

Table of Contents
1 Letter from the Editors-in-Chief
Neha Skandan and Wassim Bouhsane
2 Letter from Vice Dean Joshua M. Sharfstein to the Editors and Readers of Epidemic Proportions
Joshua M Sharfstein, M.D.
3 Letter from Dean Christopher S. Celenza, for Epidemic Proportions: Celebrating 50 Years of Public Health Studies
Christopher S. Celenza, Ph.D.
4 A Note on the Cover
Rose Chen
Features
8 Addressing Social Needs in Gynecology Oncology: Insights from a Hopkins Community Connections Advocate
Aminata Sinyan
10 Grace House - My Experience Witnessing Recovery and Resilience Within New Orleans
Isabelle Jouve
11 Community Close to Home: My Summer at Baltimore Harm Reduction Coalition (BHRC)
Atri Surapaneni
12 An “Eye” Opening Experience
Tabatha Alegria
14 Hopkins Past the 21218: Baltimore, DC, and Beyond
Habin Hwang, Features Team
15 Why I (and Many Others) Chose to Double Major
Vivan Guo, Features Team
16 Looking Back, Looking Forward - the Past 50 Years of Undergraduate Public Health Education
Habin Hwang, Features Team Editorials
20 The Gun Violence Epidemic: Why This Issue Is More Severe Than We Realize
Samuel Yeboah-Manson
22 Revolutionizing Healthcare: A Proactive and Patient-Centric Approach to Preventable Chronic Conditions
Jayvik Joshi
24 Telemedicine: The Future of Patient Consultation
Hyeongmin Cho
26 The Impacts of Climate Change on the Future of Public Health
Pearl Shah
28 A Case Study on How a Country’s Dependence on Tourism Can Affect Its Healthcare System: Thailand
Sittha Cheerasarn
32 A Gift of Fire: Guiding the AI-driven Healthcare Revolution for a More Equitable Future
Annie Huang
38 Beyond the Statistics: Young Women, Breast Cancer, and Self-Advocacy
Ananya Gulati
42 Breaking Barriers: Unveiling the Structural Risk Fueling the Gender Gap in HIV Vulnerability in Southern Africa
Prisha Batra Policy
48 Evergreening and Patent Warfare Between Pharmaceutical Companies Underlie Deeper Controversy on Intellectual Property Policy Across the World
Pranav Kotamraju and Tanisha Taneja, Policy Team
52 Weight Loss in Public Health: To Drug or Not to Drug?
Pranav Kotamraju and Tanisha Taneja, Policy Team
54 Introducing the Center for Gun Violence Solutions at the Johns Hopkins Bloomberg School of Public Health
Junwoo Park
56 Vaping: New Age Smoking With the Same Old Problems
Alicia Berger
58 Why Are You Studying Public Health?
Wanli Tan and Kevin Mao
59 What Does Public Health Mean to You? Research
62 FDA’s Project Optimus: Dose Optimization During Oncology Drug Development
Chujun Liu
65 Antibiotic Overprescription: Analyzing Possible Causes Within Asian Immigrant Communities
Timothy Huang
68 Navigating Public Health Research as Hopkins Students Research Team
70 Epidemic Proportions Staff 2023-2024
Letter from the Editors-in-Chief
To Our Readers,
It is with great pleasure that we share with you this very special edition of Epidemic Proportions.
Celebrating its fiftieth anniversary this year is the Johns Hopkins Undergraduate Program in Public Health Studies, a program which has inspired multiple generations of public health practitioners since its founding. Epidemic Proportions is in every respect a product of the program’s commitment to improving public health at the local, national, and international levels through curricular and extracurricular education and training. We are therefore proud to concurrently celebrate our journal’s twentieth anniversary this year. Since 2004, Epidemic Proportions has provided a platform for undergraduate students to share their experiences engaging in public health fieldwork and research, as well as to voice their perspectives on public health issues that resonate with them. As we commemorate not one but two anniversaries this year, it is only fitting that we reflect on the tremendous advancements that public health has made over the past twenty and fifty years. During this time, communities across the world have considerably enhanced their ability to respond to the myriad of health crises that have taken the global spotlight. In spite of this monumental progress, however, significant work remains in ensuring how moments from the past can inform the navigation of the future public health scene.
The desire to bridge historical experiences in the field with the modern face of public health has inspired the theme for the twenty-first volume of Epidemic Proportions: “Historical Horizons”.
As you peruse our journal, you will travel from Baltimore, our hometown, to New Orleans, and across the world from Southern Africa to Thailand, visiting a number of places along the way. In doing so, you will encounter a plethora of experiences and opinions on topics ranging from breast cancer and harm reduction to gun violence and telemedicine, all of which will challenge you to critically evaluate the status and direction of public health. The convergence of these two milestone anniversaries calls for the meaningful and thoughtful reflection required in public health, which will shed light on how society can maximize our potential to lead longer, happier, and healthier lives.
Once again, thank you so much for taking the time to read this very special edition of Epidemic Proportions. We hope that you enjoy “Historical Horizons” as much as we enjoyed composing it.
Sincerely,

 Neha Skandan Wassim Bouhsane
Neha Skandan Wassim Bouhsane
1
Letter from Vice Dean Joshua M. Sharfstein to the Editors and Readers of Epidemic Proportions
To the Editors and Readers of Epidemic Proportions:
Congratulations on this anniversary issue!
Fifty years of undergraduate public health education at Johns Hopkins represent a tremendous milestone, as does twenty years of this very journal. It is dizzying to think of all of the changes that have occurred both in public health and in public health education during this time. Fifty years ago, smallpox still existed in the wild – though the fight to eradicate it was being waged, and being won. Twenty years ago, the world had just survived an outbreak of a novel coronavirus, ushering in a new era of threats that would come to include the SARS-CoV-2 pandemic.
Public health education has changed over the decades as well. Certainly, core disciplines such as epidemiology and biostatistics have remained pillars of the field. But joining them are now public health ethics, community-based participatory research, and health equity. To succeed, technical proficiency in data analysis is still necessary, but hardly sufficient. Community engagement, policy development, and advocacy are essential skills for understanding key health challenges and opportunities for making tangible progress for health, well-being, and justice.
In 2006, as health commissioner of Baltimore, I reached out to the undergraduate public health program at Johns Hopkins about a new initiative that I was hoping to bring to the city, then called Project Health (and now called Hopkins Community Connection). I was amazed by the students' enthusiasm, commitment, and leadership, which made the program possible. In the years since, hundreds of Hopkins students have helped thousands of Baltimore families obtain essential resources for their health. I am eternally in debt to you for these ongoing efforts, even as I marvel at the inspiring new projects that students create, develop, and implement.
In short: Thank you for the brilliance, light, and hope that you bring to our field and to our world.
And again, Congratulations!
Sincerely,
 Joshua M. Sharfstein, M.D.
Joshua M. Sharfstein, M.D.
Vice Dean for Public Health Practice and Community Engagement
Distinguished Professor of the Practice
Johns Hopkins Bloomberg School of Public Health
2
Letter from Dean Christopher S. Celenza, for Epidemic Proportions: Celebrating 50 Years of Public Health Studies
As dean of the Krieger School of Arts and Sciences, I am pleased to congratulate our undergraduate program in Public Health Studies on its 50th anniversary.
In many countries—especially developed ones like the United States—the accomplishments credited to public health are often taken for granted: access to clean water and air, vaccine availability, effective sanitation services, and safe food production. But the contributions of public health practitioners have improved, and in many cases saved, the lives of millions of people around the globe.
Here at Johns Hopkins, our world-renowned Bloomberg School of Public Health has played a huge role in alleviating countless diseases and conditions that are harmful to various populations. And for 50 years, undergraduates in the Krieger School of Arts and Sciences have learned from and worked beside experts from the Bloomberg School.
Public health studies is now one of our largest and most popular majors. When it first debuted 50 years ago, 29 students declared the major. Today, it is home to more than 500 students. In fact, Hopkins helped pioneer the idea of undergraduates studying public health, and more and more colleges are looking to us as the model.
Our public health students are curious, driven, and passionate about the work they do and the research they conduct. They are eager to play a role in improving the lives of others and making a real difference in the world. Whether walking along the steamy banks of Uganda’s Lake Victoria talking to fishermen about their health concerns and poor working conditions, or sitting in a small room in Baltimore City helping low-income residents access the social services they so desperately need, our students are on the front lines. These applied experiences give them the kind of beyond-the-classroom exposure to public health issues that help prepare them for careers in public health.
As the planet’s population hovers near the 8 billion mark, public health challenges also grow, whether 7,000 miles away in equatorial Africa or several blocks away from the Homewood campus, in neighborhoods where the majority of people live below the poverty level.
With the Krieger School’s Program in Public Health Studies reaching its 50th-year mark, I can’t help but reflect on the impact our thousands of students have had—and will continue to have—on multiple global populations. Many of our graduates have gone on to graduate school, medical school, and health policy careers, where they will continue to advocate for positive health outcomes for all and action in the face of public health emergencies. This is their calling, and I am so proud of them.
I send warm wishes, heartfelt congratulations, and deep thanks for all of the students and faculty members associated with our public health studies.
Sincerely,
Christopher S. Celenza, Ph.D.
James B. Knapp Dean
Zanvyl Krieger School of Arts and Sciences
Johns Hopkins University
3

A Note on the Cover
Public health is not just about the confrontation between the destructive and powerful virus and the rapidly developing biomedical fields, but also the social construction of a system dealing with medicine administration, standardizing treatments, and resolving health disparities. By depicting cities of medicine containers and the collision between a virus and a robot, I hope to show the close relationships of public health issues with various other fields, including policy, biology, epidemiology, and hospital administration. The interdependence of multiple fields will be crucial for improvements in community health. Combining with the futuristic view, this issue will take us down a memory lane to appreciate previous Epidemic Proportions issues and the journey of discovering and discussing real-world issues.
-Rose Chen
4
Shannon Wang Zao

5
Shannon Wang Zao

 Features
Shannon Wang Zao
Features
Shannon Wang Zao
Addressing Social Needs in Gynecology Oncology: Insights from a Hopkins Community Connections Advocate
Aminata Sinyan
Serving as a Hopkins Community Connections (HCC) advocate in the Summer of 2023 for the Kelly Gynecologic Oncology Services, a clinic that aids patients suffering from cancers or diseases of the female reproductive system, I addressed problems revolving around an individual’s social determinants of health (SDOH) and social needs. The Department of Health and Human Services defines SDOH as conditions in the environment where people are born, live, work, and age: all of which impact health, quality of life outcomes, risk, and an individual’s social needs (U.S. Department of Health and Human Services, 2024). At HCC, we targeted multiple disparities faced by our Gynecology Oncology patients by connecting them to resources within the Baltimore community and beyond. A significant focus within the clinic was targeting the issue of food insecurity. Numerous referrals screened positive for food insecurity in their social needs screening. Throughout the experience, I will also highlight accomplished goals and share newfound perspectives that became clearer to me.
During my fellowship, my primary goal was to enhance adaptability in the patient care setting, navigating challenges that arose when juggling an increased workload and maintaining timely patient follow-ups. The pressure of failing to reach patients promptly led to heightened anxiety, prompting a pivotal decision to balance my time by reducing work hours and accommodating my other summer job. The GYN/ONC staff emerged as crucial pillars of support, playing an integral role in my journey. As I took on the responsibility of crafting
weekly emails detailing the number of enrolled patients, case closures, and triage patients for the Equity through Quality Improvement Partnership meetings, I found myself immersed in the narrative of healthcare dynamics. Beyond mere tasks, my goal extended to learning about diverse resources available to patients and their specific demographics, aiming to streamline referrals and integrate social needs screening seamlessly. Throughout the summer, my experience transformed from navigating struggles to making compromises and ultimately, to insightful observations. As I grappled with challenges, I honed my ability to comprehend patients’ situations, adeptly document them, and promptly identify appropriate resources.
reported 13.7 million households were food insecure, and 5.6 million experienced very low food security” resulting in some household members altering their food eating patterns (Gregory & Todd, 2021). This includes a reduction in food intake to accommodate for low funds in that area of expenses for lack of sufficient resources for food (Gregory & Todd, 2021). I encountered patients expressing the need to forgo specific meals each day due to insufficient resources to adequately support themselves or their families. These patients may have also been going through difficult health situations or In this case, food pantries, food stamps, and fresh food delivery services are the immediate line of action to address their needs. Expansion into

This journey not only fulfilled tasks but deepened my understanding of patients’ unique needs and the resources suitable to address them, fostering a more nuanced perspective in the realm of public health.
Delving further into this exploration, the research article, “SNAP Timing and Food Insecurity”, the “USDA
working with other community based organizations that help supply certain food pantries and food programs is how the work is upscaled—examples include Moveable Feast and Hungry Harvest.
Consequently, involving other community organizations and members allows for expanded outreach to
8
National Cancer Institute/Unsplash
patient needs. Targeting larger patient populations involves partnership with physicians, nurses, providers, and policymakers. Physicians, providers, and researchers delve into the impact of screening for social needs and referral outcomes. This allows for funding to accommodate the growing patient field and for more resources to address their needs. Research also provides evidence in support of legislation to target community members’ social determinants of health. Examples of such legislation include amendments to government benefits or even regulations within the hospital setting. Some amendments to the Supplemental Nutrition Assistance Program Food and Nutrition Service (SNAP) are one of the many ways that accessibility has been made easier for people in need of more food resources. While households can receive an average of “$258 in monthly benefits,” authors Gregory and Todd argue that this amount may not even be enough to curb food insecurity based on under-represented numbers of survey food scarcity and “declines in expenditures and dietary intake at the end of the benefit month” (Gregory & Todd, 2021). This is where additional support programs take effect for patients.
I gained substantial insight into the challenges faced by the lower middle-class population. GYN/ ONC patients in this socioeconomic bracket/class encountered difficulties: they were not affluent enough to manage the increasing cost of living, yet their income did not qualify them for assistance or benefits. In most cases, referred patients qualified for aid due to their lower income status. This facilitated easier connection to resources and approved assistance upon application review. However, individuals maintaining incomes just above subsistence struggled to meet the cost of healthcare, food, housing, and utilities. These patients live in precarious financial situations, heavily affected by the rising cost of living. Challenges not only lie in identifying
available resources for these patients, as fewer options cater to their needs due to eligibility. Grants, in addition to assistance, primarily benefit those experiencing those with severe financial hardship, a criterion posing greater difficulty in validation for middle-income patients. Witnessing these individuals ensure such challenging circumstances is not only disheartening for patients themselves, but also deeply distressing for the limited capacity to provide comprehensive support.
The experiential journey detailed as an advocate for HCC encapsulated pivotal themes in addressing social determinants of health and catering to the pressing social needs of Gynecologic Oncology patients. It helped illuminate the pervasive issue of food insecurity among patients, calling attention to its multifaceted impact on health outcomes. The micro-level interventions employed by HCC underscore the importance of tailored support for individuals, emphasizing the value of localized assistance strategies. The challenges faced by middle-income patients, falling within the gap of support systems, highlight the nuanced complexities of financial aid eligibility; revealing the inadequacies of existing programs. Ultimately, this narrative advocated for targeted interventions, increased collaboration, and policy amendments to bridge
“
They were not affluent enough to manage the increasing cost of living, yet their income did not qualify them for assistance or benefits.
gaps and provide more inclusive and comprehensive support for vulnerable populations facing health-related social hardships.
References
1. U.S. Department of Health and Human Services. Healthy People. Social Determinants of Health. [Online]. Available at: https://health.gov/healthypeople/priority-areas/social-determinants-health. Accessed January 20, 2024.
2. Gregory, C. A., & Todd, J. E. (2021). SNAP timing and food insecurity. PLOS ONE, 16(2), e0246946. https://doi.org/10.1371/ journal.pone.0246946
Organization Information
Moveable Feast
Moveable Feast’s food delivery program focuses on the vital role of nutrition in supporting clients’ health and disease-fighting efforts. The program’s dietitians and chefs collaborate to craft medically appropriate, nutritious, and delicious menus, prepared in a state-of-the-art kitchen using fresh ingredients. Although home visits are currently on hold due to the COVID-19 pandemic, the program utilizes a secure telehealth platform for nutrition counseling, where Registered Dietitian Nutritionists work with clients to create personalized nutrition plans, set realistic goals, and discuss lifestyle changes aimed at improving long-term health.
Hungry Harvest
Hungry Harvest’s food delivery program is a culinary adventure for those who love experimenting in the kitchen, embracing every color and shape of the harvest to bring joy and variety to their plates. The program focuses on rescuing farm-fresh fruits and vegetables that would otherwise go to waste, delivering them affordably and conveniently to your doorstep. Beyond the culinary experience, Hungry Harvest strives to make a positive impact by saving at least 10 pounds of food per delivery, closing food access gaps, and reducing environmental impact, contributing to a more sustainable future.
9
”
Grace House - My Experience Witnessing Recovery and Resilience Within New Orleans
Isabelle Jouve
Within minutes of arriving to shadow at Grace House, a long-term substance-use disorder treatment facility in New Orleans, a woman named “Allie” in her early fifties walked into the clinic. Her brilliant, blue eyes lit up the room, and she excitedly greeted me. I followed Allie and two medical students into a small exam room that smelled faintly of disinfectant.
After reviewing her medical history, we joined the facility’s internal medicine physician, Dr. Elyse Stevens, to develop Allie’s plan of care. Seated together at a round table, we sought to provide Allie with an army of support, empowering her journey towards recovery. Allie pulled out a lengthy hand-written list from her purse, detailing questions that had been left unanswered for far too long.
In each patient appointment I shadowed, I always noticed Dr. Steven’s tactful questioning, while simultaneously connecting a web of clues to a diagnosis. I also admired her ability to brighten up the atmosphere by encouraging Allie, who expressed her daily struggle to remain sober following decades of addiction. As Allie pointed to a massive lump on her lower stomach, she grimaced describing the pain she felt and her battle to obtain treatment.
Dr. Stevens then asked about her STI diagnosis and if she was still taking the medication listed in her chart to treat gonorrhea. Confusion shadowed Allie’s face as she asked, “What is an STI?” She only knew her medications by each pill’s color and shape, rather than their purpose. Allie had no idea what was happening inside of her own body.
Every patient I met at Grace House bravely shared their story, revealing obstacles such as access to transportation, difficulty finding child care, and a gap in health education. “Natalie”, 59, spoke about how her late cancer diagnosis caused life-long health issues, while “Christie”, a 28 year old mom, shared that she didn’t know she was pregnant until her third trimester. One key question prevailed: how could the women at Grace House advocate for themselves and effectively seek medical care without healthcare education on fundamental topics, such as STIs, cancer prevention, and menopause?
These patient interactions inspired me to create a reproductive healthcare workshop program for the residents. The program’s focus has been to provide an engaging, comfortable setting for residents to learn key health information and promote a proactive, rather than reactive, approach to their care. Understanding that it is unrealistic for residents to memorize facts from a two-hour workshop, my goal is to teach them how to identify and communicate their health concerns.
During workshop sessions, residents are often shocked upon learning fundamental health facts, such as the difference between menstruation and the menstrual cycle or that symptoms they have been experiencing for years are irregular. They will often remark that the workshop inspired them to discuss their newfound understanding and concerns at an upcoming clinic appointment, which is a pretty powerful outcome.
I have also observed that workshop sessions become safe spaces for residents to recount past medical
difficulties and hear others’ stories. A few weeks ago, “Natalie”, 25, shared that she had an IUD inserted at 18, but her provider refused to remove it after its expiration. Her IUD remained in place for two more years until excruciating pain sent her to the emergency room. Physicians found a 14-centimeter ovarian cyst, and she subsequently had surgery that resulted in her losing an ovary. Natalie expressed that education on birth control methods and potential complications as a teen could have prevented this.
“
The residents remind me why I decided to go into medicine in the first place, and I’m so thankful for the chance to work with them each week.
”
Since last summer, I have recruited a team of medical students and undergraduates to facilitate the workshop regularly. The program provides students the chance to gain meaningful patient interaction while becoming increasingly popular among the residents.
Rowan Miskimin, the director of the Grace House Student-Run Clinic, shared, “The residents remind me why I decided to go into medicine in the first place, and I’m so thankful for the chance to work with them each
10

week. The journey through recovery brings so many unexpected challenges, and these phenomenal women are all here choosing to love and care for themselves no matter what it takes. It’s a reminder to all of us to fight for our own joy and wellbeing, and to nurture the relationships that keep us going. It’s an honor to learn from Grace House residents and staff, and I hope to use my education to further support this wonderful place in the future.”
Over the last seven months, I have gotten to know so many women at Grace House who are survivors with unimaginable strength. I look forward to chatting with them in the hallways and witnessing their progress in recovery. The Grace House Workshop Program empowers the women we teach and honors their resilience. In the words of Dr. Elyse Stevens, “Taking care of women recovering from substance use is life-changing. It is tremendously humbling and eye-opening listening to the stories of women who have been through some of the most horrible moments imaginable. From the outside, other people don’t see the story behind how or why the patient fell into substance use. When you actually listen to what they have to say you realize that this could have been me - this could be anyone. What would I have done in that situation? Would I have even survived? I love that I get to celebrate with
these incredible women how strong and resilient they have been in order to survive all they have been through and come out thriving.” teach and honors their resilience. In the words of Dr. Elyse Stevens, “Taking care of women recovering from substance use is life-changing. It is tremendously humbling and eye-opening listening to the stories of women who have been through some of the most horrible moments imaginable. From the outside, other people don’t see the story behind how or why the patient fell into substance use. When you actually listen to what they have to say you realize that this could have been me - this could be anyone. What would I have done in that situation? Would I have even survived? I love that I get to celebrate with these incredible women how strong and resilient they have been in order to survive all they have been through and come out thriving.”
Organization Information
Grace House is a 24/7 residential treatment facility that provides substance-use disorder treatment women. With a male equivalent called Bridge House, both residential facilities provide programs that have continuum of care that aims to increase the quality of life of people with addictive disorders. While sobriety is the highest priority of treatment, Grace House also aims to rebuild client relationships with their family, friends, and the surrounding community.
Biography
Isabella Jouve is a Sophomore that is majoring in public health studies. She wants to focus on health policy in her career.
Community Close to Home: My Summer at Baltimore Harm Reduction Coalition (BHRC)
Atri Surapaneni
On the first day of my summer internship with Baltimore Harm Reduction Coalition (BHRC), I took a scenic stroll down Calvert Street to a row home, a small flier hung by its entrance. The place was home to a nonprofit that focused on the health, safety, and dignity of people in the Baltimore community who were affected by the war on drugs and the opioid epidemic. The three-story row home was deceptively spacious. Every corner was organized with shelves and supplies in a methodical chaos. For a few hours each day at BHRC, I spent time making a variety of safer drug use supply kits, Narcan kits, hygiene kits, and other essential items that were to be distributed. It was during these hours of repetitive motions and zipping up Ziplocs that I got to connect with my coworkers. Working in an assembly line made the process much more efficient and enjoyable.
It was during these times that I got to connect with my coworkers. One of my colleagues told me stories about his time playing college basketball, casually name-dropping a few future NBA talents he competed with. Being an avid basketball fan, I was enthralled by his stories of his team’s run to the semifinals of the NIT. Another one of my coworkers had been studying for the Bar exam while working, and one went to college for music and
11
Brother Swagler/Unsplash

skillfully played his guitar during a few lunch times. I was so fortunate to be welcomed by a passionate and diverse staff who created a collaborative environment and an enriching experience for me. Building camaraderie with my coworkers allowed me to help out on service shifts in the final weeks of summer.
During these shifts, I helped distribute snack bags and harm reduction supplies and filled out the blue sheets BHRC uses to keep track of how many kits were distributed. This experience prepared me for conducting BHRC’s satisfaction survey, where I got to speak with over a dozen Baltimore residents living near Maryland Avenue about BHRC’s services, how they get food, and their utilization and experience with governmental supplemental nutrition programs such as SNAP. Talking to community members was always memorable. My interactions and conversations while conducting the surveys had mixed feedback about the process of applying for SNAP and food stamps, but there were concerns about this decreasing funding each month, especially in a time of inflation and economic uncertainty. Prior to working on this project, I thought
that nonprofits and government were largely disconnected and sometimes at odds with one another, but I believe one of the responsibilities of nonprofits should be to collaborate and inform the government.
Organization Information
Baltimore Harm Reduction Coalition, Inc. (BHRC) is a community-based organization located in Lower Charles Village, with a focus on harm reduction for people who use drugs or engage in sex work. Not only do they provide trainings, resources, and help advocate for harm reduction policies, but have a mission to address the war on drugs and anti sex-worker policies at individual, societal, and systematic levels.
An “Eye” Opening Experience
Tabatha Alegria
In high school, I worked as a medical technician which exposed me to patient care. I especially liked optometry because I felt like optometrists and assistants at their offices could build a long-term relationship with a patient. It always warmed my
heart to see how the optometrist and patients could talk freely about more than just medicine, like last night’s sports game or a recent event in the community. Although optometrists are doctors one should see annually, possibly more if one has any issues relating to vision such as dry eye syndrome, being able to establish this connection with each and every patient is something that amazed me.
I live in a community with a large Hispanic/Latinx population. As a Spanish speaker, I observed how language barriers and other healthcare disparities affected marginalized groups and decided to translate eye exam instructions and results to make eye care more accessible to my community. This experience along with one of the doctors in my office who majored in public health inspired me to major in the same field. She shared how much she enjoyed learning about the interaction between medicine and communities along with the inherent flaws of the US healthcare system, and this sparked a passion in me, and something I would like to combat by helping as many as possible overcome language barriers in healthcare so that medicine can truly reach everyone.
I want to be a part of public health research and public health activism at Hopkins. Research that works on studying and solving healthcare barriers for immigrants, and activism that directly involves these communities. I want to ensure that healthcare is truly for all; at Hopkins, I will work towards that goal.
12
Atri Surapaneni
Atri with members of the Baltimore Harm Reduction Coalition.

