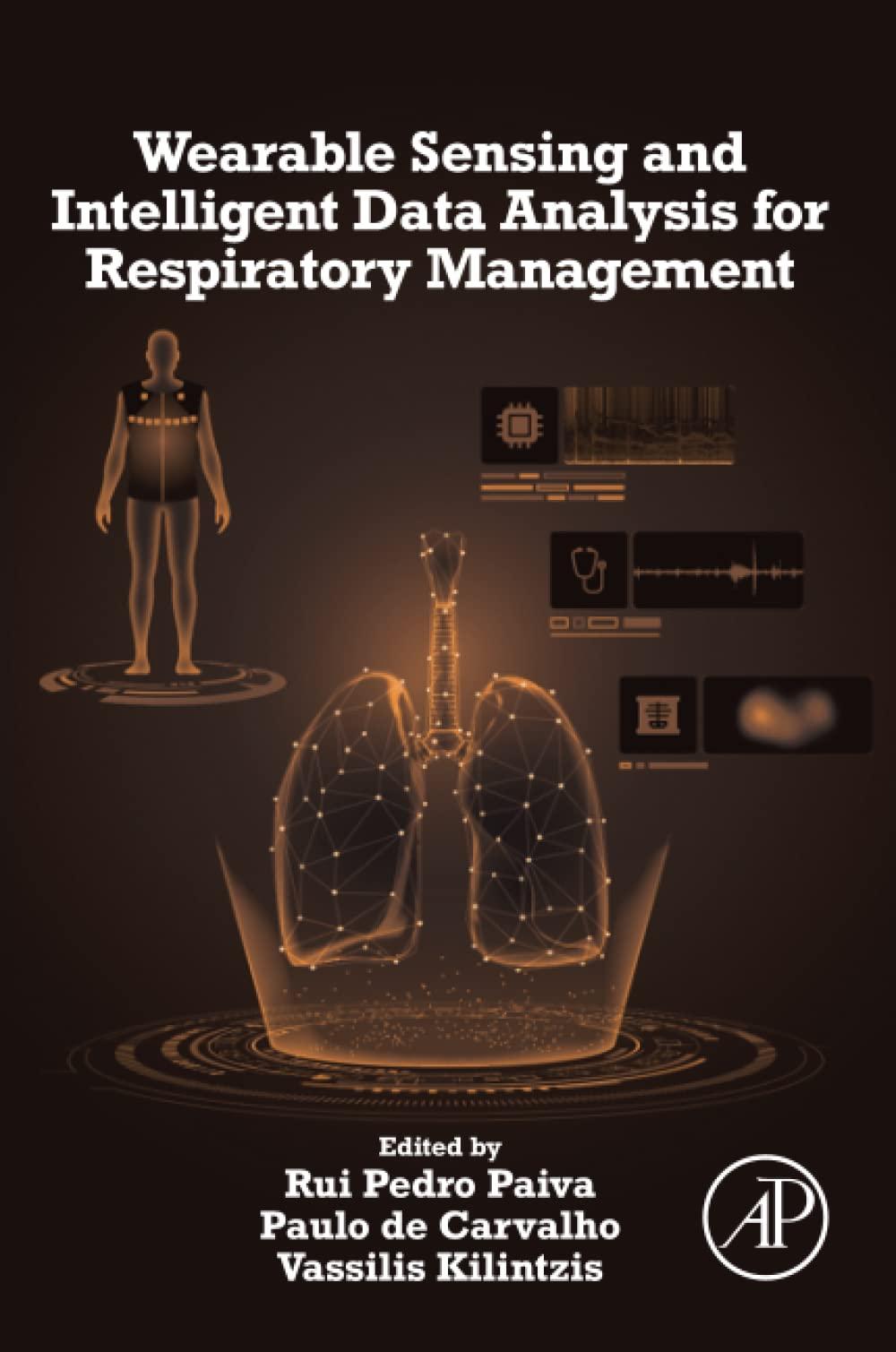
WearableSensingand IntelligentDataAnalysis forRespiratory Management
Editedby RuiPedroPaiva
DepartmentofInformaticsEngineering,CentreforInformaticsand SystemsoftheUniversityofCoimbra,Coimbra,Portugal
PaulodeCarvalho
DepartmentofInformaticsEngineering,CentreforInformaticsand SystemsoftheUniversityofCoimbra,Coimbra,Portugal
VassilisKilintzis
SeniorResearcherattheAristotleUniversityofThessaloniki,Greece
AcademicPressisanimprintofElsevier 125LondonWall,LondonEC2Y5AS,UnitedKingdom 525BStreet,Suite1650,SanDiego,CA92101,UnitedStates 50HampshireStreet,5thFloor,Cambridge,MA02139,UnitedStates TheBoulevard,LangfordLane,Kidlington,OxfordOX51GB,UnitedKingdom
Copyright 2022ElsevierInc.Allrightsreserved.
Nopartofthispublicationmaybereproducedortransmittedinanyformorbyanymeans, electronicormechanical,includingphotocopying,recording,oranyinformationstorage andretrievalsystem,withoutpermissioninwritingfromthepublisher.Detailsonhowto seekpermission,furtherinformationaboutthePublisher’spermissionspoliciesandour arrangementswithorganizationssuchastheCopyrightClearanceCenterandtheCopyright LicensingAgency,canbefoundatourwebsite: www.elsevier.com/permissions .
Thisbookandtheindividualcontributionscontainedinitareprotectedundercopyrightby thePublisher(otherthanasmaybenotedherein).
Notices
Knowledgeandbestpracticeinthis fieldareconstantlychanging.Asnewresearchand experiencebroadenourunderstanding,changesinresearchmethods,professional practices,ormedicaltreatmentmaybecomenecessary.
Practitionersandresearchersmustalwaysrelyontheirownexperienceandknowledgein evaluatingandusinganyinformation,methods,compounds,orexperimentsdescribed herein.Inusingsuchinformationormethodstheyshouldbemindfuloftheirownsafety andthesafetyofothers,includingpartiesforwhomtheyhaveaprofessionalresponsibility.
Tothefullestextentofthelaw,neitherthePublishernortheauthors,contributors,or editors,assumeanyliabilityforanyinjuryand/ordamagetopersonsorpropertyasamatter ofproductsliability,negligenceorotherwise,orfromanyuseoroperationofanymethods, products,instructions,orideascontainedinthematerialherein.
ISBN:978-0-12-823447-1
ForinformationonallAcademicPresspublicationsvisitour websiteat https://www.elsevier.com/books-and-journals
Publisher: MaraConner
AcquisitionsEditor: SonniniR.Yura
EditorialProjectManager: IsabellaC.Silva
ProductionProjectManager: SuryaNarayananJayachandran
CoverDesigner: MilesHitchen
GreekDesigner: CostasPlatides TypesetbyTNQTechnologies
Preface
Respiratorydiseases,suchaschronicobstructivepulmonarydisease(COPD), lowerrespiratorytractinfections,orasthma,havesignificantimpactonpatient’s health-relatedqualityoflife,health-caresystems,andsocietyingeneral.Recent studiesestimatethat,worldwide,around339millionpeoplesufferfromasthma andthat,by2030,COPDwillbecomethethirdleadingcauseofdeath.This posessevereburdenstohealth-caresystemsintermsofoutpatientandinpatient care,aswellaspharmaceuticalcosts,whicharehighlycorrelatedwiththe severityofexacerbationepisodes.
Inthisscenario,theuseofwearablesensingandintelligentdataanalysis algorithmsforrespiratorymanagementassumesparticularrelevance,offering severalpotentialclinicalbenefits.Namely,itallowsfortheearlydetectionof respiratoryexacerbationsinpatientswithchronicrespiratorydiseases,allowing earlierand,therefore,moreeffectivetreatment.Earlyinterventioninexacerbationsoftheseconditionshasbeenshowntodecreasehospitalizationratesand improvelong-termoutcomes,includingsurvival.
Assuch,presently,theproblemofcontinuous,noninvasive,remote,andrealtimemonitoringofsuchpatientsisdeservingincreasingattentionfromthe scientificcommunity.Wearableandportablesystemswithsensingtechnology andautomatedanalysisofrespiratorysoundsandpulmonaryimagesaresomeof theproblemsthatarethesubjectofcurrentresearchefforts.Suchsystemshave thepotentialforsubstantialclinicalbenefits,promotingtheso-calledP4medicine(personalized,participative,predictive,andpreventive).
Tothisend,thisbookcoversthemostrecentresearchanddevelopmenton wearabletechnologiesforrespiratorymanagement.Thebook,organizedinto4 partsand11chapters,startswithanintroductoryoverviewoftheprocessof respiration,itsphysiology,pathologies,andtreatment,followedbythecurrent needsandgapsofrespiratorymanagementindailylife.Thesecondpartaddressestheaspectsinvolvedonwearablesensing,namelyportableandnoninvasivesensortechnologiesformobileandwearableapplications,andtextilesand smartmaterials.PartIIIcoversthedataanalysisandmanagementpipeline,from dataacquisition,transmission,storage,andrepresentation,tofeatureengineeringandmachinelearningforrespiratorysoundandimageanalysis.Finally,Part
IVaddressesthecurrentkeychallengesofrespiratorymanagementsystems, namelytheedge-cloudcontinuuminwearablesensing,strategiesforlong-term patientadherence,decisionsupportsystems,andintegratedcareinrespiratory management.
