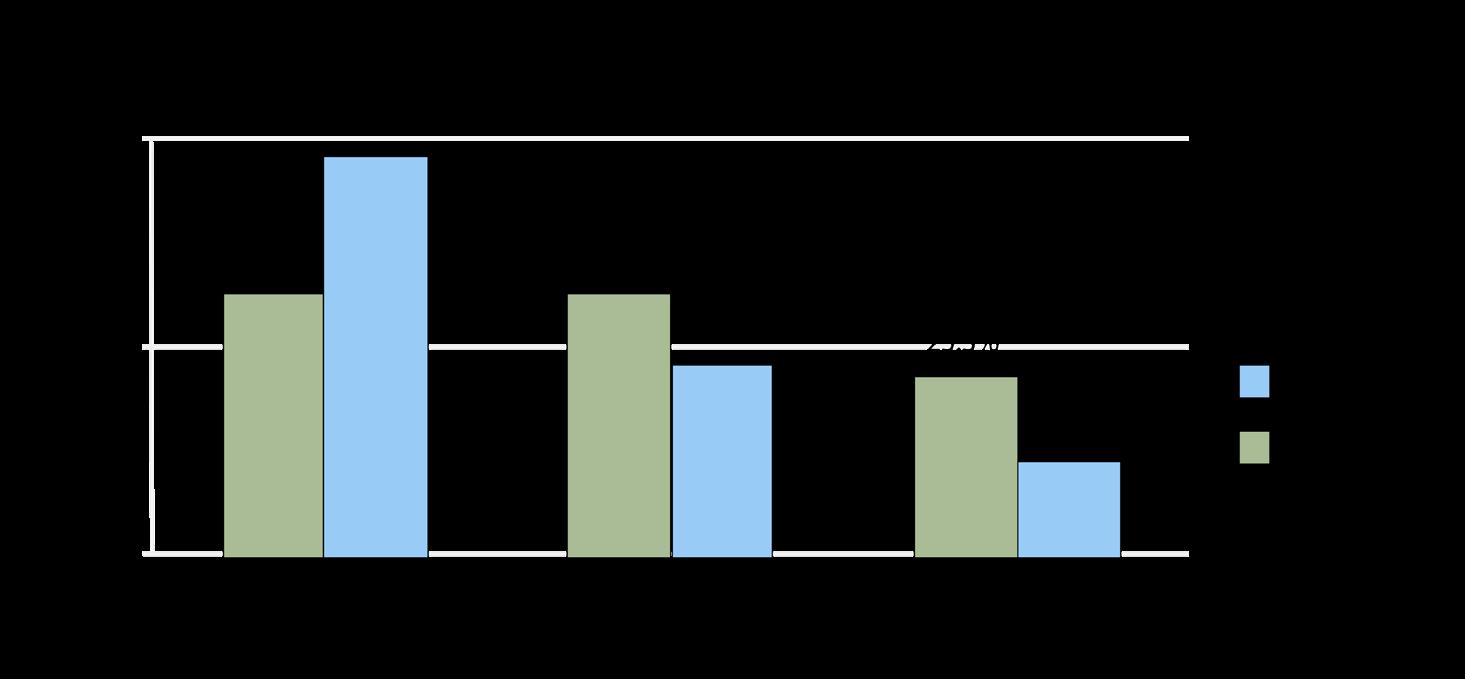
Smoking is defined as the action or habit of inhaling and exhaling the smoke of tobacco.2 Smoking rates in Maryland may be lower than the national average (Figure 1a)3; however, the negative impact of smoking remains significant and concerning. According to the CDC, smokers are very likely to develop “cancer, heart disease, stroke, lung diseases, diabetes, and chronic obstructive pulmonary disease.”4 Cigarettes contain chemicals known as carcinogens and inhaling the smoke itself damages the alveoli in the lungs.4 The complication to addressing the epidemic of smoking is the fact that nicotine, the active chemical in tobacco, is a highly addictive substance, comparable to “heroin or cocaine”.5 This leads to the premature deaths of over 7,500 adults from Maryland each year.6 Additionally, secondhand smoke can cause these problems in smokers’ family members and children, magnifying the impacts of smoking by affecting vulnerable populations such as children and the elderly.7 In general, smokers have a lower average well-being compared to non-smokers (Figure 1b).6
Figure 1a - Smoking rates in Maryland vs Nationally over Time (www.americashealthrankings.org/)
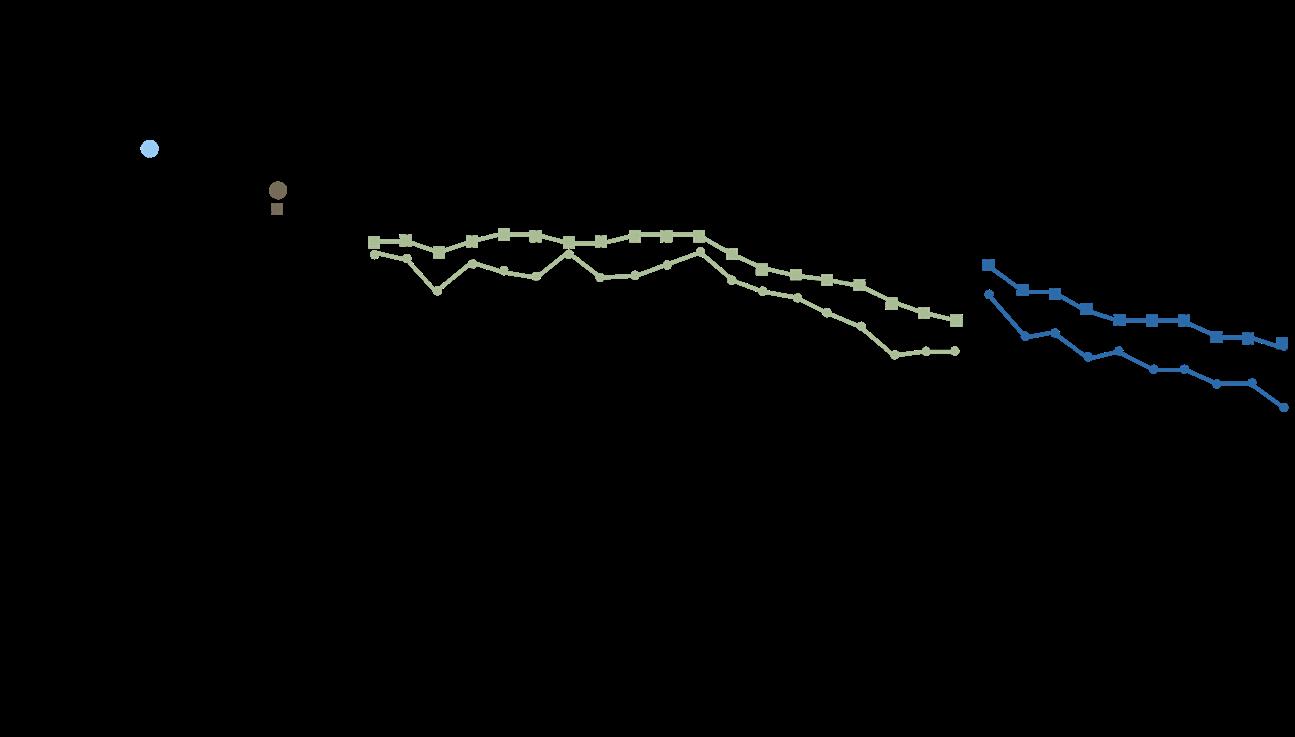
Figure 1b - Health Status of Smokers vs Non-smokers (health.maryland.gov/)
These severe consequences of smoking demand attention and categorize smoking as a public health emergency. Smoking itself also lacks a severe societal stigma found with other illicit substances, resulting in 16.6% of adults in Maryland, a sizable amount of the state’s population, smoking any kind of tobacco.8 Managing smoking requires a lot of resources; people who smoke require primary care doctors, end of life care, cancer treatment, and COPD medication -- all of which can be billed to the taxpayer in certain cases (such as with Medicaid or Medicare).9 2.71 billion dollars is spent each year in Maryland to care for individuals that have health problems due to smoking. This has resulted in an increased tax burden of $1,120 dollars per household, regardless of smoking status.9 Thus, in addition to preserving human life, the incidence of smoking must be reduced to prevent economic pain to low income households. This issue brief will describe the smoking’s consequences and discuss theoretical ways to alleviate the worst harms to solve the widespread social impacts of smoking.
The proportion of smoking is about the same for each Race/Ethnicity except for Native American/Alaska Native subgroups (Figure 2a).6 So, it would be reasonable to assume that these communities should receive more resources for smoking related treatment.
However, the disparity of health related problems due to tobacco does not exactly match this table. According to the Maryland Department of Health, “despite lower tobacco use rates, Black/African-Americans are dying from lung and bronchus cancer at a similar rate to Whites (44.2 and 44.3 per 100,000 respectively).”6 Thus, Black/African Americans should be receiving substantial healthcare resources to combat the health disparity. This surprising disparity between smoking and smoking related health problems shows that a comprehensive measure of health issues due to smoking is necessary to determine exactly where public health resources are allocated.
One theory that explains this disparity is the heavy marketing of mentholated cigarettes. According to the FDA Tobacco Products Scientific Advisory Committee, mentholated cigarettes are more addictive and easier to smoke than regular cigarettes, causing individuals that use mentholated cigarettes to “binge smoke.” Binge smoking increases the probability of negative health effects due to smoking and reduces the probability of quitting.10 Evidence seems to support the Mentholated cigarette theory (Figure 2b).6 Studies have also found that in the 1950s, mentholated cigarettes were heavily marketed to African American Communities.11 The FDA has banned the use of flavors in cigarettes, however, it still permits the use of menthol.11 Regulation
Figure 2aSmoking by Race (https://health.maryland. gov)
Figure 2bUse of Mentholated Cigarettes (https://health.maryland.gov)
on menthol could be highly effective in reducing smoking related health disparities in Maryland and across the country.
Incidence of smoking is highly linked with socioeconomic status. Individuals are less likely to smoke as their income or education level increases (Figure 3).6 Thus, intervention efforts should be focused on low-income communities. Large-scale poverty alleviation through mechanisms such as increased financial assistance, raising minimum wage, or expanding state education grants would likely address the smoking crisis by uplifting low-income communities and increasing access to rehabilitation programs.
Smoking rates by geography is a more complicated trend. Heavily urban areas and rural areas of Maryland both suffer from high rates of Lung cancer.6 For example, Somerset County (population 25,699) has a similar rate of mortality and incidence as Baltimore City (population 602,274). Therefore, it is difficult to determine or predict disparities through geogrpahic location alone. A possible solution, albeit expensive, could be to fund survey and community out-reach programs to provide surveillance on communities that most require interventional assistance.
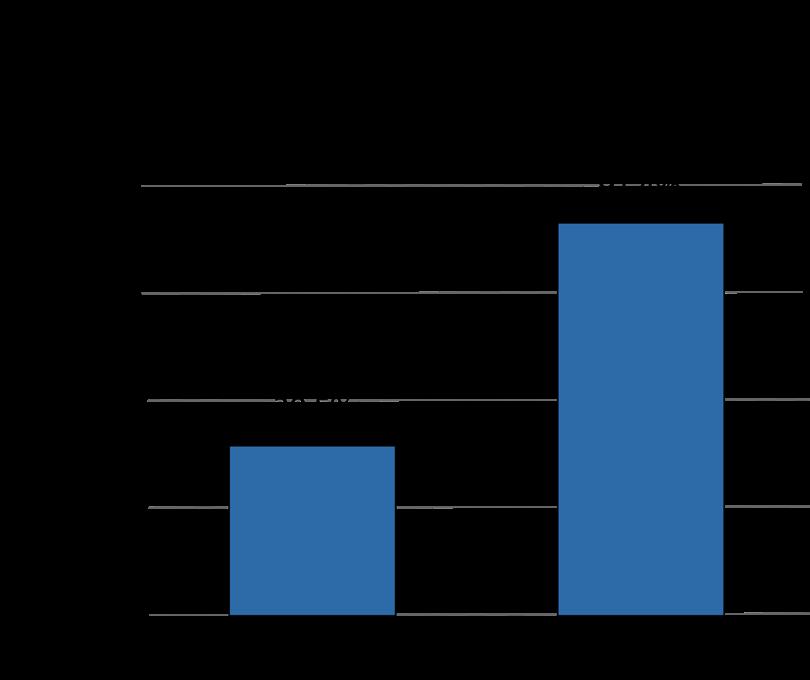
Most concerning, perhaps, is that younger individuals are smoking at the same rates as adults. Rates of smoking in high schoolers in Maryland are comparable to rates of smoking of adults, differing by about two percentage points.6 Furthermore, because younger individuals are more susceptible to the health problems from smoking, high smoking rates among children and young adults significantly compounds smoking’s health and financial consequences. Furthermore, they are also more likely to develop other substance use
