What the astronaut experience tells us about the brain
• SPRING
EMERGING IDEAS IN BRAIN SCIENCE
2021 SPACE IBetween the ea - rs

Mark Shelhamer, Sc.D.
Space Between the Ears
Page 12

Peter Campochiaro, M.D.
Eye of the Needle
Page 20

Kayt Sukel
Losing Face
Page 26

Carl Sherman
The Brain and Covid
Page 30
Mark Shelhamer, Sc.D., is professor in the Department of Otolaryngology— Head & Neck Surgery at the Johns Hopkins School of Medicine, where he started as a postdoctoral fellow in 1990. He has bachelor’s and master’s degrees in electrical engineering from Drexel University, and a doctoral degree in biomedical engineering from MIT. At MIT, he worked on sensorimotor physiology and modeling, including the study of astronaut adaptation to spaceflight. He then moved to Johns Hopkins where he continued the study of sensorimotor adaptation with an emphasis on the vestibular and oculomotor systems and nonlinear dynamics. From 2013 to 2016, he served as chief scientist for the NASA Human Research Program. His research since that time has emphasized multi-system and crossdisciplinary interactions that contribute to personal and mission resilience in spaceflight.
Peter Campochiaro, M.D., is the Eccles Professor of Ophthalmology and Neuroscience at the Wilmer Eye Institute, Johns Hopkins University School of Medicine. He is a clinician-scientist whose laboratory research studies ocular neovascularization and excessive vascular leakage, which occurs in age-related macular degeneration, diabetic retinopathy, and retinal vein occlusion. The clinical trial group under Campochiaro provided the first demonstration of the benefits of suppression of VEGF in diabetic macular edema and retinal vein occlusion. He has developed strategies for sustained suppression of VEGF that are currently being tested in clinical trials. Campochiaro trained at the University of Notre Dame, Johns Hopkins School of Medicine, and the University of Virginia.
Kayt Sukel‘s work has appeared in the Atlantic Monthly, the New Scientist, USA Today, the Washington Post, Parenting, National Geographic Traveler, and the AARP Bulletin. She is a partner at the award-winning family travel website Travel Savvy Mom, and is also a frequent contributor to the Dana Foundation’s science publications. She has written about out-of-body experiences, fMRI orgasms, computer models of schizophrenia, the stigma of single motherhood, and why one should travel to exotic lands with young children. She is the author of Dirty Minds: How Our Brains Influence Love, Sex and Relationships and The Art of Risk: The New Science of Courage, Caution & Chance
Carl Sherman has written about neuroscience for the Dana Foundation for ten years. His articles on science, medicine, health, and mental health have appeared in national magazines including Psychology Today, Self, Playboy, and Us. He has been a columnist for GQ and Clinical Psychiatry News, and is the author of four books. He holds a doctorate in English literature and has taught at various universities. When not writing about the mind, the brain, and the interesting things people do with them, he enjoys travel, listening to music, looking at art, and copyediting. He lives and works in New York City.
2 DANA FOUNDATION CEREBRUM | Spring 2021 CONTRIBUTORS
COVER ILLUSTRATION: ZOË VAN DIJK
12 Space Between the Ears
Our author, former chief scientist for the NASA Human Research Program, examines what spaceflight can teach us about cognitive performance and mental abilities.
By Mark Shelhamer, Sc.D.
20 Eye of the Needle
A clinician and professor of ophthalmology and neuroscience advises a retired attorney about strategies to treat macular degeneration, a condition that affects 200 million people worldwide.
By Peter Campochiaro, M.D.
26 Losing Face
Newborns and toddlers, as well as K-12 students, have spent the past year living in a world where mask-wearing is the new normal. Is it affecting their brain development and mental health?
By Kayt Sukel
30 The Brain and Covid: Strides and Speculations
A little more than a year into the pandemic, scientists around the globe continue to learn how Covid-19 affects the brain and mental health—and how patients can overcome nagging symptoms.
By Carl Sherman
36 Between Thought and Expression
A sampling of work by Greg Dunn, who was on his way to a Ph.D. in neuroscience when he realized that bringing the brain's beauty to life was a more suitable role for him than lab work.
By Bill Glovin

POINTS OF INTEREST NOTABLE FACTS IN
4 A common observation among astronauts refers to a phenomenon known as “space fog” or “space stupids”—a sense of cognitive slowing and the need for increased mental effort to perform routine tasks.
Space Between the Ears, Page 12
4 With people living longer and longer, it is estimated that by 2040, there will be 300 million individuals with macular degeneration throughout the world.
Eye of the Needle, Page 20
4 There are a lot of things that are really important for human communication. And human faces are definitely one of the most important of them.
Losing Face, Page 26
4 The National Institutes of Health is allocating more than $1 billion to research investigating Long Covid in all its multiorgan complexity—causes, manifestations, natural history, and treatments.
The Brain and Covid, Page 30
4 Microetching, which consists of creating animated images by precisely controlling light’s reflection off of surfaces, was invented by Dunn and collaborator Brian Edwards, Ph.D. Between Thought and Expression, Page 36
2
Dana.org 3 SPRING 2021 | VOLUME 2, ISSUE 2
FEATURES
Briefly Noted • By the Numbers, Brain in the News, In Memoriam
Advances • Notable brain science findings
Bookshelf • A few brain science books that have recently caught our eye
Awards •
SECTIONS 5
6
7
8
Brain Prize Winners
Philip M.
9 Clinical Corner • Following Your Instincts, By Angela M. Reiersen, M.D. 10 Neuroethics • Big Data, Big Concerns, By
Boffey
Contributors | 4 From the Editor | 44 Advisory Board | 46 Cerebrum Staff
THIS ISSUE
The Johns Hopkins Connection
 BY BILL GLOVIN Editor-in-Chief
BY BILL GLOVIN Editor-in-Chief
It’s no coincidence that two features in this issue are written by Johns Hopkins School of Medicine neuroscientists. The institution, which has been crucial to the evolution of neuroscience, has helped save countless lives, been crucial to educating many of the nation’s top scientists, and provided Cerebrum with many of it authors and advisers over the years.
As a lifelong New Jersey native, I never expected such a personal connection. My first encounter occurred in 1999, when I traveled by train to Baltimore to write a Hopkins Medicine cover story about my cousin Michael’s experience in a pioneering outpatient transplant program to treat leukemia.
So, I already had a connection with the institution when I became editor of Cerebrum in 2012 and inherited an advisory board that included Don Price and Kay Jamison—Hopkins’ professors and giants in their fields. My advisers, today, include three who passed through the Hopkins pipeline: Harvard professor Joe Coyle, who joined the Hopkins faculty in 1975 and was a former Distinguished Service Professor of Child Psychiatry; Helen Mayberg, a renowned neurologist at the Icahn School of Medicine at Mount Sinai, once a Hopkins post-doctoral fellow; and Dana’s senior consultant Carolyn Asbury, who also trained there. I also worked closely with another giant, Dana scientific adviser Guy McKhann (now retired), founding director of Hopkins’ Zanvyl Krieger Mind/Brain Institute.
Over the years, we’ve published articles by a number of Hopkins professors: the late John Freeman on epilepsy, Ellen Silbergeld on drinking water and the brain, Michael Kim and Christopher Jackson on glioblastoma, Susan Magsamen on neuroaesthetics, and Frank Lin on the link between dementia and hearing loss. Writing for us in this spring issue are two more Hopkins professors, Mark Shelhamer on spaceflight’s connection to cognition and mental health (page 12), and Peter Campochiaro on macular degeneration (page 18).
Many of our other Cerebrum authors were trained at Hopkins, including Fred “Rusty” Gage (stem cells), John Ioannidis (research study validity), Michael Miller (heart and the brain), and Paul Worley (memory). And with this issue, we welcome new Dana Foundation President Caroline Montojo, former director of Life Sciences and Brain Initiatives at the Kavli Foundation. Guess where Caroline completed her M.A. and Ph.D. programs?
Hopkins loomed again for me in a big way in 2018, when—20 years after his transplant—my cousin Michael developed an even more lethal form of leukemia and was admitted into the program for a second time. I returned to the hospital to shadow Michael again for Hopkins Medicine—and wrote about how the technology and experience had drastically improved for patients. This second transplant bought Michael another two-and-a-half years of life, but all of the improvements in the world couldn’t save him a third time. Michael S. Billig, 64, a professor of cultural anthropology at Franklin & Marshall in Lancaster, PA, passed away in January at the hospital.
But thank you Johns Hopkins, for extending Michael’s life and doing what you could to help him, for making the world a better place, and for making Cerebrum a better magazine. We couldn’t have done it without you. l
EMERGING IDEAS IN BRAIN SCIENCE
Bill Glovin Editor-in-Chief
Seimi Rurup Assitant Editor
Brandon Barrera Editorial Assistant
Carl Sherman Copy Editor
Carolyn Asbury, Ph.D. Scientific Consultant
Bruce Hanson Art Director
Cerebrum is published by the Charles A. Dana Foundation, Incorporated. DANA is a federally registered trademark owned by the Foundation. © 2020 by The Charles A. Dana Foundation, Incorporated. All rights reserved. No part of this publication may be reproduced, stored in a retrieval system, or transmitted in any form by any means, electronic, mechanical, photocopying, recording, or otherwise, without the prior written permission of the publisher, except in the case of brief quotations embodied in articles.
Letters to the Editor
Cerebrum Magazine 505 Fifth Avenue, 6th Floor New York, NY 10017 or cerebrum@dana.org
Letters may be edited for length and clarity. We regret that we cannot answer each one.
4 DANA FOUNDATION CEREBRUM | Spring 2021 FROM THE EDITOR
BY THE NUMBERS
$0
How much it costs to become a Brain Awareness Week partner.
30 countries have joined together to participate in a study to trace a possible path from Covid-19 to neurodegenerative diseases, particularly dementia.
hallmarks of environmental exposures detailed in a study that chart the biological pathways through which pollutants contribute to disease.

1664 the year English physician Thomas Willis published his Anatomy of the Brain, which ushered in the era of modern neuroanatomy.
75 is the percentage of people predicted to get Alzheimer’s disease in an artificial intelligence program that measured writing test results.
2 0 5 3 9 0 4
The number of studies and articles listed (as of March) when the word “brain” is searched on PubMed.gov, the website of the National Institutes of Health national library.
20,000 neuroscientists are represented by the Federation of European Neuroscience Societies (FENS) across 33 countries. Their mission is to advance neuroscience education and research.
“Unlike your genome, which you can’t do much about except blame your parents and grandparents, your microbiome is potentially modifiable. And that gives great agency to patients. That’s really exciting.”
—

John Cryan, Ph.D., a neuroscientist at University College Cork in Ireland
BRAIN IN THE NEWS
Links to brain-related articles we recommend
> New York Times: What Can Covid-19 Teach Us About the Mysteries of Smell?

> New York Times: Alzheimer’s Prediction May Be Found in Writing Tests
> Nature: How gut microbes can drive brain disorders
> Science Daily: How a single gene alteration may have separated modern humans from predecessors
> Star-Ledger: How telehealth strengthened its grip on future of our medical care
> New York Times: Can Zapping Our Brains Really Cure Depression?
> Washington Post: A brain researcher on what Freud got right
> NBC News: Exclusive look at NIH investigation into Covid ‘long haulers’
IN MEMORIAM

