PRESIDENT’S MESSAGE
Cooperation and the Common Good
It is my pleasure to report to our Association that the CPMA Board has been hard at work addressing the issues that affect us all. It is difficult to know what each year will bring, but the challenges that present themselves must be attacked with an end goal in mind. Win or lose, we must play the game and play hard.
I find myself and our Board in the heart of a very important time of transition for our profession. The changes that will occur in the next few years will advance our profession more than any other segment of time in our history. We have been working diligently for the past ten years building relationships with our Allopathic and Osteopathic Physician Colleagues in the hopes that one day the end result would be a better future for all. The idea of collaborating with our MD and DO counterparts was at one time considered a distant reality. It was our goal to not identify our differences but to
recognize our similarities, and we have done just that.
As the healthcare system evolves, it continually demonstrates the need for a more collaborative healthcare model. With the onset of the Affordable Care Act and the Accountable Care Organization’s requirements that we all work together to bring healthcare costs down, Podiatric medicine has evolved as one of the most cost-effective and integral parts of that system. The value a Podiatric physician brings to any organization or group is tremendous, and this will be our biggest advantage in these changing times.

DOCTORS ARE PATIENTS’ BEST

CPMA LEGISLATIVE LEADERSHIP CONFERENCE
W ednesday, M arch 4 ~ 9 a M to 5:30 PM t he c itizen h otel • 926 J s treet • s acra M ento , ca




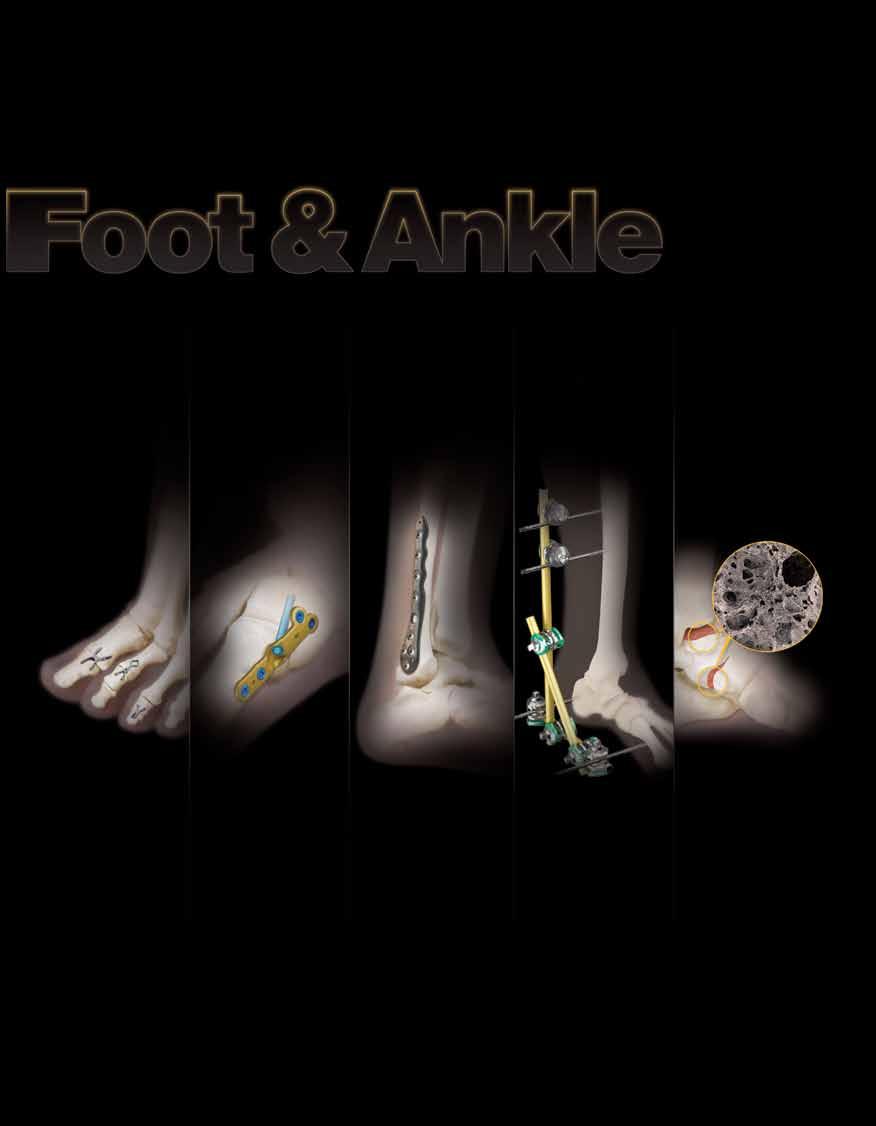
Western Foot and Ankle Conference
June 25 – 28, 2015
Disneyland Hotel & Convention Center Anaheim, California

• Economically conscious registration rates
• 25 CE contact hours
• 10 radiology CE contact hours
• Dynamic lecture tracks
• Distinguished faculty
• Innovative instructional courses
• Hands-on surgical workshops
• ICD-10 Updates
• PICA presentation
• 3-day educational seminar for podiatric medical assistants including radiology credits
• 3 days of exhibits
• Exceptional room rates at the Disneyland Hotel and Grand Californian Hotel & Spa
• Significant savings on Disneyland & California Adventure Park Passes
• Optimal location near shopping, dining, entertainment and more!
Come for the meeting; Stay for the magiC of DiSneylanD’S DiamonD Celebration
You are invited to attend the party of the year, as the Happiest Place on arth celebrates its 60th Anniversary with thrilling new rides, dazzling displays, peppy parades, and spectacular shows and surprises!
After mornings of inspired earning in innovative instructional courses, hands-on-workshops and hot topic lectures, attendees of the 2015 Western Foot and ankle Conference (one of the nation’s premier podiatric surgery, medicine, management conferences and exhibitions) will be able to enjoy evenings with families and friends as they join in the celebration. And, Western attendees receive significant savings at Disneyland Resort hotels, and on Disneyland and Disney’s California Adventure theme parks tickets.
The 2015 Western Foot and Ankle Conference (June 25-28) is your e-Ticket to education and fun!
B ECOME AN A DVOCATE f OR YO u R PATIENTS AND P RO f ESSION !
Mark your calendars now and plan to attend the California Podiatric Medical Association’s (CPMA) 2015 Legislative Leadership Conference on Wednesday, March 4. The conference will take place at the lovely Citizen Hotel, just three short blocks (a quick 10 minute walk) from California’s majestic State Capitol Building.
The morning breakfast briefing will be followed by luncheon with invited guest speakers, after which attendees will head to the Capitol Building to meet with their legislative representatives.
Following their legislative visits, attendees will return to the Citizen Hotel for refreshments and to share their experiences.
This is a unique event for podiatric physicians and is free of charge to all CPMA members. Plan to join more than 100 podiatric physicians, residents and medical students who will be coming to Sacramento to educate their legislative representatives about the critically important role podiatric medicine has in the healthcare system, and to help ensure that the people of California have access to necessary, quality podiatric medical treatment and care.

CPMA staff continues their tradition of personally donating to provide food and toys to needy families during the holiday season.

Time TO Talk Turkey
Like it or not, politics have a major impact on the podiatric medical profession. All licenses to practice podiatric medicine in California are issued by the State of California. The statutes and regulations which govern your practice are ultimately determined by our state legislators in Sacramento. These one hundred and twenty elected representatives are routinely called upon to approve or reject legislation that has a direct bearing on the nature and practice of all health professions - including podiatry.
The California Podiatric Political Action Committee (CalPPAC) is a non-profit, non-politically aligned organization run by DPMs for the betterment of DPMs . CalPPAC educates elected and appointed government officials about the critical role podiatric medicine plays in California’s healthcare delivery system. It also assists those legislators and candidates for public office who appreciate and support the podiatric medical profession.
CalPPAC opens doors for dealing with an array of legislative and regulatory issues of interest or concern to California’s DPMs, including: licensure, hospital privileges, scope of practice, insurance, professional discipline, and practice regulations … to name just a few.
Your contribution will help to ensure that the voice of podiatric medicine is heard in Sacramento, where the important decisions are made that affect your patients, practices and profession as a whole.
Remember, a single stroke of the pen can write podiatry into - or out of -the law.
Please send your contribution today to:
CalPPAC, 2430 K Street, Suite 200 Sacramento, California 95816.
To use your VISA , MasterCard or American Express call toll free (800) 794-8988 Or, donate online at CalPPAC.org
Ask yourself -

Common Good
I recently came upon a website for a nonprofit organization in Europe called “Association for the Advancement of the Economy for the Common Good”. They outline 20 principles that describe their values and guide their mission.
Their first principle states that the basis for the Economy of the Common Good are “collectively shared values that contribute to fulfilling interpersonal relationships… confidence building, cooperation, appreciation, democracy, solidarity”. These relationships are a key factor in happiness and motivation. I was so moved by this idea as I saw it consistent with what we at CPMA strive to achieve on a daily basis.
We must all cooperate and appreciate each other for what we have to offer. Degree aside, we are all on the same team: the team that provides healthcare for the state of California and the patients it serves. We win together, or we lose together. Aligning our strategies can only be accretive in the end. If we shift our strategies from competition to cooperation, the common good will prevail. And while profit and competition is still possible, it becomes less of the focus and more of the byproduct. Most of us in private practice have realized this over time by hiring an associate, consolidating offices and taking advantage of economies of scale. Those in larger HMO healthcare centers and medical groups have realized the benefit of this model for quite some time. This can also happen on a larger scale locally, statewide or even nationally.
Cooperation
Our Physician and Surgeon initiative here in California exemplifies a cooperative effort with our allies as we pursue a common good. The Task Force has had a very active year, finishing up its school and residency site visits just a few months ago. The results of our hard work have shown that we are in fact much more similar than we are different. We are all going to be affected by the inevitable outcome of this Task Force and the stakeholders therefore include all of us; for we will all benefit from the changes associated with the outcome of a Physician and Surgeon license.
Earlier this year the executive leadership of CPMA was invited to participate as fellow physicians at the Western Healthcare Alliance meeting in San Diego. The relationships we have built with CMA allowed us to participate at a level that has been unprecedented. While at that meeting we were personally invited by the Executive Director and CEO of the California Medical Association, Dustin Corcoran, to attend a private training session on MICRA, the Medical Injury Compensation Reform Act. We were privy to the ground floor discussions about how to approach the potential threat to the stability of healthcare in California. What emerged from that meeting was a CPMA strategy for aggressive fundraising
and patient education on what eventually became Prop 46. This cooperative effort initiated by CMA including our Association has paid big dividends for everyone. Thanks to all of your efforts we were able to fundraise aggressively in the first 6 months of this year followed by development and implementation of a comprehensive physician and patient education plan to defeat Prop 46.
Our Cooperative efforts did not stop there! While our Medi-Cal Bill AB 1868 was stalled in the Senate Appropriations Committee due to opposition from the Department of Finance, it was the DHCS that admitted their policies were unclear and confusing for Podiatric providers. What this did was allow us to open up discussions on the topic resulting in a change in their administrative policy allowing our services to be covered in emergency room and in-patient hospital settings. None of this would have happened without the right people in the right place looking for a common good and a common goal. Our legislative advocate Jodi Hicks has been busy behind the scenes strengthening her relationships, and this has resulted in a positive outcome for our members. CalPPAC funds have been instrumental in supporting those efforts. Please continue to donate as you have in the past so we can continue to support those legislators who support our agenda.
Let us continue to embrace the idea that we will always achieve much more together than we will apart. The Economy for the Common Good is neither the “best” economic model nor the finished product. It is simply the next possible step to a better future for all.
Your parent organization CPMA and its leaders are here to provide the tools and resources to guide you through those next steps. Please be sure to visit the www.calpma.org website often to keep up on these changes.
I wish you all a Happy and Healthy Holiday Season.
Thomas Elardo, DPM President, CPMA

2014 Norcal oNe Voice a Spectacular SucceSS!
Those attending the 3rd Annual Northern California One Voice event enjoyed an evening of big band music, comedy, casino games, camaraderie, fine food and fun. Attendees included CPMA leaders, representatives from the California Medical Association (CMA) and keynote speaker Senator Jim Beall (D), who represents CA Distinct 15, which covers the Silicon Valley area.
Event proceeds go to CalPPAC to help ensure that the voice of podiatric medicine is heard when and where it counts.

























