13
Elen Sher/Unsplash
Hopkins Past the 21218: Baltimore, DC, and Beyond Habin Hwang, Features Team
“The university’s new home in Washington, DC – the Hopkins Bloomberg Center – offers a wonderful venue for public health studies courses and events. It’s just a short train ride from Baltimore, and hopefully it will foster the development of a truly bidirectional portal between our students, faculty, and staff in Baltimore and Washington, DC.” Lainie Rutkow, PhD, MPH)
‘What is Democracy?’
The question that welcomed the undergraduate Class of 2026 to Johns Hopkins University echoed into the opening of the DC Bloomberg Center in Aug. 2023. Formerly housing the Newseum, the museum of American journalism, Johns Hopkins’ dedication to further exploring this question is reflected in acquiring this collaborative space. With intent to streamline the world-class School of Advanced International Studies (SAIS), Krieger School of Arts and Sciences (KSAS), Carey Business School, and Peabody Institute, the space serves to integrate each of their strengths. Sandwiched between the U.S. Capitol building and the White House, the school is a beacon of education within the prestigious and diverse DC community.
Johns Hopkins acquired the Newseum building in 2019, and invested $650 M towards its acquisition and renovation. Shortly after its opening in 2023, school leadership declared their intent to open a School of Government and Policy there, and began offering undergraduate courses there through its Carey Business School and Krieger School of Arts and Sciences.
“What this represents is the physical manifestation of the university’s commitment to national and international engagement,” said Ronald J. Daniels,
Hopkins’ president, to the Washington Post. “The idea was to create a place for the university in Washington proximate to power.”
Reflecting a “reciprocal connection” between DC and its surrounding community, the University not only hopes to create an infrastructure that promotes collaboration between students, but also increases student and faculty engagement with DC policymakers, analysts, and think tanks. While faculty and students would bring their expertise, passion for learning, and ideas to DC, the policymakers and analysts in the Nation’s Capitol would interact more regularly and deeply with the students of Johns Hopkins.
“
Students here have access to worldclass faculty doing research on just about every area of public health.
”
The first cohort of students who will be pursuing the 5th year Master’s Degree with SAIS will be matriculating to the campus in fall of 2026, while various undergraduate courses will be offered each semester until then.
“We are honored that the Johns Hopkins University Bloomberg Center chose to open a new space on Pennsylvania Avenue in the heart of our downtown,” said Washington, D.C., Mayor Muriel Bowser to Forbes. “We
have set the bold goal to win back our downtown by making Washington, D.C., a place for successful businesses and opportunity-rich neighborhoods. Johns Hopkins University Bloomberg Center brings a new hub for global leaders to convene, and new employment and educational opportunities to our downtown.”
Furthermore, the campus is exciting news for the faculty and students in the undergraduate Public Health Studies (PHS) department.
“There is no better place to study public health than Johns Hopkins,” stated Maria Bulzacchelli, director of the PHS department. “Students here have access to world-class faculty doing research on just about every area of public health. Hopkins also offers so many funding opportunities for students to pursue research—you don’t have that everywhere.”
With the opening of the interdisciplinary Bloomberg Center, students from various undergraduate programs will have opportunities to work directly on Capitol Hill with policy makers, and will give a new meaning to the “applied experiences” that the PHS department emphasizes. With the hopes of opening the doors for more valuable learning opportuni-

14
Raymond Zhang
ties for undergraduates, many faculty members have high hopes for what the Center will mean for the advancement of undergraduate PHS education.
“I can imagine students spending a semester in DC working with policy makers,” Dr. Bulzacchelli elaborated, “A lot of federal public health agencies have their headquarters in DC. And then of course there’s Congress— they are always debating legislation with public health implications.”
Since the COVID-19 pandemic, infrastructure and public health policy have become more important and relevant in the public eye. While it is the hope of everyone that another pandemic could be avoided, being able to better detect and respond to future pandemics by improving infrastructure and streamlining public health policy is one of the current goals of many at Hopkins. With the many bright minds to be housed in the new Bloomberg Center and the connections they will form with the community around them, Hopkins’ commitment to research, innovation, and discovery is highlighted in these many investments made.
Additional Information
The new DC building has a “beach” reminiscent of the one present on Homewood campus, where students can have informal and social gatherings in a common space. This space is present in the atrium of the building, and is surrounded by a “room stair” and a “room bridge.”
The DC building was originally the Newseum, a building that highlighted American journalism and its contribution to democracy. The building was reconfigured by the Ennead Design team led by architects Richard Olcott, Kevin McClurkan, Felicia Berger, and Alex O’Briant to highlight Johns Hopkins’ commitment to transparency, health, and wellbeing. In order to honor the Newseum and
all that it symbolizes towards the American Democratic process, Johns Hopkins ensured that the original Newseum building was as preserved as possible while highlighting the school’s mission and values.
Why
I (and Many Others) Chose to Double Major
Vivan Guo, Features Team
With a LinkedIn headline that reads ”Public Health & Anthropology at John Hopkins University,” I am more inclined to connect with those studying at least one of the aforementioned subjects. More often than not, it is the former major that I share with my fellow undergraduate classmates— an observation that holds even while sitting in my only Anthropology class this semester. However, it still excites me to know that in our graduation diplomas, there will be a line of subtext that reads: “with a secondary major in,” connecting Public Health Studies with other departments like Computer Science and Molecular and Cellular Biology that students endearingly refer to as MolCell.
From pursuing personal interests to fulfilling pre-med requirements, undergraduate students at Johns Hopkins cite a variety of reasons for pursuing a double major in addition to Public Health Studies. Thankfully, the versatility of interdisciplinary courses at the Bloomberg School of Public Health (BSPH) and Hopkins’ flexible major requirements encourage student exploration which can be reflected in some of the responses below:
Alina Galaria (Class of 2025) is currently pursuing a double major in Public Health and Natural Sciences and an Islamic Studies Minor. This interdisciplinary approach aligns with her aspirations to attend medical school and attain a master’s in Public Health.
Christine Kim (Class of 2025) is also a Molecular and Cellular Biology double major and pre-med student but for the exploration of “the macroscopic and microscopic aspects of health” through the combination of these disciplines.
Kevin Mao (Class of 2027 and fellow Epidemic Proportions editor) intends to double major in Molecular and Cellular Biology because “the major requirements overlap nicely with pre-med requirements.” He mentions how the combination of these majors touches on mental health, medicine, and public health, making it an ideal path for pursuing forensic psychiatry.
Tabatha Alegria (Class of 2027) plans to double major in Spanish to “learn more about her Latina culture,” motivated by her future aspiration for a job in healthcare. The application of such knowledge would facilitate meaningful interactions with patients in multicultural settings.
Personally, I, Vivian Guo (Class of 2027), hope to delve into the field of Urban Planning by leveraging the offerings at the Bloomberg School of Public Health (BSPH) and the Krieger School of Arts and Sciences’ Anthropology department. For those contemplating a public health double major, consider how the field offers unparalleled versatility. The holistic understanding of various health disciplines allows students to prioritize academic interests that resonate with them— even more so with an additional major.
15
Looking Back, Looking Forward - the Past 50 Years of Undergraduate Public Health Education
Habin Hwang, Features Team
“A couple of decades ago, when— for the most part—public health education was available only at the graduate level, a lot of people ended up in public health later in their careers, discovering the field only after starting their working life in something else. Offering public health education at the undergraduate level means the field can attract bright and passionate young people at the start of their careers.”
-Maria Bulzacchelli, Director of Undergraduate PHS
In the first half of the 20th century, Public Health education was first marketed as a graduate level track designed for medical professionals striving to take on governmental public health roles. The School of Hygiene and Public Health (now Bloomberg School of Public Health) was established for this purpose in 1916 as one of the first graduate education programs for Public Health. Though its establishment was groundbreaking towards Public Health education as we see it today, education was not geared towards undergraduates, and MPH’s were solely offered as a graduate level track.
However, with Dr. Abraham Lilienfield’s advocacy for public health topics, namely epidemiology, to be taught at the undergraduate level, the School of Public Health (SPH), in collaboration with the undergraduate School of Arts and Sciences, began laying the groundwork for the undergraduate Public Health Studies major.
Johns Hopkins University’s School of Arts and Sciences began offering a B.A. degree in Public Health Studies (PHS) with an emphasis in either natural or social/behavioral sciences in 1974, the first in the nation to accom-
plish the feat. Many other liberal arts universities followed suit shortly after in establishing their own undergraduate PHS departments.
Within the next five years, the number of graduating seniors increased from under 25 to nearly 75, making it one of the most popular majors at the School of Arts and Sciences. With the full support of John Chandler Hume, the Dean of SPH from 1967-1977, undergraduates were encouraged to take graduate level classes. The growth of the major was additionally caused by the rising interest in community service, as well as the newly added full time advising programs.
Despite its rapid growth, the PHS department didn’t hit its breakthrough until the early 2000’s. In 2000, the major’s core curriculum was rewritten to include statistics, epidemiology, environmental health, health policy and management, biology, english, and calculus. Furthermore, a critical marriage was made between the SPH and PHS department that exists to this day, requiring students to take at least
one year of elective graduate courses at the SPH.
“About ⅔ of my [undergraduates] are second-generation immigrants,” stated Dr. Peter Winch, who currently teaches at the Bloomberg School of Public Health. “Often their interest in public/global health starts from seeing how their relatives in their parents’ homeland are served or not served by the health system. Whereas if you look at the graduate students, many of them have been out working already. They have work experience, while the undergraduates have more family experience. Both kinds of experiences are very important.”
The growth in the early 2000’s was also accompanied by the movement to increase accessibility for undergraduate public health education. Between the years of 2003 and 2005, the then Association of Schools of Public Health (ASPH)* established the Undergraduate Public Health Task Force, which advocated for the many accredited programs across the nation. In 2006, the Council of Colleges of Arts

16
Dr. Bulzacchelli and Dr. Winch (Dr. Winch is receiving the Golden Apple award in May of 2023)
and Sciences sponsored the Consensus Conference on Undergraduate Public Health, leading to a stronger national cohesiveness in ‘101’ and core courses in the field of public health.
*Footnote: the ASPH became the ASPPH in 2013
In the past two decades, the B.A. in Public Health has evolved to include an applied experience as a degree requirement, where students could gain hands-on experience with experienced professionals in the field. The major increased rapidly in popularity over the years due to how it was flexible and adaptable, in addition to adapting well to the pre-medical curriculum.
“Another thing that happens—and this is not something we do on purpose—but another thing is that some students who come to Hopkins on the pre-med track discover public health and realize they can help people and do something health related without necessarily working in a clinical setting,” stated Maria Bulzaccheli, the current director of the undergraduate PHS department. “Offering public health education at the undergraduate level means the field can attract bright and passionate young people at the start of their careers.”
With over 500 declared PHS majors today, a vibrant community has formed at Hopkins since the conception of the department in 1974. Currently, fourth year students in the department can take classes at the SPH in all 10 areas, and can gain exposure to public health topics in the following areas: health education, environmental health sciences, epidemiology, health finance and management, health policy, human genetics, immunology and infectious diseases, international health, maternal and child health, mental health, nutrition, occupational medicine/health protection and practice, population studies, toxicology, and tropical medicine among others.
“I really think [public health education] creates students who are more well rounded in their understanding of how people make choices around their health and the ways interventions either work or don’t work for human health,” stated Dr. Margaret Taub, who teaches Biostatistics to PHS undergraduates. “It gives this perspective that there are so many factors outside of individual physician interactions with patients that determine people’s health. And all of those things are really important to keep in mind.”
Most recently, the Johns Hopkins University Bloomberg Center at 555 Pennsylvania Avenue was established, with its opening in August of 2023. Though it is primarily associated with the School of Advanced International Studies (SAIS), PHS officials hope to open up more opportunities for students to interact with public health policymakers and to explore more interdisciplinary policy-centered fields.
Additional information
Abraham Lilienfield, MD, MPH
Dr. Abraham Lilienfield’s, one of the “founders’’ of the undergraduate PHS department, was one of the main contributors towards the 1982 Surgeon General’s report stating that smoking was harmful for health. He also is known as the “father of contemporary chronic disease epidemiology.”
According to the Bloomberg School of Public Health, ‘Dr. Lilienfeld’s students and colleagues recall his “singular lack of self-interest, great willingness to help others, and tireless devotion to the advancement of public health science.”’
Maria Bulzacchelli, PhD
Dr. Bulzacchelli, often endearingly referred to by her students as Dr. B, had her beginnings at the Bloomberg School of Public Health. Prior to entering graduate school she held positions at the Harvard School of Public Health and Massachusetts General
Hospital. After getting her doctorate degree at the School of Public Health, she adopted the PHS director position in 2016. Her research primarily focuses on injury prevention and workplace safety.
Peter Winch, MD, MPH
Dr. Peter Winch currently teaches seminars in Global Sustainability and Health at the Bloomberg School of Public Health. His research and work primarily focuses on global health.
References
1. Brieger H, Gert. Goodyear D, James. C. Public Health Studies: A Popular New Major at Johns Hopkins University. In: The 129th Annual Meeting of APHA ; 21 Oct. 2001; Atlanta, Georgia. Accessed January 20, 2024. https://apha.confex.com/ apha/129am/techprogram/paper_29685. htm
2. Garcia X, Martinez Y, Rodriguez Z. Undergraduate Public Health Studies at Johns Hopkins. In: The 131st Annual Meeting of APHA; 15 Nov. 2003. Accessed January 20, 2024. https://apha.confex.com/ apha/131am/techprogram/paper_73844. htm
3. Riegelman RK, Albertine S, Wykoff R. A history of undergraduate education for public health: from behind the scenes to center stage. Front Public Health. 2015;3:70. Published 2015 Apr 27. doi:10.3389/fpubh.2015.00070
4. Johns Hopkins University. Public Health Studies. Accessed January 20, 2024. https://e-catalogue.jhu.edu/arts-sciences/full-time-residential-programs/degree-programs/public-health-studies/
5. Johns Hopkins University. Public Health Studies: Fifty Years of Excellence. Accessed January 20, 2024. https://krieger. jhu.edu/publichealth/about/fifty-years/
17


Editorials
Shannon Wang Zao
The Gun Violence Epidemic: Why This Issue Is More Severe Than We Realize
Samuel Yeboah-Manson
The National Rifle Association (NRA) is an important organization to understand this issue. The NRA was originally a recreational group aimed at encouraging rifle shooting on a scientific basis.2 Today, the NRA has 5.5 million members and trains one million gun owners annually.2 Most importantly, this organization is heavily involved in lobbying, spending $2.5 million on advocating for legislation that expands access to guns.3 According to the NRA, since 2013, 382 “pro-gun” bills have been enacted.4 Such laws have been adopted by the Governors in Arkansas, Georgia, and Texas, which have allowed people with concealed carry licenses to bring guns into public spaces like college campuses.
One reason gun violence should be declared an epidemic is that it meets the very definition of one. Although gun violence is not an infectious disease that can not be diagnosed or treated, gun-violence related deaths certainly reach numbers close to that of various diseases. In 2021, while 56,000 individuals died from chronic liver disease, gun violence took the lives of almost 48,000 individuals.4,5 Given these comparable numbers, it is safe to say that the burden of gun violence is significant and warrants extreme attention. The effects of gun violence also mirror those of any conventional infectious disease. Victims of gun violence often suffer from long-term physical and psychological effects, either from being shot and injured or from witnessing these events. Victims and bystanders alike are likely to experience stress, depression, and PTSD.6 These effects may be further exacerbated by the lack of accessible mental health care in the
United States; 42% of the population sees the cost of mental health services and poor insurance coverage as a barrier to obtaining necessary mental health services.6
The overall firearm death rate in the United States is ten times higher than in other high-income countries.7 Furthermore, the number of people dying from mass shootings in the U.S. surpasses that of other countries. 82% of all firearm deaths in two dozen populous, high-income countries, occurred in the United States; additionally, 91% of children ages 0-14 who were killed by firearms were from the United
“
Incidents of gun violence are only increasing in the United States.
”
States.8 Gun violence not only affects the victim, but also affects everyone around them, including parents, siblings, friends, and other members of their support system. Furthermore, the financial toll of gun violence is compounded by the already high cost of healthcare. According to the American Academy of Family Physicians, expenses associated with the aftermath of gun violence like medical bills, daily care/support, and criminal justice expenditures cost the United States economy approximately $229 billion annually.8
Enumerating the reasons why gun violence is an epidemic is certainly
satisfactory and constructive, but it does nothing if we do not propose solutions to end this issue. Overall, gun violence needs to be addressed with evidence-based strategies that also take into account the input of the communities in which its effects are disproportionately felt. Instead of blaming gun violence on mental health, which exacerbates already existing stigma and prevents others from seeking care, we should focus on understanding systems of violence that make people more likely to act violently. Scientists should work with leaders in disenfranchised communities to develop interventions that reduce risk factors responsible for gun violence. Overall, we need a community-based and scientific approach.
Reducing the risk factors that can lead to gun violence is a good first step when it comes to reducing the actual incidence of gun violence. Additionally, advocacy for these issues is also a great first step. Institutions like The Center For Gun Violence Solutions at Johns Hopkins University are using research to inform advocacy for greater gun legislation by directly engaging with affected communities to implement changes, further involving disenfranchised groups in the process and tackling the systematic causes of firearm-related violence rather than putting band-aids over bullet holes.9 Their research provides a contextual and scientific basis for defining—and even solving—an issue, but such research is futile if we do not know if it is effective or not. We must invest in ways to evaluate the effectiveness of developing strategies to improve the safety of individuals, families, and larger communities.
20

In conjunction with research and assessment, legislation is also essential to addressing this epidemic. One way to achieve this goal is by passing a prevention policy that serves as an effective foundation. Such a policy includes an universal background check law, which effectively works by preventing firearms from reaching the hands of dangerous individuals. Passing strong laws that also promote equitable enforcement of specific gun laws should also be a top priority.
Some people who do not view gun violence as an issue often state that the second amendment guarantees all Americans the right to bear arms. However, these people fail to consider the potential consequences of an amendment established over two hundred years ago. It is improbable that the founding fathers of the United States envisioned the use of assault weapons in the tragic and senseless loss of lives, endangering the very right they aimed to safeguard—the right to live.
References
1. National Rifle Association. About the NRA. Nra.org. Published 2023. https:// home.nra.org/about-the-nra/
2. OpenSecrets. National Rifle Assn Lobbying Profile. OpenSecrets. Published 2023. https://www.opensecrets.org/federal-lobbying/clients/summary?id=D000000082
3. PBS NewsHour. NRA Has Backed Most State Gun Laws Passed since Sandy Hook. PBS NewsHour. Published March 2, 2018. https://www.pbs.org/newshour/politics/ nra-has-backed-most-state-gun-lawspassed-since-sandy-hook
4. Centers for Disease Control and Prevention. FastStats. CDC. Published October 11, 2019. https://www.cdc.gov/nchs/fastats/ liver-disease.htm
5. National Council for Mental Wellbeing. Study Reveals Lack of Access as Root Cause for Mental Health Crisis in America. National Council for Mental Wellbeing. https://www.thenationalcouncil. org/news/lack-of-access-root-cause-mental-health-crisis-in-america/#:~:text=Mental%20health%20services%20in%20 the
6. Harvard Injury Control Research Center. Overall. Harvard Injury Control Research Center. Published August 27, 2012. Accessed February 2, 2024. https://www. hsph.harvard.edu/hicrc/firearms-research/overall/#:~:text=The%20overall%20firearm%20death%20rate
7. AAFP. Gun Violence, Prevention of (Position Paper). aafp.org. Published 2018. https://www.aafp.org/about/policies/all/ gun-violence.html
8. CDC. Funded Research. cdc.gov. Published 2020. https://www.cdc.gov/violenceprevention/firearms/funded-research. html
Author Biography
Samuel Yeboah-Manson is a freshman at Hopkins majoring in Public Health and Molecular and Cellular Biology. He is particularly interested in the social determinants of health and healthcare policy. Outside of his academics, Samuel is an avid reader and enjoys spending time with friends and family.
21
Jay Rembert/Unsplash
Revolutionizing Healthcare: A Proactive and Patient-Centric Approach to Preventable Chronic Conditions
Jayvik Joshi
Almost half of all adults, 117 million Americans, suffer from preventable chronic conditions that can be linked to poor diet and lifestyle choices.1 These conditions not only diminish quality of life, but account for more than 85% of all health care costs,2 which for the US is almost double per capita compared to other developed countries.3 This epidemic demands an urgent need for a comprehensive approach to address the root cause of these chronic issues.
The solution lies in moving away from our reactive system to a proactive and personalized approach. Although most individuals resort to life-saving medical interventions, maintaining a healthy lifestyle through adequate nutrition and physical activity could at times prevent the very diseases we seek out to treat. New technologies aiming to tackle these problems have also begun to signal a paradigm shift towards patient-centered care, prioritizing long-term well-being over transient treatments.
Our health hinges on the day-to-day choices we make. Many individuals are raised in environments that overlook the enduring consequences of lifestyle decisions, leading to longterm repercussions. When it comes to addressing conditions like heart disease, obesity, or cancer, it may seem like only miraculous interventions can make a difference. However, the cumulative effect of small lifestyle choices can have a significant impact over time and play a crucial role in preventing potential health complications. Our laxity towards nutrition and lifestyle is demonstrated by concerning realizations. America is littered with food deserts not only contributing to the 1 in 5 children experiencing mal-

nutrition4 but also the rising 42% obesity rate.5 Nearly 60% of the American diet consists of ultra-processed foods linked to obesity, diabetes, and cancer.6 Light physical activity is linked to a 20-30% decrease in all-cause mortality7; however, more than 60% of US adults do not engage in 150 minutes of activity per week likely caused by widespread sedentary lifestyles.8 With recent breakthrough drugs such as Tirzepatide for obesity9 or Lecanemab for Alzheimer’s disease,10 we must not overlook the importance of nutrition and physical activity even when medical interventions are available as options.
Many recent healthcare technology advancements attempt to emphasize proactive, continuous monitoring and personalized care when and where it’s needed. Wearable devices such as an Apple Watch or Fitbit not only track day-to-day activities to encourage physical activity,11,12 but also enable early detection of complications such as cardiovascular irregularities.13 DexCom’s continuous glucose monitoring systems allow for close tracking for diabetic patients.14 These solutions allow for continuous feedback, timely intervention, and encourage long-last-
ing habits that compound over time. The recent surge in artificial intelligence has enhanced remote patient monitoring through diet or mental health monitoring apps backed by deep learning models.12 Generative AI, such as ChatGPT, has valuable applications in increasing accessibility of medical information and educating patients on healthcare literacy - ultimately empowering more people to take control of their health.15 Other innovations such as Augmented Reality (AR) and Virtual Reality (VR) demonstrate promising applications in healthcare. Possible applications include personalized rehabilitation exercises for motor skill enhance-
“
” Augmented Reality (AR) and Virtual Reality (VR) demonstrate promising applications in healthcare.
ment, mental health therapy for anxiety and stress management, exposure therapy for phobias and PTSD, and VR-assisted pain management.16 The personalized and remote nature of such technology allows for a seamless integration of treatment into a person’s social and cultural constraints. By embracing these innovations, healthcare has begun to shift away from a “when it’s needed” and “one-size fits all” approach and evolve towards a future that is active and patient-centric.
22
Eiliv Aceron/Unsplash

