Continuous Quality Improvement (CQI) Workgroup
Session 1: Foundations, Data, and Strategic Planning for CQI & VBC Success



Continuous Quality Improvement (CQI) Workgroup
Session 1: Foundations, Data, and Strategic Planning for CQI & VBC Success
This session lays the groundwork for measurable impact using data to drive quality improvement.
Participants will explore CQI strategies in a Value-Based Care (VBC) environment, focusing on data-driven decision-making, FUH performance, SMART goal setting, and structured planning for reporting and sustainable improvement. VBC participation is not required—this group is open to all providers.
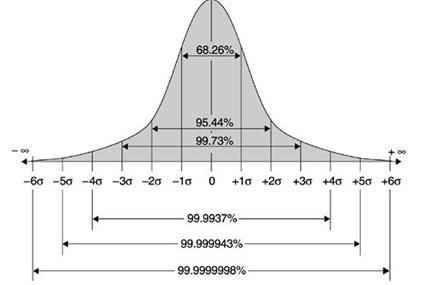
• Six Sigma is a data-driven, disciplined methodology for improving processes by identifying and eliminating defects and reducing variability.
• The name "Six Sigma" comes from statistics: achieving six standard deviations between the process mean and the nearest specification limit means very few defects — about 3.4 defects per million opportunities (DPMO).
• Originally developed at Motorola in the 1980s and popularized by GE in the 1990s.
• It combines quality management tools and statistical methods, with a strong focus on process improvement and operational excellence.

https://www.6sigma.us/
• CQI is a philosophy and management approach that emphasizes ongoing improvement of products, services, or processes.
• It relies on teamwork, data-driven decisions, and incremental changes.
• Often used in healthcare, manufacturing, education, and human services to improve outcomes and efficiency – today we will adapt to BH and IDD services in North Carolina.
• Six Sigma is one of the most structured CQI methodologies

Sustainable improvement isn’t about doing it all at once — it’s about building progress over time.
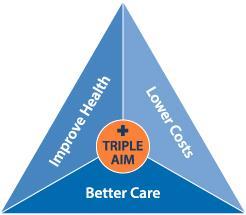
Berwick, D. M., Nolan, T. W., & Whittington, J. (2008). The Triple Aim: Care, health, and cost. Health Affairs, 27(3), 759–769. https://doi.org/10.1377/hlthaff.27.3.759
Example for Today: The HEDIS FUH-7 (Follow-Up After Hospitalization for Mental Illness within 7 Days) measure tracks the percentage of individuals discharged from a psychiatric hospitalization who receive an outpatient mental health visit within 7 days.

Triple Aim Goal How Follow-Up After Hospitalization (FUH) Supports The Triple Aim Goal
Better Experience of Care Provides reassurance, reduces isolation, and ensures continuity during a vulnerable time following psychiatric discharge.
Improved Population Health Early outpatient engagement reduces symptom relapse, improves medication adherence, and lowers suicide risk.
Supporting Data / Source
Nearly 2 out of 3 Medicaid beneficiaries do not receive follow-up within 7 days. FUH-7 national Medicaid average: 37.1%.1
Risk of suicide is highest in the first 7–10 days after discharge.2
Lower Cost of Care Reduces emergency room revisits and psychiatric rehospitalizations, which are significantly more expensive than outpatient follow-up. Timely FUH follow-up significantly reduces unplanned readmissions. 3
1. National Committee for Quality Assurance. (2023). State of Health Care Quality Report: 2022 HEDIS results. https://www.ncqa.org/report-cards/health-plans/state-ofhealth-care-quality-report/
2. Chung, D. T., Ryan, C. J., Hadzi-Pavlovic, D., Singh, S. P., Stanton, C., & Large, M. M. (2017). Suicide rates after discharge from psychiatric facilities: A systematic review and meta-analysis. JAMA Psychiatry, 74(7), 694–702. https://doi.org/10.1001/jamapsychiatry.2017.1044
3. Centers for Medicare & Medicaid Services. (2020). Reducing avoidable hospital readmissions: Technical specifications and implementation guide. Medicaid Innovation Accelerator Program. https://www.medicaid.gov/state-resource-center/innovation-accelerator-program/iap-downloads/reducing-readmissions/rr-technical-guide.pdf
Example: A behavioral health agency noticed that many individuals discharged from inpatient psychiatric care weren’t engaging with their Targeted Case Managers (TCMs) within 7 days — affecting both care continuity and performance on the FUH (Follow-Up After Hospitalization) metric.
One Time Fix Attempt:
• The agency told staff to check hospital portals daily and encouraged hospitals to fax discharge summaries directly to the TCM supervisor.
• Initial Result: Slight improvement but still missing many follow-ups.
• The team assumed they had fixed the issue by “asking hospitals to notify them.”
Example: A behavioral health agency noticed that many individuals discharged from inpatient psychiatric care weren’t engaging with their Tailored Case Managers (TCMs) within 7 days — affecting both care continuity and performance on the FUH (Follow-Up After Hospitalization) metric.
CQI Mindset: Continuous Learning + Root Cause Discovery: Core Issue: The team often didn’t know the member had been hospitalized until it was too late.