Philip Seeman, M.D., Ph.D., a molecular neuropharmacologist who discovered the importance of the dopamine D2 receptor in 1974, showing that the schizophrenia drugs of that era— which were widely used but poorly understood—targeted this brain receptor — A Dana Alliance for Brain Initiatives member while at the University of Toronto, Seeman’s was made an Officer of the Order of Canada for his research on dopamine receptors and their involvement in diseases such as schizophrenia, Parkinson's, and Huntington’s disease. The company he founded, Clera Inc., developed small-molecule therapies for schizophrenia and other dopamine-related brain diseases. Paul Garfinkel, staff psychiatrist with the Center for Addiction and Mental Health in Canada, said that before Seeman’s research, “our theories about what causes schizophrenia were primitive and blaming. They blamed the mother or the family dynamic. His studies showed there’s a biology to this brain illness that’s nobody’s fault.” l
Dana.org 5 BRIEFLY NOTED ILLUSTRATION: ISTOCK
8
ADVANCES
Notable brain-science findings
 BY NICKY PENTTILA
BY NICKY PENTTILA
The idea that doctors might restore motor function in people with SPINAL CORD INJURIES by using stem cells derived from the patient’s own bone marrow got a big boost in April 2021. In a case-study description of a Phase 2 study, 13 people with relatively recent spine injuries caused by falls or other minor trauma had marrow drawn, converted in the lab to stem cells, and then re-inserted intravenously. The trial aimed to confirm that the method was safe for humans, which it appears to be. But in addition, more than half the patients showed significant improvement in key functions such as bowel function, coordination, and ability to walk. l
We know that keeping physically active in later life is important for preserving cognitive function, and now we’re learning how it may help adolescents build their cognitive capacities.
ADOLESCENCE is one of the brain’s sensitive periods, when busy connections strengthen as others are pruned. It can also be a time when children grow more sedentary, spending longer hours at school desks and in front of computers. In a study of 50 12-year-olds over the course of one week, using wrist activity-trackers, interviews, health exams, and magnetic resonance imaging, researchers found that those who were physically healthier and more active had signs of healthier brains: more gray matter, stronger white-matter connections, better blood flow, and more. l
Scientists in four labs (in France, Germany, the Netherlands, and the US) are finding evidence against the common wisdom that it’s pointless to try to communicate with sleeping people. After being trained to signal when they were in a lucid part of dream sleep (by making a series of left-right
In adults, twitches occur for about an hour during rapid eye movement (REM) sleep, while in infants, twitches dominate the sleep cycle, helping shape young brain development. Mark Blumberg, a professor of psychological and brain sciences at the University of Iowa, found that twitches in baby rat pups trigger activity in the spinal cord, sensory and motor areas, and the hippocampus. He talked about his research findings in a presentation at the Society for Neuroscience’s Global Connectome conference in January.
eye movements), some volunteer dreamers were able to follow researcher instructions to solve simple math problems, answer yes-or-no questions, or signal the difference between different sensory stimuli (such as flashing lights vs. spoken sounds). After waking, some remembered what the questions or stimuli were, but in the contexts of the stories they were dreaming, such as hearing the researcher’s voice among others during a surreal party. “INTERACTIVE DREAMING,” if it proves out, could help researchers better study dreams and dreaming without having to rely on morning reporting, by which time most of us have forgotten our dreams. l
People going under anesthesia during surgery who listen to soothing talk and music via headphones may wake up feeling less PAIN and asking for less pain medicine. In a blinded randomized controlled study of 385 patients, researchers found that those who had listened to music and positive suggestions such as “everything is going well” reported an average of pain scores 25 percent lower, two hours after their operation, compared with those whose earphones gave them only silence—and 70 percent of the audio-plus group asked for no opiates at all, compared with 39 percent of the silence group. l
Female mosquitoes love blood—they suck so strongly they can damage an animal’s capillaries. But blood is complex, a combination of components all with their own taste signatures. It’s not a single TASTE like the simple sugars in nectar; how can the mosquitoes be sure this complicated combination is the thing they crave? Researchers have found a group of neurons in the female mosquito’s syringe-like stylet that activate only when a combination of sugar, salts, and other blood components are present. “We knew that the female stylet was unique, but nobody had ever asked what its neurons like to taste,” says Veronica Jové, who led the study. “These neurons break the rules of traditional [single] taste coding, thought to be conserved from flies to humans.” l

6 DANA FOUNDATION CEREBRUM | Spring 2021
PHOTO: WILL LANDIN
BOOKSHELF
A few brain-science books that have recently caught our eye
 BY BRANDON BARRERA
BY BRANDON BARRERA

So You Want to Be a Neuroscientist? by Ashley
Juavinett (Columbia University Press)
Does the thought of dedicating your academic and professional career to studying the brain ever cross your mind? Maybe you’re already in the workforce, searching for ways to transition into neuroscience but uncertain of how that road unfurls. An insightful and practical guide, So You Want to be a Neuroscientist? is the north star for the aspiring brain scientist in you. Having launched her own career recently, Ashley Juavinett, Ph.D., assistant teaching professor of neurobiology at the University of California, San Diego, writes candidly about what neuroscientists-in-training should expect when venturing forth on their own paths. The book covers the current state of neuroscience and where it might be headed, what graduate school entails and the importance of networking and finding mentors, what to expect from conducting research in a lab, and the many career possibilities open after training. Juavinett leaves no stone unturned, making her book invaluable for students, educators, and everyone in between.

Models of the Mind: How Physics, Engineering and Mathematics Have Shaped Our Understanding of the Brain by
Grace Lindsay (Bloomsbury Sigma)
Using the precision and elegance of mathematics to understand the brain is part of the work computational neuroscientist and author Grace Lindsay, Ph.D., performs regularly. Scientists in her burgeoning field— those unifying mathematics and biology—reduce complex biological processes into painstakingly accurate equations and variables when creating useful, predictive mathematical models. In Models of the Mind, Lindsay charts how physics, engineering, statistics, and computer science have influenced brain science and provide the groundwork for the discipline’s future. The chapters cover the history of the different mathematical tools applied in understanding neuronal mechanisms, memory formation and maintenance, the motor and visual cortexes, decision-making, and more. Mercifully, lay readers can jump in and comfortably enjoy the subject matter as Lindsay shies away from requiring special mathematical knowledge on behalf of readers; she instead features the ideas behind the equations, the reasons why scientists employ
mathematical modeling, and the insights these models reveal about the brain. According to Lindsay, the brain will ultimately be understood through mathematical and computational theories, imperfect though they may be. Models of the Mind is a captivating and compelling anthology of why she may be right.

Smellosophy: What the Nose Tells the Mind
by A.S. Barwich (Harvard University Press)
A nascent investigative arena, the scientific study of smell experienced a breakthrough in 1991 with the discovery of olfactory receptors, rapidly propelling the branch of research into the realm of mainstream neuroscience. Celebrating this influx of new, sophisticated, “smelly” research, cognitive scientist and empirical historian A.S. Barwich, Ph.D., ventures into the laboratorial trenches and reports from the “experimental frontier,” offering a historical and philosophical analysis of odor perception. Despite the remarkable progress made in recent decades, Barwich says, the puzzle of olfaction—understanding what perceptual information odors represent and how the brain comes to understand it—remains unsolved. Deftly using interviews with experts in psychology, chemistry, neuroscience, and perfumery, Barwich probes the biological underpinnings of odor, identifying the uncertainties and knowledge gaps in current thinking about odor perception—and perception overall. Perfumed with an inviting bouquet of philosophy, history, and neuroscience, Smellosophy is Barwich’s charmingly compelling love letter to olfaction.

Stories and the Brain: The Neuroscience of Narrative by Paul B. Armstrong (Johns Hopkins University Press)
In Stories and the Brain: The Neuroscience of Narrative, professor of English and author Paul B. Armstrong, Ph.D., explains how the brain interacts with the social world and why stories are so important. Expanding on the questions of how our brains are suited to the telling and following of stories, Armstrong investigates the neurobiological underpinnings of narrative, shedding light on what our storytelling abilities reveal about language and the mind. Across four chapters, the book explores the roles between stories and experience, discussing neuroscience and narrative theory, the correlations between neuronal and cortical timing processes to paradoxes of narrative temporality, story plots and their use of patterns of action, and bringing different worlds into relation with each other through the exchange of stories. Stories and the Brain is a well-researched, engaging discussion on what narrative theory and neuroscience stand to gain from continued collaboration. l
Dana.org 7
DABI Members Win Brain Prize: Migraine Research Recognized
This year, two of the four winners of the Brain Prize—the world’s most prestigious award for brain research—are
Dana Alliance for Brain Initiatives (DABI) members: Michael A. Moskowitz and Jes Olesen. The award, sponsored by the Lundbeck Foundation in Sweden, were all awarded for research on migraine, and provides close to $400,000 in US dollars to each winner. The other two winners are Lars Edvinsson, M.D., Ph.D., professor of internal medicine at Lund University in Sweden, and Peter Goadsby, M.D., Ph.D., director of the NIHR-Wellcome Trust King’s clinical research facility at King’s College in London.
Moskowitz, M.D., a professor of neurology at Harvard Medical School, showed “that a migraine attack is triggered when trigeminal nerve fibers release neuropeptides that lead to dilated (opened up) blood vessels of the meninges, inflammation, and pain …. He was the first to propose that




blocking the action of released neuropeptides could be a new approach to treating migraine.”
Olesen, M.D., a professor of neurology at the University of Copenhagen, gave migraine patients a gene-related peptide called calcitonin (CGRP), which triggered migraine attacks. He then found that certain drugs—known as antagonists—blocked the peptide and effectively treated migraine.
Working collaboratively, Edvinsson and Goadsby showed that CGRP—a particularly potent dilator of blood vessels in the meninges—may be of crucial importance in migraine and the key molecule in primary headache disorders.
This Issue’s Cerebrum Podcast Episodes

Mark Shelhamer, Sc.D., former chief scientist for the NASA Human Research Program and a professor at the Johns Hopkins School of Medicine, is the author of our cover story, “Space Between the Ears.”
"There's something that astronauts sometimes call space fog or the space stupids… the sense that things that I used to be able to do on earth seamlessly without thinking about them, now, all of a sudden, they're a little bit more challenging for me to do.”




Peter Campochiaro, M.D., the Eccles Professor of Ophthalmology and Neuroscience at the Wilmer Eye Institute, Johns Hopkins University School of Medicine, and the author of our feature on macular degeneration, “Eye of the Needle.”
“In general, most patients with the wet form of macular degeneration require injections of these medications every four to six or eight weeks for the remainder of their life.”