Webelievethisbookoffersthreemaindistinctivefeatures:(i)anintegrated, unified,andholisticcoverageofthemaintopicsandtrendsinwearablesensing andintelligentdataanalysisforrespiratorymanagement;(ii)anup-to-datereviewofthecurrenttrendsandhottopicsinthedifferentsubfields(e.g.,wearable technologies,respiratorysoundanalysis,andpulmonaryimageanalysis, particularlyelectricalimpedancetomography);(iii)acomprehensiveguidefor startingresearchers,namely,PhDstudents,offeringthemthenecessarytoolsto startperformingcutting-edgeresearchintheirareaofinterest.
Hence,thisbookwillbestsuittheneedsofresearchers,particularlyPhD students,workingondifferentaspectsofengineeringissuesforrespiratory functionmanagement,namelyintheareasofbiomedicalengineering,informaticsengineering,electricalengineering,anddatascienceandengineering.It willalsoworkasanintegratedandcomprehensiveentrypointforanyresearcher whoneedsaholisticoverviewofthefield.Health-careprofessionalswillalso benefitfromthetopicscoveredinthebook,whichaimattheactivepromotionof P4medicine.
Assuch,thereaderwillbeabletomakeuseofthebookmainlyintwoways: (i)assomeonewithabroadinterestinthewholeprocessoftechnologyusefor respiratorymanagement,wherethewholebookwillofferthereaderabroadand deepunderstandingofthearea;(ii)asaresearcheraimingtoacquirespecific knowledgeinsomeoftheidentifiedsubtopics,inwhichcasethereadermightbe interestedinthechapterssettingthebigpictureofthewholefieldandthen focusingonaspecificsubtopic.
RuiPedroPaiva PaulodeCarvalho VassilisKilintzis
Contributors
AndyAdler,SystemsandComputerEngineering,CarletonUniversity,Ottawa,Canada
NikolaosBeredimas,LaboratoryofComputing,MedicalInformaticsandBiomedical ImagingTechnologies,MedicalSchool,AristotleUniversityofThessaloniki, Thessaloniki,Greece
BenjaminBonnal,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
FabianBraun,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
LauraCaldani,Smartexsrl,Prato,PO,Italy
GeorgiaChasapidou,PulmonologyDepartment,“G.Papanikolaou”GeneralHospital, Thessaloniki,Greece
ArisCheimariotis,LabofComputing,MedicalInformaticsandBiomedicalImaging Technologies,AristotleUniversityofThessaloniki,Thessaloniki,Greece
IoannaChouvarda,SchoolofMedicine,AristotleUniversityofThessaloniki, Thessaloniki,Greece
OlivierChe ´ telat,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
MengDai,DepartmentofBiomedicalEngineering,FourthMilitaryMedical University,Xi’an,China
PaulodeCarvalho,DepartmentofInformaticsEngineering,CentreforInformatics andSystemsoftheUniversityofCoimbra,Coimbra,Portugal
DamienFerrario,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
AnaxagorasFotopoulos,EXUSAILabs,Athens,Attika,Greece
Ine ´ zFrerichs,DepartmentofAnaesthesiologyandIntensiveCareMedicine, UniversityMedicalCentreSchleswig-Holstein,CampusKiel,Kiel,Germany
KostasHaris,LabofComputing,MedicalInformaticsandBiomedicalImagingTechnologies,AristotleUniversityofThessaloniki,Thessaloniki,Greece;Departmentof InformaticsandComputerEngineering,UniversityofWestAttica,Athens,Greece
ImanHesso,KingstonUniversityLondon,KT,UnitedKingdom
LauraRomeroJaque,UniversitatPolitecnicadeValencia,Valencia,Spain
EvangelosKaimakamis,1stIntensiveCareUnit,“G.Papanikolaou”GeneralHospital, Thessaloniki,Greece
xiv Contributors
ReemKayyali,KingstonUniversityLondon,KT,UnitedKingdom
VassilisKilintzis,LaboratoryofComputing,MedicalInformaticsandBiomedical ImagingTechnologies,MedicalSchool,AristotleUniversityofThessaloniki, Thessaloniki,Greece
PantelisZ.Lappas,EXUSAILabs,Athens,Attika,Greece
LiviaLasarow,DepartmentofAnaesthesiologyandIntensiveCareMedicine, UniversityMedicalCentreSchleswig-Holstein,CampusKiel,Kiel,Germany
IriniLekka,LabofComputing,MedicalInformaticsandBiomedicalImaging Technologies,AristotleUniversityofThessaloniki,Thessaloniki,Greece
MathieuLemay,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
BrunoMachadoRocha,DepartmentofInformaticsEngineering,Centrefor InformaticsandSystemsoftheUniversityofCoimbra,Coimbra,Portugal
NicosMaglaveras,LabofComputing,MedicalInformaticsandBiomedicalImaging Technologies,AristotleUniversityofThessaloniki,Thessaloniki,Greece
AldaMarques,Lab3R-RespiratoryResearchandRehabilitationLaboratory,Schoolof HealthSciences(ESSUA),InstituteofBiomedicine(iBiMED),Universityof Aveiro,Aveiro,Portugal
AlexisMelitsiotis,EXODUSSA,Athens,Attika,Greece
ShereenNabhani-Gebara,KingstonUniversityLondon,KT,UnitedKingdom
RuiPedroPaiva,DepartmentofInformaticsEngineering,CentreforInformaticsand SystemsoftheUniversityofCoimbra,Coimbra,Portugal
RitaParadiso,Smartexsrl,Prato,PO,Italy
EleniPerantoni,SchoolofMedicine,AristotleUniversityofThessaloniki,Thessaloniki, Greece
DiogoPessoa,DepartmentofInformaticsEngineering,CentreforInformaticsand SystemsoftheUniversityofCoimbra,Coimbra,Portugal
GeorgiosPetmezas,LabofComputing,MedicalInformaticsandBiomedicalImaging Technologies,AristotleUniversityofThessaloniki,Thessaloniki,Greece
MartinProenc¸a,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
Michae ¨ lRapin,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
PhilippeRenevey,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
VicenteTraverSalcedo,ITACA UniversitatPolitecnicadeValencia,Valencia, Spain
SaraSouto-Miranda,Lab3R-RespiratoryResearchandRehabilitationLaboratory, SchoolofHealthSciences(ESSUA),InstituteofBiomedicine(iBiMED), UniversityofAveiro,Aveiro,Portugal
PaschalisSteiropoulos,MedicalSchool,DemocritusUniversityofThrace, Alexandroupolis,Greece
ClaasStrodthoff,DepartmentofAnaesthesiologyandIntensiveCareMedicine, UniversityMedicalCentreSchleswig-Holstein,CampusKiel,Kiel,Germany
BarbaraVogt,DepartmentofAnaesthesiologyandIntensiveCareMedicine, UniversityMedicalCentreSchleswig-Holstein,CampusKiel,Kiel,Germany
JosiasWacker,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
NorbertWeiler,DepartmentofAnaesthesiologyandIntensiveCareMedicine, UniversityMedicalCentreSchleswig-Holstein,CampusKiel,Kiel,Germany
Gu ¨ rkanYilmaz,SwissCenterforElectronicsandMicrotechnology(CSEM,Centre Suissed’ElectroniqueetdeMicrotechnique),Neucha ˆ tel,Switzerland
ZhanqiZhao,InstituteofTechnicalMedicine,FurtwangenUniversity,VillingenSchwenningen,Germany;DepartmentofBiomedicalEngineering,FourthMilitary MedicalUniversity,Xi’an,China
Respiration:physiology, pathology,andtreatment
EvangelosKaimakamis1,GeorgiaChasapidou2
11stIntensiveCareUnit,“G.Papanikolaou”GeneralHospital,Thessaloniki,Greece; 2PulmonologyDepartment,“G.Papanikolaou”GeneralHospital,Thessaloniki,Greece
Introduction
Humanrespirationisthephysiologicalprocessenablingthegases(oxygenand carbondioxide O2 andCO2)exchangebetweentheatmosphereandthe respiratorycirculation.Itisachievedbymeansoftherespiratorymovements ofthethoraciccavityandthelungsandisgovernedbyaseriesofphysiologicallawsandparameterswhichdescribetherespiratorymechanicsandthe gasexchangeitself.
Respirationiscontrolledbysuperiorcentersinthebrainstemandis affectedbynumerousinternalandexternalstimuli.
Normalrespiratoryfunctioniscompromisedwhencertaindiseasesaffect thelungparenchyma(lungtissue),thethoracicwallformations,orthe vascularnetworkofthelungs.Therangeofdiseasestatesthataffectthe respiratoryfunctioniswide,includingdiseasesofthelungitselforother systematicpathologieshavingadirectorindirecteffectonrespiratoryfunctionality.Treatmentofsuchdiseasesishighlydependentonunderlying pathophysiologyandtheextentofthedamage.