What’s one small thing your team could test to improve outreach, scheduling, or follow-up?
Who needs to be involved?
What data will tell you it’s working?
Example: A behavioral health agency noticed that many individuals discharged from inpatient psychiatric care weren’t engaging with their Targeted Case Managers (TCMs) within 7 days — affecting both care continuity and performance on the FUH (Follow-Up After Hospitalization) metric.
Hospital alerts weren’t automated or timely.
Discharge faxes were often delayed or incomplete.
Some members were hospitalized out-of-county or in unaffiliated hospitals.
Staff were wasting time manually checking multiple sources with no guarantee of accuracy.
• Define: Improve timely TCM outreach post-hospitalization
• Measure: FUH (Follow-Up After Hospitalization) rates by program and by source of hospitalization
• Analyze: How/when staff were learning about admissions
• Improve:
• We can partner with the Tailored Plan and NC Health Notify to set up realtime ADT (Admission-Discharge-Transfer) alerts
• We can create a regular huddle process to review alerts and assign same- day outreach
• Control:
• Set up a feedback loop and write out the process
• Each month, audit the hospitalizations by running a report on the alerts.
• Can be a subset (3-5 hospitalizations) to look for any process breakdowns

“You can’t follow up if you don’t know it happened.”
A true CQI mindset means asking not just why aren’t we doing it, but how do we know about it in time to act — and designing smarter systems that learn and adapt.
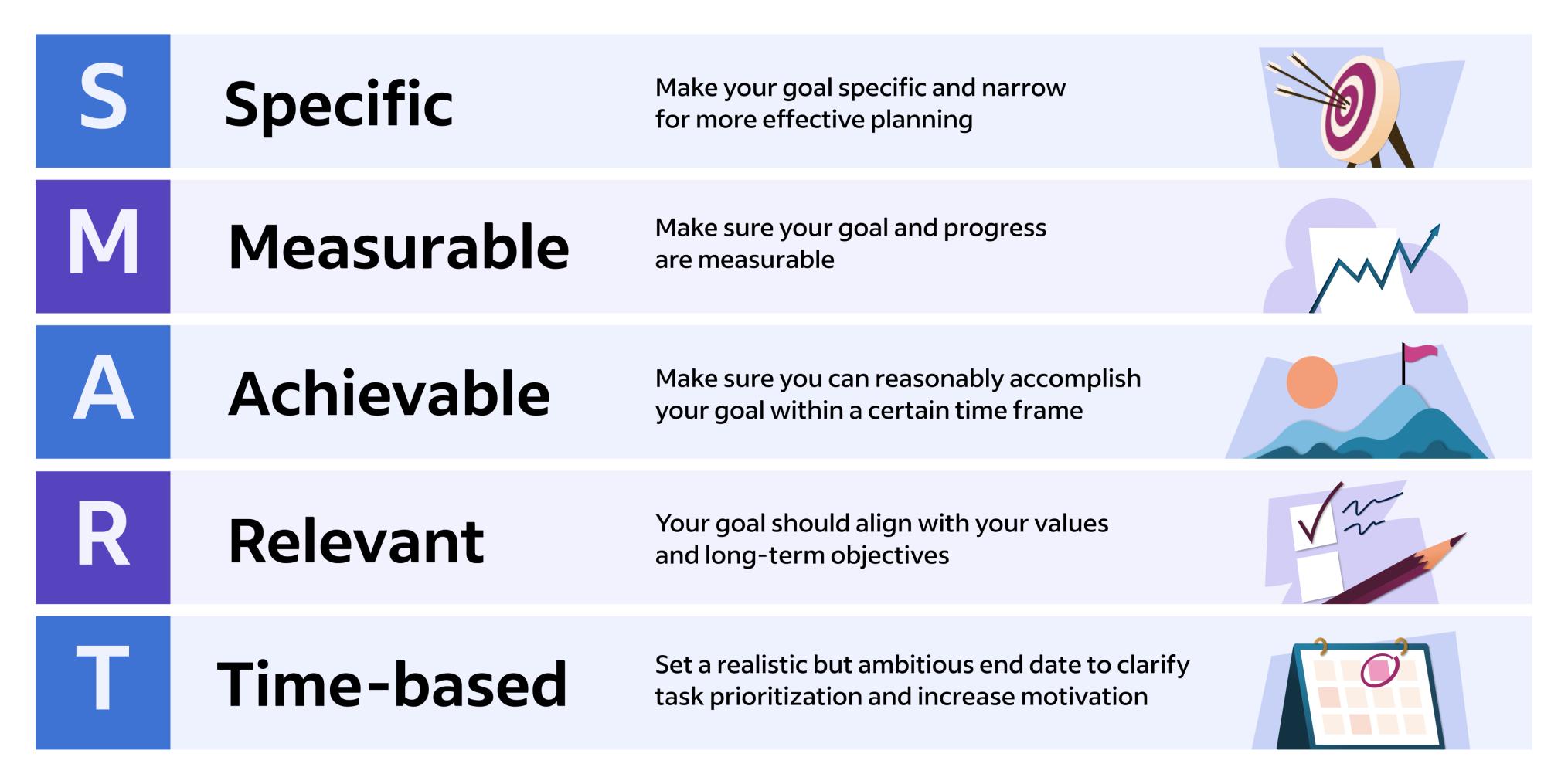
“We want to improve FUH performance as soon as possible.”
•Not Specific: Doesn’t say how or what will improve.
•Not Measurable: No number or benchmark.
•Not Achievable: No baseline or plan to track.
•Not Relevant: No reference to population, staff, or program.
•Not Time-bound: No deadline or timeframe.
“Increase the percentage of members with completed 7-day FUH follow-up from 42% to 60% by December 31, 2025, by implementing real-time hospital alert tracking and same-day outreach by TCMs.”
•Specific: Targets a defined metric (7-day FUH rate).
•Measurable: From 42% to 60%.
•Achievable: A 18-point gain is challenging but realistic.
•Relevant: Tied to CQI work, staff actions, and a performance measure.
•Time-bound: Deadline set (December 31, 2025).
Pick one issue your team has faced recently, such as missed program attendance, gaps in behavioral support plans, or delays in medication refills
What’s one small thing your team could test to improve the root cause of the issue?
Who needs to be involved?
What data will tell you it’s working?
The process doesn’t have to be perfect. The focus isn’t on how or where you track data but what informs your decisions.
CARE TEAM & STAKEHOLDER ENGAGEMENT
DATA REVIEW & COACHING UTILIZATION
SHORT-TERM WINS & BRIGHT SPOTS
VBC MEASURE MONITORING & RESPONSE
RISK STRATIFICATION & PANEL MANAGEMENT
BARRIER IDENTIFICATION & MITIGATION PLANNING
GOAL SETTING & RESOURCE ALIGNMENT