The California Podiatric m edical Association and the Santa Clara valley Podiatric m edical Society wishes to thank the following for their outstanding support of the 2014 NorCal One voice event.
• Bako Integrated Physician Solutions
• Berkshire
• BioMedical Enterprises
• Bioventus
• Dermatran Health Solutions
• Footwear, etc.
• Game Ready
• Guardian
• Health Diagnostics
• Insight Imaging
• Integra Life Sciences
• Merz Pharmaceuticals
• Organogenesis
• Osiris
• Osteomed
• Pamlab
• Qmed
• Stryker
• Tetra
• Tornier
• Valeant
T HE VA lu E O f R E l EVANT DATA
Manufacturing quality guru W. Edwards Deming has written, “In God we trust; all others must bring data.” Deming, a consultant for Toyota in the 50s, was a visionary – the first to apply raw data and statistical sampling to manufacturing processes in ways that improved quality while simultaneously lowering production costs. There are numerous ways that doctors too can utilize data and benchmarks proactively to achieve similar quality and production results within their medical practices – that is, make positive improvements and advancements in both their quality and costs. This is, in fact, something that every practitioner should be working towards now. Unfortunately, data can also be misused in ways that can negatively impact a practice when employed incorrectly by others – such as when a payer compares a doctor’s data with the “average” physician in his/her specialty to determine whether or not to initiate an audit – or when Medicare asks a practitioner to return payments because his/her coding levels have been compared with “peers” and it has been determined that this coding was “above the average.” How does one counter such an accusation when it seems out of line? This is when access to relevant data can assist the doctor.
Our future healthcare environment will be ever more driven by data. This includes the use of clinical data for measuring quality, operational data for improving practice performance, benchmark data for comparing a medical group’s performance with that of groups of equivalent size or focus, and variance data for assuring compliance with rules and regulations. Databases currently being used to compare DPMs with their peers do not accomplish these tasks well. On most, a podiatric practitioner is being compared with an “average” that includes a wide range of practitioners – from DPMs who limit their practices to palliative care to ones who perform complex, reconstructive procedures or have chosen to focus primarily in areas such as wound care or sports medicine. It is
not typically accurate to directly compare data from such diversely focused practices. The training of today’s practitioners may vary widely too. They may, or may not, be board certified, and training ranges from no residency at all to three year programs followed by fellowships. In other words, when a DPM is being compared with those in his/her “same” specialty, those with whom any individual is being compared are often not actually “peers.” Consider too comparing E/M code levels used by any one DPM with the “average.” Logically, 50% of the time, the practitioner is going to be above the average and suspected of over-billing. It is not that the data with which the doctor is being compared is incorrect, but rather, that the sample being utilized to make the comparison may not be representative for the particular doctor being monitored. Data can lead to erroneous conclusions in multiple other ways – for example, when the sample size being utilized is either too small (to few DPMs in the sample to make a broad generalization) or is not representative of the training and/or practice type of the doctor with whom s/he is being compared (yet another example in which apples are not being compared to apples).
One of the reasons that CPMA exists is to “advance and protect the profession.” I feel that an effective way of accomplishing this in the future would be to collect and analyze a large sample of relevant data from our members – data that could be used to put each practitioner on a level playing field for the purpose of comparison with his/her peers. By collecting data from its members, CPMA could create a much larger DPM sample size than that currently provided by MGMA (Medical Group Management Association) – or any other organization, for that matter. Its data could include relevant information regarding training, practice focus, patient volume, and other pertinent factors that differentiate each practitioner from the “average.” There are numerous categories of data to which access would be of value for CPMA members. Let us look at a few examples in order to understand some of the possibilities.
E/M Frequency and Distribution
Similar to the manner in which the IRS compares the type, size, and number of our deductions on income tax returns with those of peers, payers compare doctors’ billing practices with one another. When a payer compares a physician with his/her peers, it is significant just who the payer is considering to be “peers.” The sample size used might be too small to be valid as well as not even representative of the practitioner’s actual peers. When a payer sees a doctor deviating from these assumed “peers” on any particular code, or distribution of codes, to a degree considered to be statistically significant, it is likely that the payer will audit him/her. This does not mean that this doctor has actually done anything wrong, but the experience can be stressful and will necessitate that the doctor take time to review medical records in order to justify the level of codes s/he has utilized. The outcome may be that that the doctor “wins” the audit – or it may be that s/he actually is not coding correctly. In either case, access to sufficient and representative data could assist the doctor in multiple ways, that is: (1) if a doctor recognizes from examining a representative database that s/he is up-coding, it would be helpful to have relevant comparative data before being audited – thus being afforded the opportunity to make the
appropriate changes to prevent such an audit in the first place, (2) if a doctor learns that s/he is under-coding, then by adjusting to correct coding, s/he will receive appropriate reimbursement without the fear of being audited, and (3) if a doctor learns that s/ he is deviating from the norm and recognizes that a payer is likely to question his/her selection of codes, relevant data demonstrating a comparison with his/her actual peers will assist that doctor in crafting his/her defense. When a comparison shows that codes are in line with those of actual peers, this data may either help the doctor avoid an audit or, if audited “out of the blue,” it will provide him/her with an effective means of challenging the auditor’s data and ultimately “winning” the audit.
An example of the use of such data analysis can be crafted utilizing Table One, below. Herein, the E/M coding distributions of five levels of outpatient E/M visits for a fictitious Podiatric Practitioner are compared with the frequencies for these same visits as recorded in four different databases for “peers” that are in actual use today by various payers. The first column shows the number of times that our fictitious practitioner billed each code, the second shows the percentage distribution of each code for this doctor, and the remaining four columns show the distribution percentages deemed “the average” by various payers. The distribution of codes for our Podiatric Practitioner are statistically within the same range as those shown in Databases 1 and 2. A payer relying on either of these databases would be unlikely to question the practitioner’s percentages. This same distribution would, however, be likely to generate a letter from a payer using databases 3 or 4. This payer would be likely to point out that our Podiatric Practitioner has a higher percentage of levels 3, 4, and 5 codes when compared with the “average” billing behavior of other physicians within the same specialty. This letter might also let him/her know that s/he will be contacted for medical records in order to identify inaccurate coding – which, in turn, may lead to eventual recovery of associated overpayments. Have you known of cases like this? To avoid this scenario, many practitioners even intentionally under-code for fear of being audited. Obviously, this practitioner would be well-served if he/she were aware of the existence of Databases 1 and 2. Better yet would be access to a CPMA database that would compare his/her practice with peers who are actually comparable instead of simply “the average.” Regardless of the issue being raised, it is important that doctors be aware of how they line up with comparable peers long before they receive such letters.
RVU Data
Physician productivity data is but one of many statistical categories that large medical groups have shared for years. Groups have used this data for determining compensation levels for each specialty. This type of data is typically shared through an independent organization that collects and “sanitizes” data for the groups.

In past years, when physician practices were acquired by hospitals and the doctors put on salary, productivity typically dropped. The “fix” for this phenomenon was to compare Work RVUs (wRVUs) data to determine relative productivity for each specialty. Based on the findings, physicians where then categorized into percentiles – ranging from the 20th to the 90th – to determine compensation levels. Compensation was then determined by multiplying the number of wRVUs by a dollar amount that was increased as the percentile increased. For example, if a DPM were to generate 5,000 wRVUs with a dollar value of $50/RVU (the multiple), his/her resultant compensation would be $250,000 (5,100 RVUs x $50/RVU). As you might expect, there is a wide variation in actual dollar value of wRVUs amongst the various specialties within any one medical group, and there is also a large variation amongst doctors practicing the same specialty across multiple groups. The maximum size of the wRVU dollar value is ultimately limited by a group’s overhead and level of efficiency, but as often happens with capitation rates and other pay scales, it can also be enhanced, based on a physician’s negotiation skills. Access to relevant data for the purpose of arguing compensation or making any other type of decision before negotiations greatly augments these skills.
Over the years, many large medical groups have been sharing their proprietary data, and others have used MGMA data. DPMs today are increasingly becoming employed by hospitals, as well as multi-specialty, orthopedic, and podiatric groups, and their compensation levels are often determined by wRVU data. Examining a couple of databases reveals that the DPM dollar multiple on one database ranges from $30 – $44, and on another from $50 – $75. Note that the highest range for the same specialty is more than double that of the lowest! If we look at the ratio of

compensation percentage to dollars collected, the percentage on one database ranges from a low of 22% to a high of 44%. Again, one doctor is receiving twice as much for his/her productivity as the other. Given that the higher multiples are also in conjunction with the higher wRVU generation (the multiple is higher for a doctor in the 75th percentile than in the 25th), a wide range in compensation levels is created within the same specialty. A problem specific to podiatric physicians is that orthotic care has not been given an RVU number and is often not even counted in the physician’s total wRVU productivity. At the same time, orthotic care often has a high reimbursement rate – sometimes at the level of a surgical procedure. This justifies an RVU value comparable to that of a surgical procedure and should, therefore, be counted when determining podiatric productivity. The point is that it is critical for anyone running a medical group or working in one to have access to relevant data, and most doctors have access to little pertinent data. One way to fix this disadvantage is to share data through a third party – again, a role that CPMA could play to the benefit of its members.
Other Data
We have barely scratched the surface of the different types of data that could be of value to practitioners desiring to protect and advance their practices and careers. One use for relevant data that is important now and will become even more essential in the future as podiatric groups become larger and pay for performance becomes more routine is the establishment of benchmarks which can be used to evaluate practice performance – benchmarks necessary for determining where a practice is doing well and where it needs to improve. This type of data is relevant to every doctor, whether practicing solo or in a large group. Evaluating
ratios is much like doing a lab screening to determine the health of a patient; each lab result tells part of the story and needs to be viewed in the context of the entire panel. Similarly, ratios are more meaningful in the context of multiple ratios, and to be truly valuable, they should be compared with benchmarks from comparable practices. This is is another area in which the comparative data currently available to podiatric practitioners falls short. There is no real value in comparing with the “average” for all practices. Ratios such as revenue/visit, overhead/revenue, cost/ patient, CPT codes billed/visit, staff size/Dr, productivity/Dr, number of treatment rooms/Dr, and multiple other operational ratios are all useful for determining how a practice is doing and where it should focus on change. These ratios are particularly valuable when a doctor knows that s/he is comparing with data from practices or groups of similar size, focus, and patient volume, and this is what a CPMA database could offer.
This is a current and future need of DPMs, and CPMA has the capability of collecting and analyzing this important data – data similar to that which MGMA provides for its members. The advantage that our database would offer is that the sample size of the data specific to DPMs would be much larger than that contained in MGMA’s database. It would also be more relevant to the specific needs of podiatric practitioners because this information could be sorted and analyzed in ways such that all DPMs and practices would not be mixed together to achieve an “average.” Instead, key differences, such as practice size and clinical focus could be differentiated – making this a vital tool for competing in a future where access to relevant and reliable data will be essential. Do we have need for something like this? The time to get started is now. When shall we start?
N OVEMBER IS D IABETES
AwARENESS M ONTH





























I NCREASE P ROD u CTIVITY w ITH P O w ER
M EETINGS AND Hu DD
l ES
One of my favorite sayings is, “None of us is as good as all of us.” I am a true believer in teamwork in the office. It is always so exciting when we sit down at a meeting, come up with a way of increasing the bottom line or improve our service quality, and everyone participates in sharing ideas. It is amazing to see what comes out of a good power meeting. You start with one thought, and in the end, come up with ideas that you never would have thought of by yourself.
It is not always like this, however; sometimes things just do not gel and nothing worthwhile comes out of the meeting.
Knowing how to run an effective power meeting is very helpful. There are many factors to consider, like location, comfort, ground rules and purpose, to name a few. Making sure that you have a good meeting facilitator is important to keep people focused and ground rules enforced. Criticism is a creativity killer and never should be allowed when brainstorming ideas together. Power meetings are not necessary to come up with good ideas, but the synergy and sense of bonding that takes place when team members all have input into the ideas is priceless.
Our team sat down for 30 minutes (setting a time limit is necessary) as we were putting together a new strategic plan for productivity and efficiency to implement in the office. The first item we needed to accomplish was to come up with our office purpose or mission statement. We all know what we do and why we do it, but putting it into words isn’t as easy as one might think. We started throwing our thoughts out there and writing them down, and with the input of all of us we were able to come up with a statement that said exactly what we all felt to be true for us - and it only took about 15 minutes. We were so excited that we were able to accomplish our goal for the meeting - and in less time than we set aside. Having a power meeting is a great and motivating way to accomplish tasks
without burnout.
In Verne Harnish’s book mastering the rockefeller Habits he states that successful businesses have daily meetings for 5-15 minutes, which he calls “huddles”. He states that by having these huddles you can actually save time because you are focusing on what is happening for that day.

There are only three questions that are covered at this meeting and they are the same each day:
1. What’s up for the day;
2. Daily measures; and
3. Where are you stuck?
Working in a medical office, the questions might translate into:
What does the schedule look like?
How can we best prepare for the patients coming in?
Is anyone having any particular work problem they need help resolving?
By just asking these three questions daily we can prepare and resolve many problems we face during the day that take more time away from being productive. It is also a good practice to have a short huddle at the end of the day to measure how the day went and gather ideas for better outcomes if there were any issues while they are still fresh in our minds.
You may think you do not have time for more meetings, but remember, this is a huddle - it is grouping those who work together to review what will be taking place that day. When everyone is on the same page and is identifying how they can resolve any issues before they arise to make for a more productive, less stressful day, how can you not take the few minutes?

2014 YEAR -E ND TAx Pl ANNING I DEAS
Whether considering your own personal tax situation or that of your business, as we near the end the year, tax considerations and planning should be on your mind. Certain decisions and actions are imperative this year to help minimize your tax situation for 2014.
Year-end tax planning for 2014 will be challenging in many respects due to tax incentives that expired at the end of the 2013 year. Although Congress could still act on some of these expired incentives and retroactively reinstate these, it is unclear as to whether the political climate will exist to support this. The end result is that there could be some truly last minute tax opportunities that open up if these tax breaks are extended.
tax breaks which expired for individuals included: opportunity to deduct state and local sales and use tax instead of state and local income taxes; an above-the-line deduction for qualified higher education expenses; tax-free IRA distributions for charitable purposes by individuals 70 ½ or older;, and the exclusion for up to $2 million of mortgage debt forgiveness on a principal residence.
tax breaks which expired for businesses included: 50% bonus first year depreciation for most new machinery, equipment and software; the $500,000 annual section 179 depreciation expensing limitation; the research tax credit; and the 15 year write-off for qualified leasehold improvement property, qualified restaurant property and
qualified retail improvement property.
2014 will also have unique consideration for higher income earners when mapping out year-end tax plans. The 3.8% surtax on certain unearned income and the additional 0.9% Medicare (hospital insurance, or HI) tax that applies to individuals receiving wages from employment in excess of $200,000 ($250,000 for married filing jointly and $125,000 for married filing separately) must be planned for.
The surtax is 3.8% of the lesser of: (1) net investment income (NII), or (2) the excess of modified adjusted gross income (MAGI)over an unindexed threshold amount ($250,000 for married filing joint or surviving spouses, $125,000 for married individual filing separate, and $200,000 for all others). Strategies to minimize this surtax depend upon the estimated NII and MAGI for the year. Taxpayers with high NII should consider ways to minimize additional NII balances for the year (possibly through income deferral). Or if high MAGI is the concern, it should be looked at how to reduce 2014 MAGI; or consider ways to reduce both NII and MAGI.
For the additional 0.9% Medicare tax (HI) year-end planning may require action. Employers must withhold the additional Medicare tax from wages in excess of $200,000 regardless of filing status or other income. However, self-employment individuals must take it into account when projecting their estimated tax for 2014. Also, there could be situations where an individual needs to have an additional amount withheld near the end of the tax year to cover this tax. This situation could occur if an employee worked at more than one employer in 2014 and cumulatively earned over $200,000 (but was under the $200,000 at each employer separately). In this case, the employee would owe the HI tax, but neither employer would have had to withhold this tax amount since neither met the thresholds.