As technology rapidly integrates into our daily lives, the swift rise of AI and advancement of personalized medicine signifies a profound shift in the fundamental roots of our healthcare system. The emergence of these solutions underscores a commitment to continuous feedback, personalization, and a point-of-care approach, offering a substantial enhancement in the overall quality of life. A focus on the accumulative effect of healthy lifestyle choices as a mode of disease prevention rather than a reliance on therapeutic interventions continues to serve as an indispensable, yet commonly forgotten guiding principle. This shared vision not only reshapes healthcare into a proactive partnership between providers and patients but also champions long-term well-being as a central goal.
References
1. Food Is Medicine: A Project to Unify and Advance Collective Action | health.gov. Accessed January 8, 2024. https://health. gov/our-work/nutrition-physical-activity/ food-medicine
2. Holman HR. The Relation of the Chronic Disease Epidemic to the Health Care Crisis. ACR Open Rheumatol. 2020;2(3):167-173. doi:10.1002/acr2.11114
3. U.S. Health Care from a Global Perspective, 2022: Accelerating Spending, Worsening Outcomes. doi:10.26099/8ejy-
yc74
4. Hunger in America | Feeding America. Accessed January 8, 2024. https://www. feedingamerica.org/hunger-in-america
5. Overweight & Obesity Statistics - NIDDK. National Institute of Diabetes and Digestive and Kidney Diseases. Accessed January 8, 2024. https://www.niddk.nih. gov/health-information/health-statistics/ overweight-obesity
6. Steele EM, Baraldi LG, Louzada ML da C, Moubarac JC, Mozaffarian D, Monteiro CA. Ultra-processed foods and added sugars in the US diet: evidence from a nationally representative cross-sectional study. BMJ Open. 2016;6(3):e009892. doi:10.1136/bmjopen-2015-009892
7. Indicator Metadata Registry Details. Accessed January 8, 2024. https://www. who.int/data/gho/indicator-metadataregistry/imr-details/3416
8. Adults | Surgeon General Report | CDC. Accessed January 8, 2024. https://www. cdc.gov/nccdphp/sgr/adults.htm
9. Wadden TA, Chao AM, Machineni S, et al. Tirzepatide after intensive lifestyle intervention in adults with overweight or obesity: the SURMOUNT-3 phase 3 trial. Nat Med. 2023;29(11):2909-2918. doi:10.1038/s41591-023-02597-w
10. van Dyck CH, Swanson CJ, Aisen P, et al. Lecanemab in Early Alzheimer’s Disease. N Engl J Med. 2023;388(1):9-21. doi:10.1056/ NEJMoa2212948
11. Ferguson T, Olds T, Curtis R, et al. Effectiveness of wearable activity trackers to increase physical activity and improve health: a systematic review of systematic reviews and meta-analyses. Lancet Digit
Health. 2022;4(8):e615-e626. doi:10.1016/ S2589-7500(22)00111-X
12. Bohr A, Memarzadeh K. The rise of artificial intelligence in healthcare applications. Artif Intell Healthc. Published online 2020:25-60. doi:10.1016/ B978-0-12-818438-7.00002-2
13. Moshawrab M, Adda M, Bouzouane A, Ibrahim H, Raad A. Smart Wearables for the Detection of Cardiovascular Diseases: A Systematic Literature Review. Sensors. 2023;23(2):828. doi:10.3390/s23020828
14. Garg SK, Kipnes M, Castorino K, et al. Accuracy and Safety of Dexcom G7 Continuous Glucose Monitoring in Adults with Diabetes. Diabetes Technol Ther. 2022;24(6):373-380. doi:10.1089/ dia.2022.0011
15. Dave T, Athaluri SA, Singh S. ChatGPT in medicine: an overview of its applications, advantages, limitations, future prospects, and ethical considerations. Front Artif Intell. 2023;6:1169595. doi:10.3389/ frai.2023.1169595
16. Yeung AWK, Tosevska A, Klager E, et al. Virtual and Augmented Reality Applications in Medicine: Analysis of the Scientific Literature. J Med Internet Res. 2021;23(2):e25499. doi:10.2196/25499
Author Biography
Jayvik Joshi is a sophomore studying Biomedical Engineering. My career goals are oriented towards translational research and applications of engineering to medical and public health problems.
23
Michael Dziedzic/Unsplash
Telemedicine: The Future of Patient Consultation
Hyeongmin Cho

Telemedicine has been a rising field in healthcare. The American Medical Association (AMA) notes that telehealth visits and remote patient monitoring increased from 14% to 28% from 2016 to 2020.1 Since the Covid-19 pandemic, it is estimated that about 60-90% of physicians use some sort of telehealth service. Needless to say, telemedicine is becoming a significant part of healthcare, and it has the potential to drastically develop and improve patient access to healthcare in the future.
Telemedicine is the practice of providing remote healthcare to patients, whether that entails going through lab results, providing mental health treatment, or guiding physical therapy. Telemedicine uses relatively less
resources than typical in-person clinic visits.2 Analysis from the National Cancer Institute (NCI) estimates that patients save on average $147 to $186 per visit through using telemedicine.3 Because in-person visits are not required for telemedicine, patients can potentially save time and money on hospital and travel expenses, especially for those living in rural communities or places distant from clinics. Indeed, the same study from the NCI states that patients save about 2.9 hours of driving time and 1.2 hours of in-clinic time per visit when switching to telemedicine.3
However, work is still needed to ensure that telemedicine remains a valid option for healthcare. There are many regulations that disincentivize or dis-
courage healthcare providers from offering telemedicine as an option.1 The initial Public Health Emergency response to COVID-19 had all 50 states waive certain aspects of their state telehealth licensing requirements for physicians.4 However, some states are now discontinuing cross-state licensing waivers, preventing physicians from providing continuity of care to certain populations, such as college students who study in a different state.4 Additionally, obtaining in-state licensure to practice can be associated with fees and lengthy processes, such as an estimated 60-day wait for all states and all health providers before becoming licensed.4 Still, the AMA has supported the continued use of telemedicine, and there is currently ongoing work to lift restrictions
24
National Cancer Institute/Unsplash

and enable remote care.1 For instance, some states have broadened crossstate licensure by recognizing licenses in other states, and multi-state licensure compacts are being utilized to simplify the licensing process in many states through a common application system.4 These compacts enable certain healthcare providers such as physicians, nurses and speech therapists to continue telemedicine in other states as long as they hold licensure in their home state.4
“Public trust and satisfaction with telemedicine are high.
”
Access to telehealth has increased in recent years, with Medicare now accepting rural emergency hospitals as eligible sites for telemedicine.5 However, there are concerns that the lack of in-person interactions may increase the difficulty in building trust and comfort in patient-physician relationships.2 Still, case studies performed during the pandemic in major metropolitan areas, such as Los Angeles, have demonstrated that public trust
and satisfaction with telemedicine are high, about 47% for study participants, suggesting the validity of telehealth as a future avenue of healthcare.6
Overall, there is much optimism about the future of telemedicine in healthcare. The convenience afforded by telemedicine has allowed physicians and other healthcare workers to provide care and maintain communication with many patients who were medically or socially unable to visit clinics.2 A remote patient monitoring system may serve as a safety net for many patients, especially for the elderly or those living in hospice care who may have a harder time visiting clinics but still need regular care.2 Furthermore, the low-resource nature of telemedicine offers a financial incentive for both providers and patients seeking care, as costs may often be lower than in-person care.2 In fact, due to such advantages, a local Baltimore hospital, MedStar Union Memorial Hospital, is currently offering telemedicine as an affordable and accessible alternative to in-person care. Eventually, telemedicine may assist in providing primary care and help patients with chronic conditions that need regular monitoring and care.2 Telemedicine is becoming increasingly relevant in the public health and healthcare sector, and has the potential to revolutionize and improve patient care.
References
1. Strazewski L. Telehealth’s post-pandemic future: Where do we go from here? American Medical Association. Published September 7, 2020. https://www.amaassn.org/practice-management/digital/ telehealth-s-post-pandemic-futurewhere-do-we-go-here
2. Jin MX, Kim SY, Miller LJ, Behari G, Correa R. Telemedicine: Current Impact on the Future. Cureus. 2020;12(8):e9891. doi:https://doi.org/10.7759/cureus.9891
3. Winstead E. Telehealth Can Save People with Cancer Time and Money - NCI. www. cancer.gov. Published February 16, 2023. https://www.cancer.gov/news-events/ cancer-currents-blog/2023/telehealthcancer-care-saves-time-money
4. Department of Health and Human Services. Getting started with licensure | Telehealth.HHS.gov. telehealth.hhs.gov. Published 2023. https://telehealth.hhs. gov/licensure/getting-started-licensure
5. Department of Health and Human Services. Telehealth policy changes after the COVID-19 public health emergency | Telehealth.HHS.gov. telehealth.hhs. gov. Published August 31, 2023. https:// telehealth.hhs.gov/providers/telehealthpolicy/policy-changes-after-the-covid-19public-health-emergency
6. Orrange S, Patel A, Mack WJ, Cassetta J. Patient Satisfaction and Trust in Telemedicine during the COVID-19 Pandemic (Preprint). JMIR Human Factors. 2021;8(2). doi:https://doi. org/10.2196/28589
Author Biography
Hyeongmin Cho is a second-year undergraduate studying Molecular and Cellular Biology. He is particularly interested in health disparities, especially those found in the healthcare costs and health insurance. Using his love for writing, he hopes to contribute towards disseminating public health knowledge through writing as an editor for Epidemic Proportions.
25
National Cancer Institute/Unsplash
The Impacts of Climate Change on the Future of Public Health
Pearl Shah
Despite being an ever-present and looming threat for the past few decades, we have only recently started to get a glimpse of the long-term consequences climate change might have on our everyday lives. These effects manifest in a variety of ways, from extreme weather conditions to changes in food safety, threatening to change the ways we experience the world around us. In fact, climate change is estimated to cause a staggering 250,000 deaths between the years 2030 and 2050.1 This will mean large changes in the state of public health and the healthcare system as a whole.
Firstly, an increase in average temperatures will result in more frequent heatwaves, especially in the summer. This is particularly concerning for regions with infrastructure lacking air conditioning or ventilation, which are not equipped to handle such conditions. Heat exposure impacts include dehydration, heat cramps, heat strokes, increased cases of food and waterborne diseases, and the development of chronic diseases, such as respiratory, cardiovascular, and renal disease. Moreover, higher temperatures raise storage concerns for drugs, as it could make certain medications less effective or have adverse side effects.2
Climate change and the activities that contribute to it also lead to changes in air composition through an increase in the abundance of certain gases, allergens and particulate matter.3 Warmer temperatures have the effect of increasing ground-level ozone, which causes respiratory issues by harming lung tissue and impairing lung function. Changes in the timing and the length of pollen season due to warmer spring temperatures, like that of ragweed, increase allergens present in the environment. Further-
more, the inhalation of particulate matter produced by human activities, such as burning fossil fuels or wildfires, has shown to cause an increase in lung cancer and cardiovascular diseases. These factors come together to demonstrate how the worsening of air quality via climate change can have various health implications.
In addition, changes in temperature and weather have led to more cases of vectorborne diseases by allowing disease vectors to be active across larger regions for longer periods of time. For example, with rising temperatures, ticks carrying Lyme disease have been able to move northward and become active for a longer season.3 As warmer temperatures favor the growth of pathogens, microbial contamination of food and water can result in gastrointestinal issues and nutritional deficiencies. Flooding caused by extreme precipitation and rising sea levels can also cause heavy metal and chemical contamination of water bodies used for drinking or harvesting crops. Additionally, rising carbon dioxide levels have been shown to lower nutrition levels in food, such as decreasing protein and mineral levels.4
Extreme weather conditions, ranging from excess precipitation to droughts, will have long-term impacts on healthcare provision both during and after the incident. Specifically, extreme weather conditions often hinder access to basic resources by decreasing the availability of uncontaminated food and drinking water. These conditions also damage infrastructure, including roads and power lines, for transport and communication needed to gain access to healthcare facilities, such as pharmacies and hospitals. Supply chain disruptions could likewise occur due to the inability to produce and distribute medical supplies. Possible power outages es-
pecially threaten patients who require constant care, such as those on life support that dependent on electricity.
In conclusion, climate change is projected to have many adverse effects on public health - a reality we must begin to anticipate and prepare for. However, despite the seemingly morbid glimpse of the future, there is a big opportunity to adapt and prevent these repercussions. The healthcare industry itself is a major contributor to this phenomenon through its resource-intensive and waste-generating nature, and it is something we must begin to work on to change.
References
1. World Health Organization . Climate Change. Published October 30, 2021. Accessed February 8, 2024. https://www. who.int/news-room/fact-sheets/detail/ climate-change-and-health
2. World Health Organization. Heat and Health. World Health Organization. Published June 1, 2018. https://www. who.int/news-room/fact-sheets/detail/ climate-change-heat-and-health
3. United States Environmental Protection Agency. Climate Impacts on Human Health. climatechange.chicago.gov. Accessed January 7, 2024. https://climatechange.chicago.gov/climate-impacts/ climate-impacts-human-health#:~:text=Climate%20change%20can%20 affect%20human
4. USGCRP. The Impacts of Climate Change on Human Health in the United States: A Scientific Assessment. Globalchangegov. Published online 2016:1-312. https://health2016.globalchange.gov/
Author Biography
Pearl Shah is a freshman majoring in Molecular and Cellular Biology. She is also interested in the environmental sciences and its related issues, which is something she aims to spread more awareness about through her writing. Outside of Hopkins, she enjoys painting and reading.
26

27
Tobias Rademacher/Unsplash
A Case Study on How a Country’s Dependence on Tourism Can Affect Its Healthcare System: Thailand
Sittha Cheerasarn
Summary
This article dives into the intricate interplay between Thailand’s burgeoning and prosperous tourism industry and its healthcare system, focusing on the profound impacts of tourism on rural healthcare disparities. Despite Thailand’s commendable strides in healthcare distribution, rural regions continue to face a progressively severe shortage of medical professionals, exacerbating the already stark urban-rural healthcare divide. The rise of medical tourism, while contributing significantly to Thailand’s economy, has also inadvertently strained the healthcare infrastructure, leading to increased medical fees and disparities in access to quality care for the middle to lower class. Medical tourism has also fueled a lucrative opportunity that has led physicians to transition from the public to private sector. The article explores the government’s attempts to address these issues, including reforms in healthcare education and the implementation of universal healthcare coverage. However, funding disparities between medical tourism and universal healthcare remains a persistent problem. As the COVID-19 pandemic began to reveal the reality of Thailand’s economy and healthcare system, the article underscores benefits and vulnerabilities of the dependence on tourism on the healthcare system.
Introduction/Background
As a Thai-American, I have had the opportunity to observe and develop a detached perspective on how Thailand operates. Thailand’s GDP per capita is mainly concentrated in two regions: Bangkok and the Eastern Re-

gion.1 The GDP per capita in these two regions is approximately twice as much as the average for all of Thailand (7 regions consisting of 76 provinces). These numbers show how important these two regions are to Thailand’s economy. One of the regions, Bangkok, is one of the largest cities in Asia, serving as the commercial center of Thailand and the rest of Southeast Asia.2 Bangkok is also the second most visited city in the world with 21.2 million visitors annually, which is the main reason why the region contributes immensely to the nation’s GDP.3
As a major hotspot for tourism worldwide, tourism has developed into the main source of revenue for the country, with regions with the highest GDP per capita corresponding to the most visited regions. The unequal revenue distribution among regions has driven widespread health inequality in Thailand. The consequences of an overreliance on tourism can be seen in the unequal distribution of medical resources toward rural areas. This article will analyze the Thailand health system, the disadvantages to those in rural areas, these attempts at address-
ing the inequalities, and how overreliance on tourism can lead to dangerous outcomes in the scope of public health.
Rural Disparities
Unlike the US, Thailand has a universal healthcare system which provides healthcare coverage to 99.9% of the population. But as it strives to improve its outreach and ability, the healthcare system is facing challenges caused by a shortage of doctors and nurses, especially in rural areas.4 In 2001, the universal healthcare system was implemented where healthcare was provided through a tiered system of public providers: large regional hospitals with a comprehensive set of specialists, smaller hospitals with capacities ranging from 200 to 250 beds, and community health centers focused on providing primary care in more rural areas. Thailand has committed to the teaching and training of thousands of medical professionals per year. Most physicians are required to graduate from a university and spend three years working at a state-run hospital, usually in a rural area.4 Even with
28
David Gardiner/Unsplash
these measures, these rural areas can not obtain enough doctors to meet the healthcare demand.
In Bangkok there is one doctor for every 850 people, while in the country’s rural northeast provinces there is just one doctor for every 5,308 people.4 There are a couple of reasons for this shortage, and one of the main reasons revolve around incentives indirectly linked to tourism. A lot of Thailand’s medical innovation and technology is located in the most visited regions in Thailand due to medical tourism. This sector of the Thai economy is crucial, which in turn has led Thailand to focus on how to improve and adhere to the interests of medical tourists. This has resulted in not only medical technology being concentrated in areas that have heavy tourism, but also the prioritization of tourists over local residents by physicians, leading to disparities in access to healthcare services. As described, doctors in Thailand have become so busy with foreigners that Thai patients are having trouble getting care.5
“
” Thai patients are having trouble getting care.
Another consequence of the booming medical tourism sector is that there is a lack of family physicians being trained in specialties essential to rural areas such as primary care and family medicine. Instead, a lot of physicians are training to pursue more financially lucrative specialties such as cardiology and neurology, with the intention of working in the private sector.4 This is correlated with the cultural norms in Thailand.6 As a Thai-American with the aspirations of becoming a physician, I am familiar with the culture in Thai families to empha-
size the importance of higher-paying specialties like neurology, orthopedic surgery, and so on. To add-on, I have many family friends that earned a medical degree in Thailand and have immigrated to the US because of the allure, pay, and cultural notions of success in a first-world country. In fact, it has been shown that pay at public hospitals is significantly less than at private hospitals.5 According to Siripanumas et al., about 33.9% of Thailand physician respondents reported not being satisfied with net income, while only 19.0% felt satisfied.7 Thus, many Thai physicians since the Vietnam War have left in droves to work in the US to earn more money or have entered the private sector.
Thailand is working to address this gap through a series of healthcare education reforms such as training future doctors by seeking out high-performing students already living in rural areas and offering them scholarships to remain. Though as it stands, according to Thailand’s Minister of Public Health, Thailand needs about 9,000 more doctors and 43,000 more nurses to address the rural shortages.4
Medical Tourism
Thailand’s healthcare system is facing a critical test amidst the rise of medical tourism. As the government looks to attract ever higher numbers of overseas patients, there are concerns that access to healthcare for its own population of 67 million may worsen.
Medical tourism adds an estimated 0.4% to Thailand’s economy every year, which raises the income for the medical services sector.8 Medical tourism has had various positive effects, including a higher standard of medical hardware in the best private hospitals.9 In the year 2022, Thailand imported $2.7 billion in medical devices, which correlate with the increase in tourism.9 However, Thailand’s medical tourism drive is also causing a growing disparity in healthcare access. This comes in the form of both a
shortage of physicians and an increase in medical fees for self-paying Thais. For those who rely on basic government health plans, which make up more than 80% of the population, staffing levels in state hospitals are being undermined by the private sector.8
There are many reasons why medical tourism all over the world is a booming industry. Healthcare in countries like the US is extremely expensive, especially among those who do not have health insurance. According to a study, the average medical tourist can expect to save 25% to 75% on various procedures and treatment options. While a heart bypass surgery in the US costs $113,000, it is nearly 9 times less in Thailand, where it only costs $13,000. A facelift costs up to $15,000 in the US, but can be as low as $3,000 in Thailand.9 Furthermore, there are countries like the UK, where free treatment can actually cause a backlog of patients seeking treatment for non-threatening conditions. This causes tourists to seek other countries that provide the treatments needed. Thailand is well-positioned for these tourists, with doctors who are welltrained in the latest treatments and hospitals that are outfitted with cutting-edge technology.10 Overall, medical tourism is a very lucrative business which results in Thailand redirecting resources and money to profit from it.
The Attempt to Fix this Issue
Implemented in 2001, the universal healthcare coverage (UHC) system in Thailand has proven to be somewhat effective on paper. The benefits of this system includes general medical care and rehabilitation services, high-cost medical treatment, and emergency care.11 Implemented to benefit people of low income, the UHC scheme was introduced as “30 baht cures all diseases.” The 30-baht scheme, the equivalent of playing one dollar in Thai currency, insures approximately 48 million of Thailand’s 69 million population healthcare. Employers or the civil servants medical benefit
29