8 DANA FOUNDATION CEREBRUM | Spring 2021
AWARDS
Left to right: Michael A. Moskowitz, Jes Olesen, Lars Edvinsson, and Peter Goadsby
FOLLOW ON YOUR FAVORITE PLATFORM
I became ill myself with probable Covid-19... with various fluctuating symptoms—nothing like any viral infection I’d experienced before.
Following Your Instincts
 BY ANGELA M. REIERSEN, M.D.
BY ANGELA M. REIERSEN, M.D.
Several years ago, a colleague supervising an annual multidisciplinary research clinic studying Wolfram syndrome in children, adolescents, and young adults asked me to use my experience as a child and adolescent psychiatrist to perform neurological and psychiatric assessments of the study participants. Most participants had experienced diabetes from a young age, progressive vision loss due to optic atrophy, and hearing loss. Adolescents and young adults often showed progressive gait and difficulties with balance.
These many problems were tied to a defect in a gene that codes for a protein present in the endoplasmic reticulum (ER), a factory and storage area inside our cells, bounded by a network of folded membranes. This protein is called wolframin. When cells are under stress, particularly if they are unable to properly fold proteins, an ER stress response kicks in to get cellular processes back into balance. If this fails, or if the ER stress response does not shut down properly after cellular processes are back in balance, a self-destruct system can kick in, leading to death of the cells. The wolframin protein helps regulate this process, so cells won’t die unnecessarily; but in Wolfram syndrome, the ER stress response is exaggerated.
Many participants and their families had come to know each other from previous visits to our research clinic; some had even kept in touch and formed their own supportive community. As I met with them, I was often impressed by their resilience. Many reported initial difficulty adjusting to their diagnosis, but they learned ways to cope with an uncertain medical future. Some reported history of treatment with a selective serotonin reuptake inhibitor (SSRI) for symptoms of anxiety, obsessive-compulsive disorder, or depression.
Over the years, I noticed a possible pattern in their responses to these SSRIs, and I became curious. A search of the literature revealed that SSRIs differ in their action on another ER protein called the sigma-1 receptor (S1R), which— like wolframin—is a regulator of the ER stress response. S1R activators (including SSRIs like fluvoxamine and fluoxetine) can down-regulate the ER stress response, while another SSRI (sertraline) may have opposite actions on the S1R. I wondered whether the differing effects on S1R might explain differences in treatment response, particularly in people with genetic disorders of the ER stress response, such as Wolfram syndrome.
I began monitoring the literature on S1R and, in early 2019, I found an article (from research in the laboratory of Alban Gaultier, Ph.D., at the University of Virginia) that indicated that mice lacking the S1R showed excessive production of cytokines (inflammatory molecules), which increased susceptibility to death when exposed to inflammatory triggers or infections. And mice with functioning S1R showed improved survival under these conditions if given fluvoxamine.
This work showed that, in addition to down-regulating the ER stress response, the activated S1R could down-regulate cytokine production during severe infections that cause sepsis. I wondered how this new knowledge might be applied to treat human diseases in the future. Then, in March 2020, the Covid-19 pandemic had begun. I became ill myself with probable Covid-19. It was a strange and long-lasting illness with various fluctuating symptoms—nothing like any viral infection I’d experienced before.
While still ill, I read that deterioration in respiratory function around the second week of illness seemed to be due to an excessive inflammatory response to the virus rather than the virus itself. The body’s own response to the virus was doing the damage. I immediately thought back to that study of fluvoxamine from the University of Virginia, and I wondered whether fluvoxamine might be effective in treating Covid-19.
I sent off some quick emails to colleagues to see what they thought. That led me to Eric Lenze, M.D., a geriatric psychiatrist with extensive experience running randomized controlled trials (RCTs). I sent Lenze an email on March 25, 2020, explaining my hypothesis. He was convinced we should do an RCT, so we got the trial going as quickly as possible.
Since patients were isolating at home, our study staff took medications and study supplies to them using no-contact delivery methods. Patients logged oxygen levels, vital signs, and symptoms electronically, and we checked in with them as needed. None of the 80 patients taking fluvoxamine experienced respiratory deterioration by our study definition, but 8.3 percent of the 72 taking placebo deteriorated. It seemed that this treatment actually worked.
If these findings are confirmed in our ongoing larger study, fluvoxamine could have huge potential to reduce hospitalizations and deaths related to Covid-19. Thinking back on all this, it has been a strange journey. As a child psychiatrist, I never expected that I’d team up with a geriatric psychiatrist to run infectious disease treatment trials. And although the connection with Wolfram syndrome is indirect, if I had not become interested in the S1R as a result of Wolfram syndrome research, I might never have thought to use fluvoxamine as a treatment for Covid-19. l
Angela M. Reiersen is an associate professor of psychiatry at Washington University School of Medicine.
Dana.org 9 CLINICAL CORNER
Big Data, Big Concerns
 BY PHILIP M. BOFFEY
BY PHILIP M. BOFFEY
An article in the Winter issue of Cerebrum magazine and a podcast episode with the author laid out a tantalizing vision of the enormous potential of advances in neuroimaging and so-called Big Data technologies to revolutionize the treatment of neurological disease. But the author made only a fleeting mention of the ethical issues raised by these advances.
Fortunately, the same author—Vince Calhoun, director of the Center for Translational Research in Neuroimaging and Data Science—co-authored a recent article with two experts from the Netherlands that did explore in-depth the major ethical issues raised by these endeavors. It is a welcome effort to flag potential ethical problems while the field is still in an early stage of development.
Calhoun’s Center is well-situated to conduct this work. It is backed by three universities in Atlanta, GA, with complementary strengths and missions. They include Emory University, which has expertise in brain disorders, Georgia Tech, which is strong in data mining, and Georgia State, which is proficient in neuroscience and psychology.
Calhoun’s Cerebrum article lays out the promise, achievements, and disappointments of the field so far. On the plus side, the knowledge gained from big data and neuroimaging have provided new insights into the working of the brain. But hopes that the discovery of functional magnetic resonance imaging would lead to a clinical breakthrough in assessing and treating mental illness have not yet materialized. Indeed, Calhoun can’t point to any specific examples where neuroimaging is beginning to help the mentally ill. Progress has been slower than he would have liked.
His hope is that within ten years we may have learned enough to update our psychiatric diagnostic criteria and refine the medications we prescribe to treat some mental health disorders.
The research has been slow to reach the scale required. Calhoun traced the evolution of the field through eras in which researchers studied small numbers of subjects, typically 5 to 20, then larger groups comprised of hundreds of individuals, then the interactions between networks in the brain both at rest and while performing tasks. Each era added to the knowledge base, but they have not yet led to clinical tools to treat mental health disorders or determine drug delivery strategies.
We are now firmly in, what he calls, “the era of big data for
neuroimaging and psychiatry.” Several studies already scan tens of thousands of individuals over time, and powerful “deep learning models” require lots of data and computer power. Previous studies have focused on group results and averages. The current goal is to make predictions for individuals of how their symptoms will progress and how they will respond to medications. Calhoun finds “considerable reason to be optimistic about the not-so-distant future.”
The article co-authored by Calhoun that explored the ethical issues was published in the journal Human Brain Mapping last July. It analyzed differing approaches in the European Union and the United States toward the use and dissemination of personal health data.
Probably, the most important distinction concerns who should be considered to “own” the data and thus have the major say in how it is handled and disseminated. Researchers and universities often believe that the data “belong” to them, and funding agencies in this country consider institutions the owners of the data. In some cases, the funding agencies dictate that the data be shared.
By contrast, recent laws in Europe give more rights to the individuals who participate in studies to determine the extent in which they want their data shared. That puts a greater burden on researchers to protect participants’ privacy and obtain their permission before disseminating personal health data.
Depending on the circumstances, research journals may also demand that data on which an article is based be uploaded at the time of publication, making them the effective owner of that data.
The chief risk in sharing data is that, if it escapes from the research realm or falls into the wrong hands, it can harm the individual whose data has been shared. For example, some studies collect information about substance use and abuse, diseases such as HIV/AIDS, or procedures such as gender reassignment surgery that can stigmatize an individual in some circles.
There are ways to protect the privacy of an individual’s health data without unduly hampering research. The trick is to strike an appropriate balance between risk and benefit.
One approach is to “de-identify” data that directly defines an individual, such as name, address and date of birth, as well as information on an individual’s physical and mental health or treatments. All such information is stripped from the dataset and replaced by artificial identifiers that can’t be linked to individuals by third parties, such as insurers, but can be traced back by the host researchers, if need be.
More robust protection is provided by “fully anonymized” data, which has all personalized data removed and any path back to the original data deleted, making it extremely hard to trace the data back to an individual. However, even this is not
NEUROETHICS
10 DANA FOUNDATION CEREBRUM | Spring 2021
The chief risk in sharing data is that, if it escapes from the research realm or falls into the wrong hands, it can harm the individual whose data has been shared.
foolproof. For example, in many cases, a large dataset may include people with rare medical conditions or only small numbers of specific ethnic minorities that machine-learning algorithms could use to identify, within certain error margins, a particular individual.
The most frightening possibility to me is that some people may actually want to link the data to an individual. It is not farfetched to worry that insurers, employers, or law enforcement agencies might want your personal data. Indeed, brain scans have already been used in court as evidence. As recently as February, the journal BioTechniques published an article online entitled “Inside the brain of a killer: the ethics of neuroimaging in a criminal conviction.”
A study published in Proceedings of the National Academy of Sciences in March 2017 found that, in a laboratory setting, brain scans were able to distinguish between hard-core criminal intent and simply reckless behavior. But a writer in Science cautioned that the approach was “far from being ready for the courtroom.”
Calhoun and his co-authors side more with the rights of individuals than with the researchers and institutions that collect data from them, but they seek a balance that will both protect their privacy and allow important science to advance. They call for the research community to work together with attorneys and ethicists to determine how best to make
important advances in medical research, while protecting the data of human subjects.
There is no question that data sharing will entail some level of risk. A leak of sensitive information might prove harmful to an individual. But the authors worry that concerns have outpaced reality. “While we do not intend to minimize the importance of data security,” they write, “there is a certain fear that has emerged regarding data sharing where it has become greater than life.” Instead of being real monsters to worry about, they are more like imaginary “monsters under the bed.”
The best path forward, the authors say, is for researchers, through discussions with participants and information provided on consent forms, to let participants decide whether they are willing to have their data shared, and under what circumstances. There may be no direct benefit to them, but those willing to share would be doing science and their fellow citizens a seminal service. l
Phil Boffey is former deputy editor of the New York Times Editorial Board and editorial page writer, primarily focusing on the impacts of science and health on society. He was also editor of Science Times and a member of two teams that won Pulitzer Prizes.
The views and opinions expressed are those of the author and do not imply endorsement by the Dana Foundation.
Dana.org 11
ILLUSTRATION: DANIEL HERTZBERG
S IBetween

12 DANA FOUNDATION CEREBRUM | Spring 2021
By
What can spaceflight teach us about the brain?
Our author, Mark Shelhamer, former chief scientist for the NASA Human Research Program and a professor at the Johns Hopkins School of Medicine, lays out how spaceflight relates to brain function, cognitive performance, and mental abilities.
SPACE the ea - rs
By Mark Shelhamer, Sc.D.
Illustration by Zoë Van Dijk

Dana.org 13
•
FEW SHORT MONTHS AGO, news programs around the globe showed NASA engineers and scientists celebrating as a robot named Perseverance successfully landed on the surface of Mars. The mission: capture and share images and audio that have never been seen or heard before. As impressed as most observers were of this major milestone, many couldn’t help but wonder when we might be ready to someday send humans. While it seems the stuff of science fiction and almost inconceivable, the answer— according to recent NASA planning—is before the end of the 2030s, less than two decades away.
There are still many obstacles to accomplishing such a feat, many of which have to do with overcoming cognitive and mental health challenges that would impact a crew: long-term isolation, eyesight impairment, and psychological effects from the stress of danger and what could amount to life-or-death decisions. For a mission to succeed, high mental and cognitive function would be absolutely critical; astronauts would be called on to perform demanding tasks in a demanding
Name something stressful in your day-to-day routine, and it is likely also present in spaceflight—along with stressors that are unique to the context. Failure is Not an Option, the title of NASA Flight Director Gene Kranz’s memoir in 2000, convincingly sums up the situation. High workload is a common feature of spaceflight. Space programs (national or commercial) do not incur the expense of sending people into space for them to rest and relax. On the contrary, astronauts’ daily schedules (at least in the US program) are planned in great detail, and their progress in keeping on schedule is tracked in real time. And there is much to be done during a mission, from normal spacecraft operations, maintenance, and repairs, to a wide range of science experiments and assessments of new space technology. Much of the science, in fact, is dedicated to understanding the human response and adaptation to spaceflight.
FINDING THE ANSWERS TO OVERCOMING THOSE OBSTACLES HAS NOT ONLY OFFERED US THE OPPORTUNITY TO ADVANCE SPACEFLIGHT, IT ALSO ALLOWS US TO APPLY WHAT WE LEARN TO HELP PEOPLE HERE ON EARTH .
environment. Losing 20 IQ points halfway to Mars is not an option.
Finding the answers to overcoming those obstacles has not only offered us the opportunity to advance spaceflight, it also allows us to apply what we learn to help people here on Earth. While we haven’t yet seen anything as a dramatic as a clear loss of intellectual capacity in space, there are enough indicators to suggest that we should pay close attention.
Stress—an emotional or mental state resulting from tense or overwhelming circumstances—and the body’s response to it, which involves multiple systems, from metabolism to muscles to memory—may be the chief challenge that astronauts face. Spaceflight is full of stressors, many of which can have an impact on brain function, cognitive performance, and mental capacities. Several changes in brain structure and function have been observed [in astronauts after spaceflight]. The full implications of these changes for health and performance are not yet known, but any adverse consequences will be increasingly important as spaceflights become longer and more ambitious (such as a three-year mission to Mars).

Along with the high workload, sleep disruptions and misalignment of circadian rhythms are not uncommon. The normal light-dark cycle, which ordinarily provides a temporal structure to the day and entrains biological rhythms, is missing. Alarms of various kinds repeatedly awaken astronauts to conduct necessary tasks, and the pervasive sense of danger, lest something go wrong, can also be disruptive. All of these contribute to fatigue and stress.
Such factors may not be unique to spaceflight, but the level of isolation and confinement astronauts experience is certainly unlikely to be found at home. As far as spacecraft go, the International Space Station (ISS) is large, but it is still small compared to the indoor and outdoor spaces we have access to here on Earth. There is no such thing as “going out for a walk,” without a great deal of preparation, special and cumbersome suits, and attendant increased risk. Add to this the fact that, while the view outside may be spectacular, astronauts aren’t tasked to look out the window but rather to work inside, where they see the same people and the same scenery day after day, month after month. The stress of interpersonal relations under such circumstances can be challenging.
Then there are factors that are even more specific to space travel. The level of carbon dioxide in a spacecraft is typically much higher than here on Earth, because it is expensive in terms of supplies and energy to reduce it. Elevated CO2 produces such effects as irritability and headache—not the
14 DANA FOUNDATION CEREBRUM | Spring 2021 A
-
PHOTO: NASA.GOV

Working in zero gravity means a shift of body fluids and could lead to changes in cognitive function and vision.
types of things that are conducive to working with others in a small space. The radiation level is also elevated—although not as high as it is on the moon or Mars, or in deep space on the journey there. The primary long-term risk from radiation is an increased lifetime likelihood of cancer, but there are possible short-term effects as well. There is some evidence from animal studies that a large acute radiation dose (as might result from a solar flare) could cause a deficit in cognitive function. While this remains to be verified in humans, the prospect of a drop in mental capacity when it is most needed—for example, in mid-journey to Mars—should give one pause.
Finally, there is weightlessness itself. It is perhaps odd to think of this as a stressor, when we see astronauts cavorting in zero gravity, free to explore the full three-dimensional scope of their confines. But this freedom comes with challenges. Objects, including people, float away if not held in place. Debris floats and can get into the eyes. There are also physiological consequences of the shift of body fluids to the head, which might lead to changes in cognitive function, and certainly contribute to sinus congestion and alterations in the senses of taste and smell.

Astronauts are asked to perform at a very high level in a very demanding situation, under constant supervision and scrutiny; this doesn’t help with the stress level. Beyond such external factors, the high standards they set for themselves may lead to self-imposed stress. A mission is often the peak of one’s professional career, a position of high visibility in which errors of judgement can have immediate and dire consequences. Astronauts are well-prepared and highly trained to overcome and cope with stressors that would be unbearable for most of us. Nevertheless, they are human. Stress takes a toll, especially over the long run and when downtime for rest and recovery is hard to come by. While we understand a great deal about these stressors individually (even if we do not yet know how to counter them effectively), their combination, over an extended period, could lead to problems that we do not yet foresee. In this regard, human spaceflight is not only an exploration of space itself, but also of human limits and capabilities.
Effects of Stress
What are the effects of these myriad stressors on brain function and mental performance? We know some, and others might become apparent on more ambitious missions such as a trip to Mars. A common observation among astronauts refers to a phenomenon known as “space fog” or “space stupids”—a sense of cognitive slowing and the need for increased mental effort to perform routine tasks
Disrupted sleep and elevated CO2 alone, in a demanding setting under intense pressure to perform, could easily produce such cognitive problems. Add all the other spaceflight stressors described above, and it is not hard to imagine having even greater difficulty concentrating and a sense of mental lethargy. Related to this is the phenomenon of “neurasthenia”: a vaguely defined sense of fatigue, lack of motivation, irritability, and related somatic sensations.
Strangely, though, objective testing of cognitive function in space does not fully support these subjective observations. Inflight cognitive testing shows variable effects and is hampered by a small number of astronaut subjects and poorly controlled conditions (differences in flight experience, fatigue level, sleep, etc.). A laboratory experiment provides a much bettercontrolled setting, but it cannot reproduce the reality of space travel that we desire to capture.
In fact, what space data we do have show few, if any, significant decrements in objective measures of cognitive function. There are some changes in reaction time, for example, but their significance is uncertain. This is similar to the case in which a terrestrial patient has a complaint but testing yields no anomalous results in the clinic. Is the test
Dana.org 15