Figure 3 - Smoking by Socioeconomic Status and Education Level (health.maryland.gov/)
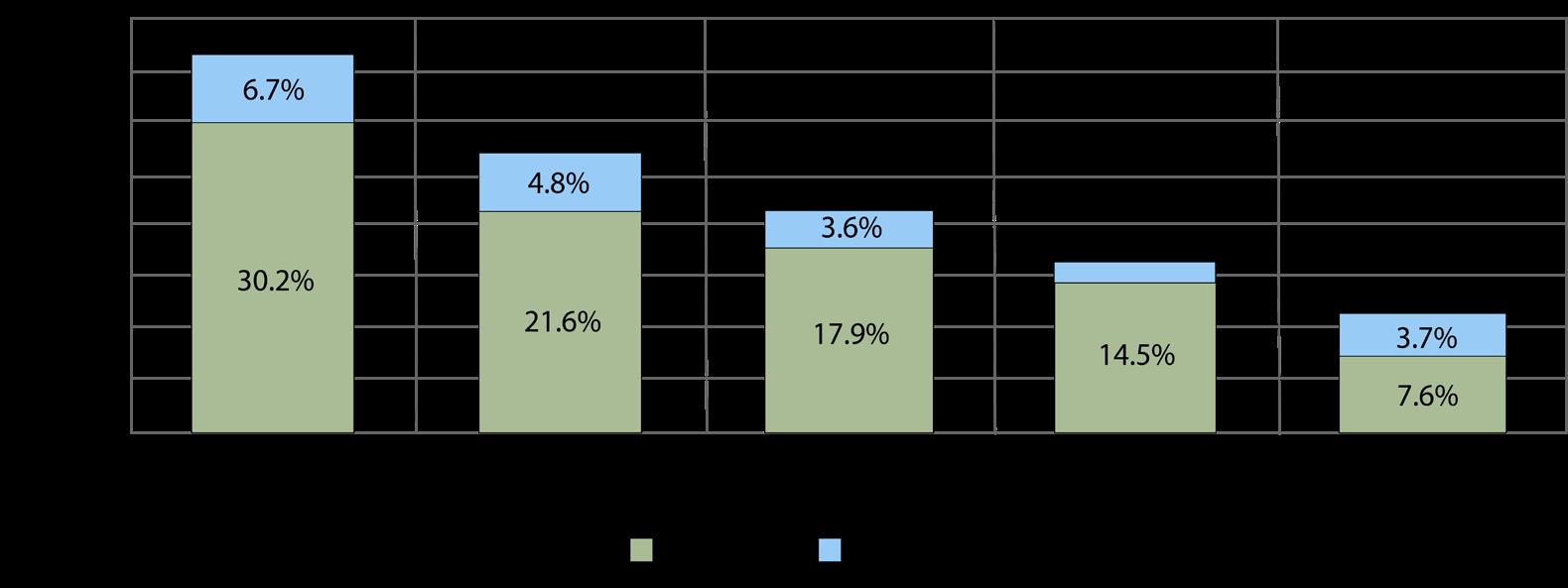
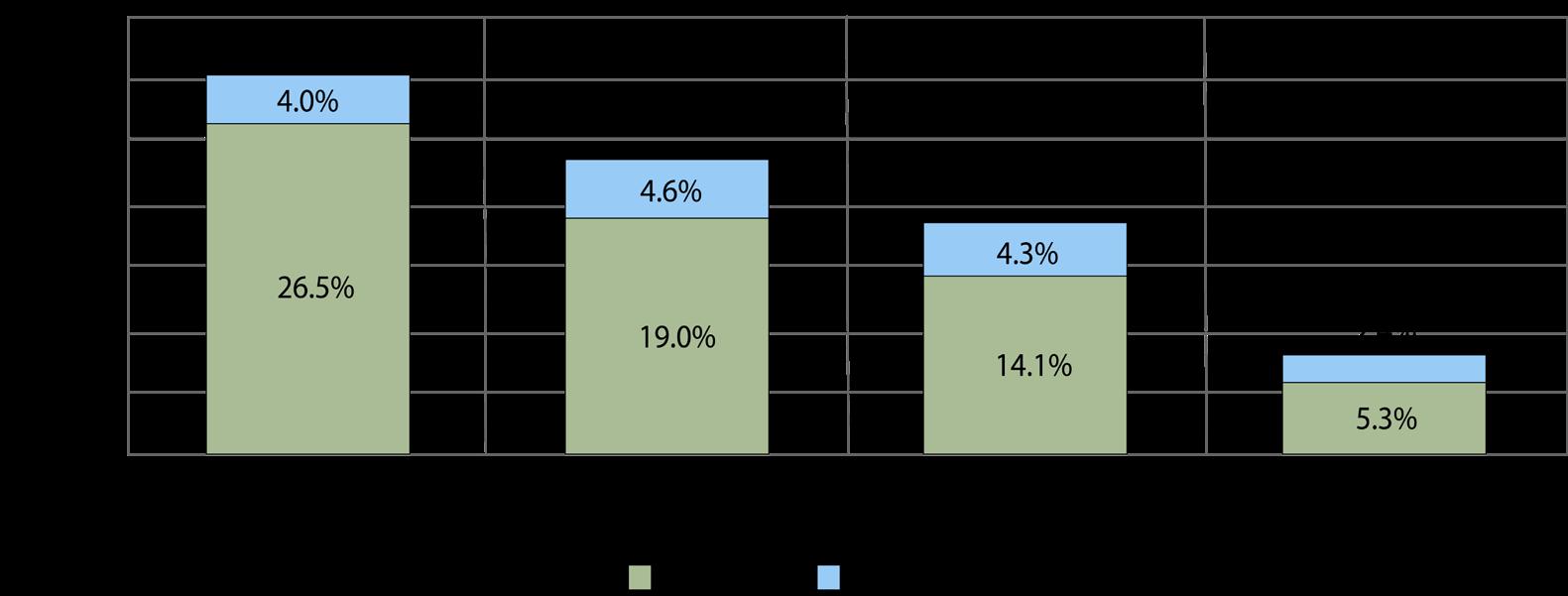
Figure 4 - High School Youth use of Tobacco Products (health.maryland.gov/)
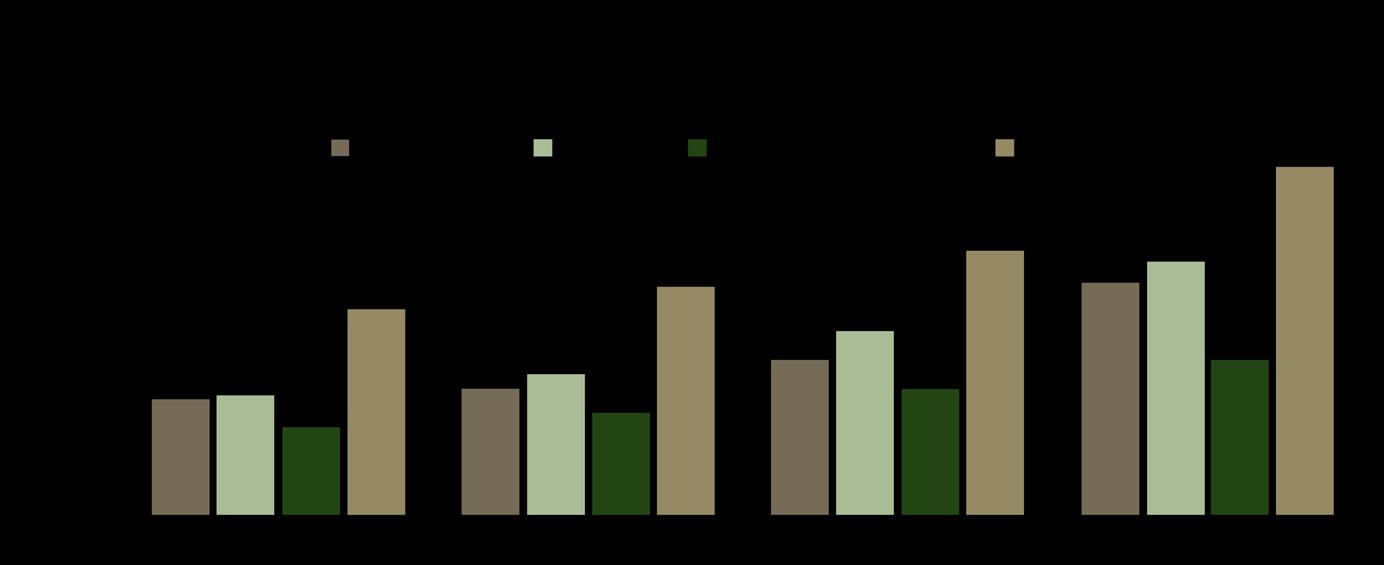
disorders if they start smoking at a young age.6 Regardless of the progress made by Maryland in curbing youth smoking,
“92,000 children have their lifespans reduced due to smoking,”
a number significant enough that increased legal enforcement and penalties should be considered to reduce this number.9 There are already some laws that attempt to regulate tobacco consumption and curb use. The most significant is the Maryland law that raised the age to consume and buy tobacco products to 21. However, these laws are unsuccessful: according to the CDC, only “37% of Maryland youth reported being asked to provide photo ID” and “70% of youth smokers reported being able to purchase cigarettes directly or by proxy.”12 However, there has been some success by increasing law enforcement presence near tobacco and cigarette stores; illegal tobacco sales to minors “declined by 56% from 2014 to 2015” with the implementation of a legal regime to control youth smoking.12
In this brief we have made a few key findings about smoking. First, smoking disproportionately affects certain races when considering health outcomes due to smoking. Second, smoking is heavily linked to socioeconomic status. Third, there is not a good way to allocate smoking treatment resources based on geography. Finally, youth smoking rates have grown considerably and become comparable to their adult counterparts in Maryland.
Figure 5 - Methods Used to Quit Smoking (health.maryland.gov/)
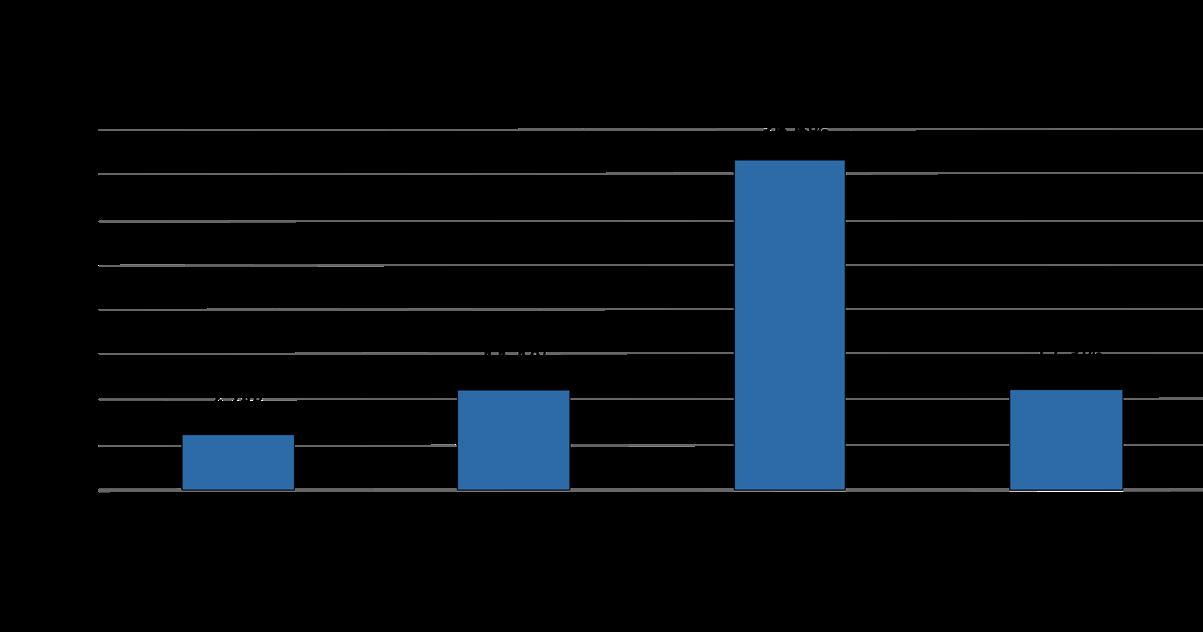
Smoking represents a relatively small portion of health problems by incidence, but has incredibly high mortality rates, meaning that elimination is of the utmost priority.6 Some solutions for reducing the incidence of smoking and negative health outcomes were already explained in previous sections.
A promising solution is to promote funding for the research and implementation of medical treatments for addiction through neurological pathways. Medication is most frequently used for addiction treatment, suggesting that it is likely the most effective (Figure 5).6 In tandem banning menthol cigarettes and expanding legal enforcement against youth tobacco sales, resources for medical treatments for addiction will be effective in reducing rates of smoking by targeting addiction neurologically. Additionally, these resources must be allocated in such a way that considers the disparities in smoking with race and socioeconomic status that were explained above.
1.Star Agritech. Virginia tobacco: How it’s grown and the history. Star Agritech Tobacco Leaf Supplier. https://staragritech.com/ virginia-tobacco-how-its-grown-and-history/. Published May 3, 2021. Accessed September 16, 2022.
2.Jack Henningfield. Smoking. Encyclopedia Britannica.
https://www.britannica.com/topic/smoking-tobacco. Accessed September 16, 2022.
3.Explore smoking in maryland: 2021 annual report. America’s Health Rankings. https://www.americashealthrankings.org/explore/annual/measure/Smoking/state/MD. Accessed September 16, 2022.
4.CDC. Health effects of smoking. Centers for Disease Control and Prevention. https://www.cdc.gov/tobacco/basic_information/ health_effects/index.htm#:~:text=Smoki ng%20causes%20cancer%2C%20heart%20disease,immune%20system%2C%20includin g%20rheumatoid%20arthritis. Published April 28, 2020. Accessed September 16, 2022.
5.Cancer.org. Why people start using tobacco, and why it’s hard to stop. American Cancer Society.
https://www.cancer.org/healthy/stay-away-from-tobacco/why-people-start-using-tobacco. html. Accessed September 16, 2022.
6.Maryland Department of Health. Monitoring changing tobacco use behaviors: Maryland 2000 - 2016. Maryland Department of Health.
https://health.maryland.gov/phpa/ohpetup/Documents/2000%20-%202016%20Legislativ e%20Report%20Monitoring%20 Changing%20Tobacco%20Use%20Behaviors.pdf. Published 2017. Accessed September 16, 2022.
7.Maryland Department of Health. No tobacco sales to minors. Maryland Department of Health.
https://health.maryland.gov/notobaccosalestominors/Pages/Tobacco%2021%20FAQ.aspx #Background%20Information. Published 2022. Accessed September 16, 2022.
8.Maryland Department of Health. Center for tobacco prevention and control. Maryland Department of Health. https://health. maryland.gov/phpa/ohpetup/Pages/tob_home.aspx. Accessed September 16, 2022.
9. Tobacco-Free Kids. The toll of tobacco in maryland. Campaign for Tobacco-Free Kids. https://www.tobaccofreekids.org/problem/ toll-us/maryland. Published January 21, 2022. Accessed September 16, 2022.
10.J Thompson. Warning to Saturday night ‘binge smokers’. The Independent. https://www.independent.co.uk/life-style/ health-and-families/health-news/warning-to-sat urday-night-binge-smokers-80638.html. Published November 30, 2003. Accessed September 16, 2022.
11.Mills S, Ribsel R. Study finds menthol cigarette marketing targets African-Americans. UNC Gillings School of Global Public Health. https://sph.unc.edu/sph-news/study-finds-menthol-cigarette-marketing-targets-african-am ericans/ 12.Smoking. This, 9-14-2021, “Extinguishing the Tobacco Epidemic in Maryland,” Centers for Disease Control and Prevention, https://www.cdc.gov/ tobacco/stateandcommunity/state-fact-sheets/maryland/index.html