Below is a list of many tax action items that should be considered for the 2014 tax year that may help to minimize your tax burden for the 2014 tax year if acted upon before the end of this year. Although 2014 is shaping up as a fairly hard year to plan for in many respects, there are actions that you can and should take now to help minimize your ending tax bill:
by Amanda Williams, CPA Gilbert Associates, Inc., CPAs and Advisors










































































































Year-end tax planning actions for individuals:
• Postponing Income & Accelerating Deductions - For higher income individuals, postponing income until 2015 or accelerating deductions could lower your 2014 tax bill and help you be able to take advantage of other tax breaks that are phased out over varying levels of adjusted gross income (AGI). These include child tax credits, higher education tax credits, and deductions for student loan interest. Postponing income would be most desirable to individuals who anticipate lower income levels for the 2015 tax year. Also, for those individuals who anticipate higher income for 2015, the opposite of this strategy may make sense to help minimize the overall tax burden between the tax years.
• Traditional IRA Conversion to Roth IRA Considerations- If you converted assets held in a traditional IRA to a Roth IRA earlier in the year and the assets in the Roth IRA have declined in value, if you leave it as is you may end up paying higher tax than is necessary. You can back out of the transaction by recharacterizing the conversion (transferring the converted amount plus earnings/loss back to a traditional IRA via a trusteeto-trustee transfer). You can reconvert later to a Roth IRA if doing so proves advantageous.
• End of Year Bonus - It may be advantageous to arrange with your employer to defer a bonus that you may be receiving until 2015.
• State & Local Tax Withholding - If you anticipate owing state and local income taxes when you file your return next year, consider asking your employer to increase your withholding of state and local taxes (or make an estimated payment to the state) before year end to pull the deduction of taxes into 2014 if doing so will not create alternative minimum tax (AMT) issues.
• AMT Considerations - Talk with your tax professional to estimate the effect of any year-end planning moves on the alternative minimum tax (AMT) for 2014 – many tax breaks allowed for purposes of calculating regular taxes on your residence, state income taxes, miscellaneous itemized deductions and personal exemption deductions are not allowed for AMT purposes.
• 70 ½? Take RMD - Make sure to take required minimum distributions (RMDs) from your IRA or 401(k) plan if you have reached age 70 ½ . Failure to take the RMD can result in a penalty of 50% for the amount of the RMD not taken.
• Retirement Contributions - One of the best ways to save on taxes is to make contributions into a retirement account including 401(k), SEP or IRA. Maximizing your contribution not only saves money for retirement, but decreases your taxable income for the current tax year.
• HSA Contribution - If you are eligible to make health savings account (HSA) contributions in December of this year, you can make a full year’s worth of deductible HSA contributions for 2014. This will be the case even if you became eligible on December 1.
• Gifting Strategies - Making gifts sheltered by the annual tax exclusion before the end of the year could save taxes in the future for gift and estate taxes. You can give up to $14,000 in
2014 to each of an unlimited number of individuals ($28,000 for married couples) but you cannot carry over used exclusions from one year to the next. The transfers may also save family income taxes where income-earning property is given to family members in lower income tax brackets who are not subject to the kiddie tax.
Year-end
tax planning actions for businesses:
• Depreciation & New Capitalization Regulations - Although the expiration of the bonus 50% depreciation expense on new equipment additions and the decrease in the section 179 dollar limitation (from $500,000 limit with beginning of phase-out amount of $2 million to $25,000 limit with beginning of phaseout amount of $200,000) will be a hard hit to business taxable income, businesses could benefit from the new “de minimus” safe harbor election in the new capitalization regulations and the provisions for expensing certain regular repair or maintenance costs which in the past may have been required to be capitalized. Business controllers and managers should become familiar with the new IRS capitalization regulations and make sure they are in compliance and maximizing their business’s benefit.
Business should make sure they have adopted a capitalization policy as required by the new regulations effective as of the end of 2013 to ensure that they are able to set the capitalization threshold which applies to their business at the highest possible level. For businesses that have annual financial audits, this threshold is $5,000, however if the business did not have an audit, the maximum of this threshold is $500. If no policy is in place or adopted, however, the automatic threshold assigned under the new capitalization thresholds is only $200.
• Half-Year Depreciation Convention - If machinery and equipment is purchased before year end, the “half-year convention” should be utilized for tax purposes which secures a half-year worth of depreciation deduction for the first ownership year.
• Acceleration & Deferral of Income - A corporation should consider accelerating income from 2015 to 2014 where doing so will prevent the corporation from moving into a higher tax bracket next year. Conversely, it should be considered to defer income until 2015 when doing so will prevent the corporation from moving into a higher tax bracket this year.
• Business AMT - If income and expense deferral or acceleration options will be considered by your business for 2014, a determination for the alternative minimum tax (AMT) consequence should be considered to determine if the taxpayer would be subjected to additional AMT.
• Pay by Credit Card- Consider using a credit card to pay deductible expenses before the end of the year. Doing so will increase your 2014 deductions even if you don’t pay your credit card bill until after the end of the year.
With careful proactive and reactionary tax planning (if Congress takes action on certain tax extender legislation) and coordination with your tax advisor, you should be able to customize your tax planning to take advantage of many positive tax strategies and help minimize your tax burden for 2014.
2015 CPMA H OUSE of D ELEGATES
will convene Wednesday, June 24, 2015 Disneyland Hotel Anaheim, CA

P RESIDENT
Thomas J. Elardo, DPM
Los Gatos, CA 95032
P: (408) 358-6234
P RESIDENT -E LECT
Ami A. Sheth, DPM
Los Gatos, CA 95032
P: (408) 358-6234
V ICE P RESIDENT
Rebecca A. Moellmer, DPM Pomona, CA 91766
P: (909) 469-8413
I MMEDIATE PAST
P RESIDENT
Carolyn E. McAloon, DPM Castro Valley, CA 94546
P: (510) 581-1484
S ECRETARY -T REASURER
Devon N. Glazer, DPM Mission Viego, CA 92691 P: (949) 272-0007
D IRECTORS
John A. Chisholm, DPM
Chula Vista, CA. 91910 P: (619) 427-3481
Adam S. Howard, DPM Cupertino, CA95014 P: (408) 446-5811
Thomas J. Tanaka, DPM Ontario, CA 91761 P: (909) 724-5052
Mark A. Warford, DPM Fair Oaks, CA 91316 P: (916) 548-0218
Vladimir Zeetser, DPM Encino, CA 95628 P: (818) 907-6100
S TUDENT
R EPRESENTATIVES
Luke Hultman (CSPM) Dayna Chang (Western U)
Ex ECUTIVE D IRECTOR
Jon A. Hultman, DPM 2430 K St Ste 200 Sacramento, CA 95816
P: (916) 448-0248 (800) 794-8988
jhultman@calpma.org jonhultman@gmail.com
G ENERAL COUNSEL
C. Keith Greer, Esq. San Diego, CA 92128
G OVERNMENTAL R EPRESENTATIVE
Jodi Hicks Sacramento, CA 95814
PARLIAMENTARIAN/ R ECORDING S ECRETARY
Roderick Farley, DPM,JD/ Nedra L. Farley
2014/2015 CO m PON e NT SOCI e TY P re SID e NT S
ALAMEDA/ CONTRA COSTA
COUNTY
Michael Grimes, DPM
Pinole, CA 94564
P: (510) 724-1530
CENTRAL VALLEY
John Abordo, DPM
Merced, CA 95341
P: (209) 383-7441
COACHELLA VALLEY
Harvey Danciger, DPM
Palm Desert, CA 92260
P: (760) 568-0108
INLAND
Diane Koshimune, DPM Pomona, CA 91766

June 25-28, 2015
P: (909) 706-3778
LOS ANGELES COUNTY
Gabriel Halperin DPM Los Angeles, CA 90063
P: (323) 264-6157
MID-STATE
Richard Motos, DPM Visalia, CA 93291
P: (559) 734-1171
MONTEREY b AY AREA
Bobby Yee, DPM
Monterey, CA 93940
P: (831) 646-8242
NORTHERN CALIFORNIA KAISER
Cristian Neagu, DPM
Santa Clara, CA 95051 (408) 851-1957
ORANGE COUNTY
Thomas Rambacher, DPM
Mission Viejo, CA 92692
P: (949) 916-0077
REDWOOD EMPIRE
Paul Weiner, DPM Vallejo, CA 94590
P: (707) 643-3687
SACRAMENTO VALLEY
Daniel Lee, DPM, PhD Sacramento, CA P: (916) 688-2030
SAN DIEGO/IMPERIAL
Nicholas DeSantis, DPM
San Diego, CA 92101
P: (619) 239-3286
SAN FRANCISCO/ SAN MATEO
Bill Metaxas, DPM
San Francisco, CA 94108
P: (415) 433-3668
SAN LUIS O b ISPO/ SANTA b AR b ARA
David Sterling, DPM
Santa Maria, CA 93455
P: (805) 928-5645
SANTA CLARA VALLEY
Mehryar Amirkiai, DPM Sunnyvale, CA 94087 P: (408) 245-3230
SHASTA REGION
Gordon Shumate, DPM Redding, CA 96001 P: (530) 246-4800
SOUTHERN CALIFORNIA HMO
Diane Branks, DPM
VENTURA COUNTY
Heather McGuire, DPM
Ventura, CA 93003 P: (805) 648-2016
The California Podiatric Physician is the official publication of the California Podiatric Medical Association. CPMA and the California Podiatric Physician assume no responsibility for the statements, opinions and/or treatments appearing in the articles under an authors’s name. For editorial or business information and advertising, contact California Podiatric Medical Association, 2430 K Street, Suite 200, Sacramento, California 95816; telephone, (916) 448-0248; facsimile; (916) 448-0258; e-mail; calpma.org.
E ff ECTIVE lY COMM u NICATING w ITH THE
We frequently receive calls from members asking for guidance when interacting with deaf and hard of hearing patients. The most common question is whether the member must provide an interpreter, and if so, who is responsible for paying the interpreter. The answer to the latter question is well settled. If an interpreter is necessary, the healthcare facility is generally required to cover the costs. Unfortunately, there is no black and white answer to the question of when an interpreter is required. Rather, each case must be analyzed individually to determine whether the chosen method of communication allows the healthcare provider to “communicate effectively” with the patient.
The most common method of communication between deaf patients who are not proficient lip readers and hearing individuals who do not know sign language, is by written dialogue. This method of communication has a number of benefits. First, it is efficient. Rather than have an interpreter intervening, the doctor and patient are able to directly interact. Conversely, when using an interpreter, the doctor makes a statement to the patient and relies on the interpreter to choose the corresponding signs and words. The interpreter then signs to the patient. The patient signs to the interpreter and then the interpreter speaks to the doctor. The inherent delays between comments and thoughts, and the risk of “misinterpretation,” are not an issue when the doctor and patient are communicating in writing. If the deaf patient is competent with reading and writing, in most circumstances a written dialogue can be an effective method
of communicating information regarding podiatric care. This can be accomplished by either sitting side by side at a computer and creating a typed dialogue, or by passing a paper tablet with a hand written dialogue. Using informational pamphlets, diagrams and written instructions is also effective. The most important thing to remember is that your obligation to effectively communicate with a patient, including the obligations to explain the reason for the condition, alternative methods of treatment and provide material information necessary for the patient to make an “informed” decision on whether to undergo or forgo treatment, including surgery, is the same for all patients, regardless of their ability to hear.
If during the course of your interaction with a deaf patient you become aware that a written dialogue is not “effectively communicating” with the patient, you may be required to engage and pay for an interpreter. As discussed in more detail below, a healthcare provider can be excused from the obligation to pay for the interpreter if it would result in an “undue burden” on the healthcare provider. Although financial burden is the most pertinent factor to be considered, the mere fact that the interpreter costs more than the amount paid for the office visit is not conclusive evidence of undue burden. Rather, other factors must also be considered, including the facility’s operating income, eligibility for tax credits and the number of visits requiring interpreter services. Having reviewed the cited court decisions on this topic, I think it is unlikely that a court would find the costs of interpreter services for a single patient to be an “undue” burden for most private practices.