inappropriate, or are the self-assessments incorrect? Or, as is more likely, is it the fact that motivated, high-performing individuals can rise to the occasion and perform well on virtually any well-defined task, as long as other distractors can be ignored? In the real world (and especially in space), people rarely have this luxury, which suggests why cognitive testing fails to capture the effects of spaceflight stressors in a realistic way.
What Happens to the Brain?
One such effect relates to changes in visual function Astronauts returning from early missions of several months on ISS sometimes reported changes in visual acuity. Given all the demands of spaceflight, and the fact that these astronauts aged several months during their missions at a time in life when normal aging often produces decrements in visual function, it was hard to know what to make of these reports. Eventually, it became clear that there were changes in the structure of the eye—mostly temporary but some apparently long-lasting—that were very troubling. Alterations in visual function in high-performing individuals in a dangerous and demanding environment is something that gets a lot of attention, and a great deal of research has been devoted to characterizing and addressing this concern.
What is the cause? It has been recognized for decades that, in weightlessness, there is a shift of fluids (i.e., blood, cerebrospinal fluid, lymph) from the lower to the upper body. This results in puffy faces (easily seen in astronaut photographs), sinus congestion, and blunted sensations of taste and smell. There are also changes in fluid drainage from the head, resulting in a buildup of fluid and, presumably, an (as yet unproven) increase in intracranial pressure. Some of the fluid makes its way down the sheath—the outer covering—of the optic nerve that leads to the eye. Among other things, this flow of fluid slightly distorts the shape of the eyeball, which changes its optical properties and hence visual acuity.
There are also indications of damage to the retina, the layer of nerve cells in the eye that senses light and sends signals to the brain and that can detach from the epithelium. In advanced degeneration, the macula may bleed and leak fluid. Yellow deposits appear and vision becomes blurry. So far, these ocular effects have not produced dramatic deficits in astronauts’ ability to perform their duties, but they are worrisome. They began to generate serious concern when they became more consistent in ISS crews who spent several months in space (as opposed to crews of Space Shuttle missions who spent a maximum of 17 days there). Particularly disturbing is the possibility that these eye changes are but the canary in the coal mine: an indication of broader and more substantial neural damage that might result from longer
flights. (A Mars mission would be about three years, albeit with a long period of Martian gravity which might halt the progression of such weightlessness-induced problems.)
In fact, a number of recent imaging studies have examined the brains of astronauts before and after spaceflight. In some cases, these studies show a slight upward shift of the brain in the skull, and an increase in the size of the ventricles (fluidfilled spaces inside the brain where cerebrospinal fluid is made and stored). Not all of these changes are reversed after returning to Earth. There are also changes in neural gray matter, which increases or decreases depending on the functions carried out by the brain area involved, and alterations in connectivity between regions, indicating neural plasticity and reorganization.
Researchers have also observed white matter changes in several areas of the brain, including the cerebellum, which is involved in motor control and vestibular processing. So far, it seems that no permanent or dramatic damage to the neural tissue of the brain has resulted from spaceflight. In fact, many of the changes seen in imaging studies may be appropriately compensatory and adaptive for weightlessness—they are the body’s natural adaptive response to an unusual environment and serve the person well as long as he or she is in space.

An astronaut's mental health challenge: seeing the same people day after day, month after month.
16 DANA FOUNDATION CEREBRUM | Spring 2021
However, even the small possibility of long-lasting neural damage due to brain shifting or increased fluid volume—along with a possibly dire impact on in-flight performance—calls for careful study and monitoring.
Underlying Brain Function Issues
There are other physiological changes that occur during spaceflight that might impact brain function, whose effects are likely to be subtle compared to those above, but could combine synergistically with stressors in ways that we do not yet understand. One example involves the gut microbiome: the millions of microorganisms that live in the intestinal tract. Among its varied functions, the microbiome appears to influence cognition and emotion through the socalled gut-brain axis; it turns out that maintaining a healthy, vibrant, diversified array of intestinal microbes is important for mental health. For reasons not fully understood, some aspects of this gut microbiome change during spaceflight—possibly the result of the stressors already discussed, along with an altered diet and use of medications for sleep, pain, and other purposes. It seems that bone health, as well, has an impact on brain health through the hormone osteocalcin. Due to unloading of gravity in weightlessness, the bones lose calcium. At least a part of this process seems associated with a reduction in the activity of osteoblasts, which are the cells that create new bone and also secrete osteocalcin.

Finally, sleep is critical for the consolidation of memories and for learning. This includes motor learning: the acquisition of skills that require physical manipulation and dexterity, as might be essential in teleoperation of remote manipulators on Mars or the moon. Impaired sleep, which, as we've noted, is common in space, could undermine the ability to learn such tasks. This is especially important because a mission that takes a long travel time might demand the performance of tasks learned during training, well before the flight began, allowing plenty of time to forget. In-flight training could provide a vital refresher for those tasks, and it would be best if this relearning were not impaired by the inability to consolidate learning during sleep.
FOR A FUTURE MISSION TO MARS , FOR EXAMPLE, SUPPORT FROM EARTH-BASED EXPERTS WILL BE EXTREMELY LIMITED, AND AUGMENTATION OF SUPPLIES THROUGH CARGO DELIVERY ESSENTIALLY IMPOSSIBLE.
Resilience
The body has compensatory mechanisms for many adverse effects of spaceflight, and they work well. But at some point, they reach their limits. Even short of that limit, at what point does the confluence of these effects reduce and erode performance margins and resilience: the ability to recover from an unexpected perturbation or anomaly? This is a perilous problem that is difficult to address.
The vestibular system—the non-auditory part of the inner ear that regulates balance—also plays a crucial role in spaceflight. The brain depends on the presence of gravity as transduced by the vestibular system—a constant throughout evolution and development—to provide a reference frame for spatial orientation. In space, the lack of normal gravitational influence on this system can result in space motion sickness, disorientation, and a variety of related effects. The resultant difficulty in spatial perception and navigation could be a contributor to space fog. In fact, more and more evidence relates vestibular dysfunction to cognitive issues. Although the astronaut’s vestibular system remains intact, alterations in its function due to changes in gravity level could have subtle but cumulative cognitive effects.
Astronauts don’t get to be astronauts without a full complement of compensatory strategies that they can call upon (volitionally or subconsciously) to work around deficits that occur. They might simply increase their level of concentration, or give themselves extra time, or seek help from a crewmate, or defer some harder tasks until they are better rested. If the brain remains able to carry out this type of logistical re-organizational process, can we say there is actually a deficit? Yet, when faced with an additional stressor such as an emergency alarm, the sudden increase in mental demand might make a latent mental or cognitive deficit manifest—at exactly the wrong time. We do not yet have standardized tests for adaptability and the ability to reorganize in the face of a decrease in brain function.
A similar effect is seen on Earth among some patients with balance disorders. They may present to the clinician performing normally on a specific test of balance, but fail when an additional demand is added. An example is walking
Dana.org 17
PHOTO: NASA.GOV
THERE ARE ALSO CHANGES IN NEURAL GRAY MATTER , WHICH INCREASES OR DECREASES DEPENDING ON THE FUNCTIONS CARRIED OUT BY THE BRAIN AREA INVOLVED.
in a straight line, and then walking that same line while turning one’s head back and forth or responding to random disturbances. The additional task draws cognitive resources away from attention to walking, and automatic walking functions suffer as a result.
The Path Ahead
Why should we care about these observations, since their effects on cognitive performance and mental health can be subtle and vary between individuals? So far, these effects have not caused a US space mission to be canceled or postponed for medical reasons.
But there is one overwhelming reason to care. Future missions will be of unprecedented difficulty and, most notably, require a tremendous amount of crew autonomy. For a future mission to Mars, for example, support from Earthbased experts will be extremely limited, and augmentation of supplies through cargo delivery essentially impossible.
Part of every mission is to capture and share images and audio that have never been seen or heard before.
One-way radio transmission time can take 20 minutes; obviously that is an enormous time span if an urgent problem needs attention from Earth.
Furthermore, almost by definition, when venturing into an unknown realm, not all of the risks can be identified and mitigated ahead of time. Astronauts on these voyages will need every possible edge to maintain the ability to carry out the mission and return safely. Part of this edge comes from understanding and mitigating the more critical of the concerns discussed here.
Research is currently underway to address some of the multiple effects of future spaceflight. But this is a daunting task, given the complexity and density of interaction, interconnection, and permutations. And as we’ve seen, it is not just intra-brain interactions that are of interest, but also their interplay with such external factors as sleep, workload, radiation, and other people.

Another question is whether any of what we have learned so far is relevant to earthbound mortals. One might make the case that what happens to highly select individuals, placed under extreme pressure in an unusual environment, has little to do with the rest of us. Astronauts are certainly not average people, as far as test subjects go. Selection requires that they are healthy, fit, and maintain healthy lifestyles. They need to be extremely compliant and follow directions; we are able to continuously monitor and measure nutrition, exercise, sleep, workloads, and task challenges.
But the overall research opportunity provided by space travel will allow us to understand how the brain adapts to multiple stressors, presented simultaneously, over long periods of time. Studying astronauts (especially while in space) dramatically reduces uncontrolled factors, which are troubling confounds in terrestrial studies. Spaceflight stressors and other challenges are indeed different and may never be matched with those on Earth. The manner in which the brain reorganizes to compensate for them, however, can tell us a great deal that is relevant to our own compensatory capacities in the face of disease and aging. l
18 DANA FOUNDATION CEREBRUM | Spring 2021
STELLAR ENDING AND MARS PHOTOS: NASA.GOV
For more, hear our podcast with author Mark Shelhamer at dana.org/cerebrum-podcast.
Our Author’s Top Ten Spaceflight Favs
Apollo 13 (1995) — “I still drop what I’m doing and watch this any time it comes on TV, even though I have it memorized. Great attention to historical and technical detail. Spaceflight is still a risky venture, and this film demonstrates not only the potential dangers but also the training and teamwork necessary to deal with the unexpected.”

The Martian (2015) — “Dealing with the unforeseen is what this book and movie are all about. Captures the need for autonomy, resilience, resourcefulness, and initiative—and the fact that the thing that will kill you is the one you haven’t thought of.”
Mars (National Geographic series) (2016-2018) — “Excellent dramatized depiction of a habitat on Mars and its crew. The fictional account is interspersed with interviews with the actual scientists and engineers who are working to make spaceflight to Mars a reality. The mix of fact and informed fiction is educational and entertaining.”
Europa Report (2013) — "Movie about an expedition to one of the moons of Jupiter to search for extraterrestrial life, which runs into technical problems. Details the consequences of lack of communication with Earth, and the attendant stressors. Gives a good sense of the psychological stresses that will face a small crew on long-duration missions far from Earth—a point that is often ignored."

Carrying the Fire by Michael Collins (1974, reprinted 2009) — "Still the best book by an astronaut. Collins was the command module pilot on Apollo 11—he’s the one who did not land on the moon but stayed in lunar orbit. His experience is dated but his depictions of life as an astronaut, and of his colleagues, is wonderful. And the writing is superb—as much poetic as technical."
Official NASA mission reports / Compiled and republished by Apogee Books — "Not exactly light reading, full of technical detail, but fascinating as an accurate picture of the early missions (up through the first shuttle flights). Formal debriefings reveal what astronauts thought about waste management on Apollo as well as how well they thought the spacecraft controls functioned; it’s all there."

A Man on the Moon: The Voyages of the Apollo Astronauts by Andrew Chaikin (1994) — "Excellent comprehensive account drawn from extensive interviews with the Apollo astronauts. Does for Apollo what The Right Stuff did for Mercury, but with more technical detail on lunar excursions and more insight into the bigger picture of Apollo."
From the Earth to the Moon (HBO series) (1998) — "Serial dramatized version of Chaikin’s book. A set of vignettes that trace the progress of the Apollo program from the perspectives of different people involved at the time. Greatly assisted by the fact that co-producer Tom Hanks is a true space aficionado."
The Right Stuff by Tom Wolfe (1979)
— "The book, not the movie. Possibly the first book to burst the bubble on the squeaky-clean, boy-scout image of the early astronauts. A rousing read thanks to Wolfe’s style and background research. Makes the point that the early astronauts, as test pilots, were in highrisk occupations for a long time before becoming astronauts—their perspectives were much different from those of the public who saw spaceflight as uniquely dangerous."

NASA official mission videos — "For real space-history geeks. Freely available online, the reports from the 1960s (Mercury, Gemini, Apollo) in particular provide a historical perspective not only on the technology of the time but also the cultural perspective on space (an admittedly skewed perspective, from NASA’s PR machine)."