Yashas is a sophomore majoring in Public Health and Biology. His interests in the field usually consist of social determinants of health and novel statistical approaches related to their interpretation. During his free time Yashas enjoys listening to the NPR politics podcast.

During my freshman year of high school in Charlotte, North Carolina, a series of wildfires erupted across the Appalachian mountains leaving behind dense smoke clouding my high school campus. Because of these conditions, our teachers urged us to stay inside to limit smoke exposure and health risks associated with such exposure. Later that November, I learned that we had experienced the effects of some of the Appalachian mountains’ record-breaking fires. These fires, despite being 100 miles away from my high school campus, had significant impacts on my daily life. If a wildfire this far away could have such pronounced effects, what could this mean for the communities directly in contact with these fires?
While taking a closer look at how wildfires are currently detected, I was shocked to learn that most fires start in remote environments and can burn for days or weeks before detection by human sight. By then, it's often too late. These mega-fires require far too many resources to contain, leaving millions of vulnerable citizens and landscapes destroyed. Whether it's deploying a skilled firefighting team to remote, hard-to-access environments requiring protective gear or using aerial firefighting tools to limit the fire’s spread, wildfire response teams are often stretched thin when fighting these threats. Ultimately, I realized the severe need for a wildfire response solution in these remote, vulnerable environments.
To make matters worse, the current climate crisis is raising global temperatures and worsening drought conditions, creating ideal conditions for wildfires to thrive. Since 1980, the average number of acres burnt in the U.S. has only increased;
"In 2020’s wildfire season, wildfires burned more acres, incurred more in damages, and released more carbon dioxide than ever before."1
Specifically, the fires in 2020 released more than double the average per year for the past two decades, with 127 million metric tons of carbon dioxide equivalent released by the fires in the U.S. alone.2
Troubled by these wildfires’ impact on communities across our country, a team of three other students and I decided to take action and began ideating a solution for early wildfire detection. After countless prototypes and environmental research over the course of seven years, we transformed what began as a giant stainless steel box with sprayable foam insulation into a real-world, commercially viable venture. Together, we’ve founded InfernoGuard, a startup dedicated to providing landowners with the tools needed to protect themselves from the world’s fastest growing climate crisis. The path to wildfire response is currently fragmented and inefficient. From proactive risk assessment and mitigating action to wildfire detection and emergency response, there are plenty of components to addressing the wildfire crisis; we’ve developed the solution that connects this dynamic process to eradicate the megafire crisis overall. Together, we have raised over $430,000 in funding towards our venture and have scaled our team to 15 employees across four universities as we bring our solution to market. We are bringing our wildfire risk assessment software to landowners in the spring of 2023, and we are incredibly excited and dedicated to our mission of limiting these impacts across the globe. In the process of founding a technology startup, I’ve gained valuable experience building and collaborating with a diverse team, navigating the unique entrepreneurial journey as a college student, and networking with industry leaders. What has truly been the most eye-opening part of this experience, though, is connecting with landowners firsthand about their diverse experiences with wildfires. I’ve spoken with over a hundred landowners, firefighters, industry experts, and citizens in areas at elevated risk of experiencing wildfires, which has provided me with a holistic understanding of wildfires and their impacts across sectors. In hearing their stories, I’ve learnt that forest fires pose much more than just a threat to land and the environment – these uncontrollable natural disasters can wreak economic damage, destroy community well-being, and pose serious health risks to both individuals and communities. This understanding of the
massive scope of this growing climate crisis fuels my team’s devotion to our mission as we bring our product to the spaces that need it most.
For citizens in high-risk areas, wildfires pose a constant threat to their livelihoods, as even a single fire can destroy decades of labor and investment. In fact, these natural disaster impacts are a regular and devas tating occurrence for farmers and landowners in these high-risk areas. When speaking with a representative of a family-owned vineyard in Napa, California, about how they were affected by the 2020 wildfires, I discovered that the owners had no choice but to forfeit a year’s vintage and associated profits due to the impacts of wildfire smoke. Some who own and operate their own farms have adopted firsthand firefighting tactics themselves because, by the time fire management officials can get to the site of ignition, it’s virtually too late, and their harvest is lost. Another farm owner in northern California shared that she had twice spotted a wildfire approaching her property by sight alone. Because she saw it early enough, she was able to take measures to protect her property–although, there are plenty of stories where it’s already too late. Collinsco Lumber, a small timber company with 100,000 acres of Ponderosa Pine in Chester, California, shared that they had lost their crop to a wildfire overnight in last summer’s Dixie Fire. Forester Corey Bingaman woke up to flames and smoke crowding the forest floor with no idea of how his property would recover. Hearing his experience highlights the immense economic risk that timber companies in particular face, as one single uncontained fire can leave behind 40 years of anticipated revenue scorched and useless due to the natural harvesting cycle of timber. These landowners face the greatest risk because they rely on their property’s environmental health for the foundation of their business and livelihood–making the wildfires’ impacts and consequences even more pressing for millions of citizens in this space nationwide.
Beyond landowners that experience these impacts most acutely, vulnerable communities can be destroyed by uncontrolled wildfires. A firefighter at the Agua Caliente Reservation in Southern California commented that wildfires pose a constant threat to cherished cultural sites on their land. Just last Fall, a series of fires in northern California near San Francisco blazed through nearly 100 homes, displacing thousands of residents.3 In a conversation with the chief fire management officials at Yosemite National Park, I learned that it's common for fires to perpetually be active at the park. In fact, within pockets of the landscape, there are barren, blackened regions devastated by massive fires. While in certain environments fires are a natural part of the ecosystem, the fire management team is trained to interfere when the fires pose a threat to people or property – and, in recent years, this is increasingly more frequent.
Yet the impacts of wildfires transcend even these environmental impacts by affecting entire communities beyond the physical site of a fire. Weeks after a fire, wildfire smoke can linger and cause permanent health damage to those exposed. Studies show that chronic exposure to wildfire smoke can cause asthma and pneumonia, increase the risk for respiratory illnesses including COVID-19, lung cancer, stroke, heart failure, and sudden death.2 In fact, a 2020 study showed that daily exposure to PM2.5 from wildfire smoke was linked to a stronger flu season in a Montana town.4 Further, these smoke impacts aren’t localized exactly to the site of a fire–in fact, the effects of smoke emissions can extend for thousands of miles across the country. Recent research reports that there were increased hospitalizations across the U.S. as a result of wildfire smoke from both Canadian & Californian fires, crossing thousands of miles to impact even cities on the East Coast such as New York City.4 Overall, these early findings warn that these impacts are widespread, uncontrollable, and detrimental to community health.
These conversations and research experiences have instilled in me a comprehensive understanding of the expansive impacts wildfires can have on individuals and communities alike. Wildfires can damage the economy, destroy livelihoods for landowners and citizens at risk, and diminish community well-being and health, clearly affecting millions of people’s daily lives.
Ultimately, this core knowledge is truly the fuel that drives me and my team as we bring our product to market. In our market and industry research, we’ve realized that the wildfire problem is only growing more urgent each year. We’ve discovered that the solution to this problem lies in a combination of proactive risk assessments and responses, and we’re now applying these insights to drive the development of our solution, which is the turnkey solution for the critical path to wildfire management. Further, we’re driven to ensure Ultimately, this core knowledge is truly the fuel that drives me and my team as we bring our product to market. In our market and industry research, we’ve realized that the wildfire problem is only growing more urgent each year. We’ve discovered that the solution to this problem lies in a combination of proactive risk assessments and responses, and we’re now applying these insights to drive the development of our solution, which is the turnkey solution for the critical path to wildfire management. Further, we’re driven to ensure that these landowners have the tools that they need to prepare for each year’s wildfire season. Every phone call with a potential customer is an opportunity to connect, build a relationship, and work with an industry expert to develop a solution to this pressing problem in the areas that need it most. We’re eager to grow so that we can collectively build a wildfire solution and move towards a future with a feasible strategy for solving the world’s fastest growing climate crisis.
1.2020 Statistics and Summary. National Interagency Coordination Center. https://www.predictiveservices.nifc.gov/intelligence/2020_statssumm/2020Stats&Summ.html. Accessed November 22, 2022.
2.Smith H. A single, devastating California fire season wiped out years of efforts to cut emissions. Los Angeles Times. https://www. latimes.com/california/story/2022-10-20/california-wildfires-offset-greenhouse-gas-reductions#:~:text=Researchers%20estimated%20that%20about%20127,in%20the%20previous%2018%20years. Published October 20, 2022. Accessed February 7, 2023.
3.Beam A. Northern California wildfire destroys 100 homes and buildings amid deep drought. PBS. https://www.pbs.org/newshour/nation/northern-california-wildfire-destroys-100-homes-and-buildings-amid-deep-drought. Published September 3, 2022. Accessed November 22, 2022.
4.Landguth EL, Holden ZA, Graham J, et al. The delayed effect of wildfire season particulate matter on subsequent influenza season in a Mountain West Region of the USA. Environment International. 2020;139:105668. doi:10.1016/j.envint.2020.105668
5. Vasilogambros M. Proliferating wildfires poison public health across the country. The Pew Charitable Trusts.https://www. pewtrusts.org/en/research-and-analysis/blogs/stateline/2022/10/17/proliferating-wildfires-poison-public-health-across-the-country. Published October 17, 2022. Accessed November 22, 2022.

Nandita Balaji is a junior from Ponte Vedra, Florida majoring in Neuroscience and Computer Science with a minor in Computational Medicine. Nandita is passionate about exploring the intersection of science, business, and technology as well as applications of these fields to high impact spaces such as healthcare and entrepreneurship.