Thischaptercomprisestwoparts.InPartA,thephysiologyofrespirationis presentedandanalyzed,coveringissuesrelatedtothedescriptionoflung function,pulmonarycirculation,gasexchange(perfusion,diffusion),respiratorymechanics,andneuralcontrolofrespiration.InPartB,themainrespiratorypathologicalstatesarepresented,withbriefdescriptionoftheireffecton lungfunctionandavailabletreatmentoptions.
PartA:physiologyofrespiration
Overviewofrespiration
Accordingtocurrentphysiologicaldefinitions,respirationisthe“interchange ofgasesbetweenanorganismandthemediuminwhichitlives”[1].Inthe
WearableSensingandIntelligentDataAnalysisforRespiratoryManagement https://doi.org/10.1016/B978-0-12-823447-1.00004-X Copyright © 2022ElsevierInc.Allrightsreserved. 3
humanbody,respirationcanbefurtherclassifiedtoexternalandinternal[2]. Theexternalrespirationinvolvesthetransferofoxygen(O2)andcarbon dioxide(CO2)thatoccursinthelungsbetweentheatmosphereandthe pulmonarycirculation.Theinternalprocessisananalogousprocessthat occursatthecellularlevel.Theexternalrespirationcomprisesofthreeprimary components:ventilation,perfusion,anddiffusion.Athoroughunderstanding ofeachofthesecomponentsandtheirpotentialimpairmentsisessentialfor researcherstounderstandtheoriginandimplicationsofthebiosignalsthatare relatedtorespiration.
Therespiratorysystem(physiology)
Theultimatefunctionoftherespiratorysystemisgasexchange[3].Thisgas exchangeconsistsofobtainingO2 fromtheatmosphereandremovingCO2 fromtheblood.ThepresenceofO2 isnecessaryfornormalcellularmetabolismandCO2 isawasteproductofthismetabolism.WhileCO2 playsarole inacid basebalance,itmustbeclearedfromthebodyinappropriatelevels throughventilation.
Airpassesthroughthenoseandmouthintotheairways,whereitis warmed,humidified,andfiltered.Fromthetracheatothealveoli,thereare23 branchinggenerationsofairways.Thefirst16(inaverage)constitutethe conductingzone,whichisananatomicdeadspace(i.e.,nogasexchangetakes place).The17 23generationsformtherespiratoryzone.Eachgenerationof branchingincreasesthetotalcross-sectionalareaoftheairwaysbutreduces theradiusofeachairwayandthevelocityofairflowingthroughthat.The exchange-effectiverespiratoryzonecomprisesoftherespiratorybronchioles, alveolarducts,andalveolarsacs.Atthisendoftheairways,approximately 300millionalveoliaresituated.Anadultalveolushasanaveragediameterof 200 mm,withanincreaseindiameterduringinhalation.Thealveoliconsistof anepitheliallayerandextracellularmatrixsurroundedbycapillaries.Each capillaryisincontactwithseveralalveoli,sothecapillariespresentasheetof bloodtothealveolarairforgasexchange.Thetotalareabetweenpulmonary capillarybloodandalveolarairrangesfrom70to140m2 inadulthumans (increasedduringexercisethroughrecruitmentofnewcapillariesinparticular intheapicalpartsofthelungs).
Turbulentflowistheagitatedrandommovementofmolecules,which accountsforthesoundsheardoverthechestduringbreathing.Thisflow developsatthebranchpointsoftheupperairwayseveninquietbreathing. Turbulencealsodevelopswhenconstriction,mucus,infection,solidtumors,or foreignbodiesdecreasetheradiusoftheairways.Vagal(parasympathetic) stimulation(bysmoke,dust,coldair,andirritants)leadstoairwayconstriction,whereassympatheticstimulationdilatatestheairways.
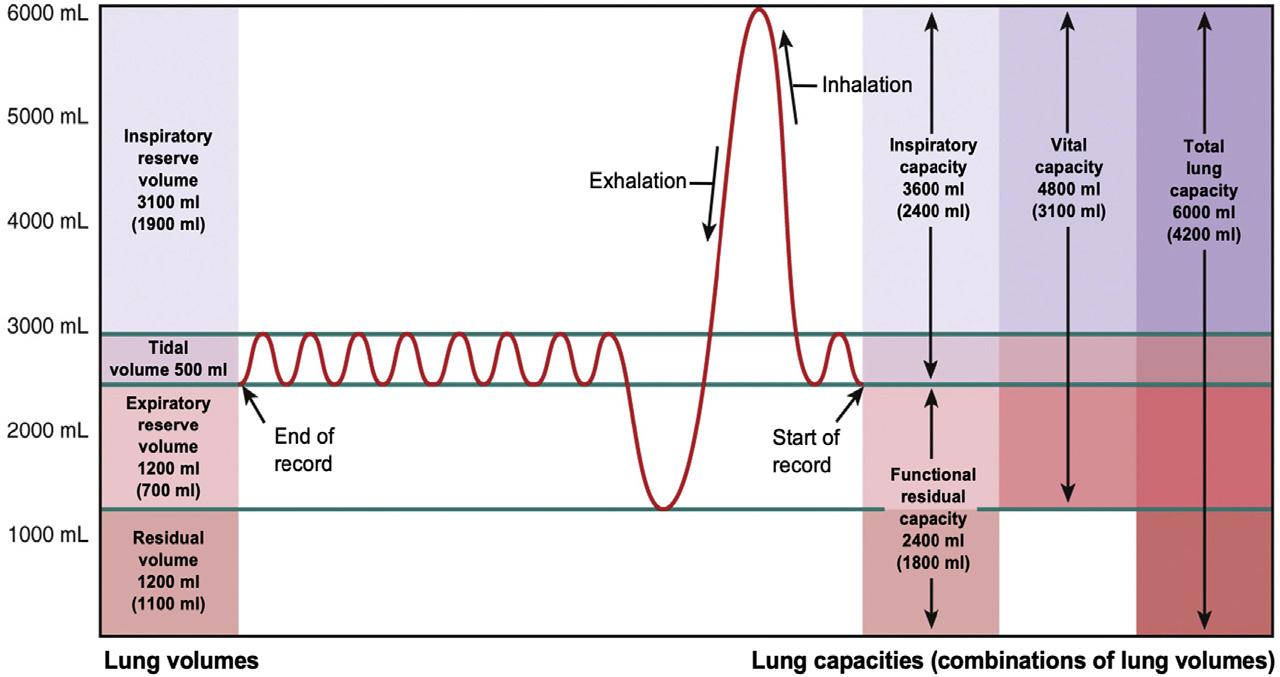
Volumesandcapacitiesrelatedtothelungfunction
Thefollowingschema(Fig.1.1)depictsthevolumesandcapacitiesthatare relatedwiththebreathingpatterninhumans.ThetermCapacityreferstoa sumoftwoormorevolumes.Ineachnormalrestingrespiratorymovement,a volumeequalto350 500mLofairenterstherespiratorytract.Thisiscalled tidalvolume(VT).Thevolumethatremainsfromtheendofatidalinspiration tothemaximuminspiratoryeffortistheinspiratoryreservevolume(IRV). Similarly,theexpiratoryreservevolume(ERV)istheremainingvolumethat canbeexpiredaftertheendofatidalbreath.Theresidualvolume(RV)isthe volumethatremainsinthelungsafteramaximumexpiratoryeffort.Thesum ofalltheabovevolumesisthetotallungcapacity(TLC),whereasthesumof IRCandVTistheinspiratorycapacityandthesumofIRV,VT,andERVisthe vitalcapacity.Finally,thesumofERVandRVisthefunctionalresidualcapacity(FRC)whichisaveryimportantmeasure,sinceitconstitutesthebalancepointofthelungexpansion(i.e.,thepointwheretheforcesthattendto expandandclosethelungsareequalandatabalanceundernormal conditions).
Twoadditionalmetricsareproducedduringthespirometrytest:forced expiratoryvolumeinonesecond(FEV1)isthe1-svolumeexhaledwith forcefulpressurefrommaximalinspiration.FEV1 isoftenexpressedinrelationtothetotalforcedexpiratoryvolume(FEV).Thesemetricsareessential forthestudyofobstructiveandrestrictivelungpathologies.
Ventilation
Themostcrucialcomponentofrespirationistheactofbreathing,during whichthelungsarefilledwithairthroughinhalingandCO2 isremoved
FIGURE1.1 Diagramshowingthevolumesandcapacitiesofthelungs(thevolumesthatare shownintheleftcolumnarerepresentativeofanaverageadultmale).