Dana.org 19
THE MARTIAN PHOTO: 20TH CENTURY STUDIOS / MICHAEL COLLINS
PHOTO: NASA.GOV APOLLO 11 MISSION REPORT: APOGEE BOOKS / THE RIGHT STUFF BOOK COVER: FARRAR, STRAUS AND GIROUX

A retired patient visits our author, who is professor of ophthalmology and neuroscience at Johns Hopkins University School of Medicine, for help with his failing vision and learns why but a single treatment option exists for macular degeneration, a condition that affects 200 million people worldwide.
EYE of the Needle
BY PETER CAMPOCHIARO, M.D. •
BY 20 DANA FOUNDATION CEREBRUM | Spring 2021
ILLUSTRATION

HANNA BRACZYK Dana.org 21
A 72 YEAR OLD LAWYER
who is pursuing his passion for photography in retirement was
suddenly unable to take sharp, well-focused photographs. An examination of each eye revealed yellow spots in the macula, the central area of the retina responsible for sharp vision. The macula in the right eye was thickened and raised in height, substantially reducing and distorting his vision.
A test called a fluorescein angiogram, in which fluorescent dye is injected into an arm vein that travels to blood vessels in the retina for imaging, revealed a spot of intense fluorescence that enlarged over time, indicating the presence of abnormal blood vessels leaking plasma into surrounding tissue. An optical coherence tomography scan provided a twodimensional optical cross section showing fluid beneath and within the right eye’s macula.
The patient had a condition known as age-related macular degeneration (AMD), common to about 200 million individuals
“I’m sorry, but LASIK or a prescription for glasses would have no effect on AMD. Both simply change the focus on the retina. If the retina is diseased, neither approach can improve vision.”
globally and referred to as “age-related” because it is rarely seen in individuals younger than 60 years old. With people living longer and longer, it is estimated that by 2040, there will be 300 million individuals with AMD throughout the world. And besides the blurred vision that this patient was experiencing, other patients often complain about difficulty recognizing familiar faces; straight lines that appear wavy; dark, empty areas or blind spots; and a general loss of central vision, which is necessary for driving, reading, and recognizing faces.
Besides age, smoking is a universally agreed upon risk factor for AMD; hypertension and high blood lipids have been identified in some studies but not others.
Prominent factors leading to development of AMD are genetic defects, particularly ones that code for proteins in what is called the complement cascade—a part of the innate immune system, the body’s first line of defense against bacteria and other invaders. The complement cascade is activated by signals or molecular signatures that stimulate pattern recognition receptors, suggesting the presence of an invader.
While the complement system’s hair-trigger response rapidly fights invaders, preventing their growth and spread, it can also lead to false alarms when activated in the absence of an invader, resulting in damage to normal cells. To mitigate this liability, the body has developed systems to turn off the complement cascade. Some of the genetic variants that predispose one to AMD disable one or more of these fail-safe systems.
“I’ve worked hard my entire life, and now that I’m finally able to do something I really enjoy, AMD is ruining it,” my patient said, clearly frustrated. “If I’ve had genetic defects my entire life that never bothered me, why are they causing trouble now?”
I explained that the wear and tear of aging exposes cells’
22 DANA FOUNDATION CEREBRUM | Spring 2021
proteins, RNA, and DNA, to the extracellular environment, in patterns that mimic those of foreign invaders. In a patient with AMD, normal aging is exacerbated by genetic differences that create abnormal deposits under the retina’s photoreceptors and/or retinal pigmented epithelial (RPE) cells. (Photoreceptors are the cells that respond to light and convert it into electrical signals, beginning the process by which the brain constructs images of the environment. RPE cells are a support system that helps to nourish photoreceptors, dispose of their waste, and provide a barrier between them and underlying blood vessels.)
These deposits, which are the aforementioned yellow spots that occur under the retina and were seen during the examination of the patient, are referred to as drusen. They develop gradually as patients with AMD age, which is why AMD most often occurs in seniors. The deposits contain aggregates of diverse proteins and other materials, particularly
the waste of photoreceptors, that collect in the extracellular space. Because they are unlike anything normally present in the retina, the deposits are easily mistaken for invading bacteria or viruses, activating the complement cascade. (We know this because analysis of drusen has found fragments of proteins seen only in tissues in which such activation has occurred.) Activating the complement system results in bystander damage, particularly to blood vessels that supply the photoreceptors. To explain things, I showed my patient a schematic picture of a retina with AMD (Figure 1). Damage to blood vessels reduces delivery of oxygen and nutrients to photoreceptors and RPE cells causing gradually progressive damage referred to as “dry” AMD.
For a while the photoreceptors can survive the lack of oxygen and nutrients but function sub-optimally, making it difficult to read without bright illumination. But over time, they and their supporting RPE cells begin to die, causing blank spots
Cystoid Spaces
Geographic Atrophy
Ganglion Cell Layer
Inner Plexiform Layer
Inner Nucleur Layer
Outer Plexiform Layer
Out Nucleur Layer
Inner Segment
Outer Segment
Retinal Pigment Epithelium
Bruch's Membrane Choriocapillaris
Choroidal Vessels

Complement Activation Dropout of Choriocapillaries Choroidal Neovascularization
PERMISSION FROM
REPRINTED WITH
Dana.org 23
Activation of the complement system causes damage to the blood vessels that supply oxygen and nutrients to the retinal pigment epithelium and photoreceptors. Severe damage causes these cells to die, resulting in advanced dry AMD (called geographic atrophy). Sometimes the damaged photoreceptors and retinal pigment epithelial cells produce vascular endothelial growth factor (VEGF), which causes new blood vessels to grow under the retina. This can keep the cells alive but, at the same time, leak fluid into the retina, resulting in pockets of fluid (cystoid spaces) that reduce vision. This is called wet AMD. Vision can be improved and maintained by injections that block VEGF. CAMPOCHIARO PA AND AKHLAQ A (2020).
Nerve Fiber Layer
FIGURE 1. Schematic of the pathogenesis of age-related macular degeneration
in central vision. This progressive loss of cells in the macula, called macular atrophy, is an advanced stage of dry AMD.
In about 20 percent of patients with dry AMD, the lack of oxygen in photoreceptors and RPE triggers production of vascular endothelial growth factor (VEGF). This protein stimulates new blood vessels to sprout from those damaged by complement, providing an alternative source of oxygen that can slow the progressive damage to photoreceptors and prevent atrophy. The new blood vessels often leak, however, and fluid collects under and between photoreceptors. The blood vessels also produce substances that recruit cells from elsewhere to congregate around them, resulting in fibrosis (scarring) under the retina, which damages the photoreceptors and leads to macular atrophy. The resulting dysfunction, called “wet” AMD, was the cause of reduced vision in my patient’s right eye.
“What about my other eye?” my patient asked.
“The development of wet AMD in your right eye and the presence of large drusen in your left eye increase the risk of developing wet AMD in your left eye, but I would like you to take an antioxidant vitamin, which can decrease that risk somewhat.”
“Is it possible my condition might be treated with LASIK (laser-assisted in situ keratomileusis—reshaping the cornea) or a pair of glasses with a strong prescription?” he asked.
“I’m sorry but LASIK or a prescription for glasses would have
no effect on AMD,” I answered. “Both simply change the focus on the retina. If the retina is diseased, neither approach can improve vision.”
Treating the Problem
My complex explanation about the cause of macular degeneration elicited a simple query: “Can anything be done?” Indeed, the bad news for my patient was that he had both dry and wet AMD, both chronic, vision-threatening conditions. But the good news was that academic and pharmaceutical research had led drug companies to develop proteins that bind VEGF, and injections of these proteins could improve his vision in his right eye.
His uneasy response to this was understandable: “Wait a minute, you’re telling me that the good news is that you want to stick a needle in my eye?”
“It sounds worse than it is,” I said. “We can numb the eye pretty well so you will feel mostly pressure and maybe a little pain, but it only lasts a second.” The injection deposits a large excess of the VEGF-blocking protein in the center of the eye. The drug diffuses into the retina and binds the vast majority of VEGF, and gradually exits the eye carrying VEGF with it. After a month there is none of the protein left in the eye. At that point VEGF can build up again, causing the vessels to leak again and fluid to re-collect in the macula. Then it would be necessary to inject the protein again.
“How many injections will I need?” he asked.
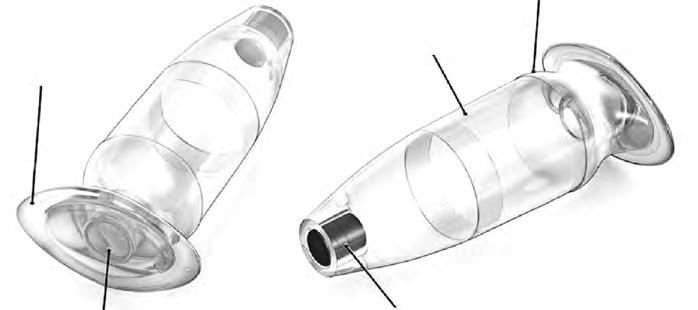
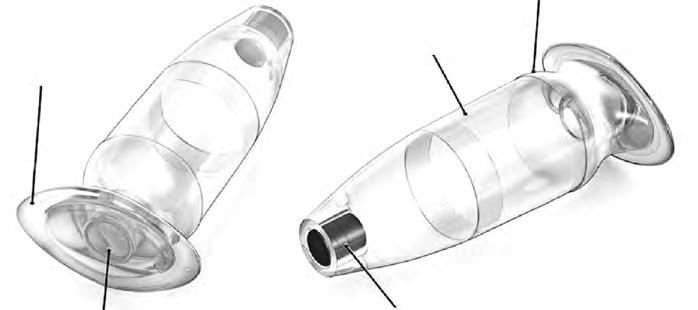
The port delivery system is a refillable reservoir consisting of a (A) flange that contains a self-sealing septum on one side and a release control element on the other. It is implanted through a small incision in the sclera.
When a patient looks straight ahead, the implant cannot be seen (B), but when looking up and out (C), the release control element can be seen within the eye, where it slowly releases a protein that blocks VEGF. When a patient looks down and in (D), the septum is seen beneath the conjunctiva.
Every six months, a needle is inserted through the conjunctiva and septum into the reservoir to replenish the protein that blocks VEGF. This allows uninterrupted delivery of the therapeutic protein to the retina of a patient with wet AMD, eliminating leakage from new blood vessels, and providing maintenance of good vision.



24 DANA FOUNDATION CEREBRUM | Spring 2021
REPRINTED WITH PERMISSION FROM CAMPOCHIARO ET AL. (2019) B
Septum
Silicone coating
C D
Body Release control element
A
Extrascleral flange
FIGURE 2. The port delivery system
“Many, probably every or one or two months for the rest of your life,” I told him.
“I hope that’s a long time, and if it is, that will mean a lot of injections,” he said. “Is there an alternative?”
Fifteen Years of Progress
I told my patient that there is simply no alternative to injections. Prior to 2006, when this treatment became available, wet AMD meant permanently reduced vision to the level of legal blindness or worse. But blocking VEGF with injections improves vision by drying out the retina, and usually stops new blood vessels from growing and recruiting cells that result in fibrosis. Proof of the value of treatment is that many of my patients who have received regular injections since 2006 have retained excellent vision.
This patient wanted a guarantee that injections would improve his vision and maintain it for the rest of his life. That was not something I could promise. While most patients do very well with regular injections, a small percentage do not have complete elimination of fluid and growth of unhealthy blood vessels. These individuals are more prone to subretinal fibrosis and loss of vision.
In addition, many patients are unable to return regularly for the needed injections. I always caution my patients that sometimes life—for any number of reasons—gets in the way. A missed appointment is generally not a problem, but longer delays make subretinal fibrosis and vision loss more likely. During the pandemic, some patients were understandably anxious about visiting a hospital or doctor’s office. Sadly, some patients missed a number of visits and consequently lost vision.
Next Steps
Research on the development of new treatments to provide sustained suppression of VEGF shows great promise for treatment of wet AMD. The most advanced approach involves a surgically implanted device that contains a flange—a rim that sits on the outside of the sclera (connective tissue popularly called the “white of the eye”)—attached to a refillable reservoir. The device passes through the sclera into the vitreous cavity, a fluid-containing chamber lined by the retina. (Figure 2). A release control element in the device slowly releases a VEGFneutralizing antibody from the reservoir into the vitreous cavity.
In the center of the flange is a self-sealing septum, covered by the conjunctiva to prevent infection from the environment. Periodically, the doctor will pass a needle through the conjunctiva and septum to refill the reservoir.
Two phase three clinical trials demonstrated that wet AMD patients who had implantation of the device, with refills every six months, had excellent visual outcomes—as good as results
Two phase three clinical trials demonstrated that wet AMD patients who had implantation of the device, with refills every six months, had excellent visual outcomes— as good as results with monthly injections.
with monthly injections. These successful clinical trials may have paved the way for Federal Drug Administration approval for this new implantation procedure by the Fall.
Another treatment now in clinical trials uses a molecule that blocks VEGF receptors that stimulate the formation of new blood vessels. The chemical is incorporated into a biodegradable polymer and injected into the eye in the form of microparticles. The microparticles slowly release the inhibitor molecule, preventing leakiness from abnormal blood vessels for at least six months.
Finally, a gene therapy now in clinical trials utilizes a harmless virus to deliver a gene that encodes for an anti-VEGF protein. Injected under the retina, the virus carries the gene into retinal cells, where it makes the protein. Any of these approaches would eliminate the need for monthly visits for injections and improve long-term visual outcomes.
While there are as yet no approved treatments for dry AMD, two phase two clinical trials involving monthly injections showed promise. Each trial involved a different protein that blocked a different component of the complement cascade, and both slowed the progression of macular atrophy. Phase three clinical trials are currently underway.
I advised my patient that a treatment plan would most likely put him on the path to taking satisfying photos again. He was encouraged about his prospects for better vision, even if his response was a bit irreverent: “I’m certainly not as despondent as I was at the beginning of our conversation and, while it feels a bit strange to say this out loud: ‘Please stick a needle in my eye.’” l
Dana.org 25

26 DANA FOUNDATION CEREBRUM | Spring 2021
LOSING FACE
Experts weigh in on the impact maskwearing may have on children's education, mental health, and brain development
BY KAYT SUKEL ILLUSTRATION BY ORI TOOR
IN THE SUMMER OF 2020, AS SCHOOL DISTRICTS AROUND the country were announcing mask mandates as part of their plans to safely re-open schools in the midst of the Covid-19 pandemic, a series of memes made the rounds on social media. While their content and images varied, the basic messaging of these posts was the same: Seeing others wearing masks would be detrimental to a student’s development. In fact, these alarming missives asserted, masking rules could lead to permanent psychological and social damage for kids across the globe.


