5 minute read
Voice of the Expert
JOURNAL OF THE INDIAN MEDICAL ASSOCIATION, VOL 118, NO 06, JUNE 2020
View of the Expert
Advertisement
The Covid-19 pandemic rages on in the World. With more than eight million people affected and more than 450 thousand dead, the end is still nowhere in sight. India is still in the ascending limb of the epidemic curve and physicians of India are at the forefront of this struggle to quell the scourge. At this juncture, we thought it worthwhile to listen to Prof Manish Soneja, one of the foremost infectious disease experts in India. He is currently working at AIIMS, New Delhi, one of the premier medical institutions of the country. In the first week of June, 2020, members of the Editorial Committee of JIMA held an online interview with Dr Soneja. The transcript of that interview is presented here, exclusively for the readers of JIMA.
Q U E S T I O N N A I R E
1. Are you using steroids in COVID-19 patients? If so, for which indication? What is the regimen, dose and duration of therapy? What is the result?
The use of corticosteroids in COVID-19 has generated considerable debate.There was a valid concern based on studies showing lack of benefit and possible harm in SARS-CoV 1 and other viral pneumonia. However, the results of these studies had significant indication bias and the dose of steroids used was high. Although, still in press release, the results of RECOVERY trial, one of the largest trials on COVID-19 management, are encouraging with a significant mortality benefit in both ventilated patients and those who are on oxygen.
At present, our protocol is to use corticosteroids in carefully selected patients with progressive moderate and severe COVID-19 with the premise that a major part of pathophysiology at this stage is mediated by aberrant cytokine response with viral cytopathic effects being predominant in the early stages of illness. • Dose : Low to moderate dose for short duration without tapering 17
• Moderate
disease : 0.5 to 1 mg/ kg methylprednisolone for 3 days in two divided doses • Severe disease : 1 to 2 mg/ kg methylprednisolone for 5 to 7 days in two divided doses
The decision of whether to shift to dexamethasone from MPS, given the Prof Manish Soneja RECOVERY trial partial data released yesterday, needs to be taken after reviewing the details.
Editorial note : The RECOVERY trial is an exciting development in Covid-19 landscape. Readers are requested to go through the results very carefully. Also, be on the lookout for similar trials which will be published in the future.
2. Are you using Anticoagulants in COVID-19 patients? What is the dosage and duration of therapy? What is the anticoagulant regimen advised in such patients post discharge?
Anticoagulation is being used in moderate and severe COVID-19 illness provided there are no contraindications. The regimen currently being used is: • Moderate disease: Prophylactic dose of UFH or LMWH (e.g., Enoxaparin 40 mg SC OD) • Severe disease: High dose prophylactic UFH or LMWH (eg, Enoxaparin 40 mg or 0.5mg/kg SC BD), if no contraindications are present • Weight based dosing is preferred in patients who are overweight
Decision on administering therapeutic anticoagulation (as a form of prophylaxis) is
individualized based on patient factors.
JOURNAL OF THE INDIAN MEDICAL ASSOCIATION, VOL 118, NO 06, JUNE 2020
At present, we are not using anticoagulation postdischarge in absence of documented thrombotic episode; however, we eagerly await results of studies assessing the need for extended prophylaxis postdischarge which may alter our future protocol.
3. Can you please describe your ventilator strategy for COVID-19 patients? What settings do you use in the beginning? Then, how do you escalate?
COVID-19 patients are being managed with conventional low-tidal volume ventilation (ARDSnet protocol) with proning as perexisting guidelines. The subsequent settings are individualized based on patient characteristics and response. In view of the high percentage of dead space fraction seen in these patients (which may worsen with high PEEP levels)close monitoring with subsequent titration remains the key to ventilatory management in these patients.
Editorial Note : Recently, many critical care units of Kolkata have reported spectacular success with Covid-19 patients. All physicians must have a basic understanding of mechanical ventilation in the future.
4. Is there any treatment strategy to reduce the risk of being put on mechanical ventilation?
Although still preliminary, use of awake prone position has been shown in several small observational studies to delay the need for intubation in a small percentage of patients, and we routinely utilize it in our patients, unless contraindicated (NIH protocol). Additionally, a cautious and monitored trial of NIV (including HFNC) is being used to delay the need for intubation.
Editorial note : In resource limited countries like India, maneuvers to avoid mechanical ventilation are of utmost importance.
18
5. How do you identify cytokine storm in COVID-19?
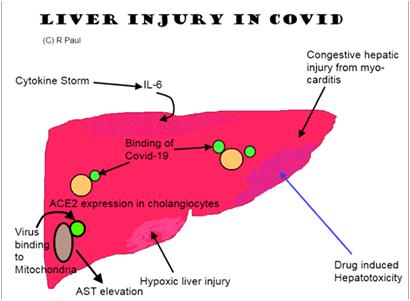
There is no single objective test to diagnose cytokine storm. There is no single biomarker which has been conclusively shown to correlate with the onset of cytokine storm in these patients. Until more studies are available, we use clinical judgement along with the trend of various available inflammatory markers including serum ferritin, CRP, IL-6 and LDH to identify cytokine storm.
6. What cut off value of IL6 in pg/ml do you use to start this drug?
Given the lack of appropriate good quality data and variability of IL-6 levels with available methods of detection, we do not use a single cut-off value for prescribing IL-6 receptor antagonist. We use clinical judgement as mentioned above along with the trend of various inflammatory biomarkers to decide on initiating anti-IL-6 agents.
7. Is there any role of identifying high risk patients to administer Tocilizumab?
It is of paramount importance to identify patients who are at high risk of disease progression particularly from moderate to severe disease wherein, selective immunomodulation may be considered. Nonetheless, there is unlikely to be a single marker for the same and clinical judgement supported by rising inflammatory markerswill most likely continue to be the criteria to consider selective immunomodulators for interrupting the inflammatory cascade.
8. Any other biomarkers can be done instead of IL6 or in addition to it to predict cytokine storm? (like CRP, IL10 etc.)
As mentioned above, there is no single objective test to diagnose cytokine storm. A host of markers of the pro-inflammatory cascade are being used in addition
to the clinical status of the patient to identify whether