As someone recently diagnosed with pulmonary hypertension, I have been spending countless hours researching my condition online and have been left frustrated, having found scarce information on vaccine safety in my situation. The little information accessible on the internet is difficult to understand due to medical jargon, and outdated due to the COVID-19 pandemic. Vaccine hesitancy has proven to be an obstacle in achieving herd immunity, and it is especially a problem when having a rare chronic illness. Systemic issues have played a large role in creating uncertainty surrounding vaccines, and this has caused many people in the rare chronic illness community to resist vaccines out of fear for their safety A study performed in 2019 found that only 27% of people in Italy with chronic liver disease received the influenza vaccine.1 According to Patricia Inacio, one reason why people with rare chronic illnesses are hesitant to receive the COVID-19 vaccine is that the “vaccine was approved under emergency use authorization instead of the routine process” causing hesitancy that chronic illnesses were properly accounted for during this quick process.2 Another concern raised by Inacio is that people with rare diseases want to make the decision to get vaccinated based on the “knowledge of a vaccine’s safety profile for their specific rare disease,” which was not readily available for them.2 Ana Wheelock and Jonathan Ives argue that vaccine hesitancy is caused by a lack of effort to establish trust from vaccine manufacturers and researchers.3 Alberto Giubilini, on the other hand, discusses ways to achieve herd immunity, suggesting that vaccine hesitancy does not outweigh the obligation people have to prevent “the collective harm that would result from the failure to realize herd immunity.”4 These views represent conflicting conversation on the topic of vaccine hesitancy in the chronic illness community.
Although there are clashing views on the problem of vaccine hesitancy, especially for those with rare and chronic illnesses, many Americans will agree that changes need to be made to promote vaccine uptake. Inacio explains, “People with rare disease are often at a higher risk of poorer outcomes with COVID-19, and generally advised to be vaccinated” yet rare diseases are still left unnoticed in many cases.2 Having a rare, chronic illness myself, I understand how difficult it can be to find information about a specific condition and feel confident enough to make a major medical decision. More steps need to be taken to make the rare chronic illness community more educated and involved in the vaccine development and distribution process.
In this essay I will examine how vaccine manufacturers and a lack of knowledge create uncertainty towards vaccines and how vaccine hesitancy can be reconciled to achieve herd immunity and protect the common good. Reducing vaccine hesitancy is particularly important for the chronic illness community, which is at higher risk of harm from vaccine-preventable diseases.
It is important to consider the causes of vaccine hesitancy when determining a strategy to achieve herd immunity, and a lack of knowledge is one of the biggest sources of uncertainty about vaccines. In my experience, I have been frustrated while searching for information and only finding outdated or irrelevant articles for my rare chronic illness. The lack of access to vaccine studies and other reliable sources of information is not limited to my own situation, and many people similarly struggle to find the knowledge they need to make an informed decision about their health. Many people with rare chronic illnesses are hesitant to make a decision that could further worsen their health. Additionally, with the internet being an unreliable source of information, I understand why “primary care physicians or specialists… were the major sources of ‘trusted information’ used by patients in deciding to be vaccinated”.2
"However, specialists for a rare chronic illness can be rarer and harder to find than the diseases themselves."
It took me months to get an appointment with my pulmonary hypertension specialists after several months of inconclusive testing. In addition, her office is a 2-hour drive from my home. It was also hard to find the time for an in-person conversation about getting the COVID-19 vaccine when her only appointments are
on Tuesday mornings, when I have classes and my parents must work. Inacio explains that it is necessary for public health officials to be “encouraging patient-doctor discussions about vaccinations,” but that proves to be very difficult when the only doctors who know about rare chronic illnesses are inaccessible.2
Vaccine manufacturers and researchers also play a significant role in the lack of confidence in pharmaceuticals. Wheelock and Ives say, “unfavorable results from industry-sponsored clinical trials led by academic researchers are not reported,” and this knowledge is a valid reason for any person to distrust vaccine manufacturers.3 People do not want to receive vaccines from researchers that only show biased results and not the side-effects. Inacio explains that knowing the side effects and overall safety of a vaccine in terms of a person’s rare illness is essential for the rare chronic illness community deciding whether to receive a vaccine.2 The uncertainty of receiving a newly developed vaccine and the concern raised from the lack of any published side effects add complications to the already difficult situation of having a chronic illness. People do not want negative effects to be hidden from them, especially when that negative information affects a person’s well-being. Also, side effects mentioned in the media are geared toward a healthy population that would not be significantly affected by the side effects of vaccines. This means that the already large amount of confusion towards vaccines by the general population is amplified in the rare chronic illness community. Even less information for rare diseases results in more uneasiness regarding vaccines and vaccine manufacturers. The lack of transparency from researchers makes it increasingly difficult for a person to feel confident enough in the vaccine to get vaccinated, leading to the vaccine hesitancy seen today in the chronic illness community.
It is very uncommon for rare chronic illnesses to be included in vaccine research, especially with the speed of the COVID-19 vaccine’s emergency use authorization (EUA), which is clearance given by the FDA to use the previously unapproved vaccine during a public health emergency. At the time Inacio’s article about the concern behind the COVID-19 vaccine was published, the vaccine was still new, and not many people had received the vaccine yet. Many people with chronic illnesses were hesitant to get the shot because it appeared that the Food and Drug Association (FDA) rushed through the authorization process and did not take all the necessary precautions when developing the vaccine.2 Because “EUA aims to shorten the testing and review given to a vaccine’s authorization,” the already lacking amount of research on the effects on chronic illnesses is further diminished.2 It is hard for people to accept the vaccine is safe when the data and statistics proving the vaccine is a healthy choice is unavailable. Additionally, because rare illnesses are, as the name suggests, rare, it is difficult to find people to test the vaccine on. It is hard to know how vaccines will affect specific diseases without proper testing. However, vaccine hesitancy can be addressed if pharmaceutical companies and vaccine researchers are more transparent and provide the public with the data that allowed the vaccine to be approved in the first place.
In addition to a lack of information, mistrust in pharmaceutical companies increases because companies’ financial motives seem to take precedence over the common good. The chronic illness community can be even more concerned because they are aware of problems created by pharmaceutical and insurance companies. For example, Beran et. al. explain that a vial of insulin is produced for about three dollars, but it is regularly sold for hundreds of dollars.5 For diabetics who need insulin on a daily basis, costs can quickly add up, making it infeasible to receive the necessary medications and care. Additionally, rare chronic illnesses require many treatments produced by pharmaceutical companies that can be hard to find. Receiving consistent treatments and specialty doctor appointments requires negotiating and communicating with insurance companies to convince them to pay for expensive, but necessary, medical supplies. Following continuous battles trying to pay for medications, it is hard to believe that pharmaceutical companies have people’s best interest at heart and are not just attempting to turn a profit. People who have had to deal with insurance companies find it hard to trust that the vaccines are being developed for the common good and instead believe it to be a money-making operation. I have had pharmacies try to charge me fifty times what my insurance company said I had to pay, even as I struggled to get the medication I need on a daily basis. Wheelock

and Ives explain, “the interests of industry, researchers and academic institutions have become more intertwined and, arguably, conflicting.”3 These interests of vaccine researchers and manufacturers are conflicting due to the academic nature of developing vaccines and the greedy mindset of the pharmaceutical industry. Additionally, the US Institute of Medicine’s report on conflicts of interest says, “researchers who develop clinical guidelines cover up their financial ties with industry.” It is concerning to hear that pharmaceutical companies are prioritizing money making schemes over the well-being of an entire population. Vaccine manufacturers lose people’s trust when they try to profit off of people’s chronic illnesses.
Despite the safety concerns of the rare chronic illness community, it is still necessary for these people to get vaccinated to achieve herd immunity. Giubilini argues that it is fair to make everyone get vaccinated because everyone benefits from herd immunity, and, therefore, everyone must get vaccinated for “the distribution of the burdens entailed by the collective obligation to realize herd immunity.”4 Giubilini makes the point that people should avoid “free-riding” and contribute to the health of our society.4 Because the rare and chronic illness communities benefit from herd immunity, we too have an obligation to get vaccinated, especially because we have a greater risk than the rest of the population if herd immunity is not achieved and are “generally advised to be vaccinated.”3 However, Giubilini also argues, “a successful vaccination policy is not only one that achieves herd immunity but one that achieves herd immunity fairly.”4 Moreover, it must be acknowledged that mandatory vaccinations place a greater burden on those with rare chronic illnesses because of the lack of information of the vaccine’s effects on these diseases. The uncertainty of not knowing how a vaccine will affect your illness is an additional hardship to the concerns that the healthy population has. The rare chronic illness community should be vaccinated to achieve herd immunity too, but steps must be taken to lessen some of the burden of uncertainties.
Although there are many concerns and considerations to account for, there are ways to begin reconciling the problem of vaccine hesitancy in the rare chronic illness community. Inacio presented one way to bring these problems to the attention of public health officials.2 She described that during February of 2020, the EveryLife Foundation for Rare Disease “sent a letter to the Biden Administration outlining the concerns of the rare disease community.”2 This letter included skepticism regarding the EUA and the resulting safety of vaccines. It also called for public health officials to create “clear templates… to use in outreach efforts” and provide “safe and accessible vaccination sites.”2 The templates included ways to address the concerns of the
rare illness community while also providing useful data. One benefit of this letter is that it provided the government with the exact problems they need to solve from the perspective of the rare illness community. Because rare and chronic illnesses can be difficult for the general population to understand, it is important for public health officials to receive this information in order to fully grasp the problems at hand. As Wheelock and Ives say, “understanding the problem holistically is an essential first step towards addressing it,” and the rare chronic illness community can play a large role in understanding the problem of vaccine hesitancy.3 The EveryLife Foundation for Rare Illnesses also presented a course of action that the government can take to resolve the previously mentioned problems. This specific agenda allows officials to take more efficient steps toward solving the problem of vaccine hesitancy. Although there are no current notable outcomes from this letter, by providing officials with a list of problems that need addressing, people in power have the tools to take the necessary steps to combat vaccine hesitancy.
Wheelock and Ives help explain how the actions needed to help the rare chronic illness community can also benefit the greater population due to the common problem of vaccine hesitancy. Wheelock and Ives define “vaccine confidence” as “the belief that vaccines are protective, safe and part of a trustworthy medical system.”3 Although the general population and the rare chronic illness community face different obstacles toward having “vaccine confidence,” there are some overlapping problems that cause vaccine hesitancy. Some common issues are a “lack of understanding” and a “mistrust of vaccine manufacturers and decision-makers.”3 These problems can be addressed using some of the solutions, such as outreach efforts and accessible vaccination sites, suggested by the letter from the EveryLife Foundation of Rare Illnesses. Outreach efforts can increase transparency from pharmaceutical companies, and safe vaccination sites can help everyone feel more comfortable to go outside and get a vaccine during a pandemic. One solution presented by Wheelock and Ives is “to cut ties between academia and industry.”3 The goal of this measure is to eliminate any ulterior motives that would interfere with the goal of improving the health of the population, and the financial ties mentioned earlier in this essay conflict with that objective. Cutting ties would therefore improve the trustworthiness of the vaccine developers in the public eye, including the rare chronic illness community. Although vaccine hesitancy in the rare chronic illness community is a problem, it may be seen as a less significant problem than vaccine hesitancy in the general population due to each group’s respective sizes.
"The problems of those with rare chronic illness may be overlooked because the problems of a specific community are not applicable to the problems of the greater population, but there are significant overlaps."
Steps taken to improve vaccine confidence in the chronic illness community can also benefit the whole population. Eliminating vaccine hesitancy in the rare chronic illness community can make herd immunity achievable and possibly prevent the need for a vaccine mandate if people receive vaccines out of their own will. Although people who have a rare illness are, by definition, rare, the combined number of all people with rare illnesses make up 3.5-5.9% of the world’s population.6 Even when a smaller community decides to get vaccinated, that moves the population one step closer to herd immunity. Also, if the tactics used to decrease vaccine hesitancy work on the general population, there may be enough people willing to receive the vaccine to prevent the need for a vaccine mandate for the general population based on the principle of the least restrictive alternative (PLRA). Although Giubilini disagrees with the convention, he explains that the PLRA prefers “the least restrictive of personal liberties” when choosing an equally effective solution.4 If reducing vaccine hesitancy in the rare chronic illness community is not enough to achieve herd immunity, it would at least be a part of the “policies aimed at increasing people’s confidence in vaccines, so that they would be more likely to comply with legal requirements” associated with a vaccine mandate.4 Relieving vaccine hesitancy in the rare chronic illness community will improve vaccine confidence and create an uptake
in vaccines to achieve herd immunity with or without a vaccine mandate. The same principles and practices can also be extended to the broader population to further decrease vaccine hesitancy since others are also affected by a lack of transparency and trust in pharmaceutical companies.
Vaccine hesitancy in the rare chronic illness community provides a significant challenge toward achieving herd immunity. The hesitancy is based on a lack of communication from vaccine researchers, a mistrust in the financial motives of pharmaceutical companies, and a lack of access to reliable sources of information. As someone who has a rare chronic illness, I have experienced these concerns myself but have found ways to improve vaccine confidence through communication and trust. To achieve herd immunity, the government must be open to hearing the concerns of people with rare illnesses and take actions, such as creating open dialogue, ensuring safe vaccination sites, and cutting ties with financial incentives. This will allow for a boost in vaccine confidence and trust in vaccine researchers. My hope is that these actions will increase vaccination rates in the rare chronic illness community and create a safer environment for all people. I am optimistic that more people can be protected from diseases if all people’s concerns are acknowledged.
1.Alukal JJ, Naqvi HA, Thuluvath PJ. Vaccination in Chronic Liver Disease: An Update. Journal of Clinical and Experimental Hepatology. 2022;12(3):937-947. doi:10.1016/j.jceh.2021.12.003
2.Inácio P. Quick Approval Given COVID Vaccines of Concern: Rare Disease Survey. Pulmonary Hypertension News. Published April 22, 2021. Accessed April 2022. https://pulmonaryhypertensionnews.com/2021/04/22/ quick-approval-given-covid-vaccines-raise-concerns-rare-disease-patients-say/
3.Wheelock A, Ives J. Vaccine confidence, public understanding and probity: time for a shift in focus? Journal of Medical Ethics. 2021;48(4):250-255. doi:10.1136/medethics-2020-106805
4.Giubilini A. Fairness, Compulsory Vaccination, and Conscientious Objection. The Ethics of Vaccination. Published online December 29, 2018:95-123. doi:10.1007/978-3-030-02068-2_4
5.Beran D, Gale EAM, Yudkin JS. The insulin market reaches 100. Diabetologia. Published online March 11, 2022. doi:10.1007/s00125-022-05680-y
6.Shourick J, Wack M, Jannot AS. Assessing rare diseases prevalence using literature quantification. Orphanet Journal of Rare Diseases. 2021;16(1). doi:10.1186/s13023-020-01639-7

Bea Manjon is a sophomore majoring in Molecular and Cellular Biology and Public Health Studies. In her free time, she enjoys playing tennis and traveling. She wrote this article in her Expository Writing class in the spring of 2022 to express her opinion of vaccine mandates.