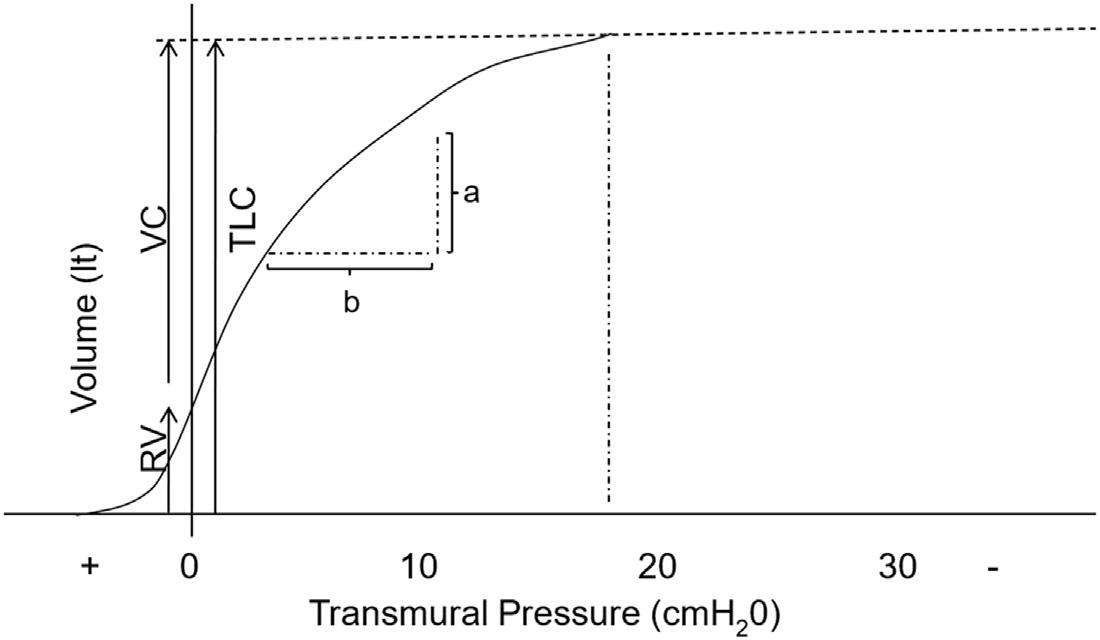
throughexhalation[1].Thisprocessofmovingairintoandoutofthelungsis knownasventilation[4].Whileitmayseemasimplisticprocess,theabilityof airtoflowintoandoutofthealveoliisdependentonanumberoffactors includingintegrityandcomplianceofthelungtissueandresistancetoairflow withintheairways[2].Compliance(C)isameasureofhowmuchthelungcan increaseitsvolume(DV)whenunderanincreasingpressure(DP)appliedon it,soC ¼ DV/DP.Theinversepropertyiscalledelastance(E),thusE ¼ 1/C. Thelungsnormallyhavethetendencytoreturntoavolumeslightly smallerthantheRVduetotheelasticforcesassociatedwiththeirstructure.In ordertomaintainavolumelargerthanthis,anexpansionpressuremustbe appliedtothelungs.Thispressureisconsideredtoequalthealveolarpressure (Palv)minusthepleuralpressure(Ppl)(thepressureinsidethepleuralcavity coveringthelungs).Byplottingthetransmuralpressureoverthelungvolume, thestaticpressure volumecurveisderived,asin Fig.1.2.Thesigmoidform ofthecurvereflectsthefactthattherequiredtransmuralpressurefortheinflow ofaspecificvolumeofairintothelungsissignificantlylowerwhenthe inspiratoryeffortstartsfromthelevelofthefunctionalrespiratorycapacity comparedtowhentheeffortbeginsafterprevioushyperinflation(i.e.,closerto theTLC).
NormallungsareverydistensibleatFRC,butstiffenprogressivelytoward TLC.Thefallingcomplianceiscausedbyanincreaseintheair liquidsurface tensionbecausetheliquidcontainstension-reducingmolecules(asubstance calledsurfactant)thatarespreadfurtherandfurtherapart.Therebythe complianceofthelungisreduced.Thecontributionofsurfacetensiontothe overalllungelasticityismorethan50%.Compliancealsodecreaseswithage; therearecorrespondingdecreasesinlungvolumes.Thepresenceofsurfactant hasmultiplebeneficiaryeffectsonthelungparenchyma:Itreducesthesurface
FIGURE1.2 Thestaticpressure volumecurveoftherespiratorysystem.Lungcompliancecan becalculatedbydividingthedifferenceinvolume(DV ¼ a)withdifferenceinpressure(DP ¼ b).
Respiration:physiology,pathology,andtreatment Chapter|1 7
tensionofalveoli,stabilizesthewallsofsmalleralveoli,reducesthework necessarytodistendthealveoli,andfinally,preventsthefillingofthealveolar spacewithextracellularfluid,therebypreventingpulmonaryedema.Absence ofsurfactantcaninducesevererespiratorydistresssyndrome.
ThedrivingpressureforairtomoveisPalv PB,wherePB ¼ Barometric Pressure.Thedrivingpressureandairwayresistancesarestudiedwhenair movesintoandoutofthelungsandtheconditionis,therefore,calleddynamic. Thedrivingpressureforinspirationisanegativealveolarpressure(Palv) relativetobarometricpressure.
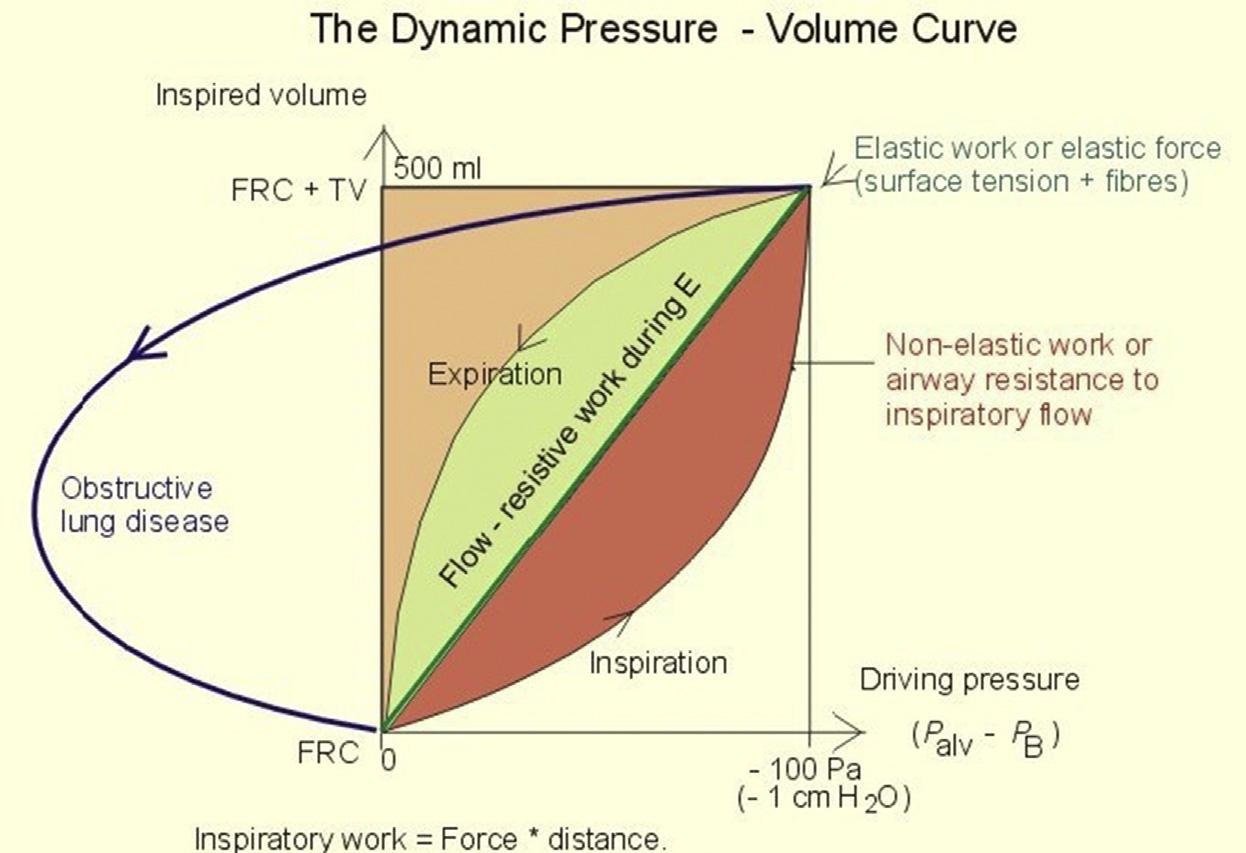
Respiratoryvolumeisrecordedgraphically.TheVTisplottedagainstthe drivingpressure,whichisequaltothedynamicalveolarpressure(Fig.1.3).
Integratingpressurewithrespecttovolumegivesthegreenareacorrespondingtotheelasticworkofoneinspiration.Thisistheworkneededto overcometheelasticresistanceagainstinspiration.Theredareatotherightof thediagonalistheextraworkofinspirationcalledtheflow-resistivework oralternativelynonelasticwork(Fig.1.3).Duringexpiration,theflowresistiveworkisequaltothegreenarea.Theinspiratoryandexpiratory curveformsaso-calledhysteresisloop.Thelackofcoincidenceofthecurves forinspirationandexpirationisknownaselastichysteresis(lag).Withdeeper andmorerapidbreathingthehysteresisloopbecomeslarger,andthe nonelasticworkrelativelyhigher.
FIGURE1.3 Tidalvolume(TV)andthedynamictransmuralpressure(Palv Pbarometric)ina healthypersonduringonerespiratorycycle:Theexpiratorycurvefromapatientwithobstructive lungdiseaseisshowntotheleft.