A review of court decisions and materials published by government agencies and various advocacy groups for the disabled reveals several topics which are particularly important, and thus more likely to warrant using an interpreter. They include explaining procedures and treatment options, obtaining informed consent and explaining medications and side effects. The vast majority of published materials on this topic also strongly encourage the use of interpreters in all circumstances. That said, it remains my opinion that for the vast majority of podiatric services, thorough written dialogues are appropriate. In fact, it would make the defense of any claim brought by a patient much easier if there was a written transcript of everything that was said. Arguably, a written dialogue is even more effective than a spoken dialogue since the doctor and the patient know exactly what was communicated, the patient can take a copy of the dialogue home with them to read again and formulate further questions, and
HEARING IMPAIRED
the doctor can read the dialogue to determine if any information was erroneously omitted or needs further discussion. Fortunately, most of the members we have spoken with have been able to communicate very effectively with deaf patients through written dialogues and supplemental written materials. In cases where an interpreter is needed, we recommend that members contact local hospitals who are generally required to have interpreters available at all times, and request the professional courtesy of allowing the member to examine the patient at the hospital with an interpreter present, or to provide the interpreter for a fee that is less than the market rate for commercial interpreting services.
The forgoing reflects my personal opinions on this topic. In order to make sure members are fully informed of the relevant law, including circumstances that warrant using an interpreter, I am providing the following excerpts and summaries of the law and other published materials.
Federal laws mandate equal access to health care services, and effective communication with individuals who are deaf or hard of hearing. These laws include the Rehabilitation Act of 1973 (the “RA”), which applies to health care providers who are also recipients of federal financial assistance, usually provided by direct funding (such as federal Medicaid funds) and the Americans with Disabilities Act (the “ADA”), which applies to all private health care providers, regardless of the number of employees. Under these laws, health care providers have a duty to provide appropriate auxiliary aids and services when necessary to ensure that communication with people who are deaf or hard of hearing is as effective as communication with patients who are not hearing impaired. Similarly, a deaf parent of a hearing child may need an auxiliary aid or service to effectively communicate with healthcare providers and give informed consent for their child’s medical treatment.
Auxiliary aids and services include the written dialogues and materials discussed above, as well as qualified interpreters, computeraided transcription services (also called CART), assistive listening devices, captioning, or other effective methods of making oral information and communication accessible. The requirement to provide auxiliary aid and services is flexible, and the healthcare provider can choose among the various alternatives, providing that the result is effective communication with the deaf or hard of hearing individual.
If the healthcare provider determines that a written dialogue and printed materials are not resulting in “effective communication,” the provider should give deference to the deaf individual’s preference for alternative methods, as they will usually have experience with certain types of auxiliary aids. The U.S. Department of Justice published a report stating that it expects health care providers to consult with the deaf patient and consider carefully his or her self-assessed communication needs before acquiring a particular auxiliary aid or service.
As discussed above, the ADA does not require healthcare providers
to use any auxiliary aid or service that would result in an undue burden or in a fundamental alteration in the nature of the goods or services provided by a health care provider.
28 C.F.R. § 36.303(a). Communicating with a deaf or hearing impaired patient is unlikely to ever result in a “fundamental alteration” of a health care service. An individualized assessment is required to determine whether a particular auxiliary aid or service would be an undue burden.

An undue burden is something that involves a significant difficulty or expense. For example, it might be a significant difficulty to obtain certain auxiliary aids or services on short notice. Factors to consider in assessing whether an auxiliary aid or service constitutes a significant expense include: the nature and cost of the auxiliary aid or service; the overall financial resources of the health care provider; the provider’s number of employees; the effect on expenses and resources; legitimate safety requirements; and the impact upon the operation of the provider. 28 C.F.R. § 36.104. Even if an undue burden can be shown for a particular auxiliary aid, the healthcare provider still has the duty to utilize an alternative that would not result in an undue burden and, to the maximum extent possible, would ensure effective communication. 28 C.F.R. § 36.303(f).
Even private healthcare providers are expected to treat the costs of providing auxiliary aids and services as part of the overhead costs of their office. So long as the provision of the auxiliary aid or service does not impose an undue burden on the provider’s business, the provider is obligated to pay for the auxiliary aid or service. This is true even if the cost of providing an auxiliary aid or service (e.g., a qualified interpreter) exceeds the charge to the patient for the healthcare service. Moreover, a healthcare provider cannot charge a deaf patient for the costs of providing auxiliary aids and services. 28 C.F.R. § 36.301(C).
A qualified interpreter is one who is able to interpret effectively, accurately, and impartially, both receptively and expressively, using any necessary specialized vocabulary. 28 C.F.R. § 36.104. There are various kinds of interpreters. The healthcare provider should determine the particular language needs of the deaf patient prior to hiring an interpreter. Some individuals need interpreters who are fluent in American Sign Language, which has grammar and syntax different from the English language. Others may use Signed English, which uses the same word order as spoken English. Although deaf patients may voluntarily bring a family member or friend to interpret for them, it is illegal to require deaf patients to bring an interpreter as a condition for providing health care services. Moreover, family members and friends may not have sufficient skills to interpret medical information effectively or may have interests that conflict See H earing im Paired on







with the patient’s and thus may not interpret “effectively, accurately, and impartially.” Using family members and friends as interpreters can also violate patient confidentiality laws. 56 Fed. Reg. at 35553.
If the healthcare provider is relying upon the patient’s ability to lip read, caution should be taken to make sure the patient truly understands what is being said. According to the National Association of the Deaf (the “NAD”): “The ability of a deaf or hard of hearing individual to speak clearly does not mean that he or she can hear well enough to understand spoken communication or to lipread effectively. Forty to sixty percent of English sounds look alike when spoken. On average, even the most skilled lip readers understand only twenty-five percent of what is said to them, and many individuals understand far less.” Thus, “because lipreading requires some guesswork, very few deaf or hard of hearing people rely on lipreading alone for exchanges of important information. Lipreading may be particularly difficult in the medical setting where complex medical terminology is often used.” Therefore, supplemental aids, such as written materials, diagrams and, in certain situations, interpreters, may be needed to insure effective communication.
Interestingly, the NAD suggests only using written dialogues for “brief and simple communication,” contending that: “Communication through the exchange of written notes is inherently truncated; information that would otherwise be spoken may not be written. Moreover, written communication can be slow and cumbersome. If a health care provider is communicating less or providing less information in writing than he or she would provide when speaking
to a patient, this is an indication that writing to communicate is not effective in that context.” I respectfully disagree with the contention that written dialogues are any more “truncated” than using an interpreter. Moreover, if the healthcare provider makes sure to provide everything in writing that would otherwise have been provided orally, the NAD’s primary concern will have been eliminated.
An important point raised by the NAD which must be considered when deciding whether to use a written dialogue, is that the effectiveness of written material also depends on the reading level or literacy skills of the patient. Reading levels of deaf and hard of hearing individuals varies as much as reading levels for the general public. More important, some deaf and hard of hearing people use American Sign Language (ASL) as their first language. Because the grammar and syntax of ASL differ from written English, using a written dialogue simply may not work. For these individuals, a qualified sign language interpreter may be the only effective way to communicate.
Although the patient cannot be charged for the cost of an interpreter, eligible small businesses can claim a tax credit of up to fifty-percent of interpreter expenses, CART services and other auxiliary aids that are more than $250, but less than $10,250. Up to $5,000 may be credited per tax year. Omnibus Budget Reconciliation Act of 1990, P.L. 101-508, § 44. To determine whether your practice qualifies, you should contact your CPA or tax advisor.
If you have further questions regarding this or other legal issues affecting your practice please call CPMA at (800) 794-8988.
(Originally printed in the 2010 October/November/December issue of The California Podiatric Physician)
Dr. Dawn Buratti (pictured left above and center below) was mistakenly identified in these two photos from the 2014 July/August/ September issue of the California Podiatric Physician. Additionally, the city in which Dr. Vladimir Zeetser resides was misidentified as Torrance, CA. Dr. Zeetser resides in Tarzana, CA.
CPMA staff goes through thousands of photos from the numerous meetings held during the CPMA House of Delegates and Western Foot and Ankle Conference meetings. Staff goes to great lengths to try to identify those pictured. But, we are not always successful, and mistakes do happen. We sincerely apologize for any inconvenience this may have caused.


w INTER HEA lTH PO l ICY REPORT
This is my last report for the year 2014. In this report, I will discuss some of the latest issues that had been developing with the private insurance world in California and we will then discuss some of the issues that we discussed at the CAC-PIAC meeting in Washington DC during the first weekend of November. The following are some of the issues in the private insurance world.
BluE SHIElD
We have gained a great deal of success with Blue Shield in the avoidance of the words on an explanation of benefits (EOB) “services are not payment when performed by providers of this classification.” For all intents and purposes, we have eliminated the majority of cases where these words occur on EOBs. However, there are still some rogue instances where this has occurred albeit much less frequently then previously noted. The reason that it has occurred, according to the principals at Blue Shield , is that they have changed their claims software and has not upgraded all services and procedures performed by Podiatrist to allow them for full reimbursement. As I stated before, in general, this is no longer an issue, but as I have told Blue Shield even one errant statement or an explanation of benefits which states that the Podiatric Physician should not be performing this service and which goes to their patient, is unacceptable. Blue Shield has taken these words to heart and is seeking to eliminate these words on ALL explanation of benefits.
Another very significant issue that has developed with Blue Shield has to do with a podiatric physician performing fungal culture tests in their office. Recently, one of our colleagues performed a fungal culture in his office and was denied by Blue Shield as not being eligible under CLIA (Clinical Laboratory Information Act), which is a provision in the federal statute that allows doctors to perform such services in their offices provided that they have a certificate from CLIA. Blue Shield stated the reason they denied this podiatric physician payment for these services, is that a podiatric physician is not allowed to perform these services without such a CLIA certificate. CPMA staff did some research at my request and determined that an MD, DO, or DPM who performs fungal cultures in their offices ALL must have CLIA certificates in order to be allowed to perform such procedures and be paid for such. I informed Blue Shield that if they discriminated against podiatric physicians and did not pay them, but proceeded to pay MDs and DOs without demonstration of them having a CLIA certificate, I would file a group dispute resolution appeal to the Appeals Department at Blue Shield. In that appeal I would state wanted this situation investigated and a formal determination made whether or not ONLY a podiatric physician was ineligible to receive payment for fungal cultures performed in their offices or was this applicable to all physicians including M.D. or D.O. dermatologists performing such procedures in their offices. What I also told Blue Shield was that if they did not handle this situation internally and proceeded to render a judgment about this situation, then they would probably have a multitude of M.D. and D.O. physicians, particularly dermatologists, who perform fungal cultures or KOH procedures in their office, up in arms. As yet, I have not heard from Blue Shield as to the direction they wish me to proceed. It is now my intention to file a group dispute resolution on behalf of our members at CPMA, which will necessitate Blue Shield to render a written decision about the performance and reimbursement
of fungal cultures in the office. This should present some very interesting future discussions.
During my trip to Washington for the CAC-PIAC on November 7th and 8th, I listened to many interesting lectures. I will discuss some of the general lectures as well as those lectures relevant to private insurance and Gabe Halperin, DPM, the CAC rep for Southern California will in a future issue of the Californian Podiatric Physician discuss those issues relevant specifically to Medicare and the changes occurring there in.
The first relevant lecture was about policy issues for DPMs by Henry Desmarais, M.D. a member of Health Policy Alternatives. Dr. Desmarais discussed the changes that will be occurring in first Medicare and then possibly in private insurance. Some of the issues that were discussed were Medicare and Accountable Care Organizations (ACO). Dr. Desmarais stated that five million Medicare beneficiaries are presently being served by more than 350 ACOs throughout the country, but only 25% of those ACOs were able to qualify for shared savings with Medicare. He stated that Medicare and Medicaid were interested in testing some new ACO concepts including transitioning ACOs to full insurance risk where the ACO would be held accountable for Medicare parts A and B and prescription drugs under Medicare part D. He also talked about the new plan to bundle payments for inpatient services. There were four models of such bundled payments and in several of them, this included physician services in and out of the hospital. He stated that approximately 68,000 organizations have expressed some level of interest in participating in the “bundle payment for care initiative”. He also stated that CMS is interested in participating in “episode-based payments” that focus on outpatient procedures and chronic conditions. These would include the diabetic patient as well as the asthmatic patient.
Of great significance to us was the idea that Medicare may eliminate the 10 day and 90 day global surgical services to zero global day services by calendar year 2017 and 2018. Of course, this would mean that we would be paid for office visits rendered after surgery, but actual surgical fees would in most likelihood decrease. Remember that when you would see the patients postoperatively, you would be able to bill for evaluation and management services, but you would still have to meet the criteria necessary to bill higher level evaluation and management services. This is going to pose a great challenge to figure out appropriate values for the actual surgery and then pay for an unspecified amount of postoperative office visits.
Also, of great significance, is the fact that with the letter writing to CMS by APMA’s President Frank Spinosa, the provisions of the Sunshine Act are now equally applicable to MDs, DOs and DPMs. That means that if there is a speaker at a program which is CME or CPME accredited, the fees generated to that speaker whether MD, DO or DPM would not be reportable under the Sunshine Act. Prior to this, podiatrists were required to have their fees for speaking at any programs subject to disclosure. Now podiatric physicians are being treated exactly like any other physician under the Sunshine Act.
Dr. Desmarais also spoke about the importance of paying attention to quality measures. He stated that there will be much more emphasis on reporting quality in doctor’s billings as payments could decline by several percentage points if a doctor did not report quality
measures. This program is applicable to all physicians including podiatric physicians. He talked about a value added modifiers where the services that are rendered by ALL physicians, MD, DO and DPM, to patients would be subject to payment increase or decrease dependent upon whether or not they satisfy the requirement of high quality and low cost services. This is a very complex issue and every body needs to pay attention as to how this plays out under Medicare. What is important to notice is that if you do not satisfactorily report a quality measure when reporting claims, then you will in future years be subject to a payment decrease for Medicare. This may in the future also apply to private insurance.
Another issue of great importance is the fact that at this present time, the conversion factor under Medicare is 35.8228. Under the conversion factor for Medicare from January to March of 2015, the conversion factor will be 35.8013, not a very big difference from 2014. However, if the sustained growth rate (SGR) is not “fixed” by congress, then from April 2015 to December 2015, we will all participate in 21.2% decrease in conversion factor to approximately 28.2239. Therefore, as it has done many times before, Congress must act to at least if not permanently, then temporarily fix the SGR so that we do not suffer a loss of revenue as compared to 2014. Also remember as goes Medicare, so goes the private sector in due time. Also please note that under Worker’s Compensation, payments will also more than likely go down if the Medicare conversion factor goes down, as Worker’s Compensation reimbursement is tied to the Medicare fee schedule. So hopefully, Congress will act to prevent any decrease in fees.
Another issue that was discussed was podiatric physicians right the pneumatic compression devices which are being challenged by Medicare in many states. The theory of many of the regional Medicare carriers is that a Podiatric Physician is not trained to deal with the complications of vascular disease including venous disease. Therefore, they should not be authorized to supervise usage of the pneumatic compression devices. This is like saying that a podiatric physician should not treat a diabetic ulcer because he/she does not manage their diabetes and is not capable of doing so. This would be a terrible precedent if passed. At the present time, in California, Podiatric Physicians are allowed to supervise the application of pneumatic compression devices.
Kelly Back an attorney and APMA consultant gave a very informative lecture on emerging issues in private insurance. Ms. Back spoke about narrow network plans, termination from provider panels, participation in Medicare Advantage Organizations, reminder of ERISA rights and the antidiscrimination provision of the Accountable Care Act.
Ms. Back spoke about narrow networks and why they developed. The primary reason was that employers were looking to decrease their expenses. As a result, 70% of plans offered through the state exchange programs generated by the ACA are offering narrow networks defined as excluding 30% of all hospitals. In a narrow network only the most “efficient” providers are invited to participate. Also fees tend to be very low so that few providers accept participation even when asked to join. These narrow network programs have resulted in tremendous scrutiny by state and
federal regulators. In California, the Department of Managed Health Care is investigating whether Anthem Blue Cross and Blue Shield violated the state law by misleading consumers into thinking their PCP’s were part of the network when in fact they had not signed up. This has created a tremendous consumer backlash.