Genetic material encodes an individual’s entire life story. It contains unique information about their family ties and ancestral history. It even holds information about their future health.1 With genetic material carrying such extensive personal data, there is a large potential for misuse.2, 3 Thus, important questions arise: should genetic material be considered property? If so, who owns it? I argue that individual rights and public benefits from genetic material can be balanced through dynamic informed consent and pseudo-anonymization of data.4
To understand the arguments surrounding genetic material ownership, it is essential to understand cell biology. Every living organism is made up of millions of cells that perform basic processes that sustain life. These cells can break down internalized species, aid in fighting infection, and even work in sync to regulate coordinated actions. The processes performed by these cells are directed by an organism’s particular deoxyribonucleic acid (DNA) sequence which stores genetic information.3, 5 Cells, tissue samples, blood, saliva, and hair are examples of genetic materials.6, 7 The United States’ Genetic Confidentiality and Nondiscrimination Act of 1996 defined genetic information as “derived from an individual or family member
[and] about genes, gene products, or inherited characteristics.”3 The Act also defined genetic information to include “DNA sequence information.”3
While humans share approximately 99.9% of DNA, the remaining 0.1% is unique to the individual.6, 8 Because DNA is semi-unique, it can serve as a personal identifier linking oneself to parents, relatives, and even ancestors.3, 6 Genetic testing companies like AncestryDNA use this principle to reverse-engineer family lineages (i.e., genealogy) to link together common genetic histories and store this genetic information in “biobanks.” 4, 9 Further, the Department of Justice (DOJ) uses public genealogy databases and forensic biobanks in criminal investigations.1,9 Recently, forensic genetic genealogy closed the multi-decade ‘Golden State Killer’ cases.4 Investigators cross-referenced public genealogy databases with forensic DNA samples to trace the sample’s lineage.10 This development not only demonstrates the power of genetic information as a personal identifier but also as a privacy concern. It begs a litany of questions: Was consent given to the DOJ to use millions of people’s genetic identification? Who has access to these sequences? Does genetic genealogy put your privacy at risk?3
Apart from being used to solve crime and retrace familial footsteps, DNA markers can also relay predispositions to future genetic diseases and health concerns.1,9 For example, cardiovascular disease, Huntington’s disease, and Type 2 diabetes are hereditary.1 The field of genomics and biomedical engineering explore the human genome to uncover interactions between genes and disease and use this information to develop tests and more effective therapies to develop personalized medicine.10 But where and how do researchers consensually obtain genetic material samples to study? Who owns the samples? Who controls their use?
There is much uncertainty when it comes to handling genetic information. Ultimately, misuse of personal genetic information can cause harm through breaches in individual privacy rights and discrimination.2 As the understanding of the human genome advances, it becomes increasingly likely that one’s DNA can provide more and more information.9 This personal information can “discriminate against people based on genetically predicted susceptibilities,”1 and could stigmatize racial groups or ethnic minorities.2, 10, 11 In fact, the public fears that insurance companies, employers, and even the government could treat persons differently by their demonstrated genetic fitness.1,9,10,11
"Much like the two ends of a balance, there are two poles in the discussion of material ownership."
First, there is the idea that material should be owned collectively by the commons. On the opposing end, there is the contrasting idea that materials should be owned privately by individuals. Treating genetic material as a common resource stimulates scientific discovery and engineering innovation. In turn, the public benefits. With genetic information readily available for use, there are fewer obstacles to data analysis or to innovative technology. However, if genetic material is a common resource, there is a possibility of misuse. A common resource is available to the many but owned by none (e.g., air, forests, and water). Thus, anyone can use it and spread (mis)information regarding it. This use leads to a “tragedy of the commons,” where everyone’s exploitation of the resource ultimately destroys it. For genetic material, discrimination and privacy concerns destroy the public’s faith in it.2, 11, 10 Further, if genetic information is a common resource, individual autonomy over it diminishes. Genetic information connects indigenous groups whose DNA could link to disease resistance.11 When these DNA sequences are commonly known, profitable and potentially life-saving research supersedes the autonomy rights of indigenous groups.11 This result violates respect for persons.
On the opposing side, treating genetic material like personal property safeguards privacy and
confidentiality. It protects the autonomy of individuals by putting control of and access to genetic information in their own hands. However, if genetic material is privately-owned or patent-protected, confidentiality thwarts scientific discovery and public benefit. Thus, ownership inflates prices for genetic testing and therapies, ultimately reducing public benefits.
The U.S. Judiciary historically defends the idea that individuals do not retain property rights to genetic material that have been excised or donated. The landmark 1990 court case Moore v. Regents of University of California depicted that, once excised from a patient, the patient no longer owns their genetic material. Without informing the patient or obtaining consent, researchers at the University of California developed a profitable cell line from the patient’s cells. Ultimately, the California Supreme Court ruled that patients do not have a property right to their excised bodily materials or claim to any profits obtained from their use.1, 6, 7, 8, 12
The context of this case is reminiscent of that of Henrietta Lacks, who initiated the discussion of bioethics and genetic material ownership. Lacks was a poor African American female whose cervical cancer cells were harvested without informed consent in 1951 at The Johns Hopkins Hospital. These cells were paramount to the discovery and commercialization of an immortal cell line.6 Lacks did not give informed consent for her sample’s storage or study, and her autonomy was overlooked. Her cell line led to scientific advancement and the development of numerous novel therapeutics, yet her family has received no profit share and feels exploited by researchers.
In both instances, material from medical biopsy was used to create medical advancements and generated immense profit. The patients did not receive adequate informed consent in relation to the downstream uses of their bodily materials. This idea of informed consent, therefore, is of paramount importance to uphold the principle of respect for persons.
Furthermore, this idea of ownership transference extends past excisions into donations. The 2003 landmark United States court case Greenberg v. Miami Children’s Hospital Research Institute clearly defined the scope of ownership as it relates to donated genetic material. After discovering that their genetic samples informed the creation of a diagnostic test that was being licensed, organ donors sued Miami Children’s Hospital Research Institute. The courts held that patients who voluntarily donate their tissue for research do not retain a property right.1, 5, 6, 7, 8
Finally, property transference even extends into patent law. The 2013 Association for Molecular Pathology v.Myriad Genetics case found that an individual’s DNA is not patentable unless it has been meaningfully transformed.5, 6, 13 Following Myriad’s restrictive scientific and business practices on the uses of its patented, isolated genes, plaintiffs argued that the genes were not patent-eligible. The courts found that isolated DNA segments are not patent-eligible unless they have been transformed into something other than a product of nature.5, 6, 13 In the case that it has been meaningfully transformed, say into a lab-mutated protein with desirable activity, then it is patentable.
Currently, in the United States, there is a lack of regulation of genetic material, genetic information, and individual privacy rights concerning both. Instead, U.S. legislation focuses on preventing discrimination based on genetic information.10 Of the three landmark pieces of legislation focused on protecting genetic information, only one was enacted. First, the U.S. Genetic Privacy Act of 1995 (GPA) sought to safeguard an individual’s genetic privacy rights.9 It was largely motivated by the belief that individuals should retain control over their genetic material since it is a valuable source of personal information.9 The GPA would have prohibited unauthorized collection and analysis of individually identifiable DNA samples.9 In other words, it held that if personal information had to be separated from collected samples then proper informed consent must have been explicitly given by individuals prior to collection and usage by other entities. Individuals would have the power to select who could use their information and for what purposes.9 While it was not enacted into legislation, the GPA was an important stepping stone towards protecting personal privacy and

defining the scope of genetic material ownership.
As genetic testing became increasingly widespread, the public began to fear the prospect of gene-based discrimination based on genetic fitness. In fact, “many genetic conditions and disorders are associated with particular racial and ethnic groups and gender. Because some genetic traits are most prevalent in particular groups, members of a particular group may be stigmatized or discriminated against as a result of that genetic information.”10 In 2008, the U.S. Genetic Information Nondiscrimination Act (GINA) sought to eliminate the threat of gene-based discrimination which was plaguing the country. GINA prohibited genebased discrimination with respect to health insurers and employers. It was enacted and put some degree of control back into the hands of the people so that they could safely explore “genetic testing, technologies, research, and new therapies.”10
The U.S. Genetic Information Privacy Act of 2019 (GIPA) emerged to fill in the protections that were offered by the GPA but left out in the GINA. GIPA sought to define standards and requirements for the handling of personally identifiable information by genetic testing services which were becoming increasingly prevalent.14 It regulated how genetic testing services could collect, use, and store personally identifiable genetic materials. Due to their natural complexity, it is important for the patient or donor to fully understand what their material will be used for. In this light, GIPA sought to codify the necessity for informed consent.14 Unfortunately, GIPA was not enacted into law, and the legal scope of genetic material ownership has yet to be defined.
On the contrary, existing European Union (E.U.) legislation has addressed the questions of discrimination, individual genetic material ownership, and privacy. The E.U.’s response to the rise of genetic material use was in stark contrast to the United States’. Instead of leaving the scope of individual privacy rights in limbo, the E.U. codified legal protections for individuals regarding their genetic information privacy.15 The General Data Protection Regulation of 2018 (GDPR) regulates genetic information access, collection, and storage in the E.U.15 It sought to safeguard an individual’s genetic privacy rights by defining the scope of allowable genetic material processing and movement.15 The GDPR not only expressly defined conditions of informed consent, but it also established principles guiding an individual’s autonomy over the processing and use of their information by other parties, including companies. Ultimately, the GDPR sought to balance individual rights with scientific necessity and benefit to the commonwealth.15
"The United States must take further action to balance individual rights to privacy and informed consent with overall benefit to public welfare as it relates to genetic information."
If genetic information is solely owned by the commons, there is risk that it will be used for malicious reasons or misused entirely. On the opposing side, if genetic information is solely owned by the individual, there is risk that scientific advancement will stagnate, putting patients with gene-linked diseases at risk. There must be balance between the two poles. The goal of my recommended guidelines is to ensure that individuals retain control over their genetic material while respecting their confidentiality. Additionally, I aim to ensure that researchers retain access to genetic material for use in scientific advancements for the public benefit.
The term “suppliers” is used to describe individuals who contribute their genetic material and the term “users” to describe individuals who use this supplied genetic material.
1.In the case of scientific studies involving genetic material, an independently contracted
Institutional Review Board (IRB) must approve the study and all disclosure letters prior to reaching out for donors or to patients. This pre-approval process aims to tightly control the intended uses of genetic material by having it subject to external review. External review can also work to promote non-maleficent practices in these studies. In ideal circumstances, only studies which have proven that they require access to genetic material and have prepared adequate informed consent disclosure would be permitted to move forward with requests.
2.Furthermore, in all cases, users must be required to fully disclose intended uses and commercial prospects to suppliers.7 This disclosure would constitute informed consent to the supplier, protecting their respect for persons. Often, informed consent documents are plagued by intense legal jargon, preventing the average individual from reading, or understanding the content. Therefore, users must relay this information in disclosure documents comprehensible by the average adult.
3.One-time consent is not enough to safeguard a supplier’s right to privacy since suppliers should be able to change their mind or rescind their consent at any time. Therefore, users must gain informed consent from every supplier each time they intend to use their genetic material (i.e., dynamic consent).4, 7, 8 In practice, dynamic consent means that users and suppliers maintain communication regarding the use of suppliers’ genetic material in further studies. Suppliers have the option to continue or withdraw their consent based on users’ disclosed intended uses and prospects. Through dynamic consent, suppliers directly support research benefitting the collective while maintaining autonomy over their provided information. Open communication between researchers and study participants can be beneficial for all involved parties.
4.A supplier’s genetic material must be pseudo-anonymized (i.e., encrypted) to protect their privacy. In other terms, no personally identifying information should be directly linked to a supplier’s genetic material. In this way, users cannot discriminate against the supplier based on their genetic material. Since encryption requires another party with encryption and decryption capabilities, a third-party subject to oversight must be responsible for communicating between user and supplier. A secure online portal where each entity can communicate would ease access and reduce the burden placed on users. Oversight is required to check the authority of the third party, ensuring that they act in good faith.
These four guidelines aim to protect the individual but also benefit the collective. They aim to promote non-maleficence and respect for persons in scientific practice while upholding an individual’s duty to the rights of others. Furthermore, these guidelines should be incorporated within novel legislation in the U.S. In practice, they may function like the following:
Researcher A wishes to use genetic material in their scientific study. Researcher A must approach the IRB with a proposal and disclosure letter for their study. The IRB either approves or denies the research proposal and disclosure letter, providing suggestions for improvement. Researcher A can refile the request with their incorporated changes until they obtain approval. Following approval, the researcher logs onto a third-party portal where they upload their eligibility criteria and disclosure letter and, then, request samples. The portal notifies eligible sample suppliers of a request to use their genetic material in a study. Eligible suppliers review the disclosure and can accept or deny the request. Following this, samples from approving suppliers are released to Researcher A by the third party. These samples are fully anonymized and only the third party can decrypt the identifying information. At any time for any reason, sample suppliers can withdraw their consent and, therefore, samples from Researcher A. If Researcher A would like to perform
follow-up studies not detailed in the initial disclosure, then they would repeat this process.
The European Union offers more expansive legislation regarding genetic privacy rights in comparison to the United States. The protections offered by the GINA are not comprehensive enough to secure genetic information, and there is still much work that must be done to secure genetic privacy rights.
1.Greely, Henry T. “Genomics, Ethical Issues In.” International Encyclopedia of the Social & Behavioral Sciences, vol. Second ed., 2015, pp. 32–41, https://doi.org/10.1016/b978-0-08-097086-8.82011-5. Elsevier.
2.Robinson, Jennifer. “Ethics and Genetic Privacy.” Online Journal of Health Ethics, vol. 1, no. 1, 2004, p. 1, https://doi.org/10.18785/ ojhe.0101.01.
3. Text - S.1898 - 104th Congress (1995-1996): Genetic Confidentiality and Nondiscrimination Act of 1996. Congress.gov, Library of Congress, 24 June 1996, https://www.congress.gov/bill/104th-congress/senate-bill/1898/text
4.Green, Melissa. Big Data. Edited by Benoit Leclerc and Jesse Cale, Routledge, An Imprint Of The Taylor & Francis Group, 2020, pp. 104–16.
5.Association for Molecular Pathology et al. v. Myriad Genetics Inc., et al., 569 U.S. 576, 2013
6.Roberts, Jessica L. Progressive Genetic Ownership, 93 Notre Dame L. Rev. 1105, 2018.
7.Petrini C. Ethical and legal considerations regarding the ownership and commercial use of human biological materials and their derivatives. J Blood Med., no. 3, 2012:87-96
8.Monica J Allen, Michelle LE Powers, K Scott Gronowski, Ann M Gronowski, Human Tissue Ownership and Use in Research: What Laboratorians and Researchers Should Know, Clinical Chemistry, Volume 56, Issue 11, 1 November 2010, Pages 1675–1682, https:// doi.org/10.1373/clinchem.2010.150672
9.Annas, G. J., Glantz, L. H., and Roche, P. A. The Genetic Privacy Act and commentary. United States: N. p., 1995. Web. doi:10.2172/395609.
10 Text - H.R.493 - 110th Congress (2007-2008): Genetic Information Nondiscrimination Act of 2008. Congress.gov, Library of Congress, 21 May 2008, https://www.congress.gov/bill/110th-congress/house-bill/493/text.
11.Spinello, Richard A. “Property rights in genetic information.” Ethics and information technology , vol. 6, no. 1, 2004: 29-42. doi:10.1023/b:etin.0000036157.14807.b0
12.National Society of Professional Engineers. NSPE Ethics Reference Guide. 2022, www.nspe.org/sites/default/files/resources/ pdfs/Ethics/EthicsReferenceGuide.pdf.
13.Kesselheim, Aaron S et al. “Gene patenting--the Supreme Court finally speaks.” The New England journal of medicine, vol. 369, no. 9, 2013: 869-75. doi:10.1056/NEJMhle1308199
14. Text - H.R.2155 - 116th Congress (2019-2020): Genetic Information Privacy Act of 2019. Congress.gov, Library of Congress, 10 April 2019, https://www.congress.gov/bill/116th-congress/house-bill/2155/text.
15.European Parliament and Council. General Data Protection Regulation (GDPR) (EU) 2016/679. 27 Apr. 2016, eur-lex.europa.eu/ legal-content/EN/TXT/?uri=CELEX%3A02016R0679 20160504&qid=1532348683434.