Theairflowintotherespiratorysystemdependsonthedriving pressure(DP)andtheairwaysresistance(RAW)tothisflow,therefore: Flow ¼ V* ¼ DP/R ¼ (PALV PATM)/RAW.Theairwaysresistance(RAW)is dependentontheviscosityoftheinhaledair,thelengthoftheairways,and theirdiameter(itisproportionaltothelengthandinverselyproportionaltothe fourthpoweroftheradiusoftheairways).Thediameteroftheairways dependsonthepositionofthelatterinthebronchialtree,thelungvolume,the constrictionofsmoothmusclesaroundthebronchi,presenceofmucous,and thetransmuralpressure.
Regardingthemechanicalworkrequiredtoincreasethevolumeofthe lungsabovethelevelofFRC,itcanbedividedintotheelasticandthefriction workcomponents.Theformerreferstotheworkrequiredtodistendtheelastic tissuesofthelungandexpandthethoraciccavity.Itisstoredintheelastic bandsofthelungstoallowforapassiveexpiratorymovement.Thelatter referstotheworkrequiredtoovercometheresistanceoftheairways.Those workcomponentsareaffectedbythelungvolumeatanygivenpointoftime, assmallerlungvolumesmeanincreasedfrictionduetohighresistance, whereaslargervolumesleadtoincreasedelasticworknecessarytofurther distendthethoraciccavity.TheFRCrepresentsthevolumeinwhichtheelastic recoilforcesofthelungsareinbalancewiththeanalogousforcesofthe thoracicwall(pointofminimumworkload).Thepressurethatmustbeapplied bytheinspiratorymusclesplusthepressureappliedatthelevelofairways (orthelevelofpressureofaventilatorincasesofmechanicalventilation) equalstheVTmultipliedbythelungelastanceplustheresistanceofthe airwaysmultipliedbytheflowofairintothelungs.Therefore,thefollowing equationiscreated:
Pmus þ Pvent ðPaw Þ¼ðVolume ElastanceÞþðResistance FlowÞ
Sincetheelastanceisreciprocaltothelungcompliance,theaboveequation canbetransformedtothefollowing:
Pmus þ Pvent ðPaw Þ¼ðVolume = ComplianceÞþðResistance FlowÞ
Thisequationiscalledthemotionequationoftherespiratorysystemandis suitableforexplainingthesettingsandparametersofmechanicalventilation (invasiveornoninvasive).
Differentlungpathologiescausesignificantalterationsintheelasticor frictionforcesoftherespiratorysystemandhaveaneffectonFRC. Obstructivelungdiseases(likechronicobstructivepulmonarydisease (COPD))causeconstrictionoftheairwaysresultinginincreasedworkto overcomefrictionandalsoincreasedvolumefortheminimumworkpoint (FRC).Conversely,restrictivelungdiseaseslowerlungcompliance,andlead toincreasedmuscularworkforthelungexpansionandreducedFRC.
Undernormalconditions,theenergyexpenditureforrespirationisminimal:onlyanoxygenconsumptionoflessthan1mL/minisrequiredforevery L/minoflungventilation,constituting1% 2%ofthetotalO2 consumption. Also,duringtidalbreathingairisnotevenlydistributedinsidethelungs,since thereisaverticalvariationinpleuralpressureduetoanatomicalandgravitationalreasons.Pleuralpressureishigherintheapicalandlowerinthebasal partsofthelungs.Thus,apicalalveolicontainlargervolumesofair.Onthe otherhand,thealveoliinthebasalpartslieatthelowerpartofthestatic pressure volumecurveandhavegreaterdistensibilitywhiletheyarealso underahighertensionduringinspirationbecauseoftheirproximitytothe diaphragm,themaininspiratorymuscle.
Respiratorymovements
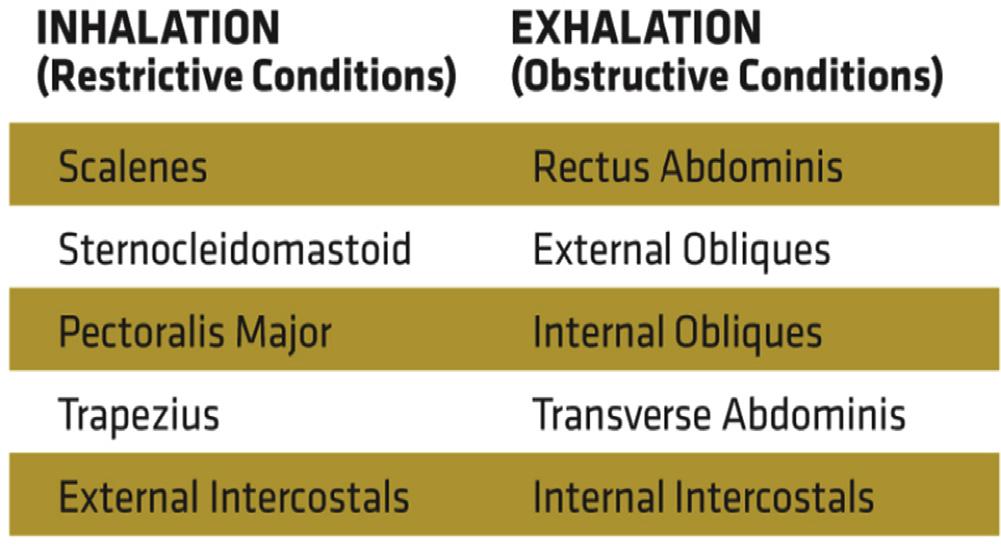
Approximately12 15timesperminuteinanadult,thediaphragmand thoracicmusclesreceiveimpulsesfromthebrainsignalingthemtocontract. Thiscontractionmovesthediaphragmdownwardandtheribcageupandout, whichincreasesthevolumeofthethoraciccavityandcreatesanegative pressurewithinthelungs.Thiscausesairfromthehigher-pressureenvironmentoutsidethebodytoflowintothelower-pressureenvironmentinthe lungs.Thisistheactivephaseofventilation,knownasinhalation[3].Air continuesflowingthroughtheairwayopeningsandintothelungswhile equalizationofpressureoccurs[5].Afterfullexpansionofthelungs,stretch receptorssignalthebrainstemandinhalationceases.Thepassivephaseof ventilation,knownasexhalation,subsequentlytakesplace.Thediaphragmand thoracicmusclesrelaxandthelungsrecoil,decreasingthevolumeand increasingthepressureinthethoraciccavity.Theairinsidethelungsflows backouttothelower-pressureatmosphereoutsidethebody[3].Sinceexhalationisapassiveprocess,ittypicallytakestwiceaslongastheactiveprocess ofinhalation[2].Duetotheacousticsinthethoraciccavity,however,the soundofexpirationlastslessthanthatoftheinspirationinlungauscultation undernormalconditions.Incaseswhentheexpirationmusttakeplacemore rapidly(duetoincreasedmetabolicdemandsforOxygen)orinlungpathologies(likeobstructivepulmonarydiseases)theexpiratoryphasebecomesan energeticprocess,withutilizationofvariousaccessoryexpiratorymuscles,as canbeseenin Fig.1.4.Thesameimagealsoshowstheaccessoryinspiratory muscles.
Throughthisprocessofinhalationandexhalation,theaveragehuman cycles5 10Lofairthroughthelungseachminute[2].Theamountofair takenintothelungsduringeachbreath(approximately500mLinanadult)is knownastidalvolume(VT),whilethecollectivevolumeoverthecourseofa minute(respiratoryrate VT)isknownastheminutevolume(VE).Dueto
thelackofgasexchangethatoccursintheconductingairways(fromthe mouthtotheterminalbronchioles),aportionofeachbreathisineffectivefor gasexchange.Thisanatomicaldeadspace(VD)isapproximately150mLin theaverageadultandmustbesubtractedfromtheVT inordertodeterminethe volumeofairthatreachesthealveoli(VA)andcanbeusedforgasexchange.
Aspreviouslynoted,CO2 iscreatedwithinthebody,anditistheroleof ventilationtoremovethisby-product.Itisalsoforthisreasonthatventilation isbestevaluatedthroughameasureofCO2 (partialpressureofCO2 inarterial blood-PaCO2 orpartialpressureofCO2 inend-tidalvolumeofair-PETCO2) [4].Ifbreathingstops(apnea)oriftheVE decreases(hypoventilation),CO2 willaccumulatewithinthebloodandrapidlyreachtoxiclevels(hypercapnia), resultinginrespiratoryacidosis.Conversely,ifVE increases(hyperventilation),theexcessiveeliminationofCO2 (hypocapnia)willresultinrespiratory alkalosis.Itisinthismannerthatourrespiratorysystemaffectsthebody’spH andcanalsoserveasacompensatorymechanismtooffsetmetabolic derangements(e.g.,hyperventilationcancompensateformetabolicacidosis duetovariedetiology).