Ms. Back also discussed the fact that there is new consumer backlash regarding states passing “any willing provider laws.” In South Dakota, an initiative for any willing provider passed by 61% of the population. This means that anyone who was willing to accept the provisions and fee schedule of an insurer would be allowed to see those patient’s at the prevailing rate.
A long discussion was held about Medicare Advantage Programs and the advantages and disadvantages of participating in such plans. To summarize, Medicare Advantage Programs are HMOs or PPOs under Medicare. They are private health plans that administer the Medicare Benefit. They are different than Medicare supplemental plans because they cover both Medicare portion of the claim and all or part of the members cost sharing. They must comply with relevant LCD’s (Local Carrier Determinations) and NCD’s (National Carrier Determinations). They are exempt from state laws including prompt payment laws, recruitment laws and external appeals laws. They may choose to cover benefits beyond Part A and Part B Medicare. If you chose to participate in such plans, there are certain benefits and disadvantages.
ADVANTAGES Of PARTICIPATING wITH MAO OR MEDICARE ADVANTAGE ORGANIZATION
1. If the Medicate Advantage participants are part of an HMO, that is the only way of furnishing services to the member.
2. You have a higher likelihood of getting referrals from physicians participating in the MAO.
3. You may negotiate a higher payment than the standard Medicare fee for service payment.
4. You may negotiate recoupment and audit provisions.
Some of the disadvantages of contracting with an MAO are:
1. They may require you to provide records for any reason at no cost.
2. You must comply with prior authorization requirement.
3. Payment may or may not be favorable.
4. They may down code at their own will.
5. The only available appeal process is the process established by the plan.
6. It may be difficult to furnish non-covered benefits to members who agree to pay out of pocket.
There are many many other benefits and disadvantages, but these are a few of the primary ones.
DOCTOR ACTING AS AGENT Of THE PATIENT

Ms. Back also discussed the issue about assigning the doctor as an agent for the patient. What this means is, is that unlike an assignment of benefits where the benefits are assigned to the doctor, the patient signs a form that indicates that the doctor is not only receiving benefits, but is actually acting as an agent for the patient. This means that even if you are not contracted with a plan and the plan has been made aware that you are an agent for the patient, they must send all communication and payment to you. If you do not have such a signed statement by the patient on file, then if you are not a contracted provider with that plan, then the insurer may send the money directly to the patient and you may have to chase down such payment. So it is a good idea to get such an “assignment as an agent” signed by the patient and send it in with your billing especially if you are a non-contracted provider with the plan. A form indicating the doctor is acting as an agent for the patient can be found on the APMA website.
ANTIDISCRIMINATION PROVISION
There is a statement in the Affordable Care Act or ACA that states that a group health plan or health insurer shall not be precluded from varying reimbursement rates based on quality or performance measures. The APMA has interpreted this, and we agree with this interpretation, to mean that this antidiscrimination provision should prevent any insurance plan from varying reimbursement to providers based solely on their degree. Therefore, as discussed many times before, the insurer, Multiplan, which clearly discriminates on the basis of licensure is in violation of the antidiscrimination provision of the ACA. To that end, the APMA is writing a letter to the attorneys at Multiplan as well as the insurance plans that contract under the umbrella of Multiplan and inform them of the fact that they are violating federal law by discriminating against Podiatric Physicians. As you may remember from my previous reports, Multiplan is the only health plan in the state of California, which clearly discriminates against Podiatric Physicians by classifying them as midlevel providers along with optometrists, psychologists, and chiropractors. Podiatric Physicians receive approximately 85% of what an MD or DO receives for the same foot and ankle services. I also want to state that the medical director at Multiplan at this time fully supports the idea that Podiatric Physicians should be placed in the category of Physician and not midlevel provider. He has written a letter to the Multiplan organization stating this. However, he has told me on multiple occasions that it is up to the network administrators whether or not they will change their policies. Thus far, they have not felt the need to abide by the Medical Director’s recommendations because they feel they have adequate Podiatric Physicians in the networks in Multiplan throughout the country.
As I stated before, I cannot tell anybody what to do in terms of signing contracts with Multiplan or any other insurer that sets out to clearly discriminate against Podiatric Physicians in their payment and provisions in their policy. However, I can tell you that if the discriminating insurer feels that they have enough providers under their plan then they do not have the incentive to change their policies and will continue to discriminate against Podiatric Physicians. Stay tuned to see what happens when APMA sends out these letters to Multiplan and their subsidiary insurers.
The last issue I am going to discuss is the break out session that we had at the CAC-PIAC meetings. During that breakout session, I facilitated the discussion between similar representatives of the Western States. Some issues that were discussed were foot orthotic coding and payment, fee discrimination, the need to develop outcome studies, and United Health Care not paying for initial evaluation and management services when procedures are performed. We had a very lively discussion and it was found that almost all states except California do not receive payment by insurance companies for foot orthotics. We are very fortunate in that we do receive payment from most health plans. It is recommended that you receive prior authorization when performing service related to foot orthotics. It is also recommended that in order to insure payment in the case of worker’s compensation, that you receive written prior authorization with fees attached to the services you are about to perform. I have learned the hard way that this is the best way to deal with the worker’s compensation world.
With regard to the need for outcomes studies, we discussed the fact that we are living in an evidence-based medicine era. The fact that many health insurance policies and payment for procedures will now and in the future will be based on good medical evidence. At this time, we have primarily anecdotal evidence for the majority of services we perform. Although we know that many such procedures work, we do not have good randomized control studies or RCTs to verify objectively that these procedures that we perform are in fact effective. We discussed the fact that it is important for the academic institutions to generate research to validate the services we perform by performing randomized control trials in such an academic setting. We are told that this will be explained to the academic institutions and hopefully we will see more evidence for what we do in good outcome studies.
We also discussed the fact that United Health Care, in some states, is not paying for initial office visits and procedures. I told the group that although we do not have this problem in California at this time, we once did. The way I dealt with it at that time was that I told the Medical Director at United Health Care that if they did not pay for initial office visit at the same time a minor procedure was performed, like an nail avulsion or a taping or cortisone injection, then I would be forced to see the patient for an initial visit, get paid, reappoint the patient for another day and then perform whatever procedure was necessary. I explained to the Medical Director that this would cause a loss of work time for the patient, general time for the patient and would probably be a greater burden on not only the patient, but the patient’s employer. With this logic in hand, United Health Care at that time rescinded their policy of only paying for initial office visit and not a procedure or vice versa. Since that time, we have not had any such problem in California. We will see if the other states adapt our strategy.
At this time, I am going to end this report. Once again, it has been a pleasure serving as the Chair of the Health Policy Committee for the California Podiatric Medical Association. Remember we are here to serve you and can only function if you inform us of problems in either reimbursement or discrimination by health plans. If we do hear from you that things are not going as well as we think they are, then we will follow through and fight to be sure our rights are preserved.
O N YO u R TOES
CPMA Members Help Defeat Proposition 46
By a 2 to 1 margin California voters rejected Proposition 46, a ballot measure that would have dramatically increased health care costs and reduced patients’ access to care by raising the payouts in lawsuits against podiatric physicians and other health care providers.
As of Nov. 5, the vote tally for Proposition 46 stood at:
Yes - 32.9%
No - 67.1%
The California Podiatric Medical Association (CPMA) was a member of No on 46, which was made up of over 600 organizations consisting of health care providers, labor, business, local governments, community clinics and many others who worked diligently during the past year and a half to educate voters about the dangers and true intent of Proposition 46. While Prop 46 proponents utilized smokescreen provisions of drug testing doctors and prescription drug monitoring in an attempt to confuse voters, the main goal of the measure was to quadruple the cap on non-economic damages under the Medical Injury Compensation Reform Act (MICRA).
“The California Podiatric Medical Association is extremely proud to have been a member of such a broad, diverse and effective coalition that opposed Proposition 46,” said CPMA President Thomas Elardo, DPM. “We have made a strong and convincing statement about our dedication to our patients and our commitment to protecting accessible health care for the people of California, and we are pleased that voters saw through the smokescreen to see the initiative for what it really was.
The No on 46 campaign utilized a multi-faceted approach that included statewide TV and radio ads, extensive social media and press outreach, and a robust grassroots outreach program.
The campaign provided information and education materials at no cost to all members of the coalition, and CPMA members played a critical role in distributing these to their patients, families and friends, as well as informing colleagues of the measure’s potential devastating impact, including increased heath cost, reduced access to care and loss of privacy.
“We saw strong participation from our members through community outreach, and I would like to express my sincere gratitude to our members for those efforts,” said Elardo. “That kind of activism throughout our coalition contributed in a major way to the defeat of Prop 46.”
Although the defeat of Proposition 46 was a resounding one, and MICRA remains intact, proponents of the initiatives have already stated that they will be back. CPMA and its coalition partners will continue its vigilance and work to ensure the Legislature and the public understand why MICRA is essential to preserving access to health care in California.
CPMA Adds Important New Tools to its Duals Resource Center to Help Doctors and Patients Understand and Navigate the Program
The 2012 California state budget authorized a three-year demonstration project that transitions dual eligibles into managed care and allows them to receive medical, behavioral, long-term supports and services and home-and-community-based services coordinated through a single health plan.
The Cal MediConnect project was approved in 8 counties: Alameda, Los Angeles, Orange, Riverside, San Bernardino, San Diego, San Mateo, and Santa Clara. No more than 456,000 individuals will be allowed to enroll into Cal MediConnect. Los Angeles’ enrollment will be capped at 200,000.
To help doctors and their patients better understand the program, the California Podiatric Medical Association (CPMA) has added important new tools to its Duals Resource Center on the Association’s website CalPMA.org
For more details on Cal MediConnect, visit www.calduals.org
Medicare Finalizes Fee Schedule Changes for 2015
The Centers for Medicare and Medicaid Services (CMS) has published its 2015 Medicare Physician Fee Schedule final rule the Federal Register. The 1,200 word payment rule contains several notable changes.
As earlier proposed, the rule expands the services eligible for telemedicine reimbursement and extends the new payment policies for non-face-to-face care coordination. It allows primary care physicians to be paid for care management of Medicare beneficiaries with two or more chronic conditions. These are tasks (including managing lab and imaging reports, medications and care plans in addition to talking with patients and families on the phone) physicians commonly provide, but have not been paid for in the past.
CMS continues to move up the implementation timeline for the Value-Based Payment Modifier (VBM). However, the final rule scales back the penalties for practices with fewer than 10 physicians. While the final rule still maintains a potential pay cut of 4 percent for larger medical groups, practices with fewer than 10 physicians will not be subject to more than a 2 percent VBM penalty.
Also removed from the final rule was a CPMA supported proposal to eliminate the CME exemption in the Physician Payments Sunshine Act, which requires reporting and public posting of financial interactions between medical device and drug manufacturers and physicians and teaching hospitals. CPMA and APMA joined dozens of other medical associations in calling on the agency to eliminate this requirement because it would “chill physician participation in independent [continuing education] programs.”
CMS is moving forward with the public disclosure of physician quality and meaningful use information on the Physician Compare website. However, at organized medicine’s urging, physicians will be allowed to review the information and correct inaccurate data
prior to publication. CMS also pulled back its proposal to publish benchmark information.
CMS is proceeding with the plan to require physicians to report nine quality measures in three “domains” and one “cross-cutting” measure in 2015 for the Physician Quality Reporting System (PQRS).
And in 2015, the Physician Quality Reporting System (PQRS) becomes a penalty-only program. No bonuses will be paid. Physicians must successfully report in 2015 to avoid penalties in 2017.
Despite strong opposition from APMA, AMA, CPMA, CMA and others in organized medicine, CMS moved forward with the elimination of all 10- and 90-day global surgical packages because CMS says it lacks the ability to verify the number, type and relative costs of postoperative visits. Packages would only include preoperative services and care given the day of surgery. CMS will be transitioning all services with a 10-day global period to a 0-day global period by 2017. All 90-day global periods will be shifted to 0-day global periods by 2018.
(Source; CMA 11/14/2014)
DME MACs Delay Implementation of PCD LCD
DME Medicare Administrative Contractors (MAC) published a notice on October 16 stating that all four jurisdictions would be delaying implementation of recently finalized local coverage determinations (LCD) for pneumatic compression devices (PCDs). The scheduled effective date was November 1. DME MACs have not published a future effective date. These LCDs would have prevented podiatric physicians from prescribing PCDs regardless of the scope of practice in their respective states. The current LCD and related policy article will remain in effect.
Working with the APMA Health Policy & Practice Department, four members practicing in each of the DME MAC jurisdictions submitted formal requests for reconsideration of the LCD in their respective DME MAC jurisdictions. CPMA Secretary/Treasurer Devon N. Glazer, DPM submitted the request for California’s designated Jurisdiction D. APMA is currently contacting congressional staff and seeking inquiry for additional information from the HHS secretary about this LCD and the role of state determination of scope of practice. CPMA and APMA are considering all alternatives to contest these LCDs because of the precedential impact they may have. CPMA will keep members updated as information is made available.
(Source: APMA, October 16, 2014)
Doctors’ Offices Encouraged to Familiarize Themselves with Exchange Plan Changes as Covered California begins Open Enrollment
Covered California began enrollment for its second year on November 15 and exchange officials are predicting a 45 percent jump in enrollment, from 1.2 million in 2014 to 1.7 million in 2015. Last year, open enrollment was a six-month process, this year it will be half as long, starting Nov. 15 and ending Feb. 15.
In anticipation of this year’s open enrollment, some payors have updated their exchange plan offerings for 2015, including plan types and plan names. The California Podiatric Medical Association (CPMA) will be publishing details of these changes as they are announced. See the most current exchange-related news and updates on the ACA Covered California Resources page on the CPMA website – CalPMA.org.
Providers are encouraged to familiarize themselves with the changes and to verify their exchange plan participation status on the plans’ websites. When searching the provider directories, it’s important to select the correct exchange product type, as