scheme insures the remaining population. Given that the 30-baht is only a little bit less than a dollar, it is certainly imaginable that this system would be exploited. However, studies have shown that utilization of UHC among beneficiaries in Thailand is only at 40%. Those who can afford other healthcare plans and private hospitals tend to not utilize UHC. Usage among low-income, older and female groups is much higher – indicating that UHC has in some ways lived up to its propoor and pro-vulnerable agenda.11 However, the funding for this program is quite large and has required help from another sector of the economy: tourism.
A dual-track plan was previously proposed as a holistic approach toward healthcare policies. The first track was the 30-baht healthcare plan, and the second was a program to promote Thailand as a hub for medical tourism. The intended outcome was to use some of the income generated from medical tourism to fund the 30-baht healthcare plan. As it turns out, this original plan did not go as planned. The medical tourism industry enjoyed double-digit growth rates, though very little of this has gone to
funding universal healthcare. 77% of funding for UHC comes from the public sector, while already limited contributions from the private sector are declining year-on-year.
In the 1990s, the private sector’s share of hospitals was 10%. It has now reached extreme proportions as the share of private sector hospitals has increased to 54% as of 2019, with doctors drawn away from district hospitals by incentives like higher pay and greater social mobility.12 With the increasing shares of private sector hospitals, public sector hospitals, like those seen in rural areas, have had to adapt by cutting costs even more. Thus, they use cheaper medicine and keep wages for medical staff low. This only increases the gap between public and private healthcare.
Even though the UHC is ‘free’, the budget for this program has been significantly reduced. Most of the remaining budget was concentrated in urban areas or at hospital operators that had good relationships with the central government, while rural operators were left with little. As Chia et al. states, “the budget goes where people are, and then healthcare access follows”.11 There have been many at-
tempts to expose these UHC schemes. There has been the emergence of an intense movement of bureaucrats and doctors against UHC. Some of them joined the “whistle street protests” of the People’s Democratic Reform Committee in 2013-14. They complained to the military government that the NHSO was poorly managing the UHC budget and causing hospitals to have financial deficits.
Conclusion
Tourism is a big contributor to the Thailand economy, and its benefits have caused damage to rural health. Though, there has also been a lot of awareness regarding this issue among officials and the public. One instance of the government acting on this awareness is when they implemented a scheme that provides identity cards to over 11.4 million registered people who can show their cards to get free transport and commodities valued at 300 baht per month for each beneficiary. This is one of the steps into implementing more programmes to help the poor. Thailand’s UHC has even shown resilience in the hardest of challenges to healthcare systems around the world. Thailand has been internationally praised for avoiding a
30
Bharath Mohan/Unsplash
COVID-19 disaster because the country saw significantly lower deaths and confirmed cases compared to many other countries.13 Even though Thailand’s healthcare system held up well, Thailand’s tourism economy reported results of -100%.14 With such a huge dependence on tourism, this result was devastating for the economy and the healthcare sector. Even though the country saw lower deaths, many speculate that this could be a result of under-reporting cases, cultural norms of mask wearing, and social distancing. In reality, the shortage of specialists, in particular intensive care nurses and critical care experts, became evident at the peak of the pandemic.13 Overall, the effects of COVID-19 have proven to be detrimental.14 Even though the economy has experienced a significant recovery since COVID-19, the economy and healthcare system remains fragile, and is in danger of collapsing if there was ever to be another pandemic.
Apart from the potentially damaging effects on the healthcare system, availability of physicians in rural areas remains a huge issue. Thailand must focus on continuing to emphasize the need for rural areas to keep a steady number of available physicians and nurses. The government could implement policies to increase the wages of physicians in rural areas. Furthermore, I believe implementing higher wages for family medicine physicians will not only minimize the effects of another pandemic, but it will also create a cohort of family medicine physicians available for rural areas. This is a big challenge for Thailand to face in the upcoming years; but if there is a country under this model that can overcome these difficulties, Thailand is the prime candidate. Not only have existing educational institutions shown positive results, medical tourism has also proven to have some benefits, such as bringing a lot of revenue that can be redirected into other sectors. Through comprehensive reforms and strategic investments, Thailand
can navigate the complex dynamics between tourism and healthcare to ensure equitable access to quality healthcare for all its citizens.
References
1. ThaiWebsites. Regions - GDP. ThaiWebsites. https://www.thaiwebsites.com/regions-GDP.asp. Accessed February 11, 2024
2. Bangkok’s Economy. Economy of Bangkok (Thailand). http://www.asianinfo.org/ asianinfo/bangkok/economy_of_bangkok.htm. Accessed February 6, 2024.
3. 54+ Thailand Travel & tourism statistics [fresh for 2024!]. RSS. https://www. dreambigtravelfarblog.com/blog/thailand-travel-tourism-statistics#:~:text=billion%20Thai%20baht.-,At%20a%20 glance%3A%20Thailand%20travel%20 and%20tourism%20statistics,from%20 January%20to%20August%202023. Accessed February 6, 2024.
4. Thailand seeks to address shortage of rural health care providers. News. May 11, 2015. https://www.hsph.harvard.edu/ news/features/thailand-seeks-to-addressshortage-of-rural-health-care-providers/. Accessed February 6, 2024.
5. Hamilton J. Medical Tourism Creates Thai Doctor Shortage. NPR. https://www. npr.org/2007/11/29/16735157/medical-tourism-creates-thai-doctor-shortage. Published November 29, 2007; Accessed February 11, 2024.
6. Seangrung RCP. Factors affecting the rural retention of medical graduates in Lower Northern Thailand. J Med Assoc Thai. 2017;100:692.
7. Siripanumas C, Suphanchaimat R, Nittayasoot N, Sawaengdee K. Distribution of Physicians to Public Health Facilities and Factors Contributing to New Medical Graduates Serving in Public Facilities, 2016-2020, Thailand. Risk Manag Healthc Policy. 2022;15:1975-1985. Published 2022 Oct 27. doi:10.2147/RMHP.S384507
8. Finch S. Medical tourism driving health care disparity in Thailand. Canadian Medical Association Journal. 2013;186(1). doi:10.1503/cmaj.109-4658
9. Thailand - Medical Devices and Technology. International Trade Administration | Trade.gov. https://www.trade. gov/country-commercial-guides/thailand-medical-devices-and-technology#:~:text=The%20average%20medical%20tourist%20can,low%20as%20 %243%2C000%20in%20Thailand. Accessed February 6, 2024.
10. Thakral S. Pacific Prime. Thailand Medical Tourism. Pacific Prime. https://www. pacificprime.co.th/blog/thailand-medical-tourism/. Published September 20, 2023; Accessed February 11, 2024.
11. Chia J. The history of Thailand’s universal healthcare coverage, and its uncertain future. Thai Enquirer. April 24, 2020. Accessed February 6, 2024. https:// www.thaienquirer.com/12090/the-history-of-thailands-universal-healthcare-coverage-and-its-uncertain-future/.
12. Limited BPPC. Health Care on Life Support. https://www.bangkokpost.com. https://www.bangkokpost.com/thailand/ special-reports/1367099/health-care-onlife-support. Accessed February 6, 2024.
13. Durongkaveroj, Wannaphong. Lifting the veil on Thailand’s covid-19 success story. East Asia Forum. December 7, 2023. https://eastasiaforum.org/2020/08/06/lifting-the-veil-on-thailands-covid-19-success-story/. Accessed February 6, 2024.
14. Thailand after covid-19 prepare to get through the Economist’s perspective. part 1: The impact of the economy and the Thai labor market. (SCB). https://www. scb.co.th/en/personal-banking/stories/ business-maker/thailand-after-covid-ep1. html#:~:text=The%20situation%20of%20 COVID%20and,the%20tourism%20business%20slowly%20recovering. Accessed February 6, 2024.
Author Biography
Sittha Cheerasarn is a freshman premed majoring in Mechanical Engineering. He is pursuing the biomechanics track with a minor in computer-integrated surgery. As a member of the Thai community, Sittha is deeply committed to the preservation and spread of Thai culture. He hopes to enter the biotechnology industry to tackle healthcare inequality around the world.
31
A Gift of Fire: Guiding the AI-driven Healthcare Revolution for a More Equitable Future
Annie Huang Summary
This editorial examines the role of artificial intelligence (AI) in healthcare, a field where it has become a significant driving force. It establishes AI as a “gift of fire” with the potential to create a safer, more equitable future for healthcare but also become a source of danger. The editorial argues for a balanced understanding of AI’s role in healthcare and emphasizes the need for informed public discourse and responsible technology use.
A Gift of Fire: Guiding the AI-driven Healthcare Revolution for a More Equitable Future
As a staff editor for the SciTech section of The News-Letter, I have had the good fortune of attending a series of guest lectures and interviewing graduate students and professors from various labs. Although I anticipated hearing distinct perspectives from various engineering disciplines, I was struck by a recurring theme across every lecture and interview – the pervasive influence of Artificial Intelligence (AI). Contrary to the common perception of AI as an immature technology primarily focused on text generation and mimicking human interactions, I discovered that AI has already revolutionized the landscape of research. It was particularly intriguing to discover its extensive role in state-of-the-art healthcare technology.
This realization marked a pivotal moment where my interests in computer science and healthcare intersected. Having always been drawn to both fields, this was the first time that I truly pondered the implication of such a convergence. As I dived deeper, I gained a profound understanding of
AI’s role in the healthcare revolution and now present the following insights:
The Dual Nature of AI in Healthcare
The intersection of public health and technology witnessed a pivotal moment during the COVID-19 pandemic when AI played a transformative role in healthcare. With platforms such as COVID-Net for chest X-ray analysis and PathAI for pathology analysis, the impact of AI in enhancing healthcare capabilities during critical periods became clear.1,2,3 Yet, the healthcare community is divided over its implications. In an interview with the Sydney Morning Herald and The Age, Dr. Anthony Fauci discussed the perceived “dangers of artificial intelligence,” believing that if people “look at it under a controlled situation, there are many advantages for artificial intelligence in every aspect of medicine and health”.4 Others, however, remain skeptical, believing that while AI can provide general insights and recommendations, it can never replace the nuanced judgment and empathy that experienced doctors bring to patient care.5
I see AI as a “gift of fire”– a powerful tool with the potential to bring a safer and more equitable future, yet a hazard if used irresponsibly. Its applications range from preventative healthcare to disease prediction, medical diagnosis, and robot-assisted surgeries. However, this advancement is not without its challenges, which include concerns about data security and accessibility. To minimize consequences, the public should be informed of both the advantages and disadvantages of medical AI and should approach this technology with responsible guidance and conscience.
AI in Preventive Healthcare
During my first bioinformatics course in high school, I was introduced to sequencing techniques such as Needleman-Wunsch and Smith-Waterman algorithms, which are classical dynamic programming algorithms that compare and identify similarities and differences between genetic sequences. By comparing the patient’s DNA with standard human genomes, doctors can pinpoint genetic variations that could be associated with genomic-based diseases. This understanding is crucial in developing tailored treatments and preventive healthcare strategies, potentially revolutionizing how we manage and prevent illnesses at the genetic core.6
“
Deep learning grapples with the complexity and “noise” inherent in realworld data.
”
When I arrived at the Johns Hopkins Homewood campus and interacted with computational biology labs, I discovered an increase in alternative use of AI, particularly deep learning, in bioinformatics. Unlike traditional methods that strip away the contexts of problems and simplify them into clear-cut models, deep learning grapples with the complexity and “noise” inherent in real-world data, offering a more nuanced approach to problem-solving.
32

Splice site recognition, one of the key research areas in bioinformatics, has brought this approach to light. The purpose of splice site recognition is to identify junctions of alternative RNA splicing, which is a mechanism that splices exons and introns in different combinations for gene regulation and expression. Traditionally, scientists found these splice sites by aligning sequences directly onto a reference genome. However, these predictions can be inaccurate due to misalignments and “noises” in data. To enhance precision, researchers have turned to machine-learning-based methods that are trained with data from known splice sites in specific species. It has been shown that these newer methods significantly reduce the false positive rate and can achieve an accuracy as high as 96%.7 This enhanced precision has great implications for the detection and prevention of genetic diseases, as a more accurate understanding of genetic variations and mutations could provide methods of intervention for individuals at risk of specific genetic disorders.
Still, this advancement is predominantly driven by large medical companies, making this software often expensive and close-source. In response, academic research communities, like those at Hopkins, are pioneering open-source alternatives, democratizing access to these cutting-edge AI analysis tools. This movement improves accessibility and drives advancement in cost-effective solutions that make healthcare more affordable.
Genomic-based analysis has not been widely adopted as the current diagnostic framework focuses more on therapeutic interventions rather than preventative care. There is a pressing need to shift this paradigm by directing more research and resources toward preventative measures and inclusive medical practices. By training AI models that cater to individual patient profiles, we can advance personalized healthcare and ultimately move toward a more equitable and effective healthcare system that benefits all.
However, an increased reliance on AI in medical diagnostics and pre-
Julien Tromeur/Unsplash
vention also poses several challenges. In recent years, security regarding health records and personal data has emerged as a major concern. As more and more hospitals and clinics transition from physical paperwork to electronic records, even well-guarded systems, like those of major healthcare providers, are not immune to data breaches. Elevance Health Inc., one of the largest health insurance providers, experienced a data breach back in February 2023, which affected over 3 million patients.8 As research in genomics expands rapidly and the amount of genomic data collected exponentiates, safeguarding sensitive personal healthcare information will become even more important. Although regulatory bodies and governments are beginning to address this issue, the measures in place are still inadequate given the pace and scale of current technological advancements.9
AI in Patient Monitoring and Clinical Decision-Making
The integration of patient-reported outcomes (PROs) into healthcare rou-
33
tines, powered by AI, offers a new avenue for predicting disease progression. PROs are data provided directly by patients throughout their healthcare journey that offer insights into their internal experiences.10 By analyzing self-reported data, AI models are adept at detecting changes in a patient’s condition, such as cancer progression, by comparing with a predefined criteria. When anomalies are detected, AI systems can promptly send an alert email to physicians and patients.
PRO’s effectiveness in monitoring patient conditions has already been demonstrated in clinical studies.11
Compared to using traditional checkups such as periodic scans, like CT and PET, and blood tests to monitor patient health and adjust treatment plans, AI’s real-time data analysis based on PROs has been shown to alert physicians to changes in a patient’s condition much sooner. This can potentially improve patient outcomes by enabling more timely adjustments to treatment strategies and extend the median overall survival of cancer patients beyond that of traditional surveillance.
In 2012, the American Society of Clinical Oncology implemented an AI-integrated platform called CancerLinQ that collects and analyzes cancer patient data, including PROs.12 By leveraging AI and machine learning, CancerLinQ identifies patterns across datasets so that oncologists can make more informed decisions on treatment options based on real-world evidence and further develop personalized treatment plans.
Another project initiated by the Memorial Sloan Kettering Cancer Center is a remote monitoring app based on AI and PROs. In a 2020 article published in the Journal of Clinical Oncology, they found that this approach allowed earlier detection of complications and disease progression in cancer patients compared to traditional follow-up methods.13 Ultimately, this AI-remote monitoring method significantly improved survival rates and
reduced hospitalizations by enabling timely interventions based on real-time patient-reported data.
There are, however, several challenges in the full adoption of PROs. The primary concern is the accuracy and reliability of self-reported data, which may hinder accuracy in the predictive model trained on those data. A lack of standardized PRO measures and interoperability standards also hinders data sharing and integration across different healthcare systems. To promote their use, standardized PRO measures, education of healthcare professionals on the benefits of PROs, and the development of user-friendly and secure interfaces for data sharing should be implemented in the future. The efforts will undoubtedly require the coordinated action of medical professionals, policymakers, and patients.
AI in Medical Diagnosis
AI’s role in medical diagnosis is increasingly evident. AI’s data-driven decision-making process currently allows for accurate and real-time medical image analysis and provides healthcare professionals with valuable insights beyond basic statistical analyses.
cate the concept of “collective insights” for different medical image modalities, such as CT scans, ultrasounds, and MRI.15 Collaborative analysis, typically consisting of expert panels, yields more diverse accurate diagnoses than the judgment of a single expert. AI can now emulate this decision-making process by generating alternative explanations to a single set of imaging data or consolidating earlier findings of doctors.
AI in medical imaging is evolving to replicate the concept of “collective insights”.
“ ”
Medtronic, a billion-dollar biotech company, has pioneered the use of AI for early cancer screening with its GI Genius intelligent endoscopy module.14 With greater accuracy in identifying seizures, a major symptom of colon cancer, the technology scans every frame in real time and locates up to 50% more cases of colon cancer.
Beyond individual diagnoses, AI in medical imaging is evolving to repli-
Besides mimicking the holistic evaluation of human expertise, this method has the potential to democratize healthcare provision, particularly benefiting remote or underserved areas where medical resources are limited. By granting access to the expertise contained within large datasets, patients in areas where on-site medical professionals are scarce can now access the same level of medical guidance as those in more developed regions. Through AI-driven diagnosis platforms, patients could receive advice, diagnoses, and treatment plans from anywhere and be directed to appropriate healthcare resources if needed. These platforms, once widely adopted, could also optimize resource allocation. By analyzing data patterns, healthcare providers could efficiently allocate medical staff and resources in areas most in need and manage drug inventory, thereby improving overall healthcare accessibility.
Still, due to a lack of available data to train machine learning models due to patient confidentiality,15 the deployment of AI in medical applications is slower when compared to other healthcare fields. Collaborations focusing on collecting and sharing data ethically and securely and between healthcare institutions and researchers should be incentivized to fuel the development of AI models.
34

AI in Robot-Assisted Surgery (RAS)
Robot-assisted surgery (RAS) is undergoing significant transformations with the integration of AI, a field where my previous research at Hopkins’s medical robotics lab provided first-hand insights into this evolution. RAS offers numerous advantages over traditional surgery, such as accuracy, reduced risk of complications, and shorter recovery times.16 However, the lack of haptic feedback when controlling a robotic instrument, which is inherent in traditional surgery, could be disorienting for surgeons and limit their abilities to perform delicate tasks. To resolve this issue, deep learning models are being developed to simulate tactile sensations, providing a more intuitive and responsive surgical experience.17
Currently, full teleoperation is employed in RAS due to FDA regulations that ensure every aspect of the surgery depends on the surgeon’s control. Recent research in medical robotics has focused on enabling systems to perform basic surgical tasks autonomously. This could significantly enhance the efficiency of RAS, reduce the cognitive load on surgeons and allow for more complex surgical procedures to be performed with robotic assistance.18 AI could provide the platform to assist in complex tasks like reconstructing the shape of blood clots,
planning optimal surgical paths, and providing real-time guidance to the medical team, thereby improving the quality of care and surgical experience for patients.
Concerns arise about the accountability of software failures when using AI in life-critical equipment. Having conducted research in the field of RAS, I believe that stakeholders will need to grapple with the tradeoffs between innovation and safety, especially as many novel concepts are still at a stage of experimentation. The current FDA approval process, often taking months to years, is intended to keep unsafe products off the market to protect the public, who may have insufficient understanding of potential risks. However, this arduous process can also disincentivize companies from inventing new technologies that are life-enriching and even lifesaving.
Accessibility remains a pressing issue. In a cross-sectional study that analyzed the proportion of outpatient procedures with robotic assistance across facility types and patient populations, it was found that the proportion of visits with robotic assistance was higher for patients with private insurance and visiting private for-profit hospitals than the rest.19 As RAS remains relatively uncommon in ambulatory surgery settings as well, the integra-
tion of AI into RAS will likely alleviate this phenomenon by reducing the anticipated increase in expense that will leave underserved communities with less access. To further bridge this gap, existing insurance coverage should be expanded to include RAS to benefit patients beyond those who can afford private insurance and visit for-profit hospitals.
Challenges and Caveats
The rise of AI in healthcare brings several challenges. One study has shown that intraoperative video monitoring may potentially undermine a surgeon’s undertaking when doctors who disagree with AI recommendations could face legal consequences if proven wrong in retrospect.5 Additionally, concerns surround the accuracy of medical advice from AI, which remains largely unverified due to the “black box” nature of neural networks that lack a transparent understanding of how AI systems arrive at their decisions.20 To address this challenge, researchers are working on developing “explainable AI” to enhance the interpretability of AI models.
Personally, the implication of medical AI has evoked mixed feelings. I experienced an underlying apprehension about a future where doctors, overshadowed by AI, are no longer needed. Yet my computer science background ignites enthusiasm with each advancement in AI technology. This complex interplay between technological and traditional healthcare is also prevalent in society.
It’s becoming clear that a future dominated solely by AI in healthcare is unlikely, and that total reliance on AI is often disastrous. Baidu, China’s largest search engine, was accused of misleading a college student into following the wrong cancer treatment, ultimately causing his death.21 As it turned out, the guidance that the student followed appeared first in his Internet search not because it was the best medical option; rather,
35
Marcel Scholte/Unsplash
it was because the sponsor had paid for it. This poses similar questions as to whether AI should be accepted in lieu of human judgment. Protecting public interests as well as ensuring the credibility of information retrieved to obtain legitimate results in life-critical situations is paramount. Indeed, when it comes to medical applications, AI works best alongside humans, not in place of humans.
Conclusion
The dual nature of AI in healthcare presents both opportunities and challenges. It has the potential to revolutionize patient care, improve accessibility, and bridge public health disparities. Nonetheless, responsible guidance is essential to realize its full potential. Collaboration between policymakers, healthcare professionals, and technology experts is crucial to drive ongoing research and to develop dedicated policy support.
As technology continues to evolve, the pressing question becomes not, “can we do it?” but rather, “should we do it?” The answer to this “gift of fire” of AI lies in discovering the delicate balance between technology and human expertise to ensure the best possible care for patients.
References
1. Coursera. AI in health care: Applications, benefits, and examples. Coursera website. https://www.coursera.org/articles/ai-inhealth-care. Updated 2023. Accessed October 15, 2023.
2. Centers for Disease Control and Prevention. COVID-NET Overview and Methods (2023). https://www.cdc.gov/coronavirus/2019-ncov/covid-data/covid-net/ purpose-methods.html. Accessed January 11, 2024.
3. PathAI. Improving Patient Outcomes with AI-Powered Pathology. https://www. pathai.com/. Accessed January 11, 2024.
4. Thomson A. Anthony Fauci on Australia’s COVID response, AI and the next pandemic. July 27, 2023. Available from: https://www.smh.com.au/national/anthony-fauci-on-australia-s-covid-responseai-and-the-next-pandemic-20230727p5drm8.html. Accessed October 15, 2023.
5. Siegel M. Will AI replace your doctor? As a physician, I’m worried new tech will hurt patient care. April 17, 2023. July 27, 2023. Available from: https://www. usatoday.com/story/opinion/2023/04/17/ ai-chatgpt-impact-health-care-patients/11656662002/. Accessed October 15, 2023.
6. Gonzaga-Jauregui C., Lupski J. R., Gibbs R. A. (2012). Human genome sequencing in health and disease. Annual review of medicine, 63, 35–61. https://doi.org/10.1146/ annurev-med-051010-162644. Accessed January 1, 2024.
7. Chao K-H, Mao A, Salzberg S. L., Pertea M. (2023). Splam: a deep-learningbased splice site predictor that improves spliced alignments. bioRxiv. https://doi. org/10.1101/2023.07.27.550754. Accessed January 1, 2024.
8. Console RJ. Elevance Health flexible benefit plan experiences third-party data breach following NationsBenefits ransomware attack. JD Supra website. https://www.jdsupra.com/legalnews/elevance-health-flexible-benefit-plan-1594932/. Updated 2023. Accessed October 27, 2023.
9. National Human Genome Research Institute. Privacy in genomics. Genome. gov website. https://www.genome.gov/ about-genomics/policy-issues/Privacy. Updated 2021. Accessed November 1, 2023.
10. 10. Quittner AL, Nicolais CJ, Saez-Flores E. Integrating patient-reported outcomes into research and clinical practice. Kendig and Chernick’s disorders of the respiratory tract in children. 2019:231-240.e3. doi: 10.1016/B978-0-323-44887-1.00013-4.
11. Denis F, Lethrosne C, Pourel N, et al. Randomized trial comparing a web-mediated follow-up with routine surveillance in lung cancer patients. J Natl Cancer Inst. 2017;109(9). Accessed October 15, 2023. doi: 10.1093/jnci/djx029.
12. George W. Sledge et al., CancerLinQ and the Future of Cancer Care. Am Soc Clin Oncol Educ Book 33, 430-434(2013). DOI:10.14694/EdBook_AM.2013.33.430
13. Robert Michael Daly et al., Pilot program of remote monitoring for high-risk patients on antineoplastic treatment. JCO 38, 2027-2027(2020). DOI:10.1200/ JCO.2020.38.15_suppl.2027
14. GI genius™ intelligent endoscopy module. Medtronic website. https://www. medtronic.com/covidien/en-us/products/ gastrointestinal-artificial-intelligence/ gi-genius-intelligent-endoscopy.html. Updated 2023. Accessed October 15, 2023.
15. Rahman A, Valanarasu JMJ, Hacihaliloglu I, Patel VM. Ambiguous medical image segmentation using diffusion models. CVPR. 2023:11536-11546. https://doi. org/10.48550/arXiv.2304.04745.
16. Bryant A, Wei B, Veronesi G, Cerfolio R. 28 - robotic surgery: Techniques and results for resection of lung cancer. In: Pass HI, Ball D, Scagliotti GV, eds. IASLC thoracic oncology (second edition). Philadelphia: Elsevier; 2018:283-288.e1. https:// www.sciencedirect.com/science/article/ pii/B978-0323523578000287. 10.1016/B9780-323-52357-8.00028-7.
17. Saracino, A., Deguet, A., Staderini, F., Boushaki, M. N., Cianchi, F., Menciassi, A., & Sinibaldi, E. (2019). Haptic feedback in the da Vinci Research Kit (dVRK): A user study based on grasping, palpation, and incision tasks. The international journal of medical robotics + computer assisted surgery: MRCAS, 15(4), e1999. https://doi.org/10.1002/rcs.1999. Accessed January 1, 2024.
18. Bodenstedt S, Wagner M, Müller-Stich BP, Weitz J, Speidel S. Artificial Intelligence-Assisted Surgery: Potential and Challenges. Visc Med. 2020;36(6):450-455. https://doi:10.1159/000511351. Accessed November 1, 2023.
19. Fingar KR, Stocks C, Gibson TB, McDermott KW, Pickens G, Utter GH, Karaca Z. Utilization of robotic technology in hospital ambulatory surgery setting. U.S. Agency for Healthcare Research and Quality. 2021. https://hcup-us.ahrq.gov/ reports/RoboticAmbulatorySurgery.pdf. Accessed November 1, 2023.
20. Amann, J., Blasimme, A., Vayena, E. et al. Explainability for artificial intelligence in healthcare: a multidisciplinary perspective. BMC Med Inform Decis Mak 20, 310 (2020). https://doi.org/10.1186/s12911-02001332-6
21. McDonell S. China investigates search engine Baidu after student’s death. BBC News. May 3, 2016. Available from: https:// www.bbc.com/news/business-36189252. Accessed October 27, 2023.
Author Biography
Annie Huang is a freshman majoring in computer science and minoring in robotics. She is also a staff editor for the SciTech section of the Johns Hopkins newspaper, The News-Letter. She is enthusiastic about translational research and hopes to contribute to disseminating public health knowledge by writing for Epidemic Proportions.
36