Perfusion
Thesecondcomponentofrespirationisperfusion.Thisprocessinvolvesthe circulationofbloodthroughthecapillaries,whichfacilitatesnutrientexchange [6].Externalrespirationrequiresadequatedeliveryofbloodtothecapillary bedsofthelungsviathepulmonarycirculation.Intheabsenceofthisblood supply,therewillbenotransportmechanismforO2
Gasesareexchangedbetweentheatmosphereandthealveolarairand diffusebetweenthealveolarairandthebloodflowingthroughthepulmonary capillaryvessels.
Oxygenistransportedfromtheatmosphere,viathealveolarventilationand thencarriedbythepulmonarybloodflow(equaltothecardiacoutput),intothe
FIGURE1.4 Thehumanaccessoryinspiratoryandexpiratorymuscles.
Respiration:physiology,pathology,andtreatment Chapter|1 11
cellsandtheirmitochondriaformetabolicpurposes.Carbondioxide,thefinal end-productofmetabolism,migratesfromthecellstotheatmosphere.
Ahealthynormalpersonatrestventilateshislungswith5L/minoffresh air(V*A).Therespiratoryquotient(RQ)isametabolicratiobetweenthe carbondioxideoutput VCO2 andtheoxygenuptake VO2 definedforall bodycellsasawhole.OnadietdominatedbycarbohydratethemetabolicRQ forallcellsofthebodyisapproachingthevalue1.
Thenormalrestingcarbondioxideoutputis10mmolor224mL/minfrom anadultperson,andthecardiacoutputistypically5L/min.Thebloodvolume of5Lcarrieseachminabout10mmol(or224mL)ofoxygentowardthe mitochondria.Followingpassageofthecapillarysystem,thesameamountof CO2 iscarriedtowardthelungsinthevenousbloodaslongasRQis1.
Bloodpassingthepulmonarycapillariesofahealthypersonisrapidly equilibratingwiththealveolarair.Oxygenfromtheairdiffusesintotheblood andbindsreversiblywithhemoglobin.Thenormaloxygencapacityis200mL perLofblood(150ghemoglobinperLcarrying1.34mL/g).
Normally,alveolarventilation(V*A)andperfusion(Q*)arematchedand thetotalV*A/Q*ratioisbetween0.8and1.2withnormalalveolarandblood gastensions.Inthenormaluprightlung,theregionalV*A/Q*ratiois approximately0.6atthelowerandabout3attheupperlungregion.The pulmonarybloodflowdecreasesfromthelowertotheupperpartsofthelung ofarestingperson.Likewise,therelativeventilationofthelungalsodecreases linearlyfromthebasetotheapex,butataslowerrate.Thus,theregional ventilation perfusionratiovariesfromzerointhelowerregion,wherethereis onlybloodflowandnoventilationtoinfinityintheupperregion,wherethere isonlyventilationandnobloodflow.Atthelowerlungregion,regionalV* approacheszeroandatthetopofthelungregionalperfusionapproacheszero. InaPO2 PCO2 diagrameachpointonthecurverepresentspartialpressuresat whichalveolarairandbloodcanequilibrateatacertainV*A/Q*ratio.Thus, foranypracticallyobtainablepoint,asinglevalueexistsforbloodgasconcentrations.LungregionsatthebasewithlowV*A/Q*havelowPAO2 and highPACO2,relativetonormalmeanvalues.Upperlungregionswithhigh V*A/Q*haverelativelyhighPAO2 andlowPACO2
Normally,upto5%ofthevenousreturnpassesdirectlyintothesystemic arterialcirculation.Thisshunt-bloodincludesnutrientbloodflowcomingfrom theupperairwaysandcollectedbythebronchialveins.Thecoronaryvenous bloodthatdrainsdirectlyintotheleftventriclethroughtheThebesianveinsis alsoshunt-blood.
Pulmonaryvascularresistance(PVR)isminimalcomparedtothatof thesystemiccirculation.Thepulmonaryvascularsystemisbasicallyalowpressure,low-resistance,highlycompliantvesselsystemwithabloodflow sensitivetogravityandtoPAO2
Thesystemismeanttoaccommodatetheentirecardiacoutputandnotto meetspecialmetabolicdemandsasinthecaseofthesystemiccirculation.The pressureintherightventricleis3.3kPasystolicand0.133kPadiastolicina healthy,supinepersonatrest.Thepressureinthepulmonaryarteryisabout 3.3kPasystolicand1kPadiastolic,withameanof1.7kPa.Thebloodflowof thepulmonarycapillariespulsatesanditsmeanpressureisbelow1kPa.The pressureintheleftatriumis0.7kPa.Thisvalueimpliesapressuredropacross thepulmonarycirculationof(1.7 0.7) ¼ 1kPa.Thisdrivingpressureisless than1/10ofthesystemicdrivingpressure.
Thewallsofthepulmonaryvesselsarethin,hencetheirpressuremustfall ateachinspiration,becausetheintrapulmonarypressurefalls.Changeof posturefromsupinetoerectpositionreducesthepressuretowardzerointhe apicalvessels,whereasitincreasesthepressureinthebasalvesselsdueto gravity.Whenthedrivingpressureintheapicalbloodvesselsapproacheszero, thebloodflowwillalsoapproachzero.Apartfromitsimplicationforgas exchange,thisphenomenonlimitsthesupplyofnutrients.Lungdisorders oftenoccurintheapicalregions.
ThePVRremainslowinhealthypersons,evenwhencardiacoutput increasesto30L/min,becauseofdistensibilityandrecruitmentofpulmonary vessels.Stretchreceptors,foundintheleftatriumandinthewallsoftheinlet veins,arebelievedtobestimulatedbydistension.Suchadistensionblocks liberationofvasopressin(antidiuretichormone)fromtheposteriorpituitary andreleasesatrialnatriureticfactorfromtheatrialtissue.Hereby,theurine volumeincreasesandtheextracellularvolumedecreases.
ChangesinPVRareachievedmainlybypassivefactors,butalsobyactive modification.Passivefactors:thelargerarteriesandveinsarelocatedoutside thealveoli(extra-alveolar);theyaretetheredtotheelasticlungparenchyma andareexposedtothepleuralpressure.Thepulmonarycapillariesliebetween thealveoliandareexposedtothealveolarpressure.
Alveolarcapillaryvolume:theintra-alveolarvesselsarewideopenatlow alveolarvolumes,sothattheirPVRmustbeminimal.Withincreasingalveolar distensionthesevesselsarecompressed.Thisincreasestheintra-alveolarPVR. However,atlowalveolar(lung)volumes,theextra-alveolarvesselsaresmall becauseofthesmalltransmuralvascularpressuregradient,andtheirPVRis high.
Withincreasinglungdistension,theintrathoracicpressurebecomesmore subatmospheric.Thiselevatesthetransmuralvasculargradientandiscoupled withtheradialtractiononthesevesselsbythesurroundinglungparenchymaas itexpands.Thus,theextra-alveolarPVRdecreases.Thegreatestcross-sectional areaexistsinthemanyintra-alveolarvessels,henceincreasingPVRinthese vesselsleadstodecreasedextra-alveolarPVR.Thus,totalpulmonaryvascular resistanceisincreasedathigheralveolarvolumeswhenintra-alveolarPVR ishigh.PVRisminimalatFRC,wherethereisairenoughtoopenthe extra-alveolarvesselswithminimalclosureoftheintra-alveolarvessels.
Respiration:physiology,pathology,andtreatment Chapter|1 13
Pulmonaryarterypressure:Ahealthypersonatrest(atthelevelofFRC) hasapproximatelyhalfofthepulmonarycapillariesopen,butwithincreasing arterialpressure,thepreviouslyclosedcapillariesopen(recruitment).Asthe arterialpressurecontinuestorise,thecapillariesbecomedistended.Thenet effectisariseinthetotalcross-sectionalareaofthelungcapillaries,leadingto decreasedPVR.
AdecreaseinPAO2 inanoccludedregionofthelungproduceshypoxic vasoconstrictionofthevesselsinthatregion.ThereducedPAO2 causes constrictionoftheprecapillarymusculararteriesleadingtothehypoxicregion. Thishypoxiceffectisnotnervemediated.Thereactionshiftsbloodawayfrom poorlyventilatedalveolitobetter-ventilatedones.Nitricoxide(NO)seemsto dilatatethevesselsofthewell-ventilatedsegmentsofthelung.Perfusionis herebymatchedwithventilation.
Diffusion
Diffusionisanotherimportantmethodoftransportwithinthebodyandisthe thirdcomponentofrespiration.Diffusioninvolvesthemovementofasubstanceinasolution(liquidorair)fromhigherconcentrationareastolower concentrationareas[7].Inthecaseofrespiration,diffusioninvolvesthedistributionofO2 fromtheatmospherethroughtheepithelialmembraneofthe alveoli,thebasicmembrane,andthepulmonarycapillary(endothelial)walls andintothebloodstream.Atthesametime,CO2 diffusesfromthebloodstreamintothealveolifollowingtheoppositeroute.Thisprocessofdiffusion isdependentonthecharacteristicsofeachindividualgas,therateofperfusion, andtheintegrityofthealveolar capillarymembrane[4].
Thesixzonesofthealveolar capillarybarrierare:(1)afluidlayercontainingsurfactant;(2)thealveolarepithelium;(3)afluid-filledinterstitial space;(4)thecapillaryendotheliumwithbasementmembrane;(5)theblood plasma;and(6)theerythrocytemembrane.Thesixzonesformanalmostideal gasexchangerforoxygenandcarbondioxidediffusion.