Dana.org 27
Despite ongoing concerns about masks interviewed for this piece were adamant being infected with Covid-19 and suffering far outweigh risks related to the loss of

“This is probably the question, as a developmental psychologist, I’ve been asked the most lately by colleagues and other parents,” says Vanessa LoBue, director of the Child Study Center at Rutgers University. “Parents are worried that making their kids wear a face mask could have unintended consequences. People are asking me whether their kids will be able to understand what their teachers are saying—or the social and emotional nuances of what’s being communicated to them so they can learn how to appropriately respond to it. They want to know if it’s going to cause unnecessary anxiety in their kids, if it’s going to get in the way of normal development. There are definitely a lot of questions.”
Human faces, to steal a line from Walt Whitman, contain multitudes. Whether it’s the righteous joy embodied by an open-mouthed laugh or the subtle contempt of a curled lip, people of all ages rely on others’ faces to help them navigate their social environments. Our expressions, whether we intend them to or not, convey all manner of vital information. Those bashful smiles and pursed lips reveal quite a bit about what we feel—and offer guidance to others on how to best respond to us. This is especially the case if our words and expressions do not match.
“There are a lot of things that are really important for human communication,” says Seth Pollak, head of the Child Emotion Lab at the University of Wisconsin-Madison. “And human faces are definitely one of the most important of them.”

Something Special About Faces
In order to make our way in the world, human beings, like other animals, need to be able to recognize objects. The world is full of things that can help us or hinder us as we navigate our surroundings; distinguishing between the two is vital. Faces, however, are a special kind of object. So special, in fact, that they have their own specific real estate in the brain, the fusiform face area in the temporal lobe, which is solely responsible for facial recognition.

Kang Lee, head of the Development Lab at the University of Toronto, says humans, as a social species, rely on faces to glean information about emotions and social interactions from quite an early age. That information then helps inform our behavior.
“As humans evolved from [non-human] primates, we shed a lot of facial hair,” he explains. “There’s good reason for it—it highlights the eyes and other facial features so we can read important information about another person. By just looking at a face you can see what group or race they belong to, their age, and whether they are male or female. Once you make social contact, the face also is a source of emotional information. The brain can very efficiently manipulate the facial muscles
to convey different kinds of emotions, even extremely subtle changes in our emotions. It’s not a surprise that the brain has set aside a special area so we can quickly perceive and process this information.”
No sooner do infants enter the world than they start looking for faces. Lee says it is a vital part of child development, even at this early age.
“A newborn will quickly lock on to any faces in the environment,” he says. “Their eyes are driven to faces and, within 28 hours of age, they can already recognize their own mother’s face. We have an incredible affinity for faces, and that comes with an innate ability to orient to and recognize faces.”
Masking Emotions?
Given that affinity, it is not surprising that many now wonder about what cloaking half the face may mean not only for development, but also for social and emotional processing. With masks concealing the suggestive contortions of the mouth and nose—which can signal the difference between a smile and a sneer—how might day-to-day mask-wearing affect how we perceive others, and they us?

Claus-Christian Carbon , a perceptual psychologist at Germany’s University of Bamberg, says he was curious about whether a mask might impede how people read emotions. He asked 36 individuals between the ages of 18 and 87 to look at photos of individuals who had standard medical masks digitally added to the picture, and determine whether the faces depicted anger, fear, disgust, happiness, sadness, or neutral emotion. Immediately following, the study participants were asked to assess their confidence in their judgment on a scale of one to seven (“very unconfident” to “very confident”). He says he was not surprised that participants had more difficulty judging emotions, especially between photos of happy and emotionally neutral faces. He has since replicated the results in a group of children between the ages of nine and ten years, though the results have not yet been published.
“If you don’t have as much information about the face, it makes sense that processing will be hampered,” Carbon says. “But what we also saw was that participants had lower confidence in their own perceptual ability when reading those faces. Given that emotional expressions are one of the most efficient ways of communicating to other people, this is something that does have an impact. People will have to rely on other cues, like context or a person’s tone or gestures, to help them understand what emotion a person may be trying to express.”

Ashley Ruba, a post-doctoral fellow in Pollak’s lab at the University of WisconsinMadison, with Pollak, conducted a similar experiment on 81 children between ages 7 to 13.
28 DANA FOUNDATION CEREBRUM | Spring 2021
masks and emotional learning, all of the scientists
adamant
that the risks of not wearing a mask—and potentially
suffering
from long-term health consequences as a result—
face-relayed
social information.
Unlike Carbon’s study, this experiment tested the children only on photos depicting sadness, anger, and fear after the photos were digitally altered to add a surgical mask or sunglasses. The Wisconsin researchers also found that study participants were less accurate at reading emotions on masked compared to unmasked faces, but their accuracy was still above chance. Given that, outside the laboratory, children will have access to the other contextual cues to emotion that Carbon mentioned. Ruba says she and Pollak don’t believe the inaccuracy caused by mask wearing will lead to any long-term deficits.
“While there was some loss of emotional information, kids were still able to make a reasonable guess about what the person in the photograph was expressing,” she explains. “I know parents are very worried about the effect of masks on kids being able to learn this kind of social information. But we found they are still surprisingly good at figuring out the information they need to make these judgments.”
Certainly, a University of Parma study supports this idea that some emotional information is coming through. The 96 adults, with an average age of about 36 years, were able to correctly recognize happy, angry, and neutral faces, even when they were covered by a mask or scarf. Carbon says the subtle differences seen across these studies may be due to the kinds of emotional photos experimenters used.
“We saw that people had difficulty distinguishing happy and neutral,” he says. “Emotional expressions in faces are a method of very fast communication between people. With a mask, you may need to use more words or find other ways to get your point across. It isn’t that you cannot get this information. It’s just that communication becomes less efficient.”
Filling in the Gaps
Despite that lack of efficiency, Carbon doesn’t think that social or emotional development will be derailed by increased mask-wearing. To start, people don’t need to rely solely on a static photo of a masked face to glean emotional data. Other dynamic cues—including gestures, tone, and posture, and contextual information—will help fill in the blanks.
LoBue adds that younger children, who may be in the process of learning how to read emotion in faces, can still interact with family and close friends without masks at home—and see the faces of their unmasked teachers through virtual platforms. They are not completely bereft of facial cues.
“If you worry a child is having trouble reading a masked face, you can encourage them to ask questions,” she says. “There’s no reason why we can’t prep children to raise their hand and ask for more information if they need it, whether the other person they are communicated with is masked or unmasked.”
Understanding the Trade-Offs

Despite ongoing concerns about masks and emotional learning, all of the scientists interviewed for this piece were adamant that the risks of not wearing a mask—and potentially being infected with Covid-19 and suffering from long-term health consequences as a result—far outweigh risks related to the loss of face-relayed social information.
“Faces are not the only place we get this important information,” says Carbon. “There is also information in what people say, their verbal descriptions, their tone of voice, their gestures. Even if part of this facial information is missing, we can compensate for it. It may be a little harder to do, but children are really quite adaptive. They will learn what they need to learn.”
For her part, Ruba worries more about other burdens, including the anxiety and social isolation many children may be experiencing. She argues that those issues may have more power to affect children’s cognitive and social development than a nose and mouth covering. Numerous studies suggest that the pandemic is leading to increased rates of depression and anxiety in both kids and adults, but it is hard to distinguish what aspects of pandemic life, exactly, may be influencing such trends.
“People are focused on the mask-wearing as something that will hurt kids, but what may be of more concern is that so many children are isolated from their friends or struggling with virtual school,” says Ruba. “We don’t know yet what may have long-term effects on development or mental health. These are things that we should be looking at carefully as we move forward.”
While headlines abound about all the things that children may be missing as a consequence of pandemic-related infection control practices, most of those stories are based on anecdotes and conjecture. With many scientists now having to work remotely to continue social distancing themselves, some researchers are unable to do their work outside the laboratory—and studies that examine issues as complex as the effects of virtual learning, reduced peer interaction, and the loss of loved ones to the virus on children’s emotional and social development can be challenging to pursue.
As such, Pollak argues that mask-wearing should be the least of those worries—and that, even with reduced emotional content in facial expressions, children will find a way to learn the social skills they need to learn, grow, and thrive. “The one thing we know is that kids’ brains really are resilient,” he says. “Generations from now, their grandchildren are going to ask them what it was like to live through the pandemic. They may have plenty of stories about the hardships they may have experienced, but no one’s cognitive or social development is going to be irreversibly damaged as a result of what we are going through now.” l
Dana.org 29

The Brain and Covid Strides and Speculations
One year on, science has discovered much about the effects on the brain, but there is still much to learn.
BY CARL SHERMAN
ILLUSTRATION
BY J.F. PODEVIN
IT WAS NEARLY A YEAR AGO WHEN LARISSA MALCOLM, 47, a social worker in the Cleveland area, tested positive for Covid-19. “I wasn’t sick enough to be hospitalized,” she says. “I never coughed.” But she did have a gallery of—then, anyway—mysterious symptoms. “I lost my sense of smell; I felt tingly, like electric shocks through my body. I felt there was a short in my brain.”
For the first time in her life, she had panic attacks. She felt generally confused and reported this to the local health department. “I was told it isn’t part of Covid,” she says.
Malcolm’s sense of smell never returned completely. She still takes medication to keep her anxiety at bay. And she still struggles with confusion and memory loss. “I go into a room and can’t remember why,” she says.
30 DANA FOUNDATION CEREBRUM | Spring 2021
k k

Dana.org 31
AS THE OUTBREAK OF A VIRULENT NEW DISEASE Covid-19—spread relentlessly across continents, doctors were not entirely surprised to see neurological problems. “If this was like other viral infections, there would be fatigue, cognitive complaints, and the like,” says neurologist Ayush Batra of Northwestern University. Reports of related coronavirus infections—SARS and MERS—cited severe central nervous system (CNS) disease, including encephalitis and stroke.
of patients in her series) may have been secondary to anticoagulation, however.

But the extent of Covid’s impact on the brain was striking. In a published retrospective study of 509 hospitalized patients, Batra and colleagues saw neurologic manifestations in 83 percent. These ranged from headaches and dizziness to strokes and seizures.

A larger prospective study reported symptoms severe and pronounced enough to meet diagnostic criteria for neurological disorders in 13.5 percent of 4,491 patients hospitalized with laboratory-confirmed Covid-19. The most common of these disorders was encephalopathy, alterations in consciousness ranging from confusion and disorientation to coma. “A lot of people came in because they were confused, and some developed it later in their hospital stay,” says Jennifer Frontera, professor of neurology at New York University (NYU) and lead author of the study. “It was often related to low oxygen levels and low blood pressure.”
In some, prolonged hypoxia and hypotension led to brain damage verified by magnetic resonance imaging (MRI) or computerized tomography (CT) scans.
Age and sex were factors: Those who developed neurological disorders were significantly older than those who did not, and more likely to be male. Comorbid disorders, such as hypertension, diabetes, and atrial fibrillation, were more common as well. Obesity did not play a role; in fact, “patients who had neurological damage had slightly lower BMI (body mass index) than those who did not,” says Frontera.
It is unlikely that neurological disorders were the effects of treatment rather than disease in either study. “At that time [early in the pandemic], hydrochloroquine and azithromycin were the most commonly used medications, and [neurological events] are not known side effects [of these drugs],” Frontera says. Some hemorrhagic strokes (seen in 0.4 percent
Nearly two percent of the patients in Frontera’s group suffered strokes (the majority ischemic), confirming what had been reported elsewhere: A study of patients with PCRconfirmed Covid-19, who were hospitalized or treated in the emergency department of two NYC hospitals, found the risk of stroke to be 7.6-fold larger than with influenza. An unlikely proportion occurred in younger patients. One New York City hospital reported that five Covid-positive patients under 50 were admitted with strokes in a two-week period, seven times the rate for this age group the year before.
Over the Long Haul
“I had a fever and a bit of a cough, but I wasn’t that sick,” says Sarah Ehekircher of her bout of Covid-19 in August. “I’d feel really good for a couple of days and think I could come out of quarantine, and then I was sick again.”
But ever since, the 52-year-old Seattle resident says, she has suffered from profound fatigue—“I can’t walk up a flight of stairs without having to stop”—and disturbing mental problems. “I have difficulty coming up with words. I constantly lose my train of thought. I can’t concentrate enough to read a book. I feel an overwhelming wash of brain fog, and I can’t function.
“A couple of months ago, I literally thought I had dementia,” she continues. “I couldn’t figure out a bus schedule! I thought I’d need to have someone come in to help me.”
Equally troubling has been the effect on her relationships. “I’d fire off hurtful text messages and ask myself, ‘why did I do that?’ It was like being a teenager with no impulse control. I didn’t recognize myself.”
Ehekircher’s symptoms are typical of what many Covid patients experience. When one thinks the disease is over, all too often it’s not all over. “The acute infection doesn’t last very long—you can’t detect it after a week or two,” says Avindra Nath, intramural clinical director of the National Institute for Neurologic Disorders and Stroke (NINDS). “The virus has gone, but the music lingers on.” Extreme fatigue, worsened by exercise, “resembles to some degree chronic fatigue syndrome, which occurs after a viral infection. As soon as the pandemic started, we knew we were going to see these patients.”