Devan is a fourth-year BS/MSE student studying Chemical & Biomolecular Engineering. Following graduation, he hopes to leverage his engineering skills to help lead the development of affordable and accessible nextgeneration healthcare technologies. In his free time, Devan is usually watching F1, traveling, or learning how to prepare new cuisines.


In the spring of 2022, I was quite excited to finally learn about outbreak investigations in my “Fun Epi” (Fundamentals of Epidemiology”) class. I was not the biggest fan of calculating odds ratios or memorizing study design types, but participating in on-the-ground work to trace an outbreak and implement prevention measures sounded thrilling. After talking to one of my professors and an alum of the class, I cold-called several Maryland hospital infection prevention departments and was lucky enough to find one willing to take on an intern.
At the hospital that summer, I was assigned to investigate and attempt to improve the use of tap water by healthcare workers (HCWs) in the hospital. This hospital’s neonatal intensive care unit (NICU) was experiencing an ongoing outbreak of Pseudomonas aeruginosa (PA) linked to the exposure of immunocompromised infants to tap water containing PA. This bacterium is classified as a serious threat by the CDC, causing around 51,000 hospital-acquired infections and approximately 500 deaths per year in the U.S. alone.1 At the hospital where I interned, PA caused dozens of cases of pneumonia and the deaths of 7 infants from February 2021 to June 2022. Motivated by the outbreak, the Infection Prevention Department tasked me with uncovering how the hospital’s most vulnerable patients were exposed to bacteria-containing tap water and creating a trial of an educational intervention to reduce tap water exposure by modifying HCW behavior.
In sinks, the growth of biofilms— bacterial colonies surrounded by slime that are extremely resistant to chemical and physical removal— are known to be the main cause of hospital-acquired bacterial infections such as PA. This bacterium is only one of the many infections that patients can acquire due to inadequate practices and environments related to tap water in hospitals. The process of bacterial spread from plumbing to patients begins with the bacteria entering the plumbing via infected patients. These bacteria settle in the sink’s p-trap, a small water reservoir in the pipe about 7 inches below the sink drain, where they can survive for up to two weeks without nutrients. When nutrients are poured down the drain in the form of bodily fluids, IV fluids, or patient beverages, the bacteria form a biofilm that rapidly grows upwards, reaching the drain of an average sink in about one week. Upon reaching the drain, the biofilm will continue to grow and are eventually carried to other spaces when water droplets splash from the sink basin onto adjacent countertops or the hands of HCWs using the sink.2
Once bacteria are dispersed in water droplets, they can be transferred to patients through a number of routes. First, any items stored on counters within 12 inches of sink basins can be directly impacted by these droplets and contaminated with bacteria, which can then be transferred onto HCWs’ hands or directly to patients. Bacteria that is dispersed onto counters can be transferred to HCWs’ hands through contact with items such as soap pumps and nutritional drink bottles. Finally, bacteria can be transferred from HCWs’ hands to patients if proper hand-washing and gloving procedures are not followed, or if contact with contaminated water or items occurs after hand hygiene is performed.3 The spread of bacteria from p-traps to patients can be mitigated in a number of ways, from those as drastic as eliminating the use of tap water in patient rooms to those as simple as the frequent disinfection of surfaces adjacent to sinks.4, 5
“Aside from their advice, my only resources were my laptop, a printer, and Amber’s clipboard.”
Investigating these mitigation strategies was challenging, given the constraints of my internship. I had no prior education in infection prevention and received minimal training upon my arrival. Infection prevention staff members were also not paid extra to work with me, nor was special time allotted in their busy schedules to assist me. I was only able to complete this project because the staff, and especially my mentor, Amber, were very generous with their time and excited to pass their skills on to me. Aside from their advice, my only resources were my laptop, a printer, and Amber’s clipboard. In addition to these challenges, I only had around two months to complete this project. Due to time and resource constraints, my investigation focused
on three ways that HCWs can decrease the transmission of bacteria from sinks to patients: storing items away from sinks, preparing sterile supplies away from sinks, and disposing of patient beverages in proper receptacles outside of patient care areas.
I focused on four units in the hospital: the NICU, bone marrow transplant (BMT) unit, medical intensive care unit (MICU), and one of the hospital’s acute cancer care (ACC) units. I surveyed each unit twice before my intervention and twice afterwards. Based on a literature review, I designed a custom audit form to collect survey data, with sinks marked as “compliant” or “non-compliant” for the storage of items near them. Following data collection, I entered my gathered quantitative data into spreadsheets organized by sink location, date, and unit.
During the pre-intervention surveys, I collected qualitative data via observations and during brief, informal staff interviews regarding practices for the preparation of sterile supplies and the disposal of patient nutrient liquids. I did not repeat these interviews during the post-intervention period. This is because over the course of one month, the physical characteristics of the environment that made behavior change related to these practices more difficult were unlikely to have changed. In one of the pre-intervention interviews, a MICU staff member reported an overall lack of counter space in patient rooms on the unit, making it necessary to use sink-adjacent counters to store and prepare sterile supplies. The charge nurse in the ACC reported similar concerns. When prompted, another ACC staff member reported dumping patient bathwater (considered to be a liquid that promotes bacterial growth) down shower drains. Although this is preferable to dumping it down patient care sinks, it is not as ideal as disposing it down a drain in the unit’s dirty equipment room. In the BMT, a staff member reported that the current practice for disposing of leftover patient beverages was to dump them down the nearest sink, often in the patient’s room, which provides sink bacteria with a lot of