Unfortunately, Covered California does not offer a central provider directory. Doctors will need to contact the Exchange’s plans individually to determine their participation status. The current plans, their website and phone numbers can be found on CPMA’s ACA/Covered California Resources page in the 2015 Covered California exchange Plans folder, which CPMA will continue to update as information is made available.
California Adopts Toughest Regulations in US to Protect Hospital Workers Caring for Ebola Patients
California now has some of the toughest regulations in the country to protect health care workers who treat patients with Ebola.
The California Occupational Safety and Health Administration has announced new requirements for the state’s acute care hospitals in regards to Ebola. Hospitals must provide workers with hazardous material suits, respirators and isolation rooms, and conduct extensive training to those working with patients suspected of having the virus.
The rules are mandatory with civil penalties for hospitals that fail to comply. The regulations go further than the voluntary guidelines recommended by the Centers for Disease Control and Prevention (CDC), which California hospitals have followed up until now. The new requirements were unveiled following a worldwide protest Thursday and a two-day strike by thousands of Kaiser Permanente nurses, who demanded hospitals provide stronger protections for health care workers treating Ebola patients.
So far there have been no cases of Ebola reported in California.
(Source: Fierce Healthcare 11/17/2014)
• Pharmacies and prescribers must use software that is certified compliant with Drug Enforcement Agency (DEA) regulations.
• E-prescribing software is certified by DEA-approved entities.
• Prescribers must go through an identity-proofing process conducted by a DEA-approved entity.
• Following identity proofing, the software company issues a twofactor credential to a prescriber. A prescriber uses the two-factor credential to “sign” electronic prescriptions of controlled substances.
• The hard token provided as part of the two-factor credential may not be in possession of anyone other than the prescriber. E-prescribing is not mandatory in California, and the state does not place limitations on it. E-prescribing is a meaningful use criterion for the federal electronic health record (EHR) incentive program. Prescription software can be used for noncontrolled substances and most are associated with an EHR. Prescribers and staff each get unique passwords. Staff may use software to add patient information, access information and queue up refill orders (except for controlled substances).
Additional information and a Q-and-A on e-prescribing controlled substances regulations are available on the DEA website.
(Source: CDA)
In Surprise, Supreme Court to Hear Challenge to ACA Subsidies
E-prescribing Hydrocodone
Drugs
Now that hydrocodone combination products, such as Vicodin and Norco, have been reclassified as Schedule II drugs, CDA Practice Support has been receiving inquiries about how to prescribe these drugs electronically.
Doctors can no longer call or fax prescriptions for these drugs to pharmacies because Schedule II drugs have more restrictions.
There is a lot of e-prescribing software available, but not all are certified for use with controlled substance prescriptions A list of software with Electronic Prescriptions for Controlled Substances (EPCS) certification can be viewed on the Surescripts website, surescripts.com/certified (click the “EPCS” option under the “Products” list to the left side of the vendor listings). Surescripts is an e-prescription network connecting prescribers, pharmacies, payers and prescription benefit managers through the certification of software for the following services: prescription benefit, medication history and prescription routing. However, Surescripts does not certify for EPCS compliance. Currently, 30 companies have EPCS certification. Prescribers should verify certification with the company directly.
The U.S. Drug Enforcement Agency issued in 2010 regulations for e-prescribing of controlled substances. The basic rules are as follows:
The US Supreme Court has agreed to take up a new challenge to the Affordable Care Act (aka Obamacare) during its current term. Their decision could determine whether the health care law lives or dies.
The case, King v. Burwell, rests on whether the federal government can legally hand out health care subsidies in 34 states that have opted out of creating their own exchanges. About 87 percent of people enrolled under the ACA receive the subsidies.
If the high court rules against the premium credits, it would gut a core component of the law that’s already gone into effect for more than 4 million people in the U.S.
The ruling would cause a “domino effect” on other parts of the law, the researchers said.
Without subsidies, they cautioned that the federal government would be forced to rethink its policies on the individual mandate, regulatory reforms and state exchanges.
Economists have predicted that if the lawsuit is successful, it would cause a “near death spiral” for the individual market, according to an October 2014 study by the independent research group, RAND.
The study found that without the subsidies, prices would jump sharply and many people simply could not afford to enroll.
A decision to strike down the subsidies in federally-run exchange states could end up making insurance unaffordable for millions of people and threaten the viability of the law’s entire health insurance program, including rules that eliminate preexisting conditions, no lifetime limits, and in the ability of insurance companies to drop enrollees that become ill.
(Source: The Hill 11/7/2014)
Health Care Sector Accounted for 15% of CA’s Data breaches in 2013
The number of data breaches reported by the health care industry and other sectors in California increased by 28% from 2012 to 2013, according to an annual report released by California Attorney General Kamala Harris.
Health care breaches in 2013 affected 1.1 million records, accounting for 6% of total records affected by data breaches in the state last year.
The report also found that in the health care sector during 2012 and 2013:
• 70% of breaches were caused by physical theft or loss;
• 20% were caused by errors; and
• 9% were caused by malware and hacking.
More than 50% of breaches in the health care sector involved Social Security numbers, while 75% involved health information.
The report recommends that the health care sector “[c]onsistently use strong encryption to protect medical information on laptops and on other portable devices and should consider it for desktop computers.”
It notes that full encryption is an “affordable solution” and should be applied to in-office computers, laptops and portable devices (Attorney General report, October 2014).
The report also cites a recent study by the Ponemon Institute, which found that criminal attacks targeting the health care system are growing.
(Source: CaliforniaHealthline.org, Oct 29, 2014) SPD Transition from FFS to Managed Care becomes Mandatory December 1, 2014
Between June 2011 and May 2012, California moved approximately 380,000 seniors and persons with disabilities (SPDs) in 21 counties from Medi-Cal fee-for-service to managed care. The change was intended to improve care coordination and access to care in the long term. The SPD transition is unrelated to the current eight county dual eligible pilot project for Cal MediConnect.
The 2014-15 state budget included language that changed managed care enrollment for the Medi-Cal only SPD population from voluntary to mandatory effective December 1, 2014. Previously this transition was scheduled for September 1, 2014.
There are approximately 25,000 SPDs expected to transition in the following counties: Alpine, Amador, Butte, Calaveras, Colusa, El Dorado, Glenn, Imperial, Inyo, Mariposa, Mono, Nevada, Placer, Plumas, San Benito, Sierra, Sutter, Tehama, Tuolumne and Yuba.
In San Benito, managed care enrollment for SPDs will remain voluntary since there is only one participating health plan in that County.
(Source: CMA 11/6/2014)
California Continues to Tweak Timeline for Duals Project
State health officials have dropped Alameda County and its 26,000 dual-eligibles from Cal MediConnect, California’s demonstration project for Californians eligible for Medi-Cal and Medicare.
The timeline for Orange County was pushed back one month for automatic enrollment to start. Orange County had already been delayed to start no sooner than July 2015 because of federal concerns about the oversight readiness of the CalOptima health plan. Enrollment still will begin in July 2015, but passive enrollment - in which beneficiaries are automatically enrolled if they do nothing - now will not begin until August 2015.
(Source: CaliforniaHealthline.org, 11/17/2014)
Anthem to Require NDC on claims for Certain Physician-Administered Drugs
On September 30, Anthem Blue Cross notified physicians that effective January 1, 2015, it will require all professional providers to bill using the 11-digit National Drug Code (NDC) for drugs administered in a physician’s office.
In the notice, Anthem says that currently, the lack of uniform coding system for drugs can result in inaccurate payments. The payor also states the change will allow it to be more consistent with Medicaid requirements and maintain consistent claims billing guidelines across all Anthem products.
While the notice said the NDC would be required for all professional providers submitting claims “for drugs administered in a physician’s office,” it also indicated that the payor would only deny claims for “Not Otherwise Classified [NOC] or Miscellaneous drug HCPCS” that did not include the NDC. Anthem later clarified that the change only applies to physician-administered drugs in a physician’s office for NOC or miscellaneous HCPCS codes.
Anthem also said that the policy change does not affect vaccine CPT codes.
Practices with questions about the policy change can contact Anthem Network Relations at networkrelations@wellpoint.com
(Source: CMA 11/12/2014)
DMHC Report Finds that Anthem and blue Shield Violated State Law
Anthem Blue Cross and Blue Shield of California violated state law by misleading consumers about the size of their provider networks, according to a report by the state Department of Managed Health Care.
Complaints of narrow networks have led to lawsuits filed against both insurers.
• In July, Consumer Watchdog filed a class-action lawsuit alleging that Anthem:
• Delayed giving its customers complete information until it was too late for them to switch their coverage choice;
• Did not inform its customers that it no longer offered out-ofnetwork coverage in four of the state’s largest counties -- Los Angeles, Orange, San Diego and San Francisco; and
• Misled or did not inform its customers about which doctors and hospitals were participating in the insurer’s new plans.
In September, Consumer Watchdog filed a separate lawsuit against Cigna and Blue Shield of California, alleging that the insurers:
• Delayed giving their customers complete information until it was too late for them to switch coverage;
• Offered inadequate provider networks; and
• Presented inaccurate lists of participating providers
DMHC filed the report after a five-month investigation into allegations that the insurers were posting inaccurate provider lists.
The report was based on surveys of doctors listed under the insurers’ provider directories. DMHC investigators asked the providers about the status of their contracts with Covered California plans and whether they were accepting new patients.
The DMHC investigation found that more than 25% of the providers listed in provider directories offered by Anthem and Blue Shield were not accepting patients with Covered California plans or were no longer at the location listed in the directory.
Specifically, among physicians listed as in-network providers for Anthem, the report found that:
• 12.8% did not accept patients with Covered California plans; and
• 12.5% had changed locations.
Among Blue Shield of California providers:
• 8.8% did not accept patients with exchange plans; and
• 18.2% had changed locations
The two insurers account for almost 60 percent of patient enrollment in Covered California. Both insurers are also utilizing networks for their exchange/mirror products that are significantly narrower than their regular PPO networks. These narrowed networks, combined with inaccurate provider directories, have led
to significant confusion and frustration for both physicians and patients.
According to the report, both insurers already implemented “corrective action,” including:
• Checking contract statuses with providers;
• Contacting providers directly to confirm their status; and
• Monitoring and improving the accuracy of the provider directories.
However, DMHC found that the insurers failed to fully correct three violations of California’s Health and Safety Code related to inaccurate provider directories.
DMHC has turned the matter over to the Office of Enforcement for additional corrective action and other remedies as needed. The department has not said if the plans will be fined, though it plans to conduct a follow up survey of in-network provider listings in six months to determine whether the violations have been corrected and whether the insurers are complying with state law.
CPMA will continue to monitor the situation closely, as it may have an impact on other actions underway in California. Such actions include the impending review of Medi-Cal managed care plan networks and directories ordered by the Joint Legislative Audit Committee, as well as the eight class action lawsuits currently pending in California courts over narrowed networks and inaccurate directories. The audits may also prove to be a popular topic in the next legislative session.
(Source: CaliforniaHealthline.org 11/19/2014)
DHCS Releases Duals Project Provider Toolkit
The California Department of Health Care Services (DHCS) has published a physician toolkit to help providers and their patients understand the Cal MediConnect duals demonstration project. The toolkit has been developed in conjunction with Harbage Consulting and various stakeholder groups, including the California Podiatric Medical Association.
The toolkit contains several documents, including an overview and several fact sheets that include information on the following:
• How to submit crossover claims to Medi-Cal plans
• Contracting with Cal MediConnect plans
• How crossover claims are processed for Medi-Cal managed care patients
• Continuity of care
• Sample patient letters (for contracted and non-contracted physicians)
The toolkit also confirms that if a patient opts out of Medicare Advantage and remains with fee-for-service Medicare, the Medi-Cal managed care plan cannot require authorizations for physician
services as the secondary payor (see the Coordinated Care Initiative Overview fact sheet for more information). It should be noted that no change has been made to the rules governing the billing of the 20 percent Medicare copay for dual eligible patients. It continues to be unlawful to bill dual eligible patients. In limited circumstances, Medi-Cal may cover Medicare coinsurance and copays. Such “crossover” claims for Medicare coinsurance and copays should be sent to the patient’s Medi-Cal plan (see Payment for Medicare Physician Services Under the CCI fact sheet for more information.)
Providers should also be aware that the new Cal MediConnect “Choice Form” that is now online is only a visual sample, indicating patients must use their unique forms sent to them in their “Plan Choice” booklets.
Lastly, if you or your patients have questions that the plan cannot respond to, you can always contact the Cal MediConnect Ombudsman at (855) 501-3077 (TTY 1-855-847-7914), Monday through Friday, 9 a.m. to 5 p.m.
CPMA Members can find the Toolkit in the Duals Resource Center on the CPMA website CalPMA.org.
(Source: CMA 11/6/2014)
ICD 10 Countdown Clock is Ticking
With less than a year until the October 1, 2015, implementation date for ICD-10, doctors should be evaluating the readiness of their practices to transition to the new code set. The one-year delay in implementation came as a welcome reprieve for many physician practices that were struggling to meet the October 2014 deadline. The extent to which practices made positive use of the delay remains to be seen.
ICD-10 (The International Classification of Disease tenth revision) is a system of coding created in 1992 as the successor to the previous ICD-9 code set. ICD-10 will include new procedures and diagnoses, which the U.S. Department of Health and Human Services hopes will improve the quality of information available for quality improvement and payment purposes.
the 2015 Western Foot and ankle Conference, June 25-28, at the Disneyland Hotel and Convention Center will feature an ICD-10 check-up to help doctors see where they are, and where they should be in the transition.
Members can find information on the ICD-10 page in the Compliance Center on the CPMA website CalPMA.org and on the APMA website.
For additional information about ICD-10, visit the CMS website at www.cms.gov/ICD10
Durable Medical Equipment (DME)
Ankle-Foot Orthosis (HCPCS L1960, L1970, & L4360) Quarterly Results of Service Specific Prepayment Review
The Jurisdiction D DME MAC Medical Review Department is conducting a service specific review of HCPCS code L1960.
The quarterly edit effectiveness results from June 2014 through September 2014 are as follows:
The L1960 review involved 213 claims, of which 170 were denied. Based on dollars, this resulted in an overall potential improper payment rate of 81%.
The L1970 review involved 335 claims, of which 284 were denied. Based on dollars, this resulted in an overall potential improper payment rate of 83%
The L4360 review involved 1,262 claims, of which 1,237 were denied. Based on dollars, this resulted in an overall potential improper payment rate of 98%
Top Denial Reasons
• The treating physician’s records did not provide detailed documentation to support medical necessity of a custom orthosis rather than a prefabricated orthosis
• Documentation submitted was insufficient to support custom coverage criteria
• No documentation was received in response to Additional Documentation Request (ADR) letter
• Documentation submitted was insufficient to support basic coverage criteria
• Documentation is insufficient to support that substantial modifications were made for the custom fitted item billed
• No proof of delivery submitted
Going Forward
Based on the results of these reviews, Noridian will continue with the Prepayment Service Specific Reviews.
Educational Resources
It is important for suppliers to be familiar with the documentation requirements and utilization parameters as outlined in the Ankle-Foot/Knee-Ankle-Foot Orthosis (AFO) Local Coverage Determination (LCD) L142 and Policy Article A19800.
Suppliers can also review a specific policy Documentation Checklist for Ankle-Foot/Knee-Ankle-Foot Orthosis on the Noridian website.
Noridian provides educational offerings by scheduling supplier workshops, training opportunities, and presentations.
Information about probe/error validation reviews may be found in CMS Publication 100-8, Program Integrity Manual (PIM), Chapter 3.
Policy Education
The treating physician’s records did not provide detailed documentation to support medical necessity of a custom orthosis rather than a prefabricated orthosis.