Fick’slawofdiffusionstatesthatthefluxofgastransferredacrossthe alveolar capillarybarrierisrelatedtothesolubilityofthegas,thediffusion area(A),thelengthofthediffusionpathwayfromthealveolitotheblood(L), andthedrivingpressure(P1 P2).
TheEarth’satmospherecontainsapproximately21%O2.Atsealevel, undernormalconditions,barometric(i.e.,atmospheric)pressureis 760mmHg.AccordingtoDalton’slaw,thispressureiscomprisedofthe partialpressuresoftheindividualgasesthatmakeupouratmosphere:primarilynitrogen(N2)andO2.Inthissituation,thepartialpressureofO2 is 159mmHg(21%of760mmHg).BythetimeO2 diffusesintothehuman circulation,itspartialpressure(PaO2)isreducedto80 100mmHg[4].While thepercentageofO2 intheatmosphereremainsconstant,theprocessof diffusioncanbeenhancedthroughacombinationofsupplementalO2 and
alteringtheairwaypressure(e.g.,continuouspositiveairwaypressureor high-flownasalcannuladevices)orbyalteringacombinationofbarometric pressureandO2 concentration(e.g.,hyperbaricchamber).
Neuralcontrolofrespiration
Thegasexchangetakesplaceinthelungs.Nevertheless,thecontrolofthe respiratorysystemisexecutedbythecentralnervoussystem(CNS)[3].While wedohavesomevoluntarycontrolofbreathing,itismainlyregulatedautomaticallyandfunctionsirrespectiveofourwill.Breathingcan,however,be suppressedattheneurologicallevelduetonarcoticorsedativeoverdose,as wellasbrainsteminjury[3].
ThelocioftheCNSthatcontrolrespirationarelocatedwithinthebrain stem,specificallywithintheponsandthemedulla.Thesecomponentsare responsibleforthenervousimpulses,whicharetransmittedviathephrenic andothermotornervestothediaphragmandintercostalmuscles,controlling ourbasicbreathingrhythm.Alsolocatedinthebrainstemarethecentral chemoreceptors.Thesespecializedcellssignalthebodytoadjustventilation basedindirectlyonthepartialpressureofarterialCO2 (PaCO2)level,thus constitutingtheprimaryrespiratorydrive.Peripheralchemoreceptors,which arelocatedoutsideofthebrainsteminthecarotidandaorticarteries,serveas thebody’sback-uprespiratorydrivebyrespondingtolowlevelsofO2.This secondarymechanismisoftenreferredtoinCOPDpatientsasa“hypoxic drive”sinceittakesoverastheprimaryrespiratorystimulationafterthe centralchemoreceptorsgrownumbtochronicallyelevatedPaCO2.Agraphic representationoftherespiratorycentersinthebrainstemcanbefoundin Fig.1.5.
Pulmonarydefensemechanisms
Duringnormalbreathingmostoftheparticlesofmorethan10mmin diameter suchaspollen aredepositedandremovedinthenoseandnasopharynx.Particlesbelow1mmaredepositedinthealveoli.Particlesbetween 1and10mmaredepositedinthebronchidependingontheirdiameter. Althoughsneezingandcoughingwithexpectorationcaneliminatemany inhaledparticles,themucociliaryescalatorassistedbybronchus-associated lymphoidtissue(BALT)andalveolarmacrophagesperformthemainclearanceoftheairways.Theairwaysareprotectedbyhumidificationallthewayto thealveoliwithamucouslayer,whichpreventsdehydrationoftheepithelium andsurroundstheepithelialcilia.Thisairwaymucousconsistsofpolysaccharidesfromgobletcellsandfrommucousglandsinthebronchialwall andformsagelatinousblanketontopoftheliquidlayer.Theciliacontinuouslymovethegelatinousblanketwithinhaledparticlesupwardtowardthe pharynx,wheretheyareswallowed[7].

FIGURE1.5 Therespiratorycentersresponsibleforthecontrolofbreathinginthebrainstem. Ontherightsideofthepicturearedepictedtheconsequencesoftransectionsinthedesignated areasonthebreathingpattern. Respiration:physiology,pathology,andtreatment Chapter|1 15
Clearanceoftherespiratorybronchiolesmaytakedays,whereasclearance ofthemainbronchiistypicallyaccomplishedwithinanhour.Smoking reducesmucociliarytransport,andindirectlyimpairsgasexchange.Italso reducessurfactantproductionandthusincreasestheworkofbreathing.
Thelungsecretionscontainbactericidallysozymeandlactoferrinfrom granulocytes.Thea1-antitrypsinnormallyneutralizeschymotrypsin,trypsin, elastase,andproteasessecretedbygranulocytesduringinflammation,andthus preventsdestructionoflungtissue.
BALTinthewallsofthemainbronchiispartofthemononuclear phagocytoticsystem.Thesetissueaggregatescontainmacrophagesoriginating frommonocytesandlymphocytes.FollowingsensitizationofB-lymphocytes tospecificantigens,thecellsproducespecificantibodiesorimmunoglobulins(types:IgA,IgG,andIgE)inresponsetonewcontactwiththeantigen. IgAinhibitstheattachmentofpoliovirus,bacteria,andtoxinsintherespiratorytract.IgEisrelatedtothepathogenesisofallergicdisorders.
Lungsadditionallyhaveendocrinefunctions[8].Alveolarmacrophagesare amebiccellsthatswallowparticlesandbacteriainthealveoli.Whilethey executemicrobesintheirphagolysosomes,thecellsmigratetothemucociliary escalator,ortheyareremovedbythebloodorbythelymphaticsystem. Smokingimpairsthenormalmacrophageactivity.
Theinactivepolypeptide,angiotensinI,isconvertedintothepotent vasoconstrictor,angiotensinII,bytheangiotensin-convertingenzyme,located onthepulmonaryendothelialcells.Angiotensinisimportantfortheregulation ofthearterialbloodpressure alsoduringshock.
Adrenergicsympatheticactivity(andsympathomimeticdrugs)relaxes bronchialsmoothmuscleviaadrenergicb2receptors,whereasparasympatheticcholinergicactivity(andparasympathomimetics)constricts bronchialsmoothmusclesviamuscarinicreceptors.
Smoke,dust,andotherirritants(perhapsalsoadenosine,histamine,and substanceP)constricttheairwaysmoothmusclesviaareflextriggeredby therapidlyadaptingirritantreceptors.DecreasedPACO2,thromboxane,and leukotrienesalsoactasbronchoconstrictors.
Vasoactiveintestinalpeptidecandilatateairwaysandreduceairflow resistance.SubstancesthatdilatateairwaysincludeincreasedPACO2,adrenergicalpha-blockers,catecholamines,andatropine.
PartB:pathologyandtreatmentoflungdiseases
Lungdiseasesaresomeofthemostcommonmedicalconditionsintheworld [9].Theyconstituteawidespectrumofpathologicalconditions,whichcanbe dividedintodiscretecategories,asdescribedinthefollowingsections.
Lungdiseasesaffectingtheairways
Asthma
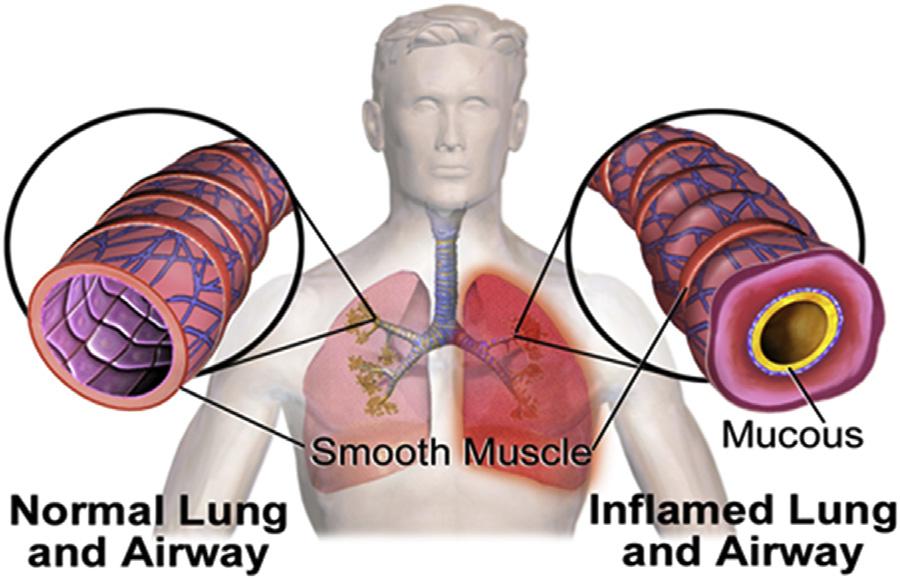
Asthmaisalungdiseaseofthebronchialairways.Inflammationand constrictionoftheairways(asdepictedgraphicallyin Fig.1.6)resultin symptoms.Patientssufferfromwheezing,shortnessofbreath,chesttightness,
Respiration:physiology,pathology,andtreatment Chapter|1 17
andcoughing.Ingeneral,symptomsareintermittentbutwhensevere,theycan becontinuous.Allergies,infections,pollution,exercise,andcoldtemperatures cantriggerasthmasymptoms.