37
Andre De Santis/Unsplash
Beyond the Statistics: Young Women, Breast Cancer, and Self-Advocacy
Ananya Gulati
Summary
This article highlights the importance of self advocacy when it comes to diagnosing breast cancer in young women, especially given the misconception that the disease only affects older women and the potential repercussions of not speaking up. It discusses the duality behind the recommended age for young women to begin screening for breast cancer. It emphasizes the importance of self-examinations and proactive communication with healthcare professionals. This piece includes personal experiences of breast cancer survivors navigating the US healthcare system at the early age of their diagnoses and highlights the unique challenges young women face afterward, including fertility and other life changing decisions.
If you’re in your 20s, 30s, or even early 40s, breast cancer is probably the last thing on your mind. However, data from the CDC estimates that 240,000 women are diagnosed with breast cancer every year, and 10% of those women are under 45.1 If you do the math, that is about 24,000 young women diagnosed with breast cancer every year. That is not an insignificant number.
Scientists have made significant advancements in early stage diagnosis of breast cancer. Mammography, ultrasounds and MRIs have been proven to be effective tools at detecting and monitoring breast cancer.2 For women without a strong family history of breast cancer, the American Cancer Society states that those in the age range of 40 to 44 years old have the “option” to get mammograms while those above 45 should get a mammo-
gram once a year.3 This recommendation may limit early action of women younger than 40, as they technically do not fit in the “at risk” population. Young women are typically not provided with the option of preventative screenings given the low sensitivity of mammograms in young and dense tissues. MRI’s, on the other hand, have high sensitivity but contribute to many false positives.4 Although there are certainly scientific or policy-oriented remedies to these issues, self-advocacy remains the most important step in early stage diagnosis of breast cancer in young women.
Jill Mull is a patient navigator at the Johns Hopkins Breast Cancer Program. As a breast cancer survivor herself, she has dedicated her life to supporting young breast cancer patients and their families. In her early 30s, Jill found a lump in her breast and was told that it was a cyst. Her intuition led her to call her doctor to order a mammogram. When she arrived at an imaging center with the doctor’s order, the person in charge told her that she should start with an ultrasound because of her youth and lack of family history related to breast cancer. Against her better judgment, Jill complied, only for the ultrasound to suggest that a mammogram was necessary. The mammogram detected abnormal tissue and a biopsy confirmed what Jill feared: Jill had breast cancer at the age of 32.
As a patient navigator, Jill is able to share her lived experiences as a breast cancer survivor and navigate all the feelings that come with such a diagnosis. She uses her professional training and personal experiences to offer counsel on diagnoses and the road
ahead. Jill has seen that the long-term consequences of breast cancer are different for young women, who must consider the impact of their condition and treatment on fertility and relationships in frightening and unique ways.
The person who inspired me to write this column was caught unaware by her diagnosis at the age of 44. She, like many other women her age and younger, had her full faith in medicine and adhered to recommended screening guidelines put forth by the American Cancer Society. A few months prior to her diagnosis, her doctor assured her she was in good health. When she asked about mammograms, the doctor dismissed the question and said that she was too young to worry about these things. Despite being a medical provider herself, she held her tongue
“
It makes me angry to think that such a common form of cancer was not caught earlier even in the US’s advanced medical system.
”
and trusted what her doctor told her. A few months later, she discovered a lump in her breast and was diagnosed with an aggressive form of breast cancer. She regrets not speaking up at that appointment. It makes me angry
38

to think that such a common form of cancer was not caught earlier even in the US’s advanced medical system. It is situations like these that have driven me to write this piece today in an attempt to spread awareness about the importance of self-advocacy when it comes to the health of young women.
In May 2023, the United States Preventive Services Task Force lowered the recommended screening age for breast cancer from 50 to 40 years of age. This decision stemmed from various studies that have shown breast cancer in young women to be associated with more aggressive forms of cancer relative to that of older women.5
A breast cancer diagnosis in younger women is also more complex to deal with due to the unique impact on women just beginning to explore their sexuality, careers, and family goals. When beginning their treatment, a
main concern for women is the impact on fertility and their ability to get pregnant in the future. Breast cancer treatment can often result in experiencing menopausal symptoms and treatment-related infertility, which is a major cause of concern among younger patients.6 Young women are forced to make rapid life-changing decisions regarding fertility preservation as treatment must begin soon after a breast cancer diagnosis. Additionally, young women are increasingly concerned about the recurrence of cancer, requiring additional counseling.6
Women, especially younger women who think they may be at risk for breast cancer because of family history or who feel changes in their breasts shouldn’t be scared to seek professional advice. Women are often silenced when expressing medical concerns, but the consequences of being passive
about our health can be dire. A study showed that women who delayed seeking breast cancer treatment by at least 3 months after symptoms arrived were 12% less likely to survive after 5 years.7 Another study found that women were diagnosed later in life than men for over 700 different diseases.8 People often believe that breast cancer only affects older women, but younger women are not immune to such diagnoses. Thus, the burden of seeking out medical care and speaking up when necessary falls on our shoulders. It’s unfair, but today it’s our reality.
If breast cancer affects young women, why aren’t healthcare professionals doing more to emphasize early detection and awareness? There are some valid reasons for the age specified in current screening requirements. Many healthcare professionals worry
39
Angiola Harry/Unsplash
that an increase in testing can potentially lead to a higher number of false positives, causing emotional trauma to the patient. Rates of false positives are shown to be higher in women aged 40 to 49 years old and decrease as age increases.9 The current wisdom is that the rarity of breast cancer in young women means that earlier testing would cause more harm than good.
This article isn’t for medical professionals or policymakers. It is for young women who are scared about their health but don’t know if they should speak up. All women should check their breasts every few weeks to understand what their normal state looks and feels like. If they notice any abnormalities, like dimpling or changes in size and shape, they should bring those concerns to their doctor rather than wait.10 Frequent self-examinations are associated with earlier stage diagnoses, thus improving chances of survival for young women.11 Some healthcare professionals might dismiss our concerns and attempt to silence us, but it’s our responsibility to push back until they hear us out. I am not a medical professional, but I am a young woman learning to navigate the healthcare process, much like the rest of you, which can often be confusing and frightening. This article is not a scientific prescription; it’s a cry to young women who might be afraid to speak up and make someone listen. We must defy the silence and advocate for ourselves.
References
1. Centers for Disease Control and Prevention. (n.d.). Basic Information About Breast Cancer. Division of Cancer Prevention and Control. https://www.cdc. gov/cancer/breast/basic_info/index.htm
2. Jafari, S. H., Saadatpour, Z., Salmaninejad, A., Momeni, F., Mokhtari, M., Nahand, J. S., Rahmati, M., Mirzaei, H., & Kianmehr, M. (2018). Breast cancer diagnosis: Imaging techniques and biochemical markers. Journal of cellular physiology, 233(7), 5200–5213. https://doi.org/10.1002/ jcp.26379
3. American Cancer Society.(n.d.). American Cancer Society Recommendations for the Early Detection of Breast Cancer. https://www.cancer.org/cancer/types/ breast-cancer/screening-tests-and-early-detection/american-cancer-society-recommendations-for-the-early-detection-of-breast-cancer.html
4. Rossi, L., Mazzara, C., & Pagani, O. (2019). Diagnosis and Treatment of Breast Cancer in Young Women. Current treatment options in oncology, 20(12), 86. https://doi. org/10.1007/s11864-019-0685-7
5. Fabiano, V., Mandó, P., Rizzo, M., Ponce, C., Coló, F., Loza, M., Loza, J., Amat, M., Mysler, D., Costanzo, M. V., Nervo, A., Nadal, J., Perazzo, F., Chacón, R., & RCM Database Contributors4 (2020). Breast Cancer in Young Women Presents With More Aggressive Pathologic Characteristics: Retrospective Analysis From an Argentine National Database. JCO global oncology, 6, 639–646. https://doi. org/10.1200/JGO.19.00228
6. Warner, E., Glass, K., Foong, S., & Sandwith, E. (2020). Update on fertility preservation for younger women with breast cancer. CMAJ : Canadian Medical Association journal = journal de l’Association medicale canadienne, 192(35), E1003–E1009. https://doi.org/10.1503/cmaj.200245
7. Ruddy, K. J., Gelber, S., Tamimi, R. M., Schapira, L., Come, S. E., Meyer, M. E., Winer, E. P., & Partridge, A. H. (2014). Breast cancer presentation and diagnostic delays in young women. Cancer, 120(1), 20–25. https://doi.org/10.1002/cncr.28287
8. Alcalde-Rubio, L., Hernández-Aguado, I., Parker, L. A., Bueno-Vergara, E., & ChiletRosell, E. (2020). Gender disparities in clinical practice: are there any solutions? Scoping review of interventions to overcome or reduce gender bias in clinical practice. International journal for equity in health, 19(1), 166. https://doi.org/10.1186/ s12939-020-01283-4
9. Nelson, H. D., O’Meara, E. S., Kerlikowske, K., Balch, S., & Miglioretti, D. (2016). Factors Associated With Rates of False-Positive and False-Negative Results From Digital Mammography Screening: An Analysis of Registry Data. Annals of internal medicine, 164(4), 226–235. https:// doi.org/10.7326/M15-0971
10. Kegeles S. S. (1985). Education for breast self-examination: why, who, what, and how?. Preventive medicine, 14(6), 702–720. https://doi.org/10.1016/00917435(85)90068-4
11. Foster, R. S., Jr, Lang, S. P., Costanza, M. C., Worden, J. K., Haines, C. R., & Yates, J. W. (1978). Breast self-examination practices and breast-cancer stage. The New England journal of medicine, 299(6), 265–270. https://doi.org/10.1056/ NEJM197808102990601
Author Biography
Ananya Gulati is an undergraduate senior studying Public Health with a minor in Business Studies at Johns Hopkins University. She is currently a Public Health intern at the United Nations and a research analyst at the Bloomberg School of Public Health studying Hepatitis C treatment adherence among people who utilize injection drugs. She has previously conducted melanoma and breast cancer research at the Jackson Laboratory for Genomic Medicine. Ananya plans to pursue a career in medicine to advance women’s health.
40

41
Colin Lloyd/Unsplash
Breaking Barriers: Unveiling the Structural Risk Fueling the Gender Gap in HIV Vulnerability in Southern Africa
Prisha Batra
Summary
This editorial begins by highlighting the alarming statistics of HIV transmission among young women in southern Africa, underscoring an urgent need to address the underlying gender-specific causes. The link between gender-based violence and HIV infection is then explored, citing research that demonstrates the heightened risk for women who experience intimate partner violence. Sociocultural factors, such as gender norms, stigma surrounding HIV/AIDS, and traditional beliefs regarding sexual practices, further compound women’s susceptibility to HIV. Economic factors also exacerbate women’s vulnerability by limiting access to healthcare and educational opportunities. Specifically, a discussion of how economic dependence can compromise women’s ability to negotiate safe sexual practices, leading to higher rates of HIV transmission, is presented. The impact of historical legacies, such as Apartheid, on socioeconomic disparities and access to healthcare services is also examined. This editorial addresses the heightened vulnerabilities faced by marginalized groups who experience intersecting forms of discrimination and stigma. Finally, this op-ed calls for policymakers to prioritize gender equality, empower women, and confront discriminatory practices to mitigate gender disparities in the HIV epidemic. This article advocates for inclusive research and interventions that involve women in the design and implementation process to ultimately strive for a more equitable approach to HIV prevention, diagnosis, and treatment.
Introduction
The Human Immunodeficiency Virus (HIV) continues to have a detrimental impact on millions of people around the world. HIV can be spread by a number of means, such as unprotected sexual contact, needle sharing, and mother-to-child contact during pregnancy, childbirth, and breastfeeding.1 Although HIV does not discriminate on the basis of gender, women are at a higher risk of contracting HIV than men in southern Africa. In 2021, the Kaiser Family Foundation reported
5,000 young women aged 15-24 in southern Africa were newly infected with HIV every week. “ ”
that approximately 5,000 young women aged 15-24 in southern Africa were newly infected with HIV every week, highlighting the alarming rates of HIV transmission among young women in the region.1 In southern Africa, young women are twice as likely to contract HIV than young men, making up 63% of all new HIV infections in 2021.2 There is an urgent need to address gender-specific issues that contribute to the increased risk of HIV among women. For the purpose of developing effective prevention methods, advancing gender equity and ensuring that particular healthcare needs of women are addressed, such as accessi-
ble reproductive health services, comprehensive sex education, and support for victims of gender-based violence, it is essential to comprehend the root causes of gender discrepancy in HIV infection. These risk factors go beyond individual behaviors and comprise social, economic, and cultural facets that influence how women live their lives and ultimately affect their susceptibility to HIV infection. By acknowledging and diving deeper into these structural risk factors, we can establish stronger preventive and supportive measures for women in southern Africa and worldwide.
Gender Inequality and Sociocultural Factors
Various studies have shown that gender-based violence increases a woman’s probability of contracting HIV. 3 Gender-based violence is defined as any act of violence against a person based on their gender, although more frequently directed toward a woman or girl.3 A 2010 cluster-randomized controlled trial conducted in the Eastern Cape province of South Africa discovered a strong correlation between intimate partner violence and HIV infection.3 Compared to those who had not experienced any violence, women between the ages of 15 and 26 years who experienced sexual or physical violence were found to be 50% more likely to be HIV positive.3 Gender-based violence, which includes controlling behavior from a partner, is typically linked to high-risk sexual behaviors, especially in developing and developed nations. Examples of these high-risk sexual behaviors include “multiple and concurrent sexual relationships, substance use, transactional sex and prostitution, and less
42

frequent condom use”.3 When women are intoxicated, drugged, dissociating, desperately seeking affection, or being otherwise coerced by controlling partners, they are especially likely to partake in these high-risk sexual practices. A fear of violence often dissuades women from seeking support, which only perpetuates a cycle of abuse that further exacerbates their vulnerability to HIV.
The process by which people pick up gender-specific societal standards, expectations, and behaviors, also known as gendered socialization, also contributes to gender discrepancies in HIV infection. In many cultures, males are frequently led to be forceful, independent, and dominant, whereas females are frequently taught from an early age to be nurturing, obedient, and submissive. These gender norms impact women’s lives in various ways, including their ability to make their own decisions about their sexual conduct. According to Higgins et al., “gendered socialization can also increase women’s susceptibility to HIV by leading them to place a premium on love and romantic relationships”.4 These culturally driven gender norms can cause
women to place unneeded emphasis on relationships and even lead them into relationships built on unequal positions of power. As a result, women may not only find themselves struggling to push for condom use but also unable to determine the frequency and timing of sexual encounters and even refuse unwanted sexual advances entirely.
Economic Factors and Vulnerability
Women’s access to high-quality healthcare, particularly HIV prevention, testing, and treatment services, is frequently limited by poverty. Women facing poverty are less likely to have a sufficient understanding of HIV, get routine HIV testing, and acquire anti-retroviral medicine.5 Often correlated with poverty, lower educational attainment contributes to a lack of understanding regarding HIV prevention and transmission. Women with no formal education might also be less aware of condom use and other safer sexual practices. Data obtained in 2014 from the Zambia Demographic and Health Survey determined that educational attainment “was strongly associated with HIV testing among 15,388 women of childbearing age”.5 In fact, uneducated women in Zam-
bia have been found to be twice as likely to contract HIV as those with some education.5 Pregnant women with higher levels of education were more likely to get tested for HIV compared with pregnant women with lower levels of education. Additionally, the prevalence of HIV testing varied significantly by socioeconomic class; a higher wealth index among women generally showed a higher uptake of testing.6 Prioritizing the improvement of HIV testing services in remote underprivileged communities will not only mitigate the risk of vertical HIV transmission but also contribute significantly to an overall reduction in HIV prevalence. However, to address the underlying issues related to educational attainment, it is crucial to call for more health and HIV education in these communities. This comprehensive approach acknowledges the intricate interplay of these challenges and strives to establish a more inclusive and effective framework for HIV prevention.6
Economic dependence pertains to a situation in which people must depend on others for financial support as a result of a lack of employment prospects and economic opportunities. A woman’s ability to negotiate safer sexual behaviors is often further constrained by this economic dependence. Women may have trouble establishing their choices, such as condom use or HIV testing, in relationships where a partner provides all the financial assistance. Moreover, women experiencing financial insecurity may also engage in risky sexual practices such as transactional sex or survival sex work, involving the exchange of sexual favors for cash, items, or other resources. Due to financial incentives and limited control over the circumstances of these sexual interactions, women are more prone to have several sexual partners and unprotected sex, thereby running an increased risk of HIV infection.
43
National Cancer Institute/Unsplashed

Acephie Joseph was a Haitian woman whose life was completely altered after the government forcibly removed her and her family from their land.7 After relocating, her family was unable to continue producing agricultural goods, lacking the resources to support themselves. Acephie began engaging in sexual intercourse with numerous men because she believed that doing so would help her escape poverty. However, Acephie contracted HIV subsequent to a sexual encounter with a soldier, culminating in her ultimate demise characterized by considerable discomfort and suffering. According to Paul Farmer’s On Suffering and Structural Violence: A View from Below, she stated, “I never dreamed he would give me a bad illness, never! I looked around and saw how poor we all were, how the old people were finished…What would you have me do? It was a way out, that’s how I saw it”.7 A “way out’’ is alsohow many poor women in southern Africa view the process of exchanging sex for an increase in status, material goods, money, shelter, and other resources. Similar to Acephie’s case, economic hardships in southern Africa drive many women toward sex work and consequently elevate their susceptibility to HIV infection. This economic imbalance is one of the underlying causes of
gender disparities in the HIV epidemic, highlighting the urgent need for interventions that address both structural inequalities and individual agency in sexual health.
Intersectionality and Key Populations
Currently in South Africa, Black African women bear the highest burden of HIV infection. The disproportionately high incidence of HIV among Black African women are caused by a number of factors, including socioeconomic inequality, restricted access to healthcare, and cultural norms.8 These disparities have been exacerbated by the lasting legacy of Apartheid and its effects on socioeconomic conditions and access to healthcare. Apartheid was a system of institutionalized racial segregation and discrimination that was enforced in South Africa from 1948 to the early 1990s. Under Apartheid, the South African government implemented laws and policies that systematically oppressed and marginalized non-white racial groups, particularly Black South Africans. The Apartheid regime classified people into racial categories, including White, Black, Coloured (mixed-race), and Indian, and allocated different rights, privileges, and resources based on these classifications. The systematic racial segregation and
discrimination inherent in the Apartheid era laid the groundwork for persistent social and economic disparities that hinder women’s access to education and healthcare. As a consequence of Apartheid, many South African young women, particularly black women, face educational disadvantages that diminish their earning potential and limit their economic mobility. This systemic inequality not only perpetuates socio-economic disparities but also exacerbates the disproportionate burden of HIV infection on black women.8
Additionally, lesbian, bisexual, transgender and other sexual minority groups in Southern Africa may be more susceptible to HIV infection. Stigma, prejudice, and restricted access to quality healthcare services all contribute to this increased risk.
Corrective rape, also known as homophobic rape, is a hate crime that occurs when a victim is sexually assaulted due to their perceived sexual orientation and with the supposed goal of turning the victim heterosexual.9 Queer women may be more susceptible to “corrective rape” as a result of homophobic views, which could make them more HIV-vulnerable. Healthcare professionals are also more likely to treat sexual minority women unfairly and stigmatize them, which could result in poor or improper care.9 Due to a fear of disclosure, sexual minority women may tend to be less willing to seek HIV-related services. As a result, access to quality healthcare, assistance programs, and social support networks for sexual minority women may be made more difficult.
Usually women are the first in their relationships or families to find out that they have HIV. 10 Often, this discovery has “attached to them as blame, since in their discovery they are also perceived as creating the disease”. Due to their “contaminating sexual promiscuity” and perceived rejection of conventional norms, sex-
44
Jacques Nel/Unsplash
ual minority women are frequently portrayed as both the cause and the spread of AIDS.10 This unfounded portrayal contributes to the perpetuation of harmful stereotypes and discrimination against sexual minority women in the context of HIV/AIDS, hindering efforts to address the epidemic equitably and effectively.
Conclusion
It is clear that gender inequality and sociocultural factors play a key role in limiting women’s agency in relation to sexual health. This vulnerability is exacerbated by the high rates of gender-based violence and age-old gender norms prevalent throughout many regions in southern Africa. Moreover, poverty and the lack of financial independence make it difficult for women to obtain educational awareness about HIV, negotiate safe sex, and receive the proper healthcare needed. Finally, there are heightened vulnerabilities experienced by women who are members of marginalized groups in South Africa, such as sex workers, black women, and members of the LGBTQ+ community. Altogether, these factors contribute to the gender disparities in the HIV epidemic, emphasizing the urgent need for comprehensive interventions that address the intersecting challenges faced by women in southern Africa.
To address these systemic issues, it is crucial for policymakers to utilize comprehensive and gender-responsive strategies that acknowledge these interwoven social, economic, and cultural causes of gender inequalities in HIV. These interventions should work towards the opposition of discriminatory behaviors, the promotion of gender equality, and the advocacy of giving equitable economic influence to women. In order to advance efforts to decrease HIV transmission rates among women, future research should focus on assessing the efficacy of the gender-responsive interventions that are already in place in southern Africa. This involves researching the
results of community-based projects, legal reforms, and programs for economic empowerment. To ensure cultural sensitivity and relevance, it is essential to include women in the design and execution of new interventions. Policymakers, healthcare providers, and communities must all prioritize gender equality, empower women, and confront discriminatory practices in order to lower the structural risk factors that escalate the vulnerable position of women in this devastating crisis.
References
1. Centers for Disease Control and Prevention. Ways HIV Can Be Transmitted | HIV Transmission | HIV Basics | HIV/AIDS | CDC. www.cdc.gov. Published November 3, 2020. https://www.cdc.gov/hiv/basics/ hiv-transmission/ways-people-get-hiv. html
2. KFF. The Global HIV/AIDS Epidemic. KFF. Published July 26, 2023. https://www. kff.org/global-health-policy/fact-sheet/ the-global-hiv-aids-epidemic/
3. Jewkes RK, Dunkle K, Nduna M, Shai N. Intimate partner violence, relationship power inequity, and incidence of HIV infection in young women in South Africa: a cohort study. The Lancet. 2010;376(9734):41-48. doi:https://doi. org/10.1016/S0140-6736(10)60548-X
4. Higgins JA, Hoffman S, Dworkin SL. Rethinking Gender, Heterosexual Men, and Women’s Vulnerability to HIV/ AIDS. American Journal of Public Health. 2010;100(3):435-445. doi: 10.2105/ AJPH.2009.159723
5. UNAIDS. WOMEN and HIV a SPOTLIGHT on ADOLESCENT GIRLS and YOUNG WOMEN.; 2019. https://www. unaids.org/sites/default/files/media_asset/2019_women-and-hiv_en.pdf
6. Muyunda B, Musonda P, Mee P, Todd J, Michelo C. Educational Attainment as a Predictor of HIV Testing Uptake Among Women of Child-Bearing Age: Analysis of 2014 Demographic and Health Survey in Zambia. Frontiers in Public Health. 2018;6. doi:https://doi.org/10.3389/ fpubh.2018.00192
7. Farmer P. On Suffering and Structural Violence: A View from Below on JSTOR. www.jstor.org. Published 1996. https:// www.jstor.org/stable/20027362
8. Muula AS. HIV Infection and AIDS Among Young Women in South Africa. Croatian medical journal. 2008;49(3):423435. doi:https://doi.org/10.3325/ cmj.2008.3.423
9. Baptiste-Roberts K, Oranuba E, Werts N, Edwards LV. Addressing Health Care Disparities Among Sexual Minorities. Obstetrics and Gynecology Clinics of North America. 2017;44(1):71-80. doi:https://doi. org/10.1016/j.ogc.2016.11.003
10. Vale B, Hodes R, Cluver L. Negotiations of Blame and Care among HIV-positive Mothers and Daughters in South Africa’s Eastern Cape. Medical Anthropology Quarterly. 2017;31(4):519-536. doi:https:// doi.org/10.1111/maq.12351
Author Biography
Prisha Batra is a sophomore at Johns Hopkins University studying Public Health and Natural Sciences. She is an aspiring surgeon and is interested in learning more about addressing health disparities and engaging in community health initiatives.
45