For custom-fabricated orthoses, there must be detailed documentation in the treating physician’s records to support medical necessity of custom-fabricated rather than a prefabricated orthosis. This information will be corroborated by the functional evaluation in the orthotist or prosthetist’s records. This information must be available upon request.
Documentation submitted was insufficient to support custom coverage criteria.
AFOs and KAFOs that are custom-fabricated are covered for ambulatory beneficiaries when the basic coverage criteria and one of the following criteria are met:
• The beneficiary could not be fit with a prefabricated AFO or,
• The condition necessitating the orthosis is expected to be permanent or of longstanding duration (more than six months) or,
• There is a need to control the knee, ankle or foot in more than one plane or,
• The beneficiary has a documented neurological, circulatory, or orthopedic status that requires custom fabricating over a model to prevent tissue injury or,
• The beneficiary has a healing fracture which lacks anatomical integrity or anthropometric proportions.
If a custom-fabricated orthosis is provided but basic coverage criteria and the additional criteria 1-5 for a custom-fabricated orthosis are not met, the custom-fabricated orthosis will be denied as not reasonable and necessary.
No documentation was received in response to Additional Documentation Request letter.
Suppliers have 45 days from the date of the ADR letter to respond. Failure to respond within 45 days may result in partial or complete denial of the claim.
Suppliers are in violation of Supplier Standard #28 when, upon request, they fail to provide requested documentation to a Medicare contractor. Medicare regulations (42 C.F.R 424.516[f]) stipulate that a supplier is required to maintain documentation for seven years from the date of service and, upon the request of CMS or a Medicare contractor, provide access to that documentation. Therefore, the consequences of failure to provide records may not only be a claim denial but also referral to the NSC. The supplier standards can be found in 424 CFR Section 424.57(c).
Documentation submitted was insufficient to support basic coverage criteria.
AFOs described by codes L1900, L1902–L1990, L2106–L2116, L4350, L4360, L4386 and L4631 are covered for ambulatory beneficiaries with weakness or deformity of the foot and ankle, who require stabilization for medical reasons, and have the potential to benefit functionally.
Documentation is insufficient to support that substantial modifications were made for the custom fitted item billed. Items requiring substantial modification by a qualified practitioner (as defined in the related Policy Article Coding Guidelines) are coded as custom fitted (L1910, L1930, L1932, L1951, L1971, L2035, L2112-L2116, L2132-L2136, L4360, L4386, L4396).
Documentation must be sufficiently detailed to include, but is not limited to, a detailed description of the modifications necessary at the time of fitting the orthosis to the beneficiary. This information must be available upon request.
Custom fitted orthotics are:
• Devices that are prefabricated.
• They may or may not be supplied as a kit that requires some assembly. Assembly of the item and/or installation of add-on components and/or the use of some basic materials in preparation of the item does not change classification from Off –the-Shelf (OTS) to custom fitted.
• Classification as custom fitted requires substantial modification for fitting at the time of delivery in order to provide an individualized fit, i.e., the item must be trimmed, bent, molded (with or without heat), or otherwise modified resulting in alterations beyond minimal self-adjustment.
• This fitting at delivery does require expertise of a certified orthotist or an individual who has equivalent specialized training in the provision of orthosis to fit the item to the individual beneficiary
Substantial modification is defined as changes made to achieve an individualized fit of the item that requires the expertise of a certified orthotist or an individual who has equivalent specialized training in the provision of orthotics such as a physician, treating practitioner, an occupational therapist, or physical therapist in compliance with all applicable Federal and State licensure and regulatory requirements. A certified orthotist is defined as an individual who is certified by the American Board for Certification in Orthotics and Prosthetics, Inc., or by the Board for Orthotist/ Prosthetist Certification.
No proof of delivery submitted.
Proof of delivery (POD) is a Supplier Standard and DMEPOS suppliers are required to maintain POD documentation in their files. For medical review purposes, POD serves to assist in determining correct coding and billing information for claims submitted for Medicare.
No proof of delivery submitted.
Proof of delivery (POD) is a Supplier Standard and DMEPOS suppliers are required to maintain POD documentation in their files. For medical review purposes, POD serves to assist in determining correct coding and billing information for claims submitted for
C l ASSI f IEDS
P RACTICE FOR S ALE
Premier Southern California Podiatry practice for sale. The practice consists of a main office, which contains Medicare Certified2 OR Surgical Center used exclusively for foot and ankle surgery. A portable fluoroscopy unit is within the ASC. A satellite office is within 30 minutes. All aspects of Podiatry are treated with a full mix of patients. Only private, PPO and Medicare insurance are taken. A new 2010 electronic billing system is included. Please email drjohns5462@yahoo.com or call 954-612-7144 for details.
A SSOCIATE WANTED
Seeking associate leading to purchase of practice. Busy office with all types of in-office and out-of-office facilities including private nursing and retirement facilities. 20% medicine; 50% c&c; 30% orthotics. Excellent terms. Email CV to sandiegopodiatry@gmail.com
Podiatry Practice for Sale East Bay Area, Ca. (Oakland, Hayward). Office, nursing homes, and private salaried positions available. To inquire contact ellwenger@comcast.net
P ODIATRY P RACTICE FOR S ALE IN b ERKELEY
Bay Area Berkeley, California. Established 34 yo practice. Able to get buyer into HMO plans. Priced based on value of equipment, instruments and goodwill. Never a malpractice issue. Good referral base. To inquire, contact footguy123@aol.com
PRACTICE FOR SALE IN SAN JOSE, CA
This Podiatry/Spa Practice has been established for 7 years with a strong brand name, internet presence and patient population. The practice consists of office based Podiatry care plus Spa Nail and Skin Care. This is a unique opportunity to take advantage of an emerging area of Podiatry practice that is cash based. It is located on the hospital campus with surgery centers nearby, and is set to grow with the right Podiatrist. The office includes licensed trained staff, a modern fresh decor, four treatment rooms, patient’s lists on EMR, web sites and a Pinpoint Foot Laser. Email: schrisdpm@sbcglobal.net and log onto the web sites for more information. www.NeatFeetPlus.com www.NeatFeetNow.com
P ODIATRIST WANTED
Established medical group, in Beverly Hills, CA, looking for an experienced podiatrist. This position entails making rounds at hospitals, skilled nursing facilities and scheduled office appointments. Must be comfortable with all aspects of podiatric care, have great bedside manner and will be doing no less than the hiring partners. Full-time position with competitive salary. Send CV to administrator@footnankledoc.com
R OCK S OLID P RACTICE
15 minutes from San Francisco. Grossing 300K and growing. All private, no HMOs. All sports/surgery. Turnkey opportunity. Call 510-214-8283
C ENTRAL CA P RACTICE F OR S ALE
I will stay for transition. Price and terms negotiable. Serious Inquiries only call/txt 209-617-0241 or email sbaileydpm@aol.com
LOOKING TO H IRE P ODIATRISTS
For new company: Platinum Podiatry
Great company, with patients already lined up! No need to market yourself!
We are currently located throughout California from Southern, to Central, to Northern and will eventually be one of the biggest nursing home podiatrist company’s in the nation!
- flexible hours/ make your own schedule
- part-time and full time available
Requirements:
- graduated from Certified Podiatry school and residency performed
- driver’s license, car registration and insurance
Briefly, we arrange all scheduling, documentation, consents, billing, and collections. This allows our practitioners to concentrate on delivering excellent and dignified clinical care.
If you’re interested in an Independent Contract Podiatrist position please contact Shelley Cable at (310) 600-1720 or SCable@PlatinumPod.com
Thank you and looking forward to hearing from you!
PART - TIME P ODIATRY A SSOCIATE (I NLAND E MPIRE )
Seeking Part-time Podiatry Associate to service skilled nursing and assisted living facilities in the Inland Empire, specifically San Bernardino and Riverside Counties. Staff and supplies will be provided. Independent contractor.
Must have:
- Valid state license
- Valid malpractice insurance
- Valid DEA license
- Reliable transportation
Please send resume with contact information in response.
Thank you for your interest, Dr. Pete Carrasco Jr., Carrasco Podiatry Corp. pcarrasco@pete-melissa.com
Medicare reimbursement. Regardless of the method of delivery, the contractor must be able to determine from delivery documentation that the supplier properly coded the item(s) submitted for Medicare reimbursement and that the item(s) are intended for, and received by, a specific Medicare beneficiary.
(Source: Nordian via Tony Poggio, DPM)
CMS Launches More User Friendly Public Open Payments Search Tool
The Centers for Medicare and Medicaid Services (CMS) has released a new online search tool for the Open Payments website, which allows consumers to see the financial relationships between drug and medical device manufacturers and physicians as reported under the Physician Payments Sunshine Act. This new tool provides the ability to search identified data for physicians, teaching hospitals, or companies making payments by name, city, state and specialty. Upon performing a search, the returned results will include all three payments types (general payments, research payments and ownership in companies) on one screen. When the website first went live on September 30, the search tool only allowed users to scroll through huge spreadsheets to look up information about physician payments.
CMS has announced that over the coming weeks, the search tool will continue to be developed to include more functionality with the objective of providing added value to users. Additional enhancements already in the works include displays of summary data, charts, graphs and more detailed data.
Doctors can visit the CMS Open Payments website to view the data and use the new search tool.
Are You Having Problems With the New Prescription Drug Prior Authorization Form?
A new law recently took effect that streamlines and standardizes the prior authorization process for prescription drugs for most patients with PPO products. The new law (SB 866), which was supported by CPMA requires all insurers, health plans (and their contracting medical groups/IPAs) and providers to use a standardized two-page form for prior authorizations of prescription medications.
The law also requires plans and insurers to make a determination on prescription drug prior authorization requests within two days of receipt. If they fail to do so, the requests will be deemed authorized. The new law does not expand the list of medications that require a prior authorization.
The requirement for HMO products, including Anthem Blue Cross and Blue Shield of California, becomes effective on January 1, 2015. The regulation for Department of Insurance-regulated products, including all other PPOs and Blue Cross and Blue Shield Life & Health products, became effective on October 1, 2014. However, in an effort to avoid confusion for practices, many plans/insurers
implemented the new form across most, if not all, of their product lines on October 1.
The California Podiatric Medical Association (CPMA) is interested in hearing from members that have experienced difficulties with the new form. If your practice has run into any problems with the form itself, integration into your EHR, submission of the form to the payor, multiple requests for medical records from the payor, delays in processing by the payor, etc., please contact CPMA at (800) 794-8988 or email cpma@calpma.org (in the subject line please put New Prior Authorization Form) to share your experience.
Correct Coding – Medicare Coverage for Shoes
Medicare has limited coverage provisions for shoes used by beneficiaries. Section 1862(a)(8) of the Social Security Act (SSA) says:
[N]o payment may be made under part A or part B for any expenses incurred for items or services … where such expenses are for orthopedic shoes or other supportive devices for the feet, other than shoes furnished pursuant to section 1861(s)(12).
SSA 1861(s)(12) describes coverage for, “extra-depth shoes with inserts or custom molded shoes with inserts for an individual with diabetes” when certain specified requirements are met. Reimbursement is available for shoes used by beneficiaries with diabetes when the applicable coverage requirements are met. The Therapeutic Shoes for Persons with Diabetes (TSD) Local Coverage Determination (LCD) and related Policy Article discuss these payment rules in detail.
In addition to TSD, payment may be possible for shoes that are an integral component of a brace. CMS Internet Only Manual 100-02, Chapter 15, Section 290.B states:
Orthopedic shoes and other supportive devices for the feet generally are not covered. However, this exclusion does not apply to such a shoe if it is an integral part of a leg brace, and its expense is included as part of the cost of the brace. (Emphasis added).
These brace-related shoes are referred to as orthopedic footwear (ORF). Note that only the supplier of the brace may bill for payment for ORF in conjunction with claims for payment of the qualifying brace. Separate payment to a different supplier for shoes that are an integral component of a brace or for inserts and modifications to those shoes is not allowed. The Orthopedic Footwear LCD and related Policy Article address the applicable payment rules for these items.
There are situations where a beneficiary may qualify for both a diabetic shoe and a leg brace. CMS Internet Only Manual 100-02, Chapter 15, Section 140 says:
In situations in which an individual qualifies for both diabetic shoes and a leg brace, these items are covered separately. Thus, the diabetic shoes may be covered if the requirements for this section are met, while the brace may be covered if the requirements of §130 (Braces Benefit) are met. (Emphasis added).
FUNGICIDAL
NAFTIN GEL, 2%
INDICATIONS AND USAGE
NAFTIN Gel, 2% is an allylamine antifungal indicated for the treatment of interdigital tinea pedis caused by the organisms Trichophyton rubrum, Trichophyton mentagrophytes, and Epidermophyton floccosum in patients 18 years of age or older.