“There’s been a lot of fantastic scientific work worldwide, and it’s been stunning to see the rate of progress… a heroic and unprecedented achievement.”
DANA
32
FOUNDATION CEREBRUM | Spring 2021
The “music” involves a good deal more than fatigue. Sufferers frequently find it hard to think, focus, or remember. Some become clinically depressed or anxious. A galaxy of physical problems, most prominently shortness of breath, but including diverse aches, pains, and troubling symptoms fill out the picture of what has come to be called “Long Covid” or “Longhaul Covid.”
“I suspect that much of this broad effect is related to some kind of neurological injury, whether to the brain, muscles, or immune system, and needs to be really studied,” says Nath. Such common problems as racing pulse, constipation, dizziness due to low blood pressure, or even shortness of breath, may reflect dysfunction in the autonomic nervous system.
In recent months in particular, research and clinical efforts have increasingly focused on Long Covid. Dozens of online support groups for sufferers have appeared, along with an expanding universe of clinics, nationwide and abroad, dedicated to their care.

In a study (which has not undergone peer review), Eric Song, a researcher at Yale University, and his colleagues found evidence of immune activity in the cerebrospinal fluid (CSF) of Covid patients who had neurological complications. This included more cytokines and activated B cells than in the bloodstream, and antibodies that target both the viral spike protein and brain tissue. “This not only suggests viral invasion, but that neurological symptoms might be driven by autoantibodies—think of an autoimmune condition like multiple sclerosis,” he says. “That one of the antibodies specific to spike protein is also binding to human tissue suggests that molecular mimicry seen in other viral diseases could also be here.”
Such a process, Song says, might explain the tenacity of Long Covid. “In a lot of these kinds of diseases, the autoimmune response persists for a decade. It’s like a floodgate: Once it’s open, you can’t close it back up.”
While estimates vary widely, from ten percent upward, chronic problems clearly bedevil an enormous number of Covid-19 survivors. One study of 143 patients who had been hospitalized for Covid found that 87.5 percent had at least one persistent Covid-19-related symptom, chiefly fatigue and shortness of breath. Two months after their disease began; 55 percent had three symptoms or more.
Neurological symptoms in Long Covid can be diverse, persistent, and by no means limited to those who had been ill enough to require hospitalization. In a series of 100 patients at a Northwestern Covid-19 clinic who had neurological problems six weeks after initial Covid diagnosis, 85 percent still had four or more symptoms an average of three months later.
“These patients had had mild Covid, in that they had never needed oxygen,” says Edith Graham, a clinical neuroimmunology fellow at Northwestern and lead author of
the study. “Some had horrible fever and were very sick for two or three weeks, but others had felt they just had a cold for a few days. There was no association between initial severity and later symptoms.”
“Brain fog”—the kind of memory, thinking, and focusing problems that Ehekircher describes —was the most common neurological symptom, affecting 81 percent of patients. [Such phenomena might arguably reflect, at least in part, anxiety or depression surrounding the illness, or the stress of living in a world in turmoil. A study now in progress might help illuminate this question.]
In addition to cognitive dysfunction, two-thirds had persistent headache, and more than 50 percent had numbness and tingling, muscle pain, and/or disorders of taste and smell. Nearly one-third had tinnitus or blurred vision.
The patients in the study were predominantly female (70 percent) and young (average age, 43), mirroring sex and age demographics for Long Covid generally.
Whether strictly biological or partly psychological, the mental effects of Long Covid are apparently substantial. A selfadministered cognitive assessment of 84,000 people in the UK found those who had had confirmed or suspected Covid-19 one to three months earlier performed more poorly than others in many ways.
“There were particular deficits in executive function— decision-making and concentration—and higher language functions,” says Adam Hampshire, of the Computational, Cognitive, and Clinical Neuroimaging Laboratory at Imperial College London, first author of the paper, which has yet to be peer reviewed. His preliminary findings accord with subjective reports, he says.

Deficits were most marked in the patients who had been sickest: the equivalent of an 8.5-point drop in IQ for those who had needed ventilators. Declines were more modest but still significant in individuals who had remained at home.
“A lot of these people say they have sleep disturbances,” Hampshire says. “And if you look at the cognitive pattern, it’s similar to what you’d expect after several days without sleep: brain fog, trouble finding words, forgetting what you’re doing. What we don’t know is: what’s cause, what’s effect?”
Depression and anxiety “had little association with cognitive performance,” Hampshire observes.
But such mental maladies are a significant problem in their own right. One study examined records of 62,354 patients, both hospitalized and non-hospitalized, weeks to months after their bouts with Covid-19, and found the incidence of psychiatric symptoms pronounced enough for clinical diagnosis (most frequently, anxiety and mood disorders) to be 18 percent. This was significantly more than the rate in comparison groups of individuals who had had other illnesses. Among Covid survivors with no prior psychiatric history, the
Dana.org 33
rate of mental maladies was 5.8 percent—double what it was in the comparison groups.
Post-traumatic stress disorder is not rare: A paper reported that one-third of 381 patients who had come to a hospital emergency department with Covid-19 were diagnosed with post-traumatic stress disorder when evaluated one to three months later.
Parsing biological, situational, and psychological factors in mental disorders can be daunting in the best of times, but all the more so in a year when psychosocial stressors and mental health problems constitute a pandemic of their own.
Although definitive conclusions in some cases aren’t yet possible pending the gathering of additional data, speculation by scientists who have studied Covid and brain patterns for months have led to some well-honed observations. In February, for example, “just after the second surge,” Frontera’s group at NYU compared individuals (999 in all) who had been diagnosed with Covid-19, but not hospitalized, with those who had not had the disease.
“We’re examining the question, ‘What is the additive effect of Covid on top of the fatigue and the mood and cognitive insults of being socially isolated, under financial stress, and threatened by serious disease?'” he says. “We asked about stuff like financial insecurity, food insecurity, homelessness, childcare, relationship problems,” Frontera says. “There was a lot of political conflict—with family, friends and colleagues.”
The survey explored the place of pre-existing psychiatric, neurological, and medical conditions. “We asked about fear of illness and about personal illness as a stressor.” The participants self-tested with a battery that evaluated anxiety, depression, fatigue, sleep, and cognitive dysfunction—“how they feel about their thinking processes,” Frontera says. Because the paper is still under review for publication, she could not disclose findings.
The Enemy Within
Research into neural effects of Covid-19 began in the earliest days of the pandemic and has accelerated ever since. “The pace has been exponential,” says Batra at Northwestern. “There’s been a lot of fantastic scientific work worldwide, and it’s been stunning to see the rate of progress… a heroic and unprecedented achievement.”
Much of this work has sought to clarify the underlying mechanisms by which Covid-19 wreaks its havoc in the CNS. But though much has been learned, answers to perhaps the most fundamental question—does the virus attack the brain directly?—are elusive. “Viral invasion? I think everyone agrees this remains controversial,” says Nath. Although some researchers have found signs of infection in neural tissue, “there’s no evidence of overwhelming virus in the brain. I don’t think that alone explains all this.”
Two recent papers suggested how the virus might gain
“A large proportion of our patients here were never hospitalized, yet still have pretty debilitating symptoms.”
access. Using an animal model, one showed the spike protein—the projection by which Covid latches onto and attacks cells—crossing the blood-brain barrier to be taken up by brain tissue. In the other, post-mortem analysis found the virus in the mucosa of the nose and throat, and along the olfactory nerve, and in a path through the brain.
At Yale, Song was also the first author of a recent paper that explores neuroinvasion using an organoid—a three-dimensional neural tissue culture—a mouse model, and brain autopsy of people who had died of Covid. “Every model has its limitations; we used all three to see what they had in common,” he says. Besides the presence of virus, “we found metabolic changes and vascular remodeling, and we think long-term changes in the CNS might have to do with destruction of vasculature.”
His own findings notwithstanding, Song sees a multifactorial picture. “The field as a whole has been approaching [mechanisms] in multiple avenues—there’s the direct neuroinvasion portion, and how systemic inflammation and hypoxemia are affecting the brain. I think it’s hard to call the neurological sequelae of Covid a single disease. You have to keep an open mind.”
Some researchers, like Frontera, lean toward a systemic explanation. In the NYU series of hospitalized Covid-19 patients, “we did not detect meningitis or encephalitis due to direct invasion by SARS-CoV-2,” she explains. “Our paper highlighted the idea that most neurological manifestations were secondary effects of the virus, related to being hypoxic, uremic, or in sepsis.”
A key to Covid injury, she speculates, may be microvascular damage. “Small vessels become leaky, prone to bleeding. We have patients with multifocal hemorrhages.”
Other researchers agree. “The SARS-COV-2 (Covid’s formal title) virus has a special predilection for the ACE2 receptors, which is expressed in [the lining of blood vessels] all across the body,” says Batra. “Pulmonary symptoms are what got all the attention early on, but it’s not surprising to see neurological symptoms as well, there’s such a vast network of blood vessels in both the lung and brain.”
A post-mortem study of 13 patients who had died of Covid-19 found signs of microvascular injury in brain tissue, thinning of the cells lining blood vessels, and signs of congested blood vessels. There were indications of microhemorrhages in the olfactory bulb and other areas.
“Quite possibly, the virus first attacks endothelial cells,” says Nath, an author of the study. “Then the immune system targets those cells, leading to blood vessel damage. There is a hypercoagulable state which leads to occlusions, and some patients develop hemorrhages, too. I suspect that’s the major initial pathophysiology.”
34 DANA FOUNDATION CEREBRUM | Spring 2021
A Bigger Picture
Other researchers are looking at larger brain structures. Kyle Pattinson, senior clinical research fellow at University of Oxford, heads an MRI project that focuses on the brainstem.

“Other coronaviruses have been shown to be neurotropic to the brainstem,” he says. “If the virus enters via the nasal mucosa, it will have a direct route through the olfactory bulb down to the ventrolateral medulla, which regulates heart and lung function.”
Brainstem structures also govern perception of internal sensations, and their dysfunction might account for “’happy hypoxia’, a condition where acutely ill Covid-19 patients don’t sense they’re having respiratory compromise,” he says. Conversely, brainstem involvement “may make breathlessness feel worse than it should be if only the lungs were affected.”
Pattinson himself struggled with post-Covid fatigue as well as breathlessness—the two most common phenomena—for six months. “Probably all the symptoms in Long Covid will be from a multitude of factors, and the brainstem will be one of these factors,” he says.
His study will look at higher centers as well; he is working with Hampshire to correlate structural changes with cognitive decline, and with fellow Oxford researchers to explore neurotransmitter systems, inflammatory markers, and neuronal integrity. “We’re hoping to get an idea just what neural effects occur,” Pattinson says. His group has a particular interest in following people who are having prolonged symptoms but were not hospitalized when acutely ill.
The Oxford brain study is one of an increasing number that are tracking the course of Covid-19 over time. How long does Long Covid last? When will the “brain fog” lift? What can help? Researchers, clinicians—and above all patients—are eager for answers. The National Institutes of Health is allocating more than $1 billion to research investigating Long Covid in all its multi-organ complexity—causes, manifestations, natural history, and treatments.
Frontera has finished a six-month follow-up evaluation of anxiety, fatigue, and other neurological symptoms in her NYU group of hospitalized Covid-19 patients and plans another at one year. “We’re looking at trajectories of recovery,” says Frontera, who is also on the steering committee of the Covid-19 Neuro Databank/Biobank, funded by the NINDS and maintained by NYU. This project will collect information on neurological symptoms and the course of the disease from health care providers, hospitals, and researchers across the country, along with biological materials such as blood and CSF.
“We may see regional variations in viral genotype and get information on different strategies used with different patients,” she says. “Hopefully we’ll answer some questions
about underlying etiology.”
A consortium of researchers from 30 countries are participating in a study to trace a possible path from Covid-19 to neurodegenerative diseases, particularly dementia. “It’s a ‘study of studies,’” says Heather Snyder, vice president, Medical and Scientific Relations, of the Alzheimer’s Association, which is funding the initial effort.

“Groups around the world will collect blood, MRI images, clinical data, depending on their resources. Some studies will involve hospitalized individuals only; other studies, patients in the community.”
The resulting trove of data will be pooled, shared, and subjected to meta-analysis “to identify associations and connections, and answer some of the big questions about the long-term impact of Covid-19 on the brain and nervous system,” she says.