 Policy
Shannon Wang Zao
Policy
Shannon Wang Zao
Evergreening and Patent Warfare Between Pharmaceutical Companies Underlie Deeper Controversy on Intellectual Property Policy Across the World
Pranav Kotamraju and Tanisha Taneja, Policy Team
Both the public and private sector pour heavy investment into the pharmaceutical industry, and for good reason. Not only is drug discovery essential for medicine, but estimations of the cost required for just one new drug can reach upwards of a billion dollars.1 Pharmaceutical companies however are not really competing for drugs, but rather the patents that underlie those drugs. Patents are the lifeblood of pharmaceutical companies, as they grant a 2 decade-long monopoly over the invented drug.2 The monopoly over distribution and manufacturing of the drug serves as a major revenue source and a way to recoup losses from all the money funneled in research and development. These monopolies have so much value in fact that companies often fight tooth and nail to stop other companies from infringing upon their patent, as well as to keep, extend, and acquire these patents. We analyze the three most relevant examples of how patents are fought for currently after drugs have been created: between countries and companies, two individual companies, and between companies and regulatory agencies. These fights can often toe the line between corporate malfeasance and standard business competition, possibly leaving the consumer as the victim in the middle of it all.
Most of the time, innovating an unprecedented product, such as a medication, is a slow and arduous process. In the pharmaceutical sector, many companies take a shortcut by evergreening, which we will define as Alkhafaji et al.3 did: the act of a company extending its monopoly over a
pharmaceutical product through various strategies, such as making minor modifications to it to brand it as a new product worthy of patent protection or interpreting patent laws in creative ways. This practice has been met with considerable controversy. Defenders argue that contrary to popular rhetoric, evergreening does not impede competition from other companies on the market as they are still allowed
of pre-existing drugs, it should not be recuperated.5 They also reason that the drugs subject to evergreening are typically each company’s moneymaker (“blockbuster drugs”), from which they infer that these drugs have been on the market for years and helped millions. Based on this assumption, they assert that making insignificant modifications to these drugs right before the expiration dates of their pat-

to produce generic drugs and make a profit from them.4 It also protects the extremely risky business of drug innovation by helping companies recover the considerable amount of financial resources invested in the research and development (R&D) of drugs, which will only occasionally lead to minor improvements.5 On the other hand, opponents contend that the justification of evergreening to recoup R&D costs is problematic because if R&D money is spent on modifying versions
ents reeks of companies seeking economic profit, not making a concerted effort to improve their products.6
The impact of evergreening is tremendous - it has been estimated that drug costs have more than tripled for the average consumer as a result.7 This can be rationalized by considering that companies that practice evergreening may engage in product-hopping, where old products are phased out in favor of “new” ones that are forced onto the general public. This
48
Roberto Sonin/Unsplash
maneuver also delays the production of generic drugs by other companies that may serve as cheaper, non-brand name alternatives on the market. The result is increased prices and reduced freedom of choice for consumers.8 The severity of the situation may have prompted United States Representative Hakeem S. Jeffries (D-NY) to introduce Term Act 2019, during the 116th Congress, requiring the owner of multiple patents for a single pharmaceutical product to demonstrate that each patent covers a distinct invention. The Resolution was referred to the Subcommittee on Courts, Intellectual Property, and the Internet in June 2019, where it has since not left.9 No resolution regarding evergreening has been proposed in the 118th Congress. Still, regulatory fights continue, if not in Congress, then between companies in front of the courts.
One specific case of evergreening was seen through the switch from Prilosec to Nexium by AstraZeneca. Prilosec and Nexium are both proton pump-inhibiting drugs that are used to combat Gastroesophageal reflux disease (GERD).10 Prilosec was approved by the FDA in 1989 but with quite a high price of $4 per pill.11 It was commonly prescribed by gastrointestinal doctors, but its high price often became a barrier for many. However, the drug patent on Prilosec was going to end in April of 2001, bringing fear to the workers of AstraZeneca. Once the patent expires, other companies can create generics of Prilosec, which are often cheaper, taking profits away from AstraZeneca. Knowing this was in the near future, AstraZeneca’s team started brainstorming ideas to avoid the creation of generics at all costs. Their final solution was to decrease the two isomers in Prilosec to just one isomer, and the new creation was named Nexium. Therefore, the active ingredient in Prilosec is Omeprazole, while the active ingredient in Nexium is Esomeprazole. While a very minor change, the company saw improvements. In one of their studies, Nexium
had a 90% healing rate for heartburn while Prolisec had an 87% healing rate after use for eight weeks.11 With a slight improvement in outcomes, AstraZeneca was able to prove their need for a new patent on Nexium. This practice of one company moving from one drug to another with very small changes is a type of evergreening, specifically called product hopping.12 AstraZeneca focused on decreasing sales of Prilosec and increasing sales of Nexium to continue expanding their profits while preventing the production of any generics. By 2003, 40% of patients switched to Nexium, bringing in $3 billion for AstraZeneca.13 AstraZeneca saw success in creating a new patent for Nexium to maximize profits.
The issue of evergreening stems mostly from the difficulty of drug discovery. This problem leads to more than just evergreening however, it also leads to fights between pharmaceutical companies on the rights to sell particular medicines. Court battles are frequently fought over who has patent rights, when patent rights run out, and why certain patent monopolies should continue.
“
” Drug costs have more than tripled for the consumer.
For example, the newly released and popular weight loss drugs, Ozempic and Wegovy, were challenged in court. Specifically, the company Novo Nordisk, the company that holds the patent, was challenged by Mylan Pharmaceuticals, whose lawsuit could obtain the rights for generic versions of the medicine to be produced.14 Novo Nordisk is fending off multiple attacks on its patent rights from other companies attempting to sell generic
versions of Ozempic and Wegovy. Although generic drugs would mean a bigger market for mediation and possibly a better price for the consumer, it would also mean less incentive for innovation. Getting a successful patent can be analogous to striking gold, and many pharmaceutical companies often end up investing in efforts to find “gold”.
However, certain regulatory agencies do take note of certain practices. For example, the Federal Trade Commission (FTC) has filed an amicus brief in an ongoing patent lawsuit. When generic drugs are set to hit the market, the original patent holder has the right to file for a sort of stay in the FDA’s “orange book”. This stay causes a 30-month waiting period before generic versions of the drug can truly be sold.15 All the while, the original patent-holding company continues to sell its drug. In the brief, the FTC argues against patent practices like these, stating that they could hurt consumers by driving down competition and driving up prices.
To make the analysis broader, we can look at the international implications of domestic issues like evergreening and fights between companies on viable patents. If patents were only applicable in the nation where they were filed, then it is easy to see how other companies in other countries could take advantage of new research. Hence, organizations like the World Trade Organization (WTO) were born, which enforce and oversee patent protections across the world16 including medical patents. The WTO often enforces the very same monopolies over the distribution, manufacturing, and selling of medicines. This often creates controversy regarding developing nations and their ability to purchase the medication.17 However, the WTO has recognized this and put in place certain provisions giving developing nations a waiver on enforcing certain patent laws on medicine in their country18 until the countries become
49
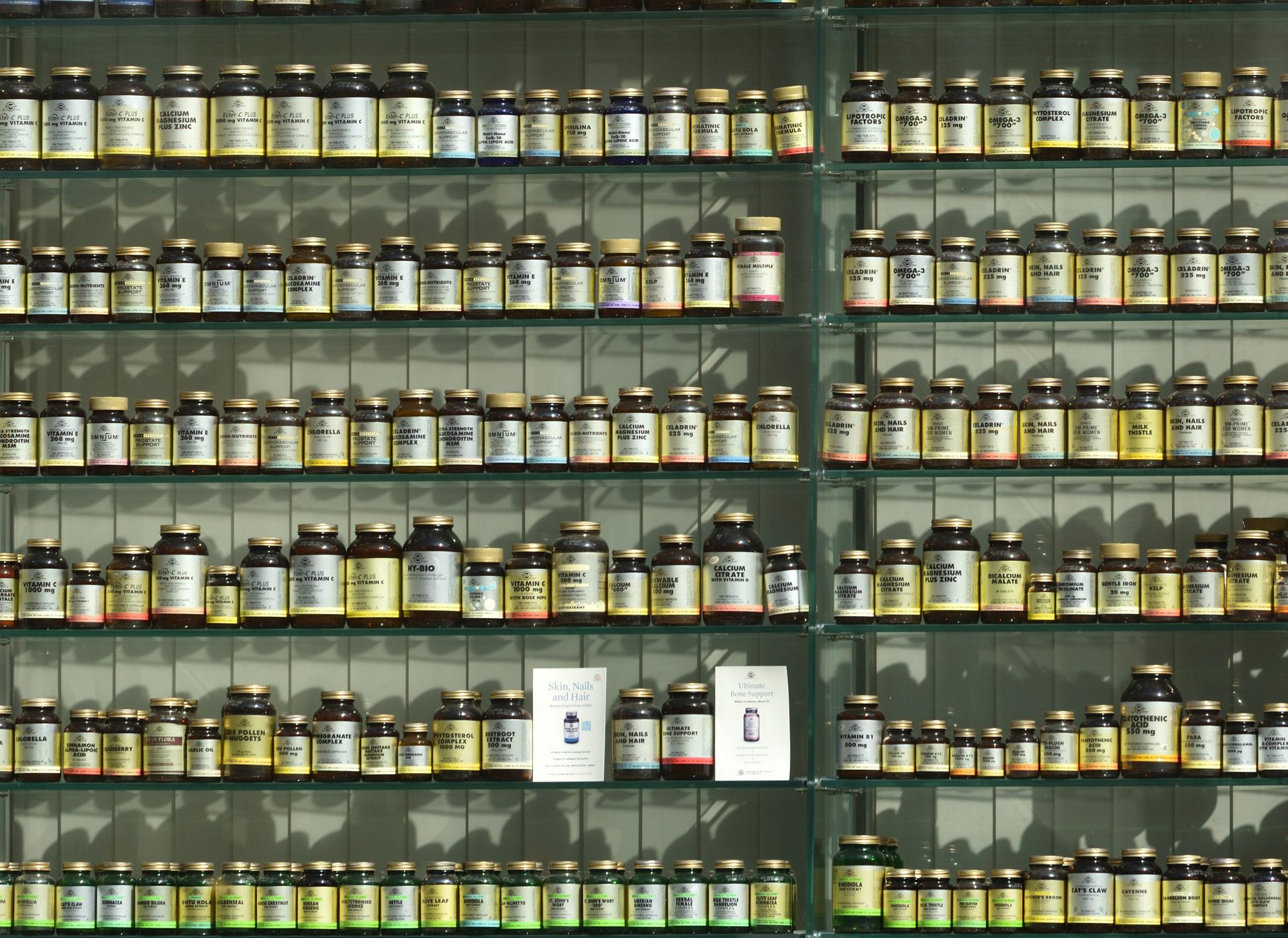
more advanced. This period is called the “transition period” for developing nations. Other forms of waivers exist as well, such as compulsory licensing, where the country (not the patent owner) allows another country to produce the medication due to extreme need.19
Even with these exceptions in place, however, international fights over medical patents persist. One example to analyze this issue took place during the COVID-19 pandemic surrounding the vaccines. India and South Africa filed a motion in the WTO to waive all patents concerning the COVID-19 vaccines, including manufacturing rights.20 Although this waiver received considerable support, there was also heavy pushback from higher-income countries. Their arguments centered around the loss of incentive that this could create in drug companies, as well as a loss of investment into medical innovation. Furthermore, the pushback was specifically tailored to the COVID
vaccines themselves, contending that even with a patent waiver, the vaccine output required was far too great and that every capable manufacturer was already making these vaccines.21 This essentially would render any such waiver useless, as it would not allow any new manufacturers to help scale production. Further, arguments surrounded errors in the distribution of medication in developing nations. Locke from the Seattle Times cites specifically a case in the Democratic Republic of the Congo where 1.3 million COVID-19 vaccines were returned due to difficulty in getting the vaccines to “rural areas”.21
Through all of this, Moderna, a company responsible for creating one of the COVID-19 vaccines, waived some of its manufacturing/selling rights to these vaccines to help developing nations.22 This could show a true extension of goodwill, or perhaps an understanding on Moderna’s part that maximum production was already in
place. Regardless, the COVID-19 vaccine patent waiver discussion exemplifies the complexity of international medical patents and the murkiness of any solutions.
These battles over patents almost always involve either keeping the monopoly or making the medicine generic. Whether or not genericizing the medicine helps consumers however is up for debate, especially when we consider the losses that companies may incur when their drugs completely hit the market. Currently, debates over patents cannot become overly simplified due to the complexity of each drug and situation. While arguments over patent law will persist, regulatory agencies like the WTO, the FTC, and Congress need to continue to ensure that innovation, investment, and the consumer’s best interest are all given equal importance when protecting patent rights.
50
Angel Sinigersky/Unsplash
References
1. Rennane, Stephanie, et al. “Estimating the Cost of Industry Investment in Drug Research and Development: A Review of Methods and Results.” Inquiry : A Journal of Medical Care Organization, Provision and Financing, U.S. National Library of Medicine, 16 Feb. 2022, www.ncbi.nlm.nih.gov/ pmc/articles/PMC8855407/#:~:text=Estimates%20of%20Industry%20Drug%20 R%26D%20Costs&text=There%20 is%20a%20significant%20increase,estimates%20are%20over%20%242%20billion.
2. Gurgula, Olga. “Strategic Patenting by Pharmaceutical Companies - Should Competition Law Intervene?” IIC; International Review of Industrial Property and Copyright Law, U.S. National Library of Medicine, 28 Oct. 2020, www.ncbi.nlm. nih.gov/pmc/articles/PMC7592140/.
3. Alkhafaji, Ali A, et al. “Impact of Evergreening on Patients and Health Insurance: A Meta Analysis and Reimbursement Cost Analysis of Citalopram/ Escitalopram Antidepressants - BMC Medicine.” SpringerLink, BioMed Central, 20 Nov. 2012, link.springer.com/article/10.1186/1741-7015-10-142.
4. Lietzan, Erika. “The Evergreening Myth.” Cato.Org, Cato Institute, 2020, www. cato.org/regulation/fall-2020/evergreening-myth.
5. Collier R. Drug patents: the evergreening problem. CMAJ. 2013 Jun 11;185(9):E3856. doi: 10.1503/cmaj.109-4466. Epub 2013 Apr 29. PMID: 23630239; PMCID: PMC3680578.
6. Stanbrook MB. Limiting “evergreening” for a better balance of drug innovation incentives. CMAJ. 2013 Aug 6;185(11):939. doi: 10.1503/cmaj.130992. Epub 2013 Jul 22. PMID: 23877665; PMCID: PMC3735737.
7. Ablorh, Tsotso. “Pharma’s ‘Evergreening’ Patent Tactics Mean High Costs and Low Benefits for Consumers.” Mad In America, 5 July 2022, www.madinamerica. com/2022/07/pharmas-evergreening-patent-tactics-mean-high-costs-low-benefits-consumers/#:~:text=These%20 %E2%80%9Cevergreening%E2%80%9D%20tactics%20result%20in,increases%20in%20prices%20 for%20consumers.
8. Siddalingaiah, Simran, and Adrian Fugh-Berman. “Evergreened Drugs or Evergreened Profits?” Journal of Evaluation in Clinical Practice, U.S. National Library of Medicine, 11 May 2022, pubmed.ncbi.nlm. nih.gov/35543377/.
9. Jeffries, Hakeem. “All Info - H.R.3199 -
116th Congress (2019-2020): Term Act of 2019.” Congress.Gov, United States Congress, 11 July 2019, www.congress. gov/bill/116th-congress/house-bill/3199/ all-info.
10. Agranat I, Marom H. In Defense of Secondary Pharmaceutical Patents in Drug Discovery and Development. ACS Med Chem Lett. 2020 Feb 13;11(2):91-98. doi: 10.1021/acsmedchemlett.9b00497. PMID: 32280427; PMCID: PMC7106985.
11. Harris, Gardiner. “Prilosec’s Maker Switches Users To Nexium, Thwarting Generics.” The Wall Street Journal, Dow Jones & Company, 6 June 2002, www.wsj. com/articles/SB1023326369679910840.
12. Xia, Lydia. “Patent Database Exposes Pharma’s Pricey ‘Evergreen’ Strategy.” UC Law San Francisco (Formerly UC Hastings), UC Law SF, 24 Sept. 2020, www. uclawsf.edu/2020/09/24/patent-drug-database/#:~:text=AstraZeneca%27s%20 behavior%20includes%20actions%20 where,protections%20were%20piled%20 onto%20Nexium.
13. Federico, Pineiro, and Alberto Fernandez. “A Case Study of AstraZeneca’s Omeprazole/Esomeprazole Chiral Switch Strategy - Gabi Journal.” GaBI Journal - Generics and Biosimilars Initiative, Generics and Biosimilars Initiative Journal , 16 Nov. 2022, gabi-journal.net/a-case-study-of-astrazenecas-omeprazole-esomeprazole-chiral-switch-strategy.html.
14. Brittain, Blake. “US Patent Office Won’t Review Two Novo Nordisk Patents for Wegovy ...” Reuters, Reuters, 2 Oct. 2023, www.reuters.com/business/healthcare-pharmaceuticals/us-patent-officewont-review-two-novo-nordisk-patentswegovy-ozempic-2023-10-02/.
15. Liu, Angus. “With Filing in Sanofi and Mylan Insulin Lawsuit, FTC Amps up Scrutiny on Pharma’s Patent Tactics.” Fierce Pharma, 21 Nov. 2023, www.fiercepharma.com/pharma/ftc-blasts-pharmas-abuse-fda-patent-system-sanofi-mylans-insulin-monopoly-lawsuit.
16. “What Is the WTO? - Who We Are.” WTO, www.wto.org/english/thewto_e/ whatis_e/who_we_are_e.htm#:~:text=The%20WTO%20operates%20the%20 global,they%20face%20with%20each%20 other. Accessed 14 Jan. 2024.
17. Peter O’Brien, Developing countries and the patent system: An economic appraisal, World Development, Volume 2, Issue 9, 1974, Pages 27-36, ISSN 0305-750X, https:// doi.org/10.1016/0305-750X(74)90086-2. (https://www.sciencedirect.com/science/ article/pii/0305750X74900862)
18. “World Trade Organization.” WTO, www. wto.org/english/tratop_e/trips_e/factsheet_pharm04_e.htm. Accessed 14 Jan. 2024.
19. “World Trade Organization.” WTO, www.wto.org/english/tratop_e/trips_e/ public_health_faq_e.htm#:~:text=What%20is%20compulsory%20licensing%3F,the%20patent%2Dprotected%20 invention%20itself. Accessed 14 Jan. 2024.
20. “Panel on the WTO TRIPS Agreement and Its Relation to the Public Health and U.S. Intellectual Property.” Panel on the WTO TRIPS Agreement and Its Relation to the Public Health and U.S. Intellectual Property | US Court of Federal Claims, United States Court of Federal Appeals, 26 Apr. 2023, www.uscfc.uscourts.gov/ node/3362.
21. Locke, Gary. “Weakening IP Protections Won’t Help Developing Countries Fight COVID-19.” The Seattle Times, The Seattle Times Company, 8 Sept. 2021, www.seattletimes.com/opinion/weakening-ip-protections-wont-help-developing-countries-right-now/.
22. “Statements & Perspectives Details.” Moderna’s Updated Patent Pledge, Moderna, 7 Mar. 2022, investors.modernatx. com/Statements--Perspectives/Statements--Perspectives-Details/2022/Modernas-Updated-Patent-Pledge/default.aspx.
51
Weight Loss in Public Health: To Drug or Not to Drug?
Pranav Kotamraju and Tanisha Taneja, Policy Team
America has had its fair share of epidemics in recent times. COVID-19 ravaged the country for nearly 2 years, but the obesity epidemic has made its presence felt for much longer. Affecting nearly 42 percent of Americans as of 2017, obesity-related issues have become a staple in the healthcare system.1 The impacts of obesity extend beyond individuals, producing strain on the healthcare system seen in costs, hospital trips, and hospital admissions.2 In terms of costs, it was estimated that obese patients cost the healthcare system $1,496 more than other patients, even after controlling for demographics and socioeconomic status.3 So it seems obvious that any way to reduce obesity should be welcomed with open arms,
but after seemingly striking gold to combat obesity through weight loss drugs, public health questions and controversies persist. It’s been almost three years since NovoNordisk’s “Wegovy” was approved for weight loss.4 The drug has been shown to help people lose on average 15% of their weight by helping them feel satiated. However, Wegovy is not covered by most insurance companies and federal health programs due to fears of side effects such as hypertension and heart valve problems, leading to a potential $1000 out-of-pocket payment. Without coverage, interest in the drug drops from 59 to 16 percent.5 The lack of coverage for a drug that could potentially heavily reduce the extensive strain on the healthcare
industry seems counterintuitive. However, the utility of the drug is a fundamental barrier that blocks its widespread coverage and implementation.
The utility of weight loss drugs can be measured by the ease of keeping the weight off after losing it. However, a paper from the Wall Street Journal reports that only 17 percent of people who stopped taking the drug could keep their weight down.6 In addition, the rush over weight loss drugs has contributed to doctors prescribing Ozempic, which has the same active ingredient as Wegovy (semaglutide), but is not yet approved for weight loss use, though it is going through the FDA approval process.7 While the subversion of FDA guidelines shows a drive to fight against societal obesity, it

52
Diana Polekhina/Unsplash

also displays a policy problem within public health: Is it right to hold doctors, consumers and the public back when the societal push is very much behind the drug’s approval? However, with a drug that may potentially have to be taken lifelong to truly have an impact, the rush over the drugs may not be justified at all.
This rush for weight loss medication seems to have outpaced approval committees and insurance companies, who remain skeptical. Drugs similar to Wegovy are already in production from many different pharmaceutical companies.8 There is something to be said about the cost reductions that weight loss drugs could result in, with one report stating that in a decade, the government could save 245 billion dollars from the drop in healthcare expenditures.9 Nearly all signs, from the willingness of doctors to trust in these medicines to the potential cost reductions, point to a true positive impact. However, while the industry and society zoom ahead to accepting weight loss drugs as a staple of medicine, the toughest policy decisions remain with
the agencies. Determining the problems that could arise from the longterm usage of these drugs, in addition to the lengthy approval period from regulatory agencies are real issues. It remains to be seen if all of the potential is too good to be true, or if we really have found gold.
Works
Cited
1. Centers for Disease Control and Prevention. (n.d.). Adult Obesity Facts. Retrieved from https://www.cdc.gov/obesity/data/ adult.html
2. Christou, G. A., & Kiortsis, D. N. (2016). Adiponectin and lipoprotein metabolism. Biochimie, 124, 61–67. https://doi. org/10.1016/j.biochi.2015.09.018
3. U.S. Food and Drug Administration. (2022, January 13). FDA approves new drug treatment for chronic weight management, the first since 2014. Press Announcements. Retrieved from https://www.fda. gov/news-events/press-announcements/ fda-approves-new-drug-treatment-chronic-weight-management-first-2014
4. Frellick, M. (2022, February 10). Should Insurance Cover Wegovy, Ozempic, and Other New Weight Loss Drugs? Scientific American. Retrieved from https://www. scientificamerican.com/article/should-insurance-cover-wegovy-ozempic-and-other-new-weight-loss-drugs/
5. Rockoff, J. D. (2023, June 11). A WeightLoss Drug Changed My Life. Will It Solve My Problem? The Wall Street Journal. Retrieved from https://www.wsj.com/health/ pharma/a-weight-loss-drug-changed-mylife-will-it-solve-my-problem-aeb79260
6. National Center for Biotechnology Information. (2019). Obesity Medicine: Management of Obesity in Women’s Health Care. In P. M. Belfort, S. A. Brown, & P. R. G. Cunningham (Eds.), Obesity Medicine: Management of Obesity in Women’s Health Care (pp. 53–72). MDText.com, Inc. Retrieved from https://www.ncbi.nlm.nih. gov/books/NBK572122/
7. Gemmill, A. (2022, February 17). Why new weight loss drugs are out of reach for millions of older Americans. PBS NewsHour. Retrieved from https://www.pbs.org/ newshour/health/why-new-weight-lossdrugs-are-out-of-reach-for-millions-ofolder-americans
8. Tolbert, J., & Claxton, G. (2023, January 11). Medicaid Coverage of and Spending on New Drugs Used for Weight Loss. Kaiser Family Foundation. Retrieved from https://www.kff.org/policy-watch/medicaid-coverage-of-and-spending-on-newdrugs-used-for-weight-loss/
9. Stein, R. (2023, June 11). More Americans are turning to new weight-loss drugs like Ozempic and Wegovy. But getting insurance coverage is another battle. The Washington Post. Retrieved from https://www.washingtonpost.com/business/2023/06/11/weight-loss-ozempic-wegovy-insurance/
53
Thought Catalogue/Unsplash
Introducing the Center for Gun Violence Solutions at the Johns Hopkins Bloomberg School of Public Health Junwoo Park