IMPORTANT SAFETY INFORMATION
ADVERSE REACTIONS
In clinical trials with NAFTIN Gel, 2%, the most common adverse reactions (2%) were application site reactions.
WARNINGS AND PRECAUTIONS
If redness or irritation develops with the use of NAFTIN Gel, 2%, treatment should be discontinued.

NAFTIN CREAM, 2%
INDICATIONS AND USAGE
NAFTIN Cream, 2% is indicated for the treatment of interdigital tinea pedis, tinea cruris, and tinea corporis caused by the organism Trichophyton rubrum in adult patients ≥18 years of age.
IMPORTANT SAFETY INFORMATION ADVERSE REACTIONS
In clinical trials with NAFTIN Cream, 2%, the most common adverse reaction (≥1%) was pruritus.
WARNINGS AND PRECAUTIONS
If redness or irritation develops with the use of NAFTIN Cream, 2%, treatment should be discontinued.
This means that the supplier of the TSD may bill separately for TSD while a different supplier may bill for the associated brace. There are no other categories of shoes that are eligible for Medicare reimbursement.
Different sets of HCPCS codes are used to identify the shoes, modifications, and inserts that may be eligible for payment. Suppliers must be sure to use the correct codes for each group of products.
Only HCPCS A-codes are used for TSD and related items. Only L-codes are used for ORF. Both the TSD and ORF related Policy Articles address these points.
• From TSD Policy Article & #9702;Codes for inserts or modifications (A5503 – A5508, A5510, A5512, A5513) may only be used for items related to diabetic shoes (A5500, A5501). They must not be used for items related to footwear coded with codes L3215L3253. Inserts and modifications used with L-coded footwear must be coded using L codes (L3000 - L3649).*
• From ORF Policy Article & #9702; Shoes, inserts, and modifications are covered in limited circumstances. They are covered in selected beneficiaries with diabetes for the prevention or treatment of diabetic foot ulcers. However, different codes (A5500-A5511) are used for footwear provided under this benefit. See the medical policy on Therapeutic Shoes for Persons with Diabetes for details.* & #9702; Depth-inlay or custom molded shoes for diabetics (A5500-A5501) and related inserts and modifications (A5503-A5511) are billed using these A-codes whether or not the shoe is an integral part of a brace. See the medical policy on Therapeutic Shoes for Persons with Diabetes for coverage, documentation, and additional coding guidelines.
& #9702; Oxford shoes that are an integral part of a brace are billed using codes L3224 or L3225 with a KX modifier. For these codes, one unit of service is each shoe. Oxford shoes that are not part of a leg brace must be billed with codes L3215 or L3219 without a KX modifier. & #9702; Other shoes (e.g., high top, depth inlay or custom shoes for non-diabetics, etc.) that are an integral part of a brace are billed using code L3649 with a KX modifier. Other shoes that are not an integral part of a brace must be billed using codes L3216, L3217, L3221, L3222, L3230, L3251-L3253, or L3649 without a KX modifier.
*Note: Transferring or otherwise attaching a TSD to a brace is NOT considered a modification to the TSD. HCPCS code A5507 must not be used to bill for this service. See Orthopedic Footwear section (below) for additional information.
Orthopedic Footwear
From the Nonmedical Necessity Coverage and Payment Rules section of the ORF Policy article:
Shoes are also covered if they are an integral part of a covered leg brace described by codes L1900, L1920, L1980-L2030, L2050, L2060, L2080, or L2090. Oxford shoes (L3224, L3225) are covered in these situations. Other shoes, e.g. high top, depth inlay or custom for non-diabetics, etc. (L3649), are also covered if they are an integral part of a covered brace and if they are medically necessary for the proper functioning of the brace. Heel replacements (L3455, L3460), sole replacements (L3530, L3540), and shoe transfers (L3600-L3640) involving shoes on a covered brace are also covered. Inserts and other shoe modifications (L3000-L3170, L3300-L3450, L3465-L3520, L3550-L3595) are covered if they are on a shoe that is an integral part of a covered brace and if they are medically necessary for the proper functioning of the brace. Shoes and related modifications, inserts, heel/sole replacements or shoe transfers billed without a KX modifier will be denied as non-covered because coverage is statutorily excluded.
According to a national policy determination, a shoe and related modifications, inserts, and heel/sole replacements, are covered only when the shoe is an integral part of a brace. A matching shoe which is not attached to a brace and items related to that shoe must not be billed with a KX modifier and will be denied as non-covered because coverage is statutorily excluded.
Shoes which are incorporated into a brace must be billed by the same supplier billing for the brace. Shoes which are billed separately (i.e., not as part of a brace) will be denied as non-covered. A KX modifier must not be used in this situation.
Shoes are denied as non-covered when they are put on over a partial foot prosthesis or other lower extremity prosthesis (L5010-L5600) which is attached to the residual limb by other mechanisms because there is no Medicare benefit for these items.
Refer to the LCDs, related Policy articles and the Supplier Manual for additional information about coverage, coding and documentation for these items.
For questions about correct coding, contact the Pricing, Data Analysis and Coding Contractor (PDAC) Contact Center at (877) 735-1326 during the hours of 8:30 a.m. to 4:00 p.m. CT, Monday through Friday.


Dear Members:
Thank you!

With membership in the California Podiatric Medical Association (CPMA), podiatric physicians are ensuring that their voices, the voice of their patients and the needs of the profession are represented on every level. CPMA provides education, practice support, protection and a stronger voice in government.
Your membership means that CPMA can carry on in its critical role of protecting and promoting California’s podiatric medical profession, its patients and physicians.
With your support your Association had a very successful year:
• CPMA’s assertive advocacy and educational efforts resulted in the Department of Health Care Services (DHCS) agreeing to utilize administrative measures to reimburse Medi-Cal services provided by podiatric physicians in hospitals and emergency rooms.
• CPMA’s unrelenting advocacy challenged the scope of the Duals (Medi-Medi) Project, which resulted in raising the awareness inherent in patient safety and access issues for this vulnerable group, which led to the Department of Health Care Services (DHCS) instituting significant changes to the program. CPMA also enhanced the Duals Resource Center on the Association’s website CalPMA.org, which contains indispensable information for members and their patients.
• CPMA joined with the California Medical Association (CMA) to successfully defeat Proposition 46, the trial lawyers’ imitative, which would have quintupled non-economic damage awards in malpractice cases and would have resulted in a tripling or quadrupling of malpractice premium rates in California.
• CPMA continued its diligent work on securing Physician and Surgeon status for California’s podiatric physicians.
Your participation and dues support made these and other valuable services possible, and will be crucial to our efforts next year to fully restore adult fee-for-service podiatric benefits in Medi-Cal and in our ongoing work to obtain the designation of Physician and Surgeon for California’s podiatric physicians.

Every member strengthens CPMA. Even when you don’t have the time to be personally involved, your membership supports the actions of other members who work to ensure that the voice of podiatric medicine is heard.
Thank you for your membership in CPMA. Your involvement is important and very much appreciated.
Sincerely,

Thomas J. Elardo, DPM


Jon A. Hultman, DPM, MBA, CVA President Executive Director


AT THE CO ll EGES

WesternU’s “A Tribute to Caring” Honorees Provide Care and Comfort to the Most Vulnerable
WesternU held its annual fundraiser “A Tribute to Caring” Nov. 8, 2014 at the Disneyland Hotel in Anaheim, California. The event raises money for student scholarships.
WesternU presented the Elie Wiesel Humanism in Healing Award, its highest honor, to Astrid Heppenstall Heger, MD, FAAP, executive director of the Violence Intervention Program at Los Angeles CountyUniversity of Southern California Medical Center and a professor of clinical pediatrics at USC’s Keck School of Medicine.
WesternU presented Inland Empire Health Plan (IEHP) its Access to Caring Award for making a difference in advancing health care access and availability to underserved people. IEHP is a not-for-profit, rapidly growing Medi-Cal and Medicare health plan in California.
WesternU Holds Cadaver Memorial
Western University of Health Sciences students honored their first teachers and patients at the student-sponsored Cadaver Memorial Service on Oct. 28, 2014.

Students who completed their gross anatomy course organized the memorial service for 52 Willed Body Program donors and their families, with special recognition by the Military Medical Student Association to the 13 donors who served in the military.
Students in the osteopathic medicine, podiatric medicine, dental medicine, and medical sciences programs shared personal thoughts and memories, read poetry and performed music and magic in honor of the donors.
Mike Reed, DPM ’18, quoted Walt Whitman’s poem, “O Me! O Life!” “…The powerful play goes on, and you may contribute a verse.”
“In some ways what he’s saying is life is relatively brief, and that humanity’s collective play is sung by the individual verses that we all get to speak in the brief time that we have here on earth,” Reed said. “I think the individuals who donated their bodies to us understood this, to some capacity. They’ve sung their verses very loudly, in my opinion, in teaching us. For me and others I talked to, I think their verses will echo on inside of us both now and on into the future.”
CPMA @ CSPM
On October 8, the California Podiatric medical association hosted its annual CPma @ CSPm day, which included a meet and greet lunch presentation for CSPm’s first and second year students. CPMA PresidentElect Ami Sheth, DPM (Los Gatos) and Director Adam Howard, DPM (Cupertino) discussed the changing face of medicine, the important role of podiatric physicians in health care delivery, and the critical role the California Podiatric Medical Association plays (CPMA) in amplifying and projecting the voice of podiatric physicians and their patients are heard, and to ensure podiatric medicine has a place at the table in order to address the needs of the profession.
the California Podiatric medical association and the California School of Podiatric medicine at Samuel merritt university wishes to thank orthrofix for it generous support of this year’s event.
www.merzusa.com

www.arthrosurface.com

www.newbalance/nbrx.com
www.bioventusglobal.com







www.bakocts.com

www.formula3.com

www.footwearetc.com
omieralabs.com
www.pedorthiclab.com
http://www.dginstruments.com/

www.dermpathdiagnostics.com

www.precisionmedproducts.com
www.blainelabs.com

www.wmt.com www.stryker.com
www.covidien.com
www.samuelmerritt.edu/

valeant.com
pacificadvisors.com/podiatry
www.integralife.com
www.picagroup.com
arthrex.com
www.televeresystems.com
vilex.com
tornier.com

Season’s