Diagnosis
Becauseasthmaisaclinicalsyndrome,thereisnogoldstandardforits diagnosis.Diagnosisisbasedonphysicalexam,symptoms,andmedical history.Moretestsareusedtoexaminethepulmonaryfunction:
l Spirometry.Thissimplebreathingtestmeasureshowmuchairisblownout andhowfast.
l Peakflow.Thistestmeasureshowwelltheairispushedoutofthelungs.It islessexactthanspirometry,butitcanbeagoodwaytotestthelung functionathome.Apeakflowmeterprovidesinformationabouttreatment effectiveness,factorsthatworsensymptoms,andwhenapatientneeds emergencycare.
l Methacholinechallenge. Duringthistest,thepatientinhalesachemical calledmethacholinebeforeandafterspirometrytoseeifitmakesthe airwaysnarrow.Iftheresultsfallatleast20%,thediagnosisisasthma. Thepatientreceivesmedicineattheendofthetesttoreversetheeffectsof themethacholine.
l Exhalednitricoxidetest. Thepatientbreathesintoatubeconnectedtoa machinethatmeasurestheamountofnitricoxideinbreath.Patient’sbody makesthisgasnormally,butlevelscouldbehighiftheairwaysare inflamed.
Othertestsinclude:
l ChestX-ray. Itisnotanasthmatest,butitcanshowotherdiseases.
l Computedtomography (CT).Ascanofthelungsandsinusescanidentify physicalproblemsordiseases(likeaninfection)thatmaycausebreathing problemsormakethemworse.
l Allergytests.Thesecanbebloodorskintests.Theseshowallergic reactionstopets,dust,mold,andpollen.
l Sputumeosinophils.Thistestlooksforhighlevelsofwhitebloodcells (eosinophils)inthemixofsalivaandmucus(sputum)thatcomesoutwith cough.
Treatment[10 14]
l Inhaledcorticosteroids.Thesemedicationstreatasthmainthelongterm. Theyaretakeneverydaytokeeptheasthmaundercontrol.
l Leukotrienemodifiers. Anotherlong-termasthmatreatment.Thesemedicationsblockleukotrienesthattriggeranasthmaattack.Patienttakesthem asapillonceaday.
l Long-actingbeta-agonists. Thesemedicationsrelaxthemusclebandsthat surroundtheairways(bronchodilators).
l Combinationinhaler. Thisdevicegivesaninhaledcorticosteroidanda long-actingbeta-agonisttogethertoeasetheasthmasymptoms.
l Theophylline. Itopenstheairwaysandeasestightness.Itisalong-term medicationbymouth,eitherbyitselforwithaninhaledcorticosteroid.
l Short-actingbeta-agonists. Theseareknownasrescuemedicinesorrescue inhalers.Theyloosenthebandsofmusclearoundtheairwaysandease symptoms.
l Anticholinergics. Thesebronchodilatorspreventthemusclebandsaround theairwaysfromtightening.
l Oralandintravenouscorticosteroids. Thesearetakenalongwitharescue inhalerduringanasthmaattack.Theyeaseswellingandinflammationin airways.Oralsteroidsareusedforashorttime,between5daysand 2weeks.Also,thepatientislikelytogetsteroidsinjecteddirectlyintoa veinforasevereasthmaattack.
l Biologics. Ifthereisasevereasthmathatdoesnotrespondtocontrol medications,biologicfactors(omalizumab,benralizumab,mepolizumab, andreslizumab)canbeselectedtostoptheimmunecellsfromcausing inflammation.
Chronicobstructivepulmonarydisease(COPD)
Itisatermthatcoverstwotypesofchronic(long-term)diseaseswherethe airways(breathingtubes)inthelungsbecomeswollenandpartlyblocked. COPDgetsworseovertime.Itcannotbecured,butitcanbetreatedand managed.
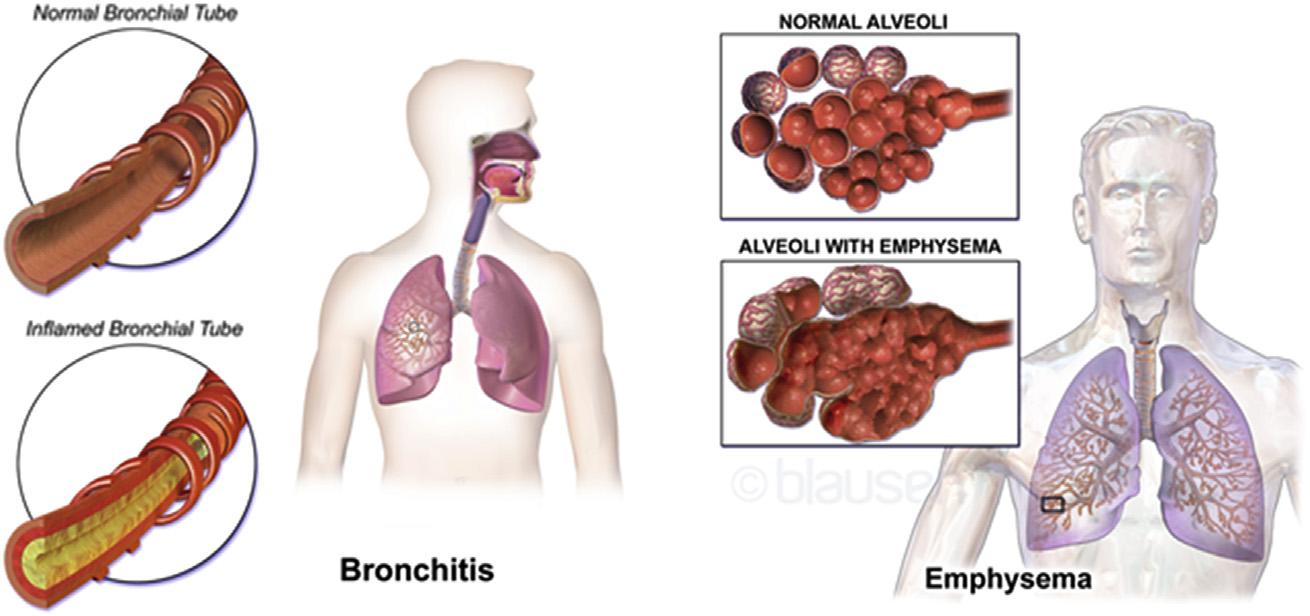
COPDconsistsoftwomajorbreathingdiseases(Fig.1.7):
l emphysema
l chronicbronchitis
Emphysemadamagesthetinyalveoli(airsacs)atthetipsofthelungs. Normallytheseairsacsstretchlikeballoonsduringbreathinginandout. Emphysemamakestheseairsacsstiff.Becausetheycannotstretch,airgets trappedinsidethem.Asaresult,theinhalationbecomesdifficult.
Chronicbronchitismakestheairwaysred,swollen,andirritated.Glandsin theairwaysmakeextramucus(phlegm),whichblockssomeairfrompassing through.Thiscausescough,largeproductionofmucus,andshortnessof breath.ManypeoplewithCOPDhavebothdiseases.
Diagnosis[15,16]
AdiagnosisofCOPDisbasedonsignsandsymptoms,historyofexposureto lungirritants(suchassmoking),andfamilyhistory. 18 PART|I
l Lung (pulmonary) functiontests. Thesetests[12]measuretheamountof airthepatientcaninhaleandexhale,andwhetherthelungsdeliverenough oxygentotheblood.Duringthemostcommontest,calledspirometry,the patientblowsintoalargetubeconnectedtoasmallmachinetomeasure howmuchairthelungscanholdandhowfasthe/shecanblowtheairout ofhis/herlungs.Othertestsincludemeasurementoflungvolumesand diffusingcapacity,6-minwalktest(toseehowfarapersoncanwalkin 6minandhowmanytimeshe/sheneedstostoptocatchhis/herbreath), andpulseoximetry.
l ChestX-ray. AchestX-raycanshowemphysema,oneofthemaincauses ofCOPD.AnX-raycanalsoruleoutotherlungproblemsorheartfailure.
l CTscan. ACTscanoflungscanhelpdetectemphysemaandhelp determineifthepatientmightbenefitfromsurgeryforCOPD.CTscans canalsobeusedtoscreenforlungcancer.
l Arterialbloodgasanalysis. Thisbloodtestmeasureshowwellthelungs arebringingoxygenintobloodandremovingcarbondioxide.
l Laboratorytests. LabtestsarenotusedtodiagnoseCOPD,buttheymay beusedtodeterminethecauseofsymptomsorruleoutotherconditions. Forexample,labtestsmaybeusedtodetermineifthepatienthasthe geneticdisorderalpha-1-antitrypsindeficiency,whichmaybethecauseof COPDinsomepeople.Thistestmaybedoneifapersonhasafamily historyofCOPDanddevelopsCOPDatayoungage.
Therapy
l Quittingsmoking
l Inhalers:
FIGURE1.7 ThetwotypesofCOPD.