Since January 1st, 2023, until November 13th, 2023, there have been a total of 887 victims who died from fatal shootings by law enforcement officers (LEO) according to The Washington Post. But what if we expand the search? How about we consider those who suffered and still suffer from trauma from either lethal or non-lethal shots?
Input with such conditions on the Gun Violence Archive (GVA) will double the number of search results.
This kind of data abstraction is precisely what I am currently working on as a research assistant under Dr. Cass Crifasi and her team at the Center
for Gun Violence Solutions – Johns Hopkins Bloomberg School of Public Health.
To provide you with a little insight, we have been proofreading the secondary data from GVA that involves officer-shooting incidents and submitting them into the prospective database of our own. So far we managed to consider half of the incidents that occurred between 2015 and 2022. For abstraction, we refer to the Archive itself, relevant news sources, and/or police reports accessible on the Internet. Doing so not only helps us to correct any mistakes by former collectors but also thoroughly investigate the nature of the incident. Here, we specifically
“ ” We aim to resolve gun violence by providng scientific insight.
consider the victim’s mental/behavioral records, blood alcohol level or evidence of substance abuse at the incident, location of the shooting, presence of social worker with LEO, etc.
54

One caveat of our work is that the Archive updates each passing second so that if there were to be any incident not reported yet, our database might have some omissions of data.
However, we will continuously update it even after it is open to the public.
The proximal goal for our team is to finish the abstraction for 2015 ~ 2022 data within the next couple of months. Then we will move on to the data abstraction for the year 2023 and hopefully publicize the database by next year.
There are already quite numerous archives about officer-involved shootings. Still, our database will be unique as it heavily focuses on the victim’s behavioral/mental status during shootings beyond the scope of sociodemographic status. As I quote Dr. Crifasi, this project “can be used for literally anything”. We hope that our database can be utilized for further analyses of erratic behaviors of patients with mental disorders and how to control
those situations without any more fatal outcomes.
That pretty much sums up the introduction of what we hope to achieve through this concurrent project.
But there are still millions of milestones: to successfully address gun violence issues, we must consider both contributing factors towards the violence (i.e., our project) and firearm access controls. Examples of the latter are ‘Permit-to’ Purchase policies and Extreme Risk Projection Orders (a.k.a., ERPO), which in simple terms provide “red flags” for certain individuals to temporarily prohibit them from purchasing and misusing firearms.
Ultimately, as the center’s name suggests, we aim to resolve gun violence throughout the nation by providing scientific insight to legislative offices for sufficient prevention policies – the beauty of public health’s multidisciplinary nature with politics, in my personal opinion.
Author Biography
Junwoo Park is a Sophomore currently studing Public Health Studies. His interests lie in health policy and management, specifically regarding the field’s relation to patient care in the United States and beyond. Alongside studying Gun Violence, he also is interested in analyzing hospital epidemics.
55
Rob Walsh/Unsplash
Vaping: New Age Smoking With the Same Old Problems
Alicia Berger
Background
Smoking has been around for about 7000 years and has been wreaking havoc on people’s health ever since. However, beginning in the 1950s, researchers began to discover the health consequences of smoking. Publicizing these detrimental effects subsequently lead to a significant drop in smoking rates.
Recently vapes and e-cigarettes have been replacing traditional cigarettes, primarily among youth ages 18-24, including teenagers and children.3
E-cigarettes have quickly gained popularity since their release, increasing from 12% to 21% in just a year with projections showing an alarming number of youth vaping in 2030. Targeting youth with these addictive products, vaping companies ensure decades of repeat customers, ensuring decades of exposure to these toxic and carcinogenic chemicals. Vaping and its consequences have become an epidemic,4 whose health consequences will last decades.
Ironically, vaping was initially developed as a way to quit smoking, however, research at Johns Hopkins University shows that over 2 million teens and young adults use vapes as their first nicotine product.6 Vaping and e-cigarettes are less likely to be used to stop smoking, they are most likely used to start smoking. Data taken in 2019 shows that just over 17% of 8th graders report vaping, which almost doubles two years later when talking to 10th graders. Overall, about a third of high schoolers have reported vaping in the last year, a number that is continuing to rise.
Proven Health Risks
Vapes and e-cigarettes contain many of the same toxins as classic cigarettes.
These toxins, which have been extensively studied in cigarettes, are known addictive and carcinogens.3 When inhaled in a cigarette, these chemicals make you 15 to 30 times more likely to contract and die of lung cancer13 and 2 to 4 times more likely to have cardiovascular disease. While these numbers have yet to be recalculated for each type of vape or e-cigarette, since the same chemicals are being inhaled, the same results will likely result. Some of the substances in vapes and e-cigarettes include the following: 4
In addition to the fatal consequences of heart disease, cancer, and COPD that smoking is known to cause, many other diseases that are chronic and debilitating which diminish a person’s quality of life result from smoking. Furthermore, the nicotine and lead in vaping causes brain damage by negatively impacting synapse formation. This especially impacts adolescents whose brains are still developing.7 Lastly, researchers, in a study at Johns Hopkins University, also state that “there is evidence that young peo-
Chemicals Other Uses Potential Effects
Acetaldehyde Disinfectants, acetic acid, perfumes Carcinogen
Acrolein Common weed killer Can cause irreversible lung damage
Benzene Found in car exhaust Blood diseases, Carcinogen
Cadmium Toxic metal Breathing problems, chronic obstructive lung disease, emphysema
Diacetyl Food flavoring bronchiolitis obliterans, aka “popcorn lung.”
Diethylene glycol Anti-Freeze Toxic, Lung disease
Formaldehyde
Nickel, Tin, Lead and other heavy metals
Nicotine
Propylene glycol
Fertilizer, resin, embalming fluid, preservative Carcinogen, systemic poison
Metallic objects
Heavy metal toxicity damages functionality of lungs, brain, liver, kidneys and other organs.
Cigarettes, other prescription drugs Addictive, cardiovascular damage
Anti-freeze, food additive Carcinogenic
56
ple who vape are more likely to go on to use illicit drugs and tobacco products such as cigarettes”.6 So, the negative effects of vaping can lead to the proven and devastating consequences of smoking classic cigarettes and using other illicit drugs.
Potential Health Risks
Unlike traditional cigarettes, many ingredients in vapes and e-cigarettes are not closely monitored by the FDA. Furthermore, there are not set standards regarding these products, leaving researchers unaware of all the ingredients. Introduced in 2006,9 e-cigarettes’ short time on the market makes it hard to determine long-term consequences. The limited research on the long-term effects of these products and lack of regulation, which allows companies to use any substance in vapes, only adds to their danger.
Next Steps
To reverse this epidemic, it is crucial to understand why people are beginning to use e-cigarettes. With almost 70 years of warnings and information about the harmful effects of smoking, most people understand the ramifications of smoking. As such, most people who smoke classic cigarettes are doing so knowing the health risks. The same cannot be said for vapes.
Vaping is advertised as “safer” and “healthier” than smoking, a claim that does not appear to be true. Many youths do not know what they are smoking; they think it’s harmless flavoring.12 Furthermore, youth are known for being impressionable, so they are likely to believe that vaping is not so bad for their health. Unfortunately, the consequences of trusting this propaganda for some will be fatal.
So how do we stop this cycle? As vaping and e-cigarettes are very closely related to traditional cigarettes, we should use the same formula that was so successful in reducing smoking by 65% over the last 70 years. This formula has 3 steps.
1) Studying the short-term and longterm effects of vaping and e-cigarettes
2) Getting vaping and e-cigarettes under FDA to standard and monitor.
3) Publicizing the detrimental effects of vaping and e-cigarettes
If we do not follow these steps, vaping and e-cigarettes will continue to escalate and it will continue to wreak havoc on people’s health just as cigarettes did in the last century.
Works Cited
1. 2000 surgeon general’s report highlights: Tobacco timeline | smoking & tobacco use | CDC. https://www.cdc.gov/tobacco/ sgr/2000/highlights/historical/index.htm. Updated 2022. Accessed Feb 10, 2023.
2. McCarthy N. Poll: U.S. smoking rate falls to historic low [infographic]. Forbes Web site. https://www.forbes.com/sites/niallmccarthy/2018/07/26/poll-u-s-smokingrate-falls-to-historic-low-infographic/. Accessed Feb 12, 2023.
3. CDC. Products - data briefs - number 365 - april 2020. https://www.cdc.gov/nchs/ products/databriefs/db365.htm. Updated 2020. Accessed Feb 12, 2023.
4. Association AL. E-cigarettes, vapes and JUUL: What parents should know. https://www.lung.org/quit-smoking/e-cigarettes-vaping/e-cigarettes-parents. Accessed Feb 12, 2023.
5. Rowan HB. Vaping by the numbers. . 2019. https://khn.org/news/vaping-by-the-numbers/. Accessed Feb 12, 2023.
6. Johns Hopkins Medicine. Will vaping lead teens to smoking cigarettes? https:// www.hopkinsmedicine.org/health/wellness-and-prevention/does-vaping-leadto-smoking. Updated 2021. Accessed Feb 12, 2023.
7. Prasedya ES, Ambana Y, Martyasari NWR, Aprizal Y. Short-term E-cigarette toxicity effects on brain cognitive memory functions and inflammatory responses in mice. Toxicol Res. 2020;36(3):267-273.
8. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7351912/. Accessed Feb 12, 2023. doi: 10.1007/s43188-019-00031-3.
9. E-cigarette ingredients | nicotine, flavorings & toxic chemicals. Drugwatch. com Web site. https://www.drugwatch. com/e-cigarettes/ingredients/. Accessed
Feb 12, 2023.
10. National Institute of Justice. The evolution and impact of electronic cigarettes. National Institute of Justice Web site. https://nij.ojp.gov/topics/articles/evolution-and-impact-electronic-cigarettes. Accessed Feb 12, 2023.
11. Best states for education 2023. . . https:// worldpopulationreview.com/state-rankings/best-states-for-education. Accessed Feb 12, 2023.
12. Maryland. . . https://sexeducationcollaborative.org/states/maryland. Accessed Feb 12, 2023.
13. Vaping rises among teens. (2022, July 25). https://newsinhealth.nih.gov/2019/02/vaping-rises-among-teens. Accessed February 12, 2023 What are the risk factors for lung cancer? (2022, October 25). https:// www.cdc.gov/cancer/lung/basic_info/ risk_factors.htm. Accessed February 12, 2023
14. Jung, K., Jeon, C., & Jee, S. (1970, January 01). [PDF] the effect of smoking on lung cancer.https://www.semanticscholar.org/paper/The-effect-of-smoking-on-lung-cancer%3A-ethnic-andJung-Jeon/d4c19f6ed7d0c3eeaedfe45cf47568ee05447727. Accessed February 12, 2023
15. Tobacco use in maryland 2021. https:// truthinitiative.org/research-resources/ smoking-region/tobacco-usemaryland-20 Updated 2022. Accessed Feb 24, 2023.
16. Maryland vaping laws + taxes, https:// casaa.org/get-involved/state-locator/ maryland/. Updated 2023. Accessed Feb 24, 2023.
57
Why Are You Studying Public Health?
Wanli Tan and Kevin Mao
While Johns Hopkins University boasts an eclectic array of undergraduate and post-undergraduate degree programs, it can’t escape the notoriety of its pre-med program. Why then, are thousands of students each year drawn to study public health at the Bloomberg School of Public Health (BSPH)? In hopes of answering this, we asked current Bloomberg students one simple question: “Why are you studying public health?” and present their responses in this article with the hope that their stories may clarify any doubts, assuage any anxieties, and inspire Blue Jays interested in pursuing the field after their undergraduate careers, whether at Hopkins or elsewhere.
The broad consensus among BSPH students is that they’re motivated by the field’s ability to improve the lives of families and communities to make the world a better place, and they enjoy the intellectually challenging courses and opportunities the school offers. Of course, each student’s experience is unique. To illustrate these diverse motivations, this article will
focus on the personal stories of two students.
Kelsey Williams, who is pursuing a Ph.D. in Population, Family, and Reproductive Health (PFRH) with a concentration in Child Health, explains that leaving the world a better place than she found it is “morally vital” to her and the field of public health allows her to make progress towards that by creating concrete change. These beliefs motivated her to work in a hospital in Tanzania, where she witnessed disparate levels of access to maternal and child health care, which sparked her interest in tackling system-wide problems. As an undergraduate at Tulane University, she began her mission to serve others by evaluating a sex education and contraceptive access program implemented at Ngong Road Children’s Foundation in Kenya. Williams aims to continue learning about how social disparities unfold in childhood and how care systems can promote resilience and mitigate inequities in preparation for a career in “locally- and globally-engaged academic research and teaching to improve women, children, and
families’ health equity.”
For Kim DeFiori, a 2nd year Ph.D. student concentrating in Health and Public Policy, her interest in public health was motivated by mental health struggles from her time serving in the U.S. Army. Despite having no prior background in public health, she applied to the BSPH believing that “a public health approach was the best way to contribute to veteran mental health research.” There, she has received the guidance of valuable mentors and connected with multiple research teams focusing on LGBTQ+ veteran research. She has taken these experiences to create a nonprofit focused on expanding mental health access for first responders. DeFiori plans “to continue researching LGBTQ+ veterans, veterans’ mental health, and suicidality.”
The diverse motivations shared by Kelsey and Kim illustrate the desires of BSPH students to create change, address systemic disparities, and promote health equity, highlighting the uniquely transformative power of the field.

58
Tanner Ross/Unsplash
What Does Public Health Mean to You?

59

 Research
Shannon Wang Zao
Research
Shannon Wang Zao
FDA’s Project Optimus: Dose Optimization During Oncology Drug Development
Chujun Liu
Summary
This article discusses the U.S. Food and Drug Administration’s (FDA) Project Optimus, a recent initiative aimed at revising oncology drug development through dose optimization. Previously, oncology drug research was mostly conducted and approved at the maximum tolerated dose (MTD), but Project Optimus advocates for a shift toward identifying the most effective and safe dosage instead of defaulting to the maximum. Relying on MTD may result in poorly characterized doses because an increase in toxicity does not necessarily imply better efficacy. Applying at the MTD not only impacts patients’ quality of life but also leads to less accurate trial outcomes. The FDA drafted the Dose Optimization Guidance, naming it Project Optimus, which recommends the evaluation of multiple doses for efficacy, safety, and tolerability during preclinical stages. Project Optimus reflects a pivotal move towards a more nuanced approach to oncology drug development, prioritizing efficacy, safety, and a commitment to patient-centric care.
Introduction
Cancer, characterized by its life-threatening nature and substantial prevalence, has been a focus of drug development in recent decades. Despite considerable therapeutic advances, unmet medical needs such as lack of treatment or cures persist in most cancers, underscoring urgency in oncology drug development.1 Such characteristics have led to less stringent approval requirements for oncology drugs than for other drugs, reflected in reduced evaluation of optimized dosage that not only maximizes efficacy but
also minimizes toxicity.1,2 Historically, oncology drugs were frequently approved for administration at the maximum tolerated dose (MTD), which may not be optimal, as such dosage may bring excessive toxicity without improving efficacy. Applying drugs at MTD may lead to severe side effects and many other less desirable consequences.1 However, the days of unusually flexible standards for cancer drug effectiveness have passed, and the Oncology Center of Excellence (OCE), a division of the U.S. Food and Drug Administration
(FDA), has recently begun to restore criteria for reviewing and approving
The Origin of Project Optimus
In the development of oncology drugs, opting for the maximum tolerated dose (MTD) rather than thoroughly assessing the most optimal dose is a common approach due to the life-threatening nature of cancer and the need to provide timely new treatments to patients desperately seeking therapeutic options (rather than spending a significant amount of time to find the optimal dose).1,6 Thus, the highest tolerated dose for patients in the short term is often used for reg istering clinical trials and, ultimately, approval.5 However, the dosage deter-

oncology drugs to a standard aligned with other therapeutic areas through Project Optimus, which emphasizes the need to identify an optimal dosage during research and development.4 To begin, we will investigate the reasoning behind Project Optimus and why cancer drug approval regulations are necessary.
mined by MTD may be a poorly characterized dose that “provides more toxicity without additional efficacy”,2 as mentioned by OCE in its initiative for dose optimization. This is because the relationship between dosage, efficacy, and toxicity is not linear. In many cases, as dosage increases, efficacy levels out, while toxicity rises expo-
62
Figure 1: Dosage Efficacy vs Safety Graph
nentially. Thus, poorly characterized dosage leads to many negative consequences, including diminished quality of life of patients, reduced effectiveness resulting from the premature cessation of clinical trials due to intolerable toxicities, the need for constant modification in dose after approval, the need for further treatment due to severe toxicities, etc.1,2
Decades ago, when there was no treatment for tumors, the FDA decided to loosen the dosage requirements for oncology drug development to allow patients to receive more effective therapeutic drugs as quickly as possible. However, after decades of therapeutic advancements, the study designs and dosing assumptions prevailing in oncology drug development over the past decade are becoming obsolete,7 and the FDA has progressively shifted the focus of oncology drug development to drugs that ensure both efficacy and safety, optimizing the benefit-risk assessment.
In early 2023, the OCE department issued the Dose Optimization Guidance, which explains in detail the FDA’s requirements for new oncology drug development and design metrics to help pharmaceutical companies better understand the criteria for determining optimal doses.7 In October of the same year, the OCE department named this initiative Project Optimus, highlighting the suggestions for pharmaceutical companies to consider efficacy but also safety and tolerability in the development of new oncology drugs.2 This transition, while not explicitly written in as a revision of the FDA’s drug approval regulations, is an effort that the FDA wishes pharmaceutical companies to pursue. Indeed, a pattern for dose optimization can be seen in the pattern of FDA approvals of oncology drugs over the past decade.
Past Signs of Project Optimus
Although the OCE department only officially introduced “Project Opti-
mus” in 2023, the FDA has been trying to push the concept of optimal dosage in oncology drug review and approval for years prior.
The FDA has utilized different protocols to closely monitor approved drugs on the market. Post-marketing requirement (PMR) is one of such protocols issued as a condition of approval that requires pharmaceutical companies to continue gathering information on the safety, efficacy, and optimal dosage of the drug after receiving approval to enter the market.8 According to FDA’s clinical reviewer Brain Heiss
At times, efficacy does not improve with an increase in dosage, yet toxicity does. “ ”
and his colleagues, between 2010 and 2022, 15% of all approved new drugs underwent PMR, in which most were required to conduct research evaluating alternative dosages.4 Senior clinical pharmacology reviewer Dr. Fourie Zirkelbach and his colleagues also highlighted a similar finding in their article, emphasizing that a majority of those drugs employed MTD as the dosage.4 They further pointed out that this number cannot reflect the most accurate data as it likely underestimates the proportion of drugs requiring dosage readjustments. This is because the research was only conducted on approved drugs, despite there being many more drugs that were disputed or withheld during the drug approval process that may also need reevaluation.4
Such data suggests that even though the FDA did not explicitly state the
need for dosage optimization during clinical trials, the FDA’s focus on this matter is evident in the requirement for several drugs to reassess optimal dosages after they have been released on the market. After the initial attention to the optimal dosage of post-market oncology drugs, the FDA has shifted its focus to earlier oncology drug research. By doing this, they are ensuring that clinical research participants can also be best protected with safe dosages. Project Optimus is the ultimate deliverable of the FDA’s commitment on addressing oncology drug’s safety concerns.
A Close Read at the Dose Optimization Guidance
The FDA’s Dosage Optimization Guidance of Project Optimus outlines several recommendations for determining the optimal dosage for cancer drugs. One of its most crucial objectives is to ensure that clinical trials were designed in ways to compare multiple dosages and examine corresponding safety and tolerability.7
This guide recommends that pharmaceutical companies shift their practice from identifying only the maximum tolerated dose to selecting several doses for further evaluation of the degree of activity, safety, and tolerability using preclinical data,6 where an optimal dose is chosen after weighing the options. The OCE stresses in the guide that the goal of this project is to “adequately characterize the doseand exposure-response analyses for safety and efficacy.”7 In other words, aiming to identify the optimal dosage that maximizes safety without compromising efficacy. The OCE directors Mirat Shah, Atiqur Rahman, Marc R. Theoret, and Richard Pazdur comment that “this will prevent exposure of a large number of patients to a dose that may cause excessive toxicity or be less efficacious.”6
Several case studies have shown the importance of testing several dosages. At times, efficacy does not improve
63
with an increase in dosage, yet toxicity does. A study has been done on the efficacy of different dosages of Pembrolizumab, a drug used to treat patients with advanced melanoma and non–small cell lung cancer, which the result has shown no clear difference in efficacy for a dose of 2 or 10 mg/kg.9 Another study on the exposure-response analysis of Batiraxcept, a drug designed to control metastatic disease of aggressive cancers, has also shown no additional benefit at a higher dose of 20mg/kg compared to that of 15mg/kg.10 Under such circumstances, where the efficacy is similar between the lower and higher doses, there would be no need to opt for the higher dosage. However, such information would not be known if the pharmaceutical company only administered the maximum tolerated dosage without conducting further research, further emphasizing the importance of Project Optimus’ role in drug research and development.
Conclusion
The FDA’s recent introduction of Project Optimus marks a pivotal shift in oncology drug development, advocating for a more nuanced approach to dosage determination. The historical reliance on the maximum tolerated dose (MTD) is being reconsidered. The shift is towards a comprehensive assessment that prioritizes both efficacy and safety. This transition, as pointed out in the announcement for Project Optimus, is a crucial step towards ensuring that patients receive the most effective treatment without unnecessary exposure to extra toxicity.
The FDA’s proactive initiatives, including PMR and an expanded focus from post-market drugs to early-stage research, signal a commitment to refining dosage strategies. At the time when there were no drugs for cancer at all, the FDA’s mission was to make drugs available to patients as quickly as possible, and all policies were enacted to serve this goal. Yet, with
more drugs entering the research and development phase or even reaching the market, the FDA must now focus more on reviewing whether the safety of the drugs meets the needs of patients, justifying the enactment of Project Optimus. As the field evolves, the FDA will likely continue revising the oncology drug development process, underscoring the commitment to a patient-centric, data-driven paradigm. With more cancer drugs on the market, the FDA’s requirements for new drug development will most likely become more stringent, raising the bar on not only the effectiveness but more importantly the safety of new drugs
References
1. Fourie Zirkelbach J, Shah M, Vallejo J, et al. Improving dose-optimization processes used in oncology drug development to minimize toxicity and maximize benefit to patients. Journal of clinical oncology. 2022;40(30):3489-3500. https://search. proquest.com/docview/2714063338. doi: 10.1200/JCO.22.00371.
2. U.S. Food & Drug Administration. Project optimus: Reforming the dose optimization and dose selection paradigm in oncology. U.S. Food & Drug Administration Web site. https://www.fda.gov/about-fda/ oncology-center-excellence/project-optimus. Updated 2023.
3. Guo B, Yuan Y. DROID: Dose‐ranging approach to optimizing dose in oncology drug development. Biometrics. 2023:1-13. https://www.ncbi.nlm.nih.gov/ pubmed/36807110. doi: 10.1111/biom.13840.
4. Heiss B, Pan L, Akalu A, et al. Dosage optimization in drug development: An FDA project optimus analysis of postmarketing requirements issued to repair the cracks. Journal of clinical oncology. 2023;41(16_suppl):1598. doi: 10.1200/ JCO.2023.41.16_suppl.1598.
5. Shah M, Rahman A, Theoret MR, Pazdur R. The drug-dosing conundrum in oncology — when less is more. The New England journal of medicine. 2021;385(16):1445-1447. https://nejm.org/ doi/full/10.1056/NEJMp2109826. doi: 10.1056/NEJMp2109826.
6. Shah M, Rahman A, Theoret MR, Pazdur R. How to get the dose right. The ASCO Post Web site. https://ascopost.com/issues/may-10-2022/how-to-get-the-dose-
right/. Updated 2022.
7. U.S. Food & Drug Administration. Optimizing the dosage of human prescription drugs and biological products for the treatment of oncologic diseases; draft guidance for industry; availability. U.S. Food & Drug Administration Documents. 2023:1-10. https://www.fda.gov/media/164555/download.
8. U.S. Food & Drug Administration. Postmarket requirements and commitments. U.S. Food & Drug Administration Web site. https://www.fda.gov/drugs/drug-approvals-and-databases/postmarket-requirements-and-commitments. Updated 2023.
9. Turner DC, Kondic AG, Anderson KM, et al. Pembrolizumab Exposure–Response assessments challenged by association of cancer cachexia and catabolic clearance. Clinical cancer research. 2018;24(23):58415849. https://www.ncbi.nlm.nih.gov/ pubmed/29891725. doi: 10.1158/1078-0432. CCR-18-0415.
10. Mcintyre G, Rangwala R, Dodds MG, Barriere O. Abstract CT506: Exposure-response analysis of batiraxcept and application to recommended phase 2 dose in platinum-resistant ovarian and clear cell renal cancers. Cancer Research. 2022: CT506-CT506. https://doi-org.proxy1.library.jhu.edu/10.1158/1538-7445.AM2022CT506
Biography
Chujun Liu, originally from Beijing, China, is a first-year undergraduate student at Johns Hopkins University, majoring in Molecular and Cellular Biology. In addition to academic pursuits, Chujun finds joy in playing the flute, engaging in handcrafts, and immersing in diverse musical genres during free time.
64
Antibiotic Overprescription: Analyzing Possible Causes Within Asian Immigrant Communities
Timothy Huang
Summary
Antibiotic resistance is a major growing public health problem, and one of the main ways of addressing this issue is understanding the main ways antibiotic over-prescription affects usage of antibiotics. Different demographics of people have different usage levels of antibiotics - this paper serves to analyze some of the possible reasons for these differences in antibiotic usage and proposes a way to study these differences.
Introduction
The discovery and widespread use of antibiotics is one of the pinnacle innovations that define modern medical practice. Many hospitals around the world use antibiotics to treat acute respiratory infections, such as pneumonia, Staphylococcus aureus, and strep throat. However, with the increased prevalence of antibiotic use comes the problem of antibiotic over-
prescription: 40% of antibiotics are prescribed when a viral infection is present, which renders the antibiotic useless as antibiotics are only used for bacterial infections.1 While the antibiotic prescription rate has decreased during the COVID-19 pandemic, antibiotic treatment rates still widely vary across the nation—some states having more than one prescription per 1,000 people.2 The effect of antibiotic overprescription results in higher risk of antibiotic-resistant bacterial infections. Antibiotic resistance is a major public health problem, resulting in increased severity of diseases, mortality rate, healthcare costs, and infection rates. As a result, antibiotic-resistant bacteria such as Methicillin Resistive S. aureus or resistant tuberculosis are responsible for more deaths than HIV/ AIDS, Parkinson’s disease, and homicide combined.3 To reduce the risk of antibiotic resistance, we need to lower the overconsumption of antibiotics. The first step towards this goal is to
identify which populations are at risk to over-consume antibiotics and receive unnecessary antibiotic prescriptions.
Upon characterizing the main consumers of antibiotics, there exists a racial gap, rather than only an economic gap, between how antibiotics are being prescribed to patients. While there is no significant difference in antibiotic prescription between social classes, White, Hispanic, and Asian patients are prescribed antibiotics at higher rates compared to Black patients.4,5 Additionally, race is a major factor in perception of antibiotics: regardless of diagnosis, non-Hispanic Whites sought antibiotic use 51% of the time for their children with a respiratory illness, while Asian and Hispanic families sought antibiotic use 80% of the time for their children.4 Latino and Asian immigrant parents were both 17% more likely to report that antibiotics were either definitely or probably