nutrients. Not all of my observations were negative however: in the NICU, a staff member was observed using the correct technique to prepare sterile supplies on a table draped in a sterile paper covering. This table had been wheeled in from outside the room to prepare these supplies in order to avoid using the contamination-prone sink-adjacent counter for this purpose.
Based on data from the pre-intervention surveys, one-page information sheets were designed in collaboration with my internship mentor, Amber. I created an initial draft based on the biggest issues that I had identified in my pre-intervention surveys. I recommended that HCWs store items and prepare sterile supplies away from sinks and dispose of liquids in drains other than patient care sinks. However, I was not familiar with the best way to design information sheets for HCWs. Amber edited and reorganized some of the content and made sure that the graphic design aligned with the hospital’s standard layout and color scheme. We wanted to communicate the scientific rationale for each of our behavioral change suggestions, but we also knew that the busy HCWs were likely to quickly skim these sheets and not have time to absorb too much text. When the sheets were completed, they were displayed on staff bulletin boards in the four target units.
“I predicted, or at least hoped, that the distribution of this information would lead to a decrease in non-compliance,”
especially regarding the storage of items near sinks, since that measure was the focus of my qualitative data collection. However, I knew there was certainly a possibility that my intervention would have no impact due to the scarce time and energy of HCWs, which they might not spend on reading my information sheet.
After repeating my qualitative data collection post-intervention, I calculated percent compliance for each unit for both the pre- and post-intervention periods, with the results of the two surveys in each period summed together. After the intervention, the percentage of sinks with items stored within 12 inches of the sink basin increased by 3.8% in the MICU, 23.2% in the ACC, and 20% in the BMT. There was a decrease of 5% in the NICU. (See Figure 1)
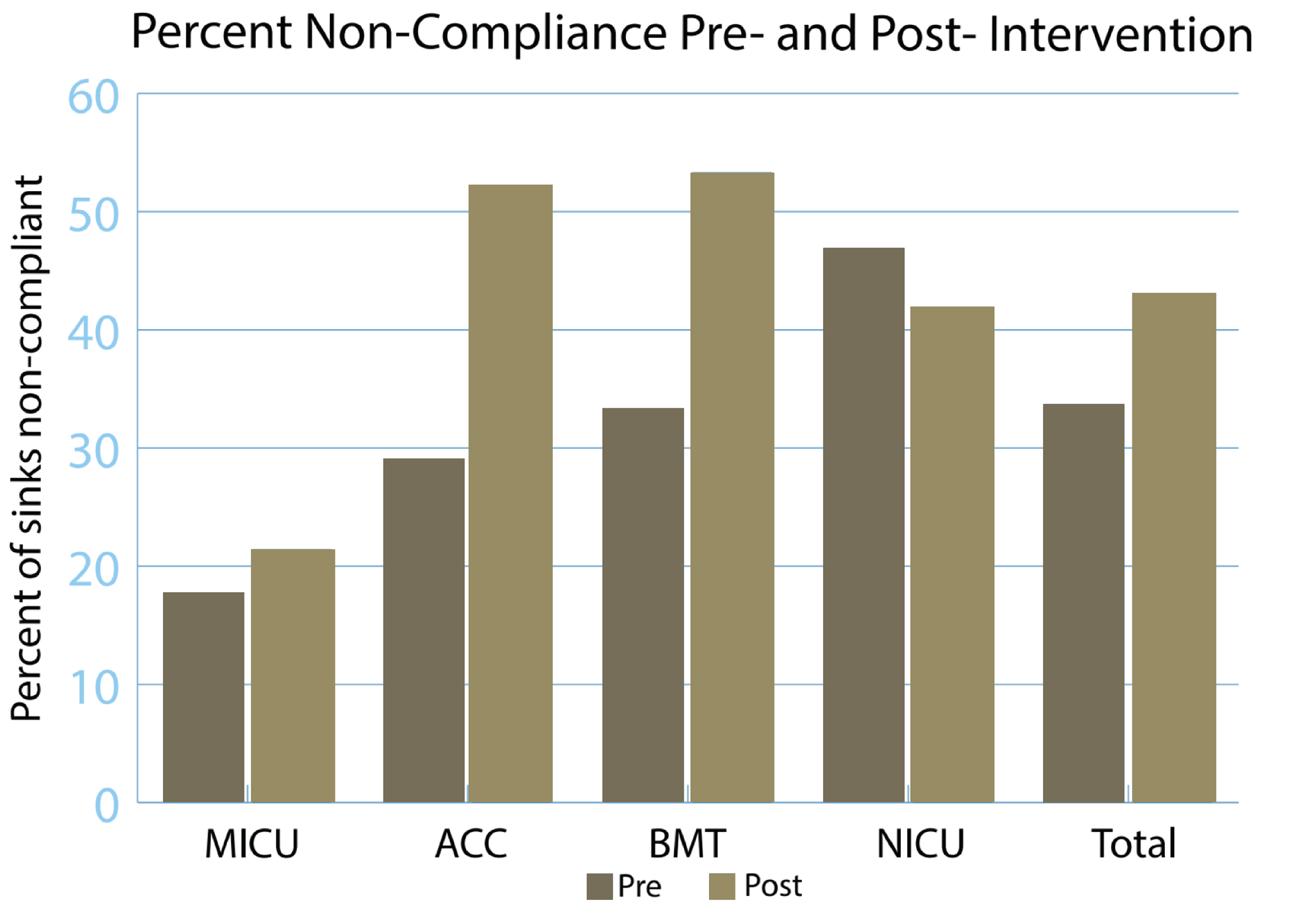
The data demonstrate that the distribution of the information sheet was not an effective intervention for altering the behavior of HCWs regarding the storage of items near sink basins. I was disappointed that the intervention did not work as intended and surprised that noncompliance actually increased post-intervention. This apparent increase may be due to my inexperience in the field of infection prevention, which could have led to some inaccuracies in data collection during the first two surveys, which I conducted pre-intervention. This may have caused me to observe a greater percentage of non-compliant sinks post-intervention, which could explain why there appeared to be increased noncompliance after the intervention on three units.
There are two possible reasons why my intervention did not have a positive impact. First, it is possible that the sheet never reached the HCWs because we did not confirm whether or not the sheet was presented at weekly meetings or displayed in staff areas. Second, even if the sheet did reach HCWs, it is possible that a brief presentation of information in this manner is not sufficient to effect unit-wide behavior change. Prior to my internship, I assumed that HCWs would be able to take careful notice of all information and guidelines that they are given. However, the results of my experiment demonstrate that increasing the safety of the hospital environment is not as simple as distributing information to HCWs. These staff, especially non-physicians such as nurses, have many competing priorities, including responding to their patients’ needs, communicating with patients’ families, fulfilling the requests of supervisors, and taking measures to prevent hospital-acquired infections. They are presented with copious amounts of information every week, including from different members of the Infection Prevention Department, about how to best care for patients. It is probable that HCWs may not have the mental and/or emotional space to be attentive to an intervention such as a one-page information handout. This sheet may seem even more inconsequential if waterborne bacterial infections are not currently a problem on an HCW’s unit. Based on the barriers that my information sheet likely encountered in being absorbed by HCWs, I learned that future interventions need to arrive in the context of pressing concerns (i.e. an outbreak of waterborne infections) and be reinforced by measures such as hospital-wide recognition of units with exemplary compliance rates.
A larger issue that I discovered over the course of my surveys was that staff are not able to adequately care for their patients under their current occupational conditions, even in a well-renowned hospital. One possible solution suggested by an HCW during an informal interview was to hire more nursing and technical staff and retain them on the same units for longer periods. This would decrease the burden placed on each HCW and ensure that everyone is trained on the particularities of their unit, increasing the likelihood that they could comply with the best tap water use procedures. The HCW suggested that each unit should also have at least one environmental services (EVS) staff member who cleans and maintains that same unit every day. Currently, EVS staff are often rotated to different units every day or every few days, so it is not possible for them to be sufficiently trained on the cleaning practices specific to each unit, such as higher sanitation standards on units with immunocompromised patients.
In addition to overwhelming amounts of information, competing priorities, and staffing shortages, HCWs also face the physical barrier of a lack of counter space, which makes it more difficult for them to avoid preparing or storing items on sink-adjacent counters. They must often acquire a rolling table from outside of a patient room for this purpose. Increased availability and convenience of these tables would enable HCWs to engage in improved patient care practices in the short term. Taking the need for non-sink-adjacent counter space into account during future hospital renovation or construction projects can help alleviate this issue in the long term. Existing hospitals are often not designed to facilitate the delivery of care according to modern standards. It is imperative that future designs carefully account for the day-to-day needs of HCWs, ideally conducting surveys similar to my own, to help prevent tragedies like the PA outbreak in the NICU at my hospital.
Overall, during this experiment, I learned that pathogens are not the only challenge that HCWs and infection preventionists face; they must also confront the organizational and physical barriers that make it more challenging to deliver the best possible patient care. Changes in individual HCWs’ behaviors can help prevent the spread of pathogens, but significant, sustained decreases in the rate of hospital-acquired infections requires systematic reforms in the functioning and priorities of healthcare institutions. Though improvements such as mass renovations and more numerous, well-paid HCWs are often regarded as prohibitively expensive and difficult, the spread of waterborne pathogens in hospitals is already dumping time, money, and lives down the drain, just as bacteria grows up it. Systemic changes are vital to the health of vulnerable hospital patients and could eventually save thousands of lives and millions of dollars every year.
1.Qureshi S. Pseudomonas aeruginosa Infections. Last updated March 3, 2020. Accessed Dec 3, 2022. https://emedicine.medscape.com/article/226748-overview#a7.
2.Kotay S, Chai W, Guilford W, et al. Spread from the sink to the patient: in situ study using green fluorescent protein (GFP)-expressing Escherichia coli to model bacterial dispersion from hand-washing sink-trap reservoirs. Appl Environ Microbiol. 2017;83(8):e03327-16. doi: 10.1128/AEM.03327-16.
3.Reduce Risk From Water. CDC.gov. Last reviewed Sept 11, 2019. Accessed July 6, 2022. https://www.cdc.gov/hai/prevent/environment/water.html.
4.Catho G, Martischang R, Boroli F, et al. Outbreak of Pseudomonas aeruginosa producing VIM carbapenemase in an intensive care unit and its termination by implementation of waterless patient care. Crit Care. 2021;25(1):301. doi: 10.1186/s13054-021-03726-y.
5.Kizny Gordon AE, Mathers AJ, Cheong EYL, et al. The hospital water environment as a reservoir for Carbapenem-resistant organisms causing hospital-acquired infections—a systematic review of the literature. Clin Infect Dis. 2017;64(10):1435-1444. doi: https://doi.org/10.1093/cid/cix132.

Eirnin Mahoney is a junior double-majoring in Public Health Studies and Sociology. When they are not reading about historical plagues, you can usually find them working with the Barnstormers theater group or snuggling with their cat, Briggs.
Ask anyone between the ages of 12 and 25, and they will be able to share a story about the mental health struggles of themselves and/or a close friend or family member. It is no secret that adolescent and young adult (AYA) mental health is a major public health issue, but its severity is not widely understood. According to the American Psychological Association, 91% of Gen Z (individuals born between 1996 and 2012) adults have experienced a physical or emotional symptom stemming from stress, but only 50% feel that they can adequately manage their stress.1 Gen Z is also far more likely to report fair or poor mental health compared to previous generations.1 These statistics, which signal a crisis, are particularly concerning since Gen Z is also more likely to seek out professional mental healthcare compared to older generations.
Despite proactively seeking mental health treatment,
“Gen Z’s aforementioned struggles continue—struggles which many experts have attributed to elevated levels of societal stressors in recent decades.”
Many members of Gen Z grew up in the shadow of the September 11, 2001 terrorist attack, experienced the Great Recession during their early childhood, and accepted school shooting drills as a part of life. In addition, the 2016 and 2020 elections were the first major elections that many Gen Z individuals could comprehend or play an active civic role. Their only concept of political discourse is a highly unusual and volatile one, marked by inflammatory debates about the economy, immigration, reproductive and social rights, and a rapidly growing climate crisis. All of these factors were already at play when the World Health Organization
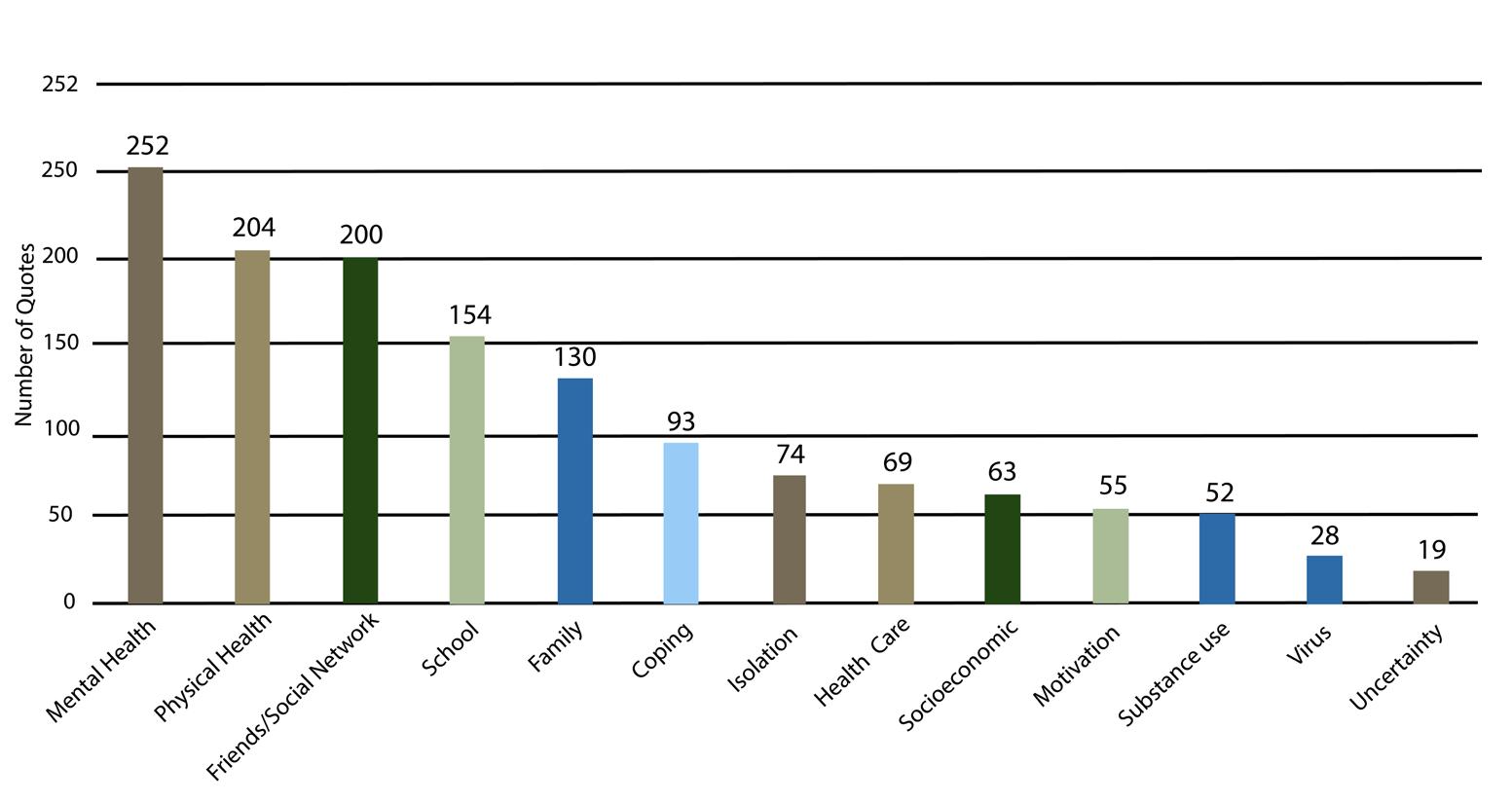

declared the novel coronavirus, SARS-CoV-2, a pandemic. 2 After being sent home during my freshman year of college in March 2020, I—like my Gen Z peers—watched as so many of us struggled due to the isolation of the pandemic. In light of these struggles, I was very excited when I was given the opportunity to work as a research assistant on a new study of adolescent mental health and substance use during the COVID-19 pandemic. The project was a collaboration between the Johns Hopkins Bloomberg School of Public Health (JHSPH) in Baltimore, MD, and the Johns Hopkins All Children’s Hospital (JHACH) in St. Petersburg, FL. The research consisted of 2 main components: a qualitative study focused on adolescents who were already struggling with their mental health before the pandemic and a quantitative study focused on substance use and mental health related visits to the emergency department (ED) during the pandemic.
In our study, we hoped to gain a better understanding of the underlying cause of severe mental health decline in adolescents during the pandemic. After interviewing 20 AYA patients at JHACH, our team developed a coding system to summarize major topics discussed by patients when discussing their experiences during the pandemic (Figure 1). Major themes included declining mental health, a loss of motivation, changes to social relationships, the negative use of social media, and both positive coping mechanisms, such as drawing, and maladaptive coping mechanisms, such as substance use. Root causes of mental health decline included social isolation from online school, family conflict, socioeconomic challenges, and difficulties associated with accessing mental healthcare services virtually. After the onset of the pandemic, patients in the ED were 45% more likely to be diagnosed with depression, 56% more likely to be diagnosed with anxiety, and 25% more likely to be experiencing a drug overdose.
When I first reviewed the data from our study, I was shocked but not surprised. While it was sobering to see the impact of our generation’s current mental health crisis enumerated on paper, this did not feel like new information to me. Whether while on social media or while interacting with my peers, I could see this rise in
mental health issues happening in real time around me. Despite numerous academic articles and popular news stories popping up about this crucial topic, I have yet to see a radical change in the quality or quantity of mental health resources for the AYA population.
While our generation is known for its activism around major societal issues such as immigration policy and gun violence, we still struggle to advocate for our personal needs. I was struck by patients’ sense of helplessness when listening to their interviews, as evidenced by the following quotes, among others:
“My mood dropped severely while COVID and the quarantine and the pandemic were at its highest.”
I became super isolated, depressed, and anxious all the time. Uh, so my mood changed drastically. Everything felt like a big deal. I always felt like the world was gonna end and my life was just overtaken by mental illness.” (17-year-old female with anorexia nervosa, binge/purge type, major depression, and anxiety) “You end up wearing the same clothes over and over again. Yeah, eating in your room, you’re watching TV in your room, and you’re working in your room, you’re sleeping in your room. You’re doing everything in your room and then all the sudden your room’s a total mess. You smell terrible. You’re exhausted, you’re not sleeping enough. And you’re pretty hungry too, because you’re probably not eating enough. And you’re just stuck there. You’re like, whoa, so is this normal now?” (16-year-old male with anxiety and depression)
I believe that part of this feeling of helplessness stems from the fact that academic, medical, and public health spaces are largely inaccessible. The processes for developing clinical guidelines for mental health treatment are not widely known. Therefore, it is essential that the public health community actively seeks input from AYA individuals who have struggled with their mental health, as well as the teachers, clinicians, and caregivers who provide day-to-day support for them. These individuals are far more equipped to help than researchers who have not spent time with the impacted population. The medical community has a duty to seek out and actively involve individuals with lived experience to design and implement effective solutions for mental illness. Although this principle is slowly but surely being adopted for adult subjects, adolescents deserve the same respect and consideration.