• We foster shared accountability by engaging multidisciplinary care teams and community stakeholders, including peer supports and external partners. Regular collaboration and inclusive participation are emphasized in all CQI activities. This includes monthly and as-needed live coaching, regular webinars and trainings, Element University, and asynchronous communications throughout the month.
• Coaches share reports with low risk, rising risk, and high-risk membership cohorts. Teams regularly use these Element dashboards, reports, and coaching sessions to guide improvement efforts. We reinforce this by integrating Element University content and offering responsive coaching aligned with emerging trends.
• We work with our Tailored Plans, CMAs, and AMH+s to track key Value-Based Care (VBC) metrics monthly, analyze trends, and tailor interventions to specific populations (e.g., youth, SMI). Teams are supported with actionable data and strategy tools to improve targeted outcomes.
• High-risk and risking-risk members are identified through regular panel reviews and categorized for tailored interventions. We support this process with risk tools and promote follow-up actions during coaching and dashboard reviews.
• Each team sets SMART goals and outlines support needs for the next month. Element CIN provides aligned tools, guidance, and resources to ensure teams have what they need to succeed.
Care Team & Stakeholder Engagement Define
Data Review & Coaching Utilization Measure /Analyze
Short-Term Wins & Bright Spots Improve
VBC Measure Monitoring & Response
Measure /Analyze / Control
Risk Stratification & Panel Management Analyze / Improve
Barrier Identification & Mitigation Planning Analyze / Improve
Goal Setting & Resource Alignment Define / Improve / Control
Identifies key roles, builds accountability, and ensures shared understanding of the problem and goals.
Uses data and coaching to assess current performance, identify patterns, and inform improvement opportunities.
Reinforces what’s working and spreads successful strategies as part of the solution set.
Tracks performance, identifies trends, and supports consistent monitoring to sustain improvements.
Categorizes populations to identify gaps, focus interventions, and prioritize action.
Diagnoses root causes (e.g., SDoH, system barriers) and co-creates mitigation strategies.
Sets specific targets, aligns support resources, and ensures structures are in place to maintain progress.
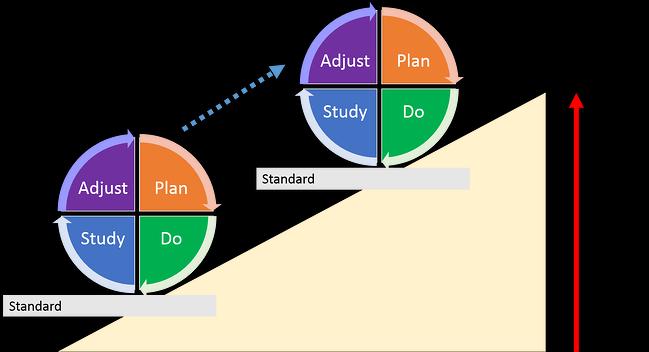
• Plan – Do – Study – Act (PDSA) is the engine of CQI.
• Plan: Identify a change to test. Set a goal and define success.
• Do: Try the change on a small scale.
• Study: Review the data. What worked? What didn’t?
• Act: Adjust and standardize — or test again with improvements.
• Repeat with each cycle — this is how small changes lead to big impact.
•Use The Standardized Templates for TCM notes and follow-up to ensure all metrics are captured.
•Flag Missed Contacts or Declined Visits with dropdowns avoidable vs. unavoidable gaps.
•Audit Your Panel monthly for overdue FUH, missed screenings, or declining adherence patterns.
Example Coaching Reporting
• Drill-Down to Member-Level