65
Myriam Zilles /Unsplash
necessary compared to non-Hispanic White parents.4 Higher expectations for antibiotic use influence physicians, who are 21% more likely to prescribe antibiotics to patients who expect antibiotic use, perpetuating the use of antimicrobial agents even when they are not needed.4 Many Hispanic immigrants believe in the idea of ‘self-diagnosing’ their own children and want antibiotics on hand, which explains why they might request more antibiotics.6 However, this same belief may not be as strongly represented within Asian immigrant populations as there is no data; thus, we cannot accurately use this belief of self-diagnosis to describe Asians are more willing to request antibiotics from physicians. Thus, the question remains: what are the main factors that explain why Asian immigrants have higher expectations for antibiotic use?
I believe that because Asian immigrants want to view the doctor-patient relationship as an informal relationship, as Asian immigrants may have difficulty forming trust and loyalty within their doctor-patient relationship, which leads them to visit their doctors only when they feel the need to be prescribed medication8. Therefore, Asian immigrants might have higher expectations for antibiotic prescription when they see their doctors, which often can lead to overprescription. Knowing the main reasons why Asian immigrants request more antibiotics can inform us more about how Asians view the patient-doctor relationship and show us how to decrease antibiotic overprescription within populations that are at greatest risk.
Doctors as Peers
Previous literature has shown that Asian communities view the doctor-patient relationship differently than other races8. Patients tend to view the doctor-patient relationship through four elements: trust, knowledge, regard/support, and loyalty.7 However, Asian immigrants put a higher emphasis on loyalty and trust
compared to other races. Studies have found that while native-born Americans expect a transactional relationship with their doctors; Asian immigrants want to form personal relationships with their doctor and view them as an informal peer.8
The difference between Asian immigrant and White perceptions of the doctor-patient relationship could be due to the American healthcare system. In America, the doctor’s main role is to diagnose and prescribe medicine to alleviate health symptoms. Thus, individualist Americans, believing in the importance of self identity, are likely to view the doctor as a vehicle for improving their own individual health and thus would not form a close connection with their doctors.
High loyalty is valued in doctor-patient relationships for Asians. “ ”
On the contrary, Asian cultures emphasize collectivism, the idea that one’s role in society is most important, and might view their doctors as caregivers for the whole community. Asians may treat doctors with great respect, trust, and loyalty, as they believe doctors provide irreplaceable services to families. Due to these beliefs, Asians may incorporate doctors into their personal circles to thank them for their services. However, these connections take time to form. In the United States, among an individualist culture, it may be harder for Asians to form deeper doctor-patient relationships as many doctor-patient connections may be seen as more transactional rather than a way to create an understanding between doctors and patients. I believe Asian immigrants spend more
time compared to other populations finding a doctor that aligns with their desired doctor-patient relationship, contributing to a higher level of initial distrust.
Failure to Trust Doctors
Since high loyalty is valued in doctor-patient relationships for Asians, I hypothesize that Asian immigrants in low-trust relationships would be more skeptical about going to the doctor for routine medical visits. As previously stated, many Asian immigrants believe in the idea of collectivism, where the doctor-patient relationship is integral for Asians to trust a doctor’s advice. As many Asian households may struggle to create this doctor-patient relationship, Asian households would attempt to provide home remedies and care to minimize the impact of disease, and try to avoid doctors unless they believe medicine is absolutely necessary. That means that only serious diseases that cannot be stopped by these home remedies would make Asian immigrants consult a doctor. Thus, Asian immigrants enter the doctor’s office already expecting their doctors to provide some sort of medical relief for their symptoms, which usually falls back to antibiotic use. Here, we find a possible main factor that cause Asian immigrants to have higher expectations for antibiotic use whenever they consult a doctor: due to the difficulty in forming good relationships with their physicians, Asian immigrant patients will only visit the doctor when they expect antibiotic use is needed for illness. With these increased expectations, Asian immigrants are more likely to receive an antibiotic prescription, even when it’s not needed.
Testing the Hypothesis
My hypothesis—the mistrust in the doctor-patient relationship between Asian households contributes to an increase in antibiotic prescription— relies on how much trust Asian immigrants have in their relationships with
66
their doctor and how often Asian immigrants visit their doctors. I propose conducting qualitative interviews with first-generation Asian immigrants in the United States regarding their doctor-patient relationships and medical behaviors. The interview could include the following questions:
- How long have you known your doctor?
- Have you had any extenuating illnesses in the past year?
- How often do you visit your doctor for routine visits?
- How often did you visit your doctor for non-routine visits in the past year? What are some of the main reasons?
- How often do you receive medication from doctor visits?
- Has your doctor prescribed you antibiotics within the last year for any disease? Did you ask for the medication?
- What is your relationship with your doctor? Is it friendly to the point of peers, or a business-like relationship?
- Do you think that your doctor provides you with adequate medical care in your best interest?
- How might you want to change your relationship with your doctor?
We would plan to include some possible confounders such as age, chronic illnesses, and family size.
Surveying Asian immigrant populations will give us insight to the closeness of their doctor-patient trust levels.If the hypothesis is correct, survey participants who indicate higher levels of friendliness with their doctors would likely correlate with lower levels of antibiotic prescriptions. While it might be necessary to stratify populations such as patients with chronic illness, the general thought is that lower levels of loyalty between the doctor and the patient would create distrust, which would also be shown through the survey results. Additionally, if patients who report higher antibiot-
ic prescriptions in the last year have known their doctor for less time, that might mean the doctor-patient relationship hasn’t matured to the level of a peer-like connection. The experiment would aim to examine if the lack of a close doctor-patient relationship within Asian immigrants is a possible cause of uncertainty within patients visiting for medical assistance, promoting the use of antibiotics.
Possible Limitations and Future Discussions
There are a few limitations with the survey. First, the Asian immigrant population is underrepresented in medical studies within the United States. Finding data for these groups could be hard and potentially misleading if Asian immigrants struggle with understanding the questions due to language barriers. Additionally, there is a lot of heterogeneity within the Asian immigrant population, such that Japanese immigrants may feel differently about the importance of the doctor-patient relationship compared to Chinese immigrants. This may make it difficult to measure cultural differences within the umbrella term of ‘Asian immigrant.’
Lastly, there is always the chance that the hypothesis is not supported. Perhaps after surveying the Asian population, we find that there is no correlation between trust and loyalty a survey participant has with their doctor and the amount of antibiotics taken or prescribed. Having more trust and loyalty could even potentially prompt patients to take more antibiotics. Both of these results would still be interesting phenomenons. If no association is found, there is likely more to the doctor-patient relationship that Asians value than just the peer relationship. If trust and loyalty are null factors in antibiotic overprescription, perhaps overprescription isn’t a judgment from the patient, but rather the doctor. Then we can refocus sociological discussion about antibiotic prescription to how doctors treat patients
differently in terms of possible preferential treatment or racial biases. If the results from the survey indicate that additional trust and loyalty increases antibiotic prescription, we can look into if a better doctor-patient relationship yields preferential treatment, and whether this correlation is greater within Asian immigrant communities.
If Asian immigrants do exhibit higher expectation levels for antibiotic use when their doctor-patient relationship doesn’t have a high level of loyalty, we could use this new causal factor to find new solutions on fixing the antibiotic overprescription crisis. This hypothesis would tell us that the ways patients view the doctor-patient relationship could be the main contributors to antibiotic overprescription. By understanding how Asian immigrants approach antibiotic use through the perception of their doctor-patient relationship, we could better understand how health and medicine are closely linked with our relations with medical professionals. Then, knowing a possible causal factor for antibiotic overprescription, it becomes possible to investigate methods that increase trust between doctors and patients and explore if that can help decrease antibiotic overprescription rates across the United States.
References
1. Barlam T.F., Soria-Saucedo R, Cabral H.J., Kazis L.E., Open Forum Infectious Disease. Unnecessary Antibiotics for Acute Respiratory Tract Infections: Association With Care Setting and Patient Demographics. Available at: https://academic. oup.com/ofid/article/3/1/ofw045/2460983. Accessed March 29th, 2023.
2. Centers for Disease Control and Prevention, CDC. Antibiotic Use in the United States, 2022 Update. Available at: https://www.cdc.gov/antibiotic-use/stewardship-report/current.html. Accessed March 29th, 2023.
3. Llor C, Bjerrum L, Therapeutic Advances in Drug Safety. Antimicrobial resistance: risk associated with antibiotic overuse and initiatives to reduce the problem. Available at: https://www.ncbi.nlm.nih. gov/pmc/articles/PMC4232501/. Accessed April 3rd, 2023.
67
4. Mangione-Smith, R, et al., American Academy of Pediatrics. Racial/Ethnic Variation in Parent Expectations for Antibiotics: Implications for Public Health Campaigns. Available at: https://doi. org/10.1542/peds.113.5.e385. Accessed April 7th, 2023.
5. Barlam T.F., et al., Infectious Control Hospital Epidemiology. Antibiotics for Respiratory Tract Infections: A Comparison of Prescribing in an Outpatient Setting. Available at: https://www.cambridge.org/core/journals/infection-control-and-hospital-epidemiol ogy/article/ antibiotics-for-respiratory-tract-infections-a-comparison-of-prescribing in-an-outpatient-setting/54A43205696D8BCE7245AA10E47C4E29. Accessed April 7th, 2023.
6. Mainous A.G., et al., Emerging Infectious Disease. Nonprescribed Antimicrobial Drugs in Latino Community, South Carolina. Available at: https://wwwnc.cdc.gov/ eid/article/11/6/04-0960_article. Accessed April 7th, 2023.
7. Chipidza F.E., Wallwork R.S., Stern T.A., Primary Care Companion for CNS Disorders. Impact of the Doctor-Patient Relationship. Available at: https://www.ncbi. nlm.nih.gov/pmc/articles/PMC4732308/. Accessed April 14th, 2023.
8. Nilchaikovit T, Hill J.M., Holland J.C., General Hospital Psychiatry. The effects of culture on illness behavior and medical care: Asian and American differences. Available at: https://doi.org/10.1016/01638343(93)90090-B. Accessed April 10th, 2023.
Biography
Tim Huang is a sophomore studying Public Health with a minor in Accounting. In his free time, he likes to play random piano songs, spin fire, and edit videos. His ultimate goal is to become a doctor in infectious disease.
Navigating Public Health Research as Hopkins Students
Research Team
Public health research at Johns Hopkins University is a rich and fulfilling journey for students like Jonathan Ye, Jasmine Wu, Davin Kim, and Christine Kim. Their diverse experiences highlight the diversity
within public health and its investigative methods, as well as providing a more personal account of growth and reflection. The research editing team at Epidemic Proportions hopes that sharing these interviews may encourage other students who have an interest in public health or research to get involved!
Jonathan Ye’s Exploration of HIV and Cognition:
Jonathan, a junior majoring in Public Health and Applied Math and Statistics, is engaged in groundbreaking research on HIV and cognition. Drawing from his high school experience in microbiome research, Jonathan employs coding, data analytics, and R, programming language, to explore patterns in cognition among HIV patients living in Uganda. His project
Be comfortable being uncomfortable!! “ ”
aims to discover more about how HIV affects daily life and generate new research. Jonathan hopes to fill gaps in existing public health literature, particularly for underrepresented groups.
Jasmine Wu’s Contribution to Opioid Use Disorder Research:
Jasmine, also a junior majoring in public health, delves into the impact of opioid use disorder on Baltimore City. Her involvement in data analysis and report writing aims to identify areas of concern and inform future prevention and treatment initiatives, particularly through the efforts of community organizations. Jasmine’s interest in seeing how policy can affect the wellbeing of millions at a time, in contrast with individualized medical care, is what first drew her to public health research. Working in a team of community experts in opioid use disorder has exposed her to the public
health work being done by grassroots organizations and community focus groups.
Davin Kim’s Exploration of Cryptococcal Polysaccharides:
Davin, a sophomore studying molecular and cellular biology, takes on the challenge of understanding the polysaccharide capsule of Cryptococcus neoformans, which is a common fungal agent impacting AIDS patients. It’s believed that the polysaccharide capsule plays an important role in establishing host infection. His research involves developing analytical techniques to characterize exopolysaccharide and capsular polysaccharide samples and identify key differences in their structure and composition. Davin’s work not only contributes to the understanding of fungal diseases but also emphasizes the significance of reliable analytical methods, laying the groundwork for future investigations.
Christine Kim’s Journey in Dysautonomia and Oncology Research:
Christine, a junior studying public health and molecular and cellular biology, navigates two distinct research paths at Hopkins. At the JHMI Department of Surgery, she conducts patient interviews and designed a study to better understand dysautonomia, or autonomic nervous system dysfunction, by identifying related symptoms. Additionally, her experience at Juntendo University Medical School in Tokyo, Japan, involves investigating the tumor microenvironments and developing cell culture techniques. Christine’s contributions extend to providing hope for patients with dysautonomia, a poorly understood disease, and advancing knowledge in oncology. She is passionate about biostatistics and epidemiology, and also works as a Direct Support Professional for young adults diagnosed with autism.
68

Shared Lessons and Advice:
There was great diversity among the four experiences in public health research, most clearly shown by the different research topics. Public health is such a broad field, and its research can take many focuses, methodologies, and scales, from the national to community level. Surprisingly, everyone interviewed has very different reasons for becoming involved in public health research, highlighting the many different paths students took to get involved. Some of the lessons learned have also influenced what these students would like to do after their time at Hopkins. Davin shares:
“Although much of my work is more technical in nature, my experiences so far have helped me realize that academic research is not conducted in a vacuum. Rather, this research occurs in the context of a “bench-to-bedside” philosophy wherein laboratory findings can also bring about practical applications in clinical settings to directly improve patient outcomes. This experience in translational research
has led me to consider pursuing medical research through a PhD after completing my undergraduate education.”
A common thread between the interviews is the collaborative nature of research, learning from mentors, and engaging in team processes to troubleshoot any bumps in the road. Jasmine mentioned that team meetings were essential to “cutting through fluff and finding key takeaways to focus on, which guide what we would work on until our next meeting.”
Challenges are embraced as opportunities for growth, and communication is key to sharing findings. As Jonathan said, “I think research is very forgiving in that you don’t have to be the best coder or writer, you just have to be consistent. It’s also a team process.”
As these students continue their journeys in public health research, they exemplify the commitment, passion, and impact that define the research culture at Johns Hopkins University. They hope to inspire future undergraduates to embark on their own
paths, contributing to the ever-evolving landscape of public health and filling in necessary gaps in existing research to better address all health needs. As students embark on their research journeys, Christine offers some valuable advice:
“Be comfortable being uncomfortable!! It’s going to be difficult cold emailing researchers, getting no response back, and even receiving a flat out rejection after waiting. Just remember to keep emailing, to keep networking, and you’ll have the opportunity to find research that suits you. If you realize after starting that you’re not as interested in the topic as you initially thought, don’t be afraid to look for new opportunities and to explore! This is the time to really find out what you’re passionate about.”
69
Bermix Studio/Unsplash
Epidemic Proportions Staff 2023-2024

Wassim Bouhsane Editor-in-Chief.

Jasmine Wu Research Editor.
Research Staff
Louie Martinez
Jaswanth Vandrasi
Lance Xu
Anush Polamraju
Akshita Kikkuru
Christine Kim
Arindam Bagga
Jason Han

Neha Skandan Editor-in-Chief.

Shaan Shabbir Policy Editor.
Policy Staff
Jason Soo
Wanli Tan
Pranav Kotamraju
Tanisha Taneja
Kevin Mao
Rongrong Yan

Habin Hwang Features Editor.
Features Staff
Tanisha Luthria
Laura Fan
Katalina Li
Ameerah Jones
Kay Mi
Greta Persian
Curie Lee
Vivian Guo
70

Godoy

Wilson Huang Editorial Editor.
Editorials Staff
Esha Cyril
Samuel Yeboah-Manson
Pearl Shah
Jayvik Joshi
Nicholas Redmond
Sittha Cheerasarn
Hyeongmin Cho



Marketing and Outreach Saff
Nella Tummala
Connie Huang
Nancy Yan
Chris Sulca
Layout Staff
Tim Huang
Rose Chen
Shannon Xiao
Niki Zouzoulas
71
Martine Bigos Treasurer.
Carlos Haring Layout Editor.
Lola
Marketing and Outreach.
Jas Vandrasi Marketing and Outreach.

72

73




 Neha Skandan Wassim Bouhsane
Neha Skandan Wassim Bouhsane
 Joshua M. Sharfstein, M.D.
Joshua M. Sharfstein, M.D.



 Features
Shannon Wang Zao
Features
Shannon Wang Zao
























 Policy
Shannon Wang Zao
Policy
Shannon Wang Zao

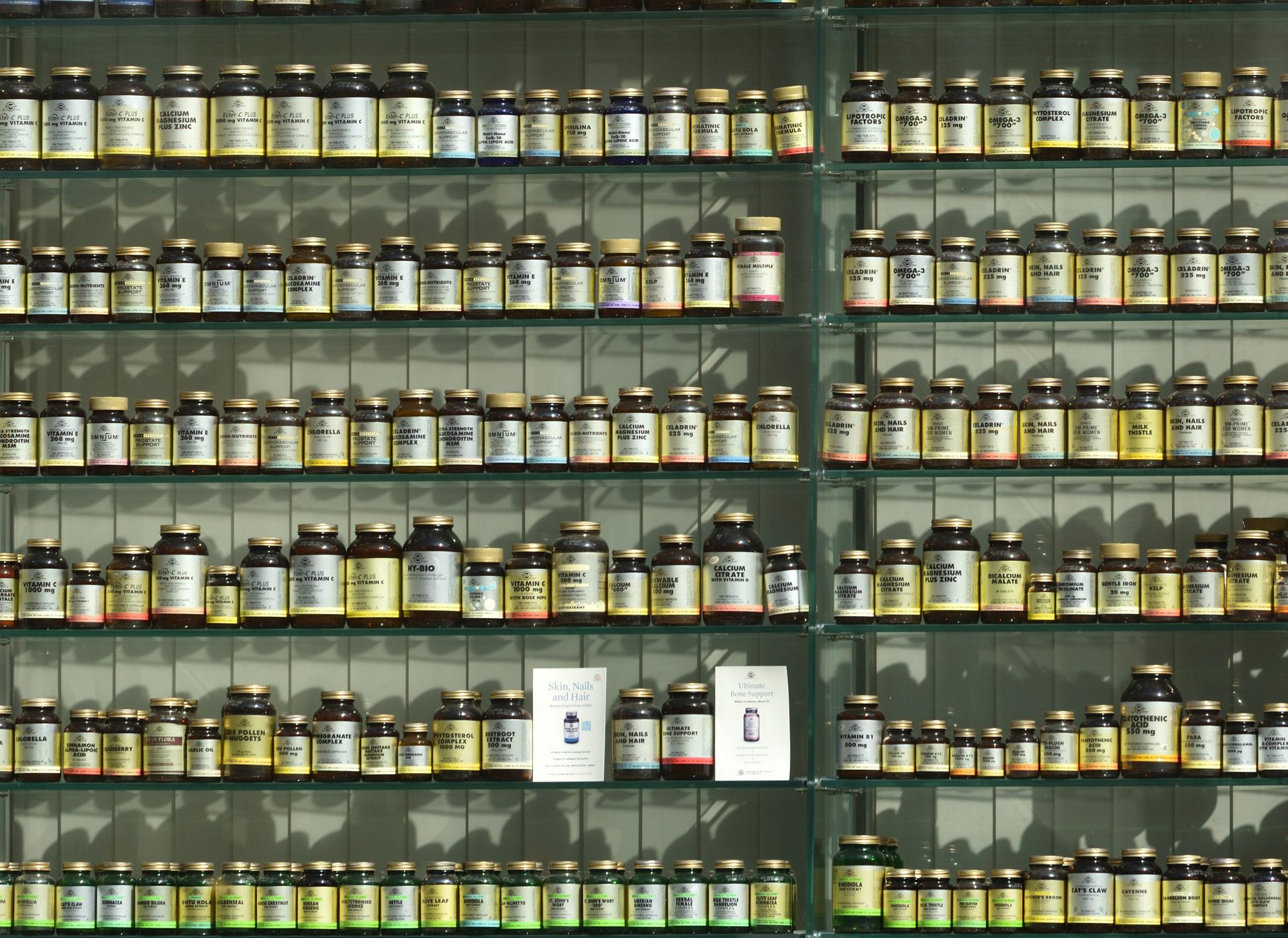







 Research
Shannon Wang Zao
Research
Shannon Wang Zao