For better and for worse, Gen Z is very different from previous generations. Well established resources and practices are simply not working as effectively as they have in the past for today’s adolescents. We must focus on involving adolescents and young adults going forward if we want to solve this major public health issue. In the meantime, teachers, parents, and clinicians need to closely watch for signs of substance use or behaviors and signs pointing to negative mental health to prevent more young people from being impacted by the mental health crisis.
Although this crisis is far from being solved, I am still incredibly hopeful that it will be. Throughout my time working on this study, I have had the opportunity to present our research findings to teachers and school administrators, counselors, and accomplished physicians and psychologists. I am continually encouraged by their attentiveness and eagerness to further explore AYA mental health. While far from perfect, there are many intelligent and influential experts who want to help young people, and if all the groups involved work together, I truly believe that we can crack the code to help young people achieve healthy, happy lives.
1.Bethune S. Gen Z more likely to report mental health concerns. Monitor on Psychology. 2019;50(1):10. https://www.apa.org/ monitor/2019/01/gen-z.
2. World Health Organization. WHO Director-General’s opening remarks at the media briefing on COVID-19. 2019.

Cate is a senior Public Health Studies major. The public health issues which most interest her include mental and maternal health, and she hopes to pursue a career in medicine and health policy after graduation. In her free time, you can find her baking, playing Animal Crossing, or listening to true crime podcasts.

In “Theorizing (Vaccine) Refusal: Through the Looking Glass”, anthropologist Elisa Sobo grapples with how to theorize vaccine refusal through the lens of social behavior. Her definition of refusal deviates from the established view, which defines refusal as synonymous with resistance and “active opposition” (342). Sobo highlights that this established view oversimplifies the act of refusal by categorizing individuals who refuse an action as outsiders rather than understanding the social dynamics that influence their decision-making. For example, individuals feel the pressures of conformity in their own social circles even for actions that appear contrary to those of mainstream society. To address the evident flaw of equating refusal to opposition, Sobo offers a thesis that portrays refusal as a “highly social act that vitalizes community ties” (345). She largely focuses on how “opting-out” of a certain action could be understood as individuals “opting-in” to another group’s values (348) and supports her argument by analyzing two case studies: a school with a predominantly unvaccinated population and a community with individuals who felt obliged to vaccinate without understanding the mechanisms of vaccines. In both these cases, Sobo depicts refusal in the context of social pressure to underline the basis of group behavior: individuals are compelled to feel a sense of belonging by basing their decisions on their broader social circles. By framing refusal as an element of conformity, Sobo encourages readers to appreciate the “underexamined, unearthed field of cultural activity”
(348)rather than shaming an individual for refusing vaccination.
Sobo is correct to draw our attention to the fact that social interactions within groups play a role in impacting one’s decision. Throughout the paper, Sobo strongly correlates group behavior with refusal as an act of conformity (347). However, this argument assumes that individuals belong to one sole community that heavily influences their behavior, or that everyone in their social circles share similar viewpoints. If refusing is simply a matter of social belonging, then
“how
As Sobo states herself, opting-in is a means of “proclaiming that ‘I belong’ and ‘I share your values’” (348), highlighting that an individual will first need to evaluate their own beliefs to determine if they even blend into a community’s cultural norm. By examining the multitude of social factors at play, we can better determine how individuals navigate valued decision-making and why the power of the group influences their behavior.
To understand the rationale of non-vaccinators that Sobo proposes, we must first explore her unique depiction of refusal. Throughout the paper, Sobo illustrates the concept of refusal as a crucial component of group behavior through case studies at the school and community levels. First, Sobo examines a study school with a rather high Personal Belief Exemption (PBE) rate at 51%, which increased to 71.5% after ten years (345-6). Sobo describes how parents felt the school fostered an environment that promoted counter-cultural health practices, so vaccine refusal “intensified or even cultivated from scratch after joining” (345). Although this particular school community could have attracted individuals skeptical of vaccines, the study suggests that the environment served as an external factor in influencing individuals’ decisions. Further, vaccinated families remained quiet due to “fear of social consequences'' (346) as they became the minority group. Put in Sobo’s words, “opting out of vaccination was an act of opting in” (346), making her arrive at the conclusion that more individuals chose to refuse vaccinating their children for the sake of conformity in the school community.
Sobo also discusses the other side of the spectrum, studying a community with predominantly vaccinated individuals to determine if similar social pressures existed. In this case study, Sobo determined a comparable pattern of social factors affecting decisions, as individuals accepted vaccines “because of custom or an everyone-does-it here point of view” even without understanding vaccine mechanisms or herd immunity (346). Sobo asserts that for both refusal and acceptance, individuals base their decisions on the practices of the overall community in order to belong, as “refusing to be separated from one’s in-group constitutes a form of insistence, not resistance” (347). From the perspective of an individual, to not follow a similar ideology as a larger group may come across as refusing membership or belonging to a community. Sobo’s examples demonstrate that these social pressures in a community may outweigh an individual’s personal values that factor into decision-making, even at the cost of deviating from the mainstream norm.
Nevertheless, it is important to note here that individuals belong to multiple social circles and are realistically not bounded by one community. These groups range from family and friends to religious communities, the workplace, and simply the physical region. If these groups embody different values, which group takes precedence in influencing an individual’s behavior? Further, which of these groups would an individual feel most compelled to conform with their actions? Sobo’s argument assumes that individuals face pressure from a singular community due to a desired feeling of “association and becoming, not disaffiliating and being sidelined” (347). The social pressure to conform would also only hold in situations where there is already a high percentage of individuals within a particular group that act in the same manner. Yet, given the sheer
diversity of communities both internally and throughout society undermines the idea of uniformity in decision-making within a community.
Sobo might respond with her overarching idea that “selection precedes rejection” (348), suggesting that individuals would need to select a particular community that they wish to belong to and act accordingly. Considering the first case study on the school community with a high PBE rate, parents who sent their children to the school chose to join that community. Rejecting the vaccine allowed parents to align their actions with the values of the school and to “proclaim one’s affiliation with significant others from beyond the mainstream” (348).
"However, Sobo’s conclusion fails to address the proportion of individuals within the school community who still chose to vaccinate."
Even after ten years, when more individuals decided to not vaccinate their children, nearly 30% still received vaccinations in a school that itself seemed skeptical about mainstream approaches to health. This observation raises the following question: did the parents who vaccinated their children feel the need to conform to the school community? Even though they may have remained quiet about their vaccination status within the community, the environment did not completely steer them away from the vaccines. Thus, pressure from a group is not always the defining factor in making decisions; rather, part of the process entails individuals evaluating their beliefs and to what extent conformity would shake their values.
Nonetheless, Sobo’s perspective on the link between group behavior and vaccine refusal still has merit, as it ties into a central concept in sociology that states the fundamental unit of human behavior is the group. Individuals usually become affiliated with groups through two mechanisms: ascribed, which is based on external forces or judgment by others, and achieved, which is based on an individual’s own experiences, capabilities, or wishes. For ascribed belonging, individuals may not have had the choice to freely select groups or have already been associated automatically. This situation would result in individuals ‘belonging’ to

communities even if their personal values differ, so pressure from the group to conform removes the selection process for individuals altogether. For the case of individuals controlling achieved affiliation, they could have already chosen to refuse vaccination and then select to associate with a community that shares their practices.
It follows that selection does not necessarily precede rejection but rather occurs simultaneously. First, individuals possess their own set of values, and the lack of uniformity within communities indicates that conformity does not force individuals into actions. Sobo compares vaccine refusal to “getting a gang tattoo, slipping on a wedding ring, or binge-watching a popular streamed TV show” (348), hinting that individuals voluntarily commit to groups if they have the choice. As individuals belong to multiple communities, they must understand their own beliefs to gauge if they could fit in when selecting a particular group. In Sobo’s analogy, an individual would have some desire to watch the TV show or get the tattoo as they invest their time and money into those actions. In the case of vaccines, an individual who strongly agrees with vaccination would still vaccinate even in a predominantly unvaccinated community (as seen in the school case study). This example also holds vice versa; non-vaccinated individuals exist in society even though the vast majority of adults in the United States are vaccinated. Sobo herself also notes that individuals can refuse vaccinations for other personal reasons, from religious beliefs to adverse side-effects (344), and this behavior is usually unrelated to group influence. In essence, valued decision-making involves an amalgam of external factors from groups and one’s core beliefs.
Altogether, Sobo’s goal to better understand the motive of non-vaccinators has unearthed a key factor in decision-making, where individuals who refuse need not necessarily act solely on personal beliefs but are rather influenced significantly by the surrounding community. Nonetheless, to categorize refusal as an act of conformity altogether removes the complexities of personalized decision-making that still affect individual behavior. Instead of creating a linear model where selection precedes rejection, viewing both elements of refusal simultaneously places greater emphasis on individual values within a group setting. Ultimately, individuals form groups, so expanding our understanding of the multitude of factors in decision-making will allow us to understand diversity within thought when individuals refuse vaccination.
1.Sobo, Elisa J. “Theorizing (Vaccine) Refusal: Through the Looking Glass.” Cultural Anthropology, vol. 31, no. 3, 2016, pp. 342–350., https://doi.org/10.14506/ca31.3.04.

Neha is from Bethlehem, Pennsylvania and is the Editorial Editor of Epidemic Proportions. Neha is passionate about adolescent health advocacy and communication, and plans to pursue a career in medicine and public health research after graduation. She is a research assistant at the Behavioral Pharmacology Research Unit and at Johns Hopkins Pulmonary and Critical Care Medicine Laboratory, both located at the Johns Hopkins Bayview Medical Center.

Devan Patel
Editor-in-Chief.


Swati Kumar
Editor-in-Chief.

 Lola Godoy
Layout Editor.
Cate Jackson Treasurer.
Ian Chiu
Research Editor.
Neha Skandan Editorial Editor.
Jasmine Wu Features Editor.
Samhi Boppana Policy Editor.
Lola Godoy
Layout Editor.
Cate Jackson Treasurer.
Ian Chiu
Research Editor.
Neha Skandan Editorial Editor.
Jasmine Wu Features Editor.
Samhi Boppana Policy Editor.






 Louie Martinez Layout Staff.
Carlos Haring Layout Staff.
Rohan Ganesh Policy Staff.
Habin Hwang Research Staff.
Timothy Huang Feature Staff.
Christine Kim Research Staff.
Wilson Huang Research Staff.
Louie Martinez Layout Staff.
Carlos Haring Layout Staff.
Rohan Ganesh Policy Staff.
Habin Hwang Research Staff.
Timothy Huang Feature Staff.
Christine Kim Research Staff.
Wilson Huang Research Staff.






 Wassim Bouhsane Editorial Staff.
Tanisha Luthria Feature Staff.
Shaan Shabbir Policy Staff.
Martine Bigos Editorial Staff.
Jaswanth Vandrasi Editorial Staff.
Enoch Toh Feature Staff.
Mikaeel Babar Policy Staff.
Wassim Bouhsane Editorial Staff.
Tanisha Luthria Feature Staff.
Shaan Shabbir Policy Staff.
Martine Bigos Editorial Staff.
Jaswanth Vandrasi Editorial Staff.
Enoch Toh Feature Staff.
Mikaeel Babar Policy Staff.

The staff of Epidemic Proportions gives thanks to the Public Health Studies Program, the Krieger School of Arts and Sciences, and the Johns Hopkins Bloomberg School of Public Health for making this journal possible. This years edition would also not have been possible without all of the authors that worked hard to write pieces that embody the spirit of public health. We give thanks to Mason Cole for many of the wonderful photos used in this year's edition. Additionally, we would like to thank Carlos Haring for designing this year's cover and the Editors-In-Cheif for the 2023-2024 academic year, Neha Skandan and Wassim Bouhsane, for helping finalized this year's journal.