Quarterly Gap Closure Reports → Review at team huddles to prioritize outreach lists.
Top 5 Barriers to Measure Performance → Identify and problem-solve (transportation, side effects, scheduling delays, etc.).
Peer Champions → Share what’s working in one CMA with others through coaching calls.
Setting Micro-Goals → Example: “Improve TCM engagement rates by 10% this quarter through increased phone calls and texts.”
Core Themes
Strategic Goal Setting
Key Tools & Resources
Deliverables
OGSM: Strategic Planning Tool SWOT Analysis Assessment & Goal Setting Plans
CQI Project Design & Implementation Gap Analysis & Root Cause Analysis Templates
PDSA Worksheets
CQI monthly reporting tool Continuous Quality Improvement (CQI) Plan
Data-Informed Decision-Making
Change Management & Staff Engagement
HEDIS, Quality, Population Health reporting
Element University training, education, resources and surveys
Sustainability & Organizational Growth Long-term goal planning worksheets
CQI Sustainability Plan
Monthly Coaching &Strategy report
CIN Member Engagement & Leadership Opportunities
CQI Summary Report Sustainability Plan
Enhanced Strategic Plan
VBC Reporting Form

Start with shared ownership by engaging care teams, peers, and external partners.
Use your data with intention by reviewing dashboards, identifying trends, and exploring root causes.
Set SMART goals that are specific, measurable, achievable, relevant, and time-bound.
Think in cycles, not fixes — apply the PDSA model to test, learn, and adapt.
Build CQI into your routine so it becomes part of how your organization improves every day.
1. Schedule your Monthly Coaching Session
2. Complete VBC Monthly form (further instructions will be provided via email)
3. Participate in Network Events
4. Bookmark our email for notifications: info@elementhealthconsortium.com