Sudra Seshadri, founding director of the Glenn Biggs Institute for Alzheimer’s & Neurodegenerative Diseases at University of Texas, San Antonio, and coauthor of a paper that outlined the rationale for the project, notes that inflammation is prominent among the effects of SARS-CoV-2. “We know that immune problems have a role in Alzheimer’ disease, too. And direct effects of the virus, such as increasing clotting tendency, might lead to small strokes, which tend to worsen dementia.”
Earlier researchers have suggested a link between diverse viral infections and Alzheimer’s disease, she points out. The plan is to follow participants for 18 months or longer, tracking variables including cognitive functioning. All ages will be involved, “but we are focusing on older people [including] some who have MCI (mild cognitive impairment) and early Alzheimer’s,” says Seshadri.
This particular area of research is poised to accelerate. The National Institute on Aging recently called for grant proposals to fund projects exploring the impact of Covid-19 on neurodegenerative disorders and the aging process.
A year-plus into the pandemic, the story is far from over. Although vaccination stands to stem the tide, Covid-19 won’t be gone overnight, and variants of the SARS-CoV-2 virus, according to many experts, are likely to be around for a long time.
And even if just ten percent of those infected develop persistent symptoms, with 130 million cases worldwide and counting, that’s a lot of need for whatever neuroscience can deliver. “If we know whether they are due to neuroinvasion, autoimmune, vascular, or other mechanisms, it will change how we manage symptoms and the disease long-term,” says Song. “We often forget why we do this research. Ultimately, it’s to help patients.” l
Dana.org 35
BETWEEN THOUGHT AND EXPRESSION
thought
Greg Dunn explores the brain through his art
Greg Dunn was on his way to a Ph.D. in neuroscience at the University of Pennsylvania when he realized that bringing the brain’s beauty to life was a more suitable role for him than lab work. He started in ink, inspired by Chinese, Japanese, and Korean paintings and the similarities he found in the microscopic world of neurons and the macroscopic world of trees, flowers, and other landscape images.
From there, he branched out to microetchings, gold leaf, scrolls, and murals. Microetching, which consists of creating animated images by precisely controlling light’s reflection off of surfaces, was invented by Dunn and collaborator Brian Edwards, Ph.D., an applied physicist at the University of Pennsylvania. ”Microetchings are made through a complex process of hand drawing, computer manipulation, algorithmic
simulation, photolithography, gilding, and strategic lighting design,” he explains. “No images are taken verbatim from a photograph or scan.”
Here is just a small sampling of work. More can be found on his website and at The Franklin Institute in Philadelphia, the National Gallery of China, the Museum of Science in Boston, some of the top universities and medical centers in the US, and in private collections. Dunn, who resides with his family in Sofia, Bulgaria, but maintains a studio in Philadelphia, sees his art “as a reference in brain-related fields due to its scientific accuracy and ability to engage the public in the complex themes of the brain.
We agree. Enjoy the show.
— Bill Glovin

36 DANA FOUNDATION CEREBRUM | Spring 2021
Brainbow Hippocampus depicts the actively firing anatomy and complex circuitry of the hippocampus, the hub of learning, memory, and integration of experience in the brain. The reflective animations highlight the circuitry and output to the entorhinal cortex and subiculum.

Dana.org 37
Glia and Blood Vessels. Glia cells, which protect neurons from one another and regulates the movement of signals, are enwrapped by blood vessels, which course through and feed neural tissue.

Right: Detail of the cerebellum—the part of the brain that plays a vital role in virtually all physical movement—from Self Reflected under multicolored light.
Below: Cortex in Red and Gold features the cortex, which is responsible for a huge variety of brain related functions. “Evolution has adapted the cortex’s unique structure to take on a staggering number of tasks, and there is no part of the human brain which greater differentiates us from other species,” says Dunn.


Dana.org 39
Left: Wisteria Neuron marries the fractallike forms of neurons and the botanical branching structures of plants. The convergent branching patterns of neurons and plants serve similar functions in interacting with their environments—synaptic neural connections for the neurons, light for the plants.

40 DANA FOUNDATION CEREBRUM | Spring 2021
Self Reflected, an artistic visualization of the human brain, was created over two years from scratch by a team that included neuroscientists, engineers, physicists, and students and is a hyperdetailed representation and simulation of 500,000 neurons in a sagittal slice. (See page 42 for a description of the brain regions portrayed.)

Dana.org 41
The brain regions shown in Self Reflected
(See page 40)

42 DANA FOUNDATION CEREBRUM | Spring 2021

Dana.org 43
ADVISORY BOARD

JOSEPH T. COYLE, M.D.
Joseph T. Coyle is the Eben S. Draper Chair of Psychiatry and Neuroscience at Harvard Medical School. A graduate of the Johns Hopkins School of Medicine in 1969, he was a research fellow at the National Institute of Mental Health with Nobel Laureate, Julius Axelrod. After psychiatric residency at Hopkins, he joined the faculty in 1975. In 1982, he became the director of the Division of Child and Adolescent Psychiatry. From 1991 to 2001, he was chairman of the Department of Psychiatry at Harvard Medical School. His research interests concern the causes of neuropsychiatric disorders. He is the past-president of the Society for Neuroscience (1991), a member of the National Academy of Medicine (1990), a fellow of the American Academy of Arts and Sciences (1993), a fellow of the American Association for the Advancement of Science (2005), and the former editor of JAMA Psychiatry

MARTHA J. FARAH, Ph.D.
Martha J. Farah is the Walter H. Annenberg Professor of Natural Sciences at the Center for Neuroscience & Society, University of Pennsylvania. She is a cognitive neuroscientist who works on problems at the interface of neuroscience and society. Her recent research has focused on socioeconomic status and brain development. Farah grew up in New York City, was educated at MIT and Harvard, and taught at Carnegie-Mellon University before joining the University of Pennsylvania. She is a fellow of the American Academy of Arts and Sciences, a former Guggenheim Fellow and recipient of honors including the National Academy of Science’s Troland Research Award and the Association for Psychological Science’s lifetime achievement award. She is a founding and current board member of the International Society for Neuroethics.

PIERRE MAGISTRETTI, M.D., Ph.D.
Pierre Magistretti is the dean of the Division of Biological and Environmental Science and Engineering at King Abdullah University of Science and Technology and professor emeritus in the Brain Mind Institute, EPFL and Center for Psychiatric Neuroscience, Department of Psychiatry–CHUV/UNIL, Switzerland. Magistretti received his M.D. from the University of Geneva and his Ph.D. from the University of California at San Diego. Magistretti’s research team has made significant contributions in the field of brain energy metabolism. His group has discovered some of the cellular and molecular mechanisms that underlie the coupling between neuronal activity and energy consumption by the brain. This work has considerable ramifications for the understanding of the origin of the signals detected with the current functional brain imaging techniques used in neurologic and psychiatric research.

HELEN S. MAYBERG, M.D.
Helen S. Mayberg is a neurologist renowned for her study of brain circuits in depression and for her pioneering deep brain stimulation research, which has been heralded as one of the first hypothesis-driven treatment strategies for a major mental illness. She is the founding director of Mount Sinai Health System’s The Nash Family Center for Advanced Circuit Therapeutics. Mayberg received an M.D. from the University of Southern California, trained at the Neurological Institute of New York at Columbia University, and was a post-doctoral fellow in nuclear medicine at Johns Hopkins Medicine. Immediately prior to joining Mount Sinai, Mayberg was Professor of Psychiatry, Neurology, and Radiology and held the inaugural Dorothy C. Fuqua Chair in Psychiatric Neuroimaging and Therapeutics at Emory University School of Medicine. She is a member of the National Academy of Medicine, The American Academy of Arts and Sciences, and the National Academy of Inventors. She is on the board of the International Society for Neuroethics and won the society’s Steven E. Hyman for Distinguished Service to Neuroethics (2018).
44 DANA FOUNDATION CEREBRUM | Spring 2021
ADVISORY BOARD

RICHARD M. RESTAK, M.D.
Richard Restak is clinical professor of neurology at George Washington Hospital University School of Medicine and Health Sciences, a member of the clinical faculty at St. Elizabeth’s Hospital in Washington, DC, and also maintains a private practice in neurology and neuropsychiatry. A graduate of Georgetown University School of Medicine, Restak has written over 24 books on the human brain and has penned articles for the Washington Post, The New York Times, the Los Angeles Times, and USA Today; and presented commentaries for both Morning Edition and All Things Considered on National Public Radio. He is a past recipient of the Claude Bernard Science Journalism Award, given by the National Society for Medical Research.

HARALD
SONTHEIMER, Ph.D.
Harald Sontheimer is I. D. Wilson Chair and professor and founder and executive director of the Virginia Tech School of Neuroscience. He is also Commonwealth Eminent Scholar in cancer research and director of the Center for Glial Biology in Health, Disease & Cancer and the Fralin Biomedical Research Institute. A native of Germany, Sontheimer obtained a master’s degree in evolutionary comparative neuroscience, where he worked on the development of occulomotor reflexes. In 1989, he obtained a doctorate in Biophysics and Cellular & Molecular Neuroscience form the University of Heidelberg. He moved to Yale University for post-doctoral studies and later founded Transmolecular Inc., which was acquired by Morphotec Pharmaceuticals. He is the author of Diseases of the Nervous System (Elsevier, 2015).


STEPHEN WAXMAN, M.D., Ph.D.
Stephen Waxman is the Bridget Flaherty Professor of Neurology, Neurobiology, and Pharmacology at Yale University, and served as chairman of neurology at Yale from 1986 until 2009. His research uses tools from the “molecular revolution” to find new therapies that will promote recovery of function after injury to the brain, spinal cord, and peripheral nerves. A member of the National Academy of Medicine, Waxman has been honored in Great Britain with the Physiological Society’s annual prize, an accolade that he shares with Nobel Prize laureates Andrew Huxley, John Eccles, and Alan Hodgkin. In 2018, Waxman received the Julius Axelrod Prize from the Society for Neuroscience.
CHARLES F. ZORUMSKI, M.D.
Charles Zorumski is the Samuel B. Guze Professor and head of the Department of Psychiatry and Professor of Neuroscience at Washington University School of Medicine in St. Louis. Zorumski is also Psychiatrist-in-Chief at BarnesJewish Hospital and founding director of the Taylor Family Institute for Innovative Psychiatric Research. Zorumski’s laboratory studies synaptic transmission in the hippocampus. Since 1997, he has served on the steering committees of the McDonnell Center for Cellular and Molecular Neurobiology and the McDonnell Center for Systems Neuroscience and was director of the Center for Cellular and Molecular Neurobiology from 2002 to 2013. Zorumski has also served on the editorial boards of JAMA Psychiatry, Neurobiology of Disease, and served on the board of Scientific Counselors for the NIMH Intramural Research Program from 2009 to 2013. Since 2011, he has also served on the scientific advisory board of Sage Therapeutics, a publicly-traded company developing neurosteroids and oxysterols as treatments for neuropsychiatric illnesses.

CAROLYN ASBURY, Ph.D.
In-House advisor
Carolyn Asbury has worked in health philanthropy for more than two decades, directing neuroscience-related health programs at the Robert Wood Johnson Foundation and directing the Pew Charitable Trusts’ Health and Human Services Program prior to consulting with the Dana Foundation. Her own research, through the University of Pennsylvania’s Leonard Davis Institute, concerns policies to facilitate development and market availability of drugs and biologics for “orphan” (rare) diseases. She undertook pro bono research and helped to design the Orphan Drug Act; authored “Orphan Drugs: Medical vs Market Value,” and has authored several journal articles and book chapters on these topics. She has served on the boards of several non-profit health-related organizations, including the National Organization for Rare Disorders, U.S. Pharmacopeia, College of Physicians of Philadelphia, and Treatment Research Institute.
Dana.org 45

Bill
Glovin Editor in Chief
Glovin has been a working journalist for more than 30 years. He is executive editor at the Dana Foundation and hosts the Cerebrum Podcast. He has served as editor of Cerebrum since 2012. Previously, he was senior editor at Rutgers Magazine, managing editor of New Jersey Success, editor for New Jersey Business and a staff writer for The Bergen Record. Glovin graduated from George Washington University with a degree in journalism. He sometimes escapes from in front of the monitor to enjoy basketball, biking, and guitar.

Seimi Rurup
Assistant Editor
Rurup oversees the production of all digital and print content at the Dana Foundation. She previously served as editor of Brain in the News, which was the Foundation’s longest running print publication, and utilizes her background in fine arts to contribute to current publications and social media. She also contributes to the Foundation’s Neuro News section. Rurup graduated from Sarah Lawrence College with a degree in writing. When she is not in the office, she can be found in one of NYC’s many museums, Brooklyn cafés, or at home cooking with friends.

Brandon Barrera Editorial Assistant
Barrera is a New York City journalist, born and raised in Queens and living in Manhattan. A public affairs assistant at the Dana Foundation, he is the host of the Dana Foundation’s Communicating Brain Science podcast and writes about books for the magazine. Before coming to Dana, he helped produce content for Bronx Net, a public access television channel. When not enthralled by all things sci-fi, Barrera is fond of cycling, film, and arguing the finer points of tabletop gaming.

Bruce Hanson Art Director
Hanson is responsible for the design and production of Cerebrum. A graduate of Rutgers University’s journalism program, he has worked in a variety of capacities in publishing and media for more than 30 years. In 1991, he founded EGADS, a studio which specializes in graphic design for education, arts and culture, publishing, and technology. When away from his desk, he'll most likely be playing guitar in a live music venue or plotting with his wife about how to book cheap flights to distant destinations.

Join us as we talk to our Cerebrum neuroscientist authors about their research, personal stories, and how their work has the potential to make a difference in people’s lives.





46 DANA FOUNDATION CEREBRUM | Spring 2021 CEREBRUM STAFF
dana.org/cerebrum-podcast WANT
MORE CEREBRUM?







 BY BILL GLOVIN Editor-in-Chief
BY BILL GLOVIN Editor-in-Chief




 BY NICKY PENTTILA
BY NICKY PENTTILA

 BY BRANDON BARRERA
BY BRANDON BARRERA















 BY ANGELA M. REIERSEN, M.D.
BY ANGELA M. REIERSEN, M.D.
 BY PHILIP M. BOFFEY
BY PHILIP M. BOFFEY